TURNING

INTO
A STRATEGIC COURSE TOWARD
WHOLE-PERSON HEALTH
OSHER CENTER FOR INTEGRATIVE HEALTH



OSHER CENTER FOR INTEGRATIVE HEALTH


It is my honor to share the Osher Center for Integrative Health’s annual report and to recognize the vision and generosity of the Bernard Osher Foundation. The foundation’s bold investment laid the groundwork for a center that champions whole-person health and advances workplace well-being in ways that strengthen individuals, teams, and communities. I am proud of our progress together, and I’m heartened at the promise of what lies ahead.
Over the past year, we have built and strengthened meaningful partnerships across our expansive campus. This spirit of collaboration has amplified our impact, ensuring that whole-person health is not simply a concept but a lived experience.
Our work is deeply aligned with the University of Utah’s Impact 2030 vision, championed by U President Taylor Randall. By advancing integrative and preventive approaches to health, promoting wellness in the workplace, and engaging in cross-sector collaboration, we are helping the university meet its ambitious goals. Together, we are responding to today’s needs while creating a healthier, more resilient future for tomorrow.
I am grateful to our partners and colleagues who support this mission. With your continued commitment, we will carry forward this year’s momentum and expand our ability to serve as a model of whole-person health and resiliency. I am moved by the amazing work of so many individuals shared in the pages of this year’s annual report.
AMY LOCKE, MD, FAAFP
Director, Osher Center for Integrative Health
Chief Wellness Officer, University of Utah
Co-Director, Driving Out Diabetes Initiative
Professor, Department of Family & Preventive Medicine
Adjunct Professor, Department of Nutrition & Integrative Physiology
Impact 2030 is the U’s strategic plan that clarifies and aligns institution-wide goals and inspires action toward positive, measurable change in the quality of life of individuals across our state resulting from our teaching, research, service, and clinical efforts.
The three pillars—student success, research and innovation, and service to community— define the ways in which the U will become a top 10 public university with unsurpassed societal impact. Throughout this report, we’ll highlight OCIH’s contributions related to each of these pillars and in support of Impact 2030.
The Osher Center for Integrative Health focuses on building strong, effective teams, clinical-community partnerships, and upstream-focused services to facilitate optimal health across campus and the Mountain West. Our efforts are grounded in a framework that is people-centered, comprehensive, holistic, equitable, and accountable.
COORDINATE
• Chief Wellness Office (est. 2014)
• Optimize wellness across campus and our community
CREATE
• Key pilots: Health Coaching, Diabetes Prevention Program (DPP), Exercise is Medicine, Food Pharmacy
• Hubs: Wellness Bus, Resiliency Center, Skaggs Patient Wellness Center
INNOVATE
• Value-based care pilots that expand services, starting with employee populations
EDUCATE
• PEAK Health and Fitness, Spencer Fox Eccles School of Medicine Pathway of Excellence, Health Coaching Certificate, Lifestyle Medicine Residency curriculum, Integrative Medicine Fellowship
Discovery through implementation and dissemination science
In May 2025, the U celebrated the grand opening of a dedicated workplace for the OCIH.
When the U offered a new space that would accommodate services provided by OCIH’s myriad programs and initiatives, the leadership team and staff jumped at the opportunity. They immediately began collaborating with users of the OCIH and the architects leading the project. This partnership inspired and informed the plans for developing the center’s new space in Research Park.
Dedicated to the physical and mental well-being of the U’s faculty, staff, patients, and community members, OCIH now has a primary location that offers multi-purpose studios for lectures and classes, rooms for consultations, a medical gym, and office space. This new space will allow the team to interact more with each other and brainstorm ways to streamline services, eliminate redundancies, and be as efficient as possible. The result will be a thoughtful expansion of programs to meet the needs of the people we serve.
As beautiful and calming as OCIH’s new space is, it will not change the focus of the team. “Our job is to meet people where they are,” Dr. Locke noted. “We are still going to be out and about campus and in the communities we serve.”


Partnership with Rural Affiliate Hospitals Seeks to Reduce Burnout and Support Well-Being in Health Care Workforce
When the Resiliency Center was awarded a $3 million grant in 2022, Amy Locke, MD, Megan Call, PhD, and Ellen Morrow, MD, knew the timing was perfect. “Only 10 groups were awarded this funding nationally,” Dr. Call noted at the time. “It is a great opportunity for the collective efficacy for U of U Health. The timing of this award comes after two full years of the Covid-19 pandemic, which is stretching health care teams and individuals in unique ways, leading to high levels of persistent stress with concern for longer-term mental health implications.”
Now, three years after the grant was funded and a full five years since the start of the pandemic, the research team is putting their findings into action. Health care providers at the U and across the affiliate group are enjoying a more supportive work life thanks to expanded programs and updated, comprehensive resources developed according to evidence-based principles and the needs of affiliates.
The Wellness Curriculum, Code Lavender, Peer Support, and Joy in Work programs were all expanded and shared across the four participating affiliate hospitals and the Utah Department of Health and Human Services. Comprehensive resources, including toolkits related to peer support, mindfulness in medicine, and resiliency, were updated and distributed. The team also shared support checklists and adverse event guides.
To ensure project replication, the team even created a “recipe book”—presentations developed into interventions with easy-to-follow instructions. Topics include decreasing burnout in nurse educators, streamlining clinic visits, anesthesia protocol, physician assistant communication culture, and operating room ergonomics.

Affiliate outreach was conducted with Blue Mountain Hospital (Blanding, Utah), Gunnison Valley Hospital (Gunnison, Utah), Madison Memorial Hospital (Rexburg, Idaho), Moab Regional Hospital (Moab, Utah), and the Utah Department of Health and Human Services.
An exciting update to WellU, including the introduction of an updated Health Risk Assessment, is putting wellness support, individualized services, and evidence-based programs directly within reach of U employees. The Osher Center offers services for both University of Utah employee wellness programs (main campus and the hospitals and clinics). Over the past year, WellU, the longstanding campus employee wellness program aimed at elevating whole-person health through healthy activities and preventive care, underwent its biggest changes since it was introduced. In July 2024, OCIH was proud to launch the redesigned, four-step WellU program, which aims to tailor resources based on the level of health risk experienced by an employee while empowering participants.
The Health Risk Assessment (HRA) allows the Osher Team to make informed recommendations and provide additional, individualized support to employees who may be at higher risk for poor health outcomes. It also gives OCIH leadership a view into the needs of the campus community and allows the team to refine programming.
This self-reported, evidence-based evaluation uses validated measures to provide participants with an awareness of their health risks across various domains of health behaviors and psychosocial wellness. More importantly, it serves as a novel coaching tool, helping individuals who are ready to make a change find an evidence-based next step towards health matched to their needs and interests.
After completing the HRA, employees receive a report with their results and a WellU Action Plan recommendation based on their self-identified health risks (if any) and health priorities. Quantifiable risk scores (as applicable) and red/yellow/green risk levels are indicated for all health areas. This document may also be shared by the employee with their health care provider for further discussion and action. The report contains information about all health areas that were assessed.
HRA survey completion rate among
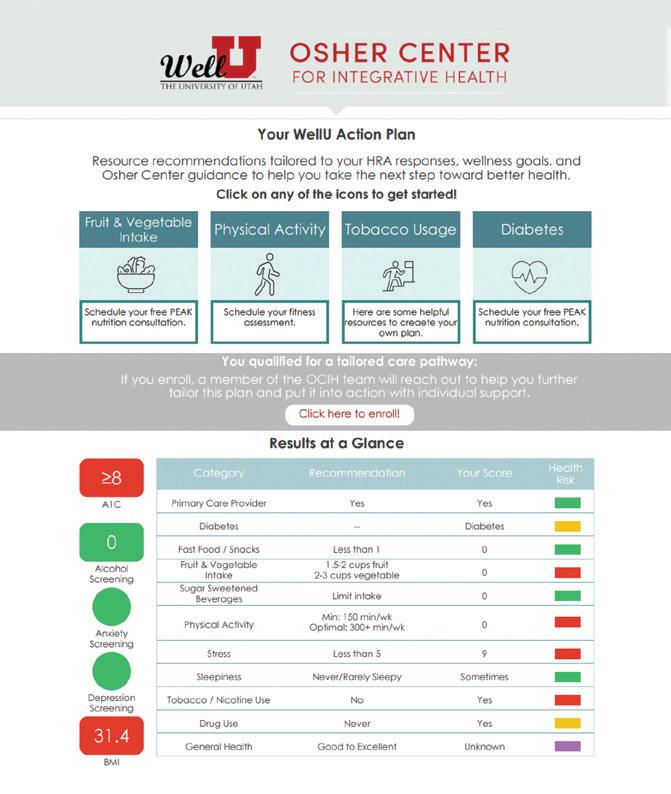
All participants are offered personalized, evidence-based programs based on their results. For those with rising health risk, a Tailored Care Pathway offers structured support.
• Increased support within a structured path for employees with rising or high risk as determined by their responses to the HRA
• Working with an OCIH Wellness Navigator, the employee selects a track that aligns with their health goals.
- The Healthy Body Track offers a variety of curated pathways.
- The Healthy Mind Track is delivered by the Integrated Behavioral Health Team within U of U Health Primary Care.
Traditional Track
• Functions like the classic, self-guided version of WellU
• Available to employees not qualifying for a Tailored Care Pathway or those who elect not to engage with a pathway recommendation
• Includes a personalized action plan requiring completion of at least four health activities aligning with the individual’s health goals
Once employees identify the route they will travel through their WellU experience, they are ready to engage in their first activity. The OCIH Team is always available to assist with questions or offer support along the way.
As part of the HRA, employees without a primary care provider were able to opt into connecting and scheduling with one via the streamlined process offered through OCIH. Of 997 primary care requests, 70% (698) ultimately scheduled an appointment, for potential cost savings of more than $2 million. (Current research shows total health care costs for patients with an established primary care provider are $3,274 lower than for those without a primary care provider: https://pmc.ncbi.nlm.nih.gov/articles/PMC9793026/).
Of the more than 10,000 employees who completed the HRA: enrolled in the Traditional Track enrolled in a Tailored Care Pathway overall completion rate 64% 36% 59%
PEAK students offer various WellU services as part of their training, including nutrition consults, health coaching visits, leisure consultations, exercise prescriptions, personal training appointments, and wellness presentations. Last year, these students coached close to 3,700 individuals through WellU and WellnessNow (offered to University of Utah Hospitals and Clinics employees).

The experience became a cornerstone of Heather Brown’s professional growth during her time in the Coordinated Master’s Program in Nutrition and Integrative Physiology. “It allowed me to actively apply and refine my nutrition counseling skills in real-world settings, including goal setting, behavior change strategies, and the use of motivational interviewing,” she noted. “I learned not just how to provide evidence-based recommendations, but how to do so in a way that is collaborative, empathetic, and centered on the individual’s values and lived experience.”
“What stood out to me most was the opportunity to form genuine human connections. Everyone faces challenges—some visible, others tucked quietly beneath the surface—and often, what people need most is simply to feel heard. Through these consultations, I was able to offer not only nutritional guidance but also encouragement and reassurance. It was an incredible gift to remind individuals that they are not alone in their struggles, and that they are worthy and enough just as they are. I’m deeply grateful for the opportunity to serve this community. The experience reinforced my passion for compassionate, person-centered care and affirmed the kind of practitioner I hope to become.”

“During my time as a student offering PEAK nutrition consultations to U employees, I was continually inspired by the kindness, humility, and openness of those I worked with. The respectful culture within the U system created a space where meaningful connection felt natural—every individual I met approached our sessions with sincerity and gratitude. It was a privilege to be welcomed into those conversations.” —Heather Brown, MS ’25


Over the past century, researchers and clinicians have made incredible progress in understanding and treating diseases. As research has informed clinical approaches, health care providers have become adept at alleviating suffering and addressing many acute and chronic ailments.
Undoubtedly, this approach is beneficial. But what if we could prevent these diseases in the first place? This is the question asked by a group of national organizations known as the Collective to Strengthen Pathways for Health Research. According to the Doris Duke Foundation, the Collective seeks to “fund, conduct, and apply research in prevention and care that mirrors the way we approach research for treatments.”
The Doris Duke Foundation, American Cancer Society, American Heart Association, Burroughs Welcome Fund, Susan G. Komen, and additional philanthropic partners lead the Collective’s efforts. The Collective started by turning to research-driven organizations nationwide to elevate conversations featuring the latest research and experiential data. Across the US, it awarded 18 organizations grants to develop and host conversations centered on “funding models, policy changes, innovative delivery approaches, systemic shifts, and cross-sector investments that can produce transformative gains in health outcomes.”
The U’s OCIH joins an impressive cohort of 2025 conversation hosts that includes Arizona State University, the Association of American Medical Colleges, Dartmouth College, Duke University, Emory University, Harvard Pilgrim Health Care Institute, Johns Hopkins University, Mayo Clinic, Morehouse School of Medicine, NYU Grossman School of Medicine, Social Science Research Council, University of Chicago, University of Southern California, and Virginia Tech. IN GOOD COMPANY


On May 22, 2025, the University of Utah hosted the symposium Extending Return on Investment: A MultiSector Approach to Whole-Person Health, led by Dr. Locke and supported by the Doris Duke Foundation and the Roberson Foundation through the Collective. The event brought together a diverse group of clinicians, researchers, payers, policymakers, community leaders, and funders to explore a new paradigm for assessing value in health and health care.
Centered on the concept of collective return on investment (ROI), the symposium challenged the limitations of traditional ROI models, such as narrow institutional perspectives and short-term financial metrics. Instead, it emphasized long-term, population-level, and equity-driven outcomes. Participants focused on building a framework for shared impact that reflects the holistic benefits of whole-person health (WPH), particularly across the urban-rural continuum.
Throughout the day, attendees engaged in keynote addresses, panel discussions, and collaborative breakout sessions aimed at advancing WPH through multi-sector investment, coordinated care, and policy transformation. Discussions explored redefining ROI to include societal and patient-centered benefits, aligning payment models with upstream interventions, and integrating community perspectives into economic evaluations. Case studies and real-world examples highlighted opportunities to scale successful interventions and reorient funding structures to support prevention, primary care, and the social determinants of health.
The symposium marked an important step toward operationalizing the collective ROI model and building the cross-sector infrastructure necessary to support whole-person care. With increasing recognition of the need to transform the US health care system, the event laid the groundwork for continued dialogue, demonstration projects, and strategic alignment to promote sustainable, equitable health outcomes across Utah and beyond.


In the evolving field of nutrition and integrative physiology, hands-on learning is a critical component of effective education. Teaching kitchens have developed into impactful tools that bridge the gap between nutritional knowledge and practical application. At the U, Theresa Dvorak, a registered dietitian and director of the Culinary Medicine program at the College of Health and an Osher Center affiliate, leads this innovative initiative.
Blending nutrition, cooking, and community engagement in a dynamic learning space where culinary skills intersect with medical education, the U’s teaching kitchen is transforming how future health professionals understand and promote nutrition in patient care. Students studying medicine, nutrition, nursing, pharmacy, and social work collaborate and learn to translate nutritional concepts into actionable behaviors to effectively guide their patients toward healthier lifestyles. They also bring this knowledge to the campus community, teaching nutrition workshops as part of the WellU program.
Research shows that a poor diet is a leading contributor to chronic diseases such as diabetes, cardiovascular disease, and obesity. Teaching kitchens have the power to transform health care by addressing critical nutrition education gaps among medical professionals, equipping future health care providers with skills to integrate dietary guidance into patient care. These efforts can promote preventive care, reduce diet-related chronic disease prevalence, and lower health care costs.
The U’s teaching kitchen collaborates with the Driving Out Diabetes Initiative and partners like Wasatch Community Gardens and the Wellness Bus to deliver nutrition education and healthy food access to underserved populations. Mobile teaching kitchens ensure accessibility, while culturally tailored curricula address specific dietary needs, promoting equity in health education. By integrating teaching kitchens into health care, OCIH is shaping better clinicians and fostering healthier communities while demonstrating the transformative power of culinary knowledge.
The inaugural Teaching Kitchen Symposium, hosted at the U November 13–14, 2024, convened 250 professionals from 40 states and six countries dedicated to advancing hands-on approaches to nutrition education. Presented by the Teaching Kitchen Collaborative, the symposium featured presentations by experts from universities and health care systems across the US on topics ranging from teaching kitchen set-up and funding to advancing nutrition education in communities for all ages.


Teaching kitchens have the power to transform health care by addressing critical nutrition education gaps among medical professionals, equipping future health care providers with skills to integrate dietary guidance into patient care.

Food Pharmacies leverage food as medicine to support the prevention and management of nutrition-related diseases by increasing access to healthy foods and nutrition resources. Throughout the past year, the Food Pharmacy at Rose Park Clinic, one of five student-led clinics within the U of U Health system, has emerged as a model for how patients, students, and providers can successfully collaborate to deploy this innovative program.
The Rose Park Food Pharmacy fosters student success and positive patient outcomes as student learners rotate through the clinic weekly and take an active role in developing processes and workflows. Student projects include:
• A re-design of the Food Pharmacy Intake and Patient
Feedback questionnaires
• Creation of training materials for learners and patient-facing resources
• Development and implementation of pantry/communitysupported agriculture user data to facilitate program tracking, utilization, and outcomes
Philanthropy has been crucial to the Food Pharmacy’s success, enhancing collaboration among faculty across the health system. This includes SFESOM faculty, registered dietitians, a community health worker, and faculty from the College of Health. These partnerships ensure a high-quality learning experience while meeting community needs.
Every year, the Rose Park Student-Led Clinic hosts learners from the Spencer Fox Eccles School of Medicine, Nutrition and Dietetics, and Wellness Coaching.
“[Most of us] really have no idea what it means to rely on places like this to get our meals for the week. I am so grateful for the opportunity to work with these amazing patients.”
—Craig Busch
Dietetic
Intern, U of U Health Food Pharmacy and Food Rescue
In January 2025, a new community-based program, Move Together for Health, launched as part of the Exercise is Medicine initiative after initial physical activity screenings revealed that over 70% of Wellness Bus visitors were not meeting recommended physical activity guidelines. These results underscore the need for accessible and supportive interventions like Move Together for Health.
Developed through a partnership between the Wellness Bus, the Sorenson Unity Center, the U’s Department of Health and Kinesiology, and PEAK Health and Wellness, this free, 12-week group-based exercise program is designed to address the low levels of physical activity observed among community members. The program is led by trained U student instructors and grounded in principles of group dynamics to foster social support and engagement.
Move Together for Health is already demonstrating its value in promoting healthier, more active lifestyles and enhancing overall community well-being. Participants report both physical and mental health improvements, including weight loss, increased strength, and improved mood. One participant shared, “I know I’ve lost weight, and I feel better.” Another remarked, “I just feel happier. I feel good. I feel healthy.”



At OCIH, we envision a future where individuals and teams feel seen, heard, and valued in the workplace and consistently find meaning in their work. By leading system-wide strategies, we support individuals, teams, and leaders. Focusing on enhancing the personal and professional well-being of U employees, we prioritize a culture of wellness, best-practice system design, and ensuring access to the resources employees need for work and personal fulfillment.
Established in 2017, the Resiliency Center strives to create a U of U Health work environment where individuals and teams can thrive. During the 2024–25 academic year, the center further defined its mission and began growing into its next stage. This included identifying and operationalizing three main domains of work: psychological health, team empowerment, and system resilience. These areas were selected based on an assessment of existing program and service utilization, an identified need from the center’s years of work and collaboration, and a recognized opportunity to uniquely contribute to occupational well-being across U of U Health—all while complementing existing offices, programs, and resources.
Working in academic medicine is meaningful. However, it is also accompanied by a unique set of stressors and risks for stress injury, like experiencing secondary trauma or moral distress. The Resiliency Center offers a suite of support services designed to meet the emotional well-being and psychological health needs of U of U Health faculty and staff. The expert clinical team includes licensed mental health therapists who are specifically trained to work with health care professionals in individual and group settings.
The Resiliency Center works directly with teams in various ways that are tailored to their locus of control to enhance their local culture of well-being and reduce administrative burden and workplace inefficiencies. Well-being specialists are available to guide team improvement projects, facilitate conversations, and provide training sessions. The center also collaborates closely with groups like Organizational Development, the Office of Faculty, and Human Resources to ensure teams benefit from a comprehensive array of local expertise and resources.
A supportive work environment continuously identifies and addresses systemic factors that interfere with employee well-being. The center aims to improve organizational structures that cause undue strain on employees and build robust institutional support that strengthens U of U Health as an organization.


U of U Health was recognized as a Joy in Medicine silver status recipient in September 2025 by the American Medical Association at the American Conference of Physician Health in Boston. A recipient since 2021, the award, granted every two years, recognizes health systems actively reducing burnout and enhancing well-being among physicians in comprehensive, pragmatic, and evidence-based ways.
The Joy in Work initiative is rooted in the Institute for Healthcare Improvement’s Joy in Work Framework and supports employees, teams, and leaders in building resilient, thriving work environments. The program recognizes that well-being is foundational to delivering high-quality care and academic excellence, and it aims to foster meaningful work, strong teams, and sustainable systems. Through structured team-based improvement efforts, training programs, and consultation services, Joy in Work helps teams identify what brings meaning to their daily work and what gets in the way—empowering them to take action. In FY25, the program expanded its capacity-building activities, including team resilience consultations, a foundational course for all U of U Health roles, and a yearlong Joy in Work Facilitator Training Program. The facilitators showcased their Joy in Work projects at the Health Care Improvement and WellBeing Poster Fair in April 2025. These offerings equip staff and leaders with tools to strengthen purpose, prevent/reduce burnout, and increase engagement across the organization.
Joy in Work is also a cornerstone of U of U Health’s BetterU listening strategy. It helps teams use engagement data to understand local drivers of well-being and apply quality improvement methods to address them. This initiative directly advances professional fulfillment and a culture of collaboration across clinical, academic, and administrative domains.













Since its full rollout in November 2024, Code Lavender has become essential to U of U Health's commitment to team member well-being. The program provides a rapid, tiered response to support individuals and teams experiencing distress following adverse clinical and workplace events. Code Lavender directly addresses the emotional and psychological impact of working in a high-stakes health care environment by offering structured communication, resources, and psychological first aid.
Code Lavender’s value is demonstrated by its rapid adoption and growth. Its increased utilization reflects growing awareness and trust in the system as a reliable source of support. The program has also proved effective at mitigating acute distress. Data collected before and after debriefing sessions shows a marked reduction in self-reported distress levels among participants. This immediate relief is critical for preventing the long-term consequences of cumulative stress and trauma. The average time-to-debrief has also improved, ensuring support is delivered more rapidly than ever.
Code Lavender's success lies in its flexible, needs-based approach. The Resiliency Center offers a range of interventions tailored to the specific situation and individuals involved:
• Team support: Group debriefs are the most common intervention, providing a space for shared experience and collective processing.
Code Lavender
November 2024 – June 2025
100% increase in average number of monthly activations following the initial pilot phase
98 activations
388 individuals
Unexpected patient death, adverse clinical outcomes, staff death, and difficult interactions are the most common triggers for a Code Lavender.
• Individual support: For personalized support, we offer one-on-one coaching and connections to the Employee Assistance Program and Spiritual Care.
• Leadership resources: The program equips leaders with tools and coaching to effectively guide their teams through challenging events.
Underscoring its system-wide relevance, Code Lavender has reached a diverse range of clinical and non-clinical roles, including non-patient-facing teams, faculty groups, nurses, physicians, advanced practice providers, and respiratory therapists. Through continued training and outreach, the Resiliency Center is dedicated to embedding this vital service into the fabric of our culture, ensuring our team members have the support they need to thrive.

Healthcare Stories is an annual storytelling event that happens live and on stage at Kingsbury Hall. Produced by the Resiliency Center, the Center for Health Ethics, Arts, and Humanities, and UtahPresents, Healthcare Stories endeavors to foster community and connection through the act and art of sharing unscripted, care-themed stories.
The impact, for both the storytellers and the audience, is profound. Interestingly, many storytellers find themselves caught up in ripple effects that impact them long after the event concludes. One storyteller was personally uplifted when her participation led to the help she needed in caring for her brother with a rare disease. Another lent their professional expertise after being invited to lecture in a university business course. Still another was impacted on a cultural level when they were asked to provide a hospital tour to a group of international medical students.
The theme for Healthcare Stories in February 2025 was Joy. Six storytellers from across U of U Health shared tales of trial and triumph, including an emergency medicine nurse donating one of her kidneys to a stranger, a nutrition services leader creating personalized sketches for patients, and a pediatrician caring for his young daughter who has a developmental disorder. Over 400 people attended, and the event was indeed joyful. Looking to the future, we are working toward ensuring Healthcare Stories is an event that all community members can afford to attend. In this spirit, we are thrilled to announce that our theme for Healthcare Stories on March 5, 2026, is Together.

One of the things that makes the University of Utah such a special place is that different parts of the organization work together, bringing expertise and skills to accomplish big, impactful projects.
The College of Health has been a tremendous partner in OCIH’s disease prevention and health promotion efforts, particularly with the center’s Driving Out Diabetes-related work. OCIH’s research, clinical, and educational efforts rely heavily on faculty and staff from the College of Health for success. Programs such as the Wellness Bus, Food Pharmacy, Health Coaching, Culinary Medicine, Employee Wellness, and the Skaggs Wellness Center are all delivered in partnership with the college.
The Office of Faculty and the Office of Human Resources (on the main campus and within University Hospital and U of U Health) are critical to the success of programs, such as the Better U Well-Being and Engagement Survey, and in helping us understand how to enhance our services for employees. The Well U and WellnessNow programs are both run in partnership with the two human resources departments.
OCIH also wishes to acknowledge the Huntsman Mental Health Institute Behavioral Health Team for their partnership in supporting the Healthy Mind Track, available through WellU. We also thank University of Utah Hospitals and Clinics for working closely with us to ensure Code Lavender is available to those who need it. We also appreciate the Patient Experience and the Accerate Teams, who have provided a longstanding partnership to develop educational materials for health care professionals. Finally, we gratefully acknowledge our colleagues at Kingsbury Hall, UtahPresents, and the Center for Health Ethics, Arts, and Humanities for making Healthcare Stories a reality.










Amy Locke, MD, FAAFP, serves as the University of Utah’s chief wellness officer, leading the design and implementation of well-being programs to empower patients, faculty, staff, and learners to live healthy lives. She is a professor in the Department of Family & Preventive Medicine, co-director of the Driving Out Diabetes Initiative, and adjunct professor of nutrition and integrative physiology in the College of Health. She earned an MD and completed a residency in family medicine at the University of Michigan.
Megan Call, PhD, MS, is a licensed counseling psychologist, assistant clinical professor of psychiatry, and associate chief wellness officer for the U. Her research and clinical interests focus on promoting resilience and well-being among health care professionals through embracing vulnerability and discomfort, incorporating mindfulness into daily practice, improving team communication and relationship skills, and addressing systematic change. She earned a PhD in counseling psychology and a master’s in health promotion and education at the U.
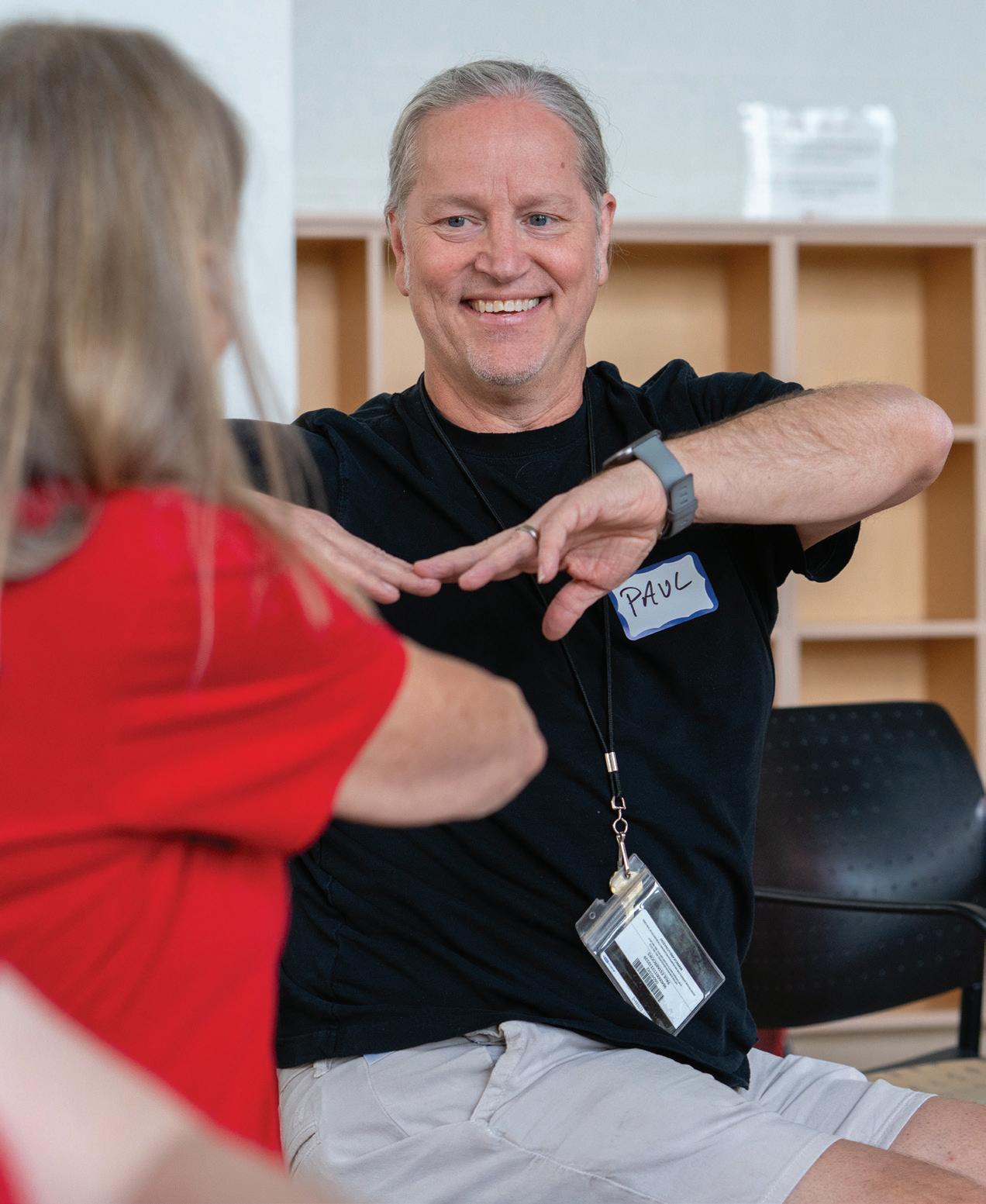
Paul Estabrooks, PhD, is the OCIH director of research, associate dean of community engagement in the College of Health, and co-director of the Driving Out Diabetes Initiative. A professor of health and kinesiology, he conducts participatory, translational research focusing on community-engaged dissemination and implementation (CEDI) science. He earned a PhD in kinesiology at the University of Western Ontario.
Justin Jackson, MS, is the director of whole-person health for the OCIH. Prior to this role, he led strategic development and implementation, business operations, and community health screenings and wellness programs in several settings across Utah. He is passionate about increasing access to health and wellness programs, especially for those in underrepresented and marginalized populations. He earned a master’s in health and human movement at Utah State University.
Selim Sheikh, DO, MBA, DipABLM, FAAFP, is the OCIH medical director. In this role, he facilitates collaboration between lifestyle and integrative programs and services to improve wellness and foster opportunities for discovery and advancement in clinical practice. Clinically, he specializes in osteopathic manipulative medicine, lifestyle medicine, integrative medicine, and family medicine. He earned a DO from William Carey University, an MBA from West Texas A&M University, and completed a family medicine residency at Ohio State University.
Traci Thompson, MS, ACSM HFD, CSCS, is the director of education for the OCIH and the director of the PEAK Health and Fitness Program. PEAK offers a variety of workshops and seminars, health assessment and fitness testing, nutrition services, continuing education opportunities, and employee fitness classes. Traci is an associate professor in the Department of Health & Kinesiology. She earned a master’s in health and exercise science at Colorado State.
Whitney Werner, MBA, MHA, is the OCIH director of administration. In this role, she leads department operations and finances, collaborating with the chief wellness officer to coordinate well-being efforts across the system. She earned an MBA and an MHA from the U.
The Osher Center’s work would not be possible without the efforts of our exceptional faculty, staff, and graduate assistants, who implement programs and services, design research interventions, and teach our students and trainees.
Resiliency Center (Workplace Well-Being)
• Mike Day, Operations Manager
• Betsy Holm, Program Manager
• Jamuna Jones, LCSW, Well-Being Specialist
• Jennifer Ellen Mueller, MSPH, CHES, Manager, Joy in Work
• Danielle Nives, LCSW, Program Manager
• Jake Van Epps, PhD, Associate Director
• Mindy Vanderloo, PhD, LCMHC, Research Associate
Central Administration
• Bethany Burtch, Marketing and Communications Manager
• Velda Michaelis, MHA, Executive Assistant
Whole-Person Health
• Vanessa Browning, MS, RDN, Dietitian
• Gracie Capps, Employee Wellness Navigator
• Michael Colvin, Mobile Health Driver
• Danielle Healis, MS, MCHES, Health Coach
• Alex Hernandez, MS, RDN, CD, Mobile Health Manager
• Maria Hernandez, Community Health Worker
• Teri Josephson, LMT, Lead Massage Therapist
• Ellen Maxfield, MSPH, CHES, Associate Director, Clinical Programs
• Megan Miller, Employee Wellness Manager
• Megan Monson, Administrative Manager
• Lucy Mower, MS, RDN, CD, Dietitian
• Emily Parrott, RYT, Administrative Assistant
• Christie Tuck, Community Health Worker
• Devin Vance, MFP, EP-C, Exercise Specialist
• Sofia Whitefields, MS, RD, Dietitian
• Sarah Zou, MPH, RDN, CDE, Dietitian

Ricker, M., Brooks, A.J., Chen, M., Weydert, J., Locke, A., Meehan, E.K., Cook, P., Lebensohn, P., & Maizes, V. (2024). The feasibility and impact of an asynchronous interprofessional well-being course on burnout in health care professionals. HCA Healthcare Journal of Medicine, 5(3), 343. DOI:10.36518/2689-0216.1778
Usset, T., Baker, L., Griffin, B., Harris, J., Shearer, R., Munson, J., Godzik, C., Torrey, W., Bardach, S., Mulley, A., Locke, A., Wright, H., Call, M., Sexton, B., Shanafelt, T., & Smith, A. (2024). Burnout and turnover risks for healthcare workers in the United States: downstream effects from moral injury exposure. Scientific Reports, 14(1), 24915. DOI:10.1038/s41598-024-74086-0
Delgado-Corcoran, C., Wawrzynski, S.E., Mansfield, K., Fuchs, E., Yeates, C., Flaherty, B.F., Harousseau, M., Cook, L., & Van Epps, J. (2024). Grieving children’s death in an intensive care unit: implementation of a standardized process. Journal of Palliative Medicine, 27(2), 236–240. DOI:10.1089/jpm.2023.0336
Abbey, B.M., Heelan, K.A., Bartee, R.T., George, K., Foster, N.L., Estabrooks, P., & Hill, J.L. (2024). Building healthy families: Outcomes of an adapted family healthy weight program among children in a rural mid-western community. Childhood Obesity, 20(7):468–475. DOI:10.1089/chi.2023.0142
Brito, F.A., Alves, T.F., Santos, N., Michaud, T.L., Eisenhauer, C., De Leon, E.B., Squarcini, C.F., Kachman, S., Almeida, F.A., & Estabrooks, P. (2024). Feasibility of a culturally adapted technology-delivered, familybased childhood obesity intervention for Latino/Hispanic families in rural Nebraska: The Hispanic Family Connections study protocol. BMJ Open, 14, 10. DOI:10.1136/bmjopen-2024-089186
Cedillo, M., Zepeda, J., Kiraly, B., Flynn, M., Elizalde, P.L., Zheutlin, E., Rudd, E.A., Kukhareva, P.V., Butler, J.M., Hess, R., Kawamoto, K., Estabrooks, P., & Conroy, M.B. (2024). Scalable and successful patient portal lifestyle coaching training for primary care clinical staff. Translational Behavioral Medicine, 14, 661–672. DOI:10.1093/tbm/ibae047
Harden, S.M., Galaviz, K.I., & Estabrooks, P. (2024). Expanding methods to address RE-AIM metrics in hybrid effectiveness-implementation studies. Implementation Science Communications, 5(1):123. DOI:10.1186/s43058-024-00646-0
Schumacher, L.M., Trilk, J.L., McNulty, L.K., Ylitalo, K.R., Eskuri, S., Brooks, J., Estabrooks, P., Jindal, M., & Stoutenberg, M. (2024; in press). Factors influencing patient enrollment in a community-based physical activity program after healthcare provider referral: A mixed methods study. Journal of Primary Care and Community Health, 15. DOI:10.1177/21501319241306710
Ansari, N., Wilson, R., Warner, E., Taylor-Swanson, L., Van Epps, J., Iacob, E., & Supiano, K. (2025). “We are not heroes”: Examining nurses’ experiences of moral distress during Covid-19. Teaching and Learning in Nursing, 20(2), e368–e375. DOI:10.1016/j.teln.2024.11.021
Kuo, P.B., Rudecindo, B., Drinane, J.M., Tao, K., Van Epps, J., & Imel, Z.E. (2025). Cultural conversations in therapy: How often clients talk about their identities. Psychiatric Services, 76(2), 133–138. DOI:10.1176/appi. ps.20230266
Ansari, N., Warner, E., Taylor-Swanson, L., Wilson, R., Van Epps, J., Iacob, E., & Supiano, K. (2025). Nurses navigating moral distress, resilience, and team dynamics: A literature review. Nursing Ethics, 32(5), 1343–1381. DOI:09697330241277992
Wu, V., Locke, A., & Rodríguez, J.E. (2025). In the journey, choose joy. Family Medicine, 57(2),75–76. DOI:10.22454/ FamMed.2025.378518
Locke, A., Rodgers, T.L., & Dobson, M.L. (2025). Moral distress as a critical driver of burnout in medicine. Global Advances in Integrative Medicine and Health, 14. DOI:10.1177/27536130251325462
Qeadan, F., Vanderloo, M.J., Call, M., Thornquist, R., Tingey, B., Morrow, E., & Locke, A. (2025). Association of communication, engagement, and well-being with turnover among faculty at a large academic health care and research system. Academic Medicine, 10, 1097. DOI:10.1097/ACM.000000000000
Vanderloo, M.J., Evans, E., Smith, A., Call, M., Locke, A., Wright, H., & Tao, K.W. (2025). Exploration of nurses’ experiences related to moral injury: a reflexive thematic analysis of nurse interviews. Journal of Advanced Nursing. DOI:10.1111/jan.16856
Stoutenberg, M., Estabrooks, P., Brooks, J.M., Jindal, M., Wichman, C., Rosemeyer, J., Schumacher, L.M., McNulty, L.K., Ewing, A., Eskuri, S., Bennett, F., & Trilk, J.L. (2025). Implementing and evaluating the comprehensive integration of physical activity into a major health system: Study design and protocol. BMJ Open DOI:10.1136/ bmjopen-2024-091556
Fiedler, D.V., Peters, D.H., Moore, L., Estabrooks, P., & Nigg, C.R. (2025). Successful implementation of evidencebased interventions: Factors to be considered. Translational Behavioral Medicine, 15(1). DOI:10.1093/tbm/ ibaf025
Thomas, J.V., Davy, D.M., Winett, R.A., Depner, C.M., Drummond, M.J., Estabrooks, P., Hardikar, S., Ou, Z., Shen, J., & Halliday, T.M. (2025). Timing of resistance exercise and cardiometabolic outcomes in adults with prediabetes: A secondary analysis. Journal of Applied Physiology. DOI:10.1152/japplphysiol.00507.2024
Estabrooks, P., Bolyard, M.L., Casucci, T., Christensen, J.T., Gibson, B., Golden, C.A., Hill, J.L., Horvath, L., Lee, S, Maxfield, E.M., McFarland, M.M., Merle, J.L., Michaud, T.L., Miller, M., Pereira, E.L., Schlechter, C.R., Simonsen, S.E., Wetter, D.W., & Locke, A. (2025). Identifying recruitment strategies to improve the reach of evidencebased health promotion, disease prevention, and disease self-management interventions: A scoping review. Frontiers of Public Health, 13. DOI:10.3389/fpubh.2025.1515042
Kim, J., Pacino, V., Koll, T., Mickles, M.S., Potter, J.F., Ma, J., & Estabrooks, P. (2025). Enhancing advance care planning in primary care: a three-year implementation study in Nebraska. Journal of American Geriatric Sociology, 73(8):2553–2561. DOI:10.1111/jgs.19478
von Oldenburg, N., Pick, N., Semin, J.N., Free, M., Ernst, W., Hill-Polerecky, D., Miller, K., Bhatt, V., Wildes, T., Estabrooks, P., Fisher, A., Jones, K., & Koll, T. (2025). Participation in life activities after hematopoietic cell transplantation in older adults. Supportive Care in Cancer, 33(5):393. DOI:10.1007/s00520-025-09399-5
Golden, C.A., Estabrooks, P., Heelan, K.A., Bartee, R.T., Porter, G.C., Pereira, E.L., Abbey, B.M., Michaud, T.L., & Hill, J.L. (2025). Developing an implementation fidelity measure for a family healthy weight program. International Journal of Behavioral Nutrition & Physical Activity, 22, 1–11. DOI:10.1186/s12966-025-01755-2
Locke, A. (2024, July). A unified listening strategy at the University of Utah. Workplace Change Collaborative Learning System, Monthly Action Call. Virtual.
Vukin, B., & Vukin, J. (Hosts). Behind the mask: Moral injury in healthcare (No. 31). In Real Talk with Kid Docs Apple Podcasts. https://podcasts.apple.com/us/podcast/episode-31-behind-the-mask-moral-injury-inhealthcare/id1730120837?i=1000666830597
Linnan, L., Locke, A., Nobrega, S., & Ozminkowski, R. (2024, October). The latest science informing best practices. Plenary Session. Health Enhancement Research Organization (HERO) Forum 24, Baltimore, MD.
Locke, A. (2024, October). Behavioral wellness in providers: Increasing resiliency to reduce provider burnout. Presentation. 9th Annual Utah Primary Care Summit, “Elevating Health: Bridging Primary Care and Behavioral Wellness in Utah,” Salt Lake City, UT.
Van Epps, J. (2024, November 20). Grief in healthcare. Presentation. Schwartz Round, Huntsman Cancer Hospital, Salt Lake City, UT.
Locke, A. (2025, February). Joy in work: Moving from surviving to thriving in medicine. Presentation. Utah Academy of Family Physicians Ski and CME, Park City, UT.
Locke, A. (2025, February). Creating belonging and connection: University of Utah Health Resiliency Center. Presentation. Utah Business of Health, “Good Health is Good Business” (sponsored by Get Healthy Utah, The Utah Worksite Wellness Council, and Utah Community Builders), Draper, UT.
Locke, A. (2025, February). Thriving in academics: A pragmatic approach to the messy work of finding a fulfilling path. Plenary Session. Women’s Leadership Day, “Resilient Leadership: Building Emotional Strength and Managing Stress,” University of Utah, Salt Lake City, UT.
Jones, J., & Van Epps, J. (2025, February). Well-being equity for healthcare professionals. Presentation. University of California, San Francisco Psychiatry Grand Rounds, San Francisco, CA.
Ricker, M., Kligler, B., Kreitzer, M., Locke, A., Maizes, V., & Mascarenhas, M. (2025, March). Leadership for advancing whole health: Cultivating purpose, skills, and impact. Pre-Conference Workshop. International Congress on Integrative Medicine and Health, Academic Consortium for Integrative Medicine and Health, Seattle, WA.
Brazeau, C., Hommema, L., Locke, A., & Abraham, J. (2025, March). Accelerator Lightning Round Panel. Action Collaborative on Clinician Well-Being and Resilience, 2nd Annual Health Workforce Well-Being Day. National Academy of Medicine, Washington, DC.
Dent, R., Erickson, W., Locke, A., Roux, A., Rushton, C., & Feist, C. (2025, April). Solutions: What’s been done? What direction do we take next? Rebuilding health workers’ trust in healthcare organizations. Panel. Health Workforce Equity Summit, George Washington University, Washington, DC.