





• Understanding Mast Cells
• Mast Cell Activation Syndrome Defined
• Symptoms and Conditions Caused By MCAS
• Underlying Causes of MCAS
• Pinpointing and Diagnosing MCAS
» Typical Clinical Signs
» Biochemical Markers
» Symptom Improvement
• MCAS Treatment: X Steps To Stabilizing Your Mast Cells
» Identify and Address Any Hidden Underlying Infections
» Address Exposure To Toxins, Mold, and Other Potential Triggers
» Soothe Stress and Prioritize Nervous System Regulation
» Focus On Nutrient Intake and Reducing Histamine
» Take Steps To Heal Your Gut and Rebalance Your Microbiome
» Follow A Strategic Supplement Protocol
» Consider Mast Cell Stabilizing Medications
• Work With A Functional Medicine Doctor
• You’ve Got This!


Mast cells are highly evolved, highly advanced, and indispensable components of your immune system. You see, these tiny immune cells are designed to serve as your immune system’s “front line soldiers” – standing guard and vigilantly watching for any potential threats. When a threat is detected, your mast cells spring into action and undergo degranulation – a process in which they rapidly release a medley of inflammation-stoking signaling molecules.
In a healthy balanced immune system, your mast cells are designed to work via a process that goes something like this:
• Your mast cells detect a threat and degranulate – releasing a cocktail of signaling molecules
• These molecules spread throughout your body and activate your immune system – revving up inflammation and preparing your body to launch an attack against the foreign invader
• Your immune system identifies, neutralizes, and eliminates the threat
• Your immune system recognizes that the threat has been neutralized and begins returning to homeostasis – down-regulating inflammation and sending your immune cells back into “standby” mode
But sometimes, this delicate balance can get thrown off-kilter and cause your mast cells to essentially get stuck in the “on” position – leading to what’s known as mast cell activation syndrome.


Mast cell activation syndrome or MCAS forms part of a spectrum of mast cell-related disorders. Mast cell activation syndrome is characterized by abnormal and excessive mast cell “activation” or degranulation. It’s officially defined by the following criteria:
• Symptoms of Mast Cell Activation: People with MCAS experience symptoms caused by their mast cells degranulating. Symptoms can wax and wane in response to certain triggers, or sometimes with no identifiable trigger.
• Symptoms Affect Multiple Parts of the Body: MCAS symptoms aren’t just limited to one area – they can affect different organs or systems in the body.
• Ruling Out Other Conditions: Doctors need to make sure that the symptoms aren’t caused by another health problem that could explain them better. This involves a careful process of eliminating other possible diagnoses.
So what exactly does that mean?
Well, normally your mast cells are great at detecting and dealing with threats – releasing their alarm-sounding substances only when there is a real threat. But sometimes, these vigilant guardian cells can get a little bit too enthusiastic and begin releasing their defense arsenal even when there’s no real danger.
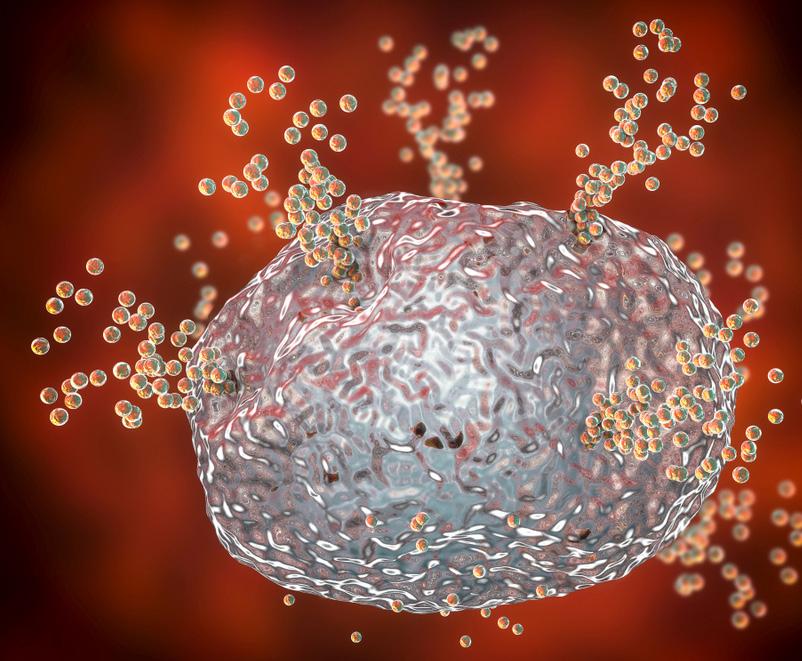
That’s mast cell activation syndrome or MCAS – when your mast cells get trigger-happy and begin hitting the alarm way too often. In MCAS you have a normal, healthy amount of mast cells patrolling your body. But these mast cells become hypervigilant –reacting rapidly and aggressively to anything that even resembles a potential threat. These overzealous mast cells spew out their inflammation-stoking contents much too often and much too aggressively – sending your immune system into high alert unnecessarily.
And what makes MCAS so tricky, is that these hypervigilant mast cells can create a whole slew of hard-to-pinpoint symptoms that can be all over the map.


The effects of MCAS can extend to every single nook and cranny of your body. Let’s break down some of the symptoms of overactive mast cells by body system:
Skin-related symptoms:
• Flushing
• Hives
• Itching
• Rashes
• Swelling
Respiratory-related symptoms:
Gastrointestinal-related symptoms:
• Abdominal cramping
• Bloating
• Diarrhea
• Nausea
• Vomiting
• Asthma-like symptoms
• Cough
• Increased mucus production
• Rhinitis
• Shortness of breath
• Sinusitis
• Wheezing


Cardiovascular-related symptoms:
• Low blood pressure
• Passing out
• Rapid pulse
• Vascular permeability (inflammation and swelling)
Brain-related symptoms:
• Anxiety
• Brain fog
• Difficulty concentrating
• Headaches
• Neuropathic pain
• Psychiatric symptoms
• Sleeplessness
• Vertigo
But the symptoms don’t end there. If left unchecked, these overactive mast cells can play a key role in sparking the early stages of many diseases. Just some of the conditions that have been identified as being associated with MCAS include:
• Allergies
• Asthma
• Atherosclerosis
• Autism
• Autoimmune diseases (Hashimoto’s thyroiditis, systemic lupus, multiple sclerosis, bullous pemphigoid, rheumatoid arthritis)
• Eczema
• Ehlers-Danlos syndrome
• Celiac disease
• Chronic fatigue syndrome
• Chronic inflammatory response syndrome (CIRS)
• Eosinophilic esophagitis
• Fibromyalgia
• Gastroesophageal reflux
• Infertility (mast cells in the endometrium may contribute to endometriosis)
• Interstitial cystitis
• Irritable bowel syndrome
• Migraine headaches
• Mood disorders: anxiety, depression, psychosis, and sleep disorders
• Multiple chemical sensitivities
• Postural orthostatic tachycardia syndrome (POTS)
This is just the tip of the iceberg when it comes to the damage that misbehaving mast cells can cause if left unchecked. With such serious consequences, you’re probably wondering what can trigger your mast cells to become overactive in the first place.
MCAS is often triggered when your immune system becomes overloaded. This immune system burnout can push your mast cells out of equilibrium – sending them into a sort of tailspin of hypersensitivity. Some of the more common underlying causes include elevated or prolonged exposure to:
• Allergens
• Chemicals
• Heavy metals
• Hidden infections
• Mold
• Stress
• Toxins
• Viruses
So how do you go about identifying whether or not malfunctioning mast cells are to blame for your health concerns?


Diagnosing MCAS can be tricky because symptoms often include a vague and broad constellation of varying symptoms. And unfortunately, many conventional medical doctors have little to no understanding of mast cell-derived conditions. For that reason, it is crucial to work with a practitioner who takes a Functional Medicine approach and has a thorough understanding of the true implications of overactive mast cells.
Diagnosing MCAS typically requires some detective work and may look a little different for everyone. However, there are a few official criteria that can be used to pinpoint and diagnose MCAS. These diagnostic criteria include:

Your doctor will look for clinical signs that indicate the presence of severe, recurrent episodes of systemic mast cell activation. Systemic is defined as including a minimum of two distinct organ systems and may include things like:
• Abdominal cramping
• Angioedema (swelling of the deeper layers of the skin, caused by a build-up of fluid)
• Diarrhea
• Flushing
• Headache
• Hoarseness
• Hypotensive syncope (fainting or loss of consciousness caused by a sudden drop in blood pressure) this can also present as POTS/dysautonomia syndrome


• Nasal congestion
• Pruritus (itching which can occur on the skin, mucous membranes, or internally)
• Tachycardia (an abnormally rapid heart rate)
• Throat swelling
• Urticaria (hives)
• Wheezing
Your practitioner will look for an increase in mast cell-derived biochemical markers that can include:
• Histamine
• Histamine metabolites
• PGD2 metabolites
• Heparin
• Tryptase
Your doctor may also administer certain drug therapies to evaluate whether or not your symptoms improve. These medications may include:
• Mast cell-stabilizing agents
• Drugs directed against mast cell mediator production
• Drugs blocking mediator release or effects of mast cell-derived mediators
Again, diagnosing MCAS isn’t always entirely straightforward. Because overactive mast cells have a domino effect that can create a myriad of underlying changes and difficult-to-pinpoint symptoms, it can sometimes require a little detective work to get to the root of the issue. But once hypervigilant mast cells are indeed identified as the underlying culprit, it’s time to get to work on stabilizing these malfunctioning cells.



Addressing mast cell activation syndrome requires a big-picture approach that helps your mast cells stabilize and return to a calm, balanced state. While treatment and healing will look a little different for everyone, some foundational aspects that are crucial to evaluate and confront include the following:
Hidden infections like Lyme disease, Babesia, Bartonella, Eppstein Barr, or even COVID-19 can put your mast cells into hyper-drive and contribute to MCAS. You see, underlying infections can not only act as a trigger for mast cell activation syndrome flare-ups, but they can also be an underlying cause. That’s because some pathogens can remain dormant in your body – evading detection by your immune system and causing low-level inflammation. As these pathogens hide out, your body senses the hidden threat and continues to produce pro-inflammatory signaling molecules. Over time, this can overwhelm and burn out your immune system.
And ultimately, this dysfunction of your immune response can result in the malfunction and hyper-reaction of your mast cells – thus triggering the flares of hyper-inflammation seen in mast cell activation syndrome. So it’s imperative to identify and address any dormant pathogens that might be lurking in your body and provoking your mast cells into overproduction mode.
Hidden infections aren’t the only things that can cause your immune system to essentially get stuck in the “on” position. Elevated exposure to environmental toxins can exceed your body’s ability to detox – allowing these toxins to accumulate and damage your immune system. This is especially problematic in today’s toxin-laden world because exposure to a concentrated dose of environmental toxins or chronic low-level exposure to these toxic compounds can spark a process known as toxicant-induced loss of tolerance or TILT.


As your immune system is exposed to these disruptive toxins, its tolerance steadily decreases until a tipping point is reached – throwing your mast cells so off-kilter that they begin malfunctioning. Some of the most problematic environmental toxins include:
• Toxic mold: Toxic mold can grow inconspicuously in many homes and buildings –exposing you to unhealthy levels of these stealthy fungi and their microscopic poisons known as mycotoxins. If you’re dealing with overactive mast cells, it’s critical to remove yourself from potential mold exposure, immediately begin mold remediation and clean up, and begin detoxing. You can learn more about how to address toxic mold in my guide: Your Complete Mold Exposure Guide.
• Health-disrupting chemicals: Thanks to loopholes in policies and lax regulations, there is little oversight to prevent the influx of countless health-disrupting chemicals from flowing into our world. It’s easy to see how industrial processes and agricultural practices can flood our world with these chemicals, but they are by no means the only way you can be exposed. Unfortunately, many conventional products – like our cleaning products, personal care products, and even our furniture can be chock-full of chemicals that pollute our homes and bodies. So it’s important to minimize your exposure to these toxins when trying to help your mast cells find a sense of equilibrium.
Once you address potential mold exposure and minimize your exposure to environmental toxins, it can sometimes be helpful to incorporate some detox-boosting strategies to help your body eliminate any toxins that may have accumulated. This might include things like infrared sauna therapy, dry brushing, or even a supplement stack (we’ll dive deeper into supplements in another section).



Studies have found that stress levels can have a monumental impact on both the development and management of mast-cell-mediated conditions. Your mast cells are an integral part of your defense system – so there are mast cells essentially standing guard at each of your nerve endings. This creates a continuous feedback loop between your mast cells and your neurotransmitters – meaning your emotional state directly communicates and influences your mast cells.
This complex interplay means your nervous system, emotional state, stress levels, and recurrent thoughts can have a massive impact on your immune system and mast cell degranulation. So an important component of treating MCAS is soothing these stressed-out mast cells and helping them return to a balanced state. That means not only minimizing stressors and finding healthy ways to cope with unavoidable stress but also taking steps to re-regulate your nervous system while addressing any compounded trauma. Some powerful ways you can begin rewiring and restoring balance to your nervous system include:
• Primal Trust
• Gupta Program Brain Retraining
• Dynamic Neural Retraining System (DRNS)
• Breathwork (like Buteyko breathing)
• Cranial sacral therapy
• Emotional freedom technique or “tapping”
• Frequency-specific microcurrents
• Integrative manual physical therapy
• Listening to binaural beats
• Medical hypnosis
• Neurolinguistic programming
• Neurofeedback
• Practice getting into a state of flow
Addressing stress and nervous system dysregulation is an often-overlooked component of healing MCAS and can be the missing puzzle piece when it comes to stabilizing these overzealous cells.


The food you eat can be a powerful tool in healing. The nutrients you consume can either contribute to inflammation or combat it. So when healing MCAS, it’s important to prioritize nutrient-dense, anti-inflammatory foods while minimizing foods that contribute to inflammation. That means building most of your meals around fresh, nutrient-dense foods that are as close to their natural form as possible – things like fresh fruits and veggies, high-quality proteins, healthy fats, and filling starches. And it means minimizing inflammatory foods like processed sugar, refined oil, and most pre-packaged foods.

But in addition to following an anti-inflammatory diet, it can sometimes be useful to also implement what’s known as a low-histamine diet. You see, when mast cells degranulate, they release a medley of molecules – one of which is known as histamine. Histamine is not only produced by our bodies but is also present in many foods. This means mast cell activation syndrome can make you highly reactive to a wide variety of food.
Here’s a list of the top high-histamine foods you might want to avoid:
• Fermented dairy products, such as cheese, kefir, yogurt, buttermilk, and cream cheese
• Fermented vegetables, such as kimchi, sauerkraut, and pickled vegetables
• Fermented soy products and some legumes, such as soybeans, red beans, green peas, sugar snap peas, and sweet peas
• Some fruits, including all citrus, berry, and stone fruits, along with bananas, grapes, pineapples, and over-ripe fruits
• Some vegetables, including avocados, eggplant, spinach, white and sweet potatoes, tomatoes, and over-ripe vegetables
• All shellfish, canned fish, cured meats, and pickled meats, eggs, and fish
• Walnuts and pecans


• All processed oils with preservatives BHA and BHT
• Some herbs and spices, such as cinnamon, clove, anise, curry, cayenne, and nutmeg
• Processed sweeteners and sugar products, chocolate, cocoa, and unpasteurized honey
• Products made with yeast and yeast extracts
• Bleached flour
• All alcohol, teas, fruit drinks, carbonated drinks, and nonalcoholic beers and wines
• All kinds of vinegar, ketchup, and mustard (with vinegar), and relish
• All artificial preservatives and food dyes
You likely won’t have to avoid these foods forever. But it can be useful to eliminate them for a period of time while your mast cells are healing and then slowly add them back in to see how your body reacts.
The health of your gut and the composition of your gut microbiome play an intricate role in your immune system thanks to a channel known as the gut-immune axis. This bidirectional communication network allows your gut to directly communicate with and influence your immune system and vice versa. Pair that with the fact that a large percentage of your immune cells are housed within your digestive tract in what’s known as gut-associated lymphoid tissue and it’s easy to see how poor gut health can lead to an off-kilter immune system – and you guessed it, hypersensitive mast cells.
So ensuring your gut is happy, healthy, and balanced is a key piece of the puzzle when it comes to calming hyperactive mast cells. Some ways to support the health of your gut include:
• Reintroducing a variety of beneficial gut microbes to support a diverse and flourishing microbiome. I recommend pairing Probiotic Daily Essentials with my Spore Probiotic Complete.


• Give your gut the nutrients it needs to build a strong gut barrier so it can keep pathogens, toxins, and wastes sealed up tight in your intestines where they can be properly excreted. To give your gut a concentrated dose of gut barrierboosting nutrients I recommend Gut Shield, Gut Immune, and Collagen Boost.
• Eat a well-rounded, healthy diet full of microbiome-supporting foods. Eating plenty of quality protein and healthy fats paired with slow-digesting carbs will help fuel beneficial bacteria while starving out harmful bacteria. It’s also helpful to opt for organic foods whenever possible to avoid ingesting microbiomedisrupting pesticides and chemicals.
Bolstering your gut barrier, balancing your microbiome, and optimizing the overall health of your gut is a pivotal piece of the puzzle when treating MCAS.
Incorporating a strategic supplement stack can be a game-changer when it comes to helping your mast cells return to baseline. While supplement regimens should be personalized based on your unique body and imbalances, there are some key supplements that can be useful to nearly everyone grappling with MCAS. These include:
• Dr. Jill’s MCAS Bundle - MCAS treatment involves identifying and avoiding triggers that exacerbate symptoms and here is what I recommend to help support and stabilize mast cells to manage symptoms. The MCAS Bundle is a great place to start and contains the most effective products to stabilize your mast cell symptoms, including Hist Assist, Buffered C, and Histamine Blocker

• Diamine oxidase (DAO): This little enzyme is responsible for breaking down histamine – one of the primary and most problematic molecules released by overactive mast cells. Histamine Blocker contains a concentrated dose of DAO to help your body degrade and eliminate excess histamine.
• Mast cell stabilizers: Some supplements proven to soothe mast cells include Hist Assist, Quercenase, ResveraMax, or Omega Curcumin.


• Micronutrients: Ongoing inflammation can deplete your stores of vital nutrients –creating a vicious cycle that further feeds the inflammatory process. You can help address any nutrient deficiencies by adding in things like Mineral Essentials and
• MitoVite.Detox-enhancers: Certain supplements can amplify your natural detoxification pathways. Some of the most potent detox-boosting supplements include Liver Essentials which supports liver health (your primary detox organ), Glutathione which maximizes glutathione levels (the master detoxing antioxidant), and ZeoBind which serves as a detox binder to trap free-floating toxins. You can find all of these detox-enhancing supplements in my Detox Bundle.
In some cases, it may make sense to incorporate some medications to help get your runaway mast cells under control while making the crucial lifestyle adjustments. Some of the treatment options that may be useful in pumping the brakes on inflammation include:
• Steroids (short-term use, ideally)
• Non-steroidal anti-inflammatory drugs
• Immunomodulatory drugs
• Benzodiazepines
• Cromolyn
• Pentosan
• Alpha interferon
• Tyrosine kinase inhibitors
• Ketotifen
• Omalizumab
• Quercetin
• H1 and H2 receptor blockers
• Leukotriene antagonists
• Bisphosphonates
Another medication that has shown some promise when it comes to stabilizing mast cells is the use of what’s known as low-dose naltrexone. Naltrexone, a drug that was originally approved to help prevent narcotics and alcoholics from relapsing is what’s known as an opiate antagonist – meaning it binds to your opiate and endorphin receptors. Taking low doses of naltrexone can essentially trick your body into producing more endorphins – the “feel good” chemical that is released during exercise. The influx of these natural endorphins stimulates your immune system and can help restore a more normal balance while pumping the brakes on overall inflammation.
The use of low-dose naltrexone or any of the above-listed medications should be prescribed and overseen by an experienced doctor with an in-depth understanding of how these drugs fit into the equation when treating MCAS. Which leads us to our next and most important point.



Treating MCAS can be tricky and often requires a significant level of personalization as well as some trial-and-error to figure out what works best for you. So if you’ve been diagnosed with MCAS or suspect you may be struggling with symptoms of MCAS, I cannot overemphasize the importance of working with an experienced Integrative and Functional Medicine Practitioner.
Unfortunately, many conventional medical doctors have a poor or nonexistent understanding of the complexities of MCAS. So it’s crucial to partner with a practitioner who will help you get to the root cause of your symptoms and help create a comprehensive and customized plan for helping you heal. If you are new to the idea of Functional Medicine and aren’t sure how to go about finding a doctor that’s a good fit for you, I highly encourage you to head over and read my article How to Choose a Good Integrative and Functional Medicine Doctor.
I walk you through what to look for, some red flags to avoid, and give you some excellent resources to help you find top-notch Functional Medicine Doctors in your area.
I hope this guide is helpful for you! Remember, healing can take time, patience, and some effort. Embarking on a journey of healing after identifying MCAS can be daunting, but you are not alone and you are not at the mercy of this diagnosis.
Making lifestyle changes can be a challenge, but I promise it is so worth it. If you implement one step at a time, give yourself lots of grace, and reach out for support so you’re not on this journey alone, I know you can do it!

