Mass Eye and Ear 200th Anniversary
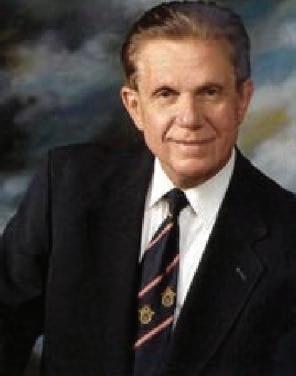
Herbert Silverstein MD, FACS










Mass Eye and Ear 200th Anniversary



Herbert Silverstein MD, FACS




Silverstein Institute




President Ear Research Foundation





Mass Eye and Ear 200th Anniversary
Herbert Silverstein MD, FACS










Mass Eye and Ear 200th Anniversary



Herbert Silverstein MD, FACS




Silverstein Institute




President Ear Research Foundation




Herbert Silverstein MD, FACS










Sixty-one years ago, I walked into MEE as a first-year resident applicant. MEEI was considered one of the best hospitals to train for otolaryngology. I never thought it possible to be accepted there. And no way that I could envision I would be standing here at the 200th anniversary celebration.






Sixty one years ago




I walked into the Mass Eye and Ear Infirmary








No way I could have imagined being here for the 200th year celebration of the MEE







Gene Myers who was one year ahead of me at Temple U medical school advised me to apply to MEEI where he was training. I was ready to go to Temple U for my residency with Gene’s Father, David Myers who was head ENT Dept there.




My father was a professor of neurology at Temple, he encouraged me to do research while in Med school. I studied the vestibular system in cats.

Alexander Silverstein M.D.























Was always interested in research and encouraged me to pursue research



My father was Neuropsychiatrist and professor at Temple University Medical School







I felt so honored to be accepted by Dr. Harold Schuknecht as a resident. Especially because I was 1.5 hours late for my interview. I got lost driving around Boston. Fortunately I had a successful interview and we had research using cats in common.


Harold Schuknecht, MD 7









Harold Schuknecht, MD





HFS was a world class histopathologist and author of three additions of Pathology of the ear.











• Chief of Otolaryngology, Mass Eye and Ear Infirmary, 1961-1987











World class histopathologist Author of three editions of PATHOLOGY OF THE EAR







He invented the fat wire prostheses for otosclerosis. He was a great teacher, surgeon and mentor. He always called me Herbie.

Harold Schuknecht, MD
























Great teacher, surgeon, and mentor








Always called me Herbie 9











I owe my career mainly to Gene Myers, he was a mentor and friend who coached me through med school and residency. He tried to prevent me from making mistakes and screwing up.






I was always interested in research and development. I always liked to find the best and improved ways of doing things.















I was always interested in research and development



I searched for ways to do procedures easier, using a more direct approach that was effective.







Three Principles of Innovation





























Dr. Schuknecht encouraged me to do research while in residency. He said, “Herbie I want you to be an expert in Meniere’s disease, and want you have a lab to do research on inner fluids which I think has something to do with the disease process. Here is $5000 to get started until you get an NIH grant. Also, Herbie it is very important that you make a contribution to science.” I had a research fellow and a technician to manage while being a fulltime resident.











• HFS encouraged me to do research










• He offered me a lab to study inner ear fluids





• Gave me $5000





• Herbie I want you to be expert in Meniere's disease







• Very important to make contribution to science






• I had a research fellow and technician






Mike Paparella knew Sigur Rauch of Dusseldorf Germany and said I had to learn microchemical techniques from him. HFS sent me to Germany for three weeks to Sigur Rauch to learn how to analyze small samples of inner ear fluid.











Mike Paparella M.D., F.A.C.S.















I worked till 10 or 11PM many nights and developed the diagnostic labyrinthotomy procedure or inner ear tap where we took inner ear fluid from patients’ to help diagnose acoustic neuroma.



We could diagnose acoustic neuroma because there was a high perilymph protein concentration vs Meniere’s disease that had high potassium levels because of the endolymphatic hydrops. This was before MRI and CT scans.




One day I was doing experiment on a cat trying to simulate a Meniere’s vertigo attack by putting endolymph type of fluid in the inner ear. HFS theory was that a rupture in the inner ear caused a flooding of perilymph space with high potassium endolymph that caused the vertigo attack in Menieres disease. The cat developed nystagmus like a Meniere’s attack. I was so excited that I ran to the private offices where HFS was seeing patients and interrupted him and said you have to come to the lab and see what I did. And he left patients and came with me to the lab up four floors .















Put endolymph like fluid into cat inner ear
















Developed Meniere like vertigo





Interrupted HFS while seeing patients and asked him to come to lab








The energy at the MEEI was intense. Constantly looking for better ways to improve patients’ quality of life.



Energy at MEE was Intense



















To make quality of life better for patients



As a first-year resident with Roger Lindeman a second year resident.







We developed the arrow tube which was one of the first flanged tubes to aerate the middle ear in chronic serous otitis media. The tube was designed to stay in place for months.



Serous Otitis Media



“Arrow Tube” with Roger Lindeman













At the same time, I developed an anesthetic of the Tympanic membrane which was pontocaine base powder dissolved in alcohol which we still used today for myringotomies.






Anesthetic of Tympanic Membrane









Pontocaine base power dissolved in alcohol













Worked for several hours



Still used today for myringotomy and PE tube






Danny Miller who was surgeon at MEEI had residents on his service. Dr Schuknecht told the us that residents were supposed to be doing a significant portion of the surgery on private patients. Danny was doing a tympmastoid and after several hours he left the room, and turned it over to his associate.

Danny Miller M.D.


















• Surgeon MASS EYE and EAR

















Tom Klein. I didn’t get to do anything during the case and complained bitterly to Dr Klein while he was kicking me under the table. Little did I know that the scrub nurse was Dr Millers personal nurse. Well, she went back to Danny and told him what I said. From then on Danny black balled me until Gene Myers who was Danny’s favorite saved me and Danny then let me start doing procedures again.

Tom Klein M.D.






Sunday school was a great part of the residency training. Gene was doing monkey business, training monkeys on Sunday and discovered by accident that Dr Schuknecht was looking at temporal bone slides on Sunday morning with his research fellows. Gene invited himself to the teaching sessions and told me to come also. We had a great time looking at slides trying to correlate the clinical picture and the pathology. At lunch time HFS would take us to the union Oyster bar. Where he would smoke a large cigar.























These were the golden years of otology and helped shape my career.






Other People who helped mold me were Dick Gacek and Bill Montgomery, Mike Paparella and Nelson Kiang.

Dick Gacek was two years ahead of me in residency. He was a great teacher and researcher. After residency he went into the private offices with HFS and Monty. When House did the first cochlear implant I said this was the most important breakthrough in our specialty. Dick responded with buzz, buzz, buzz. We had an altercation about the importance of the cochlear implant.

One day I asked Nelson a research question. He said sure I will see you here at 3 am. Of course I went there at three AM.

Nelson Kiang PhD






My fellow residents were Joel Bernstein, MD, who was very interested in research, and we did many projects together. Joel went into private practice in Buffalo. Charlie Gross, MD became a professor at University of Virginia. John Knowles, MD went to Vermont to practice. Peter Van Orman, MD went into private practice in a Boston suburb.

Residents 1966







Joel Bernstein, M.D.







Charles Gross, M.D.







Peter Van Orman, M.D.





John Knowles, M.D.




When I finished residency I was obligated to enlist in the Army for 2 years. But I was able to keep the research lab going at MEEI going while I was serving in Hawaii. After two years I came back to join the private office for three years.























Kept MEE research lab going Back MEE for three years



During my teaching years at MEE, I had the pleasure of taking KJ Lee a resident through his first tympanoplasty.
KJ was first to use computer punch cards to do clinical research. I knew then that KJ would be a leader in our field.







Then I joined Gene Myers at U of P for three years. Gene got the chairmanship of University of Pittsburg and wanted me to join him.


















research lab 3 years











At Penn, I met Jeff Harris, MD who was a medical student and told him to go MEE for his training. Look at what a great career he has had.

Jeff Harris M.D., F.A.C.S.






In 1973, I decided to retire from academic medicine at 38 and move to Sarasota, Florida.















Herb retired at 38 from academic medicine to Sarasota

















HFS was appalled by my choice and said what’s a Sarasota. Never heard of it. And you are no longer my favorite son. He wouldn’t speak to me for years.











Dr. Schuknecht was appalled at my decision













I won back his respect after I invited him to be guest of honor at the first Neurological Surgery of the Ear meeting in Sarasota 1977.



















Made him guest of Honor at first Neurological Surgery of the Ear Symposium in Sarasota 1977





20th anniversary party of my move to Sarasota He roasted me. Remembered every detail of my life.



HFS surprised me at my 20th anniversary party of being in Sarasota by coming to roast me. He had details of my entire career.



When moving to Sarasota I was not welcomed by the ENT physicians, they told me that another ENT was not needed in this small town. But If I did come, I would be on my own with no coverage.











Local ENT physicians said I was not needed, not wanted, and told to move on No coverage














I had no money, an old corvette, and one suitcase.



There was no place to rent but I found a 1000 sq ft storage closet in an ortho office that I renovated. The Bank lent me $100,000 on my signature. I took call 24/7. Somehow I persevered but retirement didn’t work out so well.

Started practice in Sarasota 1974













No space to rent










Found 1000 sq ft closet to renovate into office








Borrowed $100,000 from bank

Took call 24/7





Persevered

This was my first office, only kidding









I started the non-profit organization, the Ear Research Foundation in 1979. This was the original 1000 sq ft building.




Our mission was doing Research into finding better ways to treat hearing loss and vertigo, Education of physicians and the public and community service taking care of indigent patients.

This our 49th fellow Allan Young who is in practice in Las Vegas.







Clinical fellowship started 1983




The Clinical fellowship program began in 1983, and this year we celebrated 50 fellows trained and 50 years in practice in Sarasota.




















50 fellows trained in Otology/ Neurotology 50 years in practice Sarasota




This is the Schuknecht conference room with pictures of the 50 fellows.


Here are the fellows at recent 50-50 celebration.
50-50 Celebration


This is the 30,000 sq ft Si building we built in 2003.


Silverstein Institute

Occupied Feb 21, 2003





This is a 3-D picture of the building.
























Now after 50 years Gene and I are back together endowing chairs at MEE.




































Gene recently visited me at Silverstein Institute.



MEEI launched my career, and gave me the foundation to develop new treatments and surgical procedures. Some of which I would like to show you now.















Gave me foundation to develop new treatments




















For long term middle aeration, the SPAT silicone tube was designed to go thru the bone of the ear canal into the middle ear. This procedure was patented and is still being used today.



































































Training young docs to do surgery near the facial nerve prompted me to improve the Gaza facial nerve stimulator to a facial nerve monitor. There was a Sensor attached to the

















A SACS device that electrifies the drill to help identify the facial nerve when drilling close to the facial nerve.





















I was doing a biopsy of a posterior fossa tumor through the retrolab approach which is going into the posterior fossa between the labyrinth and lateral sinus. I noticed the I could see the eight nerve easily and the Retrolab Vestibular neurectomy was born. This approach was improved when we entered the post fossa behind the lateral sinus. 250 procedures were done. This stopped the vertigo attacks and preserved hearing in many patients.














Dr Norrell a neurosurgeon and I organized the first Neurological surgery of the Ear meeting in 1977 where 50 neurosurgeons and 250 oncologists came together. After that meeting we had five meetings every other ear. At that time Neurosurgeons didn’t think much of ENT physicians.



















Organized first skull base conference in 1977


















Held five bi annual Neurological surgery of the ear conferences





Dr Norrell had significant impact in creating the team approach to skull base surgery. At first he wanted to stop me from doing any neurotologic procedures because I was invading his turf.


Horace Norrell M.D.


























Dr. Horace Norrell had significant impact creating team approach in neurotologic surgery





In fact, Dr Norrell cancelled my first middle fossa vestibular neurectomy. The next day, he checked me out with DR Ojemann at Mass General, and Dr Langfitt at U of Penn. They told him don’t stop Silverstein, he is qualified to do neurotologic procedures. After that he let me do the procedure that he cancelled and we became a team for 25 years, and wrote many papers.






Dr. Norrell Cancelled My First Middle Fossa Vestibular Neurectomy
















• He checked me out at Mass General and Penn






• Silverstein qualified to do neurotologic procedure’s




• We became a team for 25 years



• Wrote many papers








In 1996, I developed the MicroWick to allow patients to self-instill medications into the inner ear for one month. It Is used with Dexamethasone ear drops 4mg/cc in Meniere’s disease to reduce symptoms of pressure, tinnitus and vertigo. It is also used for Sudden deafness along with oral Prednisone.




















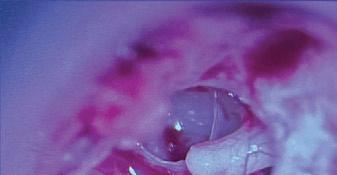
I developed the Laser Stamp procedure for minimal Otosclerosis at the fistula antefenestrum that didn’t require a prosthesis. I asked HFS if it would last and he said yes if you pick the right cases.
























For minimal otosclerosis of the anterior footplate No prosthesis needed 75 cases done




Laser probe performing Anterior crurotomy



LASER STAMP





































Laser transection of the anterior portion of foot plate. if the otosclerosis is confined to fissula antefenestrum the stapes becomes mobile. If it is fixed we enlarge the opening and place a prosthesis.


















Linear laser stapedotomy: anterior onethird of footplate



















I developed cartilage reinforcement of the round window for SSCD. The results are being presented at upcoming AAO in Miami.





• The round window reinforced by tragal cartilage and perichondrium






Also developed a surgical procedure to reduce hyperacusis by temporalis Reinforcement of the Round and Oval windows.










Temporalis Fascia Reinforcement of the Round and Oval Window








There are four types of sound hypersensitivity. Hyperacusis, recruitment, Misophonia, and phonophobia. The surgery is designed only for hyperacusis.
































Hyperacusis is a condition where a person cannot tolerate normal sounds. They become anxious and avoid places like the movies, restaurants and sporting events. It often affects their quality of life, 6 - 17% of population are affected. Noise trauma in history 62%



















• A condition where a person can not tolerate normal sounds



• They become anxious and avoid places like the movies, restaurants and sporting events








• Often affects their quality of life







• 6 17% of population affected




• Noise trauma in history 62%

Normal LDL is 90-100Db







Their loudness discomfort level LDL is below 90Db.
Treatment: is using ear plugs, tinnitus retraining therapy (TRT), cognitive therapy. Non surgical treatment may not be effective.











Uncomfortable loudness level (LDL) below 90dB Normal LDL 90-100 dB

















Treatment: ear plugs, tinnitus retraining therapy (TRT), cognitive therapy, long term treatment Results are variable and may not be effective







Cause often unknown
Noise trauma in 62%
Cochlear trauma
SSCD
Perilymph fistula
Adverse reaction to medication
Hypermobility of stapes - new finding

















• Often unknown


• Noise trauma 62%




• Cochlear trauma





• SSCD



• Perilymph fistula




• Adverse reaction to medication











• Hypermobility of stapes new finding




Possible mechanism of Hyperacusis
Hypersensitivity of the cochlea to sound.
Hypermobility of Stapes.

















• Impaired neuroplasticity in noise suppression






Impaired neuroplasticity in noise suppression.

• Hypersensitivity of the cochlea to sound



• Hypermobility of Stapes






Temporalis fascia is shown reinforcing the round window
Reinforcement
Round Window
RW Reinforced




Reinforcement
Oval Window
OW Reinforced




Temporalis fascia is shown reinforcing oval window.




Reinforcement
Oval Window
OW Reinforced













Results divided into two discomfort groups. Moderate discomfort to sound with LDL above 70dB, 52 patients. And High discomfort to sound with LDL below 70dB, 21 patients.








Divided patients into two loudness discomfort level (LDL) groups:







52 LDL Group above ( > 70dB)













Moderate discomfort to sound














21 LDL Group below( < 70 dB)












High discomfort to sound




In the moderate discomfort group 81%, are happy with the result and would recommend the surgery. The result lasted in many patients.















LDL Group >70 dB:











Moderate discomfort















80.8% would recommend surgery




72.9% stated improvement lasted









• Follow up 1 6 years




In the high discomfort group only 47% would recommend the surgery.














High discomfort





LDL Group <70 dB










47.6% would recommend surgery







To improve the results in the high discomfort group we are now enhancing the amount of fascia for reinforcement.










• Enhanced reinforcement of oval and round window









• Patients with LDL<70dB (high discomfort)









Extra temporalis fascia is placed over the reinforced windows.





Fascia is then placed beneath the posterior tympanic membrane.



The results in last 4 of 5 patients have been encouraging.






Four



of five patients have had good results






In the last patient LDL went from 65 pre op to 95 post op.




Well this is my story. I have enjoyed the specialty of Otology/neurotology and never felt it was work. I feel honored to have had the privilege of training 50 fellows and counting, and contributing to science as I was ordered to do by HFS. All this has improved the quality of life for many patients.








This is My Story












Have enjoyed specialty of Otology/Neurotology


Training fellows











Making contributions to science


Improving quality of life for patients











And owe my success to the training I received at MEE.

















