SUMMER 2023 | VOL. 2
THE EMPRESS PULSE
QUARTERLY REVIEW OF ALL THINGS EMRESS EMS
EMPRESS EMS NEWS INSIDE UPDATES ON THE COMPANY & MORE

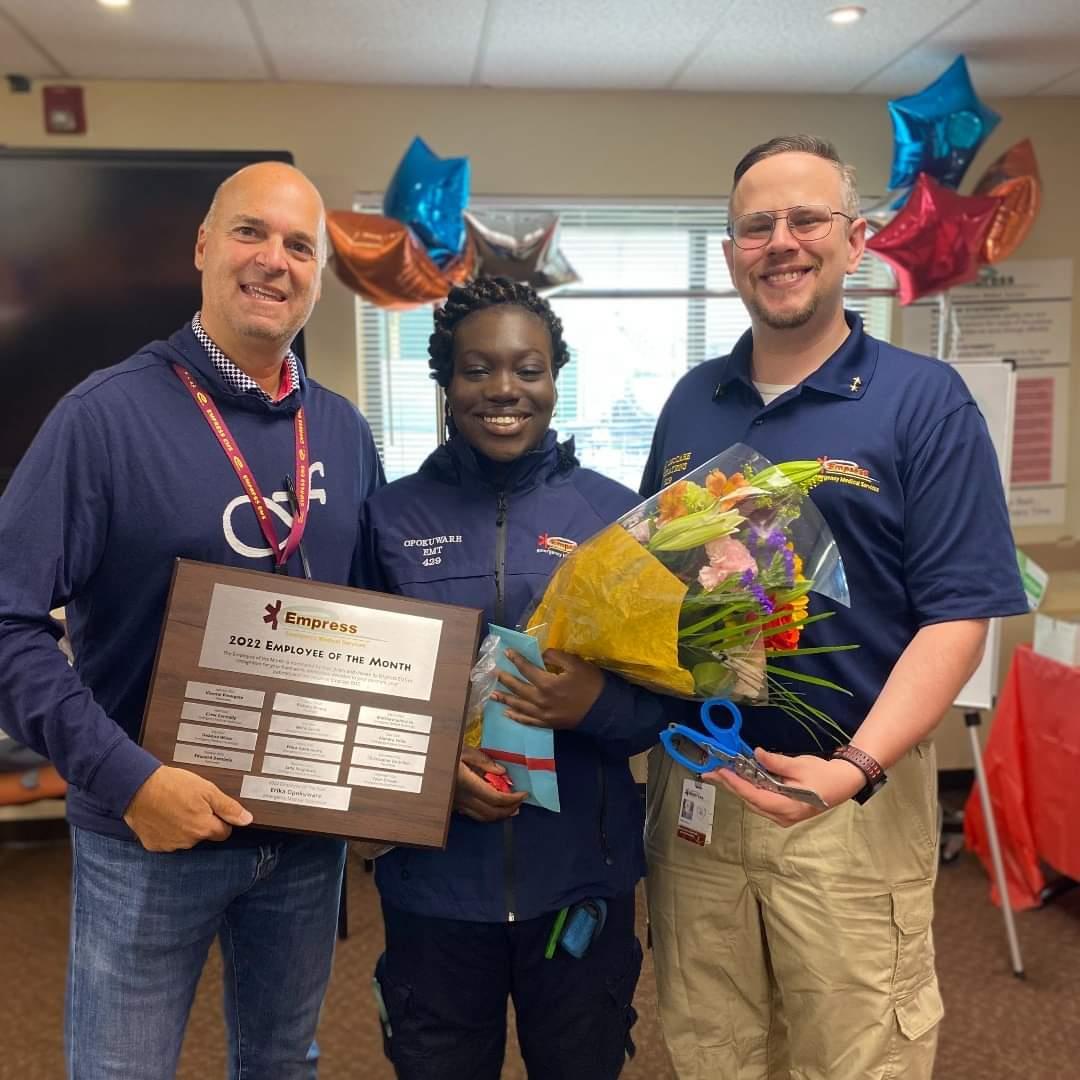
Hello again everyone and welcome to the 2nd issue of the Empress Pulse. We continue to figure out the best way to publish each issue. We have news including the announcement of last years employee of the year Erika Opokuware! There are updates on new equipment coming and more interesting call audits. We have more people joining the Pulse team with different areas of expertise. Please feel free to contact me with ideas for upcoming issues.
TO BE PART OF THE NEXT ISSUE CONTACT: PAUL MELLAMPHY

Meet the 2022 Empress Employee of the Year, Erika Opokuware. Although young, she is always ready to learn new things and face various challenges that the 911 system throws at her. At the end of each tour, she would go over her protocols and ask for feedback from the road supervisors she has had the pleasure to work with on the road when given the opportunity. Only working at Empress for almost two years, she stated that what drove her to become an EMT and serve her community she loved as a local resident of Yonkers all started back when she was In the 11th grade. She took an EMS class that showed her how to be a first responder. She also attended an AFTER-SCHOOL program associated with Empress known as the “Phoenix Cadets” and from there her interest and overall fascination grew for EMS. Once a surreal dream for her, has now become a reality when she decided to put on her navy-blue Empress uniform everyday dedicated to serving others. When asked what her overall experience with patients has been like working in EMS, Erika would go on to say “It’s a natural instinct for me...when it comes to helping individuals in distress, I put my patients first above everything else!” Not only is she service-oriented, but she also has been a mentor to her fellow partners, especially her former A22 partner on Thursdays, EMT Matthew Jones, who has learned what it truly means to be an EMT from following in her footsteps. To add, when she is not on the clock, she attends City College and is further pursuing a career in helping others as a psychology major. Furthermore, if there’s one word to sum up EMT Opokuware, it would be an “inspiration” for all future first Responders to emulate.
WRITTEN BY EMT MATTHEW JONES June 25, 2023
EMPLOYEES OF THE MONTH TO DATE 2023.
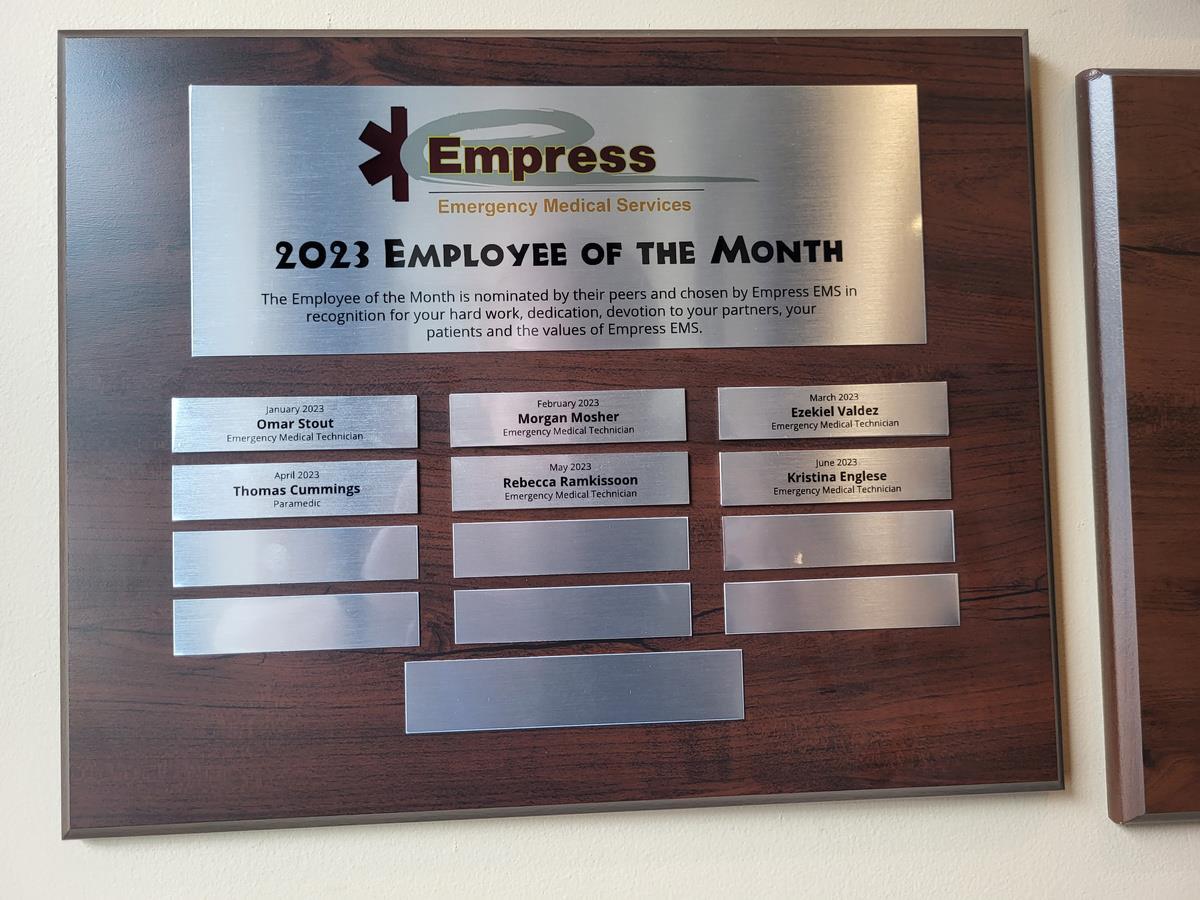


As you enter the visitor area in post 7 you'll notice on the wall the plaques celebrating our employees of the month. The employee of the month is rewarded with a choice of stethoscope or Raptor shears, and a $100 gift card, and a pass to park at post 7 for the month!


The Employee of the Month is Nominated by you! Please be sure to submit a commendation for any of your coworkers that you believe are deserve it! Lt. Jamiel Cunningham is the officer in charge of the program, but he can’t do it without your help!
LIFE SAVERS AWARD
ON MAY 23RD WE GOT TO CELEBRATE 52 LIVES SAVED FROM LAST YEAR. BELOW IS A LIST OF THE PERSONEL WHO RECIEVED RECOGNITION OF THE LIFE SAVES FROM EMPRESS CREWS. SOME EVEN GOT MULTIPLE LIFE SAVE AWARDS!



YARITZA ABREU, JANET MARTINEZ X 2, JOSEPH ADELFIO-RIVERA, PAUL MELLAMPHY, CHRISTINA AYALA, GISELLE NOGUERIA, SOSHANA BONNICK, TIFFANY NUNEZ, MICHAEL BROWN, X 2 SEAN O'BRIEN, WINSTON BOGLE, THOMAS ORPIKOWSKI, CHRISTOPHER CASEY, TYSHAWN PAYNE, MICHAEL CERIANI, X 2 JOEL PEGUERO, ROBERT CONDON, CHRIS RAMIREZ-APPUZZO, JENNIFER COUTSOURAKIS, CHRISTOPHER REDDICK, JAMIEL CUNNINGHAM, NATALIE RIVERA, EDOUARD DEMBELE,PATRICIA RODRIGUEZ X 4, PALMIRO ECHEVARRIA X 2, ANGELO RONDON, BRIAN FLEMING, SAMJO SAMSON, MICHAEL FRUHLING, MICHAEL SETIABUDI, FAITH GUEVARA, KEYANI SINGLETARY, ANDREA HOPE, ARI SHAPS, ALEX HORVATH, MEGAN SLATTERY, JOHN JUAVINETT, NEYLA SOTO, DESMOND KOOMSON, DANIELLE TARDIO, PRISCILLA LAMPEL, ALEX VEGA, ROBERT LOCKWOOD, GENNER VILLON, STEPHANIE LOOR.
TOTAL 52 SAVES


Cortlandt call audit

On Tuesday May 23rd there was a triple call audit which primarily focused on trauma calls. There were interesting cases with many lessons learned. As expected, we had good food, an open bar and music. Representatives from Boundtree, Zoll, Intersurgical, and Medline show cased what they have coming to EMS providers. Most importantly we got to meet up outside of the workplace. I know I'll be marking my calendar for the next one!









EMS week came and went with not too much rain, which meant 302 got behind the grill at Post 7 to everybody's delight!
EMT Joel Peguero started his shift with bagels & coffee, while SSC Carletta Bethea and the dispatch team ensured those working the road got to enjoy.
COMING TO A BUS NEAR YOU

We are awaiting the arrival of many updates. These include new Stryker power stretchers which will replace all of the manual stretchers we have right now. The IGEL supraglottic airway devices will be replacing the King LT, and EMT's will be using them as soon as it is included into the protocol. TXA will be part of our medication kit very soon and we are all aware of the updates with the new PCR system. Issues are all being weeded out everyday. Make sure you inform the PCR group of the issues you encounter to make it better for all of us.



INFORMATIONS FROM THE DC'S OFFICE
The PCR Program Update Is Finally Here!
Hello Team, we are aware of a lot of the recurring issues and difficulties historically with the PCR program. I am happy to announce that after a lot of work behind the scenes, we have launched our upgraded software! Here is a brief list of some of the changes that have occurred. Some you may have noticed already:
Updated UI - TabletPCR will have a new color scheme, with improvements to the fonts and text sizes to give a more user-friendly experience.
Sortable Inbox - When at the inbox screen, you will be able to sort your open charts by any field displayed.
Quick-Fill Templates - Tired of clicking all those check boxes for cancelled calls? We can help! As of this writing, Quick-Fill templates for cancels and standby charts have been made available. To use, simply open the dispatch copy, and click “Quick Fill” at the bottom, and select which template you want to use.
Driver's license/ID scanning - To make getting patient information easier, you will be able to scan the barcode on any state ID to populate the fields on your PCR. This feature should be live soon!
Medical Device Uploads - You will soon be able to upload your ECG monitor file to "the cloud", which is expected to make data uploads much easier and faster. More to come soon!
Vitals Fields - You will now be able to select multiple vital sign sets at once to quickly delete entries you don't need.
Blood Glucose Level - You will be able to select "High" or "Low" if that is the value you got when checking a BGL.
Search Fields - Have you ever tried to enter a piece of information, but you can't find the right field? Now you can just search for it!
Camera Integration - You will be able to upload pictures directly to the PCR. Want to show the accident scene to provide context for the receiving MD? Now you can, using the built-in camera on the tablet!
Resource optimization and stability improvements - With the new software, we expect to see a dramatic improvement in tablet and server performance once everything gets situated
With the updates to our hardware and software, we have updated to the most current NYS reporting protocol, NEMSIS 3.5. While there are some new fields, and some repetitive ones, I am working with the State and Zoll to simplify the system as much as possible. We understand there will be a learning curve for you all as you adapt to the changes, and we ask that you be patient with us, since we are going to be learning right along with you. We did extensive testing to ensure everything works smoothly, but there have been some gremlins hiding along the way that we didn't catch. If you encounter any issues, please be sure to reach out to any supervisor, or the PCR task force at PCR@EmpressEMS.com.
Thank You All, DC Walt McCabe

Pedestrian struck
Medic 60 was dispatched for a pedestrian struck. The patient is a 60-year-old female who was found in the prone position in the middle of the street surrounded by police, fire department and a big crowd. The patient disembarked the bus and was crossing the street when a vehicle travelling in the wrong direction hit her. She has type 2 diabetes, is compliant with her Metformin and has no known allergies & denies blood thinner use. She appears to be in extreme pain and is Spanish speaking only. She complains of neck, back and full body pain. The patient is A&Ox4. She denies any loss of consciousness, chest pain, shortness of breath, headaches, dizziness, light-headedness, blurred vision, fevers, or any recent illnesses. Minimal blood was noted in the oral cavity with missing broken teeth, gum pushed back, multiple abrasions and road rash were noted to the patient’s extremities. Her BP and heart rate are within normal limits. BGL on scene is 324mg/dL. HEENT are normal, patient reports pain 10/10, skin is normal condition other than the road rash to extremities. Lung sounds are clear in all fields with regular respiratory effort. S-LAMS score is zero. There is tenderness in all 4 abdominal quadrants with no distension noted. There were no life-threatening injuries or deformities to the posterior after a cervical collar was fitted. A left ankle closed fracture was splinted and stabilized with soft splints. Circulation, sensory and motor functions are intact both before and after the fitting of splints.
Cervical spine precautions were observed, fire department assisted with head stabilization and a rapid trauma assessment was performed. The patient was transferred onto a scoop stretcher. For pain management, 5mg of Morphine was administered intramuscular There was minimal effect, so a second dose of 5mg was given intramuscular prior to IV access. IV access was then achieved on the right forearm with an 18 gauge and normal saline was administered up to 400ml. The patient’s SpO2 was found to be 8991% on room air, so she was placed on supplemental O2 via nasal cannula raising it to 98% with EtCo2 to be 35-38mmHg BLS crew arrived, and the patient was lifted onto the stretcher using the scoop. The patient was then transported ALS to Jacobi ER. Goood work Paramedic Patricia Rodriguez and EMT Ashley Scott.

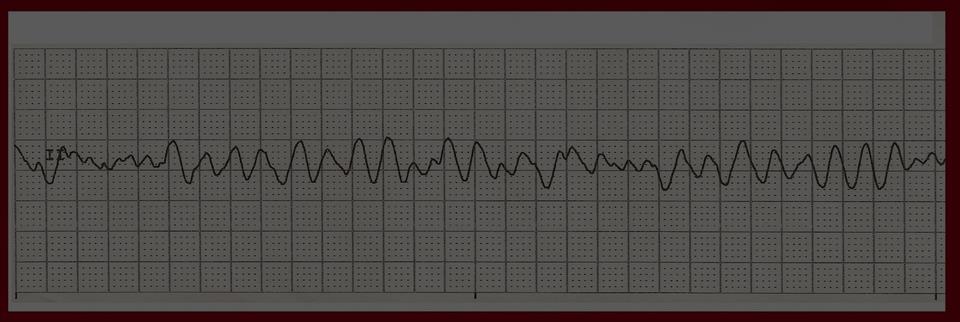
Cardiac arrest with ROSC MEGACODE!!
Medic 60 was dispatched to a cardiac arrest at a home with CPR in progress. The patient is a 69-year-old male with a medical history including CHF, anxiety, coronary artery disease, hypercholesteremia, and hypertension. He is compliant with his Albuterol, Finasteride, Sertraline, Atorvastatin, Klor-con, Torsemide, Valtrex, Metolazone, Xalatan, and Midodrine. His wife witnessed him go unconscious and initiated CPR. YPD and Lt Ceriani were already on scene prior to M60’s arrival. A defibrillation shock was administered when V-fib was seen on the monitor. The patient was intubated, and IV access was gained, using an 18 gauge to the left AC. The first dose of Epinephrine 1mg 1:10,000 was given. CPR was continued with the Lucas device and manual ventilations. The patient was shocked a total of 5 times! The patient received 300mg of Amiodarone, then another Epinephrine 1mg 1:10,000, then another 150mg of Amiodarone. At one stage the patient was found to be in torsades de pointes, so he received 2 grams of Magnesium. ROSC was achieved! A 12 lead EKG was obtained which showed a sinus tachycardia with ST depressions in leads V4, V5, & V6 with some occasional PVCs. The patient was extricated to the ambulance with the use of a Reeves. During the transport the patient was found to become bradycardic and hypotensive. 1mg of Atropine was administered with improvement in BP and heart rate. The patient was transported to Lawrence Hospital ER and handed over unresponsive, but with a pulse.
Paramedic Andres Rivera
EMT Anne-Marie Mancuso

Stabbing
Mount Vernon ambulance 1 was dispatched for a stabbing. The patient was found alert and orientated sitting on the sidewalk in the care of PD and FD. They had already bandaged the patient’s wounds. They had him stand up and walk to the ambulance without incident. He reports that stabbed multiple times before calling 911. The trauma assessment found a small knick-type puncture wound to the right lower flank/back which was not bleeding and did not require bandaging. He had 3 lacerations to the right wrist which were already bandaged by FD. There were two deep lacerations to the posterior upper left arm which were bandaged by EMS on arrival in the ambulance. There was a deep stab wound approximately 1 inch in length to the right chest. It was through his pectoral muscle, approximately mid clavicular in the third intercostal space. An occlusive dressing was applied to the wound by EMS. Lung sounds were clear in the left lung and diminished in the lower right lung but clear in the right apices. The patient denies falling, head injuries, or loss of consciousness. The patient was placed on a 3-lead monitor and found to have a sinus tachycardia. His EtCO2 reveals normal waveform with a value of 35mmHg. Transport was initiated without delay.
En route to the ER a 16 gauge IV was established in the right and left AC. Normal saline was hung and ran wide open into the left AC to treat traumatic injury en route. The patient complained of chest tightness. The pulse ox at the time was 94% with more diminished right sided lower lung sounds, so the occlusive dressing was burped on the one side to release air. Shortly after the patient coughed causing blood and air to release from the chest injury into the occlusive dressing. The dressing was replaced at that time to recreate seal and release blood.
The patient’s SpO2 increased to 100% after these events with increased right lower lung breath sounds. The patient’s vital signs remained stable throughout the remainder of the transport with no other acute changes in status. The bandages on the injuries to the arms had maintained control of bleeding without further need of intervention. A further detailed physical assessment did not reveal any other obvious injuries or complaints. The patient was handed over to Jacobi Hospital ER. Paramedic Alanna Badgley & EMT Jonathan Alviar

ROSC at the Casino
The casino unit was dispatched to a security booth for the unknown casino employee down. The patient is a 27-year-old male found supine on the ground surrounded by staff. The patient was unresponsive and seizing. Witnesses claim that he fell and hit his head on the floor. It is unknown if the patient had any complaints prior to the event. Midazolam was drawn up, but the patient stopped seizing. The patient started to have agonal respirations and his skin was pale, cool, diaphoretic, and he had a strong alcohol-like odor. Manual ventilations were initiated with a BVM. The patient was placed on four lead monitor and found to be in ventricular fibrillation, so CPR was started. A defibrillation shock was delivered. The patient was found to be in pulseless electrical activity (PEA). An IO was placed in the left tibial plateau. The first Epinephrine 1:10,000 was given along with a fluid bolus. Lt Ceriani & Lt Tardio arrived and assisted. The patient was intubated with a 7.0mm endotracheal tube. It was confirmed correctly placed 22cm at the lips with an EtCO2 of 13mmHg, equal breath sounds in the lungs and negative bowel sounds. The BGL on scene was 127mg/dL. HEENT are normal, pupils are sluggish, +CTC pale/cool/diaphoretic, inconclusive stroke scale. The second rhythm check revealed ventricular fibrillation. A second defibrillation shock was delivered and 300mg of Amiodarone was drawn up but not given as the IO access became dislodged. A second IO was placed in the right tibial plateau with a second dose of epinephrine administered and CPR continued. ROSC was achieved! CPR was stopped and the rhythm showed a sinus tachycardia in the 130s. The 12 lead was suspicious for hyperkalemia, and had ST depressions in inferior leads with an elevation in AvR. The patient began to bite the tube and was sedated with 10mg of Midazolam. Manual ventilation continued with the EtCO2 ranging between 15-36mmHg. The initial BP was 65/40 and rose to 142/90. SpO2 ranged from 88-96%. The patient’s medical history included seizures and ETOH/drug abuse. The patient was transported to Lawrence Hospital ED, and transferred to their care in critical condition.
Paramedic Patricia Rodriguez
EMT Kelby Martinez
EMT Christopher Pinnock

Shooting with cardiac arrest
Unit was dispatched for the possible gunshot victim. Upon arrival manual compression CPR was being performed on a 19-year-old male by Yonkers Police Department. They stated they he had been shot multiple times. YPD ESU arrived and placed the patient on the Lucas device. The patient’s EKG on combi pads revealed asystole. The patient’s airway was clear and an OPA was inserted while BVM ventilations were performed. Gunshot wounds were found superior to the right nipple with no exit wound which was sealed with an occlusive dressing. The left shoulder had entrance and exit wounds both sealed. The left buttock had two entrance wounds with no exit sealed. No other gunshot wounds or traumatic injuries were noted besides a bulge to the right hip that appeared to be a lodged projectile that did not pierce the skin. The pupils were fixed and dilated. The abdomen was non distended.

With the gunshot wounds addressed and CPR in progress, IO access was gained in the left tibial plateau and secured. Epinephrine 1mg 1:10,000 was pushed and a normal saline infusion was started wide open. The patient was intubated with a 7.0 endotracheal tube by direct laryngoscopy. The placement was confirmed by present lung sounds, absent epigastric sounds, EtCO2, and condensation in the tube. Pulse and rhythm checks showed the rhythm changing from asystole to a pulseless electrical activity. Scene time was expedited, and the patient was transported code 3 to St Joseph’s Hospital ER for traumatic arrest. The patient received a second Epinephrine and Sodium Bicarbonate 50mEq. There were no changes in the patient’s condition throughout the transport. Patient was handed over at the ER.
Paramedic Palmiro Echevarria
Paramedic Jazmin Garth
Lt Kristina Rella
OUTCOME
Unfortunately, resuscitation efforts were ceased in the ER and time of death was declared.
STEMI CALL
Mount Vernon Ambulance 1 was dispatched to a residence for a 52-year-old male feeling numbness. On arrival the patient was in front of his home. He sat onto the stretcher and was strapped on in the semi fowler’s position. He complained of stabbing chest pain, left sided neck, arm and leg numbness. The arm and leg numbness started 2 days ago and progressively got worse. The patient reports a medical history including diabetes, hypertension, and hyperlipidemia. He is compliant with his Lipitor, Metformin, Glipizide, and Amlodipine. The patient was brought to the ambulance and assessed. He is A&Ox4, airway is clear and self-maintained. His breathing is un-labored, lung sounds were clear with equal chest rise and fall. His skin is pink, warm and diaphoretic. His cap refill is normal, his radial pulses are strong and regular. His abdomen is soft and non-tender. His pupils had PEARRL. His S-LAMS is zero. His BP is 216/137, his heart rate is 72 sinus rhythm with 12 lead showing an acute ST elevation inferoapical infarct. (marked ST elevations in leads 2/aVF/3/V4-V6, & ST depressions in aVL/aVR). His chest pain was rated as 10/10, non-radiating and constant.
The patient was given 324mg of Aspirin orally. An 18 gauge IV was established in the right AC. He was then given 0.8mg of Nitroglycerin sublingually. Notification was given to Montefiore Moses Cath lab on departure of scene. The patient reported the pain decreasing from a 10 to an 8/10 and the BP improved to 120/96. A second dose of Nitroglycerin brought his pain to a 7/10. The patient was given 50mcg of Fentanyl IV push. The patient was monitored throughout the transport with no change in condition otherwise than reduced pain. The patient was handed over at Montefiore Moses ER and then taken to the coronary catheterization laboratory.
Paramedic Dan Kashtan
Paramedic Kim Jordan
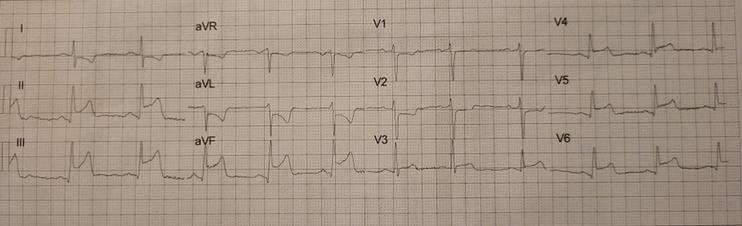
OUTCOME!!
The patient went for emergent coronary catheterization due to ST elevations. A 100% occlusion of the right coronary artery was discovered. The patient required a percutaneous coronary intervention. During the coronary stent placement, he had an episode of ventricular fibrillation requiring a defibrillation which resulted in a normal sinus rhythm. The stent was successfully placed. He spent 2 days in the coronary care unit and then was transferred to a telemetry unit in a stable condition. He was discharged home with medications and arranged cardiology follow up. A part of this positive outcome is thanks to the crew’s early notification, and appropriate pre-hospital care!


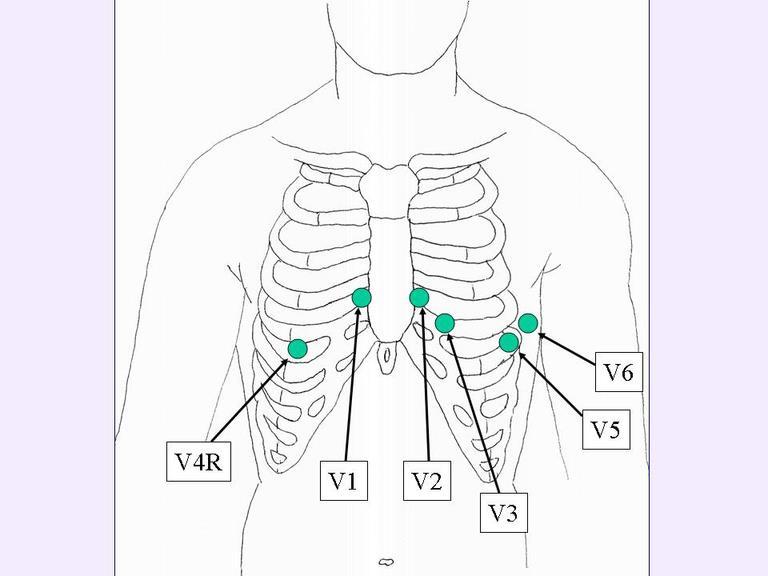
12 lead EKG placement
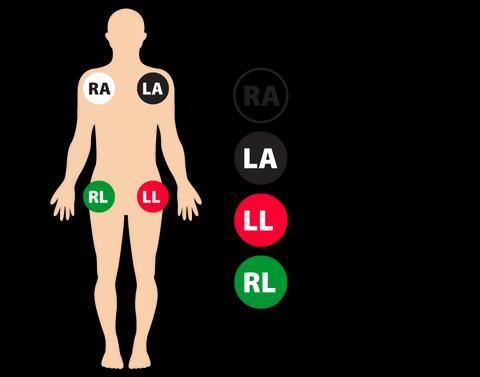
Curious about 12leads? Want to know where all the stickers go? The picture on the right will show you!
The picture includes “V4R”, which is used to visualize the right side of the heart in special circumstances.

FDA DRUG RISK CLASSIFICATION FOR
PREGNACY
We all studied drug risk classifications in medic or EMT school. Trying to recall our medications for the pregnant patient can be hard in the heat of the moment. Here is a list of the classifications of the medications that we carry on our kits at Empress.
PREGNANCY CATEGORY Description
A Appropriate human studies-no risk
B Insufficient human studies, but animal research suggests safety or animal studies show issues but human studies show safety
C Insufficient human studies, but animal studies show problems Or no animal studies, and insufficient human studies
D Human studies, with/without animal research shows fetal risks, but the drug is important to some women to treat their conditions
X Fetal risks are evident, there are no situations where the risk/benefit justifies use
- C
- Not assigned
– C

– C

ACROSS
3. DESCRIBES A COMBINATION OF EXHAUSTION, CYNICISM, AND REDUCED PERFORMANCE RESULTING FROM LONG-TERM JOB STRESS.
4. EMPRESS 2022 EMPLOYEE OF THE YEAR.
6. THE UNOFFICIAL COFFEE OF EMPRESS.
12. A FIELD OF STUDY THAT FOCUSES ON THE PHYSICAL STRUCTURE OF THE BODY AND ITS SYSTEMS.
14. THE MANNER IN WHICH PRINCIPLES OF ETHICS ARE INCORPORATED INTO PROFESSIONAL CONDUCT.
15. WHERE WE FIND OUR FAVORITE 14P.
17. THE DETERMINATION OF __________IS BASED ON DUTY, BREACH OF DUTY, DAMAGES AND CAUSATION.
18. DEPARTMENT RESPONSIBLE FOR CDI'S.
20. THE PROPER TERM FOR A BLOOD PRESSURE CUFF.
21. THE ADO OF FEW WORDS, AND MANY FACIAL EXPRESSIONS.
22. THE MOVEMENT OF AIR BETWEEN THE LUNGS AND THE ENVIRONMENT.
DOWN
1. Common Type II Diabetes medication.
2. questions can be answered in very short responses as in “Yes” or “No.” 5. is the unilateral termination of care by the EMT without the patient’s consent and without making any provisions for care to be continued by a medical professional who is competent to provide care for the patient.
7. The foundation of consent where a person can understand the information provided in order to make informed choices regarding medical care.
8. Examines the normal functions & activities of the body and its systems.
9. Better than OT.
10. Federal legislation passed in 1996. Its main effect in EMS is in limiting availability of patients' health care information and penalizing violations of patient privacy.
11. The new Jotform King.
13. The physician who authorizes or delegates to the EMT the authority to provide medical care in the field.
16. questions require some level of detail in the response by the patient.
19. A code of conduct that can be defined by society, religion, or a person, affecting character, conduct & conscience.

Peer Support Burnout..Is
it REAL?
Burnout can be difficult to describe. However, it’s not a medical condition. According to the APA Dictionary of Psychology, burnout is defined as “physical, emotional or mental exhaustion, accompanied by decreased motivation, lowered performance and negative attitudes towards oneself and others.”
Sometimes you may not realize that you’ve hit burnout until you’ve gone from “really tired” to “too exhausted to function.” As a person who is usually extremely busy, sometimes I don’t realize when I’m doing too much.
Burnout can happen during any stressful time in your life or even when your work life balance gets thrown off. As EMS providers, sometimes the double time is more tempting than a day off sleeping or with family and friends.
Signs of burnout include fatigue, decreased appetite, irritability and a multitude of other things.
Burnout looks different in everyone!
People experiencing burnout may have temporary feelings of sadness and hopelessness.
Fun fact: Burnout is NOT the same thing as depression.
Things to do to break the chain:
Take that extra day off.
Go to the gym or for a hike regularly.
Eat good… not McDonald’s at 3 AM when nothing else is open.
Talk to your family and friends…don’t bottle feelings in. Remember… you are NOT alone.
If you or someone you know is experiencing feelings of burnout, feel free to reach out to myself, any member of the supervisory team or the peer support group at Empress for guidance. This can be regarding a recent call/ traumatic experience you’ve been involved in or just to vent! It’s okay to not be okay!
Suicide and Crisis hotline: 988
Trevor Project (LGBTQ friendly): (866) 488-7386
-Kristina Rella
Local 20 IAEP With Alanna Badgley
June and July have been busy for our Local! We’ve added more than 200 new members and are representing EMS professionals in three more counties! A warm welcome to those of you who are joining us. Everyone please introduce yourselves to one another when you see each other and remember that we are all on one team and are stronger united than divided!

We are moving away from the Yonkers designation, and now have a new domain name to reflect our growing geography and growing membership. iaepyonkers.org will now redirect you to the new domain for one more year, before we retire it entirely. The website is now also new and improved, thanks to the hard work of our Secretary, Cecilia Korn. Please go check it out!
We now represent EMS providers in eight counties and take this responsibility seriously– it’s our job not only to ensure you are treated fairly at work but also to ensure that the laws and systems are working for you. As such, we will continue to lobby for improvements to the EMS systems here in New York and beyond.

Make EMS essential movement
In June, President Alanna Badgley met with Sarah Jessica Parker, who will be the new voice of the “Make EMS Essential Movement.” She expressed her full support and gratitude for all of us and necessary changes in our field and is going to be the narrator of the upcoming documentary film “Honorable But Broken: EMS In Crisis,” which features interviews with Local 20 members past and present, as well as Empress’ Vice President, Jim O’Connor. The film is set to premier in September and will go a long way to help our cause!



EVENTS:
July 24: Nominations are due for the Mobile Life Board Liaison position! This person will serve as a non-voting member of the board for a term of one year, to assist us in the transition and bring a direct voice of MLSS to our conversations and decision making. Please think of someone who will serve you well and nominate them!
July 27: President Badgley will attend Senator Kirsten Gillibrand’s First Responder Summit in Washington, DC. Please reach out to Alanna before then with any ideas or legislative asks for our senator!
September 23: Annual Local 20 Picnic (now also a Corn Hole Tournament) at Thomas Bull Memorial Park in Montgomery, NY. More details coming soon!
Driving Safety tips
• Seat belts - seat belts are to be worn by everyone in the vehicle while it is in motion, this applies to staff/patients and family members both in the front and rear of the vehicle.
• Following distance - the camera system (Samsara) is set up to alert the operator when following distance is less than 1 second. Please keep this in mind when driving behind other vehicles and adjust your following distance accordingly. A good rule of thumb is to keep three lines of separation between you and the vehicle in front of you.
• Rolling stops - reminder that you are required to come to a full and complete stop at all stop signs and red lights. This applies to all vehicles at all times regardless of whether or not you are going code 3.
• Harsh braking - the best way to avoid this is to pay attention to the road ahead of you and limit distractions in the cab. There should be no reason why the operator of the vehicle is holding a phone and using as a map, either utilize EMS loop on the installed iPad (where applicable) or have your partner direct you to the call.
• Speeding - be aware of posted speed limit and do not exceed that unless operating in an emergency mode. You are only allowed to exceed the posted speed limit by 10MPH in an emergency and only if safe to do so.
• Backing up - use a spotter whenever possible, this applies whenever you are backing up, not just in the lot.
• Driving forward - do not try to squeeze through tight spaces with the ambulance.
• Maintain situational awareness at all times when operating an emergency vehicle.
Thank you and keep up the great work, be safe out there.
Quote of the day: In every day, there are 1,440 minutes. That means we have 1,440 daily opportunities to make a positive impact. - Les Brown

So that wraps up the Summer issue of The Empress Pulse. I apologize for the delay in getting this issue out. As I said we are still figuring it out. What I do ask is if anybody can help in any way please reach out. I am looking for great pictures to share and your stories. If you have had an interesting call, please let me know and I will see if we can feature it in the call audits. I am hoping to add a section with life hacks like using hydrogen peroxide to get rid of blood stains from your uniform (game changer)!!

Congratulations again to our employee of the year Erika and to the employees of the month. We look forward many more life saver awards again next year. Keep up the great work everyone. I’m very proud to work with you all. Be safe out there!
Lt Paul Mellamphy 316

