




Eric Barna MD
Director of Education, Division of Hospital Medicine


Start Time
Begin rounds no later than 9:00 AM on the teaching service, though coming in early will help with streamlining tasks and remaining efficient.
Finish Time After completing rounds with all patients, resident/NP teams, and conducting afternoon huddle with your respective teams.
Remain accessible via Epic Secure Chat and/or telephone until at least 5:00 PM, though standard practice is to be available into evening hours especially for trainee support.
For urgent issues arising after your departure, the night team can be looped into communication. Your responsiveness ensures continuity of care during weekend coverage.
❑ Lead hospitalist divides all service patients across weekend on-call physicians
❑ "Weekend divvy" email sent Friday afternoon outlining patient assignments
❑ You'll typically cover a teaching service + secondary service (heme malignancy and likely other ADS patients)
If You Don't Receive the Patient Assignment
1. Message the "Weekend Divvy Doc" (found on AMION)
2. Contact Lead Hospitalist for the day
3. If unreachable, message Eric Barna or Vinh Nguyen

The DHM AMION landing page: Hospitalists/ADS Medicine NP-MSH

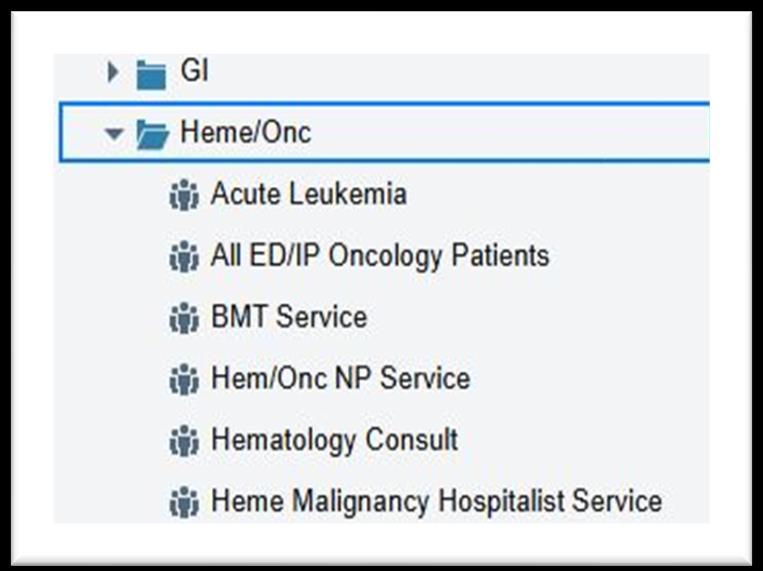
Heme Malignancy Patients
Unlike most other patient teams, the HMHS lives in the oncology folder.
MSH Provider Teams →
Heme/Onc folder → Heme
Malignancy Hospitalist service
ADS Patients
Check AMION to identify team folder (GP ADS, KCCC5-ADS, ED-ADS, KP-ADS).
MSH Provider Teams—>
Medicine—> Locate the team folder you identified above
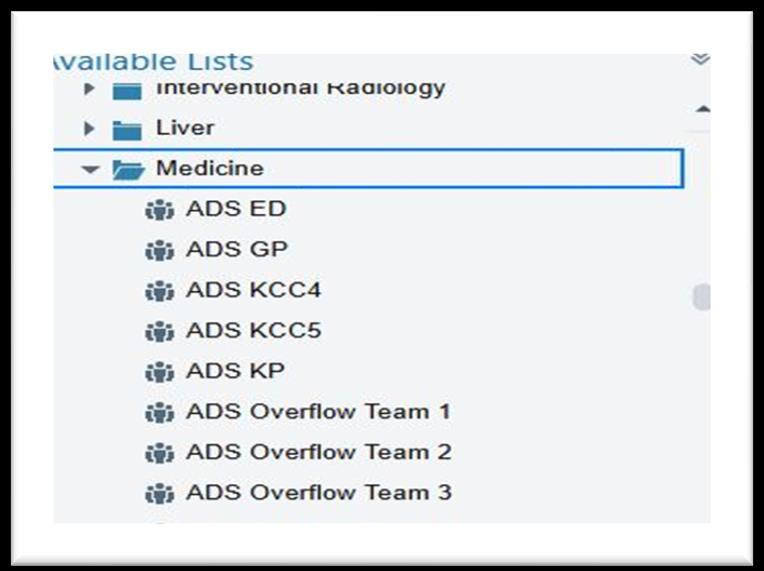
Add all patients to your personal Epic list for ease of tracking.

ADS patient names should be communicated directly by the Friday Attending via Epic Secure Chat or email by 5:00 PM. If you haven't received this information, proactively reach out to ensure complete patient coverage.
Your Weekend "New" Admissions:
❑ New admissions to your core service lines (teaching, heme malignancy etc.)
❑ Assigned ADS admissions for each weekend day
Finding New Patients:
❑ Teaching patients: Under your respective teaching teams
❑ Heme Malignancy: In the HMHS folder
❑ ADS patients: The weekend lead hospitalist will send an Epic Secure Chat listing new ADS assignments
Note: ADS patients have already been "admitted" with activated orders, but you'll be assuming care and modifying plans as needed.

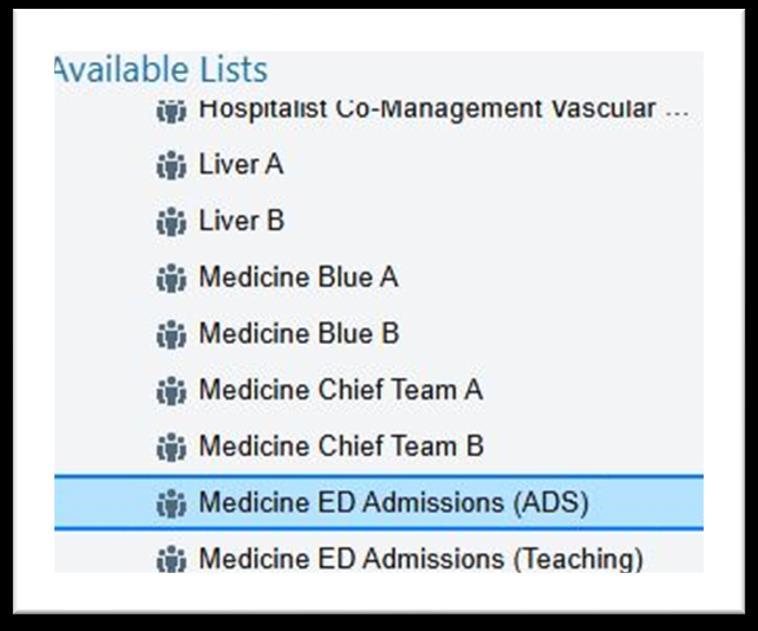
Key Tip for Finding ADS Admits: Find these patients in Epic under MSH Provider teams → Medicine → Medicine ED admissions folder. Sort the list by Attending to see patients assigned to you, then drag them to your personal folder.

Navigate to Signout Medicine→
→ Epic Handoff
Review "Weekend to do" section for your core tasks.
Update all patient signouts with "weekend events" section with key events from the weekend and follow up items for the coming week.
Create comprehensive signouts for new arrivals
Include brief clinical history, disposition items, barriers, and to-do list. Please do not cut and paste your H&P from your note into the signout. The summative clinical paragraph should be short and targeted.

Key Tip: In order to view "hospitalist" signout elements, you must change your handoff context in the right upper corner to MSH Hospitalist

Patient Type Daytime Handoff
ADS Patients Handoff to frontline NP covering the patient (on call until 7 PM)
Night Hospitalist Coverage
If more critical follow up is needed by a night attending: Email #DHMnightteam and message swing shift nocturnist (begins 5 PM) and who can be located on AMION.
Heme Malignancy
Same as ADS but with HMHS NPs
Teaching Patients Residents carry handoff
Same as ADS night coverage
Same as above



Organize patient lists in advance Template note drafts for efficiency

Assign yourself as Attending of record for all patients on your lists (even if day teams should have future-assigned you)
• Must write daily progress note (NPs cannot write billable notes)
• Required to write your discharge summaries independently and sign them. These can count as the daily progress note for the day.
• NPs write notes that you can modify and take ownership of with your key elements
• Add your own exam, assessment and plan adjustments
• Oncology NP can draft discharge summary for your co-signature
• Attestation of intern/acting intern notes with robust additions
• Include clinical evaluation, exam, and care direction
• Co-sign resident discharge summaries
On co-management service patients a full progress note is required but all other notes are the responsibility of the primary team.

Critical Documentation Note: Avoid isolated nonspecific generic statements like "patient seen and examined and agree with plan of care." Your documentation must demonstrate your independent assessment and medical decision-making.
All patients require attending documentation for billing and legal purposes every day. For teaching patients admitted later in the day, you can review the plan with residents and provide guidance, with the H&P signed within 24 hours of arrival.
❑ Serve as FLP's
❑ Primary focus: discharge coordination
❑ Place discharge orders and prescribe medications
❑ Can handle simple consults and routine orders
❑ Do not complete discharge summaries
❑ Serve as FLP's
❑ More comprehensive care involvement
❑ Can call consultants, order imaging/testing
❑ Complete discharges including discharge summaries

Please be sure to schedule mandatory huddles with your NP’s
Morning huddle ~ 8 or 9 am
Afternoon huddle ~ 3pm

❑ You have discretion to upgrade patients to the teaching service
❑ Consider care intensity, interventions, and anticipated decompensation
Notification process:
Alert MCR and your NP + Floor RN
Provide direct handoff to accepting team
Remain primary until team assigned
Ensure patient transfer from your list

Accurate documentation ensures proper reimbursement for services rendered and provides legal protection for you and the hospital.

Different E/M codes apply to initial admissions, follow-up visits, discharges, and observation care. Coding queries will be routed to you via the iodine/Interact app.

Avoid not documenting complexity, omitting time, or missing key details like consultant discussions, social determinants, or risk factors that justify higher codes.

The core of billing is the Evaluation & Management (E/M) code, reflecting the complexity of the patient encounter and documented decision-making.

History, physical exam, and most critically, medical decision-making. Time spent can also be a billing factor, especially for prolonged care.

As attendings, you are the billing provider. Your attestation must reflect your direct involvement and independent medical decision-making, even if residents document.
❑ Start rounds no later than 9 am
❑ Focus on clinical care alignment
❑ Provide focused and clinically relevant teaching
❑ Remain available until at least 5pm (typically into the evening)
❑ Support resident teams with new admits
If you need any support during the weekend:
1. Contact the lead hospitalist
2. If unavailable reach out to: Eric Barna or Vinh Nguyen


So… while weekends may be short, your impact is long!
Thank you in advance for your dedication to our service…