THE ADDICTION ISSUE
Substance use disorder management in primary care 12
Dr. Jillian Horton on getting beyond burnout 20

Prepping for rising cyber threats 31

Substance use disorder management in primary care 12
Dr. Jillian Horton on getting beyond burnout 20

Prepping for rising cyber threats 31
Representing physicians and their families at MD
MD Financial Management is the only national financial services firm committed to the financial well-being of Canada’s physicians and their families. That’s why we established the MD Physician Council, a diverse group of physicians who collectively help us remain accountable so that we continue to know and serve you better than any other financial institution.
We’re thrilled to welcome these three new members to the MD Physician Council!

Dr. Jesse Kancir MD, MPhil, CCFP, FRCPC, Family Medicine Halifax, N.S.

Dr. Susanna Martin B.Sc., MDCM, FRCPC, PGDip Med ed, Pediatrics Saskatoon, Sask.

Dr. Yordan Karaivanov MD, CCFP, FCFP, Family Medicine Goose Bay, N.L.
Thank you to all our Council members for sharing their valuable time and experience with us.
Learn more about the Council’s impact and members by visiting md.ca/mdphysiciancouncil.
MD Financial Management provides financial products and services, the MD Family of Funds and investment counselling services through the MD Group of Companies and Scotia Wealth Insurance Services Inc. For a detailed list of the MD Group of Companies visit md.ca and visit scotiawealthmanagement.com for more information on Scotia Wealth Insurance Services Inc.
Meth, opioids see largest rise in costs and harms
Dr. Ted Jablonski
Addicted to medicine: Driven by perfectionism and external reinforcement, some doctors become trapped in workaholism
Dr. Raj Waghmare
Brothers: Working together in the ER
Prepping for rising cyber threats
Substance use disorder management in primary care
Mobile docs
Caring for the unhoused: Dr. Roger Walmsley and Dr. Naheed Dosani
Tips on prescribing incretin therapies for cardio-renal protection
Hindsight is 20-20
the
Enter our contest and win
Burned out on burnout
A Q&A with Dr. Jillian Horton
How can I make my clinic as environmentally friendly as possible?
Winner of two Gold awards


Cover artist
Each year we choose a new artist to create all six of the magazine covers for that year: For 2025, it is Jim Tsinganos. We asked him a few questions.
Why did you become an illustrator?
I always drew as a kid. When I was about seven years old, my dad would proudly announce to house guests that I could draw and would sit me down in front of them to draw them, which I did in either a blue or black bic biro!
So when it came time to select a course to go into after high school, I figured I’d do something that involved drawing as it was the only thing I could really do.
What is your work space like?
For about 20 years I worked out of a fabulous shared warehouse space in the city. There were designers, writers, even wine merchants, fish merchants and a boxing promoter there over the years. At one point there were about six top notch illustrators in there and some of the funniest people I’ve ever worked with. It was riotous and I couldn’t wait to go to work.
About 10 years ago I had to move out as we’d moved quite a way from the city.
So I’ve been working out of a tiny desk in my bedroom, which has been the reason I’ve had to streamline and get photoshop and the Cintiq tablet up and running.
In the coming months I hope to get my home studio construction completed and then I can spread out and maybe even break out the easel and paints again!
THE REGULATORY ISSUE: Hitting doctors’ mailboxes in midApril: We’re going deep on malpractice, CMPA and colleges of physicians and surgeons issues. As well: challenges of selfregulation and practising in a resource-restrained environment.

DERMATOLOGIST RECOMMENDED ANTI-DANDRUFF BRAND WORLDWIDE [1] AVAILABLE



LAUNCHING FEBRUARY 26TH NEW INNOVATION

Our changing language, blessedly, reflects more nuanced thinking
“Raging alcoholic.”
“Crackhead.”
“Wino.”
“Addict.”
Addiction is such a powerful force. But when I think back to terms used when I was young—or even recently— our language and thinking about addiction is evolving. And that is good. We now say a person has substance use disorder which, of course, is exactly what we know is happening. Addiction spares no demographic, geography or profession. This issue of the Medical Post takes a deep dive into addiction.
On page 12, our cover feature, “Busting myths” examines fallacies some have about family doctors’ ability to provide substance use disorder management in primary care. Of course, there are frustrations for family doctors treating addiction, but it is also interesting work—and so valuable. We know that the majority of people who go
through a period of harmful behaviour with substances ultimately go on to be productive members of society.
On page 17, we profile two doctors who provide care for unhoused people, many experiencing addiction, many living in tents in city parks.
Addictive behaviour isn’t always a bad thing per se. There are so-called “good” addictions—like chocolate or running or travel or collecting teacups.
I’m not sure I would want to live in a world without people who didn’t have some aspects of an “addictive personality.” I’ve known lots of people who maybe have had challenges with addiction at some point but gosh, those are also super-interesting humans. Our evolved thinking on addiction is good—and needs to go further. The Q&A interview with author Dr. Jillian Horton (page 20) looks at the
DESIGN/PRODUCTION/MARKETING
CREATIVE DIRECTOR Nancy Peterman npeterman@ensembleiq.com

issues underlying burnout in the physician community. She talks about the importance of the words we use to describe things that could be seen as triggers behind burnout. For example, when we spoke, she described different ways she said parents could describe their kids: “I live with three parasites who are freeloaders, who don’t pay any rent, who I have to clean up after, and when they’re 18 they’re just going to leave, and I’m going to be in debt,” versus, “I have three children. I love them. They love me. They’ve given my life more meaning than I ever could have imagined, and raising them has been the greatest privilege.” The language we use, even when talking to ourselves, matters. Enjoy this issue and be kind to your own addictive traits and to your patients with substance use disorders.
PHYSICIAN ADVISORY BOARD
DR. ALYKHAN ABDULLA family medicine
DR. ALAN KAPLAN family medicine
DR. DUNCAN ROZARIO general surgery
2300 Yonge Street, Suite 2900, Toronto, ON M4P 1E4 (877) 687-7321 Fax (888) 889-9522 www.canadianhealthcarenetwork.ca
BRAND MANAGEMENT
SVP, HEALTHCARE CANADA
Donna Kerry (416) 786-6315 dkerry@ensembleiq.com
EDITORIAL
EDITOR-IN-CHIEF
Colin Leslie cleslie@ensembleiq.com
EDITOR, CANADIAN HEALTHCARE NETWORK
Martha Porado mporado@ensembeiq.com
CONTRIBUTING EDITOR Louise Leger lleger@ensembleiq.com
ADVERTISING SALES & BUSINESS
SENIOR ACCOUNT MANAGER
Norman Cook (647) 290-3967 ncook@ensembleiq.com
SENIOR ACCOUNT MANAGER
Scott Tweed (416) 230-4315 stweed@ensembleiq.com
ACCOUNT MANAGER
Samir Iggui (647) 679-6368 siggui@ensembleiq.com
SALES & BILLING COORDINATOR
Sylvie Graveson (514) 805-0634 sgraveson@ensembleiq.com
HEALTHCARE PROJECT MANAGER Tiffany Kim tkim@ensembleiq.com
PRODUCTION MANAGER Lisette Pronovost lpronovost@ensembleiq.com
HEALTHCARE MARKETING MANAGER Aline Kirimli akirimli@ensembleiq.com
DR. BENJAMIN BARANKIN dermatology
DR. MELANIE BECHARD pediatrics
DR. ALI DAMJI family medicine
DR. MARIO ELIA family medicine
DR. FERRUKH FARUQUI family medicine
CORPORATE OFFICERS
CHIEF EXECUTIVE OFFICER
Jennifer Litterick
CHIEF FINANCIAL OFFICER Jane Volland
CHIEF PEOPLE OFFICER Ann Jadown
CHIEF OPERATING OFFICER Derek Estey
Mail Preferences: Occasionally we make our subscriber list available to reputable companies whose products or services may be of interest to you. If you do not want your name to be made available please contact us at medicalpost@canadianhealthcarenetwork.ca Contents copyright © 2025 by EnsembleIQ; may not be reprinted without permission. The Medical Post receives unsolicited features and materials (including letters to the editor, press releases, promotional items and images) from time to time. The Medical Post, its affiliates and assignees may use, reproduce, publish, re-publish, distribute, store and archive such unsolicited submissions in whole or in part in any form or medium whatsoever, without compensation of any sort. ISSN-0025-7435, PM PM42940023, The Medical Post, established 1965, is published 6 times per year by Stagnito Partners Canada Inc. Printed in Canada.
DR. CHRISTINE NICHOLAS plastic surgery
DR. BRIDGET REIDY family medicine
DR. NATHAN RIDER public health & preventive medicine resident
DR. FRANCO RIZZUTI public health
SUBSCRIPTION SERVICES
DR. DAVID SATOK family medicine
DR. MIKE SIMON family medicine
DR. CHRISTOPHER SUN family medicine
DR. HIROTAKA YAMASHIRO pediatrics
SUBSCRIPTION QUESTIONS contactus@canadianhealthcarenetwork.ca
Subscriptions (PRINT): $84.00 per year, 2 year $154.00, Single Copy $15.40, Groups $59.06 Outside Canada $128.00 per year, 2 year $238.00,
Subscriptions
To subscribe or renew, go online to: www.canadianhealthcarenetwork.ca/subscribe or email: medicalpost@canadianhealthcarenetwork.ca


Fee deal innovations (Dec.)
This article looking at compensation for indirect care and also examining details of a new physician services agreement in Prince Edward Island, got a number of comments. “It seems most governments still don’t understand everything that they (through health authorities) and the rest of the health system expect from us. Never mind patient expectations, which can be infinite. Pay for time during visits is also necessary if we are to cultivate a positive relationship not dominated by always saying ‘no,’ and get a little prevention and surveillance done,” wrote Dr. Bridget Reidy of Saanichton, B.C.
“And not a peep from Ontario,” wrote Dr. Ferrukh Faruqui of Ottawa in an online comment.
“In addition, the College of Physicians and Surgeons of P.E.I. has cut its normal $2,300 annual licence fee to $1,250 for doctors aged 65 and greater. New Brunswick reduces the licence fee from $2,300 to $775 for physicians who are at least age 70,” noted Dr. Charles Shaver of Ottawa. “I wrote to Dr. Nancy Whitmore, CEO of the CPSO on Nov. 22, 2024, and strongly urged her to offer senior Ontario physicians a licence fee reduction, but I have not yet received a reply.”
Slow decline (Dec.)
The column by Dr. Raj Waghmare, about a middleaged woman with persistent vomiting and abnormal creatinine, got praise from readers.
“Wow! Great case. Thanks for sharing. Glad the patient is doing well,” wrote Dr. Andrey Blitzer of Thornhill, Ont.


The Medical Post has a rich Canadian history. At 60 years old, it has witnessed, reported on and celebrated many innovations, challenges and changes in medicine (and in publishing!).
Years ago we were a newspaper, printed weekly. While we’ll be looking back on our 60-year legacy throughout this anniversary year, today I want to focus on who we are in 2025. In contrast to the Medical Post of 1965, today we publish not only the magazine you’re holding in your hands, but also extensive digital content via our online home—CanadianHealthcareNetwork.ca—as well as our well-read Doctor Daily e-newsletter. What hasn’t changed is who we are at our core: We’re journalists, 100% focused on helping Canada’s working doctors by curating and sharing the most relevant news, information and insights—and creating and supporting a community where physicians can share their sometimes-difficult experiences and their hard-won wisdom.
As we celebrate our brilliant past this year, I am proud of our bright present and excited for our bold future—always with our original mandate to serve Canada’s doctors front and centre.
COLIN LESLIE Editor-In-Chief The Medical Post
Got views?
Have a letter to the editor about something that appears in this issue of the magazine? Send it to editor-in-chief Colin Leslie at cleslie@ensembleIQ.com

CABTREO (clindamycin phosphate, adapalene, and benzoyl peroxide) is indicated for the topical treatment of acne vulgaris in patients 12 years of age and older.

Consult the Product Monograph for complete details on recommended dosing and administration.
Scan here to learn more about CABTREO

Consult the Product Monograph at https://bauschhealth.ca/wp-content/uploads/2024/08/CABTREO-PM-E-2024-08-01. pdf for contraindications, warnings, precautions, adverse reactions, interactions, dosing and conditions of clinical use. The Product Monograph is also available by calling 1-800-361-4261.
BY COLIN LESLIE
Addiction has wide costs in Canadian society beyond the healthcare expenditure: everything from criminal justice (policing, courts and correctional services) to lost productivity (long- and short-term disability and death) and other direct costs (such as social assistance and motor vehicle damage). The Canadian Centre on Substance Use and Addiction recently released a report looking at substance use costs and harms from 2007 to 2020 and it found that the costs for opioids and CNS stimulants (such as methamphetamine) rose the most. Costs attributable to opioid use increased by 66.4%, from $112 per person in 2007 to $186 in 2020. Costs attributable to other CNS stimulants (excluding cocaine) increased by 71.8%, from $46 per person in 2007 to $80 in 2020.
Source Canadian Centre on Substance Use and Addiction
Recent surveys have found that when asked Canadians report their drinking of alcoholic beverages has returned to pre-pandemic levels. The Canadian Community Health Survey (CCHS) recently found that over half (54%) of adults aged 18 and older reported not consuming any alcohol in the previous seven days. Those findings are similar to those found in 2019, before the COVID-19 pandemic lockdowns led to increased alcohol consumption. (24% of Canadians reported increased consumption in 2021.)
Could it be that alcohol consumption naturally reverted to its pre-pandemic levels? Or did the 2023 release of Canada’s Guidance on Alcohol and Health, which provides new stricter recommendations on alcohol consumption, influence consumption?
“I think it’s still too soon after the COVID pandemic to see a lessening yet,” said Dr. Ryan Chuang, an emergency doctor, adding that he has not seen any improvement in alcohol substance abuse cases in the ER. “Too many people are addicted to alcohol and still not concerned about its long-term harms.”
The CCHS also found a higher proportion of younger Canadians (18-22) reported not drinking any alcoholic beverages in the past seven days (67%) compared with those in all other age groups (from 51% to 57%). A lower proportion of 18- to 22-yearolds also reported drinking seven or more drinks in the past seven days (8%) compared with those in the other age groups (14% to 17%).
“I know during the pandemic we were actually seeing more severe liver disease in younger people who were alcoholics. Delivery services now can just deliver alcohol directly to addicts, which makes obtaining alcohol easier than ever,” noted Dr. Chuang. “Hopefully we will eventually see the younger generation not using alcohol as much.”
From 2019 to 2021, the number of alcoholrelated deaths among Canadians aged 64 years and younger rose 27%, according to Statistics Canada.
—LOUISE
LEGER

“Great day for Alberta’s healthcare system and our patients.”
—Dr. Shelley Duggan, Alberta Medical Association (AMA) president, about announcement of new primary care physician compensation model set to be implemented in the spring and is contingent on enough doctors expressing interest.
“Pharmacists are respected team members, but they are not physicians. Full stop.”
—Dr. Sarah Bates, acting president of the AMA’s section of family medicine, saying it is concerning that pharmacies are being positioned as the answer to primary-care shortfalls.
Source Globe & Mail • Globe & Mail • CanadianHealthcareNetwork.ca
An Ontario doctor was cleared by his college and the appeal board after making commitments to educate himself and his staff following a discrimination complaint from a transgender woman.
The Dec. 9 ruling from the Health Professionals Appeal and Review Board affirmed the decision made by the Inquiries, Complaints and Reports Committee of the College of Physicians and Surgeons of Ontario to take no action against Dr. Esmat Dessouki.
In this case, the complainant had been a participant of a clinical trial in February 2022 and according to her account, she was asked to put her birth gender (male) on the intake form. However, when she had gone to use the women’s washroom, she said she sensed a staff member looking at her in a way that made her feel like it was a problem for her to be using the female washroom.
The complainant then spoke with Dr. Dessouki,

“They have another way (now) to have more certainty for their retirement.”
—Kimberly Moran, CEO of the Ontario Medical Association, about the massive Healthcare of Ontario Pension Plan (known as HOOPP) extending membership to selfemployed doctors as of January.
who was a sub-investigator for the clinical trial, and told him that she was transgender. However, the complainant said the doctor informed her that she couldn’t use the women’s washroom because she had put “male” on the intake form. “What do you mean you’re transgender?” Dr. Dessouki said, according to the complainant’s account. “You don’t use the female washroom, we don’t have accommodation.”
According to the conclusions of the college’s committee, a nurse had expressed concern to Dr. Dessouki over the complainant using the women’s washroom because she had ticked the “male” box on the intake form. The doctor then spoke to the complainant and said she was making female staff members uncomfortable, and that the facility did not have any gender-neutral washrooms.
Dr. Dessouki maintained that he did not intend to make the complainant feel disrespected or humiliated. The doctor said he was unfamiliar with how to deal with these situations and after the encounter, he read up on the Ontario Human Rights Commission’s policy on preventing discrimination based on gender identity and gender expression.
The doctor indicated he would handle things differently in the future and both the committee and the board (on appeal) said this was satisfactory.
—TOM YUN

What is Awiqli® indicated for?
Awiqli® (insulin icodec injection) is indicated for the once-weekly treatment of adults with diabetes mellitus to improve glycemic control. 2
How is Awiqli® supplied? Awiqli® comes in a 1.5 mL and a 3.0 mL FlexTouch® pen. 2


• Awiqli® should be injected subcutaneously once weekly on any day of the week, but preferably the same day each week. 2
• Awiqli® FlexTouch® pens are co-packaged with the NovoFine® Plus needles.
• A new needle must be used for each injection. 2
How should insulin-naïve patients with T2DM be started on Awiqli®?
The recommended once-weekly starting dose of Awiqli® for insulin-naïve patients with T2DM is 70 Units. 2

What is the starting dose for patients with T2DM already on basal insulin therapy and switching to Awiqli®?
The recommended once-weekly starting dose for patients with T2DM already on basal insulin therapy is the current daily basal insulin dose x7. 2
For patients requiring a one-time additional dose
Depending on the patient’s glycemic control and hypoglycemia history, for the first dose only (week 1), a one-time additional dose of 50% of Awiqli® may be administered. When assessing the need for a onetime additional dose, the risk of hypoglycemic events (due to potential medication errors) should be weighed against temporary worsening of glycemic control (hyperglycemia). 2
The one-time additional dose MUST NOT be added for the second injection onward.
Since patients may forget to remove the one-time additional dose after the first injection, instruct them to check that they inject the correct dose, especially for the first and second injections. 2
Please refer to the Product Monograph for complete dosing information and additional dosing information for patients with type 1 diabetes.
What is the titration schedule for Awiqli®?
Titration should be based on the patient’s metabolic needs, blood glucose monitoring results, and glycemic goal. 2
Example titration schedule
In the ONWARDS clinical trials, the dose of Awiqli® was titrated weekly in ±20 Unit increments.3,4
Weekly dose adjustments were based on three pre-breakfast SMBG values.†
Titrate up
If mean pre-breakfast SMBG value is above target range
No change
If mean pre-breakfast SMBG value is within target range
Titrate down
If lowest pre-breakfast SMBG value is bellow target range
Awiqli® may be covered by private insurance. Instruct your patients to check with their provider.5







* Comparative clinical significance not established.
** For complete dosing and administration information, please refer to the Product Monograph.
† In ONWARDS 1 and 3, dose adjustments were based on three pre-breakfast SMBG readings (on the two days prior to and on the day of titration). Titration was based on the lowest reading value, if any of the three SMBG readings were below the lower limit of the target glucose range. If all three SMBG readings were above this limit, titration was based on the mean of the readings.3,4
‡ Glycemic control was defined as change in A1C from baseline.
SMBG: self-measured blood glucose.
How did Awiqli® compare with Tresiba® and insulin glargine U100 in head-to-head trials in insulin-naïve patients with T2DM?
Awiqli® demonstrated greater glycemic control‡ vs. once-daily basal insulins Tresiba® and insulin glargine U100. 2
ONWARDS 3 study¶: Awiqli® vs. Tresiba®
Patients: Insulin-naïve with T2DM on OAD(s) or GLP-1 RA
At week 26, the estimated mean A1C change from baseline was -1.57% with Awiqli® vs. -1.36% with Tresiba®; non-inferiority and superiority were confirmed. 2,3
ETD (95% CI): -0.21% (-0.34, -0.08). Non-inferiority of Awiqli® vs. Tresiba® confirmed (p<0.001). Superiority in favour of Awiqli® confirmed (p=0.0016). 2,3
(n=294) Tresiba® (n=294)

No statistically significant differences in hypoglycemic events (clinically significant or severe£§) observed with once-weekly Awiqli® vs. Tresiba® at week 26. 2
Incidence per PYE: Awiqli®, 0.31 (n=293); Tresiba®, 0.15 (n=293; p=0.1091)2
ONWARDS 1 study¥: Awiqli® vs. Insulin glargine U100
Patients: Insulin-naïve with T2DM on OAD(s) or GLP-1 RA
At week 52, the estimated mean A1C change from baseline was -1.55% with Awiqli® vs. -1.35% with insulin glargine U100; non-inferiority and superiority were confirmed. 2,4 ETD (95% CI): -0.19% (-0.36, -0.03). Non-inferiority of Awiqli® vs. insulin glargine U100 confirmed (p<0.001). Superiority in favour of Awiqli® confirmed (p=0.021).2,4
(n=492)

No statistically significant differences in hypoglycemic events (clinically significant or severe£§) observed with once-weekly Awiqli® vs. insulin glargine U100 at week 52. 2 Incidence per PYE: Awiqli®, 0.30 (n=492); insulin glargine U100, 0.16 (n=492; p=0.0611)2
Contraindications:
• During episodes of hypoglycemia
• In patients who are hypersensitive to this drug or to any ingredient in the formulation, including any non-medicinal ingredient, or component of the container
Most serious warnings and precautions: Hypoglycemia is the most common adverse effect of insulin products including Awiqli®. As with all insulin products the timing of hypoglycemia may differ.
• Glucose monitoring is required.
• Uncorrected hypoglycemic or hyperglycemic reactions can cause loss of consciousness, coma, and/or death.
• Switching a patient between another type, brand, or manufacturer of insulin and Awiqli® should be done under medical supervision and may result in the need for a change in dosage. Changes in insulin regimen from other insulins to Awiqli® may result in increased risk of hypoglycemia or hyperglycemia. Awiqli® must not be administered more frequently than once a week.
• Medication errors have been reported in which patients accidentally administer shortacting insulin instead of basal (long-acting) insulin. Specific attention should be paid when switching from a daily basal insulin to Awiqli®, which is administered weekly.
• Inspect Awiqli® visually prior to administration and use only if the solution appears clear and colourless.
• Never mix Awiqli® with any other insulin.
• Awiqli® must not be used in combination with other long-acting (basal) insulins (e.g., insulin detemir, insulin glargine, or insulin degludec).
• Never administer Awiqli® by intramuscular (IM) injection, intravenously (IV), or with an insulin infusion pump.
Administration:
• Inspect visually prior to administration and use only if the solution appears clear and colourless
• Do not mix with any other insulin, administer intravenously, administer intramuscularly, or use in insulin infusion pumps
• For patients requiring a one-time additional dose please refer to the Product Monograph Other relevant warnings and precautions:
• Refer to respective product monographs for concomitant oral antidiabetic agents for their warnings and precautions
• Stress or concomitant illness, especially infections and febrile conditions, may change insulin requirements
• Risks associated with sharing insulin delivery devices
• Fluid retention and congestive heart failure with concomitant use of a peroxisome proliferator-activated receptor (PPAR) gamma agonist
• Driving and operating machinery
• Changes in insulin regimen
• Hypokalemia
• Patients with hepatic or renal dysfunction
• Risk of immune responses (e.g., hypersensitivity reactions, lipodystrophy and cutaneous amyloidosis, injection site and local allergic reactions)
• Antibody production
• Diabetic retinopathy
• Pregnant and nursing women or women of childbearing potential
• Pediatrics
• Geriatrics
For more information:
Please consult the Product Monograph at www.AwiqliPM-e.ca for more information relating to adverse reactions, drug interactions, and dosing information which have not been discussed in this piece. The Product Monograph is also available by calling us at 1-800-465-4334.
Scan to visit Awiqli.ca�
¶ ONWARDS 3: 588 insulin-naïve adult patients with inadequately controlled T2DM on ≥1 oral antidiabetic agents or a GLP-1 RA were randomized to Awiqli® once weekly or Tresiba® U100 once daily in a 26-week, randomized, double-blinded, active-controlled, parallel-group, multicentre, multinational, treat-to-target trial. Pre-trial non-insulin antidiabetic medications were continued as background therapy in both treatment arms throughout the entire trial except for sulfonylureas and glinides, which were reduced at randomization by approximately 50% at the discretion of the investigator. The primary endpoint of the trial was the difference in change from baseline in A1C between insulin Awiqli® and Tresiba® after 26 weeks of treatment to a non-inferiority limit of 0.3%.2
# Missing values were imputed using multiple imputation based on the change from LAOT-WOB value (last available on-treatment without initiation of bolus insulin for more than 2 weeks) for subjects who had an intercurrent event, but have a measurement at the landmark visit. In ONWARDS 3, there were 3.8% of subjects in the Awiqli® arm and 3.1% in the Tresiba® arm for whom A1C data were missing at week 26.
£ Clinically significant hypoglycemia was defined as a plasma glucose <3.0 mmol/L, confirmed with a blood glucose meter.2
§ Severe hypoglycemia was defined as hypoglycemia associated with severe cognitive impairment requiring external assistance for recovery.2
¥ ONWARDS 1: 984 insulin-naïve adult patients with inadequately controlled T2DM on ≥1 oral antidiabetic agents or a GLP-1 RA were randomized to Awiqli® once weekly or insulin glargine U100 once daily in a 52-week, randomized, open-label, active-controlled, parallel-group, multicentre, multinational, treat-to-target trial. Pre-trial non-insulin antidiabetic medications were continued as background therapy in both treatment arms throughout the entire trial except for sulfonylureas and glinides, which were discontinued at randomization. The primary endpoint of the trial was the difference in change from baseline in A1C between insulin Awiqli® and insulin glargine U100 after 52 weeks of treatment to a non-inferiority limit of 0.3%.2
� Awiqli.ca is open to the general public.
A1C, glycated hemoglobin; CI, confidence interval; ETD, estimated treatment difference; GLP-1 RA, glucagon-like peptide-1 receptor agonist; OAD, oral antidiabetic medication; PYE, patient-years exposure; T2DM, type 2 diabetes mellitus.
References:
1. Data on file. 2. Awiqli® Product Monograph. Novo Nordisk Canada Inc. March 12, 2024. 3. Lingvay I, et al. JAMA . 2023;330(3):228–237. 4. Rosenstock J, et al. N Engl J Med 2023;389(4):297–308. 5. Data on file – Coverage.
All trademarks and registered trademarks are the property of their respective owners. Awiqli® is a registered trademark of Novo Nordisk A/S and used under license by Novo Nordisk Canada Inc. Novo Nordisk Canada Inc., Tel: (905) 629-4222 or 1-800-465-4334. www.novonordisk.ca
People with addiction issues around alcohol or opioids benefit from the holistic care family physicians can provide
BY KYLIE TAGGART
JUST LIKE OTHER CHRONIC DISEASES, substance use disorder (SUD) management is well-suited for primary care. Ideally, family physicians have a long-term knowledge of the patient, an established relationship and, hopefully, the patient’s trust.
It’s also a condition that includes working on both a series of physical symptoms (e.g., chronic pain) and mental health symptoms. Physicians practising in primary care can make sure that these aren’t treated in silos, but as part of a holistic management of the patient’s health. Despite addiction medicine being a mainstay of primary care, myths remain that can make physicians hesitant to incorporate substance use management in their practice.
MYTH: All SUD cases are difficult
A 2024 paper in Canadian Family Physician featured results from a survey
of 218 Saskatchewan family physicians asking why they don’t prescribe opioid agonist therapy (OAT) to treat opioid use disorder. One reason was that they were “difficult” patients.
People with SUDs are like other patients with a chronic condition who need an initial flurry of support and care, but who stabilize and need less care. Like in other chronic conditions, there’s a variety of cases. There are some patients who benefit from an intervention, a medication and other resources and do very well, noted Dr. Jennifer Wyman, medical director of the substance use service at Women’s College Hospital in Toronto, and clinical programs lead for META:PHI (Mentoring education and clinical tools for addiction: Partners in health integration). “Not everyone has multi-layered, complex medical and psychiatric conditions, even though there is a lot of trauma.” Clinicians have
to figure out their scope on balancing all these aspects and when to seek help in complicated cases.
MYTH: It takes too much time
“I think it’s a bit of a myth that it has to take a lot of time,” Dr. Wyman said. “Just like with other patients with chronic conditions that require a lot of support with a new diagnosis, there’s often a lot of effort, counselling and coordination in the early stages that then settles into much more routine check-ins and followup when the person stabilizes.” She compared it to providing mental health counselling in primary care. It does take time, but, “It’s not forever, and not always super complex and involved,” she said.
Time is, of course, linked to a physician’s concern about appropriate remuneration. Comparing physician payment for SUD management across
jurisdictions is tricky, since each one tackles it in different ways. Some have billing fee codes that take time into account. Others acknowledge complexity in other ways. In Manitoba, family physicians get additional payments for caring for people with a SUD (excluding caffeine and tobacco) as part of Manitoba’s new longitudinal primary care funding model, Family Medicine Plus. Medical associations across Canada are working to increase family physician pay in this area. For example, family physicians in Saskatchewan should see an increase in fee codes for managing SUD in April 2025 (pending Ministry of Health approval).
Abstinence is the only goal Treating substance use isn’t only about abstinence, but more of a continuum of harm reduction, explained Dr. Wyman. It’s engaging and supporting patients where they are to help them become healthier and move them towards recovery.
When physicians don’t grasp this concept, “I think sometimes physicians don’t understand the point of some of our interventions,” Dr. Wyman said. Evidence suggests that OAT allows people to build their “recovery capital,” a concept that helps the patient gain a better quality of life that will support SUD recovery in a holistic way.
For alcohol use, some treatments are indicated for reducing alcohol use, while others are used to support a goal of abstinence. Patients’ goals may differ, but evidence-based medicines exist to help patients, and family physicians should be comfortable prescribing them.
That “initial flurry of care” can often be managed outside the primary care clinic. Most provinces have clinics that provide rapid access to addiction medicine (RAAM) care. In Ontario, Manitoba, Saskatchewan and Alberta, these are called RAAM clinics, and RAAC (the C is for care) clinics in British Columbia, with similar services having different names in other regions. The goal is to stabilize the patient and then transition them back to their primary care
provider, said Dr. Erin Knight, president of the Canadian Society for Addiction Medicine (CSAM) and a family physician who practices general and addiction medicine in Winnipeg.
Transitioning back to primary care can be challenging if family physicians don’t prescribe the medications that RAAM clinics use. Regulatory requirements differ across jurisdictions for prescribing opioid agonist therapies such as methadone or slow-release oral morphine. In most provinces, prescribers need a specific authorization from their medical regulator to prescribe those medications, but often not to prescribe buprenorphine or buprenorphine/ naloxone (Suboxone). Regardless of regulatory requirements, like with all medications, physicians must have sufficient knowledge and competencies to prescribe OAT. Most medical regulators provide or recommend training courses for various types of SUD management. CSAM has some training, including a one-day course run during its annual conference in October. The B.C. Centre on Substance Use also has an online addiction training program.
“It’s really great when physicians have enough of an understanding of medications like buprenorphine and methadone that they can support their patients around co-prescribing or transitions of care or disruptions of care,” Dr. Wyman said. Disruptions in care can occur when a person receiving OAT gets another medical procedure, and the physicians in the hospital are reluctant to provide OAT. This leaves the patient dealing with the pain from the procedure as well as withdrawal from medication on which they’re physiologically dependent.
Physicians should also familiarize themselves with medications to support patients who are wanting to change their alcohol use. As a physician who works in an addiction clinic, “I’m really gratified to see family doctors initiating medications before referring their patients,” Dr. Wyman said.
For physicians interested in incorporating more SUD treatment in their practice, Dr. Knight advises starting with taking referrals from RAAM (or similar) clinics and/or taking new
patients who are stabilized. “Then you can build your comfort level in more straightforward situations and then gradually increase your knowledge base over time,” she said.
British Columbia has a telephone consult service available for primary care and other physicians working with patients with SUD. Dr. Wyman said this would be useful to have in Ontario, both for community-based and hospital-based physicians.
“It’s really a challenge, not only in community practice, but for when patients are admitted to hospital and when clinicians don’t know how to manage alcohol withdrawal well or opioid withdrawal or chronic pain on top of opioid withdrawal or methadone withdrawal,” Dr. Wyman said.
Another complex part of SUD management in primary care is differentiating if a person needs opioids to combat chronic pain, or if they seek opioids because of an addiction.
“Honestly, the overlap between chronic pain and opioid use disorder in particular is probably one of the more challenging clinical situations to manage,” Dr. Knight said. “One of the things I encourage people to think about is that it’s not specifically the dose of medication that they’re using, or the total amount. What’s important is their relationship with the substance use—so, trying to work with patients who identify the impact of that substance on their lives.”
Addiction care needs to be traumainformed care. “Think about what happened to them that got them to this situation, as opposed to what’s wrong with them,” Dr. Wyman said. These patients often have faced a lot of stigma within the healthcare system and may be reluctant to seek care, making them seem non-compliant, Dr. Wyman said. “Building trust is really important.”
Physicians need to recognize that addiction is common human behaviour, Dr. Knight said. She urged physicians to, “normalize talking about it and incorporate it into periodic health exams as much as possible so we can help people to live well, despite substance use.”
Have you considered
for your patients?

More than 156,000 patients in Canada have been prescribed REXULTI across its 3 indications since its launch in 2017.1,2*
What is REXULTI indicated for?
PrREXULTI® (brexpiprazole) is indicated for:5
• Treatment of schizophrenia (SZ) in adults.
• Use as an adjunct to antidepressants for the treatment of major depressive disorder (MDD) in adult patients with an inadequate response to prior antidepressant treatments during the current episode.
• Symptomatic management of agitation associated with Alzheimer’s dementia (AAD) in patients with aggressive behaviour, unresponsive to non-pharmacological approaches.
What is an example of a patient with MDD for which Rexulti may be considered?

• 34-year-old teacher diagnosed with MDD
• Current episode ongoing for 6 months
▶ Treatment: Currently on antidepressant treatment.
▶ Current presentation:
• Has experienced some improvement but expresses frustration that her medication is not providing enough relief.
• Complains of pervasive sad mood and anxious symptoms due to her depression.
• Has not been able to fully engage in routine family activities in the past months.
CANMAT guidelines recommendation

* Clinical significance is unknown.
** See guidelines for complete recommendations.
† Fictional case. May not be representative of the general population.
‡ Results from a phase 3, 6-week, randomized, double-blind, placebo-controlled fixed-dose trial in adult patients who fulfilled the DSM-IV-TR criteria for MDD, with or without symptoms of anxiety, had an inadequate response to 1–3 prior antidepressant treatment(s) in current episode and an inadequate response during 8 weeks of prospective antidepressant treatment. Patients remained on background antidepressant treatment and were randomized to receive adjunct placebo (n=191) or adjunct REXULTI (0.5 mg/day for week 1, 1 mg/day for week 2, 2 mg/day for week 3 onward; n=187).
What was the efficacy data for REXULTI in the PYXIS clinical trial?
As shown in the pivotal PYXIS trial, REXULTI demonstrated efficacy as an adjunctive treatment for MDD at week 6 for both primary and secondary endpoints.5,6‡
▶ Primary endpoint
When taken with an antidepressant, adding REXULTI improved depression symptoms, as measured by MADRS at week 6 (clinician-rated).5,6‡
Depressive symptoms (MADRS Total score)

Demonstrated improvement as early as week 1
3.12-point greater reduction for patients treated with antidepressant + PrREXULTI® 2 mg/day vs. antidepressant + placebo at week 6 (p=0.0001) 2
Adapted from Product Monograph and Thase et al. (inclu. Supplementary Material)
▶ Key secondary endpoint
REXULTI demonstrated improvement in functioning at week 6, as measured by the SDS Mean score.5,6‡
Functional impairment (SDS Mean score)
Statistically significant greater improvement in SDS Mean score for patients treated with antidepressant + PrREXULTI® 2 mg/day than with antidepressant + placebo at week 6 (p<0.05)
Adapted from Product Monograph and Thase et al. Supplementary Material
Demonstrated SDS domain results at week 6
The social life and family life domains showed statistically significant improvement for patients taking antidepressant + REXULTI 2 mg/day vs. antidepressant + placebo (-1.54 vs. -1.04, p=0.0323; -1.33 vs. -0.73, p=0.0129; respectively), while the work/school domain did not (-1.09 vs. -0.90, p=0.4771).
What was the efficacy data for PrREXULTI® in the AAD clinical trial Study 11?
In REXULTI’s AAD pivotal trial, REXULTI demonstrated efficacy in improving the frequency of manifestations of agitation symptoms at week 12.5,7§
▶ Primary endpoint
REXULTI demonstrated improvement in the frequency of manifestations of agitation symptoms, observed at week 12 as measured by the CMAI (clinician rated).5,7§
CMAI Total score at week 12
Adapted from Product Monograph and Lee et al. 2023
What is the tolerability profile of REXULTI
REXULTI was demonstrated to be generally well tolerated. The tables below outline the most commonly reported adverse events in trials of patients with MDD and AAD.
MDD: Treatment-emergent adverse events (TEAEs) with incidence of ≥5% in any antidepressant + REXULTI dose group (1 to 3 mg) and greater than antidepressant + placebo group in short-term Phase 3 clinical trials.5
AAD: TEAEs with incidence of ≥2% in any REXULTI dose group (0.5 to 3 mg) and greater than placebo group in 12-week, placebo-controlled, fixed-dose and flexible dose trials.5
Adapted from Product Monograph
Adverse events reported as reasons for discontinuation of treatment in four phase 3, 6-week, placebo-controlled trials.5
• REXULTI + antidepressant: 2.4% (37/1520)
• placebo + antidepressant: 0.7% (8/1132)
The maximum approved dose of REXULTI for MDD in Canada is 2 mg/day. No additional benefit was demonstrated at doses greater than 2 mg/day.
§ Results from a 12-week, randomized, double-blind, placebo-controlled fixed-dose trial in adult patients with: a probable Alzheimer’s disease diagnosis as per NINCDS-ADRDA Criteria; MMSE ≥5 and ≤22; Total score of ≥4 on the agitation/aggression item of the NPI/NPI-NH; exhibited sufficient agitation behaviours at time of entry to warrant use of pharmacotherapy, after excluding other factors; and met criteria for CMAI Factor 1 Aggressive Behaviours (To meet this criterion, one of the following must be displayed: 1) aggressive behaviours occurring several times per week, or 2) ≥2 aggressive behaviours occurring once or twice per week, or ≥3 aggressive behaviours occurring less than once per week.). Patients received REXULTI 2 mg/day or 3 mg/day (n=225), or placebo (n=116).
Discontinuation rates due to adverse events5
• REXULTI: 6.3% (41/655)
• placebo: 3.4% (13/388)
from Product Monograph
REXULTI provides simple once-daily dosing and can be taken with or without food. Dosage should be maintained at the lowest effective level and patients should be periodically reassessed to determine continued need and appropriate dosage for treatment.5
▶ Recommended dosing




Adapted from Product Monograph ▶
The required length of adjunctive treatment with REXULTI is not known. When prescribed as an adjunct to antidepressants in the treatment of MDD, REXULTI should be used for the shortest period of time that is clinically indicated.
CANMAT: Canadian Network for Mood and Anxiety Treatments; MADRS: Montgomery-Asberg Depression Rating Scale (a 10-item physician-administered questionnaire rating patients’ symptoms of apparent sadness, reported sadness, inner tension, reduced sleep, reduced appetite, concentration difficulties, lassitude, inability to feel, pessimistic thoughts and suicidal thoughts, on a scale from 0 to 6 with higher values reflecting more severe symptoms); LS: least squares; SDS: Sheehan Disability Scale (a 3-item self-rated instrument used to assess functional impairment in three domains, with higher values reflecting greater impairment); DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; CMAI: Cohen-Mansfield Agitation Inventory (a clinicianrated questionnaire consisting of 29 items, which assess the frequency of manifestations of agitated behaviours in elderly patients, based on caregiver input); CGI-S: Clinical Global Impression Severity; NINCDS-ADRDA: National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association; MMSE: Mini-Mental State Examination; NPI/NPI-NH: Neuropsychiatric Inventory/Neuropsychiatric Inventory Nursing Home.
▶ Recommended dosing
1.



from Product Monograph
▶ Recommended dose titration
▶ Recommended dosing


▶ Dose
Adapted from Product Monograph


Adapted from Product Monograph
See the Product Monograph for complete dosing, titration and administration information.

Clinical use:
PrREXULTI® is not indicated as an as needed (PRN) treatment for AAD. It may take up to six to eight weeks after REXULTI initiation to demonstrate significant clinical efficacy. The efficacy and safety of REXULTI in the treatment of AAD were demonstrated in two 12-week, randomized, double-blind, placebo-controlled, fixed dose trials in adult patients. When considering the use of REXULTI for the treatment of AAD, clinicians are advised to assess the risks and benefits of the use of REXULTI in elderly patients with AAD keeping in mind the increased risk of mortality in this patient population treated with antipsychotics and the risk predictors for stroke or existing cardiovascular comorbidities.
When considering the use of REXULTI as adjunctive treatment in MDD, clinicians must take into account the safety concerns associated with antipsychotic drugs, a class of drugs to which REXULTI belongs. Safety concerns of this class include: weight gain; hyperlipidemia; hyperglycaemia; tardive dyskinesia; and neuroleptic malignant syndrome. REXULTI should only be prescribed in patients with MDD by clinicians who are aware of the importance and are experienced in the early detection and management of the safety issues associated with this class of drugs. The efficacy and safety of REXULTI in the adjunctive treatment of MDD were demonstrated in 6-week, double-blind, placebo-controlled trials in adult patients. Therefore, the required length of adjunctive treatment with REXULTI is not known. When prescribed as an adjunct to antidepressants in the treatment of MDD, REXULTI should be used for the shortest period of time that is clinically indicated. It
is not known whether efficacy in adjunct treatment is due to REXULTI alone or from combined treatment with an antidepressant.
• The safety and efficacy of REXULTI have not been systematically evaluated in SZ or MDD patients ≥65 years of age, or in AAD patients ≥90 years of age. Use caution when treating geriatric patients.
• REXULTI is not indicated in pediatric patients (<18 years) and its use is not recommended in this population.
Most serious warnings and precautions:
Increased mortality in elderly patients with dementia: Elderly patients with dementia treated with atypical antipsychotic drugs are at an increased risk of death compared to placebo. Analyses of 13 placebo-controlled trials with various atypical antipsychotics (modal duration of 10 weeks) in these patients showed a mean 1.6-fold increase in the death rate in the drug-treated patients. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature.
Other relevant warnings and precautions:
• Body temperature regulation
• Risk of falls and somnolence
• Contains lactose
• Orthostatic hypotension
• Risk of QT prolongation
• Evaluate patients for a history of drug abuse
• Driving and operating machinery
• Reports of hyperglycemia and diabetic ketoacidosis
• Weight gain
• Dyslipidemia
• Hyperprolactinemia
• Priapism
• Risk of leukopenia/neutropenia
• Venous thromboembolism
• Serious hypersensitivity reactions
• Neuroleptic malignant syndrome
• Tardive dyskinesia
• Risk of seizures/convulsions
• Risk of suicide
• Risk of impulse-control disorders/compulsive behaviours
• Severe cutaneous adverse reactions
• Dysphagia
• Should not be used during pregnancy or breast-feeding
• Caution when used in geriatric patient populations due to potential increased risk of cerebrovascular adverse events, including fatalities.
• Monitoring and laboratory tests: blood glucose, fasting lipid profile and body weight, complete blood count (CBC), white blood cell (WBC) and differential counts, prolactin and blood pressure, should be monitored at baseline and periodically throughout treatment.
For more information:
Please consult the Product Monograph at www.rexultimonograph.ca for important information relating to adverse reactions, drug interactions, and dosing information, which have not been discussed in this piece. The Product Monograph is also available by calling us at 1-877-341-9245
References:
1. Health Canada. Notice of Compliance information, February 2024. 2. Data on File. Lundbeck Canada Inc., February 2024. 3. Lam RW, Kennedy SH, Adams C, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2023 Update on Clinical Guidelines for Management of Major Depressive Disorder in Adults. Can J Psychiatry. 2024;1–47. 4. Data on File. Lundbeck Canada Inc., July 2024. 5. REXULTI Product Monograph. Otsuka Pharmaceutical Co., Ltd. 2024. 6. Thase ME, Youakim JM, Skuban A, et al. Efficacy and safety of adjunctive brexpiprazole 2 mg in major depressive disorder: A phase 3, randomized, placebo-controlled study in patients with inadequate response to antidepressants. J Clin Psychiatry. 2015;76(9):1224–1231. (incl. supplementary) 7. Lee D, Slomkowski M, Hefting N, et al. Brexpiprazole for the Treatment of Agitation in Alzheimer Dementia: A Randomized Clinical Trial. JAMA Neurol. 2023;80(12):1307–1316.
All trademarks identified by a ® or a TM are protected trademarks (registered or unregistered) of their owners or licensors.
For more information, please visit www.otsukacanadatm-mc.ca

BY ANN GRAHAM WALKER
IF YOU’RE AN EMERGENCY MEDICINE SPECIALIST, you are used to responding quickly to incoming patients’ needs, with all the drugs, equipment and diagnostic tools you need at your fingertips. Dr. Roger Walmsley has dual certifications in emergency medicine and addictions. He works that way about half the week. For the other half, instead of reaching for scrubs, he might grab a good raincoat. He lives on Vancouver Island, on Canada’s wet coast, and—together with a team of nurses and social workers—he works on the feral streets of Nanaimo or in tent encampments.
His panel of patients? “A lot of homeless individuals, some of them quite senior, some of them younger and just living out of vehicles or living in the woods,” Dr. Walmsley said in an interview.
Anyone who is out there is in need of care, he said—many of them with mental health and/or addictions, along with sometimes-undiagnosed medical issues.
It’s called the PCO team, as in primary care outreach—an initiative that started in 2020 with Dr. Walmsley and a couple of nurses, driving their own cars with some COVID-19 funding.
Now it’s been formally evaluated and is fully supported by Island Health, the local health authority. The Nanaimo and District Hospital Foundation has purchased them a five-metre (17-foot) “Sprinter” van where they can see patients privately,
draw blood, do wound care, manage diseases doctors normally treat in the safety of their office, coordinate with hospital specialists as needed, and so on.
Former teachers, librarians, mill workers, construction workers. . . . “I’m just running through my list of the people that I’ve dealt with over time that have had good careers and for some reason—marital setbacks in some cases, mental health issues, traumatic brain injury or whatever, they’re now on the street, struggling to get by day to day,” Dr. Walmsley said.
Sometimes people get forced into using substances by the homelessness itself, Dr. Walmsley said, “to be able to stay warm and alert in the cold weather, so they don’t lose everything.”
He estimated that over a three-month period, out of Nanaimo’s population of roughly 2,000 street people, about 1,000 would be seen by the PCO nurses, and 600 or so would be seen by the physician.
Having the van has made a huge difference to the PCO team’s ability to care for patients. “Before, they wouldn’t be able to access care for virtually anything. Now, we can co-ordinate their internal medicine care, their heart function—if they’re struggling with congestive failure or need a respiratory consult because of their years of smoking and inhalation products. We can at least offer to connect people with some of the services they deserve.”
Dr. Walmsley is also involved with a substance use support outreach team that works on the streets. “Yes, we do see people who really do get on the road to recovery. . . . They’re living back with their partner, in a good, stable home setting, they’re providing—doing some work and feeling like they’re getting back to being a valuable citizen and participant in society.”
“It’s very fulfilling,” he said. “I think what we lack in the way

of four walls we make up for in terms of the connections that we make with individuals who have been very disenfranchised.
“I don’t want to glamorize this in a way that or say that it’s better than other forms of care,” Dr. Walmsley is careful to add. “That’s not it. It’s providing care for those people who have otherwise not been able to access care. And in doing so, you’re providing an open door and connecting them in a way that is not stigmatizing.“
It’s very different from working in a clinic or ER—and yet it’s not: “Most doctors know that when they are one-on-one with a patient, there’s a story,” Dr. Walmsley said. “There’s a need to listen and provide the care that’s needed at the moment. That goes whether you’re sitting in an emergency room, in a cubicle, or beside the road tending to someone who’s got, you know, a broken limb, or just (someone) struggling with an infection. It’s the patient that sets the agenda, wherever you meet them.”

DR.
“I GREW UP THE SON OF TWO REFUGEES who came to Canada from Uganda in the 1970s, fleeing war and persecution. I always knew that the social determinants of health and community well-being were an important part of what it means to be healthy in a country like Canada.”
That’s Dr. Naheed Dosani, the medical director of Kensington Hospice at Kensington Health in Toronto, and a palliative care physician at St. Michael’s Hospital. Most of the time, though, you won’t find him in those corridors. He’s driving around the city in his black Mazda, providing palliative care for those experiencing homelessness.
As a family medicine resident at the University of Toronto he found himself caring for Terry, an unhoused man in his early 30s who struggled with mental illness and neck cancer. Terry had presented in a pain crisis at a local shelter where Dr. Dosani was working. “I got to work the next day, and found that Terry had died overnight. It was very traumatic, not only for his street family, but for me,” he said
Traumatic and life-changing. “I realized there was a lot of work to do in bringing about health equity for unhoused people. That’s kind of how it all started,” Dr. Dosani said. His priority became to learn everything that was known about providing healthcare for unhoused people. He then pitched models to organizations dedicated to health justice and equity. In 2014, he founded the Palliative Education and Care for the Homeless (PEACH) program, which he still leads in Toronto. PEACH is a partnership between Inner City Health Associates, Toronto Central Health at Home and Kensington Health. It has provided palliative care for a thousand people in its 10-year history, carrying caseloads of about 120 people at any given time.
“There can be harsh weather—working outdoors. There’s the emotional toll of witnessing immense suffering,“ Dr. Dosani acknowledged.
But, through these hardships, he believes that when you offer unhoused people palliative care that’s trauma-informed and person-centred, care that recognizes the social determinants of health, “incredible things can happen.”
That can include being able to help people get basic food and medications, housing, or income support through social assistance.
PEACH does what it can to support every person with a “home” death, providing them space in a shelter, rooming house or a hospice, depending on where the person is comfortable.
“We hold grief circles with the shelter community, where we gather people who are working with people who are dying in the shelter system, or have died in many cases. We gather to talk about our grief in structured spaces that are supportive.”
Dr. Dosani said the memories of his patients live on in his heart. “They remind me of why this work really matters and why we need to continue to advocate for a more just and compassionate society.”
He is a young physician and the father of young children. “I don’t see myself ever stepping away from this kind of work. It has defined who I am as a physician and as a human,” he said. “I would argue, though, that the work is just as (medically) rigorous and academic as traditional office-based work or academic roles.”
People experiencing homelessness are 28 times more likely to have hepatitis C, he pointed out. They are five times more likely to have heart disease and four times more likely to have cancer. Average life expectancies for unhoused people in Canada range from 34 to 47 years old.
“Homelessness cuts a person’s lifespan by 50% and so it goes without saying that people experiencing homelessness are arguably Canada’s sickest sub-population. And given the strength of this data, clearly and unfortunately, palliative care must be a fundamental part of any homeless healthcare system that we develop,“ Dr. Dosani said.
Photo supplied
PrCONTRAVE® is indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with an initial body mass index (BMI) of:1
• 30 kg/m2 or greater (obese) or

• 27 kg/m2 or greater (overweight) in the presence of at least one weight-related comorbidity (e.g., controlled hypertension, type 2 diabetes mellitus, or dyslipidemia).

The discount is applied when the CONTRAVE card is presented at a pharmacy. The CONTRAVE card is included in the starter kit.
* At most retail pharmacies across Canada based on usual and customary mark up and dispensing fee. Patients may be required to pay additional pharmacy costs out of pocket.


Dr. Jillian Horton on why burnout hits doctors particularly hard, what to do about it, the core structural problems and more
BY COLIN LESLIE

“I know how I’m going to die. It’s in a tin can of a plane at an altitude so low that birds will see the whites of my eyes as I go down screaming. Whichever nondescript great lake abuts Toronto and Rochester—okay, Lake Ontario—that’s the lake I’m dying in, today, on this plane.”
So begins Dr. Jillian Horton’s 2021 book We are all perfectly fine. A memoir of love, medicine and healing. At the time, she was on her way to Chapin Mill Retreat Center in Batavia, N.Y., halfway between Rochester and Buffalo.
Dr. Horton had initially focused her energy on medical education, however over time, she experienced a profound shift in perspective. Inspired by the work of Stanford medical educator Dr. Kelly Skeff, who highlighted the need to care for faculty and practising physicians, Dr. Horton realized there was a significant
void in addressing the well-being of those tasked with nurturing the next generation of doctors.
This realization prompted the general internist to reflect on her own professional life and the pervasive nature of burnout in medicine. A turning point came when she attended that evidencebased program at the University of Rochester, designed to equip physicians with tools to navigate the complexities of their work environments.
Now the best-selling author has started “Conversations with Jillian,” a video and podcast series sponsored by the Royal College of Physicians and Surgeons of Canada.
Dr. Horton spoke to the Medical Post via video from her home in Winnipeg, delving into her journey and sharing insights into combating physician burnout.
Q: You’ve talked before how the “type A” characteristics of doctors may explain why burnout is more common among physicians. Anything else behind this?
Well, also our systems have expanded and changed at a rate that is far more rapid than anything we can process. Medicine has changed so much in the 20 years since I finished my fellowship. So you look at the people, the rapid change, (plus) the decisions that we’ve made in terms of where we’ve put our money in the healthcare system. And you can start to see how all of these things create the circumstance for the most perfect storm for highly conscientious people who are driven to do a lot of good to suddenly say, “I cannot do anything and my personality and the environment that I’m trying to
work in are actually the worst possible match.” You know, the most driven people working in the most dysfunctional systems may actually struggle more with acceptance, being able to adapt and being able to change their cognitive or emotional stance in those moments.
Q: A physician friend said she’d been through a period of burnout trying to keep her small-town ER going. So it is almost like perfectionism: a high degree of responsibility and not being able to practise medicine the way you feel it should be. There’s this weird, if you can’t do it the best way, it’s hard to “half-ass” it.
I totally agree. An analogy I sometimes use is: Imagine that you’re a neurosurgeon trained to put in a drain in a very sophisticated way in a tertiary care centre. And then, suddenly you are asked to go do that same procedure out in the middle of a baseball field with a corkscrew and a bottle of vodka. It sounds absurd, but it’s actually not all that off base. We sometimes talk about it as a moral injury. I do think moral injury is a term that has been so overused— maybe almost like burnout.
One other thing I would add is we’ve had a long history of medical exceptionalism: being unwilling to acknowledge the ways in which our physiology is identical to the physiology of most other human beings on Earth. So, failing to acknowledge that profound sleep deprivation also has profound impacts on our performance, profound impacts on our mental health, profound impacts on our mood and our reactivity. And I think that is another shift that I see that is really a long time coming: reframing those types of considerations as occupational safety issues. Medical exceptionalism has long prevented us from being able to say: “You know what? I don’t think I’m safe when I’ve been up for 24 hours.” (You get back:) “What? You’re not safe. Well, nobody else is saying they’re not safe.” So this must (mean), “You’re not strong enough. You’re not good enough, You don’t have what it takes.” And again, I think we’re moving slowly but surely into a more
reality-based conversation about what it means to be human, not just physically, but emotionally, in this profession.
Q: We have a healthcare system that is struggling, and people lose their mind when they are having a hard time and are told, “Oh, here’s an online wellness exercise.”
Totally. And it’s actually an affront, right? I’m really glad you said that. In my book, it talks heavily about my own experience with learning skills related to mindfulness. And I get to do a lot of speaking and work with different groups all over North America, and sometimes when I go, I know for sure there are people who think, “Oh, great! She’s going to tell me that mindfulness is going to fix my life.” I am never going to tell anyone that mindfulness is going to fix their life! And specifically, I’m never going to tell an organization or anyone working within an organization that that organization should (promote mindfulness) as their primary approach to physician wellness and the crisis that we’re facing right now. Mindfulness is important. It’s had a huge impact on me and helped improve my quality of life immeasurably. But it’s a personal decision to engage with that.
I get where people start feeling angry. “You’re telling me to make myself more resilient. What? So you can just pile more work onto my back so I can be immune to all the things that are happening around me?” That’s, I think, where some of that tension comes from, and I often relate it back to Maslow’s hierarchy of needs. When we say to people, “It’s Staff Wellness Day: Here’s a hot dog.” People (see) there’s such a mismatch between that and what people are experiencing. This just tells (someone), “You don’t see me. You don’t see what’s happening to me, what my needs are.” (It’s) adding insult to injury.
A lot of my work with groups is around when they’re going to roll (programs) out and trying to begin to address where people are at. Then at least, we can contextualize, even if we are going to offer people programs relating to deep breathing, mindfulness, selfregulation, etc. Again, these programs
“I am never going to tell anyone that mindfulness is going to fix their life!”
have a high degree of value. (But) we first had better spend time explaining to staff: “We’re not doing this as our only thing that we’re addressing. We’re doing it as one offer as part of a multi-phase component.” The truth is, in healthcare, most organizations are not at that stage of a multi-pronged approach.
Q: I hear you. But people may say, “My problems are because our hospital doesn’t have enough staffing.” There are many system issues that are beyond the control of a physician leader.
Well, two things come to mind. The first thing is the personal piece for all of us working in this system. One of the best quality of life things we can possibly do for ourselves is learn to manage our own reactivity. If during the course of a day at work, my reaction is a 10 out of 10 every time something goes wrong, every time I have to deal with a frustration, the person who that actually ends up costing the most at the end of the day is me, because I’m going to have nothing left to devote toward the things that I must deal with and get through my life.
We have to . . . control what we can control. This means asking ourselves: “Is there anything I can do to better manage my reactions in the clinical environment?” Because if I’m setting the emotional tone for others in a way that’s

AREXVY is a vaccine indicated for the prevention of lower respiratory tract disease (LRTD) caused by respiratory syncytial virus (RSV) in:
• adults 60 years of age and older;
• adults 50 through 59 years of age who are at increased risk for RSV disease.


DEMONSTRATED EFFICACY AGAINST RSV-LRTD FOR PATIENTS AGED 60 YEARS AND OLDER*†
82.6% efficacy demonstrated in first occurrence of RSV-associated LRTD in patients ≥60 years of age (primary endpoint; incidence rate per 1,000 person-years: 1.0 vs. 5.8 for placebo; 96.95% CI: 57.9–94.1)†‡



IN PATIENTS WITH ≥1 COMORBIDITY OF INTEREST (secondary endpoint)










(incidence rate per 1,000 person-years: 0.4 vs. 6.6 for placebo; 95% CI: 65.9–99.9)
Relative risk reduction versus placebo (96.95% CI for overall; 95% for all subgroups) for vaccine efficacy is derived based on Poisson model adjusted by age categories and regions. 94.6%







COPD,









COMORBIDITIES OF INTEREST IN ADULTS 60+ YEARS OF AGE:










Clinical use:
Pediatrics: Safety and efficacy not assessed. Geriatrics: Clinical studies include participants ≥65 years of age, and their data contributes to the overall assessment of safety and efficacy of AREXVY.
Relevant warnings and precautions:
• There is no data for the use of AREXVY in pregnant individuals. Not recommended during pregnancy or in breast-feeding/lactating individuals
• Postpone vaccination in individuals suffering from an acute severe febrile illness
• Syncope
• Caution driving and operating machinery
• Caution in individuals with thrombocytopenia or any coagulation disorder
• Protective immune response may not be elicited in all vaccinees
• Systemic immunosuppressive medications and immunodeficiency
For more information:
Please consult the Product Monograph at gsk.ca/ AREXVY/PM for important information relating to warnings, precautions, adverse reactions, drug interactions, and dosing. To request a Product Monograph or to report an adverse event, please call 1-800-387-7374.
Reference: AREXVY Product Monograph. GlaxoSmithKline Inc.
CI = confidence interval; COPD = chronic obstructive pulmonary disease.
* Data from Study AReSVi-006, an ongoing, Phase III, placebo-controlled, randomized, observer-blind clinical study conducted in adults ≥60 years of age in 17 countries from Northern and Southern Hemispheres. Adults with pre-existing, chronic, stable disease, with or without specified treatment, such as diabetes, hypertension, or cardiac disease, were allowed to participate in the study if considered by the investigator as medically stable at the time of vaccination. The primary population for efficacy analysis included patients receiving 1 dose of AREXVY (n=12,466) or placebo (n=12,494) and who did not report an RSV-confirmed acute respiratory infection (ARI) prior to Day 15 after vaccination.
† LRTD was defined based on the following criteria: the participant must have experienced ≥2 lower respiratory symptoms/signs including ≥1 lower respiratory sign for ≥24 hours, or experienced ≥3 lower respiratory symptoms for ≥24 hours. Lower respiratory symptoms included: new or increased sputum, new or increased cough, new or increased dyspnea (shortness of breath). Lower respiratory signs included: new or increased wheezing, crackles/ rhonchi, respiratory rate ≥20 respirations/min, low or decreased oxygen saturation (O2 saturation <95% or ≤90% if baseline is <95%) or need for oxygen supplementation.
‡ The primary endpoint for vaccine efficacy was defined as the first occurrence of RT-PCR-confirmed RSV-A and/or B-associated LRTD with an onset from 15 days after vaccination.
unhelpful, it’s not serving them or me. Emotional contagion is real, and managing that is just part one—the microcosm.
From a systems and strategy perspective, what can we do? We can make things easier by teaching and providing clear approaches. Organizations like the CMA are already working on national initiatives to build this kind of literacy. For example, when healthcare workers voice concerns like “the EMR is (challenging); the leadership in my facility is impersonal and nobody acknowledges me. I don’t even feel respected or cared for,”—well, leaders need to understand how to incorporate these issues into a broader, systems-based approach. They need to connect the dots and see how these problems impact physician health, healthcare worker well-being, and professional fulfillment. A good leader or decision-maker should be able to say, “Here’s where this issue fits, and here’s how it connects to the larger picture.”
You know, in medicine, we have schemas for almost everything we do. Whether it’s heart failure or kidney failure, our training provides us with diagrams, flowcharts or models that help us organize and address each patient’s problem systematically. And I would just point out that (we) struggle to have anything like that when it comes to an approach to physician well-being.
(So) when a hospital wants to offer resilience training—that is part of personal resilience. But it’s important to recognize that personal resilience may only account for 10% of the (broader) problem.
The key is being able to place these concerns into their respective categories, understanding that addressing physician well-being requires a systems-based approach. It’s not just about resilience training or Staff Appreciation Day. It’s about creating a sophisticated, evidencebased strategy grounded in literature— something foundational and actionable, not a series of ad hoc measures.
I would note, as others have, that most hospitals, every cohort, every group, now have wellness leads. However, they don’t have a common vocabulary. They don’t have a framework for where to start or how to repeat. So those are some of the problems I see.
Q: Reframing can help doctors address burnout?
There’s a concept often discussed in work: Is it a job, a career or a calling? When it comes to burnout, people sometimes think, “I don’t feel like it’s a calling anymore, so I’m burnt out.” But I say to people that, throughout the day, this can shift. At 9:30 a.m., what I’m doing might feel like just a job. By 11 a.m., it’s part of my career. By 2 or 4 p.m., it might connect to my sense of calling. We can be (in medicine) pretty rigid in our thinking—and that is OK if that is just right here and now. That’s why mindfulness is such a beautiful complement to working through the reality of doing a really difficult job. “Right now, I feel this way. I love this part. I hate this part.” But I’m going to work with it a bit more non-judgmentally.
How can I be more able to tolerate what is sitting on me like a rock? Can I actually be curious about it? Can I start to say, you know what? Maybe I’m labelling and this is not helping. Maybe there’s another way to look at it.
This connects to the stories we tell about our work. Behavioural psychologist Adam Grant popularized the concept of task perception: Is a bricklayer merely laying bricks from 9 to 5, or are they building a bridge that will connect communities for generations? Which story is more motivating? That’s great research that shows just talking about something—“I love my dog. I love writing”—illuminates the reward centre of the brain.
Ultimately, a multi-pronged approach is essential. Focusing solely on personal resilience or reframing stories isn’t enough—it can even harm if it’s the only strategy. But as part of a broader, evidence-based, systemic approach, it becomes a powerful tool. Mindfulness, I believe, has the power to influence our perceptions and our experience of working in this profession.
Scan this QR code to read more of Dr. Horton’s exclusive interview wherein she discusses the value of narrative in helping doctors—and her advice on writing.


What is Vyepti® indicated for?
Vyepti® (eptinezumab for injection) is indicated for the prevention of migraine in adults who have at least 4 migraine days per month. 2
How is Vyepti® administered?
Recommended dose: 100 mg administered as one 30-minute IV infusion every 12 weeks 2
Vyepti® is given as an intravenous infusion (after dilution) by a healthcare professional.
Infused over approximately 30 minutes.
The treatment benefit should be assessed 3-6 months after initiation of the treatment. Any further decision to continue the treatment should be made on an individual patient basis and determined prior to each dose. 2 See the Vyepti® Product Monograph for complete dosing and administration information.
What are the select pharmacokinetics of Vyepti®?† Absorption
Administered by intravenous infusion which bypasses extravascular absorption and is 100% BIOAVAILABLE 2
Median time to peak concentration was attained at the end of infusion 30 MINUTES2
See the Vyepti® Product Monograph for complete pharmacokinetic information.
What were the efficacy data for Vyepti® in chronic migraine patients in the PROMISE-2 trial?
In PROMISE-2, Vyepti® 100 mg demonstrated significant reductions in mean monthly migraine days (MMDs) during weeks 1-12 vs. placebo in chronic migraine. 2,3‡§
• The mean migraine frequency at baseline was 16.1 migraine days/month and was similar across treatment groups. 2
• 41% of patients were taking concomitant preventive medication for migraine.2
What were the efficacy data for Vyepti® in episodic migraine patients in the PROMISE-1 trial?
In PROMISE-1, Vyepti® 100 mg demonstrated significant reductions in mean MMDs during weeks 1-12 vs. placebo in episodic migraine. 2,4‡¶
• The mean migraine frequency at baseline was 8.6 migraine days/month and was similar across treatment groups. 2
• 96.4% (n=856) of patients were taking at least 1 acute concomitant headache medication and 4.6% (n=41) of patients were taking at least 1 prophylactic headache medication. Regular use (greater than 7 days per month) of other treatments for the prevention of migraine was not allowed.2
What were the efficacy data for Vyepti® in episodic and chronic migraine patients with 2-4 prior migraine preventive treatment failures in the DELIVER trial?
In DELIVER, Vyepti® 100 mg demonstrated greater reductions in MMDs vs. placebo from weeks 1 to 12 and from weeks 13 to 24.
MMDs=monthly migraine days
*Comparative clinical significance is unknown.
† Clinical significance is unknown.
‡ Baseline was the average over the 28-day screening period prior to receiving treatment. The change from baseline in MMDs (weeks 1-12) was analyzed using ANCOVA with baseline MMDs as covariate and treatment and prophylactic medication use (Yes/No) as fixed effects.
¥ Baseline was the average over the 28-day screening period prior to receiving treatment. The change from baseline in MMDs (Week 1-12) was analyzed using ANCOVA with baseline MMDs as covariate and treatment as a fixed effect.
§ PROMISE-2: A parallel-group, double-blind, placebo-controlled global trial to evaluate the efficacy and safety of Vyepti® for the preventive treatment of chronic migraine in adults (defined as ≥15 to ≤26 headache days, of which ≥8 were assessed as migraine days). A total of 1,072 patients were randomized and received placebo (n=366), Vyepti® 100 mg (n=356), or Vyepti® 300 mg (n=350) every 12 weeks for 24 weeks (2 infusions). During the trial, patients were allowed to use acute or preventive medication for migraine or headache on an established stable regimen (except for onabotulinumtoxinA). Patients with a dual diagnosis of chronic migraine and medication overuse headache (associated with the overuse of triptans, ergotamine, or combination analgesics >10 days/month, or acetaminophen, acetylsalicylic acid, or non-steroidal anti-inflammatory drugs ≥15 days/month) were included in the study population. Patients using opioids or butalbital-containing products >4 days/month were excluded.
¶ PROMISE-1: A parallel-group, double-blind, placebo-controlled global trial to evaluate the efficacy and safety of Vyepti® for the preventive treatment of episodic migraine in adults (defined as ≥4 and ≤14 headache days of which at least 4 had to be migraine days during the 28-day screening period) in adults. A total of 888 patients were randomized and received placebo (n=222), Vyepti® 30 mg (n=223), Vyepti® 100 mg (n=221), or Vyepti® 300 mg (n=222) every 12 weeks for 48 weeks (4 infusions). Patients were allowed to use concurrent acute migraine or headache medications, including migraine-specific medications (e.g., triptans, ergotamine derivatives), during the trial. Regular use (greater than 7 days per month) of other treatments for the prevention of migraine was not allowed.
# DELIVER: A parallel-group, double-blind, placebo-controlled efficacy and safety study of Vyepti® for the preventive treatment in episodic migraine (defined as migraine occurring on ≥4 days and headache occurring on ≤14 days) and chronic migraine (defined as migraine occurring on ≥8 days and headache occurring on ≥15 days) in patients with two-to-four prior migraine preventive treatment failures. A total of 892 patients were randomized and efficacy analysis was based on 890 patients (eptinezumab 300 mg n=293, eptinezumab 100 mg n=299, placebo n=298). During the trial, patients were allowed to use acute antimigraine medications. The mean migraine frequency at baseline was 15 migraine days/month and it was similar across treatment groups. The primary efficacy endpoint was the change from baseline in mean MMDs over weeks 1-12. The key secondary endpoints included the proportion of patients with ≥50% and ≥75% reductions from baseline in MMDs over Weeks 1-12 and change from baseline in the number of MMDs over Weeks 13-24.
• The mean migraine frequency at baseline was 15 migraine days/month and was similar across treatment groups. 2
• 94% of patients were taking concomitant preventive medication for migraine.2
In DELIVER, for patients with prior preventive treatment failure, Vyepti® 100 mg demonstrated ≥75% and ≥50% MMDs reduction from baseline in patients taking Vyepti® vs. placebo (key secondary endpoints). 2,5#
The safety profile of Vyepti® was evaluated in clinical trials in more than 2,000 patients with episodic and chronic migraine who received at least one dose of Vyepti®, representing more than 1,600 patient-years of exposure; of these, approximately 1,500 patients were exposed to 100 mg or 300 mg. 2
The most common adverse reactions in the placebo-controlled clinical studies (PROMISE 1 and PROMISE 2) for the preventive treatment of migraine were nasopharyngitis and hypersensitivity reactions. 2
Adverse reactions in Vyepti®-treated patients (and more frequently than in patients receiving placebo)2
The following treatment-emergent adverse events were observed in ≥1% of Vyepti® 100 mg patients and equal to or greater than placebo. 2
Treatment-emergent
Exclusion criteria: Both studies excluded patients with a known history of cardiovascular disease (hypertension, ischemic heart disease), neurological disease, cerebrovascular disease, morbid obesity and diabetes, alcohol/ drug abuse, and severe mental disorders. 2
Is there a patient support program for Vyepti®? Yes—staffed by qualified healthcare professionals and reimbursement specialists, the Vyepti TODAY® Patient Support Program is designed to support the patient journey from prescription to infusion.
Ask us to find out if Vyepti® is covered or has public funding in your province (criteria in addition to the indicated condition apply).
Contact us for more information and to get your patients started: Call 1-833-8-VYEPTI (893784) Email support@vyeptitoday.ca Fax 1-833-9-VYEPTI (893784)
Clinical use:
• Vyepti® should be prescribed by healthcare professionals experienced in the diagnosis and treatment of migraine.
• No data are available in the pediatric population (<18 years of age). Therefore, Vyepti® is not authorized for pediatric use.
• The safety and efficacy of Vyepti® has not been established in geriatric patients (≥65 years of age). The clinical study program of Vyepti® did not include sufficient numbers of these patients to determine whether they respond differently from younger patients.
Most serious warnings and precautions:
Hypersensitivity reactions: Serious hypersensitivity reactions, including angioedema, urticaria, rash and anaphylactic reactions have been reported with the CGRP-class products including Vyepti®. These reactions may develop within minutes of the infusion. If a serious hypersensitivity reaction occurs, administration of Vyepti® should be discontinued immediately and appropriate therapy initiated.
Other relevant warnings and precautions:
• Patients with cardiovascular diseases
• Patients with diabetes or morbid obesity
• Patients with hereditary fructose intolerance (HFI)
• Hepatic insufficiency
• Patients with HIV, Hepatitis B and C
• Patients with autoimmune disorder
• Patients with neurological disorder
• Renal Insufficiency
• Fertility
• Pregnancy
• Breastfeeding
For more information:
Please consult the product monograph at https://www.lundbeck.com/content/ dam/lundbeck-com/americas/canada/products/files/vyepti_product_ monograph_english.pdf for important information relating to adverse reactions, drug interactions, and dosing information which have not been discussed in this piece. The product monograph is also available by calling us at 1-800-586-2325.
References:
1. Data on file. Lundbeck Canada Inc. 2. Vyepti® Product Monograph. Lundbeck Canada Inc. 3. Lipton RB, et al. Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology. 2020 Mar 31;94(13):e1365-e1377. 4. Ashina M, et al. Eptinezumab in episodic migraine: A randomized, double-blind, placebo-controlled study (PROMISE-1). Cephalalgia. 2020 Mar;40(3):241-254. 5. Ashina M, et al. Safety and efficacy of eptinezumab for migraine prevention in patients with two-to-four previous preventive treatment failures (DELIVER): a multi-arm, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2022;21:597-607.
Vyepti® is a registered trademark of H. Lundbeck A/S, used under license by Lundbeck Canada Inc.
Vyepti TODAY® is a registered trademark of H. Lundbeck A/S, used under license by Lundbeck Canada Inc.
Vyepti TODAY™ is a trademark of H. Lundbeck A/S, used under license by Lundbeck Canada Inc.

Driven by perfectionism and external reinforcement, some doctors become trapped in workaholism
Dr. B. was well-respected for his long and dedicated medical career. He was also well-loved in his hospital circle as the doctor who always seemed to be there and on call when you needed him. He was unfortunately divorced and estranged from his two children and seemed quite lost at times.
Dr. M. was always known for going the “extra mile” for her devoted patients. She was available to her clinic panel by cell phone on weekends and rarely went on vacations. She always ran behind time and seemed to be forever catching up on charting and overly meticulous paperwork.
Most doctors believe their career is a vocation or a higher calling. There is a distinct difference, however, between a deeply felt passion and an addiction. Addiction is conceptualized as a physical dependence on substances or behaviours, but a growing body of research suggests that work, particularly in high-stakes, emotionally charged environments, can become an addictive pursuit. Unlike a deep and meaningful vocation, addiction doesn’t lead to growth or fulfillment but rather to a cycle of dependence and suffering. While an addiction to the practice of medicine is not a formal diagnosis it is likely still
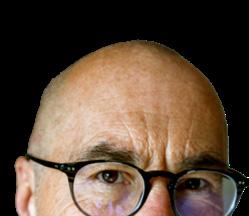

BY DR. TED JABLONSKI
common and a negative phenomenon that should be addressed.
First off, this is not what is paradoxically described as a “healthy addiction.” The characteristics of addiction to the practice of medicine align with those of behavioural addiction. This is an obsession with unhealthy compulsive behaviours that become detrimental to a doctor’s wellbeing, leading to negative consequences such as physical harm, psychological distress and impaired relationships. As per any addiction, there is a persistent need to continue the deleterious behaviour despite the cost. This is an addiction that can destroy lives.
Work addiction is defined as excessive work engagement that leads to negative physical, emotional and social outcomes. But is addiction to practising medicine more complex than general workaholism, which can occur in any profession? If so, what makes this addiction a nuanced affliction when applied to doctors?
The perfect set-up
Being a medical doctor is an identity that comes with purpose and a sense of meaning. This is a truly beautiful thing. The altruistic nature of this profession leads to respect and social reinforcement. Physicians generally have perfectionistic personalities and well-developed work ethics. Dedication and hard work are traits positively reinforced by patients, as well as peers and colleagues, and are easily habituated, forming a comfortable, if not sometimes
strained, routine. Long hours and overwork is rewarded and glamorized. There is an unending pressure to meet expectations and always be error-free.
The practice of medicine can be all-consuming. If there are no other aspects of life that are as fulfilling, why seek alternatives? This sets the stage for a potential problem. Financial security can further reinforce and perpetuate this cycle of overwork.
Neuroscience tells us that the brain’s reward pathways can be involved in the practice of medicine just like other forms of addictive behaviours. The satisfaction of clinical success can be immense.
Complex problem-solving, alleviating suffering or helping someone be healthy, can trigger our reward system, flooding our brains with dopamine. This is especially true if the patient, family or the medical system, expresses gratitude for our work. And it feels good—really good. The more positive reinforcement we get, the more we want it. In addition, direct compassionate interactions with patients can stimulate the release of oxytocin, the “breastfeeding” hormone associated with bonding and caregiving—further neurochemical reward that reinforces even more engagement.
For some, the practice of medicine can serve as an escape from one’s own feeling of inadequacy, an escape from personal struggles or emotional pain. The profession provides a highly structured environment where unending external demands can effectively distract from internal struggles. If a doctor is burning out, the intense stimulation and high demands of the job may be the only thing they still “feel” to maintain any sense of control or self-worth. The most challengingly, insatiable and problematic aspects of a medical career are managed by digging even deeper and giving even more. The cure becomes the irresistible poison.
The extent of this addiction can only be speculated on. Those afflicted may
not see themselves as addicted and their colleagues may only perceive an exceptionally dedicated and hardworking colleague with a less-than-stellar personal life. The official diagnosis is therefore not made or grossly underestimated.
What do we know? A widely cited study conducted by the Mayo Clinic suggests that approximately 10% to 15% of physicians will experience some form of substance use disorder during their careers. However, some studies suggest that the rates of addiction may be slightly higher than the general population due to occupational stress, high workloads and emotional burnout. According to a 2015 study, approximately 13% of male physicians and 21% of female physicians met diagnostic criteria for alcohol abuse or dependence.
In a large-scale study, Dr. Liselotte Dyrbye and others reported in 2017 in Mayo Clinic Proceedings that nearly 50% of physicians experienced symptoms of burnout, and about 10% exhibited clinical depression. These factors, while not directly linked to addiction, highlight the psychological toll of medical practice, which can create conditions conducive to addictive behaviours.
There are consequences
The consequences of addiction to the practice of medicine are farreaching, not only affecting the medical professional but also their patients, colleagues and the healthcare system as a whole. Doctors addicted to their practice may neglect their own physical and mental health, which can lead to long-term consequences, including fatigue, depression, anxiety and substance abuse. These conditions may impair their ability to provide optimal care to their patients, leading to a vicious cycle of work, exhaustion and further addictions. Studies show that burnout and exhaustion are linked to a decline in medical judgment and increased rates of medical errors.
Workaholism often leads to a lack of personal time, which can foster feelings of isolation, guilt and emotional disconnection. The overwork and emotional strain not only impacts individual doctors but also places a
burden on the healthcare system, leading to staffing shortages and a decrease in the overall quality of care.
Rehabilitating from addiction to the practice of medicine requires a multifaceted approach. The process can be complex as it involves emotional, psychological, professional and potentially physical healing.
The primary step must be self-awareness—recognizing and acknowledging the problem and then seeking help. This means a physician putting their own health ahead of their patients, which might be a first. There may be a period of “detoxification” and treatment of other mental health diagnoses (dual diagnosis). This might mean pharmacologic measures, professional counselling and physician support groups/mentorship through provincial medical associations. There may be guilt and shame involved.
A physician must start to adopt the healthy lifestyle they prescribe to their patients, including regular exercise, adequate sleep and a nutritious diet. Formal stress management and mindfulness courses could be undertaken, and importantly, the incorporation of boundary-setting and the practice of saying “no.”
Burnout and “compassion fatigue” need to be addressed while confidence is re-established to create new career goals and a healthier path forward. As in any addiction treatment, the overall goal is to prevent relapse and ensure a long-term recovery.
There is no dishonour in a doctor seeking help for an addiction. There is an element of tragedy if the addiction is to their own medical career at the expense of their own health and the well-being of those around them. Even more so if the diagnosis is never made or even considered. The biblical phrase, “Physician, heal thyself” is thus paraphrased to “Physician, heal thyself first from being a physician only.” Easier said than done.
DR. TED JABLONSKI is a southern Alberta family doctor.
HERE


YOU . Our domestic manufacturing site, located in Québec, will manufacture up to 100 generic products for the benefit of Canadians.*



A























BY DR. RAJ WAGHMARE




















It’s mid-January and I’m working with Ajay. We call each other “paaji,” which loosely translated from Punjabi means brother. Neither of us is from Punjab, but that doesn’t matter
Ajay (all names changed) is a physician assistant, but he practised as a physician in India, the same country from which my parents emigrated six decades ago. He doesn’t drink, he doesn’t eat meat, he doesn’t swear. He doesn’t listen to Van Halen and he doesn’t watch baseball or hockey. He has two teenaged girls and I have two teenaged boys. We have almost nothing in common. Almost.
He’s working in fast track, seeing one-touch patients—sprains and strains, cellulitis, coughs—while I’m taking care of more complex complaints. Just after 11 a.m., he brings me a chart. “Your favourite,” he says. “Foreign body in ear.”




removal and the occasional fine stitch removal. Alligators are a simple, yet elegant tool: fine-toothed forceps with a scissor-like handle that’s angled away from the forceps’ grasp.














“We’ve tried everything for two days,” Edward’s mother says, exasperated. “We’ve tried holding his ear open and flushing it with water, we’ve tried an ear curette, we’ve tried shaking it out. He won’t sleep and he won’t eat. He won’t do anything other than pick at it and moan. It’s been two days of hell.”
“What’s in there?”




kernel of corn stuck in the ear of an ‘autistic, non-verbal, sometimes aggressive,’ large 14-year-old male
“You can do it,” I say. “I’m swamped.”
“You’ll have to do it,” he says. Before I can ask why, he says he’ll help me. “This one will be tricky.”
I look at the chart. “Fourteen years old.” I shrug. “Should be able to cooperate.”
“Fourteen,” Ajay says. “But autistic, non-verbal, sometimes aggressive and about twice the size of both of us.”
“OK,” I say. “Whenever you’re ready.” “Alligator forceps are in the room. Ready to go whenever you are.”
Of the many possible methods to extract foreign bodies from ears, I use alligator forceps or irrigation (high pressure water from a syringe) for the vast majority. I love alligators. When I first discovered them in residency, I ordered a pair for home use. They were $100, and I still have them in my medical kit. I’ve used them mostly for sliver
“A kernel of corn,” Ajay says. “They were eating popcorn two nights ago and he took an un-popped kernel and stuffed it inside his ear.”
I turn to Ajay. “Do you think we can do this without sedation?”
“Sure,” Ajay says, just as Edward’s mother says. “No needles, please. The last time he had blood work it took four nurses to hold him down and he pulled out the needle just as the blood was being drawn.”
While Edward’s mother gives him a firm embrace, I have a quick look into his left ear. Although Ajay wants me to use the forceps, the kernel is wedged deep into the canal. If I’m able to get him still enough to feed the alligator tip to the kernel, I doubt I’ll be able to grasp it because not only is there no room around the kernel, it’s spherical and very likely to slip from my tool’s grasp.
We need a nurse to help us and Ajay leaves and returns with Jennifer. She’s one of our newer nurses, but she’s tall and broad-shouldered. To us, she is a Goliath and I’m glad she’s here. Edward is in our ENT room, seated in something similar to a dental chair. His father takes the right side, Ajay takes the head while
Jennifer and I are on the left—the side with the kernel. Edward’s mom has her hands on his legs—she’s probably going to have the toughest job, especially if he kicks. They all slowly lean down on him, using gentle but forceful restraint. After three minutes, we think we have him immobilized. I take the water-filled syringe and direct the small cannula into his ear, using one hand to steady the other so I don’t inadvertently touch his ear canal or the kernel. In one smooth, quick motion, I depress the plunger as quickly as I can. Edward roars and one of his arms breaks free. His father grabs it and forces it back toward his side. His mother buries her chest onto his legs and grabs the sides of the chair. Ajay and Jen are using all of their strength to control his head and the left side of his body. Edward’s flexed muscles are so tight and his face is maroon. He’s like Bruce (“David” if you grew up in the 80s) Banner about to turn into the Incredible Hulk. His moans turn into a roar of anger. I have a quick look with the light. The kernel hasn’t budged.
As quickly as I can, I reload the syringe and direct it toward a target that’s now moving. I give another long squirt as Edward struggles against our grasp. As soon as the second syringe is empty, I flash an otoscope and all I see is that freaking brown kernel staring back at me.
“I think you’re right,” I tell Ajay, breathless. “Alligators may be my only option.” I’m sweating now, and I’m stressed. “Let’s give him a break,” I say, knowing that he’s not the only one in the room who needs to rest. Everyone slowly eases off Edward, and once he’s free, he’s calm and comfortable. After several minutes, I have the alligators in my hand and I’m calculating my approach. Edward sees the tool, but doesn’t seem to care, seemingly unaware that shortly I’ll be prodding the inside of his ear with this pointed appliance.
On Edward’s right, his father kneels and hugs him, holding his arms tightly to his body. Ajay wraps his arms around his head once again while Jen leans into Edward’s body and holds his chin. His eyes are wide with fear as his mom once again lowers herself onto his legs. It’s tougher this time. Despite
everyone’s effort, his head is moving back and forth. It’s like the classic board game Operation, where players use metal forceps to collect tiny bones and organs out of holes punched from the silhouette of a chubby plastic man. If you miss, a buzzer goes off and his nose lights up. Taking the kernel out of Edward’s ear will be like playing Operation game on a speedboat. Minutes have passed by the time my alligator is finally entering the ear canal. I’d love to take even more time, and wear Edward out, but the other four people in the room are struggling and they’re tiring too.
“We didn’t solve a mysterious case, we didn’t save anyone’s life, but it’s the best thing we’ll do all day, maybe all week, maybe all month.”
break free. I edge closer to him and lean my left forearm gently on his cheek until his head is pinned against the chair-back. Jen and Edward’s mother are now on top of him, and he seems to have stopped fighting—for the moment. I direct the light onto the kernel, and I see an edge of fluff (the kernel must have been a splitsecond from popping) coming off the tiny brown ball. I open the jaws of the alligator, just two to three millimetres, edge them deeper and then pinch them closed. I pull out just before Edward moves again.
Edward’s arm breaks free and knocks me away. His head is now unrestrained and he roars and shakes his head vigorously. We all back away. My right hand is held high in the air, my thumb and index fingers snug inside the looped handles of the alligators. And nestled secure within the alligators’ grasp is the kernel.
I see Edward’s dad first, at the foot of the bed. His face is red and he’s sweating. He’s exhausted. He’s so happy he has tears in his eyes. He holds his hand up; I give him a hard high-five. It’s like we’ve just won game seven in overtime. His mother is shoving her husband out of the way as she walks toward me, arms open. I accept her embrace and hug her back. She’s so happy, she won’t let go, but when she finally does, Ajay is there, and we give each other high fives, along with Jen, and trade slaps on the back.
Every few moments Edward grits his teeth, grunts and tries to break free. After each episode, Ajay repositions Edward’s head. If he moves like that while I’m in there, I might push the kernel further or impale his ear canal with the tip of the forceps. I stop. My hands are moist. My forehead is wet. The glasses I’m wearing above the mask are fogging up. I’m about to tell them that I can’t do this because he’s moving too much. He’ll have to be sedated and this should be done in the operating room under the control of a general anesthetic. But this means many more hours of waiting, a needle—and it would mean that I’ve let everyone down.
I take a deep breath. His head is jerking back and forth as he tries to
We didn’t solve a mysterious case, we didn’t save anyone’s life, but it’s the best thing we’ll do all day, maybe all week, maybe all month.
We don’t think about the word much, “paaji.” But although we were raised in different countries, with different opportunities, and in different cultures, this is what we are. Brothers. Day after day, we share experiences that others might consider once-in-a-lifetime. Whether it’s an athlete with a season-ending fracture, a woman losing her first pregnancy, or an elderly man taking his last breath, this is what life is like in the ER, and this is what we, the people who work in the ER, are to each other. We’re family.
DR. RAJ WAGHMARE is an ER physician. He blogs at theoverheadpage.com. His stories come from more than 20 years of practice.
Clinics
don’t often have cybersecurity insurance, but
some experts say that is a
mistake
BY NORM TOLLINSKY
The Information and Privacy Commissioner of Ontario’s (IPC) office reported 27 ransomware attacks under the province’s Personal Health Information Protection Act over a period of three years ending December 2023. Among them was an unnamed diagnostic imaging clinic that lost access to as many as 550,000 patient records and 1.6 million case files.
The ransomware group, “encrypted and exfiltrated files from the electronic medical records and file sharing servers, deleted the backups and demanded ransom payment,” according to the IPC incident report. The clinic had to pay the ransom to get its data back. PHIPA Decision 249 on the IPC website goes into detail on how the threat actor, a known hacking group, penetrated the clinic’s system and recommends measures to prevent such attacks. The report doesn’t divulge the amount of the ransom paid, nor does it say if the clinic was covered by cybersecurity insurance.
More recently, on March 6, 2024, the Barrie Community Family Health Team in Ontario experienced “a cybersecurity incident” resulting in the theft of personal health information. The incident was reported to the IPC as required, but there was no public admission of a ransom being paid.
Given the increasing risk of data loss and the costs associated with it, do doctors and medical clinics have cybersecurity insurance? “I don’t believe most do,” said Ariane Siegel, general counsel and chief privacy officer of OntarioMD. “I think it’s a very important coverage to consider because regular commercial insurance will not
ransomware attacks that target specific institutions—hospitals, for example— because of their ability to pay lucrative ransoms, but also untargeted attacks by actors, “who send out thousands of emails trying to get someone to click on a link. If that individual happens to be a doctor or a clerk in a doctor’s office, they’ll get hit,” said Beggs.
The cybercriminal may start out demanding $150,000 but settle for $8,000 once they realize they’re negotiating with a sole practitioner or a small medical clinic that doesn’t have deep pockets. However, having paid the $8,000 in Bitcoin, there is no guarantee they’ll get their data back, cautioned Beggs.
Sole practitioners and small clinics are also vulnerable because they don’t generally have the IT support and protections in place to thwart an attack.


generally pay for a privacy breach or the expenses that accrue with it. So depending on the scale of your practice and how bad the damage is, you’ll be responsible for footing the bill.”
Cybersecurity insurance is widely available. OMA Insurance, a subsidiary of the OMA, offers it as, “a side-rider,” but doctors and medical clinics have been slow to take advantage of it. Why?
Siegel isn’t sure. In some cases, it’s not available because insurance companies insist on, “a certain maturity in your systems, practices and procedures in order to qualify for it,” she said.
Doctors may also downplay the risk, thinking cybercriminals are more interested in “bigger fish,” but that isn’t necessarily true, according to Roger Beggs, CEO of DigitalDefence, a cybersecurity consulting company with a Canada-wide clientele. There are
The cost of cyberinsurance could also dissuade doctors from taking advantage of it. Beggs estimates the cost of a policy at between $5,000 and $20,000. Brandon Bowie of Toronto-based Zensurance Brokers acknowledges that the cost could go that high but says, “We have quoted tons of medical professionals for cyber liability policies that are under $1,000 a year.”
The cost depends on the size of the practice, how a clinic stores its data, how its system is secured and how diligent it is about cybertraining.
Protection begins with using a certified EMR with built-in security and privacy safeguards, said Siegel. In Ontario, 95% of doctors use an OntarioMD certified EMR and 80% of EMRs store data in the cloud, which is safer than local storage. If data isn’t stored in the cloud, doctors should back up their data locally every night and store it offline. Also recommended are multi-factor authentication, prompt installation of software and hardware patches, strong passwords, regular cybersecurity training, and managed virus protection software as an alternative to the free stuff.
However, even with all this, there are no guaranties. Every doctor and medical clinic has to weigh the risks to their practice and make their own decision about purchasing cybersecurity insurance.

to introduce GLP-1 receptor agonists and GLP-1/GIP dual agonists in the clinic
BY KYLIE TAGGART
The past year has seen major trials report the benefits of glucagonlike peptide-1 (GLP-1) receptor agonists and GLP-1/glucose-dependent insulinotropic polypeptide (GIP) dual receptor agonists in people with chronic kidney disease and/or heart failure. There’s now good evidence to add these treatments to protect the heart and kidneys, but existing guidelines have yet to catch up to the findings. Experts gathered at the Canadian Cardiovascular Congress in October to discuss these therapies.
The evidence
Results from the SELECT trial showed that people with diabetes and obesity
had fewer cardiovascular events when randomized to receive semaglutide over placebo. Yet it was the results from STEP-HFpEF (heart failure with preserved ejection fraction) and STEP-HFpEF-DM trials, published in the New England Journal of Medicine (NEJM) in August 2023 and April 2024 that firmly established semaglutide as a cardiologist’s drug, said Dr. Shelley Zieroth, a cardiologist and director of the heart failure and transplant clinics at St. Boniface Hospital in Winnipeg and professor of internal medicine at the University of Manitoba. The trials included patients with obesity and symptomatic heart failure, with or without diabetes. Those on 2.4 mg
semaglutide a week had fewer symptoms and better physical function than those on placebo. The trial results provide evidence for, “another layer of treatment for patients with HFpEF and an obesity profile who often have limited treatment options available,” noted Dr. Abhinav Sharma, a cardiologist and assistant professor at McGill University and the research institute of the McGill University Health Centre in Montreal.
The SELECT-HFpEF trials showed that the effects on cardiovascular outcomes are beyond weight loss and blood sugar control, with reductions in C-reactive protein (CRP) and N-terminal pro–B-type natriuretic peptide (NT-proBNP) levels. “It’s not just weight loss but other physiologic changes as well that drive these outcomes,” Dr. Sharma said.
Data are now available from the SUMMIT trial, published in the NEJM in December 2024, showing patients with HFpEF and obesity significantly benefited from the GLP-1/GIP dual agonist tirzepatide over placebo. More data are coming, including the results of the SURPASS CVOT trial, a comparison of tirzepatide and dulaglutide in patients with type 2 diabetes.
In May 2024, NEJM published the results of the FLOW trial, involving patients with chronic kidney disease and type 2 diabetes randomized to 1 mg semaglutide (the more common dose at the time of trial initiation) or placebo. The findings add to evidence from other trials (e.g., LEADER, REWIND, SUSTAIN-6) showing GLP-1 inhibitors are renal protective. These studies are in patients with diabetes and kidney disease, but smaller randomized control trials are showing benefits of incretin therapies in people with chronic kidney disease (CKD) with or without diabetes, noted Dr. Navdeep Tangri, nephrologist and professor of medicine at the Max Rady College of Medicine at the University of Manitoba in a conversation with the Medical Post
“As an endocrinologist, I absolutely love using GLP-1s in the setting of CKD,” said Dr. Julie Lovshin, a clinicianscientist at Sunnybrook Health Sciences Centre and assistant professor at Temerty
faculty of medicine at the University of Toronto. “Why? Because their A1C and their body weight loss effects have nothing to do with their glomerular filtration rate (GFR) and that’s very different from SGL2 inhibitors. They’re also safe in the setting of CKD and can be used at any GFR and any dialysis.”
When introducing these drugs, frame your discussion around organ protection instead of blood sugars, suggested Dr. Alice Cheng, an endocrinologist with Unity Health at St. Michael’s Hospital, and Trillium Health Partners in Toronto and associate professor at the University of Toronto. This way, patients won’t want to stop the medications once their blood sugars are at the target level. Dr. Cheng starts with: “I’d like to offer you medication to protect your brain, your heart and your kidneys.”
GLP-1 receptor agonists and GLP-1/ GIP dual receptor agonists need to be titrated. When it comes to introducing the medications, “Start slow and stay in it for the long-term,” Dr. Tangri said. Focus on the end-organ benefit, even if it takes six months to get the right dose.
Dr. Sharma said he usually lets the patients auto-titrate, making them aware of the desired regimen and the baseline dose, but allowing them to escalate only when side-effects are under control.
“The key thing is, as you escalate the dose, if people develop side-effects, you can always go back to the previous dose they were tolerating, stay there for a little longer, and then go back up,” Dr. Sharma said.
The important thing is to maintain a baseline dose. “I always say to them, ‘Don’t quit it without calling,’” Dr. Cheng said.
Physicians should counsel patients to exercise to counteract muscle loss.
Whether or not patients choose to take these medications depends on cost, Dr. Tangri said. Publicly funded coverage for these medications in Canada is currently limited to people with diabetes or obesity, Dr. Cheng said.
The most common adverse events, seen in about 10% to 20% of patients, are
“that lovely trio of nausea, vomiting or diarrhea,” Dr. Lovshin said. Constipation is another adverse event. She warns patients that they might not feel well.
“It is basically a transient effect, and it goes away,” Dr. Lovshin said. Advise patients to stop eating when no longer hungry, to eat smaller meals, avoid spicy food and stay hydrated.
Dr. Lovshin warned physicians to expect patients to have an elevated heart rate thanks to a GLP-1 receptor in the sinoatrial node in the heart. This could be difficult for patients with atrial fibrillation.
“I’d like to offer you medication to protect your brain, your heart and your kidneys.”
Some patients should not take GLP-1 receptor inhibitors, including those who are pregnant or breastfeeding. Physicians should also not offer them to people with chronic pancreatitis or a family history of medullary thyroid cancer.
Whether or not to hold GLP-1 receptor agonists prior to surgery is a hot topic. They cause delayed gastric emptying and retain gastric contents, leaving a potential risk of pulmonary aspiration. Dr. Cheng noted that the decision is best left to the anesthesiologist.
Patients with peripheral retinopathy should get the retinopathy treated by an ophthalmologist prior to starting GLP-1 receptor agonist treatment, Dr. Lovshin said.
The benefits of incretin therapies are additive. Current evidence (e.g., from STEP-HFpEF) suggests there are no or few negative interactions with other medications, including SGL2i (sodium
glucose co-transport inhibitors), Dr. Zieroth said.
However, be sure to stop DPP-4 inhibitors (“gliptins”) before adding a GLP-1 receptor agonist or a GLP-1/ GIP dual agonist. Note that while oral semaglutide has the same safety profile as injected semaglutide, it may affect absorption of other drugs.
While Diabetes Canada guidelines recommend starting on metformin first for patients with diabetes, cardiovascular risk factors and uncontrolled A1C, European and American guidelines differ, explained Dr. Akshay Jain, endocrinologist at TLC Diabetes and Endocrinology in Surrey, B.C., and clinical instructor at the University of British Columbia. He said he’d start on a GLP-1 receptor agonist first because he’d, “want to use a medication that not only works on blood sugars but other organ systems as well.”
These therapies don’t cause hypoglycemia, but if a patient is on insulin or insulin secretagogues and their A1C is 8% or lower, consider lowering the dose of insulin or insulin secretagogues, Dr. Cheng said. This should be in consultation with the patient and the physician responsible for managing diabetes treatment.
For some patients, the weight loss associated with incretin therapies isn’t needed and, “If the patient says that they’ve lost too much weight and aren’t feeling well, then that’s when you take action,” Dr. Cheng said. Consider switching the patient to a lower dose, which is still cardioprotective, or a GLP-1 receptor agonist with lower weight-loss effects.
To get organ protection, patients should remain on the treatment, Dr. Jain said. For those who need it for weight loss, it may be another conversation, Dr. Cheng noted. Patients should recognize that, “If you stop a GLP-1, people will regain the weight,” Dr. Lovshin said.
There will be more data on these therapies available in the coming months that will further influence practice. “It’s a pretty exciting time,” Dr. Zieroth said.

$1.7 million in damages awarded for a delayed thoracic MRI that led to a patient’s paraplegia
Hindsight bias is the tendency to see past events as having been more predictable than they really were. For example, sports fans often claim they could see their team’s loss coming, and it could easily have been prevented (so-called “Mondaymorning quarterbacking.”) Another example is that people might say they could tell a couple in their social circle was about to break up, re-interpreting any past disagreements or questionable behaviour as obvious harbingers of marital malaise. It happens to medicine too: In a recent study, doctors were asked to consider a hypothetical case of a patient with a swollen leg and to evaluate the treatment given. The treatment was scored as “poor” when they were
told the patient died the next day, but “good” when the patient was said to have recovered. In both scenarios, the treatment was exactly the same. The law of medical malpractice has a long history of trying to make sure hindsight bias does not taint justice. A classic example is the 1954 English case Roe v. Minister of Health, where patients were paralyzed after being given cinchocaine as a spinal anesthetic. The cinchocaine had been stored in sealed glass capsules floating in phenol, which leaked into the capsules through invisible cracks in the glass. This kind of leakage was unknown in 1947, the time of the incident, but by 1951 it had been discovered, and there were even warnings about it in a leading medical


BY BILL ROGERS
textbook. The court held the doctor blameless, ruling that, “We must not look at the 1947 accident with 1954 spectacles.”
In a recent Ontario case, a doctor who was found negligent by a jury appealed the decision, complaining that hindsight bias had worked mischief. He lost. The story began when the patient went to emergency with lower back pain, numbness down the left leg and pelvic area, and difficulty urinating and voiding. A lower spine MRI showed enhancement of the conus (the terminal end of the spinal cord) and of the cauda equina nerve roots below. The patient was told his condition warranted further neurological assessment and treatment. Months went by during which his condition did not improve—in fact, he came back to emergency on more than one occasion.
At one point it was thought he might be suffering from post-infectious myelopolyradiculopathy, an inflammatory reaction to his previous respiratory tract infection. He was accordingly treated with anti-inflammatory intravenous immunoglobulins, which failed to resolve the problem.
Ultimately he returned to hospital by ambulance, in a state of paraplegia. This time a thoracic MRI was done, revealing a dural AV fistula, which was surgically repaired. After therapy he regained the ability to walk, but still had nerve pain in his legs and pelvis, and leg spasms. His gait remained uneven, because his left leg was much weaker than his right, and he required help to walk any distance. He continued to have bowel and bladder symptoms that significantly impacted his day-to-day activities. He required ongoing therapy and medication.
The trial
The trial lasted more than three weeks. After deliberating for three days, the jury awarded just under $1.7 million in damages on the basis that the thoracic MRI should have been done sooner. If it had been, the fistula would have been detected and diagnosed before paraplegia set in, and the patient would have ended up in much better condition. The defence had argued that the defendant doctor did not breach the standard of care of a reasonable neurologist, given the difficulty in diagnosing a dural AV fistula, the rarity of this condition in a patient so young— he was in his 30s. Plus, there were no specific clinical symptoms suggesting this ailment. The jury didn’t buy it.
The issue of hindsight bias came into play because the defendant doctor told the appeal court that one of the patient’s expert witnesses was guilty of it. Specifically, the expert testified at trial that it was “hard to ignore” the ultimate diagnosis of a dural AV fistula when reviewing what transpired in the months leading up to it. This, said the defendant doctor, amounted to an admission of “retrospective analysis.” The appeal court disagreed, noting that, “The trial judge instructed the jury to avoid hindsight bias in determining the appropriate standard of care for a general neurologist in Ontario in 2010. The jury is presumed to have heeded this instruction.”
But did they? It is interesting to note that, during his cross-examination, this expert admitted that a dural AV fistula is a very rare type of malformation, and it is unusual or atypical in a patient in their early 30s. He admitted that some of the patient’s symptoms were inconsistent with this diagnosis and did not point to a problem with his thoracic spine. He admitted that the defendant doctor did not breach the standard of care when he failed to diagnose the fistula, or even consider it as a differential diagnosis in the early days of the unfortunate saga. Nevertheless, the expert concluded that a thoracic MRI should have been done earlier than it was. And even though he testified that it was “hard to ignore” the fact that a fistula was ultimately diagnosed, the appeal court
accepted that he did ignore it during testimony, and the jury ignored it also. We will never know for sure, but it sounds an awful lot like some Monday morning quarterbacking might have been going on.
The defendant doctor also challenged, unsuccessfully, the jury’s monetary award, arguing that it was too high in terms of compensating the patient for income loss. Noting once again that a jury’s verdict is entitled to a high degree of deference, the appeal court explained that, “The trial judge correctly instructed the jury that, to award the patient damages for future income loss, it would have to find a real and substantial risk that he would earn less than he would have, but for the injuries caused by the defendant doctor’s negligence.”
The patient testified that he had trouble working due to bladder and bowel incontinence, a lack of stamina and pain. One of the patient’s experts, a physiatrist and rehabilitation specialist, testified that a person with neurological impairments may age more quickly: “The way I would describe it is all of us, as we age, are more likely to have more problems physically, whether we have degenerative changes in our hips, knees or our back. But for someone who suffers from significant neurological impairments, where there already is, in my medical opinion, manifestations of secondary areas of pain, including his back and hips, it results in what I call acceleration of normal age-related changes.”
It is usually an uphill battle in an appeal court, especially when you are trying to overturn a jury verdict. As the appeal court noted, “Juries are not infallible, and their verdicts should not be regarded with awe,” but their decisions will be upheld unless they are “so plainly unreasonable and unjust as to satisfy the court that no jury reviewing the evidence as a whole and acting judicially could have reached it.” That was not the case here.
It was further noted that, “Appeal courts do not fine-comb jury answers, but accord them the respect of a common sense interpretation even where there may be some ambiguity
“The court held the doctor blameless, ruling that, ‘We must not look at the 1947 accident with 1954 spectacles.’”
in the answers. Juries do not write reasons for judgment, and their answers must be taken against the background of the evidence from which they are entitled to select, without manifesting their selection, what is credible, what is significant, what is persuasive to them. It is very often easy for an appeal court, in the leisurely scrutiny of the transcript, to find significance in pieces of evidence to contradict jury findings, and in so doing to usurp the jury’s function. . . . It is one thing to interfere with a jury’s verdict where there is simply no evidence to support its findings or to support a critical one; it is a different thing, and not to be encouraged, to interfere with its findings where there is evidence, however slight, on which they may be based, but where because of offsetting evidence a question of credit and weight arises. These are matters for the jury alone.”
BILL ROGERS is a Toronto lawyer and writer covering medical and pharmaceutical issues.




British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Nova Scotia, PEI & Newfoundland
Join the health care evolution with Enhanced Care Clinic, where doctors thrive. Set your own schedule/number of visits per hour or per day. Efficient medical admin and backend support (billing, scheduling, call back). Collegial environment with experienced peers. EMR on-site with remote access. Over a decade of practice support experience. Attractive compensation.
For location details: visit: yournewclinic.ca | call: (647) 254-5578 supportyourpractice@enhancedcare.ca





WHAT WOULD BE A FUNNY LINE FOR A CHARACTER TO SAY HERE?
Use your smartphone to scan the QR code above—or go online to www. canadianhealthcarenetwork.ca/ caption-februarys-cartoon-littledoctor—and you can enter your answer on the Medical Post’s online home. If your answer is selected, you’ll receive a $75 Amazon gift card and this cartoon will re-run in the next issue of the Medical Post magazine with your caption! So you get money—and doubtless esteem and accolades from your colleagues!

‘So, I’m afraid that you are going to need a transplant.’
We had a lot of great entries for the caption-thecartoon contest in the last issue of the Medical Post magazine, but we thought Dr. Darren Thompson’s entry above was the funniest. Dr. Thompson, a psychiatrist in Vancouver, will receive a $75 Amazon gift card as a prize.
I’m setting up practice. How can I make it as environmentally friendly as possible?
Tips for daily practice
Some things I have implemented in my family practice: no more plastic speculums, we use metal and autoclave. Fax referrals/ requisitions/prescriptions are sent directly from the chart. Incoming faxes are not printed but stored electronically for easy filing. We use no table paper and buy 100% recycled printer paper. We use reusable/ washable drapes and gowns and have a mask recycling bin from Vitacore. Virtual care is used when appropriate for the clinical situation as well as batching home visits based on location. Lastly, deprescribing medication and prescribing dry powder inhalers over metered-dose inhalers.
—DR. REBECCA RAPPAPORT
Mindful prescribing and more
At first glance, many of us think that setting up an environmentally friendly practice means reducing plastic waste (e.g., switching from paper gowns and plastic speculums to cloth and metal), cutting down on paper (e.g., setting up an e-fax system) and installing LED lights. About 20% of healthcare facilities’ carbon footprint comes from the power they use, so choosing energy-efficient equipment and consistently powering down computers and lights when they’re not in use are certainly good steps.
“Greening your practice is not only good for the planet, but it . . . saves you money, and is surprisingly easy to do.”
While these actions are helpful, the truth is that treatment of preventable diseases, and the tests and interventions we order, have far more impact on the planet. For example, about two-thirds of greenhouse gas emissions in primary care come from the pharmaceuticals we prescribe. Ensuring patients are engaging in evidence-based screening, and Choosing Wisely what we prescribe and order, are essential.
We should also remember that sustainable practice involves planning a professional life that’s sustainable for you as an individual. That means doing work that keeps you inspired. If you have the capacity to do more than greening your practice, consider Dr. Ayana Elizabeth Johnson’s Venn diagram when choosing your ideal climate action, which lies at the intersection of three things: the work that needs doing, what you’re



good at and what brings you joy. Whether you’re passionate about food, nature, or plastic waste, or a good communicator and connector or researcher, there’s a role for everyone in improving the sustainability of our healthcare system.
—DR. MELISSA LEM
Resources to help
There are many resources to help you green your practice on the Canadian Coalition for Green Health Care website, such as the Green Office Toolkit. You can also join their newly created Green Teams Networking Hub. Another great resource is CASCADES, with a variety of green healthcare playbooks and free virtual education events (cascadescanada.ca). Greening your practice is not only good for the planet, but it is also better for your patients, saves you money, and is surprisingly easy to do.
—DR. LAURETTE GELDENHUYS
How do you deal with an employee in your clinic who is generally good at their job, but gets touchy and defensive whenever they get feedback to help them improve performance?
Send solutions (and new questions!) to lleger@ensembleIQ.com by March 10. Get a $25 gift card if your answer is chosen.



























































The first and only PDE4i indicated in the topical treatment of seborrheic dermatitis* ONCE-DAILY STEROID-FREE* PDE4i

ZORYVE is indicated for topical treatment of seborrheic dermatitis in patients 9 years of age and older. FOR SEBORRHEIC

Designed for simple administration
• Can be used on all affected areas of skin, including the face, body, and/or scalp†
• Once-daily topical application
Please consult the Product Monograph at www.arcutis.ca/zoryve-pm-hcp for contraindications, warnings, precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The Product Monograph is also available by calling us at 1-844-692-6729.
PDE4i: phosphodiesterase 4 inhibitor
*Comparative clinical significance has not been established.
†When they are not wet.
‡Subject to restrictions. For program terms and conditions, go to www.zoryveassist.ca and click “Terms and Conditions”.
Reference:
1. ZORYVE® Product Monograph. Arcutis Canada, Inc. October 2024.
ZORYVE AssistTM Patient Assistance Program is designed to provide financial support to eligible patients receiving a ZORYVE prescription.‡