


About The Epic Almanac

You’re holding the first volume of the Epic Almanac, a compendium of knowledge designed to give you an inside look at the important work happening across the Epic community, programs that are available to help you, and some fun facts about Epic. We hope to publish a new volume each summer, in time for UGM. Like the Farmers’ Almanac, we hope it’ll give you an idea of where the winds are blowing so you can plan for the seasons ahead.
Our Team
WRITING
Anna Cacciaglia
Anna Losacano
Cassie Feltz
Celia Groff
Dan Seeger
Eric Rieth
Jesse Atkins
Jonathan Carroll
Kelly Conne
Kyle McCaffrey
Lucca Hermes
Peter Jorsch
Philosophy Walker
Rachel Salter
Shashank Raghu
Shawn Kiesau
Tim Rebholz
EDITING
Anna Siferd
Ashley Gibson
David Jalensky
Elle Kemp
Hannah Ostrow
Judy Faulkner
Leela Vaughn
DESIGN
Emily Korsmo
PHOTOGRAPHY
Matt Debnar
2023–2024 Edition | 1
VOLUME 1 | 2023–2024 EDITION 2 How Healthcare Organizations Are Using Epic to Address the Nurse Shortage 6 Epic Emeriti Share What They’ve Learned from Decades of Healthcare Experience 10 Epic Helps Write a New Chapter for Amélie 14 A Look Inside Epic’s Campus 20 Ninjas and Power Hours: Strategies for Taming the In Basket 26 New Frontiers: Toward a More Unified Healthcare System 32 Specialty Steering Boards: Networking, Camaraderie, and Getting Things Done 36 Clinical Informatics 101: Designing Residencies That Grow New Physicians into HIT Leaders and Epic Experts 40 What's in a Name? 42 Strong Epic Users Start with Great Training 46 Getting Ahead of Trends in the U.S. Regulatory Landscape 48 Art at Epic 50 We’ve Got You Covered 52 An Epic Recipe 53 Rooted in Sustainability
to the resources mentioned in this issue can be found by scanning the QR code
Illustration
In This Issue
Links
below.
by Tommy Washbush
Contact Us TheEpicAlmanac@epic.com
How Healthcare Organizations Are Using Epic to Address the Nurse Shortage

Virtual nurses, team-based care models, and Epic efficiency tools are helping fill the gap.
The long-predicted nurse staffing shortage is impacting organizations around the country.1 Median nursing tenure dropped by 19.5% from 2021 to 2022, with the greatest number of shifts filled by nurses with less than one year of tenure.2
To address this crisis, organizations are taking creative and innovative approaches. They’re pairing new staffing strategies with technology available in Epic to meet patient care demands and keep nurses satisfied with their work. 1 U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, and National Center for Health Workforce Analysis (July 21, 2017). Supply and Demand Projections of the Nursing Workforce: 2014-2030. 2 Epic Research (June 2, 2020).
2 | The Epic Almanac
‘The New Nurse’ Is the New Normal. Epic Research.
Photo: Shutterstock
UnityPoint Health created a virtual nursing team staffed by a dozen experienced nurses who provide extra support for bedside nurses. Virtual nurses complete admission questionnaires in Epic, review education materials with patients and their families prior to discharge, and act as a second set of eyes during highrisk medication administration and procedures.
Bedside nurses save an average of 12 minutes per admission and 15 to 29 minutes per discharge, and feedback from patients and both bedside and virtual nurses has been positive.
How they did it:
► Repurposed tele-hospitalist carts into virtual nurse carts that include cameras and speakers, allowing virtual nurses to support patient care anywhere in the hospital.
► Placed high-definition cameras in each patient room so virtual nurses can clearly monitor patients when they’re asked to “enter” the room and support bedside nurses.
► Scaled the program to support 12 hospitals and 34 inpatient med-surg units across the health system.
For more information, check out UnityPoint’s story on EpicShare.org.
Trinity Health
Our care ministry crosses 26 states, and the cultures locally are all different. We work to find commonality of purpose and direction while recognizing the local nuances. When something works well at one facility, we reflect on how to leverage what we learned and scale it to raise all boats across our organization. Effective change must include the right mix of people, process, technology, and culture all working together. You can’t work effectively as an organization if you leave any of these elements out.
— Michael Slubowski President and CEO
We’ve seen our virtual nursing program become a great nurse retention tool that keeps our seasoned nurses’ knowledge and expertise within the organization and helps grow a new generation of nurses. One of our nurses who has been here for 20 years moved from our acute rehab department to the virtual nursing program, which has brought in a whole new era of her career. She is engaged and excited and is using all the wisdom and experience that she has built over so many years.
— Sarah Brown, RN, MSN, CMPE, NEA-BC Chief Nursing Officer at UnityPoint Health – Waterloo
Trinity Health designed a new care team model to maximize experienced nurses’ time and support and retain newer nurses. Newer nurses are paired with a care partner, such as an LPN or nursing assistant, and an experienced virtual nurse, creating a trifecta that they call “TogetherTeam.”
The more experienced nurses help guide patient care and provide mentorship to the newer nurses.
Patient, family, and nurse satisfaction measurements all improved. They are scaling this new care team model to 88 hospitals spanning 26 states
How they did it:
► Assigned remote nurses so bedside nurses could focus on in-person tasks, like medication administration. Using high-definition cameras, remote nurses can even review infusion pumps and document skin exams in Epic.
► Care partners take on care duties that don’t require a nursing license so that the nurses can practice at the top of their license.
► Remote nurses provide discharge education from a screen in the room and take additional time to answer patient and family questions.
For more information, check out Trinity Health’s story on EpicShare.org
2023–2024 Edition | 3 How Healthcare Organizations Are Using Epic to Address the Nurse Shortage
Health
UnityPoint
Kaiser Permanente, Northwest Region
We know that [the nursing] field is hard. We have to reduce the cognitive load and make documentation less stressful for nurses. When they’re in moral distress over what’s happening out there, every extra task adds to what they’re carrying. I am extremely protective of our nurses and their work, and I’ll do anything I can to help them. When they feel that level of support and they know that any changes we’re making are for a good reason, that creates greater nurse happiness.
— Meredith Farrell, RN, MSN, RNBC Lead Nurse Informaticist at Kaiser Permanente Northwest
Bronson Healthcare paired recent graduate nurses with mentors and offered targeted training for complex workflows as part of a program to improve nurse job satisfaction. They grew the pool of experts with quarterly training sessions for nurses who demonstrated strong skills with the system and then assigned those nurses to work with newcomers to the organization.
They achieved a 10 percentagepoint reduction in first-year nurse turnover from 17% to 7% between 2019 and 2020.
Kaiser Permanente, Northwest Region shares data from Epic’s Nursing Efficiency Assessment Tool (NEAT) directly with nurses so they can see where they stand. Seeing the data helped nurses start thinking about ways they could make the system work better for them, and their resulting suggestions were incorporated into system changes.
They saved an average of three minutes per nurse, per shift Nurse job satisfaction numbers improved dramatically, and nurses took more ownership of suggesting changes and optimizing their use of recommended tools in Epic.
How they did it:
► Presented efficiency data from NEAT in one-on-one conversations with nurses and asked the nurses to help identify specific things in the system that slowed them down.
► Created targeted training opportunities for nurses and made the lessons available to all.
► Incorporated nurse feedback into the decision-making process around system changes.
For more information, check out UGM 2022 Executive Breakout 23 on sessions.epic.com
How they did it:
► Reviewed system efficiency data gathered from NEAT and identified the nurses who used Epic most efficiently to act as mentors to newer nurses.
► Organized shift schedules strategically to ensure that newly graduated nurses worked at the same time and in the same space as their mentors.
► Created short videos that covered efficiency topics and added them to the Learning Home Dashboard in Epic so nurses could review them when they had time.
New nurses want good mentors, people to show them the best way and grow them in their career. You need those relationships, the feeling of belonging on the unit, to have a high-functioning team. Investment in new nurses is always worthwhile. We’ll never eliminate turnover completely, but this program speaks to how we value employees and their growth.
— Jacqulynn Maher, MSN, RN Chief Nurse Manager of Talent Development
For more information, check out Bronson Healthcare's story on EpicShare.org
4 | The Epic Almanac
Bronson Healthcare
The Guthrie Clinic looked across the trends in supply and demand for nursing care hours and saw that it just didn’t add up—there was a far higher need for patient care than they could provide using traditional staffing models. They designed a teambased model that distributes nursing work across both licensed and unlicensed care team members. To help support newer nurses—78% of nurses on one critical care unit at Guthrie had less than three years of experience—they established a centralized team of remote, experienced clinicians who support bedside care.
The new model resulted in a drop in hospital-acquired infections for patients and an improvement in nurse-reported job satisfaction. The amount of time it takes to get nurses to
dual-verify high-risk medications in Epic dropped from 22-36 minutes to 90 seconds
How they did it:
► Focused on hiring LPNs to round out the team-based care model because they can complete a degree in less than a year and are certified to handle a wide array of patient care tasks.
► Created the Pulse Center, a large virtual call center staffed with nurses, telemetry techs, and others who nurses can reach out to for assistance.
► Transitioned some documentation and high-risk medication verification to the virtual nurses, who also act as a second set of eyes for procedures like Foley catheter insertion.
We all know that innovation is key to the future, and we absolutely understand that investment is needed pave a new path. We can’t let bureaucracy slow us down. A critical piece of that path is building a resilient, sustainable workforce. Every single month, I reduce the number of travel nurses needed because more and more people are attracted to come here. The money I save from the reduction of travelers’ agency staff adds to our investment in our teams and technology.
— Deb Raupers, MSN, RN, CENP EVP/Chief Nurse Executive
For more information, check out The Guthrie Clinic's story on EpicShare.org
Written by Dan Seeger
Action List: Identify opportunities to improve nursing efficiency
Ask your Epic representative for your data from the Nursing Efficiency Assessment Tool (NEAT) and share it directly with nurses.
Review the report created by the Care Plan Utilization utility to identify and remove unused care plans and details that nurses document in other places.
Implement a Thrive After Go-Live program to provide nurses with training on efficient use of Epic.
Links
resources:

2023–2024 Edition | 5 How Healthcare Organizations Are Using Epic to Address the Nurse Shortage
The Guthrie Clinic
Use data from NEAT to identify flowsheets where nurses are spending an above-average amount of time and evaluate whether you can streamline associated flowsheet template content or enable Epic features to automate portions of the process. to
Epic Emeriti Share What They’ve Learned from Decades of Healthcare Experience
Through Epic’s Emeritus Program, former executives and clinicians partner with Epic organizations to do anything from providing extra hands for an implementation to filling an interim executive position. They offer flexible expertise, critical guidance, and a nuanced understanding of how to navigate the business of healthcare.

Amy Maneker, MD
I went to a medical school that taught us to change the world, to go beyond seeing one patient at a time, and I fully bought into that mindset. After my residency and fellowship, I started at a health system in Cleveland, Ohio, where the administration routinely asked me to organize things, which I’m very good at—it’s a family specialty. I picked up skills like coding, billing, and running satellite emergency departments, but I didn’t have a passion for it, and I certainly didn’t feel like I was changing the world.
Around 15 years ago, the health system I was working for started implementing an EHR. I was asked to help support it, and I had an epiphany: this is what will drive change. Now, when someone asks what I do, I answer, “I leverage data to improve the quality and value of healthcare.”
To that end, I eventually became the CMIO of a
children’s hospital six months before they went live with Epic.
Bob Wachter, who is often called the father of hospital medicine, said, “Early in your career, you say yes to everything, and late in your career, you say no to everything.” I’m the opposite. After several years as CMIO, I decided to just say yes to every opportunity. So, around 2018, I became an Emeritus, which keeps me connected to Epic and working on some interesting projects—mostly implementing Epic at large organizations. For example, I got to go back to my hometown and support New York Health + Hospitals .
At these go-lives, I do all kinds of different things. A CMIO has to see everything from a very high level, but as an Emeritus, I can get really in the weeds on a go-live. I can help with build, support physician personalization, identify upstream issues and fix processes, or provide broader insights based on my experience. I can act as a neutral third
6 | The Epic Almanac
Epic organizations turn to experienced healthcare leaders for help navigating technical and organizational change—from Epic go-lives to organizational transformation and expansion.
Over the course of the past year, I’ve seen five different organizations and how they approach and solve problems, which is more than I ever would’ve seen as a CMIO.
party and work with the executive team to say, “I’m not telling you you’re wrong, but consider this.” At the end of the day, I’m just there to help and do what I can.
I’m continuing to learn as an Emeritus. During one go-live, I worked with eight physician informaticists who provided virtual support to users from a central command center. That was a really unique approach—I’d never heard of it, and I don’t know how they came up with the idea—but it was great! Over the course of the past year, I’ve seen five different organizations and how they approach and solve problems, which is more than I ever would’ve seen as a CMIO.
When people have an Emeritus come in, they realize the value. It’s not just that I know where to click, it’s that I’ve been there, done that. People have to leverage us appropriately, though. I’m fine walking into a go-live to pitch in wherever, but CMIOs can get a lot more value from me if we can have a conversation beforehand and figure out where I best fit in to help them change the world through healthcare.
first so I could act as the glue between users and analysts. I eventually retired, but I had no intention of stopping working. Now, as an Epic Emeritus, I continue to enjoy being involved, helping organizations, and helping Epic understand what their community partners need—even sometimes being constructively critical of the way Epic does things.
Jay Eisenberg, MD, MMI, and Bob Warren, MD, PhD, MPH
Jay: I started with informatics work when I was in my clinical years—in the ‘90s, pre-EHR—making decisions about systems and technology. Then, as a hybrid physician-executive-implementer, I got experience with transforming care at large organizations. I later become a CMIO and faced my first Epic implementation at a system in southwest Washington state. I chose to learn Epic build
And it doesn’t hurt that now, when people ask me how much I work, I can answer, “about one week per quarter.”
Bob: I’ve been doing Epic since about 2005. I’m a certified Physician Builder and Power User, and I worked as a CMIO at both Texas Children’s Hospital and the Medical University of South Carolina. I directed the implementation of Epic while getting physicians to embrace the change, which eventually led to a focus on governance around both implementation and ongoing optimization. Like Jay, I figured out I wasn’t done after retiring, so I got engaged with the Emeritus Program. I joined after I retired in 2018, and as an Emeritus, I have supported many go-lives, mentored customer leaders, and served as an interim CMIO for much of 2020. But a key thought: the critical skill set of an Emeritus isn’t necessarily technical; it’s working with people and figuring out how to help them get to where they want to be.

So, Emeritus work can be truly innovative and “out of the box.” A great example is the 2022 joint Emeritus project that Jay and I had the privilege to

2023–2024 Edition | 7 Epic Emeriti Share What They’ve Learned from Decades of Healthcare Experience
The critical skill set of an Emeritus isn’t necessarily technical; it’s working with people and figuring out how to help them get to where they want to be.
work on. Our involvement in this project started back at UGM in 2021, on a shuttle bus when the CIO of a university hospital happened to sit next to me, and we started chatting. His organization was looking to build a clinical informatics team, but they weren’t sold on the bids they’d received from a consulting firm. I then introduced him to the Epic Emeritus Program, which led to a phone call with him, the hospital’s CHIO, the Epic Emeritus Program lead, and Jay and me.
Jay: The CIO and CHIO were interested in using the Emeritus Program, but they wanted to hear how we’d approach the project. We emphasized the length and breadth of experience that CMIO Emeriti can offer for creating and using informatics teams successfully that a typical consulting company might not. In this case, they’d even have two heads put together to compare and contrast experiences.
Bob: Their CIO and CHIO were also wary about simply being handed a ready-made product. They instead wanted a solution that they helped build and would then own, implement, and improve after we departed; in other words, they wanted to learn how to fish, not a seafood dinner. And that’s exactly what Jay and I wanted to do: teach them how to fish.
Jay: The organization engaged us to help them build a clinical informatics team. The project lead saw other organizations with teams of 20-plus people while he didn’t have anybody else. He wanted to learn what that looks like: how should a team be structured? What would team members do? What should a charter say? So, we partnered with the CHIO and others to build a charter with job descriptions, proposed budgets, and a plan for personnel involvement.
Bob: Jay and I learned while conducting background leader interviews for the charter that there were also great opportunities to advance IT governance and project prioritization, such that it would mirror prioritization of work throughout

the organization. We offered our ideas for the CHIO to refine and incorporate into the informatics team design, which he presented to very receptive colleagues and executive leaders.
Jay: Circumstances prevented them from establishing a clinical informatics team at the time, but Bob and I didn’t want to abandon the project lead. After wrapping up our engagement as Emeriti, we chose to continue to help and mentor him. Now, as soon as he gets the go ahead, their team has a threeyear plan to get to where they want to be.
Peter Churgin, MD
My involvement with Epic started when I was working as a physician in Arizona attending a demo for this new EHR technology. When I saw the system warn a user who tried to order penicillin for a patient who was allergic to it, I leapt to my feet and exclaimed, “Sign me up! This is a great idea.”
Twenty-some years later, I’m still enthusiastically working with Epic. When the Emeritus Program launched, I had already worked with at least a dozen large Epic organizations at that time, and so it felt like a great fit for me. I like being a free agent, both helping the organization and helping Epic by calling out when I think there’s a better solution on either side.
One of my more memorable experiences as an Emeritus came from Orlando Health. They were integrating a large orthopaedics group that was highly respected in the community, and while Orlando Health had been live on Epic for a few years, the orthopaedics group had its own homegrown software—developed by its then-current physician lead—that was still working well. Orlando’s CMIO was looking for help in showing the orthopaedic group the benefits to an integrated system and that they could, in fact, learn and adapt to new software.
8 | The Epic Almanac
One of the first things I did was to meet with the CMIO and request a partner from within Orlando Health who knows Epic's orthopaedics application, Bones, well, and is good at using it. I knew a peer could help me spread good cheer and show that workflows had new and powerful options while still allowing the specialists to see 30 or 40 patients a day. We found a physician assistant who was a highly enthusiastic and skilled Epic user. Soon, folks started saying, “This doesn’t look so hard. I can handle this.”
Time and again, I’ve found that one of the most successful strategies to bring people on board is to make them builders. After a few months of working together, the lead physician at the orthopaedics group could sit side by side
Action List: Learn how an Emeritus could help your organization
Read more about the types of engagements on the Epic Emeriti Program white paper on Galaxy.
Ask specific questions about programs or Emeriti, including how to begin an engagement of your own, by contacting emeritusepicteam@epic.com
Contact emeritusepicteam@epic.com if you’re interested in becoming an Emeritus with Epic.
and build SmartSets with me. That required an enthusiasm for the software’s—and the organization’s—success that was a complete shift from the start of the merger.
Another role of the Emeriti is to work with one or more people at the organization who will continue to share our expertise and enthusiasm after we’ve left. In this case, my physician assistant partner is now a certified Physician Builder and trainer and an excellent replacement for me. Looking back, the many obstacles to making the merger a success also made this an exciting Emeritus engagement for me; however, I’m even more excited to see what successes my friends at Orlando Health achieve with an integrated EHR. •
Interviewed by Jonathan Carroll
Learn more about the engagements discussed in this article by contacting the Emeritus involved with each:
► Amy Maneker: amaneker@epic.com
► Bob Warren: bwarren@epic.com
► Jay Eisenberg: jeisenbe@epic.com
► Peter Churgin: pchurgin@epic.com
Links to resources:

2023–2024 Edition | 9 Epic Emeriti Share What They’ve Learned from Decades of Healthcare Experience
Another role of the Emeriti is to work with one or more people at the organization who will continue to share our expertise and enthusiasm after we’ve left.

Epic Helps Write a New Chapter for Amélie
Lesley Chan is a midwife and mother of four who lives in Manchester, England. Her youngest daughter, 18-year-old Amélie, was born deaf and blind with a rare genetic disorder and has other profound disabilities that require 24/7 care. Until recently, Amélie’s medical records were stored on paper—about 22 volumes from five different hospitals. Because it was impossible to review her entire history before every visit, it sometimes felt like doctors didn’t really know Amélie, and the burden was often on Lesley and her husband to explain Amélie’s entire medical history.
“If it's not her lead consultant seeing us that day, I have to relay everything,” Lesley said. “So I tell them about all of her conditions. I have to go back through it all in my brain, and that just triggers sadness, really. I get a bit frustrated because I think, ‘I'm here today for 15 minutes to talk about this specific issue. But now I've got to talk about
her whole history and everything that's gone before.’ Now that she’s 18 with a long history of surgeries and things that have happened to her, it's massive. After explaining all of that history, I worry I’ve forgotten something important.”
Lesley also used to keep a diary on her phone to record notes about previous visits to the doctor and details of the medications Amélie was taking. There were many times when doctors didn’t have the paper notes in time for the visit, and Lesley was the only one who could provide them with crucial information.
In the past, doctors who were new to working with Amélie often entered the room and started speaking to her—“Hi, Amélie, how are you today?”—not realizing she couldn’t hear them or talk back. That frustrated Lesley because it showed that they hadn’t even read the most basic notes about her daughter.
2023–2024 Edition | 11
Opposite: Amélie Chan with her parents, Lesley and Darren, at their home in Manchester, England.
A mom shares her story about how caring for her daughter, who has profound disabilities, has been transformed by using EpicCare and MyChart.
Epic Helps Write a New Chapter for Amélie
After Manchester University NHS Foundation Trust transitioned to Epic, Lesley experienced an eye-opening moment. She brought Amélie to a visit with a doctor who’d never seen her before, and when the doctor entered the room she said, “I’m really sorry, I don’t know any sign language, so I won’t be able to communicate directly with Amélie.” In the entire 18 years of Amélie’s life, nobody had ever started with that because they didn’t know her history or understand that she couldn’t see or hear them. The fact that the doctor could see this information at a glance (along with notes that Amélie still has some peripheral vision and the ability to use British Sign Language) and read it before the visit made Lesley feel like the doctor
was personalizing Amélie’s care, understanding her, and paying attention to her as a human being.
With the transition to Epic, Manchester launched MyChart (MyMFT), which gives Lesley more timely information about her daughter's care. When Amélie contracted COVID-19, it was important for her to start medication right away because she was at greater risk of complications due to having chronic lung disease and using oxygen. Lesley had been waiting several hours for a call back from the hospital about
whether the drug was available and to see whether Amélie could get in during the small window of time when it had to be administered. She received a notification on her phone through MyChart



12 | The Epic Almanac
“Being able to review Amélie’s information and update it in the portal just makes me feel like I’m a part of the care, not ‘we are the clinician, you are the patient.’”
The hospital has become Amélie’s home away from home as she receives care for her complex medical conditions.
that a time had been assigned for Amélie. After Amélie was in the hospital and had received the treatment, Lesley was again waiting to hear back from clinicians. She had been told that if Amélie’s bloodwork came back normal and the treatment had gone well without any issues, Amélie could go home for the day. Lesley received Amélie’s test results through MyChart, and by the time a nurse was able to stop by a couple of hours later, they were already packed and ready to head out. The nurse hadn’t seen the test results yet herself— MyChart was getting information to patients in real time, even while clinicians were busy with other things.
“Being able to review Amélie’s information and update it in the portal just makes me feel like I’m a part of the care, not ‘we are the clinician, you are the patient,’” Lesley said. “It feels like more of a team effort now.”
Having MyChart has also made managing Amélie’s care so much easier for Lesley and her
family. She and her husband no longer worry about letters lost in the mail or delayed due to postal strikes, misplaced paperwork, or having to spend hours on the phone to try to get through to someone at the clinic.
“My husband and I used to find ourselves in silly arguments about who put the mail where or whether we’d written down an appointment, and that used to drive me mad,” Lesley said. “We don’t need to have those conversations anymore.”
When a new appointment is scheduled for Amélie or a new medication is prescribed, everyone in the family, including Amélie’s three sisters, can see that through MyChart, so everyone involved with Amélie’s care is kept up to date and can help when needed.

“MyChart has given us the tools to work smarter at home and manage her care together,” Lesley said. “I can’t explain the absolute ease of it. It has just been life-changing.” •
Written by Cassie Feltz
2023–2024 Edition | 13 Epic Helps Write a New Chapter for Amélie
Amélie’s three sisters all have proxy access in MyChart to help with her care.
I nside Epic’s ALook Campus
Journey through time and space to learn how we got here.

Today, Epic’s campus sits on 1,670 acres of Wisconsin farmland, with 83 buildings, 1 treehouse, and 2 slides. But we began in 1979 in a much smaller space: the basement of 2020 University Avenue in Madison with just 1.5 employees.
Humble roots (in the basement)
2020 University Avenue • 1979-1986


1.5-18 EMPLOYEES
Our first office was small, with just two rooms in the basement of an apartment building at 2020 University Avenue. The space was a good business incubator—Subject Index, which later became the Pleasant Company, made American Girl dolls and had an office next door. We had a 50 MB disk drive that looked like a washing machine. You couldn’t get close to it, or the data would be corrupted.

We painted our large, used, metal desks purple, put up hanging plants, and painted the walls in bright colors. When Subject Index moved out, we took over its office space and bought its old furniture. It looked so nice that people thought we were a marketing company.
Glass and brass vs. peace and quiet
When we outgrew our basement office, we had to choose between two places to move into—one was a “glass and brass” techy-looking building with lots of open space, and the other was an old French Provincial–looking building with lots of individual rooms.
We thought about how programmers often work. You wake up with your head filled with ideas, run to the computer, and program and program in peace and quiet until you realize you’re starving and need to eat. We wanted to create that kind of environment for our staff—a place that’s comfortable and friendly to be in, where you can close the door, have quiet, and be able to think (with food nearby). We chose the place with the many rooms and fireplaces on Medical Circle, and in December 1986, we moved in.
A cozy compromise
5609 Medical Circle • 1986-1994
18-73 EMPLOYEES
By the time we moved into our portion of the Medical Circle building, we had outgrown it. We were able to extend to other sections of the building, but we realized we needed something bigger, and that meant buying a building of our own.
But one of our customers from the South wouldn’t hear of it. “You can’t move,” he said. He loved that the Medical Circle office had fireplaces in the conference rooms and insisted that we had to stay there because those fireplaces kept him warm when he came to visit during the chilly Wisconsin winters.
“Make you a deal,” we said. “We'll put fireplaces in the conference rooms if you let us move.” He agreed.
2023–2024 Edition | 15
Epic’s first office in the basement of an apartment building on University Avenue, Madison, WI.
Epic’s second home at 5609 Medical Circle.
Computers in the Medical Circle building circa 1985.
A Look Inside Epic's Campus
Opposite: The Farm Campus welcomes visitors to our current home: Epic's Intergalactic Headquarters in Verona, WI.
Good bones and a great bargain
5301 Tokay Boulevard • 1994-2006
73-2,550 EMPLOYEES
We found an old school on Tokay Boulevard that we thought would work well. It had been damaged in a fire in 1976. Even though it was a bit run-down, we thought it had beautiful bones.
At the closing, immediately after we signed the papers, the previous owner of the building rolled up the deed, slapped it into Judy’s hand, and said, "I finally got rid of that shack!" And he walked out the door.
The building didn’t require much work. We took down the Styrofoam that covered the beautiful wood ceilings, replaced the worn-out carpets, added fresh paint—and it was restored to being a beautiful building.
As promised, we put a fireplace in one of the conference rooms. The fireplace was massive, and we felt that the room didn’t look professional. It looked like a lodge. When we raised the concern to the designers, they said, “No problem. We can fix that.” In the meantime, before the designers began changing the room, just for fun, staff started bringing in their old snowshoes, wooden skis and poles, and even an axe buried in a stump of wood.
Customers started asking to have meetings in the Lodge because it was their favorite meeting place. We scrapped the plans to change it, and over time, we started to theme the other conference rooms, too—the Lake, then the Galaxy, and then the Farm. A tradition was born.

No eye for acreage
By the time we finished moving into Tokay, we were almost out of space again (another tradition already taking form). In May 1996, we broke ground on an addition. On the day the addition was finished, as folks were sweeping up the dust from the construction, we started looking for new space.

We had about 300 staff at the time, and we figured that the maximum size we would grow to was 10x our current size; that is, we needed a campus for up to 3,000 people. Judy’s son worked for Microsoft then, and his office was at RedWest in Washington, which held about 3,000 people. We decided to visit.

By the time we finished moving into Tokay, we were almost out of space again (another tradition already taking form).
We had a very nice tour of RedWest, returned to Wisconsin, and began looking at land for sale. We looked at many locations around Dane County, including a piece of land that had about 350 acres of cornfield in Verona. It was nice, the price was acceptable, and it appeared to be about the same size as RedWest. We bought it.
One of our architects had designed the RedWest campus. “How many acres is it?” we asked. “Twenty-nine,” he said. So, our purchase of 350 acres was because we had no ability whatsoever to judge land mass correctly.
16 | The Epic Almanac
Cozy seating around a roaring fireplace in Tokay.
Staff gather for a monthly Staff Meeting at Westgate Cinema. Popcorn is still a staple of Staff Meetings, which are now held in Deep Space.
Staff break ground with commemorative trowels for Tokay's second phase of construction. Yes, they kept the trowels—mud and all.
Our forever home
1979 Milky Way • 2006-Present 2,550-13,000 (AND GROWING) EMPLOYEES
After we bought the land, our architects asked us what the #1 thing was that we wanted to achieve with our new campus. “Productivity,” we said. We wanted the campus to allow our staff to feel that they can be productive to their full potential. And enjoy it.

Much thought has gone into the campus to achieve that goal:
► Individual offices rather than cubes. This is a huge boost in productivity. We keep building new buildings so staff can have their own office without doubling up (unless it’s their choice).
► Food nearby. Lots of venues where staff can get good food and don't feel they have to leave campus to get a decent lunch.
► Cozy spaces. Comfortable seating areas and conference rooms are scattered around for meeting and discussion (plus fireplaces, of course).
► Easy travel between buildings. Cow bikes (bikes painted in spotted cow colors) available all over
campus so staff can easily grab a bike and get from one building to another, cow carts (golf carts painted in spotted cow colors) that travel the campus all day, and cow vans (similar).
► Underground travel. All buildings are connected with underground tunnels or above-ground enclosed skyways, so in bitter weather you can stay warm inside as you go to another building.
► Underground parking. Staff don’t have to scrape ice off their cars in the winter, and the campus stays green by not having hundreds of acres of parking lots.
► Mixed-up offices. Those working on the same product are together. If you're working on radiology, then you’re with implementers, quality management, tech support, software developers, and others who also work on radiology, all mixed up, so an implementer might be next to a quality manager. Mixing up allows staff to learn more about others' jobs and appreciate them.
► Buildings of 350 to 400 people. Go any bigger than that, our architects say, and you lose a sense of community. Most of our buildings are three stories. That encourages people to meet in person. In general, people will walk up two flights of stairs but not more.
2023–2024 Edition | 17 A Look Inside Epic’s Campus
Architect John Cuningham's artist rendering of the Verona campus, 2008.
Why not have fun?
When we started working with the interior designers, we assumed that one person would design bathrooms, one stairways, one hallways, and so on. In an early meeting with the designers, we asked one of them about the bathrooms. “I'm not doing bathrooms,” she said. Oops, wrong approach.
So, we assigned whole buildings to designers and told the bathroom-avoider that each person would do the bathrooms in the assigned building.
The designers then asked how to design their buildings. Thinking back to our themed conference rooms in Tokay, we quickly came up with Scandinavia, Jungle, New York, and Garden. And from then on, all our office buildings have been themed.
For the first campus, the Prairie Campus, the theming is visible only on the inside of the building. The architects did not want the exterior of the building to be themed. We did. They won.



For the second campus, Central Park, we arm-wrestled the architects and compromised on the front entrances being themed. The third campus would be visible from the highway, and we wanted people driving by to feel that they
were still in a rural area. So, the third campus became the Farm campus, and the buildings were fully themed, inside and out—Barn, Stable, Shed. That was successful, and the rest of our campuses, Wizards and Storybook, have been themed inside and out. It's more fun that way.

Still growing
As you can see, we’re still building new buildings. Next time you visit, stop by the Sci-Fi building on the Storybook campus. In the Wizards Academy, keep an eye out for Guilds (Skullkinhiss, Dragonden, Wufflegust, and Eaglebeak) and Creatures (dragons, bats, and board members). •
18 | The Epic Almanac
In an early meeting with the designers, we asked one of them about the bathrooms. “I'm not doing bathrooms,” she said.
Prairie campus viewed from its central courtyard.
Wizards Academy’s King’s Cross cafeteria.
On the morning of UGM’s 2022 Executive Address, Epic’s campus cows welcomed baby Midnight.
Storybook campus’s Oz building.







A Look Inside Epic’s Campus
An aerial view of Epic's Verona campus, 2018.
Heaven’s slide gives folks a quick and fun way to travel between floors.
Dillyd Alley in the Wizards Academy. Stand clear of the closing doors, please. The next stop is Fomalhaut.
Cows and their prehistoric friends can be found grazing in the fields around campus.
The Endor treehouse was constructed from leftover building materials.
20 | The Epic Almanac
Ninjas and Power Hours
Strategies for Taming the In Basket
In the halcyon days before most people had smartphones, patients had one option when they had a quick question or needed medical advice: to call the clinic. Organizations set up call centers and created processes to triage incoming calls thoroughly instead of giving patients a direct line to their doctor. There was a team for that.
More recently, patient messages have begun to quiet those ringing phones—a trend that accelerated during the COVID-19 pandemic when message volumes increased to 157% of pre-pandemic levels.1 Many patient messages are sent directly to providers, filling In Baskets and getting worked during “pajama time”—a term coined to describe time spent in the system outside of
normally scheduled hours. Many agree: things need to change.
Today, organizations across the Epic community are redefining processes for patient messages to reduce volume and distribute the work across the care team. Here's how they're tackling the problem.
A team-based approach
To slice through message volume and protect physicians’ time, Kaiser Permanente Northern California trained In Basket Ninjas—a new rotating physician role to allow clinicians to focus on face-to-face time with patients while knowing time-sensitive messages are handled by another provider. Ninjas
2023–2024 Edition | 21
Ninjas and Power Hours: Strategies for Taming the In Basket
1 Holmgren, A Jay, Downing, N Lance, Tang, Mitchell, Sharp, Christopher, Longhurst, Christopher, Huckman, Robert S (2022). Assessing the impact of the COVID-19 pandemic on clinician ambulatory electronic health record use. Journal of the American Medical Informatics Association. 29(3), 453–460.
36% reduction in messages to PCPs by sending responses to pools instead of directly to the PCP
Refill requests were 4x faster than the previous average
Various recent improvements to reduce message volume eliminated over 200 million messages per year across the Epic community.

Reduced average message chain length from 5.5 to 4.5 by redirecting patients to video visits or e-visits for complex messages
Over 90% of messages are triaged in 1 day, addressed within 5 days, and resolved within 7 days with the coordination of In Basket Quarterbacks at each clinic.
also cover the In Baskets of physicians on vacation or out sick.2 Because every problem can’t be solved by bringing in a ninja, clinics can earmark dedicated time for physicians and other staff to co-manage the In Basket.

To provide clean handoffs and avoid fumbling responses, Parkland Health created an “In Basket quarterback” role in each clinic. All messages go to a pool—no messages go directly to a physician or APP—and a rotating member of the clinic staff “runs the huddle” by owning the pool, triaging each message to the right person, and escalating if the message isn’t responded to within a 1-5-7
time frame—triaged in 1 business day, addressed within 5 days, and resolved within 7 days. To give clinicians time to respond to messages, they carve
APP.
out a percentage of protected time based on the amount of time historically spent on messages per specialty.3
22 | The Epic Almanac
All messages go to a pool— no messages go directly to a physician or
2 Lieu, T.A., Altschuler, A., Weiner, J.Z., et al (2019). Primary Care Physicians’ Experiences With and Strategies for Managing Electronic Messages. JAMA Network Open. 2(12).
3 Moran, B. (2023). In Basket Quarterbacks and Other Strategies for Tackling Message Volume. EpicShare.
Acting quickly on messages
Many organizations succeed in reducing physician volume by sending all incoming patient messages to a pool, mirroring the call center workflows of the past. Like the call center days, nurses and MAs working these pools need efficiency tools and clearly defined protocols to handle messages efficiently. QuickActions are tools that allow clinicians to use a single click to pull in a SmartTool-based response template and take other actions on a message, such as setting a priority or forwarding a message.
UCLA Health, Kaiser Permanente Colorado, and Denver Health recognized the need to move beyond “just sending messages to a pool” and created QuickAction responses with SmartTool-based
templates to make it easy for staff managing the pool to document their actions and provide clear instructions on how to respond to the patient.4 After these organizations shared their work, Epic’s Physi-
cian Well-Being Team created a virtual build-along session as part of the Taming the In Basket webinar series that provides a step-by-step walkthrough for building SmartTool-based protocols.
Meaningful work to retain staff
Michigan Medicine noticed a 40% turnover rate of MAs within a year of starting a position, often changing roles, titles, or locations. Leaders at Michigan Medicine found that it required 8-9 months to replace and train an MA. To foster a stronger provider–MA relationship and improve retention, they worked with clinicians to define a set of competencies and expectations for all MAs by specialty. They then created a program focused on training MAs centrally on core competencies, revamped
clinic-based training by pairing MAs with a preceptor, and introduced annual training to reengage staff, reinforce workflows, and train new skills.5
Other organizations have also gotten positive reactions from ongoing training. After participating in training at OCHIN, an MA remarked, “It was nice seeing everything that you could do … and how easy it is. I was just like shocked … I didn’t know you could do that … I’m playing with [the
EHR dashboard] more than I ever did, because I was kind of intimidated by it and I didn’t want to touch it.”6
2023–2024 Edition | 23
QuickActions are tools that allow clinicians to use a single click to pull in a SmartTool-based response.
Ninjas and Power Hours: Strategies for Taming the In Basket
4 Strodtman, G., Rogers, E (2022). Taming the In Basket with Epic: Build-Along MyChart Message Protocols. Epic-Hosted webinar.
5 Elhaddi, B., Fletcher, S. (2019). Confronting Burnout: Michigan Medical Group’s Journey to Elevate Provider Experience.
6 Gold, R., Bunce, A., Davis, J.V., Nelson, J.C., Cowburn, S., Oakley, J., Carney, S., Horberg, M.A., Dearing, J.W., Melgar, G., Bulkley, J.E., Seabrook, J., Cloutier, H (2021). “I didn't know you could do that": A Pilot Assessment of EHR Optimization Training. ACI open. 5(1):e27-e35.
Action
Prioritize the most useful updates for system efficiency and performance by completing the In Basket and Patient Messaging Tune-Up.
Learn from other organizations and share best practices by having champions participate in Epic’s Taming the In Basket webinar series
Target your training and workflow improvement efforts by using Signal to drill into physician efficiency metrics and compare against benchmarks.
Guide team members through protocols for common messages by creating QuickActions and SmartTool templates
Allow patients to do it themselves by making selfservice options in MyChart more prominent for scheduling appointments, refilling medications, and reviewing and requesting chart updates.
Reduce pajama time by incorporating time into clinician schedules to read and respond to messages before the end of the day.
Links to resources:

Better paths for patients
Patients can help reduce message volume by using self-service options in MyChart rather than sending a general advice message—which is often more convenient and resolves the patient’s needs more quickly. Salem Health nudged patients toward these self-service options by making paths to scheduling and refill requests more prominent than the option to send a general message. To speed
time from two days
half a day.
the processing of refill requests, Salem Health also scheduled MAs for “power hours”—dedicated time away from in-person patient care to work on only these messages. These power hours reduced refill response time from two days to half a day.7
Physician builders to the rescue
When Penn Medicine saw increases in message volume, its physician builders and IT team collaborated to build a workflow for clinicians to upgrade a patient message into a video visit later that same day, reducing the average number of messages in a conversation and helping patients receive care for visit-worthy issues more quickly.8
Physicians at Scripps Health implemented a similar program, turning appropriate messages into e-visits with a workflow that provided patients an overview of the e-visit process, including potential costs based on insurance coverage, and invited them to complete a short questionnaire to capture details about symptoms before beginning the visit.9 • Kyle McCaffrey, Physician Well-Being Team Peter Jorsch, Technical Communications
24 | The Epic Almanac
These power hours reduced refill response
to
7 Jorsch, P. (2023). Save Time for PCPs with a Team-Based Approach to Patient Messages. EpicShare.
8 Mollanazar, N. Fedor, R., Bowie, L. (2022). Let Me Upgrade You Moving MyChart Messages into Scheduled Visits to Increase Patient + Physician Satisfaction. Epic-Hosted webinar.
9 Wetherhold, D., Hope, N. (2021). E-Visit Expansion: Billing for Time Spent Messaging Patients. Presentation at Epic UGM 2021.
List: Declutter In Basket and save your clinicians time
Cool Stuff Ahead: An Intelligent In Basket
To help care teams keep pace with a growing number of patient messages, In Basket is getting smarter. Generative AI will provide first drafts of messages, and predictive analytics will help triage, categorize, and— when appropriate—even filter messages, helping the care team get patients the responses they need as quickly as possible.
Organizations including UC San Diego Health, UW Health in Madison, Wisconsin, and Stanford Health Care are among the first to start deploying enhancements to automatically draft message responses in Epic.
Sort it out
In Basket reads each incoming patient advice request message and uses predictive analytics to categorize and route the message to appropriate recipients. For example, it can send a message about a medication to a clinical pool and a message about the timing of an upcoming visit to the scheduling pool.
First draft responses
In Basket drafts text for a potential response to the patient’s message based on the message text and information
from the patient’s record, including current prescriptions and recent results. Clinicians can review and revise the response before sending—or ignore it and draft their own reply from scratch.
An ear for languages
To help reduce disparities for patients who speak other languages, In Basket can detect the language the message is written in and route it to an appropriate pool.
Shashank Raghu, In Basket R&D Peter Jorsch, Technical Communications
Refill protocols have saved an estimated 500 years across the Epic community since they were introduced.
2023–2024 Edition | 25
Ninjas and Power Hours: Strategies for Taming the In Basket
New Frontiers: Toward a More Unified Healthcare System

Q&A with Alan Hutchison, Epic
Over the last several years, one of our focuses has been building new connections between provider organizations and the broader healthcare ecosystem. Learn about the history and future of three new areas: Payer Platform (large commercial insurers), Aura (specialty diagnostic labs), and the Life Sciences program (pharmaceuticals, medical device manufacturers, and more).
Payer Platform












































Q: Payer Platform is Epic’s first foray with large commercial health plans. What inspired the idea?
A: When I started working on our population health team back in 2015, everyone talked about—and still talks about—value-based care. There was a lot of lip service paid to it, but when we looked at the reality of how providers were reimbursed, we found that about 10% of patients were treated under value-based relationships, many of which were upside-only and generally resembled a fee-for-service chassis with a few quality metrics attached.
26 | The Epic Almanac
PAYERS Health Plans Real-Time Prescription Benefits LIFE SCIENCES Pharma Precision Medicine Specialty Diagnostics HEALTH SYSTEM Inpatient Outpatient Home Health Hospice Hospital at Home Home Infusion Home Dialysis CARE IN THE HOME SOCIAL SAFETY NET Social Care Behavioral Health State Systems Dental Orthopaedics Urology Nephrology Cardiology STANDALONE SPECIALTIES Urgent Care Retail Clinics National Telehealth Providers Employer Health CONVENIENT CARE Rehab Long-Term Care Long-Term Acute Care RECOVERY
Alan Hutchison
One of the most effective mechanisms for changing how the healthcare system works is changing the reimbursement model. We see this with Medicare Advantage and HMO models like Kaiser Permanente. We realized that there might be some good opportunities to help by working directly with payers.
Q: How did you get started? How did providers respond to the idea?
A: Here’s a cultural fact about Epic: we have eight salespeople for the whole world. No commissions, no quotas, no cold calls. Our sales approach is reactive. If you see an opportunity to work with a group, you’ve gotta wait for an inquiry.
Eventually, we got one. It was from BCBS Minnesota for medication therapy management, which we had done for many years with providers but never with a health plan. Let’s just say that we went into our work with BCBS MN pretty naively. We know much more now, but at the time we didn’t
What is Payer Platform?
Providers and payers use Payer Platform to reduce administrative complexity, speed up prior authorization, monitor and meet quality measures, help patients get the care they need, and prepare patients for the costs associated with their care. The goal is a simpler, higher-quality experience for everyone.
The Community
The Payer Platform community includes the nation’s seven largest health insurance companies, which together insure more than 150 million Americans, and a number of state Blues and provider-sponsored plans. On the provider side, more than half of
know the difference between HIPAA for treatment and HIPAA for payment and operations. We went through the selection process, learned a lot, and in the end, BCBS MN selected us.
The night before BCBS MN planned to make their announcement, they called the provider organizations in Minnesota to give them the heads-up. Our provider customers were…let’s just say…not particularly happy. They wrote us a letter and made it clear: if BCBS MN joins the network, we’re leaving.
Q: Yikes. What did you do?
A: We flew up to Minnesota to meet with our provider executives and shared where we were coming from: “We believe that stronger collaboration between payers and providers is an important part of the future—how do we make this work?” They gave us a list of things they thought they could improve in their interactions with payers. Then, we went back to BCBS MN and Humana— we’d just started talking to them, too—and had
our eligible community members have signed up, and more than 800 hospitals and 17,000 clinics are live.
Community Outcomes
► Ochsner Health and Humana completed 53% of prior authorizations for in-scope services instantly, saving roughly 500 staff hours over seven months—the equivalent of more than three months’ work for a full-time employee.
► Mayo Clinic saw an 80% reduction in denials that required additional clinical documentation and sped up payment for high-dollar claims by 22 days.
► At Baptist Health, 27% of the conditions that providers readdressed were known to them only because of insights from Humana that were shared over Payer Platform. With a betterinformed approach to risk documentation, Baptist provided more comprehensive care for chronic conditions and received financial reimbursement that was more appropriate to the clinical complexity of its patients, resulting in more than $1 million in additional revenue.
► Humana has eliminated manual chart requests for risk adjustment for the last two years.
2023–2024 Edition | 27 New Frontiers: Toward a More Unified Healthcare System
Looking Ahead at the Payer Platform Roadmap
► Helping patients prepare for the costs of their care by showing estimates informed by their insurance coverage. These estimates will also indicate whether coverage for a service requires prior authorization, so patients will be able to plan ahead for that step.
► Helping patients avoid surprise out-of-network costs by letting them search for and schedule with in-network providers.
► Helping patients take advantage of supplemental benefits, like rideshare and food-as-medicine programs, by encouraging signup in MyChart.
► Simplifying communication by connecting patients with the right customer service team— their providers’ or their payers’— depending on what they need.
► Improving health plan literacy by giving patients the ability to review their insurance information and their use of yearly benefits, including their progress toward deductibles and maximum out-of-pocket expenses.
► Speeding up registration by giving patients and front desk staff electronic access to insurance ID cards.
the same conversation. They gave us a big list of their own. When all was said and done, we crossmapped the two lists, and those were the first five features in Payer Platform.
We still hear skepticism from people who are new to the idea of Payer Platform, but now our providers have become champions of the platform. In fact, a group of c-level executives across a state in the northeast got together independently of
us and wrote a letter to all of the health plans in their state asking them to adopt Payer Platform. We had to gain providers’ trust and demonstrate value, but now that we have, the Payer Platform provider community is growing faster than we ever expected and now covers more than 100 million people.
Q: Let’s look forward now. What new Payer Platform development has you most excited?
A: Much of our upcoming work focuses on the patient experience, especially in MyChart. With more than 160 million active users, MyChart can improve the patient experience in a unique way and at immense scale.
Putting more information in patients’ hands will go a long way for helping payers and providers, too. One of our payer customers told us that every patient call costs them $35 and that they employ tens of thousands of people to meet their call center needs. Creating a better patient experience that cuts down on those calls would make a big difference.
28 | The Epic Almanac
We had to gain providers’ trust, but now that we have, the Payer Platform provider community is growing four times faster than Care Everywhere grew and now covers more than 100 million people.
Q: Commercial insurance isn’t the only part of healthcare that’s new to Epic. Let’s talk about specialty diagnostic labs. What excites you about working with them?
A: Specialty diagnostic tests can save lives. Genetic testing, for example, has already helped the medical and research community develop better ways to detect and treat cancer, predict the success of organ transplants, diagnose rare diseases, and speed up the often months-long trialand-error process of finding the right medication to treat depression. As the medical and scientific communities discover more connections between genetic variation and health, they’ll also develop more and more use cases for genetic testing.
Specialty diagnostic tests are really where precision medicine begins. By helping providers use them more effectively, we hope to help more patients benefit from precision medicine.
Q: Set the stage a bit. What challenges have providers and labs shared with you?
A: One of the challenges is connectivity. Specialty diagnostic labs are usually standalone companies— they typically aren’t parts of health systems, and they haven’t used the technology that health systems use
to work with each other, like Epic. Instead, they’ve connected with providers through paper requisitions, faxes, and online portals. This meant that labs often received orders without enough patient information to get started, and providers often received results that weren’t easy to use because they weren’t integrated into patients’ health records.
The other challenge is scalability. When providers did receive discrete results from a given lab, it was because their health systems had completed months of technical work to set up interfaces. One connection, one lab, up to six months of work. That’s not a scalable solution, and you can imagine how it stifled collaboration between providers and labs.
Q: How can Epic help?
A: Aura, our specialty diagnostics suite, makes it possible for provider organizations to collaborate with specialty diagnostic labs in a fraction of the time necessary to configure traditional interfaces. Each lab that uses Aura contributes to a single compendium of tests, and from that compendium providers can download tests into their local Epic instances. These downloads replace the work to establish pointto-point interfaces.
When all’s said and done, providers can use their existing Epic workflows to send orders to and receive discrete, actionable results from any lab
Community Outcomes
As of July 2023
► Adaptive Biotechnologies
► Caris Life Sciences
► Exact Sciences
► Foundation Medicine
► Guardant Health
► Invitae
► Myriad Genetics
► Natera
► Tempus
► After connecting with Exact Sciences through Aura, Ochsner Health screened nearly 5,000 patients for colorectal cancer. Of those patients, 77%—more than 3,700 people—had never been screened for colorectal cancer before.
► For the first time in history, a person’s complete genetic information—including sequence data—was integrated with the electronic health record.
► Tempus reported that Aura sped up health system integration by 78% and reduced implementation times to as little as three weeks.
2023–2024 Edition | 29
New Frontiers: Toward a More Unified Healthcare System
Aura
Labs Participating in Aura Today
that uses Aura, with as little as two weeks of work to connect to a new lab.
Q: What’s next for Aura?
A: Aura unlocked the power of connectivity for diagnostics companies. We’re now thinking about how to bring that to other parts of the healthcare ecosystem. How could we create more pathways
Life Sciences
Q: OK, we’ve talked payers and specialty diagnostics. What’s next in the health grid for Epic?
A: We’re currently working on a new Life Sciences program. Our goal is to unify care delivery and clinical research by building a stronger connection between patients, providers, and study sponsors.
Q: Talk about the challenges in the industry. What have you heard from providers and sponsors?
A: Providers have told us that they want it to be easier to give patients access to novel therapies, but the challenge is knowing about the right study opportunities at the right time. A patient’s chance to join a clinical trial—to access potentially life-changing treatment—shouldn’t depend on word of mouth.
Study teams have told us that participating in clinical trials can require outsized investment. To borrow one analogy, activating studies can feel like building an arena for a concert, tearing the arena down, and building a new arena for the next show. Jumping between the technological requirements of each study is inefficient—even prohibitive.
Study sponsors have told us how much effort it takes to generate evidence. These companies aren’t just pharmaceutical companies or medical device manufacturers—they’re also evidence-generation companies. They need to prove, as quickly as possible, whether a therapy works, and they need to reduce the inefficient, duplicative work that slows down the generation of that proof.
that are easy for the Epic provider community to turn on and relatively lightweight for other organizations? How do we continue to create value for patients, providers, and other parts of healthcare? It’s beginning to take the shape of a digital services platform for device manufacturers, large national labs, tech-enabled service providers, digital therapeutics, and more.
Q: The clinical trials process is no small nut to crack. What’s Epic’s initial focus?
A: We have a lot to learn whenever we enter a new area, so the key is to maximize our strengths and avoid trying to boil the ocean. Here’s a list of our R&D team’s focus:
► Helping sponsors quickly determine study feasibility with help from Cosmos.
► Matching participating provider organizations with clinical trial opportunities suited to their patients.
► Sending those organizations purpose-built Cosmos queries that help them confirm that a trial is right for them and get started on cohort identification. We call this concept Cosmos Teleport.
► Democratizing access to clinical trials by lowering the technical and staffing barriers to study activation. Doing so can make participation an option for new study sites and patients.
► Increasing clinical trial efficiency by eliminating duplicative workflows and connecting researchers, care teams, patients, and sponsors through a single system.
► Supporting clinicians with point-of-care insights into when their patients might qualify for a clinical trial and using predictive models to assist with the timing of therapy administration.
► Helping study teams guide patients through decentralized or hybrid trials through electronic consent and patient-reported outcomes, guided interactive protocols, telehealth, remote patient monitoring, and connected devices.
30 | The Epic Almanac
Q: Are there any community outcomes that demonstrate the potential of the Life Sciences program?
A: One of our customers used Epic to increase the speed of study recruitment twenty-fold while reducing costs five-fold. For context, recruitment accounts for 40% of a clinical trial’s budget on average. A specific component of their success was direct-to-patient recruiting through MyChart, which helped them achieve a participant enrollment rate of 7.8%.1 Traditional healthcare marketing would be lucky to generate a 3% click rate…and these patients are actually enrolling and participating in the trial.
Those outcomes are a result of just one organization’s efforts. Imagine how streamlining something similar across the entire Epic community could benefit patients, providers, study teams, and sponsors.
Q: How do you decide which life sciences groups are a good fit for the program?
A: Our partners need to see the patient as the most important part of all of this and the provider experience as crucial to the overall success of sponsored research. They need to be leaders who are ready to re-engineer clinical trials rather than patch up old processes. Together, we need to be able to balance the strength of our collective experiences with an eagerness to imagine new solutions from a new perspective.
Q: How far along is the program today?
A: The first components of the Life Sciences program, Clinical Trials Matchmaking and Cosmos Teleport, are available now. These are crucial to helping study sites find and evaluate trial opportunities with minimal time investment. In the fall of 2023,, we’ll release the first phase of our Life Sciences platform: the software that study sponsors and sites will use to centralize study configuration, connect with patients, and share outcomes.
Partners & Pals
Q: Let’s end by zooming out even more. Are there areas beyond care delivery where Epic can make a positive impact?
A: You might have heard about our collaboration with Press Ganey. Through that partnership, we’ll reduce overhead for our health system customers by making it easier for them to monitor and improve how their patients experience care. We’ll also give them the ability to embed Press Ganey patient satisfaction surveys directly in MyChart and bring compiled results and actionable insights back into Epic. For example, a patient experience manager picking up a phone call will be able to quickly learn about that patient’s experience during their last visit and use that information to make that phone call and the next visit even better.
More broadly, our work with Press Ganey marks the beginning of a new approach to working with companies that can help our provider customers reduce waste, improve processes, and build stronger connections with the many kinds of organizations that make healthcare run effectively. These include patient satisfaction groups like Press Ganey, ambient voice products, and even logistics companies, to name a few.
These companies will be able to work with Epic through two new programs, Partners and Pals, that provide more technology, experience, and collaboration opportunities for our customers. The Partners program is for leading products and services in established market segments. They have strategic alignment with Epic and a major impact on healthcare, and our collaboration will provide even greater value. The Pals program is for newer, innovative products and services. They're interesting ideas that could become very impactful for our customers, and we work closely with their teams as they develop those ideas. •
Interviewed by Jesse Atkins
2023–2024 Edition | 31 New Frontiers: Toward a More Unified Healthcare System
1
(2022, December). Using Technology to Transform Recruitment Strategies in Clinical Research. HIMSS.
Specialty Steering Boards: Networking, Camaraderie, and Getting Things Done
Hundreds of providers, elected by their peers, serve on more than 50 specialty steering boards that drive prioritization of content and development in Epic, which includes workflows and configuration options that represent best practices for their specialty. Physician board members Yaa Kumah-Crystal, Holden Groves, Allison Weathers, and Howard Levy share why they got involved, some of the meaningful projects they've worked on, and how their work benefits healthcare delivery.
The boards are a directed way for specialties and subspecialties to participate in development prioritization and ensure that our specialty’s needs are being met. When we communicate those needs to our Epic partners, they work with us to understand the reason behind our request and to figure out the
The boards are a directed way for specialties and subspecialties to participate in development prioritization.
Yaa Kumah-Crystal, MD Vanderbilt University Medical Center

Pediatric Endocrinology Steering Board
I got involved with a steering board to learn from other pediatric endocrinologists about ways to configure our system to meet our specific needs. Most boards have an open door policy so you can be a fly on the wall and listen in even before you become a voting member. Over time, I started contributing ideas myself and realized becoming an official board member was a great opportunity to effect meaningful change across the country or even the world.
best way to build it into the Foundation System so that it's useful for specialists across all organizations. For example, our steering board’s work to improve insulin instructions made it possible for me to send updated insulin dosing rates directly to MyChart so they’re available to the patient at the end of a visit. It used to be a much more arduous and complicated process, but now patients have the information readily available, so they know the right dose to take.
32 | The Epic Almanac
For me, the camaraderie is another important part of the steering board. I have a good sense of who my fellow board members are, and I consider them all friends. We're able to converse about the challenges we face and the different kinds of patients we see while we work through solving problems.
available, quickly, to deal with this crisis. When Epic created a brand-new critical care steering board, I was eager to join to help translate the work people have already done and make it available across the Epic community.
ICUs in particular benefit from the steering board work because the size and scope of projects is so big compared to the relatively small number of patients we see and the proportionate size of our departments. For any individual organization to corral the resources and prioritize something really specialized like the ICU Liberation Bundle, which aims to prevent delirium in the ICU, is a tall task. When we make changes at the Foundation System level, it's possible to get the resources to build and share a high-quality product.
Groves, MD New York Consortium Critical Care Steering Board
New York Consortium—a collaboration between NewYork-Presbyterian, Weill Cornell Medicine, and Columbia University Irving Medical Center— went live on Epic in early February 2020. A month later, we had our first COVID-19 patient in the ICU, and pretty soon, we were setting up ICUs in cafeterias and ORs. Suddenly, it became all critical care, all the time, across all of our hospitals.
I led a lot of the critical care work during our Epic implementation, so I knew how configurable the system was. When COVID-19 hit, I acutely felt the gap between what was possible with Epic and the setup we were using. People I worked with said, “There are a lot of amazing ICUs out there that have been using Epic for 20 years. Why can’t we have all of the setup that they have?” I wanted to be a part of putting those best practices into the Foundation System so that everybody could have the best tools
Lately, our board has been focused on making inpatient rounding better. It saves people minutes or even hours a day, and it helps them feel confident about the decisions they're making in the EHR. We're seeing people transition from dreading documentation to becoming adept EHR users who understand how to find the important information they need to make complex care decisions quickly.
Steering boards are also the best possible way to connect to other leaders in the field—people who’ve gone through similar trials and tribulations and have a wealth of experience. Every change in the EHR is

Steering Boards at a glance
56 steering boards
639 members representing 194 organizations
a risk and a costly endeavor. It’s foolish to take on a project as a single hospital when allies across other organizations and at Epic have incredible experience, technical knowledge, and vision. Through the steering board, you can shape how things work.
.
2023–2024 Edition | 33 Specialty Steering Boards: Networking, Camaraderie, and Getting Things Done
Holden
Steering boards are the best possible way to connect to other leaders in the field.
Links to resources:

Allison Weathers, MD Cleveland Clinic

Neurology Steering Board
When I was a junior neurologist, I would hear prominent neurologists say that Epic wasn’t working for them. I remember thinking, “What are you talking about? My organization’s neurology build is excellent!” I started looking for ways to connect with others who are also passionate about the subject and who wanted to make a difference, and I found Kelly Mundth, a former neurology nurse who had just started working at Epic.
Kelly and I formed a precursor to the neurology steering board before steering boards existed. It was a labor of love. We started as a rag-tag group with around
50 members, but different people participated each time, so we kind of had to start over every month. When Epic introduced steering boards, our group became a formal board. I know how unique and special it is that it’s been Kelly and me working on this together for a decade. It’s a true friendship and partnership.
I think steering boards work well because they’re a two-way street. We’re a trusted resource for Epic, and we bring up pain points to help Epic prioritize the most important projects for our specialty. Many of our board members are also active members of the American Academy of Neurology (AAN), participating in committees and workgroups, which gives us a tight connection with our specialty society. When we hear about something that we know will be a priority for our fellow neurologists and patients, like a new Alzheimer’s treatment, we can make it our top priority to understand what build is needed. Each organization doesn’t have to reinvent the wheel and respond to something new.
A few years ago, our board redesigned the tool neurologists use to document a neurology exam. Neurologists are unique in how we think and talk and document, so we improved the NoteWriter tool and its text generation to actually sound like a neurologist. Before, looking at a note, you could tell only that a patient had a neurology exam. Now, it’s clear from the note what the patient’s specific problem is.
Action List: Participate in the direction of specialty content and features in Epic
Nominate a clinician who should be considered for a specialty steering board. Find the nominations form in the Resources section of the Specialty Steering Boards guide on Galaxy.
Vote in the annual specialty steering board election held on Epic Earth in June.
Connect with your specialty's steering board members to share your ideas. A list of current members is available on Galaxy.
Sit in on a specialty steering board meeting. Email Greg Strodtman (SSB@epic.com) for meeting details.
34 | The Epic Almanac
Other people are realizing the power of building things in the Foundation System, too. I get approached almost every week by neurologists asking to present to the board or share their ideas. The board works with Epic to prioritize all of those ideas and make sure we’re working on things that affect the most lives.
Howard Levy, MD, PhD Maryland Primary Care Genetics Steering Board

There are lots of channels for us to tell Epic what we want—ideas.epic.com, BFFs, TS—but steering boards are unique because they provide an opportunity to have conversations with developers and leaders about which projects are important—and why—so Epic can work on the right thing first and the next thing next.
It’s not enough for Epic developers to have one or two people telling them what they want. They need guidance from a steering board to make sure the right things are being built and prioritized. That’s the difference between a brain trust and a steering board. A brain trust is an opportunity for Epic to bring in experts and show them cool development they’re working on. The steering board does that but also brings new things to the development roadmap. We tell Epic what we need them to work on, and Epic takes that information and strives to make the feature as robust as possible.
For example, I had been telling Epic that we needed a pedigree tool to show patients’ family history information. The developers took that a step further and made sure that pedigree was integrated with other parts of the software, not just a standalone tool.
Another important piece of content that came out of the genetics steering board is the Ehlers-Danlos syndrome diagnostic SmartForm, which helps screen for a group of inherited disorders that affect connective tissues. The first time a colleague saw my consultation report after I started using the SmartForm, she was bowled over. She was still using paper or an online form that had to be transcribed back into the note. She
was amazed when I showed her what was possible— and it's available to all organizations that use Epic through the Foundation System.
Steering boards also give us the opportunity to bring a multidisciplinary team of smart people together to work on a project that crosses specialties. If, in the future, we work on a project related to multiple endocrine neoplasia, which is a condition that predisposes patients to cancers of endocrine glands, we’d need experts in genetics, oncology, and endocrinology. There are steering boards that specialize in those areas for both adults and kids. That’s great not only for making a better product, but also for helping people connect. You can sit together in a smaller group and share ideas, trade stories, and just get to know each other.
If you’ve ever considered getting involved with a steering board, do it. They can be powerful microphones to give your ideas a voice. •
Interviewed by Kelly Conne
2023–2024 Edition | 35
Specialty
Steering boards give us the opportunity to bring a multidisciplinary team of smart people together.
Steering Boards: Networking, Camaraderie, and Getting Things Done
Clinical Informatics 101: Designing Residencies That Grow New Physicians into HIT Leaders and Epic Experts
Rethink residency curriculum to cultivate informaticists and patient advocates in the next generation of physicians.
For residents today, the computer is as important a tool as the blood pressure cuff or the thermometer. Many new physicians are digital natives and are often interested in learning how to use technology in new ways to improve patient care and operations. Over 90% of
medical students and residents use Epic as their EHR through the majority of their training. Children's Hospital of Philadelphia (CHOP) and UCLA Health have been trailblazers in including clinical informatics electives in residency, each using different approaches to foster residents’ skills. This year,

36 | The Epic Almanac
Lexington Medical Center’s new residency program includes a required rotation in clinical informatics.
as part of its new residency program, Lexington Medical Center plans to integrate clinical informatics training fully into first-year curriculum for its first incoming class. By folding HIT skills into education, these organizations hope to grow physicians who can usher in the technology-driven future of medicine.
CHOP case study: A variety of options to meet residents at their interest level
Residents at Children’s Hospital of Philadelphia all get an overview of what clinical informatics means in practice, and if they want to learn more, they have the option to make it an area of focus. An introduction featuring lectures and case simulations in Epic is part of CHOP’s required orientation, which leads into education on topics like clinical knowledge management and EHR efficiency.
“It’s crucial for resident wellbeing,” said Brooke Luo, MD, an attending physician in pediatrics at CHOP, medical director for health IT safety, and herself a graduate of a CHOP Clinical Informatics fellowship. “What you spend a lot of your time doing has a huge impact on job satisfaction. When we poll residents who are several years out of residency, the vast majority confirm that they’re using these skills.”
Those who are interested in more in-depth topics can elect to intersperse clinical informatics education in their rotations, including attending committee meetings and conferences and completing an independent project in clinical informatics.
“For some residents, the experience sets them on a career path they might not have considered otherwise,” said Tony Luberti, MD, director of

CHOP’s Clinical Informatics fellowship program. “This program can be the catalyst that gets them thinking beyond what it’s possible to build in the system and interested in the human factors of design and change management, what it really takes to be an informaticist.”
Any resident can also join the New EHR Resident Development (NERD) Squad, a group of 15 to 20 residents who meet to discuss points of friction and opportunities to use informatics tools and brainstorm together. The group’s user-centered design process accelerates the incorporation of new build in the Epic system so all of CHOP’s physicians can take advantage of improvements sooner. Past projects include a documentation template for medically complex foster children and a discharge summary template for common diagnoses.
“For hospitals, clinical informatics options for residents are a great investment,” Luo said. “Residents practically live in the hospital; they understand the problems the way no one else can. Empowering them to make changes improves life for everyone else, too.”
UCLA Health case study: Dedicated mentors and real-world application build residents’ ownership of system improvement



UCLA Health’s inclusion of clinical informatics as a residency elective started with the goal of growing physician champions to help with its initial Epic go-live in 2013. It quickly saw the value of introducing residents to clinical informatics early and made it a permanent part of the program.
The curriculum includes a monthly lecture with an expert, journal clubs, and other assigned reading, but focuses primarily on interactive learning through a one-year longitudinal project.
2023–2024 Edition | 37
Clinical Informatics 101:
That
New
into HIT Leaders and Epic Experts
Designing Residencies
Grow
Physicians
Jennifer Singer
Kevin Baldwin
Brooke Luo
Tony Luberti
Action List:
Help physicians and residents become strong Epic users by giving them an opportunity to complete Physician Builder or Power User certification
Make sure physicians and residents know about the Here's How videos they can watch in Epic and where to find the video catalog so they can quickly pick up efficiency tips.
Encourage system mastery by offering Thrive training to physicians and residents to help them establish good efficiency habits and tailor their workspaces to their personal workflows.
Use system data to focus refresher training by measuring efficiency with Signal and follow the guidance in the Improve Clinician Efficiency and Wellness with Epic Strategy Handbook to address physician and resident feedback.
Consider requesting Epic Supply Shop support to help you increase physician efficiency and satisfaction.
Links to resources:

All residents who apply to participate must include a plan to either enhance patient care or refine physician workflows in their application. Over the course of the program, they work with a mentor to polish their ideas and then with IT staff to finalize the build in their Epic system. At the end of the year, they present their projects to a panel of physician informaticists and health system leaders. Residents have the freedom to pursue areas that interest them, and past project topics vary widely, including a bilirubin screening tool for the NICU, pain management assessments, clinical decision support tools, and dashboards for specialists. Since the beginning of the program, residents have completed more than 170 of these projects, and ACMIO Jennifer Singer, MD, estimates that almost half of these improvements remain in UCLA’s system today.
“Our IT team benefits, too,” said program manager Kevin Baldwin, MPH. “They have immediate buy-in and excitement about projects from end users. It sets a great precedent for the kind of relationship that physicians and the project team can have working on the system together.”
The future: Lexington’s planned program introduces informatics as a core skill for all

In its residency program, launching in 2023, Lexington Medical Center plans to build on lessons from programs like CHOP’s and UCLA’s by making a standard four-week rotation in clinical informatics required for all residents. The curriculum was designed with contributions from Physician Builders and other leaders in areas such as surgery, family practice, and cardiology, and it accounts for parts of medical practice that previous generations of physicians didn’t have to consider. For example, Anna Shalkham, MD, the CIO and CMIO at Lexington Medical Center, notes that managing the patient digital experience is a growing part of care today.
Anna Shalkham
38 | The Epic Almanac
Grow residents and physicians into strong Epic users
“Patients expect to be able to schedule appointments online, send their doctor a question in MyChart, and get a response,” Shalkham said. “Our future providers need to anticipate these expectations and be able to meet them efficiently for their own well-being.”
In addition to traditional clinical informatics topics like navigating the quality landscape, using decision support, and improving patient safety, Lexington also plans to cover areas recommended by its IT team, like cybersecurity, technical support, and system storage. Lexington is one of several health systems in its community, and its patients are often seen elsewhere, so they’ll also train residents on interoperability tools like Care Everywhere so

they can use comprehensive patient information in their care decisions.
“The more we talked about what residents needed as we put the program together, the more we recognized how crucial technology is. Regardless of which specialty these residents go on to choose, we know this knowledge will serve them well,” Shalkham said. “We also hear from many physician peers that work fatigue and burnout are often unjustly attributed to the informatic platforms necessary in today’s work environment. Our hope is what used to be viewed as a time-consumer will be rightfully recognized as a time-saver with this additional exposure and training.” •
 Written by Anna Cacciaglia
Written by Anna Cacciaglia
2023–2024 Edition | 39
“It sets a great precedent for the kind of relationship that physicians and the project team can have working on the system together.”
Residents in UCLA Health’s clinical informatics program complete projects designed to enhance patient care or refine physician workflows.
Clinical Informatics 101: Designing Residencies That Grow New Physicians into HIT Leaders and Epic Experts
All residents at Children’s Hospital of Philadelphia get an overview of clinical informatics and can opt to make it an area of focus.
What’s in a Name?
Happy Together
Happy Together connects organizations so patients and providers can see information from all organizations they visit in one place without needing to log in to different systems. The name for our network that brings patient data together came from another kind of happy marriage: Judy’s daughter Shana’s wedding. The Turtles’ 1967 hit “Happy Together” was played at the wedding reception, and when someone asked Judy a few days later what we should name the new network, the song was still in her head.
Jabberwocky
When we built our Alice in Wonderland-themed building, we needed a matching name for its parking garage. So, we took our vorpal sword in hand and sought a name from a nonsense poem in Lewis Carroll’s Through the Looking-Glass. When you park in Jabberwocky, every day is a frabjous day. Callooh! Callay!
Shake, Rattle, and Roll
There’s a double meaning behind the names for the three sections of the Epicenter amphitheater in the Learning Campus: Shake, Rattle, and Roll. They’re both the famous lines from a song and allude to the seismologic definition of an epicenter.
40 | The Epic Almanac
Ever wonder how we come up with the ideas for our fun names? Here’s the story of how some of our delightful designations came to be.
Cupid
When we released our cardiology suite of tools, we thought “Thumper” would be a fun and memorable name, but there was a lot of pushback from our sales staff. During a site visit, Judy met a pediatric cardiologist wearing a clown nose, and when she asked for his card, he handed her a Joker.
“We’re trying to think of a name for our new cardiology module,” Judy said. “What do you think of the name ‘Thumper?’” The cardiologist scratched his red nose and said, “It’s not dignified enough.”
So that was the end of Thumper. Instead, we turned to the winged god of love, Cupid, to name an application for hearts.
BFFs
When we decided to assign every customer a BFF (Best Friend Forever), people asked what it meant. We said, “Do you have a teenage daughter?”
At UGM and XGM, you’ll see executives putting their arms around their BFF, saying, “This is my BFF!” Sometimes we even hear arguments: “My BFF is better than your BFF.” “No, mine is the best!”
Cogito
Cogito means, “I think,” part of René Descartes’ famous first principle, “cogito ergo sum” (Latin for “I think, therefore I am.”) We chose this name for Epic’s analytics suite because it helps you think about problems in new ways.
Kit & Caboodle
A caboodle is a whole made up of many parts, and Epic’s data warehouse stores every piece of a patient’s data, no matter the source. Most people are familiar with the phrase “the whole kit and caboodle,” and that’s what we have at Epic, too—Caboodle is our data warehouse, and Kit is the tool that lets you share that data.
Willow Pharmacists know that the bark of the willow tree contains salicin, a chemical similar to acetylsalicylic acid— commonly known as aspirin. This medication that has stood the test of time made sense as the name for Epic’s pharmacy system for tracking and dispensing medications.
Beans
Naturally, our dialysis application had to be named for the shape of the kidney (bean) organs it's designed to help nephrologists treat.
Canto
“Canto,” Italian for “song,” is also the name of Epic for tablets. It’s both a beautiful word and a beautiful image—singing the song of the patient’s journey from anywhere in the hospital the doctor might need it.
Haiku
“Epics” are poems, But we needed something short. Thus, “Haiku” was born.
Limerick
There once was a busy physician
Who found workstations an imposition. We came up with a name— “Limerick,” we proclaimed, For an Apple Watch app name audition. •
Written by Philosophy Walker
2023–2024 Edition | 41 What’s in a Name?
Strong Epic Users Start with Great Training
Learn how a collaborative new approach to training—Epic’s system expertise combined with your trainers’ unique, local knowledge about your organization—is helping users start with a strong foundation.
When clinicians feel that their initial training prepared them to use the EHR effectively, they have an average Net EHR Experience Score 89.7 points higher than clinicians who don’t feel prepared after initial training.1 When installing an add-on application or onboarding new staff, organizations use multiple techniques to prepare staff to use the EHR, including classroom and hands-on learning. A new way to provide quality training to your staff is through End User Training Services (EUTS)— role-based training led by Epic trainers.

The evolution of Epic’s training offerings
Lauren Wons, Epic, Training Project Manager and Implementer
Preparing end users for go-live has long been a principle central to our implementation strategy. When I think about EUTS, it is a natural next step in how we support initial training. The pandemic changed things for implementing organizations by creating a barrier to in-person, classroom-based education. Our customers

42 | The Epic Almanac
1 Manzione, L. (2021, July 16). Clinician Training 2021 Update. KLAS Research
Lauren Wons
Andrew Armstrong, Epic clinical apps trainer, leading a virtual training session.
needed help continuing to provide high-quality training. Virtual quickly became the new norm, and we learned how to train a lot of users with a group of knowledgeable Epic trainers.
Courses are taught in the Foundation System, which includes best practices and content that evolves to meet the needs of academic, pediatric, and community organizations. This makes it possible to start training earlier because the organization doesn’t need to spend time building and testing a new training environment before training begins.
As the people working directly to train thousands of staff, we’re motivated to get end-user feedback to the right people across Epic, benefitting the software, Training Wheels, and our Foundation System.
Flexibility to meet evolving needs
Rich Harwell, Salem Health, Training Program Lead

EUTS Keys to Success
No pass, no access
Day-in-the-life exercises
Required personalization labs
What we bring:
Planning and strategy documentation to guide you through the process
Project management tools to track and report on your staff
A learning management platform where users can log in, enroll in classes, track their own progress, and access materials
Rich Harwell
We started using EUTS in summer of 2021 when we needed to onboard new inpatient clinicians but didn’t have an inpatient principal trainer. Most of the training at our organization is handled by our informatics coordinators who have limited time for maintaining curriculum and build, which
Trainers and a training environment
E-Learning lessons, in-class curriculum, and assessments
What you bring:
A deep understanding of who your users are and what they do
Principal trainers and super users who lead trainees through day-in-the-life activities customized to your workflows
made new-hire training a challenge. We did a cost analysis of hiring a principal trainer compared to using EUTS and decided to go with Epic. Paying per user was a clear cost savings, and we like the scalability and flexibility to go with the ebb and flow of hiring.
A physical space for users who might not have the appropriate technology at home
Administrative staff who enroll users and track certification
2023–2024 Edition | 43
Strong Epic Users Start with Great Training
Paying per user was a clear cost savings, and we like the scalability and flexibility to go with the ebb and flow of hiring.
The program was really successful for our inpatient physicians, so when we needed to add several anesthesiologists to the team, we enrolled them in EUTS as well. The training recordings were really helpful for meeting people where they were at. Some of the physicians had used Epic before, so they came in, completed the training and assessments, and left after a few hours. Others had never used Epic before and could spend the whole day working through the material at their own speed.
After our success with inpatient physician and anesthesiologist training, we decided to use the same strategy for our lab users when we went live with Beaker. We have a small lab, so our users wear a lot of hats and do a little bit in a lot of different areas. We received feedback from our users that the curriculum went too deep into workflows they complete only rarely, so they ended up spending more time in training than they really needed. We learned that it’s important to know what each role does and to think critically about how to tailor training to unique roles. The day-in-the-life exercises were especially important for them, because it gave them hands-on experience working in the system on tasks they’re responsible for.
Shifting your focus from onboarding to efficiency
Amy Vines
Amy Vines, Catholic Health, Manager of IT Education and Training System Development

When we went live with Epic in November 2020, we shifted from our usual live class approach to virtual—and our users loved it. But after our install, the super users who helped train their peers and the principal trainers we had contracted went back to their regular jobs, and we needed to decide how to approach new-hire training.
During one of our check-ins with Epic, they asked whether we'd be interested in being the first post-live organization to try EUTS.
We reviewed Epic’s training curriculum for the program, and because our version of Epic is very close to the Foundation System, the curriculum was almost identical. In roles that we hire
infrequently, our principal trainers spend a lot of time updating the materials and refreshing their own memory of the system. It felt duplicative for us to be maintaining the same components when Epic is already doing it. Now, almost all of our users receive initial training through EUTS.
As a trainer, you want to be in the classroom and it’s scary to hand that off to someone else. But the biggest thing we learned from EUTS is that it’s not your new hires who need you. It’s your current users who need your help because they have so many more questions now than they did when they first walked through the doors of your organization. Handing our new hires off to Epic freed up our trainers to go out and do rounds on the floors and work with users at the elbow to troubleshoot and improve efficiency.
Tackling a large-scale rollout with the trainers you have
Lisa Hammond, Atrium Health, DirectorClinical Apps Education
When Epic announced the EUTS program in summer of 2020, we were rethinking our install training approach. We needed to

44 | The Epic Almanac
Lisa Hammond
It felt duplicative for us to be maintaining the same components when Epic is already doing it. Now, almost all of our users receive initial training through EUTS.
train nearly 70,000 staff in a year on Epic while continuing to train new staff on our old EHR, and we had the challenges of the COVID-19 pandemic to deal with. We were the first organization to use EUTS, so we had to take a bit of a leap of faith. The collaborative training method appealed to us—a combination of our own trainers, who have a deep understanding of how we do things at Atrium Health, and Epic trainers, who are experts in how to use the system—and met our need for a solid technical foundation and deep understanding of organizational policies and workflow.
We decided to use Epic for our clinical applications—about 50,000 users—and had our trainers handle the revenue and business applications. The way you use the system to provide patient care is really similar across organizations, so it makes sense to us that Epic trainers lead clinical training. We had our own trainers focus on the revenue and business space where we had some specific local nuances.
While Epic trainers led the class, principal trainers were often in the room to help troubleshoot and provide hands-on support, like helping users
find the right environment. We provided a dedicated space with workstations where staff could attend classes virtually, access the playground environment, or review recorded sessions. Using recordings wasn’t part of our original plan, but we worked with Epic, and they accommodated and expanded
Get a high-level overview with Epic’s End User Training Services white paper
Take a deeper dive with the Epic-Led End User Training Strategy Handbook
Connect with your BFF and Lauren Wons (lauren@epic.com) to discuss how your organization could use EUTS.
the recordings, which was a saving grace. After our system was ready, principal trainers met with clinicians to wrap up training with some tasks specific to our policies and workflows—day-in-the-life training, personalization labs to increase documentation efficiency, and security validation. •
Interviewed by Lucca Hermes
Learn more about the EUTS experiences discussed in this article by contacting the participants interviewed:
► Rich Harwell: richard.harwell@salemhealth.org
► Amy Vines: avines@chsbuffalo.org
► Lisa Hammond: lisa.hammond@atriumhealth.org
Links to resources:

2023–2024 Edition | 45
Strong Epic Users Start with Great Training
Using recordings wasn’t part of our original plan, but we worked with Epic, and they accommodated and expanded the recordings, which was a saving grace.
Action List: Determine how End User Training Services can support your team
Getting Ahead of Trends in the U.S. Regulatory Landscape
Epic and members of the Epic community are preparing for the future of healthcare IT regulations.
The Epic community in the U.S. participates in dozens of regulatory and quality measurement programs, from national programs like Promoting Interoperability to state-specific public health programs. To help you stay ahead of emerging standards and regulatory trends, Epic advocates for common-sense, easy-to-implement regulations and participates in industry associations to help shape future requirements. Here are some of the recent trends we’ve seen.
Standards for social determinants of health
Many recent regulatory changes in the U.S. have focused on collecting and exchanging data related to patients’ social determinants of health. CMS plans to require inpatient organizations to report SDOH screening and positivity rates, and ACO REACH participants must both collect this information and form a plan to address health inequities. The Joint Commission also requires healthcare organizations to create health equity plans, and NCQA recently created a HEDIS measure for evaluating and intervening on SDOH-related needs. With SDOH reporting starting for many programs in 2024, collecting and exchanging SDOH information will become increasingly important in the next decade.
Epic and many members of the Epic community
help set standards for how SDOH information should be collected and exchanged through our work with the Gravity Project, an industry collaborative working to develop consensus-based standards for exchanging SDOH information. Last year, ONC announced a Gravity Project Pilots Affinity Group that will help establish norms for SDOH interoperability by implementing the standards defined by ONC’s United States Core Data for Interoperability, Version 2 (USCDI v2). Many Epic-released SDOH assessments are mapped to codes recommended by the Gravity Project, and Epic organizations can already exchange these assessments through Care Everywhere.
We’re also working to make it easier to meet SDOH-related requirements regardless of the mix of programs you participate in, with standard support for the most common programs, like CMS’s inpatient screening measures, and recommendations for when you need to develop a health equity plan or deviate from Epic content to meet less-common proprietary screening requirements.
TEFCA: A step toward universal interoperability
Fifteen years after the first patient record was exchanged over Care Everywhere, interoperability remains a core focus for both regulators and the Epic community. Epic’s engagement with emerging interoperability
46 | The Epic Almanac
frameworks like the Trusted Exchange Framework and Common Agreement (TEFCA) and the Epic community’s work to implement industry-standard methods of data exchange help make the interoperability challenges of the future achievable.
Epic TEFCA Interoperability Services was among the first set of applicants accepted to continue to the testing phase of the QHIN Designation process under TEFCA in February. We’ve also participated in the
already facilitates data exchange with more than 4,200 hospitals in the U.S. With TEFCA, we hope to connect the remaining hospitals to ensure clinicians have comprehensive patient information, no matter where patients received care in the past.
Making medical authorization manageable
Health Information Technology Advisory Committee (HITAC) to provide recommendations directly to the Department of Health and Human Services about the implementation of the 21st Century Cures Act that established TEFCA. This network of networks will help broaden and simplify connections both to other healthcare organizations and to other groups like patient-access vendors. The Carequality framework
In the last year, proposed rules from CMS and new legislation in the House of Representatives have included requirements for completing medical prior authorization requests quickly and electronically. Most of the Epic community in the U.S. has already signed on to join the Payer Platform network, where prior authorizations are exchanged for more than 17,000 patients each month between health systems and health plans using industry-standard specifications. Several members of the Epic community also participate in HL7’s Da Vinci project, a group working to define standardized formats for data exchange between health plans and health systems that will form the backbone of proposed interoperability requirements of the future.
Regulators want to hear from you, too. Your firsthand experience delivering care and implementing standards helps you provide meaningful feedback before proposals become universal requirements. •
Written by Tim Rebholz
Action List: Prepare for and influence health IT regulation
Links to resources:

2023–2024 Edition | 47 Getting Ahead of Trends in the U.S. Regulatory Landscape
Epic TEFCA Interoperability Services
was among the first set of applicants accepted to continue to the testing phase of the QHIN Designation process under TEFCA in February.
Follow the Meaningful Use forum on the UserWeb.
Join the Carrot, our weekly regulatory call, to
hear
from Epic experts about regulation and groups to get involved in. Head to the Regulatory Programs & Quality Measurement Advisory Council every UGM and XGM. Talk to your Epic BFF about the Digital Health Policy Workgroup, a group of organizations working to communicate their perspective directly to regulators. RPQM
at Epic
The story behind the one-of-a-kind collection


Each year, Epic staff volunteer to visit local art fairs and select new pieces that are destined to join our assortment of paintings, sculptures, furniture, and other objects. These volunteers can be spotted selecting items that embody the imagination and creativity of the collection. And while it’s not required, volunteers consider it a bonus when a piece reflects one of the building’s themes.
Many of the items , like the kaleidoscope (1) in the courtyard of Andromeda, are meant to be moved by the viewer. Other pieces, like Rockin’ Ralph (2) in the Heaven building and the Banana (3) in Voyager Hall, literally move the viewer.
Also in Voyager Hall, an authentic antique carousel (4) evokes childhood memories for long-time Madisonians.
Relocated from the former site of a Madison classic, Ella’s Deli, the carousel, along with the display tables and mobiles on the ceiling, remind us all to enjoy a little color and music when we can.
As you round a corner, you might find a papier-mâché starving artist (5) waiting patiently for her kibble. In a bustling common area, a ceramic figure (6) invites you to take a moment to gather your thoughts. Near a warm fireplace, a regal ostrich (7) keeps a watchful eye on you as you pass by.
Art at Epic helps staff and visitors navigate our campus, and it also helps you understand the type of people who work here. We work hard, we do good, and—with the help of the beauty and whimsy that surrounds us—we have fun. •

 Written by Celia Groff
Written by Celia Groff
48 | The Epic Almanac
This fearsome dragon guards a treasure of technology in a Dungeonsand-Dragons-themed building.
1
A kaleidoscope of color in the Andromeda courtyard.







2023–2024 Edition | 49 Art at Epic
A ride on Rockin’ Ralph puts body and mind in motion.
It’s hard to resist riding the larger-than-life banana between training sessions in Voyager Hall.
Taking a spin in Voyager Hall.
A pooch with a painterly style.
The watchful mosaic ostrich keeps an eye out for newcomers.
A peaceful spot to gather your thoughts.
2 3 4 5 6 7
A gift from metal workers on the job during campus construction, the Tin Man points you in the right direction.
We’ve Got You Covered
Do more with the Epic software you already own.
You get a lot out of an Epic license—more than you might realize. As healthcare evolves and third-party vendors provide niche solutions, we’ve seen community members struggle to understand those solutions in the context of the Epic software already available to them.
We’ve outlined several examples of Epic functionality that overlap with the healthcare apps that Epic community members encounter most often.
Patient Arrival & Intake
Give current and prospective patients ownership over their care so that they can enjoy a more convenient, efficient experience and free up time for your staff. No MyChart login required.
► Open your doors with online scheduling
► Let patients skip the front desk with eCheck-in and self-arrival
► Get clinical documentation started by collecting health histories and questionnaire responses online


► Share documents and obtain consent online


► Manage appointments and arrivals through two-way text










Patient Financial Experience
Give patients the convenience and transparency they need to manage the costs of their care.
► Offer online payments, payment plans, and financial assistance— no MyChart login required
► Personalize payment plans based on the patient’s ability to pay
► Provide a digital-first experience with real-time balance notifications
► Receive payments and establish payment plans with two-way text

► Provide a single bill for professional and hospital balances
► Automatically generate and share estimates for upcoming visits
► Collect self-pay payments automatically through Visit Auto Pay
► Help patients plan for future balances by establishing payment plans prior to service
In the Works
► Consolidate statements across your service areas and billing systems In the Works
50 | The Epic Almanac
OR Management and Utilization
Get more out of your ORs by helping surgeons and staff release and fill underutilized time, better understand their block utilization trends, and schedule future cases more efficiently.
► Automatically send block owners their utilization statistics

► Improve scheduling accuracy with case length predictions







► Use predictive modeling to spot potentially underutilized blocks
► Automatically remind block owners to fill or release potentially underutilized time
► Create a marketplace where surgeons and staff can easily claim open OR time
► Automatically broadcast open OR time to the surgeons most likely to use it In the Works
Hospital Patient Flow
Bring efficiency up and length of stay down by maximizing your bed space, running a tight OR, and keeping everyone on the same page.
► Orchestrate systemwide patient flow with real-time analytics and a capacity command center
► Automatically create and complete discharge milestones to head off delays
► Identify and prioritize patients who face discharge barriers
► Calculate surge scores to track capacity bottlenecks
In the Works
► Estimate expected length of stay and use predictive analytics to anticipate tomorrow's discharges In the Works
► Forecast capacity and staffing for the next shift In the Works
Want to learn more? Contact your BFF to review the full list of current and future features in these areas.
Automation
Eliminate repetitive tasks, save time, and focus your staff’s attention where it can have the greatest impact.
► Show clinicians whether orders require prior authorization before they’re signed
► Request prior authorization and receive payer responses electronically
► Create coverages automatically when patients scan their insurance card.
► Identify coverages available from health plans that use Payer Platform
► Predict the likelihood of payment to prioritize follow-up on high-value denials
► Generate claims attachments to reduce denials
► Prioritize clinical documentation review to mitigate lost revenue

► Respond to payer requests for additional information
In the Works
► Simplify coding for physician services using generative AI
In the Works
2023–2024 Edition | 51 We’ve Got You Covered
An Epic Recipe From our kitchen to yours
Jacques’ Chocolate Chip Cookies
Recipe by Jacques Torres and adapted by the Epic culinary team Makes: 20 cookies

INGREDIENTS
2 cups minus 2 tablespoons cake flour
1 ²⁄₃ cups bread flour

1 ½ teaspoons baking powder

1 ¼ teaspoons baking soda
1 ½ teaspoons coarse salt
2 ½ sticks (1 ¼ cups) unsalted butter, room temperature
1 ¼ cups light brown sugar, packed
1 cup plus 2 tablespoons granulated sugar
2 large eggs, room temperature
2 teaspoons pure vanilla extract
1 1⁄₃ pounds bittersweet chocolate disks or fèves, at least 60 percent cacao content Sea salt or fleur de sel, for sprinkling
INSTRUCTIONS
1. Sift together the cake flour, bread flour, baking soda, baking powder, and salt into a medium-sized bowl and set aside.
2. In the bowl of your mixer, cream together your butter and sugars until light and fluffy, about 3-5 minutes. Add in the eggs, one at a time, until combined, scraping down the bowl as needed. Add in the vanilla and mix. Gradually add in the dry ingredients, until just moistened. Fold in your chocolate until evenly added throughout the dough. Press plastic wrap against the dough, making sure it is completely covered, and refrigerate for at least 24 hours, or as long as 72 hours. (I left mine for 36 hours.) This is an important step, because it allows the gluten in the dough to loosen up. (You know how if you beat your dough too much, your cookies will be rock hard? Allowing it to rest for a period of time helps to undo some of this damage.) It also helps the cookies to not spread out too much; warm dough spreads, cold dough stays in nice, uniform circles.
3. When you are ready to bake, bring the dough to room temperature so that you can scoop it out (I usually let it just sit on my counter for an hour or two), and preheat your oven to 350 degrees F. Line and/or grease your baking sheets. Scoop your dough out onto the sheets. We recommend a #40 ice cream scoop, which is about the size of 2 tablespoons, but you can make them even larger, if you like. Do not press the dough down—let it stay the way it is. Sprinkle the cookies lightly with a bit of fleur de sel or sea salt. Bake 10-12 minutes for smaller cookies (mine took about 11 minutes), or 18-20 minutes for larger cookies.
4. Allow the cookies to cool slightly on your baking sheet, and then move them to another surface to cool completely. You can enjoy these warm, room temperature, or cold. Store in an air-tight container at room temperature for up to 3 days, or freeze for up to 2 months.
52 | The Epic Almanac
Rooted in Sustainability
Horticulture that’s more than just beautiful
As you meander across Epic’s campus, you’ll experience a range of biodiversity in our landscaping and green spaces that reflects each building’s theme. Trek through the desert outside our wild-west-themed building, Juno, and notice the native prickly pear cactus. Wander past Alice and see the white daisy garden growing alongside the Queen of Hearts and her croquet mallet. Take a hike to the Farm Campus and check out the fruit trees in the orchard on the hill beneath the barn.
Our horticulture team is responsible for maintaining beautiful, ecologically diverse interactive spaces for our staff, customers, and visitors. Here’s how our green-thumbed gardening aficionados think about designing outdoor areas filled with fun and interesting plant life.

Aesthetically pleasing. We use plants to create special places. By highlighting natural features, creating scale that can bring large features to a human level, and choosing plants that have interest across multiple seasons, we can provide a space that is functional and beautiful throughout the year.
Functional. The landscape connects staff across campus and provides a place for people to rest, meet, and have fun. Paths provide access to buildings via an outdoor route, and landscape theming acts as a wayfinding tool to help visitors know where they are on campus.

Diverse. With more than 1,500 species and cultivars across campus, we provide a high level of ecological diversity. This diversity in turn supports a wide range of pollinators and birds, creates resiliency against things like drought and disease, and creates a space that will last for decades to come. Our landscape is home to some threatened and endangered species, including Blanding’s Turtles!
Sustainable. With more than 90 acres of green roof, many on top of parking structures, we prevent excess runoff and soil erosion, reduce urban heating effects, and allow staff and visitors to keep their cars out of the elements.

Interactive. Attractive green space is meant to draw users to interact. Outdoor events such as our summer farmers’ market, Epicnic, and UGM invite users to take advantage of the landscape. Staff can also reserve space for team meetings, games, and celebrations.
 Written by Eric Rieth and Rachel Salter, Horticulture Team
Written by Eric Rieth and Rachel Salter, Horticulture Team

2023–2024 Edition | 53






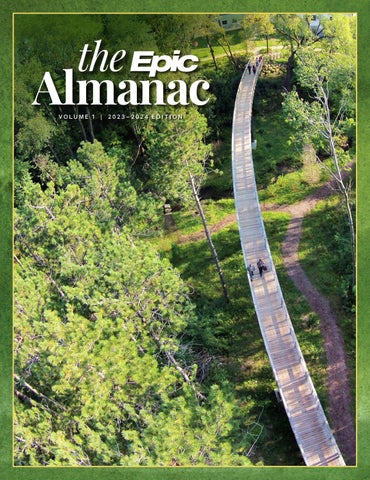











































































 Written by Anna Cacciaglia
Written by Anna Cacciaglia








 Written by Celia Groff
Written by Celia Groff






















 Written by Eric Rieth and Rachel Salter, Horticulture Team
Written by Eric Rieth and Rachel Salter, Horticulture Team

