HEADlines
Spring- Summer 2024

Spring- Summer 2024
Greetings to all of our neurosurgery department constituents. This includes patients, caregivers, friends, donors, community members, alumni and colleagues. It does “take a village” to care for the many needs of our patients who are experiencing neurological conditions. It is our privilege and honor to be in a field that is so rapidly changing and growing. Research, new treatments, innovations – this newsletter is filled with examples of all of this and more. I am quite proud of our faculty and staff, as well as those in our neighboring departments of neurology, psychiatry, physiology, bioengineering, cell & developmental biology and more.
In this issue you will hear about a new community educational program that just launched. You’ll also hear about new faculty, research news, media coverage, and conferences involving our faculty – both locally and around the world. This is just a small slice of all that is happening in Neurosurgery and in Neurosciences in general on this campus, and beyond.
Although sometimes overwhelming, it’s truly an exciting time to be involved in this work. Join us on this journey and help make Colorado the healthiest brain state in the country! Contact us to find out how YOU can help. Email Tami Lack, our Director of Neurosurgery Department Strategic Planning. Tami.lack@cuanschutz.edu

Sincerely,
Kevin O. Lillehei, MD Chair, Department of NeurosurgeryOgsbury-Kindt
Professor of NeurosurgeryUniversity of Colorado

Presented by the Department of Neurosurgery University of Colorado School of Medicine and The Colorado Neurosurgical Society, and sponsored by the University of Colorado School of Medicine Office of Continuing Medical Education, another successful and international conference was held in Vail in February.
The Honored Guest Speaker was Dr. Allen K. Sills. Sills is the NFL’s Chief Medical Officer (CMO), a full-time position dedicated to advancing the health and safety of the sport of football. He became the NFL’s first CMO in March 2017, joining the league from Vanderbilt University Medical Center. As a neurosurgeon specializing in the treatment of athletes, Dr. Sills continues to serve at Vanderbilt as a Professor of Neurological Surgery, and he is also the Founder and former Co-Director of the Vanderbilt Sports Concussion Center.
As the NFL’s CMO, Dr. Sills works closely with team medical staffs across the league, the NFL Players Association and its advisors, and the many medical and scientific experts who comprise the NFL’s medical committees. He coordinates with these medical experts to lead the league’s efforts to make advances, on and off the field, to protect players from unnecessary risk through rule changes, evolution of equipment, and robust injury reduction plans.

Dr. Sills spearheaded the league’s Head Injury Reduction Plan—a three-pronged approach aiming to reduce the incidence of concussions—which has continued to deliver results since its implementation, resulting in increased reporting and lower numbers of injuries, while continuing efforts to remove head impacts from the game.
Dr. Sills is an active researcher, having published over 200 scientific articles and presentations, including over 40 in the last five years on a number of sports medicine topics including concussion, spine injuries, emergency care of athletes, lower extremity injuries and COVID issues in athletes. He has been a member of the Concussion in Sport Group, which publishes international standards regarding concussion in sport. Dr. Sills is also a fellow of the American Board of Neurological Surgery and the American College of Surgeons.
Dr. Sills and his wife Shawne have lived in Franklin, Tennessee since 2009 and have four children and nine grandchildren. His hobbies include trail running, cycling, fly fishing, skiing, and kayaking.
Neurosurgery in the Rockies is a truly international endeavor! In addition to the invited guest speaker, and local neurosurgeons from across Colorado, we had many speakers from all over the world. These included: Ladislau Albert, MD from Texas; Das Kaushik, MD from New York; Colin Gold, MD from Iowa; Costas Hadjipanayis, MD, PhD from Pennsylvania; David Langer, MD from New York; Mark Luciano, MD from Maryland; Mick Perez-Cruet, MD from Michigan; Yasin Temel, MD from The Netherlands; Nikolay Velinov, MD from Bulgaria; Shelly Timmons, MD from Indiana; and Kevin Foley, MD from Tennessee

Many thanks to the meeting director, D. Ryan Ormond, MD, PhD and to the Scientific Committee: Peter Lennarson, MD – Chair, Ernest Braxton, MD, and Richard Hughes, MD

Under the direction of Dr. Kevin Lillehei, Chair of the Department of Neurosurgery, a virtual community “mini-medical-school” style course was launched in late April. It was a tremendous success, with over 280 registrants, including University Trustees, community members, patients, caregivers and colleagues. Faculty from several departments have participated in a wide variety of “basic brain” concepts and issues. The course was set up via zoom, every Tuesday evening for six weeks. This course is an effort to bring basic brain education to the public, to inform constituents about the Neuroscience Innovation Initiative, and to bring together likeminded individuals across the state that are interested in the Neurosciences. IF YOU MISSED THIS ONE, WE HOPE TO CREATE ANOTHER
Topics have included basic brain anatomy, stroke, aneurysm, Traumatic Brain Injury, Neuro oncology, neurodegenerative disorders (including Alzheimer’s Disease), an Introduction to Movement Disorders and Neural engineering, and a session on Psychiatry and Substance Abuse Science. Many thanks to the many faculty from across several departments who have contributed!

The Department of Neurosurgery has had a long-standing mission, to help develop neurosurgical care in Tanzania. This mission started 15 years ago with Dr. Kevin Lillehei’s initial involvement in a group called Madaktari Africa (Madaktari meaning doctor in Swahili). The premise of this group was not just to come in and perform surgery, but to teach and educate those individuals in the country, so they have the tools to perform these interventions themselves. Starting about five years ago, we began a partnership with Muhimbili Orthopedic Institute (MOI), in Dar Es Salaam, the center which employs 13 of the 20 neurosurgeons in the country. Over time this relationship has blossomed, with the development of shared educational programs, physician exchanges, and help with the formation of a formal Neurosurgery residency program at MOI. The meeting, a joint effort by the neurosurgical community at MOI, and the University of Colorado, occurred in February and was a huge success. The educational program developed by Dr. Ryan Ormond (Colorado) and Dr. Nicephorus Rutabasibwa (MOI) covered many broad topics and breakout sessions included several live operative cases. This year the educational program curriculum expanded to include neuro critical care, pediatric neurosurgery, and vascular neurosurgery. Along with the faculty at MOI, the University of Colorado brought along 15 members of our NeuroOncology team, representing both Children’s hospital and the University of Colorado Hospital.
Muhimbili Orthopedic Institute, Dar Es Salaam, Tanzania
Marie Lenart is originally from Seymour, India, is a Physician Assistant, and is now working with our Neurosurgical Spine program. She loves her coworkers and enjoys reading and hiking.

Edin Nevzati, MD was born in Kosovo before moving with his family to Switzerland in the early ‘90s. He completed medical school in Zurich, Switzerland, and trained in neurosurgery at the busy centers of Aarau and Lucerne. After achieving board certification in neurosurgery, he pursued two fellowships with our Department here at Anschutz, including one year in neuro oncology and another in complex spine. Edin is an associate professor at the University of Basel, Switzerland, as well as CU Anschutz. He joined the Denver Health neurosurgery team in early March. Edin is married and has three children, they enjoy hiking and skiing together.

Nancy Lennarson is an Instructor and Nurse Practitioner in our department, working mostly with spine patients. She is the wife of Peter Lennarson, one of our neurosurgeons and an Associate Professor. Together, they live in Arvada and have five boys! Nancy enjoys fitness, the outdoors, and helping others. She also plays violin/fiddle and has played in Europe for USO shows!

Hannah Miller is originally from St. Louis, MO and is an instructor and nurse practitioner with the pediatric neurosurgery team at Children’s Hospital Colorado. She likes the variety of work there. She says, “every day is different so I’m constantly learning.” She is grateful for an amazing and supportive team and, in her spare time, she likes to enjoy all the outdoor activities Colorado has to offer with her husband and dog, Wally

Cristin Welle, PhD, Vice Chair of Research in the Department of Neurosurgery has been getting a great deal of press with her work on Vagus Nerve Stimulation (VNS), which is now a treatment for epilepsy, depression and stroke. Dr. Welle and her colleagues are finding that VNS activates the cholinergic system, which is important for learning and plasticity. In addition, they are demonstrating that VNS improves learning in complex motor behavior. See her interviews on CNN and Fox news here: https://video.snapstream.net/Play/ haSLcm1wAFv59uLHt50RX?accessToken=c7b1n5afy6any https://www.livenowfox.com/video/1430118
Congratulations to Xiaoli Yu, PhD for her novel blood based screening method for the detection of specific types of Multiple Sclerosis. MS is a chronic inflammatory disease of the Central Nervous System and the most common neurological disability in younger adults, with nearly 1 million people being affected in the US. Diagnosing MS early is crucial to facilitating proper interventions and treatments. Current laboratory diagnostics rely entirely on elevated total lgG levels and the presence of oligoclonal bands in spinal fluid obtained through a lumbar puncture.
The blood based screening tool developed by Dr. Yu and her colleagues detects higher levels of serum lgG1 and lgG3 antibody subclasses in MS. It mitigates the need for invasive spinal taps and adds the ability to reliably distinguish secondary progressive MS from relapse remitting MS/primary progressive MS, a function not possible using total lgG levels. This innovation is also more cost effective than current standards and allows the monitoring of disease-modifying therapies.




Michael Graner, PhD co-chaired and organized the SelectBIO Conference; Extracellular Vesicles & Nanoparticles, along with the Space Summit 2024 – both held in April, in Miami Florida. Dr. Graner was also able to secure “Bridge Funding” from the School of Medicine Dean’s Office. Congrats!
Dr. Graner, along with many colleagues, has recently published Specific Binding of Alzheimer’s AßPeptides to Extracellular Vesicles.
Alzheimer’s disease (AD) is the fifth leading cause of death among adults aged 65 and older, yet the onset and progression of the disease is poorly understood. What is known is that the presence of amyloid, particularly polymerized Aß42, defines when people are on the AD continuum.
Congratulations to Robert Kowalski, MD and colleagues working with the Mobile Stroke Units. They just received the American Heart Association’s Transformational Project Award ($300K over 3 years), effective July 1st, bringing recent program support for ultra-early acute stroke biomarkers research to nearly $1M. In addition, Dr. Kowalski was awarded funding with the Chancellor’s Discovery Innovation Fund for a similar project in early stroke detection.

John Thompson, PhD and a colleague, Drew Kern (MD –Department of Neurology) have secured funding from Medtronic for the Implementation of adaptive deep brain stimulation to offset subthalamic dysregulation during exercise and reduce exertion in Parkinson’s disease.
Dr. Lotta Granholm-Bentley received funding from the Jerome Lejeune Foundation for her work with the International Brain Bank for Down Syndrome-related Alzheimer’s Disease.
She presented “New technology for neurodegenerative disorders using machine learning, AI, and spatial transcriptomics” at the American Society for Neural Therapy and Repair (ASNTR) meeting in Clearwater Florida in April. She is also the Chair of that organization.
She also presented “Long-term effects of glial cell-line derived neurotrophic factor (GDNF) in patients with Parkinson’s disease” at a poster session of The Alzheimer’s and Parkinson’s Diseases Conference (AD/PD™) in Lisbon, Portugal in March
Lastly , she has become Chair of the Neuropathology Work group, Trisomy 21 Research Society (an international society with 30+ member countries) and she has been Nominated as President, T21 RS (election ongoing).
In addition to her publications listed at the end of this section, she also has had two more big publications. Congrats!
Iban Aldecoa, Isabel Barroeta, Steven Carroll, Juan Fortea, Anah Gilmore, Stephen D. Ginsberg, Samuel J. Guzman, Eric D. Hamlett, Elizabeth Head, Sylvia E. Perez, Huntington Potter, Laura Molina-Porcel, Ruma Raha-Chowdhury, Thomas Wisniewski, William H. Young, Shahid Zaman, Sujay Ghosh1 Elliott J. Mufson, and Ann-Charlotte Granholm The Down Syndrome Biobank Consortium: A perspective. Alzheimers Dement. 2024 Mar;20(3):2262-2272. doi: 10.1002/alz.13692. Epub 2024 Jan 25. PMID: 38270275; PMCID: PMC10984425. Impact factor: 16.6.
Ann-Charlotte Granholm, Elisabet Englund, Anah Gilmore, Elizabeth Head, William H. Yong, Sylvia E. Perez, Samuel J. Guzman, Eric D. Hamlett, and Elliott J. Mufson. Title: Neuropathological Findings in Down syndrome, Alzheimer’s disease and control patients with and without SARS-CoV-2: Preliminary Findings. Accepted for publication, Acta Neuropathologica. Impact factor: 12.7
Colvett I, Gilmore A, Guzman S, Ledreux A, Quintero JE, Ginjupally DR, Gurwell JA, Slevin JT, Guduru Z, Gerhardt GA, van Horne CG, Granholm AC. Recipient Reaction and Composition of Autologous Sural Nerve Tissue Grafts into the Human Brain. J Clin Med. 2023 Sep 22;12(19):6121. doi: 10.3390/jcm12196121. PMID: 37834764; PMCID: PMC10573749. Link: https://pubmed.ncbi.nlm.nih.gov/37834764/
Zhou W, Graner M, Beseler C, Domashevich T, Selva S, Webster G, Ledreux A, Zizzo Z, Lundt M, Alvarez E, Yu X. Plasma IgG aggregates as biomarkers for multiple sclerosis. Clin Immunol. 2023 Oct 8;256:109801. doi: 10.1016/j.clim.2023.109801. Epub ahead of print. PMID: 37816415. Link: https://pubmed.ncbi.nlm.nih. gov/37816415/
Aldecoa I, Barroeta I, Carroll SL, Fortea J, Gilmore A, Ginsberg SD, Guzman SJ, Hamlett ED, Head E, Perez SE, Potter H, Molina-Porcel L, Raha-Chowdhury R, Wisniewski T, Yong WH, Zaman S, Ghosh S, Mufson EJ, Granholm AC. Down Syndrome Biobank Consortium: A perspective. Alzheimers Dement. 2024 Jan 25. doi: 10.1002/alz.13692. Epub ahead of print. PMID: 38270275. Link: https://pubmed.ncbi.nlm.nih.gov/38270275/
Johnson KA; Dosenback NU; Gordon EM; Welle CG; Wilkins KB; Bronte-Stewart HM; Voon V; Morishita T; et. al. Proceedings of the 11th Annual Deep Brain Stimulation Tank: Pushing the Forefront of Neuromodulation with Functional Network Mapping, Biomarkers for Adaptive DBS, Bioethical Dilemmas, AI-Guided Neuromodulation and Translational Advancements. Frontiers. 05Feb2024. doi: 10.3389/fnhum.2024.1320806 Link: https://www. frontiersin.org/articles/10.3389/fnhum.2024.1320806/full
Granholm A-C, Hamlett ED. The Role of Tau Pathology in Alzheimer’s Disease and Down Syndrome. Journal of Clinical Medicine. 2024; 13(5):1338. LINK: https://doi.org/10.3390/jcm13051338
Coughlan C, Lindenberger J, Jacot JG, Johnson NR, Anton P, Bevers S, Welty R, Graner MW, Potter H. Specific Binding of Alzheimer’s Aβ Peptides to Extracellular Vesicles. International Journal of Molecular Sciences. 2024; 25(7):3703. https://doi.org/10.3390/ijms25073703 LINK: https://www.mdpi.com/1422-0067/25/7/3703

Congratulations to Dr. Allyson Alexander for her NIH K08 Grant, “Getting Excited about Cortical Malformations: Discovering the Mechanisms Leading to Seizure-prone Neurons in Malformations of Cortical Development. The National Institutes of Health provide K08 awards as career development opportunities. Like most NIH grants, they are very difficult to obtain, so we are especially proud of Dr. Alexander!
Dr. Alexander was also featured on the front page of the Denver Post for her work with a special epilepsy patient. Kennady, now 19 and a senior at Columbine High School has a particularly difficult to treat form of Epilepsy, called Lennox-Gaustaut Syndrome, in which she seizes multiple times per day, some for as long as 20 minutes. This has left Kennady with several impairments, including vision, motor and intellectual. Because this syndrome is so resistant to treatment and medications don’t help, Kennady is now the youngest person in Colorado to receive deep brain stimulation (DBS). “Because the seizures aren’t coming from just one part of the brain, we placed the electrodes in a sort of “relay station” that sends signals between the rest of the body and the brain,” said Dr. Alexander.
Dr. Mohammad Alshareef, our newest neurosurgeon at Children’s Hospital Colorado is studying the association of hydrocephalus and neuroinflammation. His proposed project evaluates how the complement immune system is activated and regulated following neonatal intraventricular hemorrhage (IVH). IVH is a devastating disease for neonates and leads to over 90% morbidity and mortality while having no viable medical or surgical interventions. Dr. Alshareef has found that complement system inhibition leads to reduced injury and lower hydrocephalus rates in an animal model. He is still seeking funding to further explore the mechanism behind complement’s involvement in IVH. He will also examine the CSF of his neonate patients from the Children’s Hospital Colorado to identify complement-related markers that may predict outcomes in these neonates. Dr. Alshareef hopes that the complement modulators and inhibitors he is exploring may be eventually used in clinical trials for the treatment of neonatal IVH.


Donson AM, Bertrand KC, Riemondy KA, Gao D, Zhuang Y, Sanford B, Norris GA, Chapman RJ, Fu R, Willard N, Griesinger AM, Ribeiro de Sousa G, Amani V, Grimaldo E, Hankinson TC, Booker F, Sill M, Grundy RG, Pajtler KW, Ellison DW, Foreman NK, Ritzmann TA. Significant increase of high-risk chromosome 1q gain and 6q loss at recurrence in posterior fossa group A ependymoma: A multicenter study. Neuro Oncol. 2023 Oct 3;25(10):18541867. doi: 10.1093/neuonc/noad096. PMID: 37246777; PMCID: PMC10547517. LINK: https://pubmed.ncbi.nlm. nih.gov/37246777/
Lee A, Le E, Kaoutzanis C, Yu J, French B, Alexander A, Mathes D, Khechoyan D, Wilkinson C. Evaluation of Complications After Pediatric Fronto-orbital Advancement Surgery: Review of National Billing Database. Plast Reconstr Surg Glob Open. 2023 Oct 18;11(10 Suppl):139-140. doi: 10.1097/01.GOX.0000992628.32134. dc. PMCID: PMC10566833. LINK: https://www.researchgate.net/publication/374823104_Evaluation_of_ Complications_After_Pediatric_Fronto-orbital_Advancement_Surgery_Review_of_National_Billing_Database
Grob ST, Miller KR, Sanford B, Donson AM, Jones K, Griesinger AM, Amani V, Foreman NK, Liu A, Handler M, Hankinson TC, Milgrom S, Levy JMM. Genetic predictors of neurocognitive outcomes in survivors of pediatric brain tumors. J Neurooncol. 2023 Oct;165(1):161-169. doi: 10.1007/s11060-023-04472-7. Epub 2023 Oct 25. PMID: 37878192; PMCID: PMC10638163. LINK: https://pubmed.ncbi.nlm.nih.gov/37878192/
Link to the full article!Coryell J, Singh R, Osterndorf A…Alexander A, …Perry S. Epilepsy surgery in children with genetic etiologies: A prospective evaluation of current practices and outcomes. Seizure Dec 2023. LINK https://doi.org/10.1016/j. seizure.2023.10.011
Hansen D, Shandley S, Olaya J, Hauptman J, Auguste K, Ostendorf AP, Depositario-Cabacar DF, Wong-Kisiel LC, Reddy SB, McCormack MJ, Gonzalez-Giraldo E, Sullivan J, Pradeep J, Singh RK, Romanowski EF, McNamara NA, Ciliberto MA, Tatachar P, Shrey DW, Karakas C, Karia S, Kheder A, Gedela S, Alexander A, Eschbach K, Bolton J, Marashly A, Wolf S, McGoldrick P, Nangia S, Grinspan Z, Coryell J, Samanta D, Armstrong D, Perry MS. A multicenter comparison of surgical techniques for corpus Callosotomy in pediatric drug-resistant epilepsy. Epilepsia. 2024 Feb;65(2):422-429. doi: 10.1111/epi.17853. Epub 2023 Dec 22. PMID: 38062633. LINK: https://pubmed. ncbi.nlm.nih.gov/38062633/
Griesinger AM, Calzadilla AJ, Grimaldo E, Donson AM, Amani V, Pierce AM, Steiner J, Kargar S, Serkova NJ, Bertrand KC, Wright KD, Vibhakar R, Hankinson T, Handler M, Lindsay HB, Foreman NK, Dorris K. Development of chromosome 1q+ specific treatment for highest risk pediatric posterior fossa ependymoma. Clin Cancer Res. 2024 Feb 9. doi: 10.1158/1078-0432.CCR-23-3156. Epub ahead of print. PMID: 38334950. LINK: https:// pubmed.ncbi.nlm.nih.gov/38334950/
Verhey LH, Kulkarni AV, Reeder RW, Riva-Cambrin J, Jensen H, Pollack IF, Rocque BG, Tamber MS, McDonald PJ, Krieger MD, Pindrik JA, Hauptman JS, Browd SR, Whitehead WE, Jackson EM, Wellons JC, Hankinson TC, Chu J, Limbrick DD, Strahle JM, Kestle JRW; Hydrocephalus Clinical Research Network. A re-evaluation of the Endoscopic Third Ventriculostomy Success Score: a Hydrocephalus Clinical Research Network study. J Neurosurg Pediatr. 2024 Feb 9:1-11. doi: 10.3171/2023.12.PEDS23401. Epub ahead of print. PMID: 38335514. LINK: https://pubmed.ncbi.nlm.nih.gov/38335514/
Prince EW, Apps JR, Jeang J, Chee K, Medlin S, Jackson EM, Dudley R, Limbrick D, Naftel R, Johnston J, Feldstein N, Prolo LM, Ginn K, Niazi T, Smith A, Kilburn L, Chern J, Leonard J, Lam S, Hersh DS, Gonzalez-Meljem JM, Amani V, Donson AM, Mitra SS, Bandohpadhayay P, Martinez-Barbera JP, Hankinson TC. Unraveling the Complexity of the Senescence-Associated Secretory Phenotype in Adamantinomatous Craniopharyngioma Using Multi-Modal Machine Learning Analysis. Neuro Oncol. 2024 Feb 9:noae015. doi: 10.1093/neuonc/noae015. Epub ahead of print. PMID: 38334125. LINK: https://pubmed.ncbi.nlm.nih.gov/38334125/
Kalter JA, Yang RA, Toland A, Milla S, Lund TC, Hankinson T, Dahl NA. IDH-mutant astrocytoma arising from a demyelinating plaque in a child with X-linked adrenoleukodystrophy. J Neuropathol Exp Neurol. 2024 Mar 20;83(4):289-292. doi: 10.1093/jnen/nlae021. PMID: 38456320; PMCID: PMC10951971. LNK: https://pubmed. ncbi.nlm.nih.gov/38456320/

Dr. Samy Youseff has been busy. This past fall he completed the 8th annual CU Skull base course, spoke at the International Federation of Neuroendoscopy meeting in Singapore, was an honored guest at the Korean Skull Base Society meeting in Seoul, Korea and served as a speaker and hands-on course faculty at the World Federation of Neurosurgery Meeting in Cape Town, South Africa.
Since then, he has spoken at the UIC Winter Forum in Steamboat Springs, Colorado and served as faculty and speaker at the North American Skull Base Society Meeting in Atlanta, Georgia.
More recently, he performed a master class in Endoscopic Endonasal and Keyhole Surgery for Brain, skull base and pituitary tumors with hands-on microdissection at a collaborative meeting between Pacific Neuroscience Institute & University of Colorado in Santa Monica, CA USA. He then traveled to Pozzilli, Italy for the IRCCS Neuromed – Neuroanatomy Lab “G. CANTORE”
PARCO TECNOLOGICO - VIA DELL’ELETTRONICA and then spoke at the World Congress for Endoscopic Surgery in Shangri-La Kuala Lumpur, Malaysia
Winston KR, Youssef SA. (2023). Convexity Approaches to the Cranial Vault. Plastic Neurosurgery. https://link. springer.com/chapter/10.1007/978-3-031-27872-3_12
Khanna O, Hogan E, Alvarez R, Youssef AS. How I do it: hearing preservation in large vestibular schwannomas using vestibular nerve fiber preservation technique. Acta Neurochir (Wien). 2024 Feb 26;166(1):105. doi: 10.1007/ s00701-024-05998-z. PMID: 38403779. LINK: https://pubmed.ncbi.nlm.nih.gov/38403779/
Kalmanson OA, Khanna O, Youssef S, Nassiri A. Modified Fisch A Approach for Resection of Recurrent Jugular Foramen Meningioma. J Neurol Surg B Skull Base 2024 Jan 85(S 01): S1-S398. Doi: 10.1055/s-044-1780447. LINK: https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0044-1780447


Congratulations to Brian Hoyt, Phd, one of our neuropsychologists who was recently published in “Deep Brain Stimulation.” Neuropalliative care (NPC) is a relatively new subspeciality of neurology. Recent studies have demonstrated the efficacy of NPC in Parkinson’s disease (PD). However, the implementation of NPC in deep brain stimulation (DBS) has yet to be addressed. Patients with PD being evaluated for and having undergone DBS potentially have unmet needs that may be best assessed and managed by neuropalliative neurologist. Specific areas include an in-depth psychosocial evaluation, exploration of patient and caregiver expectations, addressing caregiver needs, providing spiritual and marital support, and discussing advance directives. Read full article below.
Congratulations to Drs. Chris Domen and John Thompson, who were published recently as part of a larger group gathering evidence for more cannabis research. They found that the brief duration and strong placebo response limited their interpretation of the effects, but there was no benefit for patients trying supervised and specific doses and types of cannabinoid. In fact, their findings suggested that there may have been worsened cognition and sleep, and there were many mild adverse events. Longer duration high quality trials that monitor cannabinoid concentrations are essential and would require improved availability of research cannabinoid products in the United States. READ full article below

Campbell JM, Kundu B, Lee JN, Miranda M, Arain A, Taussky P, Grandhi R, Rolston JD. Evaluating the concordance of functional MRI-based language lateralization and Wada testing in epilepsy patients: A single-center analysis. Interv Neuroradiol. 2023 Oct;29(5):599-604. doi: 10.1177/15910199221121384. Epub 2022 Aug 17. PMID: 35979608; PMCID: PMC10549711. LINK: https://pubmed.ncbi.nlm.nih.gov/35979608/
Leib KE, Sciulli SA, Domen CH, Greher MR. 63 Examining TOPF Performance in a Neurodegenerative Population. Journal of the International Neuropsychological Society. 2023;29(s1):573-574. doi:10.1017/ S1355617723007348 LINK: https://www.cambridge.org/core/journals/journal-of-the-internationalneuropsychological-society/article/63-examining-topf-performance-in-a-neurodegenerative-population/ D51C7A701F3047E87862FD7F17C5CE70
Liu Y, Bainbridge J, Sillau S, Rajkovic S, Adkins M, Domen CH, Thompson JA, Seawalt T, Klawitter J, Sempio C, Chin G, Forman L, Fullard M, Hawkins T, Seeberger L, Newman H, Vu D, Leehey MA. Short-Term Cannabidiol with Δ-9-Tetrahydrocannabinol in Parkinson’s Disease: A Randomized Trial. Mov Disord. 2024 Mar 15. doi: 10.1002/ mds.29768. Epub ahead of print. PMID: 38487964. LINK: https://pubmed.ncbi.nlm.nih.gov/38487964/
Goldin CT, Vaughan CL, Hoyt B, Kern DS. Neuropalliative care in deep brain stimulation for Parkinson’s disease: Potential impactful areas of care. Deep Brain Stimulation. 2024 https://doi.org/10.1016/j.jdbs.2024.03.001 LINK: https://www.dbsjournal.com/article/S2949-6691(24)00003-4/fulltext
Dr. Domen Dr. Thompson
Dan Kramer, MD, Assistant Professor of Neurosurgery, continues to lead our brain-computer interface lab as he studies higher level cognition, movement and sensation. Having just received FDA approval, Dr. Kramer and his colleagues will be recording signals coming from the brain, and then interpreting them to control external effectors, like a cursor on a computer screen or a complicated robotic arm. They will be using something called a Utah Array, which is surgically implanted into the brain tissue of patients with paralysis to record movement and restore functions. It’s a technology that’s been successfully used with patients for 10+ years.
But, the CU Anschutz Lab has a couple of unique features that differ from other labs in the country. Dr. Kramer is working on somatosensory mechanisms. “In our lab, we can stimulate both primary sensory areas and higher-order sensory integration areas. We’re able to read the signals coming out of the brain, and we can also stimulate and send sensory information back into the brain. The idea is to restore sensation, for example, in paralyzed individuals with spinal cord injury or ALS.”
“Another thing that’s unique to this lab is that we’re using higher-level cognitive areas. Most of the BCI programs in the country do motor cortex, which is basically the final stop between the movement you want to do and sending the plan down through the spinal cord to the muscles. We’re working with higher-level cognition, which is closer to conscious thought. It’s helping us understand motor planning and how people make decisions about things to do,” Dr. Kramer stated in a recent interview.
To read the entire article, click here: Link: https://news.cuanschutz.edu/news-stories/cu-anschutz-lab-works-to-restore-paralyzed-patients-senses
Baker S, Fenstermacher E, Davis R, Kern D, Thompson JA, Feslen G, Baumgartner AJ. Ethical considerations in closed loop deep brain stimulation. Deep Brain Stimulation. Oct 2023. doi.org/10.1016/j.jdbs.2023.11.001 LINK: https://www.sciencedirect.com/journal/deep-brain-stimulation/vol/3/suppl/C
Duffy KA, Fenstermacher E, Thompson JA, Tanabe J, Patel M, Ojemann S, Davis RA. Case report: clinical efficacy of deep brain stimulation contacts corresponds to local filed potential signals in a patient with obsessive compulsive disorder. Front Psych. Oct 2023. doi: 10.3389/fpsyt.2023.1279972 LINK: https:// pubmed.ncbi.nlm.nih.gov/38076699/
Carver, K., Saltoun, K., Christensen, E. Abosch A, Zylberberg J, Thompson JA. Towards automated sleep-stage classification for adaptive deep brain stimulation targeting sleep in patients with Parkinson’s disease. Commun Eng 2, 95 (2023). LINK: https://doi.org/10.1038/s44172-023-00150-8
Chee K, Hirt L, Mendlen M, Machnik J, Razmara A, Bayman E, Thompson JA, Kramer DR. Brain Shift during Staged Deep Brain Stimulation for Movement Disorders. Stereotact Funct Neurosurg. 2024 Jan 29:110. doi: 10.1159/000535197. Epub ahead of print. PMID: 38286119. LINK: https://pubmed.ncbi.nlm.nih. gov/38286119/
Thompson JA, Baker S, Radcliffe E, Kramer D, Ojemann S, Case M, Zarns C, Holt-Becker A, Raike R, Baumgarner A, Kern D. Towards an objective, standardized beta frequency peak detection algorithm to inform adaptive deep brain stimulation programming in Parkinson’s disease 2024/02/27 DO - 10.21203/ rs.3.rs-3994762/v1 LINK: https://assets.researchsquare.com/files/rs-3994762/v1/33c3b77a-33cf-49f8-959fb34d9a550509.pdf?c=1711131371

Jan Lea Sherrod was born three minutes after her identical twin, Lucretia Anne Sherrod, on April 11, 1960. They had a wonderful childhood and were very close, as many identical twins are. Although Denver natives, they spent five of their younger years with their family in an isolated Indian Village in Manitoba, Canada. This formed their dual love of nature, the outdoors, wildlife, hiking, native culture and more.
They both attended Colorado State University in Ft. Collins, where Jan became a veterinarian and married “the love of her life,” Dr. Jerry Mossberg, also a Veterinarian. They worked together on Jerry’s family farm in Greeley while each participated in an active veterinarian practice. Lucretia’s field was the study of soil science. She worked for the Agricultural Research Service of the USDA and did lab work and some field work, which both fit her passions. She called this her “dream job” and, in fact, she invented a method to analyze inorganic carbon in soil samples which is now used worldwide.
Both women enjoyed their respective lives in northern Colorado and spent lots of time together with their combined families until, in 2019, Jan unexpectedly lost her husband to a sudden heart attack and became a young widow at the age of 59. As always, Lucretia was there to support her. But, unfortunately, just two short years later (in May of 2021), Lucretia was diagnosed with a malignant brain tumor (glioblastoma). With their chosen fields and scientific backgrounds, both women knew what was probably to come. Lucretia passed away on May 8, 2022 –almost exactly one year after her diagnosis. She was 62 years old.
Still grieving her husband, and now her twin sister, Jan continues her veterinarian practice in Ft. Collins, runs and maintains the family farm in Greeley, and (per her sister’s wishes) has moved into her sister’s home in Ft. Collins which is now her “home base.”

Jan has been searching for the right way to honor her sister’s legacy, Lucretia’s love of science, and their combined desire to make sure others do not have to suffer the way Lucretia did. Jan found the “right fit” in early May, when she met some of the researchers in CU’s Neurosurgery Brain Tumor Research Program.
She was introduced to a newer type of research that is being done on this campus, thanks to the work of Neuro pathologist, Sam Guzman and our own researcher, Dr. Lotta Granholm. Jan chose to make her first gift as the “start up” of our newest gift fund for spatial transcriptomics. “More than anything, I just hope this kicks off new and more interest in this field of research. Glioblastomas have taken way too many lives.” On behalf of our department, and the entire CU Campus, we are grateful to Jan, Lucretia, and so many other donors who make our research possible. To find out how YOU can give to our new spatial transcriptomics fund, or any other area of research which interests you, please reach out to Tami Lack, Director of Neurosurgery Strategic Development. Tami.Lack@cuanschutz.edu

Congratulations to Dr. Sam Guzman, one of our colleagues in Neuropathology. He was just named “Pathologist of the Quarter” at CU Anschutz, for his work in spatial transcriptomics.
Lucretia and Jan Lucretia in the labSo what IS Spatial Transcriptomics? It’s a mouthful! And it is also a cutting-edge technique used in molecular biology to study gene expression patterns within tissues while preserving their spatial organization. Traditional transcriptomic techniques like RNA sequencing provide information about gene expression levels but lack spatial context. Spatial transcriptomics, on the other hand, allows researchers to map where different genes are expressed within tissue samples, providing insights into the spatial distribution of cellular functions and interactions. By integrating spatial information with gene expression data, researchers can better understand the complex biological processes occurring within tissues, such as cell differentiation, cell-cell communication, and tissue development.
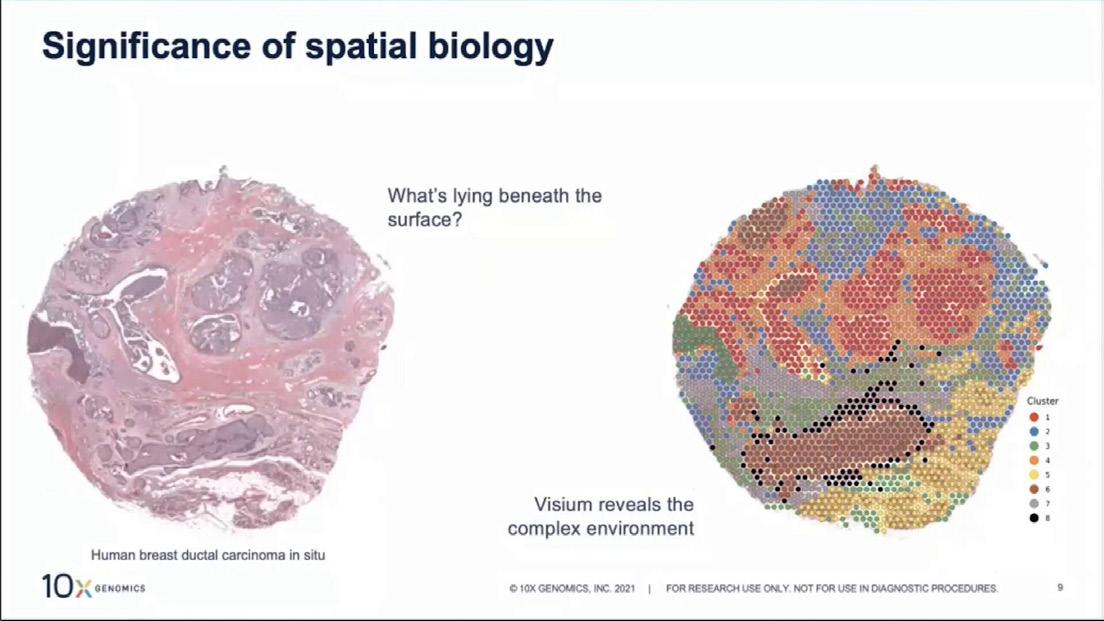
Spatial transcriptomics has applications in various fields, including developmental biology, neuroscience, cancer research, and immunology. It enables researchers to study tissue heterogeneity, identify cell types and their interactions within complex tissues, and gain insights into disease mechanisms and therapeutic targets.
Interested in Neurosurgery Research? Come and take a tour of one of our labs and see what’s happening in all of our many areas of research. We love to give tours. Contact Tami Lack for more information: Tami.Lack@cuanschutz.edu
Contreras-Zárate MJ, Alvarez-Eraso KLF, Jaramillo-Gómez JA, Littrell Z, Tsuji N, Ormond DR, Karam SD, Kabos P, Cittelly DM. Short-term topiramate treatment prevents radiation-induced cytotoxic edema in preclinical models of breast-cancer brain metastasis. Neuro Oncol. 2023 Oct 3;25(10):1802-1814. doi: 10.1093/neuonc/ noad070. PMID: 37053041; PMCID: PMC10547511.
Anuzis, A, Lillehei KO. Outcome Measures for Medical and Surgical Treatment of Prolactinomas. Is the Role of Surgery Underestimated? J Neurol Surg B Skull Base. Dec 2023. DOI: 10.1055/a-2212-0504
Malta TM, Sabedot TS, Morosini NS, Datta I, Garofano L, Vallentgoed WR, Varn FS, Aldape K, D’Angelo F, Bakas S, Barnholtz-Sloan JS, Gan HK, Hasanain M, Hau AC, Johnson KC, Cazacu S, deCarvalho AC, Khasraw M, Kocakavuk E, Kouwenhoven MCM, Migliozzi S, Niclou SP, Niers JM, Ormond DR, Paek SH, Reifenberger G, Sillevis Smitt PA, Smits M, Stead LF, van den Bent MJ, Van Meir EG, Walenkamp A, Weiss T, Weller M, Westerman BA, Ylstra B, Wesseling P, Lasorella A, French PJ, Poisson LM, Consortium TG, Verhaak RGW, Iavarone A, Noushmehr H. The epigenetic evolution of glioma is determined by the IDH1 mutation status and treatment regimen. Cancer Res. 2023 Dec 20. doi: 10.1158/0008-5472.CAN-23-2093. Epub ahead of print. PMID: 38117484.
Shrestha K, Kleinschmidt-DeMasters BK, Ormond DR. Diagnostic challenges of neurosarcoidosis in nonendemic areas. Front Neurol. 2024 Jan 11;14:1220635. doi: 10.3389/fneur.2023.1220635. PMID: 38274870; PMCID: PMC10809150.
Demetriou AN, Chow F, Craig DW, Webb MG, Ormond DR, Battiste J, Chakravarti A, Colman H, Villano JL, Schneider BP, Liu JKC, Churchman ML, Zada G, ORIEN Consortium, Profiling the molecular and clinical landscape of glioblastoma utilizing the ORIEN brain cancer database, Neuro-Oncology Advances, 2024;, vdae046, https:// doi.org/10.1093/noajnl/vdae046
Megan V. Ryan and Kevin O. Lillehei. Book Chapter: “Surgical Treatment of Low-Grade Gliomas” for the Encyclopedia of the Neurological Sciences, third edition. © 2024 Elsevier, Inc



Congratulations to several of our neurosurgical faculty and residents for their fascinating work involving COVID-19 and Moyamoya. L to R: Blake Wittenburg, Chief Resident; Jessa Hoffman, Chief Resident; Joshua Seinfeld, Vascular Neurosurgeon; Corbett Wilkinson, Pediatric Neurosurgeon.
Moyamoya disease is a rare neurological condition characterized by the narrowing or blockage of the blood vessels in the brain, particularly the arteries at the base of the brain. This narrowing restricts blood flow to the brain, increasing the risk of stroke or other neurological complications.
The term “moyamoya” is Japanese and means “puff of smoke,” describing the appearance of the small, collateral blood vessels that form as a compensatory mechanism in response to the blocked arteries.
So what happens when a 13 year old with Down Syndrome and Moyamoya also has COVID-19?
Drs. Wittenburg, Hoffman, Seinfeld and Wilkinson were recently published in Cureus, an online medical journal and collaborative platform. Their findings suggest that patients with moyamoya arteriopathy may be at risk for rapid progression of their moyamoya pathology when exposed to catalysts, including infection, such as COVID-19, and vascular injury, such as thrombectomy-induced injury. In these circumstances, high suspicion and close monitoring are essential for addressing ischemia related to the stenosis before permanent injury.
See full article, next page, under “publications”

Congratulations to Dr. David Case for securing funding for a fellowship in Neurovascular techniques from Medtronic.
Simpson JR, VanCoevering RJ, Jeppson K, Case D, Seinfeld J, Roark C, Poisson SN. Clinical Decision Support for Patients Presenting With Large Vessel Occlusion. The Neurohospitalist. Dec 2023;0(0). doi:10.1177/19418744231220699
Sethi A, Chee K, Chatain G, Wittenberg B, Seinfeld J, Milgrom S, Kavanagh B, Breeze R. Time-Dosed Stereotactic Radiosurgery for the Treatment of Cerebral Arteriovenous Malformations: An Early Institution Experience and Case Series. Neurosurgery Practice 4(4):e00060, December 2023. | DOI: 10.1227/ neuprac.0000000000000060
Hoffman JE, Morel B, Wittenberg B, Kumpe D, Seinfeld J, Folzenlogen Z, Case D, Neumann R, Cava L, Breeze R, Wiley, Roark C. Periprocedural management of ruptured blister aneurysms treated with pipeline flow diversion. Surg Neuro Intl. 08Mar2024 15:73. DOI: 10.25259/SNI_482_2023
Wittenberg B, Ryan M, Hoffman J, Bernard T, Seinfeld J, Wilkinson C. (March 20, 2024) Rapidly Progressive Contralateral Internal Carotid Artery Stenosis After COVID-19 Infection in a Down Syndrome Patient With Unilateral Moyamoya Arteriopathy. Cureus 16(3): e56575. doi:10.7759/cureus.56575
Nguyen, K. N., Freeman, L. M., Ung, T. H., Ojemann, S., & Grassia, F. (2024). Immunocompetent isolated cerebral mucormycosis presenting with obstructive hydrocephalus: illustrative case. Journal of Neurosurgery: Case Lessons, 7(13), CASE23672. https://doi.org/10.3171/CASE23672
MacLaren R, Farrar J, Stefanos SS, Cava L, Kiser T, Mueller S, Neumann RT, Reynolds P, Sherman D. 993: SERUM AND CSF CONCENTRATIONS OF MIDAZOLAM AND 1-HYDROXY-MIDAZOLAM IN NEUROSURGICAL PATIENTS WITH EVD. Critical Care Medicine 52(1):p S468, January 2024. | DOI: 10.1097/01. ccm.0001002136.61707.77
Kowalski, RG; Ledreux A; Violette J; Neumann R; Grotta JC; Ornelas D; Thompson JA; Monte A; Dylla L; Coughlan C; Yu, X; Graner M; Jones W. Circulating Interleukin-6 Levels Early During Active Stroke Estimate Time of Stroke Onset: Potential New Clinical Biomarker Tool From a Mobile Stroke Unit. Stroke 1Feb2024. doi/10.1161/str.55.suppl_1.106
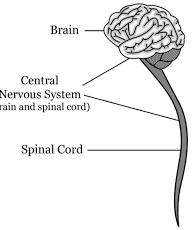
Although often left out of our general “brain discussions,” neurosurgery involves the diagnosis, treatment, and management of conditions affecting the entire nervous system, which includes the brain, spinal cord, and peripheral nerves. Since the spine is an integral part of the nervous system, neurosurgeons often specialize in treating spinal conditions such as herniated discs, spinal cord injuries, spinal tumors, and deformities like scoliosis. So, neurosurgeons must be able to perform surgeries on the spine as part of their practice.
Neurosurgeons treat a variety of conditions affecting the spine, including:
Herniated Discs: When the soft, gel-like center of a spinal disc pushes through a tear in the outer layer, it can compress nearby nerves, causing pain, numbness, or weakness. Neurosurgeons may perform procedures like discectomy or microdiscectomy to relieve pressure on the nerves.
Spinal Stenosis: This condition involves the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves. Neurosurgeons may perform decompression surgeries like laminectomy or laminoplasty to relieve pressure and alleviate symptoms.
Spinal Cord Injuries: Traumatic injuries to the spinal cord can result in paralysis or loss of sensation. Neurosurgeons may perform stabilization surgeries to prevent further damage and may also explore options for nerve repair or regeneration.
Spinal Tumors: Tumors can develop within the spinal cord or along the spinal column. Neurosurgeons may perform tumor removal surgeries to alleviate pressure on the spinal cord and nerves and to address any associated symptoms.
Spinal Deformities: Conditions like scoliosis (sideways curvature of the spine) or kyphosis (excessive forward rounding of the upper back) may require surgical correction by neurosurgeons, often in collaboration with orthopedic surgeons. PIC-spine deformity
Spinal Trauma: Fractures or dislocations of the vertebrae may require surgical intervention by neurosurgeons to stabilize the spine and prevent further damage to the spinal cord.

Degenerative Disc Disease: As discs in the spine wear down over time, they can cause pain and reduced mobility.
Neurosurgeons may offer procedures such as spinal fusion or artificial disc replacement to address these issues.
Spinal Infections: Infections of the spine, such as spinal epidural abscesses or discitis, may require surgical drainage or debridement to remove infected tissue and prevent further complications.
These are just some examples of the many conditions of the spine that neurosurgeons diagnose and treat. Each case is unique, and treatment plans are tailored to individual patient needs.
For a link to more information about our Neurosurgical Spine Program, click here: https:// medschool.cuanschutz.edu/neurosurgery/programs-of-excellence/spine-program





 Terri Baker, PA-C Instructor
Michelle DeGrave, PA-C Instructor Lawrence Cloutier, PA-C Instructor
Sonemala Phommatha, PA-C Senior Instructor
Ana Redington, PA-C Instructor
Marie Lenart, PA-C Instructor
Terri Baker, PA-C Instructor
Michelle DeGrave, PA-C Instructor Lawrence Cloutier, PA-C Instructor
Sonemala Phommatha, PA-C Senior Instructor
Ana Redington, PA-C Instructor
Marie Lenart, PA-C Instructor

Kerry Brega, MD Associate Professor Director, Residency Program

Jens-Peter Witt, MD
Associate Professor Director, Neurosurgical Spine Program










Chee K, Chatain GP, Kortz MW, Serva S, Shrestha K, Ung TH, Witt JP, Finn M. Neurologic outcomes for adult spinal cord ependymomas stratified by tumor location: a retrospective cohort study and 2-year outlook. Neurosurg Rev. 2023 Sep 29;46(1):258. doi: 10.1007/s10143-023-02166-2. PMID: 37773424; PMCID: PMC10542475.
Chatain, G, Schmidt MH, Finn M. (2023). Occipital Cervical Stabilization with Rod-Screw Systems. In Vieweg U, Grochulla F. (Eds.), Manual of Spine Surgery 2nd Ed (257-63). Springer. doi.org/10.1007/978-3-662-64062-3_38
Witt JP. (2023). Plastic Neurosurgical Approaches for Spinal Surgery. Plastic Neurosurgery. https://link.springer.com/ chapter/10.1007/978-3-031-27872-3_14
Lillehei KO (2023). Exposure of Peripheral Nerves. Plastic Neurosurgery. https://link.springer.com/ chapter/10.1007/978-3-031-27872-3_15
Chatain GP, Oldham A, Uribe J, Duhon B, Gardner MJ, Witt JP, Yerby S, Kelly BP. Biomechanics of sacroiliac joint fixation using lag screws: a cadaveric study. J Orthop Surg Res. 2023 Oct 28;18(1):807. doi: 10.1186/s13018-023-04311-5. PMID: 37898818; PMCID: PMC10613391.
Daniel Cavalcante, MD Assistant Professor Michael Finn, MD Associate Professor Mohammed Alshareef, MD Assistant Professor Pediatric Spine Program Daniel Craig, MD Assistant Professor Evan Winograd, MD Assistant Professor Muhammed Riaz, MD Assistant Professor Edin Nevzati, MD Associate Professor Peter Lennarson, MD Associate Professor Donny (Mark) Melton, MD Assistant Professor Angela Downes, MD Assistant Professor