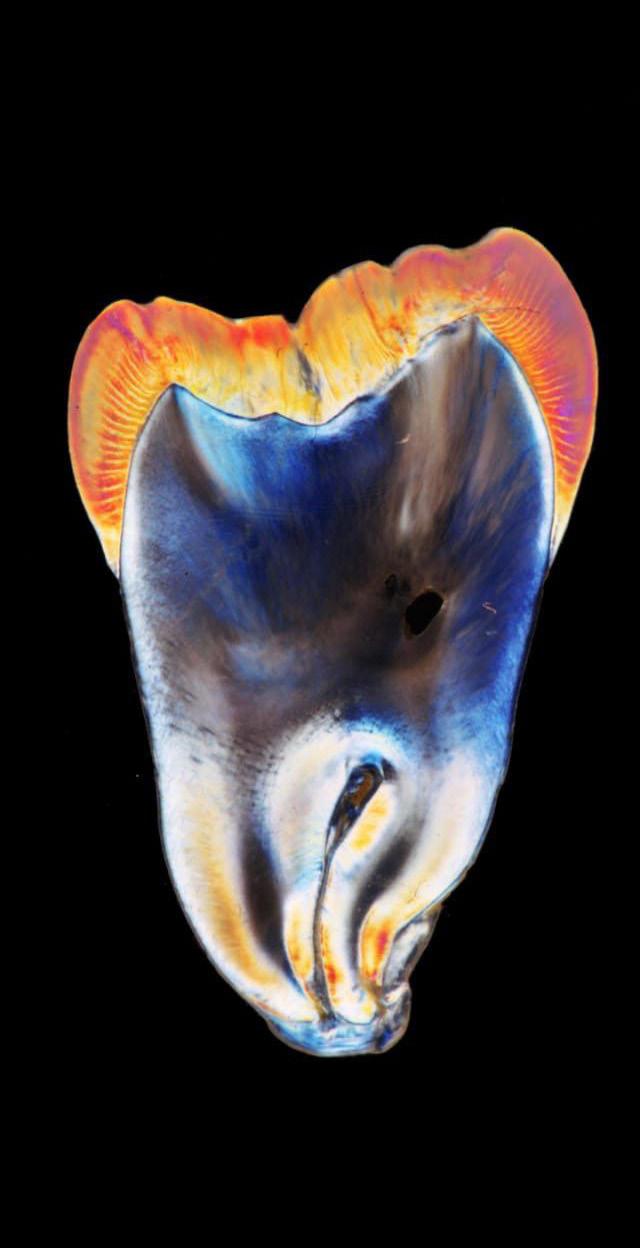

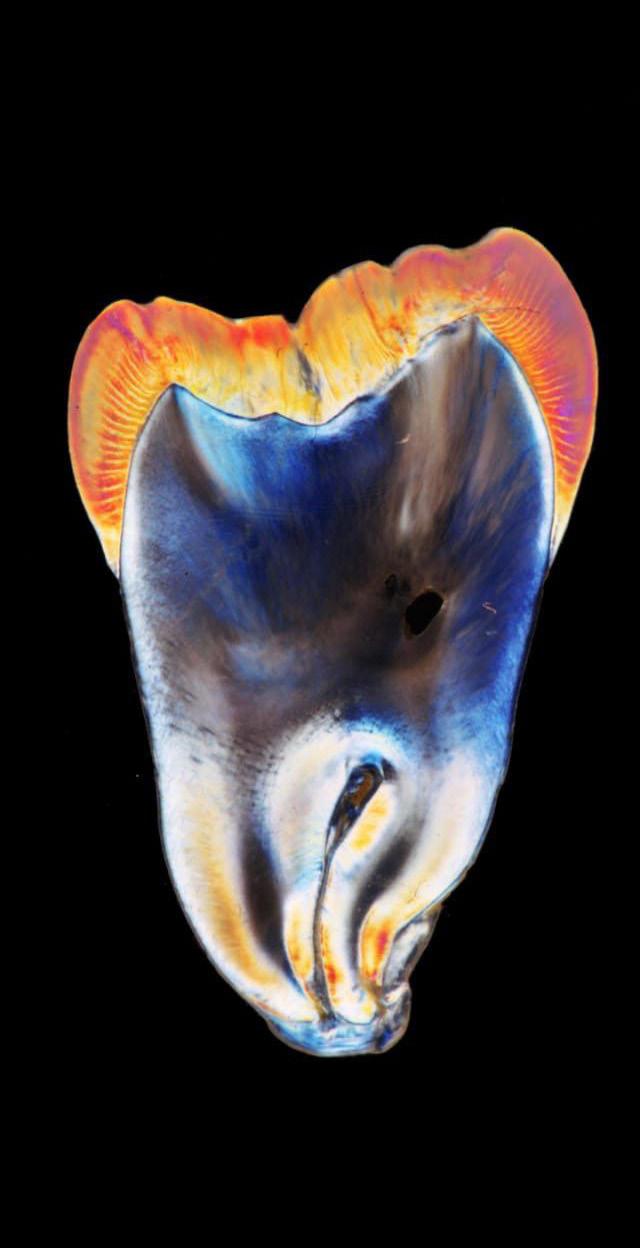

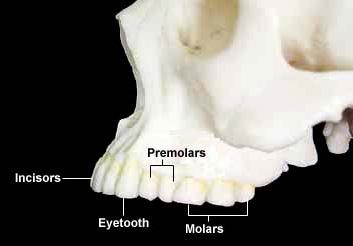
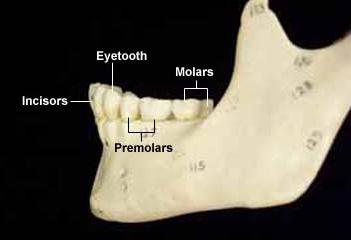
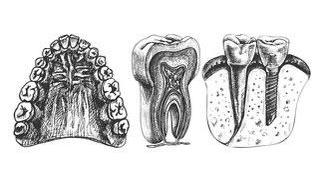
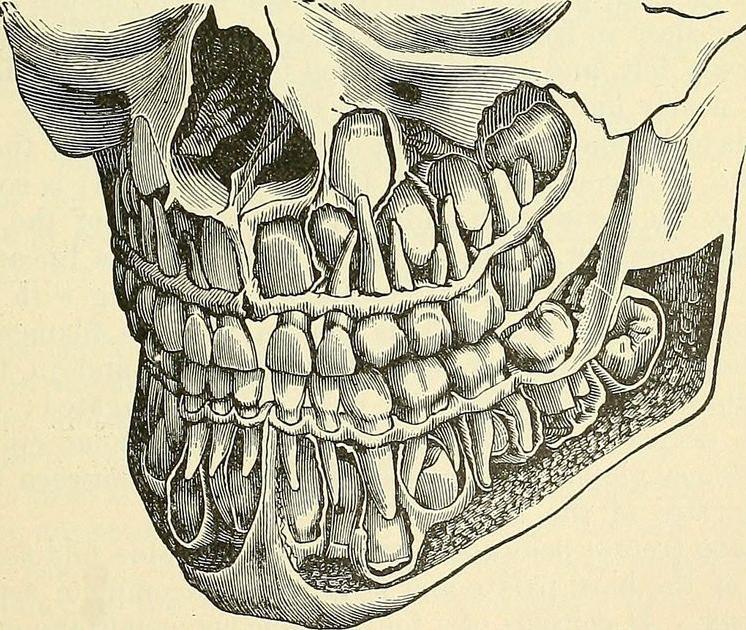
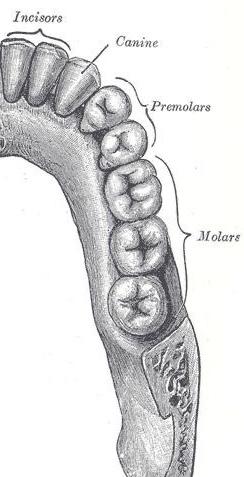
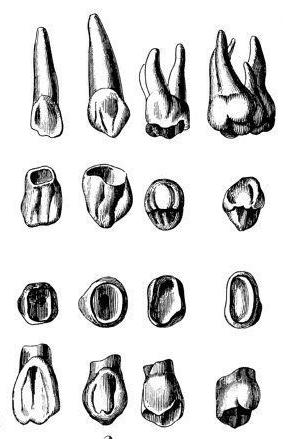
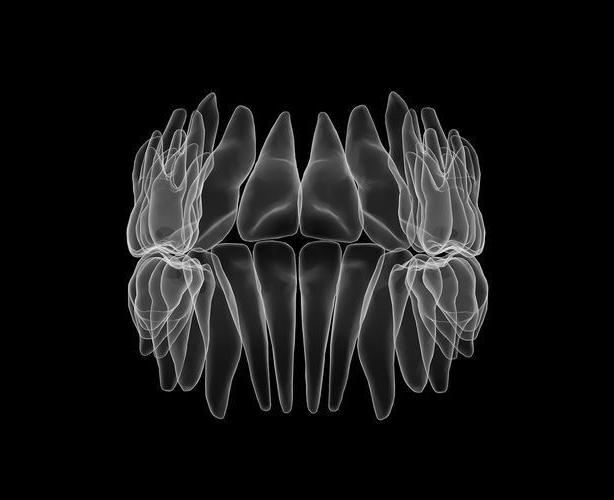
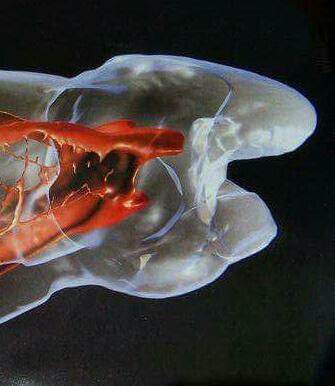
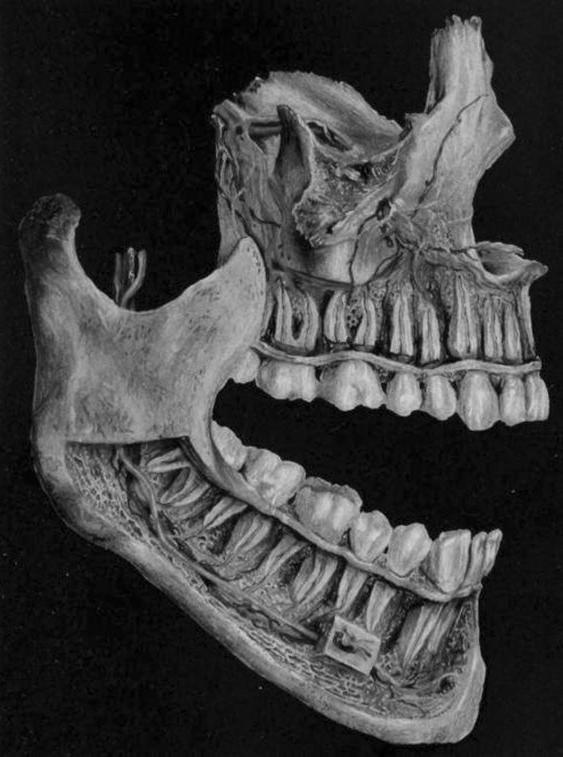
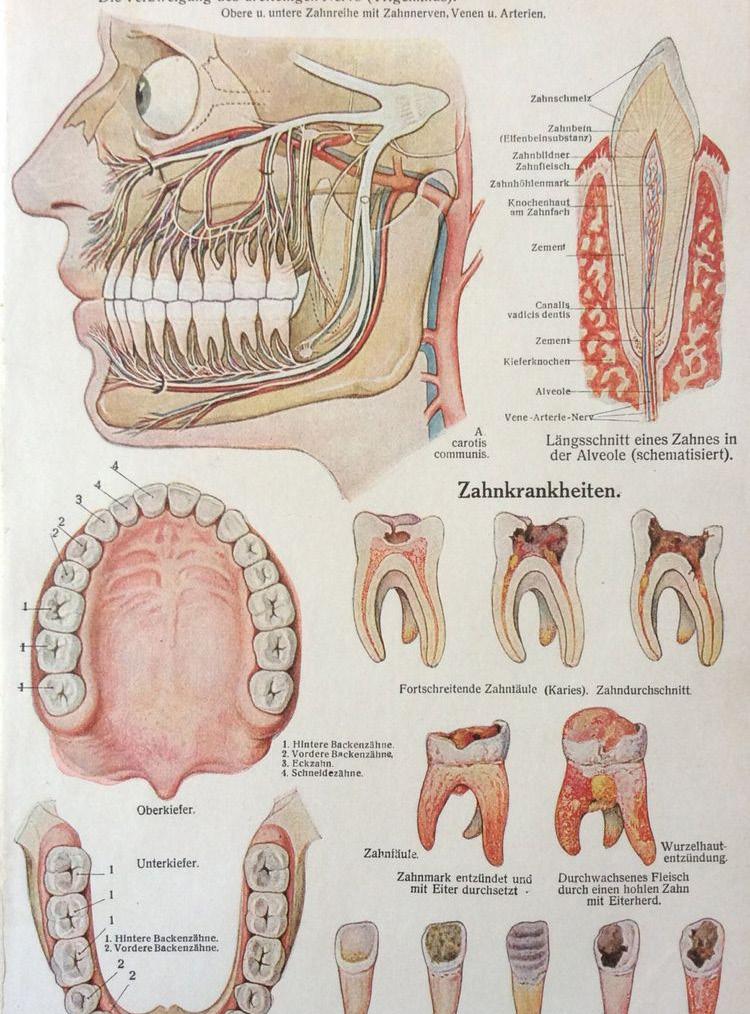
Dental anatomy ex amines the structures that make up the teeth of a human being. Those studying den tal anatomy will learn the classification, ap pearance, and development processes of the teeth. It is con sidered to be a taxo nomical science due to the nature of clas sifying the various teeth and structures. Each tooth has defin ing structures that make up its general composition. These main components are known as the crown, root, surfaces, cusp, cingulum, ridges, developmental groove, embrasures, and mammelons.
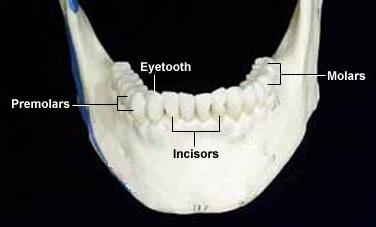
Humans evolved as omnivores, and our teeth reflect this history. We have relatively pathetic canine teeth compared to cats and even other primates such as ba boons. Our premolars and molars and not nearly as efficient as those of ruminants or horses for grinding tough plant material. Nonetheless, our teeth gener ally serve us well for the kind of diet we consume.
The third molars of humans are also known as “wisdom teeth”. These teeth typically emerge be tween 17 and 25 years of age, and of ten crowd other teeth such that they must be pulled. Some peo ple don’t have wis dom teeth, which spares them this trau ma. If you enjoy arts and crafts, and have your wisdom teeth pulled, a fun project is to create a neck lace with the teeth, as shown to the right. Dental anatomy is a field of anat omy dedicated to the study of human tooth structures.
Aztec dentists used to mix Iron fillings, water and navel lint bake and insert into the cavities to seal it




Long ago, people used to ground up chalk or charcoal, lemon juice, ashes or even a mixture of tobacco and hon ey to clean their teeth. It was only about 100 years ago that someone finally created a minty cream to clean their teeth and it came to be known as Toothpaste



Smiling is one of the most natural things sal language that is understood by all people es or cultures. From the most modern society the same t hing. Our instincts compel us to you ever wondered about the science behind posed to like people who smile and why does Let us delve a little bit
When we see something that makes us happy work), a signal is sent to the brain-stem, the transferred to the facial muscles that translate feedback signal that is sent back to the brain that ous cycle can go on and on, translating to increased
When you smile, the brain releases endorphins ing thing is that we don’t even have to mean still give us the good feelings that a real smile often told to smile even when we don’t feel that if you smile, the endorphins that your lead to a more positive predisposition than
Smiling helps the body to reduce stress and linked to a weakened immune system and eliminating health outcomes. The reason why we are generally on the same principle. Children smile more pany, their smiles activate our smiles and leads
With such health benefits, it is important to people don’t smile a lot is that they are simply need to learn to be comfortable smiling. You ant memories such as a funny thing you read that you like. This simple mental trick will have mood will immediately lift when you start smiling.
things for human beings. It is also a univer people across the planet, including all rac society to the most traditional, a smile means to warm up to people who smile at us. Have behind smiling? Why are we always pre-dis does a perfect smile open door for a person? into the science behind smiling .

happy (such as seeing your child after a long day at the oldest part of our brain. This signal is then translate it into a smile. When this happens, there is a that makes us feel happy and at peace. This virtu increased happiness and joy by the smiling person.
endorphins which make us feel happier. The interest mean it. Simply smiling without even a reason will smile triggers in our brain. This is why we are feel like smiling. It is based on the proven fact your brain releases as a response will eventually than the one you started with in the first place. and this then leads to improved health. Stress is eliminating it from our lives often leads to better generally happier around young children is based more than adults and when we are in their com leads to an overall improvement in our mood. learn to smile more. One of the reasons why simply not used to smiling. For this reason, we can make this task easier by picturing pleas read or thinking about the company of someone have you smiling and you will notice that your smiling.

The provision of dental treatment expos es clinicians, their team members, and their patients to a variety of pathogen ic microorganisms; therefore, acquiring an understanding of how infectious dis ease develops and adhering to CDC’s Stan dard Precautions as part of a robust infec tion control program is essential to prevent transmission in dental practice settings.
This article examines the risks of infection asso ciated with the practice of dentistry and explains the steps involved in the development of infec tious disease, including methods of transmis sion and routes of entry into the human body. Infection prevention and control procedures are discussed, including complying with hand hy giene recommendations, utilizing appropriate PPE, adhering to sharps safety practices, and en suring the proper disin fection and sterilization of equipment and envi ronmental services. Rec ommendations are made regarding the routine immunization of dental health professionals and the need for training and education is emphasized
Dental healthcare profession als may be at risk of exposure to numerous workplace haz ards. These hazards include, but are not limited to, a spec trum of bloodborne and other microbial pathogens, pharma ceuticals and other chemical agents (ie, liquid, solid, gas eous), ergonomic hazards, ra diation, noise, vibration, heat, traumatic injury, and work place violence.1 Although there are no Occupational Safety and Health Administra tion (OSHA) standards spe cific to dentistry, regulations regarding exposure to numer ous biological, chemical, envi ronmental, physical, and psy chological workplace hazards that may apply to dentistry are addressed in OSHA’s stan dards for General Industry.
DDS


The Roundtable is a forum for debate on key topics, trends, and techniques in dentistry. For each edi tion, a panel of experts examines a subject to help expand your knowl edge and improve your practice. This month, our panel discusses esthet ic dentistry, focusing on patient expectations in the esthetic zone, prepa rations, restorative op tions, and recommenda tions for bonding success. To watch the whole conversation, go to: insidedentistry.net/go/ roundtable-indirect
Inside Dentistry (ID): How
successfully navigate patient demands and expectations with your clinical protocol, and is it you or the patient who is ultimately answer able for the smile design?
do youDennis Wells, Peter Harnois, DDS David Hornbrook, DDS
Dennis Wells,
Successfully navigating expectations with after 35 years, is still my practice, we approach “prototypes,” a word Eubank, DDS, years to test-drive and approve we move forward with the ceramist. Swatches, and photographs are nothing can compare smile in their mouth, being able to test ally, and esthetically. a co-effort between Dentists have the expertise and knowledge chewing system, as of esthetics and their and marry that with tastes, and specific tient to take too much don’t have enough tist has too much you’re going to miss subjectivity that is Beautiful smiles present ber of looks, feels, if we don’t create design is vulnerable tice, we try to be We’re not dictators but we sometimes have what his or her role and where they ultimately

navigating patient demands and my clinical protocol, even still a difficult process. At approach every case using word I borrowed from Jimmy years ago. We want our patients approve their smiles before with ordering the case from Swatches, computer simulation, are helpful, but for patients, compare to having their new mouth, under their lips, and it phonetically, function esthetically. As for the design, it’s between the dentist and patient. responsibility to use their knowledge of teeth and the as well as their knowledge their own personal taste, with the patient’s interests, wishes. If we allow the pa much control, they simply enough information. If the den control, then many times miss the arena of patient is inherent in smile design. present in a limitless num feels, and artistic designs, and create a partnership, then the vulnerable to failure. At my prac coaches and consultants. in the smile design process, have to explain to the patient role is, the limits of that role, ultimately do have to trust us.
The more that I do this, the more I ap preciate just how tricky the communi cation is and that there is a sweet spotyou just have to know how to get to it.

Dennis is absolutely right. There comes a point when the patient has to trust that we know what we’re doing. We allow the patient to become part of the process by introduc ing them to a trial smile that they can wear inside their lipline and function with for 3 to 4 weeks before the laboratory finishes the ceramic work. We’ve all been trained by the American Academy of Cosmetic Dentistry to work from patient-approved provisional restorations, and when a patient likes their temporaries, it removes some of my stress. Before that came to fruition, we could hope that a patient would be happy with their new smile, but we wouldn’t know for sure. Now, patients have the ability to approve a resto ration that the laboratory then reproduces. To ensure success in complex cases, when the patient is chairside, I take off half of the tem poraries to see that the lab has actually mir rored them correctly. It’s very helpful to get information from the patient about what they want. If a patient brings in picture of a celeb rity and tells me that he or she wants to have those teeth, it makes my job quite a bit easi er, and the design becomes a co-partnership.
 David Hornbrook, DDS (DH):
David Hornbrook, DDS (DH):
We demand that our patients trust us, but I can guarantee that in the past, when patients have said, “Do whatever you think is right. I trust you,” we’ve had to redo some cases. The trial smile, prototype, mockup, and provisional restorations address the things that need to be done and how the patient wants to look, but they are also about defin ing variables. These are things like shape, length, contours, surface tex ture, and incisal edge characterizations. When I consult my patients, I believe that they are building what I call a “brain smile.” They might say that they want white teeth, but I’m not just going to go with sing shade guides, my own teeth, my dental assistant’s teeth, or photographs. My goal is to have them look at that shade tab or another smile and say, “Yes, that is what I meant.” Then they’ll put that exact shade in their brain smile. I do this with any smile variable because even though they trust me, some of the variables that I like, they may not like. I make sure that I use examples for the different aspects of those variables so they’ll put them in their brain smile. They’re the homeowner, the ceramist is the builder, and I’m just the architect. My goal is to make sure that everything is done properly so it lasts a long time, but I want to take my patients in put, add nuances to make sure it’s going to look esthetically pleasing, and try to guide them in the direction that I feel is going to be best for them. that. I’m going to show them examples of what “white” is using shade guides, my own teeth, my dental assistant’s teeth, or photographs.
My goal is to have them look at that shade tab or another smile and say, “Yes, that is what I meant.” Then they’ll put that exact shade in their brain smile. I do this with any smile variable because even though they trust me, some of the variables that I like, they may not like. I make sure that I use examples for the different aspects of those variables so they’ll put them in their brain smile. They’re the homeowner, the ceramist is the builder, and I’m just the architect. My goal is to make sure that everything is done properly so it lasts a long time, but I want to take my patients input, add nuanc es to make sure it’s going to look esthetically pleasing, and try to guide them in the direction that I feel is going to be best for them.
ID: There are many material options available today from feldspathic porcelain, to lithium disilicate, to the ever-popular zirconia esthetic. What are your considerations and go-to materials to satisfy expectations?
DW: I have a personal bias, which is toward feldspathic pow der liquid ceramics. I feel pretty strongly that those are the gold standard in terms of pure esthetics and the ability to assemble a restoration in a way that mimics nature like none other. With that said, I think the harder materials that we have now-the zirconias and the lithium disilicates-are gifts sent from the dental gods because there are definitely pa tients whose muscle forces and parafunctional habits are going to exceed the limits of their own natural teeth as well as feldspathic porcelains. You can set the teeth up as perfectly as you want in their mouths and have the occlusion dialed in, but if patients bite their nails, then they’re more than like ly going to challenge their ceram ics in the same manner as their natural teeth. Lithium disilicate is a material that we go to from time to time without cutting it back and weakening it, but it’s always a second choice if we’re talking about really demanding esthetics.
PH: I agree with everything that Dennis said. There was a time when the only thing that I wanted to use was feldspathic porcelain.
Then IPS e.max (Ivoclar Viva dent) and the lithium disilicates came out. With those materials, you get flexural strength that ranges from less than 100 MPa to more than 400 MPa. I’ve be come a strength person, and I’ve never looked back. I use lithium disilicate, and Dennis made an other great point in that it can’t be cut back, or you’ll lose the advan tage of using it in the first place. There’s a process using an Additive-Reductive Template (DenMat) for which I’m now a part of the education team. With this pro cess, you put reduction templates over the patient’s teeth and minimally reduce only what is necessary to get an ideal arch form. You can get lithium disilicate down to 0.3-mm thick and use a bur or rubber disk at the mar gin, and then you do not have to necessarily prepare a margin in these cases. I’ve started to com bine all of the best elements of minimally invasive dentistry. And yes, I’m giving up some esthetics, but when I make the decision for my patients, the strength al lows me to sleep better at night.
ID: Peter, there seems to be fear associated with esthetic bond ing. Is there any key advice you can pass along to help others ensure the predictable outcomes that you achieve for your patients?
PH: I may be giving a very simplistic response to this, but my advice is to read the directions and look at the science be hind them. Google the components and become a student of the chemistry behind the materials. Once you take some time to re search and understand the systems, it takes away the stress.
DH: Well, I think Peter is exactly right-reading the directions is number one. Unfortunately, those are the first things that are thrown out by the average dentist. Fortunately, these can now be retrieved from the internet if thrown away. It’s also important to slow down.
Everyone wants something that is faster, easier, and cheaper, but it doesn’t always work that way. I think newer dentists believe that they need to put these restorations in the mouth in 1 hour or that they need to have four or five hygiene checks during a smile design insertion appointment. Instead of rushing, do everything possible to make sure that you’re doing the very best that you can for the patient you’re working on. Follow mentors, look at research instead of flashy advertise ments, take your time, isolate properly, and read the instructions.
DW: You should also have a very strict protocol that is followed by you, your team, and your laboratory. The entire process should be cinched down tight so that each step runs smoothly. Bonding can be re ally fun and exciting as long as you’re in control.
Dennis Wells, DDS, is a member of the American Academy of Cos metic Dentistry and maintains a private practice in Nashville, Ten nessee.
Peter Harnois, DDS,is the president of the Illinois American Academy of Facial Esthetics and is in private practice in Hinsdale, Illinois.
David Hornbrook, DDS, is the director of education at Utah Valley Dental Lab and maintains a private practice in San Diego, California.

The world’s oldest-known formula for toothpaste, used more than 1,500 years before Colgate began marketing in 1873, was discovered on a piece of dusty pa pyrus in the basement of a Viennese museum
Sleep-related breathing disorders are conditions of abnormal and difficult respiration during sleep, including chronic snoring and sleep apnea. Some sleep-related breathing disorders have limited health impact, but others can have serious consequences because of their potential ef fects on sleep and the balance of oxygen and carbon dioxide in the blood. The American Academy of Sleep Medicine (AASM) identifies several types and subtypes of sleep-related breathing disorders. The symptoms, severity, causes, and treatment of sleep-disordered breathing varies based on the type. In complex cases, a person may be diagnosed with more than one type.
Obstructive sleep apnea (OSA) is one of the most common and serious sleep-re lated breathing disorders. In OSA, the airway repeatedly collapses during sleep, causing lapses in breathing that both fragment sleep and affect the body’s oxygen levels. Upper airway resistance syndrome (UARS) is a milder form of OSA in which sleep is disrupted but oxygen levels are not affected to the same degree. OSA may affect as many as 30% of adults and is more common in men than wom an. The condition is likely underdiagnosed, and many experts anticipate that its prevalence will increase in the future along with growing rates of obesity, which is one of the major risk factors for OSA. Snoring, gasping, or choking during sleep, and excessive daytime sleepiness are central symptoms of OSA. When left un treated, the condition can cause significant health problems including cardio vascular issues like high blood pressure and stroke. A range of treatment options are effective in addressing obstructive sleep apnea and reducing its symptoms.
Obstructive sleep apnea occurs in infants and children although considerably less often than in adults. It is estimated to affect 1-5% of children of all ages. Compared to adults, children are more likely to have OSA that is relat ed to enlargement of the tonsils and adenoids, which are masses of tis sue at the back of the throat that are part of the immune system. For this reason, surgery, specifically removal of the adenoids and tonsils (adenotonsillectomy), is more frequently part of treatment for pediatric OSA. In addition, OSA goes away on its own in some children as they get older, so the condition does not always require immediate treatment.

In central sleep apnea (CSA), lapses in respiration during sleep occur because of a lack of effort to breathe. This happens when either the brain does not properly send signals to the re spiratory muscles or the respiratory muscles don’t activate in response to the brain’s signals. In this way, central sleep apnea is distinct from obstructive sleep apnea, but people can have symptoms of both conditions at the same time. In addition, sometimes the treat ment for OSA triggers CSA, which is called treatment-emergent central sleep apnea. CSA is much less common than OSA, affecting just under 1% of people over the age of 40. It is more common in males and in people who are over 65. There are dif ferent types of CSA based on the nature of the underlying problem prevent ing proper respiration. Some established risk factors include cardiovascular prob lems, use of narcotics, and high altitude, but not all cases are tied to these issues. A key focus of treatment for central sleep apnea is addressing its underlying cause.
Sleep-related hypoventilation disor ders involve elevated blood levels of carbon dioxide during sleep that result from a lack of air moving in and out of the lungs. This insufficient breath ing is commonly tied to other health problems. Often, people with sleep-re lated hypoventilation disorders have lung conditions like chronic obstructive pulmonary disease (COPD) or pul monary hypertension. Disorders that affect the nervous system and some types of medications can also affect breathing and trigger hypoventilation. A specific type of sleep-related hy poventilation disorder is called obesity hypoventilation syndrome (OHS). This condition can occur in obese patients and normally co-occurs with obstructive sleep apnea. It is frequently associated with poor sleep and can lead to detrimen tal effects on the cardiovascular system. Many people with sleep-related hy poventilation disorders struggle to breathe properly when they are awake, but the problem normally intensifies during sleep. As with central sleep ap nea, treatment for sleep-related hy poventilation disorders is often direct ed at managing an underlying illness contributing to breathing problems.
Snoring occurs when air moves around floppy es that tissue to vibrate. Estimates hold that as en, and 57% of adult men snore. Light snoring every ple and is not harmful. Snoring that occurs more than as a sleep-related breathing disorder. It may be al snoring, and it is differentiated from frequent snoring Risk factors for chronic snoring include things that either Examples include obesity, use of alcohol and sedatives, back. Some people are more inclined to snore because The main health concern associated with snoring is case of obstructive sleep apnea, so it is important to talk toms such as daytime sleepiness, recent weight gain, If no other symptoms are present, the greatest impact of or family members who are bothered by the noise and can be helpful in reducing snoring so that it is less bothersome

Catathrenia is a pattern of abnormal breathing and vocalization that is often referred to as sleep-relat ed groaning. During episodes of catathrenia, a sleeper takes in a long-inhaled breath and then exhales slow ly while making a monotone, groan-like sound. As this occurs, the sleeper is not aware of the vocalizations. Catathrenia is uncommon and does not pose any known health risks to the sleeper. However, it can be annoying or disruptive for bed partners or others within earshot. Peo ple with catathrenia may also be embarrassed about the sounds once they are made aware of the condition. When desired, treatments for obstructive sleep apnea, such as the use of a continuous positive airway pressure (CPAP) device, have achieved reductions in catathrenia episodes.
tissue near the back of the throat and caus many as 27% of children, 40% of adult wom every once in a while is normal for most peothan three nights per week, though, is classified be referred to as primary, chronic, or habitu snoring associated with obstructive sleep apnea. either constrict the airway or cause tissue to relax. sedatives, chronic nasal congestion, and sleeping on your because of the anatomy of their mouth, nose, and throat. the possibility that it is indicative of an underlying talk with a doctor if snoring occurs with other symp teeth grinding during sleep, or morning headaches. of chronic snoring may be on a bed partner, roommate, and find it harder to sleep. Various types of treatments bothersome to other members of the person’s household.
Hypoxemia is a low level of oxygen in the blood. Sleep-related hypoxemia disorder is when oxygen concentrations drop, but the levels of carbon dioxide don’t rise high enough to cross the threshold for diagnosis as a sleep-related hypoventilation dis order.Sleep-related hypoxemia disorder occurs mostly as the result of another health problem that affects breathing, includ ing a number of types of lung conditions, and addressing hy poxemia frequently involves a focus on that underlying issue.
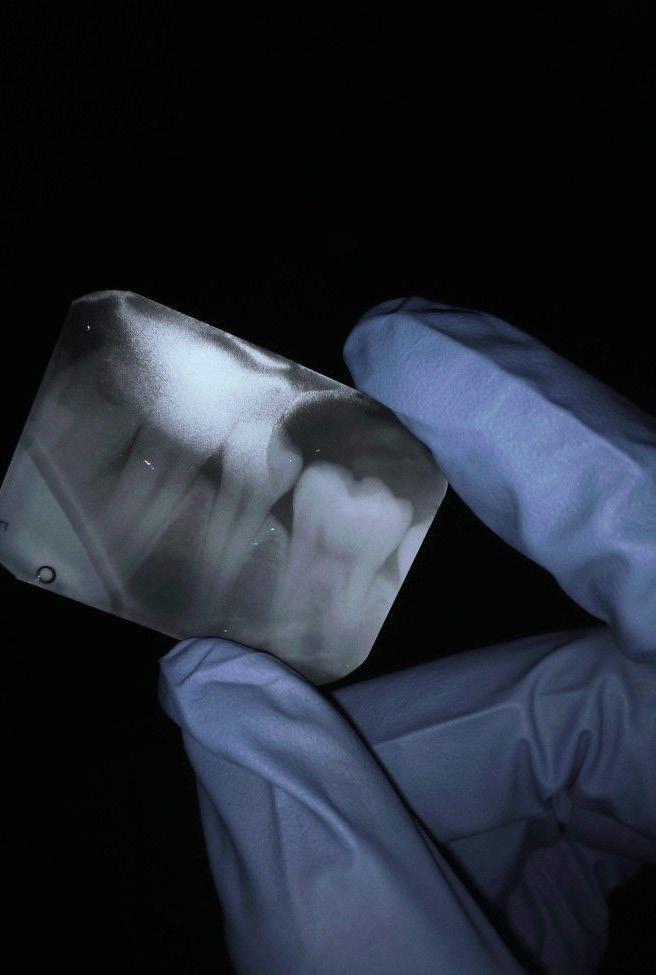
Early in dental school training, students learn to identify the radiographic appearance of ed with pulp capping or a pulpotomy. Clinicians who perform these types of endodontic procedures ment, and the radiographic images of these procedures are distinctly different. With the tal pulp therapy procedures (ie, for vital pulps) being performed in clinical practice, the This article discusses regenerative endodontics, changes in vital pulp therapy procedures,
Regenerative endodontics involves the performance of biologically-based procedures ing dentin, root structures, and the pulp-dentin complex. It should be noted that in tion are often used synonymously and interchangeably. Clinically, a regenerative endodontic ic pulp to obtain root-end closure with the goal of obtaining continued development of for apexification on these types of teeth is performed by placing calcium hydroxide over oxide aggregate. Based on outcomes, these apexification treatments have demonstrated the Clinical treatment of an immature permanent tooth with necrotic pulp using regenerative tial appointment, after local anesthesia is administered and isolation is achieved thin dentinal walls) in conjunction with irrigation using 1.5% sodium hypochlorite cells. After preparing the canal, it is irrigated with sterile saline and dried, then an antimicrobial medication between treatments. Following this, the canal access is temporized it™ Temporary Filling Material, 3M; IRM® Immediate Restorative Material, Dentsply Sirona),
At the second regenerative endodontic treatment appointment, a 3% solution of mepivacaine HCL procedures, the induction of periapical bleeding into the canal space is necessary, and the absence of a vasoconstrictor 17% ethylenediaminetetraacetic acid (EDTA) is used to irrigate the canal. Next, the canal is dried, the canal to around the level of the cementoenamel junction (Figure 2). This induced bleeding brings those that were released by the dentinal matrix when the 17% EDTA was irrigated into the canal. The After a resorbable collagen matrix is placed over the blood clot, a bioceramic material is placed directly composite restoration is then placed over the glass ionomer, and a final radiograph is taken (Figure 4). The

Recently, there have been reports in the literature that describe the use of regenerative endodontic mature permanent teeth with necrotic pulps, teeth with persistent apical periodontitis following resorption, teeth with horizontal fractures, and avulsed teeth. One reason for the increase manent teeth with necrotic pulps is the belief that obturating a disinfected canal with the host’s
The tissues generated in canals after a regenerative endodontics procedure are similar to those Although none of these tissues are true pulpal tissue, they are the host’s own vital tissues; One problem in clinical practice is that many clinicians are not familiar with regenerative endodontics. root canal treatment was not completed. They often proceed to either extract the tooth or access it and
of a tooth that has been treated with a root canal as well as teeth that have been treat procedures on their patients confirm their success by taking a final radiograph after treat increasing number of regenerative endodontic procedures (ie, for necrotic pulps) and vi appearance of the final radiographs taken after the completion of treatment has changed. and how these changes have impacted the new appearance of radiographs in endodontics.
procedures that are designed to physiologically replace damaged tooth structures, includ in the endodontic literature, the terms regeneration, revascularization, and revitaliza endodontic procedure is one that is performed on an immature permanent tooth with necrot the root and thickening of the canal walls (Figure 1).Historically, the clinical treatment over a period of several months or delivering a single-step treatment with mineral tri the ability to obtain root closure but not continued root development and wall thickening.
regenerative endodontics usually involves two treatment appointments. At the ini achieved with a rubber dam, minimal canal instrumentation is performed (due to the hypochlorite (NaOCl). This lower concentration is used to limit the killing of stem calcium hydroxide or a triple antibiotic paste is placed in the canal to serve as temporized with a sterile cotton pellet or sponge and a temporary material (eg, Cav Sirona), and the patient is asked to return in 1 to 4 weeks for the final treatment appointment.
HCL without an added vasoconstrictor is used to achieve local anesthesia. In regenerative endodontic vasoconstrictor will help facilitate this process. A rubber dam is placed, and after the tooth is accessed, and bleeding is induced 1 to 2 mm beyond the apical foramen with a hand file. The blood should fill with it scaffolding, stem cells, and additional blood-derived bioactive growth factors to complement The triad of stem cells, scaffolding, and growth factors is what enables tissue regeneration to occur. directly over the collagen matrix, and a glass ionomer is placed over the bioceramic material (Figure 3). A final patient should be put on a 6-month recall schedule for as long as 3 years, dictated by the process of healing.
endodontic procedures not only on immature permanent teeth with necrotic pulps but also on following conventional endodontic treatment, traumatized teeth with external inflammatory in the use of regenerative endodontics for cases other than those involving immature per host’s vital tissue may be better than using foreign materials (eg, gutta-percha and sealers).
those of the cementum, bone, and periodontal ligament and contain blood vessels and nerves. tissues; thus, they are inherited with immune defense mechanisms to protect a gainst infection. endodontics. When they view a radiograph of a patient who has had this procedure, their initial thought is that the and perform conventional endodontic re-treatment, consequently destroying the bioactive obturation.

Although the use of calcium hydroxide for vital pulp therapy was first reported in the literature more than 79 years ago, during the last couple of years, there has been a paradigm shift in vital pulp therapy. This shift has included the replacement of cal cium hydroxide with bioceramic materi als, sodium hypochlorite with EDTA, and temporary fillings with a composite or amalgam restoration. In addition to this paradigm shift, another recent advance ment in vital pulp therapy is cryotherapy.
The goal of cryotherapy is to lower the tem perature of the tissue. Lowering the tempera ture of human tissue has been shown to de crease nerve conduction velocity as well as reduce hemorrhage, edema, and inflamma tion. Cryotherapy has also been shown to re duce the number of leukocytes that adhere to the endothelial walls of the capillaries, which limits the migration of these types of cells to the affected tissue, reducing endothelial dysfunction and further reducing inflam mation. In addition, cryotherapy can dimin ish the clinical need for pharmacologic in tervention via narcotics or local anesthesia. Vital pulp cryotherapy is a new technique that involves the placement of sterile shaved ice on vital pulpal tissue that has been direct ly or indirectly exposed by a carious lesion (Figure 5). For endodontic treatment, it is used in conjunction with 17% EDTA, bioce ramic pulp capping materials, and restorative materials. Vital pulp cryotherapy has been shown to reduce postoperative tooth pain.

This procedure can be performed on teeth with a pretreatment pulpal diagnosis of nor mal, reversible pulpitis or symptomatic, ir reversible pulpitis as well as on teeth with a pretreatment periradicular diagnosis of normal or symptomatic apical periodon titis (ie, by percussion and/or palpation tests without radiographic evidence or by a periapical radiograph and/or a cone-beam computed tomography scan indicating a periradicular radiolucency [lesion]). It is im portant to note that the performance of vital pulp cryotherapy necessitates that the tooth be restored with a composite or amalgam restoration immediately following the pro cedure. It is contraindicated to place a tem porary filling or prepare a tooth for a crown after a vital pulp cryotherapy procedure.
After the definitive restoration is placed, the final radiograph taken demonstrates a sim ilar appearance to the final radiograph tak en after a regenerative endodontic treatment (Figure 6). When comparing the final radio graph of a vital pulp cryotherapy treatment with one taken after vital pulp therapy with calcium hydroxide, the vital pulp cryothera py radiograph exhibits increased radiopacity and can demonstrate deeper material place ment on the coronal portion of the pulp.
Unlike the distinctively different radiograph ic appearance of teeth that have been treated with conventional endodontic treatment and teeth that have been treated with vital pulp therapy, the radiographic appearance of a regenerative endodontic procedure is quite similar to that of a vital pulp cryotherapy pro cedure. The future direction of endodontic treatment is moving toward a more biologic approach to treating inflammation and infec tion of the pulpal tissue, and the procedures of regenerative endodontics and vital pulp cryo therapy demonstrate a better clinical ability to do this than the traditional methodology.
This change in conventional endodontic treatment has made it more about func tion than form (ie, bioactive obturation vs gutta-percha and sealer obturation).
As with any change in healthcare tech nology and treatment protocols, there is a “technology adoption life cycle.” This life cycle is a bell curve that divides cli nicians into the categories of early, early majority, late majority, and laggards re
The plaque that is on a person’s teeth is loaded with bacteria. There are actually over 300 dif ferent kinds of bacteria that make up this nasty substance that the den tist cleans off for you. That means dentists are exposed to more bac teria every day than a majority of other pro fessions, including fam ily doctors. This fact should also make you think twice about put ting a mouth wash on your next shopping list.
