OCULAR SURFACE DISEASE











ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Publishers Therese Dolan, Operations Director ESCRS
Barbara Calderwood, Divisional Director Engagement Associations and Communities MCI UK
Mark Wheeler, Finance Director MCI UK
Executive Editor
Stuart Hales
Editor-in-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Design Director
Kelsy McCarthy
Designer Jen Basel
Circulation Manager
Vanessa McCourt
Contributing Editors
Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales Roo Khan MCI UK Tel: +44 203 530 0100 email: roo.khan@mci-group.com Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes ISSN 1393-8983



Prevention is better than cure when it comes to dry eye disease (DED) and ocular surgery.
Dermot McGrath reports
Under-diagnosed, underestimated, and poorly understood, dry eye disease (DED) can negatively affect cataract and refractive surgery outcomes and lead to significant postoperative symptoms that can last anything from days to a lifetime for some unfortunate patients.
The stakes are high, yet screening for DED remains a hit-and-miss affair which too often leaves patients suffering a broad spectrum of complaints that can severely impact their quality of life and well-being.
The incidence and prevalence of DED after cataract surgery are widely underestimated, according to Béatrice CochenerLamard MD, PhD, Professor and Chairman of the ophthalmology department at the University Hospital of Brest, France.
“The rates in the scientific literature are anywhere between 10% to 34%, so it is quite common. There is a peak of severity that usually occurs around day seven postoperatively, but it may persist in some patients and become a chronic disease,” she said.
Dry eye symptoms are also very common in patients before and after refractive surgery. “Post-surgical tear dysfunction is the major cause of complaint after premium surgery including corneal refractive surgery,” said Jesús Merayo-Lloves MD, PhD, Director of the Instituto Universitario Fernández-Vega and Professor of Ophthalmology at the Universidad de Oviedo, Spain.
The prevalence of dry eye symptoms before undergoing LASIK is estimated to be between 38% and 75%, with contact lens intolerance due to dry eye a key reason why many patients pursue excimer laser ablation. Although post-LASIK dry eye usually peaks in the first few months after surgery and improves gradually thereafter, chronic dry eye disease has been reported to occur in anything from 20% to 40% of patients at least six months or longer after surgery.
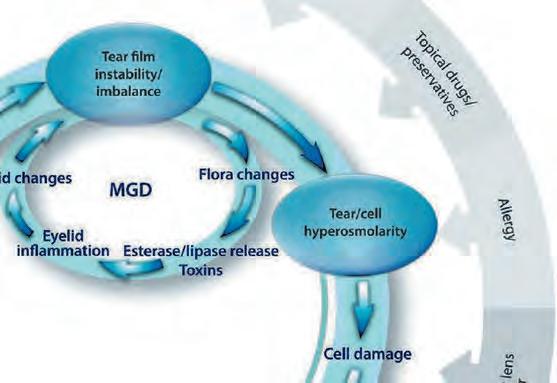
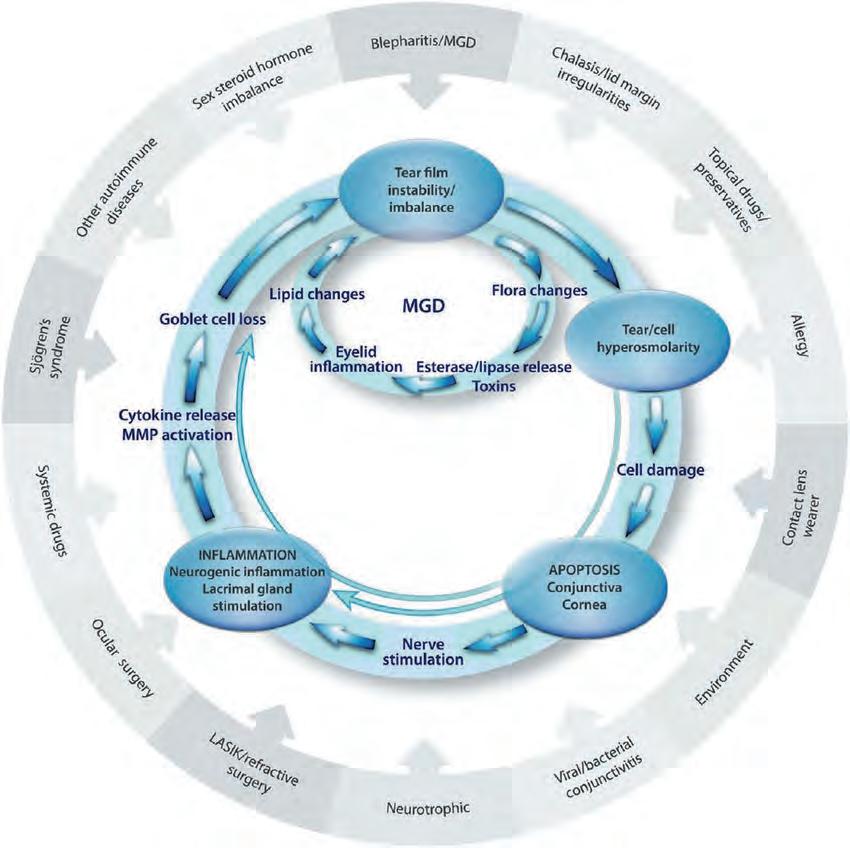
There are several reasons why DED tends to slip under clinicians’ radar so easily, according to Christophe Baudouin MD, PhD, Professor of Ophthalmology at Quinze-Vingts National Ophthalmology Hospital, Paris, France, and President of the newly formed European Dry Eye Society (EuDES).
“Dry eye is often not considered as sufficiently deserving of interest to many ophthalmologists. Compared to glaucoma, keratoconus, or other diseases, it seems far less severe. The attitude is ‘OK you have dry eye, you put in some drops, and it will be fine, end of problem,’” he told EuroTimes.
Another problem is patients with clinical signs of DED under slit-lamp examination are often asymptomatic.
“This is really a major problem. We regularly see patients with meibomian gland disease (MGD) or eyelid inflammation who never complain and tell us they are okay. However, these are the patients who will develop problems after surgery. Why are they asymptomatic despite the fact they have clinical signs? We really don’t know,” he said.
Marc Labetoulle MD, PhD, Université Paris-Saclay, Paris, France, believes many of these patients have active ocular surface disease that lies just below a threshold where the dry eye is not really apparent to them.
“However, this changes once they have cataract or refractive surgery, which takes the DED from below the threshold into something very real and tangible for the patient. They will then have the impression the dry eye problem is because of their surgery rather than the reality of the surgery bringing to light a pre-existing condition,” he said.
An impaired ocular surface will affect preoperative planning, biometry, and IOL calculation. The workup to identify patients with ocular surface problems before cataract or refractive surgery typically involves a combination of patient history (comorbidities, medications, and epidemiological factors), a dry eye questionnaire, and clinical evaluation with corneal staining and tear breakup (TBUT) assessment.
Other tests such as Schirmer, meniscometry, meibography, or point-of-care exams such as MMP-9 or TearLab’s Osmolarity System may also obtain more detailed information in the presence of an abnormal result after staining or TBUT.
In addition to the Ocular Surface Disease Index (OSDI), Prof Labetoulle said he regularly uses a questionnaire called Pentascore, developed in association with Prof Baudouin and other co-workers, to assess DED quickly.
“A lot of dry eye questionnaires are very detailed and not very practical for everyday clinical use. Pentascore uses five short questions to obtain a quick assessment of whether the patient has DED or not. We have validated its use in a recent study published in the British Journal of Ophthalmology, ” he said.
Prof Baudouin says careful discussion with the patient using targeted questions can raise potential red flags before any clinical examination.
“Ask the patient if they have a stinging sensation, foreign body sensation, or a burning sensation. If they do, look closely at the eyelid. If the patient has swollen, red, or crusted eyelids, be careful, as they probably have MGD,” he said.
Fluorescein staining can quickly reveal potential issues with the ocular surface to an experienced observer, Prof Baudouin said.
“Put one drop of fluorescein in the eye and look for three key factors in less than 10 seconds: does it stain the cornea, does it stain the conjunctiva, and how does the tear film react. We are not necessarily calculating the TBUT very precisely, but if you observe a TBUT of fewer than five seconds, be very careful, as the patient probably has DED,” he said.
If a patient has dry eye prior to surgery, surgeons need to establish whether it is mild, moderate, or severe and treat accordingly. A wide array of treatment options is available depending on the type of ocular surface problem present, including artificial tears, hyaluronic acid, punctal plugs, autologous serum, anti-inflammatory topical drugs, oral omega-3 supplements, lid hygiene measures, warm compresses, thermal pulsation, and meibomian gland probing. Several algorithms such as the TFOS DEWS II and CEDARS are available to help guide DED management for clinicians. Patients with uncontrolled or severe DED may need to be referred to a specialist and the cataract or refractive surgery deferred until the ocular surface has stabilised.
“If the DED is severe, the main problem is not the cataract or refractive error anymore,” Prof Labetoulle noted. “The priority is to optimise dry eye disease with all the tools in our arsenal. I will explain to the patient the severity of their DED and why it is important to improve the disease before proceeding to the surgery.”
There are several measures to take to reduce the risk of inducing or aggravating DED during cataract surgery. Avoiding femtosecond-laser-assisted cataract surgery (FLACS) might be advisable in patients identified preoperatively with DED.
“Some reports in the scientific literature [say] FLACS is more damaging to the ocular surface than traditional phacoemulsification,” Prof Baudouin said. “However, we have performed a lot of FLACS in our hospital without seeing any major complications, so I don’t think the technique is the major factor in causing DED. It’s just probably safer to avoid FLACS in confirmed DED patients.”
Surgeons should also take care with anaesthetic and mydriatic eye drops that are potentially toxic to the corneal epithelium. “I have seen a lot of improvement in the ocular surface of my patients since I switched to intracameral mydriasis with Mydrane (Thea Laboratories), which works to dilate the pupil and reduce the pain because it contains an anaesthetic as well,” Prof Labetoulle said.
Other tips include avoiding the use of aspirating speculums and limiting light exposure from the operating microscope by using appropriate filters and reducing surgical time.
For refractive surgery, Prof Merayo-Lloves stressed the importance of rigorous surgery to reduce trauma and epithelial defects.
“We need to watch for lack of lubrication, reduction in tear flow and inflammation, exposure to medication and anaesthetics, trauma to sensory nerves, and any deterioration in corneal sensitivity,” he said.
Some studies have also touted the benefits of using small incision lenticule extraction (SMILE) instead of LASIK to reduce possible postoperative dry eye problems.
“We conducted a study on this a few years ago, showing there was less dry eye after SMILE,” Prof Baudouin said. “However, even with less transection of the nerves, unfortunately some patients may still develop neuropathic pain with or without dry eye because the procedures are similar but not exactly the same. So, the complication may occur whatever the technique.”
In terms of postoperative care, surgeons advise using preservative-free artificial tears, exercising caution with non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotics, and ensuring rigorous follow-up to intervene rapidly in the event of DED symptoms.
“If we observe corneal damage or corneal stinging in a patient when using a NSAID, it is very important to stop it immediately because there is a risk that the toxicity can progress up to corneal melting,” Prof Baudouin warned. “It is often not necessary to use high-dose antibiotics or maintain treatment for a long period after the surgery, even if the cornea is not perfect.”
Another helpful measure in refractive surgery patients may be to consider using plasma rich in growth factor (PRGF) eye drops to promote regeneration of the ocular surface, Prof MerayoLloves said. “We have been using regenerative PRGF eye drops both before and after LASIK surgery with very good results over the past few years.”
During the last five years, Marc Labetoulle has acted as a consultant for Alcon, Allergan, Bausch & Lomb, DMG, Dompé, GSK, Horus, MSD, Novartis, Quantel Medical, Santen Pharmaceutical, Shire, SIFI, Théa Pharmaceuticals, and TopiVert Pharma.
Contact:
Christophe Baudouin MD, PhD: cbaudouin@15-20.fr
Béatrice Cochener-Lamard MD, PhD: beatrice.cochener@ophtalmologie-chu29.fr
Marc Labetoulle MD, PhD: marc.labetoulle@aphp.fr
Jesús Merayo-Lloves MD, PhD: merayo@fio.as
In an interview with Contributing Editor Dermot McGrath, Professor Christophe Baudouin, President of the European Dry Eye Society (EuDES), explains why he believes the time is right for a new society dedicated to dry eye disease.
I think there are a few good reasons why the timing is right. Some ophthalmic societies already deal to some extent with dry eye. There are several important regional dry eye societies such as the Japanese Dry Eye Society and the Asian Dry Eye Society, and internationally we have the Tear Film and Ocular Surface Society (TFOS). I was part of TFOS from the outset and worked with other European colleagues as part of the different dry eye workshops. That planted the idea perhaps there was a need and space for a society made up of European dry eye experts. The collaboration between our European colleagues was already very strong and we have been extremely active in dry eye research in recent years, publishing a number of consensus papers and literature reviews. So, it made sense to try to extend that collaboration further and bring these dynamic European research teams together in a more formal structure.
We have seen a lot of breakthrough research in many aspects of dry eye disease in the past few years, including inflammation, corneal nerves, wound healing, neuropathic pain, and many others. Our scientific research in the pathophysiology of the disease has advanced considerably and focused a lot of interest in the field of dry eye. One of our key goals will be to share this cutting-edge scientific knowledge and practical skills with other European experts, as well as anyone interested in dry eye disease. We already had an excellent programme for the first EuDES Congress in June and plan on building on this success for our future meetings.
Another goal will be to foster national societies. I hope the existence of a European Dry Eye Society will serve as a catalyst for experts to form their own national groups. The advantage is that the experts are well-identified country by country and can also collaborate and participate at a European level. The European Glaucoma Society has achieved this type of structure in its own speciality, and we would like to develop something similar in dry eye as well.
More information on EuDES at https://www.dryeye-society.com/
Christophe Baudouin MD, PhD is Chairman, Department III of Ophthalmology: Centre Hospitalier National d’Ophtalmologie des Quinze-Vingts, Paris, and Editor-in-chief of the French Journal of Ophthalmology. cbaudouin@15-20.fr

I think it is not really disputed that dry eye has been something of a neglected disease for the past few decades, especially when we compare it to blinding diseases such as glaucoma, AMD, corneal dystrophies, keratoconus, and so forth. It was often considered an inconvenience or annoyance rather than a serious condition. But it is a very common and potentially disabling disease and can have a huge impact on patients’ quality of life.
There has been a shift in this perception over the past few years with a broader recognition of the importance of dry eye and its relevance to contact lens wear, cataract and refractive surgery, autoimmune eyelid diseases, skin or eyelid diseases, glaucoma, topical or systemic medications, and so forth. Dry eye is present in many diseases, and it makes sense to try to bring our knowledge together under one umbrella.

“I hope the existence of a European Dry Eye Society will serve as a catalyst for experts to form their own national groups.”
Cosmetics and cosmetic procedures pose an underestimated risk of contamination to the ocular surface and can induce several symptoms ranging from mild irritation and red eye to more serious infections and potentially sight-threatening complications, according to Jutta Horwath-Winter MD.
“There are a range of cosmetics and cosmetic procedures on the market that can disrupt the homeostasis of the ocular surface and tear film directly and indirectly via multifactorial pathways. We need to keep up to date with new beauty trends and ingredients used to assess potential risks to the ocular surface,” she said at the first European Dry Eye Society Congress.
Dr Horwath-Winter stressed the importance of patient education in reducing potential risks to the ocular surface from cosmetics.
“We should improve our communication with patients to inform them about cosmetics and the risk they can pose to the anatomy of the ocular surface and meibomian gland orifices. We should also advise our patients to ensure regular replacement of cosmetic products every three months,” she said.
In an overview of the negative effects cosmetic procedures can have on the tear film and ocular surface, Dr Horwath-Winter noted the list of chemicals used to create cosmetic products— including preservatives, retinoids, prostaglandins, and endocrine disruptors—runs to more than 12,000 possible ingredients.
Although European regulations concerning the use of cosmetics have been in place since 2013, vigilance is still required to avoid contamination through misuse or overuse, Dr Horwath-Winter said.
“Even commonly used products such as mascara can be a source of contamination via bacteria, fungi, or demodex mites, especially in humid conditions. One study showed that after

three months of use, 36% of mascara products were contaminated,” she explained.
Eyelash dyeing or tinting may cause an allergic reaction, and eyelash extensions and artificial lashes contain glue which may also be toxic to the ocular surface, Dr Horwath-Winter said.
Particular care should be taken with eyeliner application at the inner lid margin, which can cause tear film contamination, blockage of the meibomian gland orifices, tear film instability, and ocular discomfort.
She advised using facial cleansers and makeup removers with caution, as these contain alcohol and fat solvents—and possibly preservatives—all of which can damage conjunctival, corneal, and meibomian epithelial cells. Anti-aging skin creams typically contain retinoic acid, which can reduce the number and size of meibomian gland acini and promote meibomian gland disease (MGD).
Prostaglandins—often used in eyelash serums and gels—may have adverse effects such as conjunctival hyperaemia, itching, irritation, blepharitis, MGD, hyperpigmentation of the skin and iris, and prostaglandin-associated periorbitopathy.
Cosmetics containing endocrine disruptors such as parabens, triclosan, and benzophenone, can all affect sex and thyroid hormones and negatively impact on the tear film and ocular surface homeostasis by accelerating oxidative stress, Dr Horwath-Winter concluded.
Aselenium sulphide ointment has the potential to be the first pharmacotherapy effective for treating the signs and symptoms of meibomian gland disease (MGD), announced Edward J Holland MD at the annual meeting.


In a phase 2 study, both a 0.5% and a 1.0% preparation of AZR-MD-001 (Azura) significantly improved the percentage of patients with normal open meibomian glands compared with placebo after three months of treatment, Dr Holland said. Both doses significantly improved ocular symptoms as measured by the total ocular surface disease index (OSDI) as well.



The higher dose also significantly improved the percentage of patients with normal meibum. Having met FDA requirements for showing both sign and symptom improvements, the compound is advancing to phase 3 development, he added.















MGD results from the formation of aberrant disulphide bonds in the meibum, which thickens and solidifies it through hyperkeratinisation. This leads to blockage and eventual atrophy of the meibomian glands, Dr Holland explained.
AZR-MD-001 addresses the disease in three ways: First, it slows both the rate of keratinocyte proliferation and keratin production. Second, it softens the keratin plug by breaking down disulphide bonds. Third, it stimulates lipogenesis to increase the number of lipids the meibomian glands produce.
In a study involving 95 patients testing 0.1%, 0.5%, and 1.0% doses with a vehicle control, the two higher doses improved the number of open meibomian glands significantly more than the vehicle and baseline, with 46% of patients on the highest dose achieving normal open glands compared with 8% on vehicle, Dr Holland reported. The 1.0% preparation also significantly improved the number of patients with liquid meibum compared with controls. Both were primary sign endpoints.
Both higher doses also significantly improved OSDI scores from baseline, with 58% of patients on 0.6% and 42% of patients on 1.0% symptom-free compared with 16% of controls. This reached the primary symptom endpoint.
No serious adverse events were observed during the study, Dr Holland said. Eye pain, irritation, and increased lacrimation were noted in the higher doses, though 96% of adverse events were mild to moderate. Dosing was twice weekly at bedtime.


In addition to meeting its primary endpoints, AZR-MD-001’s “safety and tolerability profile was certainly satisfactory,” Dr Holland concluded.
Edward Holland MD is the Director of Cornea Services at Cincinnati Eye Institute and Professor of Ophthalmology at the University of Cincinnati, Ohio, USA. He is also a past president of ASCRS. edward.holland@uc.edu, eholland@holprovision.com
Magnetic cell delivery is a platform technology that holds promise as a replacement for damaged corneal endothelial cells, reducing the need for corneal transplants, Jeffrey L Goldberg MD, PhD told the Innovators Session of the 2021 ASCRS meeting.

The therapy has recently begun a phase 1b US FDA clinical trial. Dr Goldberg helped develop the magnetic cell delivery system, designed to overcome three key barriers in cell therapy—how to deliver cells to the desired spot, retain them there, and integrate them into surrounding tissues.
The treatment starts by expanding human corneal endothelial cells in culture. “A single donor cornea can produce enough cells to treat hundreds of patients, addressing donor supply,” Dr Goldberg said. He credited Shigeru Kinoshita MD, PhD and others with developing techniques supporting endothelial cell expansion and replacement.
First-in-human trials studied two formulations in 21 patients, mostly with end-stage corneal oedema due to endothelial dysfunction. Even though the patients had long-term scarring, nine out of 21 gained three lines or more of vision, and there were no safety issues after 12 months.
The expanded cells then combine with magnetic nanoparticles that coat the cells and get injected into the anterior chamber, Dr Goldberg continued. A magnetic eye patch is then applied for a period of one hour up to overnight. This patch attracts the coated cells to the posterior surface of the cornea, facilitating localisation and integration of the magnetic cells into the endothelial layer.
The treatment could allow general ophthalmologists to identify patients needing endothelial cell treatment, order a treatment kit consisting of the cells and magnetic patch, and treat the patient in their clinic, Dr Goldberg said.
“It addresses the fundamental problem in these diseases of too few endothelial cells. It is a non-surgical procedure, easy to perform, has rapid recovery, gets rid of this donor limitation element, and is safe and repeatable.”
The treatment entered a US-based phase 1b clinical trial for FDA approval with the first patient dosed in July 2021, Dr Goldberg said. The study will include up to 18 patients testing three cell dosages, with and without endothelial cell brushing. There is a plan for a phase 2 study for the most successful dosage.
Dr Goldberg anticipates the therapy will eventually greatly expand the patient population eligible for endothelial treatment, addressing vision loss and significant unmet need around the world.
“It addresses the fundamental problem in these diseases of too few endothelial cells.”
Cheryl Guttman Krader reports from ASCRS 2021 in Las Vegas, USA
Medical management for severe ocular surface disease associated with limbal stem cell deficiency (LSCD) requires a multipronged approach that incorporates reducing aggravating factors and optimising the microenvironment,” Charles S Bouchard MD, MA said.
Speaking at ASCRS Cornea Day 2021, he outlined general management strategies. He also discussed published articles describing care regimens for eyes with various aetiologies of LSCD that illustrated how to customise treatment based on underlying cause and clinical features. Potential aggravating factors to address include the preservatives in topical medications such as benzalkonium chloride and contact lens wear (overwear).
“The pathogenesis of LSCD associated with contact lens wear is multifactorial. Limbal epithelial stress can occur from mechanical trauma, hypoxia, dry eye, exposure to lens care solutions and their preservatives, and inflammation,” Dr Bouchard said.
Strategies for optimising the ocular surface microenvironment include reducing aggravating factors, using preservative-free ocular lubricants, punctal occlusion, and/or autologous serum/plasma to improve the tear film. Other strategies include managing existing lid disease (ego, meibomian gland dysfunction, ocular rosacea) and controlling inflammation with agents such as topical corticosteroids, calcineurin inhibitors, lifitegrast, and/or amniotic membrane. Additional treatments that help restore homeostasis and promote the health of the ocular surface epithelium include recombinant human nerve growth factor (cenegermin, OXERVATE™), vitamin A ointment, and scleral contact lenses.
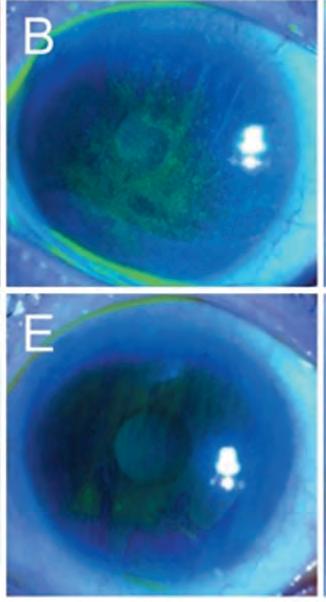
Focusing on contact lens-induced LSCD, Dr Bouchard noted that it can take time to achieve an optimal outcome when initiating medical management after stopping contact lens wear. He illustrated his point by showing images depicting various levels of improvement achieved among three patients treated for periods ranging from six weeks to five months. He also mentioned a report describing how to treat corneal neovascularisation using the PROSE scleral lens to deliver bevacizumab.
Citing other literature, Dr Bouchard highlighted medical (and surgical) management of eyes with LSCD associated with ocular rosacea, atopic and toxic keratoconjunctivitis, graftversus-host disease, and Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN).
Finally, Dr Bouchard introduced the concept of the currently under-recognised role of the microbiome in the pathophysiology and immune regulation of ocular surface microenvironment. He presented a patient with a history of toxic epidermal necrolysis suffering chronic bilateral recurrent keratitis for many months. After conferring with Elmer Tu MD, University of Illinois, Chicago, Dr Bouchard prescribed topical linezolid 0.2%.
“The keratitis cleared when the patient started on linezolid, and when the patient stopped the treatment because of the cost, the inflammation returned,” he said. This probable MRSA immune keratitis in patients with SJS/TEN was also previously reported by Chei Sotozono et al.
“The keratitis cleared when the patient started on linezolid.”
Anew treatment for Demodex blepharitis has been shown safe and effective in a pivotal phase 2b/3 US FDA trial, Elizabeth Yeu MD said. It is the first of two FDA studies, she added.

According to epidemiological studies, somewhere between 9 million and 25 million people are affected by Demodex blepharitis in the USA alone. “And yet there is no FDA-approved prescription therapeutic for the management of this disease,” Dr Yeu said.
Caused by an infestation of Demodex mites, Demodex blepharitis is also likely involved with many cases of dry eye. In a recent study conducted at six busy eye centres across the United States, 57.7% of 1,032 patients had collarettes or about the same number as had dry eye diagnoses, Ehsan Sadri MD said. Among patients who were using cyclosporine or lifitegrast for dry eye, 60% had collarettes—a major sign of Demodex blepharitis.
A separate study reported demodicosis newly diagnosed in 53.3% of eye patients, with 61.8% and 63.3% having blepharitis and dry eye, respectively, Dr Sadri said (Teo et al. ARVO 2021). Extrapolating numbers from these two studies, about 25 million of 45 million eye patients seen annually in the USA may have Demodex blepharitis, though this is higher than the 9 million estimated in population studies. A prospective study is needed to better understand its prevalence, he added.
The randomised, controlled double-masked FDA pivotal trial involved 421 patients at 15 clinics across the USA. A test of a 0.25% ophthalmic solution of lotilaner called TP-03 (Tarsus
Pharmaceuticals) against the medication vehicle alone in patients with confirmed Demodex blepharitis. A total of 206 treated patients and 204 control patients completed the sixweek study, Dr Yeu reported. Zero patients in the treatment group and one patient in the control group dropped out due to a mild treatment-related adverse event, while five dropped out due to COVID-19.
Demodex waste and by-products create collarettes, which can easily be seen on patients’ upper eyelashes when they look down. Patients included in the study needed to have at least one eye with more than 10 upper lid eyelashes with collarettes, 1.5 or more Demodex mites per lash on the upper and lower lids, and mild or worse lid margin erythema. Patients using lid hygiene within 14 days of screening were excluded.
Lotilaner has previous FDA approval as an oral medication to control fleas and ticks in dogs and cats. “It is a very well-known and utilised anti-parasitic agent,” Dr Yeu said. In Demodex blepharitis, it works by paralysing and killing Demodex mites.
“And yet there is no FDA-approved prescription therapeutic for the management of this disease.”
On day 43 of treatment, 44% of the treated group and 7% of the control group reached the study’s primary endpoint—a complete collarette cure, defined as grade 0, or no more than two lashes with collarettes (p<0.0001). A clinically meaningful collarette cure, defined as grade 0 to 1 or no more than 10 collarettes, was achieved by 81% of the treated group and 23% of the control group (p<0.0001), Dr Yeu reported. Greater numbers of treated patients also achieved complete and meaningful collarette cures after 11 and 22 days of treatment, results also statistically significant (p<0.001 at all time points). Mean collarette grade before treatment in both groups was 2.8, or between about 50 and 100 collarettes.
At 43 days, 68% of treated patients achieved complete mite eradication compared with 18% of controls (p<0.0001), Dr Yeu said. Mean mite density dropped from about 3.2 mites per lash before treatment in both groups to 0.14 in the treated group and 1.34 in the control group (p<0.0001).
Overall, 13.9% of treated patients and 1.0% of controls achieved a complete composite cure, defined as collarette and erythema grades of 0, while 68% and 20% respectively reached a clinically meaningful cure, with collarettes and erythema at grades 0–1. Grade 0 erythema was achieved in 19% of treated patients while 45% saw one grade or more decline.
Adverse events were also very low, with less than 1% occurring at any time during the trial, and none were serious in either group, Dr Yeu said. At day 43, there was minimal change in corneal staining and IOP in both eyes in both groups. Among 21 patients at one centre with endothelial cell results, change from baseline was less than 1.2%.
“It’s very exciting to see TP-03 proven a potentially safe and effective treatment for Demodex blepharitis,” Dr Yeu said. In addition to reaching all primary and secondary endpoints, TP-03 was well-tolerated, had a good safety profile, and 92% of patients rated it neutral to very comfortable, she concluded.

Dr Elizabeth Yeu is the Medical Director of the Virginia Eye Consultants—CVP Mid-Atlantic Cornea, Cataract, External Disease, and Refractive Surgery. She is an Assistant Professor of Ophthalmology, Eastern Virginia Medical School, Norfolk, Virginia, USA. She is also the co-host of the popular Ophthalmology Quicksand Chronicles podcast. eyeulin@gmail.com
Dr Ehsan Sadri is the CEO and Founder of the Visionary Eye Institute based in Newport Beach, California, USA. drsadri@visionaryeyeinstitute.com
The available evidence suggests the risk of COVID-19 transmission through corneal transplantation is low. Nevertheless, with an abundance of caution, Eye Bank Association of America (EBAA) guidelines on donor screening should continue to be implemented as the understanding of SARS-CoV-2 and corneal transplantation evolves, according to Shahzad I Mian MD.
In his discussion of the impact of SARS-CoV-2 on corneal transplantation, Dr Mian presented research relating to viral presence in the cornea, the risk of COVID-19 transmission through corneal transplantation, and the effect of the pandemic on donor supply.
He noted studies of SARS-CoV-2 ocular infection show conjunctivitis, not keratitis, is the most common ocular manifestation in patients with COVID-19. However, there is a poor correlation between presence of ocular signs and symptoms and presence of SARS-CoV-2 on the ocular surface.
Other research on ocular infection shows SARS-CoV-2 entry proteins/receptors express in the limbus, conjunctiva, and corneal epithelium. In addition, researchers have detected SARS-CoV-2 in ocular tissues harvested from donors who died of COVID-19, those with signs and symptoms of COVID-19, and individuals without manifestations of the novel coronavirus infection who were otherwise surgically eligible.
“The important question, however, is whether the presence of the virus translates into infection transmission through the cornea. Currently, information relevant to this issue is limited. So far, however, there is no evidence that SARS-CoV-2 replicates in human corneal tissue, and there are no reports of transmission of infection through corneal transplantation,” Dr Mian said.
Dr Mian noted there are zero reported cases of SARS-CoV-2 transmission from blood or blood components when screening excludes donation by individuals who recovered from COVID19 within the previous 14 days. In fact, the only published case of COVID-19 transmitted through donor tissue involved a lung transplant recipient who was given an organ from a donor that tested negative for COVID-19 by nasopharyngeal swab. The donor was determined to be infected with SARS-CoV-2 only after the completed lung transplant through testing of bronchoalveolar lavage fluid.
Most importantly, data from the EBAA show no cases of SARS-CoV-2 transmission among nine patients who underwent corneal transplantation using tissue from donors who were COVID-19 positive.
Emphasising the point that the risk of transmission through corneal transplantation is low, Dr Mian said, “Of the nearly 50,000 transplants performed in the US during the pandemic, there were only nine cases of inadvertent transplantation of a graft from a COVID-19-positive donor, and there [weren’t any] transmission events among any of the transplant recipients.”
Asked during the discussion following his talk whether, in light of existing knowledge, he thought the EBAA might change its recommendations on protocols for donor screening, Dr Mian said only time will tell.
“Early in the pandemic, there seemed to be a great need to implement strict screening criteria to avoid using tissue from COVID-19-positive donors because we did not know anything about the risk of transmission to recipients. As we gain more clinical data, we are learning that the risk of transmission is likely extremely low, and we have a better understanding [of] which screening criteria are valid,” he said.
“Although this raises the question of whether there is really a need to screen for COVID-19, it seems the COVID-19 positivity of a donor is still a good indication not to use the corneal tissue. However, criteria for donor exclusion relating to close contact with an infected individual may need to drop because there is a growing concern for having a sufficient supply of tissue to meet demand.”
Dr Mian also observed EBAA guidelines on screening are only recommendations. Ultimately, individual eye banks establish their own protocols.
“What we are seeing now is that because the risk of COVID-19 transmission to cornea transplant recipients seems to be essentially zero, a lot of the testing policies and practices are being dropped,” he said.
The easing of restrictions would be welcome news for those involved with meeting the demand for transplant tissue. Dr Mian noted because elective surgeries were placed on hold early during the pandemic, demand for corneal tissue was very low. Thus, a surplus of corneal tissue accumulated despite the implementation of stricter donor criteria.
“For the 2020 calendar year, the EBAA processed about 56,000 grafts, about 30,000 fewer than the average number processed in recent pre-pandemic years. Even with that shortfall, the supply was adequate because of low global demand. Now, however, from a global perspective, the supply volume is approximately 15% below the need,” Dr Mian commented.
Safety supported by accumulating research and clinical experience, with caveats. Cheryl Guttman Krader reports from ASCRS 2021 in Las Vegas, USAShahzad I Mian MD is Professor of Ophthalmology, University of Michigan Medical Center, Ann Arbor, and a medical director for the Eversight Eye Bank. smian@umich.edu
“The important question, however, is whether the presence of the virus translates into infection transmission through the cornea.”
The first two patients implanted with a completely synthetic keratoprosthesis (CorNeat KPro, CorNeat Vision) are doing well during follow-up ranging from three to seven months, reported Gilad Litvin MD at the Innovators general session.
His key message, however, was the preclinical and early clinical experience with the device shows the ability to achieve seamless integration of artificial material with resident human tissue.
“I think the technology ushers in the way to a new era of medical devices,” said Dr Litvin, inventor of the keratoprosthesis.
The novel device has two elements—a central PMMA optic and a surrounding synthetic nanofabric integrating skirt. Unlike existing keratoprostheses that integrate with corneal tissue, the CorNeat KPro anchors in the subconjunctival space, and its integrating skirt provides a scaffold onto which fibroblasts from Tenon’s capsule can migrate.
“Whereas the cornea is devoid of blood vessels and lacks a significant cellular component, the subconjunctival space is a vascularised site that heals vigorously,” Dr Litvin explained.
The skirt’s nanofabric material is manufactured by a chemical engineering process called electrospinning. This process can create a nonwoven matrix in the nanometre and micrometre scale. It fuses to the optical element of the keratoprosthesis at the rim of the PMMA lens, an area designed with features facilitating implantation, future surgery, device integration, and retention.
The rim contains three pairs of suturing holes for passing nondegradable sutures that anchor the device to the eye wall. In addition, it has four ports that allow future access into the anterior or posterior chamber. The rim also has grooves filled with the nanofabric that promotes tissue invasion, helping to secure the PMMA optic to the eye.
The optical element has a posterior undercut that houses the remnant cornea while ensuring centralisation of the device and a watertight seal. Flanges in the undercut help the surgeon with inserting the cornea and then securing it.
Rabbit studies helped establish surgical feasibility and biocompatibility.
“Histological evaluations show the presence of abundant cell nuclei interspersed between the fibrils of the nanofabric skirt, collagen, and even capillaries coursing their way from one end of the skirt to the other,” Dr Litvin stated.
Irit Bahar MD, Rabin Medical Center, Petah Tikva, Israel, performed the first in-human implantation of the novel keratoprosthesis in January 2021. The surgery begins with a 360-degree peritomy followed by epithelial debridement to avoid downgrowth. Then the centre of the cornea is stamped with a specially developed marker tool. The markings identify the locations of the
access ports, suturing positions, and the trephination’s edge, thus assisting the surgeon in locating the paracenteses and visualising the trephination’s edge, Dr Litvin explained.
After filling the eye with viscoelastic, the surgeon places three non-degradable sutures, first through the device and then through the corneosclera. Trephination follows, and then the surgeon pulls on the distal ends of the corneal sutures to approximate the device to the eye wall.
“This seals the eye and stops the open sky segment of the procedure,” Dr Litvin said.
The trephined corneal edge is inserted into the posterior undercut of the optical element using another specialised tool known as the Snapper. Finally, the conjunctiva is repositioned, sutured over the integrating skirt with biodegradable sutures, and sealed with fibrin tissue glue.
The first recipient of the synthetic keratoprosthesis had one functioning eye that had undergone four corneal transplantation procedures. After the fourth procedure, which was performed about 10 years earlier, he developed an Acanthamoeba infection that left the transplant completely opaque.
“The patient has optic nerve damage, but at seven months after implantation, he is seeing 6/90 (~20/320) and is very pleased,” Dr Litvin said.
The second patient had a history of ocular cicatricial pemphigoid and had not been able to see for 30 years. At three months following keratoprosthesis implantation, his visual acuity was 6/9 (~20/30).
Some conjunctival retraction was observed during the first few weeks postoperatively in both patients. However, it stabilised after the tissue adhered to the skirt material, and the retraction has not been associated with any untoward sequelae.
“In the rabbits, histology revealed that the skirt was filled with collagen, fibroblasts, and even capillaries. This was also evident in the areas where there was conjunctival retraction, blocking any access into the anterior chamber,” Dr Litvin said.
“In the first patient, conjunctival retraction has left approximately 1.5 mm of the device rim without conjunctival covering, but the patient is not bothered by it, and his anterior chamber remains quiet.”
Currently, IOP monitoring occurs through digital palpation. Patients are also being followed for glaucomatous damage with serial optical coherence tomography imaging of the retinal nerve fibre layer and visual field testing, which is possible because the PMMA lens has a large, 6.5 mm optical zone. Work is underway to develop a second generation of the keratoprosthesis that will have an embedded IOP sensor.
Neuropathic corneal pain (NCP) can present a treatment challenge, but patients suffering from this disorder can do well when they receive compassionate multimodal and multidisciplinary care, Majid Moshirfar MD told a Cornea Day session.
“Most patients can lead functional lives whilst managing their debilitating neuropathic pain. My take-home messages are to show compassion, provide diligent care, use rating scales to characterise pain severity, adjust the treatment regimen accordingly, and try to get other disciplines involved,” Dr Moshirfar said.
Patients with NCP complain subjectively of severe ocular pain and symptoms associated with dry eye disease that are greatly out of proportion to clinical findings.
“Some patients might have mild meibomian gland disease or ocular surface staining, but overall, the ocular surface condition will be very good. Because of the benign clinical picture, clinicians may doubt whether patients are telling the truth about their symptoms,” Dr Moshirfar said. “Now we know these are neuralgic symptoms.”
NCP diagnosis is made by exclusion. Although confocal microscopy can reveal aberrations in corneal nerve architecture consistent with the concept that the pathophysiology of NCP involves aberrant regeneration of injured nerves, the findings are not sensitive or specific.
“I have also seen the same nerve abnormalities in post-LASIK patients without NCP. Furthermore, a normal appearance of the corneal nerves on confocal microscopy does not rule out NCP,” Dr Moshirfar said.
He discussed a recently published paper in which he undertook a retrospective review of his LASIK cases to identify and characterise patients with NCP (Moshirfar M, et al. Ophthalmol Ther. 2021; 10: 677–689). A total of 18 patients were found in a medical search encompassing 26 years, translating into a prevalence of approximately 1 in 900. All patients with NCP had uncomplicated LASIK. Fifty percent of patients had a prior neuropsychiatric disorder, including depression and anxiety. Other common medical history findings included functional pain syndromes, autoimmune diseases, and endocrinological abnormalities.
“These comorbidities have been noted by other authors, and NCP may occur more often in females than males,” Dr Moshirfar said.
Dr Moshirfar said his treatment for NCP includes autologous blood serum at a concentration ranging from 20% to 50%. Noting the therapeutic benefit of the autologous serum is likely related to the delivery of neurotrophic growth factors, Dr Moshirfar said he once sought authorisation to prescribe recombinant human nerve growth factor (cenegermin, Oxervate) for a patient but could not gain approval.
“There are two different thoughts about using neurotrophic growth factors. On the one hand, it may be beneficial by acting as a ‘fertilizer’ to enhance the growth of nerve endings and induce regeneration. On the other hand, perhaps the treatment may lead to more aberration and make the micro-neuromas worse. In terms of providing nerve growth factors, I truly think we should try to help these patients by using autologous blood serum.”
Other therapeutic modalities include artificial tears, antiinflammatory agents, and other treatments typically used to manage dry eye, along with ocular surface protection (scleral contact lenses, bandage contact lenses, amniotic membrane). Oral treatments include nutritional supplementation with omega-3 fatty acids and vitamins D3 and B12 that may have neuroprotective activity, tricyclic antidepressant medications, and anticonvulsants, particularly gabapentin.
In addition, Dr Moshirfar said he prescribed naltrexone 1.5 mg at bedtime for some patients. He has also referred patients with peripheral hypersensitivity to see an anaesthesiologist for trigeminal nerve ganglion ablation, which has provided transient benefit. Other interventions include meditation, biofeedback, acupuncture, and botulinum toxin injections.
“Although I have not personally done so, there are also reports intrathecal injection with fentanyl and bupivacaine at the level of C1 has been helpful for patients with a presynaptic condition who are refractory to other treatments,” Dr Moshirfar said.
He emphasised the importance of identifying mental health problems in patients with NCP and encouraging them to seek help from a psychiatrist.
“Neuropathic corneal pain can worsen underlying neuropsychiatric conditions. There are reports of suicide and suicidal ideation among these patients. Some patients may ask for enucleation, which is shocking,” Dr Moshirfar said.
Refractive surgery can be a trigger for NCP. This underscores the importance of obtaining a thorough medical history preoperatively, with an awareness that certain conditions may be predisposing factors. This can help in identifying patients who may be at risk for developing NCP after refractive surgery.
“If I see that a patient has functional pain syndrome, fibromyalgia, or is on chronic pain medications, I talk to them specifically about this rare postoperative complication and tell them I think they are at high risk,” Dr Moshirfar said.
Majid Moshirfar MD is Director of Clinical Research at Hoopes Vision and Adjunct Professor at John A Moran Eye Center, University of Utah, Salt Lake City, USA. He is also co-director of the Utah Lions Eye Bank, Murray, Utah. cornea2020@me.com


Several promising new approaches to neuroprotection in glaucoma patients are now in preclinical and clinical trials, bringing them a step closer from the laboratory to the patient, Jeffrey Goldberg MD, PhD told the virtual meeting.
Professor Goldberg noted the fundamental problem underlying irreversible vision loss in glaucoma is retinal ganglion cells do not regenerate after optic nerve injury but instead undergo a retrograde degeneration of their axons, ultimately leading to cell death. However, there is this window between retina ganglion cell injury and death where therapeutic intervention might protect the cells and promote axon regeneration down the optic nerve and dendrite regrowth into the retina.
Therapeutic candidates for neuroprotection include neurotrophic factors that could prevent RGC apoptosis, blocking the complement protein C1q, or enhancing insulin or insulin-like growth factor signalling. Another potential new strategy is to target the enzymes that mediate axon regenerative failure, like Rhokinase (ROCK), for which there are now commercially available Rho-kinase inhibitors.
There are now several trials using these approaches in various stages. One recently completed trial tested topically applied nerve growth factor, while another recently completed trial involving intravitreal injection of a C1q-blocker showed a great reduction in C1q levels in the eye. There is also a phase-two randomised controlled trial currently underway testing ciliary neurotrophic factor, which research has shown to prevent the death of retinal ganglion cells and promote regeneration of their dendrites and axons.
In addition, Prof Goldberg noted studies conducted by several research groups demonstrated very clearly over the years that ROCK-inhibitors promote cell survival and regeneration. For example, in a recently published study he and his associates conducted, topical netarsudil promoted survival and RGC regeneration and strongly promoted axon regeneration down the optic nerve in a rodent model of glaucoma.
Prof Goldberg noted that in the past, conducting neurotrophic trials was a daunting prospect because of the disease’s slow progress. It was also assumed necessary to have large study populations with a long follow-up to show a treatment effect. However, new emerging trial designs allow primary neuroprotection endpoints that can be measured in a year or a year-and-a-half with hundreds rather than thousands of patients.
“What we’ve learned is that neurotrophic factors, Rho-kinase inhibition, and other strong candidates are ready for neuroprotection testing in glaucoma, that these therapeutic candidates can be studied in our glaucoma patients, and that merging neuroprotection testing with biomarker exploratory endpoints to crossvalidate are going to give us particular power as we launch these trials,” Prof Goldberg concluded.
New neuroprotection and neuroregeneration strategies for glaucoma now entering clinical trials.
Many new non-IOP-lowering therapeutic strategies show promise for glaucoma treatment, from interventions as simple as vitamin B supplementation and exercise to gene therapy designed to stimulate repair and regeneration of retinal ganglion cells.
“I think we are moving beyond IOP being the only way in which we can treat glaucoma. I think there are many promising approaches,” Professor Keith Martin MD told the virtual gathering.
As an example, he noted there is early evidence suggesting vitamin B3 modulates the vulnerability of the retinal ganglion cell mitochondria. In a study using a mouse model of glaucoma, boosting nicotinamide either by diet or supplementation was shown to be strongly protective of the dendritic trees of the RGCs and preserved vision. In addition, there was a dose-dependent effect in the mice receiving the higher doses of nicotinamide.
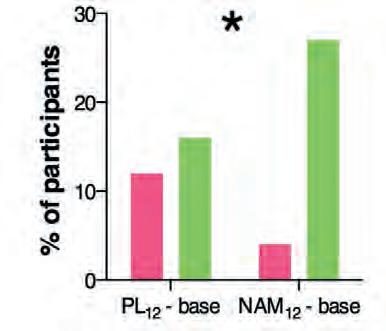
The findings of a recent crossover clinical trial indicate vitamin B3 supplementation may have the same neuroprotective effect in glaucoma patients, Prof Martin said. It showed after 12 weeks of vitamin B3 supplementation, patients had a statistically significant improvement in inner retinal function, as measured by their photopic negative electroretinography (ERG) response.

In addition, 27% of the patients receiving nicotinamide had more than a decibel of improvement in their visual field mean deviation, compared to only 16% in the placebo group. Furthermore, the visual field got worse in only 4% of patients in the vitamin B3 group, compared to 12% in the placebo group.
“The findings of this trial are interesting. Given that vitamin
B3 is well-tolerated and has a good safety profile, the hypothesis here is that it has the potential to be combined with existing clinical therapy as a supplement,” he noted.
Recent research suggests exercise may also have a role in preventing glaucomatous neurodegeneration, he said. For example, in a study in which mice were given increased exercise, the vulnerability of the optic nerve to IOP-induced injury was restored in older mice to that of much younger mice.
The future may see the development of gene therapies for common eye diseases without single-gene defects, including glaucoma, Prof Martin said. For example, he and his associates have developed a gene therapy that upregulates brain-derived neurotrophic factor (BDNF) signalling. Their research has shown it greatly reduced optic nerve damage in a laboratory glaucoma model. The therapy is now in preclinical development by a major pharmaceutical company, with trials to begin in due course.
keith.martin@unimelb.edu.au
New neuroprotective treatment approaches may help preserve vision in glaucoma patients where IOP-lowering strategies fail.
Roibeárd O’hÉineacháin reports from the ninth World Glaucoma E-CongressKeith Martin MD, FRCOphth is Professor and Head of Ophthalmology at the University of Melbourne, Australia, and Managing Director of the Centre for Eye Research, Australia.
When normal-tension glaucoma (NTG) patients progress despite low IOP, it is important to consider potential lifestyle factors, out-of-office IOP spikes, genetic predisposition, and potential non-glaucomatous causes for optic nerve degeneration, advised Professor Louis R Pasquale MD.
“In most instances, we don’t identify the real reason patients are progressing. There are no proven ways to halt progression in NTG, either by IOP lowering or non-IOP lowering approaches,” Prof Pasquale told the congress.
He noted progressive NTG is a public health problem with an estimated unilateral blindness rate of 10% and an estimated bilateral blindness rate of about 1.4% at 20 years. He also put out a call for an international consortium devoted to solving the problem of progressive NTG.
“We need a ‘wisdom of crowds’ approach to halt NTG progression, which is really one of the scourges of the twentyfirst century,” he added.
Prof Pasquale noted that sometimes what may appear to be progressive NTG may not be glaucoma at all. He cited the case of a 74-year-old white male referred for NTG evaluation. The patient had increased cupping in his left eye, and visual field testing revealed a unilateral superior temporal hemianopsia.
“Whenever you see this, this is a pituitary tumour until proven otherwise. In this case, neuroimaging studies confirmed that diagnosis and prompt neurosurgical intervention resulted in resolution of this defect,” he said.
Other red flags for non-glaucomatous optic neuropathy include a rate of visual field loss greater than one decibel per year (compared to a more typical progression rate for NTG of 0.2 dB to -0.5 dB per year); non-congenital dyschromatopsia; and visual field defects that respect the vertical meridian, which can indicate lesions in the optic chiasm or the post-chiasmal visual pathway.
When assessing a case of progressing NTG, it is also important to take the patient’s lifestyle and occupation into consideration,
Prof Pasquale said. He described the case of a 48-year-old yoga instructor referred for a third opinion regarding her apparently “normal tension” glaucoma. When asked about her occupation, she responded that she did a lot of headstand posturing in the yoga classes she ran. Subsequent IOP measurements taken while she performed a headstand showed a pressure of 50 mmHg.
Another aspect of a progressing NTG patient’s history to consider is their sleep habits. Patients with a tendency towards daytime somnolence may benefit from a sleep workup.
One should also inquire whether they are receiving medication for systemic hypertension, as taking evening doses closer to dinner time than to bedtime may reduce early morning peaks in IOP.
PREDISPOSITION TO HIGHER OUT-OF-OFFICE IOP NTG progression despite IOP in the low teens during in-office readings may indicate a greater genetic predisposition to higher early morning IOP, Prof Pasquale said. He cited a study involving 176 patients with suspected or established primary open-angle glaucoma. It showed iCare HOME tonometer readings in the early morning hours were 4.3 mmHg higher among those with the highest polygenetic risk score for elevated IOP than among those with the lowest scores.
“IOP tends to be highest in the early morning when nitric oxide signalling tends to be lowest. These outside-of-the-office intraocular pressure readings could be very important in explaining why these patients progress,” he said.
Prof Pasquale also recommended investigating the possibility of Mendelian variants in patients with a family history of glaucoma in young adulthood. Variants associated with NTG include optineurin (OPTN), TANK binding kinase 1 (TBK1) and myocilin (MYOC) which are present in around 3% of NTG cases. In the case of TBK1 duplication NTG, single-digit target IOPs are necessary because although its progression rate is slow, the disease starts at a young age.
Patients who have undergone corneal refractive surgery might also require single-digit IOP targets because of low corneal hysteresis. Low corneal hysteresis is associated with greater IOP fluctuations and more rapid visual field progression, he noted.
Prof Pasquale emphasised there is an abundance of evidence in the literature showing single-digit target IOPs slow progression in eyes with open-angle glaucoma. Research has consistently shown trabeculectomy reduces visual field progression in patients with pre-operative IOP in the mid-teens.
“Trabeculectomy must survive because trabeculectomy represents a relatively safe and effective way to achieve singledigit intraocular pressures,” he said.
Recent studies suggest that mindfulness meditation can reduce IOP still further in eyes that have already undergone trabeculectomy. In one study, patients who performed daily 45-minute mindfulness meditation sessions had significantly lower IOP and less IOP fluctuation compared to the control patients. The meditation group also had significant changes in trabecular meshwork gene expression, including upregulation of neuroprotective genes, downregulation of pro-inflammatory genes, and upregulation of nitric oxide synthase 1 (NOS1) and NOS3.
The pandemic’s damaging effects on eye health are now coming to light. Some of the most pressing problems were highlighted during a special session, “Better Patient Counselling: Using Epidemiological Evidence in Day-to-Day Clinical Practice.”
Caroline Klaver MD, PhD opened the session with her presentation, “Myopia and Quarantine.” It has been known for quite some time that near work, which includes screen time, can contribute to the progression of myopia. In contrast, outdoor time has been shown to be beneficial. These findings have been distilled into the anti-myopia lifestyle advice for children, resulting in the 20-20-2 rule. For near work, this means after 20 minutes of near work, children (as well as the adults) should gaze into the distance for 20 seconds. In addition, children should spend 2 hours per day outside.
time for children less than two years of age. Children two to five should spend less than an hour with a device, while those from six to 10 should stay under two hours and 11-to-15-year-olds should spend less than three hours per day, with breaks every 20 minutes.
“Quarantine is risky for myopia, and awareness of increased myopia risk with severe homebound quarantine is warranted,” Dr Klaver concluded.
She urges eye care professionals to “vocalise these risks to those responsible for managing pandemic behavioural policy.”
Quarantine and isolation requirements in the COVID-19 era have made following these guidelines very difficult. “During COVID-19, we’re not only experiencing a viral pandemic, but also a myopia pandemic,” she emphasised.
All children are at risk, including teenagers, although the younger the child, the greater the risk of myopia progression, she stressed.
“According to a recent study of more than 100,000 children in China, the risks are greatest for school children aged six to eight years. The prevalence of myopia in six-year-olds more than doubled from 2019 to 2020. This correlates with an enormous increase in screen time pre- and post-COVID-19 and a corresponding decrease in time spent outdoors.”
In another study, the percent of Chinese children spending more than two hours per day using digital devices increased from approximately 20% to nearly 80%.
“A significant percentage of children were found to be spending seven hours per day online,” Dr Klaver said.
But what does “screen time” mean, exactly? And is there a difference amongst screen types and between handheld devices and other near activities, such as reading? The primary risk factor seems to be the distance between the eyes and the object viewed.
“Desktop computers seem to cause a milder increase in myopia than smartphones, which are held closer to the eyes. And books seem to be worse than desktop computers.”

What seems to matter most is the distance to the object read and the continuous duration of use. Farther is better, and frequent breaks are also beneficial.
So, what should we tell our paediatric patients? Practically speaking, the WHO guidelines for screen time still apply: no screen
“We’re not only experiencing a viral pandemic, but also a myopia pandemic.”
Femtosecond laser-based technique offers opportunities for customised manufacturing and post-implantation modification.
Cheryl Guttman Krader reports from ASCRS 2021 in Las Vegas, USA
Femtosecond laser-induced refractive index shaping (RIS) represents the future for advances in IOL technology and could be the solution for providing perfect refractive outcomes for patients undergoing cataract surgery, Susan MacDonald MD said.
“Refractive index shaping, created with the femtosecond laser, could offer the opportunity to create more sophisticated and customised optical designs that are not possible with currently available manufacturing techniques, which depend on frozen lathing or moulding processes,” Dr MacDonald said.
“In addition, RIS allows for micro-adjustments to implanted IOLs to correct residual spherical or cylindrical errors or add or remove multifocality. These postoperative modifications would reduce the burdens of managing the 20/unhappy patients.”
The RIS technique uses femtosecond laser energy within the IOL optic to create highly localised changes to the lens material’s hydrophilicity. Exposure to the laser pulses results in a photochemical reaction in which esters within the hydrophobic lens material convert into acid and alcohol groups that attract water, increasing in the lens polymer hydrophilicity.
Evidence of RIS technique efficacy is available from preclinical research that also demonstrates the procedure is highly reproducible and does not adversely affect the IOL quality. Citing experiments conducted at the John A Moran Eye Center, University of Utah, Dr MacDonald reported measurements that showed less than 98% of the lens optical transmission was preserved following the femtosecond laser treatment. Measured IOL light transmittance was 97.77% before the RIS procedure, reducing to 96.48% following the laser treatment.
The same researchers also showed modulation transfer function did not significantly change from the RIS procedure. In addition, they reported on the accuracy and repeatability of the technique for creating refractive change.
“The refractive changes are repeatable within 0.1D,” Dr MacDonald said.
This dioptric power precision contrasts with the tolerance limits for manufactured IOLs.
“We know there are many variables affecting our ability to reach our refractive target in patients undergoing cataract surgery, and we are unable to control all of them,” Dr MacDonald said.
“Variation in the power of the manufactured lens is one very important factor. For a 20D IOL, there can be a 0.2D difference between the labelled power and the actual power of the lens. This technology will change the accuracy of lenses produced.”
A lot is going on in this area of research. One approach, laserinduced refractive change index change, LIRIC (Clerio), aims to correct refractive changes in the cornea. The company believes the same approach could also work on IOLs or contact lenses. Another company, PerfectVision, is reportedly working on an approach that uses the laser to adjust an IOL after surgery.
Susan MacDonald MD is Associate Clinical Professor of Ophthalmology, Tufts School of Medicine, Boston, Massachusetts, USA. susanmacdonaldeyecorps@gmail.comMany corneal complications—including over- and undercorrection, infections, and haze—often can be avoided using careful technique and dodging known pitfalls, Jonathan B Rubenstein MD, told a session of the ASCRS Refractive Surgery Day.
This principle applies whether the technique is astigmatic keratotomy (AK), photorefractive keratectomy (PRK), or LASIK, Dr Rubenstein said.
For AK, overcorrection can be due to nomogram errors, toolong incisions, or too-central incisions, Dr Rubenstein said. He warned against trying to correct overcorrections by adding incisions at 90 degrees away from the original incisions. Correct by suturing gaping wounds instead, he advised.
AK undercorrection often results from incisions that are too short, too shallow, or made without holding the blade perpendicular to the cornea, Dr Rubenstein said. Remember, the cornea is a dome, and there must be a conscious effort to ensure the blade remains perpendicular to the cornea at all points to achieve a uniform incision at the correct depth. Inexperienced surgeons often plunge the blade in deep at first and make the cut progressively shallower, which he noted leads to under-correction.
In case of a perforation in AK, stop and suture the incision, Dr Rubenstein advised.
“You can take out the suture later and titrate the refractive result based on postoperative keratometry and refraction.”
AK infections are unusual but do occur, especially in with-therule procedures when the incisions are closer to the lid margin. Good lid hygiene and postop antibiotic drops for at least a week or until the epithelium seals are essential to help prevent infections.
AK glare can be reduced by keeping incisions peripheral and outside the 7.0 mm optic zone. Surgeons can avoid irregular astigmatism by keeping incisions paired and symmetrical, Dr Rubenstein said.
Overcorrection and undercorrection can both occur with PRK, especially in patients with higher refractive errors and older age, Dr Rubenstein said. Undercorrection may be primary or due to regression. He recommended waiting six months for refractive stability after surgery before attempting an enhancement.
For PRK cases with haze, he suggested waiting for maximal haze resolution and refractive stability before retreatment with PRK and mitomycin C. The length of postoperative steroids also can influence over- and undercorrection, with a longer course of steroids used for undercorrection and shorter course for overcorrection, he added.
Delayed epithelial healing, sometimes leading to infectious keratitis, is more common in patients with dry eye and concomitant ocular surface disease. Dr Rubenstein recommended treating ocular surface aggressively pre-operatively and not performing PRK until there is a normal surface. Smoking, diabetes, and connective tissue disease can also lead to delayed healing.
Stromal haze and scarring are more common in high refractive-error patients and those with high ultraviolet light exposure, Dr Rubenstein noted. “Warn your patients about wearing protective sunglasses after PRK.”
Haze usually peaks at one to three months and usually regresses by 12 months. If it persists, remove or scrape the haze away and treat with mitomycin C.
“Try to treat the haze with scraping only and avoid additional laser treatment because you are treating an unpredictable refractive error,” Dr Rubenstein said.
Decentred ablations are much less common with modern small-spot lasers but do occasionally happen. They often can be corrected with retreatment, especially with topographicguided ablations. Ectasia is also a risk with PRK and LASIK, Dr Rubenstein noted.
Overcorrection and undercorrection risks in LASIK are similar to PRK, though refractions usually stabilise earlier with LASIK by three months after surgery. LASIK flap complications can occur whether using a blade or a laser to cut the flap, he observed.
Irregular or incomplete flaps are possible with both technologies. Buttonholes are a larger risk with blade-created flaps. Vertical gas breakthroughs are possible with laser-created flaps. Inadequate side cuts also can cause incomplete laser flaps. Flap striae and traumatic dislocations are also possible with both.
Unrecognised occult epithelial basement membrane dystrophy is always a risk as a complication in LASIK, Dr Rubenstein said. This condition can lead to epithelial defects,
delayed surface healing, and increased risk of diffuse laminar keratitis (DLK). DLK can be treated with intensive topical steroids, but if grade III or IV, lift the flap and debride and replace the flap.

Central toxic keratopathy leads to corneal thinning and stromal loss, resulting in a central hyperopic shift. It is a noninflammatory process that can occur late after DLK or with no precursor, Dr Rubenstein said.









Epithelial ingrowth can occur as pearls or a sheet from the flap edge. To treat, lift the flap and clean both the stomal interface and under the flap surface. A tight bandage contact lens, sutures, or glue helps keep the flap in place to prevent recurrence. LASIK infections are rare, but when they occur, lift the flap, culture, and treat with appropriate antibiotics.


Pressure-induced stromal keratitis (PISK) can occur due to increased intraocular pressure and should be distinguished from corneal swelling due to inflammation—they require opposite treatments. Reduce steroids in the event of PISK, Dr Rubenstein advised. Dry eye should be treated aggressively and usually will resolve after six to 12 months when corneal nerves reinnervate the LASIK flap, he added.
Jonathan B Rubenstein MD is the Deutsch Family Professor and Chairman, Department of Ophthalmology, Rush University Medical Center, Chicago, USA. jonathan_rubenstein@rush.edu






Dermot McGrath reports from the EURETINA 2021 Virtual Congress
An important milestone in gene therapy research has been attained with the first case report of the partial recovery of visual function in a blind patient with late-stage retinitis pigmentosa (RP), according to JoséAlain Sahel MD.
“We published the report in Nature Medicine in May 2021 detailing the partial recovery of visual function in a 58-yearold patient who has been blind for 15 years and who was first diagnosed with RP 40 years ago. After optogenetics therapy, he could locate and count objects on a table and identify crosswalks in the street,” Prof Sahel reported.
RP is an inherited retinal disease with more than 100 known mutations, he explained. It causes sequential photoreceptor degeneration with a slow and irreversible evolution leading to blindness, which affects an estimated 1.5 to 2 million people worldwide.
“Once the photoreceptors have degenerated, we can try to reactivate the remaining cells using optogenetics, especially on the remaining cone photoreceptors or ganglion cells. And once everything has disappeared in terms of photoreceptors, we can try to use the remainder of the retinal circuitry to activate therapy by a prosthetic source,” he said.
In this trial, the GS030 therapy uses an optimised viral vector to express the light-sensitive opsin ChrimsonR in retinal ganglion cells. This is then combined with proprietary light-stimulating goggles to project the right wavelength and intensity of light onto the treated retina.
The patient in the case report had only light perception prior to receiving GS030. Training using the special goggles began four months after his intravitreal injection. Seven months after the start of his training, he started to report signs of visual improvement. Visual function tests showed he acquired the ability to perceive, locate, count, and touch objects when his treated eye was stimulated with the goggles. Without the goggles, he could not perform the tasks.
While the patient performed vision-oriented tasks, multichannel electroencephalography (EEG) signals showed distinct neurophysiological activity in the visual cortex, Prof Sahel said.
Prof Sahel said the 58-year-old male was one of nine patients enrolled in the ongoing PIONEER clinical trial of GS030 optogenetic therapy (GenSight Biologics). The phase 1/2a safety and tolerability study is underway at three sites: Moorfields Eye Hospital in the United Kingdom, Quinze-Vingts Hospital in France, and the University of Pittsburgh Medical Center in the United States. The work is a collaboration with Botond Roska in Basel, Switzerland, with the Institut de la Vision and sponsored by GenSight, where Dr Sahel is a co-founder.
The study population is end-stage, non-syndromic RP patients who received a single intravitreal gene therapy injection in the worst-affected eye.
Optogenetic therapies combine cellular expression of lightsensitive opsins with light stimulation using a medical device, Prof Sahel noted.
Summing up, Prof Sahel said the interim results showed the therapy was safe and well-tolerated and represented real progress for inherited retinal disease treatment.
“The clinical site in France reports visual improvement after training in real-life conditions. New tests have been implemented and existing tests modified to avoid ceiling/ flooring effects and detect improvements observed in realworld scenarios,” he said.
“The clinical site in France reports visual improvement after training in real-life conditions.”
Alot of us had virtual clinics before COVID but keeping our patients and staff safe during COVID made us rethink our clinical pathways,” Tunde Peto MD, PhD told the virtual session, “Better Patient Counselling: Using Epidemiological Evidence in Day-to-Day Clinical Practice.”
Dr Peto’s presentation provided details on how clinicians might best reduce patient time in the clinic and thus chances of COVID-19 infection while still providing top-notch care. She can speak from experience: besides working as a professor of clinical ophthalmology, Dr Peto is also the clinical lead for diabetic eye screening in Northern Ireland.
“Diabetic eye disease-related blindness is still on the rise by 8% per year, representing a very real problem for patients, caregivers, and society at large,” she reminded delegates.
As such, it is worthwhile to study the details of diabetic eye care during the pandemic. Further, diabetes mellitus is a risk factor for a more severe disease course, so avoiding infection is of utmost importance. The clinical pathways patients with diabetes must travel bring them in contact with many people, each of whom may be a source of contamination.
“What are the prerequisites for these redesigned clinical pathways? Do you have enough space, time, and trained personnel to take the images? Do you have suitably qualified, trained personnel to assess the images using a set protocol and communicate the results to the patients? And do you have dedicated time to read and analyse the images?” she asked.
Dr Peto also reminded the audience discussing these potential changes with the relevant legal team is essential, especially if implementing artificial intelligence as part of the pathway.
Upgraded equipment might even be necessary when switching from funduscopic examination at the slit lamp to imaging modalities. While many practices have fundus cameras for photographing the posterior pole, more than 10% of patients with diabetic retinopathy have clinically relevant severe disease only visible on wide-field imaging, Dr Peto said.
Appropriate triage of patients is also crucial. “Patients requiring urgent lasers or injections are not suitable for virtual clinics,” she said, as these cannot be performed virtually or with any form of social distancing.
For the remaining patients, limiting time in the clinic should be a primary goal. Dr Peto offered several suggestions, such as ringing the patient before their visit to take relevant history over the phone and having clear protocols in place for imaging so that all staff knows the requirements in all situations, such as a protocol for those patients with ungradable images.
Dr Peto urged candidates to be inventive.
“For example, use handheld cameras in dialysis clinics to identify and subsequently prioritise high-risk patients,” she suggested. “After all, 38% of patients with diabetes say that long wait times for an appointment were a barrier to eye exams.
“Well-planned, evidence-based services are the only way to prevent blindness due to diabetic eye disease,” she concluded.
Popular and prestigious video competitions such as those held at ESCRS conferences attract many entries. These competitions are a great place to win recognition for yourself and your work. But what do judges look for in a winner for a video competition? What makes a great one stand out?
Making a video for a competition is different from routine surgical videos. First, as in all good movies, the content is king. It should be interesting and informative for the entire duration of the video. Choosing a topic that you are passionate about or very good at makes your excellence shine through. A thorough review of literature is essential and can help prevent scientific or academic gaffes.
Remember that judging involves going through many videos in a short time, and therefore, it is important to make your video stand out. Making it clear within the first minute to two minutes what is trying to be discussed is crucial to retain the judges’ attention. Having a well-scripted, scientific narrative that flows from introduction through techniques; results; discussion of advantages, disadvantages, and alternatives; and finally concluding with limitations and what the future holds/should be is one great way to set out a story.
There are, of course, many other ways—and like movies, one can explore different genres of filmmaking, such as some lighthearted humour, suspense, etc., but make sure to keep it limited and not overpower the scientific content.
Various other elements need to come together for video competitions. The footage used should be of good quality, scien-
tifically and aesthetically. Well-focused, well-centred, and highresolution videos help make a good film. Equally important are clear audio and avoiding grammatical or syntax errors as well as heavy accents. Music and sound effects can add to the overall viewing experience.
Get your creative juices flowing for the opening title of your film, as a great opening makes the viewer want to delve further. Proper editing software allows great titles, exciting special effects, good transitions, and more to be incorporated. Having multiple video and audio tracks can help add visual appeal—for instance, through overlays or insets and sound effects.
Finally, read the rules for the competition and make sure to adhere strictly to them in all respects, including time limits, allowed formats, use of copyrighted material, etc. Start early and leave enough time for corrections. Getting comments from mentors, teachers, colleagues, and friends can be invaluable in enhancing the content. In addition, critically viewing the video yourself a few times can help detect errors and correct poor editing before submission. Remember the deadline and upload early enough to avoid any last-minute problems and glitches.
Happy winning!!
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India. dr_soosanj@hotmail.com
VOL: 47 ISSUE: 10 OCTOBER 2021


Blurred vision and dysphotopsias are the main complaints reported by patients dissatisfied with their multifocal IOLs, but most cases can be resolved by treating the cause of the visual disturbance, said Nick Mamalis MD in a guest editorial commemorating the 25th anniversary of the combined JCRS Journal. He notes the reported aetiologies for visual disturbances include residual ametropia, PCO, and a large pupil. Most cases are amenable to interventions such as refractive surgery, spectacles, and YAG laser capsulotomy, and IOL exchange is seldom required. The loss of contrast sensitivity can also give rise to dysphotopsias such as haloes and starbursts. Patient personality significantly affects perception and tolerance of these phenomena.




N Mamalis, “Complications of multifocal intraocular lenses: What have we learned?”; 47(10): 1256–1257.








































A new study suggests the combined biomechanical index (CBILVC) is highly sensitive and specific in distinguishing stable corneas from those with ectasia after laser vision correction. The CBI-LVC index is based on the Corneal Dynamic Response to air pressure, as recorded with the CorVis ST (Oculus) Scheimpflug camera. The retrospective, multicentre, clinical study included 736 eyes of 736 patients, 51 of whom had postLVC ectasia. The authors first used logistic regression analysis to determine the combination of corneal dynamic response parameters with the strongest correspondence to ectasia. In the validation dataset, the CBI-LVC index had a sensitivity of 93.3% and a specificity of 97.8%. The authors noted since the CBI-LVC index involves only biomechanical parameters, it can detect ectasia in eyes that have undergone laser vision correction, even when their corneas are normal in terms of topography and pachymetry.

P Vinciguerra et al., “Detection of post laser vision correction ectasia with a new combined biomechanical index “; 47(10):1314–1318.



A mobile laminar airflow (LAF) device appears to be highly effective in reducing the amount of particulate matter and lint fibres within the sterile surgical field during cataract surgery, new research suggests. In a prospective case series involving 116 patients undergoing cataract surgery, those who underwent the procedures using a mobile LAF device had a significantly greater reduction, compared to controls, in the number of airborne particles sized 0.5 mm, 1.0 mm, and 1.5 mm entering the sterile surgical field. A companion study showed that significantly fewer lint fibres fell into the sterile surgical field in eyes undergoing cataract surgery with the LAF device compared to surgeries conducted without it.
RH. Osher et al., “Purifying air over the operating field with a new mobile laminar airflow device to reduce the possibility of airborne contamination”, 47:1327–1332.




Glaukos sent a supplemental premarket approval application to the US FDA for the iStent® infinite Trabecular Micro-Bypass System. Intended for refractory glaucoma treatment, the iStent infinite Trabecular Micro-Bypass System Model iS3 is a sterile, single-use injector system preloaded with three G2-W stents and designed to deliver the stents into Schlemm’s canal. The three G2-W stents are heparin-coated and manufactured from implant-grade titanium. Once in place, the stents are designed to lower IOP by restoring the natural, physiological outflow of aqueous humour. The company’s two-stent iStent inject® W Trabecular Micro-Bypass System already received US FDA approval for reducing IOP in adult mild-to-moderate primary open-angle glaucoma patients undergoing concomitant cataract surgery.
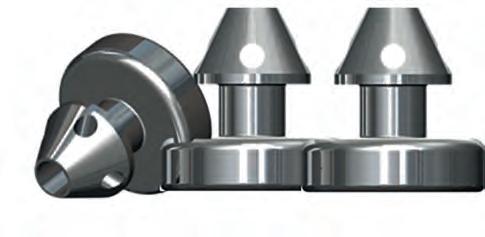
www.glaukos.com
ZEISS introduced several new products and updates in a three-day online event. The company emphasised integration of digital systems and smoothing workflow as the unifying themes, referring to the ‘ZEISS Medical Ecosystem’.
For cataract surgery, the company introduced the QUATERA® 700 phaco system featuring the QUATTRO Pump, which delivers chamber stability independent of intraocular pressure (IOP) and flow. According to the company, the QUATERA 700 increases a surgeon’s workflow efficiency from the clinic to the operating room, enabling one digitally integrated surgical workflow. Also new on the cataract front, the EYEGUIDE® patient software application, designed to help patients and clinics stay connected through the entire cataract treatment process. An app for surgeons, the Surgery Optimizer application provides a way to utilise surgical videos to enable selftraining of physicians and standardization of surgical techniques. Speakers also presented the latest information on the new aspheric CT LUCIA 621 monofocal along with the OPTIKIT, a customizable surgical pack.
Haag-Streit announced the launch of its Swiss-engineered MR Q Combo device in the UK market. The space-saving MR Q Combo is a specially designed slit lamp offering the option to safely combine the MR Q YAG 1064nm laser with either a Merilas 532a, Merilas 532nm, or Merilas 577nm short pulse laser. The latter of the two configurations deliver microsecond pulses for subthreshold retinal treatments. Safe handling of the two lasers is ensured by the specially designed slit lamp adapter.
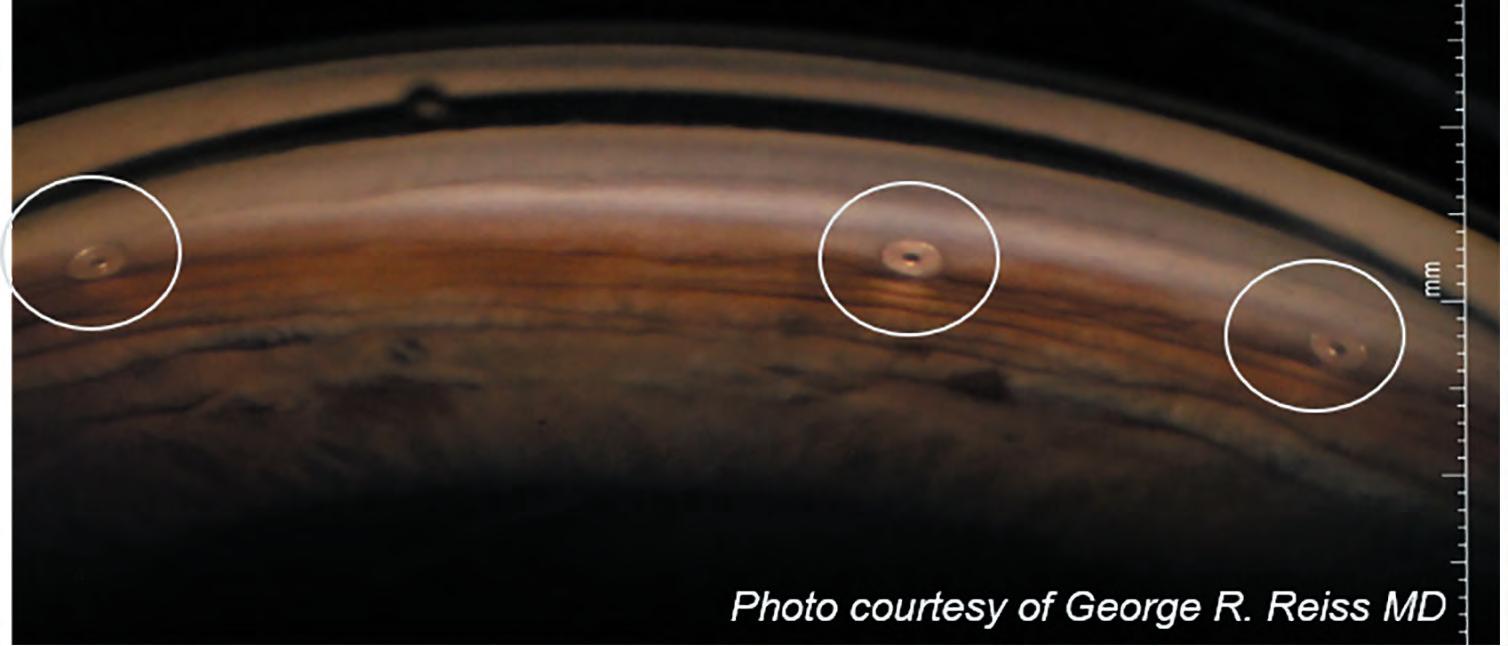
https://hsuk.co/MRQ
“It is our mission to contribute to the progress of medicine, enabling more efficient and cost-effective treatments and providing access to high-quality medical care to as many people as possible. Our investment in digital technology will continue to make the adoption of digitalization easy and intuitive,” said Dr Ludwin Monz, President and CEO of Carl Zeiss Meditec AG.
www.zeiss.com/med
Support, encourage, and fund individuals interested to start clinical research activities in the eld of cataract and refractive surgery
Introduce and develop a body of clinical research work, addressing a challenging “problem” in order to devise a practical “solution”
Facilitate and support an independent culture of study for the ultimate bene t of patients
Announcement of 2021/2022 Pioneer Award
Meeting
http://pioneeraward.escrs.org
Digital media in all its forms has become the most widely used means of communication, education, entertainment, and marketing. It has certainly come to play a key role in ophthalmology. I personally like using digital media as an educational tool, harnessing YouTube, messaging apps, and my social media handles to transmit information. My YouTube educational channel has more than 10,000 subscribers. It is my favourite since I get to do something I am passionate about—teaching and demonstrating surgical techniques!
Video-based education has many advantages. The entire surgical concept can be presented in a clearly and crisply. The video, or a part of it, can be repeatedly viewed if required. The surgeon’s explanations for the surgical choices made or the events that happened can be understood. If recorded through the surgical microscope, the viewer gets the surgeon’s view. Creating a video and making it educational and useful to the viewer needs preparation and time. In this article, I will discuss some tips on preparing good surgical videos and optimizing them for streaming.
If planning to demonstrate a routine surgery, a case may often be picked from the surgical list for the day. If a special type of cataract or a particular surgical manoeuvre is planned as a video, it may be necessary to wait till a suitable case presents. For videos on complex cases, planning starts right in the clinic while seeing the patient and deciding management.
It is good practice to keep the recorder on for all cases when facilities are available to get videos on a wide variety of situations, both planned and unplanned. Often rare and interesting videos get captured when something unanticipated happens while operating.
When planning to demonstrate a routine manoeuvre, it helps to select a good case, for instance, a cooperative patient, an eye that is not deep set, a clear cornea, and a well-dilated pupil.
A superior quality surgical microscope with clear optics and good coaxial lighting is essential in making high quality anterior and posterior segment videos. An understanding of the coaxial and paraxial lights—as well as the balance to be maintained between them—is necessary since the coaxial gives a good red
reflex, thereby making the rhexis, cortical aspiration, and margins of a PCR clearly visible. On the other hand, the paraxial gives a larger view of the operating field while also giving better depth perception due to the shadows created from the slightly off-centred light.
The Monoglots is a stereo-coaxial red reflex device—an accessory designed by Jagdeep Kakadia that can enhance the red reflex of lower-end microscopes. Extra-ocular surgeries need special tactics while recording. Though these may be recorded under the microscope (the author personally prefers recording strabismus, lid surgeries, and even blow-out fracture repairs using the surgical microscope), there is some loss of freedom of movement. To avoid this, and for those accustomed to operating through surgical loupes, a camera fixed on a tripod can give excellent results.
Kruger et al have described an excellent and simple technique of attaching a divergent lens just below the objective of the operating microscope, thus increasing the working distance while still allowing high-quality recording through the microscope. For any recording, it is essential to get clean, in-focus images that show the entire operating field. Mediocre quality, low-resolution, outof-focus video with inadequate zoom, show of gloves in the field, etc., distract from the object of the video.
A good video very often does not end with surgery but also shows postoperative outcomes. Therefore, it is useful to have a good slit-lamp image capturing system to take pre- and postoperative photographs. Surgeons can use any of the excellent commercial systems available, such as those from Appasamy Associates or Haag-Streit. The videos can also be made very inexpensively using a slit-lamp adapter and a smartphone camera.

Many of the new higher-end microscopes have built-in cameras and the output can be recorded on an HD recorder. Alternately, an external camera may be connected to the beam splitter using a C-mount. High-quality 3-chip HD-cameras (e.g., Sony MCC-500MD) give excellent output but do add to cost. New and simple attachments are also available that can be connected both to the video output port of the microscope and to a smart phone camera for surgeries to be recorded, shared, and even streamed live.
There are many editing software programmes available—e.g., Pinnacle, iMovie, Wondershare Filmora®—which are user-friendly and easy to learn. For those who like to add an extra finish to their videos, there are more sophisticated software programmes such as Final Cut Pro and Adobe Premiere.
Software such as Adobe Photoshop, MS Paint, PowerPoint, and even many smartphone apps are available to create still graphics for the video.

Adding a voiceover helps greatly. Make sure to give clear and crisp narration. Adding some background music also adds to the video’s appeal; however, it should not be overpowering or drown the narration.
Finally, the entire video should be crisp and to the point so as not to waste the viewer’s time or lose attention. Once done, the output can be saved in many formats depending on the intended use. When sharing on messaging apps, there is generally an upper limit to the file size accepted. In addition, when viewing is intended for a small screen such as a mobile phone or requires downloading before watching, a smaller size, lower resolution video is desirable. If uploading to YouTube, higher resolution keeps the image clear, irrespective of the screen size.


As mentioned earlier, videos may be shared on many platforms, including YouTube, Vimeo, Facebook, WhatsApp, and LinkedIn. YouTube has many advantages. It is free, and if one has a Google account, is quite easy and intuitive to begin with. It is a good idea to share the link, short URL, or QR code (for example, the QR code shared in this EuroTimes article!) with the intended audience through social media handles and direct messaging. Adding a description and keywords and encouraging viewers to subscribe helps spread the video faster and makes it more searchable.
Remember that educational ophthalmic videos need not always be surgical. There are excellent opportunities for making nonsurgical teaching videos with the cases seen in the clinic daily. Videos can also be a combination of clinical and surgical tips. Use the format for scientific articles such as reviewing literature, discussing a new technique, showing results with the new technique—adding a discussion that includes advantages and disadvantages—and ending with a conclusion.
Discussion with peers on current topics of interest both clinical and non-clinical such as balancing work-life, starting a new practice, navigating through the COVID crisis, educational videos for patients or staff—all make for interesting viewing and can have a far-reaching audience.
There are many video types and formats, making it possible for anyone to create videos. So, don’t wait any longer! Whatever you may be doing, whatever it is that you are passionate about—now is a wonderful time to grab a camera and start making videos.
SFO Autumn E-Congress
6 November Virtual Meeting https://www.sfo.asso.fr/
NOVEMBER
AAO 2021: Re/Create 12 – 15 November

New Orleans, Louisiana, USA https://www.aao.org/annual-meeting

FEBRUARY
26th ESCRS Winter Meeting
18 – 20 February Vilamoura, Portugal https://wintermeeting.escrs.org/

18
www.haag-streit.com

Fundus image acquisition with macula and disc capture in one image on OCT, for enhanced screening and clinical efficiency

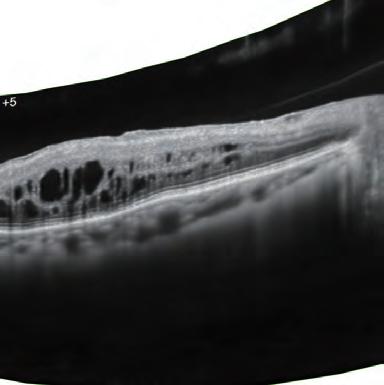

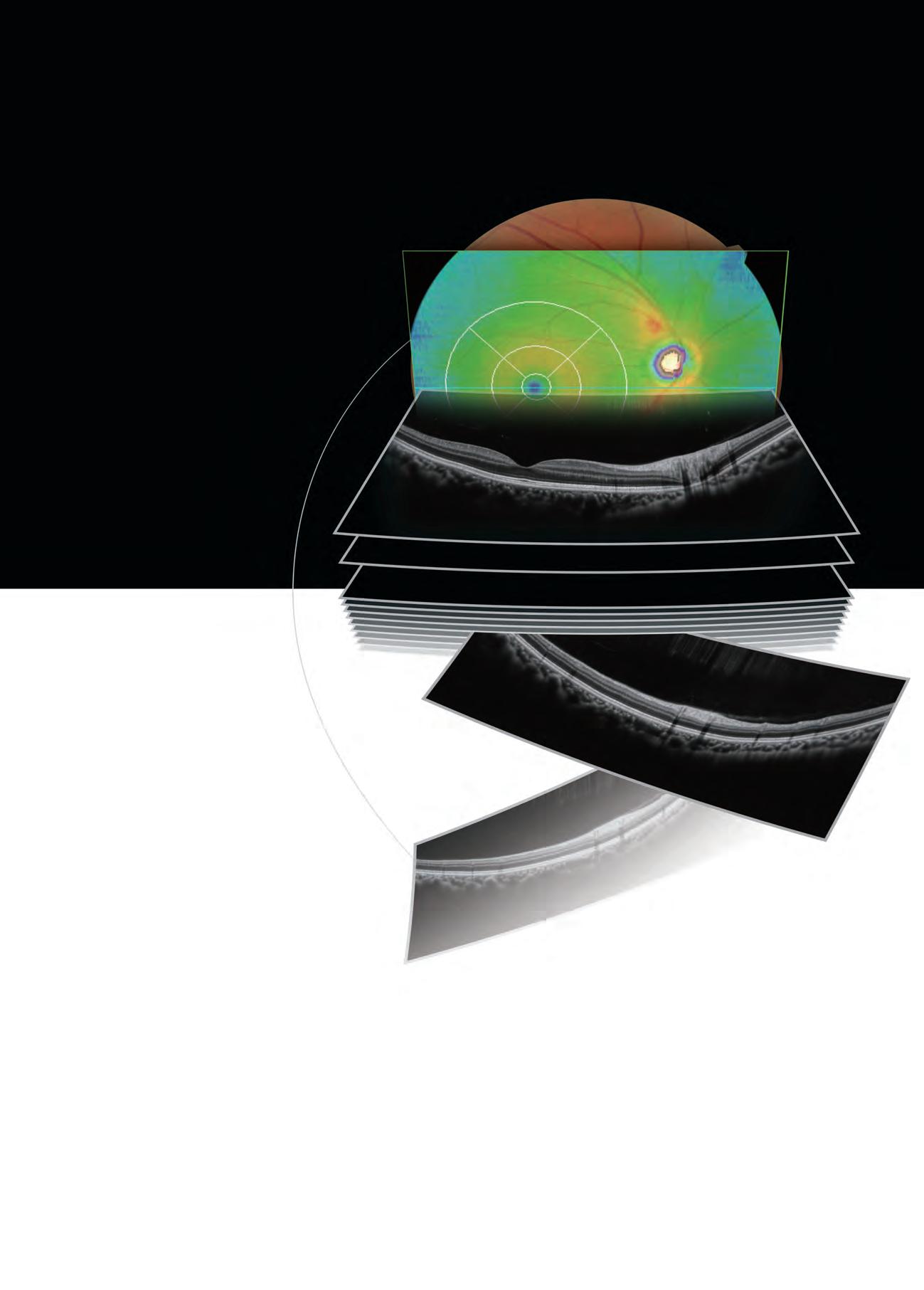
Standard model







Widefield image capture in a single shot
High definition OCT image for all scans


