BATTLE OF THE ABBREVIATIONS:

NAFLD, NASH, CIRRHOSIS (NOT AN ABBREVIATION)
THE LIVER: OUR UNSUNG HERO AND GUARDIAN OF LIFE
HOW DO WE GET NASH?
ONE IN FOUR PEOPLE HAVE THIS DISEASE, COULD YOU?
WHAT CAN YOU DO ABOUT NASH TODAY?
NEW LIVER MEDS TAKE NEW APPROACHES
WHY YOU SHOULD CONSIDER GETTING A FIBROSCAN
NASH GETS RENAMED MASH
Medicalissuesarecomplex.OurmissionwithMedEvidenceisto providethetruthbehindthedatainmedicine,healthcare,and researchtoourcommunity.Weprovideatrustedsourceofreliable informationsoyoucanmakeinformeddecisionsaboutyourhealth.
PLEASE NOTE: THE INFORMATION PROVIDED IN THIS MAGAZINE IS FOR GENERAL EDUCATIONAL, SCIENTIFIC, AND INFORMATIONAL PURPOSES ONLY AND IS NOT INTENDED AS, AND SHOULD NOT BE TREATED AS, MEDICAL OR OTHER PROFESSIONAL ADVICE FOR ANY PARTICULAR INDIVIDUAL OR INDIVIDUALS IF YOU ARE EXPERIENCING ANY MEDICAL ISSUE OR HAVE ANY MEDICAL CONCERNS, YOU SHOULD CONSULT WITH A DOCTOR OR OTHER MEDICAL PROFESSIONAL.







Fats are tasty in food, but not particularly good in the bloodstream. They can also be toxic to the liver and cells in general. We have special cells called adipose cells that store fat in our body. These cells have defenses against dangerous fat components called free fatty acids. Free fatty acids are the high-energy parts of fats, the part that gives you energy. Fatty acids are a great way to store energy and can be turned into power for your body, but the high energy content can also be dangerous in the wrong places.
The liver transforms free fatty acids into usable energy. From here, the energy is delivered to cells all over the body. The liver is part of the system that makes sure the body’s energy demands match the available energy. Unfortunately, when too many free fatty acids are delivered to the liver, they can start to build up in the liver tissue and cause damage.
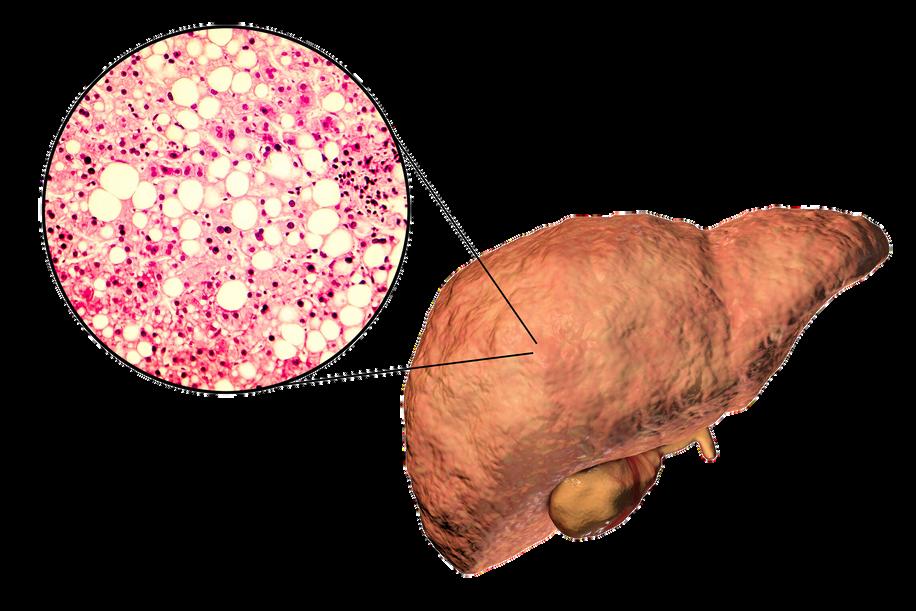
Fatty liver is one of the most common ailments in Western countries. One in every three to four people in the US have a fatty liver. Excessive alcohol consumption can cause a fatty liver, but most sufferers develop non-alcoholic fatty liver disease (NAFLD). Either way, people have steatosis. Steato- means fat, and -osis indicates a condition, especially an abnormal one. Steatosis of 5-10% is problematic and is the earliest indication that the liver is starting to suffer damage. Many people with fatty liver and no other abnormalities can make a full recovery, usually by stopping whatever is causing the steatosis.
We know that alcohol can directly damage the liver, but how does NAFLD start? The causes are complicated, but some similarities exist. Excess fat released from fat cells, excess fat created by the liver, and excess fats from the diet all find their way into the liver. These are normally not an issue, but all are affected when the body isn’t regulating insulin properly. Insulin lets body parts know when you have food or are starving. When insulin isn’t
processed correctly the body thinks it’s starving and tries to compensate – even when there is plenty of food present. In the middle of this the liver suffers.
After a prolonged period of fat accumulation, a patient with NAFLD may develop nonalcoholic steatohepatitis, or NASH. Steato- for fat, hepat- indicating the liver, and -itis, which means inflammation. This second leg of the terrible journey develops when fat causes inflammation in the liver. The gut changes and gives the wrong signals to the liver. Cells develop insulin resistance and can’t convert sugars into energy or fats correctly. Free fatty acids cause cell problems and elicit an immune response. Stresses on the liver cause a feedback loop, where inflammation disrupts cell function. The body tries to fix the liver but can’t overcome the massive amount of dangerous fats. Cells in the liver die, and the living cells can be damaged trying to compensate. With NASH, the inflammation is long-lasting, also called chronic.
The liver can regenerate from NAFLD and NASH. It can’t sustain forever, however. When the liver is permanently damaged, the tissue can scar and die. This is a permanent reduction in liver function. We call this scarring Cirrhosis. Cirros- is the Greek word for yellow-brown (the color of a dying liver), and -osis refers to a condition, especially an abnormal one. Cirrhosis has multiple stages and can be asymptomatic but cannot be recovered from without intervention. The current treatment for cirrhosis is a liver transplant.
Though we’ve been talking about the dangers of fats in the bloodstream and liver, it should be noted that the body makes a lot of these fats out of carbohydrates – sugars. A healthy diet without too many sugars and with lots of exercise are the best preventative measures for these conditions. Conditions related to insulin resistance, such as type 2 diabetes and metabolic syndrome, can both cause and be caused by these conditions. Also, even though we have presented these as a pathway, note that you can revert from NASH to NAFLD or become symptom-free; it’s not a one-way journey! If you have any of these conditions, talk to your primary care physician to look for solutions. Also, keep an eye out for clinical research trials that may alleviate symptoms or the underlying fat buildup.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA

Is the liver the most amazing organ? Yes. It turns food into usable molecules. It makes proteins, bile, and hormones. It filters dangerous drugs and toxins. Without it, you would die within minutes. Also, the liver can regenerate (like a lizard’s tail!), which is basically magic. The liver is estimated to have over 500 individual functions and interacts with most body systems. In this article we’ll look at the liver, zooming in from basic facts to its cellular units. Then we’ll explore the functions of the liver.
If you were to guess the largest organ in the body, would you guess the liver? I hope not, because it’s the skin. But the liver is in second place! It makes up around 2% of your body weight and usually contains about 10% of your blood. It’s located under the ribs, right below the diaphragm that inflates the lungs. It’s smooth and reddish brown when healthy (note: if you can see your liver’s color you are probably having a bad day). The liver can be divided into four parts called lobes and thousands of sub-parts called lobules. These are hexagonal columns of cells arranged so that blood can travel through carrying nutrients in and toxins and waste out.
Four types of cells make up the liver: hepatocytes, epithelial cells, Kupffer cells, and stellate cells. Most of the liver is composed of hepatocytes. These are the workhorses of the liver. Hepatocytes convert fats (called lipids), sugars (called carbohydrates), and proteins (called proteins) into usable forms. They detoxify dangerous things and excrete bile and cholesterol. The barrier epithelial cells line the walls (including blood vessel walls) inside the liver and do some filtering of small particles. It is thought that these may also do some clearance of viruses. Kupffer cells are the resident immune cells. These large cells eat bacteria and debris that enter lobules. They are always touching these dangerous particles and exhibit a constant, low-level inflammation. Disruption of these cells can result in widespread, damaging liver inflammation. Finally, stellate cells store vitamin A, a critical vitamin. They are critical for promoting the liver’s amazing ability to regenerate. They form temporary scars that allow for healing. When they are damaged, however, they lose vitamin A. Damaged stellate cells can “activate” and run amok, secreting a lot of collagen that causes fibrosis and permanent scarring called cirrhosis.
To understand the liver’s major functions, let’s first look at our body cells. Cells need to have a balance of chemicals to function properly. Normally cells control what goes in and
out of them using special proteins. To keep unwanted things out, cells are separated from the environment around them. This separation is done by a membrane made of phospholipids. The –lipid at the end is another word for fat. Since the borders of our cells are made of fats, things that can pass through fats (called fat-soluble) can easily pass through the cell membranes. Cells can’t control this very well, so we use the liver instead.
Let’s run through the liver’s major functions of storage, conversion, and creation. Storage is fairly simple. The liver stores fat-soluble vitamins and converts some of them into usable forms. It stores a quick supply of energy in the form of glycogen. Blood is stored in large quantities in the liver. This makes sense because the liver is filtering the blood. Usually, it holds a little more than 10% of the body’s blood, but the liver can expand to hold much more if needed. It can also squeeze blood out if the body is bleeding profusely. This probably isn’t great for the liver, but then again neither is bleeding out and dying.
The liver converts a huge amount of material from one form into another. It acts as a gatekeeper for nearly all the blood in the body, including blood directly from the digestive tract. This includes tasty nutrients like fat and sugar and dangerous toxins like alcohol and methamphetamine. Blood is carried across the lobules and filtered through the hepatocytes and Kupffer cells. The liver doesn’t just remove dangerous particles, however, it metabolizes them! Metabolism is the conversion of chemicals from one form to another. One of the most important metabolic functions is detoxification. To make drugs and toxins less dangerous, the liver converts them from being fat-soluble (able to pass through cell membranes) to being water-soluble (able to be released through urine but much harder to enter cells). Carbohydrates are converted to glycogen for storage. The liver changes fats into energy for use. Proteins are broken into building blocks and waste products are removed. Remnants of dead blood cells called bilirubin are turned into bile and used for digestion.
The conversion of materials into component parts helps the liver’s third broad function, creation. The liver creates or synthesizes many molecules that are used all around the body. It creates important hormones like angiotensin and thyroxine. It makes chemicals for the blood like prothrombin, fibrinogen, and clotting factors. It also makes the aforementioned bile, which is critical for digesting fats.
The liver is the ultimate hero. Through all of these functions, the liver acts in the best interest of the body. It takes the hit from dangerous chemicals and sacrifices its own blood when we need it most. The liver is a team player of the highest degree. When it goes wrong, we suffer throughout our whole body. Take care of that liver!

The liver is an amazing and necessary organ. It can regenerate from a minor injury, break down dangerous chemicals and drugs, and help maintain the proper balance of nutrients, fats, and sugars in the body. It also has hundreds of other important roles. With all this responsibility, we are in trouble when the liver stops working.
One way the liver stops working is through non-alcoholic steatohepatitis (NASH). Steatomeans fat, hepato- indicates the liver, and -itis means inflammation. Steatohepatitis is inflammation of the liver caused by fat accumulation. It is a progressive form of nonalcoholic fatty liver disease – the most common liver disorder in Western countries. Progressive means that this disease gets more severe over time.
NASH is a significant problem in America, affecting 3-12% of adults. Furthermore, NASH can lead to cirrhosis, where the liver is permanently damaged, and lead to possible liver transplantation. Over a million adults in America have NASH-related cirrhosis.
How do we get NASH? As the name indicates, this is not caused by alcohol. There are many pathways to developing NASH, but the underlying cause may be excess carbs and fatty acids. This can be due to diet or behavior, underlying genetics, or associated syndromes.
Some of the syndromes associated with NASH are:
Metabolic syndrome
Obesity
Type 2 diabetes
High blood pressure
Dyslipidemia
Hypothyroidism
Cardiovascular risk
Advanced liver problems
The underlying mechanism of NASH can be very complex. A leading precursor to NASH is insulin resistance, where cells fail to respond to insulin. Conditions that cause or are caused by insulin resistance, such as type II diabetes and metabolic syndrome, may increase your chances of developing NASH. They also may develop or worsen as NASH symptoms get worse.
Insulin resistance causes different types of fats to accumulate in the liver. This makes it very difficult for the liver to process the fats and they ultimately build up in liver cells. These fats, especially ones called nonesterified fatty acids (NFEAs), are very dangerous. They cause damage to liver cells and can also activate cytokines that start the inflammation process.
Eventually, we get NASH, an inflammation cascade in the liver caused by fats. Cytokines start inflammation in the liver. Cell death attracts the immune system, which enters and causes inflammation while trying to help. Liver cells die and are less able to process fats, which leads to a compounding effect. Eventually, we may transition to cirrhosis, where permanent liver scarring and damage occur.
There are few treatments on the market for NASH. As usual, the primary therapy for NASH is a good diet and regular exercise. Medicinal remedies are all in the experimental phases. Potential targets include increasing insulin sensitivity, decreasing fat creation, decreasing circulating fats, breaking fats down, and anti-inflammation treatments.
One way to decrease circulating fats is by expelling them through the digestive system. In the liver, moving fats to the gut is regulated by thyroid hormones. Thyroid hormones activate receptors, which exist all over the body and cause many different effects. Thyroid hormone receptor Beta (THR-β) exists almost exclusively in the liver. Scientists are working to create medicines that activate THR-β and help clear fats from the liver in NASH patients. If you are interested in participating in a research study, contact your local ENCORE Research Group site today!
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Low Exercise
On March 14, 2024, the US FDA granted accelerated approval for Madrigal Pharmaceuticals’ Rezdiffra (resmetirom) with diet and exercise for the treatment of Nonalcoholic Steatohepatitis (NASH), also known as Metabolic Dysfunction-Associated Steatohepatitis (MASH). NASH, a form of fatty liver, affects around 5% of adults in the United States and can lead to debilitating liver failure over the long term. Rezdiffra selectively activates thyroid hormone receptor-β. When combined with diet and exercise, this significantly decreases liver fibrosis and can lead to NASH resolution. Rezdiffra has been the target medication of multiple clinical trials at ENCORE Research Group sites. Jacksonville Center for Clinical Research, Nature Coast Clinical Research – Inverness, and St. Johns Center for Clinical Research have all participated in trials involving Rezdiffra.



Date: June 22, 2022
Liver disease is a type of illness like high cholesterol or blood pressure issues, where the patient is not always aware that they have a problem. Those kinds of problems that are under the surface are really compelling for us as primary care doctors. Somebody may have liver disease and not know it, so generally, when folks come in, and they're a little overweight or their blood sugar is high, we are concerned about the possibility of liver issues. We generally begin in the office by getting some basic lab work. Sometimes, their blood sugar is elevated, or their liver function testing is slightly abnormal. We know that when the liver cells die, they have enzymes that they release into the blood.
If you are overweight and you find out from your doctor that your blood sugar is high and your liver tests are a little bit high, then you are the perfect patient to find out exactly what's going on with the liver. We run a scan over the liver (like an ultrasound) and measure whether there's a problem with too much fat in the liver or if there's some scarring. The scarring leads to liver stiffness. We call that fibrosis. It decreases the blood supply to the liver, which can ultimately cause cirrhosis. The liver shrivels up and is not functional anymore.
This problem is reversible: start exercising, lose five to ten percent of your body weight, and start changing your diet. What you eat does make a difference in terms of fatty liver and the progression to more significant liver disease.
Michael J. Koren, MDAs a cardiologist, I usually argue that the heart is the center of the universe, but I must admit that the liver is important also, and we like to say that you can't LIVE without your LIVEr. There's some wisdom to that, and I remind people that the liver is basically the body's pharmacist, and it provides some very, very important functions. It neutralizes toxins, helps us metabolize our foods, and also has a vital role in clotting. Without these functions, you can't live.
 MedEvidence Podcast "One in Four People Have This Disease, Could You?" Recorded
MedEvidence Podcast "One in Four People Have This Disease, Could You?" Recorded Date: June 22, 2022
MedEvidence Podcast "One in Four People Have This Disease, Could You?" Recorded
MedEvidence Podcast "One in Four People Have This Disease, Could You?" Recorded Date: June 22, 2022


We want to let the community know that, as a research group, we provide free services, and one of the free services we provide is a ibroscan. This is what we call ultrasonic elastography, which is a form of ultrasound that tells us what the tissue characterization is, how healthy t is, if it is sick and in trouble, and if it is beyond help. This is a neat part of what we do. We provide the service for free, and we also encourage people who have been diagnosed with liver disease to participate in our clinical research.
MedEvidence Podcast "One in Four People Have This Disease, Could You?" Recorded Date: June 22, 2022
I think it's important to remember that the global prevalence or the risk is about one in four people. About 25 percent of the global population is affected by non-alcoholic fatty liver disease (NASH). Still, when we progress to fibrosis, that's about 12 – 15 percent of the general population. It's not rare. I pay most attention to those patients who are overweight with a BMI over 30 and are insulin resistant. I'm starting to see that people with diabetes have about a 95% chance of developing non-alcoholic fatty liver disease. About 20% of those have fibrosis. So again, this is not a rare thing.
Sometimes, we place patients on statins, and the liver function tests go up because they don't have a fully functioning liver. There may be a little scarring, and often, we look and see that they have non-alcoholic fatty liver disease.
For treatment, we've tried Pioglitazone, which is a diabetic drug that has a very mild reduction in fibrosis. Weight loss, exercise, and changing your eating habits can make a big change. Newer GLP-1s, like Semaglutide, have worked well, but we now have new drugs that we're researching in our community that are showing great promise, and that's very exciting.
To emphasize the point about imaging and the next steps, we use fibroscanning all the time in the research setting. Still, it’s not used that often in the clinical setting, and maybe you can comment on why that's so difficult for some practices to get access.


It all comes down to payers. It's very often not covered by insurance. They don't see the great value. But if we don't identify this early, it can lead to more progression and scarring, which could lead to coronary disease, liver cancer, etc., and those costs are very expensive. The bottom line is coverage.
Well, the interesting thing about fibroscanning is that it's a relatively simple technology that's relatively cheap. Still, the payers have set the reimbursement so low that practices can't make a living by providing fibroscans. The nice thing about research is that we have external funding, and we can hire experts in it and do more screening that we provide for free because we never actually take any money from our patients, nor do we collect any insurance information. We're doing this all based on study grants that we've been fortunately awarded, so it’s an important little point for people to understand.


Fatty liver disease is the number one reason people are getting liver transplants these days. It's completely replaced hepatitis as the main reason.
Our options for fatty liver treatment are not great. Vitamin E is supposed to help a little bit. There's a diabetic drug called pioglitazone that is a treatment option. A lot of fatty liver patients are pre-diabetic or diabetic, so you can add on some pioglitazone or Omega-3s to slow it down a little bit. We are hoping GLP-1s show some decreased percentage of fat in the liver. We're already using GLP-1s for multiple other indications like diabetes and heart failure. I strongly hope that the GLP-1s will be a good avenue of treatment for this in the future. We need something. Obviously, diet and exercise, losing weight, and losing abdominal fat will help. Dr. Lopez just got the last version of the Internal Medicine News magazine, highlighting this whole fatty liver disease issue, so this is front and center regarding medical communication and medical research.


NASH can lead to cell death, cells going rogue, collagen accumulation, fibrosis, cirrhosis, and liver cancer. One problem with treating NASH is that it is a multifactorial disease, meaning there are many possible causes that all lead to the same outcome. The current best methods for treating NASH are exercise, weight loss, and treating other conditions that may contribute. We will discuss scientifically backed information regarding these treatment options, but it is critical that any medical advice be discussed with your doctor. NASH has many many causes and affects a lot of body systems. Medical professionals that may be involved in NASH treatment include your primary care physician, a hepatologist, a dietitian, an endocrinologist, a cardiologist, and others. Every person is an experiment of one, and your specific circumstances may contraindicate one or all of the methods discussed below. Talk to your doctor.
Weight loss is the go-to method of treating NASH. A combination of diet and exercise is the best method to achieve weight loss. This ensures fewer calories enter the body than exit it and that the body is burning fat instead of muscle. Losing weight rapidly can be dangerous, so be conscientious of your body’s overall health (and speak with a professional!) Research has shown that reducing weight by as little as 5% (12.5 lbs for a 250 lb person) can help improve steatosis, the fat buildup in the liver. Losing 7% or more (17.5 lbs for a 250 lb person) shows reduced inflammation and improved health of liver cells. When patients, particularly obese patients, lose 10% of their body weight (25 lbs for a 250 lb person) the structural liver changes known as fibrosis start to regress or stabilize. For NASH, patients of normal weight may see results when losing as little as 3-5% of body weight.
Exercise is a great way to lose weight, and exercise can also help your liver even when you aren’t losing weight. The exact mechanisms for how this works are complex and not fully known. Scientists have found that exercise helps make the body more sensitive to insulin –which helps it regulate blood sugar. It can also help cellular metabolism. Exercise is associated with a reduction in the markers of liver inflammation and may help liver cells stay healthy. Aerobic exercise, also called “cardio,” is highly recommended. Resistance training, called strength training, is helpful especially if aerobics are not possible. NASH patients start seeing benefits when doing exercise for 150 - 300 minutes (2 ½ – 5 hours) per week of moderate intensity exercise or 75-150 minutes (1 ¼ – 2 ½ hours) per week of high
“My Liver isn't Fatty, it's Big-Boned.”

new exercise routine to avoid injury. Talk to a medical rcises (there is a theme to this article).
Exercise burns calories, but to lose weight we also want to manage what calories we take in. Consult with your doctor or dietitian, but reducing caloric intake to 500 fewer than the daily recommended value may help. Further, the number of calories is not directly correlated to the quality of the calories. NASH patients find improvements when reducing damaging foods, including fructose and saturated fats. Fructose is a form of sugar that is often added to sugary beverages (often as high fructose corn syrup) and contributes to insulin resistance. Saturated fats are found in meats, including red and processed meats. As for specific diets, research is ongoing. The Mediterranean diet has the most research backing its success in NASH patients. It is rich in fruits, vegetables, whole grains, seafood, nuts, legumes, and olive oil. Other diets may be suitable as well, including intermittent fasting, ketogenic diet, and others. One recommendation is to take the Mediterranean diet and adjust it to fit you. Regardless of the diet choice, alcohol should be limited. Anyone who
cohol entirely. It should go without saying that making major adjustments to your diet should be consulted with your doctor.
Other than diet and exercise, treatments for NASH are all achieved by treating other conditions that contribute and will vary depending on the individual. Conditions that contribute are obesity, diabetes, high blood pressure, high cholesterol, cardiovascular disease, and obstructive sleep apnea. Cardiovascular disease and obstructive sleep apnea are major contributors of mortality for NASH patients and should be taken seriously. Obviously, these conditions are best treated by going to your doctor.
NASH is a progressive disease that gets worse over time and leads to serious, occasionally deadly complications. Clinical trials may give us more medical NASH treatment in the future. Until then, give yourself a leg up (or liver) by consulting your doctor about treatments through diet, exercise, and underlying condition management.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
At this time, there are few widespread therapies for the treatment of NASH. The current standard of care is exercise and weight loss. Unfortunately, much like trying to lick your elbow, this is easier said than done. The consequences of an impaired liver include liver failure, cirrhosis, cancer, cardiovascular disease, and more. To alleviate this burden, scientists generally target the underlying mechanisms that lead to a fatty liver, aiming for a long-term solution. The broadest categories for investigative NASH medication manage fat, sugar, and inflammation in the liver.
One of the liver’s major jobs is to balance the body’s energy storage needs by managing fat. Thyroid hormone receptor beta (THR-β) can help us dump extra fats out of the body through the digestive system. THR-β may help reduce the accumulation of fats in the liver by telling the body to move fats from the liver to the gut.
Unfortunately, some people create an unhealthy amount of fat. They may have a mutated gene called PNPLA3. PNPLA3 genetic disorder affects how the fat cells in the body deal with triglycerides. This mutation can increase liver fat and possibly lead to NASH. Scientists are working on ways of suppressing this gene.
Nonselective and Selective Peroxisome Proliferator-Activated Receptor alpha (PPARα) medications may limit fat production. They target a chemical receptor on liver cells that regulates how fats are processed and can lower fat creation and lead to lower blood triglycerides (the most common type of fat). These medications also target and activate a very interesting hormone called fibroblast growth factor 21 (FGF21).

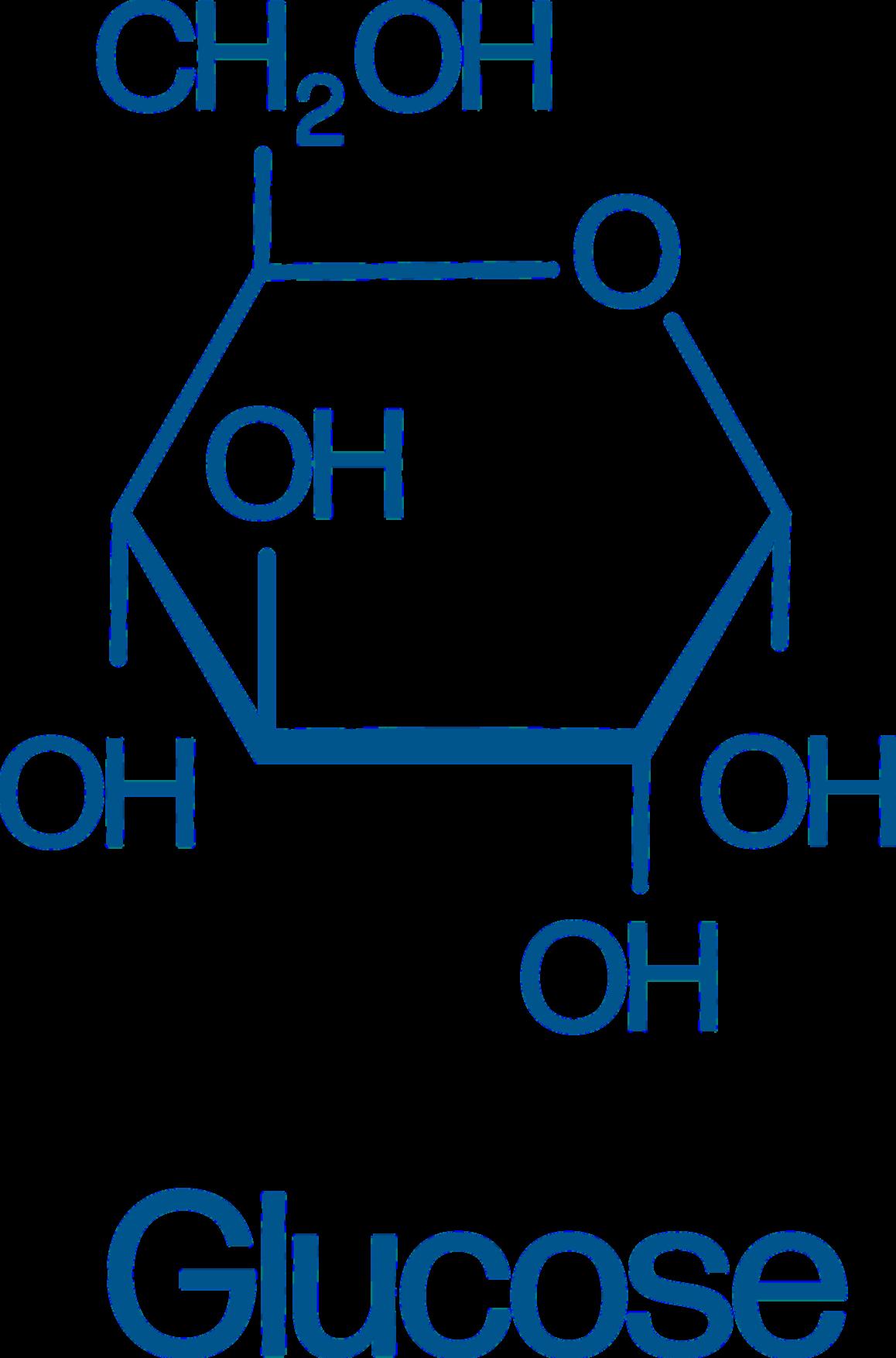
Fats can’t take all the spotlight, though, because one of the biggest culprits of liver damage is actually sugar. As a cookie lover, this makes me very sad. Sugars, also called glucose, are converted into fats (stored in the liver) and can damage the liver, metabolic system, heart, etc. The body detects high levels of sugar in the pancreas. High blood sugar signals the release of insulin and amylin from the pancreas to the liver. The liver then starts breaking down, converting, and storing sugars. A couple of medications look to target this system to lower the burden on the liver and help with NASH.
Fibroblast growth factor 21 (FGF21), mentioned above, has broad effects, including in the pancreas. It helps manage the body’s metabolism and homeostasis and makes the pancreas more sensitive to insulin. This may be particularly helpful for people with insulin resistance, which leads to type 2 diabetes. FGF21’s other effects appear to include increasing energy use, potentially leading to weight loss.
Glucagon-like peptide-1 (GLP-1) agonists, like Semaglutide, Trulicity, and Mounjaro, act on the same system. These directly attach to pancreatic cells, preparing them for a large insulin release when they detect high glucose levels. It is hoped that this can help the liver deal with high blood sugar without taking damage.
Sodium-glucose cotransporter-2 (SGLT2) inhibitors deal with blood sugar by expelling it out of the body with urine.
The final target of potential NASH treatments is inflammation. NASH stands for nonalcoholic steatohepatitis, which literally means “non-alcoholic inflammation of the liver (due to) fat.” Inflammation is like a visit with the inlaws: good when it doesn’t last too long. Researchers hope that reducing chronic inflammation may help limit the damage of NASH and prevent a worsening of the disease. Luckily, two avenues of treatment above also target inflammation.
One complication of the PNPLA3 genetic mutation is an increase in cyclophilin, a protein that can increase inflammation. By reducing excess cyclophilin through PNPLA3 management – or by targeting it directly, inflammation may be relieved. FGF21, which may be used to lower blood sugar, appears to lower inflammation in the pancreas. The hope is that these medical interventions may also help the liver downstream.
Overall, the liver is complex, and trying to keep it from being damaged is difficult.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Fatty liver disease is incredibly prevalent in the United States. Some estimates place the number of Americans with non-alcoholic fatty liver at over 30%, that’s around 100 million people in this country! Liver diseases are deadly serious; the liver is a critical organ and without it we cannot survive. The biggest problem with all liver diseases is that they frequently progress without symptoms. Because of this, the disease may progress to a dangerous or irreversible stage before it is even detected. Clearly, early, and routine testing for people at risk is critical.
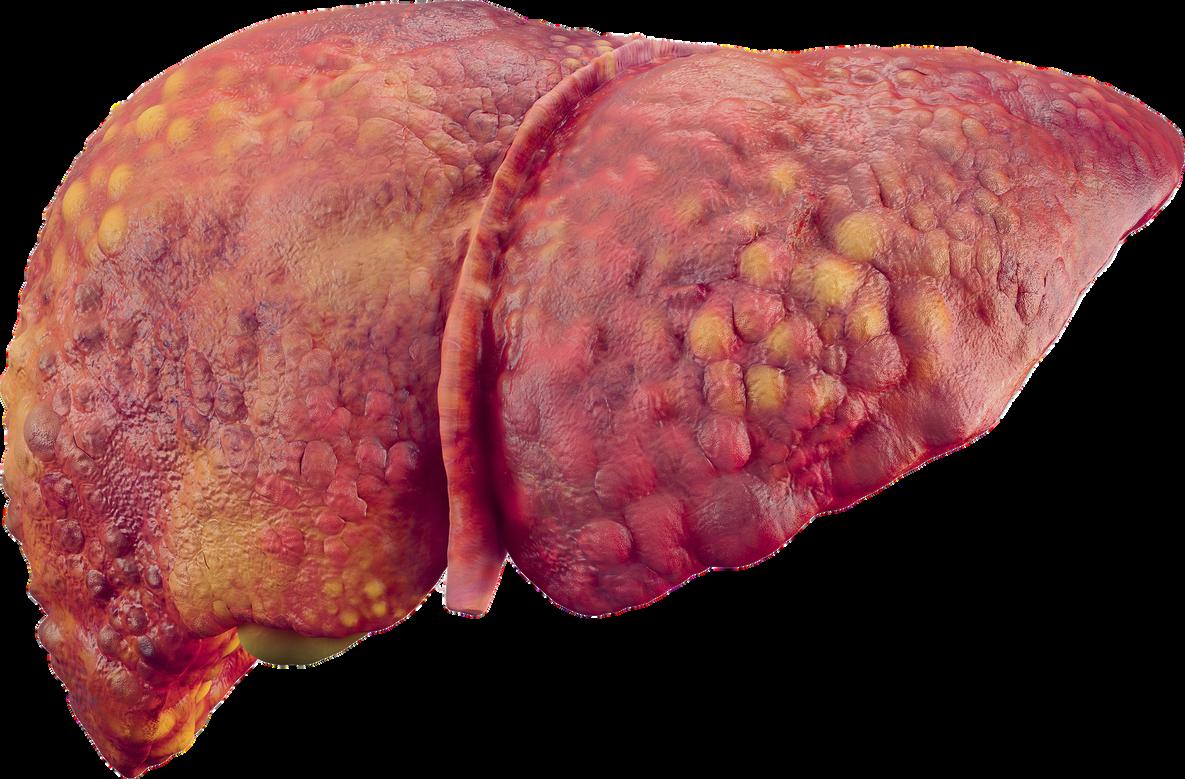
Healthy liver TheSpectrumofNAFLD
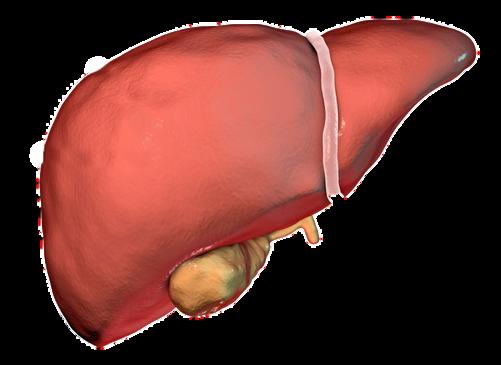
Fattyliver (Simplefat accumulation)
NASH (Non-Alcoholic steatohepatitis)

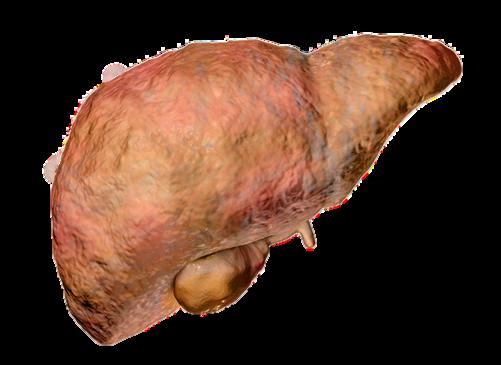
Cirrhosis (Scar-tissue)

We can’t see the liver from the outside, so the only way to learn about how it is doing is by looking at it. We can look through the skin using technology or under a microscope using a biopsy.
A biopsy – looking at a section of the liver under the microscope – is the “gold standard” of liver diagnostic techniques. This has drawbacks, however. Patients typically need to dedicate half a day to the procedure, and there can be rare complications. A biopsy is an invasive procedure requiring a piece of the liver to be taken and examined. It is a critical piece of the liver diagnosis pie but is not a routine procedure to be done without cause.
Imagining techniques can be very effective in diagnosing a fatty liver. Some techniques, such as a CAT scan and ultrasound, can’t diagnose the amount of scarring on the liver but can give an indication that there is fat present. CAT scans use x-rays, but imaging is otherwise safe. An ultrasound is fast and non-invasive. It is an excellent first step that many doctors use when they suspect a fatty liver. Magnetic Resonance Imaging (MRI) is the next best diagnostic procedure to a liver biopsy. With an MRI, doctors can clearly see the state of the liver. They are expensive, however. This again means they are an excellent tool for those who are known to have fatty liver but may not be an option for all patients to use regularly. eversible rreversible eversible

Ultrasonic elastography is a different technique. It is commonly called Fibroscan, after the manufacturer of the diagnostic tool. Fibroscan uses sound waves to gently shake the liver and measure how it responds. The liver will stretch slightly. In a healthy liver, the tissue stretches more, but hard scar tissue is less elastic. The fibroscan can interpret the difference and determine how much fat and scar tissue is present. The test is very similar to an ultrasound; it is painless, fast, and safe. The fibroscan does not replace other imaging techniques but is cheap and effective at determining the stage of fatty liver present. Unlike other techniques, a Fibroscan can be done routinely for anyone who is at risk of having fatty liver.
Fibroscans are very popular around the world, including in Europe, Asia, South America, and Canada. It is a cheap procedure with little reimbursement for practitioners, which unfortunately prevents widespread use in the USA. Risk factors for non-alcoholic fatty liver include being overweight or obese, being prediabetic or having diabetes, and eating a highfat diet. If you are concerned about fatty liver, talk to your primary care physician and/or contact ENCORE Research Group for a complimentary Fibroscan.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Medical terminology can be hard to understand. Much of it is in Latin, some is in Greek, several words are named after people, and terminology can change. Sometimes that change is a good thing, though. In June 2023, a collaboration of hundreds of experts in liver disease released new names for the liver diseases previously known as Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH).
Alcohol-Associated Liver Disease (ALD) Metabolic Dysfunction Associated Steatotic Liver Disease (MASLD)
Progresses to Metabolic Dysfunctionassociated Steatohepatitis (MASH)
Metabolic AlcoholAssociated Liver Disease (MetALD)
Other Liver Diseases
Females 20-50g/day or 140-350g/week
Males 30-60g/day or 210/420g/week
"Standard" drinks, such as 1 regular beer or 5 oz of wine, contain ~14g alcohol
Under the broad category of Steatotic Liver Disease (SLD) we now have Metabolic dysfunction Associated Steatotic Liver Disease (MASLD), which can progress to Metabolic Dysfunction-Associated Steatohepatitis (MASH) and Metabolic Alcohol-associated Liver Disease (MetALD, which is MASLD and increased alcohol intake). This change was made for many reasons. The terms “non-alcoholic” and “fatty” may have been confusing, stigmatizing, or inaccurate. People who are not overweight may still have the disease, and those with the disease may still be consuming alcohol. Finally, naming a disease after what it isn’t (“nonalcoholic…”) is less than ideal.
The new system describes the same symptoms but with more specific language. Steatosis is the accumulation of fat inside of cells, and the disease is caused by changes in the metabolic system, how our cells change food into energy. A critical change has also been made with the adoption of the new term MetALD. MetALD describes people who have MASLD but who still consume some alcohol. Alcohol affects the disease progression, but metabolic disruptions do as well. Hence, a term was developed to describe this overlap.
An international group of clinical researchers, scientists, educators, industry experts, and patient advocates planned and adopted these terms. The American Association for the Study of Liver Disease (AASLD), European Association for the Study of the Liver (EASL), Asian Pacific Association for the Study of the Liver (APASL), and Asociación Latinoamericana para el Estudio del Hígado (ALEH) made up most of the participants and have ensured widespread adoption of the new terminology.
Staff Writer / Editor Benton Lowey-Ball, BS, BFAGallbladder
Right Lobe Left Lobe Falciform LigamentNASH Gets Renamed MASH
Rinella ... & NAFLD Nomenclature consensus group. (2023). A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Annals of Hepatology.
New Liver Meds Take New Approaches
Fisher, & Maratos-Flier, (2016). Understanding the physiology of FGF21. Annual review of physiology, Geng & Xu, (2020) The therapeutic potential of FGF21 in metabolic diseases: from bench to clinic Nature Reviews Endocrinology.
Prasad, (2019). Biochemistry and molecular biology of mechanisms of action of fibrates–an overview. International Journal of Biochemistry Research & Review
Shen… & Huang, (2015). The rs738409 (I148M) variant of the PNPLA3 gene and cirrhosis: a meta-analysis. Journal of lipid research.
Sinha & Yen, (2019) Nonalcoholic fatty liver disease and hypercholesterolemia: roles of thyroid hormones, metabolites, and agonists. Thyroid.
Ure… & Foster, (2020). Cyclophilin inhibition as a potential treatment for nonalcoholic steatohepatitis (NASH). Expert opinion on investigational drugs
US Department of Health and Human Services, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Diseases. (April, 2021). Definition & facts of NAFLD & NASH.
Wang, & Heitman, (2005) The cyclophilins Genome biology
Why You Should Consider Getting a Fibroscan
Afdhal, (2012) Fibroscan (transient elastography) for the measurement of liver fibrosis Gastroenterology & hepatology
Koren, (Host). (2022, July 20). Common fibroscan technology questions [Audio podcast episode]. In Medevidence! Truth behind the data ENCORE Research Group
Koren, (Host) (2022, July 13) You cannot live without your liver [Audio podcast episode] In Medevidence! Truth behind the data. ENCORE Research Group.
What Can You Do About NASH Today?
American Liver Foundation. (March 16, 2023). What are the treatments for NAFLD and NASH? NASH Treatment
Van der Windt & Huang, (2018) The effects of physical exercise on fatty liver disease Gene Expression
The Journal of Liver Research.
Younossi & Lim, (2021) AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: expert review Gastroenterology
How Do We Get NASH?
Noureddin, & Sanyal, (2018) Pathogenesis of NASH: the impact of multiple pathways Current Hepatology Reports.
Parthasarathy & Malhi, (2020) Pathogenesis of nonalcoholic steatohepatitis: an overview Hepatology communications
Pierantonelli, & Svegliati-Baroni, (2019). Nonalcoholic fatty liver disease: basic pathogenetic mechanisms in the progression from NAFLD to NASH Transplantation
Pramfalk & Parini, (2011) Role of thyroid receptor β in lipid metabolism Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease.
The Liver: Our Unsung Hero and Guardian of Life
Eng, & Friedman, (2000). Fibrogenesis I. New insights into hepatic stellate cell activation: the simple becomes complex American Journal of Physiology-Gastrointestinal and Liver Physiology
Geerts, (2001) History, heterogeneity, developmental biology, and functions of quiescent hepatic stellate cells. In Seminars in liver disease.
Kalra & Tuma, (2018) Physiology, liver
Lautt ,(2009) Hepatic Circulation: Physiology and Pathophysiology Chapter 2, Overview
Ozougwu, (2017). Physiology of the liver. International Journal of Research in Pharmacy and Biosciences, Vaja, & Rana, (2020) Drugs and the liver Anaesthesia & Intensive Care Medicine
Yin & Stainier, (2013) Hepatic stellate cells in liver development, regeneration, and cancer The Journal of clinical investigation.
Battle of the abbreviations: NAFLD, NASH, Cirrhosis (not an abbreviation)
Pierantonelli, & Svegliati-Baroni, (2019). Nonalcoholic fatty liver disease: basic pathogenetic mechanisms in the progression from NAFLD to NASH Transplantation
Sanyal, (2019) Past, present and future perspectives in nonalcoholic fatty liver disease Nature reviews Gastroenterology & hepatology.

BIOPSY
DIET
CIRRHOSIS
EXERCISE
FIBROSCAN
FIBROSIS
HEPATITIS
INFLAMMATION
LIPID LIVER
MASH METABOL NASH
STEATOSIS
SUGAR