

































































































































































































































































































































































































































































































































































































































































































The Next Generation Of Contamination Monitoring Technology
For the cleaning verification of surgical instruments, endoscopes, and surfaces, ATP Complete 2 by Ruhof a cloud-based cleaning monitoring system used to help hospitals and other healthcare organizations achieve optimal standardized cleaning levels.






















Sourcing & Logistics
8 > ASCs Remain Challenged, New Tech is Here to Help
JANETTE WIDER
36 > Reducing the Environmental Impact of Medical Devices
KAREN CONWAY
Surgical/Critical Care
10 > Shifting Our Focus on Surgical Site Infections
MATT MACKENZIE
Infection Prevention
14 > Collaboration is Key for Interdepartmental Relationships
JANETTE WIDER



























KARA NADEAU



Sterile Processing
16 > Considerations for Reusable Instrument and Device Cleaning and Verification
SARAH B. CRUZ
DAVID TAYLOR










































































22 > Education Nation: Sterile Processing Quality Management Systems
32 > Quarterly Check-ins Give SP Leadership a Boost
34 > Tagging Instruments
STEPHEN M. KOVACH
Special Report 26 > HPN’s 2024 40 under 40
WIDER





























BY JANETTE WIDER, EDITOR-IN-CHIEF
This month, we featured a new program for Healthcare Purchasing News : 40 under 40. The program celebrates individuals under 40 years of age who are making waves in the healthcare industry under HPN ’s many verticals.
Right now, in our industry, we’re seeing a shortage of healthcare professionals. For example, a 2021 Washington Post-Kaiser Family Foundation survey found that nearly 30% of healthcare workers were considering leaving their profession, and nearly 60% reported impacts to their mental health stemming from their work during the COVID-19 pandemic. Further, according to the American Hospital Association, hospital employment decreased by nearly 94,000 from February 2020, including a drop of over 8,000 between August 2021 and September 2021 alone.
These numbers are certainly alarming, yet all hope is not lost. I’ve noticed a growing trend of hospitals and health systems targeting high school students about careers in healthcare.
Recently, Cleveland-based University Hospitals (UH) announced it is expanding the UH Future Nurse Academy to three locations. The program, which was introduced last year, is a two-week paid summer program designed to expose high school students to a career in nursing.

UH has partnered with local colleges to have an Academy on the east and west sides of the city and a central location to make it more accessible for students.
“The UH Future Nurse Academy sets students up for success by connecting them with UH clinicians and partners and providing an array of opportunities for hands-on learning. The Academy builds on students’ existing skills to help them navigate healthcare career paths following high school graduation,” said Michelle Hereford, MSHA, RN, FACHE, system chief nurse executive and Ethel Morikis Endowed Chair in Nursing Leadership.
My last two editorials celebrated sterile processing professionals and environmental services professionals, which are just two of the departments that HPN covers in its daily news coverage, magazine features, online stories, and now, our podcast, Healthcare Hodgepodge. The HPN team is committed to giving a voice to not only these departments, but also supply chain, infection prevention, surgical and critical care, healthcare IT, and more. Be sure to check out the featured winners in print and online and reach out to us if you have a story to tell (even if you’re over 40!) so HPN can continue to highlight those who are making a difference.
VP & Market Leader
Healthcare and Dental
Chris Driscoll
cdriscoll@endeavorb2b.com | 978-880-8345
Editor-in-Chief Janette Wider jwider@hpnonline.com
Associate Editor Matt MacKenzie mmackenzie@endeavorb2b.com
Senior Contributing Editor Kara Nadeau knadeau@hpnonline.com
Advertising Sales
East & West Coast
Kristen Hoffman khoffman@endeavorb2b.com | 603-891-9122
Midwest & Central
Brian Rosebrook brosebrook@endeavorb2b.com | 918-728-5321
Advertising & Art Production
Production Manager | Ed Bartlett
Art Director | Tracy Arendt
Advertising Services
Karen Runion | krunion@endeavorb2b.com
Audience Development
Laura Moulton | lmoulton@endeavorb2b.com
Endeavor Business Media, LLC
CEO Chris Ferrell | President June Griffin
COO Patrick Rains
CRO Paul Andrews
Chief Digital Officer Jacquie Niemiec
Chief Administrative & Legal Officer Tracy Kane
EVP Medical & Healthcare Technology Kylie Hirko
EVP Endeavor Business Intelligence Paul Mattioli Healthcare Purchasing News USPS Permit 362710, ISSN 1098-3716 print, ISSN 2771-6716 online is published 11 times annually with an additional issue in November - Jan, Feb, Mar, Apr, June, Jun, Jul, Aug, Sep, Oct, Nov, Nov IBG, by Endeavor Business Media, LLC. 201 N Main St 5th Floor, Fort Atkinson, WI 53538. Periodicals postage paid at Fort Atkinson, WI, and additional mailing offices. POSTMASTER: Send address changes to Healthcare Purchasing News, PO Box 3257, Northbrook, IL 60065-3257. SUBSCRIPTIONS: Publisher reserves the right to reject non-qualified subscriptions. Subscription prices: U.S. $160.00 per year; Canada/Mexico $193.75 per year; All other countries $276.25 per year. All subscriptions are payable in U.S. funds. Send subscription inquiries to Healthcare Purchasing News, PO Box 3257, Northbrook, IL 600653257. Customer service can be reached toll-free at 877-382-9187 or at HPN@omeda.com for magazine subscription assistance or questions.
Printed in the USA. Copyright 2024 Endeavor Business Media, LLC. All rights reserved. No part of this publication June be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopies, recordings, or any information storage or retrieval system without permission from the publisher. Endeavor Business Media, LLC does not assume and hereby disclaims any liability to any person or company for any loss or damage caused by errors or omissions in the material herein, regardless of whether such errors result from negligence, accident, or any other cause whatsoever. The views and opinions in the articles herein are not to be taken as official expressions of the publishers, unless so stated. The publishers do not warrant either expressly or by implication, the factual accuracy of the articles herein, nor do they so warrant any views or opinions by the authors of said articles.



















































































Vizient, Inc., Kaufman, Hall & Associates, LLC (“Kaufman Hall”) and Madison Dearborn Partners (“MDP”) announced that Vizient has exercised its option to acquire the remaining interest in Kaufman Hall, an advisor to the healthcare industry.
In 2021, Vizient became a minority investor of Kaufman Hall. A press release on the acquisition says that the two organizations aim to deliver high-quality patient care to their communities through their combined data assets and clinical, strategic, and financial experience.
Read on: hpnonline.com/55091437
A new episode of HPN’s podcast, Healthcare Hodgepodge
Maes is a product specialist for Medline in Phlebotomy and blood collection. Prior to working for Medline, he worked as a Pediatric ER Nurse at the University of Chicago Comer Children’s Hospital for 6 years. Maes leverages his clinical background and provides tailored support and solutions to healthcare facilities, in this episode as he discusses needlestick safety best practices with Editor-in-Chief Jane e Wider. Watch at: hpnonline.com/55093259
On June 26, Southern California Hospital at Culver City (SCHCC) announced that it has reached a noteworthy milestone for low rates of two healthcare-associated infections (HAI). SCHCC has now achieved more than 1,000 days free of central line-associated blood stream infections (CLABSI) and more than 750 days free of catheter-associated urinary tract infections (CAUTI). HHS has reported that CAUTI and CLABSI are associated with increased morbidity, mortality, healthcare costs, and length of stay.
Read on: hpnonline.com/55092137

Jimmy Chung, MD, MBA, FACS, FABQAURP, CMRP, Chief Medical Officer, Advantus Health Partners and Bon Secours Mercy Health, Cincinnati, OH
Joe Colonna, Chief Supply Chain and Project Management Officer, Piedmont Healthcare, Atlanta, GA; Karen Conway, Vice President, Healthcare Value, GHX, Louisville, CO
Dee Donatelli, RN, BSN, MBA, Senior Director Spend symplr and Principal Dee Donatelli Consulting LLC, Austin, TX
J. Hudson Garrett Jr., PhD, FNAP, FSHEA, FIDSA, Adjunct Assistant Professor of Medicine, Infectious Diseases, University of Louisville School of Medicine
Melanie Miller, RN, CVAHP, CNOR, CSPDM, Value Analysis Consultant, Healthcare Value Management Experts Inc. (HVME) Los Angeles, CA
Dennis Orthman, Consulting, Braintree, MA
Janet Pate, Nurse Consultant and Educator, Ruhof Corp.
Richard Perrin, CEO, Active Innovations LLC, Annapolis, MD
Jean Sargent, CMRP, FAHRMM, FCS, Principal, Sargent Healthcare Strategies, Port Charlotte, FL
Richard W. Schule, MBA, BS, FAST, CST, FCS, CRCST, CHMMC, CIS, CHL, AGTS, Senior Director Enterprise Reprocessing, Cleveland Clinic, Cleveland, OH
Barbara Strain, MA, CVAHP, Principal, Barbara Strain Consulting LLC, Charlottesville, VA
Deborah Petretich
Templeton, RPh, MHA,Chief Administrative Officer (Ret.), System Support Services, Geisinger Health, Danville, PA
Ray Taurasi, Principal, Healthcare CS Solutions, Washington, DC


















Designed to protect both patients and healthcare professionals, while providing confidence in dose-delivery, Unifine® SafeControl® affords you the right balance of safety and control, from injection to retraction.
Unifine® SafeControl® provides:
• enhanced user control preventing premature activation1
• visual confirmation of dose-delivery1
• dual needle protection
• cost-effective solution

Scan here to learn more or request free samples!
BY JANETTE WIDER, EDITOR-IN-CHIEF
Ambulatory surgery centers (ASCs) are an integral part of our healthcare system and are, unfortunately, not immune to today’s supply chain challenges. Leaders of supply chain at ASCs are facing pressures from all different directions, including staffing and lack of resources.
Healthcare Purchasing News had the opportunity to speak with two suppliers about what trends, challenges, and solutions they are seeing from their customers and clients. Here’s what they had to say.
Brendan Dooley, senior vice president, ambulatory surgery centers, Medline, says that from an inventory management perspective, ASCs share many of the same supply chain challenges and priorities as other healthcare settings. “One difference between supplying ASCs vs. other facilities,” he said, “is the ability of an ASC to focus on equipment, surgical packs, and supplies best suited to their specialty services vs. sharing supplies used in other lines.”
Jason Grzyb, vice president, non-acute sales for Cardinal Health’s U.S. Medical Products and Distribution business, added, “The ASC model offers patients a cost-effective option that may be more convenient than a full-service hospital for certain surgical needs. As more procedures are receiving approval and being performed in outpatient settings, we

are seeing the volume and scope of care within ASCs grow significantly.”
“Additionally, new builds and existing ASCs are regularly experiencing complex issues like keeping up with evolving regulations, supply chain management, storage optimization, and logistics within a fast-paced market,” he said. “This means that ASCs have unique needs that other facilities may not. One need that stands out is optimizing storage, as ASCs typically don’t have the storage capabilities of a large hospital facility.”
As for the biggest challenge when it comes to supplying ASCs? Dooley commented, “ASC supply chain challenges can include the following:
• Size of facility – Smaller ASC footprints mean less storage space, and centers that may not be equipped with loading docks facilitating regular supply deliveries
• Hours of operation – ASCs’ receiving hours are more restrictive than a hospital’s
• Staffing and vendor partnerships – Because ASCs are rightfully focused on providing quality care, some ASCs may not have a dedicated team member or vendor partner responsible for supply chain solutions, managing inventory, pricing integrity, and ordering to drive efficiencies and cost savings
• Limited back-up resources – ASCs cannot borrow supplies from other in-hospital units when supplies run out”
Interestingly, Grzyb noted, “The ASC market is highly competitive and growing quickly. Our customers face a variety of complex issues that range from optimizing storage space, monitoring product usage, limiting waste, and managing inventory and logistics. ASCs also face staffing challenges – for example, a materials manager at a surgery center may wear many hats throughout their typical day.”
And for solutions? Grzyb said, “For new ASCs, collaborating with a distributor at the very start, especially when they’re planning a new build, can help them get ahead of these challenges. For example, an experienced distributor
can help create and manage project plans and building timelines, as well as share clinical and operational insights to help maximize the investment in a new facility. A successful facility opening depends on a distributor who understands the unique needs within an ASC and can provide recommendations for equipment, supplies, optimal layout, and storage solutions.”


Dooley Jason Grzyb
“Speaking of storage, as demand for ASCs grows, optimizing storage is becoming increasingly important. Both new and existing ASCs benefit from working with a distributor that has expertise in creating actionable plans to increase usable space and improve efficiencies by maximizing storage,” he added.
Further, Grzyb said, “ASCs can also benefit from clinician-led assessments, in which a team of consultants with clinical backgrounds provides onsite support and product expertise. Assessments may include identifying process improvements, evaluating efficiency of current procedure supply, and reviewing existing procedural pack components for waste. Consolidating procedure-specific items can reduce costs as well as pick and setup time.”
Dooley commented on costs. He said, “One of the ways to overcome supply chain challenges is to look at the total cost of supply chain – the dollars and time spent from ordering and acquisition to point of use and disposal. ASC leaders that make decisions and investments around ‘processes’ vs. ‘pricing’ will build a more efficient and resilient operation overall.”
“It is also a major advantage when an ASC works with a supplier or distributor who understands and can reference real-time information about what’s working for other ASCs, hospitals, and physician offices in the area,” he added.
Medline’s Dooley noted that the migration of surgical procedures from hospital settings to ASCs continues to accelerate as healthy patients are increasingly choosing to have surgery in healthy ASC environments. ASC leaders need to stay ahead of the procedures, reimbursements, and cost capture that support ASC revenue generation and growth. “Look for vendor partners who can support and enable expansion of services and specialties, increased caseloads, and center expansions,” he said.
“ASCs also need to consider that staffing is an even larger issue now than it was during COVID,” he asserted. “Clinicians continue to exit healthcare en masse, and ASCs may find it challenging to find and keep experienced clinicians. For staff retention, consider keeping clinicians working at their credentialed levels, allowing them to stay focused on quality outcomes and patient care. Also, consider how
automation of certain processes benefits staff members – saving time and streamlining repetitive tasks.”
Medline’s Dooley also noted that automation is now making an impact on supplying ASCs. He said, “Over the years, Excel spreadsheets have been the go-to for data management and automation for ASCs and other providers. But for many, this manual process is becoming increasingly inefficient for managing inventory and pricing. Working with data-heavy spreadsheets lacks real-time collaboration; has higher potential for errors, discrepancies, and multiple versions; and is limited in terms of integration with external systems -- among other challenges that hinder supply chain efficiency and transparency.”
He added, “With ASC becoming the preferred setting for patients and payors alike on a growing number of outpatient procedures, proactive ASC leaders are turning to automated supply chain technology scaled to support the ASC setting. Supply chain automation benefits include effectively predicting product demand and preparing for possible shortages, improved fill-rate performance translating into less disruption to the clinical end user, time savings for staff, and pricing integrity.”
As for other innovations assisting with supplying ASCs, Cardinal Heath’s Grzyb noted, “Delivery via Sprinter van is well suited to meet the unique needs and footprint of ASCs. These vans offer the flexibility of more regular deliveries and final mile support. Also, the ability to leverage technology on-the-go can offer ASCs a new level of convenience and flexibility.”
And Medline’s Dooley noted, “Auto-substitution programs are designed to ensure that clinically approved substitutes for high-need medical supplies automatically get to a hospital’s dock, supply rooms, and most importantly, into the hands of clinicians who need them. One of the primary benefits of auto-substitution is time savings, which is as important to ASCs as flow of product because staff are typically stretched in many different directions.”
Dooley also noted other technologies that are positively impacting ASC supply chain on the inventory management side, including:
• Platforms that give ASCs complete control over surgical and other custom packs
• Periodic automatic replenishment systems that can identify optimal minimum and maximum inventory levels for specific supplies
• Weighted bins that track high-volume items
• Electronic shelf labels that can provide real-time inventory updates and alerts HPN
BY MATT MACKENZIE, ASSOCIATE EDITOR
Surgical site infections are all too common, even as hospitals try desperately to weed them out and prevent them.
In April, Healthcare Purchasing News reported on a study that
suggested that the majority of surgical site infections stem from bacteria acquired before the patient enters the hospital in the first place. This could perhaps explain why their prevalence has not improved much in
recent decades – we may be focusing on the wrong places.
HPN had a chance to speak with Dustin Long, M.D., an anesthesiologist and critical-care physician at Harborview Medical Center at the

University of Washington and the paper’s lead author, about what he found while performing his research and where clinicians need to focus their energy moving forward to prevent surgical site infections.
Could you tell our readers a little about your background?
I am a critical care anesthesiologist at Harborview Medical Center. So clinically, I spend my time performing anesthesia in the OR mostly for traumas and burns, as well as working in our trauma surgical intensive

care unit. At the University of Washington, I perform research on healthcare associated infection with an emphasis on surgical site infection and antibiotic resistant bacteria.
How would you characterize conventional wisdom about surgical site infections?
I would say that there is a disconnect between the guidelines and clinical practice and commercial product development. What we see in day-today operations and, to some extent, the commercial product development pipelines related to surgical site infection, is heavily focused on environmental sources of infection within the hospital. That’s not to say that those aren’t important, but the science has shown that the vast majority of surgical site infections, at least those caused by the bacterium Staphylococcus aureus, come from the patient, not from the hospital environment. The science and the associated medical guidelines really emphasize measures that are focused on the patient. What our study adds is broadening the scope of that association beyond Staphylococcus aureus by using some new genomic methods.
Was there an inciting event that led you to undertake this study?
The main thing I would point out is that the authorship team that led this study is a team of physician scientists. We are surgeons, anesthesiologists, and infectious disease physicians who take care of these patients on a regular basis. We do this because we want to provide high quality care, and it’s very dissatisfying to us and to patients following all of the best practices to have a significant number of infections, and when this happens, there’s typically no explanation as to why this occurred in this particular patient. We really
just wanted to understand this in more depth so that we could have a sense of what was not working and what we might be able to do better.
Can you expand on what is meant by patientcentered models for infection prevention?
If you were standing in an OR today, there is a lot of emphasis and a lot of eyes on things like door openings and closings, ultraviolet light for surface decontamination, hospital garb, caps and masks, surgical attire, these types of things. A lot of the hospital’s energy is focused on these environmental sources, and yet we know from the science, with modern antiseptic practices and modern environmental hygiene in a hospital, that that’s not where most of the residual infections are coming from. They’re coming from patient flora that are not effectively being addressed by our antiseptics, our surgical antibiotic prophylaxis, and our preoperative decolonization regimens.
Instead of putting all our focus on our own hospital, we really want to shift that focus of infection prevention to the patient and ask ourselves if we are tailoring our interventions to that patient. We know that most of these infections are resistant to the antibiotic prophylaxis that we give, so how can we personalize that for the patient? We know that our approach to preoperative decolonization is imperfect, so how can we make that more effective and more consistent in terms of how we’re doing preoperative bathing and nasal decolonization?
This is not to say that we want to take our foot off the gas pedal in terms of keeping the hospital clean. Instead, we want to put the focus on the individual level of figuring out how we can better control the patient microbiome coming into this vulnerable state of surgery.
Is there anything individuals can do to prepare before they undergo a surgery to prevent this from being as big of a risk?
There’s still a lot of research that needs to be done to inform more effective prevention measures. With what we know today, if I was a patient coming into surgery, I would want to take very seriously the recommendations given for preoperative bathing with Chlorhexidine for skincare and for adhering to the protocols of nasal decolonization. You want to reduce that bioburden of bacteria on your skin as much as possible. There’s no way to completely sterilize skin tissue, even with antibiotics and antiseptics that we use in the OR, but knocking down that bioburden starting days or weeks before surgery is likely to be beneficial.
Is there anything clinicians or surgeons can do to inform the patient of these risks, or to minimize infections carried by the patient prior to surgery?
In the short term, there is still room to practice standardization around best practices in terms of things like screening patients for organisms such as MRSA before surgery and then providing targeted prophylaxis for those patients. Other things like control of perioperative blood sugars for patients with diabetes and intraoperative temperature management – these things can be improved throughout healthcare systems broadly. People try really hard, but we’re kind of hitting the point of diminishing returns in terms of how much more adhering to these established guidelines is going to get us closer toward zero. I think what we really need is new approaches and new technologies that are very different than what
we’re doing now. These would be things like preoperative screening of the microbiome to identify patients with strains that are resistant to our standard surgical prophylaxis and then tailoring that so the antibiotic matches the patient instead of just providing the same antibiotic to every patient which we know is not effective. We have sequencing based tools for measuring that now, and we just need to apply those. If we’re not effectively providing deep decontamination of the skin before starting a surgery, what other tools than antibiotics can we use to eliminate those bacteria from the skin? Focusing our thinking more on those patient sources to develop new protocols could be beneficial.
What can be improved upon in the short term?
We’re really focusing on low-tech stuff. We’re reassessing how we do simple things like daily bathing for our inpatients who are awaiting surgery. We are completely restructuring and overhauling our preoperative MRSA screening program and changing our approach to nasal decolonization for patients. We’re simply going back to the basics.
How can patients be protected from themselves prior to surgery?
What we know is that there are bacteria that colonize our bodies and, in normal states of health, they usually don’t cause any problem. But once a medical procedure is performed, like a surgery or inserting a urinary catheter or a tracheal tube, that disrupts these normal protective anatomic barriers that keep those bacteria in their place. The vulnerability of major illness or surgery allows those bacteria an opportunity to make this switch from being colonizers to kicking in as pathogens and signaling to each
other that there’s an opportunity to mount an infection.
There’s a lot of work exploring what we call “anti-virulence therapeutics” so that we don’t have to kill the bacteria – we merely have to keep them in check. We can change the way they signal to each other so that they stay more as these indolent colonizers and don’t try to mount an infection when the host is susceptible.
What do you think should be looked at next given the results of the study?
One of the immediate next things that we would like to do is do this type of research in other surgical populations and procedural groups. Longer term, we’re very interested in tailored approaches to infection prevention. We’re starting to develop some of the tests and molecular techniques needed to test a patient before surgery and get a result rapidly so we could use that information just a couple of days later at the bedside.
How can we get that “one in 30” number for surgical site infections down?
Changing the way that we talk about the issue of surgical site infections is important. There is a culture of shame around surgical site infection that leads to there not being good quality transparent data sharing. I think that has really hammered the advancement of patient care in this area. We hope that doing research like this moves this beyond the culture of shame and helps us understand what we are doing that is effective and ineffective and how we can fill ni some of those gaps.
Until we start looking at this as a more scientific issue and start sharing data and investing in basic research, I think, if anything, we’re going to see that one in 30 number heading in the wrong direction. HPN







Unwrap the future of sterile supply management. With features that help streamline processes and reduce the possibility of wet sets, Aesculap’s next generation rigid container is everything you’d expect from the market leader.
Visit aesculapusa.com/aicon to learn more about how this breakthrough technology can help your SPD Operate With Greater Precision.
BY JANETTE WIDER, EDITOR-IN-CHIEF
In today’s climate, collaboration between departments at a hospital or health system is crucial to success. Yet, with the demands faced by both infection preventionists and those who work in value analysis, effective communication is not always simple.
Barbara Strain, Barbara Strain Consulting, LLC, formerly director of Value Management at University of Virginia Health System, and current member of Healthcare Purchasing News’ Editorial Advisory Board, spoke with HPN about the relationship between value analysis and infection prevention. Strain urges these two departments to truly work together in partnership.
What should a relationship between infection prevention and value analysis be like?
I like to use the analogy of a duck swimming across a lake, and its legs are moving really fast, but it looks very calm and collected. That’s kind of the way it is in healthcare: we can make it very simple by understanding what everyone is bringing to the table, what their interests are, and how they can influence the decisionmaking process across an organization. When you bring all the right people together at the right time to
the right place, then we can make value-based decisions that really improve not only patient care, but staff workflow and also the utilization of equipment and supplies.
What’s a major challenge between these departments?
What people may not understand is value analysis [departments] do want to pull all the key people together, but sometimes they look at it like, “Well, wait a minute, they’re taking some of our work away.”
Value analysis is tasked by infection control committees, and they
know all the regulations and standards that they need to. If we get together and understand each other’s worlds, we can move ahead more effectively because every decision in value analysis involves infection prevention and control in some way.
There are various checklist items that we have in value analysis, one of which is instructions for use (IFU)— every product that is reusable has one of those. It is not just about how the piece of equipment for the product is reusable, it is how one sets it up, what is to be done with it, how does it function, etc. Also, the IFU instructs one on how to clean, maintain, and disinfect it. If it is a sterilization product, the IFU also tells one how to sterilize it and for how long to do these things and when to do them and how to do them. So, you need to sit down with a variety of individuals from different departments like IP and EVS, and value analysis is an integrator that brings those folks together to say, “OK, we’re about to make a decision
and it’s between these two or three products or pieces of equipment that have a reusable or IFU that we need to discuss.”
It is really important for everyone to get together and understand and come to an agreement on a piece of equipment, asking questions like can we adopt this product with these sets of conditions? Do we have the foundational aspects in place? Will this product be really helpful to patient care? We can sustain this by following the IFUs and understanding that infection control is part of the whole continuum of making these decisions. Infection prevention has to be included and invited to meetings and make themselves available for not only decision making and hearing all the various data but also for implementation and follow-up. For example, if a change is made and then all of a sudden there is an increase in X, what changed over the, for instance, last six months.
If infection prevention is part of the whole process, it can shorten time to decision making and also make it more effective. Then we can monitor what is going on with said product and determine, for example, when education might need to
take place again or bring in the supplier to do some work. Overall, it is most successful when it is a big collaboration.
Can you share a few thoughts on how infection prevention departments save hospitals money in the long run?

In value analysis, we follow processes that have been developed over many years. We really look toward how we can get to high value, meaning our outcomes are improved and no other harm is coming to patients or staff or the environment in which we practice. Then, any of the workflows and the dollars that we spent on the poorer outcomes get changed over.
You want to make sure that whole continuum is more effective at care getting done, and [patients are being] effectively treated or [having conditions] prevented sooner. The dollars that are being spent on that come back four or five-fold and your metrics toward quality are improving and you have something that you can then throw up against the wall and see what sticks.

Are there any new technologies to note that can assist with bettering relationships between value analysis and infection prevention?
Artificial intelligence (AI) is going to be one of the most helpful tools. We’ve learned so much about AI, especially through applications like ChatGPT, and its ability to create charts and graphs and make predictions is invaluable. It is all about the questions you’re asking; an infection prevention department could leverage their own software that gives them information about how they’re tracking patients.
There is so much data today that you need an aggregator to at least help you directionally. AI is not meant to replace any of the intelligence and experience that a human has it is just there to assist and lead humans in the right direction.
If an individual is trying to do a lot of work in infection prevention and relying on maybe a homemade or not off the market application, I would suggest subscribing to something specifically for infection prevention and control. It is very hard for IP to get budgeted money and show that return on investment.
Any final words of wisdom?
It is important to know and understand what the regulatory bodies and regulations are and educate each other in your organization. You don’t want to prepare for inspections when they come, you want to always be inspection ready. When I was managing laboratories, we operated every single day as if we were going to be inspected. It did not matter if they were coming that day or in three years, we operated the same way. So, understanding regulations is key to success. HPN
BY KARA NADEAU, SENIOR CONTRIBUTING EDITOR
If anyone questions the need for another article on instrument and device cleaning, consider this: Findings related to cleaning, disinfection, and sterilization have been among the top five drivers of The Joint Commission Immediate Threat to Health or Safety (ITHS) declarations during the past five years.
In its Guide to Reprocessing Reusable Medical Devices, The Joint Commission stated:
“Not only are deficiencies pertaining to medical device reprocessing among the most frequently cited, but they also are among the most immediately hazardous.”1
Why is the cleaning process so challenging for sterile processing (SP) teams?
The reasons are many but, in this article, HPN revisits the topic of manufacturer instructions for use (IFU) based on new research in this area, presents information on the new ANSI/AAMI ST108 water quality standard, and offers insights on cleaning and verification from SP








experts. Additionally, we share the story of the New York University (NYU) Langone Health SP team, highlighting their success and best practices.
The elephant in the room: IFUs



Before we get into specific aspects of cleaning and verification, let’s start at a high level with the overarching topic of manufacturer IFUs given recent research and reporting on compliance challenges.
For the February 2024 issue of HPN, I wrote an article featuring commentary from SP professionals on the problems they face complying with IFUs and their recommended improvements.
In parallel, the Association for Professionals in Infection Control and Epidemiology (APIC) was conducting its own research on the topic of IFU challenges, culminating in a report published in May 2024.2
In the report, entitled Modernizing Medical Device Instructions for Use (IFUs): Infection Preventionists Speak Up for Patient Safety, infection preventionists (IP) say they struggle with many of the same IFU issues voiced by their SP counterparts.
Kelly Zabriskie, vice chair of the APIC Public Policy Committee and enterprise vice president, Infection Control for Jefferson Health, spoke to the significance of the research findings, noting how they validate on a broad scale the struggles IPs – and SP professionals – face in their individual work to ensure patient safety.
“The research revealed how so many people are feeling the same way – that IFUs are a problem,” said Zabriskie. “The majority of IPs feel IFUs are difficult to find, read, and interpret. And this feedback was from IPs in all sizes of institutions – large ones with multiple IPs, small ones with a single IP, and those in between.”
More than half of IPs surveyed (65%) agreed or strongly agreed that the primary challenges they faced were for devices that fall into the low and intermediate levels of disinfection based on the Spaulding criteria.
When reporting on common problems, the top two complaints among IPs were IFUs that are unnecessarily complex, difficult, or time consuming to read, and instructions that are designed to address product lifespan more than prevention of healthcare acquired infections (HAIs).
With regards to cleaning and disinfection, challenges raised by IPs include:
• Lack of specifciity/clarity about how to appropriately clean the product
• Information that is outof-date/inconsistent with currently available products or technologies
• Unnecessarily targeted to a specic brand of cleaner
• Recommendations for cleaning products that are not hospital grade
• Require use of a product that is unavailable or difficult to purchase in the U.S.
“A personal pet peeve of mine is IFUs that recommend cleaning products that are unavailable,” Zabriskie commented. “This can happen when the IFU is outdated or when the item to be cleaned/disinfected is from outside the U.S. For example, some IFUs call for a product that is 70% alcohol, which cannot be found on the U.S. Environmental Protection Agency (EPA) list of approved disinfectants. In these cases, end users are left questioning, ‘what should I do?’”
When asked what SP professionals and IPs should take away from the report, Zabriskie stated:
“The report is intended to communicate validation of IFU issues among IPs and other IFU end users, and how APIC is taking steps to drive change in this area. We hear you. We understand there is a problem, and we are trying our best to engage others to move forward with a more standardized approach to IFUs.”
Published in August 2023, the ANSI/AAMI ST108 Water for Processing Medical Devices standard is the first of its kind.3 It establishes requirements for the quality of water used to process medical devices; revises and replaces AAMI TIR34:2014/(R)2021; and provides clear requirements for every stage of medical device processing.
“It makes the use of critical water for the final rinse a requirement and ups the game for bacterial and endotoxin levels for critical water and water for endoscopy processing to a maximum of 10 cfu/ml bacteria and 10 Endotoxin units/ ml,” Jonathan A. Wilder, Ph.D., managing director, Quality Processing Resource Group, explained. “In my water audits, I have seen a number of failures in facilities where one would not expect failures. If you aren’t testing, and since there is an American National Standard concerning these items, you don’t know if you are endangering patients.”
Seth Hendee, AS, CRCST, CIS, CHL, CER, CSPDT, SLH Consulting, spoke to the importance of water quality in cleaning and sterilization activities, stating:
“Water is a major factor in both cleaning and sterilization activities, but when it comes to cleaning reusable devices, the negative impact of poor water quality is widespread. It can have adverse effects on cleaning equipment and its
performance, cleaning chemistry performance, and the instruments themselves.”
Speaking to compliance with the ANSI/AAMI ST108 Water for Processing Medical Devices standard, Hendee said:
“Bringing water quality responsibilities to the ‘point-ofwater-use’ will mean involving SPD staff in something they have previously had little experience with. It is an important update as more and more stories come out of poor water quality halting surgeries in facilities across the country. Understanding the quality of the water touching your devices, regularly monitoring it, and fixing issues when they are identified are key components to delivering high quality instrumentation to your patients.”
Hendee and Wilder also offered key considerations for cleaning and verification and recommendations for improvement.
“If you have a tool, use it,” said Wilder. “Lumen racks are a great help in avoiding cleaning failures in lumened items or even in items as simple as suctions. If you do not use these for lumened devices, you will have less than effective cleaning of their interiors. This applies to any cannulated device, as discussed by Cori Ofstead at the last HSPA national meeting. However, I have seen a number of facilities who own washer racks that are specifically designed processing lumened devices but do not use them.”
Wilder pointed out how this is “bad practice” for two reasons:
“One is that if you inspect a lumened device after cleaning and you didn’t use the proper tool to clean it, you will have rework and decreased productivity.”
“The second is, if you own a washer rack and don’t use it, and
a patient gets an HAI that could be expected to have been eliminated by proper cleaning of the interior of a lumened device, personal injury attorneys will have a field day in court.”
“Inspection of lumened items using borescopes and improved inspection of non-lumened devices using lighted magnifiers for proper cleaning is a growing practice,” Wilder added.


Speaking on the topic of washer/disinfectors and cleaning indicators, Wilder stated:
“Every SPD wants to increase productivity, and therefore would like faster washer cycles. Washer manufacturers are willing to do what they can to shorten cycles, but it is critical to ensure that the shorter cycles are actually doing a good job cleaning the instruments.”
“The cleaning indicator space has not seen much change, with the exception of the introduction of the Mesa Labs T-EZ Pro that has recently come to the U.S. market,” Wilder continued. “I do not know how this compares in process resistance to the existing market leaders (TOSI, Verify), but it is similar in design to TOSI.”
Cleaning verification (CV) for endoscopes is commonly practiced in SP departments, being part of the American National Standards Institute (ANSI)/ Advancement of Medical Instrumentation (AAMI) ST91:2021 Flexible and semirigid endoscope processing in healthcare facilities standard.
But according to Hendee, far fewer SP departments are performing CV for devices other than endoscopes. He stated:
“The need for cleaning verification for devices other than endoscopes is a topic I often discuss with SPD leadership. Many SPDs are processing endoscopes now, and most that do are performing CV at an established frequency. When I ask if they are performing CV on any other devices, the answer is usually ‘no.’ That always baffles me.”
Hendee continued: “For years ST79 has had a recommendation that departments perform periodic cleaning verification, and we know there are plenty other complex devices out there that are hard to clean and inspect. Shavers, like endoscopes, have been identified as difficult to adequately clean even when the IFU is followed. Why isn’t CV on shavers talked about in the same way as it is with endoscopes? Cleaning verification is a tool in the SPD quality assurance toolkit, and in my opinion, should be used more widely.”
Perhaps lack of CV is related to lack of time in SP departments. The January 2024 issue of Clinical Endoscopy featured a study on the costs and staff time associated with ST91:2021 compliance. The researchers concluded that the new standards “represent a potential 24.3-minute increase in reprocessing,” including an additional 8.4 minutes for endoscope-cleaning verification.4








Read the articles. Take the test. All online, in one easy-to-use portal.
https://educationhub.hpnonline.com/



Members of the New York University (NYU) Langone Health Sterile Processing Department (SPD) work across the health system’s four hospitals and seven ambulatory units in Manhattan, Brooklyn, and Long Island, handling more than 25 million instruments per year.
From 2019 to 2023, NYU Langone Health procedural case volume increased by 31.7% with specialty & complex case volume increasing as follows: Endo ~59%, Neuro ~19%, Ortho-Spine ~21%, Transplant ~69%. This equates to ~4,000 cases performed per month and ~23,700 instrument sets reprocessed by SPD per month.
The NYU Langone Health SPD and OR teams recently engaged in a collaborative effort to reduce reprocessing defects, including bioburden, holes in wraps, case carts delivered without sets, missing instruments, and wrong instruments in sets.
The result: 99.93% of instruments provided to surgical teams accurately and on time, and a 0.75% defect rate by case volume, down from 12.9%.
When it comes to cleaning improvements, NYU Langone Health Director of Sterile Processing Conner Brazil and Director, Outpatient/Business Initiatives Sterile Processing Department Marc Aquino, point to OR pre-treatment compliance as a key factor.
“There is nothing that can replace pre-treatment at the end of the case,” said Brazil. “When it is performed


in the OR, the instruments coming into our department are much easier to clean. We perform audits of pre-treatment compliance, as well as audits on instruments that come through decontamination into the clean side to identify cleaning failures. The OR performs its own audits as well. If they fi nd a defect, which is very rare, we perform an investigation into the root cause and address it, such as by staff re-education.”
One way Brazil and Aquino are helping support pretreatment compliance of robotic instrumentation, which they note is notoriously difficult to clean, is through the deployment of enzymatic fi lled caps that OR staff place on the end of these instruments post-procedure.
Speaking on the topic of manufacturer IFUs, Aquino said the health system has a verification system in place to ensure the SP department receives up-to-date IFUs on all new products entering the system. The challenges come with legacy instruments and devices, as Aquino explained:
“With items that have been in use for many years, it’s likely the original product manufacturer has been acquired or merged with another company at some point, making it challenging to know where to fi nd the latest IFUs.”
This aligns with APIC research fi ndings where 66% of IPs surveyed either agree or strongly agree that IFUs are difficult to locate.1
Brazil also spoke to challenges of having device and instrument inventory that contains similar items from different manufacturers with varying instructions for cleaning. He provided these examples:
“We have 40 different types of reusable vaginal speculums and only two have IFUs that specify they must be reprocessed assembled, while the other 38 must be dissembled prior to reprocessing. It gets confusing so now we are moving to disposable speculums across the board. We are making the same move with Gomco clamps for circumcisions.”
When asked for keys to success in delivering clean instruments to the patient bedside, Brazil stated:
“It is really about the collaboration between SP and the OR. We are fortunate at NYU Langone Health that the OR team is willing to work with us.”
“It has been helpful to have an auditing process and schedule where we routinely review all inventory,”
Aquino added. “In the case of peel packs, some have been in circulation and stored in various locations for quite some time, so routine audits provide the opportunity to evaluate their integrity and remove those that are compromised.”
Lastly, Brazil pointed to the importance of ongoing staff education and training, stating:
“We arrange for quarterly in-servicing of items that are complicated to clean, such as scopes. The manufacturers come into our facilities every three months to provide education for everyone. I would highly recommend this practice to other hospitals.” HPN
References:
1. The Joint Commission Guide to Reprocessing Reusable Medical Devices, 2023, https://store. jointcommissioninternational.org/assets/1/7/EBCDS21SL_sample_pages.pdf
2. Modernizing Medical Device Instructions for Use (IFUs): Infection Preventionists Speak Up for Patient Safety, APIC, May 2024, https://apic.org/modernizing-medical-device-instructionsfor-use-ifus/
3. AAMI Publishes First National Standard on Water Quality for Medical Device Processing, AAMI News, August 16, 2023, https://array.aami.org/content/news/aami-publishes-first-nationalstandard-water-quality-medical-device-processing#:~:text=ANSI%2FAAMI%20ST108%20 specifies%20the%20minimum%20requirements%20for%20the,be%20used%20during%20 each%20stage%20of%20sterile%20processing.
4. Hoffman D, Cool C. Costs involved in compliance with new endoscope reprocessing guidelines. Clin Endosc. 2024 Jan 26. doi: 10.5946/ce.2023.164. Epub ahead of print. PMID: 38273218, https:// pubmed.ncbi.nlm.nih.gov/38273218/

BY SARAH B. CRUZ, CSPDT, CRCST, CHL, CIS, PRESIDENT AND FOUNDER, PRETREAT CSS
Quality” appears to be the healthcare industry’s new buzzword. Sitting high amongst other phrases like “let’s take that offl ine” and “stateof-the-art,” a variety of professions use the word in their own ways. Originating from the craftsmen of the medieval era, guilds would compose strict guidelines that required their products to be inspected for defects. These practices remained present,
surviving through the Industrial Revolution,1 and have evolved into the quality management systems seen in the 21st century. From medieval craftsmen that created the fi rst quality control program to the fi rst quality assurance program in the 1920s, quality control has been present throughout history.1 Over time, quality programs began to emerge in industries not necessarily specific to the factory setting. As the healthcare
1. Define quality in the context of the healthcare industry, particularly in Sterile Processing.
2. Understand the purpose of a Quality Management System and key factors to consider when developing one.
3. Be able to differentiate between Quality Assurance, Quality Control, and Quality Culture, and explain how they contribute to better outcomes in the Sterile Processing department.
Sponsored by:




industry incorporates quality systems into daily operations and patient care, professionals face the challenge of defi ning what it means to provide “quality care” within an organization that serves patients. There is an even greater challenge to professions like Sterile Processing (SP), whose quality management systems are directly linked to an entirely separate profession’s ability to perform their quality of care.




While the application of quality in the healthcare setting may vary from profession to profession, the concept of quality is not so ambiguous. Quality is “the standard of something as measured against other things of a similar kind; the degree of excellence of something.”2 Quality sets the foundations for the expectations of our work, therefore it is a tangible, physical, and measurable concept. Thus, if it is accurately defi ned in accordance with the outcomes a Sterile Processing department is expected to achieve, then a program for consistency can be trained.
Quality is essentially the fulfi llment of promises that have been defi ned by the collective individuals involved. In order to do this successfully, Sterile Processing must know how success is defi ned by its partnering perioperative professions. A Surgical Technologist may define this as having the accurate instruments in an instrument set. The circulating Nurse may achieve success when the wrappers do not have holes, all while the Surgeon anticipates a surgical site infection-free recovery for the patient. An effective quality practice permits SP departments to fulfill these promises to their patient care colleagues. This is why a successful quality program feels like any other smooth day on the job for all parties involved. It is also why multiple professionals are negatively impacted when a quality defect is discovered. Hence, robust SP quality programs must specifically defi ne indicators within their own departments that will inevitably create the outcomes other departments depend on.
With this working knowledge of what quality is, SP leadership can develop a structure for professional expectations and practices to grow upon. This structure is a quality management
system (QMS). A QMS is a system of documented processes, procedures, and responsibilities that SP use to achieve objectives (Figure 1).3 QMS permits SP leadership to conceptualize the direction that they need their frontline professionals to move towards. A few key factors to consider when a QMS is in development is that they:
• Are unique to the organization (i.e., facility, industry, association, etc.).
• Should align with the purpose & strategic direction of the organization and contributing departments.
• Enhance satisfaction of their customers (the patient, the OR team, etc.).
This is how leadership moves from a reactive state of decision making to a proactive expectation of outcomes. It also provides them with the opportunity to make quality a collective department effort by essentially incorporating strategic markers for their team to strive towards.
This is achieved through the three major components of any healthy and sustainable QMS: quality assurance, quality control, and quality culture. These components are made up of standard works, best practices, and standard operating procedures that detail how to perform a process in order to achieve a quality outcome. More often than not, these terms are used interchangeably and are treated like synonyms. This could not be further from the truth. Quality assurance, control, and culture are their own entities that contribute to a QMS (Figure 2). Too much of one and not enough of another affects the outcome of processes and misses opportunities to articulate the actions necessary to achieve and maintain quality in SP.
Quality assurance and control are key components of a QMS. Quality assurance programs ensure that the correct processes are performed to
This lesson was developed by Solventum. Lessons are administered by Endeavor Business Media.
After careful study of the lesson, complete the examination online at educationhub.hpnonline.com. You must have a passing score of 80% or higher to receive a certificate of completion.
The Certification Board for Sterile Processing and Distribution has preapproved this in-service unit for one (1) contact hour for a period of five (5) years from the date of original publication. Successful completion of the lesson and post-test must be documented by facility management and those records maintained by the individual until recertification is required. DO NOT SEND LESSON OR TEST TO CBSPD. www.cbspd.net


Healthcare Sterile Processing Association, myhspa.org, has pre-approved this in-service for 1.0 Continuing Education Credits for a period of three years, until June 25, 2027.
For more information, direct any questions to Healthcare Purchasing News editor@hpnonline.com.
achieve the anticipated final outcome, taking a proactive approach to preventing defects and failures. For example, opening surgical instruments and placing them neatly in the tray or on the stringer before sending them through the washers is an SP industry best practice. The department’s standard works describe this step in detail, resulting in debris-free instruments on the clean side. The steps are evaluated for compliance and technical ability. This ongoing process is quality assurance in practice. The practices are consistently evaluated for adherence.
Quality assurance programs rely on quality control follow up. Quality control is a reactive method as it is focused on the outcomes, good and bad, at the end of the process. Quality control identifies whether a process has failed or passed by providing a foundation to detect mistakes. Auditing is an effective way to carry out quality control programs. For example, if a sterile instrument set
is randomly inspected, leading to the discovery of no indicator, this audit has caught a quality defect before the end user is impacted. This is quality control in practice, as the end result was inspected for completion. When quality assurance and control are implemented together in an SP department the desired outcomes and processes are defi ned, leading to recognition of success and prevention of patient safety concerns.
The only way to make quality more than a buzzword in the SP department is to assess how it is viewed by the Perioperative team. This team is made up of SP, Nurses, Doctors, Surgical Technicians, and every other profession that contributes to the overall positive patient outcome. The separate impressions held by each group defines the collective belief in everyone’s ability to sustain quality programs. Quality assurance, control, and QMS need to be rooted in the team’s day-today operations. At that point, quality will develop a culture of its own.



In a sense, quality culture is quality that is achieved for its own sake. This culture is based on the successes or failures of setting the foundations underlying the team’s expectations. The ability to maintain quality programs is based on the professionals’ views on quality improvement. An SP department could have the best quality management systems in place, but without participant buy-in, it will not result in improved outcomes. Take a quick assessment of how the OR team reports bioburden, evaluate how the SP technician determines what instrument is requested on a phone call, and/or analyze the general disposition of the entire team when process failure is reported. These scenarios, and many others, can provide insight into the current disposition towards quality.
The SP department has a significant opportunity to incorporate the quality concepts that have developed over the years. If department foundations include clear expectations, then



everyone involved can achieve consistency in quality outcomes. Appropriately designed quality programs provide opportunity to reach clearly articulated goals by utilizing QMS. Through a robust quality assurance process and quality control protocol, the SP department learns to collaborate and support each other. As a result, quality culture can provide opportunities for growth, collaboration, and incorporating all aspects of the positive patient safety outcome. HPN
References:
1. “History of Quality - Quality Management History” American Society for Quality , asq.org/ quality-resources/history-of-quality. Accessed 18 June 2024.
2. “Quality, N. & Adj.” Oxford English Dictionary , Oxford UP, March 2024, https://doi. org/10.1093/OED/1145670898. Accessed 18 June 2024.
3. Cruz, Sarah B. “Education Nation: Creating Sterile Processing Department SOPs”. Healthcare Purchasing News , Dec. 2022, 2212_CEU.637268f05e032.pdf (imgix.net)
4. “Quality Assurance vs Quality Management.” SimpliAxis , 2022, www.simpliaxis.com/ resources/difference-between-quality-assurance-and-quality-management. Accessed 18 June 2024.
5. Cruz, Sarah B. “Quality: The Newest Sterile Processing Buzzword”. On Demand Course, 3M Healthcare Academy, 2023, www.3m.com/3M/en_US/3m-health-care-academy-us/. Accessed 18 June 2024.
Quality Culture
Quality Management
Quality Assurance
Quality Control
2. Illustration of how quality components arrange together to improve outcomes
1. The concept of quality originated in the 1920s industry boom.
A. True
B. False
2. Quality culture is defined by positive and negative quality instances.
A. True
B. False
3. The Perioperative team consists of Doctors and Nurses only.
A. True
B. False
4. A robust quality management system includes:
A. Quality Culture
B. Quality Control
C. Quality Assurance
D. All of the above
E. None of the above
5. Quality management systems provide SP leadership with an opportunity to tell their team what to do.
A. True
B. False
All CEU quizzes must be taken online at:
6. QMS key factors to consider include:
A. They are not unique to the facility
B. Leadership is responsible for its success
C. The needs of contributing departments
D. All of the above
E. None of the above
7. Quality control and quality assurance can be used interchangeably.
A. True
B. False
8. Quality programs provide a foundation for expectations.
A. True
B. False
9. Quality:
A. Is a measurable concept
B. Specific to the SP department
C. Do no consider department goals
D. All of the above
E. None of the above
10. QMS, Quality Assurance, and Quality Control need to be rooted in the team’s day-to-day operations
A. True
B. False

















































































































































































































Congratulations to the winners of the inaugural Healthcare Purchasing News 40 Under 40 Awards! The winners represent some of the best, brightest, and hardest working young people in the industry.
This year’s class comes from all different backgrounds and works across Healthcare Purchasing News’ many verticals. As you read you will find winners who work supply chain, sterile processing, infection prevention, and more. Whatever path their career has taken them, they are truly contributing to their organization’s success.
On behalf of the entire team here at Healthcare Purchasing News, I want to congratulate our winners and I am so excited to see what they do to continue to help innovate and advance healthcare.
Chris Driscoll VP & Market Leader , Healthcare and Dental









































Reduce risk of wire contamination, free up hands, and organize wires in the sterile field
Invented by an interventional radiologist, CaraClip™
• is a sterile, self-adhesive device that can remain in place for at least 8 hours on dry surfaces, can be repositioned, and withstands fluids such as blood, saline, iodine, contrast, and sterile water
• allows technologists to easily curve, redirect, and advance guidewires without fear of falling outside the sterile field

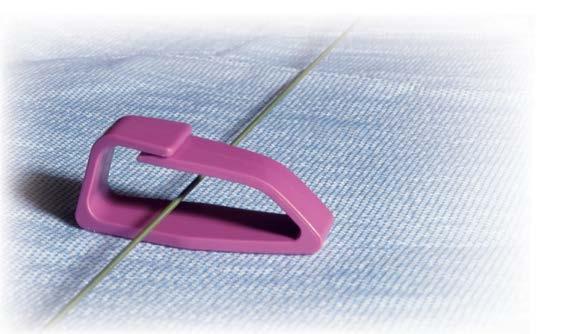












• instills confidence that devices will be contained in the wire protector, freeing up hands to focus on other important tasks Call 1.800.233.5539 or email info@beekley.com to request a sample of CaraClip wire protector today Visit beekley.com/caraclip for Product Safety Information


Jennifer Hunt East Tennessee State University Graduate Program Coordinator and Academic Advisor
Mario Zamarripa HonorHealth Director of Supply Chain Management
Claudia Pacheco Communities Lifting Communities / Hospital Association of Southern California Health Equity Program Manager
Justin Klinfelter NorthShore – EdwardElmhurst Health System Assistant Vice President, Category Management
Krystal Westmoreland Ascension Regional Director, Sterile Processing
Ashley Shepherd Children’s Hospital of Philadelphia Senior Manager of Value Analysis
Katie Sauber MultiCare Health System System Director of Contracting and Strategic Sourcing & Corporate Counsel of Myriadd Supply
Kevin Phelps Northeast Georgia Medical Center Executive Director, Supply Chain Management
Ryan Burke Pandion Alliance Vice President, Strategic Sourcing
Tiffany McCarthy UPMC Shadyside Hospital Supervisor/Educator Central Sterile Processing
Brandon Meachem Georgia Vision Institute Surgery Center Director
Rebecca Peplau Maine Medical Center Manager - Sterile Processing
Sarah Catania Chastain Surgery Center Inventory Manager and Administration Manager
Joshua Yisrael OU Health
Administrative Director, Inventory Control Cameron Evans
Good Samaritan Supply Chain Purchasing and Receiving Manager
Clara Whitney Caribou Medical Center Infection Preventionist/ Occupational Health Nurse
Sarah B. Cruz, CSPDT, CRCST, CIS, CHL The Bone and Joint Institute CS Quality & Education Program Development Coordinator
Devin Sumaoang UW Medicine Supply Chain Director/Site Lead
Kate Polczynski Geisinger Vice President, Enterprise Supply Chain
Jessica Gehrke Froedtert & Medical College Manager, Value Analysis
Amanda Hayes Sioux Falls VA Medical Center Asst. Chief SPS
Heather Duffy Sioux Falls VA Medical Center Chief, SPS
Carmen Henriksen Sioux Falls VA Medical Center RMD Coordinator
Eric Swaim HealthTrust Performance Group Vice President, Strategic Sourcing
Julia Anthony SOLUtion Medical, LLC COO
Jennifer Bender PDI Healthcare Science Liaison
Dustin Dzwonkowski Belimed, Inc. Co-CEO/Chief Commercial Officer
Rebecca Hou Vizient Environmental Sustainability Program Manager
Drew Mays Alliant Purchasing Senior Vice President, Member Success
Lindsay E. Collazo University of Miami Health System (UHealth) Director, Supplier Diversity
Josh Andrade
HonorHealth Director, Supply Chain Management
Vetannie Morton
Hospital Association of Southern California Coordinator of Diversity, Health Equity, and Inclusion Programs
Tasha Acevedo Montefiore Nyack Hospital Support Service Asst Director
Brandon Gottlieb Artesia General Hospital Director of Plant Ops
Ashlee Harden Choctaw Nation Health Services Authority Assistant Chief Pharmacist
Aditya Sanjeevi
Rochester General Hospital Internal Medicine Resident
Ashley Wilson Children’s National Health System
Executive Director of Supply Chain Services
Kerrie Guerrero
Houston Methodist Vice President/Chief Nursing Officer
Truly Garcia
Memorial Hospital of Carbon County Materials / Purchasing Tech
Nish Parekh Omnicell
Senior Vice President, Chief Product Officer
Drew Mays
Alliant Purchasing
Senior Vice President, Member Success
Age: 39
Hometown: Henderson, KY
Alma Matter:
Bachelors: Murray State University, MBA:
University of Southern Indiana
Number of Years of Experience in Healthcare: 20
Favorite thing about healthcare: It’s a new challenge every day!





Drew’s leadership role as the Senior Vice President of Member Success at Alliant Purchasing speaks volumes about his dedication to bettering the healthcare industry. Under his guidance, Alliant Purchasing experienced significant growth, with purchasing volume soaring from 2.2 to 5 billion. The Alliant expansion of members directly results from Drew’s focus on fi nding savings for rural healthcare facilities, particularly in underserved areas of Texas, Alabama, and Mississippi. His commitment to addressing the unique challenges faced by these communities demonstrates a socially responsible and
industry-bettering approach. Furthermore, Drew’s career progression, marked by five promotions, highlights his consistent pursuit of excellence and ability to deliver results. His rise to the role of Senior Vice President is a testament to his leadership capabilities and the trust placed in him to drive the success of Alliant Purchasing. In conclusion, Drew Mays’s commitment to the healthcare industry and his dedication to professional development are evident in his diverse experience, academic achievements, leadership role, and the tangible impact he has had on the growth and success of Alliant Purchasing.
The Bone and Joint Institute
CS Quality & Education Program
Development Coordinator
Age: 37
Hometown: Connecticut
Number of Years of Experience in Healthcare: 16
Favorite Hobby: Crossword Puzzles and Reading
































Favorite thing about healthcare: The opportunity it provides me to improve upon patient safety, contribute to a positive surgical outcome, and elevate the Sterile Processing profession.














Sarah has emerged as a true leader in our facility, se ing a remarkable example for her colleagues. Beyond her “day job” accomplishments, she has also achieved significant success in initiatives that have positively impacted the well-being of our patients and the community we serve.


Clara Whitney
































Favorite thing about healthcare: Our purpose. We have the opportunity to save lives and improve the health of our patients. Supply Chain is behind the scenes focused on providing our clinicians with the right tools at the right time to provide excellent care!

























Josh strives to grow his knowledge on how he can positively impact an organization. His largest investment since joining the healthcare field has been in his continuous pursuit of education since entering healthcare. The aim of his educational pursuits is to increase capabilities and effectiveness for the healthcare organizations and people he serves.



Caribou Medical Center


Infection Preventionist/Occupational Health Nurse
Age: 38






Hometown: Soda Springs, Idaho
Alma Matter: POST University/ American Sentinel College of Nursing & Health Sciences



Number of Years of Experience in Healthcare: 15

























Favorite Band or Musician: George Strait Favorite thing about healthcare: Having the ability to make a difference in other people’s lives every day.












Clara has shown commitment by being an active and engaged interdisciplinary team member on commi ees including Safety Commi ee, Antimicrobial Stewardship Commi ee, Clinical Team Commi ee, and Operational Excellence commi ee. Clara has continually advanced her education and experience shown by achieving her professional accomplishments listed above and is always bringing new ideas and evidenced-based practice to the table.


Josh Andrade
HonorHealth








Director, Supply Chain Management
Age (as of today): 36 years old
Hometown: Mesa, Arizona

Alma Matter: Grand Canyon University

Number of Years of Experience in Healthcare: 15 years in healthcare with HonorHealth










Claudia Pacheco














Communities Li ing Communities / Hospital Association of Southern California Health Equity Program Manager Age: 32

















Favorite Hobby: Traveling with wife and two sons. We love spending time at any beach in Southern California. There is something about watching the waves that helps reset my mind and rejuvenate my spirits.



Hometown: Los Angeles, CA





Alma Matter: UC Berkeley

Number of Years of Experience in Healthcare: 11
























Favorite Hobby: Reading thriller books
Favorite Movie of All-Time: Bridesmaids










Favorite thing about healthcare: What captivates me about healthcare is its perpetual innovation and evolution, particularly when it integrates an equity lens to drive transformative change for enhancing community health outcomes.





















































Claudia is invaluable to the organization and was recently promoted from Program Coordinator to Program Manager in just one year. Her leadership and innovative ways of looking at set challenges have made our initiatives successful, such as our Birth Equity Initiative, Supplier Diversity Initiative, and Diversity, Equity, and Inclusion education sessions. In the almost two years she has been with our organization, she received her National Commission for Health Education Credentialing, became a Certified Diversity Professional, and was awarded earlycareer scholarship recipients for a ending the American Public Health Association Policy Action Institute conference that brings together public health leaders, students, and advocacy experts for a collaborative event to discuss proven and proposed policy solutions to tackle today’s most pressing health threats at the local, state and federal levels. She has received awards from Pa’lante Fellow and a 4.0 Tiny Fellow.








































































Eric Swaim



HealthTrust Performance Group
Age: 32





Vice President, Strategic Sourcing





Hometown: Houston, Texas.
Alma Matter: Auburn University for Bachelor in Supply Chain and University of Houston for MBA in Finance











Number of Years of Experience in Healthcare: 10
















Favorite Movie of All-Time: Shawshank Redemption


Favorite thing about healthcare: The challenge, no day is ever the same. And the mission of healthcare and knowing the impact of ensuring the caregivers have the right supplies at the right time to offer top care to our patients.











































Eric is a skilled supply chain leader, possessing a rare combination of strategic vision and tactical mindset that bolsters how HealthTrust serves its members amid supply disruptions, shortages, and inflationary pressures. His professional accomplishments are a testament to his contributions to healthcare. He was recognized at Texas Children’s Hospital with the coveted Nursing Excellence Award for Friend of Nursing for supporting nurses across the system during COVID-19. The accolade validated his leadership and recognition as a trusted partner in problem solving. At HealthTrust, he utilizes data in providing guidance to advisory boards on topics like supply chain resiliency, risk mitigation and holding vendors accountable to performance standards. He leverages all resources— people and technology—in addressing members’ needs and does not differentiate between serving large systems and independent hospitals.





















































































































BY DAVID TAYLOR
For sterile processing (SP) employees to remain engaged and become high-level performers, they need to feel connected to their daily work as well as the mission and goals of the organization. That connection fundamentally develops over time through collaborative working relationships and bonds with peers and other leaders within the workplace.
According to a Gallup poll, highly engaged teams can contribute to reduced absenteeism (81%) and a drop in turnover rates—between 18% and 43%, depending on the size of the business unit.1 Gallup also notes that engaged employees not only show up to work with enthusiasm but tend to be more committed to quality and safety.
How employees feel about their work contributions and commitment to their healthcare organization can be a direct reflection of their engagement, either positive or negative. Direct interaction is among the most effective ways to gauge an employee’s or team’s engagement and satisfaction. An informal way SP leaders can check in with employees is through employee rounding in the department and meeting with individuals or small groups at set times throughout the year. A more formal and highly effective approach is to schedule quarterly check-ins with all employees. Ideally, these check-ins will involve private conversations between the SP leader and each employee and support employees’ success through reflection, planning, problem solving, and constructive feedback.
To prepare for these check-ins, employees should be able to provide a self-assessment of their performance, and the SP leader should be able to speak to specifics regarding the employee’s performance. The following topics can be used as a guide:
• Progress, strengths, events and accomplishments.
• Areas where good performance can be elevated or where improvement is needed.
• Development of short– and longterm goals as well as opportunities such as additional training (to include certification opportunities). When conducting a check-in, the focus should be on the employee’s successes and areas where improvement is needed. Feedback about each employee’s performance should be specific and focus on the behavior, not the person. SP leaders should consider the following when preparing for the meeting:
• Summarizing progress, strengths, events and accomplishments: This can include recognizing good performance reviewing and progressing toward goals, citing strengths exemplified by actions throughout the quarter, examining events the employee was a part of, organized or managed, reviewing accomplishments during that quarter, reviewing recent education, training and certification(s) completed that quarter; and focusing on special assignments, projects, task force or committee participation, and reviewing outcomes and results with numerical data, when applicable.

• Indicating areas where good performance can be elevated or where improvement is needed: This can entail identifying professional development opportunities, highlighting improvement techniques and processes, noting aspects of overall improvement that may be deficient, clarifying expectations about appropriate behavior, identifying goals, skill development, and growth opportunities; providing an action plan and resources to help the employee improve in certain roles, discussing potential training, conferences, and other developmental opportunities; setting reasonable goals for the next quarter; and offering mentoring and coaching support.
Quarterly check-ins help provide a structured approach to drive better staff engagement, foster collaboration, and increase productivity, safety, and output. A strong SP culture keeps employees actively engaged and aligned with the organization’s mission and goals. By fostering an environment that sets clear expectations and equips employees with the necessary tools and resources to excel, SP leaders can create a workforce that is driven and committed, while also promoting a departmental culture where employees’ needs and voices are heard and respected. HPN
Reference: 1. https://www.gallup.com/workplace/231602/right-culturenot-employee-satisfaction.aspx



BY STEPHEN M KOVACH, BS, CFER, CLINICAL EDUCATOR EMERITUS AT HEALTHMARK, A GETINGE COMPANY
Q“We use repair tags, and they do not work on all the variety of instruments we have, such as medical devices that do not have ring handles. What do you suggest?”
AFrom your question, it sounds like we are talking about medical devices such as curettes having round or flat handles without a place to clip a traditional repair tag that easily clips onto ring-handle-type instruments. I understand the need to identify (or tag) customer instruments returned to you (e.g., the operating room [OR] found instruments while being used during a procedure). Tagging helps ensure instruments will not appear again on the sterile field. They either need to be rejuvenated or see the scrap yard after inspection by a medical device reprocessing professional.
Back in the day, the OR staff would just tie a piece of suture around the medical device that needed some attention, and the staff would know that device had to be placed in the repair bin. Thus, the suture (as simple as it was) could be put on any device whether it had a ring handle or not.
But the question remains: what method is good to identify medical devices that need repair and do not have a ring handle for the traditional repair tag to be affixed to? The good news is that there are many options from various vendors.
One possible method I found is the use of cable ties. Staff can use these single-use, heat-resistant cable/instrument ties to affix on the devices identified as needing repair. Once the device is handed off the sterile field, then a cable tie is placed around it. Note that the tail part of the cable guide is not cut off because it “sticks out nicely” for the staff to notice when the device needing repair is returned. It can then be placed in the repair bin with the tie on after it has been decontaminated.
As always, I would make a policy on how to identify instruments so that if asked, you have all the correct documentation. Your policy can have a simple statement that states a red identifier (i.e.,

cable tie, repair tag, pre-printed tags [Fig. 1]) is used for any instrument in need of repair or further inspection for damage. Also, make sure your policy matches up with your various customers for consistency. Remember, whatever methods you use, make sure you have a policy in place that you and your staff can talk about. If not, then you do not have a policy.
Various guidelines/standards organizations offer support that many departments follow to help justify their practice. If you do not have these specific standards or guidelines, buy them for the complete wording and intent of them. Here are some statements you can use in your policy to support your practice of using various methods to “tag” devices from your customers that are damaged or in need of repair.
• ANSI/AAMI ST79:2017 (Section 6.3.5 Prevention of instrument damage) makes the following statement: “. . . have a process in place to identify instruments in need of repair/maintenance and removal from service (for example, a tag).”1
• ANSI/AAMI ST79:2017 (Section 7.5.2.1) states, “General operating instruments should be segregated from delicate items that require special handling, sharp items, and those identified for repair. Repair tags that are designed for surgical instrumentation should remain on the instrumentation throughout the cleaning process.”2
• [The] Association of Surgical Technologist (AST) in their AST:2018 Guidelines for Best Practices for Breaking Down the Sterile Field Section II, 4.C3a, states, “The surgery department should have a process in place for identifying instruments that need repair and removing from service to be sent out for repair, such as a pre-printed tag.”3

Final Note: Regardless of the type of tag or tie you use, I would suggest doing a few sample-run tests in your washer disinfector to make sure they do not melt. Save the data for your records. HPN




Midmark Steam Sterilizers are designed inside and out to make instrument processing as easy and as automated as possible.
01 Navigate cycle setup and other processes with a clear, fi ngerprint-resistant 5-inch touchscreen you can utilize while wearing gloves.
02 Determine cycle status—cycle in progress, cycle complete and cycle error—from a distance with a progressing color-coded LED light bar, large cycle countdown clock and audible cues.
03 Stay audit-ready with device reminders, user authentication, unlimited storage of routine care events for the life of the sterilizer, and automated cycle recordkeeping.
See what makes them different at: midmark.com/nextgeneration

BY KAREN CONWAY, CEO, VALUEWORKS
Anew research paper1 published in the United Kingdom provides some valuable insights into the growing number of U.S. healthcare organizations seeking to reduce the negative environmental impact of their operations. As of April 2024, 140 healthcare delivery organizations, suppliers, not-for-profits, associations, and other related businesses have voluntarily signed the White House Health Sector Climate Pledge, committing to taking specific and transparent steps to cut their carbon emissions in half by 2030. Because the supply chain has been identified as a primary contributor to healthcare’s carbon footprint (which in the U.S. approaches 10 percent of our nation’s total emissions), the paper focuses on the impact of medical devices and how to translate a growing interest in better environmental performance into actions that achieve measurable improvements.
While the paper is focused specifically on the lifecycle of medical products in the U.K. from regulatory approval through to adoption, many findings in the paper are relevant to the United States and other developed nations. One of the paper’s recommendations is to reduce the variation in how healthcare delivery organizations evaluate the environmental impact of the devices they already use or are considering using. Even in the U.K., where healthcare systems are required to give a minimum 10 percent weighting to the social value (including climate change) of procurement decisions, the approach taken by the individual organizations varies, making it hard to use their collective


analyses more broadly to compare products. Further, variation increases compliance costs for suppliers who must respond to varying requests from providers.
The challenge variation poses is highlighted throughout the paper. There is variation in which factors different procurement teams prioritize when sourcing products, how new product introductions are handled, and which products are used by clinicians for the same procedures. Add in the ongoing challenges with supply continuity, and it is hard for healthcare systems to standardize the purchase and use of products that are deemed better for the environment.
Much of the literature reviewed by the authors focused on the benefits of reusable vs. single use devices. According to research cited in the paper, reusable devices on average reduce carbon emissions by 38-56 percent across the product lifecycle, and often lower costs by optimizing the use of procured resources. Despite these compelling statistics, single use devices often win out over reusable products, sometimes simply because their lower acquisition price garners less scrutiny than a reusable product that has a higher initial price tag but is lower in total costs over its longer lifespan.
When it comes to products and the environment, most discussions have focused on which products are better, but the paper also highlights some other important considerations beyond product choice. For example, when manufacturing a product, its total carbon emissions could be reduced if the factory uses renewable vs. fossil fuels. In the distribution stage, consolidating orders and using ground freight vs. air can lower emissions. And repairing damaged products for reuse is better for the environment than discarding the broken device. In the end, however, the most impactful thing we can do is to stop delivering care that is duplicative, unnecessary, or potentially harmful. Research has estimated that the U.S. alone could save $30 billion in healthcare spending per year just by eliminating low or no value healthcare. Further, any care that is not delivered is a 100 percent reduction in carbon emissions and other harmful environmental impacts. HPN References:


































































































































