

























SEASON’S










A massive congratulations to Dr. Lui on her new position as Doctors of BC President elect! To learn about the amazing work she’s done with PQI, check out this article! You can read the article about her appointment here.


Dr. Hwang was Health Quality BC’s Runner-Up for the Everyday Champion award. Click here for the full article. In addition, he has recently been appointed to Doctors of BC Board Director.
Dr. Goecke has recently been awarded Runner-Up for the Returning to Health and Wellness award for her Radioactive Breast Seeds for Cancer Surgery. about this major accomplishment.









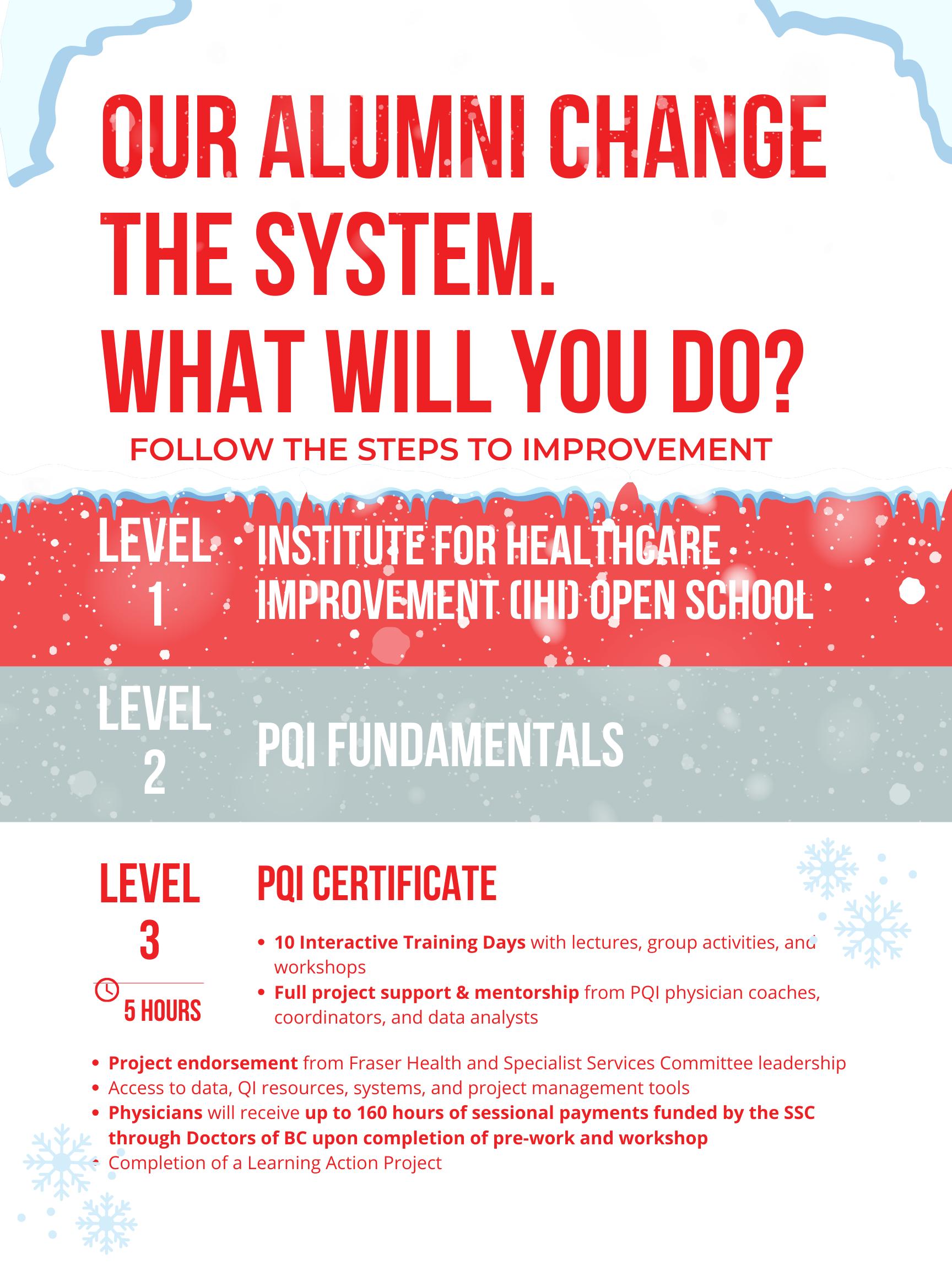
Our overarching goal is to continue to stimulate growth by cultivating capability and capacity for quality improvement, which means delivering top-tier education within Fraser Health.
Incorporate the new curriculum into the FH PQI program, enhancing our upcoming CPD application for accreditation by integrating topics such as equity, diversity, inclusion (EDI), and planetary health.
Prioritize exploring diverse methods and crafting a comprehensive strategy to incorporate these learning experiences, enabling our team to address the varied needs of our learners effectively.
The Fraser Health team has designed its activities for alumni and spread to align with the Complete Quality Impact (CQI) cycle. We aim to provide comprehensive project management, data, and coaching support to alumni and system projects. By ensuring these projects are executed with rigorous QI methodology, and that the appropriate partners in the healthcare ecosystem are made aware of their outcomes and successes, we believe we would see amplified impact and value.






For faculty, staff, and patient partners, we continue to provide learning and development activities through engagements including, but not limited to:
• train the trainer: Faculty can develop skills in content design and teaching methodologies.
• monthly cme sessions: Faculty enhance teaching and coaching skills across various topics.
• arecci certification: Expanding our faculty pool & staff for second opinion reviews, aiding PQI projects.
priorities and enhancing team unity and growth.
• leadership training: Staff encouraged to pursue FH courses on leadership, coaching, cultural safety, and workplace relationships.
• staff development budget: A $10,000 annual allocation for staff external learning opportuni ties.
• patient partners QI course enrollment or conference attendance; encouraged to complete our PQI training levels.






To highlight achievements in QI, we highly encourage physicians to seek out opportunities to publish, pres ent, and discuss their work wherever possible. The PQI team is dedicated to providing project support in developing and designing compelling project posters, manuscripts, and engaging presentations. Through these endeavours, we can effectively demonstrate the benefits of QI training and how the work aligns with the stra tegic priorities of the SSC, Shared Care Committees, (SCC), Fraser Health Authority, and the Ministry of Health.


Priorities for alumni and spread are as follows:
CQI Cycle: Opportunity Identification
Be intentional in building relationships with partners to identify system opportunities.
CQI Cycle: Project Proposal à Project Closure & Evaluation
Develop process and templates to implement the CQI project cycle
CQI Cycle: Communication & Publishing à Spread
Better demonstrate/report our project impact
Create a database to track alumni activities
Continue to offer monthly accredited CME events and advanced training workshops to PQI Alumni

















with the ongoing challenges related to the opioid crisis, we are seeing an increase in patients presenting to hospital with concerns related to substance use. There have been several services and steps taken to support harm reduction and clinical services focused on improving care of patients who struggle with addictions. At Burnaby Hospital, the Addiction Medicine Consult Team (AMCT) was established in mid-2021 with the aim of providing consultative care for inpatients. The AMCT is comprised of physicians from diverse specialties and offers consultative care for individuals with substance use concerns. While this service implementation has improved addiction medicine care within the hospital, initial environmental scans suggested gaps in care, highlighting opportunities for quality improvement.

In late 2022, sixty Burnaby Hospital staff were surveyed and we found that 41% reported not having proficient knowledge on relevant addiction medicine resources, despite 83% agreeing that learning more would be beneficial to their practice. Most notably, 55% did not know where to seek out this information. Altogether, this highlighted a need for improved accessibility, education, and information consolidation to better support our clinicians. Many of the patients seeking care at Burnaby Hospital live on both sides of boundary, and provider knowledge is a predictor for improved patient accessibility to outpatient services.


Thus, we sought out to improve provider knowledge in the most effective way possible.
In collaboration, Dr. Lingsa Jia (Department Head for the Burnaby AMCT) and Vanessa Kong (UBC medical student from UBC) spearheaded the creation of a website to consolidate community-based resources –www.BRSU.ca. This involved engagement with several hospital-based and community organization, including Fraser Health, the Burnaby Division of Family Practice, the local Mental Health Team, and the local MSA.




providers to potentially bridge the gap between in-hospital and out-patient care. To further support patient education, we crafted succinct summary handouts with the most important community services.
www.BRSU.ca went through multiple revisions with feedback and suggestions from Burnaby staff.
In 2022, an evaluation of our website revealed that 81% of surveyed providers accessed four or more substance use resources within just five minutes of navigating the site!




Contributed by Daniel Wong & Dr. Lingsa Jia
Also in 2022, a retrospective chart review was completed by Daniel Wong (UBC medical student) and Dr. Jia based on the first year of the AMCT’s service to better understand patient demographics and interventions made in hospital.

While it was reassuring to learn that 100% of patients with opioid use disorder were started or continued opioid agonist therapy in hospital, only 51% of eligible patients were given a take-home naloxone (THN) kit before discharge. In the context of the ongoing opioid crisis in BC and the harm reduction potential of this simple intervention, the AMCT aimed to improve this rate to at least 80% by July 2023 on wards 3B and 3D.
Interventions involved a multi-pronged approach first starting with the ward 3B, followed by 3D. Frontline nursing education was spearheaded by Adrienne Lutzke, a new nurse prescriber hired by the AMCT. Adrienne led at least 5 different education sessions for RNs and LPNs about when to offer THN kits to patients and how to counsel patients and their families about their use. To optimize and ensure adequate supply of kits on the wards, Daniel collaborated closely with the pharmacy department, including distribution co-

When reflecting on these projects, some les sons learned were:
• Accessibility and Convenience: A cen tralized hub ensures that information is easily accessible to a wide audience. Hospital staff and patients can access information with little time and effort.



• Consistency: Having a single source of information promotes consistency in the dissemination of guidelines, services, and educational materials that is up-to-date.
• Resource Optimization: By consolidating information, duplication of efforts is minimized. This promotes better resource utilization.
• Adaptability: The shift from the initial setback of the THN kit PPO to the successful M.A.R. sticky labels demonstrated that QI work requires the ability to quickly adapt and collaborate with frontline staff to see what works





detail is a nuanced endeavor in healthcare communication.
• Data Accuracy and Quality: Maintaining accurate information with resources is crucial and requires consistent upkeep to ensure users are accessing appropri- ate information.
• Distribution: Promoting use of the web- site is a current challenge, and we are currently identifying ways to integrate this into workflow. A tool cannot be useful if it is not used!
• Staffing Shortages: Creating change on wards that are short-staffed can be extremely challenging. Success of a QI project is therefore highly dependent on recognizing workload issues so that sus- tainable change can be made.






An Interview with Dr. Dave Konkin REGIONAL MEDICAL DIRECTOR | REGIONAL DEPARTMENT HEAD SURGERY



In general surgery/orthopedic surgery postoperative patients at Fraser Health acute care sites, decrease trama dol discharge prescriptions by 25%, decrease long-acting opioid prescriptions by 25%, and increase by 25% adher ence to quantity of 30 tablets or less, or 60 tablets in total knee arthroplasty, by June 2024.


What inspired you to take on this project?
I’ve been interested in quality improvement through my career. I probably did this on the side of my desk without any formal training. So finally I took the jump and I’m really happy I did. I think the one thing for me, to take this a little differently than some of the others is, yes I’m a frontline physician but I’m also an administrator and I wanted to see how PQI could help my job as an administrator as well.
What is one piece of advice you would give to an upcoming cohort member?
Have a plan of what you want to accomplish, so having a goal - having that thought process. And having a team; I think that’s so important! Having multiple members in a team to gage different perspectives and support, because it is a lot of work.
What are your goals and wishes for your QI project this upcoming year?
How has your project progressed so far?
I’m lucky because I have a team. I’ve linked up with the graduates of this program from pharmacy, so the opioid stewardship pharmacists. I have 2 of them on my team and that’s helpful to have someone who’s actually graduated and continues their work. I also have some NSQIP nurses helping.
My goal is to reach my aim! And I think that we can. I think we’re gonna make a difference, and the cool thing is with this QI project, yes we’ll get the start of it but we’re going to continue on; this is just one part of it. My goal will be to continue on. Would you say your goal would be to move into SQI afterwards?
Potentially. And because I have my hat in the regional thing I would be continuing this project anyway.



How has your project developed in a way that has surprised you?
How I can use data to support my arguments...I think that’s no. 1. No. 2 is how we all have a responsibility [opioid crisis]. We had one of our education sessions with the general surgeons across the region and there was a lot of reception so clearly people want to improve in this.
What part of the training process, so far, have you found to be the most valuable?
What are your next steps?
We’re just continuing with our PDSA cycles. The main focus right now is education. And then of course finding the data, so looking at the data to see what we have.
Anything to add?
The data! Which is funny, because that’s why I didn’t want to take this course. I was intimidated by the stats and data, but it turns out to be what I’ve liked the most
I would encourage all physicians to take this course. I think this is something committed, certificate training is a great course and the support is amazing. If there’s anyone that really wants to make a difference, this is the course to take.





Dr. Ross is a family physician in Coquitlam and New Westminster, British Columbia. Her clinical work includes Community Primary Care and Obstetrics and Surgical Assist in Car diovascular Surgery at Royal Columbian Hospital (RCH). She holds an MSc in pathology as well as an MD from the University of British Columbia. Dr. Ross teaches in the UBC Department of Medicine undergraduate and postgraduate programs.


In an interview with McMaster University, Dr. Ross describes her experience as a part of the first cohort of National Health Fellows with the Health Leadership Academy, emphasizing that collaboration is key. With healthcare managers, medical organizational leaders, Indigenous health leaders, innovative clinicians, patient advocates, and academics, we are able to envision how we achieve our goals of more accurately meeting the health needs of our community and patients’ in the future.

“Healthcare has an access problem that is in part linked to a productivity problem. We can no longer deliver the same level of intensity in healthcare to everyone as our population ages. Innovation is required.”
She adds that different perspectives contribute to a rich culture of learning.

“These aggregated data points could then be used to assess service level needs, staffing needs, effectiveness of specific treatments and many other quality improvements.”


Dr. Ross spent time in Palo Alto, and mentions that the problems that plague Canadian healthcare are prevalent on a global scale:
“No one has this right yet… inno vation in healthcare is really the elegant integration of many aspects of care: moving from cus tomization to personalization; standardizing and decentralizing records and data; sharing learnings and keeping a human in the loop.”

What are the disruptive forces happening in healthcare that we need to prepare for?
In no particular order:
Aging population demographics, both the increased medical complexity of aging patients and the increasing age of healthcare workers in general.

The rise of misinformation and distrust in the healthcare system and those who deliver care, including undermining substantial public health prevention processes such as immunization
Climate change, including the increasing dis ease burden of infectious and other diseases, poor air quality, lack of food, water, resources,
migration, widening social gaps, global violence.
• Advancing technology, particularly AI, and both the opportunity and substantial risk as we increase the use of tech and move further from our human-to-human care connections.
• Evolving models of healthcare delivery, largely driven by the aging work force and limited Health Human Resources (HHR) challenges.
• Funding for healthcare services at a time when

She says this is an “access” problem, and explains that AI and large language models may have a role to play in improvement, allowing for more time allotted to “human-to-human connection”, as computers han dle the data. She mentions that AI has its benefits and risks, however by fearing the risks we may leave behind opportunities to explore improvement oppor tunities “as they arrive”.






















Every year faculty retreat allows us the opportunity to connect in the same space and engage in conversations about QI, its future, and where it fits into the bigger healthcare picture.
Through workshopping, team-building exercises and hot spring networking, the QI Faculty discussed improvements to coaching, brainstorming for future training sessions, and a preview of the PQI 3-Year Proposal.























Happy New Year!
We’ve had immense success in PQI this year and we’d like to thank everyone involved for their hard work and dedication to the Physician Quality Improvement and Spreading Quality


We welcomed many new faculty, we saw the graduation of 3 successful cohorts, we celebrated the journal publications of some of our alumni, and according to the SSC PQI Survey we were the no. 1 PQI program out of 6 in the province.
We hope to continue this success into 2024, and we know we can’t do it without you all. We can’t wait to share all the excit ing things happening in the months to come.













