20 minute read
Factors that influence the risk of post-operative delirium in general anaesthesia patients
Factors that influence the risk of post-operative delirium in general anaesthesia patients
Rosalie Gibbs
Northmead Creative and Performing Arts High School
Abstract
Postoperative Delirium (POD) is a complex and unexplored condition that often occurs after general anaesthesia. Not promptly diagnosed and treated can lead to permanent neurological impairment. This study aimed to understand factors such as age, sex, baseline cognitive dysfunction and history of health issues at increasing POD risk in general anaesthetic patients and optimise prevention strategies and treatment plans. Results showed a strong correlation between older age, maleness, and preoperative cognitive dysfunction, increasing the risk and severity of POD. These findings influenced effective treatment methods such as the CAM-ICU assessment, and the alternate hypothesis was accepted, indicating that these factors significantly influence the risk of POD in general anaesthesia patients.
Literature review
General Anaesthesia:
Throughout medical history, general anaesthetics have been used to ease the pain and suffering of surgical patients by inducing a state of controlled unconsciousness. 1 Surgery used to be a painful and brutal procedure, but it is now recognised as a routine and essential aspect of modern medicine. Coined in 1846 by Oliver Wendell Holmes, the term “anaesthesia” describes the drug-induced insensibility to sensation, particularly pain. 2 Yet, how anaesthetics suppress human consciousness has been a mystery since Holmes’s original demonstration, as they do not simply suspend all brain functions while receiving anaesthesia. General anaesthesia produces widespread neuro-depression in the central nervous system by enhancing inhibitor neurotransmission (e.g. GABAa) and reducing excitatory neurotransmission (e.g. Epinephrine). 3 Thereby changing oscillation patterns, stopping neurons from firing throughout the brain, causing complete unconsciousness, and preventing a patient from feeling pain. There are many risks and complications when having a general anaesthetic, such as infection, nerve damage, breathing problems, organ failure, etc. This report will investigate one of the risks: postoperative delirium (POD).
1 Robinson, H Daniel and Toledo, H Alexander, “Historical Development of Modern Anaesthesia”, 2012
2 Britannica, The Editors of Encyclopaedia, “Oliver Wendell Holmes”, 2022
3 Son, Yong, “Molecular Mechanisms of General Anaesthesia”, 2010
Post-Operative Delirium:
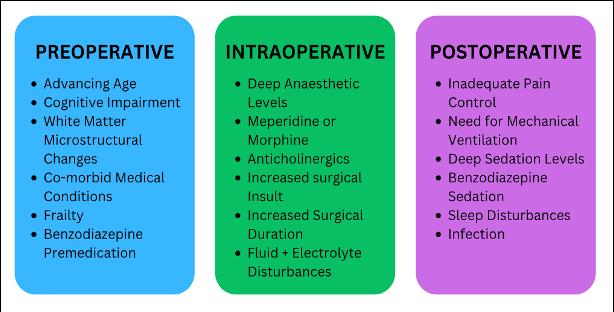
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), POD is recognised as a disturbance of consciousness, such as a reduced ability to focus, sustain or shift attention, and a change in cognition. 4 POD can occur between 10 minutes after general anaesthesia and until discharge from the hospital. Several pre-operative, intraoperative and post-operative factors contribute to POD, such as older age, previous drug use, alcohol use, dementia or previous delirium, persistent effects of drugs, metabolic abnormalities, hypoxia, electrolyte imbalance, and infection. The various types of POD factors can be seen referring to Figure 1. Depending on the patient demographic, the standard of medical treatment, present risk factors or comorbidities, and the operating stress level, the incidence ranges from 9% to 87%. 5 In addition, there are three types of POD: hyperactive, hypoactive and mixed.
Hyperactive POD patients experience agitation, irritation and restlessness. Hypoactive patients experience lethargy, unawareness and diminished motor activity. The mixed subtype of POD makes patients experience hyperactive and hypoactive delirium traits. Despite being the most common type, hypoactive POD patients have a poorer prognosis than those with hyperactive POD, which is less frequently diagnosed. 6

Aetiology:
According to the Cambridge Dictionary, aetiology refers to the study of the causes of a disease. 7 Due to the complexity of POD, the aetiology is still being discovered and not fully understood. However, various hypotheses explain this phenomenon, such as Acute Central Cholinergic Deficiency (ACCD) being one of the most widely accepted explanatory theories. ACCD occurs when decreased GABBA-ergipc activity, abnormalities in melatonin and serotonin pathways, noradrenergic hyperactivity (limbic and cortical arousal), inflammation with increased release of Interleukin-1 and Interleukin-6 (inflammatory and immuneamplifying stimulants) leading to neuronal damage, and cerebral hypoperfusion (reduced amount of blood flow) and other possible pathogenic mechanisms. 8 Although this theory is widely accepted, many scientists cannot concisely prove this hypothesis, as the influence of various factors and comorbidities on the prevalence and incidence of POD is unknown. Thus, the need for this research report.
Economic Implications:
Furthermore, the financial costs of POD are substantial. Delirium is associated with increased days of mechanical ventilation and ICU length of stay, increased hospital length, and patients’ functional decline. In a study of the economic impact of delirium in Australia, there were an estimated 132,595 occurrences of delirium in 2016-2017, with more than 900 deaths attributed in that time. Furthermore, the total costs of POD in Australia are estimated to be $A8.8 billion, ranging between $A5.3 to $A12.1 billion. 9 In a systematic review of POD, using published records from the USA, Australia, South Korea and Canada from 2010 to 2020, the researchers found that in comparison to patients who weren’t delirious, patients with POD incurred costs that varied from a minimum of $A2385 to a maximum of $A36452. Thus elucidating that increased length of stay in hospital and increased hospital costs are strongly associated with POD after surgery. 10
Social Implications:
A person’s independence may be lost when POD occurs as it causes cognitive deterioration and functional impairment. Their capacity to carry out everyday tasks, keep their jobs and partake in social or recreational activities decreases. Furthermore, the extended length of stay in the hospital can disrupt their daily routines, work schedules, and family responsibilities, which leads to increased stress and inconvenience for both patient and their loved ones. 11
As such, this project will investigate the factors that influence the risk of POD in general anaesthetic patients. This investigation will extend our current understanding of POD and what triggers it, thus increasing knowledge for treatment plans and strategies to help prevent the risk and severity of the medical occurrence.
4 Salman, Muhammad, et al., “Postoperative Delirium”, 2023
5 Salman, Muhammad, et al., “Postoperative Delirium”, 2023
6 Maxwell, Megan, et al.” Preventing Postoperative Brain Injury”, 2022
7 Dictionary, Cambridge, “Meaning Of Aetiology in English”, 2023
8 Whitelock L, Elizabeth, et al., “POSTOPERATIVE DELIRIUM”, 2013
9 Pezzullo, Lynne, et al, “Economic Impact of Delirium in Australia: A Cost of Illness Study”, 2019
10 Mosharaf, Parvez, et al. “Hospital Costs of Postoperative Delirium: A Systematic Review”, 2022
11 Arias, Franchesca, et al. “Neighbourhood-Level Social Disadvantage and Risk of Delirium Following Major Surgery”, 2021
Scientific research question
How do different factors influence the risk of postoperative delirium in general anaesthetic patients to compare, and as a result of this comparison, can we optimise the prevention strategies used for postoperative delirium and the treatment plan options?
This project can be broken down into subaims:
1. How different ages and sexes influence the risk of POD.
2. How a patient’s history of health issues and cognitive baseline function influences the risk of POD.
3. Strategies and treatment plans to help prevent the risk and severity of postoperative delirium in general anaesthesia patients.
Scientific hypothesis
Factors such as age, sex, baseline cognitive dysfunction and history of health issues significantly increase the risk of postoperative delirium in general anaesthetic patients.
Null Hypothesis:
There is no relationship between age, sex, time, baseline cognitive dysfunction and history of health issues on the risk of postoperative delirium.
Methodology
Meta-study
Cross-referencing between reports was vital for my methodology to gather secondary data to establish a broad understanding whilst evaluating the validity of particular findings or experimental techniques. This report conducted a meta-study on various scientific reports about POD, assessing the effectiveness of the theories surrounding the factors influencing this occurrence.
Inclusion Criteria
To elucidate this, reports including keywords such as “medicine,” “anaesthetic,” “anaesthesia,” “general anaesthesia,” “neurotransmission,” “delirium,” or “postoperative delirium” were deemed relevant to filter a large volume of data. I also used resources from within the last 15 years to increase validity and ensure data accuracy. Moreover, I tried to use studies with a vast sample size to increase the extent of the data gathered.
Key variables
Aim 1:
Aim 1 was investigated by conducting a retrospective study by reviewing past medical records of patients who underwent surgery, thus comparing the incidence of POD between various age groups and sexes.
Aim 2:
Moreover, aim 2 uses descriptive statistical analysis to inquire into pre-existing health conditions and histories, seeing the correlation and likelihood of POD. Specifically,
how neurological illnesses, diseases and addictive materials affect the incidence of POD.
Interview
Using aims 1-2 findings, aim 3 utilises interviews with various medical professionals such as an anaesthesiologist, clinical neuropsychologists, and geriatrician, providing a primary and personal perspective when handling POD and the treatments and strategies they have found helpful to prevent the risk and severity. Using the same questions for each interview provided and controlled a considerable breadth of knowledge to the report.
Statistical analysis
A regression analysis was utilised to make inferences about the relationship between data sets. Collecting the mean, median and standard deviation of multiple data sets helps normalise various levels of data between the type of surgery and the prevalence of POD.
Results




By normalising and finding the difference between the incidence of POD in both men and women, the overall mean difference between both sexes is 11.2%. Moreover, the median is 8.8%, with a standard deviation of 8.2%. Thus, the incidence of POD is higher in men than women.



* Sensitivity – is the probability of a positive test result, conditioned on the individual truly being positive
* Specificity – is the probability of a negative test result, conditioned on the individual truly being negative
Discussion
The complexity and severity of POD is only a recent research topic, yet, it is an everincreasingly needed enquiry into the effects of general anaesthesia. Research findings showed a significant increase in the probability of POD as an individual ages, showing that 75% of patients aged between 80+ are susceptible. It was elucidated with Table 3’s findings to investigate neurological resilience to anaesthesia. The results from secondary research reveal that POD risk and severity are influenced by the balance between surgical stress and neurological resilience, which decreases with age, confirming the same theory of baseline cognitive dysfunction (Taewook, 2020). Furthermore, the normalisation of data from various studies revealed that the incidence of POD is higher in men than women. With my secondary research, I could not find any reliable studies that hypothesise why the incidence of POD is higher in men, yet many data sets show this occurrence, as seen in Figure 3. Through these findings, comparisons of effective treatment options were evaluated, again supported by primary interview trends.
Aim 1:
Resilience is the ability to return swiftly to a previous good condition after a problem. This is true for the brain and its ability to bounce back after experiencing general anaesthesia. However, with age, neurological resilience is lessened due to the immense stress brought on during surgery. A strong positive relationship between ageing and the prevalence of POD is shown in Figure 2, with 13% of patients exhibiting POD between 4049 years old and increasing to 75% at 80-89 years old. Interviewer Five, a POD nurse, confirms that older patients over 80 with over 4-hour surgery are at a significantly increased risk of POD, which is expected, as per her
experience. As seen in Table 3, secondary research supports the idea that elderly patients have a higher prevalence of POD due to reduced physical activity, a smaller brain, and decreased generation of cerebral neurotransmitters (Taewook, 2020), significantly impacting their risk of POD. In addition, there is a strong correlation between sex and POD, with the incidence of POD being higher in men than women. To investigate this relationship, various research papers examined multiple areas of surgery and the incidence of POD. This data had a large spread, but through the normalisation process, patterns emerged from comparing the difference between men and women experiencing POD, showing that men had an increased prevalence with a mean of 11.24% (+/-8.2%). Furthermore, through the analysis of data from Maria Wittman’s research in geriatric surgery (2022), the difference between the sexes was the highest at 24%. This is significant as geriatric surgery refers to a branch of medicine that deals with the problems and diseases of old age and ageing people. With evidence that POD is also influenced by old age, we can infer that the comorbidities of age and sex also increased the high sex difference of 24% in this study.
Aim 2:
Throughout the investigation, various peerreviewed studies were evaluated about how a patient’s history of health issues and cognitive baseline function influences the risk of POD. Although it is mutually agreed that preoperative mental and neurological problems before surgery significantly affect the risk and severity of POD, many were unable to discover why due to many cases not being formally recorded. Furthermore, referring to the qualitative interview analysis, cognitive dysfunction patterns emerged. Interviewer one discussed the impact of Postoperative Cognitive Dysfunction (POCD) and its strong correlation with the risk and
severity of POD. POCD is where cognitive impairment arises after surgery. This is brought on by preoperative neurological issues such as Dementia and Parkinson’s Disease and is a biomarker of POD, as mentioned in Ganna Androsova’s research about biomarkers of POD and POCD (2015). This correlation between baseline cognitive dysfunction and POD would remarkably benefit from further analysis.
Aim 3:
Furthermore, with data gathered from aims 1 and 2, strategies and treatment options for POD were evaluated through peer-reviewed secondary research and qualitative interviews. Referring to Table 4, four standard assessment methods were evaluated by their sensitivity and specificity coefficient, which showed that the CAM-ICU assessment was the most effective and beneficial POD diagnostic tool. Its sensitivity and specificity coefficient were 83% and 100%, indicating that this test could conclusively tell if a patient was negative for POD. In addition, the MMSE strategy was the most unreliable as research had a vast range of how efficient the assessment results were, with a sensitivity ranging from 27% to 89% (Health Direct, 2023). In addition, the interviews provided a more holistic approach to treating POD, emphasising the importance of social and personal environments in reducing the severity. Interviewer 5 states, “Attempt to reorientate a patient, create a calming environment (dark, quiet, warm) when the patient wakes up, ensure pain is well controlled, and re-introduce familiar items.” This notion is elucidated with secondary research that states that making a soothing environment could reduce confusion and delirium in patients (Padideh, 2023). Both sources highlight the importance of keeping a patient calm, and cognitive awareness is a significant and effective treatment to reduce the severity of POD.
Reliability, Validity and Accuracy of the Research:
All secondary research studies were published in various high-impact journals, with many peer-reviewed and multiple researchers that decreased bias, ensuring validity. Furthermore, the articles all provide a thorough, well-reasoned theory and extensive discussion based on primary data. Moreover, to guarantee that the results were reliably sourced, all of the effects used in this metastudy came from studies published within the last 15 years and met the inclusion criteria. However, this report can be considered valid due to the absence of presented statistical data such as standard deviation, mean and median in every result set.
Limitations of the Investigation:
There were few publications to gather research because the elements that affect the risk and severity of POD following general anaesthetic is a highly specialised study issue, which decreased the report’s reliability. Furthermore, many studies about the effects of POD lacked clarity and breadth since all the results were gathered from secondary research. Therefore, a more thorough examination would have been possible from first-hand investigations or accessing a more extensive database that included particular POD patient data. In addition, to gather comprehensive qualitative data, interviewing more than five medical professionals would increase the amount and minutiae of details about POD.
Future Direction of Scientific Research:
This secondary study intends to enhance knowledge of the factors that increase the risk of severity of POD because there is relatively little research on the condition. More studies and tests on this particular subject must be published in the future for a thorough assessment. Studies can look at understanding ‘WHY’ age, sex and baseline cognitive dysfunction increases the risk of POD. The current theories on why age is a factor, resilience, sex and baseline cognitive dysfunction could be further investigated to clarify this anecdotal data.
Conclusion
In conclusion, this metastudy offers a thorough understanding of the variables, such as age, sex, and baseline cognitive dysfunction, that affect the risk and severity of Postoperative Delirium. After the data and results were analysed, the null hypothesis was rejected, and the scientific theory was accepted that "factors such as age, sex, baseline cognitive dysfunction, and history of health issues significantly increase the risk of postoperative delirium in general anaesthetic patients." To analyse the influence of age on POD, the retrospective study found that the risk significantly increases with age, most likely due to decreased neurological resilience. Furthermore, the descriptive statistical analysis proved the strong correlation between sex and POD, with normalisation of mean differences between sexes showing that men were 11.24% more likely. Additionally, the influence of preoperative cognitive dysfunction can also be related to neurological resilience, further validated with secondary research that hypotheses that biomarkers such as Dementia and Parkinson’s Disease are correlated with the risk of POD. Moreover, by understanding the factors that influence the risk of POD, various strategies and treatments were evaluated and considered for optimisation. With data from the qualitative interviews, nature remedies such as controlling the social and physical environment improved patient awareness. Results reveal that the CAM-ICU assessment is the most effective POD diagnostic tool, with a sensitivity and specificity coefficient of 83% and 100%, respectively. The MMSE strategy is the most unreliable, with a sensitivity ranging from 27% to 89%, and the research had a vast range of efficiency in its assessment results. By assembling secondary research, all objectives of this study which was to increase awareness of the factors that increased POD in general anaesthesia patients have been met.
Reference list
Arias, F., Chen, F., Fong, T. G., Shiff, H., Alegria, M., Marcantonio, E. R., Gou, Y., Jones, R. N., Travison, T. G., Schmitt, E. M., Kind, A. J. H., & Inouye, S. K. (2020). Neighborhood-Level Social Disadvantage and Risk of Delirium Following Major Surgery. Journal of the American Geriatrics Society, 68(12), 2863–2871. https://doi.org/10.1111/jgs.16782
Boone, M. D., Sites, B., von Recklinghausen, F. M., Mueller, A., Taenzer, A. H., & Shaefi, S. (2020). Economic Burden of Postoperative Neurocognitive Disorders Among US Medicare Patients. JAMA Network Open, 3(7), e208931. https://doi.org/10.1001/jamanetworkopen.202 0.8931
Cambridge Dictionary. (2019). AETIOLOGY | meaning in the Cambridge English Dictionary Cambridge.org. https://dictionary.cambridge.org/dictionary/en glish/aetiology
Delirium , N. (2018). Instrument Memorial Delirium Assessment Scale. https://deliriumnetwork.org/wpcontent/uploads/2018/05/MDAS.pdf
Galyfos, G. (2016). Risk factors of postoperative delirium after elective vascular surgery in the elderly: A systematic review. International Journal of Surgery, 35, 1–6. https://doi.org/10.1016/j.ijsu.2016.09.001
Garcia, P., Kolesky, S., & Jenkins, A. (2010). General Anesthetic Actions on GABAA Receptors. Current Neuropharmacology, 8(1), 2–9. https://doi.org/10.2174/157015910790909502
healthdirect. (2018). Mini Mental State Examination (MMSE). Healthdirect.gov.au; Healthdirect Australia. https://www.healthdirect.gov.au/mini-mentalstate-examination-mmse
Janjua, M. S., Spurling, B. C., & Arthur, M. E. (2022, May 15). Postoperative Delirium. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534831/
Lee, S. S., Lo, Y., & Verghese, J. (2019). Physical Activity and Risk of Postoperative Delirium. Journal of the American Geriatrics Society, 67(11), 2260–2266. https://doi.org/10.1111/jgs.16083
Lin, X., Liu, F., Wang, B., Dong, R., Sun, L., Wang, M., & Bi, Y. (2021). Subjective Cognitive Decline May Be Associated With Postoperative Delirium in Patients Undergoing Total Hip Replacement: The PNDABLE Study. Frontiers in Aging Neuroscience, 13. https://doi.org/10.3389/fnagi.2021.680672
MacLullich, A. M., Shenkin, S. D., Goodacre, S., Godfrey, M., Hanley, J., Stíobhairt, A., Lavender, E., Boyd, J., Stephen, J., Weir, C., MacRaild, A., Steven, J., Black, P., Diernberger, K., Hall, P., Tieges, Z., Fox, C., Anand, A., Young, J., & Siddiqi, N. (2019). General introduction. In www.ncbi.nlm.nih.gov. NIHR Journals Library. https://www.ncbi.nlm.nih.gov/books/NBK5449 24/
Maxwell, M., Michael, M., & McDonagh, D. L. (2022, January 1). 7 - Central Nervous System Risk Assessment: Preventing Postoperative Brain Injury (M. F. Newman, L. A. Fleisher, C. Ko, & M. (Monty) Mythen, Eds.). ScienceDirect; Elsevier. https://www.sciencedirect.com/science/article/abs/pii/B9780323567244000071
Miranda, F., Arevalo-Rodriguez, I., Díaz, G., Gonzalez, F., Plana, M. N., Zamora, J., Quinn, T. J., & Seron, P. (2018). Confusion Assessment Method for the intensive care unit (CAM-ICU) for the diagnosis of delirium in adults in critical care settings. Cochrane Database of Systematic Reviews https://doi.org/10.1002/14651858.cd013126
Neufeld, K. J., Joseph Bienvenu, O., Rosenberg, P.B., Mears, S. C., Lee, H. B., Kamdar, B. B., Sieber, F. E., Krumm, S. K., Walston, J. D., Hager, D. N., Touradji, P., & Needham, D. M. (2011). The Johns Hopkins Delirium Consortium: a model for collaborating across disciplines and departments for delirium prevention and treatment. Journal of the American Geriatrics Society, 59 Suppl 2(0 2), S244-248. https://doi.org/10.1111/j.15325415.2011.03672.x
Neufeld, K. J., Yue, J., Robinson, T. N., Inouye, S.K., & Needham, D. M. (2016). Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalised Adults: A Systematic Review and Meta-Analysis. Journal of the American Geriatrics Society, 64(4), 705–714. https://doi.org/10.1111/jgs.14076
Nunns, M., Shaw, L., Briscoe, S., Thompson Coon, J., Hemsley, A., McGrath, J. S., Lovegrove, C. J., Thomas, D., & Anderson, R. (2019). Multicomponent hospital-led interventions to reduce hospital stay for older adults following elective surgery: a systematic review. In PubMed. NIHR Journals Library. https://www.ncbi.nlm.nih.gov/books/NBK5517 62/
Oh, E. S., Sieber, F. E., Leoutsakos, J.-M., Inouye, S. K., & Lee, H. B. (2016). Sex Differences in Hip Fracture Surgery: Preoperative Risk Factors for Delirium and Postoperative Outcomes. Journal of the American Geriatrics Society, 64(8), 1616–1621. https://doi.org/10.1111/jgs.14243
Pezzullo, L., Streatfeild, J., Hickson, J., Teodorczuk, A., Agar, M. R., & Caplan, G. A. (2019). Economic impact of delirium in Australia: a cost of illness study. BMJ Open, 9(9), e027514. https://doi.org/10.1136/bmjopen-2018-027514
Psych, B. (2021, December 14). Clock-Drawing Test (CDT). PsychDB. https://www.psychdb.com/cognitivetesting/clock-drawingtest#:~:text=The%20Clock%2DDrawing%20T est%20(CDT
Robinson, D. H., & Toledo, A. H. (2012). Historical development of modern anaesthesia. Journal of Investigative Surgery : The Official Journal of the Academy of Surgical Research, 25(3), 141–149. https://doi.org/10.3109/08941939.2012.690328
Robinson, T. N., & Eiseman, B. (2008). Postoperative delirium in the elderly: diagnosis and management. Clinical Interventions in Aging, 3(2), 351–355. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2546478/
Schenning, K. J., Murchison, C. F., Mattek, N. C., Kaye, J. A., & Quinn, J. F. (2019). Sex and genetic differences in postoperative cognitive dysfunction: a longitudinal cohort analysis. Biology of Sex Differences, 10(1). https://doi.org/10.1186/s13293-019-0228-8
Shepherd, J., Jones, J., Frampton, G. K., Bryant, J., Baxter, L., & Cooper, K. (2013). Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-Entropy, Bispectral Index and Narcotrend): a systematic review and economic evaluation. In PubMed. NIHR Journals Library. https://www.ncbi.nlm.nih.gov/books/NBK260910/
Son, Y. (2010). Molecular mechanisms of general anesthesia. Korean Journal of Anesthesiology, 59(1), 3. https://doi.org/10.4097/kjae.2010.59.1.3
The Editors of Encyclopedia Britannica. (2018). Oliver Wendell Holmes | American physician and writer. In Encyclopædia Britannica https://www.britannica.com/biography/OliverWendell-Holmes
Wang, H., Guo, X., Zhu, X., Li, Y., Jia, Y., Zhang, Z., Yuan, S., & Yan, F. (2021). Gender Differences and Postoperative Delirium in Adult Patients Undergoing Cardiac Valve Surgery. Frontiers in Cardiovascular Medicine, 8. https://doi.org/10.3389/fcvm.2021.751421
Whitlock, E. L., Vannucci, A., & Avidan, M. S. (2013). POSTOPERATIVE DELIRIUM. Minerva Anestesiologica, 77(4), 448–456. https://www.ncbi.nlm.nih.gov/pmc/articles/PM C3615670/
Wittmann, M., Kirfel, A., Jossen, D., Mayr, A., & Menzenbach, J. (2022). The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics, 7(3), 65. https://doi.org/10.3390/geriatrics7030065
Yamamoto, K., Shimakawa, N., Mizumoto, T., Shiroyama, K., Shichino, T., Yuzawa, K., Kataoka, M., Horiuchi, T., Teshima, S., Shibasaki, S., & Hirao, M. (2020). Emergency surgery and male gender are risk factors of postoperative delirium after general or gastrointestinal surgery in elderly patients: A multicenter cohort study. International Surgery. https://doi.org/10.9738/intsurg-d-1600112.1

