NURSING



The demand for nurses continues to grow, and the Nell Hodgson Woodruff School of Nursing has responded to the challenge – growing from fewer than 500 students in 2011 to almost 1,300 in 2022.


Critical to supporting this increasing enrollment is financial aid, which provides greater access to nursing education. Over 1,500 scholarships are awarded annually to over 900 students across the School of Nursing.
These need- and merit-based scholarships ensure we attract and retain the best and brightest students while providing increased access to a world-class education, particularly among underrepresented students and working nurses pursuing advanced degrees.
information
nursing.emory.edu/alumni-and-giving
Alumni Engagement
With your support, we will continue to attract students who will become visionary nurse leaders and shape the future of nursing – providing the best in care along the way.
time of year. New students are acclimating to classes and clinical rotations, and some students are looking forward to their December graduation. This year, these emotions rose to great heights as we celebrated the opening of the Emory Nursing Learning Center in downtown Decatur, marking a new era for our school.
The opening of the Emory Nursing Learning Center is the culmination of three years of dreaming and planning to prepare students and nursing professionals to face the challenges of addressing the critical nationwide nursing shortage.


Our center provides 70,000 square feet of additional state-of-the-art space to accommodate our remarkable growth in student enrollment, research, and education programs. By expanding our footprint to Decatur, students have easy access to simulation, clinical skills, and continuing education in one location.
When planning for the center began, we asked faculty, staff, students, alumni, Emory Healthcare nurses, and Emory leaders what was most important to them. It was agreed the center should immerse students fully in caring for patients across the lifespan in hospital, ambulatory, and home health settings. As a result, the Emory Nursing Learning Center is the largest facility of its kind in Georgia.
The center’s crown jewel is our state-of-the-art simulation and clinical skills labs, where we can accommodate over 50 different patient care scenarios at a time. The center also features flexible classroom spaces, in-person and remote learning capabilities, and an Innovation Hub for nurturing new ideas in patient care. It also houses the Emory Nursing Experience, our professional development partnership with Emory Healthcare Nursing.
Just days before the ribbon-cutting celebration for the Emory Nursing Learning Center, our bachelor’s degree program was ranked No. 2 in the nation by U.S. News and World Report, rising from last year’s No. 4 ranking and joining our master’s degree programs in the No. 2 position. Initiatives like the Emory Nursing Learning Center and our commitment to preparing visionary nurse leaders have propelled us to this top ranking.
With this issue, we invite you to share in our excitement and join us in celebrating the results of our dedication to our students and our Emory School of Nursing community.
Linda A. McCauley, 79MN, PhD, RN, FAAN, FRCN Professor and Dean Nell Hodgson Woodruff School of NursingDean, Nell Hodgson
A.
79MN,
Chief Engagement Officer
Tricia Benson, 86MN
Senior Director of Communications and Marketing
Melanie Kieve
Director of Communications and Marketing Lauren Powers
Managing Editor Pam Auchmutey
Art and Creative Director Erica Endicott
Director of Photography Kay Hinton
Director of Digital Media Stephen Nowland
Editorial Contributors
Jim Auchmutey Patty Gregory Michelle Hiskey
Kristin Baird Rattini Chelsea Shackleford
Photography Contributors Jim and Pam Auchmutey Stella Clarke-Dubose Javier De Jesus
Erica Endicott
Full Tilt Consulting
Jonathan Hillyer
Jack Kearse
Ann Watson
Production Manager Stuart Turner
Executive Director, Communications and Marketing
Tionna Carthon
Executive Director of Content Jennifer Checkner
Associate Vice President, Health Sciences Communications Nikki Bartholomew Troxclair
Emory Nursing is published by the Nell Hodgson
School of Nursing (nursing.emory.edu), a component of the Woodruff Health Sciences Center of Emory University. ©2022


Emory University is an equal opportunity/ affirmative action employer fully committed to achieving a diverse workforce and complies with all federal and Georgia state laws, regulations, and executive orders regarding nondiscrimination and affirmative action.
Emory University does not discriminate on the basis of race, age, color, religion,
origin
status,
ancestry, gender,



Some years back, it was clear that the Nell Hodgson Woodruff School of Nursing had outgrown the building at 1520 Clifton Road. There were so many students, one faculty member joked, they were stacked to the ceiling.
It was a healthy problem to have, a sign of the school’s record growth in enrollment, degree programs, and research funding.
Along with success came greater national visibility. Emory has placed among the top nursing schools ranked by U.S. News & World Report since 2017 and the National Institutes of Health since 2015. Greater visibility brought more students, now almost triple the number in 2012.
“We had become one of the top-ranked nursing schools in the nation,” says Dean Linda McCauley, PhD, RN, FAAN, FRCN. “Yet we had inadequate space for enrollment. We could all feel it.”
To ease the crunch, the school leased space at Emory University Hospital at Wesley Woods (for graduate-level simulation), the Executive Park office complex (for con tinuing nursing education), and Emory School of Medicine (for DNP nurse anesthesia simulation). The arrangement had its downside. “When you operate at multiple sites, it affects your sense of community,” says McCauley.
Emory and Decatur officials prepare to cut the ribbon to open the Emory Nursing Learning Center. They include (L-R) Kelly Walsh (Decatur), Ravi Bellamkonda (Emory), John Rice (Emory), Sharon Pappas (Emory Healthcare), Linda McCauley (School of Nursing), Jadaria Thomas (School of Nursing), Greg Fenves (Emory), David Stephens (Emory), and Frankie Atwater (DeKalb Chamber).

She faced a dilemma: How do you build a state-ofthe-art facility to better educate nursing students and practicing nurses, all in one place?
Remaining at 1520 Clifton Road was a given. The four-level building, open since 2001, would still house administrative, faculty, program, and research offices. But there was no room to expand on or next to the site.
For some time, McCauley and Sharon Pappas, PhD, RN, NEA-BC, FAAN, chief nurse executive for Emory Healthcare, had dreamed of a new interprofessional education building with simulation, clinical skills, and classroom space for nursing, medical, and physical therapy students. The idea had its proponents but never gained the traction needed to move forward. McCauley then looked to renovate existing space somewhere on the Emory campus, but the buildings she considered were either too small or slated for use by other schools and units. So she went back to school.
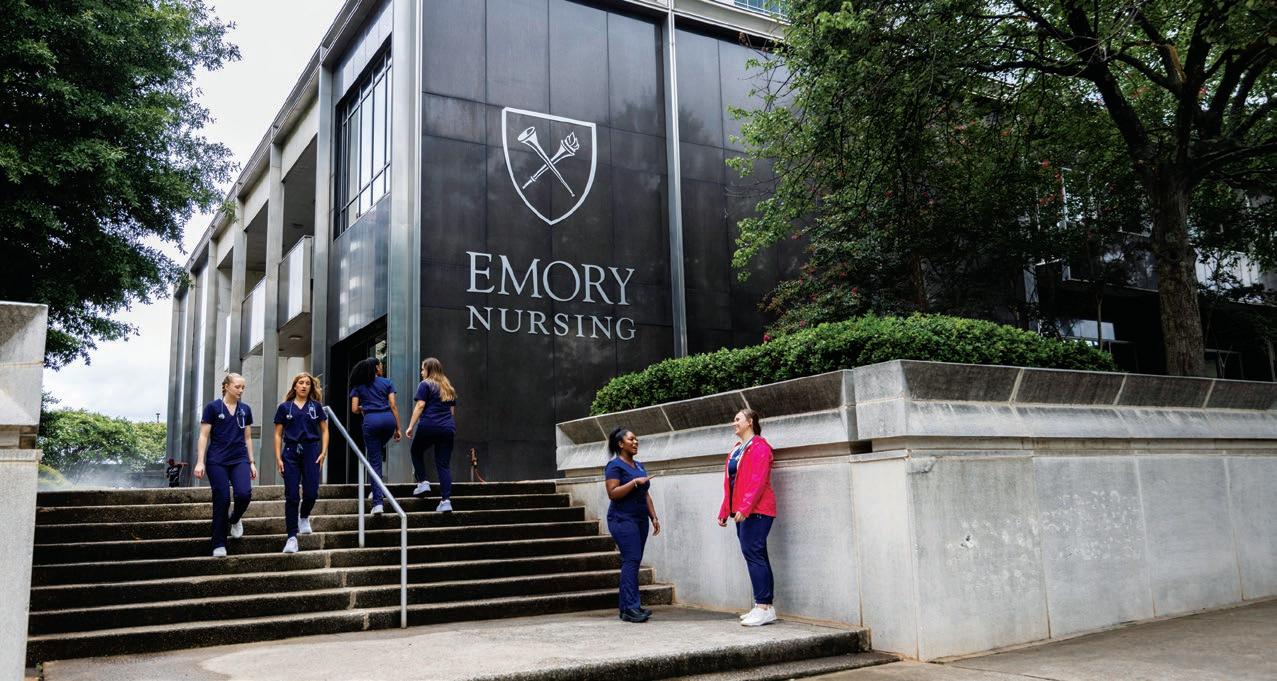
THE EMORY NURSING LEARNING CENTER IN DECATUR EXPANDS THE FOOTPRINT OF A SCHOOL SHAPED BY RECORD GROWTH AND THE DEAN WHO MADE IT HAPPEN
The lobby of the Emory Nursing Learning Center, known as the student commons, is an open, light-filled space intended to make everyone who enters feel welcome.

“I began educating myself about how to get a build ing by drawing more attention to the growth of the school,” McCauley says. “People would say to me, ‘When are you going to stop growing?’ I would tell them, ‘When are people going to stop needing more nurses?’ Then the COVID-19 pandemic showed us why. The School of Nursing now prepares more nurses than any other school in the state of Georgia.”
It also had the resources to invest in the school’s expansion. “We’re able to use our income to invest in the infrastructure that students need for the quality education they’re paying for,” she adds.
McCauley formed a team to explore purchase and leasing options around Atlanta. They looked at several properties, but nothing clicked until they toured 250 East Ponce, an eight-story office building in Decatur, a short drive or bus ride from Emory. Four lower floors were coming up for lease when team members toured the space.
“It was a wreck,” says McCauley of the basement, or terrace level, which still had the original 1962 bank vault. But the terrace, first, second, and fourth floors had plenty of room. In her mind’s eye, McCauley could see a spacious state-of the-art simulation lab for students of all levels, classroom and study space, and an inviting lobby. Students could walk to Decatur restaurants, shops, a hotel, and a rapid rail station nearby.
Less than three years later, the Emory Nursing Learning Center is now open for business. The $20.6 million, 70,000-square-foot center includes high-tech simulation and skills labs, where students learn to care for patients of all ages in hospital, clinic, and home apartment settings. It also offers classrooms, study spaces, a student lounge, faculty touchdown space, a telehealth office, and the Innovation Hub, where students and faculty can develop and test ideas to improve patient care and nursing workflow systems.
In July 2021, the Emory Nursing Experience, the professional development partnership between the School of Nursing and Emory Healthcare Nursing, moved from Executive Park to the fourth floor of the learning center.

Outside, at the top of 250 East Ponce, “Emory Nursing” stands out in large blue letters. The signage reflects the ties the School of Nursing and Emory Healthcare Nursing share around education, clinical practice, and research.
Pappas and other Emory Healthcare nurses helped conceive the design and build-out of simulation and other spaces at the learning center. Currently, she is looking to fill 1,000 nursing positions across the
Emory Healthcare system. Many were held by nurses who were impacted by the COVID-19 pandemic. The learning center can provide students with the clinical and leadership skills that Pappas and her staff look for when hiring nurses to fill those vacancies.
“Simulation reinforces what students learn in the classroom,” she says. “It’s about the experience but also the debriefing and discussion afterward about what they learn. All those things work together to prepare nurses who connect well with patients and their team. Emory Healthcare is the nursing school’s biggest employer. Those are the kind of nurses we need.”
Recently, Emory Clinic became the fifth Emory Healthcare entity to achieve Magnet status, the national gold standard for nursing excellence. One requirement for designation is that nurses have opportunities to learn and grow professionally. The Emory Nursing Experience makes professional
People would say to me, ‘When are you going to stop growing?’ I would tell them, ‘When are people going to stop needing more nurses?’




The Emory Nursing Learning Center comes to life with a dual history. It expands the footprint of the Nell Hodgson Woodruff School of Nursing, founded in 1905 as a small training program in Atlanta.
The learning center occupies four floors at 250 East Ponce, an eightlevel office building constructed in 1962 in Decatur. Four different banks operated branches there until the School of Nursing began renovations for the learning center in 2020.
Transforming space in a 60-yearold building to create what is
now one of the largest nursing simulation centers in Georgia was an exercise in collaboration and creative thinking for everyone at the School of Nursing.
“Many of our faculty and staff par ticipated in focus groups to plan what types of learning spaces were needed, what they would look like, and how they would be equipped, down to the last detail,” says Tricia Benson, 86MN, the school’s chief engagement officer. “Everyone loved the loca tion and history of the building. The challenge was figuring out
development easily accessible for the 8,000 nurses who work for the health system.
“The technology and distance learning capability of the Emory Nursing Learning Center is tremendous,” says Pappas. “Instead of putting nurses on the road to come to class or grand rounds, we’re able to deliver education to them.”

In many respects, the Emory Nursing Learning Center embodies how nurses use their critical thinking skills to solve problems collabora tively. When the learning center was an empty shell, McCauley sought input from faculty, staff, and students on how to use the space.

“Her vision, drive, and openness set the tone for the school,” says Beth Ann Swan, PhD, RN, FAAN, associate dean and vice president for academic practice partnerships and exec utive director of the ENLC. “It has allowed all of us to think big and dream big to transform nursing education.”
John Coffin, an Atlanta businessman, has known McCauley for more than 10 years. Their friendship led him to serve on the Dean’s
Top left: Linda McCauley leads a meeting in the conference room named in her honor at the Emory Nursing Learning Center.
Left: This 1960s-era postcard shows the original bank building that now houses the new Emory Nursing Learning Center in Decatur.
how to configure 70,000 square feet of space to better educate pre-licensure and post-licensure students.”
The task required a special skill set. The Beck Group, which has designed and built simulation centers for schools in other states, was awarded the job.
When architect Ken Higa, Benson, and others first saw the space, each floor had a different look and feel. The first and second floors still housed a bank, where tellers waited on
customers in an open two-story lobby. The fourth floor was a long, plain series of offices. The terrace level, or basement, was a dizzying maze of drab corridors. In the middle was a huge bank vault installed by Decatur Federal Savings & Loan, the original owner of the building.
The vault, Higa knew, would have to stay. Its massive metal door and two-foot-thick walls were immovable. Higa and the School of Nursing agreed on a solution: convert the vault into the ENLC’s largest skills lab.
BETH ANN SWAN, PHD, RN, FAAN
vision, drive, and openness set the tone for the school.
Faculty member Dorothy Doughty leads a professional development course in the Emory Nursing Experience.


Advisory Board, whose members counsel McCauley on strategic initiatives such as the learning center.
“Growth is challenging,” says Coffin. “Linda has been very persistent and focused on finding a location that complements the 1520 Clifton Road building to address the growing needs of the student body and the faculty. The Emory Nursing Learning Center provides a vibrant learning environment in downtown Decatur that will benefit the entire Emory community.”
In a show of support, the advisory board, the School of Nursing’s leadership team, and local business partners made a naming gift to honor the dean for her visionary leadership. The McCauley Conference Room is located on the lobby level, where students, faculty, Emory Healthcare nurses, and visi tors now come and go daily.
“It’s right in the center of the action,” says Coffin. “The McCauley Conference Room is a testament to Linda’s passion and care for Emory nursing students and her colleagues.”


“Everyone embraced the vault as a touchstone for honoring what the bank used to be while transforming it into something unique to support nursing education,” says Higa.
Another feature he envisioned was a social stairway and digital wall to connect the first and second floors. The first floor is now the student commons, a bright and open lobby with a reception area, comfortable seats and tables, meeting and study spaces, conference rooms, and a kitchen.
From there, students and faculty head up to the second floor for classes, brainstorming sessions in the Innovation Hub, independent practice time in the open skills lab, and simulations in a home lab and telehealth office.
Throughout the learning center, Emory-themed colors and photographs link it to the main university campus. Audiovisual and IT experts have installed the latest technology to run multiple complex simulations and support continuing education provided by
the Emory Nursing Experience on the fourth floor.
The Beck Group designed the learning center using 3-D computer technology that allows users to “walk” through the space. The technology was a bonus when online meetings became the norm during the COVID-19 pandemic. “It allowed everyone at the School of Nursing to see the space as we saw it,” Higa says.
COVID had another effect on Higa and his colleagues. “It
deepened our appreciation for how vital nurses are in caring for patients,” he says. “It was more important than ever to make sure the Emory Nursing Learning Center was done successfully.”
For Benson and her colleagues, making students feel they are part of the School of Nursing, whatever their location, was essential. “Whether students are doing a simulation at the learning center in Decatur or attending a lecture at the 1520 Clifton Road building, the quality of their education is our priority.”
The technology and distance learning capability of the Emory Nursing Learning Center is tremendous.
SHARON PAPPAS, PHD, RN, NEA-BC, FAANSharon Pappas By Jim Auchmutey

Atornado strikes a nursing home in metro Atlanta. Multiple people have been killed and severely injured. Downed power lines and ruptured gas pipes imperil the wreckage. The first emergency workers arrive on the scene, along with police, frantic family mem bers, TV news crews — and nurses.
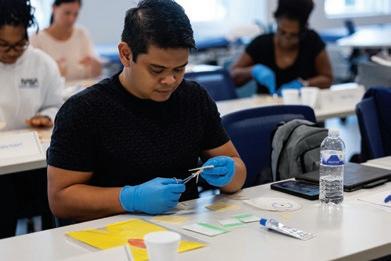
In this case, they are students, because this is a disaster simulation, one of many that will be staged at the new Emory Nursing Learning Center to help pre pare nurses for the world of crises and complications they may face in their practice.
Simulations are one of the key parts of nursing education, and the learning center will provide ample space and employ the latest technology to let students and instructors work through real-life scenarios.


On the terrace level of the facility, in what had been for six decades the basement of four Decatur banks, instructors will use a warren of exam rooms and skills labs to train nurses with scenarios they will
face the rest of their careers: everything from child birth to geriatric care, not to mention traumas like those depicted in the disaster drill.
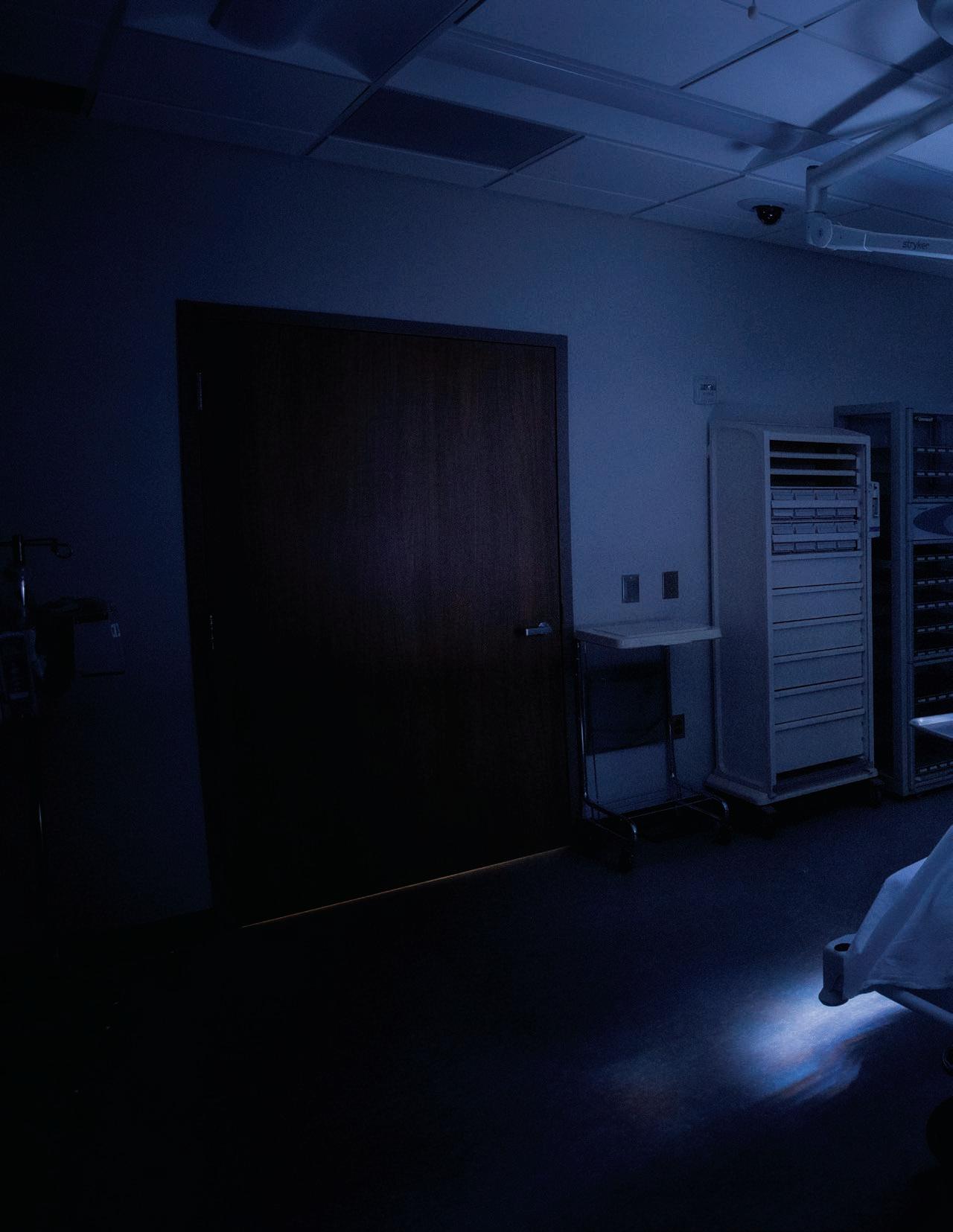
At the center of the honeycomb, the former bank vault has been remodeled into the Vault Skills Lab, a large rectangular space with eight patient beds and a control room behind mirrored glass where instructors will oversee classes and operate the high-tech manikins that nurses will practice on.
“It mimics what students will see in an actual clinical environment,” says associate dean Beth Ann Swan, PhD, RN, FAAN, executive director of the center. “The latest bed. The latest headwall. Computers on carts. The same electronic medication
Simulations are at the heart of nursing education, so it figures that they’ve been used to fight the COVID-19 pandemic.
Almost a third of the U.S. population has not been fully vaccinated against COVID. To increase confidence in the vaccine, Quyen Phan, DNP, APRN, FNP-BC, assistant clinical nursing professor at Emory, designed a simulation that is part of an initiative led by the American Association of Colleges of Nursing (AACN).

Using recent COVID vaccine coverage and refusal data, Phan and a colleague, Deborah Silverstein, DNP, APRN, FNP-BC, wrote five scenarios where student nurses encounter actors portraying patients who have various reservations about the vaccine:

• A Black male professional who doesn’t feel at risk from the virus.
• A white farmer and veteran in rural Georgia who doesn’t trust the government.
• An undocumented Hispanic woman who fears she will be deported if she seeks vaccination.
• A Black mother who is expecting another child and worries that the vaccine might harm her baby.
• A Native American truck driver who thinks the vaccine was developed too hastily.
“The goal is for the student nurses to use motivational interviewing technique to engage and inform people,” Phan says. “Not necessarily to persuade them, but to build their confidence in the vac cine. It’s a simulation that prepares them for encounters with real people.”
A video of Phan’s work will be shared online by AACN as part of its initiative, “Building COVID-19 Vaccine Confidence Among Nurses and in Communities.” The project, funded by the Centers for Disease Control and Prevention through AACN, involves 10 nursing schools nationwide.
dispenser machines that Emory Healthcare has. What the students will see in the Vault and all the skills labs are in hospitals around the city.”
Swan started nursing school during the 1970s and marvels at how far nursing education has come since she was practicing injections by sticking oranges and occasionally her friends. But to truly appreciate the advances represented by the learning center, you must go back even further to the experience of another nurse. She’s the one whose name happens to be on the plaque outside the Vault.
When Kay Chitty, 65N, 68MSN, EdD, attended Emory’s nursing school during the 1960s, the skills lab was on the sixth floor of Emory University Hospital, and students used manually cranked beds to practice on loose-limbed dolls that were little more than crash test dummies. There was a baby doll and an adult model everyone knew as Mrs. Chase.
“I remember moving Mrs. Chase to one side so we could practice how to make a bed,” Chitty says. “You could put a tube down the baby’s mouth and put it in her nose, but you couldn’t do much else.”
Chitty went on to a distinguished career as a nurse practitioner and nursing
It’s the difference between Galileo’s telescope and the Webb telescope. We couldn’t have imagined this when I was a student.
KAY CHITTY, 65N, 68MSN, EDD
Nursing students can learn a lot training on high-tech manikins, but there are some situations that are so sensitive they require human interaction. Forensic nurses, who treat victims of child abuse, elder abuse, and sexual assault, usually practice their skills with standardized patients, or actors. The Emory Nursing Learning Center was designed to make those scenarios more vivid and instructive.
“I’m stoked because we’re going to be able to do so many more simulations,” says associate professor Trisha Sheridan, DNP, WHNP-BC, SANE-A, SANE-P, FAANP, CFN, coordinator of the Women’s Health/Gender-Related Nurse Practitioner Program. “You can read a book, listen to a lecture, and take a test. But that’s not enough. Simulations allow you to put that knowledge into practice and show that you are trauma informed.”
Sheridan is one of fewer than 30 nurses in Georgia certified as a sexual assault nurse examiner through the International Federation of Forensic Nurses. The School of Nursing last year received a $1.2 million federal grant from the Health Resources and Services Administration to train more of them.


“People are finally realizing the long-term health effects of trauma,” she says. “Research shows that survivors who interact with forensic nurses have better outcomes.”
Sheridan got into the field when she was a young nurse practitioner in Washington state and witnessed a sexual assault victim’s unfortunate encounter with a doctor who examined her and then asked whether she had ever had herpes. “No,” the patient answered. “Well, you do now,” the doctor said.
“It was horrible,” Sheridan says.
To train forensic nurses, she and other instructors will stage simulations in the terrace-level patient exam rooms at the learning center, which are equipped with the latest examination technology, such as a black-light scan that reveals bite marks and bodily fluids. Forensic Teaching Associates will use their own bodies to depict various scripted trauma scenarios, complete with bruising and laceration makeup.
Encounters will be observed, often videotaped, and discussed afterward in debriefing rooms. Students will also simulate gathering evidence and giving testimony in court proceedings.
“I tell students they have to give themselves over to the experience and not think, ‘Oh, this is not real, this is acting,’” says Sheridan. “Statistics tell us it is likely that that they, or someone they know, have had a similar experience in real life. Simulations are key as students transition from classroom to patient room.”
school administrator in South and North Carolina and Tennessee. Now retired and living with her husband near Charleston, South Carolina, she has been supportive of her alma mater for years. When she considered philanthropic opportunities at the learning center, she thought back to her days as an Emory student.
“I got a fabulous nursing education at Emory,” she says, “and most of us passed our boards on the first try. But somewhere in my reptilian brain I could hear what people sometimes whispered about Emory nurses back then. They said we could theorize and conceptualize, but we couldn’t catheterize. They meant that we had book learning but didn’t have as much practical, hands-on experience.”
The Vault appealed to her because she didn’t want anyone to say that about an Emory nurse again. She and her husband made a naming gift. As a result, the terrace-level room designed to be the nerve center of simulations and hands-on learning for students is now called the Kay & Charles Chitty Vault Skills Lab.
The Chittys toured the facility late last year, donning hard hats and face masks to see a space that was in the process of being transformed from bank vault to state-of-the-art laboratory. They could see oxygen and suction lines in the open walls and what seemed liked miles of wiring in the unfinished ceiling.
Chitty thought about her days at Emory and the days to come in the learning center. “It’s the difference between Galileo’s telescope and the Webb telescope,” she says. “We couldn’t have imagined this when I was a student.”
Simulation operations specialist Kim Fugate (right) talks about Emory Hal, the center’s newest manikin. Thus far, Emory is the only nursing school to have the manikin, which operates via artificial intelligence.


Without exception, the nursing professors who will use the new learning center say the added space is one of its greatest attributes. On the terrace level alone, there are 12 exam rooms, eight debriefing rooms, three highfidelity simulation rooms, a high-fidelity operating room, a high-fidelity labor and delivery room, a classroom, a lounge for actors who play standardized patients, six control rooms, and four skills labs in addition to the Vault Skills Lab.
“It’s going to be so much easier staging simulations in the new center,” says associate professor Jeannie Rodriguez, PhD, RN, who directs Emory’s pediatric nurse practitioner primary care program. “Until now, we had to run primary care simulations at Wesley Woods and acute care simulations across Clifton Road at the School of Nursing. Now we can do it all at one location. I foresee that this will be the primary building where many of our students will do their work on campus.”
Having more space will also allow instructors to run more simulations in a given day. “It takes time to set up childbirth scenarios because it’s so messy,” says senior instructor Wendy Gibbons, DNP, CNM, who teaches midwifery. “We’ll have more room to debrief and discuss in a confidential manner.”
Nursing professors were consulted early and often in the design and outfitting of the skills labs. Concentrating instruction in one place will allow for scenarios that can anticipate the continuum of care that many nurses will face after graduation. Students might practice simulations on a patient who comes
in for emergency care, for instance, and then follow up with the patient during outpatient encounters, telehealth conferences, or visits to a simulated residence — the home lab — created for such training on the second floor.

Tracey Bell, DNP, NNP, assistant director of the neonatal nurse practitioner program, is looking forward to using the new — and larger — space for the progressively challenging simulations that faculty devise. Students will experience a variety of scenarios involving preterm, freshly born, and older infants, some of whom will have mothers and parents portrayed by standardized patients with different skin tones and ethnicities. Scenarios will play out in delivery room and clinic settings, where students will fine tune their skills in teamwork, triage, and delegation.
“One of the problems we see with students is their inability to suspend disbelief,” Bell says. “This is going to be one of the most up-to-date simulation situations at any nursing school. It’s as close to real life as we can get it.”
The learning center has 25 manikins, two-thirds of them high-fidelity models. The artificial patients allow students to practice the clinical skills they will need for the rest of their working lives.
Most of the manikins have proprietary names given by their manufacturers: preemie Hal, pediatric Hal, child-bearing Victoria, newborn Super Tory, adult Nurse Anne. The newest addition is Emory Hal, which operates via artificial intelligence and is the first of its kind in the world. Emory is the only nursing school to have this model to date. The manikins can breathe, hemorrhage, have seizures and heart murmurs, and change color to exhibit jaundice. Nurses can place catheters and chest tubes in them and even check their breasts for lumps. Two instructors typically run simulations, one focused on students and the other on operating the manikin, sometimes talking on behalf of the patient through a two-way audio system.
This summer, several Emory nursing students vis ited the learning center to look around. They did a dry run checking vital signs on a manikin named Susie, a middle-aged woman with mocha-colored skin — like patients, manikins come in all skin tones. With her neat, medium-length reddish hair, she looked like she could have been a bank employee — except that she wore an oxygen mask. She made breathing sounds and periodically blinked her eyes.
“Blood pressure normal,” one student said, looking at the monitor. Another took Susie’s pulse and listened to her computer-generated heartbeat.
“This is really something,” said Shannon Martensen, an MN/MSN student from San Diego, as she took in the room. “When you see that vault door, it feels like you’re robbing a bank.”
For a nursing student, the Vault holds something incredibly valuable: the opportunity to acquire experience.
This is going to be one of the most up-to-date simulation situations at any nursing school. It’s as close to real life as we can get it.
TRACEY BELL, DNP, NNP
No one is happier to be moving into the Emory Nursing Learning Center than Kelly Wiltse Nicely, PhD, CRNA, FAANA, who directs the DNP Nurse Anesthesia Program. Until now, the 36-month program has conducted simulations at Emory Wesley Woods.



“Our previous simulation space served its purpose,” says Nicely. “Now we have a hightech OR with multiple cameras and big screen monitors and the latest manikins. It’s light years ahead of where we were.”
Started in 2017, the program trains nurses not only to administer anesthesia during surgery but also to monitor pain and vital signs while the surgeon concentrates on the task at hand. It’s a critical job that can mean the difference between life and death or disability.
On the terrace level of the learning center, instructors will lead students through every possibility starting with basic induction: assess ing patients, hooking up monitors, putting patients to sleep, and placing an airway.
“We do that simulation dozens of times,” Nicely says. “We want our students to have a lot of muscle memory before they ever go into an OR for real. It gives them a huge boost of confidence.”
Students will work with a wide range of manikins, from infants to children to mature adults to geriatric models. “These manikins can do everything,” Nicely says. “We can adjust their tongues and make them harder to intubate. They’ll turn blue from lack of oxygen. We can make one lung ventilate while a surgeon operates on the other lung.”
The manikins can bleed, too, but only through stage blood released from hidden containers.
The new set-up even has a smoke machine to simulate fire. “When you combine oxygen, cautery, and draperies, there’s a risk of fire,” Nicely says. “We hope that never happens in our students’ careers, but it can, and they need to know how to respond.”
For all its advances, the high-tech OR has one relatively old-fashioned feature that Nicely is just as excited about: a one-way mirror that takes up an entire wall facing the patient’s bed.
“This is a physical profession,” she explains, “and we want to watch how students are doing their job to make sure it’s ergonomically correct. We don’t want our students to hurt themselves because we want them to be able to do this for years to come.”
Margaret’s life isn’t easy. Now 72, the widow has lung, kidney, and heart problems related to diabetes. In recent months, she’s been admitted to the hospital five times. After she’s discharged, she resumes life as best she can, aided by her pregnant daughter, until her health worsens once again.
A small group of Emory nursing students have come to know Margaret. They’ve seen her in the doctor’s office, at the hospital, at home, and in her neighborhood — all without leaving the classroom. They entered her world after donning a virtual reality (VR) headset to test a program developed by Emory nursing professor Beth Ann Swan, PhD, RN, FAAN, and her team.
Swan devised the VR program to teach students about hotspotting. The health practice approach targets “super utilizers”— frequent users of health care services like Margaret — to reduce the dispropor tionately high cost of their care by addressing their complex medical and social needs.

IN THE INNOVATION HUB, THERE ARE NO LIMITS TO IMAGINING WAYS TO IMPROVE PATIENT CARE
To develop the program, Swan collected data on Emory Healthcare patients through Project NeLL, an electronic learning library that provides nursing faculty, researchers, students, and nurses at Emory and other U.S. locations with access to vast stores of patient data. Swan sorted through the data to create Margaret and four other diverse virtual patients.
The project is one of many that faculty believe will come to life in the Innovation Hub at the Emory Nursing Learning Center. Located at the top of the staircase on the second floor, the hub is a place “where ideas will collide,” says Swan, executive director of the ENLC. “It will serve as an incubator space where students will learn to think outside the box. How that takes shape might depend on the day and how they end up using that space.”
The rectangular-shaped hub has glass walls, white boards, and movable furniture designed to ebb and flow with the ideas that take shape there. Students of all levels, from BSN to PhD, will use the space to collaborate with School of Nursing faculty and scientists, Emory Healthcare nurses, and technology and industry experts to design and test a host of ideas. Among them: phone apps, patient care devices and sensors, artificial intelligence (AI) and machine learning programs, and nursing workflow systems.
Their ideas will align with the nursing school’s Innovation Strategic Initiative. Led by Swan, the initiative provides a framework for projects in digital
health technology, care delivery, simulation, design thinking, and computational health sciences.

More and more, the school’s highly ranked research and education programs are attracting students who want to be innovative nurses. Colette Masunaga, a Master of Nursing student who grew up on the island of Hawaii, is one of them. After working in administration and health policy at a hospital in Honolulu, she decided to enroll in nursing school to work directly with patients. The Nell Hodgson Woodruff School of Nursing was her top choice.
“I decided to go to Emory because I knew I would get a strong clinical foundation in nursing, and that’s what I was looking for,” says Masunaga.
She is well on her way. This past summer, she completed a pediatric and maternity rotation at Emory Decatur Hospital, which proved both eyeopening and fulfilling.
“I felt so connected to expectant and new mothers and their babies,” she says. “Where I come from, we have very low access to health care. When my mom was planning to have me, the plan wasn’t about which hospital to go to. The plan was how to get to another island with acute care services in case something went wrong. Being in a health system like Emory’s, which has so many resources and so much innovation and research going on, is just amazing.”
Masunaga has been exploring her innovative side as part of a research team led by biomedical engineer Xiao Hu, PhD, associate director of the school’s Center for Data Science.
More than 10 years ago, as a faculty member at UCLA Neurosurgery, Hu developed an algorithm to help prevent nurse alarm fatigue. Typically, ICU monitors emit a host of alarm sounds, many of them false or non-life-threatening. His solution was to create a super alarm, a learning software that captures trending patterns, filters out false alarms, and more critically identifies clusters of alarms that co-occur consistently as harbingers of impending patient events. When a super alarm sounds, it indicates when a patient truly needs attention, such as when the heart or lungs begin to malfunction.
Hu has refined the algorithm to perform more effec tively: It works by combining data from a bedside mon itor and an electronic health record to look for patterns in a patient’s condition and treatment over time.
How does it work? Consider a male hospital patient who is experiencing cardiac arrhythmia. Meanwhile, two hours earlier, his electrolytes showed a minor imbalance.
[The Innovation Hub] will serve as an incubator space... How that takes shape might depend on the day and how they end up using that space.
BETH ANN SWAN, PHD, RN, FAAN
Nadine Matthie and EaseVRx
When adults with sickle cell disease are admitted to the hospital because of an acute pain episode, what health care providers see is only the tip of the iceberg, says School of Nursing assistant professor Nadine Matthie, PhD, RN, CNL. What health care providers don’t see is the chronic pain that these patients often experience at home.


Matthie is using a grant from the National Institute of Nursing Research to determine if a therapeutic virtual reality (VR) pain management program, EaseVRx, can help sickle cell patients manage their chronic pain in the home setting.
“Studies have been done using VR to manage chronic pain among individuals with

“The algorithm can put the two factors together,” Hu explains. “The patient’s heart is not beating well because of an electrolyte imbalance. This information gives clinicians a more precise picture of cardiac arrhythmia to explain why it’s abnormal.”
In another instance, a patient’s heartbeat interval is longer than on the previous day. The electronic health record shows the patient is on an anti-arrhythmia drug that elongates the heartbeat interval.


“The challenge is the information is there, but in two or even more different systems,” Hu says. “It takes time and attention to pull the information together. That’s where machine learning comes in. It can put existing data together to determine where the patterns matter.”
Masunaga is interested in learning how biomedical engineers and computer scientists work together to build algorithms like the one Hu has developed. In particular, she will look at how to improve nurses’ charting process so the data they enter will help the algorithm learn better.
“Nurses spend the most time with the patient,” says Masunaga. “They’re the ones who document any changes in a patient’s status.”
Going forward, the Emory Nursing Learning Center will enable Hu to test the algorithm and other projects in a simulated hospital setting. In the Innovation Hub, he can gather clinicians and industry experts together to solicit their feedback on current and future projects.
“The learning center,” he says, “will allow us to mature our algorithm so it can gather information to let nurses know when and how to intervene quickly to help their patients.”


fibromyalgia and back pain,” says Matthie, whose study targets Black adults, ages 18 to 50. “Why couldn’t sickle cell disease patients use it at home as part of their daily practice to control their pain? I first need to see what that would look like in this population because it hasn’t been tested among adults with sickle cell for home use before.”
In her study, Matthie will randomize individuals into one of two groups. One group will use EaseVRx, and the other group will hear the audio-only version of the pain management program via an audio stream.
Matthie’s study will continue through the end of 2023. If it proves successful, she would like to expand the idea, possibly in partnership with the Georgia Institute of Technology, through the Innovation Hub in the Emory Nursing Learning Center.

Sarah Febres-Cordero, a postdoctoral fellow in the School of Nursing, will never forget the summer of 2021.
It was a challenging time, as witnessed by stu dents in her public health practicum. COVID-19 cases had surged once more. And summer began with a rash of overdose deaths — five in one week — in the Atlanta community.

Febres-Cordero, 17N, 20MS, 21PhD, RN, wanted students to document what they learned in a meaningful way. Instead of writing papers, she had them capture their experiences with the Atlanta Harm Reduction Coalition on their iPads and iPhones. The coalition works to reduce the impact of



substance use, HIV/AIDS, and other conditions in marginalized communities.
Students told their stories through photos, reflective writing, videos, and podcasts. They used them to create an electronic publication (EPUB), A Summer of Innovative Public Health Nursing at the Atlanta Harm Reduction Coalition.

Their EPUB was a product of the Graduate Student Nursing Academy’s Digital Innovators Program, sponsored by the American Association of Colleges of Nursing. FebresCordero was among the first nurses selected for the Digital Innovators Program, whose participants work with executives and digital innovation experts from Apple.
“Students don’t always see the value of public health nursing in the curriculum because they’re preparing to work in a hospital,” says FebresCordero. “I wanted to find an interesting way to engage them. It was meaningful to see students create something memorable and inspire them to consider working in public health.”
The Emory Nursing Learning Center affords faculty and students with something they’ve never had before: a lab for learning how to care for patients in their homes.

The home lab, resembling a two-room apartment, was made possible by a gift from CenterWell Home Health, part of Humana, Inc.
Learning to care for patients in the home, nursing experts believe, provides a deeper understanding of how various factors — loneliness, access to nutritious food, mental health, and other social determinants of health — can impact their lives.
The CenterWell Home Health Lab will expose students to the com plexities of home health nursing.
“With this lab, students will receive valuable experience to prepare them for practice and perhaps inspire them to start a career in home health,” says Kathy Driscoll, vice president and chief nursing officer at Humana.
Located on the learning center’s second level, the home lab has a combined living room, dining room, and kitchen, and a bed room and bath. Each room has an observation room for faculty.
Students will work with manikins and standardized patients in the apartment while instructors and classmates observe from a debriefing room next door. A telehealth and simulation office, located nearby, will allow students to engage in simulated remote consults — a part of home health nursing that proved
critically important during the COVID-19 pandemic.
During telehealth scenarios, prelicensure students in the apartment will consult with post licensure students and faculty in the telehealth office. Students can also use telehealth technology to provide simulated remote patient monitoring such as blood pressure, blood glucose, and heart rate.
The CenterWell Home Health Lab, the largest of its kind in Georgia, will expose students to a variety of possible scenarios: an elderly man transitioning home following a heart attack, a young girl with asthma, a teenage boy with autism, a new mother who delivered her baby by C-section and is learning to breastfeed, a 30-something man on home chemotherapy, and a 50-something woman receiving end-of-life care.
“Home health care is not just about patients who transition from acute care in the hospital,” says assistant clinical professor Quyen Phan, DNP, APRN, FNP-BC, who provided feedback in the design of the home lab.
“It’s about patients who receive ongoing care.”
“The home lab will help our stu dents think about nursing practice outside the four walls of a hos pital,” Phan adds. “It will provide them with the skills, knowledge, and competencies they need when they aren’t in total control in the hospital. They will learn how to deliver care in the home, where patients spend most of their lives.”
As nursing faculty and alumni will tell you, students can never have too much classroom, study, and chill-out space. The second floor of the Emory Nursing Learning Center is designed to meet those needs.

Around the corner from the Innovation Hub are three flexible classroom spaces, all equipped with interactive technology to create an active learning environment for students. Two smaller classrooms seat 45 students each. A large classroom seats up to 150 students, but not in typical theater style. Instead, students are grouped at large tables within easy view of large portable display monitors.
“We designed this classroom for peer-to-peer learning,” says Tricia Benson, 86MN, who helped guide how learning center spaces would be used. “Students will learn from each other as they work on projects and select the best ones to share with the class. The classroom setup will ensure students know how to work collaboratively as part of a clinical team when they begin to practice as nurses.”
Often, before and after classes, students can use the open skills lab to learn and practice on their own. The lab has hospital beds, tables, chairs, and adult, child, and infant manikins. It is named for the late Charles F. and Peggy Evans, whose bequest in 2003 made clinical skills and simulation learning possible at the 1520 Clifton Road building.
The second floor features a variety of other spaces just for students: a lounge, a wellness and meditation room, a room for nursing mothers, and a study area and outdoor balcony. It also includes a home lab with data collection capability resembling a small apartment, a telehealth office, conference rooms, and touchdown space for faculty, appointed with original wood paneling.
Emory nursing alumni are bound by the rewards and challenges they experienced in nursing school. Several spaces on the second floor are named for alumni whose gifts are intended to make the path easier for current and future nursing students.


Donté Flanagan, 04OX, 06N, 10MSN, DNP, is a certified registered nurse anesthetist who lives with his family in Philadelphia, Pennsylvania. He still recalls how daunting nursing school can be, especially for students who are underrepresented because of race, ethnicity, or gender. He and his wife, Ashlee, made a gift to name the student lounge in that spirit. They see the Flanagan Solidarity Lounge “as a place for students, especially those with marginalized identities, to feel safe and inspired to learn, achieve, and excel,” says Donté.
“Sometimes, going from the classroom to various clinical settings can be an unexpected and overwhelm ing experience as a novice,” he adds. “The Emory Nursing Learning Center will help alleviate some of those early missteps while preparing nurses who can step into their new roles and have immediate impact.”
Mary McCabe, 72N, MA, devoted her career to improving survivorship for patients at Memorial
Sloan Kettering Cancer Center in Manhattan. As an under graduate nursing student at Emory, she found it difficult at times to find a quiet, relaxing place to study. In that spirit, she made a gift to name the Mary and Thomas McCabe Student Study Area and Balcony.
“It seems ideal to me to have an informal place for students to spend time in solitary study or collaborative learning,” says McCabe. “Having such space is a treasure, and it makes me want to grab my laptop and find a seat!”
Tucked between the study area and a student locker room is a new mothers room named for Rose Cannon, 74MN, 95PhD. Her gift stems from her 37-year career in maternal and newborn practice and education at Emory’s nursing school.
Nancy Langston, 72N, PhD, FAAN, ANEF, retired dean of the Virginia Commonwealth School of Nursing, knows what it’s like to open a new build ing. She oversaw planning and construction of a four-level building, which had plenty of open spaces for nursing students. After the building opened, she learned that some students preferred quiet, closed spaces for studying, often in an unoccupied classroom.
The large classroom features high-tech monitors and group seating to foster collaborative learning.
Toward that end, she designated a gift for the Langston–McCain Conference Room on the second floor of the new learning center. “Given the opportunity to support a space that I knew from past experience would be put to good use by individuals and small groups of students, I was sold on the idea,” says Langston.
 By Pam Auchmutey
By Pam Auchmutey
The Emory Nursing Learning Center lives in a mid-20th century bank and office building with what project architects call “good bones.” Emory nursing leaders couldn’t agree more.

“We love the location and history of the building in Decatur,” says Tricia Benson, 86MN, chief engage ment officer for the School of Nursing. “We’ve been
able to retain several unique features — the bank vault, marble walls and terrazzo floors in the terrace lobby, the wood paneling in the faculty and staff lounge on the second floor, and a 1960s-era starburst clock in the student commons.”
The Beck Group, the design/build firm behind the Emory Nursing Learning Center, worked closely with Benson and others to retain the building’s historic elements and its welcoming presence.
“Nursing is about serving the larger community,” says Ken Higa, lead architect for the project. “It’s about connecting with people.”
By design, the two-story lobby is the heart of the learning center — a place where students, practicing nurses, faculty, staff, visitors, and Decatur community members can gather and connect with each other. An open staircase rises from the lobby, or student commons. A tall, vertical video sign, featuring a colorful rendering of the learning center by local artist Sergey Cherep, welcomes everyone there.

“The sign anchors the space, much like a tower in a town square,” says Higa. “It provides information while visually connecting the lobby and second floor.”
Today, the lobby brims with activity just as it did in 1962, when the eight-level building opened. Back then, tellers with Decatur Federal Savings & Loan Association waited on bank customers. Area residents hurried to appointments at doctors, lawyers, and busi ness offices on the upper floors. Rotary Club members met for lunch every Friday in the Sky Room, an event venue with a panoramic view, on the eighth floor.
Linda Harris was in high school when she first saw the building, where her father practiced with a law firm and later served as president of Decatur Federal.

“My father took me up to the Sky Room and told me, ‘This is the tallest building in the city of Decatur. You can see Stone Mountain from here,’” recalls Harris, now assistant city manager for Decatur. “My mother used to go to a beauty parlor downstairs.”
Her family walked everywhere in Decatur – to school, to the library, and to a movie theater and shops. Harris bought comic books in the pharmacy on the front of the Decatur Federal building. A restaurant serves breakfast and lunch at the same spot today.
Decatur has changed and grown in the years since Harris’s own children had savings accounts at Decatur Federal. She and other leaders have worked hard to preserve the small city as a vibrant, walkable community and grow its economy by attracting

Nursing is about serving the larger community.
KEN HIGA, LEAD ARCHITECT
businesses and partners like the Emory Nursing Learning Center to downtown.

“Having the learning center here creates a new type of synergy for all of us,” says Harris. “We can’t wait to see what lies in store for our community.”
Once a month, students in Emory’s Wound, Ostomy, and Continence (WOC) certification program arrive in Decatur for Bridge Week, the hands-on clinical skills segment of their continuing education training, offered through the Emory Nursing Experience (ENE). Students travel to Decatur from other states and other countries.
The nearby Courtyard by Marriott offers them a comfortable, convenient place to stay. The hotel provides students with breakfast and a shuttle to the Emory Nursing Learning Center a few blocks away. The hotel lobby provides them with a place to socialize and with quiet nooks where they can study. Students in the nursing school’s Distance-Accelerated BSN program also stay at the hotel.
“Emory has been a phenomenal partner for us,” says Shirley Senior, the Courtyard’s director of sales and marketing. “It’s been a huge revenue stream for
It’s a seven-minute walk from Decatur High School to the Emory Nursing Learning Center. It’s a 12-minute bus ride from Charles R. Drew Charter School to the same destination.
Twice a week, seniors from both schools — 14 in all — make their way to the learning center for three hours of class. When they graduate from high school next spring, all will be qualified to enter the workforce as a certified nursing assistant (CNA) and attend college.
The CNA program exemplifies the community partnerships that Linda McCauley, PhD, RN, FAAN, FRCN, had in mind when the learning center began taking shape in the 250 East Ponce building in downtown Decatur.
“We’ve been working for the past three years to open the center for nursing students,” says McCauley, dean of the School of Nursing.
“Now we can open the doors to share it with the community.”
Introducing high school students to careers in nursing is critical to growing the workforce. “The COVID-19 pandemic showed us
why we need nurses more than ever,” says McCauley. “Nursing requires a continual investment in education, whether you’re a high school student or an advanced practice nurse.”
The CNA program is a step in the right direction. It evolved after Duane Sprull, director of the Decatur Career Academy, and Juliet Karanja-Pinder, director of student services at Drew Charter School, approached Laika Steiger, MBA, FACHE, senior assistant dean at the School of Nursing, with the idea. The CNA program thus became the first offering in a health career track for Decatur High and Drew Charter school seniors.
Both schools offer their own programs to prepare students for college entry or vocational and technical employment after graduation. Often, when students choose an employment track, they forgo taking prerequisite courses for college. What was needed, the schools agreed, was a program that provided both options for students. The schools formed a partnership, called
D Squared, to create a health career track for their students, starting with the CNA program.
“D Squared ensures we are preparing students to be the best they can be,” says KaranjaPinder. “When students graduate, their prerequisite courses, CNA certification, and high school diploma will make them eligible to attend a four-year college, whether they choose to enroll right away or after they’ve worked as a CNA.”
Nursing faculty from Georgia Piedmont Technical College, some five miles from Decatur, began teaching the 14 high school students at the Emory Nursing Learning Center in August. Students take their
courses online in space provided by the Emory Nursing Experience, the professional development program for nurses, and receive hands-on training in one of the learning center’s skills labs.
“Getting real-world experience can change the trajectory of our students,” says KaranjaPinder. “They may decide that a career in nursing is for them and continue their education in college. The opportunities are endless. They can go in so many different directions.”
Her colleague at Decatur High School concurs. “We wouldn’t be able to do this program if the Emory Nursing Learning Center had not come to Decatur,” says Sprull.
JULIET KARANJA-PINDER, DREW CHARTER SCHOOLthe hotel, and the partnership and the camaraderie we enjoy with Emory nursing leaders makes that possible. We want to provide excellent service for the students. That’s what keeps the partnership going strong.”
When WOC students arrive for Bridge Week, it has a huge impact on the community, notes Laika Steiger, MBA, FACHE, senior assistant dean of transformative clinical practice operations at the School of Nursing. “They’re staying in a hotel and dining at restaurants within walking distance of the learning center. That’s the beauty of being in downtown Decatur.”
Word about the Emory Nursing Learning Center is spreading. The Georgia American College of
Midwives held a meeting there in late September. Hosting events related to Decatur’s arts, book, and food festivals are possibilities as are community talks on topics such as prenatal care, caring for an elderly parent, healthy eating, houselessness, preventing gun violence, and making health care more accessible.
This past May, the Emory Advanced Practice Nurses group hosted a one-day NICU.IMPRINT Conference at the ENE. The group has booked space again for next year.
“There are all kinds of events and conferences that can’t wait to be here,” says Steiger.
Getting real-world experience can change the trajectory of our students. They may decide that a career in nursing is for them and continue their education in college. The opportunities are endless. They can go in so many different directions.
Outside of the ENE’s highly interactive classroom are invaluable “touchstone spaces” where students and presenters can take calls, check email, and participate in their own Zoom staff meetings.

The Emory Nursing Experience (ENE) provides strong evidence that being part of the Emory Nursing Learning Center in Decatur is an excellent idea.


In July 2021, the ENE moved from Executive Park, an office complex near the Emory cam pus, into newly renovated space at the learning center. The space and amenities there have further enhanced the ENE’s ability to provide continuing education for professional nurses.
Established in 2019, the ENE hosts the platform for accredited content taught by Nell Hodgson Woodruff School of Nursing faculty and Emory Healthcare nurses. Over the past three years, more than 9,300 learners from all 50 states and more than 30 nations have enrolled in the 340 courses offered online or in a hybrid setting by the ENE.

“Our mission has always been to provide quality education opportunities for nurses,” says Laika Steiger, MBA, FACHE, senior assistant dean of
transformative clinical practice operations at the School of Nursing. “They come to the ENE for a variety of reasons: for continuing nursing education credit to renew their license, to stay on top of what’s new, but most importantly to learn something that enables them to be better at what they do, in their current job or a new one.”
The course catalog has evolved to reflect current best practices and the changing needs of nurses. Naturally, numerous courses have focused on COVID19-related subjects, especially early in the pandemic. A new one-credit course, inspired by the pandemic and the social justice reckoning that followed George Floyd’s death in May 2020, examines the historical foundations of racial disparities in U.S. health care.
The most significant shift in course offerings has been from individual classes to in-depth certification programs. “We want you to get more than just a continuing education credit,” Steiger says. “We want you to have an Emory Nursing certificate, which says you invested a significant amount of time, we’ve assessed your knowledge, and you truly can apply what you’ve learned.”
Accredited in 1976, Emory’s acclaimed Wound, Ostomy, and Continence (WOC) certification program is the most successful continuing education
The Emory Nursing Experience includes a studio for recording videos and podcasts for online and hybrid continuing education courses.

Dorothy Doughty (top left) and Janet Ramundo (bottom left) instruct students during Bridge Week, the in-person segment of the popular Wound, Ostomy, and Continence certification program.
Our mission has always been to provide quality education opportunities for nurses.
LAIKA STEIGER, MBA, FACHEThe Emory Nursing Experience is designed to look and feel like a conference center. Amenities include classrooms, conference rooms, a media recording studio, and open and private work spaces.

program offered by the ENE. It is one of seven such accredited programs in the United States. Emory faculty — particularly Dorothy Doughty, MN, RN, CWOCN, FAAN — pioneered the field. The program has a stellar word-of-mouth reputation among nurses, nationally and around the world.
Participants first complete their classroom courses online, asynchronously, at their own pace. “I was very impressed with how rigorous and in-depth the pro gram was,” says Marty Costa, DNP, MSN, RN, WON, a recent WOC program graduate from Roseville, California, who teaches full time at Chamberlain University. “As an instructor, I really appreciated how well Dorothy laid out the information and made the concepts easy to understand.” Both the lessons and an accompanying podcast — which enables students to reinforce lessons while on the go — were recorded in the ENE’s recording studio.
Participants then complete their program at the ENE with an onsite Bridge Week, which allows them to network with their fellow WOC students, meet instructors, clarify concepts, and perform hands-on skills and competencies.
The ENE’s design “recognizes that our students are professionals who have lives outside of our build ing,” says Steiger. Outside of the highly interactive classroom — well equipped for Zoom presentations with six monitors and multiple microphones for audience participation — are invaluable “touchstone spaces.” Students and presenters retreat to these nooks to discreetly take calls, check email, and partici pate in their own Zoom staff meetings. There’s even a nursing room for new mothers, a feature utilized and highly praised by recent participants.
The ENE’s location — on the fourth floor of the Emory Nursing Learning Center in downtown Decatur — has been a major selling point of the ENE
from the start. Out-of-town students can take MARTA rail from the Atlanta airport to the Decatur station, just two blocks from the ENE and its partner hotel, the Courtyard by Marriott. The hotel provides break fast, a study room, and a shuttle. Students appreciate having the hotel and multiple restaurants close to the ENE.
“The whole city of Decatur has been so accommodating,” Steiger says. “They’re always asking, ‘What do you need? What can we do for you?’ Our students absolutely love it, and it has made a world of difference for the ENE to be in this space.”
As word of the ENE has spread, more School of Nursing faculty and Emory Healthcare nurses have partnered with the ENE on new grant-driven training programs and taken advantage of its expertly designed spaces.
For example, the ENE teamed with School of Nursing associate professor Trisha Sheridan, DNP, WHNP-BC, SANE-A, SANE-P, FAANP, on an initiative to increase the number of certified sexual assault nurse examiners in Georgia. The training includes online courses, an in-person clinical skills experience at the ENE, continuing education, and certification prep courses so that nurses can earn and maintain their certification. The grant covers all costs for participating nurses. “We can make a big impact on the community by providing this course and not allowing finances to be a barrier to entry,” Steiger says.
Assistant professor Nicholas Giordano, PhD, RN, and his interdisciplinary team, developed a new initiative on nurse resiliency and well-being. The ENE created a central platform for all curricula as well as individual interactive online courses, recorded by subject-matter experts in the ENE’s recording
Our nurses have been through so much over the past three years. I’m grateful to have an opportunity to give something back to them in such a beautiful space.
TRINA GEYER, PHD, RN, NPD-BC, NEA-BC
Cynthia Harris (left) directs the clinical placement program for School of Nursing students. Laika Steiger oversees ENE operations for the nursing school in partnership with Emory Healthcare colleagues.
studio. A Health Resources Services Administration grant will ensure the material is provided for free to nurses across Georgia so they can become wellness champions in their respective communities.
An increasing number of internal Emory Healthcare programs are making full use of the ENE as well. “I am so incredibly thrilled to have this space for our nurse leadership development and well-being programs,” says Trina Geyer, PhD, RN, NPD-BC, NEA-BC, director of nursing leadership and development. Three leadership cohorts — ranging from informal front-line leaders to formal unit-level leaders to aspiring associate vice presidents, vice presidents, and chief nurses — meet at the ENE throughout the year. Emory’s Building Resilience and Compassion Enculturation (emBRACE) Peer Support Program will also use this space to develop Emory’s network of employees dedicated to well-being and joy

through interprofessional education and collaborative practices. “Our nurses have been through so much over the past three years (during the COVID-19 pandemic),” Geyer says. “I’m grateful to have an opportunity to give something back to them in such a beautiful space.”
Cynthia Harris, MHA, BSN, RN, CPC, director of clinical placement for the School of Nursing, values having her office in the ENE. “It’s wonderful to have a space that students can feel is their own and where we can meet with them face to face,” she says. “It allows us to create a better relationship with them and make a positive impression, so they’ll want to come back at some point and serve as a preceptor.”
The opening of the ENE has been a lifesaver for Carrie McDermott, PhD, APRN, corporate director of nursing professional practice for Emory Healthcare. McDermott directs the New Graduate Residency Program, a yearlong series of monthly four-hour seminars for nurses in their first year on the job. In 2021, 512 residents participated in the program, split into 17 cohorts. The program had outgrown its previous spaces; the ENE was the perfect venue for hosting each seminar’s presentations from subject-matter experts and small-group reflective practice exercises.
The ENE has certainly made a positive impression on residency participants. “It’s really important for these nurses who are entering their career at Emory Healthcare to be able to take classes in such an impressive, state-of-the-art facility,” McDermott says. “They can see how Emory Healthcare is showing so much pride in nursing and making such a big investment in them.”
The U.S. Public Health Service (USPHS) is among the federal agencies that respond when disaster strikes the country. It’s critical that USPHS officers responding to the scene be prepared, regardless of the resources and circumstances. The ENE has partnered with an Emory emergency preparedness expert to create a disaster-response skills
refresher training program for 2,500 clinical personnel — nurses, nurse practitioners, physicians, and physician assistants — in the USPHS Commissioned Corps.
The initiative is led by Sam Shartar, MSN, RN, NRP, CEN, FAAN, senior director of operations for Emory University’s Office of Critical Event Preparedness and Response, also known as CEPAR. “The USPHS approached us because of our operational expertise, our history of delivering disaster responserelated training programs through the National Disaster Life Support Foundation, our biosafety training
program, and our work with the National Emerging Pathogens Training and Education Center,” Shartar says.
Sam ShartarThe course curriculum draws on Emory’s expertise in the field, with nearly two dozen online course lessons that include mass casualty and emergency triage, airway management, and radiation emergencies. The ENE will host in-person assessments of psychomotor skills with subject matter experts four times a

year, welcoming approximately 160 participants for each two-day session.
“These officers are from various backgrounds, not all of which include emergency or disasterresponse training,” Shartar says.
“This course is an opportunity to refresh or build new skill sets for them so that they’re missionready and better prepared when they’re deployed to help augment health care delivery in various settings in times of disaster or a patient surge.”

A record number of School of Nursing faculty were named award winners by the Friends of the National Institute of Nursing Research (FNINR). The annual awards recognize national nursing research leaders who have made significant contributions to nursing science.
The Emory recipients — who won four of the five award categories — were cited for their accomplish ments and contributions to various fields of inquiry.
“These distinguished researchers are advancing nursing science and join the echelons of other nation ally recognized FNINR award winners contributing to the enhanced health and well-being of all Americans,” says Cathleen Wheatley, DNP, RN, CENP, FAAN, pres ident of Atrium Health Wake Forest Baptist Medical Center and current FNINR board president.
The honored faculty include:
Linda McCauley, PhD, RN, FAAN, FRCN, received the Ada Sue Hinshaw Award for her seminal research in environmental exposures. Her work has influenced national environmental health policies on how to reduce exposure to pesticides and measures to reduce the probability of exposure in pregnant women and children. The Hinshaw Award is the top honor given by FNINR. McCauley earned the recognition for her substantive and sustained program of science that continues to have a revolutionary impact on populations across the world.
Sandra Dunbar, PhD, RN, FAAN, FAHA, FPCNA, is the recipient of the President’s Award for her exceptional research career in cardio vascular nursing science. Her body of work focuses on psychosocial responses to serious cardiac illness. It also addresses the social determinants of health in pub lished papers on socioeconomic status discrimination and neighborhood incarceration rates as predictors of cardiovascular markers such as C-reactive protein. Dunbar’s findings have improved cardiovascular out comes nationally and globally and have been adopted by other researchers.

Deborah Watkins Bruner, PhD, RN, FAAN, is an internationally renowned researcher whose contributions have changed clinical practice guidelines and impacted cancer care internationally. She received the Welch/Woerner Path-Paver Award for changing clinical practice by pioneering the development of the radiation oncology nursing role and the required training. Her work has altered and improved how nurses and other clinicians approach cancer symptoms and treatment outcomes.

This is an unprecedented and impressive recognition for our nursing colleagues...who have achieved outstanding accomplishments in their respective areas of research.
JANIE HEATH, PHD, APRN-BC, FAAN, FNAP, FAANP, FNINR AWARDS CHAIR
Eun-Ok Im, PhD, MPH, RN, CNS, FAAN, was honored with the Faye Glenn Abdellah Award for her commitment to eliminating gender and ethnic health disparities. Her groundbreaking body of research spans disciplines and cultural settings. An early influencer and leader in Internet-based research, Im has since investigated ways in which emerging technologies may optimize data collection and health inter ventions among ethnic minority women. Since the late 1990s, she has used innovative tools and data analytic techniques to capture women’s health experiences with more nuance and precision than traditional methods allow.
“This is an unprecedented and impressive recognition for our nursing colleagues at the Nell Hodgson Woodruff School of Nursing who have achieved outstanding accomplishments in their respective areas of research,” says Janie Heath, PhD, APRN-BC, FAAN, FNAP, FAANP, dean of the University of Kentucky College of Nursing, who serves as FNINR awards chair.
The School of Nursing has earned accreditation for its Psychiatric Mental Health Nurse Practitioner (PMHNP) programs from the Southern Association of Colleges and Schools Commission on Colleges and welcomed its first cohort of students this fall.
Candidates in the post-BSN DNP and post-master’s certificate programs will develop exceptional clinical and leadership skills to help close the current gap in mental health care. The United States, and particularly the state of Georgia, face a crisis-level shortage of qualified mental health professionals — a need heightened during COVID-19.
Dorothy Jordan, 82MN, DNP, APRN, PMHNP-BC, PMHCNS-BC, FAAN


The School of Nursing’s Bachelor of Science in Nursing and master’s degree programs have been recognized among the very best — ranking No. 2 nationally, according to U.S. News & World Report



The BSN program rose two spots from last year’s No. 4 ranking, and the MSN and MN programs retained their No. 2 ranking. The Doctor of Nursing Practice program rose two spots to No. 6.
Multiple graduate specialties at the School of Nursing are ranked nationally, including:
• Family (MSN) – No. 5
• Adult/Gero Acute Care (MSN) – No. 4
• Adult/Gero Acute Care (DNP) – No. 7
• Adult/Gero Primary Care (MSN) – No. 4
• Family (DNP) – No. 6
The School of Nursing was also named among the top five nurs ing programs for total grant funding from the National Institutes of Health (NIH). The school posted the third-highest total, with approximately $10.5 million in research grants, fellowships, training grants, and other awards from NIH in the past fiscal year. This marks the seventh straight year the school has earned a top-five designation.
The pandemic led to “a significant increase in rates of depression and anxiety in our adult population,” says associate professor Dorothy Jordan, 82MN, DNP, APRN, PMHNP-BC, PMHCNS-BC, FAAN, who leads Emory’s psychiatry and mental health nursing program. “Children and adolescents are particularly vulnerable as most mental health disorders are diagnosed during this sensitive developmental period.”
To learn more about the PMHNP programs, visit links.emory.edu/qf.
The school’s NIH-funded research grants support many areas of study, including health disparities and health equity, preg nancy outcomes, aging, dementia caregiving, health promotion, disease management, HIV, symptom management, and quality of life.
“The rankings are a huge honor and recognition of the hard work taking place at the School of Nursing,” says Dean Linda McCauley, PhD, RN, FAAN, FRCN. “This is validation of our mission to prepare visionary nurse leaders and scientists with a thirst for discovery and a heart for patients and communities.”
As the nationwide nursing shortage lingers and as staffing challenges grow, the Robert W. Woodruff Foundation hopes to bolster the workforce and advance nursing education at Emory with a $3.5 million grant to the School of Nursing to create a nurse fellowship program.

The Nell Fellows program will provide continued nursing education for recent School of Nursing alumni who have chosen to work at Emory Healthcare as clinical staff nurses. Fifteen students started in the four-year, postgraduate Master of Science in Nursing (MSN) program this fall, and 60 additional students will begin studies in fall 2023.
“I am extremely thankful for the opportunity to demonstrate another model of how academic and practice leaders can collaborate to address the acute national shortage of nurses,” says Linda McCauley, PhD, RN, FAAN, FRCN, dean of the School of Nursing. “This program will help us move the needle in increasing the retention of nurses at Emory Healthcare by enhanced investment into their journey of lifelong learning.”
“There are no easy or quick answers to the nationwide crisis in nursing, but we hope that our grant will help nurture a new generation of Emory nurses and propel them into satisfying nursing careers,” says P. Russell Hardin, president of the Robert W. Woodruff Foundation.
The Robert W. Woodruff Foundation seeks to improve the quality of life in Georgia by investing in health, education, economic opportunity, and community vitality. Robert W. Woodruff, the late legendary leader of The Coca-Cola Company, became a major benefactor of Emory beginning in 1937. In 1979, he and his brother, George Woodruff, gave Emory a then-record sum of $105 million. Since then, the Woodruff Foundation has continued to support Emory University and its entities.
Seven members of the Emory nursing community have been named to the 2022 American Academy of Nursing class. More than 3,000 members, known as Fellows, comprise the academy and are among nursing’s most accomplished leaders in edu cation, management, practice, and research.
As Fellows, they will create and execute evidence-based and policy-related initiatives to advance health care. They join 67 School of Nursing alumni and faculty members who have already been tapped for the honor.
The 2022 honorees include the following School of Nursing faculty and Emory Healthcare nurse leaders:
Desireé Clement, DNP, APRN, CNM, FNP-BC, FACNM, FAANP, assistant professor and assistant dean of graduate clinical programs, School of Nursing
John Cranmer, DNP, MPH, MSN, EBP(CH), CPH, ANP, associate professor, School of Nursing

Rose Horton, MSM, RNC-OB, NEA-BC, specialty director of women and infant services, Emory Decatur Hospital



Bonnie Proulx, DNP, APRN, PNP-BC, director of advanced practice providers, Emory Healthcare, and adjunct faculty member, School of Nursing
Honorees also include three alumni from the School of Nursing: Dalmacio Dennis Flores, 12N, PhD, ACRN, assistant professor, University of Pennsylvania School of Nursing
Safiya George, 01MSN, 06PhD, APRN-BC, FAANP, FNAP, dean and professor, Florida Atlantic University, Christine E. Lynn College of Nursing
Tingting Liu, 15PhD, RN, associate professor, Florida State University College of Nursing
Assistant professor Priscilla Hall, PhD, RN, CNM, contributed to a recent meta-analysis study on water births that is gaining far-reaching recognition. The study – which shows that water births provide clear benefits for mothers and babies – is receiving attention from medical professionals and media sources such as “Good Morning America.”

A process of giving birth in a deep bath or birthing pool, water birth is relatively uncommon in the United States. The study’s focus on hospital-based care led to increased attention among physicians, as 98 percent of U.S. births occur in hospital settings.
A synthesis of evidence led the team to conclude that water births in an obstetric setting led to lower pain levels and reduced heavy bleeding in labor, higher satisfaction levels for mothers, and improved odds of avoiding perineal tears or lacerations.
Hall was part of a team that included primary investigator Ethel Burns, PhD, from Oxford Brookes University as well as researchers from the University of Nevada Las Vegas and King’s College in London.
A $1.5 million Reimagining Nursing Initiative grant from the American Nurses Foundation will enable Emory Healthcare’s Integrated Memory Care (IMC) Clinic to expand primary care for people living with dementia.

Created in 2015, the IMC Clinic is an innovative, nurse-led, patient-centered medical home that provides memory and primary care for people living with dementia and their care partners. It is a unique “one-stop shop” practice model, recognized nationwide and available only at Emory Healthcare.
“I would like to see water tubs in every hospital,” says assistant professor Priscilla Hall, PhD, RN, CNM.
The expansion of the clinic program — called IMC in Community — will allow dementia-sensitive primary care to be provided within participants’ senior living communities. The model incorporates occupational therapists and dementia care assistants to maintain participants’ independence for as long as possible.
The IMC Clinic team meets to develop an individualized plan of care for a patient.
The practice also includes registered nurses, licensed practical nurses, and clin ical social workers to support participants and their care partners.
The grant allowing for the expansion was awarded to Carolyn Clevenger, 02MSN, 18DNP, GNP-BC, AGPCNP-BC, FAANP, FGSA, a School of Nursing professor and gerontological nurse practitioner, and Deena Gilland, 07MSN, 18DNP, RN, NEA-BC, FAAN, Emory Healthcare's ambulatory practice vice president of patient services and chief nursing officer.
“Despite the considerable successes of the IMC Clinic, we have seen a critical gap in the continuum of care for our clients,” says Clevenger, clinical director of the clinic. “The grant from the American Nurses Foundation will enable us to pilot an expansion of IMC’s comprehensive care model into a new home-based setting — senior living communities.”
According to Gilland, expanding this nurse-led care model fully supports a National Academy of Medicine report emphasizing how nurses can reduce health disparities, promote equity, and maintain patient and family-focused care.
us
The Atlanta Business Chronicle has named assistant professor Roxana Chicas, 16N, 20PhD, as one of its Health Care Heroes for 2022. She won the award in the Rising Star category.

Chicas came to the United States from El Salvador at age four, crossing the Rio Grande on her mother’s shoulders. Undocumented, she later received temporary protective status that allowed her to work at a pediatrician’s office — the beginning of a journey that led to earning bachelor's and doctoral degrees from the School of Nursing and an appointment to the faculty.
Fueled by her experiences, Chicas uses nursing science to increase research inclusiveness through engagement with and empowerment of farmworker communities. She conducted the first field-based intervention study of methods to reduce the risk of heat-related illness using biomonitoring equipment among farmworkers. She also launched the first fieldbased study to test hydration interventions in the same group.
Additionally, Chicas works with School of Nursing professor Vicki Hertzberg, PhD, FASA, an inter nationally recognized expert on the impact of big data on health care.

The inaugural group of fellows included (L-R) Brenda Ramirez (Emory College), Kennedy Payne (Spelman College), Valerie Atieno (Spelman College), Anthony Udell (Clark Atlanta University), Jasmine Ofodu (Spelman College), and Joseph Fonseca (Morehouse School of Medicine).
The School of Nursing’s Diversity, Equity, and Inclusion Office has launched a Fellowship in Nursing Development, a recruitment effort to diversify the school’s pipeline of students inclusive of gender, race, and ethnicity. Students from these backgrounds, figures show, are underrepresented in nursing.
The inaugural group of six fellows participated in a twoweek immersion experience in June, where they learned about nursing specialty practice areas, research, and community engagement. They represented three historically Black college and university partners – Clark Atlanta University, Morehouse School of Medicine, and Spelman College – and Emory College.

The fellows met with Emory School of Nursing leaders and faculty as well as leaders from the U.S. Department of Veterans Affairs, Emory University Hospital Midtown, Emory University Hospital, and Emory Hillandale Hospital. They participated in seminars, clinical observations, and hands-on simulation experiences with Certified Registered Nurse Anesthetist program leaders.
Fellows also took part in the School of Nursing’s Farmworker Family Health Program in Moultrie, Georgia, an interprofessional, service-learning experience involving students from the school and other academic institutions.
The National Institute of Dental and Craniofacial Research has awarded a five-year, $3.9 million grant to School of Nursing associate professor Canhua Xiao, PhD, RN, FAAN, and Emory University School of Medicine professor Lisa Flowers, MD, MPH, FACOG, to study the role of the oral microbiome and periodon tal diseases in oral human papillomavirus (HPV) infection among people with HIV.

HPV infection is a known carcinogen for oropharyngeal cancer, the most common HPV-associated cancer in the U.S. For people with HIV, rates of oral HPV infection and oropharyngeal cancer are higher than in the general
population. The R01 project will examine the immunological underpinnings of oral HPV infection and whether social determinants of health play a role in the oral microbiome and oral HPV infections for people living with HIV.
Xiao also received a $3 million, R01 grant from the National Institute of Nursing Research to fund a multisite study assessing the role of the gut microbiome in the development of neuro psychological symptoms among head and neck cancer patients.
Symptoms such as fatigue, cognitive dysfunction, sleep problems, and pain are the most common and debilitating
side effects of head and neck cancer and its treatment and can be prognostic to survival. Xiao will study the association between the gut microbiome and these symptoms through the role of short-chain fatty acids (products of the fermentation of dietary fibers by gut bacteria) and inflammation in the gut-brain axis (the communication network connecting the gut and brain) among patients receiving radiotherapy.
Findings from both projects may indicate new biomarkers and novel therapeutic targets for those with oral HPV infection and head and neck cancer.
Ask Kylie Smith, BA (Hons), PhD, why the humanities are important to health care, and she will tell you that the answer is in the word itself.
“To administer effective health care, you have to be able to understand humans and their complexities,” says Smith, an associate professor at the School of Nursing. “Many health care problems we are trying to fix are caused by historical or policy issues, so you really can’t get the whole picture if you are not thinking about how it got to be this way.”
To that end, Smith is leading an effort to launch a Center for Healthcare History and Policy in the School of Nursing — with the aim of solidifying the place of the humanities in health care education and research.
A north Georgia family nurse practitioner (FNP) residency program has received accreditation from the National Nurse Practitioner Residency and Fellowship Training Program –the result of a strong partnership between the School of Nursing and MedLink Georgia, a nonprofit community health center that serves the state’s northeast region.
The North Georgia Advanced Practice Provider (NoGAPP) residency program provides new family nurse practitioners with a structured clinical experience to enhance their transition into practice. It was created through a Health Resources and Services Administration (HRSA)

grant focused on building an infrastructure to support an FNP residency program in rural Georgia.
NoGAPP is the first FNP residency program in a Federally Qualified Health Center to receive accreditation in the state of Georgia.
Since it began in 2020, NoGAPP has graduated nine residents. The program has expanded its footprint to eastern, central, and southeast ern parts of the state in partnership with the East Georgia Healthcare Center and Community Health Care Systems. It now covers 40 counties.
Bethany Robertson, DNP, CNM, FNAP, serves as the academic practice partnership liaison for the School of Nursing and HRSA project director.

The center will bring together Emory scholars and students from various disciplines who seek to understand the impact of history, legislation, and policy on health outcomes and the factors that affect health care delivery, especially to marginalized populations. Also, the center will create discussion forums, enhance collaborative grant application and publication initiatives, and host research events. Other activities will include working with faculty on curriculum, supporting student projects, establishing service-learning partnerships, and developing continuing education opportunities.
Through its work, the center will espouse a historically informed, “bottom-up” view of health care where patients are the experts, and their life and health experiences are used to enhance approaches to care.
“Nurses are agents of change and have been historically,” says Smith, the Andrew W. Mellon Faculty Fellow for Nursing and the Humanities at Emory. “But if you don’t know that, and if you are not taught tools from the humanities — like sociology or history or even creative writing and the arts — then how are you going to connect with people and bring change to the world? That’s my big pitch for the humanities — understanding humanity.”

Assistant professor Fayron Epps, PhD, RN, FGSA, FAAN, is one of 12 nurse scientists in the nation receiving the Betty Irene Moore Fellowship for Nurse Leaders and Innovators.

The National Institute of Nursing Research has awarded a $2.7 million grant to professor Eun-Ok Im, PhD, MPH, RN, CNS, FAAN, and research professor Wonshik Chee, PhD, to test the effectiveness of a technology-based, physical activity promotion program to reduce symptoms of depression among midlife racial and ethnic minorities, particularly Korean American women.


With an increasing multicultural aging population in the U.S., depression among midlife racial/ethnic minorities is becoming increasingly significant. The prevalence of depression among Asian Americans is about 4.5 times higher than that of Americans in general. Within the Asian-American demographic, Korean Americans
have the highest rate of depression, with midlife Korean American women experiencing even higher rates.
Korean Americans also have a cultural preference for natural lifestyle management strategies to treat depression and embrace a cultural emphasis on one’s ability to handle stress without outside assistance.
Im and Chee will examine the use of a web app to promote physical activity and improve depressive symptoms in ways that appeal to cultural prefer ences. Goals for their study include accelerating the translation of tech nology-based programs into primary care settings and contributing to the reduction of racial and ethnic disparities in health and diseases.
Funded by a $37.5 million grant from the Gordon and Betty Moore Foundation, the program recognizes early- to mid-career nursing scholars and innovators with a high potential to accelerate leadership in nursing research, practice, education, policy, and entrepreneurship.
As part of the three-year program, fellows receive $450,000 to conduct an innovative project that addresses a knowledge gap, meets a vital need, alters care delivery, or provides a new solution to advance health. Epps’ project is an education initiative called “Caregiving While Black.” It seeks to enhance Black caregivers’ competence and confidence in addressing challenges encountered in navigating social and health care systems on behalf of persons living with dementia.
The prevalence of depression among Asian Americans is about 4.5 times higher than that of Americans in general.Wonshik Chee, PhD Eun-Ok Im, PhD, MPH, RN, CNS, FAAN


Shawana Moore, DNP, MSN, CRNP, WHNP-BC, recently joined the School of Nursing faculty to serve as the Doctor of Nursing Practice program director.

Moore comes to Emory from Thomas Jefferson University in Philadelphia, where she served as an assistant professor and director of the Women’s Health – Gender-Related Nurse Practitioner program. A board-certified women’s health nurse practitioner, she focuses on providing women’s and reproductive health care to underserved populations and maintains a clinical practice.
Her expertise includes women’s health, adolescent female empowerment, prepregnancy counseling, well-woman care, contraception, maternal obesity, gynecological disorders, telehealth in the women’s health care setting, diversity, inclusion, and equity. She is a key collaborator on a National Institutes of Health grant, “Sexual Health Empowerment for Jail-Involved Women’s Health Literacy and Prevention,” and president of the National Association for Nurse Practitioners in Women’s Health.

The Woodruff Health Sciences Center has established an Office of Inter professional Education and Collaborative Practice (IPECP).
Launched in March 2022, the office prepares the health care workforce through interprofessional opportunities that improve the health of communities served by the Woodruff Health Sciences Center. The center includes Emory’s schools of medicine, public health, and nursing; the Emory National Primate Research Center; the Winship Cancer Institute; and Emory Healthcare.
Linda McCauley, PhD, RN, FAAN, FRCN, dean of the School of Nursing, and Ira Horowitz, MD, executive associate dean of faculty and clinical affairs at the School of Medicine, led the effort to create an IPECP Council in 2018. The new IPECP office is led by Jodie Guest, 92MPH, 99PhD, senior vice chair of the Department of Epidemiology at the Rollins School of Public Health, and Beth Ann Swan, PhD, RN, FAAN, associate dean and vice president for academic practice partnerships and executive director of the Emory Nursing Learning Center.
The office’s work involves enhancing interprofessional curricula, accelerating the adoption of team-based care models, and supporting research on interprofessional collaborations.

“I saw Deena’s skill and compassion as a clinical nurse,” recalls mentor Mary Gullatte, 81MN, PhD, RN, AOCN, FAAN, Emory Healthcare corporate director of nursing research and evidence-based practice. “She always seemed to look for ways to improve care for patients while also engaging staff in change. I wanted to help give her the confidence to soar — and soar she has.”
When the pandemic jeopardized the Magnet goal, Gilland negotiated with the AANC for four extra months to prepare documentation. She weighed asking more of nurses and team members who were already stretched so thin. Would six years of building trust and creating a shared vision be enough fuel?
As health care’s gold standard, Magnet stands for professionalism, teamwork, and superiority in patient care. Driven by data and based on evidence, it signals to nurses a commitment to their well-being and professional growth.
For six years, Deena Gilland 07MSN 18DNP had led Emory Clinic’s pursuit of this rigorous achievement for ambulatory nursing care when the coronavirus threatened to derail it all.

In March 2020, her team was deep into compiling years of carefully collected data, stories, and other proof of nursing practice, research, and patient outcomes.
“Then bam! The world changed,” says Gilland, DNP, RN, NEA-BC, FAAN, vice president of patient services and chief nursing officer of Emory Ambulatory Care Practice. “We had a pivotal point of asking ourselves, ‘What do we do? Do we keep on trying?’ It was chaos. That was our lowest point.”
Gilland and the Emory Clinic nursing teams steered through. In May 2022, the American Nurses Credentialing Center (ANCC) announced that Emory Clinic was the first ambulatory or outpatient practice in Georgia to receive Magnet status. The clinic network relies on 1,000 nurses and more than 500 nurse practitioners. “Tangible evidence of our nurses’ commitment to providing the very best care to our patients and their families,” Sharon Pappas, PhD, RN, FAAN, chief nurse executive for Emory Healthcare, called it.
Long before Gilland started visualizing Emory Clinic’s journey to Magnet status in 2014, others saw and nurtured her lead ership potential. Her uninterrupted 34 years at Emory Healthcare began as a clin ical nurse at Emory University Hospital; in 2007, her MSN degree led to leadership positions including one with oncology nursing at Winship Cancer Institute.
“Whether we receive Magnet designation or not, we’re committed to improving care and our practice environment for nurses, patients, and care teams,” Gilland says she concluded. “That was my ‘aha’ moment. To continue to improve patient care and enhance nurses’ professional governance and development, that's the right thing to do.”
Magnet appraisers visited and conducted interviews with nurses, physicians, leaders, and care team members. They subsequently recognized Emory Clinic for excellence in quality of care in its ambulatory surgery centers, opportunities for nursing professional development, and a fair and just culture environment where nurses practice.
Going forward, Magnet standards represent “our North Star,” Gilland says.
“We have a responsibility to direct and guide newer nurses, but not overwhelm them,” adds Gilland. “Emory nurses practice at a high level, which the Magnet designation exemplifies. We have a responsibility to share that expertise with others.” — Michelle Hiskey
with family and friends. She is survived by a daughter, two sons, five grandchildren, and three great-grandchildren.
Beth Singel 96N is team leader of neurosurgery at Children’s Health Dallas, where she has worked for more than 23 years.
Brandy Wendler 07N 09MSN joined the Virginia Center for Plastic Surgery as a master’s prepared nurse aesthetic specialist. The center serves patients in Northern Virginia and the Washington, D.C., area.

Whitney Thornton 19N is a 2022–2023 Nurses Educational Funds Scholar. She is the first

recipient of the Terry Fulmer Scholarship, named for a lead ing expert in geriatric nursing. She is enrolled in the adult gerontology primary care nurse practitioner program at Duke University, where she is also seeking certification in veterans health care. She works at the VA Clinic in Tallahassee, Fla., as a Patient Aligned Care Team RN manager in primary care.
Alexis Perkins 20N began working as a neonatal intensive care nurse with Emory Healthcare in June.
Viviana Coronado 15Ox 18C 22N passed the NCLEX and now works in the emergency depart ment at Emory Decatur Hospital.
Judith (Judy) C. Sundberg
51N of Atlanta on August 20, 2022. She married Richard Sundberg shortly after graduating from nursing school. They settled in her hometown of Jacksonville, Fla., and began to raise a family. They later moved to Tennessee and South Carolina before settling in Augusta, Ga. While in Augusta,
she worked in private practice after receiving a master’s in mental health nursing from the Medical College of Georgia.
Judy and Richard retired to Jacksonville in 1990. Following his death, she moved to Atlanta to be near her daughter. Judy excelled in china painting and won awards for her work, which was featured in magazines and museums. She enjoyed travel, holidays, and celebrations
Ann Garner Rinaldi 52N of Atlanta on February 21, 2022, at the age of 80. She received her BSN degree from Emory, an MS degree in nursing education from St. John’s University, and nearly completed a PhD in curriculum and instruction at Georgia State University. Ann grew up in Atlanta’s Buckhead community. Her nursing career spanned more than 50 years, primarily in teaching and working with staff and patients. She loved teaching the most. After retiring, she became a professional artist and volunteered as a docent at the Oglethorpe University Museum of Art. She took art courses at Oglethorpe and gave workshops in conscious aging. For the last 40-plus years of her life, she worked with recovering alcoholics, primarily women. Ann is survived by a daughter, two grandchildren, and several extended family members.
Muriel Kaiser Taylor 53N of Greenville, S.C., on August 25, 2022, at the age of 91. A native of South Carolina, she attended Newberry College prior to receiving her BSN degree from Emory. She was a member of Immanuel Lutheran Church in Greenwood, SC. She is survived by two sons, two daughters, a sister, seven grandchildren, and two great-grandchildren.
Carol N. Worley 53N of Marietta, Ga., on December 2, 2021, at the age of 90. She was born in Marietta and remained a lifelong resident of Cobb County. She attended Wesleyan College before receiving her BSN degree from Emory. She
married her husband, Dan, in 1953 and practiced nursing before and after raising their family. Carol was active in the Cobb-Marietta Junior League, the Cherry Laurel Garden Club, PTA, and Girl Scouts. She also served the Marietta First United Methodist Church, which was a special part of her life since childhood. She is survived by three daughters, nine grand children, 13 great-grandchildren, and numerous nieces, nephews, and family members.
Nancy S. Hartley 54N of Lilburn, Ga., on July 15, 2022, at the age of 90. A native of Johnson City, Tenn., she moved to Atlanta in 1950 and became a proud graduate of the Emory University School of Nursing. She worked for Emory University Hospital as an OB/ GYN nurse and later at Emory Rehabilitation Hospital. Nancy raised two children on her own following the death of her hus band, Virgil. She enjoyed read ing and spending time with fam ily. She loved animals, especially cats, and was also fond of beach trips and sports, especially golf, basketball, and tennis. Nancy remained a country girl at heart. She is survived by a daughter and son, two grandchildren, and two great-grandchildren.
Helen M. O’Connor 55N 57MN of Atlanta on July 13, 2022, at the age of 90.
Mozelle Liner 63N of Phoenix, Ariz., on October 7, 2010, at the age of 80. She lived most of her life in Haywood County, N.C., where she practiced nursing and attended Ratcliff Cove Baptist Church in Waynesville. She also taught nursing at Southwestern Community
College in Sylva, N.C. She lived in Arizona for seven years.
Francis “Frank” A. Creegan 68N of Gainesville, Ga., on August 28, 2021, at the age of 78. Born in Scotland, Creegan moved to North Arlington, N.J., when he was 7. He served in the U.S. Army during Vietnam. Following his military service, he became a trailblazer as the first male BSN student to attend nursing school at Emory. After completing his degree, Frank spent 30 years serving Hall County in many different positions at Lanier Park Hospital until his retirement. He was an amazing and devoted father who loved his children dearly. He is survived by a daughter and son.
Editor’s note: The Spring 2022 issue of Emory Nursing stated that Frank Creegan received an MSN degree, which was incorrect. He was the first male BSN nursing student to enroll at Emory and graduated in 1968.
Jayne Gosnell Helm 68MSN of Raleigh, N.C., on August 7, 2022, at the age of 80. She was born and reared in New Jersey and went on to earn a BSN degree from the University of Virginia (UVA) School of Nursing and an MSN degree from Emory. She taught nursing at Columbia University and UVA. She married for the first time in 1969 and lived in Hawaii, Chester, Va., and Columbia, S.C., where she raised two children. After divorcing, Jayne graduated from law school in 1989 and practiced family law and then medical malpractice defense. In 1997, she moved to Mount Pleasant, S.C., where she started a solo practice focused on elder and probate law. She also served as an associate probate judge in Charleston, S.C. She retired from law practice in 2010 following a massive stroke and
moved to Raleigh to be closer to family. She spent her retirement years with her husband, Michael Joseph Helm, who never left her side. Jayne was a skilled pianist, gourmet cook, gardener, and jigsaw puzzle enthusiast. She is survived by her husband, a daughter and son, two grandchildren, a brother, and other family members and friends.
Helen Elizabeth Everett 75N of North Carolina on March 23, 2022, at the age of 78. Helen completed bachelor’s and master’s degrees in nursing and taught as an instructor at the VA Hospital, East Carolina University, and Wake Technical Community College. She attended the Church of Jesus Christ of Latter-day Saints for many years. She is survived by two nieces, three nephews, and other close family members.
she loved most in Crystal Lake, Wis. In 2009, she received an MSN/MPH degree from the University of Illinois in Chicago. In 2020, she retired as a program coordinator of health screening disease management after more than 25 years of service with the Cook County Department of Public Health. After retiring, she focused on her family, traveling, and spending summers lakeside in Wisconsin. Nancy is survived by her husband, four children, two grandchildren, and many other family members, including her dog, Belle.
Lauren Knight Mason Gueriera 91N of Glenwood Springs, Colo., on August 25, 2022, at age 53, following a two-year battle with colon cancer. An Atlanta native, Lauren practiced nursing at Grady Memorial Hospital and Inner Harbour Hospitals before moving to Colorado, where she continued to practice with Denver Public Health. She found her true home in Colorado, where she met her husband, Mike Gueriera. She received her MSN degree from Georgetown University and was certified as a family nurse practitioner. Lauren worked tirelessly to advocate for women and children, primarily as a Sexual Assault Nurse Examiner at Valley View Hospital, the Children’s Advocacy Center at Childhelp River Bridge Center, and Sacred Cycle. In 2018, she joined Premier Medical Center, where she treated her patients and coworkers like family. She is survived by her husband and son, and Yoda the Chihuahua.
Chatsworth, Ga. She is survived by Arthur, her husband of 43 years, two daughters, and three cousins.
Anne Byrd Free 97MSN of Fayetteville, Ga., on July 1, 2022, at the age of 67. Born in Pensacola, Fla., Anne received a BA degree in psychology from Huntington College in Alabama. While raising her two children, she completed a BS degree at Georgia Baptist College of Nursing and an MSN degree at Emory. She practiced as a family nurse practitioner and ended her career teaching health occupations at the high school in Lovejoy, Ga. She is survived by her daughter and son.
Kendra Monique Lumpkin 22N of Humble, Texas, on July 27, 2022, at the age of 30. She was a student in the Master of Nursing Pathway to Master of Science in Nursing program.
Nancy Ruth Angelopoulos 78N of Arlington Heights, Ill., on July 31, 2022, at the age of 66. She passed away at the home



Beverly Head Sutton 95N of Dalton, Ga., on July 23, 2022, at the age of 71. She was a wellknown and highly respected member of the health care communities in Dalton and
Please send your news and latest contact information to alumni@ nursing.emory.edu. Or visit alumni.emory.edu/ updateinfo.php.



Emory University Alumni Records Office 1762 Clifton Road NE Atlanta, GA 30322
Hear from our students about the Emory Nursing Learning Center.


In every focus group and every meeting about the design of the Emory Nursing Learning Center our focus —our mantra — was, ‘What is in the best interest of the students?’ We have created each corner of this space to prepare visionary leaders in nursing.
DEAN LINDA MCCAULEY