DAILY NEWS





















The EACTS Annual Meeting was last held in Lisbon in 2019 just before the COVID pandemic shut down the world. Its impact has been felt for the past few years, but there is no doubt that the Annual Meeting today is stronger than ever, attracting thousands of members of the cardiothoracic community from all corners of the world.
submitted for presentation. A selection of the highest-ranked abstracts will be shared with delegates during two innovation sessions taking place on Friday. This includes presentations on the use of XR, AI and physics-based modelling in thoracic surgery as well as robotics in mitral valve surgery.
Improving
Three


We bring different experiences and perspectives, but we share one vision: to achieve better patient outcomes. The Annual Meeting provides an important platform to showcase the latest science and clinical data, which are critical to our evolving field, but it is also truly special to be able to spend time together, sharing our thoughts and experiences on the issues that we face in our daily practice.
We are joined by members of the cardiothoracic surgical community from across the world: surgeons, allied health professionals, researchers and scientists, colleagues from industry and many other professionals, giving us an opportunity to meet and learn from each other.
This year I am delighted to also welcome more pre-trainees to the Annual Meeting, part of EACTS’s commitment to supporting the next generation of surgeons. The scientific programme includes bespoke sessions specifically for pre-trainees to ensure they receive the guidance and knowledge they need to thrive in their early careers. We have provided new educational grants to enable pre-trainee members to attend the Annual Meeting and support their career development.
As we invest in our people for tomorrow, we also look to the future of cardiothoracic surgery and to the innovations which have the potential to change the cardiothoracic landscape.
Our Innovation Summit earlier this year was a huge success, with over 55 high quality abstracts
In the Auditorium later this morning we will also be introduced to a new robotically enabled structural heart platform, which is just one of many user-centred medical products developed by our honoured guest, Amy Kerdok. With over 16 years’ experience in product development, I am delighted she can join us today to share some fantastic insights into the process of innovation.
These disruptive technologies have the potential to reshape our specialty, so these sessions are not to be missed. But as well as looking to the future, it is important that we also keep up to date with changes impacting our daily practice now.
I strongly recommend this afternoon’s session ‘Updated EACTS guidelines’ to learn more about major updates to guidelines on topics including perioperative medication and patient blood management. The ‘Trial Update Session’ on Saturday is an opportunity to dive deep into the latest data from current trials such as 5-Year Data of the PARTNER 3 and EVOLUT-LRT trials and 1-Year results of the DEDICATEDZHK6 trial, and get insights from experts in the field on how these will impact our practice.
Over the next couple of pages our domain Chairs share details of some of their highlight sessions. I am immensely grateful for their work, alongside their task forces, to develop another brilliant scientific programme.
Thank you, once again, for travelling to Lisbon. This is the highlight in the EACTS’ calendar – a time for you to make new connections and meet old friends, but above all a time for learning and discovery. Enjoy the Annual Meeting.
Delegates arrived in Lisbon yesterday to learn more about the latest surgical advances that will impact clinical practice in the future. This year’s Techno-College, a full-day event which traditionally marks the first day of the EACTS Annual Meeting, included two concurrent streams – cardiac and thoracic – and featured live demonstrations of new technologies and techniques as well as expert insight to support better patient outcomes.
The Techno-College programme is designed to cover all experience levels, helping those at the start of their surgical careers understand key concepts and providing guidance on the practical application of new technologies. For more experienced surgeons, TechnoCollege is an opportunity to refine skills and explore complex surgical techniques alongside leading experts.
For those keen to keep pace with the evolving landscape of cardiothoracic surgery, Techno-College is an unmissable day.







A new technique for full arch replacement, the latest left ventricular assist device and new technologies in paediatric cardiac surgery were just a few of the innovations showcased as part of the cardiac stream at this year's Techno-College.
The full-day programme highlighted some of the trends and advanced concepts that have potential to change the way certain procedures are performed in the future. This includes new options for transaxillary aortic valve replacement and frozen elephant trunk, which were amongst a number of procedures demonstrated live to delegates during Techno-College.
For the first time in Techno-College history new technologies in paediatric cardiac surgery were part of the programme focusing, on minimally-invasive options to treat young adults.
The Ross procedure was the featured surgical technique, responding to renewed interest in this operation and new positive data from the US. Delegates were able to see firsthand reinforced Ross with beating-heart harvesting of pulmonary autograft performed as part of a live-in-the-box presentation for which Techno-College is renowned.

Marco Di Eusanio
Polytechnic University of Marche – School of Medicine Ancona, Italy
Frozen Elephant Trunk: think next step
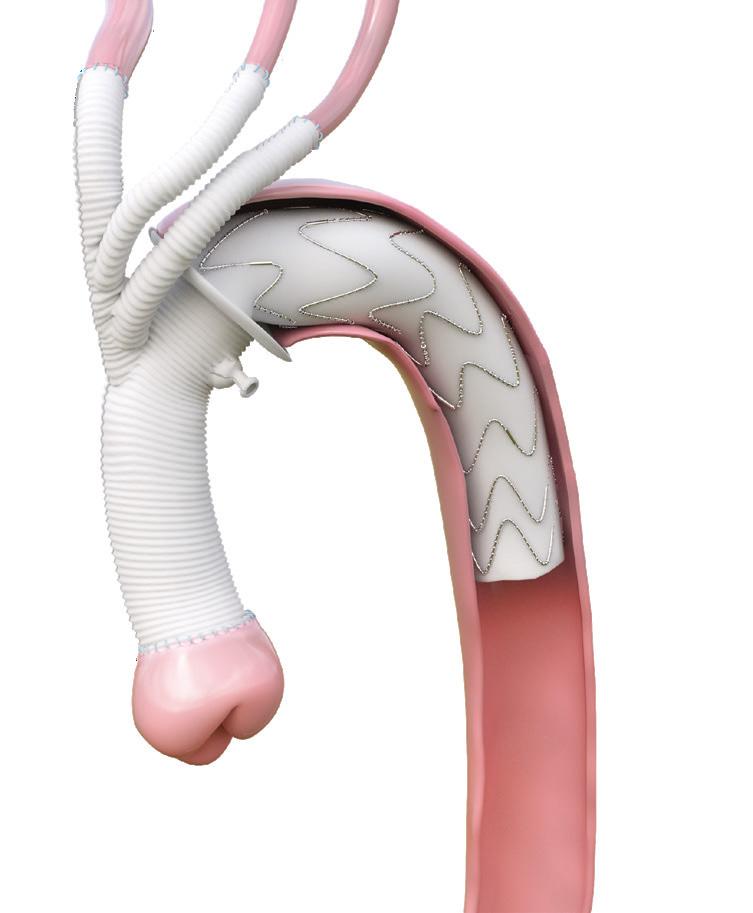
Aortic pathology is progressive in its nature and aortic reinterventions, proximal on the aortic root and distal on thoraco-abdominal aorta, are often required following a frozen elephant trunk (FET) operation. Therefore, it is crucial that primary FET operations adequately prepare patients for subsequent procedures. Currently available FET grafts frequently fail to achieve this goal because distal anastomoses are increasingly performed in zones 0, 1, and 2, resulting in a very proximal emergence of the arch vessel branches. This configuration can hamper both proximal root and distal endovascular thoraco-abdominal aorta repair (ETAR) reinterventions. Specifically, with the proximalisation of the side branches, access to the aortic root becomes hampered as it requires a very low aortic clamp.
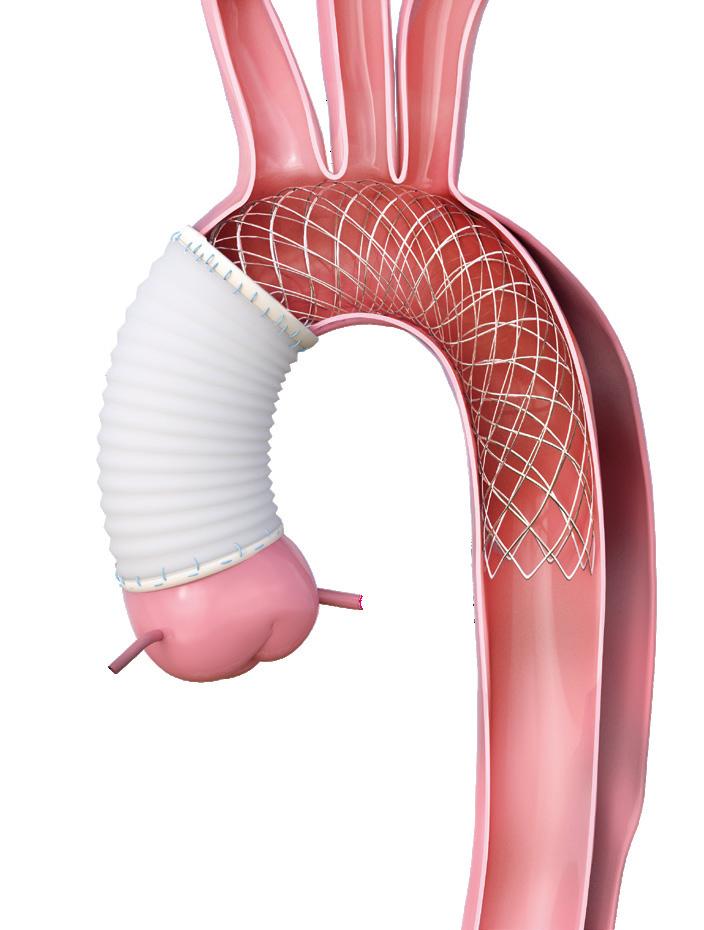
Additionally, ETAR can be more challenging as the visceral vessels are arduously cannulated from an upper body access due to the double angulation generated by current FET grafts (figure 1A-B). Here, we present a new custommade Thoraflex graft, named T-NEXT (Terumo Aortic, Inchinnan, Scotland), specifically designed to facilitate proximal and distal reinterventions (figure 2).
Unlike the conventional proximal-to-distal disposition of the neck-vessel branches, the T-NEXT graft features a distal and transverse arrangement of these branches. This design allows for a longer proximal graft segment, free from other prosthetic structures, and enables a more comfortable distal aortic clamping during root reintervention.
Additionally, this new branch arrangement provides a straight antegrade route for wires destined for upper access to the visceral vessels, simplifying ETAR (figures 2 C-D and 1). We believe the T-NEXT graft represents a promising advancement in FET surgery, addressing the limitations of current devices by facilitating both proximal aortic root and distal ETAR reinterventions.
As interest in cardiac robotic procedures continues to increase, and with more companies entering this market, Techno-College offers a fantastic forum to discuss the latest advancements in the field of robotic cardiac surgery and learn more about the current developing platforms.
Procedural analysts were on hand to provide their expert analysis during the live procedures, which encouraged great audience interaction and lively discussion.


Kim Hyun Koo was last year’s winner of the Techno-College Innovation Award in recognition of his innovative miniatured endoscopic C-arm with ultra-low radiation exposure for imageguided surgery. He outlines how work on this innovative device has progressed since winning the award.

What impact has the Techno-College Innovation Award had on the ongoing development of the miniatured endoscopic C-arm?
Receiving the Techno-College Innovation Award has been a great promotional asset and has provided significant help. Whenever I present on the endoscopic C-arm technology, I proudly mention that I received the Techno-College Innovation Award. I believe that in the future, this award will continue to have a positive impact on starting and successfully completing projects.
What feedback did you receive from the cardiothoracic community following your award success?
Since there are not many doctors in the cardiothoracic community involved in technology development, I

have mainly received encouraging feedback. Many colleagues have shown strong support for the commercialisation of the technology, which reassured me that we are developing the technology in the right direction to meet the unmet needs of surgeons.
What are the next steps for the ongoing development of the endoscopic C-arm?
Although I haven’t achieved commercialisation yet, I am continuously preparing for it. The next step involves researching the development of an endoscopic C-arm that can be installed on robotic surgical systems, in collaboration with a joint research team in Korea and a team from Harvard University.
In addition, I am working with the Harvard research team on hybrid contrast agents. Lastly, I am in the process of preparing to start my own company. By the next Annual Meeting, I might just show up as the CEO of my own company!
How will this technology help to achieve better patient outcomes?
This technology has the potential to improve the success rate of limited pulmonary resections and significantly enhance patient safety. Moreover, it can increase the success rate of minimally invasive thoracic surgery. Ultimately, it will lead to a better quality of life for patients.
Maximizing the internal orifice area expands treatment options for Today, Tomorrow, and The Road Ahead.








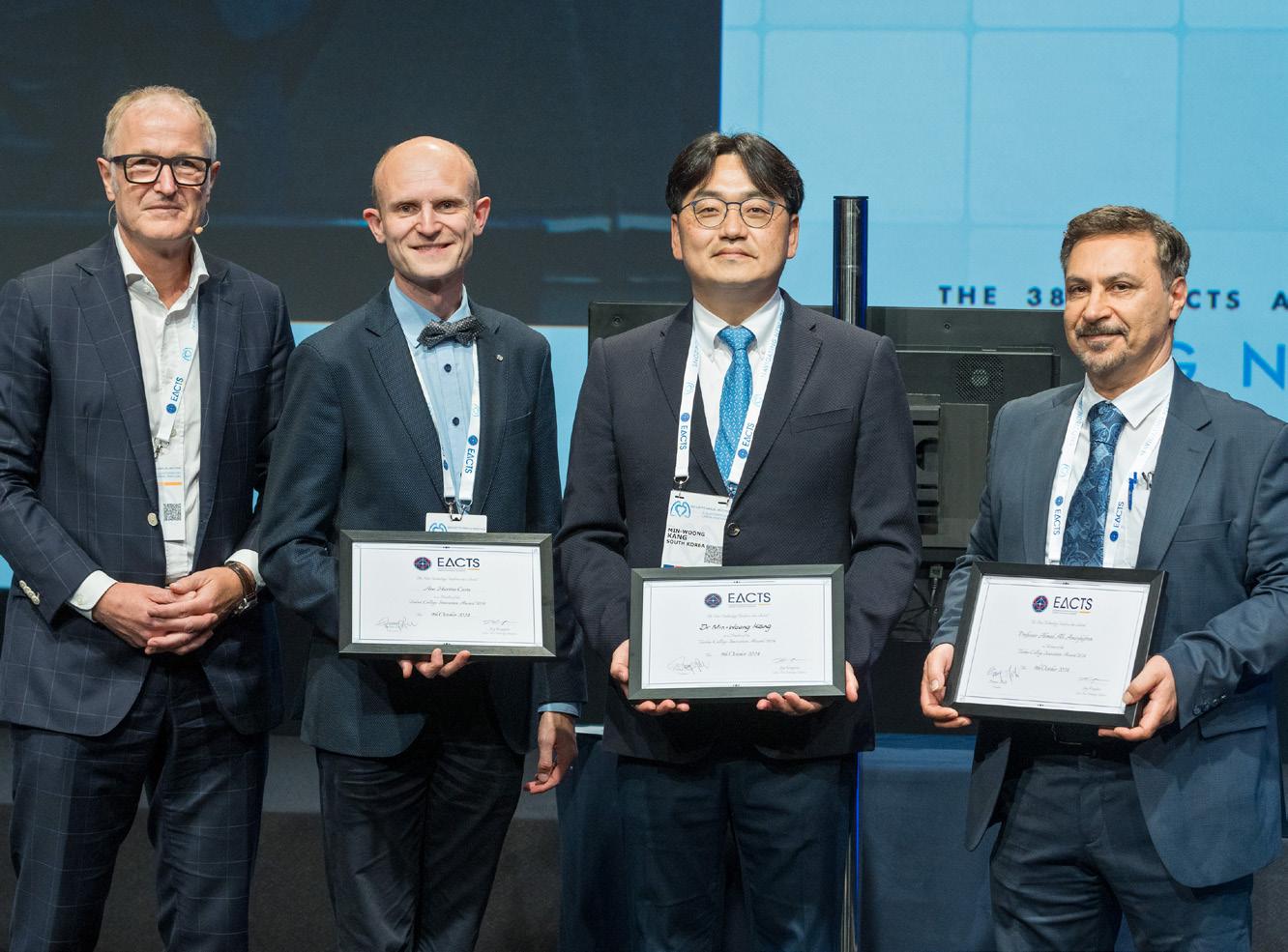
Congratulations to Ahmad Ali Amirghofran, winner of the 2024 Techno-College Innovation award in recognition of the SRAA valve, a stented Biologic Valve with the Native Right Atrial Appendage Tissue.
Commented on the award, Ahmad Ali Amirghofran said, “Being awarded the Techno-College Innovation Award is an incredible honor and a significant recognition of our work in advancing cardiac valve technology. This prestigious award acknowledges the years of research, innovation, and dedication that went into developing the stented right atrial appendage (SRAA) valve.”
Finalists:
Ana Martins Costa
RenOx: Combined Lung & Kidney Support in a Highly Integrated Artificial Lung Device
Min-Woong Kang
First Oncologic Specialty Linear Stapler: Novel Asymmetric Linear Stapler (NALS) for Accurate Pathologic Examination of Surgical Margins
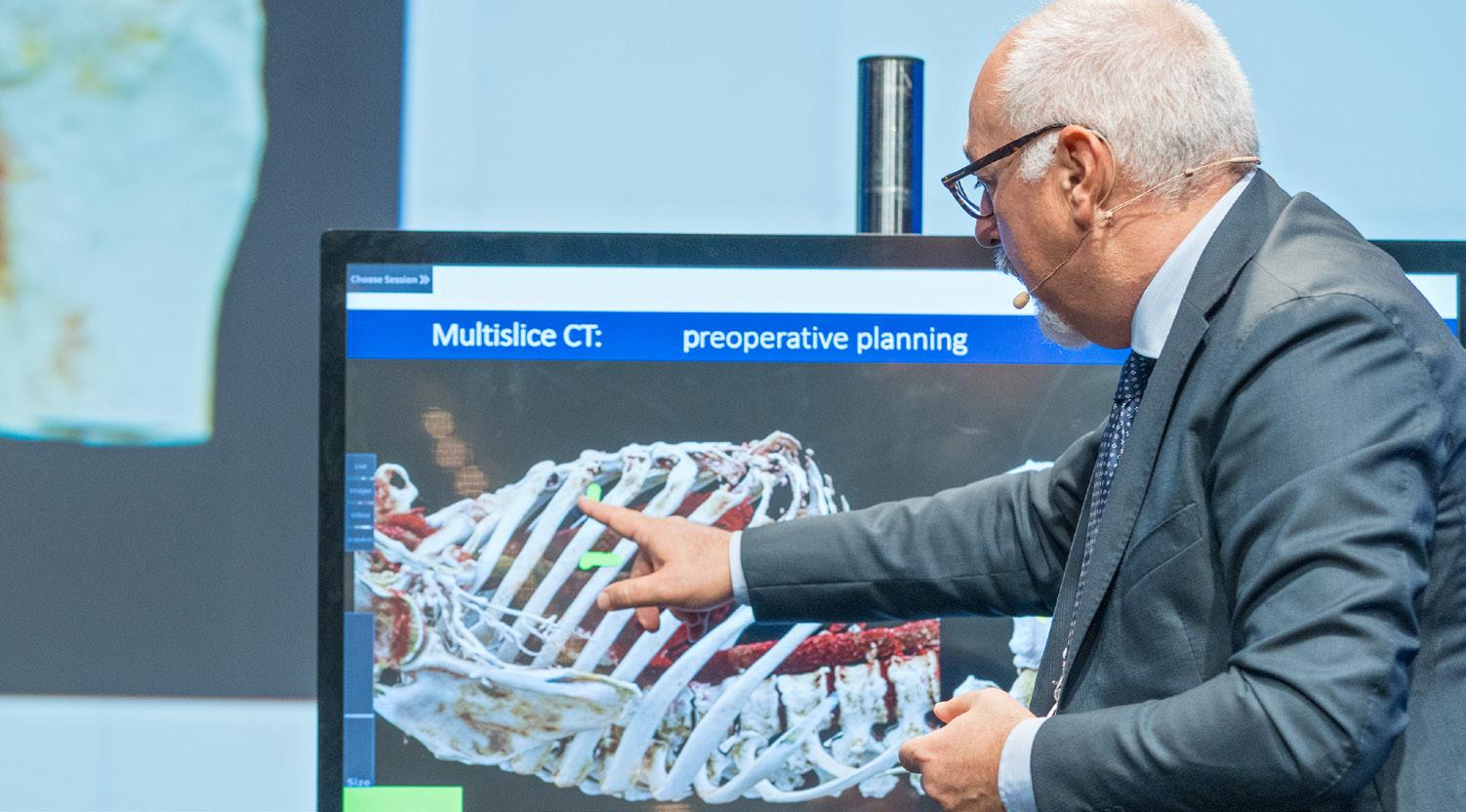
The thoracic stream of Techno-College kicked off with a showcase of the 3D reconstruction helmet, an exciting new platform that supports preoperation planning. Delegates were guided stepby-step through the process of 3D reconstruction to better understand the benefits of this technology, particularly for sublobar resection.
The opportunity to get hands-on experience working with the latest innovations is always a highlight of Techno-College. This year, delegates were able to advance their skills in the Integrated Technologies workshop which included several platforms currently used in clinical practice, including the Da Vinci robotic system.
Robotic segmentectomy featured in another interactive session led by recognised proctors including EACTS President Franca Melfi and Marion Durand, Chair of the Robotic Thoracic Surgery Task Force. A live-in-a-box segmentectomy enabled delegates to see new robotic technology in action through 3D glasses to ensure a unique experience. Endobronchial navigation is an interesting and exciting new trend in thoracic oncology, that is well suited to the practice of a modern thoracic surgeon. It is imperative that surgeons understand how these treatments are developing and engage fully with the processes involved.
In a session on endobronchial navigation on Wednesday afternoon delegates had the opportunity to see a demonstration of the Ion system, a new cutting-edge platform that allows the possibility of navigation to the target lesion, in a live-in-a-box bronchoscopy. Experts from the US also shared their insights on how to implement such a programme in a thoracic department.
Minimally invasive surgery and robotic surgical techniques have changed the dynamic of the operating room, but the development of non-technical skills is equally important. This year’s thoracic stream included presentations on non-technical skills as well as discussions surrounding ligation control of vessel as opposed to stapling, elevating surgeons’ skills and autonomy.
The friendly informal environment of Techno-College, with its combination of theoretical, and practical sessions, is always a fantastic way to open the EACTS Annual Meeting.


ACQUIRED CARDIAC DISEASE / CONGENITAL HEART DISEASE / THORACIC DISEASE / VASCULAR DISEASE

A lot of hard work goes into preparing the scientific programme for the EACTS Annual Meeting and, as always, I am indebted to the members of the Acquired Cardiac Disease Domain and the twelve task forces who provide their expertise and knowledge to deliver a very attractive programme that covers new aspects of cardiac surgery and includes some critical topics. We have so many interesting sessions planned that it is very difficult to choose specific highlights, but our task forces have selected some key sessions.
• 'Revolutions in coronary' surgery will be a fascinating session, taking place on Thursday. We will cover several topics including the use of AI to improve surgical performance, moving away from MACE as an endpoint in clinical trials, how advanced imaging could replace coronary angiography to guide CABG , and we will ask whether Ozempic will change the landscape for coronary surgery.
• The tricuspid valve was once called the forgotten valve, and now it gets everybody's attention, so I’m looking forward to Thursday’s focus session ‘Tricuspid disease: once forgotten, now all the rage’. This session covers the latest science behind the tricuspid valve, and looks at the different treatment options, for example surgical versus catheter-based techniques.
• We also have a session on robotic coronary surgery. It takes place on Thursday – don't miss it. The usual approach for coronary surgery is well known, but minimally invasive techniques are rapidly expanding and can obtain very good results. This session looks in detail at the options available and makes the case that robotic coronary surgery is here to stay.
• In an important session on Thursday afternoon, we explore the technical and technological evolutions in transcatheter, mitral and tricuspid valve procedures, looking at the latest evidence and considering what the future is going to look like.
• ‘Knowledge every Cardiac Surgeon should have prior to performing a CABG’ on Friday promises to be an interesting session, with a focus on coronary ischemia and reversibility of ischemia by improving regional myocardial perfusion.
• We expect lots of discussion during Friday’s video session on minimally invasive aortic valve replacement. There are various techniques available to perform either minimally invasive aortic repair or replacement. And there's still considerable debate about the advantages and disadvantages of each technique. This focus session will examine the long-term results and evidence of the different aortic valve replacement strategies and identify the best treatment option for a specific patient.
• We explore new science in a fascinating abstract session on Friday morning focused on the closure of the left atrial appendage, which is an important topic within atrial fibrillation.
• On Saturday a video session 'Mastering Mechanical Circulatory Support' will cover everything surgeons need to know on this topic, including standard and alternative LVAD implantation techniques, long-term mechanical circulatory support in failing Fontan patients, and total artificial heart implantation. This is one of a number of video sessions we have introduced this year.
This is just a snapshot of the focus and abstract sessions in this year’s fantastic scientific programme. Please also remember the e-poster sessions provide you with more high-quality science and there are opportunities to gain hands-on experience via the EACTS Learning Lab and industry learning labs. And, of course, it is also important we all find time to get together for some fascinating conversations.
PRESIDENT'S CHOICE:

Auditorium 1 / 08:30 - 09:30
Feasibility of Valve-in-Root
Transcatheter Aortic Valve
Implantation: A computedtomography analysis of 363 patients after aortic root replacement and repair
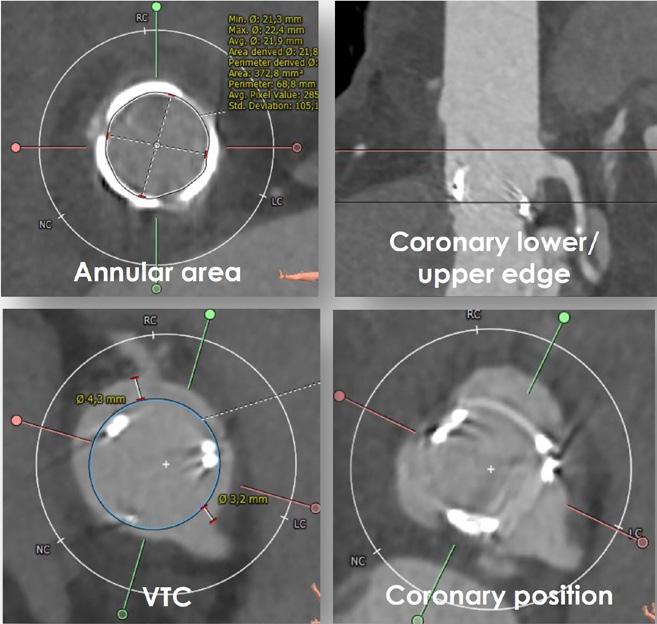
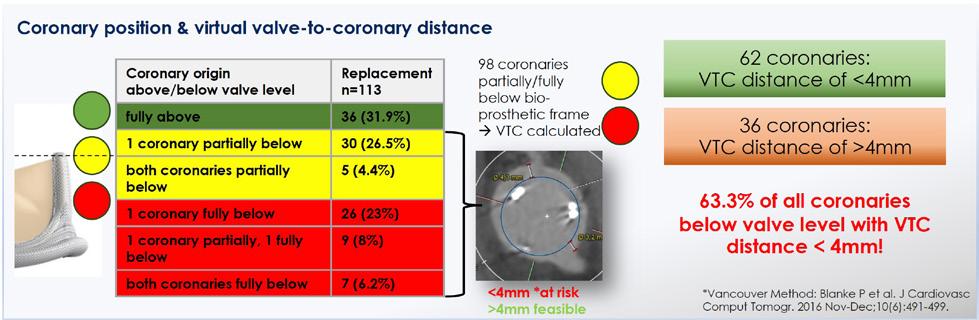
The aim of the study was to evaluate the feasibility of TAVR in patients that underwent biological root replacement or root repair. From 2012-2022, 760 patients in our institution underwent either a biological root replacement or root repair.
In 363 patients, postoperative CT scans (repair n=250; replacement n=113) were available and were analysed using the 3mensio Software, measuring annular area, coronary distance, coronary position in relation to the annular plane, and the valve-to-coronary distance. The main finding is that coronary ostia were significantly higher after root repair compared to root replacement (p<0.001). In the root replacement group, 42 (37%) of patients had at least one coronary ostium completely below the valve, complicating a future Valve-in-Root option. Root replacement with a Valsalva-Graft had a significantly higher valve-to-coronary distance of the left coronary artery (p<0.001). 37 (32.7%) patients had a risk for coronary obstruction in a potential trans-catheter Valve-in-Root procedure due to a low offspring of a coronary ostium or a low coronary-to-valve distance. After thorough examination of the CT scans, together with our interventional specialists, in 21 cases a simple Valve-in-Root would be possible, while 15 patients would require additional interventions like chimneys or the Basilica manoeuvre. One patient was not suitable for a Valve-in-Root procedure and would require open surgery. Our study shows that high re-implantation of the coronary buttons and the use of a Valsalva-graft are simple surgical measures that can be taken during root replacement and root repair to facilitate later trans-catheter Valve-in-Root procedures.

This is an exciting time in the development of new treatments for thoracic disease and the EACTS Annual Meeting is a great opportunity to enhance our clinical practice, learn from some of the foremost experts in the field, and take time to network with colleagues and friends.
This year we have ten dedicated thoracic-focused sessions, including Thursday morning’s highly anticipated session on cardiothoracic trauma, which will
explore the latest advances and techniques in managing traumatic injuries to the chest. Alongside other leading experts, we are delighted to welcome Yaroslav Telushko from the Ukraine who be discussing strategies for managing severe chest trauma, particularly in resourcelimited settings, using his experience from treating casualties on the front line. Any cardiothoracic surgeon might be exposed to trauma, so this is a session that is relevant to thoracic and cardiac surgeons.
On Friday we welcome three giants of thoracic surgery. Experienced thoracic surgeon Alper Toker, and former EACTS President Peter Licht, will each present a challenging case from their careers and Valerie Rusch, a world-renowned thoracic surgeon from the US, will share some of her career highlights. This will be a fantastic session.
Among other topics of interest will be a discussion on the legal aspects of cardiothoracic surgery, which are increasingly important. ‘Not guilty your Honour – the importance of medicolegal aspects of cardiothoracic surgery’ is a shared session on Thursday with the Acquired Cardiac Disease Domain. We will explore how to avoid pitfalls in both cardiac and thoracic surgery and will be joined by a barrister who will provide guidance on how to be an expert witness.
I would also like to highlight our EACTS Learning Lab. This year we will expose delegates to thoracoscopic resection using the Stupnik Simulator, and separately surgeons will be able to advance their skills in tracheal
resection and reconstruction. This will be an immersive, hands-on lab with a focus on techniques. It really is a unique opportunity to learn directly from leading experts in the field and gain invaluable practical experience. I hope you will agree we have put together a programme that has a wide appeal and covers many different topics. I look forward to seeing you over the next few days.
This year we have ten dedicated thoracic focused sessions, including Thursday morning’s highly anticipated session on cardiothoracic trauma, which will explore the latest advances and techniques in managing traumatic injuries to the chest.

Auditorium 1 / 08:30 - 09:30
A Machine Learning Approach to Facilitate Selective Cervical Lymphadenectomy in Thoracic Esophageal Cancer
Objective: Accurate determination of lymph node metastasis is key to minimising surgical complications while maintaining survival rates in patients with esophageal squamous cell carcinoma (ESCC). The goal of this study is to investigate the use of machine learning (ML) techniques to facilitate a non-invasive assessment of cervical lymph node involvement in patients with ESCC.
Methods: The dataset contained 887 surgically treated ESCC patients whose cervical lymph nodes were removed for pathological examination. ML models were developed using baseline ultrasonographic and clinical findings to predict the risk of metastasis in cervical nodes. The models were trained and tested using a fivefold cross-validation method and benchmarked against a baseline nomogram. The importance of each feature was measured by the permutation score.

Results: Of the patients, 285 (32.1%) had pathologically confirmed metastasis in cervical lymph nodes. ML models were effective in predicting cervical nodal metastasis in more than two-thirds of the patients, significantly outperforming the baseline nomogram (p<0.05). The random forest model exhibited the highest accuracy (0.68, [95% CI: 0.65-0.71]), negative predictive value (0.82, [0.800.83), and area under the receiver operating characteristic curve (0.72, [0.71-0.74]). No significant difference in overall performance was noted among these models (p>0.1). Key predictive factors were consistent across the models, with ultrasound measurements of cervical node diameter being the most influential. Adding pathological findings in adjacent paraoesophageal nodes did not enhance model performance.
Conclusion: This study demonstrates the viability of using ML to predict cervical lymph node metastasis in patients with ESCC. These models hold the potential to guide decisions on cervical lymph node dissection, thereby diminishing the risk of unnecessary surgical trauma.


Jürgen Hörer, Chair, Congenital Heart Disease Domain
I’m very excited about this year’s scientific programme which offers a combination of the classic focus sessions on important topics such as pulmonary stenosis, transposition of the great arteries (TGA) and Fontan, as well as introducing some special sessions designed to provoke fascinating discussions and provide opportunities to learn from the experiences of others.
The ever popular ‘Nightmares’ session returns on Saturday morning with four surgeons discussing difficult situations they have faced when treating a patient. This session is highly interactive, encouraging delegates to discuss the best approach in each scenario. I hope that by sharing some ‘nightmares’ we can provide some reassurance, particularly to residents, that errors do happen and provide us with a learning opportunity to deliver better patient outcomes.
Another interesting session on Saturday explores ethical dilemmas in congenital heart surgery. We’ll be asking some important questions in this session, such as: is a learning curve acceptable in training, and what do we do when we change a patient’s therapy?
Our domain received over 180 abstract submissions for consideration at this year’s Annual Meeting. From these we have selected 56 of the highest ranked abstracts to be presented as part of our five abstract and rapid response sessions or as e-Posters. It is particularly encouraging to see an increase in abstracts derived from registries or databases, thus providing robust evidence.
The President’s Choice for the congenital domain on Thursday morning is a great example. This presentation features a 25-year summary of congenital heart surgery outcomes from the European Congenital Heart Surgeons Association's Congenital Cardiac Database.
This database now includes more than 350,000 operations so this is a very interesting abstract and a session I strongly recommend.
Finally, the EACTS Learning Lab is always very popular and this year we are giving delegates an opportunity to gain experience of the Senning Procedure – a complex procedure that is rarely performed. In the USA for example, there are only three centres which do more than 2-3 Senning operations a year, but it is important to have an understanding of this procedure. We have an excellent faculty of Senning surgeons leading this lab so it is certainly one not to miss.
With a scientific programme packed with thoughtprovoking sessions, e-Posters and learning labs there’s lots to keep us all busy over the next few days. I hope we can all make the most of this opportunity to get together with past colleagues and forge new connections.
Our domain received over 180 abstract submissions for consideration at this year’s Annual Meeting.
PRESIDENT'S CHOICE: HIGHEST RANKED ABSTRACT - CONGENITAL

Protopapas Eleftherios
Iaso Children's Hospital, Marousi, Greece
Auditorium 1 / 08:30 - 09:30
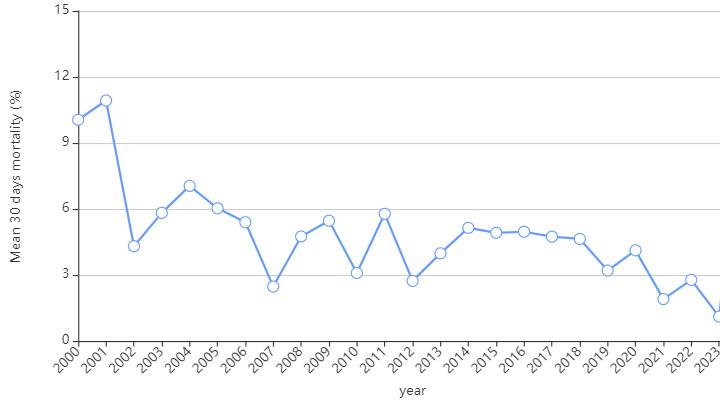
The European Congenital Heart Surgeons Association Congenital Cardiac Database: A Twenty-Five Year Summary of Congenital Heart Surgery Outcomes
The European Congenital Heart Surgeons Association Congenital Cardiac Database (ECHSA CCDB), has grown steadily over the last 25 years and, today, it is the second largest in the world and the largest in Europe. Until August 2024 it has captured data from 377,606 procedures in 294,206 patients of all ages with congenital heart disease (CHD) from partipating centres around the world. Multiple preoperative risk factors relating to each patient’s pathology and thier clinical status are stored. Outcome parameters include 30-day and hospital mortality, postoperative ventilation time, length of hospital stay, as well as various important complications.
The goal has always been to promote clinical research and facilitate the self-assesment and quality improvement efforts of participating centres, as it allows advanced risk stratification and benchmarking. A unique feature of the ECHSA CCDB is that users have 24-hour direct online access to their own and cumulative data, while powerful filters permit self-selection of any specific subpopulations, instantly obtaining standardised analytical reports, or for the user’s own analysis.
Since 2022, in collaboation with MIT, the database has developed unique Artificial Intelligence and machine learningderived methodology permitting accurate centre-specific and case-adjusted risk prediction, as well as automatic casemix-adjusted centre performance analysis. Performance is analysed both cumulatively and by similar-risk patient cohorts, stratified by benchmark procedures or STAT mortality categories.
Also, importantly, since 2023, in partnership with the AEPC, the ECHSA Database is now collecting Interventional Cardiology Data, thereby becoming the first international, multi-institutional database where both surgical and interventional patient data are recorded and analysed.
In this meeting, we report a summary of 25-year real-world outcomes of pediatric and adult congenital heart surgery in our participating centres from Europe and around the world, stratified by age groups, major diagnoses, and procedures. Improvement in outcomes both overall and in various patient subgroups is documented. Still, the data shows persistent challenges especially in neonatal heart surgery. This information should be of great value for individual centre quality improvement programmes and can contribute to improved quality of care for patients with CHD, which is the primary goal of our Association.
Figure 1: 25 year, 30 day mortality trend


As the Chair of the Vascular Disease Domain, I would like to welcome you to the 38th EACTS Annual Meeting. It will be a very busy three days with a great scientific programme designed to engage, inform and of course, challenge.
We kick off on Thursday morning with a focus session on the very important topic of left subclavian artery management. There are many ways to deal with this issue and each has its own risk and benefits; it is a frequent talking point amongst aortic surgeons. We will be joined by four speakers who will each present a different way to manage the left subclavian artery during aortic arch treatment, supported by a video presentation.
Surgical videos will feature heavily in this year’s vascular programme. In addition to providing some engaging content, video footage is an excellent way to demonstrate a procedure or specific technique.
Another interesting focus session explores issues surrounding vascular graft infection, which I consider to be a silent epidemic. When infection occurs, it can be dangerous to redo the operation. In Thursday’s session ‘Vascular graft infection – the silent epidemic’ we will share best practice around reducing the risk of reoperations for infection and the best way to treat a patient.
Examining the impact of aortic guidelines
It has been one year since the introduction of the new aortic guidelines, and therefore it is timely to examine how these guidelines have impacted clinical practice. Four patient cases will be presented and we will consider how best to implement the new recommendations. This session is a great opportunity, particularly for surgeons who don’t deal with these cases on a daily basis, to see actual patients being presented and discuss the possible solutions alongside experts who were involved in writing the guidelines.
This year we received a record number of abstract submissions, including a high number of multi-centre studies, which really is testament to the high-quality science that we see at the Annual Meeting.
Heritable thoracic aortic disease is a topic that's becoming more and more prominent in our field, so I recommend Friday’s abstract session ‘Taking care of
patients with heritable thoracic aortic disease - from pregnancy to aortic arch repair’. With abstracts from Canada, China, Australia and Europe, this session covers many different topics that influence the treatment of patients with heritable thoracic aortic disease.
The President’s Choice session on Thursday morning features a remarkable study on ascending aorta overangulation. The study shows that the angle between the heart and the aorta is an important risk factor for dissection, and the findings could have an impact on our clinical practice in the future, as well as becoming part of future guidelines.
The EACTS Annual Meeting is truly the leading event for the cardiothoracic community to discover the latest science. Have a fantastic stay in Lisbon.
We kick off on Thursday morning with a focus session on the very important topic of left subclavian artery management. There are many ways to deal with this issue and each has its own risk and benefits; it is a frequent talking point amongst aortic surgeons.
PRESIDENT'S CHOICE: HIGHEST-RANKED ABSTRACT - VASCULAR

Federica Lo Presti University of Campania Naples, Italy
Auditorium 1 / 08:30 - 09:30
Ascending aorta over-angulation is a risk factor for acute type A aortic dissection: evidence from advanced finite element simulations
New Evidence from Finite Element Analysis Supports a Predictive Role of Ascending Aorta Over-angulation in the Determinism of Acute Type A Aortic Dissection.
In the last decade, the role of aortic elongation in the risk of acute type A aortic dissection (ATAAD) development has been emphasised. Our research group, led by prof. Alessandro Della Corte, has recently observed in a multi-centre study that in only a proportion of patients with elongation, narrowing of the ascending-arch angle (degree of angulation between the axis of the tubular tract to the axis of the proximal arch, zone 1) coexists: this parameter showed very good predictive power in distinguishing patients with ATAAD from those with chronic dilatation (with an AUC of 0.815) with the cut-off value of <130° including the totality of ATAAD study patients.
Now we have expanded our research on this topic, collecting data from our Centre, Monaldi Hospital in Naples, Italy,
and from the Ospedali Riuniti “Torrette” in Ancona, Italy, on CT scans performed on 16 ATAAD patients for any reason at any time before they experienced ATAAD. At the Department of Electronics, Information and Bioengineering of the Polytechnic University of Milan, Italy, parametric finite element models (FEMs) simulating different degrees of ascending-arch angulation were created, which showed that the narrower the angle, the higher the longitudinal stress in the ascending aortic wall (Figure 1). Then patient-specific FEMs were developed from the pre-dissection CT-scans, revealing a highly consistent correspondence between the location of the peak longitudinal stresses and the site of main entry tear in post-ATAAD CT-scans (Figure 2).
This study further confirms that the ascending-arch angle is a potential risk-marker for ATAAD, moreover showing its stability from pre- to post-dissection imaging. Patient-specific simulations might become a prognostic tool to predict ATAAD risk, e.g. in patients with over-angulation.
Figure 1: Parametric FEMs. Left: exemplary models with ascending arch angle 145° (normal aorta) and 110° (elongation with over-angulation) with color-coded longitudinal stress maps; Right: box-plot showing that models with progressive narrowing of the ascending-arch angle display higher longitudinal stress values, with significance starting from angles narrower than 130°.

Figure 2: An example of patient- specific FEMs showed that the aortic wall area (at the outer curvature in this case) with highest longitudinal stress before dissection corresponded with the area where the entry tear developed.
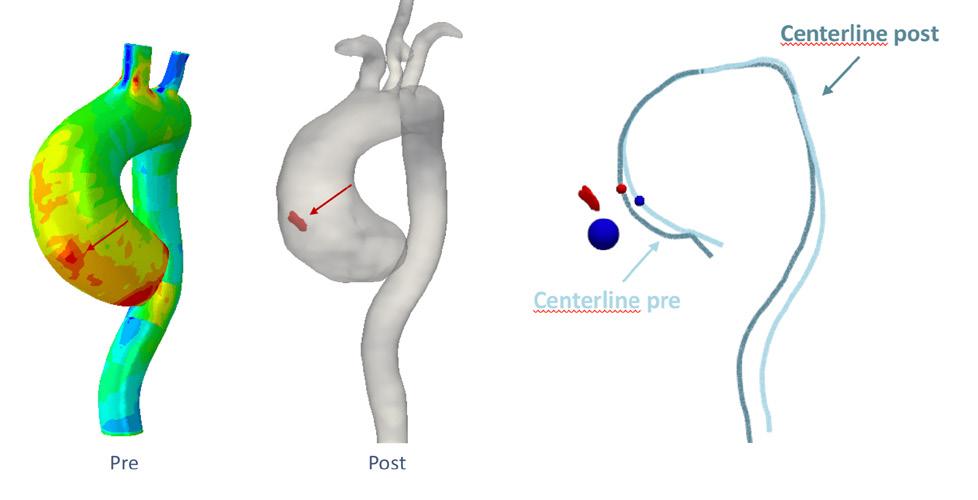
This study further confirms that the ascending-arch angle is a potential riskmarker for ATAAD, moreover showing its stability from pre- to post-dissection imaging.


This year we welcome Amy Kerdok, inventor and Head of Product at Capstan Medical, as our Honoured Guest. From working on multiport surgical and vision systems at Intuitive to developing a novel hemodialysis system at Outset Medical, Amy Kerdok has played a critical role in developing and delivering user-centred medical products worldwide.
Ahead of her presentation ‘Innovation in Surgery: Looking back to look forward’, she shares her reflections on product development and how we can encourage more innovation in cardiothoracic surgery.
You have over 16 years of experience in developing new medical products. How did you get into product development?
I’m a curious person and I've always wanted to solve problems. I started in academia, which was great, but the faster pace of med tech was very appealing. I wanted
to see the products come to fruition and actually help people. You can build a new app or a gizmo all day long, but I want to help people have better cancer surgery or life-changing therapy.
What led you to develop robotics for use in cardiothoracic surgery?
Everyone wants to work on the heart! But it is also a personal issue for me. Heart and lung disease have affected my family. I lost a grandfather and an uncle to valvular heart disease when they were really young, and two uncles to lung cancer.
Robots are just a tool like any other. I start by figuring out what needs to be achieved, and then find the best tool to do it. Sometimes it's a robot, sometimes it's an instrument, sometimes it's a vision. The important piece is really understanding the problem that you're trying to solve. And when that solution fits a robot, that's when you use a robot.
How can we encourage more innovation within the surgical community?
Innovation isn’t possible without evolution and collaboration. There are so many new technologies or ways of thinking that can lead to us doing something better, or even something completely new. To do that, you need to be able to understand the issue facing surgeons and translate it to the engineers. It’s really important that we help surgeons and engineers better understand each other.
If we can cast a wide net to include interdisciplinary teams then we will really boost innovation. When you bring minds together, it is possible to develop more effective solutions.
And finally, we must stay curious! Once you solve the problem, you've probably opened the door to six more!
What can delegates expect from your presentation ‘Innovation in Surgery: Looking back to look forward’?
My presentation will offer a little history of my time at Intuitive Surgical with four generations of multi-port robots, and introduce delegates to my new product at Capstan Medical which is a robotically enabled structural heart platform that will be going into first-inhuman trials by the end of this year.
I will also be urging a little bit of caution about data and AI and machine learning and making sure technology is not being shoehorned into a problem when it is not necessarily the right solution. Regulatory bodies like to know that a human is still in the loop to manage decision making, and I agree with this approach. It's called the art of surgery for a reason.
We must stay curious! Once you solve the problem, you've probably opened the door to six more!
THANK YOU
With grateful thanks to the members of the Executive Programme Committee who have worked tirelessly to shape this year’s EACTS Annual Meeting.
Patrick Myers
Filip Casselman
Jürgen Hörer
Nabil Hussein
Milan Milojevic
Richard Milton
Rafael Sadaba
Florian Schoenhoff
Alicja Zientara
Working alongside the Events Team:
Sharon Pidgeon
Ikode Agbi
Katie Bingham
Amanda Cameron Marina Gueli

Good leadership practices are the focus of a powerful session, taking place this morning, exploring bias and leadership in cardiothoracic surgery. Organised by the Women in Cardiothoracic Surgery Committee (WiCTS) but open to all delegates, the session features a keynote presentation from leading thoracic surgeon Valerie Rusch, who is renowned for her dynamic leadership.
A panel featuring EACTS President Franca Melfi and VicePresident Volkmar Falk, as well as members of the WiCTS Committee - Maroua Eid and Lorena Montes, will discuss their outlooks and wide-ranging perspectives on leadership and bias.
This is a highly interactive session with delegates invited to share their experiences of leadership training and any bias, positive or negative, that they have faced during their surgical career.
Indu Deglurkar, Chair of the Women in Cardiothoracic Surgery, said, “In addition to mastering complex technical skills, surgeons requires leadership, verbal and nonverbal communication skills and a high level of emotional intelligence to effectively interact with other team members without bias or prejudice. This focus session will explore the inherent gender bias across the globe and provide useful insights on the challenges ahead. It will benefit all members of the cardiothoracic community, and I hope will provide a catalyst to deliver important cultural and legislative change as we strive to achieve equity in cardiothoracic surgery.”
Leadership masterclass
A new EACTS Academy course designed to provide tailored education in leadership skills for surgeons has been developed by the Women in Cardiothoracic Surgery Committee. Details of the course, in which participants will be taught ways to recognise their leadership style, explore their emotional intelligence, learn how to lead through complex transitions and overcome bias and discrimination, will be shared during this morning’s focus session.
Bias and Leadership in Cardiothoracic Surgery
10:00 - 11:00
Room 3B, Pav 3
Tune in to EACTS TV for a discussion about the role of women in cardiothoracic surgery and ways to create an equitable, diverse and inclusive culture.
14:45 - 15:10
TV Studio
Forge new relationships and reconnect with old colleagues at an informal networking breakfast hosted this morning by the Women in Cardiothoracic Surgery Committee. This is an exciting opportunity for all delegates to come together to share experiences, broaden professional networks and make lifelong connections to support career development now and in the future.
Thursday 10 October
WiCTS networking coffee break 09:30 -10:00


The new EACTS Adult Cardiac Database (ACD) is being launched today, marking a significant milestone in the journey towards enabling trustworthy use of cardiac data for quality improvement and research.
The Adult Cardiac Database is a collaborative registry and benchmarking tool of anonymised cardiac surgical data for centres across Europe. Use of this data allows surgeons to better understand clinical practice in their hospitals and inform best practice. Chair of the EACTS Quality Improvement Programme Committee (QUIP) Edgar Daeter will showcase the advanced data tools and insights available through the ACD during this afternoon’s ‘QUIP’ focus session.
Edgar Daeter said, “We believe the ACD will be the leading European database collecting cardiac data from around the world. More than a repository of data, the database is a powerful instrument for benchmarking and research. The ACD holds huge potential to identify areas of improvement in clinical practice, drive innovation and ultimately improve patient outcomes.”
Benefits of the ACD include:
• Bringing participating hospitals, national registries and surgeons together to advance the field of cardiothoracic surgery through comparative data analysis and sharing of best practice.
• Supporting surgical training and education and informing evidence-based practices for current and future cardiothoracic surgeons.
• Providing a controlled access mechanism for researchers to request access to the data, regulated by a scientific committee and in line with established governance frameworks. Researchers’ proposals need to have clear patient benefit.
New features of the ACD include an interactive viewer which allows users to filter different types of interventions and outcomes, making it easier to derive valuable insights. Uploading data is now much simpler and faster for national registries, hospitals and surgeons following changes to the database’s code.

Paola Quattroni
Paola Quattroni, Quality Improvement Director, said, “I encourage hospitals to sign up and start submitting data to the database. Using data will drive improvements in cardiothoracic surgery. There is a wealth of information already available, recorded at all stages of patient care, including pre-intra and post operative care. The Adult Cardiac Database will maximise use of this data by enabling consistent and standardised collection from different sources, helping surgeons to improve their clinical practice.”
Only EACTS members and participant hospitals will be able to access the EACTS Adult Cardiac Database and researchers can request access to data via submitting a data request application. Sign up and submit your data at eacts.org to improve patient outcomes!

Using data to drive improvements in cardio-thoracic surgery is key. There is a wealth of information already available, recorded at all stages of patient hospital care, including pre-intra and post operative care.
The EACTS Quality Improvement Programme champions continuous improvement in cardiothoracic surgery through a set of activities aimed at delivering better skills, better surgery, and better patient outcomes. To enable this, we are developing collaborative data registries and benchmarking platforms that can provide insights for quality improvement.
EACTS also continues to invest in the Quality Improvement Programme with new appointments to strengthen the QUIP team. Paola Quattroni joins as the new QUIP Director to provide leadership and ensure data-driven insights are at the core of quality improvement initiatives. Kevin Veen joins as Scientific Lead to provide oversight on data standards, mapping and statistical analyses. Mazen Ahmed is a new Data Analyst with responsibility for data curation and management of data requests. They will work alongside Edgar Daeter, QUIP Committee Chair and Stephanie Halksworth, Consultant Programme Manager.


Late breaking science: coronary artery bypass grafting and perioperative care Video session - mastering advanced surgical procedures: techniques and insights
and

Yaroslav
Telushko Zaporozhzhia State Medical University, Ukraine
Auditorium 2 / 10:00 - 11:00
The start of the war in Ukraine in February 2022 focused attention on medical problems that had not been noticed before. The scale of hostilities and the nature of the weapons used significantly affect the provision of medical care. The limitations of the modern military health care system are a shortage of military personnel and obstacles to the use of medical evacuation transport (air and ground). Increasing the evacuation time, on the other hand, requires the approach of specialised assistance (including thoracic, neurosurgical and angiosurgical). Modern specialised assistance to patients is based on a detailed examination and the use of high-tech tools, the experience in which is practically absent in the military sphere, and publications have access restrictions.
The long delivery time to the medical evacuation points significantly affects the nature of the injury of servicemen who can be assisted. Damage to the main vessels, heart, destruction of the chest wall, tense pneumothorax, massive hemothorax - linger on the battlefield and, not infrequently, such an injury is fatal.
The use of a large number of weapons with a fragmentation mechanism (the number of bullet wounds 1.5-2%) leads to numerous injuries of various body segments or significant destruction, which depends on the distance to the place of explosion and the size of the fragment, its energy. In such conditions the goal of providing assistance is not directly saving life, but predicting further complications and their surgical prevention. Is it possible to use DCS tactics in the classical sense under these conditions?

Marc Ruel
University of Ottawa Heart Institute Canada
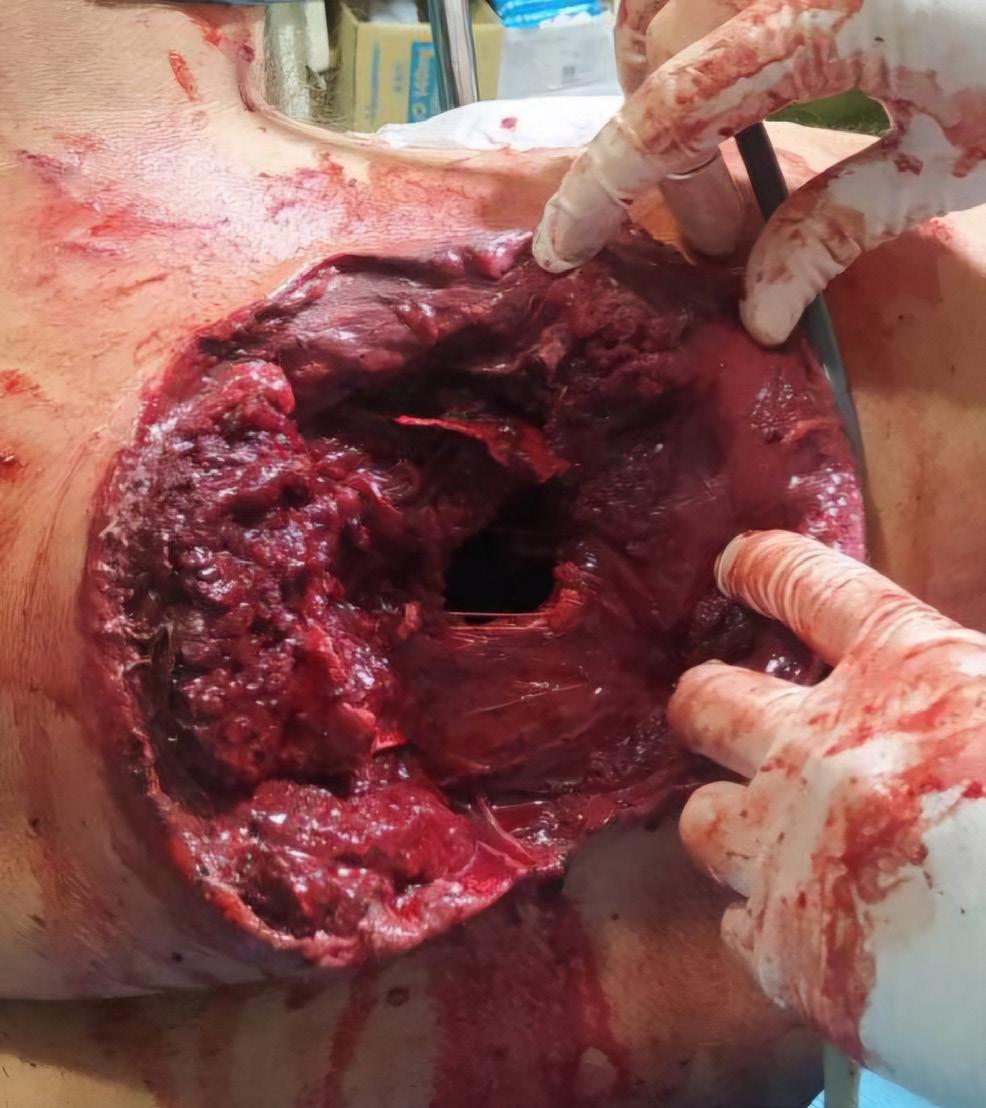
The presence of gunshot fractures of the ribs and significant skin defects make it difficult to close the pleural cavity, but this is key in achieving its tightness and preventing inflammatory complications.
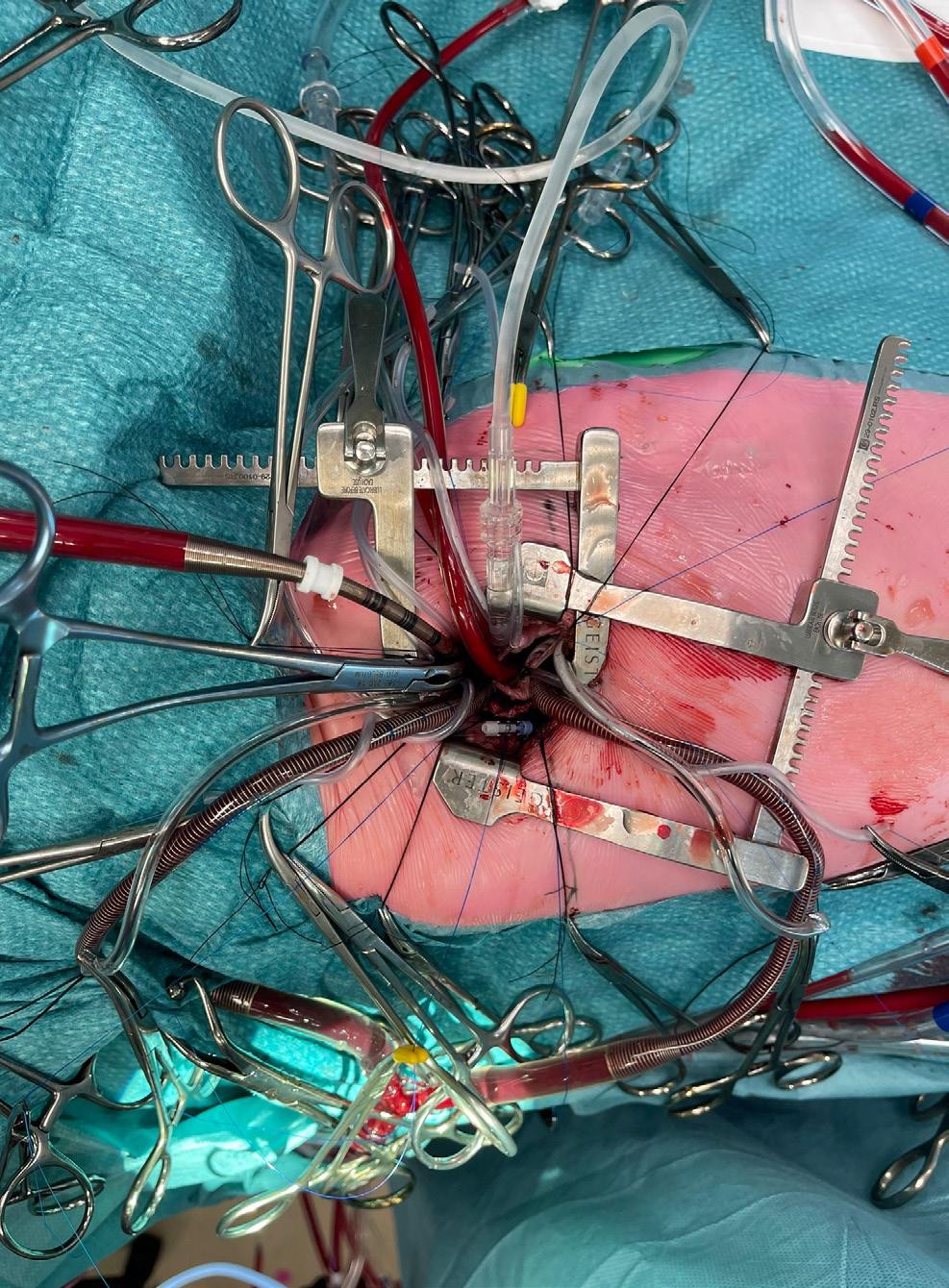
The first surgical aid at the Role 1 point plays the role of the first stage of DCS: decompression and sealing, achieved by drainage and dressing. This is usually enough to stop most of the bleeding and prepare for evacuation. Evacuation, as an integral part of medical care, organically, should be considered as the second stage of DCS - the intensive care unit becomes a mobile intensive care ward, which ultimately provides the most important thing: time. Lack of adequate treatment during evacuation deepens pathological disorders and will have extremely negative consequences. Role 2 point is the territory where the thoracic surgeon is able to influence the course of the injury with maximum efficiency within the available conditions and assuming sufficient means for examination, appropriate operating room, and viability of post-operative stay, even short-term.
most technically challenging operations that a cardiac surgeon can learn and perform nowadays. Through a small incision, reconstructive microsurgery must be performed flawlessly, with a different exposure for the harvesting of each conduit, the sourcing of inflows, and the grafting of each myocardial territory. In our presentation, we highlight the techniques and results of less invasive CABG. We also propose a stepwise path to achieving safe, high-quality, reproducible, and durable forms of multiarterial MICS CABG. Ultimately, the close involvement of interventional cardiology colleagues to supplement the minimally invasive performance of robotic-assisted, bilateral internal thoracic artery harvest at MICS CABG effectively avoids the pitfalls of sternotomy, cardiopulmonary bypass, aortic manipulations, vein grafts, and incomplete or unvalidated myocardial revascularisation.
Technical methods include classic drainage, thoracotomy, video thoracoscopy, metal osteosynthesis, plastic closure of chest wall defects, and VAC therapy. Careful diagnosis with MSCT allows planning of surgical interventions according to the nature of the injury. Commonly used methods of working with damaged organs (lungs, diaphragm, intercostal vessels, heart, esophagus, main vessels, large bronchi) require some experience. The presence of gunshot fractures of the ribs and significant skin defects make it difficult to close the pleural cavity, but this is key in achieving its tightness and preventing inflammatory complications. Special attention should be paid to the diagnosis and elimination of iatrogenic injuries after invasive procedures at the previous stages (errors in catheterisation of the superior vena cava, intubation, drainage of pleural cavities, etc.). Combat significantly changes attitudes towards the DCS paradigm in thoracic surgery.


Coronary artery bypass grafting is the world’s most often performed cardiac surgery operation. However, CABG often remains as invasive today as it was 50 years ago. Minimally invasive coronary artery bypass grafting (MICS CABG) can take many forms and represents one of the
Coronary artery bypass grafting is the world’s most often performed cardiac surgery operation. However, CABG often remains as invasive today as it was 50 years ago.



EACTS has today published new recommendations on the important topics of perioperative medication, cardiopulmonary bypass in adult cardiac surgery, and patient blood management. The impact of these new recommendations on clinical practice and patient care will be discussed during this afternoon’s session ‘Updated EACTS Guidelines’ which will give delegates an unmissable opportunity to hear direct from the guideline authors and evaluate the evidence and rationale behind the changes in the updated guidelines.
The work of our Clinical Practice Guidelines Committee and task forces is vital, helping to produce evidence-based clinical practice guidelines and other scientific documents to help the surgical community improve patient care and outcomes.

Updated EACTS Guidelines
13:45 - 14:45
Auditorium 1
Watch live on EACTS TV
Anders Jeppsson, Bianca Rocca, Emma Hansson, Milan Milojevic
READ THE RECOMMENDATIONS HERE
Clinical practice guidelines are crucial tools for synthesising and evaluating all available evidence on a specific topic, assisting physicians in determining the most effective management strategies for patients. Medications play a vital role before, during and after surgery. Yet patients are often undertreated, which can have tremendously negative effects on both short- and long-term outcomes, as well as overall quality of life.
In 2017, under the leadership of Miguel Sousa-Uva and Ulf Landmesser, the inaugural edition of the EACTS guidelines on perioperative medication in adult cardiac surgery were published. Since then, significant new and practicechanging evidence has emerged, prompting the EACTS Clinical Guidelines Committee to initiate an update with a dedicated task force of experts.
We are excited to announce that the 2024 guidelines on perioperative medication will be unveiled today, with simultaneous

publication in the European Journal of Cardio-Thoracic Surgery.
This comprehensive guideline covers sixteen sections, offering in-depth guidance and recommendations on pre-, peri- and post-operative management of antithrombotic medications, antiarrhythmic drugs, and heart failure and hypertension treatments. Additional sections focus on lipid-lowering medications, steroids, antibiotics, blood glucose management and antidepressants.
Notably, the updated guidelines introduce two new sections: one on postoperative optimisation using guideline-directed medical therapy in both coronary and noncoronary cardiac surgery, and another addressing gaps in current evidence.
The primary aim of this guideline is to equip clinicians, surgeons and healthcare professionals with clear, actionable and evidence-based recommendations, ensuring optimal care and improved outcomes for patients undergoing cardiac surgery.
We look forward to collaborating with the medical community to explain these guidelines further and support their implementation in daily clinical practice.
Alexander Wahba, Gudrun Kunst, Filip DeSomer, Milan Milojevic
READ THE RECOMMENDATIONS HERE
The 2019 EACTS/EACTA/EBCP Guidelines on Cardiopulmonary Bypass (CPB) in Adult Cardiac Surgery provided the first comprehensive European clinical guidelines in the field. We now present the 2024 EACTS/EACTA/EBCP comprehensively revised document, updating previous content and incorporating a broader range of new topics, including organ protection, temperature management during CPB, and perfusion during aortic surgery.
The section on cardioplegia has been redesigned and expanded. In addition, significant new scientific evidence has been incorporated, such as findings on the use of hemadsorption.
All subchapters related to different aspects of monitoring, including neuromonitoring, have been consolidated into a single monitoring chapter. A new chapter addressing specific situations, particularly adverse events, has also been added. The use of CPB during

cardiac surgery is characterised by close collaboration between cardiac surgeons, thoracic anaesthetists and perfusionists.
The creation of these clinical guidelines required multidisciplinary input from various experts across all professions involved. This was achieved through close cooperation among the relevant societies: EACTS, EACTAIC and EBCP. The recommendations of the revised CPB guidelines were discussed and coordinated with task forces for both patient blood management and perioperative medication in adult cardiac surgery, when applicable. The management of CPB in paediatric cardiac surgery was not included and will be addressed in a separate expert consensus document. The task force aimed to provide comprehensive coverage of the most current and relevant aspects of CPB, ensuring that these guidelines remain a valuable resource for all stakeholders in adult cardiac surgery.
Footnote: The guidelines are currently in production for simultaneous publication in EJCTS, ICVTS, and BJA. For conference purposes, the guideline document can be accessed via the provided link to better inform attendees and provide rationale for the presented recommendations. Sharing the content with third parties is strictly prohibited.
Milan Milojevic, Maroua Eid and Filip Casselman
Evidence-based guidelines play a crucial role in the management of cardiac surgery patients, with patient blood management (PBM) being an integral part of treatment. In this afternoon’s session ‘Updated EACTS Guidelines’, a comprehensive revision of the 2017 guidelines will be presented, reflecting the evolving patient profiles and treatment modalities in adult cardiac surgery. These changes are driven by factors such as increasing patient age at the time of surgery, a rise in comorbidities, and the growing complexity of preoperative antithrombotic treatments. Bleeding and transfusions remain major complications associated with cardiac surgery, and comprehensive treatment guidelines should help in timely recognising and managing these issues, ultimately improving patient outcomes.
READ THE RECOMMENDATIONS HERE

These guidelines are a joint effort between the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association for Cardiothoracic Anaesthesiology and Intensive Care (EACTAIC), in collaboration with the European Board of Cardiovascular Perfusion (EBCP).
In addition to updates in the preoperative section regarding bleeding risk estimates and preoperative anemia management, as well as the intraoperative section with more detailed information about the preservation of the patient’s own blood and hemostatic interventions, the guidelines introduce essential aspects of postoperative management. This includes recommendations on transfusion and hemostatic therapy, particularly in cases involving mechanical circulatory support.
The guidelines also emphasise the importance of organising an institutional patient blood management programme in each centre. Collaboration between surgeons, intensivists, and perfusionists through these programmes is key to improving both surgical and postoperative management for our patients.
INFORMING THE GLOBAL CARDIOTHORACIC COMMUNITY WITH THE LATEST EVIDENCEBASED GUIDELINES AND SCIENTIFIC DOCUMENTS
View the latest EACTS clinical practice guidelines


Y.J.H.J. Taverne Erasmus Medical Center Netherlands
Auditorium 6 / 17:45 - 18:45
How to set up a minimally invasive program in congenital cardiac surgery
Full midline sternotomy remains the most common incision to correct congenital cardiac defects. Although many minimally invasive programmes exist for the adult population worldwide, only a few centres have adopted such a programme for the pediatric population. The rise of novel interventional cardiology techniques and the main advantages of earlier recovery and cosmesis have prompted some groups to explore alternative approaches to median sternotomy. However, the steep learning curve and technical difficulties associated with minimally invasive procedures have discouraged many surgeons from adopting this approach as their new “gold standard”. Few reports have been published on starting such a programme and in our opinion, the success is dependent on a step-by-step approach with attention paid to the full cycle of care. This includes preoperative awareness and screening, as well as postoperative care, where much reluctance might be present based on inexperience and mostly fear of the unknown.
We already have extensive experience in minimally invasive surgical in the (congenital) adult population and used this knowledge when designing and developing the minimally invasive children’s programme. Selected conditions to continue the programme encompassed central cannulation possibilities, mid-axillary approach, optimal post-operative pian management, and no increase in residual defects

We already have extensive experience in minimally invasive surgical in the (congenital) adult population and used this knowledge when designing and developing the minimally invasive children’s programme.
as compared to the sternotomy group. After one year, we have performed more than 20 minimally invasive pediatric surgeries (from 5kg) ranging from ASDII and pAVSD to VSD closure without residual defects, conversions or other comorbidities. All cases were discharged around day 4 with a maximum stay of one night at the ICU. Pain management was optimised where early full mobilisation was key.



EACTS is a very special association, enabling the cardiothoracic surgical community to work together enhancing our skills for the benefit of patients, and it is an honour for me to be EACTS President.
As well as several members of staff, we are fortunate to have 4,000 EACTS members. You join us for Academy courses, read our publications and, of course, attend the Annual Meeting. One of our core values at EACTS is: ‘Act with integrity’ and it’s important all of us embrace this value, which is why I welcome the progress made this year by the Working Group on Professional Behaviours.
The group was set up in 2023 to support our members and staff to create a professional and inclusive environment that respects diversity, promotes equality and supports us all as surgeons and other healthcare professionals. The group is working to raise awareness of the importance of professional behaviours, what to do if you experience or witness behaviour that falls short and to learn more from our members about their experiences.
This behaviour can take many different forms. It could be verbal abuse or intimidation, excluding a colleague, aggression or sustained harassment. We know that these behaviours can have a serious impact on the recipient's wellbeing and mental health. As EACTS President, I want to make sure we are doing everything we can to support you to recognise and deal with unacceptable behaviour when it happens.
The working group, which includes EACTS members, staff representatives and an external consultant, is developing guidance to outline our expectations for professional behaviour. The guidance, which will be published soon, will provide examples of disruptive behaviour, what to do if you witness or experience disruptive behaviour, how to report it within EACTS and what we will do to support you through the process.
While it's not EACTS’ role to set policies for individual hospitals, we hope that the guidance will also support members feel respected and act with integrity wherever you’re working.
Thank you for being part of EACTS. Let’s work together to ensure everyone in EACTS is respected.
One of our core values at EACTS is: ‘Act with integrity’ and it’s important all of us embrace this value.
How can we address this hidden danger?
Meet us at booth no. 201 & 202 in hall 2
Medela AG Lättichstrasse 4b 6340 Baar, Switzerland www.medela.com 36 % of chest tubes occlude after cardiac surgery1 86 % of these occlusions occur inside the patient and are not visible to doctors and nursing staff1
1 Karimov JH, Gillinov AM, Schenck L, et al. Eur J Cardiothorac Surg 2013;44(6):1029-36.
Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. These specialist hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions.

You will gain practical experience using the latest devices, practice on simulators and interact with expert faculty and industry proctors. EACTS Learning Lab sessions are available for just an additional €75 each. Spaces are limited and offered on a firstcome, first served basis. Don't miss out—book today to guarantee your opportunity.
Thursday 10 October
08:30 – 10:30 Coronary
08:30 – 10:30 Endoscopic Dry Lab Training
11:15 – 13:15 AV Repair – Valve Sparing Aortic Root Surgery: The Reimplantation Technique
11:15 – 13:15 Endoscopic Dry Lab Training (Mitral)
13:45 – 15:45 AV Repair – Annuloplasty with remodelling valve sparing root replacement and isolate aortic valve repair
13:45 – 15:45 Endoscopic Dry Lab Training (Mitral)
16:15 – 18:15 Learning Lab for Left-handed Surgeons
16:15 – 18:15 Endoscopic Dry Lab Training
Join our industry partners to explore new technologies and try different techniques and approaches at this year’s industry learning labs.
Visit their booths in the Exhibition Hall to find out more.
Friday 11 October
09:00 – 11:00 Congenital – The Senning Procedure
09:00 – 11:00 Endoscopic Dry Lab Training
12:15 – 14:15 Mitral Valve
12:15 – 14:15 Endoscopic Dry Lab Training (Aortic)
15:00 – 17:00 Segmentectomy and Airway reconstruction
15:00 – 17:00 Endoscopic Dry Lab Training
Saturday 12 October
09:00 – 11:00 Transcatheter
09:00 – 11:00 Endoscopic Dry Lab Training

Thursday, 10 th October, 12:15 - 13:30, Auditorium 6
Moderators:
Dr. M. Moon (Edmonton, Canada)
Dr. K. Tsagakis (Cologne, Germany)
Speakers:
Dr. W. Szeto (Philadelphia, USA): AMDS in the Management of Acute DeBakey Type I Aortic Dissection: Updates from the PERSEVERE and DART Studies.
Prof. J. Kempfert (Berlin, Germany): Further Clinical Insights on How to Manage Malperfusion and Aortic Remodelling in Acute DeBakey Type I Aortic Dissections.

Watch live and recorded content from this year's Annual Meeting on EACTS TV. Educational and entertaining, EACTS TV features compelling panel debates, Annual Meeting highlights and interviews with the world’s leading cardiothoracic surgeons.
THURSDAY 10 OCTOBER
09:15-09:30 Exhibition "in the making" (behind the scenes clips of build up)
09:30-09:50
10:00-10:20
10:30-10:45
The Daily Preview – Today at the Annual Meeting
Standout Articles from the Multimedia Manual of Cardio-Thoracic Surgery (MMCTS)
Francis Fontan Fund updates & new projects
10:50-11:15 The Residents 'Navigate New Horizons'
Filip Casselman
Milan Milojevic Soi Avgeridou
Anton Pechenenko Tornike Sologashvili
Sam Burton
Bernhard Moser
Manuel Castella
Gowthanan
Santhirakumaran
Polina Danchenko
Tom Bracco Gartner
11:15 - 12:00 Live broadcast: Honoured Guest Amy Kerdok
Milan Milojevic
12:00-12:20
The President’s Choice – Examining New Research at this year’s Annual Meeting
13:30-13:45 Meet the Giants in CT Surgery - Q&A
13:45 - 14:45 Live broadcast: Updated EACTS guidelines
14:45-15:10 WiCTS: The Changing Dimension
Federica Lo Presti
Eleftherios Protopapas
Alicja Zientara Yiliang Zhang
Pedro del Nido
Valerie Rusch
Indu Deglurkar
Lorena Montes
Miia Lehtinen
Maroua Eid
15:10-15:25 In focus with… Patrick Myers Patrick Myers
Jan Vojacek
15:30-15:50
Countdown to the 3rd Aortic Forum: Key insights and programme highlights
16:00-16:15 QUIP
16:15-16:35 The Robotic Revolution in the OR
16:40-16:55 EACTS Membership
16:55-17:10
The Big Debate - Joint Guidelines Methodology
17:20-17:40 Science Friction - The Daily Review
Joe Bavaria
Rafa Sádaba
Ruggero De Paulis
Edgar Daeter, Paola Quattroni and Kevin Veen
Marion Durand
Marc Ruel
Thierry Folliguet
Faisal Bakaeen
Milan Milojevic
Joseph Sabik
Florian Schoenhoff
Polina Danchenko
Soi Avgeridou
FRIDAY 11 OCTOBER
09:15 - 09:30 On the Pulse: Exploring the Exhibition
09:30-09:50 The Daily Preview – Today at the Annual Meeting
10:00-10:20 Shaping the Future of Aortic Dissection: The Power of the Patient's Voice
10:30-10:55 Preview: The CT Surgery Resident Showdown
11:00-11:15 CT Surgery in LMICS
Florian Schoenhoff
Jürgen Hörer
Nabil Hussein
Cristina Ruizsegria
Catherine Fowler
Bob Harris
Juan Grau Nabil Hussein
Patrick Myers
Richard Milton
Carlos Mestres
Charles Yankah
Emily Farkas
11:15-12:15 Live broadcast: Presidential Address Franca Melfi
CT Surgery Resident Showdown: Live European Final! Finalists:
• Marco Gemelli and Francesco Bertelli - University of Padova
Juan Grau (host)
12:15-13:00
• Riccardo Orlandi and Giovanni Mattioni - University of Milan
• Joeri Van Puyvelde and Katrien Vandendriessche - University Hospitals Leuven
Richard Milton (host)
13:15-13:30 In focus with… Volkmar Falk – Incoming EACTS President Volkmar Falk
13:30-13:45 The Big Debate - Artificial Intelligence & Augmented Reality Hazem Fallouh Tomaz Štupnik
Evgenij Potapov
14:45-15:10 Next month in Prague – Presentations of new pumps and Ideas from the world of MCS
15:15-16:15 Session broadcast: Highlights of the 2024 Innovation Summit – Part 2
16:15-16:30 The Big Debate - Cardiology & Cardiothoracic Guidelines
Gloria Färber
Julia Riebandt
Pia Lanmüller
Faisal Bakaeen Jeroen Bax
Milan Milojevic Volkmar Falk
16:35-16:45 EACTS 3rd Innovation Summit (2025) Friedhelm Beyersdorf
Mark Hazekamp
16:45-17:10 Latin heart rounds live with EACTS Victor Bautista Hernandez
Filip Casselman
17:20-17:40 Science Friction - The Daily Review
Milan Milojevic
Rafa Sádaba
SATURDAY 12 OCTOBER
09:15 - 09:30 On the Pulse: Exploring the Exhibition
09:30-09:50 The Daily Preview – Today at the Annual Meeting
10:00-10:15 Innovation in CT Surgery
10:20-10:30 Previewing the 2025 Annual Meeting
10:35-10:55 EACTS Award Winners 2023 - One year on
11:00-12:30 Live broadcast: Trial Update Session
Roy Sheppard
Jeroen Bax
Richard Milton
Can GollmannTepeköylü
Joe Bavaria
Volkmar Falk
Volkmar Falk
Patrick Myers
Debora Brascia
Giuseppe
Comentale
Justin Ren
12:30-13:20 Live broadcast: Keynote Lecture & Awards Ceremony R. J. Canessa Urta



Peters Surgical designs, manufactures and distributes quality medical devices dedicated to surgical practices. Our mission is to improve patient’s quality of care, developing high performance medical devices and supporting education programs.

HAND-ON SESSIONS
With Peters Academy try it on booth!
TALK&PRACTICE AT 5:30PM
On Thursday at Peters Surgical booth:

Engage, Exchange & Experience with experts about Enclose® II, Cygnet® Adams Yozu, and Peters Academy residents program.




Join experts as they discuss the latest clinical data, current and future approaches to patient care and much more in a wide range of satellite sessions hosted by industry.
These sponsored programmes do not form part of the official Annual Meeting scientific programme.
THURSDAY 10 OCTOBER
TIME ROOM
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30






FRIDAY 11 OCTOBER
Future-Proofing Aortic Valve Replacement: An Interactive Showcase for the Next Era of Cardiac Surgery
Now and Next: The Beginning of a New Era for Surgical AF Patients
Optimising patient outcomes: strategies and techniques to reduce post operative complications in cardiothoracic surgery
Auditorium 8 (Interactive-RR)
Auditorium 3+4 (Interactive)
Room 5A, Pav 5
Rigid Sternal Fixation. Why, When and How Room 5B, Pav 5
Aortic Dissections: what ‘AORTists’ do and what is the latest clinical data available?
Aortic regurgitation – treating patients across the spectrum
Auditorium 6
Auditorium 7
TIME ROOM
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30
12:15 - 13:30






Advancing Cardiac Surgery: Integrating Innovation and Patient-Centric Care in the next decade
Reconsidering current approaches to valve and LVAD therapies
Auditorium 8 (Interactive-RR)
Auditorium 3+4 (Interactive)
Hybrid Technologies: Many ways to simplify the arch with the Gold Standard Room 5A, Pav 5
Reshaping Heart Recovery: Impella's Role in Improved Outcomes
New frontiers in mitral valve replacement
Structural Heart Innovation | Science, Clinical Experience & Landmark RCT
Auditorium 6
Auditorium 7
Auditorium 2

Sitting across seven hills and overlooking the majestic river Tagus, Lisbon has enchanted visitors for centuries. The city’s rich history is evident from the 12th century Moorish St George’s Castle to the 16th century Bélem Tower. A huge earthquake destroyed much of Lisbon in 1775, and the distinctive red roofs and patterned tiles we see today were built as part of the city’s reconstruction.
The best way to explore Lisbon is on foot. Away from the seafront you’ll find cobbled streets, shady plazas, brightly tiled churches and plenty of shops and cafés. Get your bearings by wandering between the city’s miradouros, a network of terraces and gardens at the highest points on Lisbon’s hills. Miradouro da Nossa Senhora do Monte, at the highest point in Lisbon, offers views across the city. On a clear day you can see all the way to the Cristo Rei statue, 5.6km away. This west-facing miradouro really comes to life in the evening, when crowds gather to watch the sunset. If time is short, enjoy Lisbon from the polished wooden seats of its famous trams. The most popular route for visitors is No 28, which runs from Martim Moniz to Campo de Ourique, through some of the city’s prettiest neighbourhoods. If you’d prefer to skip the crowds, take the No 15 or 127 from the central Praça do Comércio to Bélem, a beautiful district west of the city along the Tagus.
Portugal’s history of sea exploration is on display in Bélem. The district is home to some of Lisbon’s most interesting historical monuments, including Bélem Tower and the 16th century Jeronimos Monastery – both UNESCO World Heritage sites. The imposing, ornate monastery was paid for by taxes imposed on the spices that flowed into Portugal during the Age of Discovery. At the entrance you’ll find the tomb of Vasco de Gama, the first European to reach India by sea, opening the era of
European colonisation of the Indian subcontinent. Be sure to take in the limestone cloisters, intricately carved with images of rope, coral or sea monsters.
Bélem is the birthplace of pastéis de nata, Lisbon’s most famous delicacy. A short walk from the monastery you’ll find Café Pastéis de Bélem, which has been making these egg custard tarts to a secret recipe for almost 200 years. The café has been open since 1837, and now sells 20,000 tarts a day. Enjoy yours with a coffee in the beautifully tiled interior, or take them with you and eat as you explore the rest of Bélem.
There’s more to Lisbon’s food scene than pastéis de nata. Round off your visit with a prego (steak sandwich) at Rui dos Pregos, or visit one of Lisbon’s food markets to sample everything the city has to offer under one roof. Mercado da Ribeira, a former fruit and veg market, is one of the largest and most popular. Come for a look around and enjoy specialties like Polvo à Lagareiro, octopus with potatoes in a garlic and olive oil sauce. If you’d rather have a more authentic taste of Lisbon, head west to Mercado de Campo de Ourique. This busy market serves traditional Portuguese food as well as selling fresh fish, fruit and vegetables to local shoppers. Sit up at the counter with a plate of salt cod fritters and a cold glass of vinho verde and watch the world go by.


Bélem is the birthplace of pastéis de nata, Lisbon’s most famous delicacy.



