





The Next Generation Of Contamination Monitoring Technology
For the cleaning verification of surgical instruments, endoscopes, and surfaces, ATP Complete 2 by Ruhof a cloud-based cleaning monitoring system used to help hospitals and other healthcare organizations achieve optimal standardized cleaning levels.






















Sourcing & Logistics
8 > Revenue Cycle Management in the Age of COVID, AI, and Cyberattacks
MATT MACKENZIE
36 > Pharmacy + Supply Chain: A Case for Collaboration
KAREN CONWAY
Surgical/Critical Care
10 > Study: Impact of Lung Ultrasounds in the Prehospital Setting
JANETTE WIDER
Infection Prevention
14 > Respiratory Roundup
JANETTE WIDER
Departments
4 > Goodbye 2024, Hello 2025
6 > What’s on the Web, Advertiser Index

Sterile Processing
16 > Smart Handling of Scopes Saves Time and Money While Safeguarding Care
KARA NADEAU
24 > The Differences Between Peracetic Acid High-level Disinfectants and Sterilants
ARTHUR HENDERSON
28 > Routine Sterilizer Maintenance Vital for Effective Operation
DAVID TAYLOR
30 > Tungsten Carbide Versus Villains: Is it Rust or Corrosion?
STEPHEN M. KOVACH
32 > We Cannot Do It Alone—We All Need Help if We Want to Be Successful
STEPHEN M. KOVACH









BY JANETTE WIDER, EDITOR-IN-CHIEF
This year, Healthcare Purchasing News went through several updates and changes to its staff, design, and offerings.
In January, Associate Editor Matt MacKenzie joined the HPN team and, over the course of this year, has taken a keen interest in technologies like artificial intelligence and topics like cybersecurity in supply chain.
We’ve also added two new sales folks to our team. Kristen Hoffman joined us late last year and Brian Rosebrook, Director of Sales, joined us in April. Both are dedicated to their roles and passionate about our industry.
In March, HPN unveiled its new look (thanks Tracy Arendt!) and tagline, Clinical Intelligence for the Healthcare Ecosystem. This brand has grown so much in the past 40+ years, that we felt a more encompassing tagline would be appropriate, even though Purchasing is still our middle name.
In May, we launched our podcast, Healthcare Hodgepodge. The podcast covers all of HPN’s many verticals including supply chain, infection prevention, surgical and critical care, healthcare IT, environmental services, and more. I’m always looking for guests to join me on the show. If you’re interested, reach out to me via email or connect with me on LinkedIn!

In October, we announced the Top 20 Companies to Work for in Healthcare, a joint program with our sister publications Healthcare Innovation and Medical Laboratory Observer. The list with rankings will be published on all brands’ websites in January 2025, as well as in the February issue of HPN. The findings are based off a 77-question survey on employee engagement and satisfaction, as well as two openended questions.
So, what’s new in 2025?
We’ve reorganized our editorial calendar. Instead of the traditional grid format, the editors of the brand will be looking at what’s topical and adjusting our coverage to keep you, our readers, up to date with the latest and greatest stories. We’ll still be featuring a Sterile Processing Department of the Year and a Supply Chain Department of the Year, to coincide with HSPA and AHRMM.
And this is where our editorial staff needs help from our audience. What is going on in your world that we should know about? Have you had any recent challenges in your hospital or health system that you’ve overcome? Any major successes worth sharing? We want to hear from you! Reach out to me directly at jwider@hpnonline.com for a fast response. Or connect with me on LinkedIn.
VP & Market Leader
Healthcare and Dental
Chris Driscoll
cdriscoll@endeavorb2b.com | 978-880-8345
Editor-in-Chief
Janette Wider jwider@hpnonline.com
Associate Editor Matt MacKenzie mmackenzie@endeavorb2b.com
Senior Contributing Editor Kara Nadeau knadeau@hpnonline.com
Advertising Sales
East & West Coast
Kristen Hoffman khoffman@endeavorb2b.com | 603-891-9122
Midwest & Central Brian Rosebrook brosebrook@endeavorb2b.com | 918-728-5321
Advertising & Art Production
Production Manager | Ed Bartlett
Art Director | Tracy Arendt
Advertising Services
Karen Runion | krunion@endeavorb2b.com
Audience Development Laura Moulton | lmoulton@endeavorb2b.com
Endeavor Business Media, LLC
CEO Chris Ferrell | President June Griffin
COO Patrick Rains | CRO Paul Andrews
Chief Digital Officer Jacquie Niemiec
Chief Administrative & Legal Officer Tracy Kane
EVP Medical & Healthcare Technology Kylie Hirko
EVP Endeavor Business Intelligence Paul Mattioli
Healthcare Purchasing News USPS Permit 362710, ISSN 1098-3716 print, ISSN 2771-6716 online is published 12 times annually - Jan, Feb, Mar, Apr, June, Jun, Jul, Aug, Sep, Oct, Nov, Nov IBG, by Endeavor Business Media, LLC. 201 N Main St 5th Floor, Fort Atkinson, WI 53538. Periodicals postage paid at Fort Atkinson, WI, and additional mailing offices. POSTMASTER: Send address changes to Healthcare Purchasing News, PO Box 3257, Northbrook, IL 60065-3257. SUBSCRIPTIONS: Publisher reserves the right to reject non-qualified subscriptions. Subscription prices: U.S. $160.00 per year; Canada/Mexico $193.75 per year; All other countries $276.25 per year. All subscriptions are payable in U.S. funds. Send subscription inquiries to Healthcare Purchasing News, PO Box 3257, Northbrook, IL 60065-3257. Customer service can be reached toll-free at 877-382-9187 or at HPN@omeda.com for magazine subscription assistance or questions.
Printed in the USA. Copyright 2024 Endeavor Business Media, LLC. All rights reserved. No part of this publication June be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopies, recordings, or any information storage or retrieval system without permission from the publisher. Endeavor Business Media, LLC does not assume and hereby disclaims any liability to any person or company for any loss or damage caused by errors or omissions in the material herein, regardless of whether such errors result from negligence, accident, or any other cause whatsoever. The views and opinions in the articles herein are not to be taken as official expressions of the publishers, unless so stated. The publishers do not warrant either expressly or by implication, the factual accuracy of the articles herein, nor do they so warrant any views or opinions by the authors of said articles.

DETECTO’s Upgraded 6745 Baby Scale

Medication errors, including dosing errors, significantly impact the US healthcare system, according to the National Library of Medicine:
Costing $21 billion annually
Causing 7,000 to 9,000 deaths per year


Using an NTEP-certified medical scale can significantly reduce the risk of preventable dosage-related medical errors. DETECTO is the only medical scale manufacturer with US compliant scales held to NTEP weights and measures standards. This NTEP accreditation means DETECTO scales have been subjected to 100,000 weighing cycles and maintained strict accuracy in a variety of testing temperatures.

A new report has revealed that 23 “previously unreported B. multivorans cases occurred during 2020-2024: 13 at a northern California hospital, eight at a hospital in Colorado, and two additional cases at one of the southern California hospitals. All environmental and clinical isolates were highly genetically similar. The same brand of ice machine and the same filters, descaling, and sanitizing products were used by all four hospitals.”
Read on: hpnonline.com/55233700
Cody Fisher is President of Concordance Innovations. Cody is responsible for the vision, mission and leadership of the overall financial and strategic plan, as well as management and oversight of key functions, policies, procedures and processes. On this episode, Cody discusses AI in Supply Chain with HPN’s Editor-in-Chief Janette Wider.
Listen at: hpnonline.com/55140869
CDC made a statement that it is aware of 26 individuals with Marburg virus disease, as confirmed by the Republic of Rwanda Ministry of Health. According to the Ministry, eight of those individuals have died. CDC is in communication with health officials in the Republic of Rwanda and across the region. To date, no cases of Marburg virus disease related to this outbreak have been reported in the United States, and the anticipated risk of Marburg virus disease to the general population in the United States is low.
Read on: hpnonline.com/55234042

Jimmy Chung, MD, MBA, FACS, FABQAURP, CMRP, Chief Medical Officer, Advantus Health Partners and Bon Secours Mercy Health, Cincinnati, OH
Joe Colonna, Chief Supply Chain and Project Management Officer, Piedmont Healthcare, Atlanta, GA; Karen Conway, Vice President, Healthcare Value, GHX, Louisville, CO Dee Donatelli, RN, BSN, MBA, Senior Director Spend symplr and Principal Dee Donatelli Consulting LLC, Austin, TX
J. Hudson Garrett Jr., PhD, FNAP, FSHEA, FIDSA, Adjunct Assistant Professor of Medicine, Infectious Diseases, University of Louisville School of Medicine
Melanie Miller, RN, CVAHP, CNOR, CSPDM, Value Analysis Consultant, Healthcare Value Management Experts Inc. (HVME) Los Angeles, CA
Dennis Orthman, Consulting, Braintree, MA
Janet Pate, Nurse Consultant and Educator, Ruhof Corp.
Richard Perrin, CEO, Active Innovations LLC, Annapolis, MD
Jean Sargent, CMRP, FAHRMM, FCS, Principal, Sargent Healthcare Strategies, Port Charlotte, FL
Richard W. Schule, MBA, BS, FAST, CST, FCS, CRCST, CHMMC, CIS, CHL, AGTS, Senior Director Enterprise Reprocessing, Cleveland Clinic, Cleveland, OH
Barbara Strain, MA, CVAHP, Principal, Barbara Strain Consulting LLC, Charlottesville, VA Deborah Petretich Templeton, RPh, MHA,Chief Administrative Officer (Ret.), System Support Services, Geisinger Health, Danville, PA
Ray Taurasi, Principal, Healthcare CS Solutions, Washington, DC

It’s more than a box.
As the leading provider of rigid sterile containers, Aesculap has developed the AESCULAP Aicon® Sterile Container System to help ensure sterile security.
With a unique design that increases the aseptic area by 200%1, this innovative system significantly reduces the risk of contamination. Trust the AESCULAP Aicon Sterile Container System to uphold the highest standards of sterility in your operating room, providing a crucial line of defense for patient safety.

Scan to learn how the AESCULAP Aicon Sterile Container System can help your SPD Operate with Greater Precision. 1
BY MATT MACKENZIE, ASSOICIATE EDITOR
Complications continue to arise when it comes to maintaining and managing revenue cycle. The COVID-19 pandemic introduced plenty of issues that continue to reverberate into the space to this day, and now, the increasing specter of cyberattacks and ransomware means that even more protections need to be taken.
Healthcare Purchasing News was able to speak with Prashant Karamchandani, senior partner at Chartis, to get his insights on how to maximize efficiency and avoid
pitfalls when it comes to revenue cycle management.
Can you tell our readers a little about your background?
I’ve been in revenue cycle for over 22 years and have been at Chartis for a little over seven years. I’m a senior partner at Chartis and I co-lead our revenue cycle transformation practice. We work with a lot of our clients, including the provider ecosystem, on optimizing revenue cycle processes. We also coordinate with our peers and

fellow practices around broader financial performance improvement, folks that work in our IT and digital practice and our supply chain.
does revenue cycle management look like today, four years into the COVID-19 pandemic?
I think the biggest change we saw right when the pandemic hit was the move to a remote workforce. When we would do our work before, we would travel to client sites, and they would have their revenue cycle operations exclusively on site. Maybe some operations were remote. During the height of the pandemic, many of our clients had to go remote, and I think some have stayed in that model. That was probably the biggest shift: you no longer could walk the floors and see what your staff is doing. We had to ask what the investment was in our tools, technology, and infrastructure to support that remote ecosystem and making sure the work is still getting done in a timely way.
unique challenges did COVID pose?
During the start of the pandemic, when organizations were canceling or postponing elective procedures and we saw a decline in volume, you had a lot of people that may not be having to go process and work all the accounts that they’re used to seeing. Revenue cycle’s largely a volume-driven function, so the question became, how
do you shift and pivot and get folks working on things that are supporting what’s happening. We began to pivot our resources to areas that are not necessarily core rev cycle issues, but just leaning into the health system or organization to drive values. Human resource coordination was another one of the key things in the pivot, and then we needed to prepare ourselves as things scaled back up to get back into the normal course of business.
There was an increase in virtual visits, so there was a lot of work done to set up organizations to be able to build and successfully build claims out and capture the information, both from a technology and an operational standpoint.
How do supply chain disruptions, especially those driven by cyberattacks and ransomware, affect revenue cycle management? How is the industry protecting itself?
Supply chain disruptions increase costs and put more pressure on the revenue cycle to be more efficient. You have to ensure that you’re collecting every expected dollar now, thinking about revenue leakage and revenue capture, whereas you may have had a little bit of latitude before. There’s a need for increased rigor no matter what we’re billing. You want to keep the revenue performing as high as possible to mitigate some of those cost impacts.
The Change Healthcare attack from earlier this year, and some more [cyberattacks] that have been in the media around provider organizations, impact things. They make it so providers are unable to get claims out the door, creating a backlog of claims that need to be billed. It forces that same rigor on things that were working well to ensure that they’re still being done. In revenue cycle, we also need to look at service vendors and outsourcers
to ensure that their security protocols are right. You need to balance the immediate need you have for that service or technology with your comfort that the vendor you’re contracting with meets all the security requirements.

Prashant Karamchandani
What sorts of things do you look for initially to help you make an informed decision on which vendors to work with when it comes to cybersecurity?
You look at a bunch of different variables, including where their operations are based and what their protocols are. If you’re a buyer as a provider organization, you’re also pressure testing by looking at the reference checks and how complex their implementation is. You also want to hear from actual existing clients who have gone through it, perhaps more recently than someone who’s an established party.
The threat and increase of cyberattacks has organizations thinking about risk mitigation strategies. The question becomes if you want to put all your eggs in one basket with a certain function to one vendor, or if you want to split it over two – basically, asking if you’d rather have some redundancy or a backup, which can be costlier. But the impact of not having claims go out the door and cash coming in can be catastrophic. At the same time, if something happens with the one party you contract with from a cyber standpoint, you’re now at the mercy of their mitigation strategy versus having a bit of your own to be flexible with.
What impact is artificial intelligence (AI) having on rev cycle?
There’s a lot of interest from a revenue cycle standpoint in this industry; it’s been talked about for years.
There have been vendors that have tried to be out front and have had some missteps. You need to ask yourself what the problem is you’re trying to solve, or the concrete use case that you’re going to apply it to, and then ask what the tangible ROI [return on investment] and benefit is. You’re not seeing it as broadly as just “you can buy an AI platform and it will automate and do all these things for your rev cycle.” You have to get more discrete with it than juts buying something, turning it on, and hoping it fixes lots of problems. It’s not an instantaneous fix; these solutions have to grow by having more data behind them for them to become more accurate and applicable.
What do you see as important next steps for the rev cycle industry?
A lot of providers out there have made large investments in technology, whether it’s their main core system or additional solutions. Asking yourself how to maximize what you’ve invested in first versus looking outside and trying to procure something new is important, or really pressure testing the core ecosystem you have and making sure you’ve maximized the functionality, the setup, the adoption, and the engagement.
Any more thoughts you’d like to share with our readers?
Better engagement between providers and payers can naturally reduce costs on both sides and make things a little bit easier; I think there’s a lot of opportunity there. You’re seeing some of that happening in the industry, and I think if that can continue, it’s a win for everyone, specifically patients and those receiving care. But the benefits are also there for providers and payers. HPN


Frances Russell, M.D., author of the study that was published last year, shares her insights on the study that focuses on patients with acute heart failure.
BY JANETTE WIDER, EDITOR-IN-CHIEF
Astudy entitled “Prehospital lung ultrasound in acute heart failure: Impact on diagnosis and treatment” was published last year in Academic Emergency Medicine.
According to that study, patients with acute heart failure (AHF) are commonly misdiagnosed and undertreated in the prehospital setting. The study said, “These delays in diagnosis and treatment have a direct negative impact on patient outcomes. The goal of this study was to determine the diagnostic accuracy of paramedics with and without the use of lung ultrasound (LUS) for the diagnosis of AHF in patients with dyspnea in the prehospital setting. Secondarily, we assessed LUS impact on rate of and time to initiation of HF therapies.”
Further, “This was a prospective interventional study on a consecutive sample of patients transported to the hospital by one emergency medical services agency. Adult patients (>18 years) with a chief complaint of dyspnea were included. LUS was performed by trained paramedics and was defined as positive for AHF if both anterior–superior lung zones had greater than or equal to three B-lines or bilateral B-lines were visualized on a four-view protocol. Paramedic diagnosis was compared to hospital discharge diagnosis which served as the criterion standard.”
As for the results, the study noted, “Of the 264 included patients, 94 (35%) had a final diagnosis of AHF. Forty total patients had a LUS
performed; 17 of these patients had a final diagnosis of AHF. Sensitivity and specificity for AHF by paramedics were 23% (95% confidence interval [CI] 0.14–0.34) and 97% (95% CI 0.92–0.99) without LUS and 71% (95% CI 0.44–0.88) and 96% (95% CI 0.76–0.99) with the use of LUS. In the 94 patients with AHF, 14% (11/77) received HF therapy prehospital without the use of LUS and 53% (9/17) with the use of LUS. LUS improved frequency of treatment by 39%. Median time to treatment was 21 min with LUS and 169 min without.”
Healthcare Purchasing News had the opportunity to speak to one of the study’s authors, Frances Russell, M.D. Russell is a tenured professor of emergency medicine and the ultrasound research director in the division of ultrasound at the Indiana University School of Medicine. She earned her Doctor of Medicine at the University of Wisconsin, Madison School of Medicine and Public Health. She has over 50 peerreviewed publications, has received grant funding from the NIH NHLBI and American Heart Association, in 2021 received the Society of Academic Emergency Medicine (SAEM) Academy of Ultrasound (AEUS) Academic Excellence award, and in 2023 received the SAEM AEUS Most Influential Researcher award. Dr. Russell currently serves as an American College of Emergency Physician (ACEP) ultrasound research subcommittee co-leader and previously served on the SAEM
AEUS executive committee as the Research Officer.
How prevalent is acute heart failure (AHF)? Is this a major problem in the U.S.?
More than a million patients are hospitalized with AHF annually. AHF refers to the rapid onset or worsening of signs of heart failure with symptoms that include severe shortness of breath, swelling in the legs and abdomen, and fatigue. AHF has a high healthcare cost burden accounting for over 20 billion dollars annually.
A leading cause of unplanned hospitalizations in the U.S., AHF is triggered by various factors, including medication non-compliance, diet non-compliance, heart attacks, and high blood pressure. As symptoms are similar to other conditions, such as chronic obstructive pulmonary disease (COPD), pneumonia, or asthma, AHF is challenging for first responders to diagnose correctly. Delayed diagnoses and treatments lead to poor outcomes for many patients - more than a quarter of patients diagnosed with AHF will die within 12 months.
How can ultrasound imaging help with AHF?
Lung ultrasound (LUS) can significantly help diagnose AHF and allows for quicker identification of AHF cases, compared to waiting for other diagnostic test results such as chest X-rays. It has also been shown to be more accurate than traditional diagnostic methods such as patient history, physical examination, and blood tests.
How common is it for paramedics to receive ultrasound training?
Ultrasound is not yet a standard skill for most paramedics in the U.S, although it has been adapted in prehospital settings for decades in other
countries. In the U.S., field use of ultrasound is in a developmental stage, with ongoing research and implementation efforts. Within the last decade, the onset of more affordable, portable, all-in-one ultrasound probes – like the ones we used in our study—have made paramedic adoption increasingly feasible, supporting this transition toward a new standard of care.
In Europe, prehospital physicians are commonly using prehospital ultrasound to help guide care in patients with shortness of breath. Other studies have shown that, with modest investments in training and equipment, ultrasound could prove helpful for flight nurses or critical care paramedics, trauma assessments, and mass casualty incidents. Really, handheld ultrasound could be used in nearly any situation where healthcare providers and other medical staff need to quickly get an idea of what’s happening within the body.
Are there any challenges associated with paramedics having ultrasound technology on their ambulance? What is the financial burden?
One challenge we encountered during our study was that about 20% of patients whose symptoms qualified them for the study did not receive LUS when one was available on the ambulance. We theorize that some paramedics might have been less confident in their skill with use of the handheld ultrasound device or did not save images or interpretations.
Ongoing training would likely be the largest investment an emergency services provider would need to make, as the cost of the devices themselves is relatively affordable as medical equipment goes – just a couple thousand dollars.
Can you talk about the results with us? Was any of this surprising?
Our study looked at training a group of 26 full-time paramedics to diagnose AHF using a handheld portable ultrasound device from Butterfly Network. The training consisted of 30 minutes of classroom education, followed by 30 minutes of hands-on scanning. Participants also had to pass a written test and demonstrate competent use of the Butterfly device.
We found that paramedics with little to no prior training in LUS were able to use this tool accurately in the pre-hospital setting and that advanced diagnostic tools increased correct diagnoses of AHF by paramedics from 23% to 71%, with a very small 2.5% rate of false positives.
The significantly higher level of accuracy achieved by paramedics with relatively minimal training was impressive. This was not unexpected as we know LUS is easy to learn and can be performed by non-physicians. From a patient care perspective, there was a significant reduction in average time to treatment – from almost three hours to just 21 minutes when paramedics used the LUS device. Since we know that earlier treatment of AHF is associated with better outcomes, this could have a significant positive impact on mortality.
Will there be further studies done with additional EMS teams?
We purposefully limited the size of this pilot study to determine if handheld ultrasound devices could be adapted into prehospital management of patients experiencing AHF. More research is needed with a larger cohort of patients and with other EMS agencies. We also have plans to evaluate paramedic performed LUS with an AI augmented interpretation to evaluate diagnostic accuracy. HPN
You may dry all your surgical devices in this general purpose dryer:
Batteries
Cameras
Cartilage crushers
Clamps
Drills
Forceps
Light cords
Orthopedic devices
Osteotomes
Retractors
Rigid endoscopes
Rongeurs
Scissors
TEE probes
Trocars


BY JANETTE WIDER, EDITOR-IN-CHIEF
On April 18, the World Health Organization (WHO) published a global technical consultation report announcing updated terminology for pathogens that transmit through the air. The pathogens covered include those that cause respiratory infections, e.g. COVID19, influenza, measles, Middle East respiratory syndrome (MERS), severe acute respiratory syndrome (SARS), and tuberculosis, among others.
A press release on the announcement says that “The publication, entitled ‘Global technical consultation report on proposed terminology for pathogens that transmit through the air,’ is the result of an extensive,
multi-year, collaborative effort and reflects shared agreement on terminology between WHO, experts and four major public health agencies: Africa Centres for Disease Control and Prevention; Chinese Center for Disease Control and Prevention; European Centre for Disease Prevention and Control; and United States Centers for Disease Control and Prevention. This agreement underlines the collective commitment of public health agencies to move forward together on this matter.”
Further, “The wide-ranging consultation was conducted in multiple steps in 2021-2023 and addressed a lack of common terminology to describe the
transmission of pathogens through the air across scientific disciplines. The challenge became particularly evident during the COVID-19 pandemic as experts from various sectors were required to provide scientific and policy guidance. Varying terminologies highlighted gaps in common understanding and contributed to challenges in public communication and efforts to curb the transmission of the pathogen.”
The following common descriptions are now being used to characterize the transmission of pathogens through the air, under typical circumstances:
• Individuals infected with a respiratory pathogen can generate and expel infectious particles containing the pathogen, through their mouth or nose by breathing, talking, singing, spitting, coughing, or sneezing— these particles should be described with the term “infectious respiratory particles” (IRPs)

• IRPs exist on a continuous spectrum of sizes, and no single cutoff points should be applied to distinguish smaller from larger particles—this facilitates moving away from the dichotomy of previously used terms: ‘aerosols’ (generally smaller particles) and ‘droplets’ (generally larger particles)
Under the umbrella of ‘through the air transmission’, two descriptors can be used:
• Airborne transmission or inhalation
• Direct deposition
On June 26, the CDC updated its recommendation for the use of Respiratory Syncytial Virus (RSV) vaccines in people ages 60 and older. For this upcoming respiratory virus season, CDC recommends:
• Everyone ages 75 and older receive the RSV vaccine.
• People ages 60–74 who are at increased risk of severe RSV, meaning they have certain chronic medical conditions, such as lung or heart disease, or they live in nursing homes, receive the RSV vaccine.

This recommendation is for adults who did not get an RSV vaccine last year. The RSV vaccine is not currently an annual vaccine, meaning people do not need to get a dose every RSV season. Eligible adults can get an RSV vaccine at any time, but the best time to get vaccinated is in late summer and early fall before RSV usually starts to spread in communities.
The updated recommendation for people 60 and older replaces the recommendation made last year to simplify RSV vaccine decision-making for clinicians and the public.
Immunizations were available last year for the first time to protect people at increased risk for severe RSV, including infants and young children, and people ages 60 and older. The updated recommendation is based on analyses of RSV disease burden among people 60 and older, as well as RSV vaccine effectiveness and cost-effectiveness studies. Those studies included the first real-world data since RSV vaccines were recommended for people 60 and older.
Healthcare providers should recommend RSV vaccines to their eligible patients, as well as discuss what other vaccines they will need this fall to help prevent respiratory infections.
In August, HHS launched a new national campaign, called Risk Less. Do More., which aimed to “increase awareness of vaccines that reduce serious illness from influenza (flu), COVID-19, and respiratory syncytial virus (RSV) in high-risk populations and to limit the spread of these viruses among all Americans.”
HHS is hoping to get ahead of a potential uptick in cases over the coming fall and winter. Last fall and winter, “these infections caused 800,000 hospitalizations. Without immunization, the risk of serious illness remains highest in certain populations, including adults ages 65 and older, residents of long-term care facilities, pregnant people, and those living in rural
areas. Some racial and ethnic groups, including Black and Hispanic populations in the United States, are also at higher risk.”
Risk Less. Do More. will “deliver research-based messages through paid advertising and media coverage on TV, radio, print, social, digital, and out-ofhome platforms. The campaign will reach all audiences, with a particular focus on those at highest risk, including older Americans and people who may have less access to healthcare information and support, with facts about life-saving vaccines that can help them avoid severe illness.”
In October, CDC confirmed two human cases of H5 bird flu in California. Both of the cases occurred in people with “occupational exposure to infected dairy cows.”
This identification in people exposed to infected animals is “not unexpected and does not change CDC’s risk assessment for the general public, which continues to be low. At this time, there is no known link or contact between the first and second confirmed cases in California, suggesting these are separate instances of animal-to-human spread of the virus.”
These cases are the first among humans in California, “where H5N1 outbreaks among dairy herds were first reported in August 2024. H5N1 bird flu was detected for the first time in cows this year in the United States.” Including this most recent case, “16 human cases of H5 have been reported in the United States during 2024, bringing the total to 17 cases since 2022. Cases during 2024 have been reported in Texas (1), Michigan (2), Colorado (10), Missouri (1) and California (2). Six of the 16 reported human cases have been linked to exposure to sick or infected dairy cows. Nine cases had exposure to infected poultry. The source of infection for the one case in Missouri has not been determined.”
HPN has reported on these H5N1 outbreaks over the past year. HPN
BY KARA NADEAU, SENIOR CONTRIBUTING EDITOR
While essential for patient care, endoscopes tend to get a bad rap when it comes to reprocessing and maintenance. Their complexity is a double-edged sword: facilitating advanced procedures, including screening, diagnosis, and treatment, but necessitating a multitude of steps to effectively and safely reprocess.
Considering these challenges, HPN presents the story of how Nemours Children’s Hospital, Delaware, minimized
complexities and costs associated with reprocessing unused endoscopes.
Additionally, Hannah Schroeder, BSHA, CRCST, CHL, CIS, CER, clinical education specialist, Pure Processing, offers her insights on endoscope cleaning.
Lastly, Michael Matthews, MBA, CLSSGB, Director of Customer Training and Education at Agiliti, and Tom Milano, president and COO, Encore Medical Device Repair, share best practices for protecting endoscope assets.

Collaboration pays off for Nemours Children’s Hospital, Delaware
With its commitment to patient care and safety, Nemours Children’s Hospital established a seven-day hang time for unused endoscopes, meaning that after the seventh day in storage, the endoscopes must be reprocessed.
The weekly reprocessing of unused scopes presented labor and cost burdens. The sterile processing (SP) team spent hundreds of hours each year on the reprocessing, and the hospital spent significant money on consumables (e.g., detergent, PPE, disinfectant), not to mention the costs associated with wear and tear on the scopes.
Edna Gilliam, DNP, MBA, RN, CNOR, NEA-BC, assistant vice president, Perioperative Services & SPD, DV, Nemours Children’s Hospital, recalled, “Someone in either the SP department (SPD) or infection prevention (IP) asked the question, ‘why do we have to do this every seven days?’”
This prompted an intensive multidisciplinary initiative led by the SP, IP, and perioperative services teams to double the time between reprocessing unused scopes, from every seven to every 14 days. But before the change could be made, they had to prove it would not negatively impact patient care and safety.



The team was led by Gilliam, Nemours Children’s Hospital’s SPD Manager Kwame Addomah Gyabaah, MHA, Mini MBA, BS, ACHE, CHL, CER, CIS, CRCST, and the hospital’s Infection Prevention and Control Director Meg Feeney Gilman, MAS, CIC, FAPIC.
The investigation
Gilliam, Gyabaah, and Gilman began their research to determine where the seven-day rule originated, starting with the American National Standards Institute (ANSI)/ Advancement of Medical Instrumentation (AAMI) ST91:2021 Flexible and semi-rigid endoscope processing in healthcare facilities standard.
“AAMI’s recommendation to determine time between unused scope processing was to follow the endoscope manufacturers’ instructions for use (IFU) or perform a multidisciplinary risk assessment,” Feeney Gilman explained. “Because the IFUs didn’t provide a hang time, we proceeded with the assessment to compare reprocessing every seven days versus every 14 days.”
Using AAMI guidance, the team completed the risk assessment, scouring standards and published research for evidence to support the proposed change. They presented their assessment to Nemours Children’s Hospital’s
infection prevention and control committee, which is comprised of not just IP professionals, but other clinical stakeholders as well, including representatives from the gastrointestinal (GI) and respiratory teams, the director of surgical operations, and outpatient services.
“In that first meeting with the infection prevention and control committee, there were a lot of questions,” said Gilliam. “One reason is the lack of a standard for the unused scope reprocessing timeframe. In perioperative services, we can go to the Association of periOperative Registered Nurses (AORN), which is very specific with their guidelines and best practices. The committee members wanted to see something similar from AAMI on the scopes, but it just wasn’t there.”
“It all came down to the quality assurance piece,” Gilliam continued. “The committee wanted us to show how this move was beneficial to our organization, but more importantly, to our patients, staff members, and equipment. With their feedback, we were able to come back together as a team and make that quality assurance argument even stronger.”
Gilliam, Gyabaah, and Gilman developed a process for random culturing of unused scopes in the SPD, which was approved by the infection prevention and control committee for a three-month trial.
“After the unused scopes passed the seven-day expiration period based on hospital policy and were presented for reprocessing, we swabbed them to test for protein buildup,” Gyabaah explained. “We did this for three months, recording the results in our SPM system.”
“We did not see any protein buildup on the tested scopes and did not identify any adverse outcomes in our patients through either our electronic surveillance system or our patient safety and risk system,” Gilman commented.
“We gathered the data and information and presented it to the infection prevention and control committee,” said Gyabaah. “At that time, they granted approval for a housewide policy change from seven to 14 days.”
Gilliam, Gyabaah, and Gilman engaged Nemours Children’s Hospital’s supply chain team to calculate consumable supply savings from the change.
“Together, we pulled figures for the supplies we were using before and after the three-month pilot period,
BY DELANEY REBERNIK
Editor’s note: This article is the final part in a three-part series exploring the challenges and opportunities facing healthcare procurement leaders as outlined in the 2024 Healthcare Procurement and AI playbook from Healthcare Purchasing News (HPN) and Staples Business Advantage (SBA). Respondents’ comments have been lightly edited for length and clarity.
For today’s healthcare procurement leader, a focus on the future is crucial to building an operation that stands the test of time.
Sourcing and logistics — the cornerstones of a thriving supply chain — are the right place to start, according to more than 170 leaders surveyed for HPN and SBA’s 2024 Healthcare Procurement and AI report. “We need to enhance our ability for technological innovation to cope with the changes brought about by various developments,” one respondent notes.
Headwinds range from a global pandemic and war to widespread cyber threats and supply chain disruption. Facing such challenges head-on requires grit, resilience, and an expansive view of innovation.
Within the realm of sourcing and logistics, leaders identify two areas that are especially ripe for innovation:
• Streamlining supplier management: For 55% of respondents, improving supplier management is a “high” or “critical” priority. Potential obstacles include selecting reliable partners and maintaining smooth communication even in the face of setbacks. “The biggest challenge is finding qualified suppliers who can quickly and stably handle after-sales issues,” one respondent explains.
• Optimizing ordering: 82% of respondents call order optimization a top priority. The practice remains difficult, however, due to factors like “out-of-stock items, delivery delays, and increased pricing,” as well as “disorganized purchasing, limited visibility, and the risk of fraud and human error,” respondents note. These issues can force procurement teams to scramble for alternatives while waiting for back-ordered products.
1. Automate routine tasks: “There are too many repetitive tasks, consuming time and elongating the procurement cycle,” one respondent explains.
According to survey respondents, procurement leaders can streamline tasks such as:
Tracking and recording routine and initial orders
Comparing supplier prices
Organizing and scheduling procurements
2. Get strategic with advanced tech: 74% of the senior executives and directors surveyed have integrated AI into some or all areas of procurement — and 92% of adopters are happy with the results. AI helps these users by:
• Increasing procurement efficiency (according to 64% of adopters)
• Reducing repetitive tasks (58%)
• Optimizing ordering (57%)
• Respondents suggest three best practices for success:
• Starting with a clear goal in mind
• Being open to experimenting
• Keeping humans “in the loop” and at the helm
3. Better forecast demand: “Accurately predicting the required products and timely procurement are quite challenging,” one leader explains. Predictive procurement is an emergent solution that uses data analytics and AI to forecast demand and proactively address challenges. With 77% of respondents citing demand forecasting as a top priority, this technology could provide much-needed relief in navigating procurement barriers.
4. Collaborate with partners: When implementing innovative solutions, such as those involving AI, leaders should seek input from peers, leaders, and experts who’ve been there.
“A lot of us are going to have to partner with third parties to bring AI-enabled tools into our organizations,” explains Jack Koczela, director, analytics and transformation, supply chain, at Froedtert Health, a Wisconsin-based system with 10 hospitals and more than 45 health centers and clinics. “Large IDNs and healthcare organizations may be able to hire AI professionals. But smaller organizations will probably expect [ERP vendors and other partners] to fold AI into the solutions they offer.”
5. Motivate your team: At a time when myriad macro forces are fueling burnout and turnover, supply chain leaders can motivate their teams with competitive compensation packages, along with evidence of how employees’ input is used to shape solutions that make their jobs easier. “Establish incentive mechanisms to encourage innovative ideas,” one respondent advises.
6. Lean on time-tested methods: Not all innovation needs to be high-tech. Many respondents point to established frameworks and guidelines that can improve team performance and satisfaction. Lean principles, for example, “focus on maximizing customer value while minimizing waste,” one respondent notes.
“Organizations can streamline processes, reduce unnecessary steps, and enhance overall efficiency.”
Procurement leaders can ensure long-term success by reinforcing foundational practices in sourcing and logistics while embracing time-tested strategies, emerging solutions, and a continuous openness to innovation.
Staples Business Advantage is a trusted partner for procurement leaders at thousands of healthcare organizations nationwide. Partnerships with top GPOs enable clients to achieve significant cost savings while streamlining purchasing across multiple product categories, including EVS, furniture, breakroom, office supplies, and more. Learn more staplesadvantage.com/healthcaresupplychain









including enzymatic detergent, personal protective equipment (PPE), and high-level disinfectant,” said Gilman. “To this, we added an estimated SP labor savings. From there, we extrapolated the consumable and labor savings over the three months for an estimated annual savings.”
The team determined the extension of unused scope reprocessing from seven to 14 days saves Nemours Children’s Hospital approximately $150,000 per year, including 576 hours of SP staff time.
“All the work the SPD team did during the three-month pilot to test the scopes and track the results really paid off,” said Gyabaah. “The switch to the 14-day reprocessing cycle definitely means less work on our part.”
Lessons learned and advice for others
When asked for their key lessons learned through the initiative, Gilliam, Gyabaah, and Gilman offered this advice to others wanting to make a similar change.
Don’t go it alone
Gilliam stressed how the multidisciplinary approach was critical to the initiative’s success, stating:
“Having everyone at the table from the very beginning was necessary because everyone looks at things from a different lens. We were able to engage in conversations, address concerns and questions, and move forward with confidence knowing we were all in this together.”
Gilman added how she found it beneficial for her team to


work with Kwame and the SP team in a different way, stating:
“The nature of our work in infection prevention is to be problem finders; therefore, our presence in the SPD and elsewhere in the hospital is often not welcome. Kwame and I had a good relationship before, but working together on this project has strengthened it even more. I think we’ve come to see each other’s perspectives a little bit more clearly. And support from Edna and surgical services was vital.”
“It’s a great partnership,” said Gyabaah. “Given their role as problem finders, rounding in the SPD with infection prevention helps keep us on our toes as they can identify things we might have overlooked. We had a visit from The Joint Commission (TJC) not too long ago and Meg and her team were great partners in helping us prepare for that as well.”
Do your legwork ahead of time
Gilman echoed Gilliam’s comment on engaging stakeholders from the beginning and added how her work with Gilliam and Gyabaah to do the research and establish the case ahead of time before meeting with the infection prevention and control committee paved a more positive path forward.
“That is something I really want to drive home: if you do the legwork ahead of time the rest is, I wouldn’t say ‘easy’ because it’s not easy, but it’s easier,” she stated. “By reviewing hundreds of pages of standards and guidelines, performing the risk analysis, creating a proposal for the body that has oversight of this work,
and securing their approval, everything was ready to go when Gyabaah and the SP team were ready to enact the change.”
Leverage the power of data Gyabaah pointed to the power of data when enacting change, stating:
“It was not an easy decision to change our reprocessing policy but the data from our pilot spoke volumes. It played a key role in convincing stakeholders that the move from seven to 14 days would not adversely impact patient care and safety.”
“We are so fortunate that we have Kwame with his ability to leverage technology in a way that not only captured the evidence but also presented it in a way that was easy for stakeholders to understand,” said Gilman.
cleaning considerations
Collaboration and communication among those departments and individuals responsible for endoscope reprocessing is critical to minimizing variations that impact quality. Standardization starts with endoscope cleaning, according to Hannah Schroeder, BSHA, CRCST, CHL, CIS, CER, Clinical Education Specialist, Pure Processing. She stated:
“Manual cleaning practices and available tools, technicians’ competency, and how technicians conduct their testing are all attributors to variance in endoscope reprocessing and cleaning verification. We are seeing reputable studies being published that speak to the consequences that come from variance in practices and it starts before test sampling.”
Schroeder pointed out how “automated processes help reduce human error, provide consistent and repeatable processes, and enhance cleaning results with calibrated pressure output and higher volumes of cleaning solution.” As for those aspects of endoscope reprocessing that
necessitate manual intervention, she said there is growing awareness for the need to evaluate technology and techniques.
“More recently, endoscope brushes are seeing new innovations, including specialized, validated brushes that have proven results to improve
channel cleaning of flexible endoscope channels,” said Schroeder. “With improved technology, materials, and designs, these brushes adapt to the wear and tear of reusable endoscope channels, while also relieving some of the repetitiveness that can lead to staff fatigue and added labor.”




Proper reprocessing, storage, and maintenance of endoscopes not only protects patients but also serves to protect the endoscopes themselves.
“Improperly cleaned endoscopes and damaged endoscopes are connected issues,” said Michael Matthews, MBA, CLSSGB, Director of Customer Training and Education at Agiliti. “When manufacturers originally design endoscope cleaning instructions, they are intended to be used with a fully functioning device. The instructions are important for reducing infection risk as part of reprocessing, but they will not be effective if the endoscope is already damaged.”
Tom Milano, president and COO, Encore Medical Device Repair, commented on the topic, offering his advice to healthcare organizations.
“Endoscopes are vital for patient care in U.S. hospitals, but they are also expensive to acquire ($40,000 or more) and maintain,” said Milano. “In some hospitals, the endoscopes budget is a million dollars or more.”
Milano pointed out how endoscopes are delicate instruments that break easily if not appropriately protected and serviced. “The original manufacturer typically offers a service contract that is often 20-30% of the price of the endoscope itself,” he commented. “However, third-party vendors play a major role in the system because they can typically service the entire portfolio of endoscopes and offer a price advantage.”
“Unfortunately, scope damage is often overlooked by end-users because they are only flagged as ‘damaged’ when the scope no longer functions as expected during the procedure,” said Matthews.
“The reality is that a scope can be damaged in subtle ways that make it difficult to clean properly,”
Matthews continued. “For example, gouges in the distal tip or scratches in the biopsy channel will likely have no meaningful impact on the scope’s performance during the procedure, but



both types of damage will create areas where bioburden will become embedded into a biofilm. This can make the cleaning process ineffective and leave facilities with contaminated endoscopes in circulation.”
According to Matthews, damage prevention begins with education. He stated:
“Many technicians have not been trained on early warning signs of damage that indicate a scope may not be able to be cleaned effectively. Unless a facility has a robust inspection and quality-assurance program that emphasizes preventive identification of damage, it is likely that their scopes are damaged already – and their patients are at greater risk.”
“Leaders should ensure their technicians receive training on how to effectively identify types of endoscope damage that can jeopardize the effectiveness of the cleaning process – and what’s causing the damage,” he added.
Matthews also noted how technicians must be given the time necessary to properly examine an endoscope during reprocessing.
“Every time a scope is handled, it could have been damaged,” he explained. “Based on the new endoscope reprocessing standard ANSI/AAMI ST91:2021, thorough inspection must be part of the regular reprocessing cycle. Unfortunately, many technicians are under pressure to reprocess scopes within tight timeframes, which makes it challenging to follow the appropriate device cleaning instructions and carefully inspect each scope for damage. To put technicians and patients in the best position, make sure technicians have enough time for effective cleaning, damage inspection, and education and training.”
Industry partners
Milano described the endoscope repair and maintenance industry as “dysfunctional,” noting how “hospitals usually spend more than they should on less than they deserve.”
“Repair and service quality is often not impressive, services are not adequate for the training and maintenance needs of the healthcare facility, prices are not transparent, turnaround times are long, and endoscopes that could be repaired are unnecessarily discarded, forcing hospitals to spend large amounts of money acquiring new endoscopes,” he stated. “Service contracts requiring hospitals to pay for ‘over-consumption’ usually lead to exaggerated, unnecessary spend levels.”
Milano believes healthcare facilities need to raise their expectations for endoscope maintenance partners, stating:


“Those partners should be invested in the preventative process that enables maximum equipment lifetime and minimum hospital costs – not in invoicing repair after repair. Pricing needs to be transparent and fair, and



the quality of maintenance and repair technologists needs to be consistent and high. The industry, including healthcare facilities, would benefit from a certification program that ensured not only technically adequate training, but also training focused on how to prevent repairs through proper handling.”
Matthews spoke to the importance of auditing, data documentation, and continuous improvement, stating:
“As a starting point, leaders should partner with a repair vendor to help them understand their unique challenges and opportunities for improvement. Data from the repair vendor is critical to targeting possible sources of damage so leaders can focus their attention and efforts on the most significant opportunities. Leaders should also make a regular practice of auditing their process and documenting their findings. Regular auditing, along with repair data, is key to making sustained, incremental improvements and establishing a culture of constant process improvement.” HPN















































































BY ARTHUR HENDERSON, SENIOR CLINICAL EDUCATION SPECIALIST, STERIS CORPORATION
In the world of sterile processing, active ingredients tend to be the focus. Often, this leads to a belief that all products with the same active ingredient perform the same. Nothing can be further from the truth. Nothing illustrates this more than pain killer medications, such as acetaminophen. Acetaminophen can include ingredients to make it a solid pill, a gel pill, or a liquid. Some ingredients cause the acetaminophen to be slowly released extending the time that it controls pain. Other ingredients help reduce the possibility of upset stomach from ingesting the medication. Though the active ingredient is the same in all these medications, the formulation significantly affects how the medication will work. Imagine if an individual with a sensitive stomach
1.

got a normal pill or a patient recovering from a procedure did not get the extended-release version.
Many sterile processing (SP) professionals assume that products using peracetic acid are all the same. Of greater concern is that this belief can lead to improper selection and use. Understanding how formulations work can help in proper selection and reinforce the need to follow the product’s instructions for use.
Peracetic acid is an oxidative chemistry. It kills organisms through destruction of bonds in proteins, enzymes, and other components necessary for cellular function. There are two key facts about peracetic acid. The

first is that peracetic acid is made by a reaction between hydrogen peroxide and acetic acid within an aqueous environment. These compounds both make peracetic acid and are byproducts of the peracetic acid breaking down. This means that acetic acid and hydrogen peroxide will be found in every formulation. By themselves, each chemical can kill microorganisms. Peracetic acid kills the fastest with acetic being the slowest. When combined, the concentration and ratio of each chemical within the high-level disinfectant or liquid chemical sterilant product will change the speed at which the product kills microorganisms. As table 1 shows, the chemical proportions vary between high-level disinfectants and liquid chemical sterilants
which affect the time needed to kill endospores.
The second fact is that oxidative chemistries are very reactive. They react to metals, minerals, and cellular components. Their corrosive nature can damage many materials. With all things equal, peracetic acid is more corrosive than acetic acid which is more corrosive than hydrogen peroxide. However, not all things are equal in oxidative chemistries. Different ratios between these chemicals can affect material compatibility. For example, a peracetic acid product with a high concentration of hydrogen peroxide may be more damaging than a formula with a lower level of hydrogen peroxide. Of course, increasing peracetic acid levels increases the solution’s acidity causing the peracetic acid to be less effective against microorganisms.
The composition of these three key elements defines the microbial activity and material compatibility… or does it?
Balancing microbial efficacy and compatibility is the responsibility of the inactive ingredients. “Inactive ingredients” is a bit of a misnomer. Though they may not be killing microorganisms, they do have important jobs to do. Their functions include:
• Enhancing microbial activity of the active ingredient
• Increasing compatibility with instrumentation
• Promoting formula stability and shelf life
Aside from water, the inactive ingredients are typically found in the buffers. Buffers can be powders that dissolve into the water to create a solution. They can also be concentrated solutions added to the water. The buffers are designed to work with the specific composition of the active ingredients. This means that a buffer from one product does not work with any other product. Additionally, the composition of the buffer can vary widely between products creating
different performance and compatibility profiles.
Surfactants are a chemical found in some formulations. Surfactants help the solution reach the surface of materials that would normally repel water. Often called wetting agents, surfactants help improve microbial activity by getting the active ingredient to the surface faster and more thoroughly.
pH buffer systems are composed of chemicals that can help balance the pH level to a more neutral level. Neutral solutions are gentler on materials. It also enhances the microbial activity of peracetic acid. Peracetic acid is most effective when at a more neutral pH.
Corrosive inhibiting agents are chemicals that help protect metals, especially soft metals like copper and brass, from being oxidized. Oxidization is the chemical process that causes metals to corrode or rust. Their job is to improve compatibility with instrumentation.
Some formulations have antifoaming agents. Foam can block the solution from reaching surfaces. These agents prevent or break up foam during processing.
Stabilizers are highly variable and dependent upon the formulation. Stabilizers help maintain the chemistries’ effectivity and usability. Some stabilizers slow the natural decomposition of peracetic acid. Others help the inactive ingredients stay suspended.
With the right combination of inactive ingredients, a high-level disinfectant or liquid chemical sterilant can maximize the killing efficacy of peracetic acid, increase compatibility, and improve the penetration of the active ingredients to the device surfaceseven those that naturally repel water.
Formulation is key to performance but external influences from temperature and water can also impact the product’s performance. In general, chemical reactions occur faster when the

Differences Between Peracetic Acid High-level Disinfectants and Sterilants
November/December 2024
This lesson was developed by STERIS. Lessons are administered by Endeavor Business Media.
After careful study of the lesson, complete the examination online at educationhub.hpnonline.com. You must have a passing score of 80% or higher to receive a certificate of completion.
The Certification Board for Sterile Processing and Distribution has preapproved this in-service unit for one (1) contact hour for a period of five (5) years from the date of original publication. Successful completion of the lesson and post-test must be documented by facility management and those records maintained by the individual until recertification is required. DO NOT SEND LESSON OR TEST TO CBSPD. www.cbspd.net.


Healthcare Sterile Processing Association, myhspa.org, has pre-approved this in-service for 1.0 Continuing Education Credits for a period of three years, until September 27, 2027.
For more information, direct any questions to Healthcare Purchasing News editor@hpnonline.com.
Quiz Answers:
1. C, 2. A, 3. B, 4. E, 5. C, 6. A, 7. C, 8. A, 9. B, 10. D


chemistries are heated. Oxidative chemistries follow this truth even as they kill microorganisms.
However, higher temperatures can damage temperature sensitive medical devices. Each high-level disinfectant and liquid chemical sterilant must balance the processing temperature for optimum performance against the temperature sensitive needs of the medical devices.
The opposite is also true. A processing temperature which is cooler will cause the chemistry to work slower, slowing the rate at which the microorganisms are killed. Effective high-level disinfection and liquid chemical sterilization can only be achieved when items are processed within the temperature range specified in the chemistry’s instructions for use.

Water is a key factor for chemistries with use dilutions made from concentrate. Though water supplied to healthcare facilities is safe to drink, it can contain metal ions, minerals, and dissolved organic material that can react with the active ingredients reducing their availability. This can interfere with high-level disinfection and liquid chemical sterilization.
Not all peracetic acid chemistries are the same
Each peracetic acid chemistry formulation has specific characteristics and performs differently. Ensure that the oxidative chemistry currently in use is a formulation that optimizes the effectiveness of peracetic acid, enhances penetration of the active ingredients, and helps protect instrumentation.
Processing temperature and water quality should be confirmed
Confirm that the processing temperatures meet the requirements of the peracetic acid chemistry. Manual processing may require periodically checking the solution and documenting the temperature. Temperature controls are built into automated processing systems. Ensure that the processor’s cycle parameters meet those listed in the high-level disinfectant or liquid chemical sterilant’s IFU.
Facilities should identify the water quality recommended by the oxidative chemistry manufacturer and ensure that the facility water meets these requirements.
Inspect the medical devices
Investigate discolorations, corrosion, blistering, bubbling, or other abnormalities thoroughly. These can be signs of incompatibility with the high-level disinfectant or liquid chemical sterilant.
It could also be signs of an interaction with residual chemicals used in the reprocessing cycle. Cleaning

chemistries, point of use treatment products, and disinfectant wipes are composed of several chemicals which may be incompatible with the chosen high-level disinfectant or liquid chemical sterilant. Ensuring thorough rinsing to remove residuals prior to processing. Consider switching to products that are compatible with the high-level disinfectant or liquid chemical sterilant in use.
Conclusion
Not all peracetic acid high-level disinfectants and liquid chemical sterilants are the same. Be aware of these differences and implement policies and procedures that optimize the performance of the peracetic acid chemistry in use today. HPN
References
1. U.S. Food & Drug Administration. (December 2023) FDA-Cleared Sterilants and High Level Disinfectants with General Claims for Processing Reusable Medical and Dental Devices. FDA. https://www.fda.gov/medical-devices/reprocessing-reusable-medical-devices-informationmanufacturers/fda-cleared-sterilants-and-high-level-disinfectants-general-claims-processingreusable-medical-and
2. Medicvators. (2011) High-Level Disinfectant Rapicide PA. https://www.medivators.com/sites/ default/files/minntech/documents/50096-959%20REV%20D.pdf
Arthur Henderson, RN, BA, CNOR, CRCST, CHL, GTS is a senior clinical education specialist for STERIS Corporation. Prior to STERIS, he served as the coordinator of education for the California Central Service Association, the assistant main OR manager at a large acute-care hospital, and the clinical educator for peri-operative services for another large acutecare facility. Henderson has developed and implemented an OR orientation program and an OR internship program for nonsurgical nurses and has coordinated performance improvement and staff development programs for peri-operative services.
1. What type of chemical is Peracetic Acid?
A. Fixative
B. Bonding
C. Oxidative
D. Reactive
2. Which microbiocidal chemicals are always found with peracetic acid in high-level disinfectants and sterilant?
A. Acetic Acid and Hydrogen Peroxide
B. Water and Acetic Acid
C. Acetic Acid and Hydrogen
D. Peroxide and Oxygen
3. The chemical proportions between peracetic acid, acetic acid, and hydrogen peroxide are the same for all high-level disinfectants and sterilants.
A. True
B. False
4. What does the ratio of peracetic acid, acetic acid, and hydrogen peroxide affect?
A. Operating temperature
B. Compatibility
C. Microbial kill rate
D. All of the above
E. B and C only
5. How can inactive ingredients help a high-level disinfectant or sterilant?
A. Lower the operating temperature
B. Prevent off gassing
C. Enhance microbial kill
D. Speed drying of the device
6. Why are antifoaming agents included in some high-level disinfectants and sterilants?
A. Foam can prevent surface contact of the solution
B. Foam can prevent solution circulation
C. Foam causes discoloration of devices
D. Foam does not rinse off instruments
7. How does cooler water affect the performance of the active ingredients?
A. Speeds up the degradation of active ingredients
B. Increases the concentration corrosive inhibitors
C. Slows the kill rate
D. Slows dissolution of concentrates
All CEU quizzes must be taken online at: educationhub.hpnonline.com. The cost to take the quiz is $10.
8. How do metal ions, minerals, and dissolved organic material normally found in tap water affect highlevel disinfectant and sterilant use dilution made from concentrates?
A. They react with the active ingredients
B. They enhance microbial kill
C. They protect metals from corrosion
D. They lower the operating temperature
9. Automated high-level disinfection and liquid chemical sterilization processors should meet the cycle parameters listed in which instructions for use (IFU)?
A. Equipment IFU
B. Chemistry IFU
C. Medical device IFU
D. Chemical Indicator IFU
10. What can discolorations, corrosion, and blistering seen on medical devices processed through high-level disinfection mean?
A. Devices were steam sterilized
B. Devices need further cleaning
C. Devices were not cleaned
D. Devices are incompatible with the disinfectant

BY DAVID L. TAYLOR, MSN, RN, CNOR, PRINCIPAL, RESOLUTE ADVISORY GROUP LLC
Routine sterilizer maintenance ensures safe and effective operation and plays a vital role in reducing the risk of contamination of sterile items. In my consulting experience, however, routine sterilizer maintenance often is not given proper attention.
For a steam sterilizer to heat and dry properly, regular chamber cleaning is required. Scheduled cleaning helps facilitate effective sterilizer function and maintain a uniform, consistent surface that is free of debris, mineral deposits, and discoloration.. The quality of water used to produce steam, high temperature, and pressure that make sterilization possible can cause unnecessary wear on the unit’s chamber and other components. Remaining residue after a cycle is run can cause buildup and surface contamination from detergents, wrapper chemicals, scale, rust, and foreign materials (e.g., autoclave tape) that can corrode the interior of the chamber, resulting in ineffective sterilization. It can also contribute to wet loads, costly unit repairs, premature replacement, and excessive downtime.
Sterile Processing leaders should stay current on standards, recommendations, and regulatory changes. For example, Section 12.4 of ANSI/AAMI ST79:2017/(R)2020 states that sterilizers should be inspected and cleaned daily. This underscores the need to follow the sterilizer manufacturer’s instructions for use (IFU) for routine inspection, cleaning, and documentation.
Sterilizer manufacturers may have different recommendations for routine servicing, including specific steps and recommended time intervals. Healthcare organizations are responsible for ensuring that routine maintenance occurs. If maintenance was part of the original purchase agreement or extended service contract, the SP leader must ensure the work is being performed. If routine maintenance is not part of the initial contract, the service can sometimes be added for older units as a service agreement. The manufacturer’s IFU will outline routine cleaning frequency, and the SPD’s responsibility should be added to the department’s policy, along with precise steps to follow.
When cleaning a sterilizer, it is essential to know the composition of the inner chamber. Stainless steel is most commonly used; however, some older sterilizer

chambers were comprised of cold-rolled steel clad with nickel. Knowing the material helps determine which chemicals or bead-blasting methods are most appropriate for the unit. Cleaning routines should be established in policy (some aspects might be done daily, weekly, monthly, or annually) and align with manufacturer recommendations. Most sterilizer manufacturers have a pre-cleaner, descaling solutions, and brushes for use with their systems; check with the unit manufacturer for clarification. When performing sterilizer maintenance, it’s essential that staff are properly trained and understand the manufacturers’ IFU for each sterilizer in the department. SP leaders must also ensure technicians have the appropriate personal protective equipment (PPE) and use it correctly during the process (autoclave gloves, for example, are essential for keeping employees safe when handling hot surfaces). Also vital is ensuring the correct supplies are available to prevent voiding the warranty. Some essential items required for proper sterilizer cleaning and maintenance include a special cleaner approved by the manufacturer to ensure it is safe for the unit’s surfaces. Ideally, solutions can remove scale, rust, and stains from both nickel-clad and stainless steel chamber surfaces. Water that is non-chlorinated or purified (deionized) is recommended for cleaning because impurities that can cause buildup and damage have been removed. Non-linting towels should be used to wipe external surfaces (never use abrasive clothes or brushes on metal surfaces).
Daily cleaning should involve inspecting various components of the autoclave and ensuring damaged parts are professionally repaired or replaced. Door gaskets should be checked for excessive wear or cracks, and the door must have a tight seal when closed. The gasket and mating surface should be cleaned with a mild detergent as needed. The interior chamber should be clean and debris-free, and pooled water should be wiped away before and after each cycle. Remove and inspect the chamber drain strain and clean as necessary. Further, clean the exterior surfaces, including doors, inner compartments, and controls with a manufacturer-approved cleaning solution. HPN
For the author’s weekly and annual maintenance recommendations, visit hpnonline.com/55143687



BY STEPHEN M KOVACH, BS, CFER, CLINICAL EDUCATOR EMERITUS AT HEALTHMARK, A GETINGE COMPANY
Q“We have tungsten carbide insert surgical devices, and some of them look like they are rusting on and around the tips. I thought tungsten carbide is not supposed to rust at all because it doesn’t contain iron. Can you explain?”
AFirst, without pictures I will share my thought process on what might be taking place.
Some basic facts about tungsten carbide (WC) inserts:
There are two grades of tungsten carbide: industrial grade and jewelry grade.1 It is important to know the quality of the tungsten used on your instruments. Most tungsten carbide inserts placed on surgical instruments are generally identified by gold on their ring handles (if they have ring handles).
Tungsten carbide should not rust when autoclaved because it contains no iron; although, it can still be damaged and even tarnished.2 Damage can be caused by exposure to acid solutions (oxidizers like acidic glutaraldehyde product and hydrogen peroxide [like Plasma sterilization]). A process called leaching can take place where the bond between the stainless steel and the tungsten carbide inserts break down (metal dissolution).
Some questions that should be asked to help determine whether it is rust, corrosion, or something else:
• Where is this taking place?
• On the tips only?
• Between the bond?
• What is the color of the stain?
• Do you have any pictures of the affected area?
• Other areas of the surgical instrument?
• Has it been repaired?
• By whom?
• When was the last repair done?
• Does it have a Unique Device Identification (UDI)?
• Is it just a few or many instruments?
• Have you changed cleaning solutions recently?
• What type of pretreatment process is being used?
• Are you sure it is rust or corrosion?
• What is the policy of the department on inspection concerning detection of corrosion or rust on instruments?
• Was the eraser test used?

• Did you test the area of concern with a hemoglobin test to help define the area better?3
• Did you review your instrument process and look for areas of concern?
• Did you interview your staff for input?
• Have you contacted the Original Equipment Manufacturer (OEM) for investigational help?
• Have you reread the IFU concerning care and handling and compared it to your process?
• Have you distinguished whether it is rust or something else?
Why rust or corrosion appears on devices is always a crapshoot. There are many possible villains. Finding which one is not always possible because they can gang up, and finding the ringleader, as with any group of villains, is tough.
Some of the possible villains include a) use of inappropriate solutions, b) poor instrument handling, c) cleaning chemicals, d) abrasive cleaners/tools, e) disinfectants, f) steam quality, g) poor water quality, h) improper loading of cleaning equipment, i) mixing of metals, and others.
To me, rust can come from two major areas of concern when talking in general about tungsten carbide inserts. First, from the area between the bond of the insert and the stainless steel. Second, from the stainless steel instrument itself and migrating to other areas of the instrument. (Again, without pictures, I had to take a general approach).
Answers to my questions and others you might have may help you find out the source of concern and hopefully resolve the concern if it is rust, corrosion, or something else on the tips of your tungsten carbide instruments.
Thus, tungsten carbide inserts do not rust, but if by rust you mean “corrode,” then the answer is “probably yes,” and you do need to find the villain(s) and correct them as soon as possible. HPN
References:
1. Alam, Mohammed. (2020). Does tungsten tarnish, warp, or rust? Quora. https://www.quora. com/Does-tungsten-tarnish-warp-or-rust
2. KDMFAB. (2024, June 3). Does Tungsten Rust – Truth about Rusting Properties of Tungsten Revealed. KDM Fabrication. https://kdmfab.com/does-tungsten-rust/#:~:text=Environmental%20 Conditions,and%20oxygen%20may%20facilitate%20rusting
3. Kovach, Stephen M. (2020, December 21). Erasing instrument errors. Healthcare Purchasing News. https://www.hpnonline.com/sterile-processing/article/21202330/erasing-instrumenterrors

Protect your staff and patients with Hygienically Clean reusable



















According to experts with the National Academies* reusable PPE is proven to help healthcare facilities:
■ Protect workers & patients
■ Lower operating costs
■ Improve environmental sustainability
■ Prepare for public health emergencies
Facilities that rely on reusable healthcare textiles trust Hygienically Clean Certification
■ Developed to improve quality processes and focused on outcomes
■ Requires ongoing third-party microbiological testing to verify compliance
■ Ensures the cleanliness and quality of the finished textiles
■ Relies on independent third-party auditors
Join the experts and other healthcare leaders
Request Hygienically Clean Certified laundries in your RFPs
*The National Academies of Sciences, Engineering and Medicine (NASEM) workshop, March 3–4, 2024

BY STEPHEN M KOVACH, BS, CFER, CLINICAL EDUCATOR EMERITUS AT HEALTHMARK, A GETINGE COMPANY
Four years ago as of this Healthcare Purchasing News (HPN ) December issue, I wrote the following in my first column:
“As this is my first column, I would like to thank my friend and mentor, Ray Taurasi, and HPN for allowing me to carry the torch of answering your questions. Ray wrote this column for 19 years, and I will do my best to follow in his footsteps to bring you evidence-based answers that are clinically relevant. We know that many of the processes we perform are ‘sacred cows’ that have been passed down to us and therefore, we may not have data or information to back up the practice. I will do my best to answer your questions, nevertheless.”1
After 4 years of doing this column, I am passing the torch to my colleague, Adam Okada (one of my fellow educators at Healthmark). My reason: I have decided to retire, and Adam has the passion that is needed to write a monthly column on issues you, the reader, are facing each day.
In 1975, I started as a sterilization orderly and had no idea I would have ended up being an educator at Healthmark, A Getinge company (previously Healthmark Industries) 49 years later.
Many have asked me over the years, “Where has your passion and enthusiasm come from,” along with, “You seem to connect with your audience when speaking. You are successful in what you do. Why or how is that?” It came from many different influencers in my life.
First, my family (parents Stephen and Irene, sister Mary Ellen, and brother David Allan) made sure I understood that each of us can make a difference. Sometimes we do not understand we can make a difference because we might not see the outcome of our impact on others.
My parents taught me to be true to myself, believe in myself and my abilities, and give back when I can. I also was taught if you do not know something, ask; do not be afraid to ask questions because many others have the same questions. How else are you going to learn? Nobody knows everything. Then you take what you learn and find a way to share it with others. Very simple. That is why I modified “Knowledge is power” to say, “The real power is when you share your knowledge with others.”
Next, as a speaker, I was taught to make sure I respected the audience: to express what I knew and what I didn’t know, say what I believe, and label them accordingly

Girls with grandpa
without obscuring the lines where knowledge stops and my opinion begins. If asked a question that I did not know the answer to, I should admit it and let them know I will do my best to find the answer and get back.
My career has been blessed with having different mentors–each one teaching me something different. Here are some of them by name: Dr. Donald Magalligan, Tim McElmurry, Marian Kirby, Ethel Durr, Mike Haas, Mrs. Fran Koch, Myrna Tuya, Al Spath, Livia Senties Zuniga, John Nies, Sue Klacik, Jonathan Wilder, Bryant Broder, Mary Ellen-Fortenberry, Ray Taurasi, Don Gordon, Martha Young, Janet Prust, Richard Schule, Cheron Rojo, Brad Catalone, Diane Gosser, Fred Alston, Karen Dulka, Rose Seavy, Scott Pass, David Jargrosse, Steve Adams, Elizabeth Berrios, Jake Mandal, Les Kowalski, Bill Nelson, Tony Thurmond, Betty Hannah, Frank Caravello, Mary Ann Drosnock, Martin Pfeifer, John Whelan, Jan Huys, Outi Lindholm-Ollikainen, Edward Andrews, Penny Sabrosky, Tom Van Gardingen, Karen Owens, Brian Trimmer, Dave Mutschler, Darby Booth, Kristen Cousino, Amanda Dupure, Tony Monaco, Nancy Chobin, Ann Cofiel, Kristine
Russell, Seth Hendee, Harry Oussoren, Nuper Jain, Steven Turtil, Jahan Azizi, Matt Smith, Kevin Anderson, Malinda Elammari, Rod Parker, Michael Cobb, Suzanne LattaAbbott, Verda Watson, Maura Basile, Natalie Whitfield, Paula Trozak, Delores Basile, Kelly Pyrek, Barb and Ed Kanegsberg, Ron Hunsucker, Bob LeSage, Alex Kirk, Karen MacDonald, Kaumudi Kulkarni, Chris Turner, Mike Kirk, Jon Fish, Hank Balch, Rick Barlow, Dr. M. Alfa, Matt Ippel, Damien Berg, Cori Ofstead, Joe Lewelling, Amanda Bennett, Donna Swenson, Denise Coatsworth, Jill Holdsworth, Jill Berends, Bobbie Smigelski, Tracy Humphries, Michelle Julio, Mike Gregory, Frank Daniles, Rebbeca Washburn, Dan Miller, Shelley Hagen, Mary Velasco, Terry Roach, Tom Hillebrand, Tom Hirzel, Cindy Mette, Ryn DiStefano, Gail Perhogan, Dan Bialt, Penny Jarman, Rebecca LaHue, John MacDougall, Deannard Esnard, Betsy Vane, Abby Markielewicz, Nate Cote, Heather Bubeck, Bryan White, Tom Schriefer, Sam Deltro, Pat Curtis, Cathy Rubin, Jakie Daley, Andy Mikos, MSHCSP membership, my staff at Botsford Hospital, and my first staff at Henry Ford Hospital (HFH) OR Reprocessing in the 1980s. Each name has a story behind them, and many of the people might not even know how they helped me, but they did.
The Basile family (Suzanne, Ralph, Mark, and Steven) allowed me the opportunity to learn and work with them and represent their company for the last 24 years. I am still humbled and honored for the trust they put in me.
Each one of the people mentioned (along with many others over these 49 years) put faith in me to do something and accomplish different tasks by working hard (with passion and purpose) and learning from those tasks to become better. They also reinforced in me that what you say and do defines who you are. Do your best each time you do something. You never know who is watching you.
We all need support outside of work. I have been blessed with family and friends who have always been there for me, regardless of what it was.
My friends: To my college buddies, Ray, Gary, Bill, Chet, and Andy, for over 50 years supporting me personally and professionally; thank you guys! My neighbors in the Aviation subdivision, the St. Alphonsus, and the University of Detroit Jesuit High School and Academy (UDJHSA) communities, and the Gyurscik family—never would have made it without them.
I want to thank everyone who works at Healthmark for always thinking of the customer first and putting out a great

















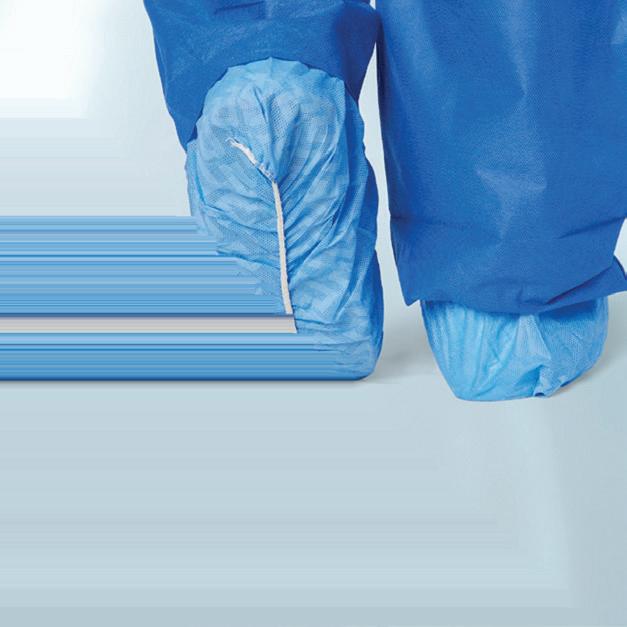
quality product. It made it easy to talk about our products knowing I had great team members behind me all the time.
My family, who have endured the many weekends away from home and long hours, allowed me to hone my craft at each step of my career. First Anne, who taught me what the meaning of “the patience of Job” is about, and when you put your faith in God, you have nothing to worry about. My two boys, Nicholas and Peter (the many hours watching me practice using a slide projector in the basement going over presentations those early years), when they could be doing other stuff. Maryjo, who has made me a better person all around and reminds me of the importance of family. At this time, my two beautiful granddaughters, Julianne and Olivia Rose, each day remind me why we do it right for each patient because that next patient could be a family member (no shortcuts). Remember, “Quality doesn’t cost, it pays!”2
My extended families of cousins and in-laws (Birosak, Badali, Lafata, Kovach, Ramkers), your support over the years helped me in so many ways. Thank you.
I always understood I could never do it alone. I did not know everything. No matter what the task was, I had
friends and family I could always turn to for help. Many times, I might not like their response, but they were always open and honest with me, and I thank everyone for that. My success reflects everyone’s input. Success is not easy. I did not seek it out; it just happened over time.
My goal has always been that if I could help even one person make an improvement, then I would have done my job. Thus, I hope over these last 4 years my columns have helped you understand your work better with sound advice and made a difference (and over my 49 years in the healthcare industry). Thank you for the opportunity, HPN. Adam, you will do an excellent job of providing sound advice for our profession.
I close with modifying my “Keep it Clean” to “Keep it Clean and Functional,” because just being clean is not enough! See, even an old dog can learn over time! HPN
References:
1. Kovach, Stephen M. (2020, December 21). Erasing instrument errors. Healthcare Purchasing News . https://www.hpnonline.com/sterile-processing/article/21202330/erasing-instrumenterrors
2. QUALITY DOESN’T COST, IT PAYS. (2013, July 1). Healthmark Digest, Issue No. 215. ht-tps:// www.hmark.com/news/quality-doesnt-cost-it-pays-issue-no-215/






HPN’s podcast features interviews with special guests and article reads on our many verticals including supply chain, sterile processing, surgical and critical care, infection prevention, and more.

Scan the QR code so you don’t miss an episode!


BY KAREN CONWAY, CEO, VALUEWORKS
A2017 article in Healthcare Purchasing News explored opportunities for health system pharmacy and traditional medical-surgical supply chain leaders to learn from one another. But despite the article citing some compelling real-world examples of where it is working, hospital pharmacy and supply chain collaboration remains the exception versus the norm seven years later.
In this column, we will revisit some of those opportunities, especially in light of broader macro trends, such as the move to non-acute care and ongoing supply and drug shortages.
Over the past two decades, the traditional medical-surgical supply chain has made notable progress toward less costly touchless orders through the use of ANSI transaction standards to automate purchase orders, confirmations, and invoices. On the pharmacy side, due to an historic reliance on group purchasing organizations (GPOs) and wholesalers for procurement, fewer pharmaceutical manufacturers compared to their device peers are able to receive electronic purchase orders (850s) or send electronic confirmations (855s) and invoices (810s). Supply chain leaders can help their pharmacy counterparts with their transition to more efficient procure-to-pay processes and the associated analytics made possible through greater integration with enterprise resource planning (ERP) systems.
Pharmacy can also benefit from supply chain’s expertise in contract and price negotiations, especially as pharmaceuticals account for an increasingly larger percentage of total hospital expenses.
Pharmacists, meanwhile, have years of experience managing the complexity of multiple classes of trade, which impact the price paid for pharmaceuticals and ultimately the cost incurred by patients. This consumer-driven approach could help inform those managing the medical-surgical supply chain as they consider the implications of the move to care settings outside of the hospital and the application of various value-based payment methodologies.

Pharmacy also has more experience using a standard identifier (the NDC, or national drug code) as the common code for prescribing, dispensing, reimbursement, and clinical decision support for pharmaceutical. The NDC was also the basis for the 2004 US FDA pharmaceutical barcode rule, which has increased barcode scanning of medicines at the point of care. This experience could help support the efforts to increase utilization of the unique device identifier (UDI) at the point of use for medical devices. Capturing data on both the drugs and devices used in patient care can support efforts to understand the total cost of patient care and continue to generate evidence on the best therapies for different patient populations.
The need to increase supply chain resiliency in the face of ongoing shortages provides an opportunity for more pharmacy and supply chain collaboration. Earlier this year, the University of Utah Drug Information Services reported the highest number of drug shortages in 20 years, while the Health Industry Distributors Association says that more than 90 percent of health systems continue to experience product shortages. Both pharmacy and supply chain leaders are tackling the problem in similar ways: holding higher inventory levels when possible, identifying alternative products and therapies, and deploying conservation practices. The interdependencies between devices and drugs often go overlooked. For example, an infusion system may be available but not the right medication formulation or vice versa. With broader visibility to shortages, pharmacy and supply chain leaders can better identify potential shortages across their respective areas of control that could impact their collective ability to deliver affordable quality care.
These are just a few ideas to promote more pharmacy and supply chain collaboration. With advances in cell and gene therapy (and associated cold chain requirements) and more care being delivered outside of the acute care setting, logistical challenges will only increase. Now is the time for pharmacy and supply chain to explore together how best to coordinate not only the delivery of products but also the trained personnel needed to deliver care across an expanding care footprint.HPN







Provides reliable stabilization of endotracheal tubes (sizes 7.010.0mm) following intubation.
The low profile design and cushioned neckband are soft and comfortable on the face and neck.
It can be used in supine or prone position.
Slide allows easy repositioning of ET tube placement.
Allows easy access for oral care.
Prevents kinking or flattening of tube.
Minimizes unintentional ET tube movement and helps prevent accidental extubation.