




You’re not just our patient. You’re our neighbor. For more than a century, Orlando Health Orlando Regional Medical Center has been honored to provide nationally recognized care for the Central Florida region we proudly call home. And because it’s your home, too, you deserve trusted healthcare within reach, so we can foster a partnership focused on health and wellness — together. Giving you more reasons to choose well. OrlandoHealth.com/ORMC choose well.

Epilepsy is one of the most common neurological disorders that causes unprovoked, recurrent seizures. A seizure is a sudden rush of abnormal electrical activity in the brain. Anyone can develop epilepsy, but it’s more common in young children and older adults. In adults aged 65 and older, the most common causes for new-onset epilepsy are ischemic stroke, neurodegenerative conditions such as dementia, tumors, and trauma. Nearly 25% of new-onset epilepsy occurs in the elderly.

With an average prevalence of 1%, sixty-five million people around the world have epilepsy. Three million four hundred thousand of those people are in the United States, and about 224,000 of them are in Florida. In addition, one in 26 people in the United States will develop epilepsy at some point in their lifetime. One-third of epilepsy patients live with uncontrolled seizures despite taking seizure medications. Six out of ten people with epilepsy have been unable to identify the cause of it. There are two main types of epilepsy: generalized epilepsy, which may affect the whole brain at the same time, and focal (or partial) seizures, which originate in one part of the brain and may spread to nearby areas, or even the entire brain.

Iam pleased to bring you another issue of Florida MD. Human trafficking is one of the horrors in today’s society. It’s modern day slavery and Central Florida is one of the worst places in the country. I have asked Paving the Way, an organization headquartered here in Central Florida that helps physicians spot signs that one of their patients could be a victim. Please check out their website and help put a stop to human trafficking..
Best regards,
Donald B. Rauhofer Publisher
According to Homeland Security, there are over 300,000 children a year trafficked in the United States. In fact, Florida ranks 3rd in the county for calls to the National Trafficking Hotline and right here in Central Florida, Orange county ranks 2nd in the state for child trafficking case. Sadly, the average age of entry is 11-14.
Those facts can be frightening, leaving most people asking, who am I to do anything about this? More importantly, what can I do?
Paving The Way Foundation was created to provide answers to those questions. We’ve educated over 13,000 youth, parents, teachers, and community leaders about human trafficking, the impact it has on families and the actions to take to prevent it.

A surprising statistic is 88% of trafficking victims reported being in a medical setting for various concerns but did not feel safe enough to ask for help. We can prevent that from happening by training our frontline teams to learn the signs of trafficking, understand grooming and recruitment tactics and how to engage with patients about this silent crime to get them to safety.
Here is one action you can take right now: put the National Trafficking Hotline number in your phone, 888-3737888, you can call 24 hours a day, 7 days a week.
To learn more about what you can do or ways to get involved in ending human trafficking we invite you to join in the fight, please go to our website, www.pavingthewayfoundation.org click on programs for information on what’s available to educate you and your staff or download one of our tool kits. Together we can disrupt the cycle of human trafficking.
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: John “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, FACP, FCCP, FAASM, Omer Abdul Hamid, MD, Paul J. Watkins, Michael Jablonski, MD, Christian Rosado, MD, John Meisenheimer, VII, MD

Art Director/Designer: Ana Espinosa
Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762. Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2023 Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.

Since opening one decade ago, Nemours Children’s Hospital, Florida has been part of a sea change in children’s health. Bringing unique programs to millions of central Florida families, providing innovative care to our region’s most medically challenged children, and ensuring a pipeline of pediatric providers across the state. While we celebrate how far we’ve come, it’s not even close to how far we’ll go to ensure every child’s world is a place for them to thrive.
 FLORIDIAN CENTER OF EXCELLENCE IN COMPREHENSIVE EPILEPSY CARE.
FLORIDIAN CENTER OF EXCELLENCE IN COMPREHENSIVE EPILEPSY CARE.
Epilepsy is one of the most common neurological disorders that causes unprovoked, recurrent seizures. A seizure is a sudden rush of abnormal electrical activity in the brain. Anyone can develop epilepsy, but it’s more common in young children and older adults. In adults aged 65 and older, the most common causes for new-onset epilepsy are ischemic stroke, neurodegenerative conditions such as dementia, tumors, and trauma. Nearly 25% of newonset epilepsy occurs in the elderly.
With an average prevalence of 1%, sixty-five million people around the world have epilepsy.Three million four hundred thousand of those people are in the United States, and about 224,000 of them are in Florida. In addition, one in 26 people in the United States will develop epilepsy at some point in their lifetime. One-third of epilepsy patients live with uncontrolled seizures despite taking seizure medications. Six out of ten people with epilepsy have been unable to identify the cause of it. There are two main types of epilepsy: generalized epilepsy, which may affect the whole brain at the same time, and focal (or partial) seizures, which originate in one part of the brain and may spread to nearby areas, or even the entire brain.
If a seizure doesn’t affect consciousness, it’s called “focal aware,”
previously known as “simple partial seizure.” If a seizure affects consciousness, it’s called “focal unaware,” previously known as “complex partial seizure.” Seizures can either be convulsive or non-convulsive, and at times, especially in critically ill ICU patients, seizures may be happening inside the brain without any obvious outward signs except altered mental status or comatose state. These are called “subclinical seizures.” Most seizures last one to two minutes, but sometimes, they may go on for several minutes. One episode of seizure or a cluster of seizures lasting more than five minutes without the patient returning to baseline is a life-threatening condition called “status epilepticus.”
Epilepsy causes people to have repeated seizures, but not everyone who has a seizure has epilepsy. Low blood glucose or sodium level, alcohol withdrawal, illicit drugs, infections, certain medications, or fever (especially in children) can also cause seizures. Other problems, such as anxiety, conversion disorder/psychogenic non-epileptic seizures (PNES), or fainting spells, can cause events that look like seizures. As a result, patients are sometimes subjected to unnecessary medications and procedures. Therefore, accurate and timely diagnosis and treatment are of paramount importance.
Since 2007, Epilepsy Freedom Center at Falcon Advanced Neurology in Orlando has been providing leading-edge diagnosis and treatment of all types of epilepsy and sleep disorders.
“Epilepsy can be due to a variety of reasons across the age spectrum, starting from newborn babies to elderly adults,” says Falcon Epilepsy Freedom Center’s medical director and neurologist-in-chief Jaivir S. Rathore, MD, FAES. “DocJ,” as he’s known, is triple board certified in neurology, epilepsy, and clinical neurophysiology.
He’s among the select few neurologists in the entire state of Florida to have received the prestigious Fellow of the American Epilepsy Society (FAES) designation in 2021 for his distinguished career and more than a decade of clinical, research, and leadership contribution to the field of epilepsy and neurology. Dr. Rathore is a Member of the American Academy of Neurology (AAN) and the Continuing Medical Education (CME) Committee for the American Epilepsy Society (AES), a Former Vice-Chairman of the Clinical Fellows Council, and Chief Fellow of the prestigious Johns Hopkins Hospital in Baltimore, Maryland, which has been ranked the number one hospital for neurology and the most number one ranked hospital in the United States by U.S. News & World Report.
Seizures may present in a variety of ways, some of which may be difficult to recognize, especially for patients or their families, and in some cases, even for healthcare providers other than trained epilepsy specialist neurologists. Most physicians know seizures as generalized tonic-clonic, often called “grand mal seizures,” in which a person has shaking, eye-rolling, foaming at the mouth, tongue biting, bowel/bladder incontinence, falling, and becoming unconscious. Many times, though, epilepsy can have subtle presentations, including abnormal taste or smell, déjà vu sensation; abnormal visual or auditory phenomenon, including hallucinations; headaches, altered mental status like staring spells or loss of consciousness episodes, “roller coaster” feeling, gastric rising sensations, palpitations, nausea; and decline in cognitive abilities, including memory deficits. Another possible presentation is outof-context smiling or laughing (gelastic seizures) or crying (dacrystic seizures).
Sometimes, seizures can cause an intense sense of impending doom or fear, which may be labeled as “psychiatric conditions” or “panic attacks” and may cause several years of delay in diagnosis and appropriate treatment. Seizures can cause labile mood, more commonly depression, anxiety, acute psychosis, and suicidal ideations. “My paper in Harvard journal ‘Epilepsy & Behavior,’ grant funded by the National Institutes of Health (NIH), on depression screening using PHQ-9 as a screening tool is one of the most commonly used tests worldwide,” informs Dr. Rathore. The paper can be found at: https://pubmed.ncbi.nlm.nih.gov/25064739/.
“Epilepsy can worsen a variety of other medical conditions. In patients with or without cardiac arrhythmias, it increases the risk of sudden death due to cardiac arrest in 1% of cases. This phenomenon is called ‘Sudden Unexpected Death in Epilepsy,’ or ‘SUDEP,’ the risk of which is higher in convulsive seizures and seizures that originate from sleep stages,” states Dr. Rathore, an Alumnus Fellow of the Cleveland Clinic Epilepsy Center. Find more information about the Center at The Charles Shor Epilepsy Center | Cleveland Clinic.

Diagnosis of epilepsy starts with a comprehensive history taking and meticulous neurological examination by an experienced neurologist, followed by a brain wave test (video EEG) and a brain MRI with epilepsy protocol. In addition, the neurologist may order lab work to rule out an electrolyte disturbance, metabolic cause, infection, or drug abuse as the cause. In some pediatric cases, the neurologist may order a genetic panel as well. There’s a series of other imaging studies that can be done if a patient needs exact localization of the seizure focus if surgery is planned (which may include FDG-PET, Ictal SPECT, fMRI, or magnetoencephalogram (MEG) and neuropsychological evaluation). For more accurate localization of seizure focus and functional brain mapping before surgery, stereotactic intracranial electrode placement for SEEG or sub-dural grid electrodes for electrocorticography/ECoG can be done. Dr. Rathore collaborates with functional neurosurgery at some of the leading tertiary care hospitals for surgical care of his patients.
“Robotic SEEG started in North America at the Cleveland Clinic in Ohio in 2010,” shares Dr. Rathore, “and I was one of the first fellows to learn that revolutionary technique during my fellowship with the world-renowned first neurosurgeon to do it, Dr. Jorge González-Martínez.”
There are more than 30 antiepileptic medications available to control seizures in nearly two-thirds of patients. Special precautions need to be taken in selecting the medications, especially in pregnant patients due to the risk of fetal abnormalities (teratogenicity) of certain medications like valproic acid, topiramate, phenytoin, etc. Unfortunately, despite trying multiple medications, nearly 36% of patients continue to have recurrent seizures, either due to not being able to take these medications because of side effects or due to the medications being ineffective in controlling the seizures. In such patients, neuromodulation, diet therapy (such as ketogenic or Modified Atkins Diet), or surgery are options.

The majority of patients do very well on medications, and most of them can be seizure free, are at lower risk of sudden death, and enjoy a significantly improved quality of life.
Per literature, the reported rates of excellent surgical outcome for non-lesional partial epilepsy range from 41% to 65% for the temporal lobe, 37% for mixed mesial temporal and neocortical sites, and 29% to 56% for extratemporal epilepsy. In the lesional group, seizure freedom rates were significantly better when patients underwent surgery early in the course of the disease.

In appropriate cases, laser interstitial thermotherapy (LiTT) may be an option for people whose epilepsy is caused by a visible abnormality in one area of the brain. Some patients who either do not want surgery or are not surgery candidates may be offered neuromodulation (brain stimulation, or a so-called “seizure pacemaker”) with responsive neurostimulation (RNS® Therapy). RNS uses an implanted device to help prevent seizures before they begin or abort them in the early stages, similar to how a pacemaker detects and treats abnormal heart rhythms. Other neuromodulation devices include deep brain stimulation (DBS) and/or vagus nerve stimulation (VNS). Dr. Rathore did a neurostimulation “J. Kiffin Penry” mini-fellowship at the Wake Forest University School of Medicine in Winston-Salem, NC. Dr. Rathore did the first ever case of RNS in Lakeland, FL area in May 2021.
“It’s very important that patients with uncontrolled seizures have a detailed discussion with their neurologist about safety precautions,” says Dr. Rathore.
“Another important aspect is that of seizure trigger identification and its avoidance for seizure prevention,” adds Dr. Rathore. “Many patients may have their personal seizure trigger factors, such as peri-menstrual ‘catamenial’ seizures, but for most, the common ones are missing antiseizure medications for any reason (forgetting it or not being compliant), sleep deprivation, excess stress, sunlight or flickering light exposure in photosensitive epilepsies; certain medications, such as bupropion, tramadol, stimulants, and some antibiotics, such as penicillin, fluoroquinolones, cephalosporins, carbapenems, etc. All epilepsy patients with frequent seizures and/or generalized tonic-clonic seizures must discuss ‘seizure rescue’ medication options with their neurologist. These have evolved from inconvenient, and at times embarrassing, rectal diazepam of years ago to today’s diazepam or midazolam nasal sprays, which are convenient, quick to administer, faster acting, and very effective. These rescue medications can play a vital role in preventing a serious seizure episode or shorten the duration of a seizure and hence can be lifesaving and, in many

cases, can avert an ER visit or hospitalization.”
Epilepsy Freedom Center at Falcon Advanced Neurology in Orlando, FL provides comprehensive epilepsy care, encompassing medications, surgery, and neuromodulation. “We also offer the ‘Epilepsy Monitoring Unit’ (EMU) diagnostic aspect of epilepsy at Falcon Advanced Neurology,” Dr. Rathore informs. “It’s the oldest and one of only two private independent diagnostic facilities with EMU in the entire state of Florida. Usually, EMU is found only in the large tertiary care hospitals, and the waiting period to get an appointment at such a facility is several months. This waiting period is a major cause for care deficit and, unfortunately, it sometimes causes ER visits for seizure patients.
“We also collaborate with various clinical trials, and we offer clinical trial participation to our patients across various neurological conditions. Also, we’re a research center for our patients,” says Dr. Rathore.
The Epilepsy Foundation of America is the largest epilepsy organization in the country, and Dr. Rathore is the co-chairman of the Florida chapter. He leads educational sessions for various school districts in Central Florida on seizure first aid and offers free consultations for patients who are underinsured or have no insurance or ability to pay. In addition, Dr. Rathore has co-sponsored and led Walk to END EPILEPSY®. The Epilepsy Foundation of America honored Dr. Rathore in 2021 with its prestigious Volunteer Appreciation Award and the American College of Physicians (ACP) also honored Dr. Rathore as one of the Young Achievers at its annual meeting in Orlando in 2014. “The Doctor Is In” on NBC Bloom TV featured Dr. Rathore in October 2019 to raise awareness about epilepsy.
The Florida chapter’s advocacy group works with the state legislature in the capital city of Tallahassee to bring about several changes to help patients. Most recently, the state of Florida passed House Bill 173 into law on March 25, 2022, thereby protecting children and teens living with epilepsies in the state.
“The most rewarding part of my co-chairmanship is reaching out to patients statewide, increasing the awareness of epilepsy, finding out the challenges that patients are facing, and identifying what we can do to help them, as well as the family members and the schools,” says Dr. Rathore, who is a Member of the Reviewer’s Panel for Neurology®, The Official Journal of the American Academy of Neurology.
“As epilepsy is a worldwide disease, I also provide global econsultations, worldwide webinars, and in-person educational lectures at some of the leading medical centers in the US, India, and multiple other countries,” says Dr. Rathore.

The epileptologist is passionate about his work and taking care of his patients. This is evident in his #1 national ranking among all neurologists in web-based, pooled patient reviews on Healthgrades, U.S. News & World Report, and WebMD’s Preferred Provider for 2022. Dr. Rathore was also included in “The America’s Best” neurologist in 2020-2022, as well as being designated the best-rated neurologist in Orlando, FL: https://threebestrated.com/neurologists-in-orlando-fl

Although a substantial portion of Dr. Rathore’s practice is devoted to caring for epilepsy patients, he offers the full spectrum of neurology services at Falcon Advanced Neurology in Orlando, FL, as well as at two additional clinics in The Villages area of Central Florida in collaboration with TriCounty
“I feel a great sense of responsibility to care for my elderly patients, especially those with seizure disorder, given one of my practice areas is The Villages, Florida, which is the largest retirement community in the world, and me being the only boardcertified adult epileptologist in this large catchment area of central to north Florida, in between big cities like Orlando, Tampa, Gainesville, and Jacksonville,” says Dr. Rathore.
“I’m the regional medical director for the southeast US – including Florida – for one of the largest home video EEG companies, called NeuLine Health. We provide home video EEG services across twenty-three states so these patients are not deprived of this testing only because they cannot go to centers or hospitals due to mobility or transportation issues,” says Dr. Rathore.
“Human brain is an enigma containing around 86 billion interconnected neurons, which makes it one of the most complex objects in the universe, which fascinates me,” says the epileptologist. This interest guided him through his medical studies. “I ended up doing an epilepsy research fellowship at Cleveland Clinic for two years and then I did a two-year epilepsy clinical fellowship at Johns Hopkins Medicine. It’s a great honor and privilege to work for the Epilepsy Foundation of America at that level, do research, serve the patients, and offer them the latest, cutting-edge technology in the field of epilepsy. I believe it’s the calling of my life, and I am truly grateful to my family, teachers/ mentors, and friends who have helped me reach this stage of my career.”
Continued on page 8
For more information about Falcon Advanced Neurology & Epilepsy Freedom Center, located at 6000 Metrowest Blvd., Suite 104-105, in Orlando, Florida, 32835, please call (407) 365-3033, or visit www.fsneuro.com. Dr. Rathore has collaborated with TriCounty Health to provide neurology clinic services in The Villages area at 17190 SE 109th Terrace Rd., Summerfield, FL 34491, and at 3990 E. FL-44 in Wildwood, FL 34785 (Suite 4056 in Freedom Plaza). Please call (352) 268-0003 to reach either clinic, or visit www.tricountyhealthllc.com for more information.
SERVICES AVAILABLE AT FALCON ADVANCED NEUROLOGY & EPILEPSY FREEDOM CENTER INCLUDE, BUT ARE NOT LIMITED TO:
Routine and long-term monitoring video EEG (inpatient and at home)
Stroke/TIA
Dizzy spells/syncope
Various headache syndromes (including chronic migraines) and BOTOX® therapy
Concussion/traumatic brain injury (TBI)
Movement disorders, including Parkinson’s Disease, Tardive dyskinesia, Dystonia etc.
Speech/language disorders
Sleep disorders
Memory and dementia disorders, such as Alzheimer’s Disease
Multiple sclerosis and its diagnosis with lumbar puncture for CSF analysis
Neuropathy
Sciatica pain
FALCON ADVANCED NEUROLOGY & EPILEPSY FREEDOM CENTER

6000 Metrowest Blvd. • Suite 104-105 Orlando, FL 32835• 407-365-3033
www.fsneuro.com
#JohnsHopkins #ClevelandClinic #Harvard #UIChicago
#NIH #TopDoctor #EpilepsyFoundation

Restless legs syndrome
Spinal cord disorders
Myasthenia gravis (MG) and other autoimmune neurological conditions
 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
When I was in medical school and revealed to my classmates that I wanted to be a dermatologist, they usually gave me a flabbergasted look and said, “You want to pop zits for a living?” Immediately followed by, “You don’t want to be a real doctor?” I wish the Seinfeld episode, when Jerry was dating a dermatologist, had been released so that I could refer them to it. The Seinfeld episode went something like this:
Jerry was having dinner at a restaurant with his dermatologist girlfriend.
Seinfield - “How’s the life-saving business?
Dermatologist girlfriend - “It’s fine.”
Seinfield - “It must take a really, really big zit to kill a man.”
Dermatologist girlfriend - “What is with you?”
Seinfield - “You called yourself lifesaver. I call you pimple popper M.D.”
A restaurant patron walks up to their table and says, “Dr. Sitarides?”
Dermatologist girlfriend - “Mr. Perry, how are you?”
Mr. Perry - “I just want to thank you again for saving my life.”
Seinfield - “She saved your life?” Jerry has a shocked look on his face.
Mr. Perry - “I had skin cancer.”
Seinfield - “Skin cancer, damn.” Jerry’s face twists in the agony of defeat.
As a Mohs surgeon, I rarely “pop” pimples anymore, not that there is anything disgraceful about helping a patient with a disfiguring skin disease that can leave them permanently scarred. As the Seinfield episode would suggest, laypeople might seem to think unless you are saving lives, you are not a “real” doctor. So, I guess in a sense, melanomas make dermatologists “real” doctors (and let’s not forget squamous cell carcinomas and basal cell carcinomas can also kill you). I know in my practice over the last 30 years, I have found hundreds of melanomas. Even to this day, when I see a melanoma, I quietly give myself a high five. When you catch melanoma in time, you have changed a person’s life for the better, even if they may not realize it. At the same time, I am also grateful that I did not miss that melanoma. There is always a degree of stress when doing a “routine skin exam” there is nothing routine about melanoma or the potential for missing a melanoma.
Melanomas come in all different shapes and sizes. They are rarely the archetypal jet black, nodular mole-like growth, in which even a first-year medical student could make the diagnosis. Melanomas may appear elevated, they can be flat, they can be multicolored, and they do not have to have pigment. Some melanomas can persist for very long periods before being discovered, such as lentigo maligna melanoma. Others can grow rapidly and deadly in a few weeks. Melanomas can develop beneath the nails, and even in non-skin areas such as the eye, oral cavity, nasal sinuses, even rectally.
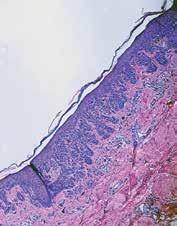

The best guidance for identifying melanomas for non-dermatologists is using the mnemonic ABCDEs of melanoma evaluation, Asymmetry of the lesion, Border irregularity, Color variation, Diameter greater than 6mm and Evolution. However, dermatologists rarely use the ABCDE guide, as most of us know by looking because of intuitive expertise. When a dermatologist observes a suspicious lesion, in our mind, it pops up, “that looks suspicious.” Intuitive expertise is ubiquitous throughout all specialties and comes with experience. The ER doc that walks into a patient room and immediately diagnoses congestive heart failure with only a glance is demonstrating intuitive expertise. Intuitive expertise can be confounding to medical students who need to look up everything online. Still, it is this intuitive expertise we all gain through training and experience that makes us “real” doctors.

Lucky Meisenheimer, M.D. is a board-certified dermatologist specializing in Mohs Surgery. He is the director of the Meisenheimer Clinic – Dermatology and Mohs Surgery. John Meisenheimer, VII is a medical student at USF.


Optimal sleep and wakefulness requires proper alignment between an individual’s intrinsic circadian rhythm and their desired sleep wake schedule. The word circadian comes from the Latin “circa” meaning “about” and “dian” meaning “day”. Our intrinsic circadian rhythm is controlled by an internal clock in the hypothalamus (suprachiasmatic nucleus). The hypothalamus receives signals from the retina that entrain the circadian rhythm to the light dark cycle. The circadian rhythm affects the timing of sleep. There is also a homeostatic sleep drive, which controls sleep intensity, and it is determined by how long an individual has been awake.
of shift rotation. It may also vary depending upon a patient’s diurnal preference. It appears to be less common in individuals who identify themselves as “night owls”. Individuals with shift work sleep disorder have been found to have higher rates of peptic ulcer disease as well as more sleepiness related motor vehicle accidents. Other consequences of this disorder include absenteeism from work, higher rates of depression and missed family and social activities as well as chronic fatigue and poor work performance. There have also been studies which link shift work sleep disorder to glucose intolerance as well as higher risk for alcohol and substance use. Sleep
Shift work sleep disorder is a recurrent or persistent mismatch between a person’s habitual sleep wake schedule and their endogenous circadian rhythm. Shift work sleep disorder can be associated with insomnia or excessive sleepiness (or both). The conventional time cues (zeitgeber = “time giver” in German) of sunlight and social activities are frequently out of phase with the altered sleep schedule in an individual with shift work sleep disorder. Many shift workers revert back to their traditional daytime schedule during non-work days. By definition, the course of shift work sleep disorder parallels the period of the shift work and remits with termination of shift work. An individual with shift work sleep disorder may use a large portion of their free time for recovery of sleep, which may have negative social consequences such as marital discord and impaired social relationships. Shift work sleep disorder tends to be more common after age 50. Between 5 and 8% of the population is exposed to night work on a regular or periodic basis.
Shift work sleep disorder is usually a clinical diagnosis. A formal sleep study (polysomnogram) may be helpful to exclude other etiologies of a patient’s symptoms. The sleep study should ideally be performed during the regular hours of sleep of the individual having the study. To diagnose shift work sleep disorder one must exclude any other medical or psychiatric conditions which could account for the symptoms. In addition, the symptoms should not meet criteria for any other sleep disorder which can produce insomnia or excessive daytime sleepiness (such as Jet-lag syndrome). Women appear to be slightly more prone to developing shift work sleep disorder. Interestingly, women tend to quit their shift work less often than men. The occurrence of shift work sleep disorder may vary depending upon the speed and direction
diaries can be helpful in assessing patients with shift work sleep disorder. Actigraphy can be useful as an adjunct to history, physical exam and sleep diary. Actigraphy recording should consist of at least three consecutive 24-hour periods. Circadian rhythm markers (such as core body temperature monitoring or timing of melatonin secretion) are more difficult and typically are not used in routine clinical settings.
Treatment for shift work sleep disorder can include exposure to bright light in the work place as well as administration of wake promoting agents during evening work hours. Other treatments include scheduled napping as well as hypnotic agents to improve daytime sleep. Maintaining a regular sleep wake schedule during both work and non-work days is also recommended (as well as minimizing light or noise in the bedroom and allowing sufficient time in bed for sleep during the daytime). Other recommendations include limiting light exposure by using dark sunglasses during the morning trip home from work. The timing of

light therapy is critical. The American Academy of Sleep Medicine recommends light exposure before the core temperature is reached in an individual with a morning/evening/night schedule (versus administrating light therapy after core temperature in an individual with a night/evening/morning schedule). Studies have utilized various light intensities from 2350 to 12,000 lux. Some but not all studies of bright light therapy have also restricted daytime light exposure. Different schedules of light exposure have also been used. Melatonin has both sleep promoting (hypnotic) and phase shifting properties. Melatonin (when given to night workers before their daytime sleep) may enhance daytime sleep and appears to have no effect on subsequent nighttime alertness. In a study published by Czeisler in The New England Journal of Medicine in 2005, modafinil resulted in decreased accidents/ near accidents during the commute home (versus placebo). Treatments for shift work sleep disorder can include modafinil (Provigil) as well as armodafinil (Nuvigil). These medications are nonamphetamine stimulants believed to act on the hypothalamus, although their exact mechanism of action is unknown.
Shifts can be permanent, fixed or rotating. Shift can rotate forward (clockwise) (from morning to evening to nighttime) or backward (from night to afternoon to early morning shift). Rotating shifts seem to cause more sleep difficulties than permanent shifts and counter clockwise rotation affects sleep wake activities more than clockwise rotation. The speed of rotation and the length of the shift may also impact an individual’s symptoms.
It appears that workers on permanent night shifts sleep one to four hours less than day workers and individuals on rotating shifts sleep about two hours less than day workers. There are several factors involved in this. Shift workers must try to sleep at a time when their circadian/wakefulness drive is exerting pressure on them to remain awake. The desire to spend time with family or take care of household or social obligations is also a factor. Environmental factors such as noise and light may also be obstacles to sleep quality for shift workers.
• Type of shifts (permanent, rotating).
• Duration of shifts.
• Speed of rotation (slow or fast).
• Direction of rotation (clockwise or counter clockwise).
• Social and family disruption.
• Exposure to natural or artificial light.
• Existing health problems.

• Age (over 50 is more adversely affected than younger individuals)
• Gender (female shift workers seem to have more difficulty coping with shift work than men).
In general, the circadian clock adjusts better to clockwise rotation because it is naturally easier to delay sleep to a later hour. Typically, longer shifts (such as 10-12 hours) cause more sleepiness than eight hour shifts. Women doing shift work tend to
get less sleep than men when they are not working because of their persistent family and social obligations. Overall, night and rotating shift workers comprise approximately 6% of all workers. About 1% of the working population in the United States is believed to suffer from shift work disorder. Increased awareness of this disorder should allow more individuals to receive proper diagnosis and therapy.
Daniel Layish, MD, graduated magna cum laude from Boston University Medical School in 1990. He then completed an Internal Medicine Residency at Barnes Hospital (Washington University) in St.Louis, Missouri and a Pulmonary/Critical Care/Sleep Medicine Fellowship at Duke University in Durham, North Carolina. Since 1997, he has been a member of the Central Florida Pulmonary Group in Orlando. He serves as Co-director of the Adult Cystic Fibrosis Program in Orlando. He may be contacted at 407841-1100 or by visiting www.cfpulmonary.com.

The neuromuscular clinic at Nemours Children’s located in beautiful Lake Nona, a thriving suburb of Orlando, is a specialty clinic supported and certified by the Muscular Dystrophy Association (MDA). Our clinic provides comprehensive medical care by a multi-disciplinary team for children who have neuromuscular disorders.
Pediatricians and other healthcare providers identify an abnormality on a child’s exam that may include low muscle tone, not meeting motor milestones, changes in physical function without cause, or regression in motor milestones, prompting them to refer the child to the neuromuscular clinic. The neuromuscular neurologist and advanced registered nurse practitioner meet the families and perform detailed evaluations to determine what diagnostic tools are needed. Common diagnostic measures used to identify neuromuscular conditions are electromyography (EMG) and nerve conduction studies (NCS) to determine the presence and extent of nerve damage, muscle ultrasound which is noninvasive and provides a dynamic way of evaluating the muscles in clinic, or muscle biopsy to have a more detailed look at the muscle fibers. Additional genetic testing is also performed to identify specific gene mutations.
Our neuromuscular care team is led by a pediatric neurologist and advanced registered nurse practitioner who specialize in neuromuscular conditions and aid in the diagnosis, treatment, and follow-up care for children with neuromuscular conditions. The team also consists of a physical and occupational therapist who assess patients’ strength, range of motion, coordination, mobility, self-care skills, and adaptive equipment needs to make recommendations for community therapies and assist in maximizing independent function. The therapists also complete all necessary performance testing required for medication authorizations. The registered dietitian nutritionist (RDN) provides evidence-based nutrition counseling to help children with neuromuscular disorders get the nutrients they need to provide favorable growth and nutrition balance for optimal health. Another important member of the team is the licensed clinical social worker who provides support for children and families to manage the emotional and financial challenges that come along with having or raising a child with a neuromuscular disorder. A neuromuscular program coordinator and neuromuscular RN support the team and families with coordinating care, prior authorizations, scheduling, insurance forms, and more.

Neuromuscular disorders are complex conditions and can affect a child’s physical, cognitive, and emotional development. At Nemours Children’s, we recognize that to provide comprehensive care for the children in our neuromuscular clinic, the entire team must collaborate and coordinate with healthcare professionals who have considerable expertise in a variety of areas. These often include cardiologists, pulmonologists, endocrinologists, physiatrists, gastroenterologists, psychologists, psychiatrists, geneticists, and orthopedists. Multidisciplinary care is essential, so our neuromuscular clinic works diligently with the other specialists to develop and provide a comprehensive treatment plan that ensures each child is receiving the best possible care.
There is no cure for most neuromuscular disorders, but there are a variety of treatments available today that can help improve a child’s quality of life. There are medications that can be prescribed to help improve muscle strength, reduce pain, and manage other symptoms of a neuromuscular disorder. Physical, occupational and speech therapies are often recommended to assist children with their physical and cognitive functions and increase their potential to interact with the environment around them. Nutrition counseling by an RDN can help children maintain a balance with nutrient intake to promote optimal growth and wellness. In some cases, surgery may be required to correct an orthopedic deformity and improve pain, posture and overall function.
In addition to traditional treatments, there is ongoing research to develop medications that can impact the root cause of some neuromuscular disorders. We are committed to conducting research and has been involved in several research trials, some of which have led to the development and FDA approval of treatments for spinal muscular atrophy and Duchenne muscular dystrophy. These treatments now offered to Nemours Children’s patients include exon skipping medications for children with Duchenne muscular dystrophy, gene transfer therapies to provide healthy copies of the SMN1 gene to children with spinal muscular atrophy (SMA), antisense oligonucleotides to reduce, restore, or modify protein expression helping produce more SMN protein in children with SMA, and immune modulating medications to help children with myasthenia gravis and chron-
ic inflammatory demyelinating polyneuropathy (CIDP) improve their muscle strength.
As one of only of only three pediatric MDA Care Centers in the State of Florida, our clinic supports patients from the entire Southeast region of United States (Florida, Alabama, Georgia, South Carolina) to Central and South America (Ecuador, Trinidad, Puerto Rico). With over 10 years of experience as a recognized MDA clinic, we have a long-established neuromuscular program. Our team has a deep understanding and efficient processes in place to diagnose, treat, and manage care for these rare plus complex diseases. The neuromuscular clinic at Nemours Children’s is also registered with the state of Florida as a newborn screening treatment center for SMA. This allows us to diagnose and treat babies quickly to minimize loss function that occurs quickly at an early age.
One of our patients was born in Florida and had a positive newborn screening for SMA. The family decided to pursue treatment
and care at Nemours Children’s Hospital, Florida in Orlando. The patient was started on Spinraza at 2 weeks of age then dosed with Zolgensma at 7 months after his titers decreased to allow treatment. Now at 9 months old, he continues to not have any observable symptoms of SMA with good vigorous movements of all his limbs, good strength throughout and normal reflexes without tongue fasciculations.
The family meets regularly with our neurologist in person, via telehealth, and over the phone. The patient completes regular functional testing with our neuromuscular therapists to track his milestones, strength, and progress. He is monitored by our dietitian to ensure appropriate weight gain and nutritional intake. Our RN is in regular contact with the family to ensure labs are completed appropriately and in a timely manner. The program coordinator has managed the prior authorizations for his expensive treatments. The social worker met with the family to offer support, asses for resource needs, provide health insurance benefit information, and offer emotional support.
To learn more about our clinic, visit Nemours.org/services/ neuromuscular-disorders.

What does your online reputation say about your practice? If you have a negative online reputation, you are missing out on new patients every day. Most medical practices now get the majority of their new patients through Google and other search engine queries, such as “Pediatrician in Orlando”. If your practice appears in these searches, the most common next step for a potential new patient would be to check out your reviews – what are other patients saying about your practice? It has been reported that 90% of consumers read online reviews before visiting a business and that online reviews influence 67% of purchasing decisions (Bright Local). For this reason, it is incredibly important to pay attention to the rating and reviews that your practice has on search engines, social media platforms, and local online business directories.
However, despite the importance of cultivating a positive online reputation, only 33% of businesses report actively collecting and asking for reviews (1). One great process to set in place at your practice is asking for patient reviews after each patient visit. It can be as simple as training your front office staff to ask each patient how their visit went while checking them out, and if they receive favorable feedback then they can ask the patient to please leave a review on Google or Facebook about their experience. If they receive negative feedback, this feedback should be taken very seriously, and management should be notified as soon as possible so that the issue can be mitigated before the patient decides to post a
negative review.
Setting up an automated text or email campaign that asks each patient for their feedback after their appointment is also a great way to improve your online reputation as well as to correct any issues that may be occurring at your practice. When you receive feedback from patients, you are then able to prompt them to leave a public review on Facebook, Google, Yelp, Healthgrades, or other applicable review platforms. However, you must be aware that legally, you are not allowed to only direct people with favorable feedback to leave reviews, which is known as review-gating – so if you are implementing an automated system like this, just make sure that you are aware of this limitation. There are online reputation management platforms which allow you to customize the messages that people see when they leave negative feedback as opposed to positive feedback, but both of those messages must still offer the option to leave a public review. However, if you create your message in such a way as to communicate to the patient who may leave negative feedback that you are working hard on resolving the issue and that someone will be in touch shortly, that may prevent them from leaving a public negative review.
When you receive a public review on Google, Facebook, or other review sites, make sure that you respond to it – either by thanking them for a good review or by asking them to contact you to discuss how you can improve their experience. Do not argue or try to defend yourself online – try to speak about it with them privately, fix the issue, and ask them to remove the review if possible. When you receive great reviews, make sure to cross-share them on your various social media platforms. You should also create a “Reviews” page on your website and add all great reviews to this page. This instantly adds credibility to your website.

Finally, make sure that when you look over the feedback and reviews that you receive, you are paying attention to what the negative reviews are saying – this is a great opportunity to identify current process challenges and improve your patients’ experience at your practice. Need help managing your practice’s online reputation? Visit www.lms-plus.com to see how Leading Marketing Solutions can help.
Sonda Eunus is the CEO of Leading Marketing Solutions, a Marketing Agency working with Medical Practices and other Businesses to help them identify the best marketing strategies for their business, create a strong online presence, and automate their marketing processes for a better return on their Marketing budget. Learn more about Leading Marketing Solutions at www.lms-plus.com.

NeuLine Health is a neurodiagnostic services provider that performs convenient, at-home Ambulatory EEG testing for patients with neurological-related medical conditions.
We are dedicated to serving qualified healthcare providers and their patients with best-in-class neurodiagnostic testing, nationwide.

Conditions that affect the nervous system are often complex and debilitating. Any patient with a neurological condition is most likely going to have other associated medical conditions and may face psychological, emotional and social challenges as well. As neurologists, we always work on that premise, because when it comes to the brain and nervous system, it’s unavoidable. These patients will reap the greatest benefit from subspecialty care in a multidisciplinary setting.
This is the basis of the structure of the Orlando Health Neuroscience Institute as a comprehensive neuroscience center offering high quality, accessible, true subspecialty care and fostering multidisciplinary collaboration. The focus is on treating patients holistically across the care spectrum, leveraging expertise in all areas we know a person will need help.
Comprehensive neuroscience care overlaps multiple domains including neurology, neuropsychology, neurosurgery, pain management, rehabilitation and behavioral health with numerous interrelated specialty centers and programs. Under neurology, centers and programs include epilepsy and seizure disorders, movement disorders, neuromuscular and peripheral nerve disorders, memory disorders, cognitive and behavioral neurology, multiple sclerosis and demyelinating disorders, headache and facial pain, stroke and vascular neurology and inpatient neurologic care. Within each of these specific areas, highly trained and experienced experts — many from the academic setting with subspecialty board certifications — leverage advanced technologies, collaboration within the multidisciplinary system and participation in research studies to ensure access to the highest level of complete care.
While all of the subspecialty centers and programs offer exceptional and innovative care, I have chosen a few that are certainly worth highlighting.

The Orlando Health Neuroscience Institute has a world-class group of epilepsy physicians, including epileptologists and neurosurgeons, working together to provide a level of epilepsy care as high as any in the nation. A patient is able to see a board-certified and fellowship-trained epileptologist and neurosurgeon on the same campus, where they can easily communicate and collaborate to create the best outcome for each individual patient. An expanding inpatient Epilepsy Monitoring Unit offers advanced evaluation with state-of-the-art testing to determine what is causing the epilepsy or seizures and where in the brain it is originating. That can then lead to a collaborative decision as to what the best surgical treatment may be among a variety of treatment options currently available. In addition to resective surgeries, alternative and less invasive surgical methods, including vagus nerve stimulation (VNS), deep brain stimulation (DBS), responsive neurostimulation (RNS) and laser interstitial thermal therapy (LITT), enable the team to coordinate the highest level of epilepsy surgical care available.
Florida has a high population of people afflicted by dementia, but there are not many places in the region where people can go for proper evaluation and vital resources. So, unfortunately, many people in our communities experience forgetfulness and memory loss but don’t get an actual diagnosis. What is the condition? Is it Alzheimer’s disease? Frontal temporal dementia? Vascular dementia? The Orlando Health Neuroscience Institute has a dedicated dementia and memory disorders center with specialty-trained neurologists and neuropsychologists who are top experts in their fields. They are first able to offer a high level of care in terms of diagnosis. And that is crucial, because without the correct diagnosis, proper treatment cannot be leveraged. In addition to medical diagnostics and treatment, dedicated social workers work hand in hand with our neurologists and behavioral and cognitive neurology specialists to assist patients and families with all their needs. Someone with confirmed Alzheimer’s disease has a very different path to navigate than someone with vascular dementia. We also address caregiver needs, helping guide them through medical decision-making as well as home safety, education and crisis intervention. This is a rapidly growing program with many different means to help these patients.
In neuroscience, there are some very rare diseases that can have extremely debilitating effects, even shortened lifespan. These rare diseases require true experts in the field. One such condition is amyotrophic lateral sclerosis, or ALS. Once called Lou Gehrig’s disease, this very rare condition causes muscles to stop working, and a person loses the ability to walk, eat, breathe. Our dedicated ALS program is led by a specialist with a vast amount of experience in the proper diagnosis and management of ALS. Muscular dystrophy also causes devastating muscle weakness and disability. Many patients diagnosed with muscular dystrophy are then told they must travel long distances to receive care, and that’s very difficult or impossible for many. Our muscular dystrophy program is something new for the community, and something that we see being able to reach and help a lot of people. Parkinson’s disease also falls into this same category. The ability to see a specialist, receive an accurate diagnosis, understand the prognosis and treatment options, and receive the best medical and surgical treatment for these conditions is something that is not possible outside of a comprehensive neuroscience center such as the Orlando Health Neuroscience Institute.
Continued on page 20
Orlando is on the verge of becoming one of the most advanced minimally invasive orthopedic surgery destinations in the world. The implications of this extend well-beyond highperforming athletes and will improve treatment and outcomes for anyone.
To understand the importance of this, it is probably a good idea to remind ourselves of how significant surgery is to any patient. Surgery is by its very nature traumatic to the human body. We are making incisions, removing matter, disrupting tissue, reattaching or replacing things, and then stitching it all back together. We do incredibly good things for our patients through surgery, but it is invasive. And patients must recover not only from what brought them to the doctor’s office, but also from the surgery itself.
So, if we can make that surgery less invasive, less traumatic, we will make our patients’ recoveries – and their lives – vastly better.
For years you’ve heard medical professionals talk about minimally invasive procedures and techniques. Arthroscopic camerabased surgery, for example, can be performed with a tool the width of a standard pencil or ball-point pen. As remarkable as that is, it still requires a patient to undergo general anesthesia.
But what if we are able to perform surgery with something even smaller? Instead of the tool being the width of a pencil, what if the tool is the width of the lead inside that pencil. That is about 2 millimeters, or the width of a 14-gauge needle. Besides being obviously less invasive, such surgery can be performed without general anesthesia; it can be done with a local anesthetic. That means less trauma, less pain and pain treatment, less risk of infection and other complications. It also means significantly less time in the hospital.
That is what is about to become reality at the Orlando Health Jewett Orthopedic Institute Downtown Campus later this summer when we open our nano-surgical suite. Once credentialing is complete, the Orlando Health Jewett Orthopedic Institute will become one of only four Centers of Excellence for orthopedic nano-surgery in the United States. While nano-surgery is available elsewhere, the Orlando Health Jewett Orthopedic Institute has specific Nano ArthrOscopy Procedural Suites within the ambulatory surgery center that are fully accredited to perform minimally invasive arthroscopic and endoscopic techniques.
Well, imagine that you have sustained an injury to your shoulder that requires surgery. You might drive to the downtown complex, and park in the garage and walk across a breezeway to the ambulatory surgery center. After checking in and

getting prepared, you will walk into the nano-suite, which is unlike any operating room you have ever seen before. For one thing, there are windows admitting natural light into the room, which we’ve tried to replicate throughout the facility. Natural light is good for people’s mental state; it makes everyone happier, and in my opinion is good for healing.
In the surgical suite you can either enjoy the view out the window or watch what the surgeon is doing on a video monitor if you wish. It’s a form of social medicine or social surgery because you can actually talk to the surgeon during the procedure.
When it’s done, you’ll be able to leave much as you would from a dentist’s office. Obviously, if it is surgery on one of the joints involving your leg or foot, you might not be able to walk on it right away without crutches, but your recovery time will be dramatically shortened.
This started out as a diagnostic tool. If a physician wanted to inspect the inside of a knee, for example, they could use the nano-camera to look for something like, say, loose cartilage instead of sending the patient for an MRI. Now, the technology has advanced to where we can use it not only to view and diagnose the problem, but also to treat it. This is the case for labral tears in the shoulder and meniscus tears in the knee.
One of the things I am especially excited about is that we are not only introducing this surgical option to our patients, but we will be helping to teach the next generation of surgeons through our fellowship and residency programs. And we will be participating in research to help continue the advancement of orthopedic surgery.
Now, it is important to note that this level of nano-surgery is not suitable for every situation. For example, the needle is not long enough to be used in treating hips. But it has many applications, especially when it comes to treating the shoulder, the elbow, the wrist, and the knee.
It is also important for doctors to help their patients understand that this level of treatment is not exclusive to highperforming athletes. Today, many people are active throughout their lives. Helping them to get back on the court, the driving range or whatever their choice of activity as soon as possible really has an impact on their quality of life. And if we can use technology to reduce the risks of complications and to deliver speedier and better outcomes, that’s a benefit to everyone.
Continued on page 20
Continued from page 19
Michael V. Jablonski, MD, is a board-certified orthopedic surgeon and the physician leader of Orlando Health Jewett Orthopedic Institute. He specializes in knee joint replacement, using Mako® Robotic Arm Assisted Surgery, as well as in sports medicine. Dr. Jablonski completed medical school and residency training at the University of Florida College of Medicine, followed by a fellowship with the renowned Dr. James Andrews at the American Sports Medicine Institute. He served as the chief medical officer for 2022 USA Special Olympics, an immensely rewarding experience that fostered a strong interest in advocating for inclusive, quality orthopedic care for people with intellectual disabilities. Dr. Jablonski grew up in Central Florida and has enjoyed practicing in the area for more than 20 years.
Continued from page 18

For these devastating conditions for which there are no known cures, we have a responsibility to mobilize every avenue for new therapies and research opportunities. Orlando Health is committed to participating in medical research as well as training and educating the next generation of neurologists. At the institute, we are expanding our research programs. Just one example is becoming a site for two national investigational studies for new multiple sclerosis therapies. These research protocols offer patients with many different neurological conditions treatment options outside what is conventionally available. New advances like this will further enhance care for an even broader range of patients throughout Central Florida and beyond.
Christian Rosado, MD, is a board-certified vascular neurologist and medical director of neurology with the Orlando Health Neuroscience Institute. Dr. Rosado works within a multidisciplinary team that includes specialists in neurology, neurosurgery, interventional pain management, rehabilitation and neuropsychology as well as neuroradiology, lung and sleep medicine, cardiology and oncology. This collaborative approach enables the institute to offer the most comprehensive, advanced treatment and management options to patients with neurological conditions. Dr. Rosado earned his medical degree from Indiana University in Indianapolis and completed all of his specialty training at the University of Florida in Gainesville, which included an internship in internal medicine followed by a neurology residency and a vascular neurology fellowship.


Florida MD is a monthly medical/business digital magazine for physicians..
Florida MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD.
It is hard to be aware of everything happening in the rapidly changing medical profession and doctors want to know more about new medical developments and technology, procedures, techniques, case studies, research, etc. in the different specialties. Especially when the information comes from a local physician specialist who they can call and discuss the column with or refer a patient. They also want to read about wealth management, financial issues, healthcare law, insurance issues and real estate opportunities. Again, they prefer it when that information comes from a local professional they can call and do business with. All advertisers have the opportunity to have a column or article related to their specialty or profession.
JANUARY – Digestive Disor ders
Diabetes
FEBRUARY – Car diology
Hear t Disease & Stroke
MARCH – Or thopaedics
Men’s Health
APRIL – Sur gery
Scoliosis
MAY – Women’s Health
Advances in Cosmetic Sur gery
JUNE – Aller gies
Pulmonar y & Sleep Disorders
JULY – Neurology / Neuroscience
Advances in Rehabilitation
AUGUST – Spor ts Medicine
Robotic Sur gery
SEPTEMBER – Pediatrics & Advances in NICUs
Autism
OCTOBER – Cancer
Dermatology
NOVEMBER – Urology

Relieve Symptoms of:
• Acne
• Allergies
• Asthma
• Cold & Flu
• Cystic Fibrosis
• Dermatitis
• Ear Infections

• Eczema
• Sinusitis
100% NATURAL TREATMENT

Kerri and Clay: “My son’s allergy medicines were causing terrible side effects. Now that we have been coming to The Salt Room we have been able to control his symptoms with salt therapy.”




Joseph Cannizzaro, MD: “I have been recommending The Salt Room for years. It has helped my patients with respiratory nuisances and skin problems, reducing symptoms while we address the root cause to improve their long-term quality of life.”
