PRESIDENT'S CHOICE
This new session recognises the top abstract presentations across all four domains.
BUILDING A HEALTHY FUTURE

This year's Honoured Guest speaker provides fascinating insights into the health challenges of Benin. Page 15



This new session recognises the top abstract presentations across all four domains.

This year's Honoured Guest speaker provides fascinating insights into the health challenges of Benin. Page 15


This year a record number of abstracts were submitted for consideration, showcasing the latest science and research. Our domains and task forces have worked hard reviewing and selecting the very best abstract presentations to feature in the scientific programme.
In fact, such was the standard of submissions this year, that we will be presenting some abstracts in poster format. These are available to view around the conference centre and I encourage you all to read them. The top four abstracts across each domain will be presented during a new ‘President’s Choice’ plenary on Thursday morning.
Techno-College leads the way at this year's Annual Meeting. Page 3
I am delighted to welcome you all to the beautiful city of Vienna for the 37th EACTS Annual Meeting. It is a city that holds many good memories for EACTS as the home of our first Annual Meeting nearly 40 years ago.
The meeting has changed considerably since that time, growing in size and international reputation to become one of the largest events for the cardiothoracic community around the world.



In addition to excellent abstract sessions, we also have a first-class programme of talks by invited experts from around the world, who will share their knowledge and insights across many subjects. Over the next few pages our domain chairs have outlined some sessions you won’t want to miss.
From a personal point of view, I am looking forward to Saturday’s ‘Trial Update’ during which we will examine
the current progress and findings of major trials in our field, including the UK Mini Mitral Trial and the EVOLUT Low-Risk Trial.
Last year we held two fantastic late breaking clinical trials sessions, and with an increasing number of highquality trials, I am delighted that we have had to increase to three late breaking sessions. We have selected the very best, high impact trials to be presented during the Annual Meeting, with selected manuscripts being published simultaneously in highimpact journals, so I urge everyone to attend these important sessions.
The ‘2023 Guideline Session’ on Saturday morning is also not to be missed. Evidence-based clinical guidelines are critical for delivering the highest standards of patient care and EACTS has an active and influential role to inform clinical practice by developing new practice guidelines. Currently, we are working on 22 guidelines, many in collaboration with different organisations globally.
We have selected some key guidelines to be presented and discussed by our different task forces and domains throughout the Annual Meeting, continued page 2
CONTINUED FROM PAGE 1
including the review on the left main chapter of the myocardial revascularization guidelines, the management of infective endocarditis and, of course, the new aortic guidelines, which have been developed with STS and AATS.
The 37th EACTS Annual Meeting marks the first time we have invited our colleagues from the European Society of Cardiology (ESC) to host their own session, reciprocating an invitation to their meeting in August. Hosting joint sessions with other societies really brings together the ‘heart team approach’ and is an opportunity to learn different approaches to some of the same problems that we experience as surgeons.

In Friday’s ‘Life and Advice from Giants in Cardiac Surgery ’ session we will pay tribute to some of the true giants of cardiac surgery – Carlos Mestres, Ernst Wolner, Sir Bruce Keogh and David Adams. We will learn about their experiences, their history and how they came into cardiac surgery. This will be a fascinating session.
When I ask peers and colleagues what they are most looking forward to at this year’s Annual Meeting they of course highlight the opportunity to learn more about the high-
quality research, the latest innovation and trials for which the meeting has become renowned, but it is striking just how much we all relish the chance to get together, meet with peers from around the world and share experiences. I am looking forward to meeting as many of you as possible over the coming days.
I have been fortunate to attend many Annual Meetings over the years and this year it is a special privilege to be here for the first time as your Secretary General. I hope you enjoy these very special days in Vienna. The Annual Meeting is a work in progress, and we are trying new ways of bringing us all together to discuss our practices and the latest science that guides this practice. Please don’t hesitate to reach out to me to discuss how we could make the meeting even better in the future.
“We have selected some key guidelines to be presented and discussed by our different task forces and domains throughout the Annual Meeting”

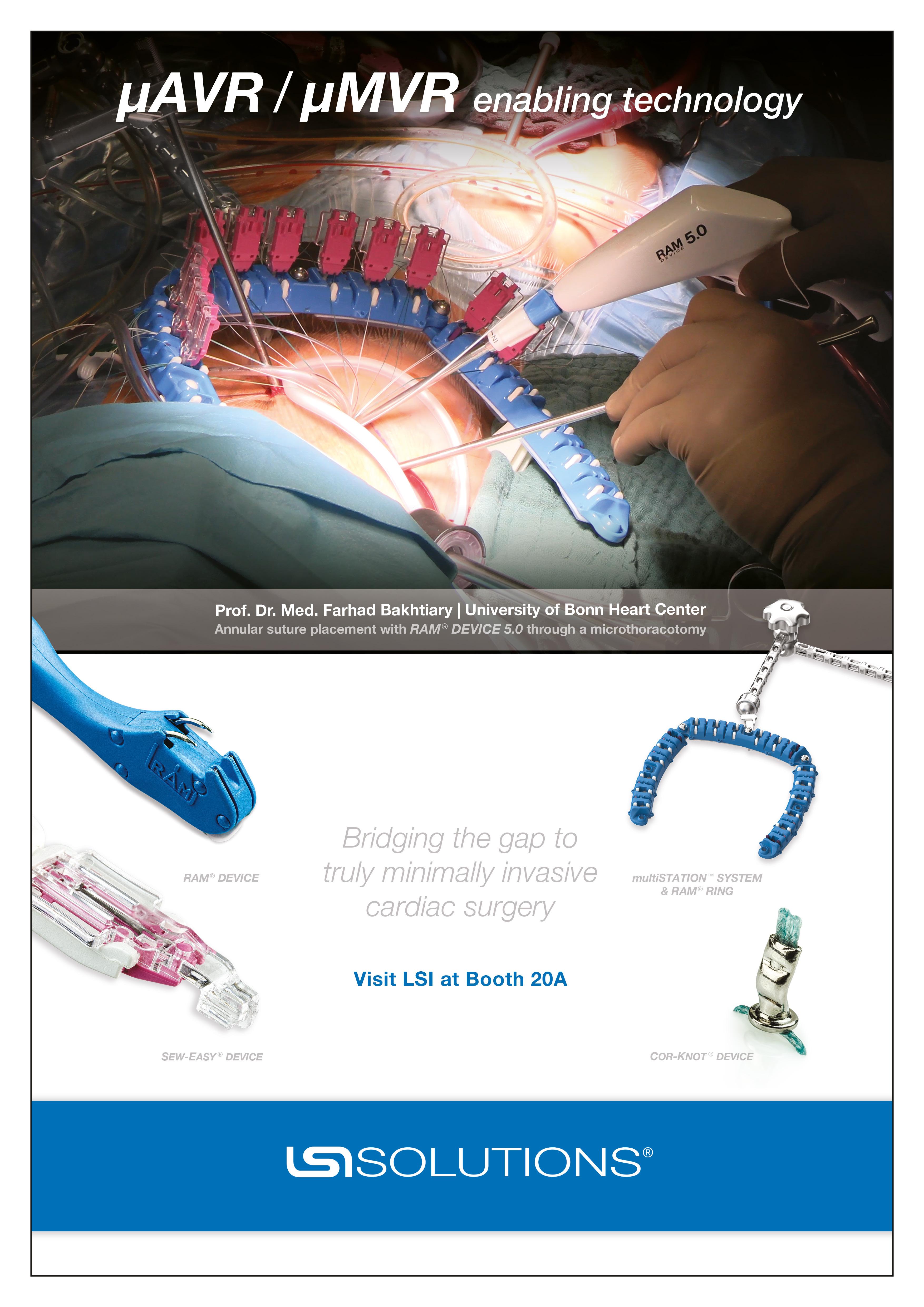
Techno-College has a fantastic reputation for showcasing the latest technologies and surgical techniques in cardiovascular and thoracic surgery. It is the place to be to experience live surgery using the most innovative devices.
Yesterday’s Techno-College once again lived up to all expectations with two ambitious full-day programmes. The cardiovascular stream included demonstrations of minimally invasive aortic valve replacement, focusing on a new technique in annulus enlargement and endoscopic mitral valve repair, which previewed a new holographic imaging technique.



Jörg Kempfert, a member of the New Technology Task Force, said, “This year’s Techno-College had a clear emphasis on new surgical techniques and innovative tools and devices to be used in surgical procedures. Through live cases transmitted in 3D video and live-in-a-box presentations we addressed the emerging topics in patient care as well as some of the prevalent issues facing cardiac surgeons today.”
With over 30 years of clinical use, our proprietary AOA tissue treatment utilizes amino oleic acid and is designed to enhance durable valve replacement — an excellent choice for patient lifetime management.‡

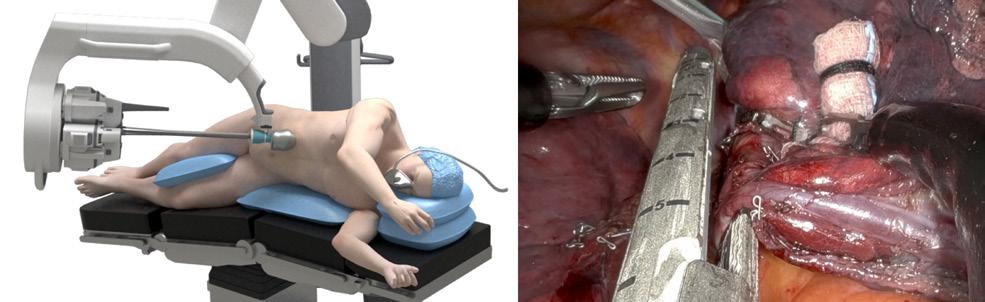
The thoracic surgery programme focused on the surgical and endoscopic management of emphysema, in a joint session with the European Association for Bronchology and Interventional Pulmonology (EABIP), and an afternoon session exploring a broad spectrum of chest wall pathology including surgery for chest wall and sternal tumours. This year we introduced exciting new additions to Techno-College to enhance the learning experience for delegates. A new robotic workshop, supported by Intuitive, gave delegates exposure to robotic devices, including the Da Vinci technology as well as the Ion platform, which is an innovative way of performing robotically-assisted bronchoscopic lung biopsies.
A procedural analyst also joined presenters to provide a structured explanation of the technical details and key features of the latest techniques and devices showcased throughout the day.
Here we share a summary of some of the presentations from yesterday’s Techno-College cardiacvascular programme.

T-next: a new frozen elephant trunk graft to simplify proximal and distal reinterventions
Marco Di Eusanio, Cardiac Surgery Department, Politechinic University of Marche, Ancona, Italy

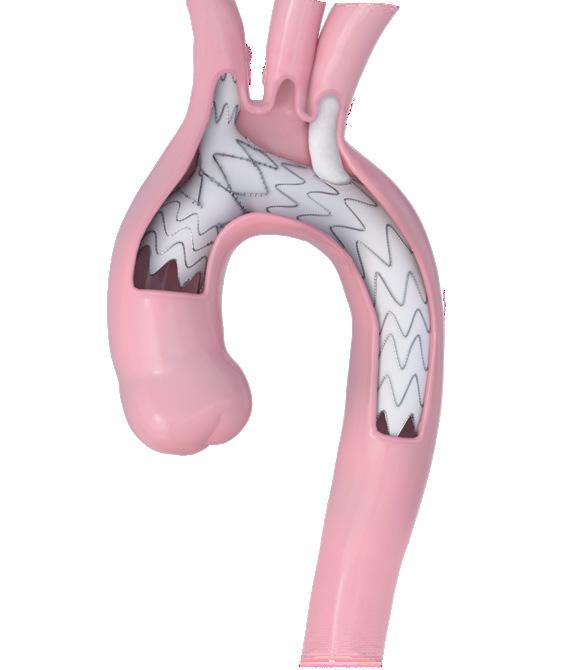
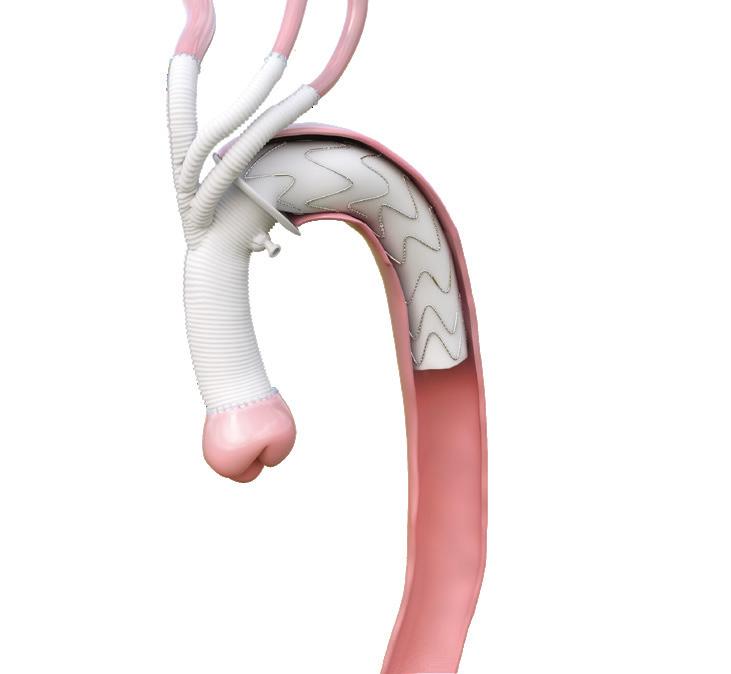
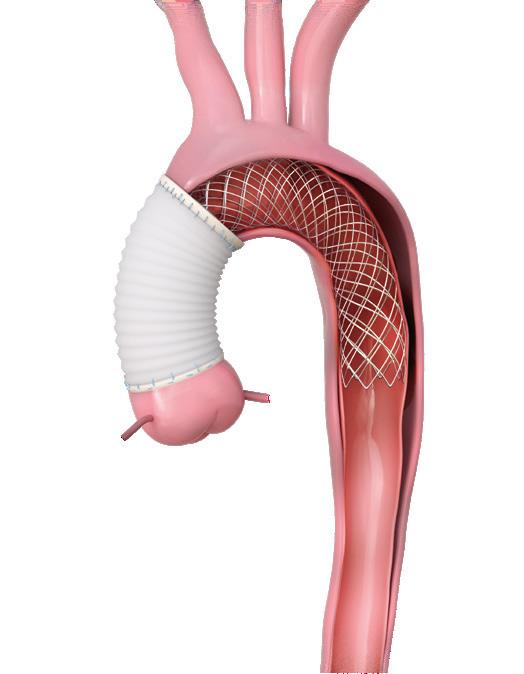
Aortic pathology is progressive in its nature and aortic reinterventions, proximal on the aortic root and distal on thoracoabdominal aorta, are often required following a Frozen Elephant Trunk (FET) operation.
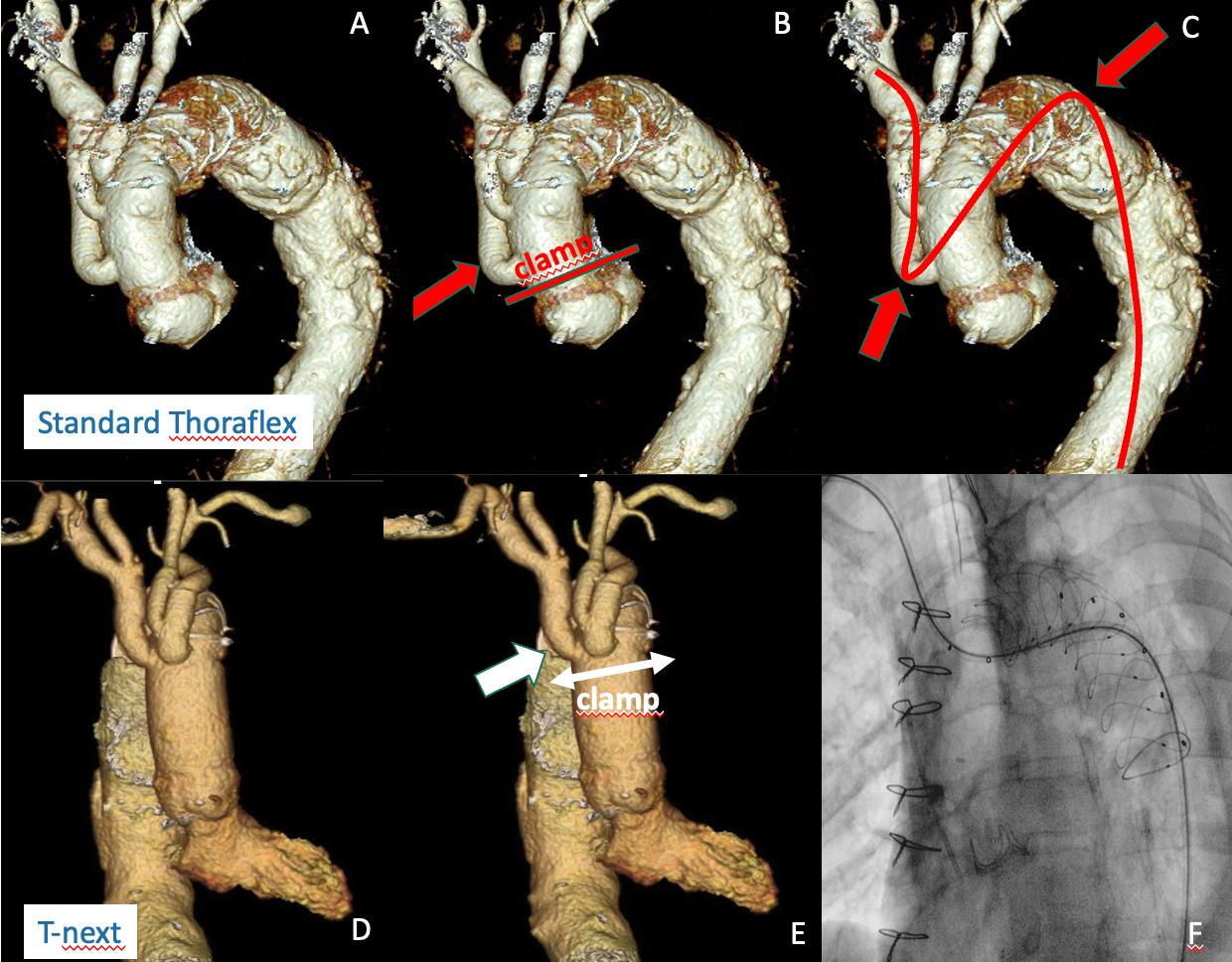
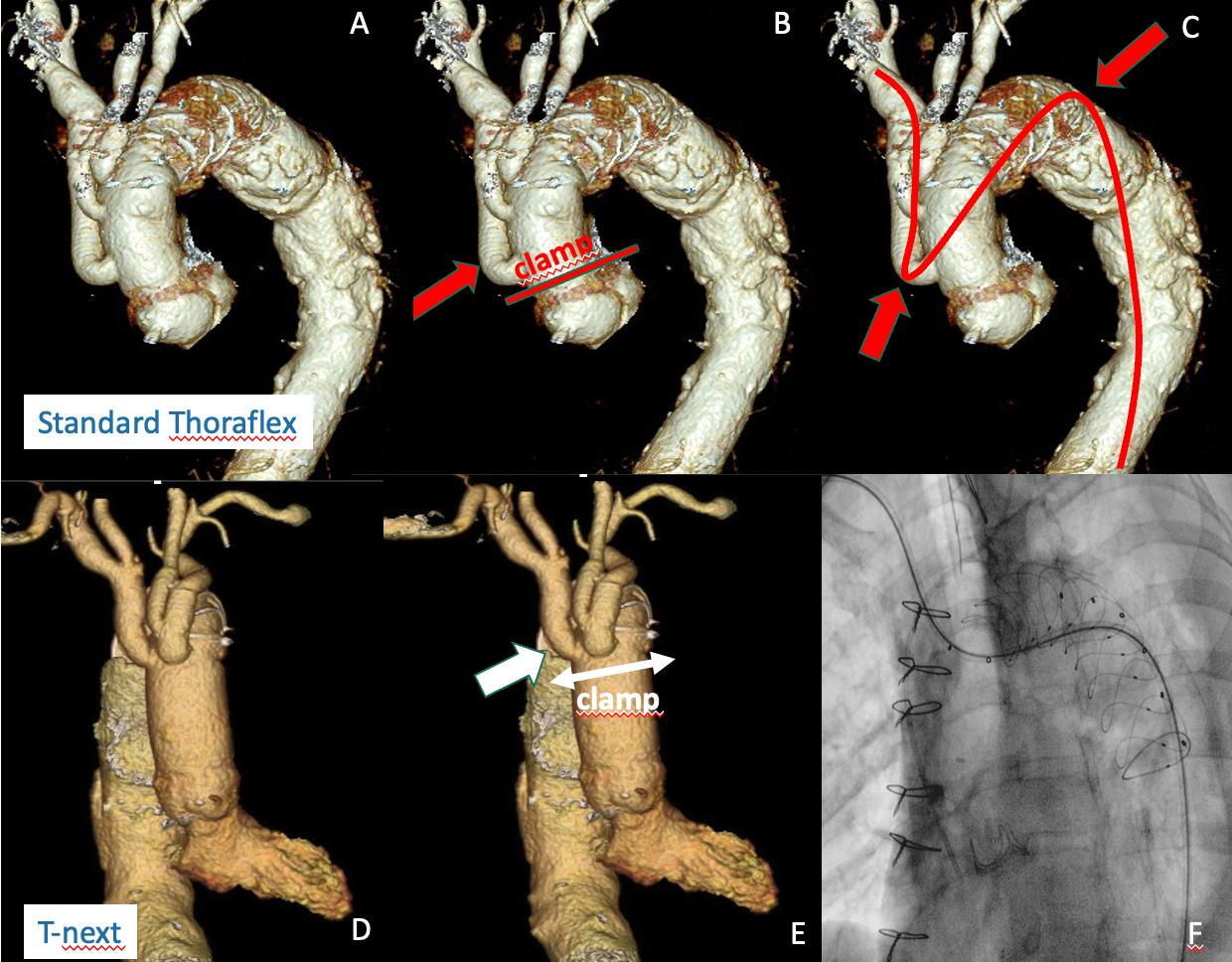
Most of the currently available FET grafts were designed to recreate normal aortic arch anatomy with the distal anastomosis performed distal to the left subclavian artery. However, most aortic surgeons now perform the distal anastomosis more proximally (zone 0, 1 and 2). With the consequential proximalisation of the side branches, access to the aortic root becomes hampered as it requires a very low aortic clamp. Moreover, endovascular thoracoabdominal aorta repairs could also be more difficult as the visceral vessels are arduously cannulated from an upper body access with the double angulation that current FET grafts generate (see Fig. 1 A, B, C below).
T-next is a modified Thoraflex graft with a new distal and transverse arrangement of the side branches that has been designed to simplify proximal root and distal endovascular thoracoabdominal secondary interventions (Fig 2) (1).
A) Currently available FET grafts fail to facilitate secondary proximal and distal interventions if distal anastomoses are being performed in zones 0, 1 and 2; B) The proximal first branch obstacles re-access to root; C, the double angulation prevent a straight antegrade route for wires and catheters from upper body accesses to visceral vessels
This design ensures a proximal graft segment, totally free from other prosthetic structures, and makes sternal reopening less hazardous and facilitates distal
In addition, as demonstrated in our preliminary experience, it preserves a good bidirectional ‘connection’ for wires and catheters between upper and lower body accesses that, after FET, maintain feasible secondary distal visceral vessels stenting during endovascular thoracoabdominal aortic repair intra-cranial cerebral circulation from the femoral arteries (down-top) (Fig.
References
1. T-next: a new custom-made Thoraflex graft to simplify proximal and distal aortic reinterventions. Di Eusanio M, Gatta E.Eur J Cardiothorac Surg. 2023 Jun 1;63 (6)
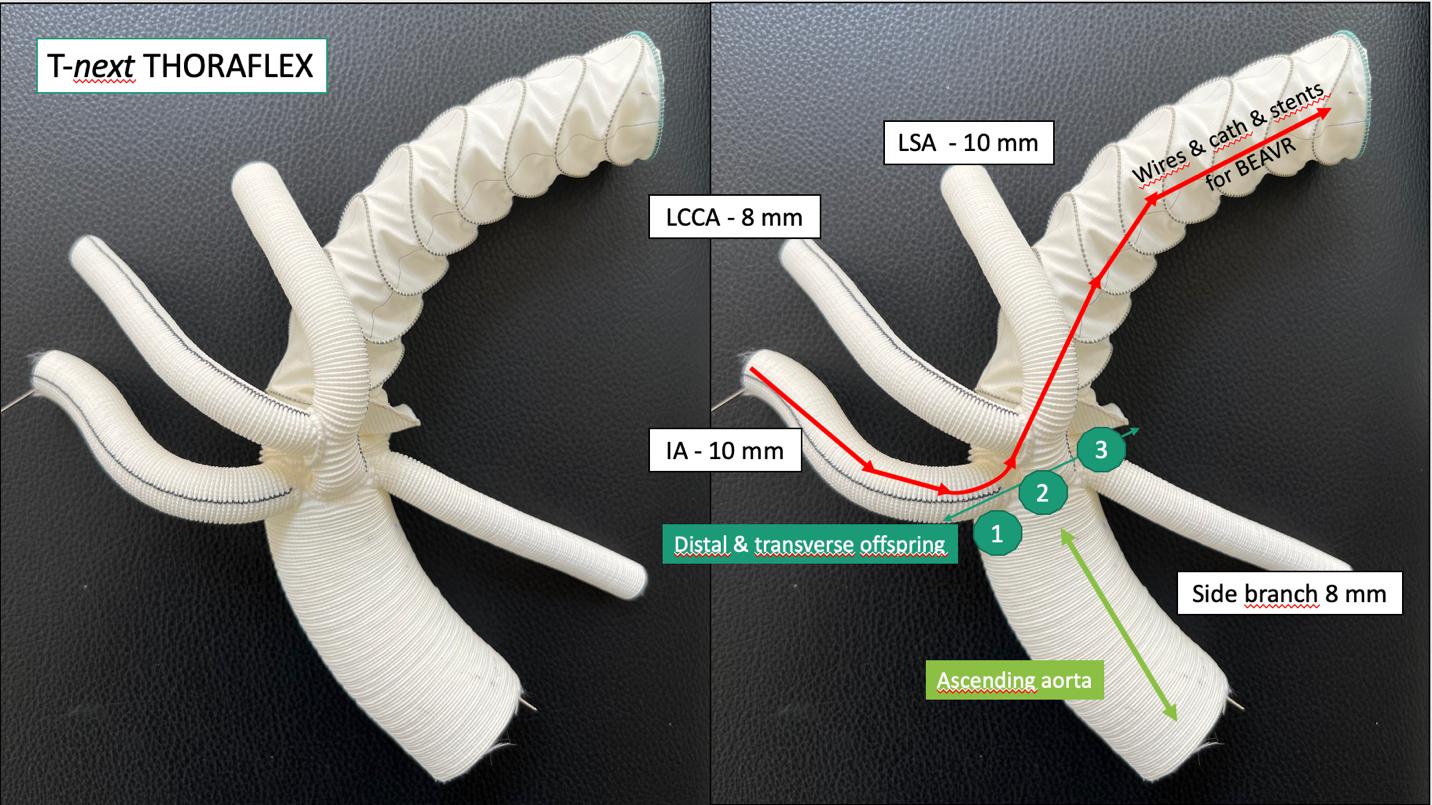

Compared to other FET grafts with one trifurcating branch, we believe that T-next, with an independent IA branch for distal catheterisation, may reduce cerebral complications.
T-next is now available on the Terumo Aortic custom-made platform.
“Most of the currently available FET grafts were designed to recreate normal aortic arch anatomy with the distal anastomosis performed distal to the left subclavian artery. ”Michela Bezzi
The "Excimer laser-assisted nonocclusive anastomosis" technique is an innovative procedure which aims to revolutionise coronary artery bypass graft surgery, improving patient outcomes and surgical efficiency.
Through a live demonstration of the Elana Heart Bypass Procedure during Techno-College delegates were able to see firsthand the benefits and capabilities of this technique and the potential impact of this technology on the field of cardiac surgery.
This advanced system aims to offer a more standardised technique for performing coronary artery bypass graft surgery resulting in predictable anastomoses. By reducing technical complexity and ensuring no interruption of blood flow or leakage during beating heart surgery, the Elana Heart Bypass System represents the potential for superior clinical outcomes, and to boost the run to off-pump and minimally invasive CABG.
The SAFECAB trial, which recently completed its Phase I at St. Antonius Hospital in the Netherlands and in close collaboration with University Hospital Charité in Berlin (Germany), has evaluated the safety and effectiveness of the Elana Heart Bypass System, which incorporates excimer laser technology. With successful short-term clinical outcomes, the SAFECAB trial has entered its Phase II, which involves a larger cohort of 75 subjects, receiving a LITA to LAD anastomosis on a beating heart.


 Marco Solinas, Heart Hospital - Fondazione Toscana G.Monasterio
Marco Solinas, Heart Hospital - Fondazione Toscana G.Monasterio


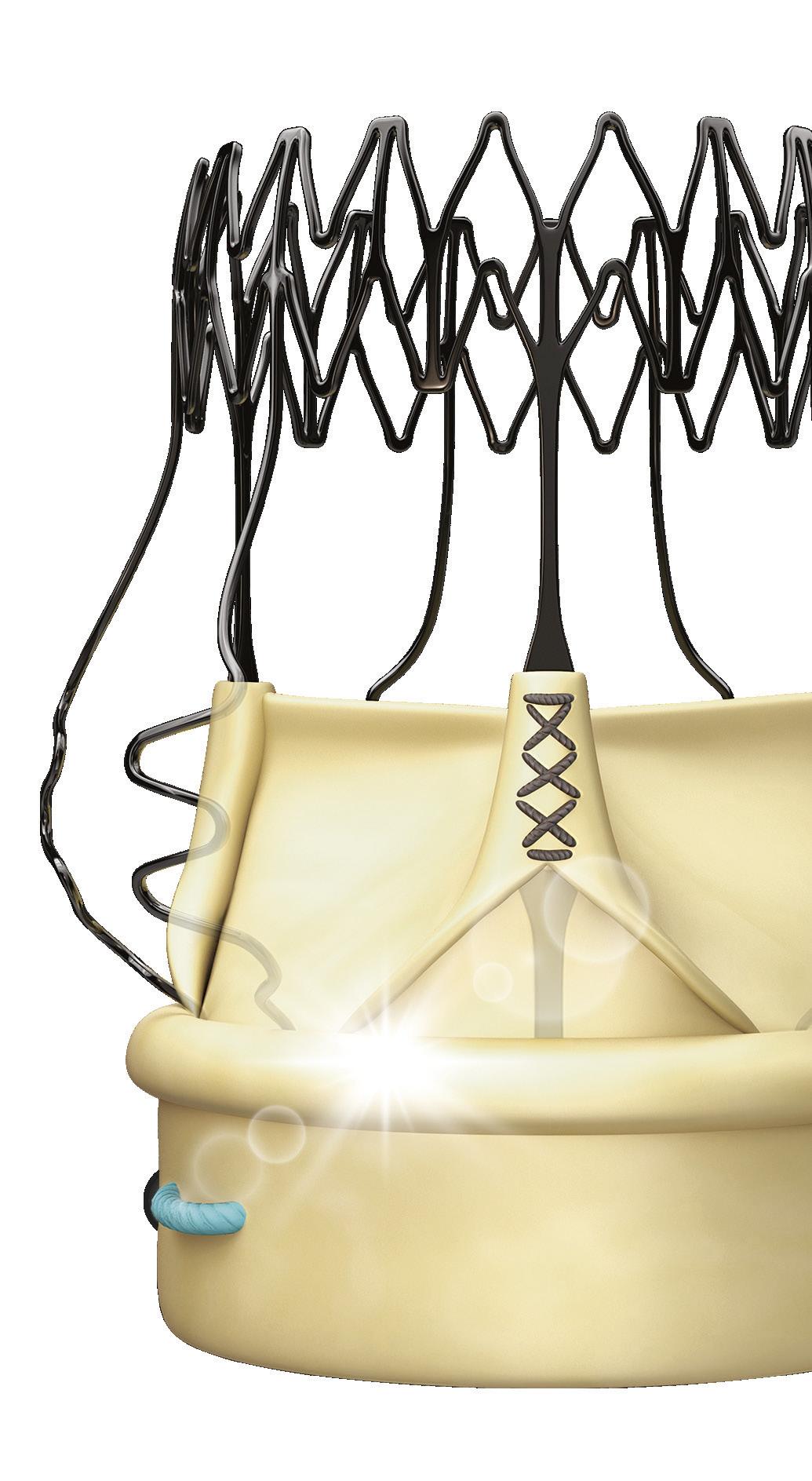
As a co-founder of the Endoscopic Cardiac Surgery Club I am a bit biased talking about endoscopic sutureless aortic valve replacement. I strongly believe that endoscopic cardiac surgery is the way to offer our patients the best procedure available, minimising surgical trauma and emphasising the well- known advantages of minimal invasive surgery.
In my view preoperative angio TC scan is mandatory providing all the anatomical features to work out accurately your procedure in terms of cannulation and surgical approach (2/3 right anterior intercostal space or axillary).
The endoscopic camera allows a perfect view of all the anatomical structures, letting you navigate the thorax to confirm your surgical plan.
Probably the trickiest part of endoscopic AVR is to stitch and knot the prothesis. It is true that nowadays we can count on surgical devices that help us, yet what’s better than working without sutures ?
Sutureless technology seems to be engineered for these procedures in that it facilitates the positioning of the prothesis and shortening the cross clamp time - the Achilles heel of this approach.




In the absence of sutures, we must pay close attention to the decalcification of the native anulus and to the sizing. The native anulus has to be decalcified completely being careful not to make any tear. It is important to let the prothesis expand to its final position preventing leaks. Obviously sizing is crucial. Under–sizing may cause leaks and migration and over-sizing may cause leaks due to folding and may harm the emodynamics performance of the prothesis and lead to a higher rate of pacemaker implantations.
Endoscopic AVR and sutureless technology is a perfect marriage.
This technology has the opportunity to shed light on the cutting-edge advancements in cardiac surgery, the collaboration between medical institutions, and the continuous quest to improve patient outcomes.

“The endoscopic camera allows a perfect view of all the anatomical structures, letting you navigate the thorax to confirm your surgical plan. ”


Hyun Koo Kim has been selected as this year’s winner of the Techno-College Innovation Award in recognition of his innovative miniatured endoscopic C-arm with ultra-low radiation exposure for image-guided surgery. The miniatured endoscopic C-arm offers a safe and convenient alternative to the C-arm used during minimally invasive surgery. Unlike the bulky C-arms, the endoscopic C-arm is suitable to use in narrow operating rooms and is very easy to handle. According to Kim, this new device has ultra-low radiation exposure, with an anticipated 1/400 times reduction in radiation compared to C-arm.
A third-generation prototype has already undergone testing and patents have now been secured in a number of countries including the US and the EU.
Hyun Koo Kim said, “It is an honour to be awarded the Techno-College Innovation Award and gain critical exposure for the endoscopic C-arm. I look forward to moving to commercialisation so thoracic surgery teams and their patients can benefit from this innovative device, which has the potential to change minimally invasive surgery including robotic surgery.”

Jamshid Karimov, Cleveland, USA
Cardiac De-airing System for Open-Heart Minimally Invasive Surgical Procedures

Henrik Bjursten, Lund, Sweden
Catheter based procedure for treating mitral prolap
Expansion zone designed for potential future valve-in-valve procedures.
*No clinical data are available that evaluate the long-term impact of RESILIA tissue in patients. Additional clinical data for up to 10 years of follow-up are being collected to monitor the long-term safety and performance of RESILIA tissue.
**Refer to device instruction for use for important warnings related to the VFit technology. This feature has not been observed in clinical studies to establish the safety and e ectiveness of the model 11500A for use in valve-in-valve procedure.
VFit technology in available in 19-25mm.


Medical device for professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards, Edwards Lifesciences, the stylized E logo, INSPIRIS, INSPIRIS RESILIA, RESILIA, and VFit are trademarks of Edwards Lifesciences Corporation or its a liates. All other trademarks are the property of their respective owners.

© 2023 Edwards Lifesciences Corporation. All rights reserved. PP--EU-6821 v1.0
Edwards Lifesciences • Route de l’Etraz 70, 1260 Nyon, Switzerland • edwards.com

THE SUPPORT OF OUR INDUSTRY PARTNERS IS IMPORTANT. WE WOULD LIKE TO THANK OUR TECHNO-COLLEGE SPONSORS.SILVER BRONZE
The only valve with VFit technology**
Our domains are member-led groups working across four specialties: acquired cardiac, congenital heart disease, thoracic disease, and vascular disease, to drive forward the Association’s mission of advancing education and promoting research to achieve better patient outcomes.
With the support of the associated task forces, experts on the domain committees are responsible for developing the Annual Meeting’s scientific programme.
To help plan your schedule at the 37th EACTS Annual Meeting, the domain chairs have outlined some of the key sessions in this year’s programme.
What are the key sessions you would recommend to delegates?
There are so many excellent sessions this year that singling out a particular focus or abstract session is always very difficult. All are worthy of a mention!
Aortic valve repair has featured in the scientific programme for a number of years, but it remains a ‘hot topic’. We can look forward to interesting discussions in Thursday’s session on ‘Aortic valve treatment – durability and lifetime management’ around the treatment of young people with aortic valve disease.

What can delegates expect from the Acquired Cardiac Disease Domain this year?
The Acquired Cardiac Disease Domain has worked hard to ensure that this year’s programme features quality scientific content. Our main goal is to provide the data behind the facts.
The domain’s task forces have identified the most prevalent and important topics across their fields of cardiac surgery for this year’s scientific programme, as well as the expert speakers from across Europe and the US who will deliver their wisdom and science.

We are also delighted to host several joint sessions with other surgical societies. There are many benefits to co-operating with other organisations, bringing together our surgical minds and sharing views.
Artificial intelligence (AI) is a topic that frequently features in the news, so it is timely that we explore the role of AI in medicine. The session ‘Artificial intelligence in procedural planning and performance in transcatheter techniques’ will consider the place of AI in cardiovascular imaging as well as the potential for AI to speed up and evaluate echo data in transcatheter procedures.
The domain has also focused on fields that are rapidly expanding and evolving, such as concomitant atrial fibrillation surgery. The focus session on Thursday afternoon ‘Innovation and experience in the latest concomitant atrial fibrillation surgery’ will consider the latest data on long term outcomes and innovations.
We can expect great discussions during Thursday’s session ‘Supporting the economics of patient management and procedures in cardiac surgery through science’. As treating physicians, we must always consider the economic impact of our decisions. This engaging session will get us all thinking about how we can be more efficient in managing our cardiac programme.
Why is the Annual Meeting so important to the cardiothoracic community?
The professional connections forged over the next few days – among peers and industry –are really what makes the Annual Meeting so special. It is always great to see friends, past fellows and former residents who may now work in other places. In my view, these are the most enjoyable moments of the meeting.
I would like to thank the task force chairs who are coming to their end of the term for their hard work and commitment over the past three years. I look forward to welcoming the new chairs who will begin their term after the Annual Meeting.
Members of the Acquired Cardiac Disease Domain
• Filip Casselman
(Chair)
• Patrick Myers
(EACTS Secretary General)
• Fabio Barili
• Manuel Castella
• Gry Dahle
• Michele De Bonis
• Ruggero De Paulis
• Gloria Färber
• Mario Gaudino
• Juan B. Grau
• Wouter Oosterlinck
Filip Casselman, Chair, Acquired Cardiac Disease DomainCan you tell us a little more about some of this year’s key sessions?
All our abstract and focus sessions offer excellent learning opportunities but there are few sessions that, in my view, are not to be missed.
This morning we have a fascinating focus session exploring some of the technical controversies in robotic thoracic surgery. This session, developed by our new Robotic Thoracic Surgery Task Force, will discuss the variations of the robotic approach.
What can we expect from the thoracic domain at this year’s Annual Meeting?


Members of the Thoracic Disease Domain have worked hard over the past few months to put together an exciting and ambitious scientific programme.
We were delighted to kick-off the Annual Meeting with yesterday’s fantastic Techno-College programme which focused on the surgical and endoscopic management of emphysema and chest wall surgery.
We have carefully reviewed and selected the very best abstracts to feature in the thoracic programme and included focus sessions that address some of the most topical issues in our specialty, such as sublobar resection for early stage lung cancer and mesothelioma.

I recommend delegates attend this morning’s ‘President’s choice’ session which features the highest scoring abstract from each of the domains. All-in-all, we are looking forward to lots of discussion, debate and audience participation.
The involvement of residents in the Annual Meeting is essential and a particular highlight of this year’s meeting is the MDT session on Thursday afternoon. Residents from across Europe will present interesting cases and we can look forward to lots of interaction with the audience as we discuss the best response to each scenario. Finally, I highly recommend one of the last sessions taking place on Saturday. when we will examine the recently released 9th TNM edition for NSCLC which will undoubtedly have an impact on our daily life as surgeons. This will be a great opportunity to discuss the latest classification and learn more about the impact of the new edition on (neo-)adjuvant treatment options.
What trials and guidelines will be discussed?
At Thursday afternoon’s focus session on Mesothelioma there will be an opportunity to hear the results of the recent MARS2 trial, as well as exploring the technical aspects of surgery for this condition.

The ‘Controversies in sublobar resection’ session on Friday morning will, I'm sure, prove to be an exciting one, where the more contentious issues in this expanding patient cohort will be discussed. In terms of guidelines, we are hosting a joint session with ERS and ESTS on Friday to discuss the recent clinical guidelines on pneumothorax
Friday 6 October 2023
17:45 - 18:30
Location: Hall K2
management, presenting the views of a respiratory physician and a surgeon. Guidelines on Ground Glass Opacities will also be discussed in a separate focus session on Friday.
What opportunities are available to gain hands-on experience?
The Learning Lab is always such a popular and successful part of the Annual Meeting so, as a domain, we think carefully about the hands-on opportunities that we can offer.
This year we incorporated a robotic workshop that ran parallel to yesterday’s main thoracic TechnoCollege programme. Supported by Intuitive, this gave surgeons, irrespective of their prior robotic experience, a unique opportunity to gain handson exposure to both the Da Vinci technology and the Ion platform.
Over the next three days we are delighted to have access to more VATS simulation as well as the opportunity to get hands-on experience in rib fixation. Tickets for these Learning Lab sessions are available on site.
• Richard Milton
• Tim Batchelor
• Korkut Bostanci

• Fabian Dörr
• Marion Durand
• Vincent Fang
• Bernhard Moser
• Tomaž Štupnik
Friday’s abstract session on ‘conotruncal defects’.
We will also explore some of the smaller problems which can still present challenges for our daily practice. For example, how to deal with a leaking atrioventricular valve after CAVSD repair.
What are the key sessions you would recommend to delegates?
Innovation in cardiac surgery is critical to achieving better outcomes for our patients. In a fascinating Friday session on ‘Innovations in pediatric and congenital cardiac surgery’, two invited speakers will share their experiences and advice about taking innovations into the marketplace.
What can delegates expect from the Congenital Heart Disease Domain at this year’s Annual Meeting?
We have a very strong scientific programme featuring invited speakers and abstract presenters. The domain received a record number of abstract submissions this year, so the standard of science is extremely high. In total, almost 50 abstracts will be presented as part of the Congenital Heart Disease Domain during the meeting or displayed in poster format.
Important topics such as single ventricle physiology feature strongly in the programme and we are also keen to address areas that haven’t been covered in recent Annual Meetings such as
We have worked with the EACTS Residents’ Committee to design a unique session on surgical training. This session, taking place on Friday afternoon, offers a trainee’s and mentor’s perspective of an ideal training programme and importantly explores the topic of resilience and how to manage stress and trauma in surgery. I recommend this session not just for residents but also to support congenital heart surgeons who have a training role and want to consider the best way to teach residents and bring them to independent practice.
What does this year’s Learning Lab have in store for delegates?
The wet lab will be very interesting as participants will have the opportunity to use a piglet heart to gain hands-on experience of enlarging the left ventricle outflow tract to insert an adult size valve
prothesis. This is not an operation carried out in adult cardiac surgery, but it is an important procedure in congenital surgery to avoid changing the valve several times until adulthood.
In your view, what makes the Annual Meeting so special?
Congenital heart surgery is a small sub-discipline so it’s wonderful to get together with colleagues from around the world.
It is always fascinating to have discussions with colleagues from parts of Africa and the Middle East, where congenital heart surgery is quite different. Having the opportunity to learn from their experiences, particularly about some special heart defects, is invaluable.
• Jürgen Hörer
• Werner Budts
• Mark Danton

• Eva Sames-Dolzer
• Amir-Reza Hosseinpour
will undoubtedly impact many patients worldwide – from those with the most common forms of aortic disease to patients with rare forms such as genetic hereditary disorders and connective tissue disorders. These new guidelines offer insights into aortic disease and consider all aspects of patient care, not just indications for surgery.
The Management of Aortic Disease guidelines will feature in many of our sessions at the Annual Meeting, with discussions around what is new and different and how we can interpret these guidelines in relation to new developments.
What can delegates expect from the Vascular Domain at this year’s Annual Meeting?
The key event for the Vascular Domain at this year’s Annual Meeting will be the presentation of the newly developed guidelines for aortic disease. These guidelines are not just significant for cardiovascular surgeons but for the entire medical community and
Today’s focus session ‘Aortic Disease - A deeper dive into Guideline Details’ is a particularly important session and will be the first opportunity to learn more. Aortic dissection also features prominently in the scientific programme as one of the most topical issues for our domain. In this afternoon’s session ‘Aortic Dissection: Concepts to improve your practice’ we can look forward to discussions on the need to differentiate treatment for patients with Type A aortic dissection.
• Kirolos Jacob
• David Kalfa
• Tomasz Mroczek
Interestingly, this session will explore data from large registries and multi-centre studies, which are still quite unusual in cardiac surgery. As a specialty we are working hard to build a solid basis of evidence and insights by analysing large registries and multicentre trials so this should be a fascinating session. I highly recommend this morning’s President’s Choice session which recognises the top abstracts across the four EACTS domains. The abstract from the Vascular Disease Domain examines whether and when to replace the aortic root in Type A dissection. It is a very important paper which we believe may impact future guidelines.
• Konstantinos
Tsagakis
• Martin Czerny
• Nimesh Desai

• Davide Pacini
• Florian Schoenhoff
• Andreas Zierer
 Konstantinos Tsagakis, Chair and Florian Schönhoff, Deputy Chair, Vascular Disease Domain
Jürgen Hörer, Chair, Congenital Heart Disease Domain
Konstantinos Tsagakis, Chair and Florian Schönhoff, Deputy Chair, Vascular Disease Domain
Jürgen Hörer, Chair, Congenital Heart Disease Domain
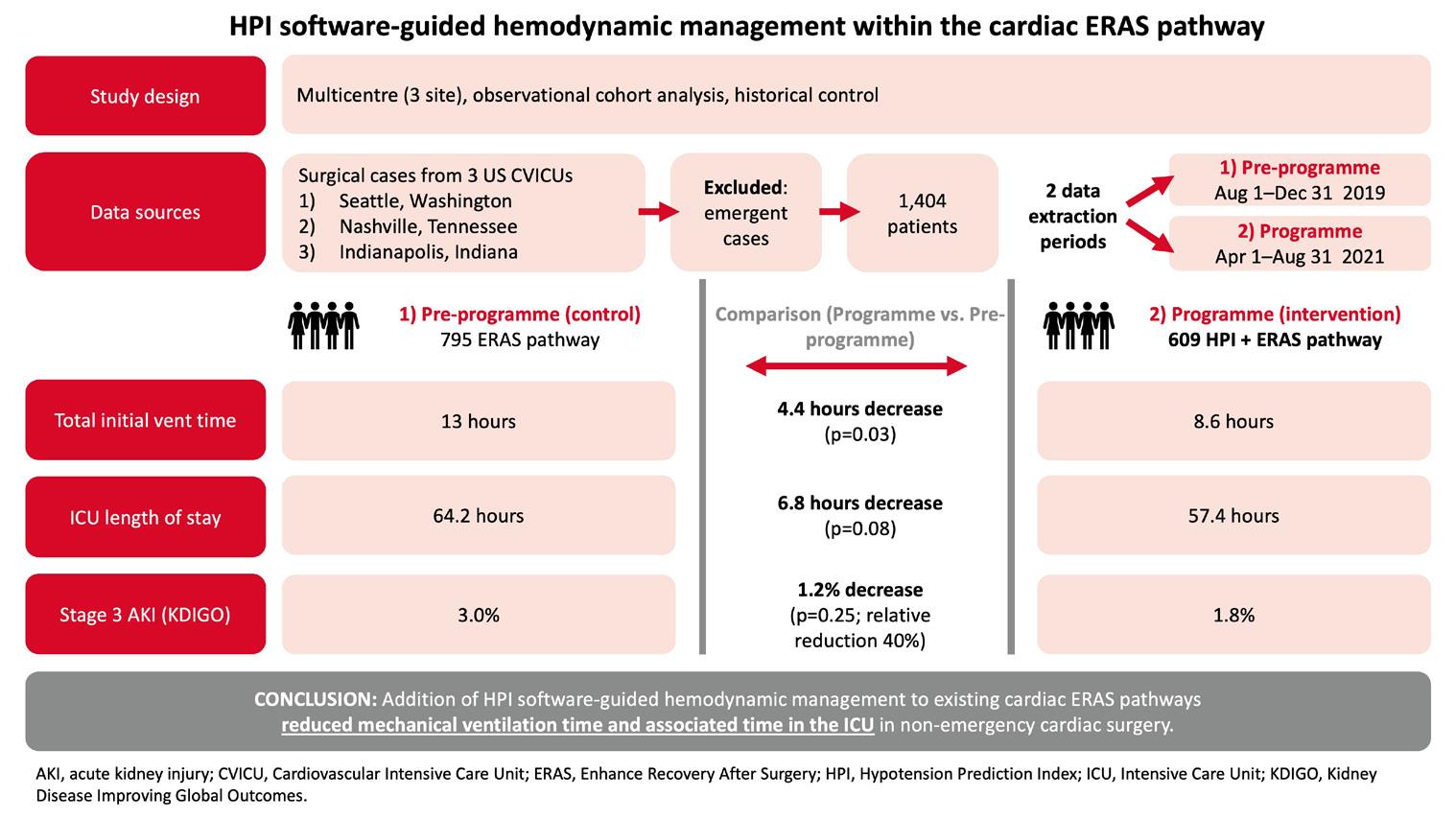
Supporting haemodynamic stability has become a key element of cardiac Enhanced Recovery After Surgery (ERAS) protocols. Now, new evidence indicates that integrating artificial intelligence (AI)-guided haemodynamic management into ERAS pathways can bring clinical benefits.
Supporting haemodynamic stability has become a key element of cardiac Enhanced Recovery After Surgery (ERAS) protocols. Now, new evidence indicates that integrating artificial intelligence (AI)-guided haemodynamic management into ERAS pathways can bring clinical benefits.
This new data was published in a multi-institution review authored by Seenu Reddy (TriStar Centennial Medical Center, Nashville, TN, USA) and colleagues1. Introducing this study, Dr Reddy first explained the rationale: “One of the recommendations of ERAS is goal-directed fluid management, but we see a lot of variation in how this is done. We hypothesised that by using an AI-enhanced tool to set a rational and visible management algorithm, we’d see improvements in ERAS pathways across different centres.”
The study involved three US centres that integrated Acumen™ Hypotension Prediction Index software (Edwards Lifesciences, Irvine, CA, USA) into their cardiac ERAS pathways. This AI-enhanced software uses arterial waveform analysis to predict the likelihood of an upcoming hypotensive event. When this likelihood exceeds a threshold, alarms are triggered and additional haemodynamic variables can be displayed to guide intervention.
The centres adopted Acumen HPI™ software in March 2021, and data was collected for five-month periods before and after the software was introduced (with the ‘pre-programme’ period set in late 2019 before the coronavirus pandemic). A total of 1,404 first-time cardiac surgery cases were included (795 pre-programme, 609 programme). Results were encouraging: total initial ventilation time was 4.4 hours lower (p=0.03) and intensive care unit (ICU) length of stay 6.8 hours lower (p=0.08) overall when Acumen HPI software was used as part of the cardiac ERAS pathway.
Reflecting on these results, Dr Reddy emphasised that the data was gathered from three different institutions. “These centres all had different capabilities and care setups, so this is very much a real-world study.”
Looking in more detail, the authors noted a reduction in cases with a total initial ventilation time of ≥24 hours (5.4% to 2.8%; p=0.016) and those with an ICU stay of ≥72 hours (26.7% to 21.7%; p=0.036) from the pre-programme to the programme period. These results are important from a health economics perspective, Dr Reddy underlined, given the associated high complication rate and cost of treatment for these patients.
The study also assessed the incidence of acute kidney injury (AKI) using modified Kidney Disease Improving Global Outcomes (KDIGO) criteria. While no significant difference was observed regarding AKI overall, a 40% relative reduction was noted in KDIGO stage 3 AKI from the pre-programme to the programme period (absolute reduction 3.0% to 1.8%; p=0.255). Given the low 3% baseline, the study was not powered to determine the significance of this reduction.
Commenting on this, Dr Reddy acknowledged that larger studies would be needed to investigate further – but also observed that the level of care in the study centres could affect the magnitude of the effect seen. “These centres were already offering advanced therapies in terms of enhanced recovery,” he noted. “Perhaps we’d see more of an effect in centres that aren’t as evolved in their cardiac ERAS plans and goal-directed fluid management algorithms.” Further examination of the data revealed a valuable insight in addition to the headline results. Improved clustering of datapoints and smaller standard deviations around the mean were observed for several endpoints when Acumen HPI™ software was used, implying lower variability of care. Dr Reddy observed that the potential for reducing variability-associated morbidity is an exciting implication of this study.
“I think this is actually the most powerful element of this study: we saw reductions in variability across all institution,” he said. “And this is even more notable because the Acumen HPI™ utilisation period was disrupted by the pandemic. Despite the very high rates of nursing turnover in that tumultuous period, we saw a clear reduction in variability of care. Standardisation and reduction of care variability are at the very heart of enhanced recovery.”
A key point here is that the benefit of standardisation was seen even though interventions were not specified; the software was used as a decision support tool, and teams were afforded freedom regarding action. This flexibility has encouraging implications for real-world adoption.
Looking ahead, Dr Reddy is optimistic about a move towards AI-guided haemodynamic management in ERAS pathways after cardiac surgery. “We should seriously consider this,” he suggested. “It gives clear benefits and no perceivable harm.”
Dr Reddy closed by emphasising the value of collaboration between teams in research such as this. “This study was led by cardiac surgery teams, but it relied on fantastic anaesthetists and critical care doctors who worked together for the benefit of patients.”
EACTS' domains have put together an exciting scientific programme featuring the latest research and very best scientific insights. Our packed three-day programme includes 220 abstract presentations selected from a record 1,300 submissions and over 80 focus sessions featuring experts in their field as well as inspiring keynote speakers.
Over the following pages a selection of abstract presenters and invited speakers share summaries of their presentations taking place today at the 37th EACTS Annual Meeting.
Don’t miss today’s President’s Choice opening session at 8:30am in Hall D, which will showcase the leading abstract presentations selected across all four EACTS domains.
PRESIDENT’S CHOICE: ABSTRACT SESSION
Breathomics: May it become an affordable new tool for early diagnosis and screening of lung cancer?
Hall D
08:30 - 09:30
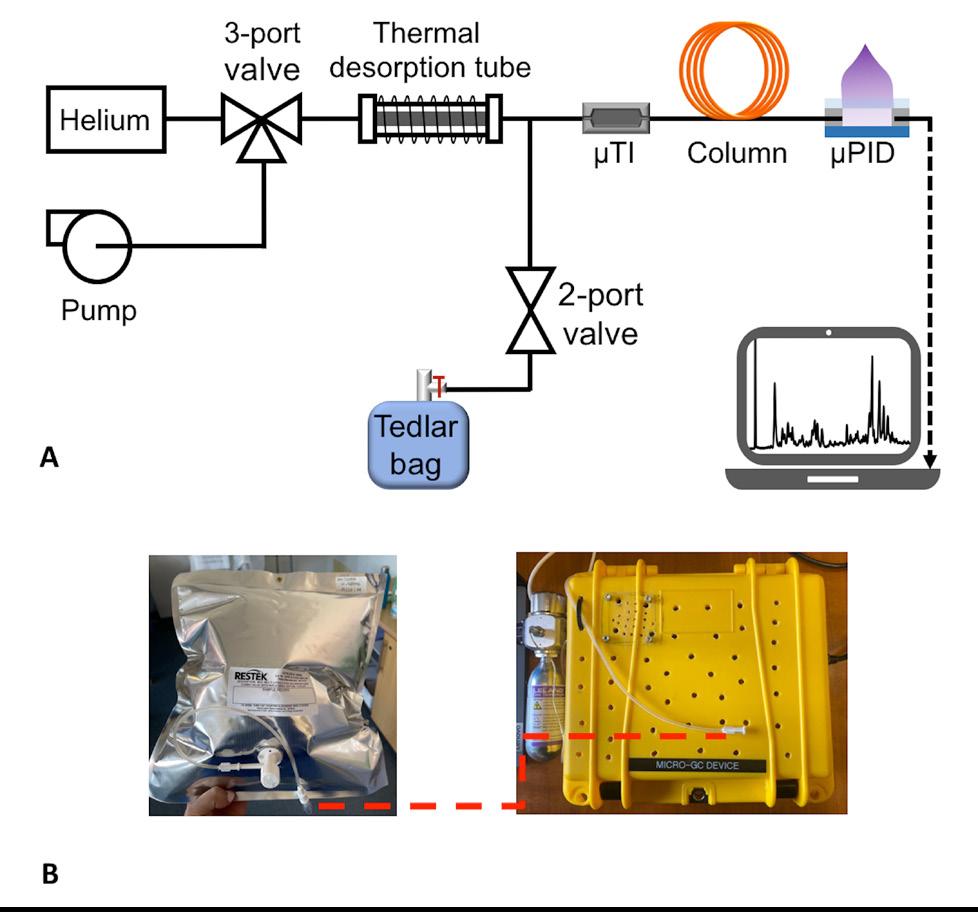
Lung cancer is the primary cause of cancer-related deaths globally. This is mainly because lung cancers are diagnosed only in their late stages, resulting in a lack of specific symptoms and delaying effective treatment. Patients with stage one lung cancer have a survival rate of greater than 60% after five years, and those detected through CT screening can have an estimated 10-year survival rate of 88%. Early detection is therefore crucial for improving survival rates. Unfortunately, current methods for early detection of lung cancer are not reliable. ‘Breathomics’ is a cutting-edge field of metabolomics that studies exhaled breath by using advanced highthroughput techniques like gas chromatography (GC) coupled to mass spectrometry (MS). Since exhaled breath contains several classes of VOCs that could potentially serve as biomarkers for lung cancer, breath analysis is a promising medical diagnostic tool due to its non-invasiveness, affordability, and ease for patients to comply with. However, previous studies on lung cancer have been limited by small sample sizes, collection methods, different analytical approaches, and data processing techniques. Therefore, there is currently no consensus on VOC biomarkers for lung cancer. GC-MS systems, which are known for their high sensitivity in detecting specific VOCs, are expensive and require expertise to operate. Additionally, breath contents needs to be captured and transported to the devices, making them impractical for point-of-care testing.
Our study uses a portable and cost-effective GC device, eliminating common disadvantages and making it usable for point-of-care analysis. Through this device, we discovered a pattern of VOCs primarily from alkane families that can differentiate between non-small cell lung cancer patients and healthy individuals with 85% accuracy. This affordable and portable advanced sensing system offers the significant advantage

Q. Where did you carry out your training?
Six months ago, I completed my thoracic surgery residency at the University of Bari, Italy. During these years, I had the opportunity to visit the University of Oulu in Finland, the University Hospital of Essen in Germany and the Massachusetts General Hospital in Boston as a clinical and research fellow.
Q. What are your main areas of interest within cardiothoracic surgery?
My primary interest lies in clinical research in the field of oncological lung cancer. By analysing the results of our clinics, I hope we will be able to improve our everyday patient management and acquire new skills to enhance our patients' quality of life. My goal is to focus on early detection of lung cancer, as it is the only way to reduce lung cancer mortality.
of enabling testing on larger population samples, with the potential to increase patient diversity. Gathering this information can also be used to improve point-of-care testing devices.

Q. What are you most looking forward to at this year’s Annual Meeting?
As a young thoracic surgeon, I am eager to be inspired and gather as many research ideas as possible from this meeting. I also hope to absorb clinical tricks from the masters of thoracic surgery. I was particularly impressed with the innovative session on AI, robotic workshops and its technical controversies, education and training sessions, sublobar resections, and the discussion on the 9th TNM edition for NSCLC. I am looking forward to learning and growing from these experiences.
Q. What are your interests outside of your work?
Over the summer, I came across a quote in a book that resonated with me: "Every form of art is another way of seeing the world. Another perspective, another window. And science - that's the most spectacular window of all." This sentence truly represents who I am. I am passionate about all forms of art, including drawing and painting, which have also helped me to better understand the technical procedures I observe in the operating room. Additionally, I love singing and I love the power that music has to accompany every step of my life and give it a sound.
Figure 1: (A) Layout of the portable GC device. (B) Photo of the portable GC, showing that a Tedlar bag is connected to the sampling port of the device.“Since exhaled breath contains several classes of VOCs that could potentially serve as biomarkers for lung cancer, breath analysis is a promising medical diagnostic tool due to its non-invasiveness, affordability, and ease for patients to comply with.”
PRESIDENT’S CHOICE: ABSTRACT SESSION
08:30 - 09:30
Statins have long been recognised for their lipid-lowering and pleiotropic properties. However, their precise role in patients with aortic stenosis, particularly those without concurrent comorbidities, remains a subject of debate.
Previous observational studies have indicated that patients might benefit from statin therapy after transcatheter aortic valve implementation (TAVI), but evidence after surgical aortic valve replacement (SAVR) is scarce.
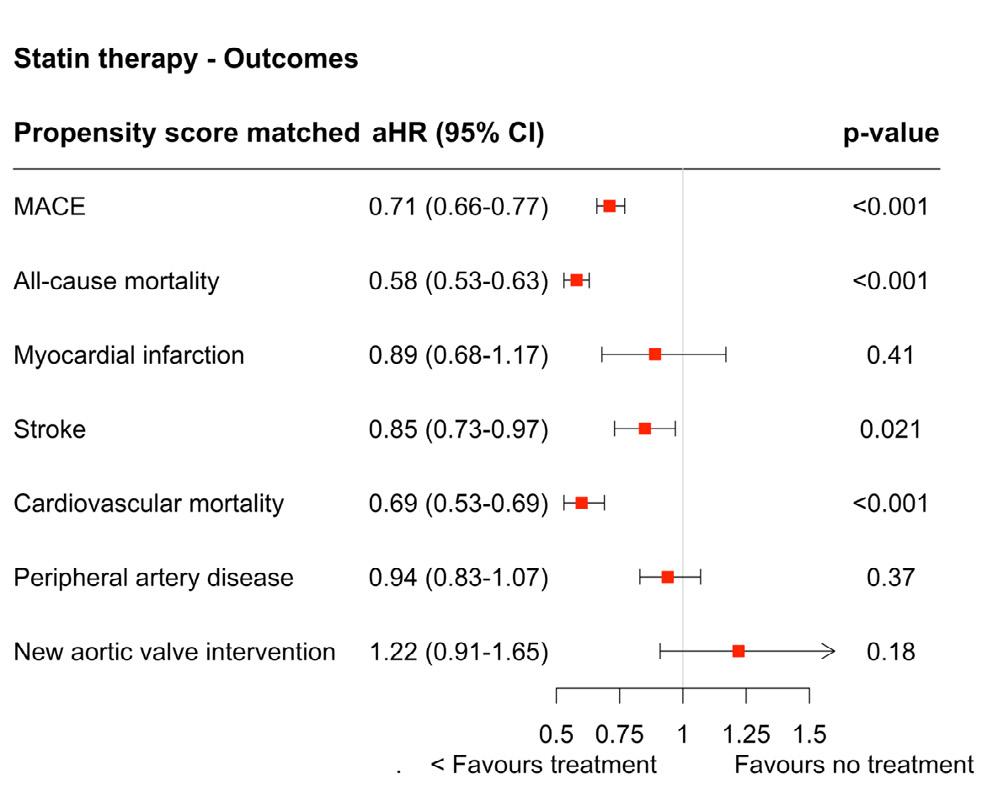
To gain greater insight, we utilised data from a nationwide cohort (SWEDEHEART), spanning 14 years, to examine the association between ongoing statin use and major adverse cardiac events (MACE, defined as all-cause mortality, myocardial infarction, and stroke) in patients who underwent isolated SAVR for aortic valve stenosis.
The SWEDEHEART registry is a prospective quality registry with complete coverage of all cardiac surgery procedures in Sweden since 1992. A total of 11,894 patients were included in the analysis and data from four additional national registries (capturing ICD-codes, mortality, prescribed drugs, and TAVI procedures) with comprehensive follow-up using distinctive personal identification numbers. Uniquely, we have acquired the status of statin use every third month during follow-up, to verify usage patterns in a time-updated manner for the analysis. Approximately 49% of patients were dispensed statin at each time point.
After propensity score matching, the adjusted Cox regression model demonstrated a 29% reduction in MACE and a more marked 42% reduction in allcause mortality in patients that had ongoing statin
Q. Where did you carry out your training?
I completed my medical training and my PhD at the University of Turku, Finland. I then continued with my postdoctoral training at Brigham and Women’s Hospital and Harvard Medical School, in Boston, US. I am currently a cardiothoracic surgical resident at the Hospital Nova of Central Finland and the University of Turku.


Q. What are your main areas of interest within cardiothoracic surgery?
I’m especially interested in the genetics and disease development of aortic diseases, such as ascending aortic aneurysms and dissections, as well as their surgical strategies and outcome research. Another area of interest is secondary
therapy after SAVR. All predefined subgroups, based on sex, age and co-morbidities, showed benefits from statin use, including more pronounced advantages observed for those with hypertension or hyperlipidemia.
Our robust data indicate that aortic stenosis patients undergoing SAVR could potentially benefit from statin use in the long-term, nevertheless, prospective randomised controlled trials in this patient cohort are necessary to establish causality. Meanwhile, clinical guideline committees need to consider whether evidence from this and other similar studies is sufficient to recommend long-term treatment with statins for aortic stenosis patients undergoing SAVR.
PRESIDENT’S CHOICE: ABSTRACT SESSION
Three decades of Fontan operation: preliminary report on early outcomes from the European Fontan registry
On Behalf of the EURO-FONTAN group'
The results of Fontan operation have improved through decades. We report our analysis on early outcomes in the largest cohort ever reported of patients who underwent Fontan completion in the
last 33 years, so as to picture the current surgical results of Fontan operation in Europe. This is a retrospective clinical study including 21 European congenital cardiac centers. Clinical and surgical data were collected by means of a shared REDCAP database between December 2021 and January 2023. We collected 3305 patients (median age 4.1 years) and functional single left ventricle affected 1711 patients (52%). Fontan completion was achieved by a total cavo-pulmonary connection in 98%; extracardiac conduit was the most prevalent technique (89%).
A fenestration was applied in 53%, according to surgeon’s preference. Early death rate was 1.6%, with a 0.8% rate in the last decade, while complications occurred in 48%. In this series, fenestration resulted to be associated to high occurrence of general complications (p < 0.001). The presence of an additional ventricular chamber was significantly associated to postoperative complication (p <0.01), while right ventricular dominance did not affect significantly the postoperative course.
In conclusion, the number of patients offered with Fontan operation has dramatically increased in
prevention medications after open heart surgery. I’m also passionate about surgical education and teaching.
Q. What are you most looking forward to at this year’s Annual Meeting?
It’s my first EACTS meeting, so I’m very excited to explore the diverse scientific topics that it offers, particularly in the field of aortic surgery and dissections. As a resident, I’m especially eager about the learning labs and masterclasses where I can learn from experts. Meeting fellow residents and established professionals, and exchanging insights, are also things I’m genuinely looking forward to.
Q. What are your interests outside of your work?
I love to spend time with my family and friends, as well as to meet new people and explore different cultures. I also enjoy playing piano, running, hiking, and simply being out in nature. I’m always up for trying new things whether it’s experimenting with a new recipe or picking up a new instrument.
Europe in the last 3 decades. Despite operative mortality is nowadays very low, postoperative morbidity is still consistent. In this series, the fenestration of the Fontan circuit did not show a significant positive hemodynamic effect in the postoperative course, probably because performed mostly in higher risk Fontan patients. The presence of an additional ventricular chamber can affect negatively the early postoperative course.
Statin treatment after surgical aortic valve replacement due to aortic stenosis is associated with better long-term outcomes.Emily Pan / Hospital Nova of Central Finland and the University of Turku Adjusted Cox regression analysis between ongoing statin use and primary and secondary outcomes after propensity score matching.
“Fontan completion was achieved by a total cavopulmonary connection in 98%; extracardiac conduit was the most prevalent technique (89%).”MA Padalino / UOC CardioPediatric Surgery, University of Padua
The non-to-moderately dilated root in acute type A aortic dissection: Outcomes of the PENN-BERN registry in young, non-syndromic patients.
08:30 - 09:30
There is an ongoing debate over whether patients benefit more from root replacement compared to a reconstruction of the sinuses of Valsalva, in acute type A aortic dissection.



In those with known or suspected connective tissue disorders, root replacement is considered appropriate. However, there are currently no diameter-based guidelines regarding the best approach in patients with minimally to moderately dilated root and no connective tissue disorders.
From January 2005 to December 2022, a two-centre registry of acute type A aortic dissection was created. Patients were included based on their age (≤60 years), the absence of root entry and dilatation >50mm, and the absence of syndromic hereditable aortic disease. Patients were divided into two groups based on the proximal procedure, root reconstruction and root replacement. Propensity score pair matching was performed based on preoperative characteristics.
Cumulative incidence of reintervention at 10 years was slightly higher after root reconstruction: 13% vs 3.9% in the matched group (p=0.040). Survival at 10 years was not affected by the procedure independently of the matching 72.1% vs 71.4% (p=0.2).
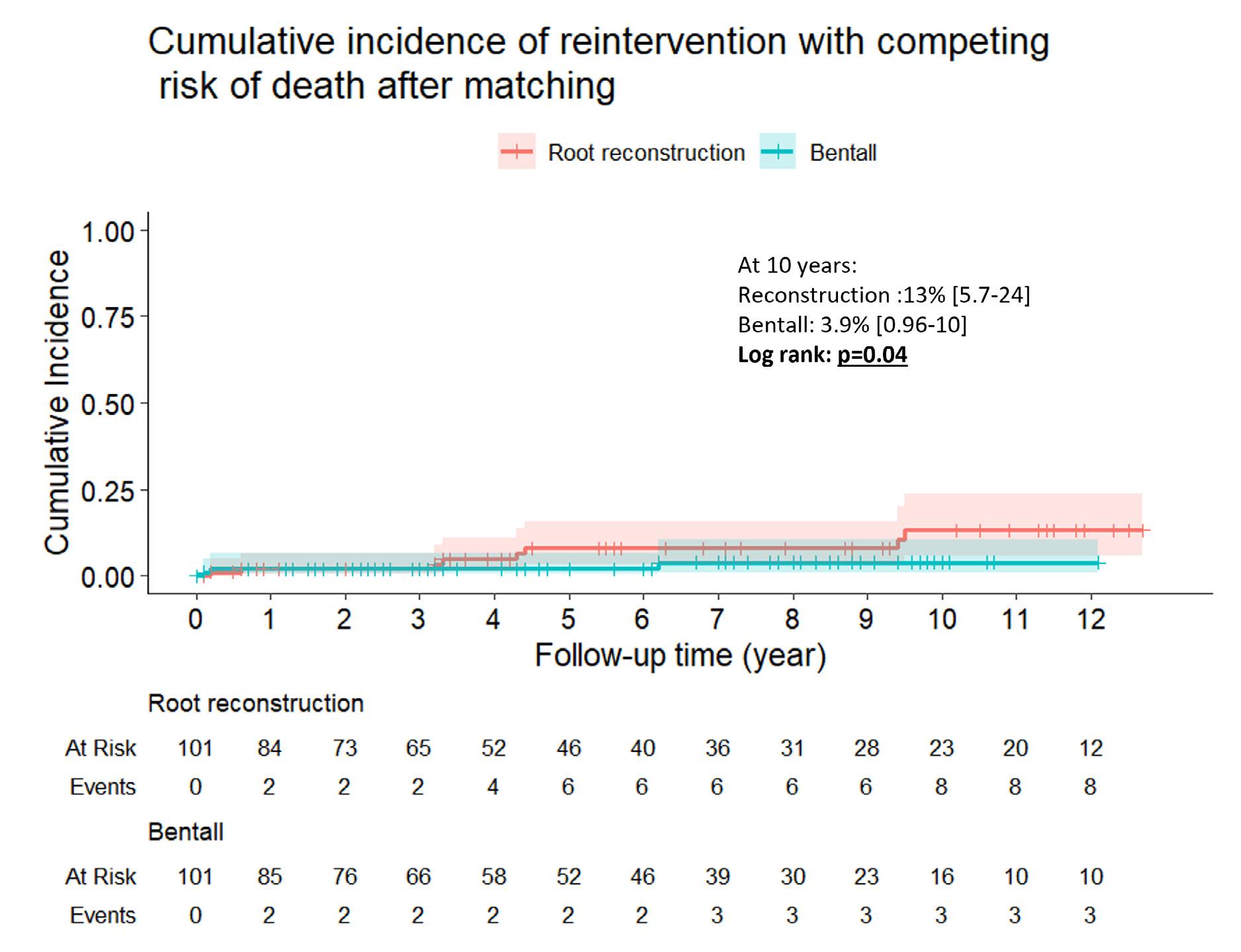
Uni- and multivariate Cox regression showed that a root diameter of >40mm was associated with a hazard ratio of 7.7 (95% confidence interval 2.623) and 5.4 (7-17) respectively, for reoperation for aneurysm and pseudoaneurysm.
The rate of reoperation due to proximal pseudoaneurysm and aneurysm could be significantly reduced with a lower threshold of 40mm to replace the aortic root in acute type A aortic dissection than in elective cases. So that the present diameter-based recommendation should be considered for upcoming guidelines of acute type A aortic dissection.
Q. Where did you carry out your training? University Hospital Bern, Switzerland
Q. What are your main areas of interest within cardiothoracic surgery? Aortic diseases and aortic valve, mainly the treatment of dissections and aneurysms of the aortic root.

Q. What are you most looking forward to at this year’s Annual Meeting?
Meeting my peers, discussing the new Aortic Guidelines. Vienna is a beautiful city, and the ACV is my favorite EACTS Venue. EACTS is really, for us surgeons that train and trained in Europe, the most important date on the agenda. It’s our Super Bowl!
Q. What are your interests outside of your work?
I play the piano, mainly late 19th and early 20th century composers and I graduated in 2012 with honors from Lausanne Institute of Music.
At this year’s Annual Meeting we are delighted to share the very best in late breaking science with three dedicated sessions taking place today and tomorrow.
Presentations, featuring the latest results and data from high impact studies, include:
• Insights from the CAST-HF trial: a potentially practice changing prospective randomised controlled trial exploring the impact of shockwave therapy at the time of CABG with patients with decreased systolic function.
• TITAN SvS trial - the first multi-centre randomised control trial comparing patients undergoing early elective ascending aortic surgery to those patients undergoing surveillance, looking at the feasibility of randomisation.
• A national database study featuring real world data on transcatheter versus surgical aortic valve replacement.
• FASTTRACK CABG - a trial investigating the feasibility of using computed tomographic angiography to refer patients for CABG. The primary outcome will be reported later this year, but this will be a great occasion for surgeons to hear from the investigators on the trial design, and how CT angiography can be used to plan CABG.
Innovation and technological advances are so important to cardiothoracic surgery, but we must be confident that new devices are safe and effective for patients. Thursday’s afternoon session ‘Breaking Science 3’ presents the latest data for two devices to treat the aortic arch – an endovascular approach with the nexus duo and a hybrid approach with a AMDS Hybrid Prosthesis. The two-year results from the REFORM-MR registry into a new device for mitral valve repair will also be presented during the afternoon session as well as the five-year clinical results of a new bioprosthetic valve using real world data from a multi-centre registry.
The Future of CABG
Friday’s ‘Breaking Science 2’ session includes a not to be missed update on the FASTTRACK CABG trial. We are privileged to be joined by Professor Serruys who will share examples of the functional imaging that can be produced by computed tomographic angiography and how it works in practice to support surgical planning.
Two major papers on hybrid management atrial fibrillation will also be presented which demonstrate the role of surgery in improving outcomes for patients with atrial fibrillation. Understanding the data is key for surgeons to help open discussions with electrophysiologists and support the greater involvement of surgeons in the treatment of atrial fibrillation.
Patrick Myers, EACTS Secretary General said, “Clinical trials are a critical part of our efforts to drive quality improvement in cardiothoracic surgery. It is encouraging that a growing number of surgeons are involved in major
trials and high-quality, impactful research, as demonstrated by the number of late breaking abstract submissions we received this year.
“The Late Breaking Science sessions feature some of the key trials in our specialty. It is important that we have an awareness of the latest data from these trials so we can understand how our practice is going to change in the coming years.”

“Clinical trials are a critical part of our efforts to drive quality improvement in cardiothoracic surgery. It is encouraging that a growing number of surgeons are involved in major trials and highquality, impactful research, as demonstrated by the number of late breaking abstract submissions we received this year.”
THURSDAY 5 OCTOBER
Late Breaking Science 1
10:00 - 11:00
Hall E2
Late Breaking Science 3
17:30 - 18:30
Hall E2
FRIDAY 6 OCTOBER
Late Breaking Science 2
13:45 - 14:45
Hall K1
Professor Hounkpatin / Beninese Minister for Health
We are delighted to welcome Professor Hounkpatin, Beninese Minister for Health, as our honoured guest speaker at this year’s Annual Meeting.
Join this special plenary session today for his talk ‘Building a Healthy future, a Spotlight on the Benin Republic’s Development’, which promises fascinating insights into the health challenges of Benin.
Professor Hounkpatin is an experienced doctor who has worked from north to south of Benin in various University Hospitals. He is a full professor of Obstetrics Gynecology at the African and Malagasy Council for Higher Education (CAMES).

Instrumental in many humanitarian projects, as well as the Health Ministry of Benin, Professor Hounkpatin has been deeply involved in the fight against obstetric fistulas, gynaecological and breast cancers, especially cervical cancer, and violence against women and girls.
Building a Healthy future, a Spotlight on the Benin Republic’s Development
Thursday 5 October 11.15am - 12.00pm
Hall D
Professor Hounkpatin has been deeply involved in the fight against obstetric fistulas, gynaecological and breast cancers, especially cervical cancer, and violence against women and girls.
Hall K1
10:00 - 11:00
Hyun Koo Kim / Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
Q. Where did you carry out your training? Korea University Guro Hospital, University College of Medicine.
Q. What are your main areas of interest within cardiothoracic surgery?
• Molecular image-guided surgery for thoracic oncology
• Minimally invasive video-assisted thoracoscopic surgery and robotic surgery
• Local chemotherapy for thoracic oncology
• Early detection of thoracic cancer with liquid biopsy.
Q. What are your interests outside of your work?
Cycling and working out.
Single-port robot-assisted thoracic surgery using the single-port robotic system: Preliminary experience
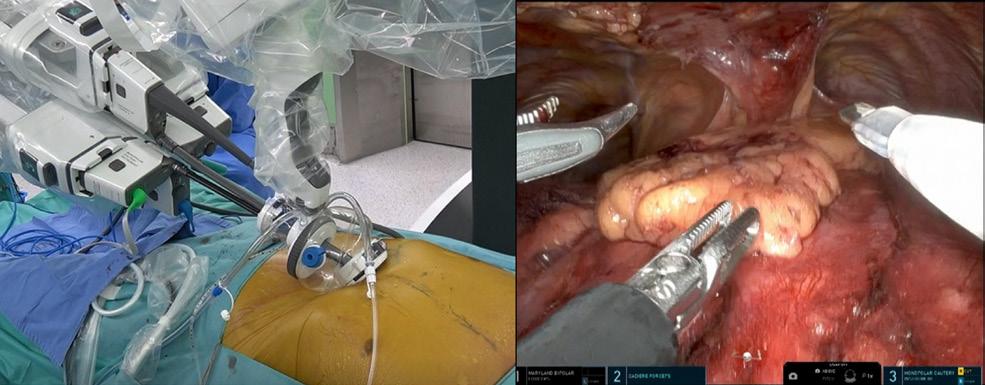
Jun Hee Lee, MD, Tae Hyun Park, MD, Hyun Koo Kim, MD, PhD Department of Thoracic and Cardiovascular Surgery, Korea University Guro Hospital, Korea University College of Medicine, Korea

Background: The da Vinci single-port system (SPS) was approved for thoracic surgery worldwide by the Korea Food and Drug Administration in August 2020. We presented our three years of experience with over 100 cases of single-port robotic-assisted thoracic surgery (SP RATS) using SPS and assessed its feasibility.
Methods: We initially performed SP RATS using SPS for simple procedures such as thymectomy and mediastinal mass excision and then progressed to relatively complex procedures such as major pulmonary resection and esophagectomy based on experience.
All procedures were performed using two extrathoracic approaches: the subcostal approach and subxiphoid approach, depending on the type of surgery. The subcostal approach is preferred for pulmonary resection, esophagectomy, enucleation of esophageal submucosal tumors (SMT), and excision of posterior mediastinal masses (Fig. 1). The subxiphoid approach is preferred for thymectomy and removal of anterior mediastinal masses (Fig. 2).
Results: The most common types of surgery were major pulmonary resection and thymectomy and
mediastinal mass excision, minor pulmonary resection, esophagectomy, and enucleation of the esophageal submucosal tumors.
The mean total operative time was around 130 minutes in thymectomy and 180 minutes in major pulmonary resection. No conversion to thoracotomy or sternotomy was performed in all cases. Conversion to video-assisted thoracic surgery was applied for one patient and an additional port was applied in two patients.
Conclusions: Single-port robot-assisted thoracic surgery using the da Vinci system is feasible and safe, and more complex thoracic surgeries could be performed using the da Vinci single-port system with the continuous advancement and innovation of instruments in robotic systems.
Hall K2
13:45 - 14:45
Q. Where did you carry out your training?
Hospital de Santa Cruz, Lisbon
Q. What are your main areas of interest within cardiothoracic surgery?
ICU, mitral valve disease, transplant, HOCM.
Q. What are you most looking forward to at this year’s Annual Meeting?
I look forward to learning about all the innovations and new surgical techniques in adult cardiac surgery.
Q. What are your interests outside of your work?
Music and volunteering with dogs.
Managing the mitral valve during surgery for HOCM

Mitral regurgitation (MR) in obstructive cardiomyopathy (oHCM) patients is mainly due to systolic anterior motion (SAM) of the mitral valve (MV). However, other mechanisms contributing to mitral regurgitation may coexist because of further structural abnormalities. SAM might occur because of the increased septal thickness alone or due to simultaneous MV or subvalvular apparatus anomalies, such as mitral leaflet elongation, papillary muscle body anomalies (hypertrophy, elongation, bifidity, and displacement), accessory papillary muscles or additional papillary muscle heads. Additionally, anomalous mitral chordae or the recently described mitral-aortic discontinuity (leading to a longer anterior mitral leaflet (AML)) can contribute to abnormal physiology. A closed aortomitral angle may also contribute. During intraoperative echocardiographic assessment, it is important to thoroughly evaluate the MV and the regurgitant jet to understand the mechanism(s) that cause MR in oHCM patients.
Although myectomy alone is frequently enough to correct SAM, concomitant MV procedures may be needed, especially when the septum is thin (<1618 mm) and/or there is intrinsic MV disease (see Figure 1). Detection of concomitant regurgitation mechanisms beyond SAM can eventually be identified preoperatively, either by direct structural detection (valve prolapse), by pharmacological palliation of SAM with vasopressors and negative inotropic agents or by identification of anteriorly and
centrally directed regurgitant mitral jets. Surgical techniques that can be employed to contribute to SAM elimination include plication/ extension/retention plasty of the AML, resection/ release/reorientation of papillary muscles, division of anomalous chordae, edge-to-edge repair, or, at times, prosthetic MV replacement. If there is structural MV disease concomitant to oHCM, appropriately tailored techniques to address the MV may be used.
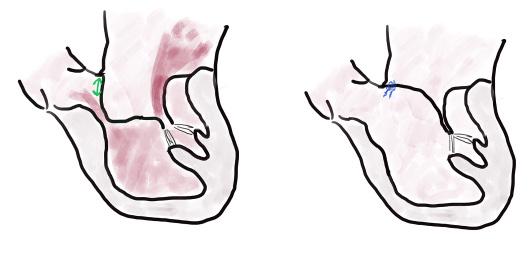
Transoesophageal echocardiography at the end of the procedure should demonstrate elimination of SAM, resolution of LVOT obstruction, and appropriate coaptation of the MV leaflets and nearly resolution of MR. Provocation with inotropes can be used to ensure no latent obstruction persists.
Thursday, 5 th October, 12:15 - 01:30pm, in Hall K1
Moderators: Dr. Moon (Edmonton, Canada), Mr De Silva (Cambridge, UK)
Speakers: Dr. Szeto (Philadelphia, USA)
Prof. Kempfert (Berlin, Germany) Dr. Luehr (Cologne, Germany) Mr Rajakaruna (Bristol, UK)
Staying alive: bridging strategies to long-term VAD
Room 0.31/0.32
15:00 - 16:00
Q. Where did you carry out your training? Japan and Australia.
Q. What are your main areas of interest within cardiothoracic surgery? Advanced Heart Failure.
Q. What are you most looking forward to at this year’s Annual Meeting? Getting in touch and sharing thoughts with colleagues and friends.
Q. What are your interests outside of your work? Wine appreciation.
Staying alive: Bridging strategies to long-term VAD
Room 0.31/0.32
15:00 - 16:00
International multi-center comparasion of various micro-axial flow pumps support as a bridge to permanent assist device implantation
In patients with advanced heart failure requiring a left ventricular assist device (LVAD), the progressive deterioration of cardiac function can adversely impact the success of surgical interventions. Preoperative implantation of micro-axial flow pump (mAFP) plays a crucial role in stabilising and preconditioning patients for a smooth transition to a durable mechanical circulatory support (dMCS). This study aims to assess effectiveness of different types of mAFP in achieving optimal left ventricular unloading, ensuring adequate preconditioning and definitive treatment for advanced heart failure patients.
A retrospective analysis utilised multicenter registry data from 19 European high-volume centers. The study examined 339 patients transitioning from different mAFP devices to dMCS between January 2015 and Juli 2022, with a median follow-up of one year.
These patients received preoperative support with an mAFP, transitioning to HeartWare HVAD (127), Heartmate 3 (204) or EXCOR VAD (7). Based on the type of mAFP used for bridging to dMCS, patients were categorised into two groups of mAFP depending the flow rate provided (up to 4L/min (92) or up to 5L/min (247) groups). Among them, (38)
Long-term outcomes of concomitant valve surgery during continuous-flow left ventricular assist device implantation
Whether coexisting valvular insufficiency should be treated during left ventricular assist device (LVAD) implantation remains controversial. This study evaluated the long-term benefit of concomitant valve surgery in LVAD patients.
All data were provided by the Japanese Registry for Mechanically Assisted Circulatory Support.
Between December 2010 and July 2022, a total of 1,398 continuous-flow LVAD recipients were retrospectively analysed using propensity score matching. Patients were divided into three groups according to the location of valve regurgitation (AR, MR, and TR), and outcomes (significant postoperative regurgitation, readmission, and survival) were compared with and without concomitant valve surgery.
After matching and excluding patients without pre-existing valve regurgitation, each group consisted of 159 patients with AR, 202 with MR, and 449 with TR. During a median followup of 3.1 years, concomitant surgery for AR demonstrated increased freedom from significant AR development (98.3% vs. 89.0% at three years; p = 0.002) and improved survival (87.9% vs. 79.0% at three years; p = 0.034). In patients with MR and TR, mortality and the risk of significant valvular insufficiency were comparable regardless of surgery. Readmission-free rates were similar with and without surgery for any valvular insufficiency,
but concomitant surgery for TR was associated with fewer readmissions overall. The study found that concomitant correction of AR during LVAD implantation may improve long-term survival by preventing AR progression. For MR and TR, concomitant surgery did not increase mortality, but the preventive effect of surgery against significant postoperative valvular insufficiency appears to be minimal with no apparent long-term survival benefit.
SVI, significant valve insufficiency (>moderate regurgitation or requiring valve surgery after implantation); AV, aortic valve; AR, aortic regurgitation; MV, mitral valve; MR, mitral regurgitation; TV, tricuspid valve; TR, tricuspid regurgitation;
Q. What are your main areas of interest within cardiothoracic surgery?
Marta Liliana Medina Estrada / University Medical Center of the Johannes Gutenberg University Mainz, Germany

Q. Where did you carry out your training?
I finished my medical studies at the University Pontificia Javeriana, Bogota, Colombia. I began my specialisation in cardiac surgery in Germany, at the University Hospital RTWH Aachen, then at University Hospital Bonn and I am currently at the University Medical Center of the Johannes Gutenberg University Mainz.
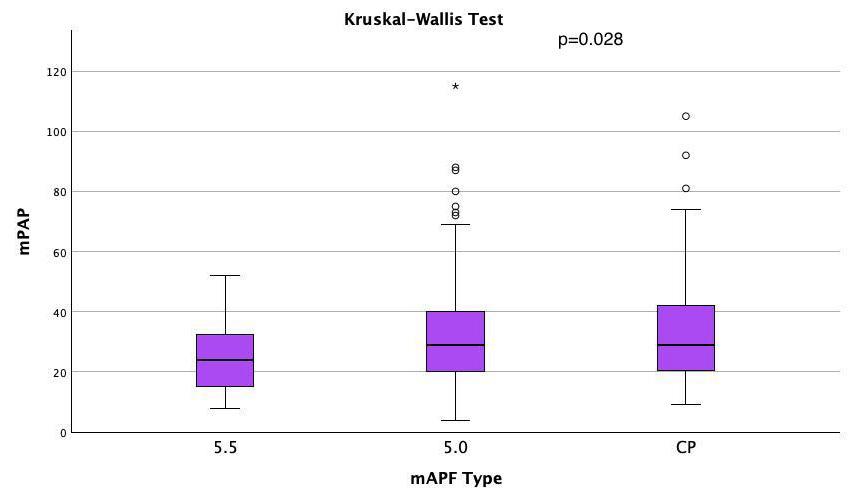
11.2% of the patients with 5+ support underwent a CP-device upgrade. 132 (40.5%) additionally required extracorporeal life support before/during mAFP therapy. mAFP-5+ significantly reduced VIS (vasoactive inotropic score) and IS (inotropic score) compared to CP group with p-values of 0.006 and 0.008, respectively. mPAP was significantly lower in the 5.5 group than in the CP or 5.0 group. RVAD Implantation was lower in the 5+ group than in the CP group (p=0.026).
mAFP which offered a support up to 5.0L/min performed a superior hemodynamic support with lower catecholamine requirement and better unloading compared to other mAFP devices with lower RVAD implantations. Additionally, a lower rate of renal and hepatic failure was observed after left ventricular assist device (LVAD) implantation.
Heart failure, coronary artery bypass graft (CABG) surgery off-pump, and mechanical circulatory support.
Q. What are you most looking forward to at this year’s Annual Meeting?
I am looking forward to being updated on new therapeutic options in the field of cardiac surgery as well as to be informed on the strategies supported by evidence-based medicine.
Q. What are your interests outside of your work?
I like to swim and ride a racing bike. I am a duathlete. I like electronic music and I am a DJ.
However, no statistically significant association was found between the types of mAFP used as a bridge to LVAD and 30-day mortality rate.
Hall G2
15:00 - 16:00
David Santer / University Hospital Basel, SwitzerlandQ. Where did you carry out your training?
I was trained at the Department for Cardiovascular Surgery in Hospital Hietzing, Vienna, Austria by Professor Martin Grabenwöger (former EACTS president). In 2017 Martin supported me to apply for the EACTS Francis Fontan Fellowship for Ablation, which I am very thankful for.
Q. What are your main areas of interest within cardiothoracic surgery?
Next to general adult cardiac surgery, my main areas of interest are surgical ablation, heart failure therapy and aortic surgery.
Q. What are you most looking forward to at this year’s Annual Meeting?
Firstly, I am excited to be a new member in the Arrhythmia Task Force and thankful to be actively involved in the arrhythmia sessions. Secondly, as the Annual Meeting 2023 takes place in Vienna, it feels like coming home for me and I am really looking forward to meeting former colleagues, collaborators and friends.

Q. What are your interests outside of your work?
My wife Lena and I love to travel, brunch and binge-watch. On 3 July 2023 our wonderful daughter Aurelia was born, and she turned our world upside down. She is our greatest gift and changed everything. What was the question again?
Preoperative non-invasive mapping for the development of a surgical ablation strategy
Background: Non-invasive mapping (CardioInsight TM , Medtronic Inc.) allows preoperative visualisation of rotors and foci in patients with nonparoxysmal atrial fibrillation.
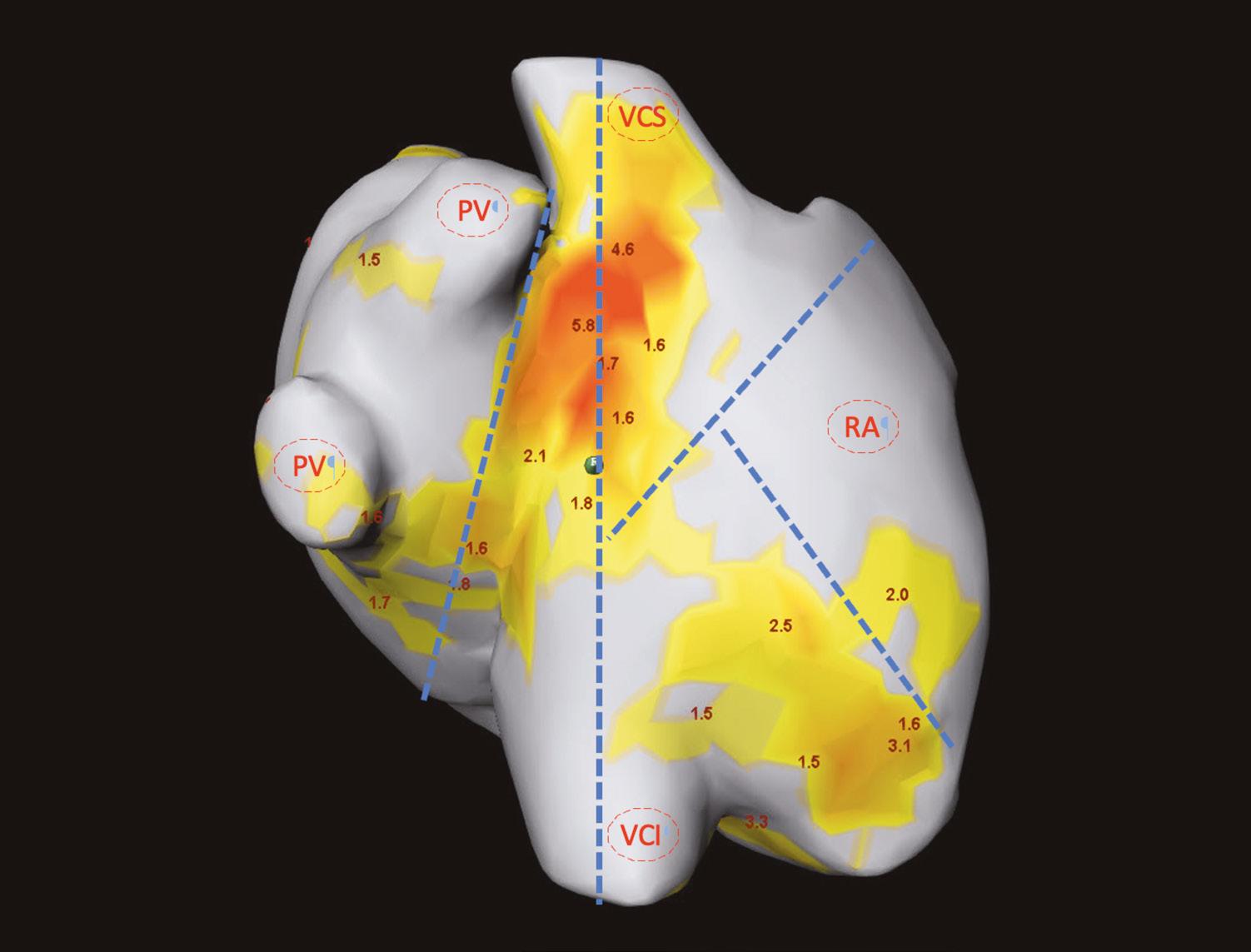
In this pilot study, we hypothesised that preoperative non-invasive mapping would affect the concomitant ablation strategy and, consecutively, increase the rate of sinus rhythm at hospital discharge after cardiac surgery.
Methods: Between 2020 and 2023, 13 patients with non-paroxysmal atrial fibrillation scheduled for cardiac surgery underwent preoperative noninvasive mapping in our outpatient clinic (PREMAP cohort).
Mapping consisted of recording body surface potentials with a mapping vest and a low-dose CT scan of the chest. Concomitant ablation was then performed according to the mapping report (Fig. 1). To investigate the association of preoperative mapping and the rhythm at hospital discharge, we pooled our PREMAP with patients having non-paroxysmal atrial fibrillation (n=33) who underwent surgical ablation according to the surgeon's preference, and calculated an odds ratio with 95% confidence interval.
“Mapping consisted of recording body surface potentials with a mapping vest and a low-dose CT scan of the chest. Concomitant ablation was then performed according to the mapping report.”
Results: Most patients underwent combined or isolated valve procedures (PREMAP vs. control: 92 vs. 81%). While the aortic crossclamp time was comparable (PREMAP vs. control: 103 vs. 102min; p=0.18), the duration of surgery was longer in the PREMAP group (285 vs. 230min; p=0.05).
Bi-atrial ablation was performed more often in PREMAP patients (54 vs. 27%). More PREMAP patients were discharged with sinus rhythm (62 vs. 55%). Preoperative mapping did not show an association with the rate of sinus rhythm at discharge (OR 0.75 [0.20 to 2.78]; p=0.67).
Conclusion: Preoperative non-invasive mapping is an intriguing tool for the preoperative development of a surgical ablation strategy. However, although mapping had an effect on the ablation strategy, we did not observe a relevant effect on the rate of sinus rhythm at hospital discharge in this small cohort.
Dr. Bart van Putte recently gave a Live-in-a-Box presentation at EACTS’s Techno-College introducing The Elana® Heart Bypass System: a new clip & laser technology that will enable less invasive and more consistent CABG surgery. If you missed this presentation, simply visit the video library in our Elana Academy: a training & education center aimed at helping surgeons explore and ultimately adopt next generation technology.
For many decades, the surgical community and its patients have dreamed of more standardized and less invasive bypass surgery. Now at AMT Medical, we are working to make it a reality.
Scan to see the Elana Heart Bypass System in action. Or, if you want to know more about this technology, simply contact us today. T: +31 85 105 7070 E: info@amt-medical.nl


Our premium TV channel makes a welcome return this year, with live broadcasts, one-to-one interviews and punditry from our expert panellists and key opinion leaders. Join us at the EACTS TV studio located in Exhibition Hall X1 and take part in live discussions on some of the day’s key topics.

VIEW THE TV SCHEDULE BELOW. IF YOU'RE NOT ABLE TO VIEW THESE IN-PERSON, YOU CAN WATCH THEM VIA THE EACTS APP.
10:00 - 10:30 The Daily Preview: Today at the Annual Meeting
10:30 - 10:40 Yesterday at the Annual Meeting
10:40 - 11:15 Let's Talk Innovation
TIME PROGRAMME PANELLISTS
09:45 - 10:00 On The Pulse: Exploring the Exhibition
10:00 - 10:30
F. Casselman, Aalst, M. Eid, Angers, M. Milojevic, Beograd
The Daily Preview: Today at the Annual Meeting
10:30 - 10:40 Yesterday at the Annual Meeting
10:40 - 11:15
11:15 - 12:00 Live Broadcast: Honoured Guest Keynote Address
12:45 - 13:00
Do we need nurses in surgery?
13:00 - 13:15 In Focus With... Franca Melfi
13:15 - 14:00 Beyond Boundaries: Innovations in Cardiothoracic Surgery for LMICs
14:00 - 14:15 In Focus With... Jose-Luis Pomar
14:15 - 14:45 Aiming for Success with EBCTS
14:45 - 15:00 In Focus With... Gebrine El Khoury
16:00 - 16:30
F. Beyersdorf, Freiburg, V. Falk, Berlin, C. Gollmann-Tepeköylü, Innsbruck, F. Melfi, Pisa
Robotic cardiac and thoracic surgery: more through less
11:15 - 12:00 Live Broadcast: Presidential Address
12:15 - 13:00 CT Surgery Resident Showdown: Live European Final!
In Focus With... Teresa Keiser
C. Ruiz-Segria, Middlesbrough, K. Freystaetter, Middlesbrough, J. L. Pomar, Barcelona
P. Zilla, Cape Town, D. Vervoort, Toronto, C. Yankah, Berlin
13:00 - 13:10
13:10 - 13:30
14:30 - 15:00
15:00 - 16:00
16:00 - 16:30
R. de Paulis, Roma, F. Doerr, Essen, J. Hörer, Munich
W. Oosterlinck, Leuven, H. Balkhy, Chicago, M. Durand, Neuilly-sur-Seine
S. Clark, Newcastle Upon Tyne, E. Quintana, Barcelona
Science Friction - The Daily Review M. Borger, Leipzig, J. Grau, Ridgewood M. Sousa Uva, Lisbon
16:30 - 16:45 On The Pulse: Exploring the Exhibition
Residents - Collaboration for transformation
From night fight heroes to routine standardized heart failure surgery
Live Broadcast: Watch and learn - Aortic Valve Repair techniques
Science Friction - The Daily Review
16:30 - 16:45 On The Pulse: Exploring the Exhibition
N. Hussein, Cottingham, M. Eid, Angers F. Nägele, Innsbruck
E. Potapov, Berlin, J. Gummert, Bad Oeynhausen, I. Netuka, Prague
A. Zientara, Freiburg, J. Kempfert, Berlin, M. Milojevic, Beograd
TIME PROGRAMME PANELLISTS
09:45 - 10:15
10:15 - 10:20
The Daily Preview: Today at the Annual Meeting J. Bax, Leiden University Medical Center, R. Sádaba, Pamplona S. Sandner, Wien
Women in Cardio-Thoracic Surgery
10:20 - 10:30 Yesterday at the Annual Meeting
10:30 - 12:00
12:30 - 12:45
Live Broadcast: Trials Update
Live Broadcast: the 2023 EACTS Awards
to catch these fantastic sessions
Gain an insight into some of the most influential figures in cardiothoracic surgery as they share their career highlights and discuss some of the most important developments in cardiothoracic surgery.






13:00 - 13:15
14:00 - 14:15
Learn more about EACTS’s commitment to fostering a culture of discovery and development to bring forward the very best technologies and techniques for the benefit of patients.
A review of the day’s programme, including key talks, takeaways, debates and anecdotes...and much more!
16:00 - 16:30
Franca Melfi
Jose-Luis Pomar
14:45 - 15:00 Gebrine El Khoury
10:40 - 11:15
This compelling session explores transformational leadership in disruptive times and the impact of belonging in high performance.
MEETING: 10:00 - 11:00
HALL K2
NETWORKING COFFEE: 09:30 - 10:00
Foyer K2
Don’t miss the great opportunity to learn specialist techniques from the world’s most experienced and expert surgeons and gain ‘hands-on’ experience using the latest devices. EACTS Learning Lab, including both wet and dry labs, are available to book now.

THURSDAY 5 OCTOBER
AV Repair – Valve Sparing Aortic Root Surgery: The Reimplantation Technique
Learn the pitfalls of the Reimplantation Technique on a model, ask questions and get advice from our experienced faculty.
AV Repair – Annuloplasty with remodelling valve sparing root replacement and isolated aortic valve repair
Dry Lab Training (Mitral)
Transcatheter
Train with the latest transcatheter devices for aortic and mitral valve procedures and develop your skills and improve your knowledge in catheter treatment of valvular disease. This is an opportunity to practice on simulators while interacting with our expert faculty and industry proctors.
FRIDAY 6 OCTOBER
Mitral Valve
Basic training on mitral and tricuspid valve access, repair and replacement
– 14:15
– 14:15
–
– 17:00
–
–
–
Coronary Masterclass
Learn how to perform coronary anastomoses and manage different types of graft configurations and find out more about techniques for proximal and distal anastomosis, sequentials, elongation and composite grafts.
Join discussions about the use of devices for conduits harvesting and graft assessment.
SATURDAY 7 OCTOBER
Congenital – Surgical Management of complex left ventricular outflow tract obstruction Understand indications and surgical techniques for ventriculo-aorto-plasty.
– 17:00
– 17:00 Endoscopic Dry Lab Training (Mitral)
–
EXHIBITION OPENING TIMES:
Thursday 5 October 09:00 - 18:30, Welcome Reception 17:00 - 18:30
Friday 6 October 09:00 - 17:00
Saturday 7 October 09:00 - 12:00
A record number of high-quality abstract presentations were submitted for consideration at this year’s Annual Meeting. The standard of submissions was very high so, in addition to those abstracts included in the scientific programme, we are delighted to present a selection of abstracts in poster format, giving you access to even more scientific insights and research.
All e-posters will be available to view during the Annual Meeting at the different e-poster terminals in Exhibition Hall X1.
The following e-posters will be presented during moderated sessions today between 09:30-10:00 with the e-poster authors for presentation and discussion.
09:30
Effect of Hemoadsorption during Cardiac Surgery for S. aureus Endocarditis - A REMOVE Trial Post-hoc Analysis
H. Kirov, Jena, T. Caldonazo, Jena, T. Doenst, Jena, G. Färber, Jena, M. Franz, Jena, T. Lehmann, Jena, M. Diab, Jena
09:36
Post-Cardiotomy Extracorporeal Life Support Cannulation in the Normal Ward? Results of the PELS-1 Observational Multicenter Study
G. Bari, Maastricht, S. Mariani, Maastricht, M. S. Matteucci, Torrette, Ancona, S. Sponga, Udine, G. Maclaren, Singapore, C. F. Russo, Milan, F. Formica, Parma, R. Lorusso, Maastricht
09:42
Del Nido versus crystalloid HTK cardioplegia in adult aortic valve replacement – early clinical outcomes from randomized trial
B. Brzeska, Gdańsk, M. Frańczak, Gdańsk, A. ŁOś, Gdańsk, P. Zelechowski, Gdańsk, N. Ulatowski, Gdańsk, W. Karolak, Gdańsk, R. Smoleński, Gdańsk, R. Pawlaczyk, Gdańsk
09:48
Early chest tube removal protocol on the first postoperative day of an enhanced recovery after cardiac surgery programme is safe
M. Kindo, Strasbourg, M. Darras, Strasbourg, C. Schneider, Strasbourg, S. Marguerite, Strasbourg, W. Oulehri, Strasbourg, P.-M. Mertes, Strasbourg, O. Collange, Strasbourg, J.-P. Mazzucotelli, Strasbourg
09:54
Influence of preoperative risk factors and causative pathogen on outcome after surgery for aortic versus mitral valve endocarditis – a multicenter analysis
C. Weber, Cologne, M. Diab, Jena, S. Saha, Munich, M. Borger, Leipzig, S.-M. Tugtekin, Dresden, A. Lichtenberg, Düsseldorf, T. Wahlers, Cologne, M. Luehr, Cologne
09:30
Clinical outcomes of reimplantation versus remodelling valve-sparing aortic root replacement in patients with connective tissue disorders: A meta-analysis
S. Burton, Plymouth, A. Reynolds, Swansea, A. Modi, Southampton, S. Asopa, Plymouth
09:36
Outcomes of the V-shaped noncoronary sinus remodeling technique for ascending aortic aneurysm and aortic root ectasia
J. Velasco, New Haven, H. Ellauzi, New Haven, M. Zafar,, New Haven, B. Ziganshin, New Haven, J. Elefteriades, New Haven
09:42
Half a Century of Experience with Bentall Procedure: Analysis of 2001 Consecutive Cases
G. Murana, Bologna, G. Gliozzi, Bologna, L. Di Marco, Bologna, C. Fiaschini, Bologna, M. Di Carlo, Bologna, F. Brandini, Bologna, G. Folesani, Bologna, D. Pacini, Bologna
09:48
Minimally Invasive Replacement of Aortic Root, Ascending Aorta and Hemiarch via Partial Upper Sternotomy: A Propensity-Score Matched Comparison with Full Sternotomy
N. Papadopoulos, Zurich, V. Ntinopoulos, Zurich, P. Risteski, Zürich, A. Haeussler, Zürich, D. Odavic, Zurich, L. Rings, Zurich, H. Rodriguez Cetina Biefer, Zürich, O. Dzemali, Zürich
09:54
Prospective, observational study to evaluate the outcomes of cytokine hemadsorption during aortic surgery: Preliminary Results
Y. Mehta, Gurugram, A. Singh, Gurugram, M. Singh, Gurugram, A. Bhan, Gurugram, N. Trehan, Gurugram
09:30
Circulating microbial analyses suggest a novel biomarker for early diagnosis of lung cancer
C. Haiming, Beijing, L. Yiming, Beijing, Q. Mantang, Beijing
09:36
NSCLC patients with skip-N2 metastases have similar survival to N1 patients, a multicenter analysis
G. Schlachtenberger, Cologne, S. Schallenberg, Berlin, R. Buettner, Köln, A. Quaas, Cologne, C. Grathwohl, Cologne, K. Hekmat, Cologne, T. Wahlers, Cologne, M. Heldwein, Cologne
09:42
Primary lung cancer in children and adolescents
Q. Chen, Hangzhou
09:48
Camrelizumab in combination with chemotherapy versus concurrent chemoradiotherapy for the conversion of locally advanced unresectable esophageal squamous carcinoma: a phase II, prospective, two-arm randomized, uncontrolled clinical study
M. Chen, Fuzhou, Z. Bin, Fuzhou, H. Yizhou, Fuzhou, L. Wei, Fuzhou, Z. Chunyu, Fuzhou, C. Chun, Fuzhou
09:54
Three-dimensional modelling in preoperative planning, quality control and monitoring after a complex tracheo-broncho-angioplasty for a centrally located lung cancer
S. Yeskov, Liasny, S. Krasny, Liasny
09:30
Impact of bilateral pulmonary artery banding on pulmonary artery growth in 104 patients with hypoplastic left heart syndrome
L. Tomkova, Bonn, B. Asfour, Bonn, B. Bierbach, Bonn, E. Schindler, Bonn, N. Mini, Bonn, M. Vergnat, Bonn, C. Staerk, Bonn, L. Duebener, Bonn
09:36
Unraveling the recovery potential of the heart: a novel translational model of pulmonary artery banding-rescue of left ventricular failure
M. Ponzoni, Toronto, A. Yeganeh, Toronto, J. Zhang, Toronto, R. Vanama, Toronto, L. Zhang, Toronto, J. Li, Toronto, J. Maynes, Toronto, J. Coles, Toronto
09:42
Outcome of Slide Tracheoplasty for Long segment congenital tracheal stenosis in Infants less than or equal to 3 Kgs
A. Beeman, London, R. Madhavan, London, B. Wang, Cambridge, C. Ng, London, M. Broadhead, London, S. Chippington, London, R. Hewitt, London, N. Muthialu, Gerrards Cross
09:48
Redo-Open Repair of Coarctation of the Aorta-A 48-year Experience in Australia
C. Tan, Sydney, A. Zhu, Westmead, L. Huang, Westmead, C. Dickson, Westmead, R. Chard, Westmead
09:54
Left Atrial Strain to Predict Myocardial Recovery in Children with Dilated Cardiomyopathy on Berlin Heart EXCOR
M. Hasegawa, Suita, M. Taira, Suita, T. Watanabe, Suita, Y. Kugo,, Suita, T. Nagashima, Suita, T. Ueno, Suita, S. Miyagawa, Suita
36 % of chest tubes occlude after cardiac surgery1
86 % of these occlusions occur inside the patient and are not visible to doctors and nursing staff1
How can we address this hidden danger?
and learn more about it
Satellite symposia, organised by some of our industry partners, are an opportunity to learn more about new-to-market technology, state-of-the-art products, innovations and developments in the cardiothoracic market. These sponsored programmes do not form part of the official scientific programme of EACTS.
Hall K1
Hall K2
Hall G1
Acute Aortic Dissections: the role of the AMDS Therapy in preventing DANE and resolving Malperfusion
Heart Failure & Atrial Fibrillation – an underestimated lethal relationship
Infections in cardio and thoracic surgeries: Trick or Treat?
Hall E1 RESILIA tissue: what does it take to become a new standard?

12:15-13:30
12:15-13:30
Hall F1
Hall G2
Discovery fire session: Experts guide to managing complex SAVR cases

Multi-country clinical experience on Novel Coaxial Drain in Cardio-Thoracic Use
Room 0.14 Living as a part of you – different tissue restoration in cardiovascular surgery
Room 0.31-0.32
Controversies in Sternal Closure


Hall K1
More than a buzzword: Patient lifetime management

Hall G1 New product innovations in pMCS and first experiences with new therapy solutions
Hall K2
Hall E1
Hall F1
Hall G2
Room 0.31-0.32
Hemoadsorption with CytoSorb after 10 years – Where do we stand?

Mitral valve replacement: current perspective
Discovery fire session: New frontiers for Mitral valve treatment

Segmentectomy with 3D Reconstruction
Empowering limitless Hybrid Solutions





Explore new technologies and gain skills in new techniques at this year’s industry learning labs which are hosted by our industry partners. Visit their booths in the Exhibition Hall to find out more.
Discover the latest innovative simulator for AF ablation and LAA management at the AtriCure learning lab located in Exhibition Hall X2 – Lab 7. Our Learning Lab training sessions on open concomitant and minimally invasive therapies are not to miss for all cardiothoracic surgeons and EPs looking to expand their AF practice. These sessions offer the opportunity to:
• Improve your understanding of Open Concomitant Surgical Ablation, Hybrid AF™ Therapies and LAA Exclusion
• Explore different techniques and approaches concomitant surgical ablation about the Maze IV lesion set
• Gain skills and hands-on experience to perform Hybrid AF™ Therapies in complex AF cases
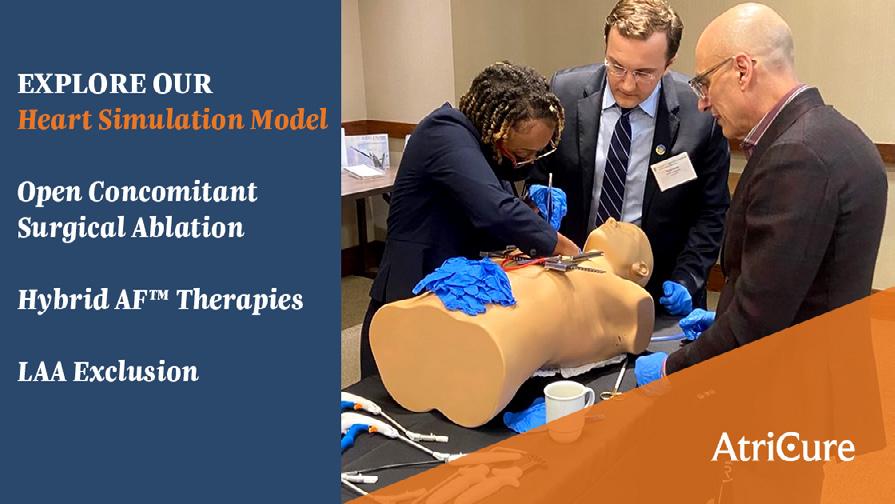

• Learn the main steps for endoscopic LAA exclusion with AtriClip® devices
To book a session at the AtriCure Learning Lab, visit our team at booth 13.

The Artivion learning lab, located in Exhibition Hall X2, has a number of practical courses led by distinguished proctors in their fields.
• On-X Open Mitral valve implantation into pig hearts with a focus on the unique design Conform-X sewing ring.
• On-X Mitral valve Minimal Invasive Implantation into a newly designed simulator with camera, MIC instruments and screen.
• Frozen Elephant Trunk implantation with the E-vita Open Neo into a full size HumanX torso, guiding with and without guide wires.
• AMDS – the new adjunct for Debakey type I dissection, whenever an ascending aortic replacement or hemiarch is planned. This course will show the stabilising of the membrane with implantation into a “see through aorta” and discuss short-, mid- and longer term results.
• On-X Aortic and mitral valve replacement into pig heart with consideration of the design specifics of the On-X aortic valve, such as the flared inlet, profile height versus implant height and the superior leaflet design, opening 90°.


The Medtronic Learning Lab, located near the Medtronic booth 002, includes three days of educational sessions on all the cardiac surgery therapies and TAVI through the use of wetlabs, drylabs and innovative simulators.

• Day 1 (Thursday 5th October) is a focus on Minimally invasive cardiac surgery therapies, simulations and aortic annulus enlargement techniques while also providing sessions on TAVI simulation.
• Day 2 (Friday 6th October) includes sessions on MICS, atrial fibrillation surgical treatment with different approaches and TAVI simulation.
• Day 3 (Saturday 7th October) is an opportunity to practice various MICS techniques in an open simulation session, dive deeper into MICS CABG and TAVI simulation.

Join fellow Residents for a relaxed lunch and share common interests and discuss key issues.
Thursday 5 October 12:15
*No clinical data are available that evaluate the long-term impact of RESILIA tissue in patients. Additional clinical data for up to 10 years of follow-up are being collected to monitor the long-term safety and performance of RESILIA tissue.
† RESILIA tissue tested against tissue from commercially-available bovine pericardial valves from Edwards in a juvenile sheep model. Flameng, et al. J Thorac Cardiovasc Surg 2015;149:340-5.
Medical device for professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards, Edwards Lifesciences, the stylized E logo, INSPIRIS, INSPIRIS RESILIA, and RESILIA are trademarks of Edwards Lifesciences Corporation or its a liates. All other trademarks are the property of their respective owners.
© 2023 Edwards Lifesciences Corporation. All rights reserved. PP--EU-6815 v1.0
Edwards Lifesciences
• Route de l’Etraz 70, 1260 Nyon, Switzerland
• edwards.com

RESILIA tissue* o ers enhanced anti-calcification technology that will potentially allow the valve to last longer than conventional bioprosthetic valves†