






















4 From the editor
May/June 2024 | Vol. 56, No. 5

CONTINUING EDUCATION
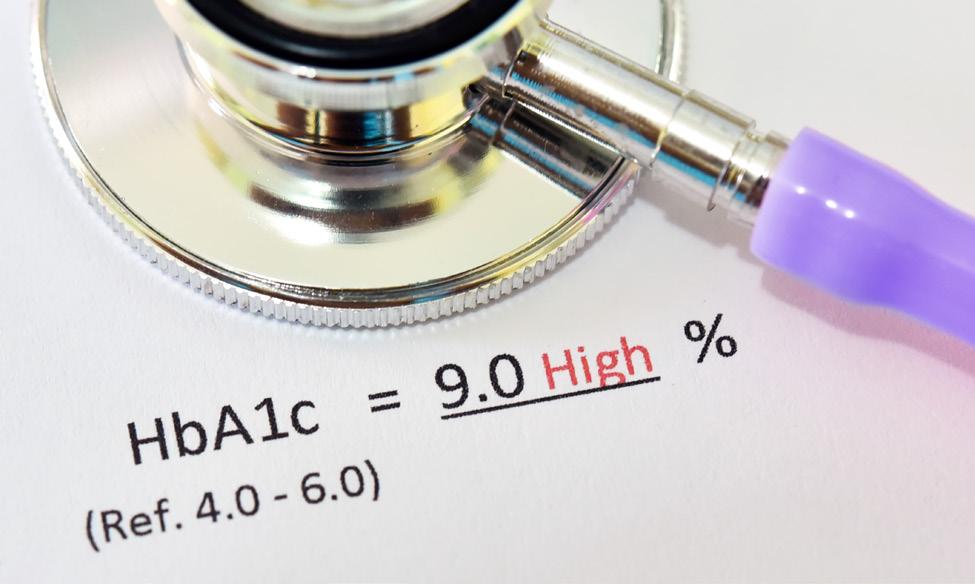
6 Navigating the new normal for A1c analysis: Interpreting recently released clinical guidelines in the lab
By Matthew C. Wagner,PhD
6




CLINICAL ISSUES
14 Dear API Abby
By Danielle Casey, MBA, MLS(ASCP)CM; Anita Hoeksema, MS, MLS(ASCP)CM; and Sue Styles, MSI
LAB MANAGEMENT
18 Dark Labs: Illuminating the future of fully automated diagnostic laboratories
By Mike Heydlauf and Mark Edwards, PhD CEng FIET
INFECTION DIAGNOSTICS
22 Molecular point-of-care testing offers hope to quell the STI epidemic
By Allison McMullenPhD, D(ABMM)
EDUCATION
26 Understanding current and future uses of anti-Müllerian hormone in both clinical practice and research
By JoDell E. Wilson,PhD
STATE OF THE INDUSTRY
30 2024 lab management best practices trend back to the basics
By Kara NadeauMOLECULAR DIAGNOSTICS
36 Next-generation sequencing in laboratory medicine
By Rajasri Chandra, MS,MBA
PRODUCT FOCUS
40 Analyzers
LAB INNOVATOR
42 Working to advance pathology practices
By Christina WichmannDEPARTMENTS
39 Index of advertisers
ON THE COVER: xavierarnau/E+/Getty Images


Vol.56, No. 5
 By Christina Wichmann
Editor in Chief
By Christina Wichmann
Editor in Chief
In this issue of Medical Laboratory Observer, we are sharing the results of our State of the Industry survey on Lab Management Best Practices. The survey results provide insights into best practices around controlling costs, optimizing contracts, capturing reimbursements, managing supplies, implementing technology solutions, navigating staffing shortages, and improving the quality and efficiency of testing. MLO has been conducting this survey with readers for several years now.
I thought it would be interesting to highlight some of the feedback we received the past three years from MLO readers.
• Continuing education (2022, 2023, 2024)
• Career ladders (2022, 2023, 2024)
• Shift changes for scheduling flexibility (2022, 2023, 2024)
• P roviding staff schedule six to eight weeks in advance, which provided ample time to make changes or trade among themselves (2022)
• Brought in lab aids to handle basic tasks, freeing up technicians’ time (2022)
• Standard lab processes and staff education materials (2022, 2023, 2024)
• I ncorporated IT solutions to reduce human error (2022, 2023, 2024)
• Ensure the LIS and billing system are integrated appropriately to prevent lost charges (2022, 2023)
• Cost accounting, which allows labs to measure profitability by test type (2023)
• Patient billing through text/email versus stuffing hundreds of envelopes a week (2022)
• Standing orders instead of just-in-time (2022, 2023, 2024)
• Work with others in the organization such as the chief medical officer and physicians (2023, 2024)
• Apply lessons learned and best practices from acute care (medical/surgical) supply management (2024)
• Turned to laboratory-developed tests (2023)
• D iversify suppliers (place orders with various suppliers on a regular basis) (2022)
• Standardized test procedures/formularies (2022, 2023, 2024)
• Adopted new tools for automation, such as analyzers (2022, 2023, 2024)
• Staff and committee review of SOPs (2024)
• Empowering staff to continuously identify and address areas for improvement (2023)
• Q uality Circle management to bring staff together to meet goals and adjust processes (2023)
As new ideas are proposed in lab management best practices, MLO will continue sharing them with you.
I welcome your comments and questions — please send them to me at cwichmann@mlo-online.com.
PUBLISHER Chris Driscoll cdriscoll@endeavorb2b.com
EDITOR IN CHIEF Christina Wichmann cwichmann@mlo-online.com
MANAGING EDITOR Erin Brady ebrady@endeavorb2b.com
PRODUCTION MANAGER Edward Bartlett
ART DIRECTOR Kermit Mulkins
AUDIENCE DEVELOPMENT/LIST RENTALS
Laura Moulton | lmoulton@endeavorb2b.com
ADVERTISING SERVICES MANAGER
Karen Runion | krunion@endeavorb2b.com
ADVERTISING
DIRECTOR OF SALES
EAST COAST/MIDWEST SALES, CLASSIFIEDS
Carol Vovcsko (941) 321-2873 | cvovcsko@mlo-online.com
SOUTH/WEST COAST/ILLINOIS SALES
Lora Harrell
(941) 328-3707 | lharrell@mlo-online.com
MLO EDITORIAL ADVISORY BOARD
John Brunstein, PhD, Biochemistry (Molecular Virology) President & CSO PathoID, Inc., British Columbia, Canada
Lisa-Jean Clifford, COO & Chief Strategy Officer Gestalt, Spokane, WA
Barbara Strain, MA, SM(ASCP), CVAHP Principal, Barbara Strain Consulting LLC, Formerly Director, Value Management, University of Virginia Health System, Charlottesville, VA
Jeffrey D. Klausner, MD, MPH Professor of Preventive Medicine in the Division of Disease Prevention, Policy and Global Health, Department of Preventive Medicine at University of Southern California Keck School of Medicine.
Donna Beasley, DLM(ASCP), Director, Huron Healthcare, Chicago, IL
Anthony Kurec, MS, H(ASCP)DLM, Clinical Associate Professor, Emeritus , SUNY Upstate Medical University, Syracuse, NY
Suzanne Butch, MLS(ASCP)CM, SBBCM, DLMCM Freelance Consultant, Avon, OH
Paul R. Eden, Jr., MT(ASCP), PhD, Lt. Col., USAF (ret.), (formerly) Chief, Laboratory Services, 88th Diagnostics/Therapeutics Squadron, Wright-Patterson AFB, OH
Daniel J. Scungio, MT (ASCP), SLS, CQA (ASQ), Consultant at Dan the Lab Safety Man and Safety Officer at Sentara Healthcare, Norfolk, VA CORPORATE TEAM
CEO Chris Ferrell
PRESIDENT June Griffin
COO Patrick Rains
CRO Paul Andrews
CHIEF DIGITAL OFFICER Jacquie Niemiec CHIEF ADMINISTRATIVE AND LEGAL OFFICER Tracy Kane
EVP CITY SERVICES & HEALTHCARE Kylie Hirko 30 Burton Hills Blvd., Suite 185 Nashville, TN 37215
800-547-7377 | www.mlo-online.com
Medical Laboratory Observer USPS Permit 60930, ISSN 0580-7247 print, ISSN 2771-6759 online is published 10 times annually (Jan, Feb, Mar, Apr, May, Jul, Aug, Aug CLR, Sep, Nov) by Endeavor Business Media, LLC. 201 N Main St 5th Floor, Fort Atkinson, WI 53538. Periodicals postage paid at Fort Atkinson, WI, and additional mailing offices. POSTMASTER: Send address changes to Medical Laboratory Observer, PO Box 3257, Northbrook, IL 60065-3257. SUBSCRIPTIONS: Publisher reserves the right to reject non-qualified subscriptions. Subscription prices: U.S. $160.00 per year; Canada/Mexico $193.75 per year; All other countries $276.25
Implementing changes to your automation system can be a complex and time-consuming process, potentially affecting your service delivery. However, with GLP systems Track, we’ve revolutionized the experience. Our solution has interlocking track components, standardized modules, and simplified software to allow you to change when you need to.


















In the United States, for the GLP systems Track, not all modules and features are commercially available and open connections to clinical analyzers/systems are under development. GLP systems Track is not approved for use in US blood donor and plasma testing laboratories.
AUTOMATION REINVENTED. FLEXIBILITY REDEFINED.

Customize tracks, clear pathways, and create personalized lab solutions.

NOW AVAILABLE!

Reduced track setup for efficient implementation, service and training.
CONTACT A REPRESENTATIVE FROM ABBOTT TODAY.

Maximize uptime, optimize workflow, and decrease turnaround time.
See test online at https://ce.mlo-online.com/ courses/navigating-the-newnormal-for-a1c-analysisinterpreting-recently-releasedclinical-guidelines-in-the-lab/ Passing scores of 70 percent or higher are eligible for 1 contact hour of P.A.C.E. credit.
Upon completion of this article, the reader will be able to:

1. Describe the goal of the “Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus.”
2. List parameters of glycemic control in different populations of patients.
3. Discuss biologic and nonbiologic interferences of testing methods of HbA1c.
4. Describe methods of QA and patient management of the disease through different result strategies.
The recent “Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus”1-2 has not been as disruptive to the hemoglobin A1c (HbA1c) testing space as expected. The 16 HbA1c-related recommendations ((a)-(p) in the executive summary 3) reflect current understanding of the diabetes testing environment and reaffirm and update previously established standards, making explicit the details only suggested before and indicating the future direction of industry best practices. This article will summarize the recommendations and explain the reasoning behind select guidelines and their repercussions within the testing laboratory.
A. Laboratory-based HbA1c testing can be used to diagnose (a) diabetes, with a value ≥6.5% (≥48 mmol/mol) diagnostic of diabetes, and (b) prediabetes (or high risk for diabetes) with an HbA1c level of 5.7% to 6.4% (39 to 46 mmol/mol). An NGSP-certified method should be performed in an accredited laboratory.
HbA1c is formed by slow, irreversible glycation of the N-terminal valine of hemoglobin’s beta globin chains. Accumulation in the blood reflects the patient’s average glycemic status over the previous 120 days. Normal glycemic control exhibits an HbA1c of <5.7%, while diabetics will have a value





≥6.5%. Values between these are pre-diabetic, with high risk for progression. HbA1c is not recommended for gestational diabetes screening, since faster recognition and treatment is required to avoid injury to mother or fetus.
B. Recommendation: Point-of-care (POC) HbA1c testing for diabetes screening and diagnosis should be restricted to FDA-approved devices at CLIA-certified laboratories that perform testing of moderate complexity or higher.
This guideline highlights concerns about the accuracy of POC methods. Their exemption from proficiency testing (CLIA waived) prevents regular collection of HbA1c survey data by these methods. Evaluating them through publications, the guidelines quote several meta-analyses4-6 showing unacceptable bias and large coefficient of variation (CVs) in current POC devices. Stipulating FDA approval and use at CLIA-certified moderate-complexity labs overcomes this by requiring documentation of objective and ongoing acceptable performance.
C. HbA1c should be measured routinely (usually every 3 months until acceptable, individualized targets are achieved and then no less than every 6 months) in most individuals with diabetes mellitus to document their degree of glycemic control.
D. Treatment goals should be based on ADA recommendations which include maintaining HbA1c concentrations <7% (<53 mmol/mol) for many nonpregnant people with diabetes and more stringent goals in selected individuals if this can be achieved without significant hypoglycemia or other adverse effects of treatment. (Note that these values are applicable only if the assay method is certified by the NGSP as traceable to the DCCT reference.)
E. Higher target ranges are recommended for children and adolescents, and are appropriate for individuals with limited life expectancy, extensive co-morbid illnesses, a history of severe hypoglycemia, and advanced complications.
The clinical use of HbA1c% is in diabetic monitoring regarding the long-term vascular damage of chronic complications: neuropathies, retinopathy, kidney failure, diabetic ulcers, heart damage, and increased incidence of stroke. The <7% target minimized progression of chronic diabetic complications in landmark studies7-8 balanced against the hazards of acute hypoglycemia. However, this update suggests promotion of “personalized” targets for some population subsets, accounting for differences in risk and clinical condition, allowing more stringent or relaxed targets, including:
F. During pregnancy and in preparation for pregnancy, women with diabetes should try to achieve HbA1c goals that are more stringent than in the nonpregnant state, aiming ideally for <6.0% (<42 mmol/mol) during pregnancy to protect the fetus from congenital malformations and the baby and mother from perinatal trauma and morbidity owing to large-for-date babies.
Diabetics during pregnancy have a more stringent (<6.0%) target, due both to fetal risk and to increased erythropoietin levels accelerating RBC turnover,9 depleting HbA1c in the bloodstream. This accounts for pregnant patients’ HbA1c% reflecting glycemic status differently. A pregnant, diabetic patient might have an HbA1c of 6.5 %, which is below the standard <7.0%, but,
for them, indicative of poorly controlled diabetes. Recognition that an analyte reflects conditions differently in some patients aligns with the current trends of personalized medicine.
G. Laboratories should be aware of potential interferences, including hemoglobin variants that may affect HbA1c test results depending on the method used. In selecting assay methods, laboratories should consider the potential for interferences in their particular patient population.
This raises several questions: What is required of the lab? Can labs with a low diversity patient population ignore this guideline? What diversity threshold is low enough? Numerous studies document HbA1c testing of inappropriate patients, although rates differ widely.10-11 One pulled a random sampling of their lab’s HbA1c orders and found sufficient S/S, S/C, and S/Beta-thalassemia patients to project 2,000 to 3,000 improperly ordered samples per year.10 These guidelines suggest checking the National Glycohemoglobin Standardization Project (NGSP) interferences website and reading limitations in manufacturer product instructions. Labs may be surprised by the cautions they find: Some immunoassays warn about high Hb F (>10%) artificially lowering measured HbA1c, and state “care must be taken” with variants;12-15 other versions cautioning against diagnosis or monitoring in sickle trait patients.16 Other enzymatic methods warn against high HbF interference without defining “high” and caution against use in trait patients except where it’s been proven to have no influence on results.17
The NGSP website acknowledges inherent HbF interference by certain methodologies, stating “In the absence of specific method data, it can generally be assumed that immunoassay, boronate affinity and enzymatic methods show interference from elevated Hb F levels.”18 The irony of these cautions in non-separation methodologies (HbA1c% produced without an Hb profile) is that they cannot see interferences, raising the alarm only for results outside the physiologic range. Separation techniques (CE-HPLC or capillary electrophoresis) display the separated hemoglobin fractions with their result, enabling better detection and evaluation of interferences, some even flagging abnormalities for review. Hb F has less impact as a result in these methods,18 e.g., capillary electrophoresis finds no interference for HbF<23% due to the isolation of the HbF peak from HbA0 and HbA1c,19 and rare variants co-migrating and distorting the HbA0 or HbA1c peaks trigger safeguards blocking result calculation, preventing misreporting events. However, there are other reasons to recognize variants in diabetes testing:
H. HbA1c measurements in individuals with disorders that affect red blood cell turnover may provide spurious (generally falsely low) results regardless of the method used and glucose testing will be necessary for screening, diagnosis, and management.
Shortening the average 120-day RBC lifespan lowers equilibrium HbA1c%, as hemoglobin will have less blood glucose exposure, counter-indicating its standard use in diabetic management. This is not a method-dependent analytical interference, but a biological one, suppressing HbA1c accumulation. All current methodologies warn against these misleading values, listing conditions like hemolytic anemia, blood loss, transfusion, iron deficiency, and spherocytosis.12-16,19 Hemoglobinopathies, typically evident by separation methods but invisible to non-separation methods, may also impact RBC lifespan or glycation rates. Although the NGSP website declares few




interferences from common variants,18 this covers analytical interference, not biological. Hb S trait, typically clinically silent (and frequently undiagnosed), has historically been shown to significantly accelerate RBC turnover,20-21 likely linked to the reduced HbA1c% in this population,22 and leading the American Diabetes Association to note “…it seems prudent to establish A1C goals in these [sickle trait and other] populations with consideration of individualized CGM, BGM, and A1C results.”23 Thalassemias, mutations limiting hemoglobin production, similarly accelerate RBC turnover,24-25 and may be incidentally detected in some HbA1c methods — capillary electrophoresis visualizes a non-reportable but indicative HbA2, whose gross elevation could indicate beta thalassemia. These incidental discoveries alert clinicians to possible HbA1c discrepancies.
I. Assays of other glycated proteins, such as fructosamine or glycated albumin, may be used in clinical settings where abnormalities in red blood cell turnover, hemoglobin variants, or other interfering factors compromise interpretation of HbA1c test results, although they reflect a shorter period of average glycemia than HbA1c.
J. HbA1c cannot be measured and should not be reported in individuals who do not have Hb A, e.g., those with homozygous hemoglobin variants, such as Hb SS or Hb EE; glycated proteins, such as fructosamine or glycated albumin, may be used.
A patient without native HbA cannot produce HbA1c. Any HbA1c reporting in this patient is analytically and fundamentally incorrect. Non-separation methodologies are incapable of distinguishing between HbA1c and most glycated variants, reporting values even in homozygous or doubly heterozygous beta variant patients. Accelerated RBC turnover or glycated variant mismatch may drive test results non-physiologically low, but those with milder impact may go undetected, possibly causing misdiagnosis noted in case studies.26-31 Separation techniques uncovering non-A patients may flag the patient or be incapable of providing results, an in-test safety factor. When biological or analytical interferences impact an HbA1c result, other glycated proteins can be used as a second-best option.
K. Laboratories should use only HbA1c assay methods that are certified by the NGSP as traceable to the DCCT reference. The manufacturers of HbA1c assays should also show traceability to the IFCC reference method.
Prescribed target values assume that all assays employ the same scale correlating HbA1c to diabetic complication risk. Manufacturers prove this by showing traceability to the IFCC HbA1c% reference method, but approaches vary widely. Immunoassay and enzymatic methods measure HbA1c by targeting glycation site epitopes, excluding glycated-HbF but including variants if mutations are located elsewhere.
“Total HbA” is approximated based on spectroscopic analysis or optical methods (respectively) that pool all hemoglobins, skewing the formula in the presence of abnormal production. Boronate Affinity sorts hemoglobins into “glycated” and “non glycated’ fractions, deriving HbA1c% from a curve fit not accounting for any abnormal Hbs. HPLC is more discriminating, as variant structures anywhere within a hemoglobin may shift elution time. However, incidental separation of a myriad of “HbA total” subspecies (labile, acetylated, etc.) requires careful re-collection, occasionally complicated by co-eluting rare variants.32-34 Capillary electrophoresis minimizes these
complications, simplifying the pattern through migration fine tuning, gathering extraneous fractions together while separating variants, and allowing HbA1c and total HbA quantification by the same detection method.
L. Laboratories that measure HbA1c should participate in an accuracy-based proficiency-testing program that uses fresh whole blood samples with targets set by the NGSP Laboratory Network.
Proficiency testing provides essential method quality checks for certified laboratories. In providing samples with established HbA1c IFCC reference method results (methods impractical in clinical labs), the pooled participant results evaluate method variance and bias, although Hb variants are typically neglected.
M. The goals for imprecision for HbA1c measurement are intra-laboratory CV <1.5% and inter-laboratory CV <2.5% (using at least 2 control samples with different HbA1c levels), and ideally no measurable bias.
These guideline CVs, a significantly tightening from prior guidelines (2% and 3.5%, respectively),35 mean that two successive patient samples differing by 0.5% have a 95% chance of reflecting a real change in glycemic status, rather than random instrument scatter. Comparison with current CAP (a popular proficiency testing resource) data36 where ±6% is the acceptable limit, highlights the new guideline’s stringency. Comparison with the EuroA1c project (a European-centered program involving 22 nations) shows that CV<2.5% lands within the “silver medal” range, a triumph consistently achieved by only few methodologies.37
N. HbA1c should be reported as a percentage of total hemoglobin or as mmol/mol of total hemoglobin.
O. HbA1c may also be reported as estimated average glucose (eAG) to facilitate comparison with the home glucose monitoring results and make the interpretation of the HbA1c more accessible to people with diabetes.
HbA1c% values are used in the United States; mmol/ mol is used throughout Europe and much of the rest of the world. However, patients require connection between the infrequently measured HbA1c and their daily glycometer reading to better manage dietary choices, insulin regiment, and alleviate anxiety about their disease progression. Offering an eAG value in parallel with their A1c result can provide this connection.
P. Laboratories should verify by repeat testing specimens with HbA1c results below the lower limit of the reference interval or greater than 15% (140 mmol/mol) HbA1c.
Regulating responses to non-physiologic results serves two purposes: troubleshooting instrument malfunction, and as a fail-safe against misreporting samples with interferences. Upon retesting, a changed result indicates instrument malfunction, and an identically repeated result indicates a hemoglobinopathy or other interference should be suspected. While important for all HbA1c methods, this is essential for the non-separation methodologies as the sole interference failsafe, while separation methods’ visualizing of unusual hemoglobin profiles can detect many interferences even without the numerical result review.






These guidelines, while reaffirming the prior version,35 expand upon advice to watch for “marked discordance between measured A1c and plasma glucose levels,” 35 indicating either analytical interferences or conditions that “alter the relationship between A1c and glycemia.”The new guidelines set tighter standards, make explicit the potential for misleading results, and define patients for whom the test is absolutely inappropriate. Previously cautioning against diagnosis by HbA1c in certain patients, now any HbA1c reporting at all is strongly discouraged in the presence of analytical interference, biological interference, or conditions of altered RBC turnover. These recommendations are in alignment with HbA1c assay package inserts stating they are not appropriate for use in patients without hemoglobin A or even in the diagnosis of patients with trait hemoglobinopathies. In conclusion, the arc of the regulatory environment defined by these updated guidelines is leaning heavily toward personalized goals for specific diabetic patients and issues that are clearly addressable only by separation methods.

1. Sacks DB, Arnold M, Bakris GL, et al. Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Clin Chem. 2023;2;69(8):808-868. doi:10.1093/clinchem/hvad080.
2. Sacks DB, Arnold M, Bakris GL, et al. Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Diabetes Care. 2023;1;46(10):e151-e199. doi:10.2337/dci23-0036.
3. Sacks DB, Arnold M, Bakris GL, et al. Executive Summary: Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Diabetes Care 2023;1;46(10):1740-1746. doi:10.2337/dci23-0048.
4. Lenters-Westra E, Slingerland RJ. Six of eight hemoglobin A1c point-ofcare instruments do not meet the general accepted analytical performance criteria. Clin Chem. 2010;56(1):44-52. doi:10.1373/clinchem.2009.130641.
5. Hirst JA, McLellan JH, Price CP, et al. Performance of point-ofcare HbA1c test devices: implications for use in clinical practice - a systematic review and meta-analysis. Clin Chem Lab Med 2017;1;55(2):167-180. doi:10.1515/cclm-2016-0303.
6. Nathan DM, Griffin A, Perez FM, et al. Accuracy of a Point-of-Care Hemoglobin A1c Assay. J Diabetes Sci Technol. 201913(6):1149-1153. doi:10.1177/1932296819836101.
7. Diabetes Control and Complications Trial Research Group; Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;30;329(14):977-86. doi:10.1056/NEJM199309303291401.
8. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;12;352(9131):837-53.
9. Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2000;93(2):185-92. doi:10.1016/s0301-2115(00)00290-6.
10. Rhea JM, Koch D, Ritchie J, et al. Unintended reporting of misleading Hb A(1c) values when using assays incapable of detecting hemoglobin variants. Arch Pathol Lab Med. 2013;137(12):1788-91. doi:10.5858/ arpa.2012-0714-OA.
11. Latzig DL, Baynes SC, Feuerhake T, Gunsolus IL. Evaluation of local hemoglobinopathy prevalence and promotion of accurate hemoglobin A1c testing using historical data retrieval. Clin Biochem 2023;114:59-62. doi:10.1016/j.clinbiochem.2023.02.001.
12. Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood and Hemolysate Application Order Information (cobas c 111) 2022-02, V3.0 English 1-6.
13. Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood Application – Standardized according to IFCC transferable to DCCT/NGSP Order Information (COBAS INTEGRA 400 plus) 2022-02, V3.0 English 1-6.
14. Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood Application Order Information (cobas c 311, cobas c 501/502) 2022-02, V3.0 English 1-6.
15. Beckman Coulter, Inc. USA. AU US Instructions For Use (AU400/ AU480, AU640e/680, AU2700/AU5400/AU5800 and DxC 700 AU Beckman Coulter Analyzers) 2020 1-19.
16. Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1cDx Gen.3 2021-02, V1.0 English.
17. Siemens Healthcare Diagnostics Inc. USA. Enzymatic Hemoglobin A1c (A1c_E) High-Volume Assay (Atellica CH Analyzer) 2021; Revy.03:1-20.
18. HbA1c Assay Interferences. Ngsp.org. Accessed March 25, 2024. https://ngsp.org/interf.asp.
19. Sebia France. Capi 3 Hb A1c Using the Capillarys 3 Tera Instrument Family. (US English release) 2019 1-23.
20. McCurdy PR. 32-DFP and 51-Cr for measurement of red cell life span in abnormal hemoglobin syndromes. Blood. 1969;33(2):214-24.
21. SUAREZ RM, BUSO R, MEYER LM, OLAVARRIETA ST. Distribution of abnormal hemoglobins in Puerto Rico and survival studies of red blood cells using Cr51. Blood. 1959;14(3):255-61.
22. Lacy ME, Wellenius GA, Sumner AE, et al. Association of Sickle Cell Trait With Hemoglobin A1c in African Americans. JAMA 2017;7;317(5):507-515. doi:10.1001/jama.2016.21035.
23. ElSayed NA, Aleppo G, Aroda VR, et al. 6. Glycemic Targets: Standards of Care in Diabetes-2023. Diabetes Care. 2023;1;46(Suppl 1):S97-S110. doi:10.2337/dc23-S006.
24. Guimarães JS, Cominal JG, Silva-Pinto AC, et al. Altered erythropoiesis and iron metabolism in carriers of thalassemia. Eur J Haematol 2015;94(6):511-8. doi:10.1111/ejh.12464.
25. Fucharoen S, Viprakasit V. Hb H disease: clinical course and disease modifiers. Hematology Am Soc Hematol Educ Program. 2009:26-34. doi:10.1182/asheducation-2009.1.26.
26. Karimi SS, Jin M, Murga-Zamalloa C. Analytical and Clinical Significance of Rare Hemoglobin Variants during HbA1c Monitoring in Patients with Diabetes Mellitus: Two Cases of Hemoglobin G-Ferrara and Hemoglobin G-Copenhagen in Diabetic Patients with Sickle Cell Trait. J Appl Lab Med. 2023;6;8(2):407-412. doi:10.1093/jalm/jfac135.
27. Higgins T, Stewart D, Boehr E. Challenges in HbA1c analysis and reporting: an interesting case illustrating the many pitfalls. Clin Biochem. 2008;41(13):1104-6. doi:10.1016/j.clinbiochem.2008.06.005.
28. Adekanmbi J, Higgins T, Rodriguez-Capote K, et al. Erroneous HbA1c results in a patient with elevated HbC and HbF. Clin Chim Acta 2016;1;462:153-157. doi:10.1016/j.cca.2016.09.017.
29. Kangastupa P, Åkerman K, Risku S, et al. The prevalence of hemoglobin Tacoma in Finland detected by HbA1c capillary electrophoresis. Scand J Clin Lab Invest. 2023;83(1):51-57. doi:10.1080/00365513.2022.2164739.
30. Rhea JM, Molinaro R. Pathology consultation on HbA(1c) methods and interferences. Am J Clin Pathol. 2014;141(1):5-16. doi:10.1309/ AJCPQ23GTTMLAEVL.
31. Shimizu S, Taira A. Two Non-diabetic Cases of Variant Hemoglobin Treated with Oral Hypoglycemic Agents Due to Spurious HbA1c Elevation. J Jpn Diabetes Soc. 2015;58(2):121-127.
32. Van Den Ouweland J, Van Daal H. The silent hemoglobin alpha chain variant Hb Riccarton [alpha51(CE9)Gly-->Ser] may affect HbA1c determination on the HLC-725 G7 analyzer. Clin Chem Lab Med. 2008;46(6):827-830.
33. Yang X, Zeng X, Zhang Y, Kuang W, He D. Evaluation of interference from 16 hemoglobin variants on hemoglobin A1c measurement by five methods. Scand J Clin Lab Invest. 2023;83(1):18-22. doi: 10.1080/00365513.2022.2155990.
34. Rodríguez-Capote K, Estey MP, Barakauskas VE, et al. Identification of Hb Wayne and its effects on HbA1c measurement by 5 methods. Clin Biochem. 2015;48(16-17):1144-50. doi:10.1016/j.clinbiochem.2015.07.100.
35. Sacks DB, Arnold M, Bakris GL, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2011;34(6):e61-99. doi:10.2337/ dc11-9998.
36. NGSP CAP Survey Data. Ngsp.org. Accessed March 25, 2024. https:// ngsp.org/CAPdata.asp.
37. EurA1c trial. Ifcchba1c.org. Accessed March 25, 2024. https://www. ifcchba1c.org/GeneralInformation.aspx?I=17.

Matthew C. Wagner PhD received his PhD in Chemical Engineering in 2006 from Georgia Institute of Technology. Since transitioning to industry, he works as a Scientific Affairs Specialist for Sebia Electrophoresis, provider of capillary and gel electrophoresis assays, including Capillary Hemoglobin A1c.

Manual entry of proficiency testing results is a time-consuming process and prone to errors. DataDirect utilizes the ability of your LIS to run a report and create a data file which is then uploaded onto API’s website. This process removes the need for manual entry, saves time, and eliminates the number one cause of proficiency testing failures, clerical errors!
The process is simple
HOURS







It’s back! Dear API Abby is here to answer a series of commonly asked questions about laboratory quality. This time, the American Proficiency Institute (API) is offering its technical expertise to respond to questions about the CLIA final rule on proficiency testing (PT) analytes and acceptable performance. The American Proficiency Institute, a global leader in proficiency testing programs, is dedicated to improving the accuracy and efficiency of clinical laboratory testing. Known for its constant innovation in the field, API offers technical expertise and checklists to help its laboratory customers become more proficient.
Dear API Abby:
It seems like it’s been a while since the federal government ordered laboratories to make proficiency testing changes. I’m responsible for ordering PT programs for my laboratory, but nobody has told me what needs to change. Would you tell me what I need to do? I want to be in compliance!
Dear Law-Abiding:
Kudos to you for keeping up with the latest regulatory activities! We understand the confusion. The Centers for Medicare & Medicaid Services (CMS) issued a final rule on July 11, 2022, that updated the CLIA regulations related to PT analytes and acceptable performance. The final rule went into effect a month later in 2022, but many of the provisions will be implemented on January 1, 2025.
CMS recognized that preparation was needed on the part of laboratories, proficiency testing providers, accrediting organizations, surveyors, and exempt States before all provisions were ready to go. This two-year time period allows PT providers time to produce appropriate samples and update their analyte scoring and reporting requirements. It gives laboratories, like yours, time to enroll in the new, and sometimes revised, PT programs.
What do you need to do? Ahead of your 2025 enrollment, start identifying analytes that you test that have been added to the required list in the final rule.You should expect details




We make diagnostics that matter

We recognize your passion for providing high quality care to patients displaying symptoms associated with respiratory infections, and we appreciate your efforts and resiliency working to reduce the number of people impacted by their spontaneous and rapid spread.
We are committed to providing high quality, molecular and antigen point-of-care tests for detecting the most common causes of respiratory infections, so you can get the answers fast and your patients back to doing what they love.
Like you, we understand there is a patient behind every answer—and that’s what matters most.
For more information, call 800-332-1042, or scan QR code



about changes to PT programs as the enrollment period draws near. Keep an eye on your PT provider’s website; most have already posted information about the CLIA changes.
Dear API Abby:
As a medical laboratory scientist of long standing, I’m well aware of the analytes that require PT under CLIA. I understand the final rule has changed the list of required analytes. Would you explain the change and which analytes are now on the list? Coming Up to Speed
Dear Compatriot:
Indeed, a few decades have passed since the initial list of required PT analytes was mandated. CMS and the Centers for Disease Control and Prevention (CDC) undertook an extensive review of the analytes to determine which ones should remain on the list, which ones should be deleted, and what new analytes should be added.

The newly required analytes are as follows: General Immunology: C-reactive protein (high sensitivity), Anti-HBs, Anti-HCV
Routine Chemistry: B-natriuretic peptide (BNP), NT proBNP, Carbon dioxide (CO2), Cholesterol, low density lipoprotein (LDL), (direct measurement), Ferritin, Gamma glutamyl transferase (GGT), Hemoglobin A1c, Phosphorus, Prostate specific antigen (PSA) total, Total iron binding capacity (TIBC) (direct measurement), Troponin I, Troponin T
Endocrinology: Cancer antigen (CA) 125, Carcinoembryonic antigen (CEA), Estradiol, Folate, serum, Follicle stimulating hormone (FSH), Luteinizing hormone, Parathyroid hormone, Progesterone, Prolactin, Testosterone, Vitamin B12
Toxicology: Acetaminophen, serum, Salicylate, Vancomycin
Hematology: Blood cell identification, White blood cell differential, Erythrocyte count, Hematocrit (excluding spun microhematocrit), Hemoglobin, Leukocyte count, Platelet count, Fibrinogen, Partial thromboplastin time, Prothrombin time (seconds or INR)
Although both blood cell identification and white blood cell differential have always been scored, only one of the scores was sent to CMS — even if laboratories reported both in their PT results. The final rule changes this practice so that now both scores will be sent to the agency.
The final rule also states that laboratories must report prothrombin time in the same way as they report patient results. This means that in addition to seconds, units of reporting for prothrombin time can include INR (international normalized ratio), which was previously not considered regulated. Laboratories not currently testing five samples, three times a year for INR will need to enroll in the appropriate PT program.
Dear API Abby:
To PT or not to PT, that is my question. It seems that there are more analytes being scored for microbiology, but we’ve been ordering proficiency testing programs for each microbiology subspecialty. How do these changes affect us?
The Hamlet of PT
Dear Hamlet:
Thou shalt PT, Dear Hamlet! You are perceptive though regarding changes in the microbiology proficiency testing requirements.
Within each subspecialty (bacteriology, mycobacteriology, mycology, parasitology, and virology), laboratories are responsible for ensuring that various types of testing are included. The final rule adds some new types of testing to some subspecialties.
Newly scored analytes include Gram Stain morphology, bacterial toxin detection (e.g. C. difficile and Shiga toxins), mycology and parasitology antigen testing (e.g. Cryptococcal and Trichomonas antigens), molecular detection of Mycobacterium tuberculosis, and molecular detection of parasites, yeast, and fungi. The final rule also requires antimicrobial susceptibility testing to be reported on two samples per test event, covering both Gram positive and Gram negative organisms. Another change is that mycobacterial susceptibility is no longer scored, so those scores will not be shared with your accreditation agency come 2025.
So, dear Hamlet, what does all this mean for you? Your proficiency testing order actually might stay the same, though your PT provider may increase the number of samples included in each test event to meet the minimum requirement. Nonetheless, it would be prudent for you to review your order against these changes to make certain your laboratory remains in compliance. Lastly, since you’ve probably already been testing and reporting results for these analytes, but they are now regulated, results for these analytes will now be included in your overall score for each subspecialty that is shown on your evaluation.
Dear API Abby:
I aim to submit my proficiency test results completely and accurately each and every time! Admittedly, sometimes, I want to make a correction or add information after the testing due date. Am I allowed to do so or may my proficiency testing provider do it for me? Only Human
Dear Only Human:
We can certainly sympathize with being human and the pressure not to make mistakes. However, CLIA does not allow laboratories or PT providers any latitude after the due date for results. The final rule reinforces this and states, “it is not appropriate for a PT program to change or add information on the PT result submission from a laboratory, including, but not limited to, the testing methodology, results, data, or units.” So, this is a strong line not to cross.
It is important to read instructions carefully to ensure you are reporting in the correct units and selecting the appropriate method. Reach out to your PT provider if your unit of measure or method is not listed. You may be asked to document this information with your results. Always proof your completed results carefully prior to submitting. If you happen to find a correction after you submitted but before the due date, your PT provider can likely help you. Unfortunately, after the due date everything must be considered your “final answer”!
Dear API Abby:
In addition to changes in the list of regulated analytes, the final rule adjusts what is considered acceptable performance. What does this mean for my laboratory?
Dear All Together:
You’re right, the final rule makes changes to proficiency testing acceptance limits (grading criteria). The new criteria are designed to reflect the analytic accuracy of methods employed today and set percentage or concentration units for all analytes, rather than using standard deviation as the grading criteria. For example, the grading criteria for TSH will change from target value ± 3 SD to target value ± 0.2mIU/l or 20% (greater). Two benefits of set percentage or concentration limits are that 1) they can be tied to objective goals for performance within the laboratory, and 2) they ensure the same evaluation criteria are used by all PT programs.
Our best advice to help your laboratory prepare for these changes is to review past PT evaluations or watch your PT performance carefully this year. Get the most out of your PT by looking deeper than your 100% scores to see how close your results are to the mean. Investigate any passing results that are not as close to the mean as your other results. While one different result can happen by chance, any trends above and below the mean, or at the high or low end of your measurable range, are potential candidates for improvement that could benefit your patients and get you in the best shape for 2025.





In recent years, advancements in technology and workflow automation have been revolutionizing the landscape of medical diagnostics, giving rise to the concept of “Dark Labs.” The potential of fully automated labs, sometimes referred to as “Dark Labs,” represents a novel, and perhaps inevitable, way to address the increasing pressure and decreasing labor force faced by diagnostic laboratories. These state-of-the-art facilities are designed to function without regular human intervention, harnessing the power of robotics, artificial intelligence (AI), and advanced data analytics. By mitigating the current challenge of staff shortages while also potentially addressing human errors like mislabeling, Dark Labs have the potential to revolutionize diagnostic laboratories and significantly enhance the accuracy, efficiency, and speed of medical testing. This article delves into the existing roles within traditional diagnostic laboratories and explores the disruptive automation technology needed to replace and/or augment these roles to usher in a new era of efficiency and accuracy in an age of workforce scarcity.
Weltpremiere - Labor Hamburg - MEDILYS Laborgesellschaft mbH. Medilys.de. Accessed March 20, 2024. https://www.medilys.de/weltpremiere/.
One of the most pressing issues in diagnostic laboratories worldwide is the shortage of skilled medical technologists. The healthcare industry has been grappling with this challenge for years, leading to delays in test results; increased workloads on existing staff; and compromised accuracy due to fatigue, burnout, and turnover. Dark Labs offer a promising solution by reducing the reliance on human personnel.
In Dark Labs, robots and automation systems take on the role of preparing and processing samples, managing consumables, and even analyzing results. This not only speeds up the testing process but also minimizes the need for a large number of skilled technicians. The available staff can focus on more specialized tasks that require human expertise, such as interpreting complex results and making critical decisions. By alleviating the burden on human workers, Dark Labs ensure that diagnostic procedures are carried out efficiently and accurately.


The ACL TOP Family 50 Series offers the most advanced automation and quality management for routine and specialty Hemostasis testing in mid- to high-volume labs. All models are standardized and offer automated pre-analytical sample integrity checks to identify under-filled sample tubes, abnormal sample aspiration potentially caused by clots, and assay-specific interference from hemolysis, lipemia and bilirubin. Plus, lab accreditation tools make compliance easier. Better efficiency and quality management for you—better quality care for your patients.
The ACL TOP Family 50 Series. Quality in. Quality out.
Human errors, such as mislabeling samples, transcription mistakes, and calculation errors have been a recurring challenge in traditional diagnostic laboratories. These errors not only compromise patient safety but also lead to retesting, delays, and increased healthcare costs. Dark Labs can substantially reduce the risk of human errors by implementing stringent automation protocols. Also, the presence of humans in the lab increases the risk of workplace and sample contamination especially as labs bring in more molecular testing modalities.
Samples in Dark Labs can be processed through automated systems that are designed to handle a wide variety of tests and tubes. With the integration of barcode and RFID technologies, samples are identified and tracked from the moment they enter the lab until the final results are generated. With modern, fully automated solutions, the whole workflow from sample arrival, centrifugation, decapping, testing, and disposal can be managed by intelligent total laboratory systems.

the operation of instruments, automation scheduling, routine maintenance, and service requests if process abnormalities are detected.
Traditional diagnostic labs often struggle with lengthy turnaround times for test results, which can lead to delays in treatment and patient management. Dark Labs excel in efficiency and speed, addressing these concerns head-on. Automated systems can more easily process a high volume of samples simultaneously, reducing the time required for testing. Moreover, AI and auto-verification algorithms can quickly analyze data and generate reports, further expediting the diagnostic process.
In semi-Dark Labs, which represent a hybrid approach, some tasks are automated while others involve human oversight. This allows for greater flexibility, as certain complex or novel cases may still benefit from human intervention. The efficiency of Dark Labs can also extend to remote areas where access to specialized diagnostic services is limited. By enabling sample collection centers to connect with fully automated labs, patients in remote locations can receive timely and accurate results without the need for extensive travel.
Dark Labs are not only about automation; they also harness the power of data analytics to provide valuable insights. The vast amount of data generated during the diagnostic process can be used to identify trends, patterns, and correlations that might otherwise go unnoticed. With the help of AI algorithms, Dark Labs could predict disease outbreaks, identify high-risk populations, and contribute to epidemiological research. Additionally, predictive analytics can aid in optimizing lab resources. By analyzing historical data on testing patterns and seasonal variations, Dark Labs can proactively allocate resources to ensure efficient operations during peak demand periods. This level of foresight is crucial for maintaining a smooth workflow and minimizing bottlenecks. In addition to patient-centric metrics, the predictive analytics can monitor
While the potential benefits of Dark Labs are vast, their implementation is not without challenges. The initial setup cost of fully automated systems requires up front investments in vessel moving, robotics, AI technology, and infrastructure. These costs may occur before the reduction in staffing costs due to a hybrid phase while laboratories transition between the two operating models. Moreover, processes such as inventory replenishment, routine maintenance, sample loading and


others do not currently have standardized, readily available solutions. There is also a need for specialized training for the personnel overseeing the automated processes and managing technical issues.
The transition to Dark Labs might lead to concerns about job displacement for laboratory technicians. However, Dark Labs enable higher throughput so labs can be more productive processing more samples with the same number of staff. In addition, existing staff are freed up to perform more specialized roles or carry out other testing modalities. Technicians could

be upskilled to manage the additional types of technology used in their new, more-automated environment.
Dark Labs represent a potential transformative shift in the diagnostic laboratory landscape. By harnessing the power of automation, robotics, and AI, these labs offer a solution to the persistent challenges of staff shortages and human errors. The benefits extend beyond increased efficiency and accuracy; they encompass enhanced speed, data-driven insights, and predictive analytics. As technology continues to evolve, Dark Labs could become an integral part of the healthcare infrastructure. Through careful implementation and continuous refinement, this technology could revolutionize the way medical tests are conducted and diagnoses are made.

Mike Heydlauf is a Senior Key Expert at the Center for Innovations in Diagnostics at Siemens Healthineers . He has been working in laboratory automation and informatics for over 18 years and is a member of IFCCs Committee on Mobile Health and Bioengineering in Laboratory Medicine and an advisor on CLSI’s Expert Panel on Automation and Informatics (AUTO).

Mark Edwards, PhD CEng FIET is a Principal Key Expert at Siemens Healthineers specializing in mechatronics, automation, and workflow solutions in Laboratory Diagnostics. Mark, a Fellow of the Institute of Engineering and Technology, has spent over 30 years designing and implementing the latest technologies to enable better outcomes for patients and the clinicians that care for them.














When expressing the breadth of the risk of sexually transmitted infections (STIs), a colleague of mine often shares the stark perspective, “If you’re having sex, you’re at risk.” And she’s right. While sex is rarely discussed in an open and candid fashion, it is important to remember that sexual health is health , and encompasses all aspects of human sexuality. Sexual health and satisfaction are key components of health and well-being.1 We are accustomed to thinking about sexual health as the presence or absence of disease — namely sexually transmitted infections. But the WHO defines sexual health as “a state of physical, emotional, mental, and social well-being,” which includes aspects such as reproductive health, access to education and care, and sexual experience free of coercion, discrimination, and violence, among others. 2 This emerging, broader conversation around sexual health is rooted in changes in communication — the more we talk about it, the more informed we are. The more informed we are, the more we can reduce the stigma associated with sexually transmitted infections and improve the uptake of testing.

syphilis, and human papillomavirus (HPV), the plan serves as a roadmap to help federal and non-federal stakeholders at all levels and in all sectors achieve the vision of making the United States “a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention, care and treatment while living free from discrimination.”
Sexually transmitted infections are inclusive of viruses, bacteria, protozoa, and parasites people can contract through sexual contact. And many STIs have no symptoms, resulting in asymptomatic infections.3 The burden of STIs in the United States is astounding. One in five people in the U.S. have an STI, equating to 68 million infections4 and $16 billion in direct medical costs per year.5 While it’s true if you are having sex you are at risk, some populations are disproportionately affected by STIs, including young people aged 15–24, gay and bisexual men, pregnant people, and racial and ethnic minority groups.6 The CDC has recommended that STIs be a top public health priority as rates of many STIs continue to increase7 despite available treatment options. Left undiagnosed or untreated, STIs can lead to harmful and lasting consequences, such as infertility, ectopic or adverse pregnancy outcomes, congenital infection, chronic pelvic pain, increased risk of HIV infection, and psychological harm through stigmatization.5 These consequences are unacceptable in a world where many STIs are treatable. In 2021, the U.S. Department of Health and Human Services (HHS) launched a first-of-its-kind national strategic plan aimed at reversing “the recent dramatic rise of STIs in the United States.”8 Focused on chlamydia, gonorrhea,
This plan’s vision and goals cannot be achieved without the important role of the diagnostics industry — supporting increased screening volumes, developing medically relevant assays and claim extensions, and advancing new technologies to support point-of-care testing, self-collection, and rapid antibiotic susceptibility testing.
Diagnosing STIs is important — because if we test, we can cure or treat, therefore reducing transmission. But challenges remain. Testing underutilization can lead to overtreatment or undertreatment of the infection, and this is if patients even have access to fast and accurate diagnostic solutions. Additionally, similar to respiratory infections, overlapping symptoms among STIs make empirical diagnosis challenging, therefore requiring appropriate diagnostic testing performed in clinical settings. In a real-world study analyzing more than 23 million instances of patients presenting with symptoms of a urogenital condition, 89% of patients who received antibiotics received their treatment within the first three days of their initial appointment, likely before results from CT (Chlamydia trachomatis)/NG (Neisseria gonorrhea) testing would be available. This data points to presumptive therapies for diseases that should be tested for and treated accordingly, contributing
to suboptimal antimicrobial and diagnostic stewardship. Due to the overlapping symptoms and varying treatment pathways across common STIs including CT, NG, MG (Mycoplasma genitalium), and TV (Trichomonas vaginalis), definitive diagnosis is critical to making treatment decisions.9 The study, which analyzed STI testing and treatment patterns in the United States, also showed that fewer than 2 in 10 individuals received CT/NG testing, despite showing symptoms,9 further demonstrating the underutilization of STI testing. Rapid and accurate STI testing is needed to inform appropriate treatment recommendations and prevent further transmission. And this is where point-of-care testing can emerge to fight this epidemic, providing broader access, faster testing, and a definitive diagnosis in less than 30 minutes.10
The COVID-19 pandemic accelerated the use of molecular diagnostics at the point of care, allowing the technology to meet evolving customer needs for quick and accurate results, improve the patient diagnostic experience, and increase operational efficiency for providers. Currently, a majority of STI testing is done in a central lab, with CDC guidelines recommending screening for asymptomatic individuals based on a variety of different risk factors. Given these tests are standard and routine, high-throughput testing is more economical, with up to 96 samples tested at once instead of one every half hour. However, for symptomatic patients in certain settings, STI testing at the point of care allows for a seamless connection of gold-standard molecular diagnostics and treatment. In less than 30 minutes,10 a patient can learn what they may have contracted and how to treat it. With the closure of STI clinics,11 in addition to changes in how people access healthcare, more patients are using point-of-care settings, such as urgent care, emergency departments, women’s health clinics, primary care physician offices, and public or student health clinics for diagnosis and treatment. In addition to its high specificity and sensitivity across a variety of diseases, molecular point-of-care testing is evolving to meet customer needs, providing rapid results directly at the site of care, and oftentimes, for multiple disease targets in one assay. Patients can also benefit from the opportunity to receive treatment during the same visit. Using PCR (polymerase chain reaction) technology, previously only used in the lab, molecular point-of-care testing provides the same high level of accuracy as the lab in a CLIA-waived setting,12 offering clinicians a high degree of confidence in diagnosis. This test-to-treat approach can help combat potentially high loss to follow-up rates making treatment more likely and contribute to thoughtful antibiotic and diagnostic stewardship efforts. Additionally, point-of-care testing has the potential to address barriers in access to care and treatment. By meeting patients where they are, through easily accessed sites of care or organized community outreach, providers have the potential to reach a variety of populations at-risk for STIs, including underserved populations who may have difficulty accessing care or those who face a variety of stigmas and discrimination.
What the future of molecular point-ofcare testing means for sexual health Laboratorians, clinicians and leaders in healthcare settings can also find value in molecular point-of-care testing beyond STI diagnosis. With already FDA-approved, CLIA-waived assays for a range of respiratory infections, an investment
in decentralized, molecular point-of-care testing has the potential to meet the same-visit diagnosis demand from patients and alleviate staffing strains due to the simplicity of the tests, freeing up laboratorians to address more complex tasks requiring highly-trained professionals. To date, there are only two FDA-approved tests to diagnose STIs at the point-of-care, including a CT/NG/TV assay and a CT/NG assay – both of which have limited indications compared to the epidemic the U.S., and the world, are facing. However, innovation in this space is well underway, and I expect one day there is the potential for molecular pointof-care testing to cover the whole spectrum of STIs, including expansion to genital lesions, mpox, causes of vaginosis or even HIV. By making STI testing more accessible, and therefore immediately treatable, there is an opportunity to stop this epidemic in its tracks. And no matter our role in implementing molecular STI testing at the point of care, let’s continue to speak up and advocate for sexual health for all. For more information on Roche’s commitment to sexual health, visit https://diagnostics.roche.com/us/en/products/ product-category/sexual-health.html.
1. Ueda P, Mercer CH, Ghaznavi C, Herbenick D. Trends in Frequency of Sexual Activity and Number of Sexual Partners Among Adults Aged 18 to 44 Years in the US, 2000-2018. JAMA Netw Open 2020;1;3(6):e203833. doi:10.1001/jamanetworkopen.2020.3833.
2. Sexual health. Who.int. Accessed April 1, 2024. https://www.who.int/ health-topics/sexual-health.
3. Centers for Disease Control and Prevention. STDs - Diseases & Related Conditions. cdc.gov. Updated July 7, 2023. Accessed March 26, 2023. https://www.cdc.gov/std/general/default.htm.
4. Diseases & related conditions. Cdc.gov. Published July 7, 2023. Accessed April 1, 2024. https://www.cdc.gov/std/general/default.htm.
5. CDC. STI prevalence, incidence, and cost estimates infographic. Centers for Disease Control and Prevention. Published January 25, 2021. Accessed April 1, 2024. https://www.cdc.gov/std/statistics/ prevalence-2020-at-a-glance.htm.
6. The state of STIs - infographic. Cdc.gov. Published December 19, 2023. Accessed April 1, 2024. https://www.cdc.gov/std/statistics/infographic.htm.
7. Sexually transmitted infections surveillance, 2022. Cdc.gov. Published January 29, 2024. Accessed April 1, 2024. https://www.cdc.gov/std/ statistics/2022/default.htm.
8. Office of Infectious Disease, HIV/AIDS Policy (OIDP). STI national strategic plan overview. Hhs.gov. Published June 19, 2019. Accessed April 1, 2024. https://www.hhs.gov/programs/topic-sites/ sexually-transmitted-infections/plan-overview/index.html.
9. Lillis R, Kuritzky L, Huynh Z, et al. Outpatient sexually transmitted infection testing and treatment patterns in the United States: a real-world database study. BMC Infect Dis. 2023;13;23(1):469. doi:10.1186/s12879-023-08434-2.
10. Point of care tests. Who.int. Accessed April 1, 2024. https://www.who. int/teams/sexual-and-reproductive-health-and-research-%28srh%29/ areas-of-work/sexual-health/sexually-transmitted-infections/ point-of-care-tests.
11. Blachford A. The rising importance of urgent care in the fight against the STI epidemic. Journal of Urgent Care Medicine. Published November 30, 2022. Accessed April 1, 2024. https://www.jucm.com/the-risingimportance-of-urgent-care-in-the-fight-against-the-sti-epidemic/.
12. Hansen G, Marino J, Wang ZX, et al. Clinical Performance of the Point-of-Care cobas Liat for Detection of SARS-CoV-2 in 20 Minutes: a Multicenter Study. J Clin Microbiol. 2021;21;59(2):e02811-20. doi:10.1128/JCM.02811-20.

Allison McMullen PhD, D(ABMM) is a Scientific Partner for Molecular Diagnostics and Infectious Diseases in Medical and Scientific Affairs, a non-commercial division of Roche Diagnostics She is the subject matter expert for Roche’s sexual health and cervical cancer solutions. Before joining Roche, Allison was the Medical Director of Microbiology at Augusta University Medical Center.


Hemostasis solutions from the #1 trusted brand in hematology*



Sysmex has been innovating hemostasis analyzers for more than 30 years, offering complete, easy-to-use hemostasis solutions for laboratories of all sizes and complexities.
The Sysmex CS-2500™ Automated Blood Coagulation Analyzer incorporates coagulation, chromogenic, immunoturbidimetric and aggregation** methodologies in full random access. Pre-analytical sample checks provide autovalidation without the need for manual sample handling.
with
A trusted reagent portfolio, coupled with the service you expect from Sysmex, ensures that the integration of hemostasis into your laboratory will be a pain-free experience.
A tru you of he expe
* 2023 IMV ServiceTrak™ Annual Survey for Hematology
** For research use only, not for use in diagnostic procedures. RUO assays must be validated before use in clinical practice. www.sysmex.com/us

As a woman ages, the consistency of ovulation and/or availability of viable oocytes (eggs) decreases, leading to difficulty in becoming pregnant. The current trend of women choosing to wait to have children until later in life has thus resulted in a larger number of women experiencing infertility and seeking in vitro fertilization (IVF) treatments at fertility clinics. Following an initial consultation with a reproductive endocrinologist, one of the first steps in IVF is an assessment of ovarian reserve — defined as the quantity and quality of remaining oocytes (eggs). The results of this testing can then be used to develop a personalized treatment plan for IVF, including consultation about the likelihood of success. One common tool used to evaluate ovarian reserve is a clinical laboratory test that measures anti-Müllerian hormone (AMH).
What is AMH?
AMH, also known as Müllerian-inhibiting hormone (MIH), is a 140 kDa glycoprotein of the transforming growth factor beta (TGF- family), produced by the Sertoli cells in males
and granulosa cells of developing follicles in females
(See Figure 1).
The role of AMH is different in males and females. AMH plays a crucial role in male sex differentiation during fetal development. In males, Sertoli cells secrete AMH during the early stages of development, leading to regression of the

Müllerian ducts; hence the name, anti-Mullerian hormone.1 In the absence of AMH, the Müllerian ducts will develop into the uterus and fallopian tubes.
The presence of AMH has been observed as early as 32 weeks gestation in females, and plays a crucial role during folliculogenesis, the maturation of ovarian follicles into mature eggs. Ovarian follicle maturation is on-going; thus, at any given time within the ovary, there are multiple follicles in various stages of development, beginning as primordial follicles and developing into large preovulatory follicles ready for fertilization. A key difference in the formation of male gametes (sperm) and female gametes (eggs) is that women are born with a finite number of eggs averaging approximately 500,000 to 1 million oocytes in the form of primordial follicles.2 Several large studies have demonstrated that the number of primordial follicles immediately declines after birth and approaches nearly zero around age 50 (See Figure 2).3,4 Throughout the lifetime of a healthy female, only a very small fraction (approximately 0.1%) will develop into a fertilizable egg.
Antral follicle
Folliculogenesis begins with the recruitment of a subset of primordial follicles for further development and is regulated by several hormones including follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone. The selected primordial follicles grow and develop into primary, secondary, and then antral follicles. During this time, the AMH-producing granulosa cells proliferate to form multiple layers around the oocyte. Ultimately, one follicle becomes dominant and continues to grow and mature in a fertilizable egg while the others generally undergo atresia.
The number of primordial follicles recruited each menstrual cycle is dependent on the overall number in the remaining pool. Although primordial follicles are too small to be visualized, the antral follicles are large enough to be visualized using transvaginal ultrasonography (TVUS)5 and can be counted to estimate ovarian reserve. Antral follicle count (AFC) continues to be the gold standard for assessing ovarian reserve but has limitations, such as the requirement of specialized equipment and highly trained staff. Thus, clinical research has focused on identifying a blood-based biomarker that can be used as a surrogate for AFC.
AMH levels have been shown to closely correlate with AFC and have become widely used as a key indicator of ovarian reserve and reproductive potential. Because growing follicles continuously produce AMH (up to ~8mm in size), a decrease in the primordial follicle pool (most often due to naturally occurring fertility changes that happen with aging) will lead to a decrease in the number of growing follicles, and ultimately a decrease in the levels of AMH produced. A higher concentration of AMH means a greater ovarian reserve or number of eggs, while a lower AMH concentration can indicate diminished ovarian reserve or even premature ovarian failure(See Figure 3).6-9
Non-invasive laboratory tests are available to quantitatively measure the amount of AMH in a patient’s blood and provide information on a woman’s ovarian reserve. This becomes important for women presenting to fertility clinics seeking information on their reproductive health. AMH provides advantages over other estimates of ovarian reserve: it’s non-invasive, is less subjective than AFC, which can vary between sonographers, and can be tested at any timepoint throughout the menstrual cycle, unlike FSH. AMH testing also offers wider accessibility, especially in countries or regions with limited resources, as it does not require specialized equipment and highly trained technicians; blood draws can be performed in a variety of healthcare settings. Some in the field predict that AMH may ultimately replace AFC as the gold standard for estimating ovarian reserve.5
Systematic reviews and meta-analyses have shown consistent positive association of AMH and AFC with 1) the intensity of ovarian response, 2) oocyte yield, and 3) live birth in IVF cycles. 10-13 AMH can be used alongside other hormone testing to predict response to ovarian stimulation during IVF. A very low AMH may indicate premature ovarian failure. This information can be used to inform family planning decisions such as whether to proceed with
IVF treatment or pursue other options such as using a donor egg. A low AMH level can also suggest suboptimal response to ovarian stimulation medications administered for IVF whereas as a high AMH may suggest over-response. Using this information, IVF treatment protocols can be tailored to optimize outcomes and reduce the risk of ovarian hyperstimulation syndrome (OHSS), a serious consequence of overstimulation. 11,14
PCOS diagnosis & predictability of treatment. A study in 2016 by Anckaert et. al. demonstrated strong correlation between increased levels of AMH and polycystic ovary syndrome (PCOS), nearly 2-3 times higher than that observed in normal individuals.6 AMH elevation in women with PCOS is due to the increased number of small AMH-producing follicles in the ovary. In 2023, the American Society of Reproductive Medicine (ASRM) included AMH as an alternative to ultrasound in the diagnostic algorithm for PCOS in adults.15 AMH can also be used to predict response to laparoscopic ovarian drilling (LOD), a procedure connected to treatment of patients with PCOS. In cases where an individual is diagnosed with PCOS and has high AMH levels (above 8.3 ng/mL), there is a lower chance that they will respond favorably to LOD.16
AMH continues to be at the center of ongoing research in reproductive medicine to better understand its role in folliculogenesis, ovarian function, reproductive disorders, and the impact on hormone therapy. AMH levels decline as females age, correlating with the natural decline in ovarian reserve as menopause approaches. Monitoring AMH levels may aid in the prediction of menopause and guide family planning. While several studies have been published, use of AMH in this capacity is not yet clear.17
In other research and clinical settings, AMH has been evaluated for its potential use in evidence-based fertility counseling prior to beginning gender affirming hormone therapy in transgender individuals. This can include counseling on either fertility preservation or contraceptive needs. In transgender men (assigned female at birth and transitioning to male), the administration of testosterone can induce amenorrhea and suppress ovarian function, however unplanned pregnancies have been reported.18 Research focused on transmasculine individuals, have shown AMH remains nearly unchanged during the course of high-testosterone treatment.19 This has given insight to cases where some long-term testosterone users have experienced “surprise” ovulation events. Taub et. al., thereby stress the need for larger studies to confirm or clarify these events.
AMH is an established, valuable biomarker in reproductive medicine that provides key information used during both fertility assessments and in the evaluation of reproductive disorders. AMH also can help to personalize patient care by tailoring IVF protocols and PCOS treatments to the needs of the individual patient. The utility of this biomarker for other uses continues to be investigated and for example has shown promise for use in the transgender community by identifying the potential for surprise or unplanned pregnancies and may eventually provide answers to the timing of menopause to inform family planning and health management.
1. Matzuk MM, Lamb DJ. The biology of infertility: research advances and clinical challenges. Nat Med. 2008;14(11):1197-213. doi:10.1038/nm.f.1895.
2. Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril 2020;114(6):1151-1157. doi:10.1016/j.fertnstert.2020.09.134.
3. Park CJ, Oh JE, Feng J, et al. Lifetime changes of the oocyte pool: Contributing factors with a focus on ovulatory inflammation. Clin Exp Reprod Med. 2022;49(1):16-25. doi:10.5653/cerm.2021.04917.
4. te Velde ER, Scheffer GJ, Dorland M, Broekmans FJ, Fauser BC. Developmental and endocrine aspects of normal ovarian aging. Mol Cell Endocrinol. 1998;25;145(1-2):67-73. doi:10.1016/s0303-7207(98)00171-3.
5. Fleming R, Seifer DB, Frattarelli JL, Ruman J. Assessing ovarian response: antral follicle count versus anti-Müllerian hormone. Reprod Biomed Online. 2015;31(4):486-96. doi:10.1016/j.rbmo.2015.06.015.
6. Anckaert E, Öktem M, Thies A, et al. Multicenter analytical performance evaluation of a fully automated anti-Müllerian hormone assay and reference interval determination. Clin Biochem. 2016;49(3):260-7. doi:10.1016/j.clinbiochem.2015.10.008.
7. Faddy MJ, Gosden RG, Gougeon A, Richardson SJ, Nelson JF. Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Hum Reprod. 1992;7(10):1342-6. doi:10.1093/ oxfordjournals.humrep.a137570.
8. Kelsey TW, Wright P, Nelson SM, Anderson RA, Wallace WH. A validated model of serum anti-müllerian hormone from conception to menopause. PLoS One. 2011;6(7):e22024. doi:10.1371/journal.pone.0022024.
9. Xu H, Zhang M, Zhang H, et al. Clinical Applications of Serum Anti-Müllerian Hormone Measurements in Both Males and Females: An Update. Innovation (Camb). 2021;9;2(1):100091. doi:10.1016/j. xinn.2021.100091.
10. Broer SL, van Disseldorp J, Broeze KA, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update. 2013;19(1):26-36. doi:10.1093/humupd/dms041.
11. Broer SL, Dólleman M, Opmeer BC, et al. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta-analysis. Hum Reprod Update. 2011;17(1):46-54. doi:10.1093/ humupd/dmq034.
12. Iliodromiti S, Anderson RA, Nelson SM. Technical and performance characteristics of anti-Müllerian hormone and antral follicle count as biomarkers of ovarian response. Hum Reprod Update 2015;21(6):698-710. doi:10.1093/humupd/dmu062.
13. La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: from theory to practice. Hum Reprod Update. 2014;20(1):124-40. doi:10.1093/humupd/dmt037.
14. Huang J, Lin J, Gao H, et al. Anti-müllerian Hormone for the Prediction of Ovarian Response in Progestin-Primed Ovarian Stimulation Protocol for IVF. Front Endocrinol (Lausanne). 2019;28;10:325. doi:10.3389/ fendo.2019.00325.
15. Teede HJ, Tay CT, Laven J, et al. Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Fertil Steril 2023;120(4):767-793. doi:10.1016/j.fertnstert.2023.07.025.
16. Paramu S. Impact of laparoscopic ovarian drilling on serum anti-mullerian hormone levels in patients with anovulatory Polycystic Ovarian syndrome. Turk J Obstet Gynecol. 2016;13(4):203-207. doi:10.4274/tjod.97523.
17. Nelson SM, Davis SR, Kalantaridou S, et al. Anti-Müllerian hormone for the diagnosis and prediction of menopause: a systematic review. Hum Reprod Update. 2023;2;29(3):327-346. doi:10.1093/humupd/ dmac045.
18. Hahn M, Sheran N, Weber S, Cohan D, Obedin-Maliver J. Providing Patient-Centered Perinatal Care for Transgender Men and Gender-Diverse Individuals: A Collaborative Multidisciplinary Team Approach. Obstet Gynecol. 2019;134(5):959-963. doi:10.1097/ AOG.0000000000003506.
19. Taub RL, Ellis SA, Neal-Perry G, et al. The effect of testosterone on ovulatory function in transmasculine individuals. Am J Obstet Gynecol 2020;223(2):229.e1-229.e8. doi:10.1016/j.ajog.2020.01.059.

JoDell E. Wilson, PhD works as a Medical Science Partner at Siemens Healthineers . Before joining Siemens Healthineers, she served as a Science Director at a large reference laboratory serving the greater part of the United States.





Be ready for anything heading your way with Puritan.® With a wide choice of single-use collection devices and transport systems, including OB/GYN, cervical health, urethral, as well as throat, nasal, and nasopharyngeal swabs, you’ll be well-prepared on your path to finding answers. Available with a variety of tip types and fibers, including our patented PurFlock Ultra® and HydraFlock® flocked swabs. There is a Puritan® device for just about every collection site. Sample with confidence and trust your results.
LEARN MORE ONLINE info.puritanmedproducts.com/ specimen-collection-24
VISIT US
APHL, Booth #215





The results of the 2024 Medical Laboratory Observer (MLO) State of the Industry (SOI) Survey on Lab Management Best Practices reveal how many lab professionals are turning to fundamental practices and priorities to make operational, clinical, and financial improvements – from a focus on staff career development to strengthening supplier relationships.
MLO gathered responses from nearly 100 clinical laboratory professionals with 42% of respondents in director, manager, administrator, or supervisor positions, and most employed by hospitals (61%). Respondents spanned labs of different sizes and testing volumes.
The survey results provide insights into best practices around controlling costs, optimizing contracts, capturing reimbursements, managing supplies, implementing technology solutions, navigating staffing shortages, and improving the quality and efficiency of testing.
Four key findings:
• Staffing : More labs are leveraging career ladder development and flexible scheduling to attract and retain staff members, while fewer are offering financial incentives.
• Technology: Labs are looking for technology to improve quality/reduce costs and/or cover broken/older equipment when prioritizing capital investments.
• Supply chain: The two most leveraged best practices to improve inventory control and consumable supply costs are the evaluation of inventory levels for basic supplies, such as assays and controls/reagents, and the development of supply utilization tracking and record keeping.
• Contracting : More lab professionals are developing good relationships with supplier support personnel to streamline contracting processes, while fewer are working with supply chain management on group purchasing organization (GPO) contracts.
Alongside the quantitative data, the article presents insights from Fontanilla Manliswe, MLS(ASCPi), MSHS(CLS), Director of Laboratory Services, Northern Nevada Medical Center (NNMC); Ryan Stephens, Roche Group Marketing Manager, Automation; and Dan Young, Medline Senior Director, Supply Chain Optimization.

Staffing remains top of mind among lab leaders. When asked which measures they implement to recruit and retain staff, half of survey respondents (50%) said they provide continuing education, which was the same percentage of respondents as last year. Slightly more lab professionals said they are facilitating shift changes to offer employees

scheduling flexibility (12-hour shifts, weekends, etc.), at 44%, up from 40% in 2023.
Career development support is growing in strategic value. Lab professionals reporting they have developed career ladders (structure to encourage professional development, such as from novice to expert) increased 10%, at 40%, up from 30% in 2023.
The percentage of labs that partner with local colleges and technical schools to offer internships remained the same as last year at 38%, while those holding daily huddles with peer recognition dropped only slightly, at 36% in 2024, compared with 38% last year.
Though still high in the rankings, labs offering financial incentives (sign-on bonuses, merit allowances, retention bonuses) to improve staff recruitment and retainment, dropped by more than 10%, at 42% compared with 53% in 2023. Succession-planning processes, where labs offer additional responsibilities to top performers and measure their results, dropped by 10%, at 19%, down from 29% last year.
Lowest in the rankings were labs offering perks, such as free parking, on-site gym, on-site day care, public transportation cost reimbursement, with 17% of respondents reporting their labs use this method to retain and recruit staff, down from 21% in 2023.
Regarding steps they have taken to ensure reimbursement covers their costs, around half of respondents reported they have standardized instrumentation workflows and checklists (58% up from 52% in 2023), created standard lab processes and staff education materials (56% up from 53% in 2023), and incorporated IT solutions to reduce human error (50% up from 40% in 2023).
Use of analyzers that provide walkaway testing to reduce staffing and full-time employee (FTE) hours was also high up on the list at 41% of respondents (up from 39% in 2023). There was a 13% jump in those that have incorporated IT solutions to help keep current with regulations (37% in 2024, up from 24% in 2023). Over a third of respondents (36%) reported using processes to review savings opportunities, such as evaluating analyzers on a regular schedule (up from 28% in 2023).
Approximately one-quarter of lab professionals (26%) reported bringing health screening tests in house (up from 19% in 2023) and/or implementing ongoing waste and efficiency studies to find potential savings in overhead (24%, up from 19% in 2023). Additionally, 21% reported implementing ongoing efforts to reduce coding frustrations and modifications (up from 18% in 2023).
Nearly half (45%) of lab professionals surveyed report being able to track whether reimbursement covers their costs. Of those facing roadblocks with tracking:
• 34% reported not enough staff time (up from 32% in 2023)
• 27% not having software to automate tracking/analysis of costs (down from 35% in 2023)
• 24% lack of interoperability between their laboratory information system (LIS) and revenue cycle management software (down from 34% in 2023)
• 6% not having enough barcoded testing supplies (down from 7% in 2023)
This year, the top two priorities for technology capital investments were reported to be technology needed to improve quality/reduce costs (62% in 2024, down from 70% in 2023), and technology needed to cover broken/older equipment (60% in 2024, up from 38% in 2023).
Next in terms of investment priorities were technology needed to cover staff shortages with automated equipment (40% in 2024, down from 52% in 2023), and technology needed to remain competitive (35% in 2024, down from 42% in 2023).
“Labs of all sizes are adopting automation and digital solutions to simplify their lab operations,” said Ryan Stephens,
Ryan Stephens, Roche Group Marketing Manager, Automation, offered lab professionals these questions to ask when evaluating technology solutions to automate processes:
• How does this automation platform help simplify our day-to-day laboratory operations?
• How does the automation solution adjust to the changing needs of our lab throughout the day?
• Can the automation solution be scaled after implementation to meet our future growth?
• Does the automation solution offer the flexibility to automate multiple disciplines?
• What pre-analytical sample integrity checks are included in the solution?
• How flexible is the automation solution to our lab space restraints? Does it have the ability to create walkways in the lab without reducing our throughput?
• How do you continuously monitor the efficiency of the automation solution?
Figure 1: Have you implemented any of the following to retain and recruit staff?
School partnerships to offer internships
A succession-planning process
Daily huddles with peer recognition
Provide continuing education
Shift changes/scheduling flexibility
Note: Respondents selected all that applied.
0
Roche Group Marketing Manager, Automation. “They’re seeking to improve laboratory efficiency by utilizing fully automated solutions that can be customized to meet their current and future needs.”
“These automated solutions help solve many challenges that labs are facing, including budget constraints and staffing shortages,” Stephens added.“Additionally, the advancement in digital solutions allows laboratories the ability to capitalize on the data that they generate to better support their patient populations.”
To support new technology adoption, 43% of laboratory professionals surveyed reported analyzing workflow processes for proper space planning (down from 55% in 2023), 37% involving the IT department early in the process (down from 51% in 2023), and 21% designating a project manager to coordinate short- and long-term planning and implementation with the vendor (down from 23% in 2023).
Among lab professionals surveyed this year, more than half reported creation of train-the-trainer models as a best practice to train staff on new software (54% down from 57% in 2023), and/or have created standard workflows for all lab employees (52% down from 56% in 2023).
About one-third of respondents said someone in their lab received LIS training to develop an in-house expert (32%, up from 31% in 2023) and/or participated in vendor-hosted, in-house, or online training (30% down from 37% in 2023).
Nearly one-quarter of those surveyed have developed mandatory training led by the IT department for new lab employees (24%, up from 20% in 2023), and 22% reported the development of lunch-and-learn training sessions (up from 15% in 2023).
During her lab’s chemistry instrumentation consolidation, Fontanilla Manliswe sent her staff to vendor training while developing her own knowledge of the technology so that she could serve as a “super user” to support them through the transition and post-implementation.
“At some point, an instrument can go down for any reason and that changes the entire mood for the day,”she stated. “Serving as the single point person and super user, my staff knew I was their lifeline – they could call me, and I would work with them to resolve the issue. And if I didn’t know the answer to a question, I could at least direct them to someone who could help them.”

Nassreen Fontanilla Manliswe, MLS(ASCPi), MSHS(CLS), Director of Laboratory Services, Northern Nevada Medical Center (NNMC), commented on her experience from her previous workplace leading the consolidation of chemistry and special chemistry instruments from seven down to two integrated lines for a 900-bed hospital.
“While the instrument vendor offered a great deal of support, it was critical for our lab to have a point person who could champion and lead the transition,” she said. “At the time we did not have a lab director at that facility and my lab manager’s background was micro, so I became that point person and it was a great learning opportunity.”
Fontanilla Manliswe noted that even if there are clear benefits to implementing new technology, lab staff are likely to resist change because of the learning curve and having to support multiple systems until the transition to the new platform is completed. She stated, “My role at that time was to acknowledge to the team that there were challenges but emphasize the positive aspects of the change and assure them that we could manage it successfully.”
Another best practice for staff training on new technology that Fontanilla Manliswe employed was customizing a standard operating procedure (SOP) to align with her lab’s specific needs.
“The vendor provided SOP templates for the analyzers and instrumentation, but they didn’t necessarily apply to how we use the platforms. I turned to my team members for their input when developing our SOPs so they matched what they were actually doing in the lab in terms of workflows and tasks. This helped tremendously with implementation because when we went live, my team already knew how to follow the SOPs because the information came from them rather than a template.”
Figure 2: What steps have you taken to improve the quality and efficiency of testing?
Standardized test procedures/formularies
Pre-approval program tests are send-outs
Implemented evidence-based test utilization
Temperature monitor equipment/procedures
Staff or committee reviewing SOPs
0








CLSI standards improve laboratory testing quality, safety, and efficiency for a healthier world.
Laboratory science leaders worldwide recognize CLSI standards as the best way to optimize patient care, maintain accreditation, bring products to market faster, and navigate regulatory hurdles.


Learn how!



With regards to steps taken to improve the quality and efficiency of testing, 52% of lab professionals reported using standardized test ordering procedures and formularies (down from 63% in 2023), 48% have implemented staff and committee review standard operating procedures (SOP), and 39% have evaluated temperature monitoring equipment and procedures (down from 51% in 2023).
Other best practices for improved testing quality and safety include implementing evidence-based test utilization backed by data (28% in 2024, up from 27% in 2023) and implementing a pre-approval program for tests that are “send-outs” (14% in 2024, down from 22% in 2023).
Having access to the right supplies at the right times is critical to lab management. While 36% of survey respondents reported having no supply chain issues, the remaining 64% cited best practices they are leveraging to mitigate issues that arise.
Topping the list of best practices is implementation of standing orders (instead of just in time) for crucial supplies at 37%, down from 58% in 2023. Next, utilization of multiple testing platforms at 30%, down from 44% last year. Lab professionals reporting the switch from disposable to reusable personal protective equipment (PPE), such as lab coats, increased, at 20%, up from 14%.
When asked what steps they have taken to improve inventory control and consumable supply costs, inventory evaluation of basic supplies, such as assays and controls/reagents, garnered the highest percentage of responses, at 69% (down from 74% in 2023). Nearly half of respondents (46%) have developed supply utilization tracking and record keeping (up from 39% in 2023).
Close to one-quarter (24%) of lab professionals reported having worked with other members of their organizations, such as the chief medical officer (CMO) and physicians, to standardize test ordering throughout the organization (up from 20% in 2023). Among those surveyed, 20% have secured access to electronic inventory tracking from the supply chain/ materials management department (up from 18% in 2023) and 19% have developed ongoing review comparing supply reports to the number of invoiced tests (down from 20% in 2023).
Fewer respondents report having implemented lease agreements that do not include volume commitments, compared with last year (14% in 2024, down from 18% in 2023) and/or implemented vendor-managed ordering (12% in 2024, down from 15% in 2023). An additional 12% indicated tasks related to inventory control and consumable supply costs are handled by a different organization/location.

There was a big drop in survey respondents who reported working with state public health officials to gain access to needed testing supplies, at 16%, down from 31%. Those using laboratory-developed tests to address supply-chain issues changed little, 13% in 2024 compared with 14% in 2023.
In general, supply shortages have eased according to Fontanilla Manliswe, but her lab and others were surprised by the intensity of the increase in SARS-CoV-2 testing volume during December 2023-January 2024. She stated:
“We use a 4-plex assay and we expected an increase but did not expect the level of the increase in need for COVID-testing earlier this year. I monitor supplies almost every other day and found each of our locations – labs in our two main hospitals and two freestanding ERs – were each consuming one box per day during December and January. It was not just our lab that was understocked; it happened all over. Labs were on allocation until February.”
Fontanilla Manliswe offered her best practice in lab supply management: making supply monitoring everyone’s responsibility, not just that of the lab manager and department leads. She explained how empowering technologists to monitor supply levels not only helps a lab avoid stockouts, but also helps technologists grow in their responsibilities and experience. She explained how this works:
“We have partnered one or two technologists with leads of each department based on their interests – for instance, one tech might want to help with hematology or chemistry, while another is interested in supporting the blood bank. The techs are responsible for monitoring supplies for their assigned department. Let’s say there are only two boxes left of a certain product. It is the tech’s responsibility to alert me, the manager, or the lead to the low levels so we can get the product ordered before we run out.”
“Lab techs typically have few opportunities for career progression,” Fontanilla Manliswe added. “Simple tasks like supply management can help techs grow toward the possibility of progressing to leads. It also gives them the opportunity to decide whether they really want that level of responsibility.”
Figure 3: What best practices have you developed to train staff on new software?
Train-the-trainer model
Lunch-and-learn training sessions
Mandatory training led by the IT department
Standard workflows for all lab employees
LIS training to develop in-house expert
Vendor-hosted in-house or online training
Other (please specify)
Turning to strategies to streamline contracting processes, 61% of lab professionals report developing good relationships with supplier support personnel to access training and product optimization suggestions, up from 48% in 2023.
The percentage of survey participants who reported working with supply chain management on group purchasing organization (GPO) contracts for additional savings was still high on the list at 55%, but down from 65% in 2023. Fewer lab professionals say they are signing longer contracts (for example, 7 years instead of 1–3 years), at 16%, down from 20% last year.
Ongoing reviews of reference lab costs and contracts continues to be a popular strategy to streamline contracting processes, with 39% of respondents reporting they have implemented this best practice, the same as last year.
Dan Young, Medline Senior Director, Supply Chain Optimization, noted how laboratories can apply lessons learned and best practices from medical/surgical supply management to improve their own supply chain performance. He stated:
“We are seeing some health systems recognize there are ways to apply supply chain best practices they have developed in the acute care space to other areas of spend, in this case labs. It helps the labs do more tests and increase their throughput and efficiency.”
“From a health system leadership standpoint, the more spend you can have under management, the more consistent methodologies and systems can be applied to manage the movement of goods and control of the dollars, and the greater the benefit to the organization overall,” Young added. “I encourage lab managers to ask how they can fit more within their health system’s central supply chain channel so some of the supply management workload can be shifted off their desks. At the same time, centralization can help supply chain leaders generate more savings.”
To alleviate lab teams of supply management, Young also encourages decisions makers to consider vendor-managed inventory programs but notes the importance of maintaining visibility into and control over supply data when taking this approach, stating:
“Having your business partners come in and take care of your inventory is a great way to alleviate some headaches but be sure you keep your arms around the data, including what’s being put into inventory and what you’re consuming.”

Kara Nadeau has 20+ years of experience as a healthcare/ medical/technology writer, having served medical device and pharmaceutical manufacturers, healthcare facilities, software and service providers, non-profit organizations and industry associations.


Advancements in sequencing techniques and the emergence of next-generation sequencing (NGS) technology have transformed laboratory medicine and clinical diagnosis. DNA sequencing results help healthcare professionals in disease diagnosis, prognosis, therapeutic decision, and follow up of patients.1
Sanger sequencing
The first DNA sequencing was conducted in the laboratory of Frederick Sanger and Walter Gilbert in 1977 to sequence bacteriophage X174. This sequencing method became known as Sanger Sequencing. It involves electrophoresis and is based on the random incorporation of chain-terminating dideoxynucleotides (dNTPs) by DNA polymerase during in vitro DNA replication. It is able to read the nucleotide sequence for entire genes (1,000 to 30,000 bases long). After polymerase chain reaction (PCR) technique for DNA amplification emerged in 1983, it became used in DNA sequencing subsequently.2 Automated Sanger sequencing was used to sequence the human genome as part of the Human Genome Project (HGP) that concluded in 2003.3
Though Sanger sequencing is considered as the gold standard in clinical cytogenetics,2 it has the following pitfalls: 3,4
• Can sequence only shorter lengths of DNA up to 800 to 1000 base pairs.
• The quality of the sequence is often not very good in the first 15 to 40 bases because that is where the primer binds.
• Cannot differentiate single base pair differences in longer segments >900 bases.
• Expensive.
From the Human Genome Project, it became known that human gene is made up of 3.1 billion base pairs5 and around
19000 to 20,000 protein-coded genes.6, 7 To utilize this knowledge in the field of diagnosis and treatment, a faster and less expensive sequencing technology was needed — and that led to the development of advanced sequencing technologies, collectively called “next-generation sequencing” (NGS). Figure 1 below captures the major milestones in the sequencing technologies.2
Next-generation sequencing (NGS)
Next-generation sequencing technologies are high-throughput DNA sequencing technologies that are capable of sequencing large numbers of different DNA sequences in a single reaction (i.e., in parallel) and hence often called as massive parallel sequencing or massively parallel sequencing. All NGS technologies monitor the sequential addition of nucleotides to immobilized and spatially arrayed DNA templates but differ substantially in how these templates are generated and how they are interrogated to reveal their sequences.3
1977 Publication of Sanger sequencing method
1983 PCR Technique development
1983 PCR Technique development
2006 The Cancer Genome Atlas (TCGA) pilot project launched
2007 First whole cancer exomes sequenced
2010 Sequencing of 70 whole cancer exomes or genomes
2013 Whole exome of circulating cell free tumor DNA from 6 cancer patients
2016 Somatic genetic landscape from cfDNA from over 15000 patients presented
Based on the read lengths, NGS can be classified as short-length reads or long-length reads. Short-read sequencing is currently the most commonly used for NGS and has a wide range of diagnostic applications. In this type of sequencing, the genome is broken into small fragments – 50 to 300 bases, before being sequenced.8 The technologies carry out sequencing by hybridization or synthesis using DNA polymerase or by ligation using ligase enzyme and extend numerous DNA strands in parallel. Nucleotides can either be provided one at a time, or they can be modified with identifying tags. Short-read sequencing technologies can be further categorized as either single, molecule-based that involve the sequencing of a single molecule or ensemble-based, which is the sequencing of multiple, identical copies of a DNA molecule that have usually been amplified together on isolated beads. Furthermore, these methods could be real-time or synchronous controlled.
Company Platform Max. Read length Max. Outputs/ Run Time
Illumina10 iSeq 2 x 150 base pairs 1.2GB/9.5 to 19 hours
MiniSeq 2 x 150 base pairs 7.5 GB/4 to 24 hours
MiSeq Series 2 x 300 base pairs 15GB/4 to 55 hours
NextSeq 550 2 x 150 base pairs 120GB/12 to 30 hours
NextSeq 1000, 2000 2 x 300 base pairs 540GB/8 to 44 hours
NovaSeq 6000 series 2 x 250 base pairs
Thermo Fisher11
Ion GeneStudio S5 Up to 600 base pairs
6000GB/13 to 44 hours depending on the flow cells
15GB/19 hours
Ion GeneStudio S5 Plus Up to 600 base pairs 30GB/10 to 11.5 hours
Ion GeneStudio S5 Prime Up to 600 base pairs
Pacific Biosciences12 Onco Systems 2 x 150 base pairs
Revio System 15 kb to 18 kb
Oxford Nanopore13
50GB/6.5 to 8.5 hours
150GB/48 hours using 300 cycle sequencing kit
90GB/24 hours
SEQUEL System Up to 25 kb 1-10GB/0.5 to 10 hours
MinION Up to 900kb Up to 48GB/~72 hours
Long-read sequencers can read long strands of DNA or RNA (between 5,000 and 30,000 base pairs) in one go, without breaking them up into smaller fragments. They have played an important role in producing the most complete human reference genome sequence by enabling sequencing of regions that short-read sequencing struggled with. Even though they offer improved accuracy for the detection of specific types of genetic variants that are difficult to detect using current short-read sequencing methods, their use in clinical practice is restricted to a few specific situations, though it may expand in the future.9 Next-generation sequencing technologies have progressively evolved. Table 1 provides examples of a few NGS platforms that are currently available. Figure 2 provides the basic workflow.
PromethION 20 bp to 4M bp Up to 13.3TB when run for 72 hours
Short-read WGS has the following major steps:16
1. Sample preparation: DNA from EDTA or citrate stabilized whole blood or surgically removed or biopsy tissue is isolated by conventional methods. To enable copy number variation (CNV), high-molecular DNA is preferred. Though a PCR amplification step was required in the past, the newer technologies no longer need it.
2. Library preparation: The library is generated by fragmenting the high molecular DNA followed by ligation of adapters that will bind to the linker DNA on the chip surface. Next, barcodes that enable pooling of samples from different patients on the same chip may be attached.
Depending on the clinical applications, different approaches can be used for NGS.15
Whole genome sequencing (WGS): A comprehensive method to analyze the entire genome. This is useful in identifying inherited disorders, rare disorders, screening for prenatal aneuploidy, characterizing the mutations that drive cancer progression, epidemiological investigations of disease outbreaks, and determining antimicrobial resistance. 16 See Figure 3 for the general workflow of WGS.
Step 1 Extraction of genomic DNA from patient samples
Step 2 Shearing of DNA with a method of choice (nebulization, sonication, etc.)
Step 3 Ligation of specific adaptors + ligation of barcodes for multiplex sequencing
Step 4 Library selection & purification using magnetic or streptavidin beads
Step 5 Library amplification using PCR
Step 6 Sequencing
Step 7 Assembly of sequences and gene annotations
Step 8 Bioinformatics analysis
3. Cluster generation: The libraries are subsequently loaded onto a flow cell and placed on the sequencer, after which the individual DNA fragments are clonally amplified by a polymerase, generating small single-stranded clusters of the particular fragments.
4. Sequencing: The sequencing uses the principle of Sanger sequencing, where elongation is initiated by the addition of a sequence primer and polymerase and the nucleotide sequence is determined by the incorporation of complementary fluorescent-tagged nucleotide terminators. The fluorescent signal from the incorporated terminators is detected by scanning the chip and the individual clusters with a high-resolution confocal fluorescence laser detector after every round of nucleotide incorporation.
5. Data compilation using a high-performance computer: The next-generation system produces a raw sequence file. Data are compiled in a fastq file that is transferred to the high-performance computer (HPC). The raw sequence data is then aligned, creating Sequence Alignment/Map (SAM) format or its binary compressed version (BAM) file. From there, variant calling identifies changes to a particular genome as compared to the reference genome. That output is stored in the Variant Calling File (VCF).
6. Data annotation and interpretation with bioinformatics: The VCF file is finally uploaded to the interpreters in the genomic laboratory for filtration, annotation, and interpretation.




Whole exome sequencing (WES): Whole exome sequencing (WES), or exome sequencing, is a technique of sequencing all of the protein-coding regions of genes in a genome. Broadly speaking, it has two main steps as shown in Figure 4. They are 1) selecting only the subset of DNA that encodes proteins, known as exons and 2) sequencing the exonic DNA. Humans have about 180,000 exons, constituting about 1% of the human genome.17
WES is increasingly being utilized in the initial stages of diagnostic evaluation, especially for disorders that are genetically heterogeneous, such as complex neurologic diagnoses and multiple congenital anomalies. It has been used as a method of gene discovery in large series of patients with autism, epilepsy, brain malformations, congenital heart disease, and neurodevelopmental disabilities.18
The Helix® Genetic Health Risk App for Late-onset Alzheimer’s disease is an FDA-approved test that uses exome sequencing.19
Targeted next-generation sequencing (tNGS): Targeted next generation sequencing (tNGS) focuses on specific regions of interest in the genome — specific genes, coding regions, or even chromosomal segments at deeper coverage. Prior to the development and use of the target sequence (TS) panels, target enrichment for the genomic regions that are of interest are compared to the genomic background. This step is crucial and ensures that the NGS process is specifically designed to sequence the genomic targets efficiently and accurately. The common sequence enrichment processes are either generating amplicon by polymerase chain reaction (PCR) or using hybrid capture-based technique.20
tNGS is a great tool for diagnosis of microbial infections (more so for those organisms that are drug resistant) and diagnosis, prognosis, and monitoring therapy of cancer patients. The WHO recently suggested using tNGS for diagnosis of drug-resistant tuberculosis.21 The following are a few FDA-approved tests that use tNGS:
• Tempus’s xT CDx, a 648-gene next-generation sequencing (NGS) assay for solid tumor profiling and companion diagnostic for patients with colorectal cancer (CRC)22
• Thermo Fisher Scientific’s Oncomine Dx Target Test finds genetic variations in the genetic material of tumor tissues from patients with non-small cell lung cancer (NSCLC) and cholangiocarcinoma 23
• Memorial Sloan Kettering Cancer Center’s MSKIMPACT targets 505 genes and profiles for mutations for both rare and common cancers24
• Foundation Medicine’s FoundationOne®CDx is a tissue-based broad companion diagnostic (CDx) that is clinically and analytically validated for all solid tumors25
Metagenomic next-generation sequencing (mNGS): Metagenomic next-generation sequencing (mNGS) is a shotgun sequencing approach in which all of the nucleic acid (DNA and RNA) in a clinical sample is sequenced at a very high depth, 10-20 million sequences per sample. mNGS can be performed for any type of clinical sample, including cerebrospinal fluid, plasma, respiratory secretions, urine, stool, or tissue. A single mNGS test can detect sequence reads corresponding to all pathogens – viruses, bacteria, fungi, and parasites. It
can thus be used to identify the potential cause of a patient’s infection. To date, there is no currently FDA-cleared or approved mNGS test, although there are a few CLIA-certified laboratories that offer such tests on clinical samples.26, 27
Conclusion
Next-generation sequencing has transformed laboratory medicine as it has enhanced our understanding of disease mechanisms, enabled identification of specific biomarkers, and tailored medical interventions based on an individual’s genetics, i.e., precision medicine. NGS has also contributed to the development of non-invasive liquid biopsies for detection of cancer and monitor disease progression and treatment response. NGS is being used for RNA sequencing and methylation sequencing to study the methylation pattern of the DNA, sequencing microorganisms, sequencing cell-free DNA (cfDNA), cell-free RNA (cfRNA), etc. Clinical laboratories have adopted NGS as a gold standard for the diagnosis of hereditary disorders because of its analytic accuracy, high throughput, and potential for cost-effectiveness.28
In spite of these benefits, NGS has several challenges. It is complex and requires skilled professionals to perform the tests, analyze and interpret data, and standardize protocols. Though NGS is evolving at a rapid pace, it is still primarily used for research purposes or in CLIA-certified laboratories as laboratory developed tests. With advancements in NGS technologies and artificial intelligence, we may envisage NGS to become an easy-to-use point-of-care test as the standard of care in future.

Rajasri Chandra, MS, MBA is a global marketing leader with expertise in managing upstream, downstream, strategic, tactical, traditional, and digital marketing in biotech, in vitro diagnostics, life sciences, and pharmaceutical industries. Raj is an orchestrator of go-to-market strategies driving complete product life cycle from ideation to commercialization.
References are available online at https://mlo-online.com/55001313.



The ACE Axcel Clinical Chemistry System boasts a small footprint and no external water system, waste drain, or analyzer cooling unit. Process up to 285 tests per hour; load and run up to 75 samples simultaneously. Liquid, ready-to-use reagents eliminate prep time, including the new fast, affordable Vitamin D assay.
Alfa Wassermann

DxC 500 AU Chemistry Analyzer: Designed for spoked/ low-volume laboratories. Featuring continuous load on-the-fly reagent and consumables, Hba1c advanced assay with no manual preparation, true random access, intuitive interface and more. Includes a broad menu of assays including high-performing, Six Sigma assays.
Beckman Coulter

Carolina Liquid Chemistries (CLC) offers two fully-automated benchtop clinical chemistry analyzers, the EasyRA and DZ-Lite c270, both offering general chemistries and urine toxicology screening tests including Fentanyl testing. Included with purchase is CLC’s installation, training, and technical support.
Carolina Liquid Chemistries
LumiraDx SARS-CoV-2 Ag is a rapid microfluidic immunofluorescence assay for use with the LumiraDx Platform:
• Objective results interpretation
• Easy to use
• Small footprint
• Room temperature reagent storage
• Authorized for use in CLIA Waived settings
LumiraDx
A five-part differential hematology analyzer with built-in autoloader and a single closed tube sample mode. The hemoglobin analysis is performed using cyanide-free reagent. The analyzer processes up to 60 samples per hour and stores up to 100,000 results with histograms and scattergram. The barcode reader and optional LIS connectivity enable seamless sample data transmission. Mindray



Stat Profile Prime Plus whole blood critical care analyzers, now with micro-capillary sampling, provide clinical value with a test menu of pH, PCO2, PO2, Na, K, Cl, iCa, iMg, Glucose, Lactate, BUN, Creatinine, Hct, Hb, SO2%, CO-Ox, and ePV.
Nova Biomedical
Diasorin’s LIAISON XL is a fully automated chemiluminescent immunoassay analyzer designed to meet the unique needs of mid to high volume laboratories by automating and consolidating over 60 specialty tests. The LIAISON XL uses a single, all-inclusive reagent format with automation track compatibility. Diasorin

advanced Unity software tools to support your lab’s risk management
Simplify your QC workflow with load-and-go efficiency and robust data management.
InteliQ quality controls automate your QC on next generation platforms. These barcoded, load-and-go controls reduce hands-on time and manual errors, streamlining your workflow and giving you more freedom. InteliQ controls, together with Unity’s advanced data management tools, improve workflow efficiency. InteliQ. It’s simply smarter QC!
Isn’t it time to bring smarter, more efficient QC to your lab? Visit: www.bio-rad.com/inteliq

patients and help pathologists to make even more precise diagnoses, but they also put added burden on pathologists.
How can laboratories alleviate the problem for their pathologists?
Perhaps it goes without saying, but laboratories must first recognize that burnout is real. In fact, burnout has been steadily increasing over the past several years as the supply and demand challenge has heightened. Hiring one or two more pathologists is not going to resolve it.
pathologists’ workloads and ensure that cases are routed to the subspecialist with the best expertise. The right digital pathology workflow solution will also centralize all diagnostic data so that pathologists no longer need to spend time toggling among screens and get a more holistic view of the patient.
Bachelor’s degree
Biomedical Engineering from Johns Hopkins University and a Master’s degree in Biomedical Innovation and Development from the Georgia Institute of Technology.
In the Medscape Physician Burnout & Depression Report: “We Have Much Work to Do” released earlier this year, fortynine percent of physicians told Medscape they feel burned out. Why are pathologists, specifically, feeling so burnt out? Pathology is facing an intensifying supply and demand challenge. The shortage of pathologists has been worsening for almost two decades now. Between 2007 and 2017, the pathologist population declined by 17.5%.1 A recent analysis demonstrated that the number of open pathologist roles is near an all-time high;2 meanwhile, the global cancer burden continues to increase. The number of new cancer cases per year in the United States is expected to cross 2 million for the first time ever in 2024.3
The resulting impact is burnout; pathologists must read more cases and work longer hours, all while maintaining the commitment to quality that they pride themselves on. On top of this, diagnostic complexity is increasing as companion diagnostics and specialty tests continue to make their way into the clinic. These advancements are great for
Alleviating the burnout problem requires laboratories to truly transform their operations, and I believe that digital pathology is a critical part of this transformation. In shifting the standard from microscope to high-resolution image, digital pathology has been proven to deliver between 15 to 20% efficiency gains while helping pathologists to improve confidence.
Digital pathology also enables pathologists to work remotely, giving them flexibility to enjoy dinner with their family or attend their child’s sports game on nights when they might otherwise have needed to work late in the laboratory. By extension, digital pathology opens a broader pool of talent from which laboratories can hire since pathologists don’t need to be in the same geographic area. This may help laboratories to relieve some of the pressure on pathologists by spreading the workload among a bigger team.
Can you share more about the benefits that digital pathology is delivering?
Let’s unpack the efficiency and confidence gains that digital pathology delivers since these are the most commonly cited benefits.
Traditional analog workflows have inherent inefficiencies associated with handling glass slides. Digital pathology can overcome them with intelligent workflows that help to not only streamline internal operations but also improve turnaround times for patients. For example, automated and dynamic case assignment can increasingly balance
We also see efficiency gains when it comes to collaboration. Pathologists can share whole slide images in just a few clicks, eliminating the need to ship glass slides. This saves them time and means that patients can receive diagnoses faster. It also means that pathologists can more easily get a second opinion, helping to improve confidence.
Finally, I’d be remiss not to point out that digital pathology also lays the foundation for AI applications that further deliver on these benefits.
Each pathology image contains over 1 billion pixels that tell the story of a patient’s disease. AI is able to unlock insights from this incredibly rich data that go beyond what the human eye can see. These insights can help to improve diagnoses, and by extension, patient outcomes.
Companion diagnostics, like PD-L1 quantification algorithms, are a great example of the AI applications that generate these insights. Such solutions consistently identify biomarkers to give pathologists more information and enable them to make faster decisions. They also mark a big step forward in realizing the promise of precision medicine. Companion diagnostics are often associated with precision therapeutics and help to determine which patients are best suited for these treatments.
These insight-generating applications represent one category of AI solutions that we see in practice today. There’s another category referred to as process automation applications, which reduce time-consuming tasks. Consider the benefits of an AI-powered quality control solution that can complete this tedious work up to six times faster than manual review. It enables laboratory staff to focus on adding value elsewhere
and positions pathologists to make a better diagnosis since they are working with high-quality data.
I should note that both categories of AI applications play a key role in fighting pathologist burnout since they empower pathologists to work faster and more confidently. Process automation applications likely also free up team members to help pathologists with other tasks around the laboratory.
What are best practices to follow for clinical laboratories considering incorporating digital pathology?
It’s perfectly fine to start small, but don’t forget to think big. Many laboratories initially go digital by focusing on a specific use case, like collaboration and consults. This makes sense since going digital is a true transformation that requires investing in technology and reshaping processes to make the most of the technology.
At the same time, it’s important to think big and plan for the future. Laboratories often quickly see the benefits of digital pathology and want to scale their operations to achieve even more impact. We are also just scratching the surface when it comes to realizing the full promise of digital pathology and AI. There are so many more use cases and innovative solutions that will emerge over time, and laboratories want to be well-situated to capitalize on them. Laboratories should also recognize that they don’t have to undergo the transition from microscope to image alone. They should seek out technology vendors that want to serve as a trusted partner. Early adopters have paved the way, and an experienced vendor will be able to help the laboratory define its goals, build a business case, and make the right technology selections to maximize ROI both today and in the future.
1. Metter DM, Colgan TJ, Leung ST, Timmons CF, Park JY. Trends in the US and Canadian pathologist workforces from 2007 to 2017. JAMA Netw Open. 2019;2(5):e194337. doi:10.1001/jamanetworkopen.2019.4337.
2. Klipp J. Pathologist Job Openings Remain Near Record High. Laboratory Economics. 2023;18(10).
3. 2024--first year the US expects more than 2M new cases of cancer. Cancer.org. Published January 17, 2024. Accessed April 1, 2024. https:// www.cancer.org/research/acs-research-news/facts-and-figures-2024.html.

NG-Test® CARBA 5 is the only rapid, multiplex, phenotypic, lateral flow, FDA cleared assay capable of detecting KPC, OXA-48like, VIM, IMP and NDM carbapenemases produced by Enterobacterales and Pseudomonas aeruginosa. Detects the gene expression!
Hardy Diagnostics

Abbott’s Alinity systems are flexible and scalable with an increased throughput and capacity, allowing you to easily add modules as volume grows without having to replace your systems.

Effortlessly upload results from your LIS and eliminate the #1 cause of PT failures – clerical errors.
• No changes to your firewall or security
• No interface required or software to install
• No additional fees – API DataDirect is free Join the 7 million results uploaded utilizing API DataDirect!
American Proficiency Institute

The LIAISON PLEX® Respiratory Flex Assay is now FDA cleared on the next-generation, multiplex, sample-to-answer molecular diagnostic platform—the LIAISON PLEX® System. The flexible respiratory assay allows for customizable results based on patient needs.
Diasorin

The KRONUS 3-Screen Islet Cell Autoantibody ELISA Kit (KR7780) is for the simultaneous and non-differential detection of autoantibodies to GAD and/or
IA-2 and/or ZnT8 in a simple, highlyrobust, and user-friendly assay format. KRONUS,

The new StatStrip meter includes many features that make hospital glucose testing easier and more cybersecure while retaining the accuracy, freedom from interferences, and FDA clearance for use with critically ill patients that StatStrip has provided for the last decade.
Nova Biomedical

Puritan® has devices for multiple sites—OB/GYN, urethral, throat, nasal, and nasopharyngeal— and many shapes, sizes, and fiber types—including our patented PurFlock Ultra® and HydraFlock® flocked swabs. Sample with confidence and trust your results.
Puritan Medical Products Company

When clinical laboratories are facing challenges with proving lot-tolot reproducibility or when their current reagents are not performing as expected, SEKURE® open channel reagents can be employed to help improve clinical performance.

Sysmex’s innovative portfolio of hemostasis analyzers, reagents and controls are designed with quality, reliability and efficiency in mind. We provide advanced hemostasis technology across multiple platforms to match the needs of laboratories of all sizes.
Sysmex America Inc.

The NEW Unistik® venous blood collection portfolio is designed for safe and simple blood collection. Unistik ShieldLock, safety winged set, and Unistik® VacuFlip, safety needle, are intuitively designed utilizing tried-andtested blood collection techniques that healthcare professionals know. Unistik® ShieldLock and Vacuflip are a cost-effective alternative and available in a broad range of sizes.
Owen Mumford
CAPILLARYS 3 provides high resolution capillary separation for A1c, Serum & Urine Proteins, Serum & Urine Immunotyping, and Hemoglobins. Proven technology, high throughput, increased walk-away capabilities, and more flexibility for medium to large volume laboratories.
Visit us at ADLM, Booth #2249 Sebia, Inc.

The Diesse MINI-CUBE is an automated ESR analyzer that evaluates whole blood directly from EDTA tubes. It produces results in 20 minutes, does not consume patient samples, requires no reagent and easily interfaces to LIS.

ACL TOP® Family 50 Series Hemostasis Testing systems offer the most advanced automation, quality management, and routine to specialty assays for mid- to high-volume clinical laboratories, including those with lab automation tracks.
Unistik® VacuFlip and Unistik® ShieldLock are engineered for intuitive blood collection, featuring easy to use safety mechanisms that can help reduce the risk of needlestick injuries. Unistik® Blood Collection devices are cost-effective and designed to not compromise quality or safety.










































• Linux® operating system with advanced cybersecurity
• Rugged external meter casing
• Wireless charging
• Sealed battery casing
• New ketone test*
• RFID option
• Hematocrit range extended to 5-75%
Only glucose meter FDA-cleared for use with critically ill patients
• Accuracy proven in study of 1,698 critically ill patients with 257 specific medical conditions
• No known clinical interferences 8,000 medications investigated
• Glucose accuracy proven in over 200 publications




*The ketone test has received CE mark but is not yet available in the U.S.
