Duffy Doings














Change Celebrating changemakers in our midst.
RESTORING HEALTH, REBUILDING LIVES FALL 2022 Agents of
Top Left to Bottom Right: Amber Rogovich, Lead MA; Danny Rodrigues, LICSW, PMH-C, Director of Substance Use Disorder Services; Denies Smith-Grant, Medical Community Health Worker; Dr. Deborah Field, Psychiatrist; Jessica Chambers, Connections Case Manager; Eryn Tomascik, Behvioral Health Care Coordinator; Christine Johnson-Staub, Board Member; Edgard Carvalho, Behavioral Health Care Coordinator; Jackie Chasey, Moms Do Care Recovery Coach; Sara Seely, Patient Access Manager; Bonnie Adkins, Connections Case Manager; Jennifer Carroll, RN, Lead Medication Assisted Treatment Nurse; Taylor Griffin, Connections Case Manager; Susan Childs, Community Health Worker
Looking Forward: A note from Heidi Nelson, CEO
Caring for the Spirit: Providing connection to our patients

Employee Wellness: Intentional, trauma-informed wellness initiatives for staff
Community Health Workers: Care based on trust and shared experiences
Reading with Purpose: Exploring diversity, equity, and inclusion
Agents of Change: Celebrating changemakers in our midst
25 Years of Trust & Impact: What our patients are saying
Connections to Care: Assisting patients in accessing the care they deserve
Partnering for Change: Strategically identifying barriers to care
Good News Stories: Vignettes that remind us of our impact
Community Engagement: Gathering in support of Duffy’s mission
National Recovery Month: Celebrating recovery while honoring lives lost too soon
Ways to Support Duffy
2 Duffy Doings
Inside Page 3 4 5 6 7 8 - 11 12 13 14 15 16 - 17 18 19
What’s
Looking Forward
A note from Heidi Nelson, CEO
At a recent staff retreat, we spent quality time together - in person - for the first time since October 2019. The room was double in size to accommodate our now-93 person team. While it was exhilirating to be there together, the opportunity to speak in person necessitated an acknowledgment of how challenging the past few years have been. It’s been emotionally, physically, and mentally draining not only to get through the pandemic, but to deal with its aftermath on so many fronts, both personal and professional.

Nevertheless, it always brings me joy to share time with our team; to have the opportunity to level-set, to sit sideby-side and discuss issues faced by our patients, and to break bread and share lighthearted moments. Throughout this year - our 25th anniversary - we’ve spent time both looking back on our Duffy history and looking forward toward the future of Duffy Health Center. Our team went through the “looking forward” exercise together, and as always, I was inspired by their vision.
Health care in Massachusetts is going through a radical change. At the beginning of 2023, the state will implement value-based payment, a model that incentivizes the quality of the care we provide over the number of visits we complete. Lucky for Duffy Health Center - and community health centers in general - our integrated model is built for this type of care. The rest of the world is just catching up to us!
Kidding aside, our team truly understands the value of providing high-quality, holistic care where the individual patient is at the center of the care team that surrounds them. I know this because I heard them talking about it in our retreat when we asked them to reflect on physical space changes we will be making to facilitate care.
“Our patients will know the members of their care team even better than they do now and build deeper trust,” they said.
“The new model will allow our patients to better understand all that Duffy offers and make it easier for them to access the services they need.”
“We’ll learn from each other and it will be easier to communicate if we’re sitting closer to teammates from other disciplines,” I heard them reflect, with a hint of excitement myself.
Duffy Health Center was founded 25 years ago in response to unmet needs in our community. A handful of people - our founders - had the courage to identify, talk about, and face these challenges head-on. Although our staff has grown, our services have broadened and deepened, and our budget is larger, the heart of our mission remains the same. We are here to provide the best care we possibly can to the individuals who need it most and who far too often go without.
Thank you for believing in our work. It wouldn’t be possible without you.
Be well, Heidi R. Nelson, FACHE CEO, Duffy
Duffy Doings 3
Health Center
Kathleen Bresette, President
Susan Harrington, Vice President
John Murphy, Treasurer
Paulette Shaw Querner, Clerk
James J. Cullen
Miguel R. DaSilva
Jeffrey Haddad
Christine Johnson-Staub
Chester H. Mohr, MD
Stuart Murphy Vanessa Proc
Kurt E. Raber
Mary Rahal Olympia Ramos
Peter Scarafile
Richard N. Smillie
Corrie Vilsaint, Ph.D.
Honorary Members: Dr. Hub Mathewson Dr. Neil Ringler Andrew Singer, Esq.
Duffy Health Center Board of Directors
Caring for the Spirit
Providing connection to our patients
Over five years ago, a local woman named Pamela Wannie was introduced to Duffy Health Center. She had just graduated with a Masters in Divinity from Andover Newton/Yale and was interning for a Clinical Pastoral Education class required for ordination. What began as an internship in May 2017 has grown into a full-time position as Duffy’s Spiritual Care Provider, through which Pam oversees both our suicide prevention program and our Waiting Room concierge volunteers.

In speaking with Pam, one of the first things she’ll clarify is that spirituality is not religion. As she puts it, “I’m not here to convert anybody or tell anybody about my belief system. My belief system is what informs the work I do, it’s the reason why I do this work.”
Spirituality, as Pam defines it, “is the thing that’s beyond our name, or job, or personality. It’s the thing that’s beyond our current circumstances that makes us who we are, and we all express it in different ways. I often describe it as the way that we connect to ourselves, to other people, to something larger than our individual human experience.”
At Duffy, the spiritual care Pam provides is traumainformed, person-centered care for the human spirit, however a person defines “spirit” and “spirituality” for themselves. This includes how a person understands and experiences meaning, purpose, connection, and direction in their lives.
In her role, Pam facilitates dialogue about what gives patients and clients hope, meaning and purpose, and supports them in incorporating this into their current circumstances, situations, or suffering. These conversations
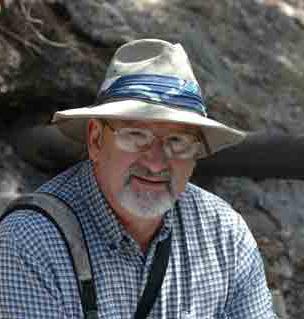
Upon retirement, Chris Ranney began volunteering in several capacities on Cape Cod. Through a confluence of factors, during the COVID pandemic he found himself making 25 breakfast sandwiches twice a week for Duffy’s community breakfast program.
Chris also volunteers at the Faith Family Kitchen once a month, a dinner program for those who need a warm meal. When he was approached about volunteering in Duffy’s waiting room it seemed like an extension of much
can help people to make meaning, develop deeper connection to self, hold a place of peace for questions that cannot be answered, and model compassion and acceptance for who and where each person is in this point in their lives.
“In talking with individuals, it’s all about connection,” says Pam. “The thing expressed most frequently and most desperately by those in our care is loneliness. There is huge value in the opportunity to connect with people right where they are in that moment and treat them with dignity and respect.”
This observation is part of what led to the establishment of the volunteer Waiting Room Concierge program. Anyone on the Duffy team will tell you that our patients just want someone to listen; to feel seen and heard. Giving them the opportunity to speak with someone who provides a compassionate presence while they wait for their appointments often helps our patients to settle enough and feel grounded enough to enter into their appointment in a mindful manner, rather than being scattered and overwhelmed as they meet their provider.
With this in mind, Pam reached out to our partners at the Cape Cod Council of Churches to see if anyone may be interested in fulfilling this role in a volunteer capacity at Duffy. That is how Chris Ranney and Doug Rodrigues became involved.
of the volunteer work he had already been doing.
“Some people have started recognizing me - they see me at the Faith Family Kitchen and at Duffy,” shares Chris. “I hope when they see me, they see a presence that’s non-judgmental, someone who’s a friend to be there if they need it. I hope they see someone who is safe to be around, someone who cares and is willing to listen.”
Chris says that he feels comfortable at Duffy; he sees the way our front desk team works with our patients and knows how much they care. “ They are so in-tune with what’s going on. They know everyone who comes in. That role is so important. My hope is to support them, and to make patients feel seen, recognized, acknowledged, because too often they don’t feel that way.”
4 Duffy Doings
Chris Ranney
Pamela Wannie
“Spiritual care is one of the most important aspects of our well-being, but it’s often the most overlooked,” says Doug Rodrigues, a former campus minister.
Doug began volunteering as a Waiting Room Concierge at Duffy in July 2022, driven by his desire to be of service to others. Having experienced some health issues and in recovery himself, he feels that he can offer his compassion to our patients in the waiting room just by listening.

“I’ve been impressed by the level of care at Duffy,” he says. “As I sit in the waiting room, I watch the staff walk in the door ready to hit the ground running each day.”
In his role, Doug’s main objectives are to offer hospitality as patients enter Duffy; to be a calming presence in the Waiting Room; and to assist with de-escalating individuals who may be upset, just by letting them talk.
“A person isn’t defined solely by their circumstances at one point in time,” Doug shares. “Everyone should be doing something like this, to get to know the individuals served by Duffy and understand what they’re going through. At the end of the day, what’s important is putting more in others’ ego jars than your own.”

Employee Wellness
Intentional, trauma-informed wellness initiatives for staff
For individuals working in the health care field, there is a basic understanding that trauma is often part of the job. As members of our Duffy team face each day working with such a complex population, it is normal to experience secondary trauma and disenfranchised grief. Our staff care deeply for the people in their care, and it can be heartbreaking to hear their stories, or worse, when a patient passes away.
The leadership at Duffy Health Center is acutely aware of the toll that working with a vulnerable population can take on members of the Duffy team. In order to ensure that employees have the opportunity for self-care, there has been an intentional shift in organizational culture to address staff well-being through trauma-informed initiatives that are specific to the population we serve.
In her role as Spiritual Care Coordinator, Pam Wannie is available to staff to process experiences in both an individual and group setting. “I’m always available to be in dialogue with staff either in my office or by phone, and happy to make time to chat,” shares Pam.
Outside of one-on-one interactions, Pam has instituted stress debriefings to give staff a chance to talk about the daily experiences of working at Duffy in a space that is safe, where people understand the work we’re doing. “We also need to process what we’re hearing and seeing. If we can do that with each other, we can - to a certain extentleave it with our job and not take it home with us or let it impact their own lives in an unhealthy way,” says Pam. Other opportunities Pam has organized include Wellness Wednesdays, with a 2 o’clock staff meditation, and some
light-hearted activity once a month such as themed group lunches.
Given the work that we do, at times we do learn of patients passing. Pam pays attention to this, and makes the first connection with staff when one of their patients has died before it’s announced to staff. “It’s important to recognize the human response that comes with hearing that kind of news,” she says. “If it catches someone offguard and they don’t have time to process, it could throw off their whole day or week.”
In addition to wellness opportunities provided internally, staff have the opportunity to engage in an Employee Wellness Program through Nove Yoga & Wellness, located in West Dennis.
The program offers staff online, virtual access to classes and resources in minfulness, yoga, and nutrition. Employees have the opportunity to attend live-streamed classes or access an online library of recorded classes at any time that is convenient for them. Another aspect of the program is that, for every staff member registered, a patient can also access this wonderful resource.
The cost of Duffy’s engagement in the Nove Employee Wellness Program is underwritten through the generosity of Greg and Jeannie Botsivales. We are grateful for their recognition of the importance of taking care of our staff, and to Nove for their partnership.
Duffy Doings 5
Doug Rodrigues
Community Health Workers
Care based on trust and shared experiences
On any given day at Duffy Health Center, you’re likely to run into Denies Smith-Grant or Susan Childs quietly and gracefully providing support to some of our patients who need it the most. Denies may be talking with someone in an exam room about how to effectively lower their blood pressure through changes in their diet. Susan is known to walk the few blocks to Cape Cod Hospital alongside a patient who may have anxiety about going on their own.
Denies and Susan are Community Health Workers (CHWs), and they are two of the most impactful members of the Duffy team. The American Public Health Association defines a Community Health Worker as “a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. This trusting relationship enables the worker to serve as a liaison between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery.” (Source: apha. org)
Study after study has shown that the integration of CHWs within the care team improves outcomes for the most high-need, high-risk patients. As they support individuals in navigating the health care system and caring for themselves, they assist in reducing Emergency Room utilization, and improve cost effectiveness for the entire system. The work Denies and Susan are doing is the perfect example of this.
Denies Smith-Grant joined Duffy Health Center in 2022 as a Medical Community Health Worker. In her role, Denies works closely with our Quality Improvement Manager and Duffy’s medical team to support patients in managing their health care. One of her primary roles is providing support to patients in managing their blood pressure to reduce hypertension. She is also an integral part of the team working on improving screening and follow-up rates for colorectal cancer.

“In my role, I’m able to provide support, educate, and help people navigate their care. When I check in with them on their blood pressure, I don’t tell them what happened, I ask them to tell me what happened. I’m not a medical
provider, but I can talk through it with them to help them understand what went right or wrong that week,” shares Denies. “They start to see me as a resource and ask me for help with other things related to their care. I never say ‘No,’ I work with them or pass them on to another team member who can help them.” From her vantage point, Denies also has a skill for recognizing systemic issues our patients are facing. She has brought several to Duffy’s Advocacy Committee for action (more on page 14).
Susan Childs is Duffy Health Center’s Case Management CHW, and she’s the first CHW at Duffy - in fact, when she first applied for the position 10 years ago, the role didn’t quite exist yet. Susan knew of Duffy through her involvement in other community organizations and felt that she could contribute to our patients given her personal experiences navigating the mental health and medical systems.
“I’ve been a patient of the mental health system since the age of 17. I had a lot of knowledge of resources and systems and first-hand experience, but I didn’t have a degree or know of a job where I could use that knowledge. I found that frustrating, because I wanted to help peers who were struggling the way I had,” shares Susan. “I know I have things to contribute, and if other people can benefit from all that I’ve been through, that gives it all meaning.”

Susan has been involved in several programs in her time at Duffy. Through our Bridge Program, she was part of a team that did outreach to patients in the psychiatric unit at Cape Cod Hospital, making meangingful connections with them before discharge and welcoming them to Duffy Health Center in order to bridge their care and set them on a good path. Susan is currently involved in Duffy’s suicide prevention program, Pathways to Hope.
“I feel like I’m in the best of both worlds,” she says. “I can contribute to Duffy’s programs by sharing my own experience; I can help peers who are struggling; and I can impact systems that are broken. I’m lucky enough to have an incredible support system around me, but not everyone has that. The most precious part of my work is compassionate listening. Letting peers know that you are here and care about them, especially in their darkest hour, is invaluable.”
6 Duffy Doings
Reading with Purpose
An opportunity to explore diversity, equity, and inclusion
A generous grant from Rockland Trust Charitable Foundation underwrites the cost of the books for any staff who are interested in the titles. Duffy provides a monthly opportunity to discuss the topics from the text and learn from each other’s perspectives.
Since 2020, Duffy Health Center has been working on our Diversity, Equity, and Inclusion (DEI) action plan with the guidance of our staff-driven DEI Committee. As part of that work, we have established a DEI Book Selection group to provide staff members with the opportunity to further explore DEI topics through a variety of lenses.

Therapist Resmaa Menakem examines the damage caused by racism in America from the perspective of body-centered psychology. He argues this destruction will continue until Americans learn to heal the generational anguish of white supremacy, which is deeply embedded in all our bodies. (Summary from GoodReads)
Below are the titles that have been offered to staff so far. We are grateful to the Rockland Trust Charitable Foundation for investing in our DEI work.

Tarana Burke and Dr. Brené Brown bring together a dynamic group of Black writers, organisers, artists, academics and cultural figures to discuss the topics the two have dedicated their lives to understanding and teaching: vulnerability and shame resilience. (Summary from GoodReads)
A sweeping global history that looks beyond European urban centers to show how slavery, colonialism, and war propelled the development of modern medicine. Boldly argued and eye-opening, Maladies of Empire gives a full account of the true price of medical progress. (Summary from GoodReads)
Set in El Paso, Texas in 1987, the novel follows two MexicanAmerican teenagers, Aristotle “Ari” Mendoza and Dante Quintana, their friendship, and their struggles with racial and ethnic identity, sexuality, and family relationships. (Summary from Wikipedia)
Books for Duffy Health Center’s DEI Book Selection Group are now purchased from local bookseller, Belonging Books. The organization is a community program provider and pop-up bookseller that centers the voices and stories of people of color and other underrepresented people on Cape Cod, creating intentional gathering spaces for joy, celebration, safety, and belonging. Duffy Health Center is grateful for partnership with a local business whose values align with our own mission and vision. Learn more at @BelongingBooksCapeCod
Duffy Doings 7
Agents of Change
Celebrating changemakers in our midst.
Building Trust to Make a Change
Amber Rogovich, Lead Medical Assistant
In the time since Amber Rogovich began as a Medical Assistant at Duffy Health Center 5 years ago, she’s adjusted to the difference of working in health care for the homeless compared to a traditional medical practice. “Some of our patients are in as often as once or twice a week, not just for a yearly physical,” she says. “When you see people that often, you really get to know them and have a real relationship with them.”
Amber was drawn to work at Duffy because she’s had a lot of life experiences similar to some of our patients. “It’s what I come from,” she shares. “I have a lot of the same history, having come from a physically and mentally abusive family, having experienced homelessness, and being a cancer survivor.”
When she recently moved into the position of Lead Medical Assistant, it was with an understanding of the important role that Duffy Health Center plays in our


patients’ lives, and the role that she and her team play on an individual level through their day-to-day interactions with patients. “Duffy is like home for some of the people in our care - a lot of them don’t have anyone in the world to trust, but by listening to them and giving them time to express what’s going on in their lives outside of their medical care, we build a bond so they can trust us and be comfortable with us,” says Amber. “My style is to just be real with people. I don’t sugar-coat things, I give my patients my honest opinions and feedback. I have different styles with different people, because you have to know what people’s triggers are or what they will respond well to.”
Ultimately, Amber’s goal is to provide exceptional medical care to Duffy patients, and to lead by example in her role. “Managing care is huge. Once someone is comfortable with you, it’s easier to help them understand the importance of doing certain screenings or engaging in care. By showing you care, you can help people to care about themselves.”
Finding Power in Sharing Your Story
Jackie Chasey, Certified Addictions Recovery Coach, Moms Do Care
“I’m a Cape Cod native, a descendent of the Mashpee Wampanoags,” says Jackie Chasey by way of introduction. “I was born into a low income family with teen parents; I endured abuse from a young age; I witnessed drug use, domestic violence, and mental health struggles. I experienced homelessness and bullying, struggled with my own mental health, and was in the foster system before being raised by my grandmother.”
Jackie feels it’s important to share these parts of herself, not because she is dwelling on her past, but because her past is what has made her who she is today: a Certified Addictions Recovery Coach. She began working in Duffy’s Alternative Peer Group for teens struggling with substance use; now she is working with pregnant and parenting women in recovery from substance use disorders. She is also an advocate for Cape Codders who are struggling with the same issues she has watched her family battle for generations.
“It’s generational,” reflects Jackie. “My parents did what they could with what they knew, but my life lacked consistency and healthy relationships. I was constantly dealing with the stigma associated with my family’s history. Adults would tell me that I wouldn’t amount to anything because they knew my whole family.”
After many years of struggling with substance use disorder herself - a means of escaping her traumasentrenched in an abusive relationship and experiencing homelessness, it was at a community health center like Duffy that Jackie finally sought help. “They treated me with dignity and respect there,” says Jackie. “All it took was one person to treat me like a human to break through.”
Jackie is an impassioned member of Duffy’s Advocacy Committee. “We all deserve the same help and services,” she says. “I want to share my story and be vulnerable to advocate for people in the same circumstances I’ve lived. I want to break generational trauma and create a space for generational triumph. My past and my children are why I strive to be who I am today. I get to show everyone that I can be part of the solution.”
8 Duffy Doings
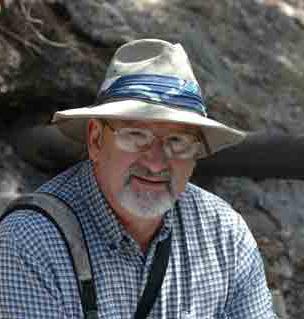
Understanding the Impact of Space Dr. Deborah Field Specialist in Psychiatry
Dr. Deborah Field has worked with individuals experiencing homelessness her entire 30 year career, both in Worcester, MA and here on Cape Cod.

“I hadn’t considered psychiatry prior to med school,” Dr. Field shares, “but I knew that I wanted to serve a marginalized, underprivileged popuation. I’ve always enjoyed working with complicated patients, and once I tried psychiatry I had found my fit.
“I’m especially drawn to individuals with schizophrenia and substance use disorder. These are the people who are the most misunderstood and stigmatized, and there’s so much room to make their lives better. It’s so lovely to see the real person behind the disease - the actual person underneath the things that society is afraid of or doesn’t like.”
Before medical school, Dr. Field studied architecture. She was particularly interested in the impact that architectural design has on human behavior, a concept that has carried through her career in psychiatry. “In the time when I
would do outreach, I learned to truly appreciate the importance of seeing where people are living,” she says.
“I think seeing people in their environments helps you to truly understand them and appreciate their incredible resilience. I’ve always been fascinated with how space impacts my patients’ mental health: why someone chooses to camp rather than stay in a crowded shelter, or even the effects of sitting in a small exam room or the waiting room here at Duffy. It’s interesting to see who can or cannot tolerate certain environments, and reminds us how important trauma-informed care is for understanding behaviors and improving our care environments.”
Given her focus on space, Dr. Field is a proponent of Housing First, the national model practiced by Duffy whereby housing is provided to chronically homeless individuals as a stabilizing element from which they can focus on other aspects of their life that need improvement, such as a job search or mental health issues. “Nothing motivates people more than having housing,” says Dr. Field. “When our patients get housed, they feel society values them so they start valuing themselves.”
Reducing Stigma Through Mentorship
Daniel Rodrigues, LICSW, PMH-C Director of Substance Use Disorder Services
In less than 4 years at Duffy Health Center, Danny Rodrigues has led a significant expansion of Duffy’s Substance Use Disorder (SUD) services. One of the most powerful aspects of this expansion is the growth of a cohort of Recovery Support Navigators and Recovery Coaches, individuals who have lived experience with substance use disorder and function in a non-clinical peer support role to those seeking recovery through Duffy’s services.
“In my opinion, individuals experiencing a substance use disorder are one of the most marginalized and vulnerable populations. There’s something meaningful about trying to provide individuals the care they deserve, to try to break through the systematic barriers that our populations have faced for decades,” reflects Danny.

When he talks about members of his team, Danny recognizes the challenges they face in other work environments. “First, we recognize that employers across the board are hesitant to hire individuals with lived experience because of stigma and fear. When someone is on their pathway to recovery or has found their recovery,
they’re no different than any other human being in the world. Having a scarlet letter on them is a tough thing to live with, and it can be devastating when you can’t share that aspect of yourself due to stereotypes. Paradoxically, having a stable, professional job is another stepping stone in the process of recovery.”
As someone coming to SUD work without lived experience, Danny recognizes the value of his team members’ perspectives. “A lot of the most successful things that we’ve done in our department have had a major influence from the voices of our team members with lived experience. From a professional standpoint, my guiding light is evidence-based best practices. But staff input is just as important and will be just as meaningful to the folks that we’re serving.”
It’s clear that Danny is proud of the peer recovery model, and of his team members in particular. “We want to professionalize a peer relationship. It takes a lot of nurturing and cultivating, and identifying the right people within the team to mentor others. For me, it’s not only about supporting the actual change but also elevating others so that they also become those agents.”
Duffy Doings 9
Change on an Individual Basis
Edgard Carvalho, Behavioral Health Partners Care Coordinator
In his 9 years at Duffy Health Center, Edgard Carvalho has worked in 3 different positions within the organization. “I first started here while working another job and going to school to become an EMT. I thought I would be here for 6 months, but I’m still here 9 years later.”
Edgard says that he’s stayed at Duffy because of the opportunities to grow and try out other departments, but also because the connection to his clients has made an impact on his personal life. “Some people teach you as much as you’re able to teach them. It’s gratifying to work with individuals and serve the community by building personal, trusting relationships with people,” says Edgard.
“As a Care Coordinator in the Behavioral Health Community Partners program, we really notice how much we can assist each individual with their care,” shares Edgard. “We see visits to the Emergency Room decrease as we support them in navigating their care. While we mostly support their health care needs, we do act like Case Managers in some ways, especially around housing. We’ll refer to another organization for support with housing needs, but still be there to help a client complete their paperwork.”
“We take a holistic approach to care management, and when you look at it on an individual level, you realize you really do make a difference in people’s lives.”
Advocating for LGBTQIA+ Rights
Eryn Tomascik, Behavioral Health Partners Care Coordinator
Eryn Tomascik is an advocate for the LGBTQIA+ community, through-and-through. Like most fierce advocates, her passion is born of personal experience. “I began transitioning to female when I was 17 years old. At that time, I did a lot of research and began educating myself on LGBTQIA+ health, medical issues, and rates of death by suicide,” Eryn shares.
When she joined the Duffy team, Eryn brought this passion with her, immediately becoming involved in Duffy’s staff-driven Diversity, Equity, and Inclusion Committee and taking a leadership role as the head of the Committee’s LGBTQIA+ workgroup. She also shares her knowledge by providing a training to all new staff on LGBTQIA+ issues.

“My goal is to eventually have LGBTQIA+ patients at Duffy
referred to me as a support person, similar to the peer relationship that our Recovery Support Navigators have. I’m someone with lived experience of what they’re going through,” she says.
Outside of Duffy, Eryn mixes advocacy with her personal interests through social media engagement. She is the moderator of a community on Discord, an online space for chatting and gaming. Her community is for queer people who play tabletop role-playing games.
“Although you can make a profit on Discord channels,” says Eryn, “Ours is about community first, over business. I genuinely want to make a change in someone’s life and give them the opportunity to join a community where they feel safe.”
Eryn has also given her time to championing the rights of transgender persons as it relates to public accommodation. As she so simply states, “Trans people just want to integrate into society.”
Making Change Through Care
Jennifer Carroll, Certified Addictions Registered Nurse
Jennifer Carroll is the Lead Registered Nurse on Duffy Health Center’s team providing Office Based Addictions Treatment (OBAT) for opioid use disorders. Although she likes to fly under the radar, there is no denying the impact of her presence on the Duffy team.


When asked about her guiding principles for care, Jen says, “It’s about meeting people where they’re at, having realistic expectations, and not being punitive. We need to keep in mind that we’re dealing with a chronic disease.”
Jen and the rest of the Duffy team are committed to providing same-day access for those seeking help with a substance use disorder - even during the COVID-19 pandemic. “Just because it was a pandemic didn’t mean
10 Duffy Doings
that substance use stopped,” reflects Jen. “It’s a big step for someone to ask for help with their substance use disorder. The day they reach out for help, if we can capture them in that moment, that’s a huge step in the right direction.”
“Even if they’re ready in that moment, the use isn’t going
to stop if someone has an appointment in a week, and each day that goes by, a person’s life is at risk,” she says. “We’re really lucky here at Duffy that we have a whole team of folks, so it’s not just the OBAT medical team, but it’s Recovery Support Navigators, it’s Behavioral Health. It takes all of us to get folks to come in and we just wrap around them with care.”
Creating Pathways to Access
Sara Seely, Patient Access Manager
Patient Access Manager
Sara Seely oversees two departments that are critically important to creating a positive first impression for patients at Duffy: the team of Access Representatives at the front desk and our Connections team, which is tasked with getting new patients connected to insurance and care, among other things (more on page13).
Sara is a fierce advocate for process improvement, with a knack for identifying how slight tweaks will improve access for our patients. “The work my teams does is so important,” she says. “I try to manage in a way that is beneficial to our patients but also protects my staff from burnout. I’m building the team in such a way that needs
are able to be met. These are the first faces and first interactions that our patients and potential patients have, and we want everyone to remember the friendly, familiar faces that are helping them get what they need.”
“Our goal is to be proactive in our work,” Sara shares. “The Connections team is moving back to our pre-COVID model where each day one team member focuses on outreach by phone, calling people whose insurance needs to be updated. That person is also available to staff and patients who need insurance support throughout the day. They work off a list produced daily where they know who is coming into the building for an appointment who needs to update their insurance. We’ve seen our uninsured rate dropping because of this initiative, which has a positive financial impact for the entire organization.”
Making Advocacy Local
Christine Johnson-Staub, Board Member, Advocacy Committee Chair

“I always knew I wanted to be involved in government, but I came at it from a different angle,” says Christine JohnsonStaub, Duffy Board member and Chair of the Advocacy Committee.
“I’ve been involved in public policy and advocacy since I was in college.”
As a self-proclaimed “latch-key kid,” Christine has always been fascinated with the family system; in particular, what factors create stability in some families and de-stabilize others, and the role that women play in this dynamic.
While working on her Master’s in Women’s Studies and Public Policy at George Washington University, Christine examined family economic stability and how public policy interacts with families and children. That led her to the Center for Law and Social Policy, an anti-poverty, antiracist organization. “In working there, I learned that you can’t look at childcare, health care, and systemic racism separately,” says Christine. “They’re all interconnected, and if you look at them individually, you’re missing the point. We need to study these issues at the root level and understand the history and policies that have impacted families in order to solve them.”
Today, Christine is working inside the government. “Under the current federal administration, the work of looking at issues in a deeper way has been welcomed. We’re doing equity work that digs deep,” she says. “I’m now an advocate with a small ‘a,’ and I’ve shifted my focus from leadership to service. I see an opportunity for leadership in lifiting the voices of communities adversely impacted by many policies all at once.”
Christine joined Duffy Health Center’s Board of Directors through a former member and advocacy chair. “When Leslie Dominguez-Santos asked me to join Duffy’s board, I recognized it as an opportunity to reconnect locally with issues that I’ve worked on at the national level.”

As with so many people drawn to the work of Duffy Health Center, Christine has experience with mental health and substance use disorders through her family of origin. “Duffy gives me an outlet to work on these issues in a meaningful way,” she says.
When it comes to Duffy’s advocacy priorities - primarily housing, transportation, and health care - Christine recognizes the importance of looking at these through an intersectional lens with our work in diversity, equity, and inclusion.
Duffy Doings 11
25 Year of Trust & Impact
What our patients are saying
“My support system, my network started here. I wouldn’t be where I am today if it wasn’t for this awesome team. I walked in here hopeless... you guys saved my life.”
- Nina, Duffy patient
“Everyone at Duffy worked with me until I was back up and running... they went 100% all the way with me. Duffy is all I know. It’s everything to me. It’s my life. Duffy is a wonderful place to regain yourself.”
- Lonnie, Duffy patient

“I feel like a person again...I basically tear up every time I’m there because Duffy Health Center is how health care should be for everyone; everyone should be treated with kindness and dignity.”


– Brittany, Duffy patient

“I have a lot of trust in this place. People here treat you with respect no matter who you are. They show that you can trust them. When you see that, you’re more likely to go back.”

- Jeff, Duffy patient & board member
“When I come here, they know my name - that's more than you can imagine. You are a person. That's what's so special about this place.”
- Richard, Duffy patient
“I’m really proud of what I’ve done, and I’m really proud of the help that I got at Duffy. I’m proud and I’m happy... and grateful for what they’ve all done for me. I can’t say ‘thank you’ enough.”
- Vanessa, Duffy patient & board member

12 Duffy Doings
Connections to Care
Assisting patients in accessing the care they deserve
The old joke is that you show up in the Emergency Room and the first thing they do is ask about your health insurance before addressing the urgent issue at hand. As satirical as that may be, the truth is that we are all functioning in a system where health insurance can be a gateway or an insurmountable barrier.
At Duffy Health Center, we work with individuals who do not always have access to health insurance by traditional means such as employment. So how do we make sure that they have the coverage they need and receive the high-quality care they deserve? The answer lies in our Connections team. Composed of three Case Managers who are certified in insurance counseling, the team provides a gateway for patients.
For any new patient presenting at Duffy, a Connections appointment consists of intake, support accessing benefits, and an initial connection to services. “I provide an overview of what Duffy has to offer and take the time to see where they are - whether they have insurance, whether they understand their coverage,” says Jess Chambers. “A lot of our patients don’t have permanent status so they have MassHealth Limited, which provides coverage for emergency services. But they can also access Health Safety Net, which covers services at community health centers like Duffy.”
“It’s important to recognize that understanding health insurance is like learning a second language,” says Sara Seely, Patient Access Manager and supervisor to the Connections department. “Then it’s a matter of translating it back to someone who may have limited literacy - or
health literacy - in a meaningful way.”
“Often, people are eligible for things that they don’t even know about, and for a lot of our patients, it is difficult to navigate,” says Jess. “I recently met with a gentleman who was having a lot of anxiety about Medicare. I was able to look into his situation, explain what the next steps should be, assist him in his application, and let him know what to expect moving forward - all in about 10 minutes. He was so relieved and told me it was a huge weight lifted off his shoulders.”
Of course, the Connections team does much more than help patients access insurance coverage. “Patients usually take the step to come in when they are in crisis,” says Bonnie Adkins. “They just want to talk to someone and share what’s going on. They often have emergent needs, so we connect them with other people within Duffy - to our staff Nurse for medicine refills, to case manager of the day, or to our Recovery Support Navigators, because a lot of people come to us through the Medication Assisted Treatment program’s same-day access. “
Once our patients meet someone who will help them, who they know they can trust, they’ll keep coming back to their Connections Case Managers, even for things they don’t necessarily do. The group agrees that beauty of Duffy is that they can connect patients to other services within the building and make a warm hand-off to a colleague.
Outside of their patient-facing work, the team is proactive in their outreach to patients. They make calls to patients who are having insurance issues or are uninsured. They contact patients who need to renew consents for care. They reach out to people who are eligible for OneCare, a MassHealth plus Medicare plan that offers much more flexibility than being enrolled in both programs separately.
“Having a strong team around us is really important,” says Taylor Griffin. “Sometimes the work can be intense - people share things I didn’t necessarily expect in this position, but I know I have my teammates for support when I need to process interactions I’ve had. It’s really rewarding work to feel like we can make a difference.”
Connections Case Managers (L-R) Bonnie Adkins, Taylor Griffin, and Jessica Chambers.

Duffy Doings 13
Partnering for Change

Strategically identifying barriers to care
In recent months, Duffy Health Center’s Advocacy Committee has identified two issues that directly impact the provision of patient care. The first is related to patients’ ability to access a colonoscopy - a life-saving screening for colorectal cancer - dependent on their insurance coverage. The other relates to transportation provided by MassHealth. The Committee first confirmed with a sister community health center on Cape Cod that their patients were experiencing similar issues, then met with our Primary Care Association, the Massachusetts League of Community Health Centers, to present the issues and discuss action steps.
Local Access to Colonoscopy
As our Quality Improvement team continues work on Duffy’s Colorectal Cancer Screening initiative, a disturbing trend has come to light: patients who are covered by Massachusetts’ Health Safety Net - primarily individuals with undetermined status - cannot be referred locally to receive a colonoscopy. Instead, they must be referred to Boston Medical Center (BMC), presenting a barrier to the screening given the distance and lack of transportation for many individuals in our care.

Of the 212 Duffy patients who have Health Safety Net coverage, 12 were referred to BMC from January 1 through August 30, 2022. While the number of patients who have been referred is relatively small, it is resourceintensive both from a referral standpoint and the patient’s ability to navigate another health care system, not to mention factors that can present barriers to completing a colonoscopy.
One specific example provided by Emily Hildebrant, Quality Improvement Manager, regards a patient who was referred to BMC for a diagnostic colonoscopy as a routine follow-up to a positive screening. In the meantime, she
was newly diagnosed with diabetes and has found the process of scheduling a procedure in Boston to be too overwhelming to handle in addition to the new diagnosis. Duffy is continuing to work with this patient to schedule and attend the colonoscopy appointments but at this point it has been almost 8 months since her initial positive test. Options closer to home would have facilitated a follow up colonoscopy in a more timely manner.
Timely Transportation to Detoxification
Patients who have insurance through MassHealth are eligible to receive non-emergency transportation to and from appointments. This transportation, called a PT-1, can be requested by their provider and is an essential resource for many of the individuals in our care.
The system works well for requesting a ride that is needed in a few days’ time. An issue that has arisen, however, is accessing transportation for a patient in crisis who is ready to take the step toward detoxification. Timing is crucial in this process - matching a patient’s willingness with an available opening in a detoxification setting is no easy feat. Once this is done, the next step is to get them there. Given the lack of available resources of this type of care on Cape Cod, patients often need to be transported over the bridge. The PT-1 system is not built for a quick turnaround; we are likely to lose patients to the grip of substance use while waiting for transportation.
Next Steps
Our partners at the Massachusetts League of Community Health Centers were extremely receptive to the Duffy team’s concerns about these issues. Their team plans to take the lead on addressing the referral issue with Health Safety Net, and will discuss expanding service area to the Cape. A Duffy representative will also be part of that conversation. They will also speak with MassHealth about the prospect of providing organizations like Duffy with a direct line for PT-1 requests for an individual with an urgent transportation need.
14 Duffy Doings
Good News Stories
Vignettes that remind us of our impact
Duffy team members’ days are full of interactions with our patients – some positive, some challenging. Often, staff do not realize how much of an impact their small acts of compassion and kindness have on the patients and clients we serve. Luckily, Case Manager Cathy Finn collects good news stories from around Duffy to remind us all of the impact we can have.
Birds, children’s voices, your favorite music - how much would your life change if you couldn’t hear? Case Manager Leah Morrissey has been working with a 74 year old man, a veteran awarded a Purple Heart, who hadn’t heard in 50 years. Due to a problem with his listed discharged status, he was not able to get hearing aids, and because he couldn’t hear to talk to Veterans’ Services, he gave up.

Then he was lucky enough to meet Leah. She got in touch with the local Veterans’ Service office, worked on completing and sending appropriate paperwork, and worked with the Providence Veterans’ hospital on his behalf. After months of work, Leah helped him get an appointment for his hearing exam and he finally got new state-of-the art, blue tooth, chargeable hearing aids.
On his next trip to the Veteran’s Center with Leah, he could finally communicate with them, and is now working to get his discharge upgraded. That day, he took out his purple heart to show Leah - something he said he rarely does, but it was a sign of his appreciation for all of her support. This gentleman told Leah that he hadn’t heard his daughter’s voice since she was 7 - until she helped him get his hearing aids.
Case Manager Arlene Crosby was working with a woman who was experiencing violence in her household. Arlene helped this woman feel safe enough to leave her home and find shelter somewhere she would be safe.
The client saw Nurse Practitioner Kyle Chaplic, who spent two hours with her, caring for her physical issues but mostly listening to her story. Kyle referred her to Spiritual Care Coordinator Pam Wannie, who was able to offer her support over several conversations.
The client notes that she has also been connected to alternative housing, to our partners at Housing Assistance Corporation, and to the Barnstable Police who are patrolling her area and helping her feel safe. She told Case Manager Cathy Finn, “I never would have imagined that the community would come together for me. With all of this outreach and support, it’s been like a blanket around me.”
When we do court-mandated mental health evaluations, it can be difficult because most individuals don’t want to be there - they feel the judge is making them do it. Therapist Lisa Perkins sees it differently: “I look at the evaluations as a precious chance to plant a seed.” Lisa often recommends 6 sessions of therapy for individuals that may not have ever had the experience of therapy or for individuals that may need support but just don’t know it yet.
One of Lisa’s recent clients has been resistant and difficult to engage, but her probation officer has been supportive of her struggle and encouraged her to complete the sessions; so she has kept her appointments.
She has mental illness that gets her into some trouble as well as health issues that need to be addressed. While Lisa discusses this with her, she is not ready to address it. Her probation is ending in November, and as Lisa was making her last 2 appointments, she asked if she could still come even if she wasn’t on probation. Lisa excitedly said, “Of course!”
Seed planted. Trust begins.
Duffy Doings 15
(Below: photo of the patient’s Purple Heart.)
Community Engagement
Gathering in support of Duffy’s mission
Summer Solstice at The West End
June 15, 2022: Duffy supporters gathered at The West End in Hyannis to hear updates on our work from CEO Heidi Nelson and Board President Kathleen Bresette.


July 19, 2022: For the second year, Duffy Health Center was invited to participate in the 6th Annual Charter Cup Fishing Tournament, organized by E. J. Jaxtimer. Sponsored by Wendy’s, the team set out under the leadership of Captain Jeff Perry of First Light Fishing, LLC. They raised over $7,500 for Duffy Health Center, and by catching the tournament’s largest bass they secured an additional $1,000 gift in support of our mission. We are so grateful!




16 Duffy Doings
Left: Brenna Lapsley, RN, member of Duffy’s Falmouth Road Race Team, and Christina Bologna of The Cooperative Bank of Cape Cod.
Above: Usama and Stephanie El Sehrawey of Wendy’s and Jitka Borowick of Nove Yoga & Wellness react to comments from CEO Heidi Nelson.
Above: Captain Jeff Perry and First Mate Derek Perry of First Light Fishing, CFO Jeff Dykens, CEO Heidi Nelson, Usama El Sehrawey of Wendy’s, Board President Kathleen Bresette, Sara Grambach, Director of Development.
Left: Duffy CFO Jeff Dykens; Right: Terry Smily of Wendy’s, Usama El Sehrawey, Jeff Dykens and Capt. Jeff Perry
Annual Client Appreciation Cookout
August 11, 2022: Duffy staff and volunteers came together to put on an old-fashioned cookout in appreciation of our patients and clients. There were hot dogs, burgers, and even an ice cream truck! Members of the Rotary Club of Harwich-Dennis ran the grill and the delicious food was from Peterson’s Market in Yarmouth. Duffy was one of two community health centers in Massachusetts to receive funding from the National Association of Community Health Centers in support of our National Health Center Week event.
During set-up for the event, Duffy patient Wayne approached the group and said, “I know this hasn’t even started yet, but I just wanted to say thank you. You don’t have to do this and it’s Mara Whitman, Sarah



Right: Brad Boyd of Harwich-Dennis Rotary, Jim Higgins of Harwich-Dennis Rotary, Duffy’s Danny Rodrigues, Melissa Payne, Jim Donnelly of HarwichDennis Rotary, Kim Katsios,

Maureen
really nice that you do.”
August 21, 2022: Fourteen runners hit the 7.1 mile course representing Duffy Health Center in the 50th Annual Falmouth Road Race (three of our runners were unable attend on race day). The race was made up of staff, board members, family members, former staff, and friends of Duffy. Our team set a lofty fundraising goal of $25,000 in celebration of Duffy’s 25th anniversary year, and not only did they reach it, but they surpassed the $26,000 mark. All funds raised will directly support Duffy’s programs and services. Thank you, Team Duffy!


Pre-race
At
Duffy Doings 17
smiles! Back row, left to right: Christina Wiseman, Kara Feidelseit, Larry Feidelseit, Abby Weber, Sara Grambach, Amanda McGerigle, Andrew Singer. Front row, left to right: Jillian Pieciak, Brenna Lapsley, Sarah Lapsley-Martin, Jessica Baecker, David Burke, Andrew Burke.
the finish: Kara Feidelseit, Jessica Baecker, Brenna Lapsley, Sarah Lapsley-Martin, Jillian Pieciak, Christina Wiseman, Larry Feidelseit
Ducie, Christina Wiseman,
Radley
National Recovery Month
Celebrating recovery while honoring lives lost too soon

In honor of International Overdose Awareness Day (August 31) and National Recovery Month (September), members of the Duffy team traveled to the Massachusetts State House to assist in placing flags in memory of the individual lives lost to overdose from 2011 to 2021 - 20,000 lives in total. They met Governor Charlie Baker and had the opportunity to talk with him about the important work being done to address substance use disorder at Duffy Health Center. The event was organized by our friends and partners at Boston Medical Center and the Bureau of Substance Addiction Services. It was truly an honor to participate in this moving event.

Left: Duffy team members Jackie Chasey, Dana DiSenso, Sarah Ducie, Danny Rodrigues, Melissa Payne, Mara Whitman and Daina Carpenter with Governor Charlie Baker.


Above: Danny Rodrigues, John Barboza; (Back Row): Daina Carpenter, Melissa Payne, Kristina Barboza, Sarah Ducie, Mara Whitman; (Front Row): Dana DiSenso, Jackie Chasey.



ROAR: Ride for Opioid Addiction Recovery
On Sunday, September 11, hundreds of bikers rode 40 miles from Falmouth High School to Barnstable Intermediate School to raise awareness - and funds - in support of recovery from opioid use disorder. Duffy has been a grateful recipient of ROAR funds - since 2018, we have received $62,000 in support of our substance use disorder services’ housing programs. We are grateful to organizers Karen and Jamie Pina (bottom left).
18 Duffy Doings
Ways to Support Duffy
Give to Housing First
Housing First is an evidence-based program that shifts funding away from emergency shelters and toward permanent, supportive housing. By eliminating the chaos of homelessness, Housing First participants can more effectively address underlying behavioral health and medical issues. Duffy was the first Cape-based organization to adopt this model.
Duffy Case Managers work with local public and private housing authorities and private landlords to help people achieve and maintain successful tenancies. The Housing First program has resulted in a decrease in risk behaviors and utilization of public services and increased positive connections to preventive health services and to the community.
Learn more and make a gift at duffyhealthcenter.org/give
Join our Community of Hope



Our monthly giving program, Community of Hope, is impactful for Duffy because it provides a steady stream of revenue on which we can depend. It’s an opportunity to make a regular, automated gift to Duffy and have an ongoing impact over time. Once you join the Community of Hope, your gifts come straight to Duffy without lifting a finger! No investment is too small; you can join the Community of Hope with as little as $10 a month.
Learn more and become a member at duffyhealthcenter.org/ give/community-ofhope
Shop with AmazonSmile
AmazonSmile is a program where Amazon donates 0.5% of the purchase price of eligible products to the organization of your choice.


Please consider choosing Duffy Health Center as your charity; proceeds from your online purchases will go towards supporting Duffy’s programs and services as we seek to improve the lives of persons who are homeless or at risk of homelessness on Cape Cod.
Learn more and register at smile.amazon.com
After their son Patrick passed away from a drug overdose in 2017, Patricia Graham and her family established the Patrick Graham Charitable Foundation in his memory. The guiding principle of the foundation is that no one should suffer alone from a drug addiction or feel shame associated with the disease.
In September, Patricia Graham and other supporters of the Patrick Graham Foundation came together to support mothers and children in Duffy’s Moms Do Care program. Their donations of diapers, wipes, bottles and other baby supplies will go directly to pregnant and parenting women with a history of substance use who are working to maintain their recovery. We are so grateful to the Patrick Graham Charitable Foundation and its supporters!
Duffy Doings 19
Members of the Moms Do Care team with items donated from the Patrick Graham Foundation and its supporters.
94 Main Street Hyannis, MA 02601



Thank You to Our Sponsors



For their ongoing support of our work!


Benefactor Supporter
Advocates
Friends
Non-Profit Org. U.S. Postage PAID Permit No. 58 Hyannis, MA