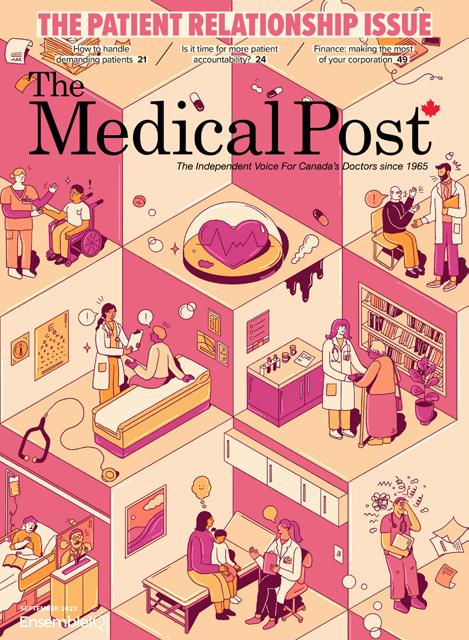
THE
ISSUE Cool and inspiring physician jobs 23 Locuming: avoiding the pitfalls 40 How to hire a good medical receptionist 46 OCTOBER 2023 Doctors talk job satisfaction 16
JOBS



















©2023 GS o f com ies o ts lice so . T em k e ow e y o ice se o t e GS o f com ies. 1102 08/23 INTRODUCING e REXVY .c /e -c /
This year we’re profiling the folks who write the Medical Post here. Up for this issue, Ann Graham Walker, who has an article on page 12.

How did you end up being a health writer?
I lived in Argentina from age two to nine and was quarantined in my house, COVID-style during the polio epidemic. This was just as I was about to start school. My mother told me I would be released as soon as the infection and death rate started to plunge. So I learned to read scanning the pages of the Buenos Aires Herald, informing myself of the disease.
Years later, after a BA in art history and an MA in modern European history, I became a current affairs morning show producer at the CBC (radio). This was in Cape Breton where coal mines and steel plant coke ovens were closely tied to serious health issues in the community. AIDS was beginning, and Canada’s blood supply was found to be contaminated. Health and medical journalism were a central and very interesting part of my work.
How did you end up writing for the Medical Post?
My husband is a doctor and I always read his copy of the Medical Post. I learned so much and was a fan. A few years later, when we left Cape Breton and moved to Halifax, I had to quit my radio job and saw a notice in the paper that the Medical Post was looking for an Atlantic Provinces staff writer. Curious, I applied and was hired! When we left Nova Scotia in 2002 and moved to B.C., I switched over to being a Medical Post freelancer.
Next Issue
THE BEGINNINGS & ENDINGS ISSUE: The next issue covers births, deaths, and some milestones in between and will be hitting doctors’ mailboxes in mid-December. Also:

• The 2023 Medical Post Awards winners: We’ll have profiles of Canadian physicians who are making a difference for marginalized communities and who are leaders in practice innovation and media engagement. TheMedicalPostAwards.ca

THE MEDICAL POST OCTOBER 2023 3 UPFRONT 5 Editorial The Jobs Issue 7 Feedback Doctors confab about fragmented care challenges 8 Rounds Doctor salaries and aggressive behaviour from patients’ families THEME 12 Not easily Can physicians retain passion for the job of medicine without changing the system? 16 Job satisfaction Doctors talk about the best and worst parts of their jobs 19 Innovative recruitment Chief physician recruiters get creative as provinces try new strategies to hire doctors 23 Cool jobs Thinking you might want to try something new? Look to these physicians for inspiration BACK PAGES 31 Column: Dr. Raj Waghmare Query iGAS 35 Clinic Tips on providing medication abortion 40 Practice management Locuming: avoiding the pitfalls 43 Finance Done with residency? Six tips for the road ahead 46 Solve my problem How do I hire a good medical receptionist? 45 Classifieds Contents VOLUME 59 NO. 5 Cover: Kathleen Fu, Photo supplied
The Medical Post AWARDS
When your patients with major depressive disorder are facing an inadequate response to their antidepressant
Consider adding PrREXULTI®



PrREXULTI® is indicated for use as an adjunct to antidepressants for the treatment of major depressive disorder (MDD) in adult patients with an inadequate response to prior antidepressant treatments during the current episode.13










For more information: Please consult the Product Monograph at www.rexultimonograph.ca for important information relating to clinical use, warnings, precautions, adverse reactions, drug interactions, and dosing information, which have not been discussed in this piece. The Product Monograph is also available by calling 1-877-341-9245.

by most public formularies
1–12*
COVERED
and private insurance plans
REXULTI is a registered trademark of Otsuka Pharmaceutical Co., Ltd., used under licence by Otsuka Canada Pharmaceutical Inc. © Otsuka Canada Pharmaceutical Inc. and Lundbeck Canada Inc. All rights reserved. OTS-REX-00060E * REXULTI is eligible by Non-Insured Health Benefits, Correctional Service Canada and Veterans Affairs Canada as a general benefit, and for formulary coverage in the following provinces and territories: Alberta, New Brunswick (regular benefit); Ontario (general benefit); Manitoba, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Northwest Territories (open benefit). References: 1. REXULTI. Data on File. Private coverage plan. 2. Alberta Health. Drug benefit list. April 1, 2021. 3. Manitoba Pharmacare. Formulary Search Results. December 1, 2021. 4. Ontario Drug Benefit. Formulary. February 26, 2021. 5. Data on File, Otsuka Pharmaceutical Co., Ltd. 2019. NIHB coverage. 6. Newfoundland and Labrador. Benefit List update. May 12, 2022. 7. Correctional Service Canada. Data on File. August 2019. 8. Veterans Affairs Canada. Formulary Search Results. November 2, 2021. 9. Northwest Territories. Data on File, NWT. November 17, 2020. 10. New Brunswick Drug Plan Bulletin #1087. September 26, 2022. 11. Nova Scotia Formulary Pharmacare News. September 2022. 12. Health PEI. PEI Pharmacare Bulletin. November 16, 2022. 13. REXULTI Product Monograph. Otsuka Pharmaceutical Co., Ltd. Is it time to choose REXULTI for your patients? Visit REXULTI.CA
The Jobs Issue
I admit at the beginning I feared the pandemic was going to be much worse: that double-digit percentages of the global population were going to die. Then in September of that first year of the pandemic some work challenges came along and I had one of my annualor-so freak outs: Argh, I thought, I should quit my job/retire!
I can’t afford to retire (I’m 59 if you’re curious) so it would have been more like becoming a minimalist and part-time freelance writer. I have a lovely boss (who occasionally has to serve a bit like a therapist for me!), and I talked to her and my friends and wisely didn’t impulse-quit my job during the pandemic.

I’ll sometimes tell someone my job is that I’m the editor of a magazine and website and they will say something like, “Oh, gosh, that must be such a great job to have!” And in many ways, it is, and I’m privileged and grateful. I enjoy the
20 Eglinton Ave. West, Suite 1800, Toronto, ON M4R 1K8 (877) 687-7321 Fax (888) 889-9522 www.canadianhealthcarenetwork.ca
BRAND MANAGEMENT
SVP, HEALTHCARE CANADA
Donna Kerry (416) 786-6315 dkerry@ensembleiq.com
EDITORIAL EDITOR-IN-CHIEF
Colin Leslie cleslie@ensembleiq.com
EDITOR, CANADIAN HEALTHCARE NETWORK
Martha Porado mporado@ensembeiq.com
REPORTER
Marjo Johne mjohne@ensembeiq.com
CONTRIBUTING EDITOR
Louise Leger lleger@ensembleiq.com
“craft” parts of being a journalist. But as doctors will often say, they love the patient care and hate the paperwork (see page 16)—there are pluses and minuses of any job.
I spent a lot of time through the pandemic reading and thinking about how we deal with the parts of our jobs we don’t like, and I think it goes like this: We want to minimize the parts of our jobs we don’t like compared to the parts we like, of course. Beyond that, when the work we do aligns with our values, it is easier to tolerate the parts we don’t care for. That is, I believe the purpose of the Medical Post is to help Canada’s doctors—through the lens of journalism. I believe helping Canada’s doctors is good for Canada and the healthcare system, and I care passionately about those things. So when I’m in the midst of the parts of my job I don’t like, I try to remember that, and it makes it easier.


DR. CHRISTINE NICHOLAS plastic surgery
DR. BRIDGET REIDY family medicine
DR. FRANCO RIZZUTI public health
DR. DUNCAN ROZARIO general surgery
DR. DAVID SATOK family medicine
SHOUTOUTS
The best part of editing a magazine is working with the team of writers, and I hope the coverage in this issue helps you with your job.
• We look at the challenges for doctors working in healthcare today, with different physicians outlining the obstacles doctors face in having passion for their jobs (page 12).
• One of the great things about being a physician is the range of possible jobs one can do, and the article “Cool jobs” on page 23 outlines some interesting options.
• Dr. Raj Waghmare’s column looks at a 14-year-old who presents with mysterious symptoms, leading to a complex diagnostic journey.
ACCOUNT MANAGER Nancy Dumont (514) 557-6660 ndumont@ensembleiq.com
ACCOUNT MANAGER Samir Iggui siggui@ensembleiq.com
PHYSICIAN ADVISORY BOARD
DR. ALYKHAN ABDULLA family medicine
DR. BENJAMIN BARANKIN dermatology
DR. MELANIE BECHARD pediatrics
DR. ALI DAMJI family medicine
DR. MARIO ELIA family medicine
DR. FERRUKH FARUQUI family medicine
DR. ALAN KAPLAN family medicine

DR. PUNEET SETH hospitalist
DR. MIKE SIMON family medicine
DR. CHRISTOPHER SUN family medicine
DR. HIROTAKA YAMASHIRO pediatrics
ADVERTISING SALES & BUSINESS
SENIOR ACCOUNT MANAGER Norman Cook (647) 290-3967 ncook@ensembleiq.com
SENIOR ACCOUNT MANAGER Scott Tweed (416) 230-4315 stweed@ensembleiq.com
SALES & BILLING COORDINATOR Sylvie Graveson (514) 805-0634 sgraveson@ensembleiq.com
PROJECT COORDINATOR Kalli Sagos ksagos@ensembleiq.com
DESIGN/PRODUCTION/MARKETING
CREATIVE DIRECTOR Nancy Peterman npeterman@ensembleiq.com
PRODUCTION MANAGER Lisette Pronovost lpronovost@ensembleiq.com
SENIOR MARKETING MANAGER, HEALTHCARE Nicola Tidbury ntidbury@ensembleiq.com
SUBSCRIPTION SERVICES
SUBSCRIPTION QUESTIONS contactus@canadianhealthcarenetwork.ca
Subscriptions (PRINT): 1 year: $65; 2 years: $120; Outside Canada: $100 per year; 2 years: $185; Single copy price: $12; Groups: $46 per year; Outside Canada single copy: $16
Subscription (DIGITAL): 1 year: $45; 2 years: $84
To subscribe or renew, go online to: www.canadianhealthcarenetwork.ca/ subscribe or email: medicalpost@ canadianhealthcarenetwork.ca
CORPORATE OFFICERS
CHIEF EXECUTIVE OFFICER
Jennifer Litterick
CHIEF FINANCIAL OFFICER
Jane Volland
CHIEF HUMAN RESOURCES OFFICER
Ann Jadown
CHIEF OPERATING OFFICER
Derek Estey
CHIEF STRATEGY OFFICER
Joe Territo
Mail Preferences: Occasionally we make our subscriber list available to reputable companies whose products or services may be of interest to you. If you do not want your name to be made available please contact us at medicalpost@canadianhealthcarenetwork. ca. Contents copyright © 2023 by EnsembleIQ; may not be reprinted without permission. The Medical Post receives unsolicited features and materials (including letters to the editor, press releases, promotional items and images) from time to time. The Medical Post, its affiliates and assignees may use, reproduce, publish, re-publish, distribute, store and archive such unsolicited submissions in whole or in part in any form or medium whatsoever, without compensation of any sort. ISSN-0025-7435, PM PM42940023, The Medical Post, established 1965, is published 6 times per year by Stagnito Partners Canada Inc. Printed in Canada.
THE MEDICAL POST OCTOBER 2023 5 EDITORIAL
When your work aligns with your values, it makes the difficult parts of a job more bearable
FIND US ONLINE The Medical Post’s online home is CanadianHealthcareNetwork.ca Registration is free and easy. Medical students and residents welcome. @MedicalPost
COLIN LESLIE EDITOR-IN-CHIEF


We’re putting physicians first. Learn about CFPC’s approach through our video and article at cma.ca/CFPCstory. MD Financial Management provides financial products and services, the MD Family of Funds and investment counselling services through the MD Group of Companies and Scotia Wealth Insurance Services Inc. For a detailed list of these companies, visit md.ca and visit scotiawealthmanagement.com for more information on Scotia Wealth Insurance Services Inc. The trademarks of the Canadian Medical Association are registered and used under licence. The Bank of Nova Scotia (Scotiabank®) provides banking and credit products and services. Visit scotiabank.com. ® Registered trademarks of The Bank of Nova Scotia, used under licence. Due to the demanding nature of the work, physician burnout is a critical issue in the Canadian health care system. With funding from a strategic partnership between the Canadian Medical Association, MD Financial Management and Scotiabank, The College of Family Physicians of Canada (CFPC) has accelerated multiple programs that prioritize physician wellness and foster professional growth, in turn driving positive change across Canada’s health care system. Innovative education tactics are improving physician wellness in Canada Dr. Farid Kakavand and Dr. Victor Ng — CFPC
Feedback
Doctors confab about fragmented care challenges
Frustration of fragmented care (Sept.)
Dr. Doug Snyder of Waterloo, Ont., wrote: “Two examples of fragmented care: Have already seen two patients this week who saw separate pharmacists to treat shingles one or two days earlier but, in their words, they were advised to also see a doctor ASAP to confirm the pharmacist’s diagnosis and treatment. There was no indication of what the patients were treated with as they falsely assumed it was automatically on their medical records. There were also no pharmacist notes of diagnosis and treatment, which both patients noted the pharmacist told them would be sent ASAP to the GP’s office but never arrived.”
Dr. Carmen Eadie of Surrey, B.C., wrote: “It would be
great if we had teams. But FPs must lead the teams. FPs should be paid good salaries with benefits with defined workloads, much like NPs. Pharmacists, PAs, mental health workers should all be housed in the same clinics. The ministries of health must pay for the bricks-andmortar and support staff to allow physicians to do what they do best: care for complex patients. If there is supervision required for NPs, PAs, pharmacists—that is, if they have questions or are looking for advice—this must also be reflected in remuneration. All practitioners would have access to patient records and the EMR must be supplied by and paid for by the health ministry.”
Dr. Tuhin Bakshi of Wetaskiwin, Alta., wrote: “If we want to save primary care, we have to work harder. This would mean accommodating extra patients in our daily busy schedule, giving the needy patient earlier and urgent appointments, contacting them virtually if we cannot see them, etc. When our patients can’t get to see us they go to the other services. This is not a brainer! If we call ourselves the true primary care practitioner, we have to change with the times or we will lose it!”
Dr. Don Witten of Rocky Mountain House, Alta., replied in an online comment to Dr. Bakshi: “Maybe we can be more accommodating if we added refills on prescriptions wherever that seems appropriate and safe. Too many appointments are only for a refill. Now that patients can get refills virtually they may not complain too much and some may like talking to their doctor every three months but it is not the best use of our time.”
Rounds: Private delivery ≠ private pay (Sept.)

Dr. Chris Williams of Burlington, Ont., wrote: “This is largely a media issue. Mainstream media loves to
use ‘private care’ to create a headline. The majority of patients have virtually no idea how care is delivered, but when the media says ‘Doug Ford has a secret plan to privatize healthcare’ they pay attention. Most healthcare delivery is already private. Government could simply not afford to have a fully public non-profit delivery model.”
Dr. Bridget Reidy of Victoria wrote: “A more important distinction is corporate versus small business run by those who have a career in doing the work. Upselling is a great danger in privatization, especially in a system where the public picks up the cost of complications and followup. I am private because I keep what ‘profit’ I make. But I am highly unlikely to work with that being my main concern unless my boss makes me.”
Handling demanding patients (Sept.)
Dr. Ferrukh Faruqui of Ottawa wrote: “The most effective way to handle this issue is to be very clear up front what clinic/MD policies are; to advise that abusive, disrespectful behaviour will not be tolerated and to stick to these policies. In other words, respect your patients and respect ourselves too.”
THE MEDICAL POST OCTOBER 2023 7
“It would be great if we had teams. But FPs must lead the teams.”
VITALS
Doctor salaries
It is a bit cheeky—but totally human nature—to be curious about how much other doctors earn. So here— for the Jobs Issue—is annual compensation for some well-known physicians. All doctors’ incomes below are current or 2022 salary from Sunshine lists—or stated if it is from a different source.
$765,337 DR. ANDY SMITH, president and CEO of Sunnybrook Health Sciences Centre in Toronto. Dr. Smith is a surgical oncologist.
$512,558 DR. JANE PHILPOTT, dean of the faculty of health sciences at Queen’s University since 2020.
$443,263 DR. BERNARD JASMIN, dean of the faculty of medicine at the University of Ottawa since 2018.
$420,612 DR. DAVID ANDERSON, dean of the faculty of medicine at Dalhousie University since 2015.
$342,292 DR. BONNIE HENRY, the provincial health officer for British Columbia since 2014.
$275,700 to $324,400 DR. THERESA TAM, Canada’s chief public health officer. (According to a federal order-in-council, as first reported by Blacklock’s Reporter, Dr. Tam’s salary was in that range for the year 2022).
$169,600 SENATOR DR. GIGI OSLER, this is the base salary for being a Senator. Senators who occupy certain offices and positions receive additional pay. Dr. Osler was appointed to the Senate in 2022.
SAYING ‘NO’ Aggression from a patient’s family
Physicians can sever the doctor-patient relationship if a patient is abusive or aggressive. But what about bad behaviour from the patient’s family members? A recent decision by Ontario’s Health Professions Appeal and Review Board upheld a physician’s right to say no to verbal abuse by family members.
It also warned doctors to document aggressive behaviours, even if the abuse comes not from the patient, but their family. That information doesn’t need to be sent to the referring physician, but it can still remain in the chart, it said.
The case in question is not without heartbreak: a devoted mother taking care of her adult son with cerebral palsy, who is non-verbal, and a hematologist in Sault Ste. Marie, Ont., trying to get adequate biopsy samples to reach a diagnosis of a rare disease. When frustrated with the delay in diagnosis, the mother was “aggressive, argumentative, intimidating, bullying, angry, sarcastic and demeaning,” the doctor told the Inquiries, Complaints and Reports Committee of the CPSO. He didn’t document all the interactions, telling the committee that he was unsure if it should be included on the patient’s chart. After all, it was the mother’s behaviour, not the patient’s.
After the initial interactions, the patient was treated by a Toronto hematologist but then wanted to transfer his care back to Sault Ste. Marie. The Sault-area hematologist declined the patient due to the mother’s previous disruptive behaviour. He suggested other hematologists who could provide virtual care for the patient. The mother filed a complaint with the CPSO. When the CPSO rejected her complaint, she appealed the decision, putting the case in front of the review board.
The board found that the CPSO’s decision was reasonable and that while the refusal was a surprise to the mother, the board stated that physicians “have a right to be treated with respect and not be subjected to verbal abuse.” It’s what all those signs in clinic waiting rooms say, but this time the mother faced consequences, causing fed-up doctors to cheer from coast to coast to coast. —KYLIE
TAGGART
8 OCTOBER 2023 THE MEDICAL POST Shutterstock
Rounds
PUBLIC-PRIVATE CARE Entrepreneurs step up in crisis
During the depths of the resource crunch that hit Canadian healthcare last fall when there was an immense demand for services, Dr. Daniel Flanders felt bereft. “It was horrific—it felt like we were failing our communities,” said the founder of Kindercare Pediatrics, a multidisciplinary pediatric health centre in Toronto. Entrepreneurial solutions are needed, Dr. Flanders told attendees in Toronto at the CMA’s first in a series of town halls on public-private healthcare to be held this fall and winter. “We need innovators. We need entrepreneurs. We need those who think outside the box.”
“We are at a point where we can comfortably have these uncomfortable discussions,” said Dr. Kathleen Ross, the new president of the CMA. Dr. Ross is a family physician in Coquitlam and New Westminster, B.C.
Last month, the Alberta government and the Enoch Cree Nation, west of Edmonton, announced
that a chartered surgical centre will open to Indigenous and non-Indigenous patients starting in June 2025. The 7,400-square-metre facility is expected to do about 3,000 publicly funded hip and knee replacement surgeries annually. It is a private facility, but Chief William Morin, past-chief, Enoch Cree Nation, said at the event that he uses the term “sovereign.”
The First Nation is partnering with Surgical Centres Inc. on the facility.
Morin said for a number of historical reasons Indigenous health outcomes are measurably much lower and have been for a long time. “If someone gets mad at me in this debate, I’m just going to throw those mortality rates (at them),” said Morin.

Dr. Brett Belchetz, co-founder and CEO of Maple, said the accusation that private care leaves equity-deserving patients behind is not true. “That is one of the biggest fallacies—that private healthcare will leave people behind,” he said. Rather, it is the lack of sufficient public healthcare that leaves some without coverage, as seen in the U.S., he said.
For Dr. Ross, it is not about whether for-profit healthcare companies are good or bad rather it is that use of such companies needs to be watched. “People worry about their healthcare dollars going to the profit of a company,” she said. —COLIN LESLIE
THE MEDICAL POST OCTOBER 2023 9 AUSCULTATIONS ROUNDS
—Dr. Sarah Giles, a family and emergency physician in Kenora, Ont., saying the CFPC’s decision to phase in three-year training for family doctors could exacerbate shortages of family doctors in smaller communities.
—Dr. Jabir Jassam, an FP and Medical Post blogger in Ottawa, on the financial challenges being faced by primary care clinics right now. Read more on our online home: CanadianHealthcareNetwork.ca.
—Dr. Andrew Park, OMA president, about the expected higher-thanusual incidences of flu, RSV and COVID infections this fall—the “tri-demic.”
Source CanadianHealthcareNetwork.ca • CBC • Press conference
“It’s a foreseeable disaster and it’s an unnecessary disaster.”
“I don’t know how we can survive.”
“Doctors really need to get prepared.”
FOR WHEN A STRIKES MIGRAINE
Pr CAMBIA® (diclofenac potassium) is indicated for the acute treatment of migraine attacks with or without aura in adults 18 years and older.


Completely dissolve one sachet of CAMBIA® in 30–60 mL of water only and drink immediately1* 30 mL = 2 Tbsp
Significantly measurable plasma levels were observed within 5 minutes of CAMBIA dosing, in fasted healthy individuals1†

Tmax was achieved1,2†:

• After ~15 minutes under fasting conditions‡
• After ~10 minutes under fed conditions§
Tmax: Time to reach maximum plasma levels.
*No other liquids should be used with CAMBIA.
† Clinical significance is unknown.
‡Range: 10–40 minutes.
§Range: 5 minutes–4 hours.
Please refer to the Product Monograph for complete administration information.
Indication and clinical use:
PrCAMBIA® (diclofenac potassium) is indicated for the acute treatment of migraine attacks with or without aura in adults 18 years and older. Efficacy and safety of CAMBIA beyond a single dose have not been studied.
CAMBIA is not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic, basilar or ophthalmoplegic migraine. Safety and efficacy have not been established for cluster headache which is present in an older, predominantly male population.
Geriatrics (> 65 years of age): Safety and efficacy of CAMBIA have not been studied in individuals over 65 years of age, and its use in this population is not recommended.
Pediatrics (< 18 years of age): Safety and efficacy of CAMBIA have not been in patients below the age of 18 years, and its use in this population is contraindicated.

Contraindications:

• Perioperative pain setting of coronary artery bypass graft surgery;
• Third trimester of pregnancy;
• Nursing women;
• Severe uncontrolled heart failure;
• History of asthma, urticarial, or allergic-type reactions after taking ASA or other NSAIDs;
• Active gastric/duodenal/peptic ulcer, active GI bleeding;
• Cerebrovascular, or other bleeding disorders;
• Inflammatory bowel disease;
• Severe liver impairment or active liver disease;
• Severe renal impairment or deteriorating renal disease;
• Known hyperkalemia;
• Children and adolescents less than 18 years of age
Most serious warnings and precautions:
Risk of CV adverse events: Diclofenac is associated with an increased risk of cardiovascular adverse events (such as myocardial infarction, stroke or thrombotic events) that is comparable to COX-2 inhibitors and which can be fatal. The risk may increase with duration of use. Metaanalysis of randomized clinical trials comparing several difference NSAIDs suggest that diclofenac, particularly at higher doses, is associated with an increased risk of cardiovascular adverse events that is comparable to COX-2 inhibitors. Large population-based observational studies conducted in the general population also support these findings. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. To minimize the potential risk for adverse CV event, CAMBIA should be used for the shortest possible duration.
Treatment with CAMBIA is not recommended in patients with preexisting cardiovascular disease (congestive heart failure NYHA II--IV, ischemic heart disease, peripheral arterial disease), cerebrovascular disease, uncontrolled hypertension, and caution should be exercised in patients with risk factors for cardiovascular disease (e.g. hypertension, hyperlipidemia, diabetes mellitus and smoking). These patients should be treated with CAMBIA only after careful consideration. Use of NSAIDs, such as CAMBIA can promote sodium retention in a dose dependent manner, which can result in increased blood pressure and/or exacerbation of congestive heart failure.
Risk of GI adverse events: Use of NSAIDs such as CAMBIA is associated with an increased incidence of gastrointestinal adverse events (such as peptic/duodenal ulceration, perforation, obstruction and GI bleeding) which can be fatal. Elderly patients are at a greater risk.
Risk in pregnancy: Caution should be exercised in prescribing CAMBIA during the first and second trimesters of pregnancy. Use of NSAIDs at approximately 20 weeks of gestation or later may cause fetal renal dysfunction leading to oligohydramnios and neonatal renal impairment or failure. CAMBIA is contraindicated for use during the third trimester because of risk of premature closure of the ductus arteriosus and uterine inertia.
Other relevant warnings and precautions
• CAMBIA cannot be replaced by any other diclofenac formulations, nor is it possible to convert dosing from any other formulation of diclofenac to CAMBIA;
• Not recommended in individuals over 65; increased risk of adverse events; safety and efficacy have not been studied;
• Special care in frail or debilitated patients;
• Caution in the treatment of elderly patients who are more likely to be suffering from impaired renal, hepatic or cardiac function;
• Hepatic, renal and genitourinary impairment;
• Patients with a history of peptic/duodenal ulcer disease or gastrointestinal bleeding;
• Use in phenylketonurics patients;
• Use in women attempting to conceive, first and second trimesters of pregnancy;
• Caution in patients with Helicobacterpylori infection, prolonged use of NSAID therapy, excess alcohol intake, smoking, poor general health status;
• Observation for patients with hemophilia or platelet disorders;
• Monitor patients taking warfarin;
• Blood dyscrasias and antiplatelet effects;
• Use in patients with asthma, seasonal allergic rhinitis, swelling of the nasal mucosa, chronic obstructive pulmonary diseases or chronic infections of the respiratory tract, Quicke’s edema or urticarial, and patients who are allergic to other substances;
• Serious skin reactions;
• May mask signs and symptoms of infectious disease;
• May cause photosensitivity and vision changes upon exposure to sunlight or UV light;
• Neurological adverse events including blurred or diminished vision, decreased alertness or depression;
• Concomitant use with: other NSAIDs, with the exception of low-dose ASA for cardiovascular prophylaxis; diclofenac sodium containing products; anti-coagulants; anti-platelet agents; oral corticosteroids; Selective Serotonin Reuptake Inhibitors; drugs that are known to be potentially hepatotoxic (e.g. acetaminophen, certain antibiotics, antiepileptics)
For more information:
Please consult the Product Monograph at: https://www.miravohealthcare. com/wp-content/uploads/2021/12/Cambia-PM-ENG-Dec2021.pdf for adverse reactions, interactions, dosing and conditions of clinical use. The Product Monograph is also available by calling Miravo Medical Information at 1-866-391-4503.
REFERENCES: 1. CAMBIA ® Product Monograph, Aralez Pharmaceuticals Canada Inc. December, 2021. 2. Diener HC, Montagna P, Gacs G, et al. Efficacy and tolerability of diclofenac potassium sachets in migraine: a randomized, double-blind, cross-over study in comparison with diclofenac potassium tablets and placebo. Cephalagia 2006:26:537–547.
F-CAM-071-04112022
Aralez Pharmaceuticals Canada Inc.* 6733 Mississauga, Ontario L5N 6J5 *d/b/a Miravo Healthcare
NOT EASILY
Can physicians retain passion for the job of medicine without changing the system?
BY ANN GRAHAM WALKER
BURNOUT.
More than half of working physicians suffer this distressing condition today, according to the Canadian Medical Association’s 2021 National Physician Health Survey (NPHS). Among 4,121 physicians surveyed, 53% reported at least one of two burnout symptoms compared to 31% in the 2017 NPHS.
Burnout is a spider that’s biting earlyand mid-career doctors. Indeed, 34% of practising physicians under 35 years old, 44% aged 35 to 54 and 61% of physicians aged 55 and up reported they are likely to “reduce or modify” their clinical work hours in the next 24 months.
What can physicians do to care for themselves and regain the passion that drew them to medicine? The Medical Post asked five physicians.
“Physicians only reach out when they’re really in dire straits,” Dr. John Chiasson, a peer support counsellor with Doctors Nova Scotia Professional Support Program, said in an interview. “I think the people who turn to our Professional Support Program are very important
to Nova Scotians and Canadians. It’s important that they be well so they can stay and give good care.”
Dr. Chiasson is a veteran of 43 years in family practice. “I’ve been in a spot myself where I felt all alone and disconnected and it was dark. Every single person is potentially vulnerable,” he said. “You feel all done when you’re in trouble. If someone asks how you are doing, and really cares about the answer, it changes everything.
“My patients give me hope. They give me purpose. I’ve seen horrible things, but when people come and sit in front of me they know I care what happens to them.”
Dr. Chiasson’s choice to work in a small town helps him to stay connected. Every morning, he walks a few blocks from his home to his clinic. He said it refreshes him, clears his mind for the day. He stops to buy a newspaper, chats with the shopkeeper. Calls people by

Getty Images
DR. JOHN CHIASSON, ANTIGONISH, N.S.
FEATURE
80% of the problem is systemic
12 OCTOBER 2023 THE MEDICAL POST
name as he picks up a coffee.
That connection and sense of belonging is key to staying mentally healthy and retaining passion for medicine, he believes. But “80% of what affects us in burnout is systemic things that are happening to healthcare.
“I believe in advocacy for system change. If you’re willing to wait 10 years, things might be better. But if you can’t wait 10 years, let’s start to make some changes happen on the ground so we can endure the 10 years and get more from it, because we can’t control it all. What we can control is the narrative—what we’re going to say and do, and where we’re going to go tomorrow.”
so many changes in policy, processes and regulations.” Physicians feel “loss of purpose, loss of autonomy”— and loss of control, she said.
“A loneliness has entered healthcare. We’re so focused on producing. Medicine has become so transactional that we’re missing out on what drew us to the healing professions in the first place.”
Dr. Lebovich said “waiting for a miracle to happen—especially from the top down”—may take a long time. “We need to unite to create a culture where it’s safe for people to express their ideas and concerns; where people feel valued, relationships matter. The status quo is no longer tolerated and we need to affect change.”
Dr. Lebovich suggested doctors start by “focusing on what we can control.
She said, “We’re seeing patientprovider relationships as just another area where we’re losing energy and getting frustrated—in fact (medicine should feel like) a fountain of energy and path to fulfillment.
DR. IRITH LEBOVICH, MONTREAL

Leverage the patient-provider relationship
Dr. Irith Lebovich, a nephrologist and founder of Yagrumo, a start-up specializing in training healthcare professionals in “human-centred care,” has been in practice for 20 years. She went through significant workplace stress in an earlier, hospital-based position. Now she has more control over her environment, working in an office she shares with several other physicians.
“We’re living in very turbulent and uncertain times, with a greater number of responsibilities and obligations as human beings,” Dr Lebovich said. “Many physicians, especially over the last three years, have seen things that have affected them in profound ways, and they no longer feel they can continue to be a part of the profession.
“It’s affecting us at a much deeper level than we think. We’re faced with
“We should be leveraging the patientprovider relationship. My patients have saved me. They give back no less than I give.
“Research has been clear that strong patient-provider relationships enhance patient experience and outcomes, and provider satisfaction as well,” Dr.Lebovich said.
Post just before his term ended.
“Historically, doctors worked 80-hour weeks, and if you chat with people who used to work that way, they were a pillar of the community. They got a lot of love. They also were the centrepiece of their hospital and had a strong voice,” Dr. Lafontaine reflected.
“There were doctors’ rooms in the hospitals back then where people interacted and maybe there’d be a birthday cake for one of your colleagues. Those doctors’ rooms are now administrators’ offices or closets where equipment is stored. I think health systems have been under so much pressure to maximize the productivity of every square foot, they cut the places where people gathered to create meaning.
“Over the last 20 years, because of cost-cutting, and the shift to an extractive kind of management, where they try and maximize the amount of value people provide the system for the lowest cost, the question has shifted to how much worth you can get out of a physician, before they feel like they can’t tolerate it anymore and move on.
“Shifting back to investing in people, really starting to humanize systems again, where people feel heard and are a valued part of decision-making . . . I think that needs to be done, moving forward.
“You can be heroic in healthcare. But if (humanizing) changes don’t happen, parallel to that, you’re eventually going to hit a wall, with nothing else to give. For years we’ve tried, as frontline providers, to be that workaround to eliminate the crisis. But as a result, the system thought we could just do more of the same.
“Health systems have still not realized that they can’t just implement solutions by making people work longer and harder, and expect to have a sustainable workforce. I have empathy for decisionmakers because I know they’re just part of a bigger system. We’re all working downstream from where decisions actually get made. But there has to come a point where people say, ‘This is just inhumane, what we’re doing.’
Dr. Alika Lafontaine, an anesthesiologist and past-president of the CMA, wrapped up his year as presidency in August and has gone back to seeing patients as an anesthesiologist. He spoke to the Medical
“We’ve done a good job of suppressing the pain of physicians over the last few decades. And I think the actual reality is that we weren’t necessarily resilient. It’s just that we buried the stories of people

THE MEDICAL POST OCTOBER 2023 13 FEATURE
DR. ALIKA LAFONTAINE, GRANDE PRAIRIE, ALTA. Our stories remain hidden
that weren’t able to tolerate the conditions they were working in. And they kind of buried them within themselves too because of being stoic. We didn’t share our stories. We didn’t talk about our highs and lows, and as a result, our stories remain hidden. And that’s a healing thing when you start to share those stories.”
Empowering H.O.P.E. (Humanizing to Optimize the Person Experience)—a fledgeling collaborative initiative aimed at creating “humanity-centred systems” that reimagine policies, procedures, protocols and leadership.

“There’s been a shift, here in B.C., from ‘accepting the things we cannot change’ to ‘changing the things that are unacceptable,’” Dr. Williams observed. “Providers, patients and communities have begun to advocate for better healthcare together.
“That momentum empowers grassroots movements, reaching a tipping point as the drivers of transformation outweigh the status quo.
B.C.
Reframe burnout as chronic workplace trauma

As a burnout survivor, “it became an opportunity for healing, growth and empowerment,” said Dr. Jennifer Williams, a gastroenterologist and a faculty member for the CMA Physician Leadership Institute.
“Physicians are experiencing a loss of belonging and institutional betrayal,” she said, describing current healthcare systems as a work environment where bullying, harassment, microaggressions and racism are too often the norm. “We seek human connection from a person/institution we trust and instead experience gaslighting or inaction. Our voice is silenced and you can’t speak up for your colleagues or your patients.
“I think what we call ‘burnout’ is a symptom-focused, downstream approach that does little to address the roots of survival behaviours,” she said. “We need to reframe burnout as chronic workplace trauma and build humanity-centred systems based on restorative principles.”
Together with her colleague, traumatologist Jodi Ploquin, Dr. Williams facilitate courses through the CMA, sharing practical skills. In 2022, Dr. Williams also helped form

“Instead of just pulling people out of the river, let’s take an upstream approach and fix the bridge. Let’s transform the system by weaving humanity into our systems, one interaction and team at a time.”
Foster a life outside of medicine
“Every week I see physicians who have symptoms of burnout,” said Dr. Maureen Mayhew, an FP and a physician counsellor with Doctors of BC Physician Health Program. “Anxiety and stress represent another large number of people, and often these symptoms are related to experiences in their workplace. Lack of staffing is one of the big challenges.”
Moral injury “by definition is related to a difference between my values as a physician and the institution I am working for,” Dr. Mayhew said. “And that discord feeds into the cynicism part, or the lack of engagement part, of the burnout triad. I see them as related, moral injury being a driver of
burnout.” (53% of the 2021 CMA NPHS respondents reported experiencing moral distress at work.)
“Burnout is really a system problem,” Dr. Mayhew said. “Physicians have been making up for deficits in the system for years. We do what it takes, to our own detriment.
“It’s hard,” she said, “for physicians to step back and say, ‘No, I’m not going to continue to do this because it’s not good for me.’ It triggers a lot of guilt . . . but it’s possible to conquer guilt and get to a happier place, with more balance.”
Physician leaders can play an important role, Dr. Mayhew said, but they’re often promoted by the system “without sufficient preparation or autonomy. I see leaders—medical doctors—who are burning out, because they straddle administration and medicine and may not have leadership training. Not knowing how to manage conflict gets to them, which is too bad because so many resources could be provided if organizations really wanted to set physician leaders up for success.”
How can physicians create a healthier environment? To begin with, “You can shift your everyday culture—the culture of your team, of your clinic, even patient encounters, to a healthier, boundaried, supportive one,” Dr. Mayhew suggested. “Make your office a place you want to be, paint it a colour you like. Put in books and artwork you like. Get a comfy chair. Play nice music. These small actions can make a difference.
“Foster a life outside of medicine. Even if it’s only 15 minutes every day. It does make a difference. Say ‘yes’ to the stuff that’s fulfilling and ‘no’ to the stuff that depletes your energy.”
Dr. Mayhew has coached physicians who’ve reached the point of leaving medicine, including younger doctors who would be walking away from decades of practice. “When they have appropriate supports, many doctors who considered leaving decide to stay in practice. Most who think about leaving are driven by fears and anxieties, related to stressful situations which they don’t believe will change. With support and guidance, that doctor can learn skills that can transform their daily life.”

14 OCTOBER 2023 THE MEDICAL POST
FEATURE
DR. MAUREEN MAYHEW, VANCOUVER
DR. JENNIFER WILLIAMS, NANAIMO,
HOT FLASH?
In clinical trials, DUAVIVE, a once-daily tablet for the treatment of moderate to severe vasomotor symptoms associated with menopause:
Significantly reduced the number (5.9 vs. 2.8; p<0.001) and severity (0.58 vs. 0.09; p<0.001) of moderate and severe hot flashes per day vs. placebo, as early as Week 4.*
<1% incidence of endometrial hyperplasia or malignancies were observed (0% and 0.30% at Year 1 and 0.68% at Year 2).†‡
Did not increase rates of uterine bleeding or spotting vs. placebo (cumulative amenorrhea at Year 1: 83% vs. 85%, respectively).†
THE

FIRST AND ONLY TREATMENT
1,3,4,§

Clinical use:
Should not be taken with a progestin, additional estrogens, or selective estrogen receptor modulators (SERMs). DUAVIVE has not been studied in women >75 years of age, therefore it is not recommended for women >75 years of age. Not indicated for pediatric use.
Contraindications:
• Active or past history of confirmed venous thromboembolism (VTE) or active thrombophlebitis
• Active or past history of arterial thromboembolic disease
• Hypersensitivity (for example, angioedema, anaphylaxis) to estrogens, bazedoxifene, or to any ingredient in the formulation or component of the container
For more information:
• Undiagnosed abnormal genital bleeding
• Known, suspected, or past history of breast cancer
• Known or suspected estrogen-dependent malignant neoplasia
• Liver dysfunction or disease as long as liver functions tests have failed to return to normal
• Endometrial hyperplasia
• Known protein C, protein S, or antithrombin deficiency or other known thrombophilic disorders
• Known or suspected pregnancy, women who may become pregnant, and nursing mothers
• Partial or complete loss of vision due to ophthalmic vascular disease
Most serious warnings and precautions: Risk of stroke and deep vein thrombosis: estrogen-alone therapy (mean age 63.6 years).
Therefore, estrogens with or without progestins:
Did not increase breast pain or density vs. placebo (Weeks 9–12: 6% vs. 5%, respectively).‡

DUAVIVE is indicated in women with a uterus for the treatment of moderate to severe vasomotor symptoms associated with menopause.

• Should not be prescribed for primary or secondary prevention of cardiovascular diseases
• Should be prescribed at the lowest effective dose and for the shortest period possible for the approved indication
Other relevant warnings and precautions:
• Possible risk of ovarian cancer
• Monitor blood pressure with hormone replacement therapy use
• Caution in patients with otosclerosis
• Caution in women with pre-existing endocrine and metabolic disorders
• Caution in patients with rare hereditary galactose intolerance
• Abnormal vaginal bleeding
• May increase pre-existing uterine leiomyomata
• May exacerbate previous diagnosis of endometriosis
Please consult the Product Monograph at http://pfizer.ca/pm/en/duavive.pdf for important information relating to adverse reactions, drug interactions and dosing information, which have not been discussed in this piece. The Product Monograph is also available by calling 1-800-463-6001.
SERM=selective estrogen receptor modulator
* SMART 2: 12-week, double-blind, placebo-controlled trial in 318 women who had seven moderate to severe hot flashes/day or ≥50/ week at baseline. Primary endpoint assessed efficacy of vasomotor symptom relief. Secondary endpoints included: number of mild, moderate, and severe hot flashes, sleep parameters (Medical Outcomes Study [MOS] scale), and overall Menopause-Specific Quality of Life (MENQOL) questionnaire. Mean daily number of moderate and severe hot flashes at baseline: 10.3 for DUAVIVE, 10.5 for placebo.1,2

† SMART 1: 24-month, double-blind, placebo- and active-controlled, dose-ranging trial of 3,397 women who were randomized to DUAVIVE (n=433), raloxifene 60 mg, or placebo. Women took calcium and vitamin D (Caltrate 600 + D™) daily. Primary endpoint was the incidence of endometrial hyperplasia; secondary endpoint was the treatment of vasomotor symptoms.1
• May increase the risk of VTE
• Risk of gallbladder disease
• Caution in patients with history of liver and/or biliary disorders
• Caution in women with hepatic hemangiomas
• Angioedema
• Caution in women with systemic lupus erythematosus
• Cerebrovascular insufficiency
• May exacerbate epilepsy
• Fluid retention
• Not recommended in renal impairment
• Not recommended in premenopausal women
• Women with higher BMIs may exhibit decreased bazedoxifene exposure which may be associated with an increased risk of endometrial hyperplasia
‡ SMART 5: 12-month, double-blind, placebo- and active-controlled trial of 1,843 women who were randomized to DUAVIVE (n=445), conjugated estrogens 0.625 mg/bazedoxifene 20 mg (n=474), bazedoxifene 20 mg (n=230), conjugated estrogens 0.45 mg/ medroxyprogesterone acetate 1.5 mg (n=220), or placebo (n=474). Women also took calcium, 600 mg and vitamin D, 400 IU daily.1 § Comparative clinical significance has not been established.
References: 1. DUAVIVE Product Monograph. Pfizer Canada ULC, January 16, 2019. 2. Pinkerton JV, et al. Relief of vasomotor symptoms with the tissue-selective estrogen complex containing bazedoxifene/conjugated estrogens: a randomized, controlled trial. Menopause. 2009;16(6):1116–24. 3. Data on file. Pfizer Canada ULC. 4. Pickar JH, et al. Tissue selective estrogen complex (TSEC): a review. Menopause. 2018;25(9):1033–45.

PrDUAVIVE® treats moderate to severe menopausal hot flashes1 DUAVIVE TM Wyeth LLC, owner/Pfizer Canada ULC, Licensee © 2023 Pfizer Canada ULC, Kirkland, Quebec H9J 2M5 PP-DUA-CAN-0211-EN
that combines conjugated estrogens with a SERM (bazedoxifene)
HELP THEM DISCOVER
Job satisfaction
BY KYLIE TAGGART
What makes physicians get out of bed in the morning? Simple, really: It’s the patients.
When anecdotal and more formal evidence suggest that physicians’ job satisfaction is waning, what is it that keeps physicians going? We asked physicians from various specialties about the best and worst part of their practice, and the answers were surprisingly similar: All said that the best part of their job was their connection and relationships with patients, whether it was a short interaction or a long-term relationship.
“I enjoy the opportunity to meet new and interesting people every day,” shared Dr. Colin Audain, president of Doctors Nova Scotia, assistant professor in the faculty of medicine at Dalhousie University and a staff general anesthesiologist at Victoria General Hospital and the Halifax Infirmary.
“Although my interactions are typically brief, they are long enough for me to learn something interesting about the person in my care.”
Obstetricians might also have a short interaction, but a meaningful one. “Obviously having the privilege of being present when a new life comes into the world is very rewarding,” said Dr. Amanda Black, president of the Society of Obstetricians and Gynaecologists of Canada and professor of obstetrics and gynecology at the University of Ottawa.
For a number of specialties, this connection is there for a foundational part of the patients’ life.
“The most rewarding thing is the relationships I develop with patients and families. I’m really lucky to get to be part of their lives sometimes for their whole childhood, sometimes for just a portion of it,” said Dr. Ayisha Kurji, a consultant pediatrician in Saskatoon and assistant professor of pediatrics at the University of Saskatchewan. Her favourite thing is when former patients return and tell her about their lives, or when a child who was struggling with development then gives her a craft that shows they’ve conquered that milestone.
Dr. Michelle Keir meets her patients after they transfer out of pediatric care.
She’s a clinical assistant professor at the University of Calgary and a cardiologist at the Libin Cardiovascular Institute caring for adult patients with congenital heart disease.
“That’s the best part, getting to know people when they’re young adults and following them through their entire trajectory and really seeing them grow as humans and helping them manage their heart disease as they get older,” she said.
PATIENT COLLABORATION
As a physician, a relationship with patients includes working together. Dr. Sandi Dumanski, a nephrologist at the Libin Cardiovascular Institute enjoys collaborating with patients in her care.
“Nephrology lends itself very well to providing personalized care and that individualized medicine that we all dream of providing,” she said. “And through that we get to build really collaborative relationships with each of our patients, who may handle their disease process very differently from each other.”
The biggest lift comes when people’s
16 OCTOBER 2023 THE MEDICAL POST Shutterstock FEATURE
Doctors talk about the best and worst parts of their jobs
health improves because of effective clinical management. Dr. Gehad Gobran, president-elect of Doctors Nova Scotia and a family physician in Bedford, N.S., has a patient who thanks him for saving his life every time they meet. Dr. Gobran suspected the patient’s chest pains were signs of an acute myocardial infarction, sending the patient for emergency, lifesaving treatment.
Addictions psychiatrist Dr. Leslie Buckley often works with patients who want to make a change in their lives. For example, a patient recently stopped using cannabis after many years of use and found a dramatic improvement in his anxiety and overall function. “Seeing dramatic changes in how someone feels and functions when they reduce their substance use is very rewarding,” said Dr. Buckley, chief of the addictions division at the Centre for Addiction and Mental Health in Toronto.
There’s a celebration in Dr. Keir’s clinic when a patient with congenital heart disease gives birth. Managing a pregnancy in this patient population is stressful because of a high risk of cardiovascular complications. “Our rule is postpartum, they have to bring the baby, so that’s always a good day when they’ve had a successful pregnancy and have done well and are feeling well and we’ve been a part of that,” she said. “We don’t take care of the baby. We just want to see the healthy, happy baby.”
Dr. Ivan Litvinov, associate professor of dermatology of McGill and director of the division of dermatology at McGill and McGill University Health Centre, finds immense satisfaction helping children in the Cree Nation of Chisasibi in Northern Quebec. There he sees children with eczema, some with up to 90% of their body covered with red thick plaques that can get infected. “Those kids are not able to sleep, they’re not able to function, they’re not able to go to school. If the child isn’t well, then it affects the entire family,” he explained. But Dr. Litvinov has been able to get them advanced treatments, and the “eczema melts away like snow in May.”
Any job gets dull when it’s repetitious, so for some it’s the constantly changing day that’s enjoyable. “My specialty is
very unique in that there is so much variety,” explained Dr. Black. “One day I am in the operating room, another day I am in labour and delivery delivering babies, another day I can be in the clinic, another day I am doing research, administrative work or advocacy work.”
Others note that an inspiring part of their job is the science: The research that lets Dr. Litvinov treat previously challenging dermatological diseases with biologics or targeted therapies; the clinical procedures and chemistry that allows Dr. Audain to manipulate patients’ physiology so they feel no pain during surgeries; or the emerging biological and psychological tools that allow Dr. Buckley to help her patients.
WORST PARTS
If the best part of the job is the patients, it’s no great leap of logic to understand that the worst parts are things that take physicians away from patients, especially a patient’s death.
For Dr. Audain, it’s “transporting patients from the ICU to the OR for an organ donation procedure. It is always difficult for the families and it makes me feel sad for the families who are losing a loved one.”
The patients under Dr. Keir’s care are young, but they often have conditions that aren’t consistent with a long life. “It can be rewarding to help them make end-of-life decisions and know what to expect, but it’s always difficult when we lose somebody.”
The nature of Dr. Dumanski’s specialty also means witnessing poor outcomes. “Kidneys and kidney disease itself can actually be very unpredictable,” she said. “Even if you feel like you’re doing a great job at managing people’s health and ticking all the boxes to get them to the next step, a lot of times, unexpectedly, you can have negative outcomes, including losing your patients.”
Seeing patients suffer, like a young child with aggressive leukemia, is an emotionally distressing part of the profession, Dr. Groban noted. Working during an opioid-use crisis and losing patients to overdose is heartbreaking, Dr. Buckley said. Dr. Dumanski said
some days she feels powerless against social determinants of health, like food insecurity, that get in the way of her patients becoming or staying well.
PAPERWORK
Apart from the pain of losing patients or seeing them suffer, a choir of physicians would no doubt sing the refrain: “The worst part is the paperwork.” It’s frustrating because it takes away from the very thing that gives physicians joy: interacting with patients and working with them to get the best outcome. Inputting data into EMRs and portals, filling out forms, dealing with insurance claims, it “is practically impossible to keep on top of that and it takes significant time away from actual handson patient care,” Dr. Black said.
Another main source of frustration is access to care, such as when elective surgeries are cancelled due to resource limitations elsewhere in the hospital, Dr. Audain said, or when there’s no OR time for gynecologic patients, Dr. Black said. There’s also stress on those practising because of a limited number of specialists. Dr. Keir talked about being understaffed, Dr. Kurji cited long wait times for kids needing treatment for eating disorders, and Dr. Litvinov worried about economic stressors causing his colleagues to take up administering cosmetic procedures, leaving patients with even fewer consulting dermatologists.
Another downside is how the practice of medicine takes its toll on physician health. The stress can be “very exhausting both physically and mentally,” Dr. Black said. Dr. Audain said that as he ages, it’s harder to recover from an on-call shift. Dr. Black also cites being up at 3 a.m. as the worst part of her work, but adds that having a great team makes it bearable.
In the end, the positive outweighs the negative, Dr. Keir said. Hopefully that’s the case for every physician: that the best parts—be it delivering a healthy baby, getting a handmade necklace from a toddler, providing pain-free surgery, or navigating care for someone with a complex disease—are far more satisfying than the worst parts.
THE MEDICAL POST OCTOBER 2023 17 FEATURE
We’ e y a d y a e . We’ e YOU’RE CHOOSING REMICADE® .
A Ja e , we ly bel eve ha ea me dec h ld be ba ed wha a hy c a de e m e a a e f each a e .
You and your patients treated with REMICADE® can continue to count on the dedicated support of the Janssen BioAdvance® Program.
REMICADE® is indicated for1:
• reduction of signs and symptoms, induction and maintenance of clinical remission and mucosal healing and reduction of corticosteroid use in adult patients with moderately to severely active Crohn’s disease who have had an inadequate response to a corticosteroid and/or aminosalicyate. REMICADE® can be used alone or in combination with conventional therapy.
• treatment of fistulising Crohn’s disease in adult patients who have not responded despite a full and adequate course of therapy with conventional treatment.

• reduction of signs and symptoms and induction and maintenance of clinical remission in pediatric patients with moderately to severely active Crohn’s disease who have had an inadequate response to conventional therapy (corticosteroid and/or aminosalicylate and/or an immunosuppressant). The safety and efficacy of REMICADE® is not established in patients less than 9 years of age.
• reduction of signs and symptoms, induction and maintenance of clinical remission and mucosal healing, and reduction or elimination of corticosteroid use in adult patients with moderately to severely active ulcerative colitis who have had an inadequate response to conventional therapy (i.e., aminosalicylate and/or corticosteroid and/or an immunosuppressant).
• reduction of signs and symptoms, induction and maintenance of clinical remission, and induction of mucosal healing in pediatric patients with moderately to severely active ulcerative colitis who have had an inadequate response to conventional therapy (i.e., aminosalicylate and/or corticosteroid and/or an immunosuppressant). The safety and efficacy of REMICADE® have not been established in patients less than 6 years of age.
Please consult the product monograph at www.janssen.com/canada/products for important information relating to contraindications, warnings, precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The product monograph is also available by calling 1-800-567-3331.
Program
Refe e ce : 1. REMICADE® Product Monograph. Janssen Canada Inc., October 15, 2021. Ja e I c. 19 Green Belt Drive | Toronto, Ontario | M3C 1L9 | © 2022 Janssen Inc. | All trademarks used under license. | CP-296507E
Innovative recruitment
Chief physician recruiters get creative as provinces try new strategies to hire doctors
Virtual reality tours. $150,000 signing bonuses. International missions. This is the new world of physician recruitment in Canada.
The country needs more physicians. A 2022 survey found that one in five Canadians does not have a family doctor. And the challenge is growing. Canada is expected to be short almost 44,000 physicians, including more than 30,000 family doctors and general practitioners by 2028, according to an RBC study.
This shortage is attributed to factors including the limited number of medical school students and a cap on residencies, as well as the challenges international medical graduates face in trying to work here.
While the country aims to fix this shortage, provinces need to get creative to recruit enough physicians to treat their citizens.
BY ABIGAIL CUKIER
“We are not graduating enough new physicians, and physicians are relocating to different regions across Canada, which benefits the community they are relocating to, but not the overall healthcare system in Canada,” said Carly Cox, lead for the Canadian Society of Physician Recruitment. “Every province and territory is striving to develop lucrative and attractive offerings to physicians. Some are more ahead than others and most are starting to break down the barriers to internationally trained physicians, which is a great sign.”
Cox says that physician recruitment has always been challenging but the pandemic shed light on the importance and gaps within the healthcare system.
Brad van den Heuvel, director of physician recruitment for the Greater Hamilton Health Network, says the pandemic also affected recruitment in his city. “If a physician’s spouse or partner
THE MEDICAL POST OCTOBER 2023 19
Shutterstock FEATURE
does not need to go into their office any more, some are willing to move further away from the Greater Toronto Area,” he says.
VIRTUAL TOURS
Rebecca Gill, director of health workforce, recruitment and pharmaceutical services for the Prince Edward Island Department of Health and Wellness, says during the pandemic, doctors, perhaps looking for a slower pace or a more COVID19-safe province, decided to return home to P.E.I. or to relocate there. It also forced the recruitment team to get creative.
In 2021, when doctors were unable to travel to P.E.I. due to travel restrictions or increased work commitments, the Physicians Recruiting Physicians program worked with a local company to create a virtual reality tour of Summerside, P.E.I., which offers 360-degree views of the beach, local ice rink, walking trails, ice cream parlours and restaurants, all narrated by chief physician recruiter Dr. Megan Miller. It also features physicians talking about what it is like to live and work in Summerside and views of the operating room and emergency department. The team also created a tour of Charlottetown.
They sent the virtual reality headsets to physician leads in other provinces and now that they have returned to conferences, they take them there too.
“It became a very effective recruitment tool and a great way to start conversations and showcase what P.E.I. has to offer,” Gill said. “We’ve had some people who saw the virtual reality content and then said they want to do a locum in P.E.I. or come visit with their family in the summer.”
The Physicians Recruiting Physicians (PRP) program, implemented in early 2021, is a partnership between the Medical Society of Prince Edward Island, Health PEI and the P.E.I. Department of Health and Wellness. “It introduced a chief physician recruiter, which meant we now had a physician working with us on the frontlines of recruitment, carrying authentic messages about what it is like to live and work as a physician and helping navigate some of the concerns that physicians might have,” Gill said.
“The program empowered our current physicians to be a part of the recruitment process and it bolstered our recruitment work. We have seen our recruitment numbers increase.” In 2021 and 2022, P.E.I. recruited 31 and 29 new physicians respectively, compared to 20 in 2020, before the PRP program started.
Gill says another draw to P.E.I. is the government’s commitment to collaborative health centres and establishing patient medical homes. “Physicians want to work as part of a collaborative team,” she said. “Another draw is our provincial
electronic medical record. No other province has that and, because of P.E.I.’s size, we can do these kinds of innovative undertakings.”
LOCUMS
Van den Heuvel agrees that doctors are looking to work in team-based care, and he believes that is a draw for Hamilton, which has many team options, including the largest family health team in the province, with more than 160 doctors.
Of course, physicians are also looking for features like good schools for their children, affordable housing and entertainment and recreation opportunities, van den Heuvel says, as well as job opportunities for partners. He says many physicians are also interested in locum positions.
In 2022, Hamilton recruited 31 family doctors for locum positions and 35 permanent family doctors. But in the same year, 32 family doctors retired or moved. Recruitment numbers are increasing though. In 2019, Hamilton recruited 20 physicians. Numbers have risen every year since (except for 2020). Hamilton has 365 family doctors, not including those on short-term contracts. Based on its 2021 population of 569,355 and the Ontario Ministry of Health recommended ratio of family doctors to residents, Hamilton at full capacity would have 438 family doctors.
To support recruitment, van den Heuvel’s team conducts annual succession planning forums to guide physicians nearing retirement on how to make their practice more attractive to new recruits. They also attend local and provincial recruitment conferences and are increasingly attending U.S. and international conferences. In fact, last year more than half of Hamilton’s recruits completed medical school and residency abroad, both Canadians and from other countries. This year, the team will attend conferences in Scotland and Ireland.
Many provinces, including Newfoundland and Labrador, are also working on ways to make it easier for physicians to work in their jurisdiction, such as reviewing licensing and registration criteria and streamlining the licence application process. The Newfoundland and Labrador government also launched the Physician Signing Bonus Program. General practice and specialist physicians who agree to provide up to five years of service in the province can receive up to $150,000, with an additional $25,000 for physicians recruited into the most difficult-to-fill positions.
Meanwhile, Horizon Health in New Brunswick is offering a $2,000 reward to community members who successfully refer a doctor to them. There is no limit to the number of candidates a person can refer.
For many of these recruitment initiatives, it will take time to determine their impact. But a physician shortage has led to innovation. “Recruitment is complex. It’s not just putting a job in front of somebody and they sign on the dotted line,” Gill said. “A lot of conversations have to happen. You are asking someone to move from a different province or a different country. A lot of work needs to happen.
“It’s a balance of quality and speed. We need to be efficient, but we also want to ensure we’re hiring quality health professionals who will be a great fit for our system and will choose to stay here for a long time.”
20 OCTOBER 2023 THE MEDICAL POST FEATURE
“Recruitment is complex. It’s not just putting a job in front of somebody and they sign on the dotted line.”
>11 years
of experience in chronic migraine
> 400 headache specialists > 3,500 patients
have enrolled at least one patient in the AbbVie Care Support Program1*





with chronic migraine have been supported in AbbVie Care since 20211*
PrBOTOX® (onabotulinumtoxinA) is indicated for the prophylaxis of headaches in adults with chronic migraine (≥15 days per month with headache lasting 4 hours a day or longer). 2
Refer your potential BOTOX candidates to a local physician experienced in treating chronic migraine with BOTOX. Visit FindABOTOXSpecialist.ca for a list of expert clinicians trained in administering BOTOX in your area.
For more information:
Please consult the Product Monograph at: abbv.ie/BotoxCanadaPMEN for contraindications, warnings, precautions, adverse reactions, interactions, dosing and conditions of clinical use. The Product Monograph is also available by calling: 1-800-668-6424.
*Clinical significance has not been established.
REFERENCES: 1. Data on File. AbbVie Corporation. 2. Current BOTOX Product Monograph, AbbVie Corporation.
© 2023 AbbVie. All rights reserved.
BOTOX and its design are trademarks of AbbVie Corporation.
CA-BCM-220074A / AL23
*
e-Prescribing improves clinical workflows, leaving more time for patient care
Dr. Rashaad Bhyat, a family physician in the Greater Toronto Area and Senior Clinical Leader at Canada Health Infoway, discusses how digital health tools like e-prescribing can help ease administrative burden by improving clinical workflows.

What are some of the most significant pain points within the physician workflow?
Canadians are living longer, and many are living longer with multiple chronic medical conditions. The more complex a patient’s concerns are, the more timeintensive the associated administrative tasks will be. As a rule of thumb, if I spend one hour on direct patient care, I’m spending 30 minutes to one hour on non-clinical tasks. This can include charting and documentation, gathering and interpreting clinical information — either in preparation for, or after a patient visit to complete a referral, for example — and preventative care measures. Even something as seemingly simple as the prescription process comes with complexities, to ensure patients receive their medication in a safe and timely manner. Beyond the time I spend on administrative tasks, there’s also the time my staff spends to retrieve and organize patients’ health information.
In recent years, the issue of the administrative burden on health care providers has become an increasingly prevalent concern. In the Canadian Medical Association’s National Physician Health Survey published last August, respondents spent an average of 10 hours per week on administrative tasks. As a result, nearly half were considering reducing their clinical work in the next 24 months, when the country is seeing a worsening shortage of family physicians.


How can digital tools like e-prescribing help improve clinicians’ workflow and ease the administrative burden?
With all the pressures on our health care system, it’s increasingly important to prioritize implementing digital health tools that streamline processes and allow health care providers to focus more of their time on direct patient care. While so many touch points in our lives have become digital, our health care system remains largely reliant on paper and fax-based communication,
with considerable ‘phone tag’ mixed in — systems that are unreliable and inefficient.
Far too often, we encounter pharmacies or specialists having difficulty receiving a fax, or communications coming through that require further clarification, all adding up to time away from patients. Tools like PrescribeIT®, a national e-prescribing service, helps streamline one of the most common processes in a physician’s workday by connecting prescribers to community-based retail pharmacies, allowing them to send prescriptions directly from their EMR to the pharmacy management system at their patient’s pharmacy of choice.
By creating a secure, direct connection between the prescribers and pharmacies, PrescribeIT® doesn’t just modernize the transmission of prescriptions, but also facilitates better, more efficient communication. Clinics and pharmacies alike are often so busy, it can make addressing even the simplest question a challenge, delaying patient care. PrescribeIT®’s integrated messaging tool allows prescribers and pharmacies to exchange secure digital clinical communications directly from their EMR and pharmacy management systems to quickly address any questions and align on next steps. In fact, 81 per cent of prescribers say that it improves their clinical workflow, according to a Canada Health Infoway survey.
How do you think broader adoption of e-prescribing will improve health care delivery and the quality of care patients receive?
facilitated by PrescribeIT®, enables increased communication. All health information exchanged throughout the process is documented directly within the physician’s EMR, eliminating extra administrative work while still ensuring an accurate and up-to-date patient record. This gives physicians better visibility into details like when a prescription is filled or when refills are requested, which helps to improve adherence to medication and continuity of care. Implementing PrescribeIT® can also significantly reduce errors within the prescription process — recent survey results show that at least 57 per cent of pharmacists believe PrescribeIT® helps reduce overall medication errors.
Do you think e-prescribing is here to stay?
Modernizing the health care system with standardized health data and digital tools is a key national priority, and in tandem, we’re starting to see provinces like Ontario commit to ending the use of fax within health care. When we consider that 55 per cent of adults aged 18 to 79 use at least one prescription medication each month, reforming the prescription process to enable more effective medication management represents a huge area of opportunity that closely aligns with these goals. Implementing PrescribeIT® is a step towards addressing these priorities, and should provide clinicians with more time to focus on patient care.
Any time an element of a patient’s care is transferred to another member of their care team, be it a pharmacist or a specialist referral, maintaining effective communication within the patient’s circle of care is essential. The direct connection between care providers, Visit prescribeit.ca to learn more about Canada’s only national, not-for-profit e-prescribing service.
*ADVERTISEMENT*
COOL JOBS
Thinking you might want to try something new? Look to these physicians for inspiration
BY LOUISE LEGER
Whether you are an ER doc, a seasoned FP or a new grad, there are plenty of opportunities for adventures in medicine. Here is a sampling of some Canadian physicians whose practices veer off the beaten track.
Anesthesiologist, Doctors Without Borders

Dr. Pamela Paquet
Can you describe your current job?
I am an anesthesiologist based in Quebec City working at CHU de QuébecUniversité Laval Hospital where I have a general practice more focused on pediatric and obstetric anesthesia. I have also been involved with Doctors Without Borders since 2021 and have done three assignments so far in South Sudan, Haiti and the Central African Republic. Right now, I am doing my fellowship in Global Anesthesia at Oxford University Hospitals (U.K.).
What made you decide to do the
Doctors Without Borders work?
One of my biggest motivations for doing this kind of work is the vision of fighting against global inequities through my passion for global health and my expertise in anesthesiology. As anesthesiologists, we are an international community and I believe we can and should engage in worldwide teamwork.
There is a lot of richness in sharing, learning and teaching in very diverse contexts.
Can you share a challenging situation you encountered?
I was in Bentiu, South Sudan, in a camp for internally displaced people seeking shelter from the extreme flooding and violence. We were providing emergency surgical care in specialized tents. Our team had one general surgeon and one anesthesiologist (me) on call 24/7 for seven weeks.
We had several challenging C-sections. One of them involved a 20-year-old woman who came to us in a critical state. Her baby was already dead and she was barely conscious. I rushed to the operating theatre to save her, but when I called the blood bank, I was told they didn’t have her blood type available. The team came together urgently, putting all efforts into saving her and finally found her sister in the camp who luckily had the same blood type. She gave her blood to save her sister. That story is one of many that stayed with me after my assignment. I am still amazed by the resilience and strength of the people we treated in the camp.
What qualities should someone have to do this kind of work?
Flexibility, teamwork, leadership, creativity and communication skills are very helpful. The work is not easy and full of challenges, so you need strong motivation to keep you going through long hours, travels, basic accommodations, safety issues, low resources and adapting to cultural differences. That being said, it can also be extremely rewarding.
THE MEDICAL POST OCTOBER 2023 23 Getty Images;
FEATURE
Dr. Pamela Paquet
Team physician for the Winnipeg Blue Bombers
Dr. Chris Morrow
Was this something you always planned to get into?
No, this was definitely not my plan. I got into it after I had already been practising for a couple of years. I had always thought I would end up being more of a generalist but was drawn to musculoskeletal care. As an active person, the practical elements of helping people move was a natural fit.
What’s your favourite part of the job?
Like any job, the best part is the people you work with. We have a great team in terms of our clinic staff as well as a great training staff with both football teams (the Blue Bombers and also the University of Manitoba Bisons Varsity Football, where I am also team physician). When we won the Grey Cups in 2019 and 2021, it was great to celebrate it with great colleagues. From a patient care perspective, I enjoy following up with patients I have gotten to know and getting to play a small but meaningful role with teams.

What are the most common conditions/ injuries you treat?
In the Winnipeg Legacy Sport Medicine Clinic where I also work, we see a lot of osteoarthritis and various tendinopathies. In football, there are more traumatic injuries of all sorts. In the span of a season, you get everything from concussions, and simple sprains to ACL/Achilles ruptures and joint dislocations, and always have to be prepared for the worst-case scenarios.
Can you share an anecdote about a challenging situation you experienced? More of a funny one. In the rivalry game between the Bombers who wear blue and Saskatchewan Riders who wear green, a Saskatchewan player had a significant wrist injury, and needed to be reduced and casted before returning home. The Bombers won by a lot, and the player
was upset that we didn’t have green casts. Going home after a drubbing with a blue cast was not his idea of fun!
What qualities should someone have to do this kind of work?
There are lots of different types of people who go into sports medicine, there isn’t one way to do it. What I have found works best are the three As: ability, affability and availability. I learned that from my grandfather who was a GP in rural Ireland; it was true then and is true today.
Flight surgeon and FP with the Royal Canadian Air Force
Dr. Joelle Thorgrimson
Was this something you always planned to get into, or did you get there by a more indirect route?
During medical school, I didn’t know about the field of aerospace medicine until I met a retired flight surgeon who educated and inspired me. With my background in physics and love of aviation, it seemed like the perfect area of medicine for me!
What’s your favourite part of the job?
As a civilian IFR-rated commercial pilot, the highlight is flying with the military aircrew to have firsthand experience of the stressors of flight and performing

military missions globally. Flying in a fighter jet or a search-and-rescue helicopter has given me a huge amount of respect for what military aircrew experience daily and helps me better understand what is needed medically to be successful and safe in these environments.
Can you share an anecdote about a challenging situation you have encountered?
Working in austere environments, whether remote or in foreign countries, can result in challenging decision-making. For example, I have been in a foreign medical facility where I have had to choose between dealing with patriarchal medical staff, language barriers, substandard care and optimizing the risk of staying in the care facility—versus leaving to ensure the best outcome for the patient. There is no right answer in these situations.
What qualities should someone have to do this kind of work?
Aerospace medicine is a growing field with a strong operational focus. Having real-world experience in these environments is paramount to be able to appropriately treat, manage and advise. Arguably the military aviation context provides the best opportunity to do this, however, there are sacrifices, such as frequent relocations and deployments overseas. If you are interested in learning more about aerospace medicine, check out the Canadian Society of Aerospace Medicine!
24 OCTOBER 2023 THE MEDICAL POST
FEATURE
Dr. Chris Morrow
Dr. Joelle Thorgrimson
Considering NORVASC?


Hypertension
NORVASC (amlodipine besylate) is indicated for the treatment of mild to moderate essential hypertension. Combination of NORVASC with a diuretic, a beta‑blocking agent, or an angiotensin converting enzyme inhibitor has been found to be compatible and showed additive antihypertensive effect.1
Chronic stable angina
NORVASC is indicated for the management of chronic stable angina (effort‑associated angina) in patients who remain symptomatic despite adequate doses of beta blockers and/or organic nitrates or who cannot tolerate those agents. NORVASC may be tried in combination with beta blockers in chronic stable angina in patients with normal ventricular function. When such concomitant therapy is introduced, care must be taken to monitor blood pressure closely since hypotension can occur from the combined effects of the drugs.1
When you purposely prescribe the Viatris original brand NORVASC, help your patient get it.
Some insurers limit full cost coverage for higher cost interchangeable drugs to patients who meet certain criteria, and in some instances, documentation from the prescriber is required. There is a possibility that the patient may need to contribute out of pocket where those conditions are not met.


1



Write the Viatris original brand name, NORVASC, and include “no sub,” when appropriate, on your patient’s prescription. Encourage your patients to visit ViatrisOriginals.ca so they can:

• Download a payment assistance card to help patients who have no insurance or whose insurance co payment amount might be a barrier to obtaining the Viatris original brand medication. This card can help patients obtain the Viatris original brand medication at little or no additional cost compared to the generic version.*


Remind your patient to ask for the Viatris original brand NORVASC at the pharmacy.

ViatrisOriginals.ca NORVASC® is a registered trademark of Viatris Specialty LLC, used under permission by Upjohn Canada ULC, a Viatris company. VIATRIS and VIATRIS & Design are registered trademarks of Mylan Inc., used under permission by Upjohn Canada ULC, a Viatris company. ©2023 Viatris Inc. All rights reserved. NORV 2022 0204E JL2023 Consult the Product Monograph at https://pdf.hres.ca/dpd_pm/00069708.PDF for contraindications, warnings, precautions, adverse reactions, interactions, dosing,
Product Monograph may also be obtained by calling 1 877 446 3679.
and conditions of clinical use. The
* Subject to change. The Viatris Originals Program is available in all provinces except Quebec. Availability and level of payment assistance vary by brand medication and province.
1.NORVASC® [product monograph]. Canada.Upjohn
Reference:
Canada ULC.
2
3
Performing arts physician
Dr. Grant Lum

What do you do every day?
I take care of a lot of athletes—from professionals to the weekend warriors. Then I have an entire other side of my practice where I take care of performing artists. For example, I have consulted for the adult school of the National Ballet, other dance companies, Cirque du Soleil, Mirvish Productions and other events. Sometimes I am backstage treating dancers, musicians or performers. Sometimes it’s more that an injury happens on a Saturday night, and they’re sent to me early Monday.
up against their shoulder for four or five hours a day. And then you have vocalists. This sometimes falls to ENT doctors, but I deal with vocalists as well.
What was your experience working at big concerts?
One of the more interesting and demanding events I worked at years ago was an outdoor Tragically Hip concert. I was the chief physician for that venue, which meant we were taking care of all the band members, the stage crew, plus 60,000 fans. We ran a little M.A.S.H. tent and over the course of about 12 hours, saw about 800 patients. It was crazy. We saw heat stroke, injuries from falling in the mosh pit, and plenty of drug overdoses. Some of the worst were head injuries or neck injuries from falling. There was a whole category of injury we were calling positional asphyxia—mainly it was young women in the mosh pit getting crushed on all sides by bigger people. The security team would reach into the mosh pit and pull them out, and they were basically hypoxic.
What is the coolest part of your job?
team hiking to base camp and to the summit of Kilimanjaro.
You are also a family physician in Sechelt, B.C. How much time does your reservist role take?
What kind of patients do you have in the performing arts?
There are three big categories. The first is dance. Dancers are incredible athletes, and like other athletes, they get strained hamstrings, Achilles tendonitis and patellofemoral syndrome, for example. There are certain injuries unique to dance because of their extremely flexible bodies. There’s a self-selection process that happens and those (flexible) bodies show promise and continue to train and achieve high-level careers. But with that excessive hypermobility, certain problems arise, like early arthritis of the hips. Then there are instrumentalists, who are doing the same movements repeatedly, sometimes in very awkward positions, like a violinist holding a violin with the side of their neck, their chin
We joke that most of us who do performing arts medicine are frustrated rock stars just waiting for a big break. I’m a jazz trombonist and singer so I appreciate the arts. To watch people, say from Cirque du Soleil, do the difficult things they do, and then to be able to help them to get back to it, to this thing they love, is very gratifying.
Reservist medical officer, Canadian Armed Forces
Dr. Paul Dhillon
What does a reservist medical officer do? There is work in traditional clinics but also the opportunity to participate in overseas operations. I’ve been lucky enough to do some basic dive medical training and qualified as a flight surgeon. I’ve had the opportunity to be the physician for the Antarctica Marathon and more recently as a physician on a
The beauty of being in the reserves is that while there is a minimal commitment of roughly one night per week and one weekend per month for eight months of the year, there are many opportunities available to spend more time working in a military environment.
I probably spend four to five months participating in military activities, research, teaching and expedition medicine.

What have been your top activities? I had the opportunity to serve on HMCS Victoria, one of Canada’s hunter-killer submarines.
On my first day on the submarine, we had a medical issue as we were heading out to sea, and I had to ask the captain of the sub to turn it around and arrange a medevac. It was an interesting and challenging experience. I am happy it happened while we were still above the sea!
More recently I did a short stint on Operation Impact in Kuwait, which gave me incredible insight into the sacrifices and challenges that Canadian military members experience when deployed overseas. I’m also heading off shortly to be the expedition physician for a small group summit in Kilimanjaro to provide medical care and summit one of the seven peaks.
26 OCTOBER 2023 THE MEDICAL POST
FEATURE
Dr.GrantLum
Dr. Paul Dhillon
Join us for the presentation of the prestigious:
HRF Medal of Honour
Prix Galien Canada - Innovative Product Award
HRF Diversity & Equity in Research Award
VOGUE HOTEL MONTREAL
WEDNESDAY NOVEMBER 15TH, 2023 | 5:00 - 7:30PM
The Health Research Foundation would like to congratulate the 2023 nominees for the P x G l - I P u Aw :
For more information, please contact: Wilma Deen at wdeen@imc-mnc.ca
x l l p u
l b g l
AbbV J M N N k N Pfiz – B NT T P m u l V x
SUMATRIPTAN 85 mg + NAPROXEN SODIUM 500 mg
+

CHEF DAD
DUAL MIGR AINE TREATMENT POWER TO THE PATIENT
Significantly more SUVEXX® patients achieved headache pain relief at 2 hours vs placebo*†

65% vs 28%, respectively (p<0.001)
SUVEXX pharmacok inetics‡:
• Median Tmax for sumatriptan when given as a component of SUVEXX was 1 hour (range: 0.3 to 4 hours) vs a median Tmax of 1.5 hours for sumatriptan succinate 100 mg alone
• Median Tmax for naproxen when given as SUVEXX was 6 hours (range: 0.3 to 12 hours), approximately 5 hours later than with naproxen sodium tablets


Recommended dosing:
• One tablet dosing taken as early as possible during migraine attack
• The maximum recommended dosage in a 24-hour period is 2 tablets, taken at least 2 hours apar t
* R † H fi ‡ fi
PrSUVEXX® (sumatriptan succinate and naproxen sodium) is indicated for the acute treatment of migraine at tack s with or without aura in adults
SUVE X X is not intended for the prophylac tic therapy of migraine or for use in the management of hemiplegic, basilar, or ophthalmoplegic migraine Safety and efficacy of SUVEXX has not been established for cluster headache, which is present in an older, predominantly male population. SUVEXX should only be used if a clear diagnosis of migraine headache has been established
The safet y and efficac y of SUVEXX in pediatric patients (<18 years) and the elderly population (>65 years of age) have not been established SUVEXX is not indicated for use in pediatric patients
Contraindications:
• Ischemic coronar y ar ter y disease (C AD) (angina p ec toris, his tor y of myocardial infarction, or documented silent ischemia) or coronar y ar ter y vasospasm, including Prinzmetal’s angina;
• In the set ting of coronar y ar ter y bypass graf t surger y;
• Wolff-Parkinson-White syndrome or arrhy thmias associated with other cardiac accessor y conduc tion pathway disorders;
• Histor y of stroke or transient ischemic at tack or histor y of hemiplegic, basilar, or ophthalmoplegic migraine because these patients are at a higher risk of stroke;
• Peripheral vascular disease;
• Ischemic bowel disease;
• Uncontrolled hyper tension;
• Recent use (i e , within 24 hours) of ergotamine-containing medication, ergot-t ype medication (such as dihydroergotamine or methysergide), or another 5-hydrox y tr yptamine1 agonist;
• Concurrent administration of a monoamine oxidase (MAO)-A inhibitor or recent (within 2 week s) use of an MAO -A inhibitor;
• His tor y of as thma, ur ticaria, or allergic-t y p e reac tions af ter tak ing acet ylsalicylic acid (ASA) or other nonsteroidal anti-inflammator y (NSAID) Severe, sometimes fatal, anaphylac tic reac tions to NSAIDs have been repor ted in such patients The potential for cross-reac tivit y bet ween different NSAIDs must be kept in mind
• T h i r d t r i m e s t e r o f p r e g n a n c y b e c a u s e o f r i s k o f p r e m a t u r e closure of the duc tus ar teriosus and prolonged par turition;
• Breast feeding women;
• Moderate or severe hepatic impairment or ac tive liver disease;
• Severe uncontrolled hear t failure;
• Ac tive gastric /duodenal/peptic ulcer, ac tive GI bleeding;
• Cerebrovascular bleeding or other bleeding disorders;
• Inflammator y bowel disease;
• Severe renal impairment (creatinine clearance <30 mL / min or 0 5 mL / sec) or deteriorating renal disease (individuals with lesser degrees of renal impairment are at risk of deterioration of their renal func tion when prescribed NSAIDs and must be monitored);
• Known hyperkalemia
Most serious warnings and precautions:
Risk of cardiovascular adverse events:
Sumatr ipt an, a comp o n ent of SU V E X X , c an c aus e co ro nar y ar ter y vasospasm SUVE X X is contraindicated in patients with uncontrolled hyper tension, ischemic CAD, cardiac arrhy thmias, and those with histor y of myocardial infarc tion SUVEXX is not recommended in patients with family histor y or risk fac tors predic tive of CAD Naproxen sodium, a component of SUVEXX, is an NSAID Use of some NSAIDs is associated with an increased incidence of cardiovascular adverse events (such as myocardial infarc tion, stroke or thrombotic events) which can be fatal The risk may increase with duration of use Patients with cardiovascular disease or risk fac tors for cardiovascular disease may be at greater risk
Caution should be exercised in prescribing NSAIDs such as naproxen sodium, which is a component of SUVEXX, to any patient with ischemic hear t disease (including but NOT limited to acute myocardial infarc tion, histor y of myocardial infarc tion and/or angina), cerebrovascular disease (including but NOT limited to stroke, cerebrovascular accident, transient ischemic at tack s and /or amaurosis f uga x) and /or conges tive hear t failure (NYHA II-IV )
Use of NSAIDs, such as naproxen sodium, which is a component of SUVEXX, can promote sodium retention in a dose-dependent manner, through a renal mechanism, which can result in increased blood pressure and/or exacerbation of congestive hear t failure
Risk of gastrointestinal (GI) adverse events:
Use of NSAIDs, such as naproxen sodium, which is a component of SUVEXX, is associated with an increased incidence of gastrointestinal (GI) adverse events (such as peptic/duodenal ulceration, per foration and obstruction of the upper and lower gastrointestinal tract, and gastrointestinal bleeding) These events can occur at any time during use and without warning symptoms Elderly patients and those with histor y of peptic ulcer disease and/or GI bleeding are at greater risk for serious Gl events
Risk in pregnanc y:
Caution should b e e xercised in prescribing SUV E X X during the firs t and second trimesters of pregnanc y. Use of NSAIDs at approximately 20 week s of gestation or later may cause fetal renal dysfunc tion leading to oligohydramnios and neonatal renal impairment or failure SUVEXX is contraindicated for use during the third trimester because of risk of premature closure of the duc tus ar teriosus and uterine iner tia
Other relevant warnings and precautions:
• Use only when a clear migraine diagnosis has been established;
• Use in cluster headache;
• Psychomotor impairment;
• Use in medication overuse headache;
• Not recommended for use with other NSAIDs, except low-dose ASA for cardiovascular prophylaxis;
• Serious cardiac events and fatalities associated with 5-HT1 agonists;
• Cerebrovascular events and fatalities with 5-HT1 agonists;
• Other vasospasm-related events;
• Increased blood pressure; use with caution in patients with controlled hyper tension;
• Congestive hear t failure and edema;
• Inter ference of platelet func tion;
• Use with anticoagulants;
• Anti-platelet effec ts;
• Blood dyscrasias;
• Increased liver enz ymes; evaluate patients with signs of liver dysfunction;
• Hypersensitivit y and anaphylac toid reac tions;
• Do not use in ASA-intolerance;
• Cross-sensitivit y to other NSAIDs;
• Masking of inflammation and fever;
• E xcluding other neurologic conditions;
• Histor y of seizures;
• Serotonin syndrome; monitor patients on other serotonergic treatments;
• Blurred and/or diminished vision;
• Renal impairment; use with caution in patients with severe dehydration or pre- existing kidney disease;
• Sodium retention and hyperkalemia;
• ASA-induced asthma;
• May impair fer tilit y; not recommended in women tr ying to conceive;
• Serious skin reactions (e g , drug reaction with eosinophilia and systemic symptoms [DRESS], Stevens-Johnson syndrome, toxic epidermal necrolysis, ex foliative dermatitis and er y thema multiforme);
• Use with caution during first and second trimesters; evaluate risk-benefit;
• Not recommended during labour and deliver y;
• Use in breast feeding women
For more information:
Please consult the Product Monograph at: https://w w w miravohealthcare com/wp - content /uploads/2022 /01/Suvex x- PM - ENG - Dec2021 pdf for adverse reac tions, interac tions, dosing and conditions of clinical use The Product Monograph is also available by calling Miravo Medical Information at 1-866 -391- 4503
SU V E X X® Pro duc t Mono gr aph, Ar ale z Pharmaceuticals Canada Inc December, 2021
Aralez
I
* 6733 M ississauga Road, M ississauga, ON L5N 6J5 * d/b/a M iravo Healthcare F-SUV-012-03242022
Pharmaceuticals Canada
nc
What is BLEXTEN indicated for?


PrBLEXTEN® (bilastine) is indicated for the symptomatic relief of nasal and non-nasal symptoms of seasonal allergic rhinitis (SAR) and for the relief of the symptoms associated with chronic spontaneous urticaria (CSU) (e.g. pruritus and hives), in patients 4 years of age and older with a body weight of at least 16 kg.1
What are the pediatric formats?
BLEXTEN offers the flexibility of two pediatric dosage formats. The pediatric formats are suitable for children 4-11 years old with a body weight of at least 16 kg.1
BLEXTEN Orodispersible Tablets (ODT)
• Grape flavour,
• 10 mg tablet once daily
• To be placed in the mouth where it disperses rapidly in saliva, so it can be easily swallowed
• Convenient tablet formulation that can be taken without water
BLEXTEN Oral Solution
• Raspberry flavour in a clear, colourless liquid
• 2.5 mg/mL oral solution; 4 ml equivalent to 10 mg bilastine per dose
• A convenient dosing cup is provided with a mark of 4 mL
Ages 12+ 20 mg tablet once daily
• No dose adjustments needed for elderly patients, kidney disease or liver disease.
Administraton1
• BLEXTEN should be taken without food or grapefruit juice or other fruit juices, as these dietary compounds may decrease the effect of bilastine.
• The BLEXTEN ODT is to be placed in the mouth where it disperses rapidly in saliva, so it can be easily swallowed. Alternatively, the ODT may be dispersed in water before administration. Grapefruit juice or any other fruit juice should not be used for dispersion.
Counselling tips for parents
• Patients should be instructed to take BLEXTEN and wait for one hour before taking food or fruit juice; or if food or fruit juice has been taken to wait for two hours before taking the medication.
• The maximum daily dose for pediatrics (ages 4-11) is 10 mg (1 orodispersible tablet or 4 mL oral solution); for ages ≥12, the maximum daily dose is 20 mg (1 tablet). See the Product Monograph for complete dosing and administration information
Demonstrated efficacy data in adults and adolescents - Seasonal allergic rhinitis
Blexten 20 mg significantly reduced Total Symptom Score area under the curve (TSS AUC) from baseline to day 14 vs. placebo (98.4 vs. 118.4, p<0.001), but did not differ from the active comparator.1‡
BLEXTEN Tolerability ProfileAdults and Adolescents
BLEXTEN was generally well tolerated with treatment emergent adverse events equal to placebo.1à
Treatment-emergent adverse reactions reported in ≥1% of subjects treated with BLEXTEN 20 mg in Phase 2 and 3 trials
BLEXTEN is covered under most private insurance plans.
Clinical use:
BLEXTEN should not be administered to children below 4 years of age and under 16 kg due to limited data in this population.
Contraindication:
• History of QT prolongation and/or torsade de pointes, including congenital long QT syndromes.
Relevant warnings and precautions:
• QTc interval prolongation, which may increase the risk of torsade de pointes.
• Use with caution in patients with a history of cardiac arrhythmias; hypokalemia, hypomagnesaemia; significant bradycardia; family history of sudden cardiac death; concomitant use of other QT/ QTc- prolonging drugs.
• P-glycoprotein inhibitors may increase plasma levels of BLEXTEN in patients with moderate or severe renal impairment; co-administration should be avoided.
BLEXTEN should be avoided during pregnancy unless advised otherwise by a physician.
• A study was performed to assess the effects of BLEXTEN and bilastine 40 mg on real time driving performance compared to placebo. Bilastine did not affect driving performance differently than placebo following day one or after one week of treatment. However, patients should be informed that very rarely some people experience drowsiness, which may affect their ability to drive or use machines.
For more information:
Please consult the product monograph at www.miravohealthcare.com/wp-content/uploads/ 2021/08/ Blexten-PM-ENG-Aug2021.pdf for important information relating to adverse reactions, drug interactions, and dosing information which have not been discussed in this piece. The product monograph is also available by calling 1-866-391-4503.
References
1. Blexten Product Monograph. Aralez Pharmaceuticals Canada Inc. 2021.

What is the worldwide patient exposure for BLEXTEN?*
BLEXTEN 10 mg
• More than 2.2 million patients treated
• Available in 58 countries
• Pediatric formats available in Canada since February 2022
BLEXTEN 20 mg
• More than 213 million patients treated Available in 121 countries
• Available in Canada since December 2016
‡ Double-blind, placebo-controlled, randomized, activecontrolled parallel-group trial of 720 patients with SAR, 12-70 years old. Patients were randomized to BLEXTEN 20 mg, desloratadine 5 mg or placebo once daily for 14 days. Primary endpoint was change in AUC of the TSS from baseline to day 14. TSS was comprised of the reflective total nasal symptom score (rTNSS) and the reflective total non- nasal symptom score (rTNNSS).
* As of August 31, 2021, the estimate from internal data of patient exposure is based on units sold of the defined daily dose of 10 mg (pediatric) and 20 mg (adult) bilastine and the mean treatment duration of 3 weeks.
Rx
Advertisement This Q&A is published by Ensemble IQ, 20 Eglinton Avenue West, Suite 1800, Toronto, ON M4R 1K8, Telephone: 416-256-9908. No part of this Q&A may be reproduced, in whole or in part, without the written permission of the publisher. © 2023
about
Adverse Event BLEXTEN n=931 Placebo n=950 Gastrointestinal disorders 28 (3.01%) 28 (2.95%) Abdominal pain upper 10 (1.07%) 4 (0.42%) Nervous system disorders 81 (8.70%) 55 (5.79%) Dizziness 10 (1.07%) 4 (0.42%) Headache 40 (4.30%) 28 (2.95%) Somnolence 38 (4.08%) 25 (2.63%)
• If it is difficult to ensure that your child does not eat anything for one hour after taking BLEXTEN, try administering it before bedtime.
Aralez Pharmaceuticals Canada Inc.* 6733 Mississauga Road, Suite 800, Mississauga, Ontario L5N 6J5
BLEXTEN is a registered trademark of FAES used under license by Aralez Pharmaceuticals Canada Inc.
*A wholly owned subsidiary of Searchlight Pharma Inc.
Back Pages
COLUMN Query iGAS
There are certain moments from a medical career that are remembered vividly. I’m in medical school, sitting at a small table with a few of my classmates. We’re waiting for an obstetrician to give us a quick talk before the beginning of a six-week rotation.
The doctor comes in—we’ve seen him before in lecture hall. He’s outgoing, has a big smile and he’s short and funny. He goes around the table and asks our names. The first thing he tells us is that medicine can be hard, very hard. He tells us that the previous year, he seriously considered leaving altogether. He’d delivered two stillbirths in one week. The

circumstances were out of his control, and there was nothing he could do to prevent these tragedies.
The student next to me (who eventually ended up in obstetrics) asked why he’d want to quit, considering that he had nothing to do with these deaths, and that it wasn’t his fault. It was exactly that, he said—that although he’d gone through so many years of training and had been a doctor for more than two decades, he was helpless and could do nothing to prevent these bad outcomes. That they’d happened so close together made him wonder whether or not it would just keep happening.
BY DR. RAJ WAGHMARE

It’s summer
It’s summer, and now I’m the one who’s been practising for two decades. I’ve had moments when I’ve felt like getting out of the ER, but they’ve been fleeting and infrequent. The sudden and severe run of invasive Group A Strep (iGAS) infections from the spring seems to have subsided. The first case I’d encountered was my neighbour, a mother of three young children who spent almost a week in our ICU after developing flu-like symptoms. Another was a child I’d seen with a fever and a sore throat, one of the dozens I see every month. She returned twice more to our ER before being admitted, and despite treatment, her clinical course spiraled into the worst possible outcome. Shortly after her, I saw another child who’d been vomiting for a week. Each day, her parents thought she’d turned the corner, and then, in the evening, she’d vomit again. By the time I saw her, she was pale and dehydrated, and once admitted, continued to worsen until she was in an intensive care unit downtown, unable to even stand. I’d heard of several others— even a young man who had died inexplicably a few weeks before the bulk of iGAS cases arrived. “It must have been iGAS,” my colleague said, “makes total sense.”
Noah, 14
Noah Okoro (not his real name) is 14. He’s wheeled into an assessment room by his mother whose panicked words hit me before I can introduce myself. “You have to help him,” she says, her words and appearance telling me she’s spent most of her life in Africa. “He’s really sick.”
THE MEDICAL POST OCTOBER 2023 31 Getty images
Noah, 14, presents with strange symptoms, leading to a complex diagnostic journey
“How long has he been sick for?”
“Oh god, I don’t know,” she says, her words quick and loud. Noah lifts himself off the wheelchair and practically falls onto the exam table. He looks terrible. His dark skin is covered by hundreds of tiny beads of sweat. I look at his vital signs. His heart rate is 130, his temperature over 40°C. “How long has it been, Noah, a week?”
“No,” he says, “since the birthday party.”
“Oh right,” she says. She turns to me. “We had a big family birthday, but he just stayed in the car the whole time, he just laid in the back seat.”
“What’s he been sick with? What symptoms does he have?”
“Look at him!” she says. “He’s so weak! He can’t even stand up!”
I go back to my original question. “How many days has he been sick?”
“When was the birthday party, Noah?” his mother says.
“I don’t know,” he says.
“What day is it now?” she asks.
“It’s Sunday,” I say.
“Almost a week?” she asks her son.
I still don’t know what symptoms he has, other than weakness, and I certainly don’t know how long he’s been sick, so I turn to the triage note. “Fever for two days, treated with Advil, complains of headache, shortness of breath, dizzy, nausea, vomiting.”
“How long has he been vomiting?”
“Just today,” his mother says.
“Is there diarrhea?”
“Oh yes, so many times today.”
“Has that been just today also?”
“Yes,” she says, “it’s just been today. All of this is today.”
“So is today the first day he’s been sick?”
“No, he’s been like this almost all week!”
A sore throat?
I turn to Noah and ask him about his symptoms, head to toe, although the first thing I ask is whether or not he has a sore throat. He’s so sick that iGAS is at the top of my list. He doesn’t have a sore throat, but that doesn’t rule it out. Two of our sickest patients had come in with shoulder pain. In fact, later that night, the pediatrician will tell me that two weeks earlier, Noah had been on antibiotics for a skin infection.
He has a headache, he’s weak, he feels short of breath and light-headed (no vertigo), and as of today, he’s had vomiting and diarrhea. His stomach is uneasy, and he has cramps, but his abdomen is minimally tender and soft in all quadrants. Other than that, he denies pain anywhere else in his body. There’s no cough, no urinary symptoms, no neck stiffness or tenderness, and no other obvious source of infection. And before this, he’d never had any medical issues.
And other than the high fever, high heart rate, and borderline-low blood pressure (95 over 50), the rest of his physical exam is normal. I consider asking his mother a few more questions, but, before I can come up with a question, she speaks. “Can you please help him, he’s so weak. I can’t take him home like this.”
I order a septic workup—routine blood work, serum lactate, blood cultures, urinalysis and a chest X-ray. I aggressively re-hydrate him, and give him anti-emetics and Tylenol. “We’re going to run some tests,” I say, “and we’ll get him feeling a little better.” With iGAS at the forefront of my thoughts, I consider intravenous antibiotics, but in the end, I decide to wait. Maybe it’s just a bad stomach bug; maybe he’ll feel better after a saline bolus.
Tests are back
Three hours later, his tests are back. He’s been moved to a hallway stretcher where he can rest. He’s had a litre of fluid, his pulse has come down to 110, but his blood pressure is still low, hovering around 90. His fever is now only lowgrade, and I order ibuprofen on top of the acetaminophen he’s already had. I ask if he feels any better, and he says no, he still feels awful, and even lying down, he feels like he could throw up, he feels like he might pass out.
The blood tests don’t tell me much—or at least I think they don’t. His creatinine is a little high, no surprise, as he’s been losing fluid through both his gut and skin all day. His hemoglobin is a little low, 104, his platelets are down too, about half normal. The urine is clear and his chest X-ray is normal.
His mother is sitting at the end of
the bed. She’s calm now and has brought Noah food, but he doesn’t have an appetite. “What’s next?” she says.
I consider taking another history from the beginning, but he’s in no shape to go home and will have to see the pediatrician for admission. The pediatrician on call is one of my favourites—easy to talk to, thorough, always willing to help. I call her and tell her the story.
She’s down within minutes, and gets a similar history, although she’s able to add some detail. A few weeks earlier, he’d been put on antibiotics for a lowerbody skin infection, and this course of antibiotics had been given just before returning from a family trip to Nigeria. She orders more intravenous fluid, and tells me that he is sick enough that she’s going to initiate transfer to the children’s hospital downtown.
An hour later, I’m home, and I log in to follow up on a few patients. I skim the pediatrician’s consultation note. “Clinical picture concerning for sepsis of unclear source. Need to consider iGAS.” She’s seen the worst of our iGAS cases and to be safe, has given Noah three different intravenous antibiotics.
As I continue to skim the note, my phone goes off. It’s the intra-hospital messaging system. “Malaria,” the note says. “Our patient has malaria.”
Having gotten a better history than I had, she was able to connect recent travel to Africa to Noah’s symptoms and his low hemoglobin. With the travel history, she’d also considered a pulmonary embolus, as the source of Noah’s shortness of breath and tachycardia, but the malaria smears that she’d ordered were key to diagnosis.
“Amazing,” I text back. “Cool case.” I wish that I’d tried harder to get a better history, and realize that while medicine can be hard, very hard, and tragic to the point of hopelessness, it is at the same time challenging, interesting, surprising, and most of all, incredibly gratifying. After a week of treatment in hospital, Noah is back to baseline and discharged home.
DR. RAJ WAGHMARE is an ER physician. He blogs at theoverheadpage.com. His stories come from more than 20 years of medical practice all over Ontario.
32 OCTOBER 2023 THE MEDICAL POST BACK PAGES
1
When you purposely prescribe the Viatris original brand EFFEXOR XR, help your patient get it.

Some insurers limit full-cost coverage for higher-cost interchangeable drugs to patients who meet certain criteria, and in some instances, documentation from the prescriber is required. There is a possibility that the patient may need to contribute out-of-pocket where those conditions are not met.
Write the Viatris original brand name, EFFEXOR XR, and include “no sub,” when appropriate, on your patient’s prescription.

Encourage your patients to visit ViatrisOriginals.ca so they can:
• Download a payment assistance card to help patients who have no insurance or whose insurance co-payment amount might be a barrier to obtaining the Viatris original brand medication. This card can help patients obtain the Viatris original brand medication at little or no additional cost compared to the generic version.*

Remind your patient to ask for the Viatris original brand EFFEXOR XR at the pharmacy.
Consult the Product Monograph at https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=60600 for contraindications, warnings, precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The Product Monograph is also available by calling 1-800-463-6001.

* Subject to change. The Viatris Originals Program is available in all provinces except Quebec. Availability and level of payment assistance vary by brand medication and province.
Reference: 1.EFFEXOR ® XR [product monograph]. Canada.Upjohn Canada ULC. 17 February 2023.





ViatrisOriginals.ca
2
3 EFFEXOR® is a registered trademark of Viatris Specialty LLC, used under permission by Upjohn Canada ULC, a Viatris
VIATRIS and VIATRIS & Design are registered trademarks of Mylan Inc.,
Upjohn Canada ULC, a Viatris company. ©2023 Viatris Inc. All rights reserved. EFFE-2022-0662E - AL2023
company.
used under permission by




CLINIC Tips on providing medication abortion
A summary of guidance from SOGC and others plus advice from leading doctors
It’s been five years since Mifegymiso was approved for use in Canada for medication abortion. The procedure itself is simple: Patients take an initial 200 mg mifepristone orally, followed by 800 micrograms of misoprostol taken buccally or vaginally 24 to 48 hours later, at home.
Yet, as with any procedure, there’s more to it than just administering pharmaceuticals.
Guidance comes from the Society of Obstetricians and Gynaecologists of Canada (SOGC) 2016 guidelines and the National Abortion Federation’s clinical policy guidelines for abortion care. There’s also advice from the growing number of physicians providing medication abortions. This includes Dr. Bruce
BY KYLIE TAGGART
Allan, an obstetrician and gynecologist and medical director of the Kensington Clinic in Calgary, who gave a presentation on medication abortion at the SOGC annual clinical and scientific conference held in Ottawa in June. It also includes Dr. Sarah Warden, a family physician and lead in the mifepristone program at the Bay Centre for Birth Control and Women’s College Hospital in Toronto, who spoke to the Medical Post about the procedure. Here’s what they said.
Determining eligibility
There are clinical parameters for eligibility of a medication abortion, the most obvious being that the gestation age is not beyond 70 days and the patient has
no underlying contraindications. Other conditions are outlined in guidelines, and include making sure patients aren’t anemic.
Health Canada changed Mifegymiso’s prescribing information in 2019 to no longer require an ultrasound, although an ultrasound is still recommended when gestational age is uncertain or an ectopic pregnancy is likely.


At the Kensington Clinic, everyone seeking a medication abortion gets a transvaginal or abdominal ultrasound to determine the location of the pregnancy, gestational age and if there are twins, Dr. Allan said. But if a timely ultrasound isn’t easy to access, a patient’s last menstrual period can be used to determine the gestational age. This allows for a no-touch protocol for certain patients who don’t have risk for ectopic pregnancy or concerning health conditions. “We listen to the patients and determine clinically whether it works or not,” Dr. Warden explained. “The vast majority of those patients don’t have to enter a health facility at all.” Being able to offer no-touch abortion at the Bay Centre for Birth Control has improved access for certain patients, especially during COVID-19, she said.
Without an ultrasound, there’s no confirmation that the pregnancy is in the uterus, and no clarification if it’s an ectopic pregnancy or not. Although, for many patients, even with an ultrasound it’s a “pregnancy of unknown location” because patients often present when it’s too early to determine the pregnancy location in an ultrasound. “We still give a medication abortion to those patients, we just watch them a little more closely,” Dr. Warden said. This practice is in keeping with National Abortion Federation Guidelines, which recommend giving patients with pregnancy of unknown location medication abortion. A drop in beta human chorionic gonadotropin (bHCG) levels on a blood test following medication abortion confirms the pregnancy was intrauterine.
“The rate of ectopic pregnancy is so low, in general it’s less than 1% in our population,” Dr. Warden said. All patients are assessed for risk factors for
THE MEDICAL POST OCTOBER 2023 35 Getty Images
BACK PAGES
an ectopic pregnancy, and patients at high risk may be managed differently.
Patients may also need to get bloodwork to determine if they are Rh negative or Rh positive. The National Abortion Federation guidelines note it is reasonable to forego Rh testing when gestational age is younger than eight weeks. The SOGC recommends Rh immunoglobulin for Rh negative patients who have a medication abortion after 49 days gestation period. Rh immunoglobulin could be offered before 49 days, although there’s no evidence to support or refute giving it during this early part of pregnancy, the SOGC says.
If the request for a medication abortion is not from the person who is pregnant or if the patient isn’t able to give consent due to significant ambivalence, they should also be considered ineligible for medication abortion, Dr. Allan said.
Counselling
Counselling is key with medication abortion. Patients need to comprehend the nature of the procedure.
“I think it’s really important that patients understand how much cramping and how much bleeding they will have,” Dr. Warden said. “We still sometimes have patients coming in and saying, ‘This is what I want because I can just take a pill and go to sleep and then my pregnancy is over.’”
At the Bay Centre for Birth Control in Toronto, they give patients two different pain medications and make sure patients realize there may be “blood clots the size of a lemon,” or they might see pregnancy tissue.
“We definitely don’t sugarcoat what that is going to be like, because then patients might go to the emergency or call us more on call,” she said.
Patients also need to understand that medication abortion cannot be reversed, despite posts on social media suggesting otherwise, Dr. Allan said.
Counselling can also help to make sure patients are proceeding with a medical abortion for appropriate reasons. Dr. Allan said that some people seek an abortion because they believe they’ve damaged the pregnancy with their behaviour, such as drinking. Dr.
Allan said these patients can be referred to a maternal-fetal medicine specialist.
Dr. Warden said they see this in their clinic as well, and their nurse counsellors try to make sure patients have accurate information about risk so they can make the most informed decision they can. For example, one patient believed she couldn’t financially support a baby and wouldn’t have access to healthcare, but when the clinic staff informed her about all the resources available to her, she changed her decision.
“We don’t ask people why they are terminating their pregnancy. We just ask if they have any questions or if there are any other factors going into it. It’s a very open-ended, holistic process,” Dr. Warden explained.
The nature of the pregnancy may also affect counselling, Dr. Allan said. For example, a person’s decision may be affected if they’re carrying twins or if the pregnancy is not viable. It’s worth noting that the experience of medication abortion for multiples is no different than for other pregnancies. “The data hasn’t shown that it makes it more difficult or makes it take longer,” Dr. Warden said.
Access
Ensure that the patient’s pharmacy will be able to order in Mifegymiso. All provinces and territories cover the cost, but the pharmacy needs to know how to properly bill the healthcare plan. Dr. Warden said that with the prescription, she often includes a tip sheet for the pharmacist on how to bill for the medication. She makes sure patients know they won’t have to pay for it.
Followup
The recommended followup is seven to 14 days. “We do all of our follow-ups remotely,” Dr. Warden said. Patients get bloodwork done seven days after taking the medication and have a pre-booked phone appointment one to two weeks later. A fall of bHCG levels by 80% indicates the successful termination of a pregnancy, the SOGC guidelines state. At the Calgary clinic, patients are asked to call in 10 days, and also if a pregnancy test comes back positive after six weeks.
Before the followup, there needs to be

a way for patients to contact a healthcare professional with questions or concerns after the procedure. The Kensington Clinic has a 24-hour call line staffed by a nurse. “A lot of the calls are reassurance calls,” Dr. Allan said. Most can be handled over the phone.
At the Bay Centre for Birth Control, the phone calls are handled with an oncall rotation between providers. “That’s one of the biggest challenges doing this as an individual primary care practitioner out in the community—if you don’t have a group of you that can answer the phone calls with these patients,” Dr. Warden said. Some sole providers have patients call provincial health phone lines, and others carry a mobile phone.
Patients in remote areas need to have a support person in case they have complications and need to be taken to the emergency department, Dr. Warden said.
Further procedures
Studies suggest medication abortion is 95% to 98% effective. “That’s exactly what we see in our clinic,” Dr. Warden said. In most cases, where medication abortion isn’t effective, products of conception remain that need to be removed by aspiration. In 0.5% of cases, the patient remains pregnant, and a second dose or an aspiration abortion may be required, since Mifegymiso has teratogenic effects.
What Dr. Allan calls the scariest potential complication is a group A streptococcal clostridial infection. “You might go through your entire career without seeing that, but it might be the second one you do,” he said. He has yet to see one, but advises others to watch for signs of infection.
Providing medication abortion
Providing medication abortions is within primary care’s scope of practice, Dr. Warden said. In fact, it may be best provided by the patient’s family doctor, said Dr. Sheila Dunn, a family physician at the Women’s College Family Practice Health Centre. Sometimes patients are lost to followup, but “They wouldn’t get lost if they were with their family physician,” she told the Medical Post at the SOGC meeting.
36 OCTOBER 2023 THE MEDICAL POST BACK PAGES
SORRY COVID









THE UPDATED SPIKEVAX™ XBB.1.5 VACCINE IS HERE















SPIKEVAX™ XBB.1.5 (andusomeran mRNA vaccine) is indicated for active immunization against coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus in individuals 6 months of age and older.




LEARN MORE ABOUT THE UPDATED VACCINE AT SPIKEVAX.COM















Consult the Product Monograph at spikevax.com/en-CA/xbb15-pm.pdf for contraindications, warnings and precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The Product Monograph is also available by calling us at 1-866-MODERNA (1-866-663-3762).
© Moderna, Inc. 2023 CA-COV-2300034 09/2023
Go further. Fuel your financial
We consulted with financial professionals from MD Financial Management and Scotiabank who, together, bring well over 50 years of physician-focused financial advice and banking expertise. Using fictional examples, we will highlight their unique ability to anticipate and address the needs of physicians through advice-led solutions.
In this second segment of the series, meet “Dr. Joanne MacDonald.” She is an experienced physician who is approaching retirement and looking to purchase a second residential property out of province.

The scenario
Dr. MacDonald is a primary care physician with over 30 years of experience. She is in her early 60s and in the process of preparing for retirement. She eventually plans to downsize from her current primary residence but doesn’t want to be rushed into a sale.
In the last year, Dr. MacDonald has been more stressed than usual about making the decision to retire. The resulting change in income combined with the increased cost of real estate has amplified this stress.
Her questions:
• Being so close to retirement, how can I buy a second home and avoid getting into a million dollars’ worth of debt?
• Should I liquidate my assets to purchase the property with cash?
• How can I maintain my financial stability during retirement?
We turned to MD Financial Portfolio Manager

Kelli Costigan to help provide Dr. MacDonald a sound financial strategy to meet her goals for retirement. Kelli worked closely with Sean Desjardins, a Scotia Wealth Management Private Banker, who brought his deep understanding of physicians’ financial needs to provide strategic borrowing solutions and customized banking support to guide Dr. MacDonald on the best way to proceed.
From the lens of the specialists
Dr. MacDonald’s first inclination was to sell her assets and buy the second residential property with cash. However, Kelli and Sean both advised that doing this wasn’t the
most favourable move given the real estate market over the last six to eight months, as well as the tax implications that would result.
Taking a holistic planning approach
“Having a thorough conversation with the physician, understanding her mindset, stage of practice and any short- and long-term goals she should consider at this career level is what allows our team to guide her and her family toward the best solutions,” says Kelli.
After learning more about Dr. MacDonald’s situation, Kelli and Sean proposed strategic financing through Scotia Wealth Management’s Total Wealth Credit SolutionTM , * which would draw on her eligible nonregistered investments and use those investments as collateral for a sizable line of credit. This solution would allow Dr. MacDonald to continue growing her wealth into retirement, while giving her access to capital to make an immediate purchase, as well as giving her the flexibility to pay down this credit as quickly as she wants.
“Dr. MacDonald can continue to grow and generate annual dividend returns, which is critically important especially since she’s close to retirement. Those annual returns are what will help to pay the bills and keep the fridge full when she is no longer practising medicine,” says Sean.
Scotiabank and MD Financial Management’s tailored financial solution gave Dr. MacDonald the flexibility to be front of the line with a competitive offer and close on a property out of province without any other dependencies. Not only that, the solution gave her the reassurance to enter retirement with the confidence of knowing she had a Total Wealth Plan that could support her during this next chapter.
Physician-focused solutions
MD Financial Management and Scotiabank deeply understand the financial concerns physicians have as they approach retirement. Scotiabank provided valuable advice and access to its Total Wealth Credit SolutionTM, enabling the immediate purchase of a second property, working closely with an MD Advisor† to ensure the physician’s retirement plan was secured for the future. Together, they are well-positioned to provide customized and integrated financial advice and solutions to physicians at any stage of their career.
Kelli Costigan
CIM®, CSP, Portfolio Manager, MD Financial Management Inc. kelli.costigan@md.ca
credit approval by Scotiabank.

® Registered trademarks of The Bank of Nova Scotia, used under licence. Scotia Wealth Management® consists of a range of financial services provided by The Bank of Nova Scotia (Scotiabank®); The Bank of Nova Scotia Trust Company (Scotiatrust®); Private Investment Counsel, a service of 1832 Asset Management L.P.; 1832 Asset Management U.S. Inc.; Scotia Wealth Insurance Services Inc.; and ScotiaMcLeod®, a division of Scotia Capital Inc.

Take your finances further MD Financial Management and Scotiabank have decades of combined experience enhancing the financial wellbeing of physicians. Together, their team of dedicated healthcare specialists and advisors deliver wealth management advice, strategic borrowing solutions and customized banking support, helping physicians take their finances further. Visit our website or contact one of our advisors directly: SPONSORED CONTENT | A PRESCRIPTION FOR FINANCIAL HEALTH
well-being. In this three-part series, we explore how Canadian physicians can take their finances further at every stage of their medical career. * Borrowing to invest is not for everyone and suitability is paramount as it can add risk. Any investment strategy should be discussed with your investment and tax advisors and should take into account your long-term and personal circumstances. † MD Advisor refers to an MD Management Limited Financial Consultant or Investment Advisor (in Quebec), or an MD Private Investment Counsel Portfolio Manager. MD Management Limited was the first of the MD Group of Companies to be founded, in 1969. MD Financial Management Inc. wholly owns MD Management Limited. MD Financial Management provides financial products and services, the MD Family of Funds and investment counselling services through the MD Group of Companies. For a detailed list of these companies, visit md.ca and visit scotiawealthmanagement.com for more information on Scotia Wealth Insurance Services Inc. All banking and credit products and services available through the Scotiabank Healthcare+ Physician Banking Program are offered by The Bank of Nova Scotia (Scotiabank). Credit and lending products are subject to
Phone: 613 290-3450 Sean Desjardins Private Banker, Scotia Wealth Management sean.desjardins@scotiawealth.com Phone: 613 612-3937


Locuming: avoiding the pitfalls
In spring 2023, when the Medical Post polled its doctor readership on the question, “Would you advise a young doctor to locum for a while today?” a sizable 89% of respondents said “yes.”
And why not? With the challenges of running a practice these days (including managing/buying/leasing a clinic), it can be tempting for physicians, especially those who are early-career, to go the locum route. It promises less commitment and potentially more adventure and can broaden exposure to different places and to more varied clinical work.
We spoke to several physicians who are experienced in locuming.
Dr. Sarah Giles, a rural family and emergency doctor in Kenora, Ont., was a locum family/ER physician in northern Ontario, Northwest Territories and other parts of the world for 14 years and has written about her experiences in the Medical Post. “Locuming has always been something new grads have gravitated to. But there are downsides, like learning new systems, doing large volumes of call, learning new EMRs, not being home,” she said.
Dr. Jemy Joseph does a blend of emergency medicine and family medicine in rural Ontario and Northwest Territories. She also recently spoke at length about locuming on Dr. Stephanie Zhou’s YouTube series Breaking Bad Debt, in the episode called, “Top 5 Career Mistakes New Doctors Make.”
Dr. Paul Johnson, a family physician in Sherwood Park, Alta., took 18 months to locum before settling down into his practice. “It’s in your best interest to get a taste of different practices, practice settings, or hospital work, etc.,” he said. “Treat yourself as a free agent so that if
there is a practice setting or something that you do not like, you are not locked in long-term.”
These locum-experienced physicians highlighted some of the top pitfalls to avoid when taking on a locum assignment.
Pitfall: Not asking enough questions Each locum assignment comes with new colleagues, new workplace culture, new demands, new patients, new technologies and a new community. It’s key to be open and adaptable, but also realistic about what is workable for you. Solution: To avoid any surprises, use available resources, like the locum checklist from the CMA available online (“Locum Evaluation Checklist”) or those provided by the provincial medical associations or the CFPC. In her Medical Post article, “How to be an effective locum,” Dr. Giles said she always asked ahead of time: “How many patients will I be expected to see each hour? What is the call schedule? Am I also covering inpatients, the ER, obstetrics or surgical assists? How much is the overhead? Who keeps the extra billings, such as workers’ compensation and money from insurance forms? Where will I be staying? Will I be sharing accommodation? Will I have access to a vehicle? Will I have any days off?”
Dr. Johnson recommends visiting the clinic where you will be working,
if possible. “You can usually observe if a clinic is a well-run organization,” he said. “It’s also good if you can talk to someone who has worked there or done rotations there.”
Pitfall: Not signing a contract
“Without getting in writing the terms and conditions of the work, locums have been surprised with discrepancies between what is said and the reality of the job they walk into,” said Dr. Joseph. “This can have grave consequences if the locum placement doesn’t work out.”
Solution: Always have a signed contract and get it reviewed by an employment lawyer. Dr. Giles said, “Get the contract and the call schedule ahead of time, so there are no big surprises.” The contract should also include details about remuneration that specify whether payment is fee-for-service (or split), a stipend, hourly or blended and who is paying overhead costs.
Pitfall: Overwhelm and burnout
Locums can involve a steep learning curve, especially for early-career physicians, and there can be a tendency to take on too much. Expecting to work at the same pace as the doctors you are covering for may be setting yourself up for falling behind, risking burnout, said Dr. Joseph.
Solution: “It is better to take on lesser work and build your way up than to sign up for a lot or longer days or larger patient loads,” she said. “It is not worth the risk to make more money at the expense of making more mistakes, risking college complaints and increasing burnout.”
Pitfall: Not surrounding yourself with mentors
Whether you are just starting out or are an experienced locum physician, every time, the situation is new.
Solution: You can’t do too much prep when it comes to locums, nor have too many people in your corner. “You don’t know what you don’t know, and leaning into the wisdom of those who did it, tried it, survived it before you goes a long way to help you prepare clinically and for living in different communities,” said Dr. Joseph.
40 OCTOBER 2023 THE MEDICAL POST PRACTICE MANAGEMENT
With the right preparation, the rewards of locuming are many
BY LOUISE LEGER
BACK PAGES
PRECISION ACNE CARE. WHEREITMATTERS. PERFORMANCEIN


The 1st topical retinoid indicated to treat facial and truncal acne.1-3




• Trifarotene molecule precisely binds to the most relevant RAR in acne (RAR-ɣ)1
• Patients may see significant results in facial acne in four weeks 3
• Patients reported substantial improvements in self-confidence, social life, and emotional well-being4 with improvement of their acne
www.AKLIEF.ca

Indication and clinical use:
AKLIEF® (trifarotene 50 mcg/g) cream is indicated for the topical treatment of acne vulgaris of the face and/or trunk in patients 12 years of age and older.




Safety and effectiveness have not been established in geriatric patients (≥65 years).
Contraindications:

• Eczema or seborrheic dermatitis


• Pregnancy or women planning a pregnancy
Most serious warnings and precautions:
• For external use only, not for ophthalmic use
• Pregnancy or planning a pregnancy: Rare reports of birth defects associated with topical retinoids during pregnancy. Women of child-bearing potential should be informed of potential risks and use effective birth-control measures
Other relevant warnings and precautions:
• Discontinue use if allergic/hypersensitivity reactions occur
• Avoid contact with eyes, lips, angles of the nose, mucous membranes, abraded skin, open wounds, cuts, and eczematous and sunburned skin
• Avoid use of other dermatologic medications and potentially irritating topical products that have a strong skin-drying effect and products with high concentrations of alcohol, astringents, spices, or limes
• Non-comedogenic cosmetics should be used
• Treatment area should not be covered with dressings or bandages
• Weather extremes, such as wind or cold, may be more irritating
• Exposure to excessive sunlight, including sunlamps, should be avoided or an effective sunscreen and protective clothing are recommended
• Certain cutaneous signs and symptoms can be expected with use
• Use of electrolysis, “waxing,” and chemical depilatories for hair removal should be avoided

• Caution when taking drugs with known photosensitizers
• Avoid use on chest during breastfeedin g
For more information:
Please consult the AKLIEF® Product Monograph at https://pdf.hres.ca/dpd_pm/00054047. PDF for important information relating to adverse reactions, interactions, and dosing information, which have not been discussed in this advertisement.


The Product Monograph is also available by calling us at 1-800-467-2081.




References: 1. AKLIEF® Product Monograph. Galderma Canada Inc. November 25, 2019. 2. Aubert J, et al. Nonclinical and human pharmacology of the potent and selective topical retinoic acid receptor-γ agonist trifarotene. Br J Dermatol. 2018;179(2):442-456. 3. Tan J, et al. Randomized phase 3 evaluation of trifarotene 50 μg/g cream treatment of moderate facial and truncal acne. J Am Acad Dermatol. 2019;80(6):1691-1699. 4. Blume-Peytavi U, et al. Long-term safety and efficacy of trifarotene 50 μg/g cream, a first-in-class RAR-γ selective topical retinoid, in patients with moderate facial and truncal acne. J Eur Acad Dermatol Venereol. 2021;34(1):166-173. RAR-ɣ, retinoic acid receptor gamma AKLIEF® is a registered trademark of Galderma Canada Inc. Galderma Canada Inc. Thornhill, Ontario CA-AFC- 2200006







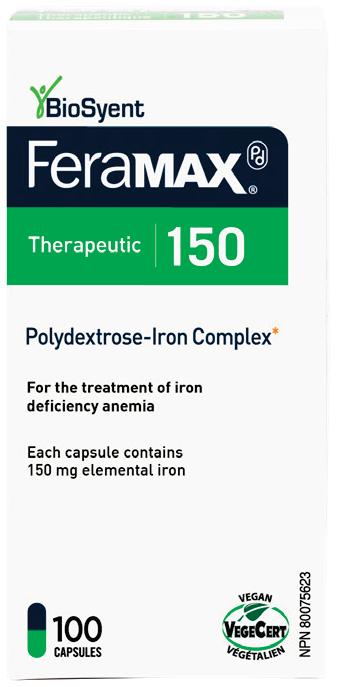
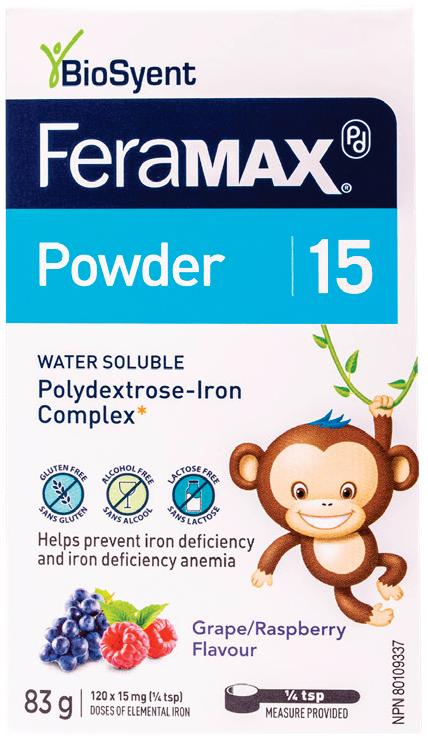
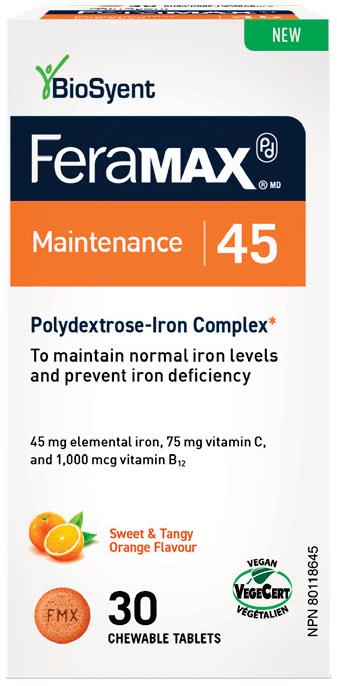





1. Klein-Schwartz W. Toxicity of polysaccharide-iron complex exposures reported to poison control centers. Ann Pharmacother. 2000 Feb;34(2):165- 9 † Pharmacy Practice + Business, The Medical Post and Profession Santé 2023 Survey on OTC Counselling and Recommendations. The SOGC Recognition logo® is a registered trademark of SOGC. BioSyent Pharma Inc. ©2023 Iron Health for Life NEW Thank you for your continued trust! FeraMAX® is the #1 recommended iron supplement, 8 years in a row!† Convenient, well tolerated1 150 mg elemental iron for once-daily treatment of iron-deficiency anemia (IDA) 150 Therapeutic Thérapeutique
FINANCE
Starting out
Done with residency? Tips for the road ahead
BY MARJO JOHNE
“Young physicians have spent years learning medicine, not business,” said Dr. John Greggain, a family doctor and president of Doctors of BC. “They don’t have MBAs, they don’t have training in human resources. So they end up either choosing work that doesn’t make them have to deal with all the things you need to do when you’re running your own business, or they cobble together whatever information and resources they can to get started.”
There’s a lot that needs cobbling together. The Medical Post asked two physicians—who’ve been there, done that and are still doing it—what early-career doctors need to know as they transition from residency to full-fledged practice.
Understand obligations
Dr. Stephanie Zhou, a Toronto-based addiction medicine physician who led the development of the financial literacy curriculum at the University of Toronto’s
faculty of medicine, said it’s generally uncommon for early-career doctors to start their own practice because high clinic overhead and startup capital requirements make that near-impossible. Consequently, many choose to start a practice with a partner or become a partner in an existing practice.
Understanding what this partnership entails—from a clinical, legal and financial perspective—is critical, said Dr. Zhou.
“Make sure you have a clear understanding of how you’ll be dividing the work, what portion of the overhead each of you is responsible for paying and how decisions that affect the business will be made,” she said.
Ideally, a young doctor entering a multi-physician practice will find someone among the group who will be willing to help their new colleague figure out the business side of running a practice, said Dr. Zhou.
“When you’re looking to join a
practice, you need to make sure the other partners in there are willing to mentor you,” she said. “Because you’re not just there to practise medicine, you’re there as part of a business. Whether or not your partners will make the time to show you the ropes around the business should factor into your decision to join a practice.”
An increasingly common situation is doctors entering into contractual agreements to practise in clinics operated by a non-physician owner or private company. Doctors of BC’s guidance in this scenario underlines the importance of paying attention to things like an indemnification clause in a contract—which stipulates that one party must provide compensation if the other party suffers harm or loss—and a confidentiality clause. With the latter, it’s critical for doctors to know their obligation to maintain electronic medical records and how long those obligations stay in place once the contract term ends.
Hiring
At some point, you’re likely going to have to hire a medical office administrator or manager.
“Finding someone with good people skills is probably the most important part,” said Dr. Greggain. “So you may end up tapping someone on the shoulder at a coffee shop and asking if they’d be interested in working for you because you see how hard they’re working and that they’re good with people.”
Dr. Zhou said many doctors go on social media platforms, such as Facebook, to post their ads for office staff while others prefer to advertise on traditional job sites like Indeed. In the clinic where she works, part of the staff recruiting strategy involves reaching out to colleges and, for summer staff, to local schools.
However you choose to recruit, make sure you’ve got employment agreements and other human resources material—such as job descriptions, codes of conduct and patient confidentiality agreements—already prepared and reviewed by an employment lawyer or an HR consultant, said Dr. Greggain.
You should also make sure you understand your responsibilities
THE MEDICAL POST OCTOBER 2023 43 Getty Images
BACK PAGES
and obligations as an employer, and that you’re prepared to manage your employees.
“Different physicians have a different appetite for HR—the applications that need to be reviewed, interviewing, hiring and firing,” said Dr. Greggain. “But if you’re a physician running your own practice, then these are things you must learn to do, and do well, because the smooth operation of your clinic depends on you hiring and managing the right people.”
Spend like a resident
“It’s definitely tempting, especially when people start making more money and they’re seeing their friends having kids and buying homes, to go out and start spending,” said Dr. Zhou. Her advice to young doctors is one she’s also heard from other doctors: Live like a resident for the first several years—some physicians suggest a decade—after you’ve finished residency. Pay down debts and start building a nest egg.
Young doctors who feel at a loss or overwhelmed by the road ahead should remember there are a number of support systems available to them. Their first outreach should be to their association, said Dr. Greggain.
Doctors of BC, for one, has a business pathways program that gives doctors access to experts and resources that can guide them through starting and running a practice and later closing it down. In Ontario, the Ontario Medical Association has a guide for starting a practice that includes advice on what doctors should do at particular milestones, starting from as early as two years before opening a practice, all the way to opening day.
The various associations also have partnerships that give their members access to third-party experts in financial services and insurance.
Dr. Zhou said early-career doctors might also want to connect online with physician peer groups such as the
College of Family Physicians of Canada’s First Five Years in Family Practice.
“We’re starting to see specialist groups too, and ones that are a mix of specialists and generalists,” she said. “I think that’s great because it gives doctors, at any stage of their careers, a network and platform to go to with their questions. At the same time, I encourage young doctors to try and find mentors who can really guide them as they’re starting out. Don’t think you have to do it alone.”
Full version
The full version of this article with more content is available online at CanadianHealthcareNetwork.ca.
Registration is free and easy for doctors, residents and medical students.
CONTEST
Caption the cartoon
Caption contest winner
We had a lot of great entries for the caption-thecartoon contest in the last issue of the magazine, but we thought Dr. Bashir Khambalia’s entry below was the funniest. Dr. Khambalia, a family physician in Stoney Creek, Ont., will receive a $75 Amazon gift card as a prize.

WHAT WOULD BE A FUNNY LINE FOR A CHARACTER TO SAY HERE?
Use your smartphone to scan the QR code above—or go online to canadianhealthcarenetwork.ca/caption-octs-cartoon-jacket-doc—and you can enter your answer on the Medical Post’s online home. If your answer is selected, you’ll receive a $75 Amazon gift card and this cartoon will re-run in the next issue of the Medical Post magazine with your caption! So you get money—and doubtless esteem and accolades from your colleagues!

44 OCTOBER 2023 THE MEDICAL POST
Johnny Hawkins, copyright 2019
‘Hugging is strictly prohibited by the College . . . I could lose my licence. Besides, I am allergic to hay!’
BACK PAGES








THE MEDICAL POST OCTOBER 2023 45 84 MP04_2020_Classified Pages.indd 68 CLASSIFIED ADVERTISING ndumont@ensembleiq.com 1 877 687-7321 ext.:1266 MP04_084_202004.indd 84 CLASSIFIED ADVERTISING sgraveson@ensembleiq.com 514 805-0634 Out of Storage Space? Let us scan or store your inactive patient records. Contact DOCUdavit Solutions 1-888-781-9083 ext. 105 medicalrecords@docudavit.com www.docudavit.com $300.00/hr Wanted: Internal Medicine (General and Subspecialist), Pediatrician, Surgeon in busy outpatient clinic in Mississauga Angela (647) 606-4399 www.torontooutpatients.com CLASSIFIEDS
How do I hire a good medical receptionist?
Hire for smarts
For several years, my strategy in hiring for the medical office administrator position has been to consider only applicants with a bachelor’s degree in any field, with or without medical office experience. These applicants are intelligent and able to see a task to completion independently. They are more adaptable to change and they are less often overwhelmed. They are more expensive to hire (but not by much) and they do sometimes leave for better opportunities. The quote I always remember is, “What if you spend all that time training someone and they leave? But, what if you can’t train them and they stay?”
The best way to keep a good employee is to pay them well and offer pension and benefits like any other good job.
–DR. TIM HILLSON


Get new grads
For our clinic, we reached out to the local college (In Ontario—Seneca, Centennial, Medix . . . etc.) to share our job offering with new graduates. In the summers, we have high school students help at the front desk as part of their summer jobs. There are also Facebook groups that physicians can use to find medical office assistants, such as Medical Office Assistants; Medical Clinic Owners Ontario; Medical Office Assistants of Canada.
— DR. STEPHANIE ZHOU

Hire slow, fire fast
Make sure there is a threemonth work trial period, and ask other staff what they think of this new receptionist as they’ll see and know better than you will. If things aren’t looking stellar, or at least promising, let them go without needing to pay severance. Once hired, if they are very good or better, do everything you can to keep them. Pay your staff well with yearly raises of at least the cost of living if they’re doing a good job. Greet them in the morning and in the hallways. Ask how their kids are doing, or where they’re travelling next. Give them cool or useful pharma samples, or occasionally bring them back something (e.g., honey, chocolate) from a trip. Ask them periodically what could be done better to improve their job and the service aspect for patients
so they feel seen and heard. Inquire as to their preferred charity, and occasionally make a donation to it in their honour.
—DR. BEN BARANKIN

Pick up the phone
I lucked into my wonderful secretary Michele Chinn 31 years ago. But if I had to hire a new one, I would advertise online. I would narrow the field and then talk to the last employer by phone. You will get the truth about why the employee left, which you won’t get in a letter. For retention, treat your receptionist well. Mine gets Wednesday afternoons off paid. She gets eight weeks’ paid vacation. I give her a cash bonus for her birthday and at Christmas take her out to a nice restaurant. I always praise her for good work, like sending patients with chest pain to the ER stat. I clean up after myself in the exam rooms. Also, pay them well or you will end up doing their job. I pay $32 per hour which is 50% tax deductible as a business expense. If you pay peanuts, you get monkeys.
—DR. JOHN CROSBY
Next Problem
How do you best deliver bad news to a patient?
Send solutions (and new questions!) to lleger@ensembleiq.com by Nov 1. Get a $25 gift card if your answer is chosen.
46 OCTOBER 2023 THE MEDICAL POST SOLVE MY PROBLEM
DR. TIM HILLSON
An eye physician and surgeon in Orillia, Ont.
DR. STEPHANIE ZHOU
An FP and addictions physician in Toronto
DR. BEN BARANKIN A dermatologist in Toronto
DR. JOHN CROSBY A family physician, in Cambridge, Ont.
BACK PAGES
“What if you spend all that time training someone and they leave? But, what if you can’t train them and they stay?”
Driving change for generations







To continue our commitment to healthier communities, Novo Nordisk partnered with Tree Canada to plant 10,000 trees in areas with the highest need across the country. This commitment will be matched by the government’s 2 Billion Trees Program. While many of us will not be here in 100 years, these trees will be. As Novo Nordisk turns 100, we renew our commitment to driving change for a healthy world – today and for generations to come.

Discover more at novonordisk.ca The Apis bull logo is a registered trademark of Novo Nordisk A/S and used under license by Novo Nordisk Canada Inc.
BUNDLE UP THIS FLU SEASON






WHEN YOU DISCUSS FLU, RECOMMEND VACCINATING AGAINST SHINGLES TOO
SHINGRIX can be given concomitantly with unadjuvanted seasonal influenza vaccine. The vaccines should be administered at different injection sites.
This FLU SEASON help prevent shingles with SHINGRIX

SHINGRIX is indicated for the prevention of herpes zoster (HZ, or shingles) in adults 50 years of age or older, and in adults 18 years of age or older who are or will be at increased risk of HZ due to immunodeficiency or immunosuppression caused by known disease or therapy.
Consult the Product Monograph at gsk.ca/SHINGRIX/PM for contraindications, warnings and precautions, adverse reactions, interactions, dosing, and administration information. To request a Product Monograph, or to report an adverse event, please call 1-800-387-7374.
SCAN TO KNOW MORE ABOUT SHINGRIX




References: 1. SHINGRIX Product Monograph. GlaxoSmithKline Inc., November 15, 2022. 2. Public Health Agency of Canada. An Advisory Committee Statement (ACS), National Advisory Committee on Immunization (NACI) – Updated Recommendations on the Use of Herpes Zoster Vaccines. Ottawa, Ontario: Public Health Agency of Canada; June 2018. Available at: https://www.canada.ca/ en/services/health/publications/healthy-living/updated-recommendations-use-herpes-zoster-vaccines.html.
3. Harpaz R, OrtegaSanchez IR, Seward JF; Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57(RR-5):1-30.
10816 06/23 Trademarks are owned by or licensed to the GSK group of companies. ©2023 GSK group of companies or its licensor.