Public Health
Chronic Diseases in 2024:
Diagnosis, Treatment, Prevention
www.delamed.org | www.delawarepha.org Volume 10 | Issue 1 March 2024
A publication of the Delaware Academy of Medicine / Delaware Public Health Association
Delaware Journal of
Delaware Academy of Medicine OFFICERS
Lynn Jones, L.F.A.C.H.E. President
Stephen C. Eppes, M.D. President Elect
Ann Painter, M.S.N., R.N. Secretary
Jeffrey M. Cole, D.D.S., M.B.A. Treasurer
S. John Swanson, M.D.
Immediate Past President
Katherine Smith, M.D., M.P.H. Executive Director
DIRECTORS
David M. Bercaw, M.D.
Saundra DeLauder, Ph.D.
Eric T. Johnson, M.D.
Erin M. Kavanaugh, M.D.
Joseph Kelly, D.D.S.
Omar A. Khan, M.D., M.H.S.
Brian W. Little, M.D., Ph.D.
Daniel J. Meara, M.D., D.M.D.
John P. Piper, D.O.
Megan L. Werner, M.D., M.P.H.
Charmaine Wright, M.D., M.S.H.P.
EMERITUS
Barry S. Kayne, D.D.S.
Joseph F. Kestner, Jr., M.D.
Delaware Public Health Association
ADVISORY COUNCIL
Omar Khan, M.D., M.H.S. Chair
Katherine Smith, M.D., M.P.H. Executive Director
COUNCIL MEMBERS
Alfred Bacon, III, M.D.
Louis E. Bartoshesky, M.D., M.P.H.
Gerard Gallucci, M.D., M.S.H.
Allison Karpyn, Ph.D.
Erin K. Knight, Ph.D., M.P.H.
Laura Lessard, Ph.D., M.P.H.
Melissa K. Melby, Ph.D.
Mia A. Papas, Ph.D.
Karyl T. Rattay, M.D., M.S.
William Swiatek, MA, A.I.C.P.
Delaware Journal of Public Health
Katherine Smith, M.D., M.P.H. Publisher
Omar Khan, M.D., M.H.S. Editor-in-Chief
Laura Lessard, Ph.D., M.P.H.
Angela Herman, D.N.P., R.N. Guest Editors
Suzanne Fields Image Director
ISSN 2639-6378

Public Health
3 | In This Issue
Omar A. Khan, M.D., M.H.S.; Katherine Smith, M.D., M.P.H.
4 | Guest Editors:
Training the Next Generation of Public Health Leaders to Tackle Chronic Disease in Delaware: Examples and Opportunities
Laura Lessard, Ph.D., M.P.H.; Angela Herman, D.N.P., R.N.
8 | Chronic Disease Risk of Family Child Care Professionals: Results of a Statewide Survey of Health and Wellbeing Indicators
Laura Lessard, Ph.D., M.P.H.; Rena Hallam, Ph.D.
12 | A Comprehensive Analysis of the Impact of the COVID-19 Pandemic on Lung Cancer in Delaware
Brian Nam, M.D., F.A.C.S.; Yeonjoo Yi, Ph.D.; Kevin Ndura, M.B.A.; Krishna Vasireddy, Pharm.D., M.S.; Claudine Jurkovitz, M.D., M.P.H.; Kiran Kattepogu, M.B.B.S., M.P.H.
26 | Social Workers, Burnout, and Self-Care: A Public Health Issue
Michelle Ratcliff, D.M.F.T., L.S.W.
30 | Community Partnership to Co-Develop an Intervention to Promote Equitable Uptake of the COVID-19 Vaccine Among Pediatric Populations
Paul T. Enlow, Ph.D.; Courtney Thomas, M.S.; Angel Munoz Osorio, B.S.; Marshala Lee, MD, M.P.H.; Jonathan M. Miller, M.D.; Lavisha Pelaez, M.P.H.; Anne E. Kazak, Ph.D., A.B.P.P.; Thao-Ly T. Phan, M.D., M.P.H.
44 | Pediatric Dentists: Frontline Public Health Providers Leading the Way in Identifying and Preventing Childhood Obstructive Sleep Apnea Syndrome
Bari Levine, D.M.D., M.P.H.; Freda Patterson, Ph.D.; Lauren Covington, Ph.D., R.N
46 | “We Are All There to Make Sure the Baby Comes Out Healthy”: A Qualitative Study of Doulas’ and Licensed Providers’ Views on Doula Care
Erin K. Knight, Ph.D., M.P.H.; Rebecca Rich, Ph.D., C.H.E.S.
62 | Global Health Matters Newsletter
January - February 2024
Fogarty International Center
74 | Paving the Way to Active Living for People with Disabilities: Evaluating Park and Playground Accessibility and Usability in Delaware
Cora J. Firkin; Lauren Rechner; Iva Obrusnikova, Ph.D., M.Sc.
86 | How Interprofessional Community Mobile Healthcare and Service-Learning Work Together to Identify and Address Chronic Health Disparities
EmmaMathias;PeytonFree;AbbyStorm,M.S.;
HeatherMilea,M.S.N.,F.N.P.-B.C.,A.G.A.C.N.P.-B.C.;ChristineSowinskiM.S.M.;
JenniferA.Horney,Ph.D.
90|A6-WeekVirtualExercise/DanceProgramImpacts Fitness Levels for Adults with Intellectual Disabilities: A DNP Project
Melanie Ayers, D.N.P., R.N., C.N.E.
98 | Navigating Risk: Understanding Chronic Disease Factors in Delaware’s College Population
AmyGootee-Ash,Ph.D.,M.S.W.,M.S.;MeganRothermel,Ed.D.,M.S.; AdamKuperavage,Ph.D.
102| ImplementingaSuccessfulInfluenzaandUpdated COVID-19 Vaccination Campaign Among Healthcare Workers in a Delaware Healthcare Facility
Lija Gireesh, D.N.P., M.B.A., F.N.P.-B.C., N.E.A.-B.C., C.O.H.N.-S.; Tabe Mase, F.N.P.-B.C., M.J., C.H.C., C.O.H.N.-S.; Marci Drees, M.D., M.S., D.T.M.H., F.A.C.P., F.I.D.S.A., F.S.H.E.A.
106 | Mapping Health Disparities: Leveraging Area-Based Deprivation Indices for Targeted Chronic Disease Intervention
Darrell Dow, M.S.
112 | Review of Pediatric Tracheostomy Training Program for Home Discharge Patients
Katlyn L. Burr, M.S.M., R.R.T.-N.P.S., A.E.-C.; Erin Nilson-Italia, R.R.T.-N.P.S.; Michael Treut, R.R.T.-N.P.S., A.E.-C.; Kimberly McMahon, M.D.; Kelly Massa, B.H.S., R.R.T.N.P.S.
116 | Lieutenant Governor’s Challenge: Motivating and Honoring Delawareans to Improve Their Health and Well-Being
Helen Arthur, M.H.A.; Lauren Butscher, C.H.E.S.; Lisa Moore, M.P.A.; Keith Warren
122 | Advancing Healthy Lifestyles: A Multicomponent Initiative to Reduce the Burden of Obesity In Delaware
Helen Arthur, M.H.A.; Lauren Butscher, C.H.E.S.; Lisa Moore, M.P.A.
130 | The Impact of Diabetes in Delaware 2023
Delaware Department of Health and Social Services Division of Public Health
152 | Lexicon & Resources
156 | Index of Advertisers
158 | Delaware Journal of Public Health Submission Guidelines
The Delaware Journal of Public Health (DJPH), first published in 2015, is the official journal of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA).
Submissions: Contributions of original unpublished research, social science analysis, scholarly essays, critical commentaries, departments, and letters to the editor are welcome.
Questions? Contact managingeditor@djph.org
Advertising: Please contact ksmith@delamed.org for other advertising opportunities. Ask about special exhibit packages and sponsorships. Acceptance of advertising by the Journal does not imply endorsement of products.
Copyright © 2023 by the Delaware Academy of Medicine / Delaware Public Health Association. Opinions expressed by authors of articles summarized, quoted, or published in full in this journal represent only the opinions of the authors and do not necessarily reflect the official policy of the Delaware Public Health Association or the institution with which the author(s) is (are) affiliated, unless so specified.
Any report, article, or paper prepared by employees of the U.S. government as part of their official duties is, under Copyright Act, a “work of United States Government” for which copyright protection under Title 17 of the U.S. Code is not available. However, the journal format is copyrighted and pages June not be photocopied, except in limited quantities, or posted online, without permission of the Academy/DPHA.Copying done for other than personal or internal reference use-such as copying for general distribution, for advertising or promotional purposes, for creating new collective works, or for resale- without the expressed permission of the Academy/DPHA is prohibited. Requests for special permission should be sent to managingeditor@djph.org

Delaware Journal of
publication of the Delaware Academy of Medicine
Association March 2024 Volume 10 | Issue 1
A
/ Delaware Public Health

Chronic Disease
According to the Centers for Disease Control and Prevention, six in ten Americans live with at least one chronic disease.1 Many live with more than one. These diseases (heart disease, stroke, cancer, diabetes, obesity, arthritis, Alzheimer’s disease, epilepsy, etc.) have significant health and economic costs, and interventions to prevent, treat, and manage these diseases can make up a large portion of our national and local health care expenditures.
These chronic diseases affect the lives of Delawareans in many ways, and also offer the potential for improvement. Often, improving one area (such as diabetes) requires a comprehensive approach uniting medicine and public health. This approach can thus positively impact many other areas of chronic diseases as well.
Prevention. Preventing these diseases is the best way to keep health care costs down. Some of the best ways to prevent chronic disease are to quit smoking; eat a healthy diet rich in fruits, vegetables, whole grains, lean protein, and low-fat dairy; get regular physical activity; limit alcohol; keep up to date on preventative screenings; take care of your teeth; and get enough sleep.2
Treatment & Management. According to Delaware’s Division of Public Health, cardiovascular disease (including heart disease and stroke) is the leading cause of death in the First State, followed by cancer, lung disease, and diabetes – all diseases of a chronic nature.3 This is the DJPH’s third issue devoted to chronic disease; the first two issues were published back-to-back in 2017, and looked at statewide initiatives working in the prevention, treatment, and management spheres.
In this issue, we welcome Dr. Laura Lessard and Dr. Angela Herman, researchers and educators from the University of Delaware and Wilmington University, respectively, and experts in the field of chronic disease. The articles within take a look at how COVID-19 fits into the chronic disease world, at how some of our frontline providers are working to prevent chronic disease in special populations, and at some of the programs offered for those groups of people living with chronic disease in the state.
As always, we welcome your feedback! We also take the opportunity to remind you to register for our Annual Dinner Meeting on May 1, 2024. This is a very special annual event and we cover many of the costs involved to make it accessible to the maximum number of attendees. Details are available on our website, at https://delamed.org
REFERENCES
1. Centers for Disease Control and Prevention. (2023, May). National center for chronic disease prevention and health promotion.
2. Centers for Disease Control and Prevention. (2023, Oct). How you can prevent chronic diseases. https://www.cdc.gov/chronicdisease/about/prevent/index.htm
3. Delaware Division of Public Health. (n.d.). Bureau of Chronic Disease Prevention. https://dhss.delaware.gov/dph/dpc/bcd.html
 Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
 Katherine Smith, M.D., M.P.H. Publisher, Delaware Journal of Public Health
Katherine Smith, M.D., M.P.H. Publisher, Delaware Journal of Public Health
Doi: 10.32481/djph.2024.03.01
IN THIS ISSUE
3
Training the Next Generation of Public Health Leaders to Tackle Chronic Disease in Delaware: Examples and Opportunities
Laura Lessard, Ph.D., M.P.H.
Department of Health Behavior and Nutrition Sciences, University of Delaware
Angela Herman, D.N.P., R.N. College of Health Professions and Natural Sciences, Wilmington University
INTRODUCTION
Chronic diseases are the number one cause of death in Delaware and across the United States, accounting for four of the five top leading causes of death each year.1 In a previous issue of the Delaware Journal of Public Health (December 2022), data on the geographic distribution of chronic illness in the state was presented, illustrating patterns of disease and their relationship to demographic patterns. Of note, the authors posit that, “an aging population [in Delaware] is more likely to develop chronic disease as a natural result of the aging process.”2 Indeed, medical treatment advancements have extended the lifespan and quality of life for many living with chronic diseases, resulting in an increased need for disease management and support. The realm of chronic diseases and public health is continually broadening, incorporating innovative approaches for both preventing and managing these conditions. As educators helping to train and support the next generation of public health professionals, we recognize that preparing our students to meet this reality takes a multi-level approach. In this paper, we present examples from our institutions of the ways that chronic disease is taught in our curricula with the hopes of both shining this light on this work but also identifying opportunities for collaboration, expansion and growth.
CHRONIC DISEASE EPIDEMIOLOGY
At a fundamental level, it is imperative that public health professionals understand the epidemiology of chronic disease, including its distribution and determinants. This can take the form of learning about sources of epidemiological data, ways to collect valid and reliable data and identifying trends in data over time.
At Wilmington University, Epidemiology for the Health Professions is a course shared by graduate students in both Nursing and Health Science majors to promote interdisciplinary communications and teamwork. Students are introduced to the principles and methods of epidemiologic investigation, data and the use of classical statistical approaches to describe the health of populations. A final project presentation provides the opportunity for them to do a thorough discussion of a specific chronic health condition from an epidemiologic focus - including the natural history of the disease, pathophysiology and transmission as
well as screening recommendations and current policy issues related to the condition. WilmU’s Doctor of Nursing Practice (DNP) program also includes a course in Epidemiology which provides an advanced evaluation and analysis of the principles of epidemiology. Students become familiar with epidemiologic approaches to causation and the use of analytic epidemiology. Assignments provide students with methods to discern measures of disease burden in the community.
At the University of Delaware (UD), our introductory epidemiology course taught to undergraduate students teaches students about the prevalence, incidence and risk factors for chronic disease like diabetes and heart disease. Course assignments frequently use chronic disease examples, showing students how data sources such as the Behavioral Risk Factor Surveillance System (BRFSS) and National Notifiable Diseases Registry can be used to understand both the current status and trends over time in chronic disease diagnoses in Delaware and how those compare to other jurisdictions. In the graduate Epidemiology of Aging course, part of the MPH curriculum at UD, students conduct research culminating in a presentation of aging, demographics, epidemiology of aging-related disorders and current issues related to aging for a particular jurisdiction of choice (country or state). Class discussion examines the similarities and differences across jurisdictions.
CHRONIC DISEASE PREVENTION AND TREATMENT
As the incidence of chronic disease increases, the population of individuals who could benefit from primary, secondary and tertiary prevention as well as treatment also expands. Students need to understand both the mechanisms and opportunities for prevention along with the current state of treatment for chronic diseases. These topics are integrated in a variety of learning experiences appropriate for student level and program.
At UD, for example, the Graduate Certificate in Health Coaching provides training to become a Nationally Board Certified Health and Wellness Coach (NBC-HWC). The curriculum teaches students the skills needed to support clients with their individualized health goals, including those to reduce chronic disease risk such as increasing physical activity, reducing stress and improving diet. Students in the program learn both the theory and practice of health behavior change and have ample practice coaching clients during their training.
Doi: 10.32481/djph.2024.03.02
4 Delaware Journal of Public Health - March 2024
At Wilmington University, Bachelor Degree students in the Health Sciences program students are prompted to consider all areas of disease and prevention through the lens of patient education, healthcare leadership, healthcare policy, evidence, public health, as well as law and ethics. The concepts of chronic care are infused through the resources and assignments as the students consider its context within their programs. In the RN to BSN program, core classes provide a thorough practice-focused learning opportunity intended to provide nurses with a deep understanding of the skills required to integrate chronic care into their nursing practices. In the Chronic and Palliative Care course nurses complete a practice-focused learning opportunity to explore the skills required to integrate chronic care into practice. Health Sciences and BSN students at Wilmington University also may incorporate a certificate in Interdisciplinary Care Management into their program. This comprehensive certification informs students about the need for care management services across all healthcare levels as the connection for patients with chronic illness to successfully navigate transitions of care using a team-based patient-centered approach. Students are provided an in-depth evaluation of the principles and strategies of care management across the healthcare continuum. The curriculum delves into a thorough analysis of value-based financial issues, healthcare quality metrics, and their impact on the provision of care for patients. Students develop skills to leverage innovative technology to optimize workflow efficiency, and foster self-care engagement strategies for patients.
SOCIAL DETERMINANTS AND THEIR IMPACT ON CHRONIC DISEASE
While health behavior and genetic factors influence chronic disease risk, we know that social determinants of health are also powerful drivers of disease incidence. These determinants include conditions in which people are born, grow, live, work and age and are known to relate to chronic disease risk.3 Exposing students to the breadth of determinants and their potential impact on health is necessary across the curriculum.
At the University of Delaware, the Social and Environmental Determinants of Health course offered to graduate students in public health and health promotion explores income, living conditions, education and other factors that impact health and longevity. Through readings and case studies, students learn more about factors and drivers of population health.
Wilmington University’s new MS in Health Sciences includes concentrations in both Public Health and Environmental Health. Both include the Foundations of Community and Health Education course that provides a focus on trends in community health disparities and health promotion strategies and education principles to combat adverse events. Within the Population Health concentration students further delve into the issues of determinants of health and their underlying causes. Interprofessional management of complex issues in population health is emphasized within the context of healthcare policy, value-based care, and the use of data analytics. Health Science students further collaborate with the MS in Environmental Science program in a course in Human Health and the Environment. Chronic illness as it relates to and is impacted by environmental factors is examined. The MSN program includes a
Public Health concentration. Within the DNP program students also gain valuable knowledge from a Population Health course. This course incorporates experiential engagement time at a site focusing on a vulnerable population. Students collaborate with healthcare peers to develop a community based action research project to improve health outcomes and utilize a logic model to evaluate the effectiveness of the program.
POLICY INFLUENCES ON LIVING WITH CHRONIC ILLNESS
Living with and often dying from chronic disease are complex and emotional experiences. Since many of our students aim to work with patients and in the community after graduation, it is important to expose them to these realities across the curriculum. In addition, policies at the local-, state- and federal-level often influence how these diseases are identified (via screening), treated and managed, with health insurance policy and access to longterm care and support at the top of the list.
At UD, the Chronic Illness in America course is a perfect example of how students can explore these topics. This innovative course was developed in collaboration with Lori’s Hands, a local nonprofit organization that pairs students with individuals in the community that are living with chronic illness. Student volunteers provide companionship and non-medical support for their clients in the home setting, affording students the chance to see firsthand the experience of their clients and their families. The course provides a wrap-around experience for students, teaching them about topics that their clients face including identity, social determinants, the health care system and the complexity of aging. This scaffolded educational experience allows students to grapple with the intersection of the evidence around chronic illness with the day-to-day realities. The service-learning component of the course, volunteering with Lori’s Hands, along with reflection opportunities maximizes the translation of the information into future practice.
At Wilmington University, All BSN students as well as Health Sciences may choose to focus their core coursework with certificates or electives that can enhance their learning in chronic disease management. The Holistic Palliative and End-of Life Care certificate offers extensive preparation for students to deal with patients facing serious illness or death. This 5 course certificate provides 5 core classes: Topics in Palliative and End of Life Care, The Process of Dying, and Families and Crisis. Through these courses, students are led to explore concepts impacting chronically ill patients such as psychosocial adjustment, social isolation, self-management and advocacy, and quality of life. Additionally, students can choose 3 other courses in a variety of applicable topics such as health psychology or healthcare policy. All Health Sciences are required to take an interdisciplinary course in Health Policy shared with their fellow students within the Law, Policy & Political Science program.
DISCUSSION
Through these examples, we’ve shown just some of the ways that chronic disease can be embedded within the curriculum and these are just a subset of the educational opportunities that exist across the state. Even with these examples, we see several themes that rise to the top. Firstly, interprofessional education is
5
essential to exploration of chronic disease. Across our programs, we see several examples of where students from different fields come together and leverage their expertise to tackle challenges of chronic disease. This collaboration allows students to think outside of their typical training about the challenges and opportunities of diagnosing, treating and living with chronic disease. This in turn prepares them for a workforce that is equally diverse. Patient-centered care provides a focus for students to view these challenges and plan healthcare provisions to meet individual needs and goals of those with chronic illness.
Secondly, our programs value real world applications and community engagement. Across both institutions, students are afforded opportunities to learn from and with communities about the realities of chronic disease. We have found that students thrive when they are challenged to apply what they learn from lectures and readings to the real world experience of patients and communities. This helps them both understand chronic disease better but also to ask more questions about why and how we screen for, care for and support individuals with chronic disease. Lastly, our programs are committed to teaching cutting edge modern and advancements, whether in the realm of epidemiologic methods, treatments or approaches to chronic disease management. The acknowledgment for the increasing use and application of data analytics and digital health technology is evident in many areas of the curricula. This leadership is facilitated by our engagement with research on chronic disease, which spans our institutions and includes others across the state and country.
Delaware
Public Health
CONCLUSION
We present examples of public health training across our institutions that are not designed to be comprehensive, indeed there are other courses and training opportunities across the state in these areas. We encourage our colleagues to share ideas and best practices in these areas moving forward and potentially identify opportunities for cross-program and cross-institutional training on topics of mutual interest.
Dr. Lessard (llessard@udel.edu) and Dr. Herman (angela.j.herman@wilmu.edu) may be contacted at their respective e-mail addresses.
REFERENCES
1. Delaware Department of Health and Social Services, Division of Public Health. (Nov 2019). Chronic Disease in Delaware: Facts and Figures, 2019.
2. Gibbs, T., & Sabine, N. (2022, December 31). Chronic disease management and the healthcare workforce. Delaware Journal of Public Health, 8(5), 176–196.
https://doi.org/10.32481/djph.2022.12.043
3. Hill-Briggs, F., Adler, N. E., Berkowitz, S. A., Chin, M. H., Gary-Webb, T. L., Navas-Acien, A., . . . Haire-Joshu, D. (2020, November 2). Social determinants of health and diabetes: A scientific review. Diabetes Care, 44(1), 258–279.
https://doi.org/10.2337/dci20-0053
Each year, the Delaware Journal of Public Health publishes five different theme issues. Article submissions are accepted on a rolling basis, and the editorial board considers all submissions, both those connected directly to a theme issue, and non-thematic submissions. The editorial board reserves the right to include non-thematic submissions in each issue.
The working publishing calendar and thematic issues for 2024 are as follows:
If you have questions about submissions, ideas for an article, or suggestions for a future theme issue, please email Kate Smith: ksmith@delamed.org
All submissions can be submitted via the online submission portal: https://www.surveymonkey.com/r/2DSQN98 Submissions guidelines can be found at: https://djph.org
Journal of Upcoming Issues Issue Submission Publication Chronic Disease February 2024 March 2024 Violence April 2024 May 2024 Cancer & the Power of Preventive Screening June 2024 July 2024 Childhood Development & Education August 2024 September 2024 After COVID - Rebuilding Public Health & Healthcare Resilience October 2024 November 2024 6 Delaware Journal of Public Health - March 2024


February - March 2024
The Nation’s Health headlines
Online-only news from The Nation’s Health newspaper
Stories of note include:
Public health girding for funding challenges in 2024
Kim Krisberg
Health care access a struggle for undocumented immigrant children
Teddi Nicolaus
Q&A with Renee Salas: Lancet Countdown brief urges US action on climate change
Minoli Ediriweera
Healthy People 2030 champions advance US health objectives
Michele Late
Report: America falling behind in global science, technology
Kim Krisberg
States using Medicaid funds for firearm violence prevention
Mark Barna
Team sports can be a home run for your child’s health
Teddi Nicolaus
Many other articles available when you purchase access
Entire Issue $12
Visit https://www.thenationshealth.org/user
HIGHLIGHTS FROM The NATION’S HEALTH A PUBLICATION OF THE AMERICAN PUBLIC HEALTH ASSOCIATION 7
Laura Lessard, Ph.D., M.P.H.
Chronic Disease Risk of Family Child Care Professionals: Results of a Statewide Survey of Health and Wellbeing Indicators
Department of Health Behavior and Nutrition, Delaware Institute for Excellence in Early Childhood, University of Delaware
Rena Hallam, Ph.D.
Delaware Institute for Excellence in Early Childhood, Department of Human Development and Family Sciences, University of Delaware
ABSTRACT
Objective: To document the chronic disease risk factors and prevalence rate of family child care professionals. Given that a significant number of young children spend time in family child care (FCC) settings, these environments are an important focus for efforts to improve children’s health. Methods: Data were collected in fall 2021 from a statewide survey of licensed FCC professionals in one mid-Atlantic state (N=541), using validated questionnaires to assess health status, including chronic diseases like high blood pressure, diabetes, and asthma, as well as nutrition and physical activity. Results: While a majority of respondents reported good overall health and adherence to healthy behaviors like drinking water, eating fruits and vegetables, and engaging in physical activity, a substantial proportion were overweight or have obesity (86.1%), and there were notable rates of high blood pressure (41.1%) and asthma (17.9%). The study found higher diabetes rates among FCC professionals compared to national averages for early childhood education workers, possibly reflecting demographic differences. Conclusions: The results highlight both areas needing support, such as managing chronic disease risks, and areas where FCC professionals excel, like maintaining healthy lifestyle habits. Policy Implications: There is a need for targeted support for FCC professionals to manage and prevent chronic diseases, thereby ensuring their wellbeing and enabling them to continue being positive health role models for the children in their care.
INTRODUCTION
Given that 60% of young children (ages 0-5) have at least one weekly nonparental care arrangement,1 these environments are important determinants of the health and wellbeing of children and families. While most of the child care literature is focused on center-based programs, home-based or family child care (FCC) programs are an important environment to consider. In family child care programs, a small number of mixed aged children (typically <10) are cared for in a home setting, generally with one or two adults. FCC programs are a popular choice for infants and toddlers,1 children from non-English speaking households, and those in rural areas.2
Understanding the chronic disease risk of FCC professionals is important for several reasons. A healthy professional ensures the safety and wellbeing of the children in their care, maintains consistency and reliability in caregiving, and contributes to the children’s emotional security. The emotional and mental health of the provider influences their interactions with children, impacting the quality of care. Research shows that child care providers who were more positive showed more optimism, provided higher quality of care and expressed less negative regard and more positive remarks towards the children.3
In addition, FCC professionals serve as role models for the children in their care. Research suggests that when staff do not engage in outdoor play, children engage in significantly less physical activity,4 and child care provider practices around
mealtime are associated with child dietary intake.5 It is important to identify opportunities to leverage educators’ positive health behaviors and address barriers to improving other health behaviors. Despite the importance of the health of this workforce, few studies have documented their chronic disease risk, which is needed in order to identify assets and opportunities to provide support.6 To address this gap, this study focused on FCC professionals and sought to determine their health status in relation to chronic disease.
METHODS
A statewide survey of licensed FCC professionals was conducted in the fall of 2021. The full methods are available elsewhere,7 but briefly, a series of email invitations were sent by the state’s licensing office to all licensed FCC professionals (N=541). Respondents were eligible to enter a raffle for one of fifteen $200 gift cards.
MEASURES
Survey items were drawn or adapted from existing, validated questionnaires. Demographic and health status items were drawn from the Behavioral Risk Factor Surveillance System.8 To measure chronic disease status, respondents were asked to report, “Have you ever been told by a doctor, nurse or other health professional that you have…” with options of high blood pressure, diabetes, pre-diabetes or borderline diabetes and asthma.
Doi: 10.32481/djph.2024.03.03
8 Delaware Journal of Public Health - March 2024
Nutrition items were drawn from the Food Attitudes and Beliefs Survey9 and included questions related to water consumption and frequency of fast food consumption. Physical activity was assessed using items drawn from the Health Information National Trends Survey (HINTS) survey,10 which asked about the frequency and duration of physical activity at the moderate to intense level.
DATA ANALYSIS
After data cleaning procedures, which included removing duplicates and respondents who answered fewer than 20% of questions, data were analyzed using descriptive statistics appropriate to the measure (e.g. frequencies, means). Body Mass Index (BMI) was classified using the standard formula and established cutoffs for adults (e.g. overweight defined as a BMI of 25-29.9; obesity defined as a BMI of 30 or higher).
RESULTS
A total of 168 responses were included in the analysis (31% response rate). The majority of respondents identified as White (53.6%), with another third (34.3%) identified as Black or African-American (Table 1). Just 12 respondents (7.3%) identified as Hispanic, Latino/a or of Spanish origin. Only 10.2% of respondents (n=17) reported currently receiving SNAP benefits in the past 12 months. The mean number of hours worked per week was nearly 50 hours.
In terms of health status, the majority of respondents rated their overall health as Excellent (14.9%) or very good (47.4%) and a high proportion reported zero days in the past 30 days when their physical (73%) health was not good. Despite those reports, 86.1% of respondents are overweight or have obesity, 41.1% have diagnosed high blood pressure, and 17.9% have diagnosed asthma.
A very small proportion of respondents reported financial barriers to health care, and nearly all respondents reported having one or more people they think of as a personal doctor or health care provider. A majority of respondents reported drinking four or more cups of water per day (71.1%), eating fast food <1 time per week (77.3%), consuming five fruits and vegetables each day (77.0%), and participating in moderate to vigorous physical activity at least three days per week (56.2%).
CONCLUSIONS
This study provided a portrait of chronic disease prevalence and risk factors among FCC professionals, identifying areas of potential support and other areas to be celebrated. The diabetes rate in our sample (12.7%) was nearly double the rate found in a recent national survey of ECE workers (6.5%), which included both center-based and homebased educators.11 This increase may partially be due to the demographics of FCC educators in Delaware; 34.3% of our sample was Black or African-American, communities that have been disproportionately impacted by diabetes.12 The asthma rate in our sample (17.9%) is comparable to other national studies of ECE workers,11,13 but much higher than population-based estimates for women, and nearly 50% higher than the rate for women in the State of Delaware (12.6%). The existing research is inconclusive regarding the reason for this elevated risk, but one possible explanation includes poor indoor air quality in home and work environments due to high rates of pesticide use.14
NumberPercentage Demographics Identifies as White 8953.6 Identifies as Black or AfricanAmerican 5734.3 Identifies as Hispanic, Latino/a or of Spanish origin 12 7.3 SNAP Recipient 1710.2 Hours per week worked at child care job (mean, SD) M = 49.54SD = 16.6 Health Status Overall health rated excellent 2314.9 Overall health rated very good7347.4 Overall health rated good 5334.4 Overall health rated fair 5 3.2 In the past 30 days, zero days when physical health was not good 10873.0 Body Mass Index Classification Normal or underweight 2013.9 Overweight 6041.7 Obese 6444.4 Chronic Disease Diagnosis High blood pressure 62 41.1 Diabetes 1912.7 Pre-diabetes or borderline diabetes 2114.1 Asthma 2717.9 Health Care Access Health insurance coverage 141 87.6 One or more person they think of as a personal doctor or health care provider 141 92.8 Needed to see a doctor but could not because of cost within the past 12 months 1711.2 Health Behaviors Drink four or more cups of water per day 9671.1 Eat fast food <1 time per week 9977.3 Typically eat five or more fruits or vegetables each day 104 77.0 Three or more days per week of moderate to vigorous physical activity 7756.2
9
Table 1. Demographics and Chronic Disease Profile of Family Child Care Professionals, Delaware, 2021
In contrast, a high proportion of our respondents reported following recommended health behaviors including water drinking, fruit and vegetable consumption and physical activity. The rates in our sample are higher than other studies of FCC educators which found closer to 50% of respondents reporting these healthy behaviors,15 compared to the 70-77% we found in our study. This difference may be due to timing; the previous study was conducted in 2014 and our data were collected in 2021. One limitation of our study was the relatively small sample size (n=168), however our response rate (31%) was significantly higher than several other published studies of FCC educators.15 Another limitation is that these data were collected during the height of the COVID-19 pandemic, and may have been influenced by pandemic-related factors such as lack of access to healthcare that influenced our respondents ability to seek care and receive chronic disease diagnosis and treatment.16
PUBLIC HEALTH IMPLICATIONS
This study paints a picture of the chronic disease related health and behaviors of FCC professionals across the state. Future work should explore whether and how existing evidence-based chronic disease prevention and management programs, such as the National Diabetes Prevention Program and others, can be successfully implemented with FCC professionals. Additional work should also be done to explore the reasons for the elevated asthma rate found in our sample and other samples of child care professionals. Dr. Lessard may be contacted at llessard@udel.edu
REFERENCES
1. U.S. Department of Education, National Center for Education Statistics. (2021). Early Childhood Program Participation: 2019 (NCES 2020-075REV), Table 1.
2. Tonyan, H. A., Paulsell, D., & Shivers, E. M. (2017). Understanding and incorporating home-based child care into early education and development systems. Early Education and Development, 28(6), 633–639.
https://doi.org/10.1080/10409289.2017.1324243
3. de Schipper, E. J., Riksen-Walraven, J. M., Geurts, S. A. E., & Derksen, J. J. L. (2008). General mood of professional caregivers in child care centers and the quality of caregiver–child interactions. Journal of Research in Personality, 42(3), 515–526.
https://doi.org/10.1016/j.jrp.2007.07.009
4. Boyle, M. H., Olsho, L. E. W., Mendelson, M. R., Stidsen, C. M., Logan, C. W., Witt, M. B., . . . Copeland, K. A. (2022, June 1). Physical activity opportunities in US early child care programs. Pediatrics, 149(6), e2020048850.
https://doi.org/10.1542/peds.2020-048850
5. Hasnin, S., Saltzman, J. A., & Dev, D. A. (2022, April 8). Correlates of children’s dietary intake in childcare settings: A systematic review. Nutrition Reviews, 80(5), 1247–1273. https://doi.org/10.1093/nutrit/nuab123
6. Lessard, L. M., Wilkins, K., Rose-Malm, J., & Mazzocchi, M. C. (2020, January 8). The health status of the early care and education workforce in the USA: A scoping review of the evidence and current practice. Public Health Reviews, 41, 2. https://doi.org/10.1186/s40985-019-0117-z
7. Lessard, L., Hallam, R., Drain, D., & Ruggiero, L. (2022, March 19). COVID-19 vaccination status and attitudes of family child care providers in Delaware, September 2021. Vaccines, 10(3), 477.
https://doi.org/10.3390/vaccines10030477
8. Centers for Disease Control and Prevention (CDC). (2020). Behavioral risk factor surveillance system survey questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
9. Erinosho, T. O., Pinard, C. A., Nebeling, L. C., Moser, R. P., Shaikh, A. R., Resnicow, K., . . . Yaroch, A. L. (2015, February 23). Development and implementation of the National Cancer Institute’s Food Attitudes and Behaviors Survey to assess correlates of fruit and vegetable intake in adults. PLoS One, 10(2), e0115017.
https://doi.org/10.1371/journal.pone.0115017
10. Nelson, D. E., Kreps, G. L., Hesse, B. W., Croyle, R. T., Willis, G., Arora, N. K., . . . Alden, S. (2004, Sep-Oct). The health information national trends survey (HINTS): Development, design, and dissemination. Journal of Health Communication, 9(5), 443–460.
https://doi.org/10.1080/10810730490504233
11. Elharake, J. A., Shafiq, M., Cobanoglu, A., Malik, A. A., Klotz, M., Humphries, J. E., . . . Gilliam, W. S. (2022, September 22). Prevalence of chronic diseases, depression, and stress among US childcare professionals during the COVID-19 pandemic. Preventing Chronic Disease, 19, E61.
https://doi.org/10.5888/pcd19.220132
12. Rodríguez, J. E., & Campbell, K. M. (2017, January). Racial and ethnic disparities in prevalence and care of patients with type 2 diabetes. Clin Diabetes, 35(1), 66–70.
https://doi.org/10.2337/cd15-0048
13. Kwon, K. A., Ford, T. G., Salvatore, A. L., Randall, K., Jeon, L., Malek-Lasater, A., . . . Han, M. (2020). Neglected elements of a high-quality early childhood workforce: Whole teacher well-being and working conditions. Early Childhood Education Journal, 1–12.
14. Querdibitty, C. D., Williams, B., Wetherill, M. S., Sisson, S. B., Campbell, J., Gowin, M., . . . Salvatore, A. L. (2021, August 11). Environmental health-related policies and practices of Oklahoma licensed early care and education programs: Implications for childhood asthma. International Journal of Environmental Research and Public Health, 18(16), 8491.
https://doi.org/10.3390/ijerph18168491
15. Tovar, A., Vaughn, A. E., Grummon, A., Burney, R., Erinosho, T., Østbye, T., & Ward, D. S. (2016, November 14). Family child care home providers as role models for children: Cause for concern? Preventive Medicine Reports, 5, 308–313.
https://doi.org/10.1016/j.pmedr.2016.11.010
16. Roy, C. M., Bollman, E. B., Carson, L. M., Northrop, A. J., Jackson, E. F., & Moresky, R. T. (2021, July 13). Assessing the indirect effects of COVID-19 on healthcare delivery, utilization and health outcomes: A scoping review. European Journal of Public Health, 31(3), 634–640.
https://doi.org/10.1093/eurpub/ckab047
10 Delaware Journal of Public Health - March 2024
Start or Advance Your Health Care Career With Wilmington University
Tremendous opportunity awaits you in the health care industry. No matter where you are in your career, WilmU has a health sciences degree designed to fit your professional goals and your busy schedule.

Associate of Science in Health Sciences
The ever-evolving health care landscape continually creates novel roles, and individuals with foundational knowledge in health care coupled with specific, concentrated skill sets can prove increasingly marketable in these new positions. WilmU’s A.S. in Health Sciences is intended to create exactly these opportunities for entry-level career starters, as well as mid-career changers, to enter health care positions with maximal career mobility.
Bachelor of Science in Health Sciences
Our B.S. in Health Sciences program is designed for students who have an interest in health care roles that provide managerial, educational and/or clinical expert direction in a health care setting. This program can be tailored to meet specific career goals by using electives to complete a related WilmU certificate and/or through meaningful, hands-on cooperative learning experiences that build skill sets and expand professional networks.
Master of Science in Health Sciences
Prepare to improve health outcomes across the continuum of care using evidence-based practice and data-driven decision making with WilmU’s M.S. in Health Sciences. This interdisciplinary program exposes students to different viewpoints and problemsolving strategies, placing strong emphasis on health care policy and environmental influences, population-based health interventions, and a cross-cultural approach toward all individuals in the prevention of illness and promotion and management of health.
Upon graduation, students will be eligible to pursue certification as a Certified Health Education Specialist. This designation demonstrates a mastery of skill sets for multiple arenas: nonprofit, government and for-profit acute or community-based health care organizations. Graduates will be equipped to deliver education both formally and informally to individuals and populations from an environmental health or population health perspective.
Part of a Series of Accelerated, Stackable Credentials
WilmU’s Dual-Credit ADVANTAGE™ lets you accelerate from one degree to the next by applying credits from the Health Sciences associate degree to the B.S. program. Go even further by incorporating graduate-level courses into your bachelor’s in Health Sciences program. It’s a great way to save time and tuition dollars! Learn
more at: go.wilmu.edu/HealthSciences
ADVANTAGE are registered trademarks of Wilmington University. All rights reserved. © Wilmington University 2024 11
WilmU and Dual-Credit
A Comprehensive Analysis of the Impact of the COVID-19 Pandemic on Lung Cancer in Delaware
Brian Nam, M.D., F.A.C.S.
Department of Thoracic Surgery, Helen F. Graham Cancer Center, ChristianaCare Health Services, Inc.
Yeonjoo Yi, Ph.D.
Institute for Research on Equity and Community Health (iREACH), ChristianaCare Health Services, Inc.
Kevin Ndura, M.B.A.
Institute for Research on Equity and Community Health (iREACH), ChristianaCare Health Services, Inc.
Krishna Vasireddy, Pharm.D., M.S.
Delaware Health Information Network (DHIN)
Claudine Jurkovitz, M.D., M.P.H.
Institute for Research on Equity and Community Health (iREACH), ChristianaCare Health Services, Inc.
Kiran Kattepogu, M.B.B.S., M.P.H.
Department of Thoracic Surgery, Helen F. Graham Cancer Center, ChristianaCare Health Services, Inc.
ABSTRACT
Background: COVID-19 has greatly impacted the U.S. health system. What is not as well-understood is how this has altered specific aspects of lung cancer care. While cancer incidence and screening have been affected, it is not known whether pre-existing racial and socioeconomic disparities worsened or if treatment standards changed. The purpose of this study is to provide a comprehensive analysis of the impact of COVID-19 on lung cancer in the state of Delaware. Methods: Health care claims were analyzed from the Delaware Health Care Claims Database for the years 2019-2020. Patients with a new lung cancer diagnosis and those who had undergone lung cancer screening were identified. Demographic and socioeconomic variables including gender, age, race, and insurance were studied. Patients were analyzed for type of treatment by CPT code. The intervention of interest in this study was the institution of restrictions at the end of March 2020. An interrupted time series analysis (ITSA) was utilized to evaluate baseline levels and overall trend changes. Results: The incidence of lung cancer diagnoses and lung cancer screenings decreased in the nine-month time period after the initiation of COVID-19 lockdowns. Demographic and socioeconomic variables including gender, race, income, and education level were not affected; however, statistical differences were seen in the most elderly subgroup. Treatment modalities including number of surgeries, chemotherapy, and radiation therapy did not change significantly. Conclusions: COVID-19 has had a significant impact on lung cancer care within the state of Delaware. Lung cancer incidence, screenings, and elderly patients were affected the most.
INTRODUCTION
The first cluster of cases of a severe acute respiratory syndrome coronavirus2 (SARS-CoV-2) was reported in Wuhan, China in December of 2019.1 The U.S. Centers for Disease Control and Prevention detected the first laboratory-confirmed case in the U.S. on January 20, 2020.2 In Delaware, a State of Emergency was issued on March 12, and stay-at-home restrictions were instituted on March 23, 2020. Since then, COVID-19 has been responsible for the deaths of around 3000 Delawareans,3 and more than one million Americans.4
COVID-19 has had a tremendous impact on health care in the US and health systems needed to adapt to this new reality. Restrictions limited the spread of infection; however, access to care was impaired. Providing timely cancer care was an ongoing challenge as health systems and physicians adopted new practice models to deal with the influx of acutely sick patients. Treatment standards, along with patient perceptions towards care, may have been altered. Pre-existing disparities may have
worsened as well. The impact on cancer care delivery is not yet fully understood, and a comprehensive examination of the effects of the pandemic on lung cancer has not been performed to date. The objective of this study is to evaluate impact of COVID-19 on lung cancer care in Delaware.
MATERIAL AND METHODS
Data Source and Study Population
Health care claims from the Delaware Health Information Network Database were collected for the years 2019-2020. Two populations were identified using ICD-10 and CPT codes: patients with a new lung cancer diagnosis (ICD- 10 code C34.9) and those who have undergone lung cancer screening (CPT code 71271). These two study populations were analyzed separately. The study population for lung cancer screening was selected according to the United States Preventive Services Task Force (USPSTF) guidelines, which recommends annual screening for adults aged 50 to 80 years who have a 20 pack-year smoking history and are current smokers or have quit within the past 15 years.5
Doi: 10.32481/djph.2024.03.04
12 Delaware Journal of Public Health - March 2024
From these claims, we obtained demographic information (gender, age at diagnosis or screening, race), type of cancer treatment – i.e., surgery (CPT codes: 32440, 32482, 32484, 32504, 32505, 32663, 32668, 32669, 32670, 32671), chemotherapy (CPT codes: 96401, 96402, 96409, 96411, 96413, 96415, 96416) and radiation (CPT codes: 32701, 77412, 77470) – as well as census tract information. We further linked the census tract data to the American Community Survey to obtain socio-economic information such as median income.6
Statistical Analysis
An interrupted time series analysis (ITSA) was used to evaluate the level and trend changes in lung cancer incidence and screenings from January 1, 2019 to December 31, 2020.7–10 Primary outcomes were defined as the weekly number of new lung cancer cases, the weekly number of screenings and the monthly number of different treatment modalities. A breakpoint in significant level changes and trends was identified corresponding to the institution of COVID restrictions at the end of March 2020.
Patient-level demographics are summarized as descriptive statistics. Median income was defined as $90,000/year based on the Pew Research Center definition for 2020.6 Continuous variables are presented as means and medians, and categorical variables are presented as frequencies. Group differences were evaluated by chi-squared and Fisher-Exact tests for categorical variables and T-test for continuous variables. All tests were 2-sided and statistical significance was set at p ≤0.05.
Segmented regression analysis used statistical models to estimate levels and trends of outcomes before the pandemic and after the institution of restrictions. The fitted model was selected using stepwise selection and AIC (Akaike information criterion). Sensitivity analyses were performed. The trend before the pandemic was added to the final model as a control variable. Segmented regression with an ordinary least-squares method was used in this analysis. Autocorrelation was assessed by examining the plot of ACF (Autocorrelation Function) and PACF (Partial Autocorrelation Function) residuals and conducting Durbin-Watson and Breusch-Godfrey tests. After detecting autocorrelations, these were adjusted for standard errors. Subgroups analyses were conducted to examine whether changes
in new lung cancer and lung cancer screening varied according to age group and insurance. Segmented regression was used to measure parameter estimates and 95% confidence interval (CI) for immediate (level) changes in the outcome as well as changes in the trend (slope). The Mann-Whitney U test was performed to compare median of monthly counts of lung cancer treatments between the two time-periods. Statistical analyses were performed using R 4.2 and SAS 9.4.
RESULTS
A total of 2,031 patients with a new diagnosis of lung cancer and a total of 4,285 patients who underwent lung cancer screening were identified during a two-year period from January 1, 2019, to December 31, 2020.
Lung Cancer Counts
The monthly counts of newly diagnosed lung cancer cases along with the number of new COVID cases in Delaware are shown in Figure 1. Several demographic and socioeconomic groups were examined for worsening of pre-existing disparities (Table 1). No significant differences were seen between the two time-periods in mean age, gender, race, insurance, geographic county, or income level. However, a significant change was seen in the most elderly population, ages 81-90 (p=0.038) for whom the frequency of new cases of lung cancer was much lower during the COVID time-period.
Segmented regression results are provided in Table 2 Autoregressive error models were used to quantify changes over time and compare patterns before and after April 1, 2020. The Durbin-Watson statistic for the regression model of lung cancer incidence was 2.0901 (p-value for hypothesis of negative autocorrelation =0.3023, p-value for hypothesis of positive autocorrelation = 0.6977), indicating no autocorrelation. The baseline level before the COVID-19 pandemic was 20.8063 (95% CI: 18.8257 to 22.7869). The trend before the pandemic was flat (0.0026; 95% CI: -0.0481 to 0.0533). The level change (p-value=0.005) in incidence of new lung cancers decreased by 4.204 (95% CI: -7.3717 to -1.0364) or 20% immediately after the institution of restrictions after April 1, 2020. There was no evidence of significant recovery or upward trend change, even though restrictions were lifted on June 1, 2020 (Figure 2).
13
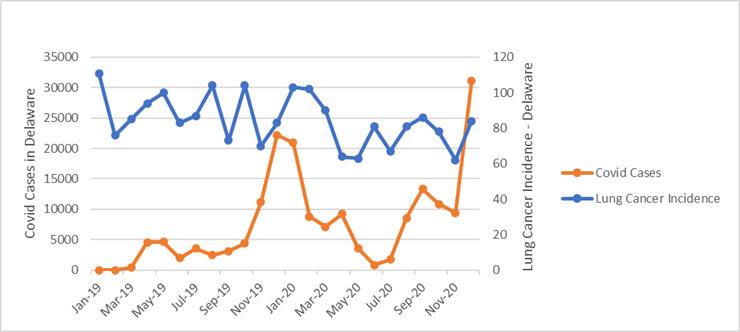
Figure 1. Monthly Lung Cancer Incidence and COVID Cases in Delaware Before and During the Pandemic
The grey circle represents the observed weekly lung cancer screening cases. The solid blue line corresponds to the fitted regression line for each of the two study intervals.
The vertical dashed red line indicates the institution of restrictions on April 1, 2020.
Results of age group sub-analyses are presented in Table 2 and Figure 2. The institution of restrictions had an immediate effect on new lung cancer diagnoses for individuals of the ages 80-90 (-1.5424, 95% CI: -2.9151 to -0.1697). This represents a 37% decrease in incidence within this cohort. Changes in age groups 20-69 and 70-79 were small and not statistically significant.
Lung Cancer Screening
Several demographic and socioeconomic groups were again examined for worsening of pre-existing disparities (Table 3). No significant differences were seen in screening frequency according to age groups, mean age, gender, race, or income level.
Compared to patients who were screened before the pandemic, those screened after April 1, 2020 were more likely to have Medicaid and less likely to have commercial insurance (p=0.0002). Differences between the two time-periods were also seen in the proportions of patients screened per county (p<0.0001).
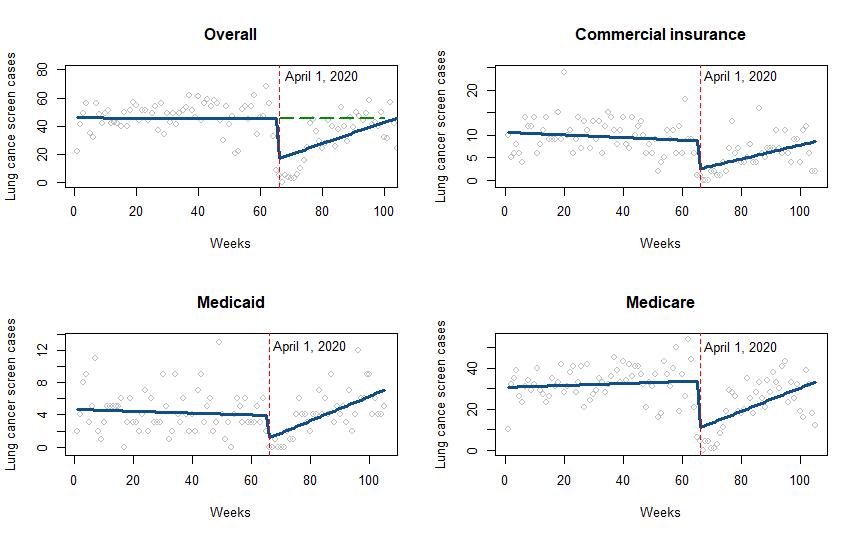
As shown in Table 4 and Figure 3, the weekly overall count of patients undergoing lung cancer screening was constant prior to the pandemic at approximately 46 per week, with a nonsignificant decrease of 0.0073 per week. However, the restriction in services due to COVID-19 led to a sharp decrease of 29 screenings per week (95% CI: -42.6616 to -15.4949) immediately after March 31 followed by a gradual and significant increase of 0.7625 (95% CI: 0.2184 to 1.3066) lung cancer screenings per week. The estimated trend for the post-COVID pandemic was 0.7552 [95% CI: 0.2851 to 1.2251], (0.7552= trend pre (-0.0073) + changes in trend after pandemic (0.7625)).
The best-fitting model estimates for each of the insurance categories are given in Table 4. The immediate decreases in the counts of patients undergoing screening in the first week just after April 2020 were significant for the three types of insurance: -6.3933 (72.83%) for commercial insurance, -2.9467 (62.95%) for Medicaid, and -23.413 (69.40%) for Medicare.
As illustrated in Figure 3, the pandemic effect diminished over time with the number of lung cancer screenings increasing. The absolute difference and relative difference between the hypothetical number of cases on the counterfactual line and the
Jan 1, 2019 - Mar 31, 2020 (n=1365)Apr 1, 2020 - Dec 31. 2020 (n=666) P-value Age, mean (SD) 71.17 (9.69) 70.51 (9.17) 0.138 Age Groups 20 - 69 553 (40.51%) 282 (42.34%) 0.038 70 - 79 537 (39.34%) 281 (42.19%) 80 - 90 275 (20.15%) 103 (15.47%) Gender Female 685 (50.18%) 336 (50.45%) 0.910 Male 680 (49.82%) 330 (49.55%) Race AA 138 (10.11%) 66 (9.91%) 0.999 White 994 (72.82%) 474 (71.17%) Other 75 (5.49%) 36 (5.41%) # of missing 158 (11.58%) 90 (13.51%) Insurance Commercial 150 (10.99%) 69 (10.36%) 0.869 Medicaid 132 (9.67%) 62 (9.31%) Medicare 1083 (79.34%) 535 (80.33%) County Kent 252 (18.46%) 122 (18.32%) 0.137 New Castle 594 (43.52%) 262 (39.34%) Sussex 519 (38.02%) 282 (42.34%) Income < 90,000 502 (36.78%) 266 (39.94%) 0.161 >90,000 83 (6.08%) 30 (4.50%) # of missing 774 (56.70%) 365 (54.80%) 14 Delaware Journal of Public Health - March 2024
Table 1. Demographics of New Lung Cancer Patients Before and After April 1, 2020

All models are unadjusted. 95% Confidence Interval (CI) in brackets, Estimates from best-fitting segmented regression. *Statistically significant with p-value ≤ 0.05.
observed number of cases was smaller six months (10.766 and -0.239) after March 31, 2020 compared to three months (19.922 and -0.439). At three months after the pandemic, the absolute difference for the number of lung cancer screening per week was 4.18 for commercial insurance, 0.99 for Medicaid, 17.153 for Medicare compared with what the number of cases would have been if the trend observed prior to the pandemic had not been interrupted, indicating that lung cancer screening recovered faster for patients on Medicaid than for patients on commercial insurance and Medicare.
The grey circle represents the observed weekly lung cancer screening cases. The solid blue line corresponds to the fitted regression line for each of the two study intervals. The vertical dashed red line indicates the institution of restrictions on April 1, 2020. The dashed green line represents the counterfactual. If the institution of restrictions had not happened, the blue line would have continued as shown by the green line.
Figure 2. Weekly Numbers of Lung Cancer Diagnoses in Delaware from January 1, 2019 to December 31, 2020
Level Before Pandemic (95% CI) Trend Before Pandemic (95% CI) Absolute Changes in Levels After the Institution of Restrictions April 1, 2020 (95% CI) Overall 20.8063 (18.8257,22.7869)* 0.0026 (-0.0481,0.0533) -4.204 (-7.3717,-1.0364)* Age 20-69 8.4961 (7.4703,9.522)* 0.0001 (-0.0262,0.0264) -1.4427 (-3.0878,0.2022) Age 70-79 8.0906 (6.7995,9.3816) * 0.0033 (-0.0297,0.0363) -1.249 (-3.3138,0.8158) Age 80-90 4.2204 (3.3621,5.0787) * -0.0006 (-0.0226,0.0213) -1.5424 (-2.9151,-0.1697) *
Table 2. Interrupted Time Series Regression Analysis of Lung Cancer Incidence Overall and Per Age Group
15
All models are unadjusted. 95% Confidence Interval (CI) in brackets, Estimates from best-fitting segmented regression. *Statistically significant with p-value≤0.05.
Jan 1, 2019 - Mar 31, 2020 (n=3023)Apr 1, 2020 - Dec 31. 2020 (n=1262)P-value Age, mean (SD) 66.133 (5.732) 65.824 (5.857) 0.1106 Age 50-59 491 (16.24%) 229 (18.15%) 0.2805 60-69 1618 (53.52%) 669 (53.01%) 70-79 914 (30.23%) 364 (28.84%) Gender Female 1514 (50.08%) 645 (51.11%) 0.5401 Male 1509 (49.92%) 617 (48.89%) Race AA 213 (7.05%) 106 (8.40%) 0.0597 White 1956 (64.70%) 759 (60.14%) Other 182 (6.02%) 87 (6.89%) # of missing 672 (22.23%) 310 (24.57%) Insurance Commercial 631 (20.87%) 223 (17.67%) 0.0002 Medicaid 280 (9.26%) 164 (13%) Medicare 2112 (69.86%) 875 (69.33%) County Kent 646 (21.37%) 257 (20.36%) <.0001 New Castle 725 (23.98%) 391 (30.98%) Sussex 1652 (54.65%) 614 (48.65%) Income < 90,000 1114 (85%) 468 (37.08%) 0.8444 >90,000 119 (3.94%) 48 (3.80%) # of missing 1777 (58.78%) 739 (58.56%)
Table 3. Demographics of Patients Undergoing Lung Cancer Screening Before and After April 1, 2020
Level Before Pandemic (95% CI) Trend Before April 1, 2020 (95% CI) Immediate Change in Level (95% CI) Change in Trends After April 1, 2020 (95% CI) Overall 45.9419 (36.8882,54.9956)* -0.0073 (-0.2429,0.2283) -29.0783 (-42.6616,-15.4949)* 0.7625 (0.2184,1.3066)* Commercial 10.6625 (8.8195,12.5054)* -0.0289 (-0.0774,0.0196) -6.3933 (-9.3671,-3.4196)* 0.1843 (0.0726,0.296)* Medicaid 4.6811 (3.5419,5.8204)* -0.0114 (-0.0414,0.0185) -2.9467 (-4.7828,-1.1106)* 0.163 (0.0939,0.232)* Medicare 30.55 (24.4714,36.6286)* 0.049 (-0.1094,0.2074) -23.413 (-32.911,-13.9149)* 0.522 (0.1557,0.8883)*
Table 4. Interrupted Time Series Regression Analysis of Lung Cancer Screening Overall and Per Insurance Category
16 Delaware Journal of Public Health - March 2024
Jan 1, 2019 - Mar 31, 2020 Median Monthly (range) Apr 1, 2020 - Dec 31, 2020 Median Monthly (range) P-value Surgery (n=283) 14 (10-15) n=191 9 (8-11) n=92 0.0848 Radiation (n=482) 21 (17-23) n=317 17 (15-22) n=165 0.3848 Chemotherapy (n=340) 12 (11-17) n=196 15 (13-21) n=144 0.1023 Median
Table 5. Comparison of Treatment Methods Before and After April 1, 2020
(the first quartile, the third quartile), n=new lung cancer patients.
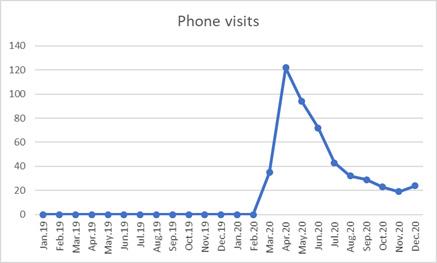
Figure 4. Monthly Phone Visits Before and After the Pandemic
Figure 3. Weekly Numbers of Lung Cancer Screening in Delaware from January 1, 2019 to December 31, 2020
17
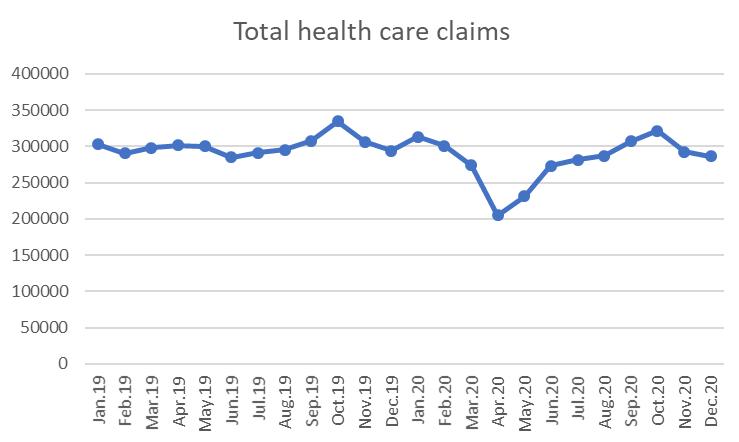
Figure 5. Monthly Number of Healthcare Claims Before and After the Pandemic
Impact of COVID on the Management of Lung Cancer
The impact of the pandemic on the treatment practice of lung cancer was also examined. The median of the monthly numbers of patients receiving surgical resection decreased from 14 to 9 after the institution of restrictions and from 21 to 17 for those receiving radiation therapy, but the differences were not significant (p=0.0848, p=0.3848) (Table 5). An increase was observed for those receiving chemotherapy (median:12 vs 15, p-value = 0.1023); however, this was also not statistically significant.
Impact on Health Care Utilization
Virtual visits in the form of phone visits were a new phenomenon in the care of lung cancer patients. The usage of this modality peaked in April of 2020 and then decreased for the remainder of the year (Figure 4). The average of the monthly number of submitted health claims (Figure 5) decreased by 27% during the months of April and May of 2020 (300,137 claims/month before April 1, 2020 to 218,220)) but returned close to pre-pandemic levels for the remainder of 2020 (292,604 claims/month).
DISCUSSION
These results illustrate the impact of the pandemic on health systems and lung cancer care.
Significant decreases in lung cancer incidence and screening were observed in this analysis are in line with findings from previous studies.11,13
Interestingly, these decreases did not correlate with the course of the virus, or the number of Americans infected; but, rather, with the institution of lockdowns. Lockdowns mitigated the spread of the virus and saved lives; however, restricting access adversely affected cancer care.12 These findings suggest that alternative mitigation plans should be considered in the future.
Screening recovered to pre-pandemic levels by the end of 2020; however, lung cancer incidence did not. These effects may have led to delayed diagnoses and an upshifting of all stages although this could not be analyzed within the scope of this study. Fortunately, a worsening of pre-existing disparities in several demographic and racial/socioeconomic groups was not observed. However, one group that was significantly impacted was the most elderly population (ages 80-90). These patients were the most vulnerable to COVID-related mortality and should be kept at the forefront when developing future healthcare policies.
In the lung screening group, a decrease was observed in those with commercial insurance while those needing Medicaid insurance increased. Likely, this was secondary to employment patterns during the pandemic with patients losing employment and necessitating Medicaid for health coverage. The differences in screening at the county level were likely due to individual health systems resuming their screening programs at different rates.
Treatment paradigms for lung cancer were possibly altered during the pandemic. Fewer patients underwent surgical
resection and more underwent less invasive treatment options such as chemotherapy, although these differences were not statistically significant. Other studies have examined these trends as well14 and are important to keep in mind, so that patients continue to receive the standard of care amidst a future health crisis.
The pandemic adversely impacted total health care claims and health care revenue for the 2020 year. Federal relief funds blunted some of these deficits; however, the need for innovation led to the development of novel alternative forms of care including virtual visits. Virtual medicine persisted even as the pandemic waned and will likely become a permanent option for accessing and delivering health care.
CONCLUSIONS
COVID-19 had a significant impact on lung cancer care within the state of Delaware. Lung cancer incidence, screenings, and the most elderly patients were affected. These findings can be utilized to help shape health policies in the event of a future pandemic. Dr. Nam may be contacted at bnam@christianacare.org
ACKNOWLEDGEMENTS
Work supported by Institutional Development Awards (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20 GM103446 (PI: Duncan) and grant number U54-GM104941 (PI: Hicks)
REFERENCES
1. World Health Organization. (2020). Pneumonia of unknown cause — China.
https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkowncause-china/en/
2. Holshue, M. L., DeBolt, C., Lindquist, S., Lofy, K. H., Wiesman, J., Bruce, H., . . . Pillai, S. K., & the Washington State 2019-nCoV Case Investigation Team. (2020, March 5). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936. https://doi.org/10.1056/NEJMoa2001191
3. Delaware Health and Social Services. (2023, Feb 24). Myhealthycommunity coronavirus COVID-19 data dashboard.
https://myhealthycommunity.dhss.delaware.gov/locations/state/deaths
4. Centers for Disease Control and Prevention. (2023, Feb 24). COVID data tracker.
https://covid.cdc.gov/covid-data-tracker/#datatracker-home
5. Krist, A. H., Davidson, K. W., Mangione, C. M., Barry, M. J., Cabana, M., Caughey, A. B., . . . Wong, J. B., & the US Preventive Services Task Force. (2021, March 9). Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA, 325(10), 962–970.
https://doi.org/10.1001/jama.2021.1117
6. Kochhar, R., & Sechopoulos, S. (2022, April 20). How the American middle class has changed in the past five decades. Pew Research Center
https://www.pewresearch.org/fact-tank/2022/04/20/how-the-americanmiddle-class-has-changed-in-the-past-five-decades/
18 Delaware Journal of Public Health - March 2024
7. Bernal, J. L., Cummins, S., & Gasparrini, A. (2017, February 1). Interrupted time series regression for the evaluation of public health interventions: A tutorial. International Journal of Epidemiology, 46(1), 348–355.
https://doi.org/10.1093/ije/dyw098
8. Bernal, J. L., Cummins, S., & Gasparrini, A. (2021).
Corrigendum to: Interrupted time series regression for the evaluation of public health interventions: a tutorial.
International Journal of Epidemiology, 50(3), 1045.
https://doi.org/10.1093/ije/dyaa118
9. Xiao, H., Augusto, O., & Wagenaar, B. H. (2021, July 9). Reflection on modern methods: A common error in the segmented regression parameterization of interrupted timeseries analyses. International Journal of Epidemiology, 50(3), 1011–1015.
https://doi.org/10.1093/ije/dyaa148
10. Turner, S. L., Karahalios, A., Forbes, A. B., Taljaard, M., Grimshaw, J. M., & McKenzie, J. E. (2021, June 26).
Comparison of six statistical methods for interrupted time series studies: Empirical evaluation of 190 published series. BMC Medical Research Methodology, 21(1), 134.
https://doi.org/10.1186/s12874-021-01306-w
11. Fedewa, S. A., Bandi, P., Smith, R. A., Silvestri, G. A., & Jemal, A. (2022, February). Lung cancer screening rates during the COVID-19 pandemic. Chest, 161(2), 586–589.
https://doi.org/10.1016/j.chest.2021.07.030
12. Van Haren, R. M., Delman, A. M., Turner, K. M., Waits, B., Hemingway, M., Shah, S. A., & Starnes, S. L. (2021, April). Impact of the COVID-19 pandemic on lung cancer screening program and subsequent lung cancer. Journal of the American College of Surgeons, 232(4), 600–605.
https://doi.org/10.1016/j.jamcollsurg.2020.12.002
13. Mariotto, A. B., Feuer E. J., Howlader, N., Chen, H., Negoita, S., & Cronin, K. A. (2023, September). Interpreting cancer incidence trends: challenges due to the COVID-19 pandemic. Journal of the National Cancer Institute, 115(9), 1109-1111.
https://doi.org/10.1093/jnci/djad086
14. Piñeiro, F.M., & Aguado, J. F. (2021, February). Management of lung cancer in the COVID-19 pandemic: a review. Journal of Cancer Metastasis and Treatment. 7, 10.
https://doi.org/10.20517/2394-4722.2020.115

Even the best rider is at the mercy of other drivers. If you go too fast, they may cut you off, change lanes, or make turns before they see you coming.
SO WATCH YOUR SPEED, WATCH OUT FOR OTHER DRIVERS, AND STAY SOBER.
ArriveAliveDE.com/Respect-The-Ride
Life'stooshorttogo
19
too fast

From the Delaware Division of Public Health February 2024
New DPH leadership team announced
Delaware Department of Health and Social Services (DHSS) Secretary Josette Manning announced a new leadership team at the Division of Public Health (DPH), led by Division Director Steven Blessing.

“This team has extensive experience in managing key areas at DPH,” Secretary Manning said. “They will help our nationally accredited division protect and promote health for all Delawareans.”
Director Blessing oversees over 1,000 staff and manages a $433 million budget in grant and state funding. He previously served as Interim DPH Division Director since September 2023. He was named DPH Deputy Director in October 2022.
For 29 years, Director Blessing has served DPH in various leadership positions, including Emergency Medical Services Director, Paramedic Administrator, and Executive Assistant to the Director. During his 12 years as Chief of the Emergency Medical Services and Preparedness Section, he led the development and expansion of response capacity for health and natural disasters. During the COVID-19 response, Director Blessing managed the State Health Operations Center (SHOC) and was the Incident Commander in the final phases. He also managed the SHOC during Hurricanes Sandy and Irene, the Ebola crisis, and other emergencies.
Director Blessing was elected by his peers as President of the National Association of State EMS Officials from 2008 to 2010. He participated in a number of meaningful projects at the state and national levels.
Director Blessing is a former U.S. Army officer and holds a Bachelor of Arts degree in Political Science from the University of Delaware and a Master's degree in Business from Webster University.
“The Division of Public Health is a large and multifaceted agency, staffed with incredibly talented and dedicated professionals,” Director Blessing said. “It is a great honor to have this opportunity to lead at such a critical time and meet the challenges of improving

the overall health status and well-being of people in Delaware.”
Shonetesha (Tēsha) Quail, PhD, LPCMH, NCC was named Deputy Director of DPH in October 2023, providing oversight for over 1,000 employees. Previously, Dr. Quail served as DPH Associate Deputy Director since December 2022 and oversaw the Birth to Three Programs and Community Health Promotion Branch. With 25 years of organizational experience working in the private and government sectors, she ensures health equity with a continuum of care approach and continues to serve as Chief Health Equity Officer.
Dr. Quail began her DPH career in 2013 and oversaw Southern Health Services for Kent and Sussex counties. She teaches classes as an Adjunct Professor at Wilmington University in the College of Health Professions and Natural Sciences.

Dr. Quail graduated from Wilmington University with a Bachelor of Science in Human Resources Management and a Master of Science in Clinical Mental Health Counseling. She became a licensed psychotherapist in 2012 She holds a second Master’s degree in Psychology and has a Doctor of Philosophy degree in Health Psychology with a concentration in Public Health, both from Walden University. Dr. Quail is currently enrolled in the Leadership Development to Advance Equity in Health Care program at Harvard University’s T.H. Chan School of Public Health.
Rebecca D. Walker, PhD, JD, MSN is the Deputy Director for Clinical Sciences. Since coming to DPH in 2020, Dr. Walker served as the Director of Nursing for two years and oversaw multiple sciencebased teams. She has over 31 years of administrative, academic, and clinical nursing experience. Her clinical background is in emergency nursing, surgical trauma, critical care transport, and pre-hospital incident response.
Continued on p. 2

 Shonetesha Quail
Rebecca Walker
Shonetesha Quail
Rebecca Walker
20 Delaware Journal of Public Health - March 2024
Steven Blessing
New DPH leadership team ― from p.1
Dr. Walker has served as the President of the Delaware Board of Nursing, the Chair of the Overdose Fatality Review Commission, an Associate Professor in Academia, Director of the International Master of Laws (LLM) program at Widener Law, a health care litigator in Philadelphia, and the Chief of Operations for the Division of Forensic Sciences. She also served the State of Delaware’s 9th District as a state representative Dr. Walker led major statewide initiatives and managed budgets at the Delaware Department of Safety and Homeland Security
Dr. Walker received her foundational nursing education at Delaware Technical Community College (ADN), Wilmington University (BSN), and Wesley College (MSN). She is a 2004 graduate of Widener Law School where she received her Juris Doctor and became a member of both the Pennsylvania and New Jersey Bars. She completed her PhD in nursing research at the Medical University of South Carolina.
Awele Maduka-Ezeh, MD, MPH, PhD, CCHP was recently named Medical Director of DPH. Dr. Maduka-Ezeh is a public health physician with expertise (research and practice) in pandemic preparedness and response among vulnerable and marginalized populations, and in managing public health laboratories.

She previously worked for DPH as State Medical Director and Chief of the Infectious Disease Prevention Section; and Director of the Delaware Public Health Laboratory. Prior to her appointment, Dr. Maduka-Ezeh was the Medical Director and Health Care Epidemiologist for the Delaware Department of Correction’s Bureau of Health Care, Substance Abuse, & Mental Health since 2018.
Dr. Maduka-Ezeh earned her Medical Doctorate from the University of Ibadan in Nigeria in 2000. She received a Master of Public Health from Harvard University in 2005 and completed her Internal Medicine residency at the Albert Einstein Medical Center in Philadelphia from 2006 to 2009. In 2011, she completed an infectious diseases fellowship at the Mayo Clinic, where she was also an instructor in medicine. Dr. Maduka-Ezeh earned a PhD in Disaster Science & Management from the University of Delaware in 2020
Dr. Maduka-Ezeh is board-certified by the American Board of Internal Medicine in infectious diseases (2011-2033) and internal medicine (2009-2029).
Christina (Tina) Farmer was recently named Chief of Staff of DPH. Farmer represents the Director and Deputies at meetings and hires Director’s Office staff. She coordinates with the DHSS Deputy Attorney General and oversees the Office of Communications, Contracts & Grants, and the Office of Performance Management.

She relays information between the DPH leadership team and other staff members while working with division and department leaders on project coordination and business administration. Farmer uses performance indicators and top-level strategies to oversee nearly 1,000 staff members. One of her primary duties is to identify employee issues and provide workable solutions.
Farmer is a native of Delaware and has spent most of her career dedicated to advancing health equity in women’s health services, especially in underserved communities.
She has held positions for over 10 years at DPH, including roles in Fiscal, Clinic Services, Informatics, Family Planning, and the Birth to Three Early Intervention Program. Most recently, Farmer served as Director of Community Health Promotions, which includes the Family Health Systems Section, the Health Systems Protection Section, the Health Promotion and Disease Prevention Section, the Office of Health Crisis Response, and the Office of Healthcare Provider Resources. She currently serves on the Health Literacy Council of Delaware, Partnership for Health Communities Steering Committee, and the Overdose System of Care Rural Subcommittee.
Farmer led the implementation of the Delaware Contraceptive Access Now (DECAN) initiative, a public-private partnership between the State of Delaware and Upstream USA to help reduce unplanned pregnancies. DECAN focuses on a set of policy changes and improves access to a full range of contraception, including long-acting reversible contraceptives.
Farmer earned a Bachelor of Science degree in Business Administration from the University of Delaware in 1997.
The DPH Bulletin – February 2024 Page 2 of 5
Tina Farmer
21
Awele Maduka-Ezeh

DPH and partners invite employers to March 14 diabetes and obesity program
The Division of Public Health (DPH) and its partners invite employers to attend a free in-person program about diabetes and obesity. “Culture of Health Boot Camp – Roadmap for Employers to Address Diabetes and Obesity in the Workforce” will be held on March 14, 2024 from 8:30 a.m. to 12:00 p.m. at the Modern Maturity Center, 1121 Forrest Avenue, Dover, DE 19904.
Presenters will share how addressing diabetes and obesity can improve employee health, productivity and retention, and reduce health care costs. Participants will gain access to resources to support well-being programming and benefit offering and create an action plan to build a culture of health. The webinar is sponsored by DPH; the Greater Philadelphia Business Coalition on Health; and the Society for Human Resources Management (SHRM), Delaware State Council. The program is approved for 2.5 SHRM Professional Development Credits (PDCs).
Tribute honors Office of Animal Welfare for 10 years of service to Delawareans
The 152nd General Assembly honored the Office of Animal Welfare’s (OAW) 10 years of service with House Concurrent Resolution 81, sponsored by Rep. Kimberly Williams (D-19) and Sen. Jack Walsh (D-9). OAW was created within the Division of Public Health (DPH) to protect the health, safety, and welfare of companion animals and to centralize services.
“For 10 years now, the Office of Animal Welfare has worked to improve the quality of life for pets and people across our state and their efforts deserve recognition,” Rep. Williams said. “Through their collaboration with local animal shelters, rescues, and the veterinary community, they have not only made Delaware a more humane and compassionate place, but have also played a pivotal role in making our state the first no-kill animal shelter state.”
According to OAW director Christina Motoyoshi, who has been with the office since 2014 and director since 2018, OAW launched a statewide Lost and Found Pet Registry; implemented training and certification regulations for animal welfare officers; established Delaware Animal Services (DAS), an enforcement unit to safeguard pets and the public; and expanded the State Spay & Neuter Program to reduce animal homelessness.
Two of the biggest health concerns facing Delaware’s workforce, diabetes and obesity, are major cost drivers for employers. Among Delaware adults, 12% have diabetes and 13% have prediabetes, at an annual cost of $1.1 billion. Among U.S. adults, 37 million have diabetes and 96 million have prediabetes, at an annual combined cost of $403 billion.
The reported obesity rate for adults for U.S. and Delaware adults is 34%. The nationwide direct medical cost of obesity is $173 billion.

To register, visit http://tinyurl.com/Culture-of-Health-Boot-Camp
Suspected influenza claims six lives
Six suspected flu-related deaths for the 2023-2024 influenza season have occurred since December, according to the Division of Public Health (DPH).
All decedents were over the age of 55 with one reportedly up to date on their flu vaccination. Cases were statewide.
Getting the annual flu vaccine is important for all people ages 5 months and older to prevent serious illness, hospitalization, and death. DPH reminds the public that it is not too late to get vaccinated against the flu. Visit flu.delaware.gov and click on the Find A Flu Shot Near You button for flu vaccination locations.
The DPH Bulletin – February 2024 Page 3 of 5
The Division of Public Health’s (DPH) Office of Animal Welfare was honored for its 10 years of service by House Concurrent Resolution 81, sponsored by Rep. Kimberly Williams (D-19) and Sen. Jack Walsh (D-9) Pictured from left to right, front row: OAW Chief Mark Tobin, DPH Director Steven Blessing, Rep. Williams, Sen. Walsh, and Rep. Sherry Dorsey Walker. Second row: Melody Purdy, OAW program coordinator, OAW Deputy Director Joanna Miller, and Rep. Bryan Shupe. Third row: OAW Director Christina Motoyoshi, Officer Kelly Gorczyk, Lt. Jessica Kramer, Officer Jenelle Leib, and Lt. Tammy Moseley Top row: Captain Philip Dixon, Captain Rebecca Stratton, Sgt. Andrew Price, and Captain Ervin Smith Photo provided by Alexis Wrease/Delaware Senate.
22 Delaware Journal of Public Health - March 2024

DHMIC’s Health Equity Champion award nominations due March 17
The 18th Delaware Healthy Mother and Infant Consortium (DHMIC) Summit will be held on April 17, 2024 from 8:30 a.m. to 4:00 p.m. at the Chase Center at the Riverfront, located at 815 Justison Street, Wilmington, DE 19801.
The summit convenes leaders in the area of family health to discuss new approaches that enhance the health of women, children, and families of all ages.
The event is free. For more information and to register, visit https://dethrives.com/dhmic.
Two Kitty Esterly, MD Health Equity Champion awards will be presented to an individual and an organization that advances equity by working tirelessly for the well-being of mothers and children in Delaware and for the health of the community. Dr. Esterly, Delaware’s first neonatologist, was an active voice, champion, and advocate on behalf of women, infants, and children. Nominate until March 17 at https://dethrives.com/dhmic/health-equity-awards
Tobacco Prevention Conference scheduled for May 8 in Newark
The Division of Public Health’s Tobacco Prevention & Control Program and the American Lung Association will host a Tobacco Prevention Conference on May 8, 2024 at the University of Delaware's Clayton Hall Conference Center, located at 100 David Hollowell Drive in Newark, Del.
The conference will share tobacco prevention and cessation topics on health equity, behavioral health, and community partnerships. It will benefit those who support current tobacco prevention programs, health care and behavioral health providers, community organizations, education administrators, student health staff, and those in public health.
Once established, registration information will be posted on healthydelaware.org.
March 10, 2024 is National Women and Girls HIV/AIDS Awareness Day
National Women and Girls HIV/AIDS Awareness Day is March 10, 2024. The observance raises awareness about the impact of the human immunodeficiency virus (HIV) on women and girls. The Centers for Disease Control and Prevention (CDC recommends HIV testing for everyone between the ages of 13 and 64. Everyone should be tested for HIV at least once and more often if they are at high risk of getting it. Both sexual partners should find out their HIV status even if they are having sex only with each other.
HIV can be prevented by not having sex, never sharing needles, and using condoms the right way every time you have sex. According to the CDC, the HIV prevention medicine PrEP (pre-exposure prophylaxis) is highly effective at preventing HIV from sex or injection drug use when taken as prescribed. In emergency situations, post-exposure prophylaxis (PEP) prevents HIV if it is started within 72 hours of a recent possible exposure.
Individuals with HIV can take antiretroviral pills or shots to lower their viral load so a test cannot detect it. If they keep an undetectable viral load, they can live long, healthy lives and prevent transmission to others through sex or sharing needles, syringes, or other injection equipment, and from mother to child during pregnancy, birth, and breastfeeding.

For social media graphics regarding National Women and Girls HIV/AIDS Awareness Day, visit
https://www.cdc.gov/hiv/library/awareness/nwghaad. html. Let’s Stop HIV Together campaign resources for women are available in English and Spanish. HIV screening and prevention tools and guidelines for clinicians are available at
https://www.cdc.gov/him/clinicians/index.html
A related observance, National Youth HIV Awareness Day, is April 10.
The DPH Bulletin – February 2024 Page 4 of 5
23
By March 4, State seeks public comment on proposed regulations
The Division of Public Health seeks public comment on the following regulations by March 4:
• A proposed new 4306 Stroke System Regulation
• Re-proposed revisions to Regulation 4459 Lead Based Paint Hazards
• Re-proposed revisions to the 4459A Regulations Governing the Childhood Lead Poisoning Prevention Act.
The lead poisoning prevention regulations are being re-proposed due to substantive changes resulting from the public comment received between December 1, 2023 and January 8, 2024
Copies of the proposed regulations are available for review in the February 1, 2024 issue of the Delaware Register of Regulations at http://regulations.delaware.gov or by calling DPH at 302-744-4700
Until the close of business on March 4, 2024, public comments will be accepted in written form via email to DHSS_DPH_regulations@delaware.gov, or by U.S. mail to:
Vicki Schultes, Hearing Officer
Division of Public Health 417 Federal Street Dover, DE 19901
The Delaware Department of State, Division of Professional Regulation is seeking public comment on behalf of the Board of Dentistry and Dental Hygiene on its proposed revised regulations that clarify that limited licensees are subject to general supervision while training and eliminate redundancies in the Supervision regulations. Read the proposed regulations in the February 1, 2024 issue of the Delaware Register of Regulations at http://regulations.delaware.gov. Select the HTML option, then “proposed regulations”.
The Board will hold a public hearing on the proposed rule change on March 21, 2024 at 3:00 p.m. virtually and at the second floor Conference Room A in the Cannon Building, located at 861 Silver Lake Boulevard, Dover, DE 19904. Written comments should be sent to Jennifer Witte, Administrator of the Delaware Board of Dentistry and Dental Hygiene at the same address. Written comments will be accepted until April 5, 2024.

Published in 2023

The Division of Public Health, Health Systems Protection Section published the following reports in 2023:
1. State of Delaware Public Drinking Water Annual Compliance Report and Summary for 2022
2. Capacity Development Program Report to the Governor, 2023
The Office of Infectious Disease Epidemiology published the Delaware Healthcare-Associated Infections 2022 Annual Report.
DPH shares more than 360 fact sheets
Three Division of Public Health (DPH) offices posted new and updated fact sheets to its Fact Sheets A-Z page The site features more than 360 fact sheets to help the public, health care providers, and others understand public health subjects.
The Office of Preparedness updated its 86 fact sheets available in these formats: public information, Frequently Asked Questions (FAQs), medical, and EMS. Topics include Sheltering in Place, Isolation and Quarantine, natural threats such as brucellosis and tularemia, and man-made threats such as ammonia and chlorine.
The Health Systems Protection Section’s 127 fact sheets address bedbugs, cockroaches, flooded septic systems, heating oil spills, mold remediation, private drinking water tests, and more. Chromium, acetaldehyde, and vinyl chloride are examples of the section’s chemical FAQs.
The Office of Infectious Disease Epidemiology’s 109 FAQs include measles, rubella, and sexually transmitted infections, plus a new set on tickborne diseases. School nurses can share FAQs on conjunctivitis, hand washing, head lice, pinworm, ringworm, scabies, and strep throat with parents, guardians, and personnel.
Reach DPH’s Fact Sheets A-Z page at https://www.dhss.delaware.gov/dph/factsheetsaz.html
The DPH Bulletin – February 2024 Page 5 of 5
24 Delaware Journal of Public Health - March 2024


chwCORE.org CERTIFICATION, OPPORTUNITIES & READINESS FOR EMPLOYMENT COMMUNITY HEALTHWORKER TRAINING PROGRAM This project is managed by the Public Health Management Corporation and supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $3 million with 0 percentage nanced with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the o cial views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov. chwCORE Training Program is: Visit chwCORE.org to sign up as a partner. If you have more questions email us at chwcore@gmail.com Fully accredited by the Pennsylvania Certification Board (PCB) Offering stipends to support trainee participation Providing peer-learning sessions for ongoing trainee growth Self-paced and online to fit any trainee’s schedule Partner with chwCORE to train and grow the community health workforce! Serving Pennsylvania and Delaware chwCORE.org 25
Social Workers, Burnout, and Self-Care: A Public Health Issue
Michelle Ratcliff, D.M.F.T., L.S.W.
Social Work Department, Delaware State University
ABSTRACT
Social workers have a complex role of providing social services with compassion and empathy while working tirelessly, enduring burnout at some level in their careers. The consequences of burnout can be harmful to workers, the people who they service, their families and careers. This public health issue is impacting social workers globally and is the impetus in exploring burnout to assist social workers with identifying the stressors that can lead to burnout and formulate plans to alleviate stress by using self-care tools. Social workers can use these tools to help prevent future stressors from their involvement in providing services to individuals, families, groups, communities, and organizations. This paper reviews the literature that explores burnout of social workers and provides self-care tools to use in daily practice.
INTRODUCTION
Social work is a highly stressful career and is notorious for creating burn out from the many tasks and services rendered, political and community demands, client advocacy, and administrative and funding issues that affect their work. Careers in social services, along with many other helping professions, have been identified as a stressinducing, time-consuming profession. The stress that is produced while providing social services is well known for many helping professionals; however, many have felt that it is their mission to provide services regardless of the stressors or potential for burnout.1 The accumulation of stress and burnout have been a complaint of many helping professionals in various fields and is widely acknowledged to play a key role in work retention and turnovers.2 Although many have found their careers to be rewarding, the ability to complete daily tasks has been proven to be cumbersome. In surveying the literature, it has been recognized that social workers may experience higher levels of stress and resulting burnout than comparable occupational groups.3 It is an occupational hazard that is a critical health issue affecting many social service providers.3 The literature provided will explore the stress that leads to burnout and the implementation of self-care practices that can be used to combat this public health issue that could ultimately affect the care that is provided to consumers.
With a constant demand for social services, social workers often find themselves overwhelmed, overworked, and emotionally fatigued. Like healthcare workers, social workers are susceptible to burnout. Due to services in stressful and complex situations, social workers are more at-risk for chronic stress resulting in burnout. Burnout is often associated with increased levels of absenteeism, higher turnover rates, and negative work attitudes.4 Additionally, literature indicates that social workers in Western countries have reported higher levels of stress, which attributed to higher levels of sicknesses among workers.4
BURNOUT
Burnout is defined as a psychological condition that results from chronic stress related to working with people.5 From literature it has been observed that burnout is a buzz word for many personal and social problems. It has been researched since the mid- 1970’s, and is a widespread and continuing threat in many humanservice-related fields.5 Burnout causes job dissatisfaction, job withdrawal, absenteeism, and turnover.5 Herbert J Freudenberger initially discovered and evaluated burnout in health and social services fields.6 He defined burnout as a display of negative feelings felt by workers in helping professions due to long-term exhaustion, diminished interest, and low feelings of personal satisfaction at work.7 It was later defined as “stress without let-up,” a sense of negativity building up while performance in many areas of your life is breaking down.8
Freudenberg suggested that high achievers were more likely to suffer from burnout and suggested that there are key factors that contribute to the person that suffers from burnout, such as environmental stress, personality, and individual response to stress.6,7 He suggested that burnout is the result of perfectionists who fail to delegate authority and who also strive hard due to constant pressure, performing at an elevated level of stress and tension.6,7 He also pointed out an important fact of childhood incongruence in the family, in which a sufferer of burnout can be the result of an attempt to live up to a role provided by an overachieving parent. Further suggesting that those that come from an impoverished background can burn out because of their desire to succeed.6 It is also believed that burnout can be a result of someone who works extremely hard, is stressed, and sets high personal standards of achievement.7
Burn out is divided into three different scopes; which are emotional exhaustion, where the person becomes emotionally drained; depersonalization, where pessimism and withdrawal can be a result; and a low sense of personal accomplishment.6,7 Burnout is also defined as “emotional collapse or breakdown that sometimes comes as the result of chronic stress”9 regarding their job-related roles and responsibilities. Freudenberg further suggests that the lack of recognition of efforts to attain achievement exasperates the condition, especially if one has elevated level of expectations, burnout can be a result.6,7
Doi: 10.32481/djph.2024.03.05
26 Delaware Journal of Public Health - March 2024
SYMPTOMS OF BURNOUT
There are many physical symptoms of burnout which are identifiable, while there are many which are emotionally hidden for fear of losing employment or being labeled. It is characterized by the state of extreme physical, emotional, and mental exhaustion, demonstrated by a decrease in motivation, and performance.5,10 It can eventually take over the body and mind resulting in physical signs such as: headaches, stomach aches, cold and flu viruses, sleeplessness, chest pain, sweaty palms, and fear of losing control and dermatological problems.5,10 Poor concentration, instability, cynicism, anxiety, and frustration are also demonstrated. Additionally, workers who experience job burnout experience psychological stress, professional dissatisfaction, lack of motivation, emotional detachment, and feelings of emotional overload and exhaustion.5 Job burnout has caused many to drop out of work and detach from their workplace where the worker is physically present but emotionally absent. For people who stay on the job, burnout leads to lower productivity and impaired quality of work.7 As burnout diminishes opportunities for positive experiences at work, it is associated with decreased job satisfaction and a reduced commitment to the job or the organization.5
Workers suffering from burnout exhibit symptoms that disrupt all levels of their beings, such as psychological, physiological, emotional, interpersonal, and spiritual. Physically, burnout can manifest in forms such as the susceptibility of catching colds and viruses, having muscular tension, irritability, and chronic exhaustion.5,7 Burnout can be displayed as depression, anxiety attacks, and lack of creativity, loss of enjoyment, irritability, mood swings, suicidal ideations, cynicism, and perfectionism.5,7,10 The consequences of burnout can be harmful to the workers, the people who they serve, their families and their employment. Additionally, interpersonal problems in marriage can cause higher rates of divorce and adultery due to burnout.11
FAMILY IMPACT OF BURNOUT
Burnout is detrimental to the family as a unit and is multifaceted. Several people attempt to hide their unhappiness and frustration; however, most families can often see beyond the charade and see the fatigue, withdrawal, and discouragement that their loved one is experiencing. It can be a costly situation to the individual, their family, and their career.6 Unfortunately, the cost of burnout and the lack of self- care affects everyone that encounters the exhausted social worker. Freudenberger found in four case examples that it is important for the therapist to untangle the family’s views and management of stress.6 He examined their responses by reviewing their changes during a period of burnout. He found that family therapy could help a family experiencing burnout if the factors contributing to the stressful situations are clearly defined and the person suffering from burnout is not blamed for the families’ problems.6
Many social workers have chosen the field in social services and helping professions due to the concerns and problems that they have experienced within their own families, which can add to the stress of provision of services. Burnout involves both personal and situational factors, and it is important that the
root of the issues are identified in order to combat burnout.7 Sometimes the incongruity of the job’s roles and the personality of the worker are at fault for the stressful situations.5,7,10 Or the ethical dilemmas between personal and agency views can lead to the issues with burnout.7 In a study of the effects of burnout and work stress on family relationships, it was found that social workers who experienced increased burn out were likely to also demonstrate episodes of depression, anxiety, irritability, and lower marital satisfaction.11
THE MASLACH BURNOUT INVENTORY (MBI)
The popular interest and study of the dynamics associated with burnout has stimulated the creation of several burnout inventories. The Maslach Burnout Inventory (MBI) is the most widely used instrument on burnout within research and has been widely used with helping professionals. There are three initial tools that were produced for human services, educators, and general professionals. However, others have adapted the Maslach Burnout Inventory to fit their own profession, with permission. The initial research regarding burnout was accomplished by completing surveys, questionnaires, and field interviews of staff in various human services fields.10 In their findings, Maslach, Jackson, &Leiter indicated that burnout is the key contributor in the worsening of quality of service and care of staff, staff turnover, absenteeism, and low morale. Their findings also found that because of burnout, staff’s personal and interpersonal lives were deteriorating.10 There were incidences of drug and alcohol use, separation and divorce, physical dysfunction and exhaustion and insomnia.5,7,10 Due to these findings and their work on further defining the concept of burnout, Maslach created an instrument, the Maslach Burnout Inventory (MBI) to assess the three phases of burnout.5,10 The tool consists of 22 items divided into 3 sections with items written in statements of personal feelings and attitudes using a 7- point scale from 0 (never) to 6(everyday). MBI specifications according to Maslach et al. (1997) the MBI should consist of 22 items, which contains 9 items for emotional exhaustion, 5 items for depersonalization, and 8 items for personal accomplishments. The instrument is timed and must be completed privately and in 10-15 minutes. The information gathered must be kept confidential and the respondents should not be sensitized to the issue of burnout and should not know that the tool is a burnout measure.10
One of the largest studies of burnout among social workers was conducted in the UK. The workers completed the Maslach Burnout Inventory which assessed their propensity for burnout. The study was conducted by Cooper12 with 1,359 frontline social workers of which 70% had six or more years of experience. The social workers in the study worked in all areas of the profession including child welfare, gerontology, and mental health.12 In most of the social workers who responded, the study found 73% of the respondents had elevated levels of emotional exhaustion. One and four (26%) reported highlevel of depersonalization. Which could cause social workers to become hardened towards the provision of services. However, there were remarkably elevated levels of personal accomplishment (91%) who also felt positively about their influence as service providers.12
27
SELF-CARE
Evident with many social workers, the neglectful push to exhaustion leading to burnout has hindered the opportunity for self-care practices. For many years, from this author’s observations, self-care has been a fad, a topic of discussion in trainings and workshops and a hashtag written by millennials. Most critical to social work practice is the application of selfcare practices. The implementation of these practices is widely recognized and can serve as a means of empowerment and personal well-being in ways that are deemed constructive and positive.13 In a culture that glorifies stress, self-care is a way to find balance while serving others and should be given sincere consideration. This author believes it is an action in which a person intentionally decides that they will participate in activities that will create a peace of mind, tranquility of soul and rejuvenation of body while serving others, working hard in their profession or enduring hardship. It challenges people to care for themselves first before they could care for others while taking the initiative to self – manage and self- correct.13 It is also an opportunity to give to self and also receive care and support from others by realizing the need for assistance from others.
SELF-CARE TOOLS
Mindfulness
Mindfulness, developed from the Buddhist traditions, is commonly defined as a way of paying attention, being on purpose and in the present moment, nonjudgmentally.14 Although adapted from the Buddhist meditative traditions, is a term used to describe a practice of meditative awareness.14 It has been shown to be effective in psychotherapy and as a self -care practice for mental health therapists asserting that mindfulness teaches awareness to deepen groundedness, presence and connection with others and the world, further explaining that self-care is essential to mental health practitioner training and professional efficacy.14 It is a simple but not easy practice that encourages moment to moment experiences, analyzing thoughts and emotions. Sitting in silence is a way to incorporate mindfulness as a form of relaxation, following breaths, Mindfulness can be experienced simply by sitting in silence allowing an opportunity to follow each breath as a form of relaxation, to reframe feelings and celebrate empathy. These practices can impact the level of tolerance for work life issues and difficulties.
In a Mindfulness- based social work and self-care (MBSWSC) research study conducted by Maddock, McGuigan & McCusker,15 on stress, burnout, anxiety, and depression, found that their MBSWSC program was a useful program that improved the mental health and well-being outcomes for social workers. The study’s findings also suggest that social workers who use the MBSWSC program are more likely to experience less burnout and improved mental wellbeing.15
Yoga
Yoga, a mind body intervention, started in India over 4000 years ago. This discipline is one in which asceticism and meditation meet with spirituality, the experience of spirituality, and the nature of existence. According to Chong, Tsunaka, Tsang Chan and Wai Ming,16 the term yoga comes from the Sansskrit word Yui, which means to unite or to yoke. To unite the mind, body and spirit is the goal of this practice.16 Although there is a spiritual element
to the discipline of Yoga, many have used it as an opportunity to enhance physical postures also called “asanas,” control breathing “ipranayama,” and meditation “dhyana”. Chong et al., defines the five traditional forms of yoga: gyan, karma, bhakti, raja and hatha yoga.16 The traditional form that most Westerners use for stress reduction, stretching, breathing and meditation is hatha yoga. This form of yoga has been proven to reduce signs of psychological stress. It is also seen as a form of mind – body therapy for many clinical disorders and conditions, as well as for maintenance and disease prevention.16
Yoga has been proven across many scenarios as an intervention that can help alleviate stress, decrease physiological disorders and conditions, and prevent burnout. Social workers and helping professionals can use a yoga way of life to get to the root of their stress and learn how to change their emotional, psychological, and spiritual way of thinking to better be able to process their stress and alleviate it while serving others.15 It is found that yoga helps a person identify their stressors and the root of their stress which makes them more aware of their situation and allows better responses.15 The results of this experiment proved that by incorporating yoga into their life, it can significantly reduce job burnout of managers.
CONCLUSION
Encouraging self-care practices should be the responsibility of administration in all social work professions. Implementing opportunities for staff to indulge in self-care practices in social work practice is vital for the continued opportunity to provide services effectively and efficiently. Many social workers have endured years of compassion fatigue, vicarious trauma, and burnout. For continued provision of services to individuals, families, groups, communities and organizations, it is absolutely necessary to encourage workers to care for themselves and understand the signs and symptoms of burnout. The tools presented may not be effective for many social workers; however, it is the responsibility of the worker to ensure that they are mindful of their effectiveness and adequately monitor whether they are deteriorating because of the services that they are providing. Ms. Ratcliff may be contacted at mratcliff@desu.edu
REFERENCES
1. Malka, M., Kaspi-Baruch, O., & Segev, E. (2021). Predictors of job burnout among fieldwork supervisors of social work students. Journal of Social Work, 21(6), 1553–1573.
https://doi.org/10.1177/1468017320957896
2. Lloyd, C., King, R., & Chenoweth, L. (2002). Social work, stress and burnout: A review. Journal of Mental Health (Abingdon, England), 11(3), 255–265.
https://doi.org/10.1080/09638230020023642
3. Lizano, E. L., & Mor Barak, M. E. (2015). Job burnout and affective wellbeing: A longitudinal study of burnout and job satisfaction among public child welfare workers. Children and Youth Services Review, 55, 18–28.
https://doi.org/10.1016/j.childyouth.2015.05.005
4. Schraer, R. (2015). Social workers too stressed to do their job according to survey. Community Care. Retrieved from http://www.communitycare.co.uk/2015/01/07/stress-stopping-jobsocial-workers-say/
28 Delaware Journal of Public Health - March 2024
5. Maslach, C., & Leiter, M. P. (2016, June). Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry, 15(2), 103–111.
https://doi.org/10.1002/wps.20311
6. Freudenberger, H. J. (1984). Burnout and job dissatisfaction: Impact on the family. In Perspectives on Work and Family, J.C. Hammer & S.H. Cramer, Eds. Rockville, MD: Aspen.
7. Freudenberger, H. J. (1986, Jul-Sep). The issues of staff burnout in therapeutic communities. Journal of Psychoactive Drugs, 18(3), 247–251.
https://doi.org/10.1080/02791072.1986.10472354
8. Nugent, P. M. S. (2013). Psychology Dictionary. What is burnout? Retrieved on July 27, 2017. From www.https://psychologydictionary.org/burnout/
9. Lee, C., & Fredrickson, K. (2012). That their work will be a joy: Understanding and coping with the challenges of pastoral ministry. Wipf and Stock Publishers.
10. Maslach, C., Jackson, S., & Leiter, M. (1997). Maslach burnout inventory. 3rd ed. Palo Alto: CA. Consulting Psychologists Press
11. Jayaratne, S., Chess, W., & Kunkel, D. (1986). Burnout: Its impact on child welfare workers and their spouses. Social Work, 31, 53–59.
https://doi.org/10.1093/sw/31.1.53
12. Cooper, J. (2015, July 14). Exhausted social workers on the edge of burnout but still achieving positive changeCommunity Care
https://www.communitycare.co.uk/2015/07/14/social-workers-on-theedge-of-burnout-but-still-achieving-positive-changes/
13. Lee, J. J., & Miller, S. E. (2013). A self-care framework for social workers: building a strong foundation for practice. Families in Society, 94(2), 96–103.
https://doi.org/10.1606/1044-3894.4289
14. Sultan, N. (2018). Embodied Self-Care: Enhancing awareness and acceptance through mindfulness-oriented expressive writing self-disclosure. Journal of Creativity in Mental Health, 13(1), 76–91.
https://doi.org/10.1080/15401383.2017.1286277
15. Maddock, A., McGuigan, K., & McCusker, P. (2023). A randomised trial of Mindfulness-based Social Work and SelfCare with social workers. [PubMed]. Current Psychology (New Brunswick, N.J.), 42(11), 9170–9183.
https://doi.org/10.1007/s12144-023-04410-w
16. Chong, C. S., Tsunaka, M., Tsang, H. W., Chan, E. P., & Cheung, W. M. (2011, Jan-Feb). Effects of yoga on stress management in healthy adults: A systematic review. [PubMed]. Alternative Therapies in Health and Medicine, 17(1), 32–38.
https://pubmed.ncbi.nlm.nih.gov/21614942

YOURSELF
You try to quit, but there are triggers everywhere you turn. You feel lost. Trapped. But you’re not alone. The Delaware Quitline has helped thousands escape their addiction and get on the path to living tobacco-free. Call 1-866-409-1858 or visit QuitSupport.com for free counseling, cessation aids, and medications to help you quit for good. 29
FREE
FROM TOBACCO
Community Partnership to Co-Develop an Intervention to Promote Equitable Uptake of the COVID-19 Vaccine Among Pediatric Populations
Paul T. Enlow, Ph.D.
Center for Healthcare Delivery Science, Nemours Children’s Hospital Delaware; Department of Pediatrics, Sidney Kimmel Medical College, Thomas Jefferson University
Courtney Thomas, M.S.
Center for Healthcare Delivery Science, Nemours Children’s Hospital Delaware
Angel Munoz Osorio, B.S.
Center for Healthcare Delivery Science, Nemours Children’s Hospital Delaware
Marshala Lee, MD, M.P.H.
Harrington Value Institute Community Partnership Fund, ChristianaCare Health System
Jonathan M. Miller, M.D.
Inclusion, Diversity, Equity, and Alignment, Nemours Children’s Health; Department of Pediatrics, Sidney Kimmel Medical College, Thomas Jefferson University
Lavisha Pelaez, M.P.H.
Inclusion, Diversity, Equity, and Alignment, Nemours Children’s Health
Anne E. Kazak, Ph.D., A.B.P.P.
Center for Healthcare Delivery Science, Nemours Children’s Hospital Delaware; Department of Pediatrics, Sidney Kimmel Medical College, Thomas Jefferson University
Thao-Ly T. Phan, M.D., M.P.H.
Center for Healthcare Delivery Science, Nemours Children’s Hospital Delaware; Department of Pediatrics, Sidney Kimmel Medical College, Thomas Jefferson University
ABSTRACT
Objective: To describe the process of engaging community, caregiver, and youth partners in codeveloping an intervention to promote equitable uptake of the COVID-19 vaccine in non-Hispanic Black (Black) and Hispanic youth who experience higher rates of COVID-19 transmission, morbidity, and mortality but were less likely to receive the COVID-19 vaccine. Methods: A team of 11 Black and Hispanic community partners was assembled to codevelop intervention strategies with our interdisciplinary research team. We used a mixed-methods crowdsourcing approach with Black and Hispanic youth (n=15) and caregivers of Black and Hispanic youth (n=20) who had not yet been vaccinated against COVID-19, recruited from primary care clinics, to elicit perspectives on the acceptability of these intervention strategies. Results: We codeveloped five strategies: (1) community-tailored handouts and posters, (2) videos featuring local youth, (3) family-centered language to offer vaccines in the primary care clinic, (4) communication-skills training for primary care providers, and (5) use of community health workers to counsel families about the vaccine. The majority (56-96.9%) of youth and caregivers rated each of these strategies as acceptable, especially because they addressed common concerns and facilitated shared decision-making.
Conclusions: Engaging community and family partners led to the co-development of culturally- and locallytailored strategies to promote dialogue and shared decision-making about the COVID-19 vaccine. This process can be used to codevelop interventions to address other forms of public health disparities. Policy Implications: Intervention strategies that promote dialogues with trusted healthcare providers and support shared decisionmaking are acceptable strategies to promote COVID-19 vaccine uptake among youth from historically underserved communities. Stakeholder-engaged methods may also help in the development of interventions to address other forms of health disparities.
FUNDING
This work was supported by NIGMS 3U54GM104941 sub-award to PTE and TLP.
ACKNOWLEDGEMENTS
We thank Kara Odom Walker, MD, MPH; Rita Landgraf; and Neil Rellosa, MD for their mentorship and guidance on this project. We are also grateful for the passionate support from our community partners (Rev. Rita Paige, La Vaida Owens White, Zorah Rothwell, Anaya Patterson, The Warehouse, Alicia Dominguez, Francisca Moreno, Susana Aranda, Ines Carino, Fatima Kaba, Dayanara Flores, Terri Price, Jason McCall, Tabita Ares, and Raye Jones Avery), health care partners (staff
at the Nemours Milford, Seaford, Becks Woods, and Foulk Road primary care offices; the Care Management, Community Engagement, and Data Analytics teams of the Nemours Value Based Services Organization), the Nemours Center for Health Delivery Innovation, and Nemours Marketing.
DATA STATEMENT
The data are available from authors upon reasonable request.
INTRODUCTION
Youth who identify as non-Hispanic Black (Black) or Hispanic have higher rates of COVID-19 morbidity and mortality than non-Hispanic White (White) youth.1,2 Despite the safety and
Doi: 10.32481/djph.2024.03.06
30 Delaware Journal of Public Health - March 2024
efficacy of COVID-19 vaccines,3–5 there are universally lower vaccination rates among Black youth compared with White youth2,6 and lower vaccination rates for Hispanic youth in some states compared with White youth.6 Furthermore, COVID-19 vaccination rates across the nation have plateaued.6 To protect underrepresented pediatric populations from the impact of COVID-19, it is imperative to promote equitable uptake of COVID-19 vaccines.
Inequitable COVID-19 vaccine uptake is due to a combination of factors including vaccine hesitancy7 and systemic barriers to accessing the vaccine.8,9 Prior work highlighted that caregivers of Black youth and youth from socioeconomically disadvantaged communities were less likely to intend to vaccinate their child against COVID-19 and viewed the vaccine as less safe and effective.10–12 Prior work also demonstrated the importance of who communicates with families about the COVID-19 vaccine, with parents of all sociodemographic backgrounds viewing their child’s pediatrician as the most trusted source of information.11,12 Finally, lower digital literacy and language barriers may make it difficult for families to schedule appointments to vaccinate their children against COVID-19.8 Therefore, interventions to promote equitable COVID-19 vaccine uptake in pediatric populations should increase awareness about the benefits and safety of the COVID-19 vaccine and decrease barriers to accessing the vaccine.13 Interventions to reduce racial and ethnic disparities in COVID-19 vaccine uptake in pediatric populations are lacking. Multicomponent, dialogue-based interventions that are tailored to community-specific concerns have reduced hesitancy around influenza and human papillomavirus vaccines.14 Successful interventions also incorporated educational materials tailored to communities’ concerns,15,16 stories from trusted persons,15,17 motivational interviewing,18,19 and community health workers.20,21 The current study aimed to develop a multicomponent intervention to equip trusted messengers with the tools and resources necessary to promote COVID-19 vaccine uptake among Black and Hispanic pediatric populations, working with community and patient partners to ensure the intervention was culturally-tailored and community-informed.22,23
OVERVIEW OF CO-DEVELOPMENT PROCESS
Our process for codeveloping and refining the intervention (Figure 1) was informed by models proposed by Leask et al.24 and Wallerstein et al.25 Throughout the co-development process, we utilized strategies from New Mexico’s Engage for Equity Promising Practices Guide,26 a set of practices for conducting community-based participatory research that has empirical support27; has been applied to socioeconomic, racial, and ethnic disparities in COVID-1928; and demonstrated utility in developing and disseminating culturally-tailored, health promotion interventions to community partners.29 We divided our process into two phases. In Phase 1, we worked with community partners to codevelop intervention strategies. In Phase 2, we elicited feedback on these strategies from youth who had yet to get the COVID-19 vaccine and/or their caregivers, which we then used to iteratively refine the intervention. As these phases were sequential, we first present the methods and results of Phase 1 and then the methods and results of Phase 2. The Institutional Review Board approved the procedures for this project.
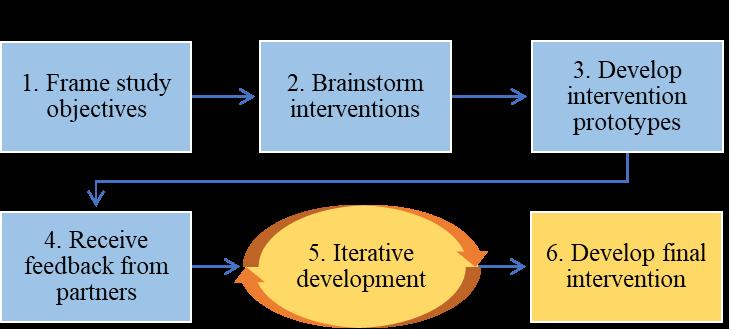
Positionality Statement
We acknowledge that the racial, ethnic, socioeconomic, and educational backgrounds of the research team influence the research being conducted. The research team for this project is demographically and professionally diverse. One author (ML) is active in the community, advocating for efforts to promote health and well-being of community members across Delaware. We acknowledge that our professional and personal backgrounds may affect how we approached the process of codeveloping interventions and the interpretation of findings. The research team worked to develop culturally sensitive research methods, had regular discussions to ensure the study was guided by their cultural knowledge, and worked closely with community partners (described in more detail in the next section) to incorporate the community’s perspective when codeveloping the intervention and interpreting findings.
PHASE 1: CO-DEVELOPMENT OF INTERVENTION WITH COMMUNITY PARTNERS
Phase 1 Methods
We employed steps 1-4 (Figure 1) to co-develop interventions in both English and Spanish.
Identifying Partners
We worked with an advisory committee consisting of health care and policy professionals with connections to Black and Hispanic community groups and expertise in community engagement to identify community partners, with consideration of community history/context and partner capacity, to develop the proposed intervention. The advisory committee helped identify 16 potential partners from the Black and Hispanic communities, including leaders from local youth groups, religious organizations, and local community advocacy groups. These potential partners were then contacted via email; 10 partners representing Black (n = 7) and Hispanic (n = 3) communities initially agreed to serve as a community partner. The final group represented youth leaders from youth or community groups (n = 4), religious leaders (n = 2), advocacy groups for communities of color (n = 3), and a community health worker (n = 1). After the first meeting, we sought to include more input from the Hispanic communities. Therefore, at the recommendation of our advisory committee, we recruited a parent who identified as Hispanic and a leader from a community center serving Hispanic families. This resulted in a total of 12 community partners by the third meeting.
Figure 1. Process for Co-Developing Intervention
31
Engaging Partners
We engaged partners across eight meetings held approximately once per month. Meetings were held by video conference and at two different times each month (over a lunch hour and after work hours) to facilitate participation. In addition, we used practices from the New Mexico’s Engage for Equity Promising Practices Guide to develop shared values, integrate historical and cultural contexts, and promote productive dialogue. We utilized parts of Wallerstein and colleagues’ Community Engagement Survey to assess synergy of the partnership after meetings.30 Community partners used a 6-point Likert scale (ranging from 1 to 6) to rate the synergy of the partnership, with higher scores indicating greater synergy. Engagement practices were refined, as needed, based on results from this survey.
Phase 1 Results
The objectives of the first meeting were to develop a shared vision for the intervention. Community partners shared that they responded well to information that came from trusted sources and addressed their specific concerns about the vaccine. The community partners also stressed the importance of targeting both youth and caregivers because many caregivers involve their child in the decision about whether to get vaccinated. Finally, youth and adult community partners shared how a dialogue with a trusted health care provider positively influenced their decision to get the vaccine. Feedback from community partners was distilled into themes (Table 1). Ten (100%) community partners attended and six (54.5%) completed the community engagement survey following the first meeting. The average score was 4.90 (standard deviation [SD] = 1.11), indicating good levels of engagement. In open-ended responses, community partners said that they wanted to hear more from the youth leaders. In response to this, during subsequent meetings, facilitators purposefully elicited input from youth leaders.
During meetings 2 and 3, we gathered feedback on pre-existing informational handouts and videos developed by other hospitals, public health departments, and outreach organizations. The community partners noted that, although they liked the content of the informational handouts and videos, it was important to employ local families and physicians to deliver the messages. The community partners also felt that the informational handouts could be tailored to local communities’ questions and concerns. Finally, the community partners suggested that handouts and
posters be less wordy and use appealing imagery featuring Black and Hispanic youth. Ten (91%) community partners attended the second meeting, and nine (75%) community partners attended the third meeting. Three partners (27.3%) completed the community engagement survey after the third meeting; the average score on the community engagement survey was 4.93 (SD = 1.22), indicating that levels of partner engagement among respondents remained high.
Based on community partner input, we developed a multicomponent intervention. Each component used a different modality to address community beliefs and motivators identified by community partners, leverage trusted messengers like primary care providers and local families, and encourage dialogue with health care providers in the primary care setting, as recommended by our community partners (Table 1). These components included (1) community-tailored educational handouts and motivational posters for distribution at primary care clinics; (2) videos featuring local youth, families, and health care providers to address misinformation about COVID-19 vaccines and motivate youth to be vaccinated, which will be distributed by primary care clinics; (3) family-centered language to routinely offer the COVID-19 vaccine to improve access and encourage dialogue about the COVID-19 vaccine in the primary care setting; (4) training primary care providers on family-centered communication skills and motivational interviewing; and (5) employing community health workers to conduct outreach to patients and families about the COVID-19 vaccine within the primary care setting using other intervention components (e.g., sharing handouts and videos).
Intervention components were developed in English and then translated to Spanish using a third-party translation company. During meetings 4-8 (average attendance 54.8%), we planned how to create the intervention components (e.g., how to engage local youth to participate in video and photo shoots), solicited feedback about the intervention components developed by our team (for example, community partners asked us to incorporate more color and photos of youth on handouts), and discussed how to broadly disseminate the intervention to the community. Ratings of partner engagement slightly declined across meetings 4-8 (mean = 4.24; SD = 0.64). In open-ended responses, partners expressed that they wanted youth partners to participate more. To address this, research team leaders made efforts to elicit more feedback from youth during meetings.
Note: “X” indicates the theme(s) that each strategy addresses.
CommunityTailored Handouts & Flyers Videos Featuring Local Families Family-Centered Language to Offer Vaccines Communication Skills Training for Providers Community Health Workers Target youth and parents X X X X Feature local families and providers X X Tailor to community concerns and motivators X X X X X Leverage pediatric clinics X X X X X
Table 1. Themes from Community Partner Meetings
32 Delaware Journal of Public Health - March 2024
PHASE 2: EVALUATING ACCEPTABILITY AND INTERVENTION REFINEMENT
Phase 2 Methods
In Phase 2 (Figure 1; steps 5 and 6), we gathered perspectives from Black and Hispanic youth and caregivers on the acceptability of the intervention components via crowdsourcing, a form of online problem-solving with individuals with relevant experience and perspectives.31,32 We then revised components based on their feedback.
Recruitment
Potentially eligible caregivers and youth were identified by reviewing the electronic health records of all youth who had received care at one of the four participating primary care clinics in the past year. Caregivers of youth between 5 and 17 years old and youth between 12 and 17 years old were eligible to participate if (1) they identified as non-Hispanic Black or Hispanic, (2) they were proficient in English or Spanish, and (3) the youth, or the caregiver’s child, had not received any dose of the COVID-19 vaccine. Youth and their caregivers were encouraged to participate as a dyad, but they could participate individually. Purposive sampling was used to obtain a diverse sample regarding race, ethnicity, and primary language.
A total of 362 families (177 Black and 185 Hispanic) were approached by phone call, text, and/or email, of which caregivers and/or youth from 36 families enrolled (27 caregivers, 19 youth). Caregivers and youth completed an e-consent process with a trained research coordinator.
Data Collection
Once enrolled, caregivers and youth were emailed instructions to create a de-identified account on Yammer.com, a secure, online social network platform for qualitative data collection, and then assigned to one of four private groups (Caregiver/English, Youth/ English, Caregiver/Spanish, Youth/Spanish) so they could only see posts and responses for their group.
Between November 2021 and January 2022, we posted 10 study questions within each group (Table 2). Follow-up questions were developed, as needed, based on participant responses. No data were collected for post 1, which was designed to engage participants by allowing them to share why they joined the study. In post 2, youth and caregivers voted for a slogan to be featured
in all content. In posts 3-10, two forms of data were collected from youth and caregivers. First, participants indicated if an intervention component was acceptable by survey responses (yes/no). Second, participants provided open-ended responses to explain why they thought the component was acceptable or not. Those in the Caregiver/Spanish group were provided all information and questions in Spanish and those in the Youth/ Spanish group were provided all information and questions in Spanish and English. Youth and caregivers were compensated for each response they provided.
Data Analysis
We excluded seven caregivers and four youth from analysis (two caregivers withdrew prior to the crowdsourcing procedures; five caregivers and one youth did not sign up for Yammer; three youth did not provide at least one response to posts 2-10), resulting in a final patient-partner group of 20 caregivers and 15 youth (Table 3). A mixed-methods approach was used to analyze the data. First, we calculated the proportion of respondents that found each intervention component acceptable, neutral/mixed, and unacceptable. An a-priori criteria of 80% of participants rating an intervention component as acceptable was established. Components where fewer than 80% of participants rated as acceptable would be revised based on open-ended responses. Next, we mixed quantitative and qualitative data through the process of building in which qualitative data were used to better understand participants’ acceptability ratings.30,33 A two-person team (PTE, CT) analyzed the qualitative data to understand what caregivers and youth did and did not like about specific intervention components.
Phase 2 Results
First, we presented the results of the polls on preferred slogan (Table 4). A majority of Black caregivers (67%), Black youth (67%), and Hispanic youth (100%) preferred a slogan that focused on how the COVID-19 vaccine would let you get back to doing things you enjoy. Most Hispanic caregivers (67%) preferred a slogan that focused on how getting the COVID-19 vaccine would protect your family and community. After consultation with our community partners, we decided that English materials would include the slogan “Get back to the moments you missed,” whereas Spanish materials would include the slogan “Protect yourself, your family, your community” since most Hispanic youth were bilingual.
Note:
Posts
Introduction & rapport building (why did you join this group?) 2 Choosing a slogan to motivate youth to get the COVID-19 vaccine 3 Educational handout addressing community myths about the COVID-19 vaccine 4 Family-centered language for offering the vaccine at primary care visits 5 Communication strategies for primary care providers 6 Community health care workers conducting outreach at primary care clinics 7 Motivational Flyers 8 Video featuring local Black youth or Hispanic families – motivation to get the vaccine 9 Video featuring local Black youth or Hispanic families – addressing concerns about vaccine safety 10 Videos to address community-specific concerns w/vaccine 11 Addressing mistrust w/medical system (youth & Black caregivers only)
Addressing questions about COVID-19 vaccine (Spanish-speaking caregivers only)
Table 2. Overview of Crowdsourcing
1
12
For posts 7 and 10 we posted follow-up posts for specific groups based on participants’ responses to the original posts. 33
Prototypes of six distinct intervention components were provided to participants and five were rated as acceptable by ≥ 80% of youth and caregivers and therefore did not require refinement (Table 5). Approximately 85% of participants rated the community-tailored handout as acceptable. Qualitative data revealed that participants felt the handout answered important questions and was easy to read. Some caregivers also noted that it could facilitate conversations about the vaccine with their primary care provider. One Black caregiver shared, “The fact sheet offers up front information which could open up questions that the families may feel more comfortable asking a health care professional after reading.” One Black youth expressed concern about serious side effects from the vaccine, so a section was added about myocarditis risk.
Around half (56%) of participants rated family-centered language to offer the vaccine at the time of a clinic visit as acceptable. Caregivers and youth felt that it was an opportunity to talk to their health care provider and learn more about the vaccine; however, many disapproved of the original wording, which suggested that the child was due for the COVID-19 vaccine. One Black caregiver explained, “The approach is wrong because the COVID shot isn’t something my children get. Perhaps more on the lines like the shot is available for your child today are you interested in them getting it or do [you] have any questions or concerns that I can answer.” Caregivers also shared that, ultimately, families should be the ones deciding whether to get the vaccine. To address this, we changed the wording to ask families about their readiness to talk to their provider about the COVID-19 vaccine.
Almost all participants rated primary care providers using family-centered communication skills (93.9%) and community health workers providing education and counseling before visits (96.9%) as acceptable interventions that would help families feel more comfortable with making a decision about the COVID-19 vaccine. For example, one Hispanic caregiver noted “I think [the communication skills do] help, and even more so if the doctors speak to us more clearly about the importance of the vaccine, one would be calmer to make the best decision.” Regarding receiving counseling from community health workers, one Black caregiver shared, “It prepares both sides, saves time & causes no pressure on the parent. Speaking ahead of time [with a community health worker] may help with making an honest, informed decision about whether or not to vaccinate.”
Over 80% of participants rated the community-tailored motivational posters as acceptable. For example, one Hispanic teen shared that the posters highlighted the benefits of getting vaccinated, such as, “reuniting with family they haven’t been in contact with since the pandemic started.” We incorporated families’ suggestions on ways to improve the poster, such as adding a website link, into the final design.
Over 80% of participants rated the videos featuring local youth, families, and health care providers as acceptable. Participants felt that youth and families featured in the videos had relatable reasons for choosing to get vaccinated. As one Black teen shared, “I say it’s helpful because they all got up there and said how they felt about the situation and a lot of them did it for the people
Caregivers (n = 20) N (%) Adolescent (n = 15) N (%) Sex Female Male 17 (85.0) 3 (15.0) 9 (60.0) 6 (40.0) Race/ethnicity Non-Hispanic Black Hispanic (any race) 12 (60.0) 8 (40.0) 11 (73.3) 4 (26.7) Relation to target child Biological mother Biological father 17 (85.0) 3 (15.0) Primary spoken language English Spanish Both 14 (70.0) 6 (30.0) 13 (86.7) 1 (6.7) 1 (6.7) Insurance typea Public Private 14 (70.0) 6 (30.0) 4 (50.0) 4 (50.0) Intend to get COVID-19 vaccine?a Yes No Maybe 6 (30.0) 3 (15.0) 11 (55.0) 1 (12.5) 1 (12.5) 6 (75.0) Mean (SD), range Mean (SD), range Age (years) 40.4 (7.3), 31.0-64.0 13.9 (1.6), 12-17 Target child age (years) 10.8 (3.6), 5.0-17.0
Table 3. Demographics and Descriptives
34 Delaware Journal of Public Health - March 2024
Note: aCaregiver responses report on all adolescents except for the eight youth who participated without their caregivers.
Note: aResults from second round of voting.
Notes: aAverage acceptability ratings across all videos; bOnly shown to Black youth and caregivers; cOnly shown to Hispanic youth and caregivers; dTwo videos shown only to Hispanic caregivers.
they love.” Youth and caregivers also appreciated that the videos answered common and important questions in a way that normalized their own concerns. For example, one Black caregiver shared, “This is by far the most informative, honest video so far! The facts and fears were talked about in a way that wasn’t demeaning.” Although Hispanic caregivers found the original videos to be acceptable, they wanted more information about the vaccine itself in the videos. Therefore, we asked the Hispanic caregivers for feedback on two additional videos that featured a local pediatrician of Hispanic background answering questions about the COVID-19 vaccine. Most Hispanic caregivers (80%) rated these videos as acceptable.
DISCUSSION
We found that a culturally- and locally-tailored intervention that promotes dialogue with trusted messengers and shared decisionmaking is a preferred way to promote COVID-19 vaccine uptake among historically marginalized communities. We successfully
engaged community partners to identify barriers and facilitators to COVID-19 vaccine uptake and develop intervention components to address these. Results from the community engagement survey indicated high levels of engagement from our community partners throughout the development phase. Findings from the crowdsourcing phase of the study indicated that the intervention components were highly acceptable to our patient partners.
The format and content of our multicomponent intervention is consistent with a systematic review on effective strategies to address vaccine hesitancy.12 In practice, the components of our cocreated intervention could be implemented independently or in concert. For example, it may be that videos or handouts are effective for families who have isolated concerns, but more hesitant families may benefit from dialogue with a trusted source like a pediatrician or community health worker outreach. However, the components are also complementary and cohesive in that they utilized shared messaging (e.g., community-
NHB Caregivers (n = 12) NHB Youth (n = 9) Hispanic Caregivers (n = 6) Hispanic Youth (n = 6) Get back to the things you enjoy 8% / --- 0% 17% Get back to the people and moments you missed 25% / 67%a 67% 0% 100% Get back to the people and things you love 25% / --- 11% 0% Protect yourself, your family, your community 25% / 33%a 22% 67% 0% For you friends, your family, your community 17% / --- 17% 17%
Table 4. Stakeholder Voting for Slogans
Component Acceptable % (n) Neutral/Mixed % (n) Unacceptable % (n) Community-tailored handouts (n = 27) 85.2 (23) 14.8 (2) 0.0 (0) Family-centered language to offer vaccines (n = 30) 56.7 (17) 30.0 (9) 13.3 (4) Provider family-centered communication strategies (n = 33) 93.9 (31) 6.1 (2) 0.0 (0) Community health workers (n = 32) 96.9 (31) 0.0 (0) 3.1 (1) Community-tailored flyers (n = 32) 87.5 (28) 6.3 (2) 6.3 (2) Videosa 90.2% 8.4 1.4 “Do I need the COVID-19 vaccine if I’m young and healthy?” (n = 25) 96.0 (24) 4.0 (1) 0.0 (0) “Why I got the vaccine.” (n = 28) 89.3 (25) 3.6 (1) 7.1 (2) “How can I trust that the COVID-19 vaccine is safe?” (n = 18)b 100 (18) 0.0 (0) 0.0 (0) “How we feel after getting the COVID-19 vaccine?” (n = 7)c 85.7 (6) 14.3 (1) 0.0 (0) “Rapid development of vaccine” & “vaccine & fertility” (n = 5)d 80.0 (4) 20.0 (1) 0.0 (0)
Table 5. Acceptability Ratings for Intervention Components
35
tailored slogans and addressing community myths), with several components also promoting shared decision-making with regard to getting the COVID-19 vaccine. This included training primary care providers and community health workers to use motivational interviewing, an approach that has demonstrated efficacy in reducing vaccine hesitancy and promoting vaccine uptake for other vaccines.16,17,34
This study highlights the importance of engaging relevant partners when developing interventions, particularly when these interventions aim to address health disparities. Although our intervention was grounded in the scientific literature on vaccine hesitancy and supported by partners within the health care system, our community and patient partners provided invaluable insights on how to tailor and implement the intervention. Their recommendations to feature local youth and normalize concerns about the vaccine, insights into what concerns and motivators were relevant to the community, and emphasis on having dialogues with trusted messengers (e.g., pediatricians, community health workers) enhanced the acceptability of our intervention. While this process of working with multiple partner groups in an iterative process can be time-consuming, it is important to ensuring that an intervention is ultimately successful. Our process of engaging community and patient partners can also be generalized to other health equity issues. Of note, we engaged partners through advisory and focus groups, and therefore partners did not need to have formal research experience or training. Although this was an effective method for engaging stakeholders, future work may benefit from including partners as more formal members of the research team.35 Regardless of the level of involvement, it is also important that partner engagement is bidirectional. Furthermore, effective partnerships should be ongoing, highlighting the need for community engagement infrastructure within health care systems.
This study has multiple strengths, including the engagement of a large and diverse group of partners, following recommendations from the Promising Practices Guide,24 and use of rigorous mixed methods when refining the intervention. However, the following limitations should be considered when interpreting results of this study. The proportion of community partners completing the community engagement survey declined over time and may have affected how we engaged community partners. However, attendance rates were higher (≥ 75%) during the initial co-development process. The sample was limited to Black and Hispanic families or community leaders in Delaware, so results may not generalize to other communities. However, the very nature of this work is to ensure that interventions are tailored to specific communities and therefore we encourage others to use this same approach when developing and refining interventions. Due to the dynamic nature of the COVID-19 pandemic, interventions needed ongoing refinement to ensure they remained relevant. Engaging community partners even after an intervention is developed is helpful in remaining responsive despite evolving circumstances. Finally, the formative nature of this study precludes any conclusions about the efficacy of the intervention. We plan to test this intervention in a future pilot randomized controlled trial.
PUBLIC HEALTH IMPLICATIONS
The current study highlights how engaging community, youth, and caregiver partners can improve the quality and acceptability of health equity interventions to promote vaccine uptake. Utilizing empirically-supported practices facilitated a productive partnership and codesign process and allowed the research team to be responsive to community, youth, and caregiver partner feedback. Input from partners suggested that strategies that addressed community concerns, featured local community members and trusted messengers, and promoted shared decision-making were most acceptable. This approach can be applied to enhance other interventions to reduce disparities in vaccine uptake.
Dr. Enlow may be contacted at paul.enlow@nemours.org
REFERENCES
1. Azar, K. M. J., Shen, Z., Romanelli, R. J., Lockhart, S. H., Smits, K., Robinson, S., . . . Pressman, A. R. (2020). Disparities in outcomes among COVID-19 patients in a large health care system in California: Study estimates the COVID-19 infection fatality rate at the US county level. Health Affairs (Project Hope), 39(7), 1253–1262.
https://doi.org/10.1377/hlthaff.2020.00598
2. Shi, D. S., Whitaker, M., Marks, K. J., Anglin, O., Milucky, J., Patel, K., . . . Havers, F. P., & the COVID-NET Surveillance Team. (2022, April 22). Hospitalizations of children aged 5-11 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 2020-February 2022. MMWR. Morbidity and Mortality Weekly Report, 71(16), 574–581.
https://doi.org/10.15585/mmwr.mm7116e1
3. Walter, E. B., Talaat, K. R., Sabharwal, C., Gurtman, A., Lockhart, S., Paulsen, G. C., . . . Gruber, W. C., & the C4591007 Clinical Trial Group. (2022, January 6). Evaluation of the BNT162b2 Covid-19 vaccine in children 5 to 11 years of age. The New England Journal of Medicine, 386(1), 35–46. https://doi.org/10.1056/NEJMoa2116298
4. Frenck, R. W., Jr., Klein, N. P., Kitchin, N., Gurtman, A., Absalon, J., Lockhart, S., . . . Gruber, W. C., & the C4591001 Clinical Trial Group. (2021, July 15). Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. The New England Journal of Medicine, 385(3), 239–250. https://doi.org/10.1056/NEJMoa2107456
5. Polack, F. P., Thomas, S. J., Kitchin, N., Absalon, J., Gurtman, A., Lockhart, S., . . . Gruber, W. C., & the C4591001 Clinical Trial Group. (2020, December 31). Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. The New England Journal of Medicine, 383(27), 2603–2615.
https://doi.org/10.1056/NEJMoa2034577
6. Ndugga, N., Hill, L., Artiga, S., & Haldar, S. (2022, July 14). Latest data on COVID-19 vaccinations by race/ethnicity. Kaiser Family Foundation. Retrieved from:
https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-oncovid-19-vaccinations-by-race-ethnicity/
7. MacDonald, N. E., & the SAGE Working Group on Vaccine Hesitancy. (2015, August 14). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164.
https://doi.org/10.1016/j.vaccine.2015.04.036
36 Delaware Journal of Public Health - March 2024
8. Njoku, A., Joseph, M., & Felix, R. (2021, September 20). Changing the narrative: Structural barriers and racial and ethnic inequities in COVID-19 vaccination. International Journal of Environmental Research and Public Health, 18(18), 9904. https://doi.org/10.3390/ijerph18189904
9. Zhang, Y., & Fisk, R. J. (2021, March). Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: Experience from the United States. Global Health Journal (Amsterdam, Netherlands), 5(1), 51–55.
https://doi.org/10.1016/j.glohj.2021.02.005
10. Fisher, C. B., Gray, A., & Sheck, I. (2021, December 27). COVID-19 pediatric vaccine hesitancy among racially diverse parents in the United States. Vaccines, 10(1), 31.
https://doi.org/10.3390/vaccines10010031
11. Phan, T. T., Enlow, P. T., Wong, M. K., Lewis, A. M., Kazak, A. E., & Miller, J. M. (2021, December 15). Disparities in Delaware caregiver beliefs about the COVID-19 vaccine for their children. Delaware Journal of Public Health, 7(5), 64–71.
https://doi.org/10.32481/djph.2021.12.015
12. Kerrigan, D., Mantsios, A., Karver, T. S., Davis, W., Taggart, T., Calabrese, S. K., Harris, K. M. (2023, February). Context and considerations for the development of community-informed health communication messaging to support equitable uptake of COVID-19 vaccines among communities of color in Washington, DC. Journal of Racial and Ethnic Health Disparities, 10(1), 395–409.
https://doi.org/10.1007/s40615-022-01231-8
13. Dada, D., Djiometio, J. N., McFadden, S. M., Demeke, J., Vlahov, D., Wilton, L., . . . Nelson, L. E. (2022, February). Strategies that promote equity in COVID-19 vaccine uptake for black communities: A review. J Urban Health, 99(1), 15–27.
https://doi.org/10.1007/s11524-021-00594-3
14. Jarrett, C., Wilson, R., O’Leary, M., Eckersberger, E., & Larson, H. J., & the SAGE Working Group on Vaccine Hesitancy. (2015, August 14). Strategies for addressing vaccine hesitancy - A systematic review. Vaccine, 33(34), 4180–4190.
https://doi.org/10.1016/j.vaccine.2015.04.040
15. Gowda, C., & Dempsey, A. F. (2013, August). The rise (and fall?) of parental vaccine hesitancy. Human Vaccines & Immunotherapeutics, 9(8), 1755–1762. https://doi.org/10.4161/hv.25085
16. Kestenbaum, L. A., & Feemster, K. A. (2015, April). Identifying and addressing vaccine hesitancy. Pediatric Annals, 44(4), e71–e75. https://doi.org/10.3928/00904481-20150410-07
17. Shelby, A., & Ernst, K. (2013, August). Story and science: How providers and parents can utilize storytelling to combat anti-vaccine misinformation. Human Vaccines & Immunotherapeutics, 9(8), 1795–1801.
https://doi.org/10.4161/hv.24828
18. Gagneur, A., Lemaître, T., Gosselin, V., Farrands, A., Carrier, N., Petit, G., . . . De Wals, P. (2018, June 28). A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health, 18(1), 811. https://doi.org/10.1186/s12889-018-5724-y
19. Reno, J. E., O’Leary, S., Garrett, K., Pyrzanowski, J., Lockhart, S., Campagna, E., . . . Dempsey, A. F. (2018). Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. Journal of Health Communication, 23(4), 313–320.
https://doi.org/10.1080/10810730.2018.1442530
20. Pérez, L. M., & Martinez, J. (2008, January). Community health workers: Social justice and policy advocates for community health and well-being. American Journal of Public Health, 98(1), 11–14. https://doi.org/10.2105/AJPH.2006.100842
21. Cosgrove, S., Moore-Monroy, M., Jenkins, C., Castillo, S. R., Williams, C., Parris, E., Brownstein, J. N. (2014, November). Community health workers as an integral strategy in the REACH U.S. program to eliminate health inequities. Health Promotion Practice, 15(6), 795–802.
https://doi.org/10.1177/1524839914541442
22. Purnell, T. S., Calhoun, E. A., Golden, S. H., Halladay, J. R., Krok-Schoen, J. L., Appelhans, B. M., & Cooper, L. A. (2016, August 1). Achieving health equity: Closing the gaps in health care disparities, interventions, and research. Health Affairs (Project Hope), 35(8), 1410–1415.
https://doi.org/10.1377/hlthaff.2016.0158
23. Batalden, M., Batalden, P., Margolis, P., Seid, M., Armstrong, G., Opipari-Arrigan, L., & Hartung, H. (2016, July). Coproduction of healthcare service. BMJ Quality & Safety, 25(7), 509–517.
https://doi.org/10.1136/bmjqs-2015-004315
24. Leask, C. F., Sandlund, M., Skelton, D. A., Altenburg, T. M., Cardon, G., Chinapaw, M. J. M., . . . Chastin, S. F. M., & the GrandStand, Safe Step and Teenage Girls on the Move Research Groups. (2019, January 9). Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Research Involvement and Engagement, 5, 2.
https://doi.org/10.1186/s40900-018-0136-9
25. Wallerstein, N., Oetzel, J. G., Sanchez-Youngman, S., Boursaw, B., Dickson, E., Kastelic, S., . . . Duran, B. (2020, June). Engage for equity: A long-term study of community-based participatory research and community-engaged research practices and outcomes. Health Educ Behav, 47(3), 380–390. https://doi.org/10.1177/1090198119897075
26. Engage for Equity Research Team. 2017, Promising Practices of CBPR and Community Engaged Research Partnerships. University of New Mexico, Albuquerque. Retrieved from https://engageforequity.org/wp-content/uploads/2017/12/PromisingPractices-Guide-12.7.12.pdf
27. Oetzel, J. G., Boursaw, B., Magarati, M., Dickson, E., SanchezYoungman, S., Morales, L., . . . Wallerstein, N. (2022, May 2). Exploring theoretical mechanisms of community-engaged research: A multilevel cross-sectional national study of structural and relational practices in community-academic partnerships. International Journal for Equity in Health, 21(1), 59. https://doi.org/10.1186/s12939-022-01663-y
28. Michener, L., Aguilar-Gaxiola, S., Alberti, P. M., Castaneda, M. J., Castrucci, B. C., Harrison, L. M., . . . Wallerstein, N. (2020, July 16). Engaging with communities – Lessons (re)learned from COVID-19. Preventing Chronic Disease, 17, E65.
https://doi.org/10.5888/pcd17.200250
37
29. Belone, L., Rae, R., Hirchak, K. A., Cohoe-Belone, B., Orosco, A., Shendo, K., & Wallerstein, N. (2020, December). Dissemination of an American Indian culturally centered community-based participatory research family listening program: Implications for global indigenous well-being. Genealogy, 4(4), 99.
https://doi.org/10.3390/genealogy4040099
30. Creswell, J. W., Klassen, A. C., Plano Clark, V. L., & Smith, K. C.(2011). Best practices for mixed methods research in the health sciences. Washington, DC: National Institutes of Health. Retrieved from https://obssr.od.nih.gov/sites/obssr/files/Best_Practices_for_Mixed_ Methods_Research.pdf
31. Dickson, E., Magarati, M., Boursaw, B., Oetzel, J., Devia, C., Ortiz, K., & Wallerstein, N. (2020, Jan/Feb). Characteristics and practices within research partnerships for health and social equity. Nursing Research, 69(1), 51–61.
https://doi.org/10.1097/NNR.0000000000000399
32. Monaghan, M., Sanders, R. E., Kelly, K. P., Cogen, F. R., & Streisand, R. (2011, December). Using qualitative methods to guide clinical trial design: Parent recommendations for intervention modification in type 1 diabetes. J Family Psychol, 25(6), 868–872.
https://doi.org/10.1037/a0024178
33. Behrend, T. S., Sharek, D. J., Meade, A. W., & Wiebe, E. N. (2011, September). The viability of crowdsourcing for survey research. Behavior Research Methods, 43(3), 800–813.
https://doi.org/10.3758/s13428-011-0081-0
34. Gagneur, A. (2020, April 2). Motivational interviewing: A powerful tool to address vaccine hesitancy. Can Commun Dis Rep, 46(4), 93–97.
https://doi.org/10.14745/ccdr.v46i04a06
35. Fetters, M. D., Curry, L. A., & Creswell, J. W. (2013, December). Achieving integration in mixed methods designs-principles and practices. Health Services Research, 48(6 Pt 2), 2134–2156.
https://doi.org/10.1111/1475-6773.12117

Y ou’re worth it. GET YOUR BREAST CANCER SCREENING. Yearly, if you’re 40 or older. Earlier, if you have a family history. The earlier you know, the easier it is to treat. HEALTHY DELAWARE Talk to your health care provider today. Don’t have one? A screening nurse navigator can help you schedule a screening. Call 2-1-1 or visit HealthyDelaware.org/Breast. 38 Delaware Journal of Public Health - March 2024
Partner with chwCORE to train and grow the community health workforce!
Who is chwCORE?
We train Community Health Workers (CHWs) in Pennsylvania and Delaware. chwCORE is fully accredited by the Pennsylvania Certification Board (PCB) and is a program of the Public Health Management Corporation (PHMC).
The process includes: TRAINING CHW CERTIFICATION SITE PLACEMENT
What is included in chwCORE training prior to placement?
After a 75 hour online training, which covers care navigation, trauma-informed care, harm reduction strategies, professional ethics, and more, trainees get placed at a partner organization like yours to assist in community health initiatives. We provide trainees peer-learning support to reinforce skills developed in online training and access to additional certifications in Mental Health First Aid and the Health Literacy Specialist curriculum.
How does chwCORE support trainees and partner organizations?
Our program offers a stipend to trainees while placed at partner organizations to help support living expenses. During this site placement, trainees acquire 300 hours of work experience in a community health role while supporting organizations’ needs. Examples of activities may include: outreach, education, informal counseling, care navigation, and more. Wherever possible, chwCORE staff work to remove the reporting and training burdens from partner organizations.
How can potential partner organizations get involved?
chwCORE
Training Program is: Fully accredited Self-paced, online Offering stipends
chwCORE will pair interested partner sites with trained CHWs. To become a program partner and share open opportunities with our program, visit chwCORE.org to fill out an application. If you have more questions, email us at chwcore@gmail.com
chwCORE.org
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $3 million with 0 percentage nanced with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the o cial views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
39

From the Delaware Division of Public Health
National Nutrition Month promotes understanding of nutrition for well-being
March heralds National Nutrition Month, an annual initiative by the Academy of Nutrition and Dietetics that promotes healthy eating and the importance of nutrition to maintain a healthy weight and reduce the risk of chronic disease
The 2024 theme, “Beyond the Table,” highlights the importance of the farm-to-fork aspects of nutrition, addressing food production, navigating grocery stores and farmers markets, and home food safety. By looking “beyond the table” and considering healthy food choices at home and on the go, individuals can learn mindful eating by savoring each bite, heeding hunger cues, and learning how to enjoy distraction-free meals.
A primary goal is to equip individuals with knowledge and skills for healthier decision-making, such as cooking at home, deciphering food labels, and understanding portion sizes. Fruits, vegetables, lean proteins, and whole grains are nutrient-rich foods that nourish lives by building meals with essential vitamins, minerals, and antioxidants.
The Division of Public Health’s Physical Activity, Nutrition, and Obesity Prevention (PANO) Program promotes healthy eating and the importance of nutrition to maintain a healthy weight and reducing risk of chronic disease. PANO suggests following the Dietary Guidelines for Americans, 2020-2025.
The website Dietary Guidelines for Americans has information about healthy dietary patterns at every age, including choosing nutrient-dense foods and beverages and understanding calorie needs, macronutrients, minerals, vitamins, and more.
Another resource is the U.S. Department of Agriculture’s MyPlate. MyPlate provides information about the food groups and how to build healthy meals by age.


Wear blue on March 26 to support
Diabetes Alert Day in Delaware
Diabetes Alert Day reminds Delawareans to assess their risk of developing type 2 diabetes, a chronic disease that can lead to kidney failure, adult blindness, lower limb amputations, heart disease, and stroke. Type 2 diabetes can be prevented or delayed by losing weight, engaging in at least 150 minutes of physical activity weekly and improving one’s diet. Wear blue on March 26 to show support. National Diabetes Prevention Programs are covered by insurance or offered at no cost for those at risk for, or concerned about, diabetes.
Individuals dealing with diabetes can seek support through clinical Diabetes Self-Management Education Programs or register for free six-week Self-Management Programs in Delaware at https://www.healthydelaware.org/Individuals Additional Delaware Diabetes Coalition resources are available at https://www.dediabetescoalition.org/ Community members can encourage friends, family, and community members to undergo a simple Diabetes Risk Test. The National Institute of Diabetes and Digestive and Kidney Diseases offers Kidney Sundays: A Toolkit to help begin essential conversations.
More than 95,000 Delaware adults reported in 2021 that they had been diagnosed with diabetes, according to the Delaware Behavioral Risk Factor Survey conducted by the Division of Public Health (DPH). The survey also shows that 84,800 additional Delaware adults reported being diagnosed with prediabetes.
For more information, contact DPH’s Diabetes and Heart Disease Prevention and Control Program at 302-744-1020.

March
2024
40 Delaware Journal of Public Health - March 2024
Getty Images

“Moving Delaware Forward: From Equity
Awareness to Action” Summit planned
Healthy Communities Delaware and 16 co-sponsors are hosting a large two-day event, “Moving Delaware Forward: From Equity Awareness to Action” Summit on April 18 and 19, 2024 from 9:00 a.m. to 4:00 p.m. each day. The event is being held at the Chase Center on the Riverfront, located at 815 Justison Street in Wilmington, Del., in the Atrium and Multiple Rooms
The free summit will convene an ongoing movement to advance equity for all as shared stewards to ensure that all people and places in Delaware are thriving (no exceptions). Attendees will gain knowledge of the vital conditions for health and wellbeing and explore "multi-solving" to advance equity. They will learn about local initiatives, find ways to build momentum, and inspire action in their communities.
As many as 500 attendees will represent non-profit and community-based organizations, community champions/residents, elected officials and policymakers, youth leaders, and representation from urban, suburban, and rural areas of each county. There are two keynote speakers:
• LaTosha Brown, co-founder of Black Voters Matter, will speak on April 18. Drawing from her experiences as a co-founder of the Black Voters Matter Foundation, Ms. Brown will share her story of power building and civic engagement that played an instrumental role in the 2017 Alabama U.S. Senate race and inspire Delaware's equity champions to action.
• Admiral Rachel L. Levine, MD, with the U.S. Department of Health and Human Services and the Assistant Secretary for Health, will speak on April 19. Admiral Levine will illustrate the powerful connections between equity work happening across Delaware's communities and the pursuit of equity on the federal level, showing how Delaware can leverage the Federal Plan for Equitable Long-Term Recovery and Resilience.
In addition to the presenters, this event includes film screenings and a poster gallery walk. It closes with a visit to the Blue Rocks game with fireworks.
The public is invited to register for this conference. There is no registration fee. Register at Equity Action Delaware

How to help children cope with a disaster
Children are not small adults. They require help to cope with emergencies or disasters that they experience or are exposed to through media coverage of war, extreme weather, and active shooter incidents. Children feel less of a sense of control, understand less, and have fewer experiences bouncing back from hard situations.
When parents and caregivers are prepared, rested, and relaxed, they respond better to unexpected events and make better decisions. Parents and caregivers should set a good example for children by eating healthy, exercising regularly, getting plenty of sleep, and avoiding drugs and alcohol Follow these tips from the Centers for Disease Control and Prevention to reduce stress before, during, and after disasters or traumatic events:
Before
• Talk to your children so they know you are prepared to keep them safe.
• Make and review safety plans to boost their confidence and give them a sense of control. During
• Stay calm and reassure your children.
• Talk to children about what is happening in a way that they can understand. Keep it simple and appropriate for each child’s age.
After
• Provide opportunities for children to talk about what they went through or what they think about it. Let them share concerns and ask questions.
• Let children help community or family members after a disaster, such as supervised volunteering in a safe environment. Children should not participate in disaster cleanup activities.
• Parents, teachers, and other adults should share information about how each child is coping.
It is difficult to predict how some children will respond to disasters and traumatic events. The American Academy of Pediatrics offers a Family Readiness Kit. For more information, visit ready.gov/kids/helpingchildren-cope.
The DPH Bulletin – March 2024 Page 2 of 3
41

DPH Office of Infectious Disease Epidemiology hosts monthly forums
The Division of Public Health’s Office of Infectious Disease Epidemiology (OIDE) now has office hours for Delaware health care providers.
OIDE hosts virtual “EpiChat” forums for health care providers to engage with epidemiologists and other subject matter experts about key public health topics. Made available via Delaware Public Health’s One Health partnership, the monthly sessions allow health care providers to learn about Delaware’s reportable diseases, ask questions, and share insights. OIDE provides information and guidance on various topics and shares resources. Forums begin at noon and end at 1:00 p.m. The March 21 EpiChat is about Lyme disease
To receive EpiChat notifications, contact Reportdisease@delaware.gov For more information, contact OIDE at 302-622-4149

The Division of Public Health, Bureau of Chronic Disease, Self-Management and Healthy Heart Ambassador programs hosted a volunteer recognition luncheon on February 16 at the Modern Maturity Center.
National Poison Prevention Week set for week of March 17-23, 2024
The third week of March (March 17-23, 2024) is National Poison Prevention Week. The U.S. Congress established the observance in 1961 to raise awareness of poison prevention, especially how to reduce unintentional poisonings.
Since 93% of poisonings occur in the home, the American Association of Poison Control Centers warns families about potentially poisonous medicines and chemicals. Follow these tips from the National Poison Prevention Week Council:
• Post the Poison Control Center’s phone number (1-800-222-1222) near every phone
• Carefully read product labels and dosages so they are used and stored correctly.
• Immediately call Poison Help at 1-800-222-1222 when accidents happen with chemicals or medicine. Call 911 if someone has trouble breathing.
• Keep household cleaning agents, prescription medications, and insecticides and lawn products out of the reach of children and pets.
• Open windows when using strong chemicals.
• Properly dispose of old household hazardous waste and prescription drugs

• Install smoke detectors on each level of new and existing one- and two-family dwellings, mobile homes, modular homes, and townhouses as required by state law Test them monthly
• Install carbon monoxide detectors in new and existing dwelling or sleeping units with a fossilfuel burning heater or appliance, a fireplace, or other feature, fixture, or element that emits carbon monoxide as a byproduct of combustion; or an attached garage. It is a state law.
For more information, visit the Health Resources & Services Administration’s Poison Help website at www.PoisonHelp.hrsa.gov Poison Control Center toolkit materials are available in Spanish.
The DPH Bulletin – March 2024 Page 3 of 3
From left to right are volunteers: Kalissa Horne, Senior Medical Social Work Consultant, Shipley State Service Center (SSC); Nikita Clark, Senior Medical Social Work Consultant, Williams SSC; and Natashia Morris-Harrison, Nutritionist II and Jasmine Smith, Senior Medical Social Work Consultant, both of Milford SSC Riverwalk. Photo by Alyssa Imprescia
42 Delaware Journal of Public Health - March 2024
The Burden of Diabetes in Delaware
Diabetes is an epidemic in the United States. According to the Centers for Disease Control and Prevention (CDC), over 3 7 million Americans have diabetes and face its devastating consequences. What’s true nationwide is also true in Delaware.
Delaware’s diabetes epidemic:
▪ Approximately 96,844 people in Delaware, or 12% of the adult population, have diagnosed diabetes
▪ An additional 24,000 people in Delaware have diabetes but don’t know it, greatly increasing their health risk.
Diagnosed diabetes costs an estimated $980 million in Delaware each year.
The serious complications include heart disease, stroke, amputation, end-stage kidney disease, blindness and death
▪ There are 268,000 people in Delaware, 35.4% of the adult population, who have prediabetes with blood glucose levels that are higher than normal but not yet high enough to be diagnosed as diabetes.
▪ Every year an estimated 6,009 people in Delaware are diagnosed with diabetes.
Diabetes is expensive
:
People with diabetes have medical expenses approximately 2.3 times higher than those who do not have diabetes.
▪ Total direct medical expenses for diagnosed diabetes in Delaware were estimated at $703 million in 2017.
▪ In addition, another $280 million was spent on indirect costs from lost productivity due to diabetes.
Improving lives, preventing diabetes and finding a cure
In 2023, the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health did not invest money in diabetes-related research projects in Delaware.
Sources include:
:
The Division of Diabetes Translation at the CDC provided $944,298 in diabetes prevention and educational grants in Delaware in 2021.
▪ Diabetes Prevalence: 2020 state diagnosed diabetes prevalence, cdc.gov/diabetes/data; 2017 state undiagnosed diabetes prevalence, Dall et al., “The Economic Burden of Elevated Blood Glucose Levels in 2017”, Diabetes Care, September 2019, v ol. 42.
▪ Diabetes Incidence: National Diabetes Statistics Report 2022, cdc.gov/diabetes/data/statistics-report/index.html
▪ Cost: American Diabetes Association, “Economic Costs of Diabetes in the U.S. in 2017”, Diabetes Care, May 2018.
▪ Research expenditures: 2023 NIDDK funding, report.nih.gov/award/index.cfm; 2021 CDC diabetes funding, fundingprofiles.cdc.gov/FundingProfiles/FundingQuery
Learn more at diabetes.org | 1-800-DIABETES (800-342-2383) 3/2023
The Burden of Diabetes in Delaware
American Diabetes Association
|
43
Pediatric Dentists: Frontline Public Health Providers Leading the Way in Identifying and Preventing Childhood Obstructive Sleep Apnea Syndrome
Bari Levine, D.M.D., M.P.H.
Pediatric Dentist, Growing Smiles Main Line Pediatric Dentistry
Freda Patterson, Ph.D.
Associate Dean of Research, College of Health Sciences, University of Delaware
Lauren Covington, Ph.D., R.N
Assistant Professor, School of Nursing, University of Delaware
OBSTRUCTIVE SLEEP APNEA IN CHILDREN
Obstructive sleep disordered breathing (SDB) causes sleeprelated breathing issues due to a partially or fully blocked airway that impairs ventilation. Up to 25% of children are affected in its mildest forms (snoring) and 1-5% in more severe forms that may include a diagnosis of Obstructive Sleep Apnea Syndrome (OSAS).1 Acutely, children with SDB may experience symptoms such as daytime sleepiness, inattention, snoring, gasping, witnessed apnea, restless sleep, mouth breathing, excessive sweating, bedwetting, and headaches.2 Several risk factors for OSAS in children have been identified in the literature including obesity, craniofacial abnormalities, tobacco smoke exposure, low socio-economic status, allergic rhinitis, asthma, and enlarged palatine tonsils.1 Diagnosis of childhood OSAS peaks around 2-8 years of age, coinciding with peak tonsil growth.1 If left untreated, OSAS contributes to lifelong morbidities, including cardiovascular and metabolic diseases as well as neurocognitive and behavioral challenges.1 Children with untreated OSAS may be inappropriately diagnosed with ADHD (Attention Deficit Hyperactivity Disorder), as chronic sleep deprivation and ADHD share similar symptoms.3 Thus, childhood is a critical stage of the life course to address this potentially chronic condition.
THE ROLE OF DENTISTS IN DIAGNOSIS OF CHILDHOOD OSAS
The oral cavity is a clear indicator of a child’s overall health, positioning pediatric dentists to be uniquely equipped at the frontline of identifying and preventing the development of childhood OSAS.
During routine exams, pediatric dentists may observe these potential indicators of SDB:
1.an elongated or high-arched palate structure, 2.enlarged palatine tonsils, 3.presence of a crossbite (malocclusion), and/or
4.the presence of a tongue-tie.
These listed morphologies suggest abnormal breathing during sleep in children.2 Narrow airways are associated with a mouth breathing pattern, and mouth breathing is one important factor associated with malocclusion in children.2 Mouth breathing also causes dry mouth, which increases risk of dental decay (caries) and gingivitis (gum disease) due to the loss of protective properties of one’s saliva.1
Pediatric dentists can also observe wear on teeth from sleep bruxism (teeth grinding), present in up to 50% of children.4
Bruxism is a compensatory mechanism for airway restriction by recruiting muscles to keep the airway open during sleep.3 Additional SDB symptoms for the pediatric dentist include a forward head posture, allergic shiners, dry, chapped lips, strain when closing lips together, a gummy smile, and a child’s facial profile (i.e., long face/vertical growth pattern, retruded lower jaw, or relatively straight profile).3
PREVENTION, SCREENING, DIAGNOSIS AND TREATMENT REQUIRES AN INTERDISCIPLINARY APPROACH
Prevention of OSAS begins at birth. Pediatric dentists have the capacity to positively influence proper craniofacial development from infancy. Breastfeeding is the first, and possibly, the most important experience to facial development.5 It fosters proper craniofacial development through encouraging proper lip closure, stimulating mandibular function, and ensures correct positioning of the tongue against the palate, leading to balanced muscular development and nasal breathing.6 Exclusively breastfed babies have a lower risk of malocclusion when compared to bottle-fed babies, and the risk of malocclusion continues to fall as the duration of breastfeeding increases.6
The presence of a tongue-tie at birth often impedes breastfeeding success and its subsequent benefits to infant craniofacial development.5 A tongue-tie is a thick, tight or short string of tissue under the tongue that restricts the tongue’s movement. A tongue-tie can lead to the development of a high palate, which takes space from the nasal cavity and thereby promotes mouth breathing and puts a child at greater risk for SDB.3 A study of school-aged children found those breastfed for only a few months had less incidence of snoring and OSAS than those who were bottle-fed.5 The sooner a tongue-tie is identified and treated in infancy, the higher the likelihood of breastfeeding success and proper craniofacial development.
Risk factors for OSAS are treated by a variety of modalities and specialists. If the child presents with enlargement of the adenoids or tonsils that is blocking his/her airway, an adenotonsillectomy performed by an otolaryngologist (ENT) may be warranted, or the patient may require a Continuous Positive Air Pressure (CPAP) device.3 In the presence of an elongated or high-arched palate, orthodontists or airway
Doi: 10.32481/djph.2024.03.07
44 Delaware Journal of Public Health - March 2024
dentists can perform rapid palate expansions (RPE). RPE can reduce adenoidal and tonsillar size, support proper tongue posture, and subsequently improve nasal air flow.7 Finally, tongue-tie releases with myofunctional therapy may effectively treat mouth breathing, snoring, jaw clenching and tension.3 Each of these treatments may prevent the development of OSAS before it becomes a chronic issue.
MORE COLLABORATIVE WORK IS NEEDED TO PREVENT AND TREAT CHILDHOOD OSAS
Screening is key to prevention and quick, efficient tools are available, but can be further improved. For all new patients, we recommend that pediatric dentists assess dental wear, malocclusion, tongue-ties, and dental caries experience in addition to administering the validated Pediatric Screening Questionnaire (PSQ).8 Although the PSQ is quick to complete, it may not be sensitive enough to predict milder forms of SDB.3 Pediatric dentists must be hyperaware of these facial and oral manifestations and should also ask sleep related questions on the six-month recall health history forms.
Effective collaboration and education are needed across specialties. Many pediatricians and pediatric ENTs are not aware that tongue-ties increase a child’s risk for OSAS or that a RPE can treat OSAS. Similarly, common practice of orthodontists is to wait to expand children’s palates until the age of 7 or 8, which to many airway dentists is too late, as 60% of a child’s facial development is complete by age 6.3
Polysomnography, a sleep study which is the gold standard diagnostic tool for OSAS, is costly and challenging to perform in children.2 Sleep study wait times are often long and may lead to prioritizing only the most severe cases, causing under-diagnosis and treatment delays. Additionally, many children will have an array of sleep symptoms indicative OSAS yet their sleep study comes back negative and there are no protocols for what happens next. A solution might be forming local sleep study clubs for cross-disciplinary treatment. Additionally, further research on the dental caries-OSAS link is needed, and we suggest that pediatric dentists consider referrals to an airway specialist for children under six years with one or more dental caries.
CONCLUSION
In this symbiotic relationship between oral health and overall well-being, pediatric dentists serve as torchbearers of holistic care, illuminating a path towards healthier mouths and healthier sleep for our children. Pediatric dentists must educate and collaborate with other specialists – pediatric ENTs, orthodontists, pediatricians, lactation consultants, and sleep medicine providers – to properly prevent, screen, diagnose and treat children suspected of SDB to halt the growing epidemic of childhood OSAS.
Dr. Levine may be contacted at office@growingsmilesmainline.com
REFERENCES
1. Arroyo Buenestado, A., & Ribas-Pérez, D. (2023, February 9). Early childhood caries and sleep disorders. Journal of Clinical Medicine, 12(4), 1378.
https://doi.org/10.3390/jcm12041378
2. Burska, Z., Burghard, M., Brożek-Mądry, E., Sierdziński, J, & Krzeski, A. (2022, June). Oral cavity morphology among children at risk of sleep disordered breathing. Eur Arch Paediatr Dent, 23(3), 429–435.
https://doi.org/10.1007/s40368-022-00701-1
3. Lim, S. (2022). Breathe, sleep, thrive: Discover how airway health can unlock your child’s greater health, learning, and potential. Sparkle Publishing.
4. Bulanda, S., Ilczuk-Rypuła, D., Nitecka-Buchta, A., Nowak, Z., Baron, S., & Postek-Stefańska, L. (2021, September 10). Sleep bruxism in children: Etiology, diagnosis, and treatment-a literature review. International Journal of Environmental Research and Public Health, 18(18), 9544.
https://doi.org/10.3390/ijerph18189544
5. D’Onofrio, L. (2019, May). Oral dysfunction as a cause of malocclusion. Orthodontics & Craniofacial Research, 22 Suppl 1(Suppl 1), 43-48.
https://doi.org/10.1111/ocr.12277
6. Boronat-Catalá, M., Montiel-Company, J. M., Bellot-Arcís, C., Almerich-Silla, J. M., & Catalá-Pizarro, M. (2017, July 11). Association between duration of breastfeeding and malocclusions in primary and mixed dentition: A systematic review and meta-analysis. Scientific Reports, 7(1), 5048.
https://doi.org/10.1038/s41598-017-05393-y
7. Yoon, A., Abdelwahab, M., Bockow, R , Vakili, A., Lovell, K., Chang, I., . . . Hong, C. (2022, April). Impact of rapid palatal expansion on the size of adenoids and tonsils in children. Sleep Medicine, 92, 96–102.
https://doi.org/10.1016/j.sleep.2022.02.011
8. Chervin, R D., Hedger, K., Dillon, J. E., & Pituch, K. J. (2000, February 1). Pediatric sleep questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness,andbehavioralproblems.Sleep Medicine,1(1),21–32.
https://doi.org/10.1016/S1389-9457(99)00009-X
45
“We Are All There to Make Sure the Baby Comes Out Healthy”: A Qualitative Study of Doulas’ and Licensed Providers’ Views on Doula Care
Erin K. Knight, Ph.D., M.P.H. and Rebecca Rich, Ph.D., C.H.E.S. West Chester University
ABSTRACT
Policymakers are exploring ways to expand access to doula care to address persistent inequities in maternal and infant health across the United States. Doulas are non-medical professionals who provide physical, emotional, and informational support to birthing people before, during and after childbirth. Growing evidence supports the role of doulas in improved birth outcomes. Delaware is among several states moving towards Medicaid reimbursement for doula care to serve those most at risk. Objective: To gain an in-depth understanding of key stakeholders’ knowledge, attitudes, beliefs and experiences regarding doula training and certification, relationships among providers, and other potential needs related to infrastructure to identify areas of agreement and inform policy change in the state of Delaware. Methods: We conducted focus groups with 11 doulas and key-informant interviews with 12 licensed providers practicing in Delaware, including six nurses, four physicians and two certified nurse midwives. Qualitative data was collected via Zoom (video conferencing) between September 2022 and April 2023. Results: Analysis revealed themes related to training, credentials and competencies of doulas, including cultural competence; logistical, administrative, and financial considerations for policy and practice change; and the whole care team—relationships between doulas and medical partners, and opportunities for growth. Conclusions: Doulas and licensed providers agree on key elements of doula training, the value of certification, the need for financial support, and the importance of relationship-building across the care team. Policy implications: Areas of agreement among stakeholders provide a foundation for state leaders to move forward to ensure the delivery of the most accessible, high quality, and culturally competent doula care for birthing people in Delaware.
INTRODUCTION
Infant and maternal mortality rates in the United States (U.S.) are among the worst in the developed world and affect Black women at strikingly disproportionate rates. In Delaware, the overall infant mortality rate has declined over the past two decades from 9.3 deaths per 1,000 live births in 2000-2004 to 6.5 deaths per 1,000 live births in 2016-2020.1 However, these data mask a significant racial disparity. The non-Hispanic Black infant mortality rate of 11.6 was three times higher than the non-Hispanic White rate of 3.8 deaths per 1,000 live births, and nearly two times higher than the Hispanic rate of 6.3 deaths per 1,000 live births, during the 2016-2020 period.1 Further, the Delaware non-Hispanic Black infant mortality rate is higher than the national rate of 10.8 deaths per 1,000 live births.1
Like U.S. trends, maternal morbidity and mortality are on the rise in Delaware and Black women are particularly at risk.2 Between 2018 and 2022 in Delaware, 11 maternal deaths occurred, seven among women of color and nine of which were determined to be potentially preventable.3 While the numbers of maternal deaths each year are relatively small, it has been well established that persons of color have the highest rate of maternal death compared to their White counterparts.4 Reasons for these inequities are complex and related to a myriad of social and economic factors, including structural racism.5,6
There is growing evidence that doulas contribute to improved outcomes, particularly among women most at risk.7–9 Doulas are professionals who provide physical, emotional, and informational support to mothers before, during, and after childbirth. They also act as advocates,10 promote self-advocacy for birthing people,11 and may help mediate the negative impacts of social determinants of health, including implicit bias in healthcare.12 In addition, doula care has the potential to reduce unnecessary medical interventions and can reduce costs.7,9 Despite evidence of improved outcomes and a positive return on investment, few birthing people use doulas. Data regarding doula care in Delaware is limited. However, a large national survey of women found that only 6% engaged with a doula during labor13 and women of color and low-income women face several barriers to access.
Given the potential benefits of doulas and the importance of policy change to help address gaps in practice,7 several states have started to reimburse providers for doula services through their Medicaid programs.14 Support for policy change is also growing at the federal level, as the U.S. Department of Health and Human Services is engaging in several efforts to expand access to doula care, including providing guidance on ways to reimburse doulas through Medicaid.10 As many states, including Delaware, work to improve access to doula care many outstanding issues must be resolved, including qualifications and
Doi: 10.32481/djph.2024.03.08
46 Delaware Journal of Public Health - March 2024
training requirements for doulas, the role of doulas in relation to other members of the care team, and other infrastructure and system needs and supports.
While doulas are expected to understand the physiological processes associated with pregnancy, birth, and postpartum health, they are not medically trained. Further, doulas’ expertise is often grounded in generational, ancestral, and experiential knowledge shared among lay birth workers, and many resist certification as it resides within what is often considered an over-medicalized approach to childbirth. At the same time, the doula community is not homogenous, and doulas bring different educational backgrounds, models, traditions, and practices to this work. Further, no standardized training or certification currently exists for doulas. Federal Medicaid policy provides states with flexibility to determine requirements for training and certification.
Beyond ensuring adequate training and qualifications for doulas, positive working relationships between doulas and other members of the maternity care team are needed to ensure quality, integrated care. Anecdotal evidence from Delaware suggests that current working relationships may be tenuous, and more systematic research in other areas finds that many licensed providers are unaware of the benefits of doulas and/ or may resist the integration of doulas as part of the care team.15 Further, doulas cite lack of respect from clinicians as a workplace challenge,16 while licensed providers have reported difficult working relationships when they perceive doulas as interfering with clinical decision-making in ways that could be harmful to the patient.17
Finally, evidence from other states that have expanded access to doula services demonstrates the need to identify and prepare for potential logistical challenges associated with implementation of policy and practice changes, such as Medicaid coverage.18–20 For example, other states have experienced difficulties in supporting doulas to become certified or in helping prepare doulas for navigating the Medicaid billing process. While the experience of others is informative, states have unique healthcare system issues, resources and existing policies, making it difficult to fully anticipate potential barriers to implementation in Delaware. Given this context, our research purpose was to engage stakeholders, including doulas and other licensed providers of maternal healthcare, from across the state and gather their insights related to these and other policy and practice issues meant to increase access to quality doula care for women most at risk of poor birth outcomes. Specifically, we aimed to gain an in-depth understanding of key informants’ knowledge, attitudes, beliefs, and experiences regarding doula training and certification, relationships among providers, and other perceived infrastructure needs to inform state policy change. This research was supported by state-level partners, including the Delaware Healthy Mother and Infant Consortium (DHMIC) Doula Ad Hoc Committee; and the Delaware Department of Health and Social Services (DHSS) who funded the development of two comprehensive reports documenting this work.21,22 This paper extrapolates on these reports by highlighting areas of agreement across stakeholder groups, to provide practical recommendations for state and healthcare system leaders and further contribute to the evidence for positive change.
This research is grounded in a philosophy of community engagement and a belief that those most affected by public health policies and practices should have a say in decisions that affect them.
The researchers recognize, respect, and value the knowledge and perspectives that doulas and other providers have gained through their experience serving birthing people in Delaware. We believe it is critical to listen to, and learn from, a variety of stakeholders to inform policy development and ensure the delivery of the most accessible, high quality, and culturally competent care for birthing people.
METHODS
Researchers used a cross-sectional research design employing a combination of key informant interviews and focus groups to engage two stakeholder groups—doulas and licensed providers of maternal healthcare (i.e., nurses, midwives and physicians). Key informant interviews provide in-depth information on a given topic from the perspective of individuals who have relevant, first-hand knowledge, experience and/or expertise.23 As such, key informants can offer insight into the nature of problems and important contextual factors, as well as recommendations for solutions. A focus group is a type of interview, offering the same research benefits, including an in-depth understanding of participants’ attitudes, beliefs, and experiences.23 However, the group interaction that occurs through focus group discussions can elicit additional understanding that might not be revealed through individual interviews. These qualitative research methods are especially useful for informing policy and practice changes and may help to advance equity, as it allows researchers to gather rich contextual insights about a particular issue from different perspectives grounded in disparate lived experiences.24
Our overarching research questions were:
1. How does each stakeholder group perceive the role and value of a doula?
2. How does each stakeholder group perceive training and certification requirements for doulas, including what core competencies should be included in approved training programs to meet the needs of women from low-income communities and women of color in Delaware?
3. With respect to doula care, what is needed to better serve birthing people enrolled in Medicaid in Delaware?
Data Collection
Focus groups were conducted via Zoom (online video conferencing) with doulas across the state of Delaware between September and November 2022. Based on a review of websites and provider directories, approximately 40 eligible doulas were identified in the state at the time of recruitment. Recruitment occurred through established networks and doula organizations, including DHMIC, the Healthy Women, Healthy Babies (HWHB) Network, and Black Mothers in Power. Research participants were encouraged to share information with their colleagues, and the sample grew through a snowball sampling technique. All individuals who met the following inclusion criteria (determined through a REDCap screening survey) were invited to participate:
47
a. Any “doula” currently practicing in Delaware. A “doula” is defined as an individual who supports a birthing person during the prenatal, labor/delivery, and/or postpartum period.
b. Given the recent Coronavirus 2019 (COVID-19) pandemic, doulas who were not currently seeing clients, but practiced at any time since July 1, 2019, were also eligible.
c. Any individual who was trained as a doula through the DHSS, Division of Public Health’s HWHB Zones MiniGrant program over the past two years, but may not yet be practicing, was also eligible.
Birth workers who do not consider themselves to be “doulas” and doulas who do not serve state-based clients were excluded. Also excluded were doulas who do not provide support during the prenatal, labor/delivery, and/or postpartum periods (e.g., death doulas, transition doulas, and abortions doulas).
Focus groups were limited to no more than eight individuals and were relatively homogenous (according to demographic profiles such as race, ethnicity, and geography) to encourage participation but also allow for diverse opinions.23 Each focus group lasted approximately one hour, and subjects received a $50 electronic gift card for their participation.
Because of challenges associated with scheduling focus groups with licensed providers, we conducted individual semi-structured interviews with this stakeholder group. Interviews were conducted via Zoom with licensed providers (i.e., nurses, midwives, and physicians) between March and April 2023. We used purposeful sampling, with an aim of interviewing different types of licensed providers representing the range of maternity care hospitals and health centers across the state. Partners at the DHSS Division of Public Health and Division of Medicaid and Medical Assistance contacted all Delaware hospitals that provide maternity care services to request assistance in recruitment. Similarly, the team contacted provider networks, including DHMIC, HWHB, the Delaware section of The American College of Obstetricians and Gynecologists, and the Delaware Health Care Association to share recruitment information. Leaders within these organizations were asked to personally invite potential participants whom they identified as having relevant experience. Potential research participants were required to contact the lead researcher, who determined eligibility and shared additional information, including an informed consent document. Like the focus groups, interviewees were encouraged to share information with their colleagues, to recruit additional participants through snowball sampling. Providers who were not licensed in Delaware and/or not currently affiliated with a maternity care hospital or birth center in the state were excluded. Interviews lasted approximately 30 to 60 minutes.
All focus groups and interviews were conducted by the lead researcher and recorded after securing informed consent from each participant (via an electronic REDCap survey). Data collection was facilitated using interview guides, which included high-level questions that were asked in all focus group meetings and all interviews, as well as prompts that varied depending on the nature of the conversations. This semi-structured approach allowed for flexibility and ensured that the key topics were covered in every session.25 Participants were encouraged (but not required) to turn on their video cameras. Zoom recordings were automatically transcribed and data were manually cleaned for analysis.
Data Analysis
Focus group transcripts were analyzed separately from the provider interviews, in order to be able to reflect upon the unique perspectives of each stakeholder group. Transcripts were analyzed using a combination of inductive and deductive approaches.23 First, the lead researcher reviewed transcripts and post-focus group reflection memos to develop an understanding of the key messages that emerged from focus group conversations.23 Data were then organized into categories which served as structured codes from which we were able to explore deeper meaning. This initial deductive analysis was informed by a review of relevant literature and the interview guide. The inductive analysis resulted in themes that emerged across all three focus groups, as well as findings that were unique to one or two groups.
While it is not uncommon for different ideas to emerge from different groups, the relatively small number of respondents may have limited the analysis. For instance, if the study had more participants, these relatively “unique” ideas may have been confirmed through additional focus group discussions, such that we could call them themes. Therefore, to explore whether there was agreement (or not) related to these unique ideas, member checking was added to our methodology. Member checking is an important qualitative method for establishing trustworthiness, whereby interpretations and conclusions are tested with study participants who have an opportunity to confirm, deny, or add to the interpretations.26 In addition to addressing potential limitations related to the number of respondents, member checking gave doulas an opportunity to provide additional comments, as appropriate; to build upon ideas described in the summary; and/or to raise concerns related to our interpretation of the focus group conversations. In this way, member checking is consistent with the team’s interest in ensuring the voices of doulas themselves are prioritized and respected.
The process of member checking involved sharing a draft report of preliminary findings with all participants and asking them to respond to the following questions27 by email, telephone, or zoom:
(1) Do our findings match your experience? (2) Do you want to change anything, or is there anything that you disagree with? And
(3) Do you want to add anything? Participants were given two weeks to respond and were sent one reminder. Three participants responded within the allotted time and their responses validated the findings. No new information was offered.
Provider interview transcripts were analyzed using the same combination of inductive and deductive approaches, resulting in themes that were evident across interviews. Member checking was deemed unnecessary, but to improve the trustworthiness of the study, a second investigator participated in the analysis.26 Specifically, the lead researcher and co-investigator jointly conducted the analysis, working together to discuss initial patterns, test alternate explanations, and refine the resulting themes. Through this process, we were able to creatively organize the data while maintaining rigor by reading and re-examining interview data, memos, and categories into assertions supported by data excerpts.28 Finally, the themes from both the focus groups and interviews are “supported by evidence from the data set in the form of excerpts from interviews that link the researchers’ assertions to what was said by speakers in interview contexts”.28 This connection between researcher interpretation and the data also increases the trustworthiness of the findings.
The research was approved by by the West Chester University Institutional Review Board.
48 Delaware Journal of Public Health - March 2024
RESULTS
The final sample of focus group participants consisted of 11 doulas, of which nine self-identified as “Black or African American,” one as “mixed” race, and one as “White”. Delaware’s three counties (New Castle, Kent, and Sussex) were represented in the sample. All participants had some type of formal training, including for example, from DONA (Doulas of North America) International, or from one of the community-based organizations in Delaware that received funding to train doulas through a mini-grant from DPH and DHMIC. Most were currently practicing the full continuum of doula care from prenatal through postpartum care. Most were relatively new to birth work (i.e., had started within the past five years) and two participants had recently gone through formal training but were not yet practicing at the time of the focus group. Finally, the majority of participants reported that they serve women of color.
The final sample of interviewees consisted of 12 licensed providers: six nurses, four physicians, and two certified nurse midwives. Six hospitals and/or healthcare systems were represented across all three Delaware counties. Four providers held positions that allowed them to participate in policy or practice at the state level (e.g., on a statewide committee or board), and three were formally trained as doulas, though were not currently practicing as doulas.
Findings are organized below according to three major categories: training, credentials, and competencies; logistical considerations for policy and practice change; and the whole care team—relationships between doulas and medical partners. Within each category, themes are expressed relying heavily on direct quotes from research participants to promote authenticity. Additional vignettes supporting the major themes can be seen in this paper’s supplemental appendix.
Category 1: Training, Credentials, and Competencies
Doulas participating in the focus groups had experience with many types of training programs, which covered a range of topics. Training format, length, and sponsoring organizations varied quite a bit, but focus group participants generally agreed that initial training, as well as ongoing professional development, is important for their practice. In conversations with licensed providers, it was clear that credentialing or certification, as well as training in specific skills and competencies, would lead to much higher acceptance of doulas in the hospital system. One such competency identified by study participants was cultural competence, with doulas emphasizing this as critically important for the population they serve. Providers also emphasized that race/ethnicity and socioeconomic status play a role in the lived experiences of birth parents when it comes to social support, expectations, and language barriers to name but three factors. Doulas can provide value in this regard, but effectively serving this population is not without challenges.
Theme 1: Cultural Competence and Supporting Vulnerable Populations
As most focus group participants identified as women of color, who primarily serve birthing people of color, in a predominantly white healthcare system, it was not surprising to find that cultural competence was identified as a critical training element for delivering quality care. Doula participants recognized that cultural competence training is essential for serving minority communities. As one doula explained, “It needs to be mandatory because the only way that people are really going to lean into that is if they are made aware.” Another focus group participant emphasized the importance of cultural competence when working with birthing people who come from communities already marginalized by structural inequities, arguing:
If you’re not made aware, or if you’re not familiar with it, if you’re not comfortable with information that’s out there, with the information that’s needed in order to properly serve, then you run the risk of literally causing more harm or more trauma in a person’s birth space.
Doulas expressed not only the need for such training but also the opportunity and benefits that cultural competence training affords. Additionally, participants recognized that cultural competence training should not be limited to issues of race or ethnicity, and that learning about other communities within the umbrella of cultural diversity are also important, including topics related to nontraditional families and transgender communities. The benefit of having doulas who are representative of the patients for whom they are providing care was also stressed. One participating provider connected this to training considerations, stating, “I think it’s really important too to make the training programs available to women from those communities so that people are being supported by other people within the community.”
Further, providers acknowledged that many of the birthing people who would be affected by potential policy change live in fear of the birth process. Thus, the doula becomes even more valuable for those birthing people from communities that have been marginalized and those with the highest risk of poor outcomes. The following interview vignettes show providers’ view of this value:
We have a very large population of people that either arrive with no prenatal care like they’re dumped off in the car, or they have folks that are severely underprivileged, severely underserved. They don’t have a lot of help, and sometimes they’re there by themselves. That’s where a good doula will earn her keep.
I think the real value in doulas in low-income populations is support. I mean, women are scared to give birth. And because of what they read and what they hear, and statistics, they are scared to give birth, and I think knowing that they have that support and have a doula is really important. And in my view, that’s probably the most important thing, just peace of mind.
49
Theme 2: Perspectives on Credentialing and Certification Policy
Participating doulas highlighted the idea that training should be comprehensive and include attention to reproductive health generally, and the full perinatal period (prenatal through postpartum). One doula explained, “I think you need a full spectrum training, something that kind of prepares you all the way from even preconception and fertility to postpartum.” Another participant elaborated:
Doula support doesn’t just start with labor, and pregnancy is a process… we typically start working with the client before, like at the beginning of their prenatal care. So that part is important. Knowing what’s normal, how a client can manage their health, and monitor their health in a way that it’s not like a last-minute emergency for something that could have been prevented.
Many focus group participants were relatively new to practicing as a doula and expressed concerns that they did not initially feel prepared to practice independently after participating in just one or two brief training programs. Several participants recognized the limitations of training and the value of practice as a complement to formal training. These points were also emphasized by licensed providers who discussed the specific skills and competencies that should be included in training. They stated that doula training should include both content and skill development and be broad in scope. Additionally, many doulas emphasized that learning is an ongoing process whereby opportunities for regular professional development are warranted.
While doula participants recognized the value of informal training, generational knowledge, and experience, none seemed to resist the idea of a certification process with formal training requirements. One doula explained, “We don’t want just anybody subscribing to and saying, ‘Yeah, I’m a doula.’ No, there absolutely does need to be some kind of certification.” However, when discussing specific training programs or sponsoring organizations, there was a clear sense that no one program was superior and that training requirements for state certification should be flexible and allow for different sponsoring organizations. While there was not a strong resistance to formal training as part of a certification process, there was a feeling that certification was a necessary hurdle but potentially in conflict with the culture and essence of doula work.
Licensed providers considered the point that certification or credentialing could lend credibility to doulas. In the words of one provider, “If [doulas are] going to get credibility in hospitals, particularly, there has to be a level of credentialing that needs to occur.” According to providers, the trustworthiness of doulas working in the hospital system would be increased by a standardized certification or credentialing process. Such a process would allow clinical care teams to feel safer and more accepting of working with doulas, as seen in these following vignettes:
From my perspective I think that doulas need to demonstrate a level of competency by having a certification from an organization ... they want to present themselves with the best credentials that they can, so that they can feel like they’re part of the team and so that they can be accepted as part of the team.
If everyone has ... at least the same certification ... you know they’ve met a certain level of competency. And you can feel safe that they are doing what they should be doing for the patient.
Category 2: Logistical Considerations for Policy & Practice Change
Should all doulas who aim to support birthing parents acquire the necesstary credentials and training, there are still logistical considerations that participating providers and doulas raised. Doulas often described their work as a calling or a mission to serve, which frequently translated into providing care to clients with limited means, resulting in limited income for doulas themselves. The added financial burden that may accompany certification training requirements was acknowledged by both doulas and licensed providers. Findings from focus groups and interviews also revealed concerns about the potential administrative burden of Medicaid billing and the need for more support in this area, particularly if the goal is to increase access to doula care.
Theme 1: Financial Considerations
Several doulas discussed financial stresses they face with their work, as well as the added financial burden that may accompany any certification training requirements. One doula even described this as an access issue, stating “I think there is a huge barrier to entry with training costs.” This concern was shared by providers, who presented the option of potentially covering certification and/or training fees:
I think what we’ve heard from the doulas that the certification is expensive. Some of them have said they haven’t gotten the certification because it’s expensive. If that’s the case, then the State could support that.
Doulas also identified the benefits that can come from addressing these financial concerns, as seen in the following vignettes:
We need to be able to sustain our own households because a lot of times as a doula, we can’t show up for our clients when we are being mentally drained and burnt out ourselves because we can’t even pay our own bills.
I have a lot of Black young women who would love a doula. A nineteen-year-old right now, and I looked at her, and I was like, ‘Listen, this is something that you need. This is not a luxury. This is a necessity’…. So, if we have more money being funneled into programs like this on top of having those who do have access to Medicaid, this is not an extra expense, but this is something that is a part of the package.
50 Delaware Journal of Public Health - March 2024
Licensed providers shared this concern, particularly regarding how doulas would be reimbursed. Providers discussed the nuance in care that doulas provide given the unique nature of childbirth and expressed apprehension surrounding the adequacy of compensation for that care. One provider explained that depending on the nature of the labor and delivery process, compensation could become complicated:
A labor can last a really long time 48, 56 hours. That doula may need to hand off to another doula. Does that mean that she misses out on reimbursement because she’s needed to do that hand off? ... And also, what does the postpartum coverage look like? ... Can we engage doulas to become postpartum doulas, and potentially help specifically like our first-time families, or those with the lower socioeconomic status? Or, again, just those without resources. I think that that would be an amazing thing to be able to explore.
Theme 2: Administrative and Legal Concerns And Assistance
Focus group discussions also revealed concerns about the potential administrative burden of Medicaid billing and the need for more support in this area, particularly if the goal is to increase access to care. One doula explained that administrative support is necessary to prevent the creation of additional barriers. Another discussed this support, and ease of billing requirements, in relation to equity and diversity in the workforce, arguing:
Historically, it’s been very challenging for people of color to get ahead when it comes to certain things…if for Medicaid billing [we] have to jump through hoops and file this paperwork that it’s ridiculous, and it’s just kind of another form of discrimination. And some people may say that it’s not, but it really is. It keeps us from achieving the goals that we really are set out to achieve. So, it would be nice if there were certain forms that need to be filled out… It needs to be minimum, and it needs to be very well compensated for all that we do.
When discussing these issues with licensed providers, ease of billing and administrative processes, and/or support for those processes was believed to be important. Additionally, providers suggested a proactive approach to legal concerns such as grievances and medical legal responsibility:
And there’s a lot of medical legal stuff going on there. So if you have a lay doula in the community, what’s the medical legal responsibility when they walk into the hospital because now the hospital takes responsibility to some degree. Unless by legislation you remove hospital responsibility, that’s a problem.
Category 3: The Whole Care Team—Relationships
Between Doulas and Medical Partners
Many licensed providers had relatively limited direct experience working with doulas but expressed a willingness to do so. Concerns they shared were usually based on a single negative experience or a story from a colleague. The nature of their experiences also varied depending on the circumstance, but
they were generally positive about the role and value of doulas. Discussions about working with other care providers also emerged in every doula focus group. Doula participants had a variety of experiences practicing alongside other licensed providers, and while some doulas recounted positive interactions, many described challenging relationships with other providers. This tension was typically perceived by doulas as being grounded in a lack of awareness and understanding of the role that they play. Still, all participants appeared genuinely interested in building positive working relationships, thereby improving quality of care and providing a better patient experience.
Theme 1: Building Cooperative and Collaborative Relationships
Focus group participants clearly saw themselves as part of a team with a single focus on ensuring a positive birth experience and outcome. One doula stated, “We are all here literally to do the same job. Get this baby first, and make sure that the birthing person is safe. Period. Period.” Another doula echoed this sentiment:
To be honest, we are all a team, the mother, the father, or whoever our support person is, the doctor, the nurse, the doula. We are all there for one particular thing, that is to make sure the baby comes out healthy. So, we are all together in this one hundred and fifty percent.
Licensed providers emphasized the importance of the doula’s presence on the care team to help connect patients to care by acting as a sort of interpreter or translator; someone who can promote better health literacy, and in doing so ensure the birthing person understands the information that providers are trying to communicate. One provider acknowledged that the doula can “serve as a liaison between the clinical providers, who kind of spit out a lot of medical jargon, and help to ensure that the birth parent understands what that jargon means, so that they can make an informed decision.” Another provider explained, “A doula is very valuable because they’re interacting with the patient; they’re in many ways a ‘go between’ between the patient and the medical team.”
According to doula focus group participants, providing licensed providers with training as well as opportunities to get to know doulas are ways to support relationship-building across the care team. Again, this was grounded in the perception that most providers simply did not understand the role that doulas play, including the value that doulas potentially offer in addressing health inequities. Doulas were generally optimistic about how both training and other relationship-building activities could support a more collaborative environment. Several participants suggested that strategies for getting to know one another better, outside the labor and delivery room, could be beneficial. For instance, as described by one doula:
I don’t want to call them ‘meet & greets,’ but something where providers are introduced to the role of doulas as well as meet doulas ... You actually sit down and talk to us. We can have an open back and forth discussion so everything can get laid out ... making sure that we come together, and having that open dialogue, I believe would be helpful.
51
Providers offered some of the same suggestions about ways that doulas and the clinical team can become more cooperative and better able to function together, such as meet-and-greets and other relationship-building opportunities. As one provider saw it, “If a doula is coming into the hospital, they should have some idea of the hospital system.” Others acknowledged that as doulas need to learn more about licensed providers and the way that the system currently functions, providers and hospital systems need to learn more about doulas. One provider explained, “You have to get together and be part of the community that’s caring for the patient.”
Finally, some licensed providers acknowledged that lack of awareness about the value of doulas (including lack of awareness of the evidence base regarding doulas) was a barrier to integration that could be addressed through education:
Start with educating the team and having that general understanding of ... the service that [doulas] provide, and fully understanding the benefits to it, and how we can partner together…. And once you understand it, then that’s how you would be able to form a partnership to be able to provide this service for the patients.
I think provider and care team education [is important] because there is definitely going to be a huge differing of opinions about doulas. And you know another thing in medicine that we view as the end all be all is evidencebased. So I know there’s evidence that doulas improve birth outcomes ... I think the medical community is always more likely to embrace things that [are] evidence-based so I think that really educating… would be really important.
Importantly, many participants recognized that relationshipbuilding, and especially trust-building, takes time. This suggests that meet-and-greets, while an important first step, may have limited value until practice becomes more common.
Theme 2: The Role of a Doula
As previously identified, doulas highlighted the need for education for other licensed providers to include building an understanding of the doula’s role as advocate for their client, particularly when working with communities who may feel marginalized in the healthcare system. Focus group conversations reflected an understanding of the need for such advocacy when supporting women of color, as they often experience a lack of power in relationships with their providers and a diminished ability to make decisions for themselves. Doulas can help address this power dynamic through their role as advocates.
Licensed providers also saw the role of the doula in this way. They expressed how doulas can help ensure the birthing person understands information that providers are sharing and empower them to ask questions when they do not understand, and to find and use their voice during labor and delivery. Providers see a particular value in the relationship between the birthing person and the doula, as this generates trust which helps to reduce fear and anxiety. One participant explained that doulas provide a “consistent presence of someone who is supportive, and who they trust and that the family trusts, which reduces the patient’s anxiety, reduces the patient’s fear, and it makes just for a calmer
birthing experience.” Another provider shared this sentiment by explaining how that trust between a doula and birthing person can also translate into more thoughtful decision-making:
If [doulas] develop a bond with a patient who’s scared… with the comfort of a doula that they know and says, “Okay, just remember, these were the things we talked about from pain control perspective. We talked about breathing, we talked about nitrous, we talked about IV medication, and we talked about the epidural,” in the moment when a nurse is saying, “Okay, your pain’s a 7 all of a sudden, are you thinking you want an epidural?” If you don’t have someone to kind of bring them back to what their full options are, they might take that as a suggestion instead [of a question].
Importantly, this support was not described as a replacement for other providers or in conflict with the role of other providers, but rather as extra support for the birthing person. One licensed provider described it like so:
I like to think of [the role of the doula] as social capital. Somebody to listen to what a provider may be saying, and a second ear at times, or to run things by, or to give primary advice to a mom. I think that works well in the labor process. It’s an extra level of support and comfort for that patient ... to help guide that mom if she needs to get to an obstetrician or if she doesn’t need to get to an obstetrician, or to run something by about the normalcy of certain findings.
Doulas echoed this sentiment, as seen in a quote from one doula who described her role in relation to licensed providers:
I’m not here to cut your pockets. I’m not here to undermine your authority. I’m not here to change, or even question your knowledge…you know your expertise. I’m just here to also offer extra because this is what the client is asking for.
DISCUSSION & PUBLIC HEALTH IMPLICATIONS
This study revealed valuable insights about what is needed to support increased access to quality doula care in Delaware—in terms of training and certification, logistical considerations, and relationship-building—from the perspective of key stakeholders. Previous research highlights areas of tension between doulas and licensed providers of maternal healthcare, as well as opportunities for promoting positive working relationships.7,16,17,29 Our research elicited similar concerns and challenges21,22; however, areas of agreement between these stakeholder groups highlighted in this paper provide a strong foundation for the state to move forward with policy and practice changes. Most notably, we heard both doulas and licensed providers share their commitment to doing what is best for their patients, and an interest in finding ways to ensure the delivery of quality care in a mutually supportive team environment. Grounded in this understanding, and in alignment with corroborating studies cited below, we offer a number of important considerations for state and healthcare system leaders.
52 Delaware Journal of Public Health - March 2024
First, while more research is needed to identify all the core competencies that should be included in doula training, any training required for Medicaid reimbursement should include the full spectrum of doula care, from prenatal to postpartum. Key competencies and skills, attained through structured training programs, are needed to improve access to quality doula care and integrate doulas into care teams. Further, continuing professional development for doulas may be warranted given their perception that competence is developed over time and through experience.30 Finally, cultural competence training should be an essential component of any training program that is required for doulas seeking Medicaid reimbursement.19,31
Certification is an important avenue for promoting quality care and it helps assure licensed providers that doulas are knowledgeable about pregnancy, childbirth, and postpartum care. In this way, certification may increase the perception of doulas’ legitimacy in the clinical setting and promote quality by building trust and respect across the care team.32 Doulas in our study also acknowledged the legitimacy that certification provided, even as they shared an understanding that it may be somewhat counter to the culture and essence of the care they provide. This is consistent with findings from Young,30 who reported that doulas may feel some ambivalence about certification; on one hand it legitimizes their role, but on the other the work of a doula does not require such validation. Some flexibility in training requirements, including allowing different training programs and/or sponsoring organizations, similar to many other states’ policies,14 may help address doula concerns about training and empower them to choose a program that most closely aligns with their approach to supporting birthing people. Financial support for doula training and certification should be considered, particularly as the state aims to improve outcomes for its most vulnerable populations.16,18
In addition to financial concerns related to training and certification, consideration of other logistical challenges is warranted. Stakeholders identified concerns related to doulas’ abilities to navigate the Medicaid reimbursement process. Training and ongoing technical assistance may be needed, and ease of processes should be prioritized.19 This is especially important for ensuring access to culturally competent care and promoting reimbursement for doulas of color, both of which are critical to addressing health inequities in birth outcomes. Further, this is consistent with research by Van Eijk and colleagues,33 who raised concerns that Medicaid reimbursement could potentially perpetuate systemic racism in the healthcare system if securing such reimbursement discouraged doulas of color from participating. Consideration may also need to be given to potential legal issues related to more fully integrating doulas into the hospital setting. To our knowledge this concern has not been identified in other research, but whether real or perceived, acknowledging and addressing these concerns from licensed providers may help to allay any persistent tension and ease the path to more positive relationship-building.
Our findings also suggest that consideration should be given to concerted efforts that support relation-building among doulas and other members of the care team. This includes opportunities for doulas to become better oriented to the systems within which they are working, as well as opportunities for licensed providers to become better acquainted with the role and value of doulas. Providers’ views of a doula’s role on the care team as a “liaison” or “bridge” is consistent with recent research in California, which found evidence of bidirectional feedback between doulas and licensed providers and noted that providers viewed doulas as a bridge to address gaps in care for pregnant and birthing people.34 Importantly, several providers in our study acknowledged that they found it difficult to build relationships with doulas when they only worked with them occasionally, which is consistent with research by Roth and colleagues,32 which found that nurses who worked with doulas more often had more positive perceptions of doulas. Therefore, education and relationship-building should be an ongoing process. There are many potential benefits of “meet-and-greets” and institutional orientations to help doulas and other licensed providers get to know each other. While hospital-based education and orientation sessions may be useful, state agencies and professional associations may have a role to play in promoting a positive culture for the integration of doulas on care teams, particularly as new doulas are trained and certified and/or new providers are established within the local healthcare system.19
Finally, it is important to acknowledge that the conclusions we have drawn from this study outlined above are based upon an appreciation of the critical role of stakeholder engagement in effective, equitable policymaking,24 and an assumption that diverse stakeholder perspectives should carry equal weight. Said differently, we aimed to identify areas of agreement between doulas and licensed providers and the considerations outlined above do not give preference to either voice. In clinical practice, however, the healthcare system is inherently hierarchical with physicians invariably possessing the greatest power in healthcare decision-making and the delivery of care.35 While potentially justified in the clinical setting given differential levels of training, care must be taken to ensure that this power imbalance does not permeate the boundaries of clinical practice. Specifically, as policymakers consider how to expand access to doula care and improve the birth experience for the communities they serve, the voices of doulas should be prioritized. Practically, this means that additional consideration should be given to finding ways to ensure doula representation in ongoing policymaking from planning through implementation. In addition, the perspectives of birthing people—especially those who experience health inequities—should be sought and included in future research and policy discussions.
LIMITATIONS
We believe this study generated valuable knowledge to inform the ongoing development of policies and practices to improve access to doula care among communities of
53
color and others at risk of poor birth outcomes. However, the research was not without limitations. First, the study included a relatively small number of doulas and those who participated were identified through established networks. Such networks were often connected to formal training programs, which means that the findings may not reflect perspectives of doulas who have not engaged in formal training. More research with a larger and potentially more diverse sample could offer additional insights.
In regard to the provider interviews, the sample was purposeful; while common in qualitative research the findings may not represent all varied perspectives of licensed providers in the state. Further, we did not collect demographic information about licensed providers (beyond provider type and affiliation) which limited any conclusions that could be drawn based on their race/ ethnicity. In addition, our analytical approach also did not allow researchers to draw conclusions based upon factors such as the type and gender of provider, location of service, length of time practicing, or other demographic information that may influence providers’ perceptions of doulas. Future investigations should aim for a more diverse sample given the focus of the state’s efforts to expand doula access particularly for birthing people of color and those from lowincome communities.
CONCLUSION
Given the potential of doulas to improve birth outcomes, reduce inequities, and lower costs, many states across the U.S. are exploring policy strategies, including Medicaid reimbursement, to increase access to doula care. For policy change to be most effective, leaders must resolve a number of questions related to doula training and certification, relationships among providers, and other practical issues. This study provides important insights about these questions from the perspective of doulas and licensed providers practicing in the state of Delaware. The findings from this work, particularly areas of agreement among stakeholders, provide a strong foundation for policymakers and healthcare organizations to move forward to ensure the delivery of the most accessible, high quality, and culturally competent care for birthing people in Delaware and beyond. Dr. Knight may be contacted at eknight@wcupa.edu
REFERENCES
1. Delaware Health Statistics Center, Delaware Department of Health and Social Services, Division of Public Health. (2023). Delaware Vital Statistics Annual Report Infant Mortality, 2020. https://www.dhss.delaware.gov/dhss/dph/hp/files////infant_ mortality20.pdf
2. Trost, S., Beauregard, J., Chandra, G., Njie, F., Berry, J., Harvey, A., & Goodman, D. (2022). Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 U.S. States, 2017-2019. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. https://www.cdc.gov/reproductivehealth/matertnal-mortality/erase-mm/ data-mmrc.html
3. Maternal and Child Death Review Commission. State of Delaware (2022). The Delaware Maternal and Child Death Review Commission 2022 Annual Report.
https://reviewtoaction.org/sites/default/files/2023-05/Delaware%20 2022%20Annual%20Report.pdf
4. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. (2023). Pregnancy Mortality Surveillance System, Centers for Disease Control and Prevention. Retrieved from
https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancymortality-surveillance-system.htm
5. Beck, A. F., Edwards, E. M., Horbar, J. D., Howell, E. A., McCormick, M. C., & Pursley, D. M. (2020, January). The color of health: How racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatric Research, 87(2), 227–234.
https://doi.org/10.1038/s41390-019-0513-6
6. Knight, E., McDonough, K., & Codes-Johnson, C. (2019). Health Equity Guide for Public Health Practitioners and Partners, Edition 2. Delaware Department of Health and Social Services.
https://dhss.delaware.gov/dhss/dph/mh/healthequityguide.html
7 Bohren, M. A. , Hofmeyr, G. J. , Sakala, C., Fukuzawa, R. K. , & Cuthbert , A. ( 2017 , July 6). Continuous support for women during childbirth. Cochrane Database Syst Rev , 7 (7 ), CD003766
https://doi.org/10.1002/14651858.CD003766.pub6
8. Falconi, A. M., Bromfield, S. G., Tang, T., Malloy, D., Blanco, D., Disciglio, R. S., & Chi, R. W. (2022, July 1). Doula care across the maternity care continuum and impact on maternal health: Evaluation of doula programs across three states using propensity score matching. EClinicalMedicine, 50(101531), 101531.
https://doi.org/10.1016/j.eclinm.2022.101531
9. Kozhimannil, K. B., Hardeman, R. R., Attanasio, L. B., BlauerPeterson, C., & O’Brien, M. (2013, April). Doula care, birth outcomes, and costs among Medicaid beneficiaries. American Journal of Public Health, 103(4), e113–e121.
https://doi.org/10.2105/AJPH.2012.301201
10. Knocke, K., Chappel, A., Sugar, S., De Lew, N., & Sommers, B. (2022). Doula care and maternal health: An evidence review (Issue Brief No. HP-2022-24). Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services.
https://aspe.hhs.gov/sites/default/files/documents/ dfcd768f1caf6fabf3d281f762e8d068/ASPE-Doula-IssueBrief-12-13-22.pdf
11. Guenther, G., Kett, P., Skillman, S., & Frogner, B. (2022). The birth doula workforce in the U.S.: Rapid response brief. Center for Health Workforce Studies, University of Washington. https://familymedicine.uw.edu/chws/publications/the-birth-doulaworkforce-in-the-u-s-rapid-response-brief/
54 Delaware Journal of Public Health - March 2024
12. Kozhimannil, K. B., Vogelsang, C. A., Hardeman, R. R., & Prasad, S. (2016, May-Jun). Disrupting the pathways of social determinants of health: Doula support during pregnancy and childbirth. J Am Board Fam Medicine, 29(3), 308–317. https://doi.org/10.3122/jabfm.2016.03.150300
13. Declercq, E. R., Sakala, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2014, Winter). Major Survey Findings of Listening to Mothers(SM) III: Pregnancy and Birth: Report of the Third National U.S. Survey of Women’s Childbearing Experiences. J Perinat Educ, 23(1), 9–16. https://doi.org/10.1891/1058-1243.23.1.9
14. National Health Law Program. (2022). Doula Medicaid Project. Retrieved from https://healthlaw.org/doulamedicaidproject/
15. Bohren, M. A., Berger, B. O., Munthe-Kaas, H., & Tunçalp, Ö. (2019, March 18). Perceptions and experiences of labour companionship: A qualitative evidence synthesis. Cochrane Database Syst Rev, 3(3), CD012449. https://doi.org/10.1002/14651858.CD012449.pub2
16. Bihn-Coss, G., & Egbert, N. (2023). Supporting in solidarity: An examination of social support, advocacy, and barriers among birth doulas. Communication Quarterly, 71(3), 243–267. https://doi.org/10.1080/01463373.2022.2164737
17. Neel, K., Goldman, R., Marte, D., Bello, G., & Nothnagle, M. B. (2019, June). Hospital-based maternity care practitioners’ perceptions of doulas. Birth (Berkeley, Calif.), 46(2), 355–361. https://doi.org/10.1111/birt.12420
18. Chen, A., & Robles-Fradet, A. (2020). Building a successful program for Medi-Cal coverage for doula care: Findings from a survey of doulas in California. National Health Law Program. https://healthlaw.org/resource/doulareport/
19. Everson, C., Crane, C., & Nolan, R. (2018). Advancing health equity for childbearing families in Oregon: Results of a statewide doula workforce needs assessment. Estacada, OR: Oregon Doula Association.
https://www.oregon.gov/oha/OEI/Documents/Doula%20Workforce%20 Needs%20Assesment%20Full%20Report%202018.pdf
20. Kozhimannil, K., Vogelsang, C., & Hardeman, R. (2015). Medicaid Coverage of Doula Services in Minnesota: Preliminary findings from the first year. Interim Report to the Minnesota Department of Human.
https://static1.squarespace.com/static/577d7562ff7c5018d6ea200a/t/58 40c791cd0f683f8477920a/1480640403710/FullReport.pdf
21. Knight, E. (2023). Doula stakeholder engagement: Focus group study report. Delaware Department of Health and Social Services, Division of Public Health.
https://dethrives.com/dhmic/committees-and-workgroups/doula-adhoc-committee#resources
22. Knight, E., & Rich, R. (2023). Doula stakeholder engagement: Report on interviews with licensed providers of maternal health care. Delaware Department of Health and Social Services, Division of Public Health. https://dethrives.com/dhmic/committees-and-workgroups/doula-adhoc-committee#resources
23. Patton, M. Q. (2002). Qualitative research and evaluation methods. Sage Publications.
24. Ford, T., & Goger, A. (2021). The value of qualitative data for advancing equity in policy. Brookings Institution. https://www.brookings.edu/articles/value-of-qualitative-data-foradvancing-equity-in-policy/
25. Bryman, A. (2004). Social research methods (2nd ed.). Oxford: Oxford University Press.
26. Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic Inquiry. Newbury Park, CA: Sage Publications.
27. Birt, L., Scott, S., Cavers, D., Campbell, C., & Walter, F. (2016, November). Member checking: A tool to enhance trustworthiness or merely a nod to validation? Qualitative Health Research, 26(13), 1802–1811.
https://doi.org/10.1177/1049732316654870
28. Roulston, K. (2010). Reflective interviewing: A guide to theory and practice. Los Angeles: SAGE. pp.151 & 153.
29. Lucas, L. & Wright, E. (2019). Attitudes of physicians, midwives, and nurses about doulas: A scoping review. Am J Matern Child Nurs, Jan/Feb;44(1):33-39. DOI:
https://doi.org/10.1097/NMC.0000000000000488
30. Young, C. (2021, May). Professional ambivalence among care workers: The case of doula practice. Health (London), 25(3), 306–321.
https://doi.org/10.1177/1363459319886115
31. Govere, L., & Govere, E. M. (2016, December). How effective is cultural competence training of health care providers on improving patient satisfaction of minority groups? A systematic review of the literature. Worldviews on EvidenceBased Nursing, 13(6), 402–410.
https://doi.org/10.1111/wvn.12176
32. Roth, L. M., Henley, M. M., Seacrist, M. J., & Morton, C. H. (2016, Nov-Dec). North American nurses’ and doulas’ views of each other. J Obstet Gynecol Neonatal Nurs, 45(6), 790–800.
https://doi.org/10.1016/j.jogn.2016.06.011
33. Van Eijk, M. S., Guenther, G. A., Kett, P. M., Jopson, A. D., Frogner, B. K., & Skillman, S. M. (2022, February 2). Addressing systemic racism in birth doula services to reduce health inequities in the United States. Health Equity, 6(1), 98–105. https://doi.org/10.1089/heq.2021.0033
34. Reed, R., Nguyen, A., Armstead, M., Cuentos, A., Mystic, M., Arcara, J., . . . Gomez, A. M. (2023). “An extra layer of pressure to be my best self”: Healthcare provider perspectives on how doulas foster accountability and bridge gaps in pregnancyrelated care. SSM. Qualitative Research in Health, 3, 1–8. https://doi.org/10.1016/j.ssmqr.2023.100259
35. Adams, C., & Curtin-Bowen, M. (2021, September). Countervailing powers in the labor room: The doula-doctor relationship in the United States. Soc Sci Med, 285, 114296. https://doi.org/10.1016/j.socscimed.2021.114296
55
APPENDIX
Categories, Themes, and Corresponding Vignettes from Doula Focus Groups & Licensed Provider Interviews
Category 1: Training, credentials, and competencies
Theme 1: Cultural competence and supporting vulnerable populations
Doula vignettes:
Regardless of the type of training that they’ve already taken, [doulas] absolutely should have some type of cultural competence training, and they should definitely be aware of how to support Black and brown people, especially since we have the highest rate of mortality in the state. You can’t properly serve any birthing people if you don’t know how to properly serve the ones that need the most support. So, if that’s not within the requirements of Medicaid reimbursement, then it’s definitely doing a disservice to the state, because a lot of our Black and brown families are using Medicaid.
If you’re not made aware, or if you’re not familiar with it, if you’re not comfortable with information that’s out there, with the information that’s needed in order to properly serve, then you run the risk of literally causing more harm or more trauma in a person’s birth space. She’s going to be able to support in a way that is needed, because she knows what’s going on, and she actually cares about what’s going on, because she sees it. I think a lot of the time people don’t see it and not because they don’t want to see it, because they can’t really relate to it. So, I think that should definitely be something added to the training so that they can understand what’s going on. This is not us just complaining or anything. This is really happening to our sisters here, and we’re dying at an alarming rate for things that could have been prevented.
In addition, there needs to be some kind of measure in place to show that the people are actually absorbing what is being taught to them, and not on a low level, but on a high level, because as I’ve mentioned before, about my nursing school textbooks… there is biased information still present in the book. So, if you have someone who is not familiar with people of color, and then they read whatever in the book, or they learn whatever, or they don’t learn whatever in a doula training, then they’re not necessarily going to get out here and know how to support people of color. So, I would definitely say, making sure that there’s some kind of teach back or test or something to make sure that they get it.
I’ve not yet worked with a trans person, and I would not take an opportunity to. I receive a person as a client, and say, ‘oh, sure I’ll be happy to come and help’ and use that as my opportunity to learn... That’s not the proper time to do that. We need to be aware. You need to be thoroughly aware of how to properly serve people from a different culture or a different background before you get into that space, because you don’t want to ever run the risk of affecting their dignity while they’re within that space.
Licensed provider vignettes:
So I do think that it’s really important to ensure that we have representation across the field – all fields in the medical industry, but that we’re also culturally humble when caring for the patient and really sensitive to the fact that we’re not able to speak for everyone, or assume culture and expectations, and all of those things for every person. So I do think that when it comes to black and brown women, or women specifically, who aren’t white, they [may] come to the table with post-traumatic experiences dealing with bias in health care. We’re getting a larger population of Hispanics and Creole, especially in the Lower Sussex County, especially with the chicken plants being here. I think it would be wonderful if we could help some of these patients, and if we were able to have some bilingual translators/doulas that would definitely make a difference. I think we have to look at it in the equity piece and access to care because sometimes they’ve not had any prenatal care at all. They’ve just arrived here a couple of days ago and come in and deliver not really knowing anything. So I think that if we had those doulas present that that would take away a lot of angst for those patients. It’s got to be pretty scary coming into a new country, a hospital, and not speaking the same language and our translation services that we have that are by phone, that a lot of them really don’t speak Creole. So that communication piece is not really happening, and it can be kind of scary, especially if they need a stat C section, and you’re not able to communicate … It pulls your heartstrings. With all the inequities that are still going on today, especially with black birthing people…I think it is another layer of support and care for them, particularly. I know there is a huge push nationwide because, really a lot of the doulas are within their community. These doulas look like them, and they can form relationships prior to coming into the hospital, especially if there were any complications going on, especially with the patients. They’re there, they have the full understanding and can really provide a lot of education and resources for these moms prior to coming into the hospital, during labor, and even post-delivery. I think that’s a real added benefit to for a lot of these moms.
I think the real value in doulas in low-income populations are support. I mean, women are scared to give birth. And because of what they read and what they hear, and statistics, and so they are scared to give birth, and I think, knowing that they have that support and have a Doula is really important. And in my view, that’s probably the most important thing right is just peace of mind. I think it’s the most important thing.
56 Delaware Journal of Public Health - March 2024
Doula vignettes:
I know after the first training I didn’t feel prepared really to serve the clients. It was only a two-day training and then we did some continuing education online. I really, honestly, I didn’t feel prepared afterward. I didn’t feel confident enough to go out and serve these clients. I didn’t feel like I knew enough. But as I started to practice, I did learn by doing.
So, training-wise, it’s important to not limit people to specific organizations just because they have bigger names. That’s actually dangerous for a doula, and for the people that they support as well.
We don’t want just anybody subscribing to and saying, Yeah, I’m a doula. No, there absolutely does need to be some kind of certification.
Licensed provider vignettes:
In that training has to be basic knowledge of pregnancy. I’m not talking, you know they don’t have to be at the level of a nurse, midwife, or anything like that, but a basic understanding of pregnancy, and a basic understanding of the process of labor, the options that patients have for different things in the labor process that can help them through the labor process. When is it time to say we’re done.
I think that doulas need to demonstrate a level of competency by having a certification from an organization such as DONA. And so they want to present themselves with the best credentials that they can, so that they can feel like they’re part of the team and so that they can be accepted as part of the team.
I ask them (other nurses), what are the things that you would want, and what are things that you don’t want, and all of them have said minimum standards. And so they either want a certification from something like DONA, or some kind of minimal qualifications. If everyone has ... at least the same certification ... you know they’ve met a certain level of competency. And you can feel safe that they are doing what they should be doing for the patient.
It cannot just be all OJT [on the job training]. There has to be a level of content in a classroom setting, whether it’s an online or whether it’s an in-person classroom setting where they can learn about childbirth. If they’re going to establish the level of trust, they have to understand the complications of childbirth…There needs to be information on, not heavy physiology and anatomy, but understanding the birth process.
1: Training, credentials, and competencies continued
Category
Theme 2: Perspectives on credentialing and certification policy
57
1: Financial considerations
Doula vignettes:
I think I think financial support is one of the biggest [challenges], because a lot of the black and brown women that I plan to support are from communities that are underserved. And so the doulas that are in those communities also may have a financial burden if they have to pay for [training], you know, extensive classes for doing what they just naturally do. So, I think that needs to be considered, because there’s some people that really cannot afford a doula, but they want a doula, and to be denied support like that because of finances, it’s just to me, that’s a travesty. And again, there are plenty of doulas who live in underserved communities, and financially may not have the money… one thousand five hundred dollars to take training…This is ridiculous.
We need to be able to sustain our own households because a lot of times as a doula, we can’t show up for our clients when we’re mentally drained and burnt out ourselves because we can’t even pay our own bills.
I have a lot of Black young women who would love a doula. A nineteen-year-old right now, and I looked at her, and I was like, ‘Listen, this is something that you need. This is not a luxury. This is a necessity. Let me show you. Here’s a resource so that you can be able to get this for free.’ So, if we have more money being funneled into programs like this on top of having those who do have access to Medicaid, this is not an extra expense, but this is something that is a part of the package.
Licensed provider vignettes:
Many of them are not businesspeople, right? This may be their first time having to go through a process like this, so I’d like it to be as simple as possible, and really be able to have a return on investment for the doulas in this community, because we are really trying to address disparities right? And likewise I think that they need to have an equitable income for these services. I think that we’ve learned some lessons in other states that have really looked at reimbursing doulas and we’ve seen that they’ve had some low salaries there, so that’s a concern for me as well.
A labor can last a really long time 48, 56 hours. That doula may need to hand off to another doula. Does that mean that she misses out on reimbursement because she’s needed to do that hand off? You know. Sometimes we may not be contacted by a pregnant person until later in their pregnancy, and so we may only be able to see them once or twice before they even go into labor. Or maybe they’re having a premature labor right? And so would that impact their reimbursement in a negative way?… And also, what does the postpartum coverage look like? We do have opportunities for postpartum care and when we’re thinking about maternal mental health and families that may not have a lot of resources. For example, maybe they don’t have a primary support person in their home. Maybe they have to go back to work early. Maybe they have a baby who’s had a NICU stay – on and on. What does that look like from a postpartum perspective? Can we engage doulas to become postpartum doulas, and potentially help specifically like our first-time families, or those with the lower socioeconomic status? Or, again, just those without resources. I think that that would be an amazing thing to be able to explore.
I think what we’ve heard from the doulas that the certification is expensive. Some of them have said they haven’t gotten the certification because it’s expensive. If that’s the case, then the State could support that. I think if there are – with accepting Medicaid again, I think there’s gonna be a lot of responsibility on documentation, record keeping, billing, to ensure that there is not any fraud. And so I think the doulas are going to need support with that. Yeah, how to how to document how to make sure that they have great a good accounting for the money trail there.
Theme 2: Administrative and legal concerns and assistance
Doula vignettes:
Historically, it’s been very challenging for people of color to get ahead when it comes to certain things…if for Medicaid billing [we] have to jump through hoops and file this paperwork that it’s ridiculous, and it’s just kind of another form of discrimination. And some people may say that it’s not, but it really is. It keeps us from achieving the goals that we really are set out to achieve. So, it would be nice if there were certain forms that need to be filled out… It needs to be minimum, and it needs to be very well compensated for all that we do. That’s [administrative support] very important, and I will say that I think it’s important to make sure that it doesn’t create a barrier, because I can see creating a barrier with it being too extensive or too much or not having adequate support to complete whatever needs to be completed…So, when it’s time, we can get out there and get it done. But yeah, definitely, having support for billing and adequate support, not just saying there’s support, but actual…like maybe aids showing like ‘click here.’ Do that, like actual things that walk people through the steps, and then having that support that’s available to teach as well. I think that’s extremely important.
Licensed provider vignettes:
A way to resolve like grievances, you know, like some sort of a responsible party within the State that can address any kind of concerns that are coming up, and you know, some way for that to be addressed if there is unsafe practices or something that’s happening. And there’s a lot of medical legal stuff going on there. So if you have a lay doula in the community, what’s the medical legal responsibility when they walk into the hospital because now the hospital takes responsibility to some degree. Unless by legislation you remove hospital responsibility, that’s a problem.
Category 2: Logistical considerations for policy & practice change
Theme
58 Delaware Journal of Public Health - March 2024
Category
Theme 1: Building cooperative and collaborative relationships
Doula vignettes:
We are all here literally to do the same job. Get this baby first, and make sure that the birthing person is safe. Period. Period. To be honest, we are all a team, the mother, the father, or whoever our support person is, the doctor, the nurse, the doula. We are all there for one particular thing, that is to make sure the baby comes out healthy. So, we are all together in this one hundred and fifty percent.
I don’t want to call them ‘meet & greets,’ but something where providers are introduced to the role of doulas as well as meet doulas ... You actually sit down and talk to us. We can have an open back and forth discussion so everything can get laid out ... making sure that we come together, and having that open dialogue, I believe would be helpful.
I think it should be required for medical providers to have some type of continuing education regarding what doulas do. Also, maternal and infant mortality - I think that they should be aware of that, and what’s actually going on, especially in their state. And I think that they should be aware that doulas are a part of the birth team.
Licensed provider vignettes:
[Doulas] can serve as a liaison between the clinical provider and you know those who kind of spit out a lot of medical jargon and help to ensure that the birth parent understands what that jargon means, so that they can make an informed decision. A doula is very valuable because they’re interacting with the patient; they’re in many ways a ‘go between’ between the patient and the medical team.
Start with educating the team and having that general understanding of ... the service that [doulas] provide, and fully understanding the benefits to it, and how we can partner together…. And once you understand it, then that’s how you would be able to form a partnership to be able to provide this service for the patients.
I think provider and care team education [is important] because there is definitely going to be a huge differing of opinions about doulas. And you know another thing in medicine that we view as the end all be all is evidence-based. So I know there’s evidence that doulas improve birth outcomes ... I think the medical community is always more likely to embrace things that [are] evidence-based so I think that really educating… would be really important.
Theme 2: The role of a doula
Doula vignettes:
I’m not here to cut your pockets. I’m not here to undermine your authority. I’m not here to change, or even question your knowledge… you know your expertise. I’m just here to also offer extra because this is what the client is asking for.
I would never argue with anybody else on the birth team, because then that’s causing more stress for my client, you know. So, I do it very respectively. If I do have to speak up about something, I ask questions, you know, and that’s just how I show up in the birth space in the hospital setting.
Licensed provider vignettes:
Doulas provide a consistent presence of someone who is supportive, and who they trust and that the family trusts, which reduces the patient’s anxiety, reduces the patient’s fear, and it makes just for a calmer birthing experience.
If [doulas] develop a bond with a patient who’s scared… with the comfort of a doula that they know and says, “Okay, just remember, these were the things we talked about from pain control perspective. We talked about breathing, we talked about nitrous, we talked about IV medication, and we talked about the epidural,” in the moment when a nurse is saying, “Okay, your pain’s a 7 all of a sudden, are you thinking you want an epidural?” If you don’t have someone to kind of bring them back to what their full options are, they might take that as a suggestion instead [of a question].
I like to think of [the role of the doula] as social capital. Somebody to listen to what a provider may be saying, and a second ear at times, or to run things by, or to give primary advice to a mom. I think that works well in the labor process. It’s an extra level of support and comfort for that patient ... to help guide that mom if she needs to get to an obstetrician or if she doesn’t need to get to an obstetrician, or to run something by about the normalcy of certain findings.
3: The whole care team: Relationship between doulas and medical partners
59

www.marphtc.pitt.edu
FIELD PLACEMENTS
Invaluable Resource for Organizations, Real World Experience for Public Health Students
Field placements (FP) embed graduate students in public health or health sciences in a public or non‐profit health organization, particularly one serving underserved areas and populations, to work on public health projects. These placements provide structured experiences that allow students to apply acquired knowledge and skills in a public health practice setting.
Does your organization need help with…
‐ launching a new program;
‐ delivering your health campaign to the public;
‐ breathing new life into a project;
‐ evaluating a specific program;
‐ collecting and analyzing data;
‐ planning public events; or
‐ research, design, and marketing?
Develop a project
When developing a project, consider how a student’s fresh perspective could help your team and what a student could learn from you.
*All projects must take place in the United States.
Submit a Request Form
Complete an FP Request Form and MAR‐PHTC will then contact you to review the project. https://pitt.co1.qualtrics.com/jfe /form/SV_1FidiMDeA0V2PfU

WHAT SUPERVISORS ARE SAYING…
The student’s placement was critical to the maintenance and growth of the POP Club for Kids at the Bridgeport Farmers Market. Her leadership helped to expose more children and their families to healthy fruits and vegetables that they may not have otherwise had.

‐Debbie W. placement supervisor

Interview applicants Start the project
MAR‐PHTC advertises the position and provides you student applications and contact information. You select students to interview and choose the student who best fits your needs.
Meet weekly with your student, set goals, and watch your plans come to fruition.
Having the student on site was tremendously helpful and successful! We wouldn't have been able to complete several projects within the organization. She was a productive member of the team and even was able to help us secure a funding opportunity!

‐Katie S. placement supervisor
v2023.02.01
marphtc@pitt.edu
I
Fact sheet developed by M. Kuzemchak as part of her FP.
60 Delaware Journal of Public Health - March 2024


WHAT HAPPENS NEXT?
Previous students have…
‐ Designed a monthly newsletter
‐ Prepared issue briefs
‐ Created a health messaging Tik Tok toolkit
‐ Advocated for state legislation that is now law
‐ Supported data analysis
‐ Updated a community health needs assessment
‐ Assisted with outbreak investigations
‐ Performed mosquito baiting
‐ Developed a podcast
What happens after a student is accepted? Who? When?
Planning meeting Site supervisor, student Prior to starting project
Complete school &/or departmental forms Site supervisor, student Prior to starting project
Completion of MAR‐PHTC forms
‐ FP Student Agreement
‐ FP Student Intake Form
‐ FP Site Supervisor Intake Form Site supervisor, student Prior to starting project
Progress meetings
Check‐in meetings
Site supervisor, student Weekly
MAR‐PHTC, student Project start & mid‐point
Complete project deliverables Student Within 1 year of start date
FP Post‐evaluation Site supervisor, student Conclusion of project
WHAT STUDENTS ARE SAYING…
[My placement] was a great experience!

Overall I learned a lot from...the program. This practicum allowed me to gain real world experience that I can to bring to my studies in my MPH program and can apply wherever my career in epidemiology takes me.
‐ Madelyn M.
University of Delaware College of Health Sciences MPH student
[My preceptor] provided me with all the resources I needed but gave me the autonomy to complete all my tasks/goals independently. I really grew as a public health professional this summer due to my field placement experience.
‐ Alexa M.
University of Pittsburgh School of Public Health MPH student

www.marphtc.pitt.edu I marphtc@pitt.edu
Fact
sheet designed by Z. Rana as part of her FP.
61
GLOBAL HEALTH MATTERS
INTERNATIONAL CENTER




$45 million USAID award goes to African HIV consortium
$45 million USAID award goes to African HIV consortium
By Susan Scutti
$45 million USAID award goes to African HIV consortium
$45 million USAID award goes to African HIV consortium
By Susan Scutti




The South African Medical Research Council (SAMRC) received a grant worth more than $45 million to implement the HIV Vaccine Innovation, Science, and Technology Acceleration in Africa (HIV-VISTA) program. SAMRC President and CEO and former Fogarty trainee, Dr. Glenda Gray guided the application process for this grant from the U.S. Agency for International Development (USAID).
The South African Medical Research Council (SAMRC) received a grant worth more than $45 million to implement the HIV Vaccine Innovation, Science, and Technology Acceleration in Africa (HIV-VISTA) program. SAMRC President CEO and former Fogarty trainee, Dr. Glenda Gray guided the application process for this grant from the U.S. Agency for International Development (USAID).
The South African Medical Research Council (SAMRC) received a grant worth more than $45 million to implement the HIV Vaccine Innovation, Science, and Technology Acceleration in Africa (HIV-VISTA) program. SAMRC President and CEO and former Fogarty trainee, Dr. Glenda Gray guided the application process for this grant from the U.S. Agency for International Development (USAID).
The South African Medical Research Council (SAMRC) received a grant worth more than $45 million to implement the HIV Vaccine Innovation, Science, and Technology Acceleration in Africa (HIV-VISTA) program. SAMRC President and CEO and former Fogarty trainee, Dr. Glenda Gray guided the application process for this grant from the U.S. Agency for International Development (USAID).
To compete for funding, Gray established the BRILLIANT consortium (BRinging Innovation to cLinical and Laboratory research to end HIV In Africa through New vaccine Technology). BRILLIANT, which includes scientists from eight African countries, will design and implement early-stage clinical trials of HIV vaccine immunogens and conduct laboratory analyses and epidemiological studies.
To compete for funding, Gray established the BRILLIANT consortium (BRinging Innovation to cLinical and Laboratory research to end HIV In Africa through New vaccine Technology). BRILLIANT, which includes scientists from eight African countries, will design and implement early-stage clinical trials of HIV vaccine immunogens and conduct laboratory analyses and epidemiological studies.
To compete for funding, Gray established the BRILLIANT consortium (BRinging Innovation to cLinical and Laboratory research to end HIV In Africa through New vaccine Technology). BRILLIANT, which includes scientists from eight African countries, will design and implement early-stage clinical trials of HIV vaccine immunogens and conduct laboratory analyses and epidemiological studies.
To compete for funding, Gray established the BRILLIANT consortium (BRinging Innovation to cLinical and Laboratory research to end HIV In Africa through New vaccine Technology). BRILLIANT, which includes scientists from eight African countries, will design and implement early-stage clinical trials of HIV vaccine immunogens and conduct laboratory analyses and epidemiological studies.
The consortium plans to test HIV vaccine concepts and advance the most promising candidates while working with existing scientific talent and community engagement channels in sub-Saharan Africa (SSA). As part of their SSAled HIV vaccine effort, consortium members plan to partner with policymakers, affected communities (including people living with HIV/AIDS), advocates, and communicators. A complementary goal of the consortium is to strengthen systems of collaboration throughout SSA while increasing career opportunities for promising regional scientists. One such scientist is Dr. Sophia Osawe, who has been working at the Institute for Human Virology in Nigeria (IHVN) for the past 16 years.
The consortium plans to test HIV vaccine concepts and advance the most promising candidates while working with existing scientific talent and community engagement channels in sub-Saharan Africa (SSA). As part of their SSAled HIV vaccine effort, consortium members plan to partner with policymakers, affected communities (including people living with HIV/AIDS), advocates, and communicators. A complementary goal of the consortium is to strengthen systems of collaboration throughout SSA while increasing career opportunities for promising regional scientists. One such scientist is Dr. Sophia Osawe, who has been working at the Institute for Human Virology in Nigeria (IHVN) for the past 16 years.
The consortium plans to test HIV vaccine concepts and advance the most promising candidates while working with existing scientific talent and community engagement channels in sub-Saharan Africa (SSA). As part of their SSAled HIV vaccine effort, consortium members plan to partner with policymakers, affected communities (including people living with HIV/AIDS), advocates, and communicators. A complementary goal of the consortium is to strengthen systems of collaboration throughout SSA while increasing career opportunities for promising regional scientists. One such scientist is Dr. Sophia Osawe, who has been working at the Institute for Human Virology in Nigeria (IHVN) for the past 16 years.
logy and immunology, writes, implements, and manages grants, and coordinates researchers and study participants. Osawe sees BRILLIANT as an opportunity “to develop more of my skills in the lab and in immunology, interact with other early career researchers, and just continue improving my ability to write grants and help implement studies in my community.”
logy and immunology, writes, implements, and manages grants, and coordinates researchers and study participants. Osawe sees BRILLIANT as an opportunity “to develop more of my skills in the lab and in immunology, interact with other early career researchers, and just continue improving my ability to write grants and help implement studies in my community.”
logy and immunology, writes, implements, and manages grants, and coordinates researchers and study participants. Osawe sees BRILLIANT as an opportunity “to develop more of my skills in the lab and in immunology, interact with other early career researchers, and just continue improving my ability to write grants and help implement studies in my community.”
logy and immunology, writes, implements, and manages grants, and coordinates researchers and study participants. Osawe sees BRILLIANT as an opportunity “to develop more of my skills in the lab and in immunology, interact with other early career researchers, and just continue improving my ability to write grants and help implement studies in my community.”
To date, a vaccine to sustainably control the HIV pandemic has been elusive. UNAIDS estimates that 1.3 million people became newly infected in 2022, with almost two-thirds of these new infections occurring in SSA. And while women and girls accounted for 50% of new infections globally, they accounted for 63% of all new infections in SSA. Already, there are twice as many young SSA women as men between the ages of 15 and 24 living with HIV, and they struggle to access treatment and prevention due to stigma and policies. BRILLIANT sees communities as a central part of its effort to design a pivotal HIV vaccine, and so it includes community representatives in all its decision-making bodies.
To date, a vaccine to sustainably control the HIV pandemic has been elusive. UNAIDS estimates that 1.3 million people became newly infected in 2022, with almost two-thirds of these new infections occurring in SSA. And while women and girls accounted for 50% of new infections globally, they accounted for 63% of all new infections in SSA. Already, there are twice as many young SSA women as men between the ages of 15 and 24 living with HIV, and they struggle to access treatment and prevention due to stigma and policies. BRILLIANT sees communities as a central part of its effort to design a pivotal HIV vaccine, and so it includes community representatives in all its decision-making bodies.
To date, a vaccine to sustainably control the HIV pandemic has been elusive. UNAIDS estimates that 1.3 million people became newly infected in 2022, with almost two-thirds of these new infections occurring in SSA. And while women and girls accounted for 50% of new infections globally, they accounted for 63% of all new infections in SSA. Already, there are twice as many young SSA women as men between the ages of 15 and 24 living with HIV, and they struggle to access treatment and prevention due to stigma and policies. BRILLIANT sees communities as a central part of its effort to design a pivotal HIV vaccine, and so it includes community representatives in all its decision-making bodies.
To date, a vaccine to sustainably control the HIV pandemic has been elusive. UNAIDS estimates that 1.3 million people became newly infected in 2022, with almost two-thirds of these new infections occurring in SSA. And while women and girls accounted for 50% of new infections globally, they accounted for 63% of all new infections in SSA. Already, there are twice as many young SSA women as men between the ages of 15 and 24 living with HIV, and they struggle to access treatment and prevention due to stigma and policies. BRILLIANT sees communities as a central part of its effort to design a pivotal HIV vaccine, and so it includes community representatives in all its decision-making bodies.
Experts believe it is crucial that HIV vaccine candidates be designed to neutralize virus types prevalent in the SSA region, where most new infections occur. Dr. Linda-Gail Bekker, a BRILLIANT scientist and a former Fogarty trainee who is now director and CEO of the Desmond Tutu HIV Centre and Health Foundation, commented, “Africa has borne an enormous burden of the HIV epidemic, and it is fitting that our continent plays a significant role in bringing an effective, affordable and accessible HIV vaccine to the world.”
Experts believe it is crucial that HIV vaccine candidates be designed to neutralize virus types prevalent in the SSA region, where most new infections occur. Dr. Linda-Gail Bekker, a BRILLIANT scientist and a former Fogarty trainee who is now director and CEO of the Desmond Tutu HIV Centre and Health Foundation, commented, “Africa has borne an enormous burden of the HIV epidemic, and it is fitting that our continent plays a significant role in bringing an effective, affordable and accessible HIV vaccine to the world.”
Experts believe it is crucial that HIV vaccine candidates be designed to neutralize virus types prevalent in the SSA region, where most new infections occur. Dr. Linda-Gail Bekker, a BRILLIANT scientist and a former Fogarty trainee who is now director and CEO of the Desmond Tutu HIV Centre and Health Foundation, commented, “Africa has borne an enormous burden of the HIV epidemic, and it is fitting that our continent plays a significant role in bringing an effective, affordable and accessible HIV vaccine to the world.”
Experts believe it is crucial that HIV vaccine candidates be designed to neutralize virus types prevalent in the SSA region, where most new infections occur. Dr. Linda-Gail Bekker, a BRILLIANT scientist and a former Fogarty trainee who is now director and CEO of the Desmond Tutu HIV Centre and Health Foundation, commented, “Africa has borne an enormous burden of the HIV epidemic, and it is fitting that our continent plays a significant role in bringing an effective, affordable and accessible HIV vaccine to the world.”
In her role at IHVN, Osawe, a former Fogarty Global Health Fellow who recently defended her PhD in medical microbio-
The consortium plans to test HIV vaccine concepts and advance the most promising candidates while working with existing scientific talent and community engagement channels in sub-Saharan Africa (SSA). As part of their SSAled HIV vaccine effort, consortium members plan to partner with policymakers, affected communities (including people living with HIV/AIDS), advocates, and communicators. A complementary goal of the consortium is to strengthen systems of collaboration throughout SSA while increasing career opportunities for promising regional scientists. One such scientist is Dr. Sophia Osawe, who has been working at the Institute for Human Virology in Nigeria (IHVN) for the past 16 years.
In her role at IHVN, Osawe, a former Fogarty Global Health Fellow who recently defended her PhD in medical microbio-
The BRILLIANT consortium also includes three other former Fogarty trainees and grant recipients: Osawe’s colleague at IHVN, Dr. Evaezi Okpokoro; Dr. Penny Moore of the National Institute for Communicable Diseases/University of Witwatersrand, South Africa; and Dr. Wilbert Mbuya of the National Institute for Medical Research, Tanzania.
The BRILLIANT consortium also includes three other former Fogarty trainees and grant recipients: Osawe’s colleague at IHVN, Dr. Evaezi Okpokoro; Dr. Penny Moore of the National Institute for Communicable Diseases/University of Witwatersrand, South Africa; and Dr. Wilbert Mbuya of the National Institute for Medical Research, Tanzania.
In her role at IHVN, Osawe, a former Fogarty Global Health Fellow who recently defended her PhD in medical microbio-
In her role at IHVN, Osawe, a former Fogarty Global Health Fellow who recently defended her PhD in medical microbio-


The BRILLIANT consortium also includes three other former Fogarty trainees and grant recipients: Osawe’s colleague at IHVN, Dr. Evaezi Okpokoro; Dr. Penny Moore of the National Institute for Communicable Diseases/University of Witwatersrand, South Africa; and Dr. Wilbert Mbuya of the National Institute for Medical Research, Tanzania.
The BRILLIANT consortium also includes three other former Fogarty trainees and grant recipients: Osawe’s colleague at IHVN, Dr. Evaezi Okpokoro; Dr. Penny Moore of the National Institute for Communicable Diseases/University of Witwatersrand, South Africa; and Dr. Wilbert Mbuya of the National Institute for Medical Research, Tanzania.
The Indian diaspora & global health
• India’s impact on global health


• India’s impact on global health
• Diaspora influence on clean cooking in India
• Diaspora influence on clean cooking in India
• Encouraging
• Encouraging knowledge circulation between India & the West
•
• Simplifying heart failure care in South Asia Read
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS JAN/FEB 2024 The Indian diaspora & global health • India’s impact on global health • Diaspora influence on clean cooking in India • Encouraging knowledge circulation between India & the West • Simplifying heart failure care in South Asia Read more on pages 6 – 9 GLOBAL HEALTH MATTERS Finding the connection between malaria and brain development ...p. 5
Photo courtesy of Sophia Osawe
www.fic.nih.gov
INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS JAN/FEB 2024
Dr. Sophia Osawe, a member of the BRILLIANT Consortium and former Fogarty Global Health Fellow, works at the international research center of the Institute of Human Virology in Nigeria.
FOGARTY
more
pages 6 – 9 GLOBAL HEALTH MATTERS Finding the connection between malaria and brain development ...p. 5
on
Photo courtesy of Sophia Osawe
member of the BRILLIANT Consortium and former Fogarty Global Health Fellow, works at the international research center of the Institute of Human Virology in Nigeria.
www.fic.nih.gov
•
INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS JAN/FEB 2024 The Indian diaspora & global health • India’s impact on global health • Diaspora influence on clean cooking in India • Encouraging knowledge circulation between India & the West • Simplifying heart failure care in South Asia Read more on pages 6 – 9
FOGARTY
NATIONAL
Finding the connection between malaria and brain development ...p. 5
Photo courtesy of Sophia Osawe
www.fic.nih.gov
INTERNATIONAL
• NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS JAN/FEB 2024
diaspora &
health
Dr. Sophia Osawe, a member of the BRILLIANT Consortium and former Fogarty Global Health Fellow, works at the international research center of the Institute of Human Virology in Nigeria.
FOGARTY
CENTER
The Indian
global
knowledge
between India & the West
circulation
in South Asia Read more on pages 6 – 9
Finding the connection between malaria and brain development ...p. 5
Simplifying heart failure care
GLOBAL HEALTH MATTERS
Photo courtesy of Sophia Osawe
Dr. Sophia Osawe, a member of the BRILLIANT Consortium and former Fogarty Global Health Fellow, works at the international research center of the Institute of Human Virology in Nigeria.
66 Read More on pages 67-70 62 Delaware Journal of Public Health - March 2024
FDA approves first chikungunya vaccine
By Susan Scutti
Ixchiq, the world’s first chikungunya vaccine, was approved by the U.S. Food and Drug Administration on November 9, 2023. The WHO describes chikungunya as a disease that causes fever and severe joint pain, often debilitating and varied in duration. Chikungunya, which is transmitted to humans by mosquitoes primarily in tropical and subtropical regions of Africa and Asia, and parts of the Americas, may also trigger joint swelling, muscle pain, headache, nausea, fatigue, and rash.
Ixchiq, also known as VLA1553, is produced by Valneva Austria GmbH, a specialty vaccine company based in Vienna, Austria.
“This virus can cause extensive outbreaks and significant morbidity,” Dr. Lesia K. Dropulic, Branch Chief, Clinical Trials Program, Vaccine Research Center (VRC) at the National Institute of Allergy and Infectious Diseases, told Fogarty. “The ability to prevent this, especially in parts of the world where the virus spreads endemically, is an important contribution to global public health.”
FDA approval of Ixchiq is based on Phase 3 clinical trial data in 4,115 adults “showing a 98.9% seroresponse rate at 28 days with a single vaccination,” according to Valneva. (In Phase 3 clinical trials a drug or vaccine is tested for efficacy and side effects; “seroresponse rate” is the percentage of people whose blood serum shows a developing antibody response capable of preventing infection.)
Ixchiq, which contains a live, weakened version of the chikungunya virus, is approved for individuals 18 years and older who are at increased risk of exposure to the virus, the FDA stated. Ixchiq is a single shot vaccine, injected into the muscle, that can cause symptoms similar to a chikungunya infection. Severe reactions occurred in 1.6% of recipients; some participants had prolonged adverse reactions that lasted for at least 30 days. The FDA requires that the company conducts a post-marketing study to assess the risk of adverse reactions. Prescribing information warns clinicians that it is unknown whether giving the shot to pregnant women can cause adverse effects in newborns.
Valneva, which develops, manufactures, and commercializes vaccines addressing unmet medical

needs, reported that the vaccine is currently under accelerated assessment by the European Medicines Agency (EMA), while a standard regulatory review is underway with Health Canada. “To make VLA1553 more accessible to low- and middle-income countries, Valneva and Instituto Butantan in Brazil signed an agreement in January 2021 for the development, manufacturing and marketing of VLA1553,” the company stated.
Dropulic noted that, previously, the Vaccine Research Center had worked on a separate chikungunya vaccine. “The VRC developed a viral like particle (VLP) vaccine that we evaluated in Phase 1 and Phase 2 trials during the 2015 outbreak in the Caribbean.” Bavarian Nordic, another global vaccine development company, headquartered in Denmark, is now advancing the clinical development of this product, known as CHIKV VLP. Currently in Phase 3 trials, CHIKV VLP has demonstrated a high seroresponse rate and fast onset of response, according to Bavarian Nordic, which plans to submit to regulatory authorities this year. CHIKV VLP has already received from FDA the Breakthrough Therapy and Fast Track designations (designed to expedite the development and review of drugs) and the PRIME designation from EMA (designed to enhance support for the development of medicines).
Given the progress achieved, the VRC is currently focusing its efforts on researching vaccines against other publicly significant mosquito-borne infections such as malaria, Zika, dengue, and West Nile Virus. Chikungunya was first identified in the United Republic of Tanzania in 1952 and subsequently in other countries in Africa and Asia, according to the WHO. Since 2004, the virus has been identified in over 110 countries in Asia, Africa, Europe and the Americas, while outbreaks have become more frequent and widespread. The FDA considers chikungunya an emerging global health threat with at least 5 million cases reported over the past 15 years.
JANUARY/FEBRUARY 2024 2
Photo courtesy of National Institute of Allergy and Infectious Diseases
Aedes mosquitoes, like the one shown here, can be vectors for the virus which causes chikungunya.
63
Research Roundup NOVEMBER 2023–JANUARY 2024
Between November 1, 2023, and January 31, 2024, Fogarty’s Division of International Epidemiology and Population Studies published studies on a range of topics related to domestic and international health in peer-reviewed journals.

Impact of cookstove use on rates of severe infant pneumonia Fogarty’s Dr. Joshua Rosenthal contributed to this analysis published in the New England Journal of Medicine. The Household Air Pollution Intervention Network (HAPIN) trial team compared rates of severe infant pneumonia in households using traditional cookstoves, which use biomass fuels (wood, dung, or agricultural waste) versus those using liquefied petroleum gas (LPG) cookstoves. There was no significant difference in severe pneumonia between the intervention group (LPG stoves) and the control group (traditional stoves), despite achieving major reductions in exposure to cooking smoke during the 18-month intervention period.
Article title: Liquefied Petroleum Gas or Biomass Cooking and Severe Infant Pneumonia
Does changing to clean cookstoves reduce the risk of stunting in infants? A related paper co-authored by Rosenthal appeared in the New England Journal of Medicine. The HAPIN team explored whether replacing biomass fuels with LPG cookstoves could reduce the risk of stunted growth in infants. (Stunting has been linked to household air pollution.) Personal exposure to fine particulate matter was monitored starting at pregnancy and continued until children were 12 months old, at which time the length of each infant was measured. The intervention resulted in lower prenatal and postnatal exposures to fine particulate matter compared to controls. Stunting occurred in 27.4% of infants born to women in the intervention group and in 25.2% of those born to women in the control group.
Article title: Effects of Cooking with Liquefied Petroleum Gas or Biomass on Stunting in Infants
Using multiple models is best for long-term disease outbreak projections Samantha Bents, a Fogarty research intern, and Fogarty’s Dr. Cécile Viboud contributed to this study, which suggests that a collection of models that preserves variation between models is consistently more reliable than any single model for longer-term projections of disease outbreaks.
Article title: Evaluation of the US COVID-19 Scenario Modeling Hub for informing pandemic response under uncertainty, Publication: Nature Communications
Lessons learned by the COVID-19 Scenario Modeling Hub A second paper co-authored by
Bents and Viboud describes the history of, and lessons learned from, the US COVID-19 Scenario Modeling Hub’s collective research effort.
Article title: The US COVID-19 and Influenza Scenario Modeling Hubs: Delivering long-term projections to guide policy, Publication: Epidemics
COVID-19 masking & behavior changes reduced RSV rates in South Africa Bents and Viboud coauthored this study that looked at how the use of nonpharmaceutical interventions to reduce SARS-CoV-2 transmission affected the circulation of respiratory syncytial virus in South Africa in 2020-2021.
Article title: Modeling the impact of COVID-19 nonpharmaceutical interventions on respiratory syncytial virus transmission in South Africa, Publication: Influence and Other Respiratory Viruses
Cross-species data is useful when designing flu vaccines This study co-authored by Fogarty’s Dr. Nidia Trovão and Dr. Josh Cherry uncovered surprising features of the evolution of influenza A virus hemagglutinin protein sequences that could inform vaccine evaluation and design.
Article title: Comparative evolution of influenza A virus H1 and H3 head and stalk domains across host species
Publication: mBio
Multiple trait subsampling improves suboptimal datasets Trovão and co-authors determined that including as many traits as possible when subsampling genetic data contained in large datasets is the best strategy to mitigate bias and optimize a dataset for analysis.
Article title: Optimizing ancestral trait reconstruction of large HIV Subtype C datasets through multiple-trait subsampling, Publication: Virus Evolution
Profile of cohort for SARS-CoV-2 study in Costa Rica Fogarty’s Dr. Kaiyuan Sun co-authored this paper describing participant recruitment, initial phase, and future goals of the RESPIRA study evaluating immune response to SARS-CoV-2 in Costa Rica.
Article title: Cohort profile: evaluation of immune response and household transmission of SARS-CoV-2 in Costa Rica: the RESPIRA study, Publication: BMJ Open
3 JANUARY/FEBRUARY 2024
Image generated using Adobe Firefly
64 Delaware Journal of Public Health - March 2024

PROFILE
Finding causes of heart failure in Western Kenya
Finding causes of heart failure in Western Kenya
Finding causes of heart failure in Western Kenya
When Fogarty first launched its Global Health Fellows and Scholars Program, now known as Launching Future Leaders in Global Health Research Training Program (LAUNCH), in 2004, many candidates were focused on some combination of HIV/AIDS, public health, or infectious disease research. Yet, as the cohorts grew, so did the diversity of specialties. An example is Dr. Gerald Bloomfield, who joined the Fogarty program in 2009 as a member of the first group of cardiologist fellows. This original cohort of heart doctors paved the way for other cardiologists to enter the program.
When Fogarty first launched its Global Health Fellows and Scholars Program, now known as Launching Future Leaders in Global Health Research Training Program (LAUNCH), in 2004, many candidates were focused on some combination of HIV/AIDS, public health, or infectious disease research. Yet, as the cohorts grew, so did the diversity of specialties. An example is Dr. Gerald Bloomfield, who joined the Fogarty program in 2009 as a member of the first group of cardiologist fellows. This original cohort of heart doctors paved the way for other cardiologists to enter the program.
When Fogarty first launched its Global Health Fellows and Scholars Program, now known as Launching Future Leaders in Global Health Research Training Program (LAUNCH), in 2004, many candidates were focused on some combination of HIV/AIDS, public health, or infectious disease research. Yet, as the cohorts grew, so did the diversity of specialties. An example is Dr. Gerald Bloomfield, who joined the Fogarty program in 2009 as a member of the first group of cardiologist fellows. This original cohort of heart doctors paved the way for other cardiologists to enter the program.
The premise of Bloomfield’s Fogarty project was to search for markers of atherosclerosis in heart failure patients in Western Kenya. At that time, atherosclerosis, a buildup of plaque and cholesterol on the wall of the arteries, wasn't thought to be a common cause of heart disease or heart failure in places like Kenya. His team conducted a casecontrolled study of patients with and without heart failure. They found that the most common causes of heart failure in the region, including untreated high blood pressure, matched precisely what was described in the literature. However, amongst men, markers of atherosclerosis were the second most common cause of heart failure in the 300 study participants. Bloomfield said, “While atherosclerosis certainly is not the number one cause of heart failure in Western Kenya, it is becoming much more common than it was decades ago.”
The premise of Bloomfield’s Fogarty project was to search for markers of atherosclerosis in heart failure patients in Western Kenya. At that time, atherosclerosis, a buildup of plaque and cholesterol on the wall of the arteries, wasn't thought to be a common cause of heart disease or heart failure in places like Kenya. His team conducted a casecontrolled study of patients with and without heart failure. They found that the most common causes of heart failure in the region, including untreated high blood pressure, matched precisely what was described in the literature. However, amongst men, markers of atherosclerosis were the second most common cause of heart failure in the 300 study participants. Bloomfield said, “While atherosclerosis certainly is not the number one cause of heart failure in Western Kenya, it is becoming much more common than it was decades ago.”
The premise of Bloomfield’s Fogarty project was to search for markers of atherosclerosis in heart failure patients in Western Kenya. At that time, atherosclerosis, a buildup of plaque and cholesterol on the wall of the arteries, wasn't thought to be a common cause of heart disease or heart failure in places like Kenya. His team conducted a casecontrolled study of patients with and without heart failure. They found that the most common causes of heart failure in the region, including untreated high blood pressure, matched precisely what was described in the literature. However, amongst men, markers of atherosclerosis were the second most common cause of heart failure in the 300 study participants. Bloomfield said, “While atherosclerosis certainly is not the number one cause of heart failure in Western Kenya, it is becoming much more common than it was decades ago.”
During his fellowship in Kenya, Bloomfield observed an epidemic of heart failure and high blood pressure and quickly realized there was a lack of expertise available. To address these issues, he and his mentors developed a Cardiovascular Center of Excellence to conduct research, provide multidisciplinary training, and enhance care delivery for heart disease patients.
During his fellowship in Kenya, Bloomfield observed an epidemic of heart failure and high blood pressure and quickly realized there was a lack of expertise available. To address these issues, he and his mentors developed a Cardiovascular Center of Excellence to conduct research, provide multidisciplinary training, and enhance care delivery for heart disease patients.
During his fellowship in Kenya, Bloomfield observed an epidemic of heart failure and high blood pressure and quickly realized there was a lack of expertise available. To address these issues, he and his mentors developed a Cardiovascular Center of Excellence to conduct research, provide multidisciplinary training, and enhance care delivery for heart disease patients.
He and his colleagues also found an interesting overlap with heart failure among people living with HIV who had well-controlled disease, something he went on to study in 2011 through a Fogarty International Research Scientist Development Award with additional funding from the National Heart, Lung, and Blood Institute. In Western Kenya, he continues this research by investigating subclinical cardiac dysfunction—heart conditions that might be asymptomatic or undetected by the usual clinical
He and his colleagues also found an interesting overlap with heart failure among people living with HIV who had well-controlled disease, something he went on to study in 2011 through a Fogarty International Research Scientist Development Award with additional funding from the National Heart, Lung, and Blood Institute. In Western Kenya, he continues this research by investigating subclinical cardiac dysfunction—heart conditions that might be asymptomatic or undetected by the usual clinical
He and his colleagues also found an interesting overlap with heart failure among people living with HIV who had well-controlled disease, something he went on to study in 2011 through a Fogarty International Research Scientist Development Award with additional funding from the National Heart, Lung, and Blood Institute. In Western Kenya, he continues this research by investigating subclinical cardiac dysfunction—heart conditions that might be asymptomatic or undetected by the usual clinical



Fogarty Fellow: 2009-2010
Gerald Bloomfield, MD, MPH
Fogarty Fellow: 2009-2010
U.S. institutions: Duke University, Brown University
Fogarty Fellow: 2009-2010
U.S. institutions: Duke University, Brown University
Foreign institution: Moi Teaching Hospital, Eldoret, Kenya
U.S. institutions: Duke University, Brown University
Foreign institution: Moi Teaching Hospital, Eldoret, Kenya
Research topic: The cross-section between HIV and heart disease
Foreign institution: Moi Teaching Hospital, Eldoret, Kenya
Research topic: The cross-section between HIV and heart disease
Research topic: The cross-section between HIV and heart disease
Current affiliation: Associate professor, with tenure, at Duke University School of Medicine and associate research professor at the Duke Global Health Institute
Current affiliation: Associate professor, with tenure, at Duke University School of Medicine and associate research professor at the Duke Global Health Institute
Current affiliation: Associate professor, with tenure, at Duke University School of Medicine and associate research professor at the Duke Global Health Institute
tests—among people living with HIV, including children and adolescents with perinatal (pre-birth) HIV infection.
tests—among people living with HIV, including children and adolescents with perinatal (pre-birth) HIV infection.
tests—among people living with HIV, including children and adolescents with perinatal (pre-birth) HIV infection.
His work in Kenya continues, yet Bloomfield also applies what he has learned globally to local settings in the United States. He currently leads a project looking at best practices in heart disease care for people living with HIV in the Southern U.S., working to understand when and how a cardiologist should get involved in their care and what types of referrals and consultations would be required. Additionally, Bloomfield is heading a study in rural areas of Southern U.S. that uses noninvasive imaging to study heart function and detect early dysfunction. When he is not involved with research, Bloomfield continues his work at Duke University as a clinician and as an associate professor in the department of medicine with a secondary appointment in the Global Health Institute, where he teaches a master’s level course in noncommunicable diseases in low- and-middle-income countries.
His work in Kenya continues, yet Bloomfield also applies what he has learned globally to local settings in the United States. He currently leads a project looking at best practices in heart disease care for people living with HIV in the Southern U.S., working to understand when and how a cardiologist should get involved in their care and what types of referrals and consultations would be required. Additionally, Bloomfield is heading a study in rural areas of Southern U.S. that uses noninvasive imaging to study heart function and detect early dysfunction. When he is not involved with research, Bloomfield continues his work at Duke University as a clinician and as an associate professor in the department of medicine with a secondary appointment in the Global Health Institute, where he teaches a master’s level course in noncommunicable diseases in low- and-middle-income countries.
His work in Kenya continues, yet Bloomfield also applies what he has learned globally to local settings in the United States. He currently leads a project looking at best practices in heart disease care for people living with HIV in the Southern U.S., working to understand when and how a cardiologist should get involved in their care and what types of referrals and consultations would be required. Additionally, Bloomfield is heading a study in rural areas of Southern U.S. that uses noninvasive imaging to study heart function and detect early dysfunction. When he is not involved with research, Bloomfield continues his work at Duke University as a clinician and as an associate professor in the department of medicine with a secondary appointment in the Global Health Institute, where he teaches a master’s level course in noncommunicable diseases in low- and-middle-income countries.
Bloomfield credits his Fogarty fellowship as the stepping stone to where he is today and welcomes opportunities to give back. Since his own fellowship in 2009, he has mentored several of the dozens of cardiologists who have gone through the program. “It’s been fantastic to see prior mentees now leading noncommunicable disease programs, holding academic positions, and doing public health work internationally and in the U.S.,” said Bloomfield. “Fogarty fellows are very engaged and passionate about their work, and it’s been great to help them get to the next stage in their career.”
Bloomfield credits his Fogarty fellowship as the stepping stone to where he is today and welcomes opportunities to give back. Since his own fellowship in 2009, he has mentored several of the dozens of cardiologists who have gone through the program. “It’s been fantastic to see prior mentees now leading noncommunicable disease programs, holding academic positions, and doing public health work internationally and in the U.S.,” said Bloomfield. “Fogarty fellows are very engaged and passionate about their work, and it’s been great to help them get to the next stage in their career.”
Bloomfield credits his Fogarty fellowship as the stepping stone to where he is today and welcomes opportunities to give back. Since his own fellowship in 2009, he has mentored several of the dozens of cardiologists who have gone through the program. “It’s been fantastic to see prior mentees now leading noncommunicable disease programs, holding academic positions, and doing public health work internationally and in the U.S.,” said Bloomfield. “Fogarty fellows are very engaged and passionate about their work, and it’s been great to help them get to the next stage in their career.”
4
PROFILE
4
PROFILE
4
65
A&Q
CHANDY C. JOHN, MD, MS
Dr. Chandy C. John is the director of the Ryan White Center for Pediatric Infectious Disease and Global Health at Indiana University School of Medicine. A practicing clinician, he also conducts research and training programs in Kenya and Uganda, focusing on malaria pathogenesis, immunology, and epidemiology. John served as the president of the American Society of Tropical Medicine and Hygiene in 2019. He currently serves on the Thrasher Research Scientific Advisory Board and Fogarty Advisory Board and is a member of the American Academy of Pediatrics’ Committee on Infectious Diseases. His authorship includes more than 250 peer-reviewed scientific publications and 30 book chapters in addition to published poems, essays, and short stories.
Tell us about your study of malaria and neurobehavioral development.
We don’t have final results yet, but I can tell you that the preliminary data are quite clear in showing that severe malaria affects cognition long-term. Children with severe malaria have lower cognitive scores for a long time afterwards, and this seems to be largely limited to cerebral malaria and severe malarial anemia. The other forms of severe malaria don’t seem to have the same strength of effect as those two, which is what we found in a previous study as well.
We have also looked at whether severe malaria in a child affects the economic productivity of their household. If the child has impairment or repeated episodes of malaria that may play into the family not doing well because of disruptions in work. Early results show that severe malaria does affect economic productivity of a household longterm. So that’s another important outcome. We’ve done a lot of analysis, so these preliminary results are unlikely to change.
Has serving on Fogarty’s board helped advance your knowledge?
Absolutely. I really enjoy being on the board because members are deliberately chosen to include not only researchers, but also people who work in public health and related areas of global health. People who are experts in education, people who work at societies and professional organizations. It’s a very broad range of expertise, deliberately chosen so that Fogarty gets the best input from people with different expertise in global health. I’ve learned a lot from the other researchers on the board, but also from people across all fields about how they evaluate questions of global health significance. Also, at the open board meetings we have experts from all over, including the heads of various NIH institutes, come in and talk to us about their global health priorities. They get input from us on what we think

might be important for global health in their particular area. And that's really great too.
What role does collaboration play in your work?
Great work gets done because of great collaborators and a great team, and I have the best. My key collaborators at Indiana University are Drs. Andrea Conroy, Dibya Datta, Nathan Schmidt, Prasida Holla, and Giselle Lima-Cooper. My primary collaborators at Makerere University are Drs. Ruth Namazzi, Robert Opoka, Paul Bangirana, Anthony Batte, and Richard Idro, who’ve led the way for many of our studies and taught me a lot. Four of my key collaborators in Uganda (Namazzi, Opoka, Bangirana, and Batte) have received Fogarty fellowships, while Idro is a joint principal investigator with me on our Fogarty training grant for Ugandan students and post-doctoral fellows.
Though we focused on my work in Uganda in this interview, I’ve also worked in Kenya with the Kenya Medical Research Institute, Moi University, and Jaramogi Oginga Odinga University (JOOU) studying the effect of malaria transmission on immunity. My chief collaborator at JOOU has been Dr. George Ayodo. Fogarty-supported training has also been critical for that work, including support of a former student and current collaborator, Dr. Bartholomew Ondigo of Egerton University. So, this incredibly strong Fogarty connection has been key to advancing research capacity and strength in our programs.
What’s ahead for you?
I’m excited about a new project called “SMART Brain,” short for Severe Malaria And Risk to the Brain, that will use mobile MRIs in Uganda to look at the brain in children with severe malarial anemia who have long-term cognitive impairment. The addition of MRI, along with EEG and transcranial Doppler testing, to our established tests should enable us to really delve into what leads to brain injury in severe malaria.
5
66 Delaware Journal of Public Health - March 2024
FOCUS
India’s impact on global health
India’s impact on global health
By
By Mariah Felipe
WWith the largest population in the world (over 1.4 billion citizens) India also boasts one of the largest diaspora populations. More than 18 million Indians lived abroad in 2022, according to the UN World Migration Report. India’s diaspora reflects the nation’s rich and diverse cultural heritage and provides an invaluable bridge between home and host societies.


ith the largest population in the world (over 1.4 billion citizens) India also boasts one of the largest diaspora populations. More than 18 million Indians lived abroad in 2022, according to the UN World Migration Report. India’s diaspora reflects the nation’s rich and diverse cultural heritage and provides an invaluable bridge between home and host societies.
Members of the diaspora have built transnational networks connecting cultural, social, and economic interests that impact almost every sector from business to engineering, health care, research, and global health initiatives worldwide.
Members of the diaspora have built transnational networks connecting cultural, social, and economic interests that impact almost every sector from business to engineering, health care, research, and global health initiatives worldwide.
When it comes to the world of global health and medicine, India is a powerhouse. According to NIH World Report, since 2016 more than 4,300 health research studies have been funded in India by some of the world’s largest biomedical research funders, including NIH, the European Commission, Institut Pasteur, and the Japan Agency for Medical Research and Development, among others. Between 2022 and 2023, Fogarty funded over 30 studies in the country covering such diverse topics as eye health, mental health, environmental exposures, women’s health, and more.
When it comes to the world of global health and medicine, India is a powerhouse. According to NIH World Report, since 2016 more than 4,300 health research studies have been funded in India by some of the world’s largest biomedical research funders, including NIH, the European Commission, Institut Pasteur, and the Japan Agency for Medical Research and Development, among others. Between 2022 and 2023, Fogarty funded over 30 studies in the country covering such diverse topics as eye health, mental health, environmental exposures, women’s health, and more.
India also plays a major global role in vaccine and pharmaceutical manufacturing. The nation supplies 60% of the world’s vaccines and exports vaccines to more than 170 countries globally, earning India the title, “the world’s pharmacy.” Having these capabilities allowed India’s Serum Institute to manufacture the Oxford-AstraZeneca vaccine in the country during the COVID-19 pandemic through the COVAX program, widely expanding vaccine access to lowerincome economies.
India also plays a major global role in vaccine and pharmaceutical manufacturing. The nation supplies 60% of the world’s vaccines and exports vaccines to more than 170 countries globally, earning India the title, “the world’s pharmacy.” Having these capabilities allowed India’s Serum Institute to manufacture the Oxford-AstraZeneca vaccine in the country during the COVID-19 pandemic through the COVAX program, widely expanding vaccine access to lowerincome economies.
Dr. Nandini Kumar, president of India’s Forum for Ethics Review Committees and distinguished scientist chair at India’s Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy (AYUSH), notes that as India’s economy continues to grow alongside its positive reputation in health care, there has been an influx of non-Indians as well as Indians returning to the country to study and conduct research across various fields.
Dr. Nandini Kumar, president of India’s Forum for Ethics Review Committees and distinguished scientist chair at India’s Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy (AYUSH), notes that as India’s economy continues to grow alongside its positive reputation in health care, there has been an influx of non-Indians as well as Indians returning to the country to study and conduct research across various fields.
India’s traditions of Ayurveda, yoga, and other holistic health practices, managed by AYUSH, gives the country a unique place in the global health space. The combination of these practices, along with conventional Western medicine, has started to gain a larger influence in India and beyond. AYUSH released official guidelines for remedies to treat mild to moderate COVID-19 in 2021, and a recent publication in the British Journal of Dermatology highlighted successful Ayurvedic treatments for filariasis, a disease caused by mosquito-borne parasitic infection, and lymphedema, swelling in the arms or legs due to a buildup of lymph fluid.
India’s traditions of Ayurveda, yoga, and other holistic health practices, managed by AYUSH, gives the country a unique place in the global health space. The combination of these practices, along with conventional Western medicine, has started to gain a larger influence in India and beyond. AYUSH released official guidelines for remedies to treat mild to moderate COVID-19 in 2021, and a recent publication in the British Journal of Dermatology highlighted successful Ayurvedic treatments for filariasis, a disease caused by mosquito-borne parasitic infection, and lymphedema, swelling in the arms or legs due to a buildup of lymph fluid.
As India and its diaspora gain more influence globally, the country continues to engage in health diplomacy by collaborating with international organizations and participating in global health initiatives. Serving as the home base for WHO’s South-East Asia chapter, India leads the region in developing public health guidelines that are appropriate and adaptable in the South Asian context.
As India and its diaspora gain more influence globally, the country continues to engage in health diplomacy by collaborating with international organizations and participating in global health initiatives. Serving as the home base for WHO’s South-East Asia chapter, India leads the region in developing public health guidelines that are appropriate and adaptable in the South Asian context.
India isn’t just a provider of medical products, services, and health information technology, it also is a source of talent in the health sector, including nurses, doctors, and researchers, many with influential positions at home and in the West.
India isn’t just a provider of medical products, services, and health information technology, it also is a source of talent in the health sector, including nurses, doctors, and researchers, many with influential positions at home and in the West.
India and its diaspora continue to play a pivotal role in shaping the future of global health.
India and its diaspora continue to play a pivotal role in shaping the future of global health. “ ”
India and its diaspora continue to play a pivotal role in shaping the future of global health. Whether through the contributions of health care professionals, advancements in pharmaceuticals, or the promotion of traditional healing practices, India's impact is felt on a global scale. Health practitioners and researchers around the world benefit from the diverse perspectives and expertise coming from the Indian diaspora. Recognizing and harnessing its potential also contribute to developing a robust medical research ecosystem in India.
India and its diaspora continue to play a pivotal role in shaping the future of global health. Whether through the contributions of health care professionals, advancements in pharmaceuticals, or the promotion of traditional healing practices, India's impact is felt on a global scale. Health practitioners and researchers around the world benefit from the diverse perspectives and expertise coming from the Indian diaspora. Recognizing and harnessing its potential also contribute to developing a robust medical research ecosystem in India.
6
“ ”
Photo courtesy of G20 India 2023 conference.
FOCUS 6
Photo courtesy of G20 India 2023
In 2023, India led the G20 summit, making One Health a key theme of the conference.
67
Mariah Felipe
Diaspora influence on clean cooking in India
Dr. Praveen Kumar’s journey into climate change research wasn’t a typical one. He began his studies as a technology major at the University of Mumbai, and went on to work as an engineer, where he says, “I started observing the detrimental impact of factories on poorer communities.” He noticed that vulnerable populations in Mumbai were constantly being exposed to toxins and pollutants due to industrial activities taking place in their surroundings which posed severe health risks.
This led him back to academia in pursuit of a master’s degree in social sciences from the Tata Institute of Social Sciences in India and later a PhD in social work from Washington University in St. Louis. Today, he works as an associate professor at Boston College School of Social Work. He’s focused on interdisciplinary research related to environmental justice and global health while emphasizing the role that climate change plays in both.
“When you start working on the environment and its impact on vulnerable communities, and you take a 30,000-foot view, climate change becomes one of the most important pieces of it,” he explains.
In 2023, Kumar was named an NIH Climate and Health Scholar for Fogarty. In this role he is currently working with Fogarty’s Center for Global Health Studies to analyze proposals for case studies to advance research on climate adaptation strategies and their impact on public health. The call for proposals received over 130 applications; eight to 10 case studies will be selected for publication.
With his academic experience in both India and the United States, Kumar acknowledges their similarities with an emphasis on technical and quantitative skills in both settings. However, he notes a significant difference in international diversity, stating, "In the U.S., the student body is quite diverse, but in India, not so much, which has a great impact on the types of perspectives available to you in a research setting."
His PhD project at Washington University was part of the Clean Cooking Implementation Science Network (ISN), led by Fogarty with support from the NIH Common Fund, and focused on using clean cooking methods to improve the health of mothers and their children by reducing their exposure to household air pollution.
Based on this study, he published a paper highlighting

some of the issues with previous clean cooking policies in India, which subsidized gas tanks needed for cooking but did not emphasize their health benefits. He identified three main obstacles for families living in rural areas in India and other parts of the world in implementing clean cooking practices: affordability, accessibility, and awareness. “It’s a global health problem,” he says, pointing out that the health implications for women and children exposed to household air pollution include heart disease, stroke, cancer, chronic lung disease and pneumonia, and even stunted growth in infants whose mothers were exposed while pregnant to household air pollutants from biomass fuels.
A major Indian news publication wrote a story based on his paper, which led to policy changes by the Indian government, exemplifying how researchers in the Indian diaspora can use their expertise and resources to address critical public health issues in India.
In addition to influencing policy on critical public health issues, Kumar hopes to help students and upand-coming researchers in India hone their skills and contribute to larger research projects, like the clean cooking initiative. “That’s where the role of Fogarty is so crucial,” says Kumar. “Because the center focuses on building the capacity and works with global health institutions, including nonprofit organizations and academic institutions.” Through such capacity building efforts, Kumar sees a future for more cutting-edge research at Indian institutions.
One type of clean cookstove is a smokeless mud model developed by the Smokeless Cookstove Foundation.
7 7
Photo courtesy of the Smokeless Cookstove Foundation
FOCUS ON INDIAN DIASPORA
68 Delaware Journal of Public Health - March 2024

Encouraging knowledge circulation between India & the West
Encouraging knowledge circulation between India & the West
Brain drain generally refers to the emigration of a group of educated individuals, often from lower-income countries to higher-income ones, in search of better economic opportunity and has long been a point of contention in the field of global health. While this phenomenon can have negative impacts, especially in countries in which the percentage of doctors is below WHO guidelines, this globalization of education, research, and medicine can also create a circulation of knowledge between two countries with differing cultures or resources.
Brain drain generally refers to the emigration of a group of educated individuals, often from lower-income countries to higher-income ones, in search of better economic opportunity and has long been a point of contention in the field of global health. While this phenomenon can have negative impacts, especially in countries in which the percentage of doctors is below WHO guidelines, this globalization of education, research, and medicine can also create a circulation of knowledge between two countries with differing cultures or resources.
This could not be more evident in India, a country with the world’s largest population and diaspora, and a growing economy. Dr. Nandini Kumar, president of India’s Forum for Ethics Review Committees and distinguished scientist chair at India’s Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy (AYUSH), says while she still sees some “brain drain” in India, it’s started to become more of a circulation of knowledge with an influx in recent years of Indians coming back and non-Indians moving to the country to study and conduct research. “I know there’s always been this fear of brain drain, but in reality, there’s a place for everyone, everywhere,” says Kumar.


This could not be more evident in India, a country with the world’s largest population and diaspora, and a growing economy. Dr. Nandini Kumar, president of India’s Forum for Ethics Review Committees and distinguished scientist chair at India’s Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy (AYUSH), says while she still sees some “brain drain” in India, it’s started to become more of a circulation of knowledge with an influx in recent years of Indians coming back and non-Indians moving to the country to study and conduct research. “I know there’s always been this fear of brain drain, but in reality, there’s a place for everyone, everywhere,” says Kumar.
Kumar has a unique perspective on this topic as an expert in bioethics who was born in India, trained abroad, and returned to India to lead a bioethics training program that has trained thousands in India over the last two decades. She began her journey into the field in 2001 as one of the first trainees in Fogarty’s International Research Ethics Education and Curriculum Development Award (or Bioethics) program. One of the things she appreciates about Fogarty’s approach is that the center puts host nation researchers in charge. “I had a professor tell us, ‘I’ll teach you about the international bioethics concepts, but we need you to show us the context so that you can apply these concepts in a way that works for India.’” She says this inspired her as she designed her bioethics program to ensure that it captured “Indian-ness” while incorporating cultural and philosophical principles from Indian and Western cultures.
Kumar has a unique perspective on this topic as an expert in bioethics who was born in India, trained abroad, and returned to India to lead a bioethics training program that has trained thousands in India over the last two decades. She began her journey into the field in 2001 as one of the first trainees in Fogarty’s International Research Ethics Education and Curriculum Development Award (or Bioethics) program. One of the things she appreciates about Fogarty’s approach is that the center puts host nation researchers in charge. “I had a professor tell us, ‘I’ll teach you about the international bioethics concepts, but we need you to show us the context so that you can apply these concepts in a way that works for India.’” She says this inspired her as she designed her bioethics program to ensure that it captured “Indian-ness” while incorporating cultural and philosophical principles from Indian and Western cultures.
Kumar notes that this transition from brain drain to a “two-way street” in India is the result of huge shifts in recent years. Economic growth and changes in policy and education practices, among other factors, have led to a growth in opportunity in India encouraging many Indians
Kumar notes that this transition from brain drain to a “two-way street” in India is the result of huge shifts in recent years. Economic growth and changes in policy and education practices, among other factors, have led to a growth in opportunity in India encouraging many Indians
to stay in the country and for others to return there for work.
to stay in the country and for others to return there for work.
Recent policies and guidelines are encouraging interdisciplinary clinical research and the integration of traditional medical systems with modern medicine. The current Indian government is behind the movement to converge traditional Indian medical practices, governed by AYUSH, with conventional Western medicine, creating more acceptance of traditional practices in hospitals and other settings.
Recent policies and guidelines are encouraging interdisciplinary clinical research and the integration of traditional medical systems with modern medicine. The current Indian government is behind the movement to converge traditional Indian medical practices, governed by AYUSH, with conventional Western medicine, creating more acceptance of traditional practices in hospitals and other settings.
I know there’s always been this fear of brain drain, but in reality, there’s a place for everyone, everywhere.
I know there’s always been this fear of brain drain, but in reality, there’s a place for everyone, everywhere. “ ”
“ ”
“The code of conduct for many of these practices protected by AYUSH was established hundreds of years ago, but the organization is now learning to adapt to the modern world, working to bring to the program more collaboration and cohesion between the two systems,” says Kumar.
“The code of conduct for many of these practices protected by AYUSH was established hundreds of years ago, but the organization is now learning to adapt to the modern world, working to bring to the program more collaboration and cohesion between the two systems,” says Kumar.
Adaptions of this approach include official guidelines from AYUSH on the use of remedies to treat mild to moderate COVID-19, released in 2021, and a recent publication in the British Journal of Dermatology highlighting successful Ayurvedic treatments for filariasis and lymphedema.
Adaptions of this approach include official guidelines from AYUSH on the use of remedies to treat mild to moderate COVID-19, released in 2021, and a recent publication in the British Journal of Dermatology highlighting successful Ayurvedic treatments for filariasis and lymphedema.
Whether it is traditional or Western medicine that is being studied at home or abroad, Kumar asks her fellow researchers in the diaspora, in any field, to impart what they’ve learned to researchers in India, and to help build their research capacity through research or workshops, “because there are no global health issues that are confined to a particular geographical area. We have to learn from each other’s shortcomings and successes to grow.”
Whether it is traditional or Western medicine that is being studied at home or abroad, Kumar asks her fellow researchers in the diaspora, in any field, to impart what they’ve learned to researchers in India, and to help build their research capacity through research or workshops, “because there are no global health issues that are confined to a particular geographical area. We have to learn from each other’s shortcomings and successes to grow.”
FOCUS ON INDIAN DIASPORA
8
Photo courtesy of Nandini Kumar
Dr. Nandini Kumar attended the 2023 G20 summit in New Delhi, India, in September 2023.
FOCUS ON INDIAN DIASPORA
8
Photo courtesy of Nandini Kumar
Dr. Nandini Kumar attended the 2023 G20 summit in New Delhi, India, in September 2023.
69
Simplifying heart failure care in South Asia
Simplifying heart failure care in South Asia
Simplifying heart failure care in South Asia
Dr. Anubha Agarwal began her research in India as a Fogarty Global Health Fellow during 2017–2018. She was co-mentored by Dr. Doriaraj Prabhakaran, executive director of the Centre for Chronic Disease Control (CCDC) in India, and Dr. Mark Huffman, professor of medicine and co-director of the Global Health Center at Washington University in St. Louis (WUSTL), Missouri. During her Fogarty year, she developed, implemented, and evaluated, using an interrupted time series design, a heart failure quality improvement intervention including discharge checklists, audit-and-feedback mechanisms, and patient education among 1,400 patients hospitalized with heart failure in eight hospitals in Kerala, India.
Dr. Anubha Agarwal began her research in India as a Fogarty Global Health Fellow during 2017–2018. She was co-mentored by Dr. Doriaraj Prabhakaran, executive director of the Centre for Chronic Disease Control (CCDC) in India, and Dr. Mark Huffman, professor of medicine and co-director of the Global Health Center at Washington University in St. Louis (WUSTL), Missouri. During her Fogarty year, she developed, implemented, and evaluated, using an interrupted time series design, a heart failure quality improvement intervention including discharge checklists, audit-and-feedback mechanisms, and patient education among 1,400 patients hospitalized with heart failure in eight hospitals in Kerala, India.
Dr. Anubha Agarwal began her research in India as a Fogarty Global Health Fellow during 2017–2018. She was co-mentored by Dr. Doriaraj Prabhakaran, executive director of the Centre for Chronic Disease Control (CCDC) in India, and Dr. Mark Huffman, professor of medicine and co-director of the Global Health Center at Washington University in St. Louis (WUSTL), Missouri. During her Fogarty year, she developed, implemented, and evaluated, using an interrupted time series design, a heart failure quality improvement intervention including discharge checklists, audit-and-feedback mechanisms, and patient education among 1,400 patients hospitalized with heart failure in eight hospitals in Kerala, India.
Today, she is an assistant professor of medicine and codirector of the Global Cardiovascular Health program at WUSTL. Agarwal received a Pathway to Independence award from the National Heart, Lung, and Blood Institute (NHLBI) in 2022, allowing her to build on her previous research to improve heart failure care in South Asia. She aims to substantially simplify heart failure management for patients with heart failure with reduced ejection fraction (HFrEF, the type of heart failure in which the left ventricle loses its ability to contract normally, and the heart can’t pump with enough force to push blood into circulation). Her goal is to shift the treatment paradigm from a multi-drug therapy to a polypill containing several guideline-directed medical therapies for HFrEF in one pill.

Today, she is an assistant professor of medicine and codirector of the Global Cardiovascular Health program at WUSTL. Agarwal received a Pathway to Independence award from the National Heart, Lung, and Blood Institute (NHLBI) in 2022, allowing her to build on her previous research to improve heart failure care in South Asia. She aims to substantially simplify heart failure management for patients with heart failure with reduced ejection fraction (HFrEF, the type of heart failure in which the left ventricle loses its ability to contract normally, and the heart can’t pump with enough force to push blood into circulation). Her goal is to shift the treatment paradigm from a multi-drug therapy to a polypill containing several guideline-directed medical therapies for HFrEF in one pill.
Today, she is an assistant professor of medicine and codirector of the Global Cardiovascular Health program at WUSTL. Agarwal received a Pathway to Independence award from the National Heart, Lung, and Blood Institute (NHLBI) in 2022, allowing her to build on her previous research to improve heart failure care in South Asia. She aims to substantially simplify heart failure management for patients with heart failure with reduced ejection fraction (HFrEF, the type of heart failure in which the left ventricle loses its ability to contract normally, and the heart can’t pump with enough force to push blood into circulation). Her goal is to shift the treatment paradigm from a multi-drug therapy to a polypill containing several guideline-directed medical therapies for HFrEF in one pill.
Her research still in its early phases, Agarwal and her team have already conducted in-depth interviews and focus group discussions with cardiologists, pharmacists, nurses, and patients throughout India aiming to understand the current context of heart failure care and acceptability, appropriateness, and feasibility of an
Her research still in its early phases, Agarwal and her team have already conducted in-depth interviews and focus group discussions with cardiologists, pharmacists, nurses, and patients throughout India aiming to understand the current context of heart failure care and acceptability, appropriateness, and feasibility of an
Her research still in its early phases, Agarwal and her team have already conducted in-depth interviews and focus group discussions with cardiologists, pharmacists, nurses, and patients throughout India aiming to understand the current context of heart failure care and acceptability, appropriateness, and feasibility of an


HFrEF polypill implementation strategy. The next phase will be a multi-center type 1 hybrid randomized clinical trial among patients with HFrEF in South Asia. It will investigate whether an HFrEF polypill implementation strategy can improve key clinical outcomes compared to usual care. Through the development, implementation, and evaluation of HFrEF polypills, Agarwal hopes to improve heart failure care in South Asia and beyond.
HFrEF polypill implementation strategy. The next phase will be a multi-center type 1 hybrid randomized clinical trial among patients with HFrEF in South Asia. It will investigate whether an HFrEF polypill implementation strategy can improve key clinical outcomes compared to usual care. Through the development, implementation, and evaluation of HFrEF polypills, Agarwal hopes to improve heart failure care in South Asia and beyond.
HFrEF polypill implementation strategy. The next phase will be a multi-center type 1 hybrid randomized clinical trial among patients with HFrEF in South Asia. It will investigate whether an HFrEF polypill implementation strategy can improve key clinical outcomes compared to usual care. Through the development, implementation, and evaluation of HFrEF polypills, Agarwal hopes to improve heart failure care in South Asia and beyond.
When asked about her motivation for this research, she states that she chose to pursue cardiology after her grandfather, who lived in India, died of a heart attack in his early 50s. She says, “It inspired me to become a cardiologist and, in many ways, inspires my continued commitment to improving cardiovascular care in India and South Asia.” As a part of the Indian diaspora, having left India at only 5 years of age, she adds, “It’s been incredibly rewarding professionally and personally to be a part of a team generating evidence-based research to improve cardiovascular care in India.”
When asked about her motivation for this research, she states that she chose to pursue cardiology after her grandfather, who lived in India, died of a heart attack in his early 50s. She says, “It inspired me to become a cardiologist and, in many ways, inspires my continued commitment to improving cardiovascular care in India and South Asia.” As a part of the Indian diaspora, having left India at only 5 years of age, she adds, “It’s been incredibly rewarding professionally and personally to be a part of a team generating evidence-based research to improve cardiovascular care in India.”
Beyond her clinical and research pursuits, Agarwal embraces the role of a mentor, particularly for aspiring female researchers in cardiovascular medicine and global health science who are often under-represented in both fields. "I have been so lucky to have been surrounded by fantastic feminist mentors who have always elevated me, and I'm trying to give that back.”
When asked about her motivation for this research, she states that she chose to pursue cardiology after her grandfather, who lived in India, died of a heart attack in his early 50s. She says, “It inspired me to become a cardiologist and, in many ways, inspires my continued commitment to improving cardiovascular care in India and South Asia.” As a part of the Indian diaspora, having left India at only 5 years of age, she adds, “It’s been incredibly rewarding professionally and personally to be a part of a team generating evidence-based research to improve cardiovascular care in India.”
Beyond her clinical and research pursuits, Agarwal embraces the role of a mentor, particularly for aspiring female researchers in cardiovascular medicine and global health science who are often under-represented in both fields. "I have been so lucky to have been surrounded by fantastic feminist mentors who have always elevated me, and I'm trying to give that back.”
As she continues her work in India, as a part of the Indian diaspora, she wants to ensure there’s an equitable partnership that builds capacity with Indian researchers and institutions to ensure all voices are heard, "While we’re helping to train the research workforce of India, we also need to acknowledge how much we have to learn from them.”
Beyond her clinical and research pursuits, Agarwal embraces the role of a mentor, particularly for aspiring female researchers in cardiovascular medicine and global health science who are often under-represented in both fields. "I have been so lucky to have been surrounded by fantastic feminist mentors who have always elevated me, and I'm trying to give that back.”
As she continues her work in India, as a part of the Indian diaspora, she wants to ensure there’s an equitable partnership that builds capacity with Indian researchers and institutions to ensure all voices are heard, "While we’re helping to train the research workforce of India, we also need to acknowledge how much we have to learn from them.”
As she continues her work in India, as a part of the Indian diaspora, she wants to ensure there’s an equitable partnership that builds capacity with Indian researchers and institutions to ensure all voices are heard, "While we’re helping to train the research workforce of India, we also need to acknowledge how much we have to learn from them.”
9
9 FOCUS ON INDIAN DIASPORA
Fogarty International Center
Photo of a busy street in Kerala, India, where Anubha Agarwal began her
9 FOCUS ON INDIAN DIASPORA
Photo courtesy of Northwestern University
Anubha Agarwal (left) speaks during the Fogarty Global Health Fellows & Scholars 20th Anniversary event in April 2023 at NIH. Roxanna Garcia (right) looks on. Fogarty International Center
FOCUS ON INDIAN DIASPORA
Photo courtesy of Northwestern University
Anubha Agarwal (left) speaks during the Fogarty Global Health Fellows & Scholars 20th Anniversary event in April 2023 at NIH. Roxanna Garcia (right) looks on. Fogarty International Center
Photo of a busy street in Kerala, India, where Anubha Agarwal began her research on heart failure care in India while a Fogarty Global Health Scholar.
70 Delaware Journal of Public Health - March 2024
Photo courtesy of Northwestern University

DIRECTOR’S COLUMN
By Dr. Peter Kilmarx, Acting Director, Fogarty International Center
Seeing is believing: My year helming Fogarty
In November, I had the opportunity to see the impact of Fogarty’s efforts during a multi-country trip to Africa and Asia. My first stop was in Kigali, Rwanda, for the third annual meeting of the NIH Common Fund program, Harnessing Data Science for Health Discovery and Innovation in Africa (DS-I Africa). This meeting brought together more than 300 data scientists and other researchers from across the continent. A total of 12 NIH institutes, centers, and offices collaborate on DS-I Africa. This broad engagement and scientific diversity are critical to the goals of both Fogarty and the Common Fund, an internal office at NIH that allows for collaboration on innovative research across institutes and centers.
While in Kigali, I also visited NIH grant recipients Drs. David Tumusiime and Vincent Sezibera at the College of Medicine and Health Sciences, University of Rwanda. Both are actively involved in DS-I Africa research and training programs. I also spent time with Dr. Gad Murenzi, who directs the EinsteinRwanda Research and Capacity Building Program in Kigali. With him, I visited an HIV clinic that participates in IeDEA (International epidemiology Databases to Evaluate AIDS). IeDEA collects observational data representing over 2.2 million people living with HIV in 44 countries and the Fogarty-IeDEA Mentorship Program (FIMP) trains researchers worldwide using this very large database. Lastly in Rwanda, I met with the Drs. Abebe Bekele, dean, and Daniel Seifu, dean of research, at the University of Global Health Equity.
the meeting was a lively and informative platform to share research findings and network with a global scientific community, including many Fogarty trainees and grant recipients.
Between meetings, I had a chance to visit Thiravat Hemachudha, director of the Thai Red Cross Emerging Infectious Diseases Health Science Centre at Chulalongkorn University, and Virasakdi Chongsuvivatwong, professor of epidemiology at Prince of Songkhla University in Bangkok, Thailand. Dr. Thiravat is a former Fogarty trainee and now a global leader in research on rabies and other emerging infections, while Dr. Virasakdi is senior infectious disease epidemiologist with a Fogarty grant to train researchers from Thailand, Burma, and Indonesia.

For my final stop, I joined 130 experts from 43 countries in the first Global Clinical Trials Forum at the headquarters of the World Health Organization (WHO) in Geneva convened by its Chief Scientist Dr. Jeremy Farrar. I’ve been keenly interested in the need to build global clinical trial capacity to address countries’ perennial health challenges that can also be available in the event of infectious disease outbreaks or other health emergencies.
My next stop was in Singapore for the annual scientific meeting of the Global Alliance for Chronic Diseases (GACD). GACD brings together 12 major international research funding agencies specifically to address the growing global burden of noncommunicable diseases in low- and middle-income countries. With a research network involving hundreds of scientists in more than 70 countries,
January 2024 marks the oneyear anniversary of my role as acting director of Fogarty, and with that, acting associate director for international research for NIH. My trip, which included stops in Africa, Asia, and Europe, was an outstanding opportunity to represent Fogarty and all of NIH in key international fora, to promote global health research partnerships, and to see firsthand the impressive impacts of our exceptional Fogarty team. It’s been a privilege to serve in this role. I enter the new year as energized and optimistic as ever about our progress toward achieving our vision of a world in which the frontiers of health research extend across the globe and advances in science are implemented to reduce the burden of disease and promote health for all people.
10
A student (right) demonstrates an “Anatomage” table while Acting Fogarty Director Peter Kilmarx (left) looks on at University of Global Health Equity, Rwanda,
71
Photo courtesy Peter Kilmarx
PEOPLE
HEALTH Briefs Global PEOPLE
HEALTH Briefs















Alex Mremi wins James G. Hakim Award
Alex Mremi wins James G. Hakim Award
Alex Mremi wins James G. Hakim Award
Dr. Alex Mremi, of the Kilimanjaro Christian Medical Centre, has been awarded the annual James G. Hakim Award on behalf of Fogarty, AFREhealth, and the Consortium of Universities for Global Health (CUGH). This award recognizes an African who is working toward their terminal degree and received the top score for their submitted abstract for CUGH 2024.
Dr. Alex Mremi, of the Kilimanjaro Christian Medical Centre, has been awarded the annual James G. Hakim Award on behalf of Fogarty, AFREhealth, and the Consortium of Universities for Global Health (CUGH). This award recognizes an African who is working toward their terminal degree and received the top score for their submitted abstract for CUGH 2024.
Dr. Alex Mremi, of the Kilimanjaro Christian Medical Centre, has been awarded the annual James G. Hakim Award on behalf of Fogarty, AFREhealth, and the Consortium of Universities for Global Health (CUGH). This award recognizes an African who is working toward their terminal degree and received the top score for their submitted abstract for CUGH 2024.
W. Kimryn Rathmell selected for top role at NCI
W. Kimryn Rathmell selected for top role at NCI
W. Kimryn Rathmell selected for top role at NCI
Dr. W. Kimryn Rathmell was selected by President Biden as the 17th director of the National Cancer Institute (NCI) in December. Rathmell was previously the Hugh Jackson Morgan Chair in Medicine, chair of the department of medicine, and physician-inchief at Vanderbilt University Medical Center. Rathmell succeeds Dr. Monica M. Bertagnolli, who left NCI to become NIH director.
Dr. W. Kimryn Rathmell was selected by President Biden as the 17th director of the National Cancer Institute (NCI) in December. Rathmell was previously the Hugh Jackson Morgan Chair in Medicine, chair of the department of medicine, and physician-inchief at Vanderbilt University Medical Center. Rathmell succeeds Dr. Monica M. Bertagnolli, who left NCI to become NIH director.
Dr. W. Kimryn Rathmell was selected by President Biden as the 17th director of the National Cancer Institute (NCI) in December. Rathmell was previously the Hugh Jackson Morgan Chair in Medicine, chair of the department of medicine, and physician-inchief at Vanderbilt University Medical Center. Rathmell succeeds Dr. Monica M. Bertagnolli, who left NCI to become NIH director.
Prajakta Adsul assumes director role at UNM’s CADIS
Prajakta Adsul assumes director role at UNM’s CADIS
Former Fogarty Global Health Fellow Dr. Prajakta Adsul has been named director of University of New Mexico’s new Center for Advancing Dissemination and Implementation Science (CADIS). Since 2019, Adsul has been a faculty member in the Division of Epidemiology, Biostatistics, and Preventive Medicine and is a member in the Cancer Control and Population Sciences Research Program.
Prajakta Adsul assumes director role at UNM’s CADIS
Former Fogarty Global Health Fellow Dr. Prajakta Adsul has been named director of University of New Mexico’s new Center for Advancing Dissemination and Implementation Science (CADIS). Since 2019, Adsul has been a faculty member in the Division of Epidemiology, Biostatistics, and Preventive Medicine and is a member in the Cancer Control and Population Sciences Research Program.
Former Fogarty Global Health Fellow Dr. Prajakta Adsul has been named director of University of New Mexico’s new Center for Advancing Dissemination and Implementation Science (CADIS). Since 2019, Adsul has been a faculty member in the Division of Epidemiology, Biostatistics, and Preventive Medicine and is a member in the Cancer Control and Population Sciences Research Program.
Mikus to lead Global Health Technologies Coalition
Mikus to lead Global Health Technologies Coalition
Mikus to lead Global Health Technologies Coalition
Global Health Technologies Coalition (GHTC) appointed Dr. Kristie Mikus as executive director. Mikus spent two decades serving the U.S. government, including as senior policy advisor for the Global Health Center at the U.S. Centers for Disease Control and Prevention (CDC), CDC deputy country director in Zambia, and Zambia country coordinator for PEPFAR.
Global Health Technologies Coalition (GHTC) appointed Dr. Kristie Mikus as executive director. Mikus spent two decades serving the U.S. government, including as senior policy advisor for the Global Health Center at the U.S. Centers for Disease Control and Prevention (CDC), CDC deputy country director in Zambia, and Zambia country coordinator for PEPFAR.
Global Health Technologies Coalition (GHTC) appointed Dr. Kristie Mikus as executive director. Mikus spent two decades serving the U.S. government, including as senior policy advisor for the Global Health Center at the U.S. Centers for Disease Control and Prevention (CDC), CDC deputy country director in Zambia, and Zambia country coordinator for PEPFAR.
SAMRC names Ntobeko Ntusi president and CEO
SAMRC names Ntobeko Ntusi president and CEO
SAMRC names Ntobeko Ntusi president and CEO
The South African Medical Research Council (SAMRC) has appointed Dr. Ntobeko Ntusi as its new president and CEO, effective July 2024. Ntusi, a cardiologist, currently heads the department of medicine at Groote Schuur Hospital. Ntusi will succeed Dr. Glenda Gray, who has been the SAMRC President for the past decade.
The South African Medical Research Council (SAMRC) has appointed Dr. Ntobeko Ntusi as its new president and CEO, effective July 2024. Ntusi, a cardiologist, currently heads the department of medicine at Groote Schuur Hospital. Ntusi will succeed Dr. Glenda Gray, who has been the SAMRC President for the past decade.
The South African Medical Research Council (SAMRC) has appointed Dr. Ntobeko Ntusi as its new president and CEO, effective July 2024. Ntusi, a cardiologist, currently heads the department of medicine at Groote Schuur Hospital. Ntusi will succeed Dr. Glenda Gray, who has been the SAMRC President for the past decade.
AACR elects John Schiller as fellow
AACR elects John Schiller as fellow
AACR elects John Schiller as fellow
The American Association for Cancer Research has elected Dr. John T. Schiller, deputy chief, Laboratory of Cellular Oncology, National Cancer Institute, as a fellow for “championed research that has reduced the incidence of human papillomavirus (HPV)-associated cancers.” He received the NIH Distinguished Investigator designation in 2016.
The American Association for Cancer Research has elected Dr. John T. Schiller, deputy chief, Laboratory of Cellular Oncology, National Cancer Institute, as a fellow for “championed research that has reduced the incidence of human papillomavirus (HPV)-associated cancers.” He received the NIH Distinguished Investigator designation in 2016.
The American Association for Cancer Research has elected Dr. John T. Schiller, deputy chief, Laboratory of Cellular Oncology, National Cancer Institute, as a fellow for “championed research that has reduced the incidence of human papillomavirus (HPV)-associated cancers.” He received the NIH Distinguished Investigator designation in 2016.
Bangladesh records worst dengue epidemic
Bangladesh records worst dengue epidemic
Bangladesh records worst dengue epidemic
Bangladesh reported more than 300,000 dengue cases, including 1,705 deaths, in 2023, a dramatic increase from the 62,000 infections and 281 deaths the nation recorded the previous year. The incidence of dengue has grown dramatically around the world in recent decades due to more frequent extreme weather events, according to WHO.
Bangladesh reported more than 300,000 dengue cases, including 1,705 deaths, in 2023, a dramatic increase from the 62,000 infections and 281 deaths the nation recorded the previous year. The incidence of dengue has grown dramatically around the world in recent decades due to more frequent extreme weather events, according to WHO.
Bangladesh reported more than 300,000 dengue cases, including 1,705 deaths, in 2023, a dramatic increase from the 62,000 infections and 281 deaths the nation recorded the previous year. The incidence of dengue has grown dramatically around the world in recent decades due to more frequent extreme weather events, according to WHO.
Gates Foundation approves record budget
The Bill & Melinda Gates Foundation’s board of trustees approved a $8.6 billion budget for 2024, the largest annual budget to date. A major focus for the foundation has been funding development of new tools and strategies to reduce the number of cases of infectious diseases and decrease causes of child mortality in low-income countries.
Gates Foundation approves record budget
Gates Foundation approves record budget
The Bill & Melinda Gates Foundation’s board of trustees approved a $8.6 billion budget for 2024, the largest annual budget to date. A major focus for the foundation has been funding development of new tools and strategies to reduce the number of cases of infectious diseases and decrease causes of child mortality in low-income countries.
The Bill & Melinda Gates Foundation’s board of trustees approved a $8.6 billion budget for 2024, the largest annual budget to date. A major focus for the foundation has been funding development of new tools and strategies to reduce the number of cases of infectious diseases and decrease causes of child mortality in low-income countries.
Cameroon rolls out malaria vaccinations
Cameroon rolls out malaria vaccinations
Cameroon rolls out malaria vaccinations
In January, Cameroon became the first nation to begin routinely vaccinating children with RTS,S (Mosquirix), the first antimalarial shot recommended by WHO. The Central Africa nation, which boasts an immunization program going back five decades, aims to inoculate almost 250,000 children against the mosquito-spread disease by 2026.
In January, Cameroon became the first nation to begin routinely vaccinating children with RTS,S (Mosquirix), the first antimalarial shot recommended by WHO. The Central Africa nation, which boasts an immunization program going back five decades, aims to inoculate almost 250,000 children against the mosquito-spread disease by 2026.
In January, Cameroon became the first nation to begin routinely vaccinating children with RTS,S (Mosquirix), the first antimalarial shot recommended by WHO. The Central Africa nation, which boasts an immunization program going back five decades, aims to inoculate almost 250,000 children against the mosquito-spread disease by 2026.
Global Health NOW turns 10
Global Health NOW turns 10
Global Health NOW turns 10
Global Health NOW (GHN) celebrated a decade of sharing global health news, reporting and perspectives on January 2. The publication from Johns Hopkins Bloomberg School of Public Health reaches more than 50,000 readers in 170 countries. Throughout 2024, GHN will post special features, campaigns, and events, stated Editor-inChief Brian W. Simpson.
Global Health NOW (GHN) celebrated a decade of sharing global health news, reporting and perspectives on January 2. The publication from Johns Hopkins Bloomberg School of Public Health reaches more than 50,000 readers in 170 countries. Throughout 2024, GHN will post special features, campaigns, and events, stated Editor-inChief Brian W. Simpson.
Global Health NOW (GHN) celebrated a decade of sharing global health news, reporting and perspectives on January 2. The publication from Johns Hopkins Bloomberg School of Public Health reaches more than 50,000 readers in 170 countries. Throughout 2024, GHN will post special features, campaigns, and events, stated Editor-inChief Brian W. Simpson.
WHO releases ethics guidance for LMMs
WHO releases ethics guidance for LMMs
WHO is releasing new guidance on ethics and governance of large multi-modal models (LMMs), a type of artificial intelligence (AI) technology that can understand and create content. LMMs are being used for health-related purposes despite documented risks. The guidance outlines recommendations for consideration by governments, technology companies, and health care providers.
WHO releases ethics guidance for LMMs
WHO is releasing new guidance on ethics and governance of large multi-modal models (LMMs), a type of artificial intelligence (AI) technology that can understand and create content. LMMs are being used for health-related purposes despite documented risks. The guidance outlines recommendations for consideration by governments, technology companies, and health care providers.
WHO is releasing new guidance on ethics and governance of large multi-modal models (LMMs), a type of artificial intelligence (AI) technology that can understand and create content. LMMs are being used for health-related purposes despite documented risks. The guidance outlines recommendations for consideration by governments, technology companies, and health care providers.
HEALTH Briefs Global PEOPLE 11
11
Global
11
72 Delaware Journal of Public Health - March 2024
Global Health Matters
January/February 2024
Volume 23, No. 1 ISSN: 1938-5935
Fogarty International Center National Institutes of Health Department of Health and Human Services
Communications director: Andrey Kuzmichev Andrey.Kuzmichev@nih.gov
Managing editor: Judy Coan-Stevens Judith.Coan-Stevens@nih.gov
Writer/editor: Mariah Felipe Mariah.Felipe@nih.gov
Writer/editor: Susan Scutti Susan.Scutti@nih.gov
Digital analyst: Merrijoy Vicente Merrijoy.Vicente@nih.gov
Designer: Carla Conway

Opinion pieces help promote research
Scientists should not rely solely on academic papers to circulate news about their research, according to a recent Nature article. Many general readers wish to keep abreast of scientific discovery, so writing an opinion piece—also referred to as an op-ed, commentary, or guest essay—is another way to share discoveries or express an informed view on important yet difficult-to-understand topics.
While such articles provide a service to readers unfamiliar with scientific journals, they also might provide personal and professional rewards for their authors. Read by colleagues and policymakers, guest essays raise writers' profiles within institutions and fields. Add to that, articles penned by global health scientists, especially those from low- and middle-income countries, can broaden the usual range of perspectives seen on op-ed pages and may help frame research priorities and funding.
International Bioethics Training go.nih.gov/BioethicsTraining Jun 6, 2024 JANUARY/FEBRUARY 2024
SUBSCRIBE: fic.nih.gov/subscribe
rare cases when a correction is needed after an issue’s printed version has been finalized, the change will be made and explained in the online version of the article.
In
SCAN AND READ THIS ISSUE ONLINE
For more information, visit www.fic.nih.gov/funding
text produced in Global Health Matters is in the public domain and may be reprinted. Please credit Fogarty International Center. Images must be cleared for use with the individual source, as indicated. Noncommunicable Disease Prevention in Cities go.nih.gov/GACD Mar 11, 2024 Mobile Health (mHealth) go.nih.gov/mHealth Mar 22, 2024
Funding Opportunity Announcement Deadline Details
All
Read our tips for writing op-eds: go.nih.gov/OpEdTips 73
Cora J. Firkin
Paving the Way to Active Living for People with Disabilities: Evaluating Park and Playground Accessibility and Usability in Delaware
Department of Health Behavior and Nutrition Sciences, University of Delaware
Lauren Rechner
Epidemiology Program, University of Delaware
Iva Obrusnikova, Ph.D., M.Sc.
Department of Health Behavior and Nutrition Sciences, University of Delaware
ABSTRACT
Objectives: To evaluate the accessibility and usability of parks and playgrounds in New Castle County, Delaware, for people with disabilities, with a particular focus on identifying environmental barriers that may impede access to these public spaces and potentially affect physical activity (PA) participation for the chronic disease prevention and mitigation. Methods: Using a cross-sectional observational design, teams of trained University of Delaware students utilized the Community Health Inclusion Index (CHII) Tool to assess the accessibility of ten suburban and urban parks and playgrounds from April to November 2023. The tool evaluated various elements of public spaces, including public transit, parking, pathways and multi-use trails, entrances, playground equipment, and health promotional materials. Descriptive statistics were calculated for the accessibility and usability of each element. Results: Significant barriers to accessibility and usability were identified. Over half of the sites lacked nearby public transit stops, and many trails and playgrounds were not fully accessible to people with disabilities. While some areas demonstrated good accessibility, such as well-maintained pathways and appropriately designed crosswalks, barriers like uneven surfaces, insufficient curb cuts, and inadequate van-accessible parking spaces were common. Most playgrounds lacked equitable play equipment, with less than half having ground materials suitable for mobility devices. Conclusions: The study underscores the need for substantial improvements in the design, construction, and maintenance of Delaware parks and playgrounds to better support people with disabilities. Enhancing accessibility is crucial for promoting PA participation. The findings support the development of inclusive recreational and PA environments, aligning with the Americans with Disabilities Act, to reduce chronic disease health disparities faced by people with disabilities. Policy Implications: This study highlights the need for revised policy measures to enhance park accessibility, advocating for infrastructure improvements and inclusive designs to ensure equitable recreation and physical activity opportunities for people with disabilities.
ACKNOWLEDGMENT
The research reported in this publication was supported by the University of Delaware Graduate College through the Doctoral Fellowship for Excellence (Firkin). The content is solely the responsibility of the authors.
INTRODUCTION
The World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) framework1 posits that a person’s level of functioning and disability, including their ability to participate, is influenced by the interaction of health conditions and contextual or environmental factors, such as the accessibility of the environment, peer relationships, and the availability of services. Additionally, personal factors such as age, gender, values, and lifestyle also contribute to this dynamic. According to the Americans with Disabilities Act (ADA), passed in 1990 and amended in 2008, a person with a disability is defined as someone with a record of or is perceived to have a physical or mental
impairment that substantially limits one or more major life activities, including bodily movements. In the United States (US), the 2023 Annual Disability Statistics Compendium reported that approximately 13.0% (42.6 million) of the community population live with a disability.2 In Delaware, the percentage is slightly above the national count, with approximately 13.1% (nearly 130 thousand) of the population identified as living with a disability.2 Notably, Delaware’s disability-associated healthcare expenditures surged by 93% in 2015, reaching 3.1 billion USD, a significant increase from 2013.3
Persistent health disparities are often faced by people with disabilities, including substantially increased risk of poor overall health status4,5 and population-level differences in preventable health conditions not predominantly attributed to the underlying impairment.6 National datasets from the US indicate that people with disabilities have significantly higher prevalence rates of chronic diseases than people without disabilities, including arthritis, asthma, cardiovascular disease, diabetes, high blood
Doi: 10.32481/djph.2024.03.09
74 Delaware Journal of Public Health - March 2024
pressure, high cholesterol, and stroke.5,7 Evidence also supports that people with a disability have significantly higher body mass index than people without disability.5,7 Nevertheless, people with disability are often an overlooked population in national public health initiatives to address chronic disease.6
In Delaware, these chronic diseases – cerebrovascular disease, diabetes mellitus, and heart disease – jointly accounted for about 30% of deaths across all ages in 2018.8 For children and adolescents, non-congenital heart diseases accounted for 3.3% of deaths in those aged 1 to 4 years and 6.1% of deaths in those aged 5 to 14.8 In addition, there is a marked discrepancy in obesity prevalence between Delawareans with a disability (45%) and Delawareans without a disability (30.2%), resulting in a +14.8% gap, which exceeds the national statistic of a +11.8% gap between people with and without a disability.2 Consequently, chronic disease prevention and mitigation is of utmost importance to Delaware, with the Delaware Division of Public Health (DE DPH) supporting the vision of “healthy people in healthy communities.”9 To achieve this vision, physical activity (PA) is an important modifiable health behavior for reducing the risks of high body mass index and chronic diseases.10 A major domain of PA is leisure, occurring during one’s free time and includes physical recreation for enjoyment, structured exercise to improve or maintain physical fitness, or sports, often involving team participation and rules or expectations. To achieve health benefits, the 2018 Physical Activity Guidelines for Americans recommend that adults with disabilities, if capable, participate in at least two days of moderate-to-vigorous muscle-strengthening activities targeting all major muscle groups. Additionally, they should aim for 150-300 minutes of moderate-intensity or 75150 minutes of vigorous-intensity aerobic PA each week, or an equivalent combination. For children and adolescents, regardless of disability status, the guidelines suggest at least 60 minutes of moderate-to-vigorous PA daily.11 However, people with disabilities are less likely to participate in any physical activity4,12 and are often less likely to adhere to the PA guidelines, resulting in higher rates of health issues related to physical inactivity than their peers without disabilities.13
Creating and maintaining community-built environments to promote PA, particularly leisure PA, is recommended by the 2018 Physical Activity Guidelines for Americans to offset the rise of chronic disease11 and is a strategic effort highlighted by the DE DPH.9 However, a persistent public health challenge lies in creating environments that effectively promote PA, particularly when taking into account the variations in individual differences, such as impairments, health conditions, and age.14 Recent studies have begun identifying the environmental quality indicators associated with increased PA (e.g., green spaces, intersection density, street connectivity, park proximity, ‘walkability’).15,16 Despite these advancements, there remains an urgent need to ensure that these environments are universally accessible to everyone. The ADA Accessibility Guidelines (ADAAG), originally mandated in 1991 and amended through September 2022, provide scoping and technical standards for the design, construction, and alteration of buildings and facilities. These ADAAG guidelines aim to ensure accessibility for people with disabilities in areas covered by Titles II (public entities and public transportation) and III (public accommodations and commercial facilities) of the ADA.17 Nonetheless, the inaccessibility of built and natural
environments continues to be a major barrier to PA participation by people with disabilities,18,19 emphasizing the perception that natural environments are ‘inherently inaccessible.’18 Public parks and play areas, such as playgrounds, integrate elements of built and natural environments. The ADA mandates stipulate that these spaces must offer continuous and unobstructed accessible routes, including maneuvering spaces and ground-level and elevated play components. Recent studies indicate that park-based interventions can substantially improve physical, psychological, and social health outcomes in people with a disability, mitigating disability-related impairments and chronic health disparities.20 For children and adults without a disability, a systematic review has also shown improvements to park and play area environments, such as installing exercise and playground equipment and renovating surfaces and lighting, are likely to increase their PA participation.21 However, as of September 2022, Section 15 of the ADAAG on Recreation Facilities,17 which incorporates key aspects of play areas, such as play and exercise equipment, accessible surfacing materials, and accessible play area routes, has not been integrated into the Department of Justice Accessibility Standards, rendering it non-enforceable. This regulatory gap is further widened as playground facilities built before March 15, 2012, are not mandated to comply with the 2010 ADA Standards for Accessible Design. Such inconsistencies in compliance potentially lead to varied accessibility in play areas for people with disabilities. Addressing these health disparities at the community level begins with a thorough assessment of the accessibility and usability of existing play areas to promote PA in people with disabilities.
The purpose of this research study is to evaluate the accessibility and usability of parks and playgrounds in New Castle County, Delaware, for people with disabilities. Employing the Community Health Inclusion Index (CHII) Tool, this research aims to comprehensively assess various aspects of these public spaces, including public transit, intersections, parking, pathways, entrances, health promotional materials, restrooms, playgrounds, trails, and other elements impacting navigational supports and barriers. This study primarily focuses on identifying key environmental barriers that may impede access to public spaces for people with disabilities. While not directly measuring the impact of these barriers on PA participation, the study recognizes the importance of accessible environments in promoting PA among all community members, including those with disabilities. The research outcomes will offer targeted recommendations for improving the accessibility and usability of these community spaces. Ultimately, this study aims to contribute to the broader objective of fostering inclusive public spaces that encourage active living and help mitigate the risk of chronic diseases in people, including those with disabilities.
METHOD
Parks and Playgrounds
Using a cross-sectional observational design, the study collected data from ten parks and associated playgrounds in New Castle County, Delaware, the state’s most populous county, with particular emphasis on Newark and Wilmington. These sites, spanning seven different zip codes, were selected to represent a diverse range of suburban and urban public spaces, ensuring a sample reflective of the broader state and county demographics
75
Note: Total population, sex, and race/ethnicity came from S1810; median age from S0101; age by disability status from K201801; household income from S1901; and poverty level from S1701. a may or may not have identified as Hispanic or Latino
Note.
Population-Level Characteristic Estimate ± Margin of Error Delaware New Castle County N (% with a Disability) 1,005,551±962 (13.8±0.8) 568,914±312 (11.9±0.9) Median Age (years) 41.5±0.3 39.8±0.5 With a disability under 18 years 9,979±2,065 5,215±1,595 With a disability 18-64 years 66,104±5,2066 34,451±3,499 With a disability 65+ years 63,051±3,695 28,093±2,581 Sex (% with a Disability) Females 519,710±1,165 (14.0±0.9) 293,320±497 (12.3±1.3) Males 485,841±1,475 (13.6±1.1) 275,594±533 (11.5±1.2) Race / Ethnicity (% with a Disability) Asian alonea 41,396±1,750 (6.0±1.7) 34,143±1,360 (4.8±1.5) Black/African American alonea 220,524±4,731 (14.1±1.9) 144,739±3,535 (13.2±1.8) White alonea 603,201±4,199 (15.0±0.9) 309,249±2,855 (12.8±1.2) Two or more racesa 96,968±6,106 (11.8±2.0) 52,209±5,298 (9.5±2.5) Hispanic/Latino (of any race) 104,293±621 (8.7±1.8) 64,937±191 (8.6±2.3) Household Income Median (USD) 82,174±2,002 86,010±4,378 Mean (USD) 105,438±2,965 109,393±4,213 % Below Poverty Level 9.4±0.9 9.6±1.2
Table 1. Delaware and New Castle County Characteristics from the 2022 American Community Survey
IDPark Name (Inaugural Year)Size (acres) Physical Activity-Related Amenities Address 1 Glasgow Regional Park (NR – 2016 for the H!gh 5 Sensory Playground) 250 Basketball Courts, H!gh 5 Sensory Playground†, Playground, Tennis Courts, Trails/Paths 2275 Pulaski Hwy Newark, DE 19702 2Kells Park (NR) 5.2 Baseball / Softball Field, Basketball Courts, Playground, Soccer Field, Tennis Practice Wall, Trails/Paths 201 Kells Ave. Newark, DE 19711 3Hillside Park (2021) 7Natural Play Area, Playground, Trails/Paths 103 Hillside Rd. Newark, DE 19711 4Paper Mill Park (NR) NR Basketball Courts, Soccer Field, Playground, Tennis Courts, Trails/Paths 1050 Paper Mill Rd. Newark, DE 19711 5Preston’s Playground (2018) 0.07 ‘All-Inclusive’ Playground 250 Old Paper Mill Rd. Newark, DE 19711 6 New Castle Battery Park (NR – 2023 for Playground) NR Playground, Trails/Paths 1 Delaware St. New Castle, DE 19720 7Brandywine Springs Park (NR)62.35 Baseball / Softball Field, Basketball Court, Playground, Trails/Paths, Volleyball 3302 Faulkland Rd. Wilmington, DE 19803 8Banning Regional Park (NR) NR Baseball / Softball Field, Fitness Circuit, Playground, Soccer Field, Tennis Court, Track, Trails/Paths, Volleyball 102 Middleboro Rd. Wilmington, DE 19804 9Canby Park (1916) 43.5 Baseball Fields, Basketball Courts, Football Field, Playground, Tennis Courts, Trails/Paths 901 S. Clayton St. Wilmington, DE 19805 10Cool Springs Park (1862) 14.7 Playground, Trails/Paths 1001 N Van Buren St. Wilmington, DE 19806
Table 2. Characteristics of the Parks with the Included Play Areas from Assessment using the Community Health Inclusion Index (CHII) Tool from April to November 2023.
NR = not reported on park website or cannot be determined † Delaware’s first playground designed for children with autism spectrum disorder. 76 Delaware Journal of Public Health - March 2024
(Table 1
). The inclusion criteria stipulated that the play areas must be outdoor, publicly accessible, and equipped with play components designed for play, socialization, or learning. Parks and associated playgrounds that required admission or parking fees were excluded from the study. The key determinant in selecting these sites was their community relevance, ensuring that the study’s insights would be meaningful across various suburban and urban contexts. Although convenience played a role in the selection process, this strategic approach ensured that the study’s findings effectively contributed to the broader discourse on public space accessibility. The characteristics of the included parks and playgrounds can be found in Table 2.
Instrumentation
The Community Health Inclusion Index (CHII) Tool, a validated instrument, is designed to assess the inclusivity of community health resources for individuals with disabilities.22 This tool encompasses an on-site assessment survey tailored to evaluate the accessibility of built environments in various community settings, including parks and playgrounds. The CHII survey methodically examines the navigability and usability of these sites for people with disabilities, focusing on identifying potential barriers and facilitators to accessibility. The tool comprehensively evaluates external factors such as sidewalks, parking, intersections, and public transportation stops, providing insights into the overall accessibility of facilities. Additionally, it explores internal environmental elements, including health promotion materials, restrooms, and playground equipment, to assess their suitability for individuals with disabilities. The survey utilizes a mix of question types—yes/no, multiple-selection, and a four-point Likert scale ranging from none to all. The CHII Tool’s reliability and validity have been rigorously tested across 164 sites in five states. This testing has confirmed its efficacy, as indicated by high inter-rater agreement and strong Cronbach’s alpha coefficients ranging from 0.70 to 0.97. Such robust validation underlines the CHII Tool’s suitability and effectiveness for use in this study.
Procedures
Data collection for this study was conducted from April to November 2023, involving two teams, each comprising two University of Delaware students. These students were either undergraduates in their junior or senior year who had previously completed an Introductory Adapted Physical Activity course or graduate students from the College of Health Sciences who had not taken this course but pursued relevant coursework. This background provided a foundational understanding of disability and how to adapt environments to promote full participation in PA. Prior to the assessments, the students underwent comprehensive instruction and training in the CHII protocol to ensure accuracy and consistency in their evaluations. Post-training, each team was assigned a specific park and given a 14-day window to conduct the full CHII observational audit. This process involved independently evaluating the park’s accessibility and usability features, guided by the official CHII instrument. For the observational audits, the teams were equipped with standard rulers and smart tools for measuring slopes in accordance with the ADAAG. These tools ensured precise and standardized data collection across all sites. Following the on-site evaluations, the students recorded their data into a central spreadsheet. This submission included detailed supporting information for each aspect of the park’s evaluation, ensuring a comprehensive data set for analysis.
Data Analysis
Initially, the collected data underwent a quality check conducted by the first and third authors (L.R. and I.O.) to ensure the dataset’s integrity and readiness for in-depth analysis. Once verified, the data were compiled into a cohesive dataset and then exported to the SPSS statistical software package (IBM Corp. Released 2023. IBM SPSS Statistics for Mac, Version 29.0.1. Armonk, NY: IBM Corp) for further analysis. Descriptive statistical methods were employed to summarize the data. Cronbach’s alpha coefficients were calculated to evaluate the reliability of the CHII. The range of these coefficients, from .69 to .99, indicated varying degrees of internal consistency across different subscales, with the lowest scores for walking support and promotional materials. Additionally, inter-rater agreement was calculated to assess the consistency of the rating conducted between the two teams, each comprising two students, across all evaluated sites. The results showed strong agreement for most parks, indicating a high level of consistency in the data collection process by the different raters.
RESULTS
Characteristics of Zip Code Areas
The ten play areas in New Castle County were distributed across various zip code areas, with one each in 19702, 19720, 19803, 19804, 19805, and 19806, and four in 19711, as shown in Figure 1. Collectively, these zip codes have an approximate population of 253,581 (range: 9,898-59,679). Notably, around 13% of the population across these areas are people with disabilities (range: 8.7-15.1%). The distribution of disability is almost equal between females (12.4%) and males (13.2%). Breaking down by age groups, the data show approximately 3,215 children and adolescents under 18 years, 16,016 adults aged 18 to 64, and 11,661 adults aged 65 and older have a disability. Racial and ethnic composition in these areas includes about 12,119 individuals identifying as Asian alone, 66,952 as Black or African American alone, 142,125 as White alone, and 17,618 as two or more races. In addition, there are 35,633 individuals identified as Hispanic or Latino of any race. Economic factors vary across these zip codes, with the estimated median and mean household incomes ranging from $55,912 to $122,853 and $71,418 to $175,462, respectively. The percentage of people living below the poverty level in these areas ranges from 3.6% to 22.0%.
Park Characteristics
The management of these ten sites is split between the City of Newark (Parks 1-5), New Castle County (Parks 6-9), and the City of Wilmington (Park 10), indicating varied stewardship by local government entities. This diverse stewardship is reflected in the physical attributes of each site, which vary considerably in size (range: 0.07-250 total acres), types of playground equipment, availability of sport and recreation fields and courts (e.g., baseball and softball fields, basketball courts, soccer fields, tennis courts), the extent of green spaces, and the presence of trails and pathways (see Table 2). Preliminary observations highlight variations in accessibility features at these sites, including available parking spaces, presence of key facilities such as restrooms and benches, and maintenance of trail and pathway conditions. According to information available on their official websites, these parks and playgrounds serve as popular spots for residents, utilized for leisure PA, recreation, exercise, sporting events, and other
77

community gatherings, thereby playing an important role in the daily lives of the community members. However, it’s important to note that our study did not directly assess the actual number of residents using these parks at the time of assessment. Therefore, while the websites provide a sense of the parks’ intended use and the range of activities they can accommodate, they do not offer specific data on usage frequency or popularity among residents.
Public Transit Availability and Accessibility
In evaluating public transit near ten park and playground sites, the study identified notable accessibility gaps for people with disabilities. Only six sites (60%) had nearby transit stops (i.e., bus, train, and other fixed route stops within a few blocks—up to a ¼ mile—from the site). During peak hours, transit frequency varied: services were available every 15 minutes or less at one site (17%), at 16-30-minute intervals at another site (17%), and at intervals exceeding 30 minutes at four sites (67%). During offpeak hours, transit services were within 30 minutes at one site (17%), 31-60 minutes at three sites (50%), and over 60 minutes at two sites (33%). Among the six sites with nearby transit stops, two (33%) were served by public transit vehicles equipped with level boarding options, such as ramps or lowered vehicles, and auditory announcements. All six sites had stops with visual displays. Transit-stop amenities varied: three stops (50%) had
shelters, and five (83%) provided features such as signage with Text-To-Voice numbers, benches, seating, and space for maneuvering mobility devices. However, stable and firm landing pads were found at only two stops (33%), and sufficient lighting was found at four stops (67%).
Pathway Supports and Barriers
The assessment of pathway supports and barriers at the ten sites revealed various accessibility features. Researchers uniformly rated all sites as safe for walking or rolling on paths. Six sites (60%) had some buffer between sidewalks and streets, such as landscaping or parking lanes, while four sites (40%) featured more extensive buffers. In terms of amenities, five sites (50%) were noted for their ample benches or seating options, although one site lacked these entirely. Trees or shade, conducive to pleasant PA-promoting environments, were abundant in eight sites (80%), with two sites (20%) having extensive green spaces.
Pathway conditions varied; four sites (40%) were rated as having thoroughly clean and well-maintained pathways, three (30%) were observed to have many clean paths, and three (30%) had some. Noise pollution was rated as generally moderate, with seven sites (70%) rated as having some noise and only one site (10%) rated as entirely free from noise pollution. The researchers infrequently
Figure 1. 2023 Park locations across New Castle County, Delaware
78 Delaware Journal of Public Health - March 2024
Note: (1) Glasgow, (2) Kells, (3) Hillside, (4) Paper Mill, (5) Preston’s Playground, (6) New Castle Battery, (7) Brandywine Springs, (8) Banning, (9) Canby, and (10) Cool Spring.
observed loitering, with six sites (60%) having no related issues and eight (80%) being graffiti-free. However, seven sites rated litter as a prevalent issue (70%).
Curb cuts, which are sloped transitions between the sidewalk and street level designed to facilitate access for individuals using wheelchairs or with mobility impairments, were deemed necessary by the researchers at five sites (50%). Six sites (60%) had curb cuts with an appropriate slope, and eight (80%) were rated free of barriers. However, complete freedom from surface breaks at curb cuts was found only at one site (10%), and two sites (20%) did not have detectable warnings in good condition.
Intersections Accessibility
The assessment of intersection accessibility across the ten sites yielded mixed results. All crossings near these sites were well-marked with stripes, paint, or bricks, demonstrating a consideration for pedestrian safety. Researchers found that seven sites (70%) had all crossings clear of obstacles or hazards, two sites (20%) had many clear crossings, and one site (10%) had some. Regarding wheelchair accessibility, curb cuts were present at both ends of crossings in eight sites (80%) and partially in two sites (20%), indicating room for improvement. Auditory crossing signals were present at three intersections (30%) near the parks, enhancing accessibility for pedestrians with visual impairments. Visual countdowns, essential for those with hearing impairments, were observed at five intersections (50%). Nonetheless, only two sites (20%) were noted to have crossing signals that provide sufficient crossing time for pedestrians with slower mobility.
Parking Availability and Accessibility
Of the ten parks and playgrounds surveyed, nine (90%) were found to have parking lots, indicating a high level of vehicular accessibility. Of the nine sites with parking lots, eight (89%) prominently displayed the International Symbol of Accessibility in their parking spaces, indicating a commitment to inclusivity. Furthermore, all nine parking lots provided access aisles of at least five feet in width adjacent to the accessible parking spots, enhancing overall usability. Notably, seven sites (78%) included designated van-accessible parking spaces, explicitly accommodating visitors who use larger mobility aids.
Entrance Accessibility
In evaluating the entrances at the ten park and playground sites, it was observed that all sites (100%) were free of stairs and doors at the main entrances, facilitating unobstructed access for individuals with mobility challenges, including those using manual or electric wheelchairs, canes, crutches, or other assistive devices. This uniform absence of staircases and doors rendered additional features, such as ramps, lifts, and separate accessible entrances, unnecessary. Consequently, elements like power assist, automatic doors, and other potential entrance barriers were also not applicable. This approach to eliminating common physical barriers demonstrates a strong commitment to ensuring the initial accessibility and inclusivity for all visitors to these recreational and PA-promoting areas.
Health Promotional Materials
The assessment of the availability of health promotional materials at the park and playground sites revealed a significant shortfall in accessible material formats. None of the sites provided promotional materials for PA or nutrition education programs in an electronically accessible plain text format,
which includes text descriptions of pictures. This omission of digitally accessible information could potentially restrict the accessibility of health promotion efforts, primarily affecting those who rely on digital formats. Furthermore, eight sites (80%) did not provide promotional materials in large print, which is crucial for individuals with visual impairments, with only two sites (20%) accommodating this need. The study also noted a lack of pictograms, a format beneficial for individuals with intellectual and developmental disabilities, such as autism, in eight sites (80%). Only two sites (20%) incorporated such materials. These findings point to a pressing need for more inclusive and diverse formats in health promotional materials at these recreational spaces.
Restrooms Availability and Accessibility
The assessment of restroom facilities revealed both strengths and areas needing improvement. Eight sites (80%) had restroom facilities, which is critical for visitor comfort. However, a notable gap was the absence of automatic doors or open corridor entrances in the restroom, which could impede accessibility for individuals with mobility impairments. The researchers rated door operability as generally good, with seven of the eight restrooms (88%) requiring minimal force to open. Nevertheless, only five (63%) featured door handles operable with a closed fist (i.e., without the necessity for pinching, grasping, or twisting the wrist), indicating a need for improvement in this area. The door opening width met accessibility standards (at least 32 inches) in seven restrooms (88%), accommodating users with mobility aids. Stall features varied: door handles and latches operable with a closed fist were present in four restrooms (50%), and grab bars, essential for safety, were available in seven (88%). Additionally, six restrooms (75%) offered adequate space within stalls for mobility devices, suggesting a general accommodation for diverse mobility needs.
Playgrounds and Multi-use Trails Accessibility
An examination of playgrounds and multi-use trails at ten parks and playground sites revealed various accessibility features. Concerningly, only half (5 out of 10, 50%) of the playgrounds offered ground material suitable for mobility devices, such as poured-in plastic rubber, pointing to a need for universally accessible surfaces. Ground-level play components were more commonly available, present in seven playgrounds (70%). However, the accessibility of elevated play components was less common, with only four playgrounds (40%) featuring ramps or transfer equipment, limiting accessibility for children with mobility impairments. In contrast, the multi-use trails demonstrated a commendable level of accessibility. All surveyed trails featured benches, rest areas, and firm, smooth surfaces essential for safe navigation with mobility devices. These trails’ design also included a minimum width of five feet and an absence of obstacles, highlighting their accessible design and maintenance.
DISCUSSION
This research study conducted a comprehensive assessment of the accessibility of parks and playgrounds in New Castle County, Delaware, with a particular focus on identifying their usability for people with disabilities. Utilizing the Community Health Inclusion Index (CHII) Tool, the study thoroughly evaluated various aspects of these public spaces. The findings illuminate the current state of these natural and built environments,
79
highlighting the accessibility, availability, and functionality of essential amenities central to fostering inclusive experiences. Importantly, the study considers the broader context of chronic disease prevention and mitigation, recognizing the significant health disparities faced by Delawareans with disabilities. Historically, people with disabilities have been inadequately represented in the planning, development, and maintenance of spaces that promote recreation and PA. By identifying existing gaps in accessibility, this research aims to advocate for equitable access and active participation in recreational and PA environments. Such efforts are vital not only for directly including people with disabilities in chronic disease prevention initiatives but also for promoting health, well-being, and overall quality of life for the entire community.
A key finding in this study is the limited availability and frequency of public transit services near parks and playgrounds, particularly during peak hours. This situation presents a barrier for nearly half of people with disabilities, impeding their ability to reach destinations in a timely manner23 and consequently reducing their opportunities for leisure PA. This finding underscores the crucial role of transit infrastructure in promoting PA participation.21,24 Enhancing public transit services, such as constructing new stops closer to park and playground entrances, adding shelters, and enhancing accessible features like platform gaps and lighting, could substantially increase PA among people with disabilities.21,25 Furthermore, the lack of essential accessibility features on public transit vehicles, such as auditory announcements and assistance mechanisms, presents challenges, particularly for people with vision23,26 or mobility23 impairments. In urban areas like Newark and Wilmington, issues like unannounced stops and overcrowded vehicles are more frequent compared to suburban or rural areas.23 Effective solutions include integrating vehicle modifications and assistive technology. As suggested by Bezyak et al.,23 equipping public transit vehicles with auditory stop announcements and text alerts can aid passengers with auditory disabilities. Developing personal assistive applications with GPS capabilities can enhance route planning and provide essential travel information, thereby improving navigation and accessibility. These improvements are crucial for facilitating safe and convenient access for people with disabilities and enhancing the universal appeal and usability of public parks and playgrounds.
In addressing availability and accessibility for those who do not use public transportation, our study identified a notable gap in the availability of van-accessible parking spaces despite most sites offering parking lots with accessible features. This barrier is not unique to our study’s sites but is a widespread concern in both indoor community fitness and recreational facilitaties18 and outdoor areas across the US25 and internationally.27,28 Notably, Perry et al.27 reported that less than a third of the 21 parks they evaluated had adequate, accessible parking spaces, often falling short in the dimension of aisles. Rosenberg et al. echoed these findings, noting barriers such as limited aisles space for vehicle access, a scarcity of available, accessible parking spots, distant placement of accessible parking from park entrances, and a lack of accessible routes within parking lots.25 Addressing these by ensuring the availability of van-accessible parking spaces is imperative for equitable access to recreation and PA.25 Furthermore, the study emphasizes the need for enhanced
intersection accessibility near recreational areas, citing the safety concerns due to the absence of traffic control devices and adequate auditory and visual signals at crossings. Although the present study observed positive aspects such as stair-free park and playground entrances, effective accessibility planning must consider all aspects of transportation and navigation from the point of entering parks and playgrounds.
Inside the parks, the present study highlighted the critical role of well-maintained pathways, appropriately designed and constructed curb cuts, and accessible parking in facilitating inclusive routes for PA, such as jogging, running, rolling, and walking. Regular maintenance of pathways to ensure level and even surfaces, effective litter management, and strategic curb-cut construction are essential for ensuring safety and ease of navigation, particularly for people with visual or mobility impairments. In a nationwide analysis of 401 local public entities, only nine reported the accessibility of curb cuts and sidewalks, of which only 35% of curb cuts and 52% of sidewalks were accessible.29 The findings of the present study mirror this national shortfall, with only one park (10%) meeting all curb-cut accessibility standards. Once on pathways, the researchers in this study consistently rated all sites as safe for walking or rolling. This finding contradicts recent findings for people with mobility impairments in urban parks and forests, who noted difficulties with uneven gravel surfaces, especially after unfavorable weather.25,28,30 Pathways composed of aggregate materials may provide suitable access to parks for people with mobility impairments and use wheelchairs.30
In this study, all multi-use trails were found to be smooth, unobstructed, and wide, contrasting with the findings of Perry et al.,27 reported limited availability of sites with adequately wide paths (about 5 feet). A key opportunity identified in this study is the enhancement of trail accessibility, particularly benefiting users with visual, cognitive, or mobility impairments. In another study, in-depth interviews with people with disabilities highlighted the need for navigational aids throughout parks, particularly in larger ones and those with varied terrain and distances between facilities. In addition, providing information about the park layouts near park entrances can significantly assist in navigation and accessibility.28 In addition, these participants revealed difficulties with navigating large parks (greater than 180 acres), particularly with layouts that considerably separate facilities.28 With park sizes in this study ranging from 0.07 to 250 acres, the addition of navigational aids providing relevant information about trail conditions, especially in larger parks, can be particularly meaningful in boosting the usability of these spaces. Furthermore, integrating features compatible with wayfinding technologies31 or adapting existing signages to include pictograms, visual aids, and interactive tactile elements could facilitate independent and safe navigation throughout the park, especially for people with visual or cognitive impairments. This approach can expand opportunities for PA across the entire park, making these spaces more accessible and usable.
The study’s examination of multi-use trails indicated significant progress in accessibility. Yet, it identified a pressing need for more comprehensive enhancements in playground designs to fully support people with disabilities. Among the ten playgrounds evaluated, only Glasgow Regional Park’s H!gh 5 Sensory Playground, tailored for children and adolescents with autism,
80 Delaware Journal of Public Health - March 2024
and Preston’s All-Inclusive Playground were specially designed to meet the needs of people with disabilities. These playgrounds exemplified inclusive design, with universally accessible ground materials, ramps, or transfer systems for accessing elevated play structures and various ground-level play elements. Consistent with existing research,27 only four of the playgrounds (40%) in the study incorporated transfer systems that seamlessly connected ground-level and elevated play components, accommodating children and adolescents with mobility impairments. Park renovations, such as the expansion of play areas or the addition of new elements, known to increase PA participation in children and adults, particularly in low-household-income areas,32 are crucial. Implementing such inclusive design enhancements, which align with established accessibility standards, serves to enhance the overall experience and enjoyment of parks and playgrounds for community members of all ages and abilities.
Another key finding of this study is the lack of diverse and accessible formats in health promotional materials. Notably, none of the evaluated sites used electronic American Standard Code for Information Interchange (ASCII) formats, and most lacked large print or pictogram options. This oversight is significant, especially since a 2018 study indicated that most cardiovascular disease health promotion programs in Delaware did not adequately serve people with disabilities.33 Enhancing the reach and inclusivity of these programs is essential. Therefore, adopting more inclusive strategies for creating and distributing these materials in person and on park websites is crucial to ensure they are accessible and relevant to a broad audience, including those with disabilities. A 2022 study reinforces this need, with 93% of participants with disabilities expressing a desire for accessible information about events in local parks.28 Events in Delaware parks, ranging from social and cultural gatherings to PA-related activities, such as sports games, practices, camps, walks, 5K races, and outdoor group fitness classes, offer community members holistic opportunities to improve their biopsychosocial health outcomes and engage in active lifestyles.20,33
Drawing upon comprehensive research, including an extensive 2018 review,34 this study contributes valuable insights into how improved accessibility in public transportation, parks, and playgrounds can potentially promote PA participation for all community members. It echoes the key principles of the WHO’s ICF framework,1 emphasizing the implicit influences of accessible environments in determining the functioning and PA participation of people with disabilities. Consistent with the ADA, Delaware Division of Public Health,8 and the 2018 Physical Activity Guidelines for Americans, 11 this research highlights the urgent need to surpass mere compliance with legal accessibility standards. Instead, it calls for the proactive design and construction of community spaces that promote PA and contribute to chronic disease prevention. The findings in the present study align with the global objective of building inclusive communities, emphasizing equitable access to health-promoting activities. This is particularly vital for people with disabilities, who may face compounded disparities across additional personal determinants,35 such as gender, race, ethnicity, or income. For example, additional public transportation barriers are faced by people with disabilities who identify as female or Hispanic/Latino or who are around the poverty level.26 To fully achieve the vision of “healthy people in healthy communities,”8
we advocate for collaborative design and maintenance strategies that embrace diverse cultural perspectives. This approach will ensure meaningful and cost-effective improvements in the accessibility and usability of parks and playgrounds for all community members.
Moreover, this study uncovers a regulatory gap: the ADAAG are not being fully implemented in some recreational sites in New Castle County. This gap points to inconsistencies in ensuring accessible play areas for people with disabilities and underscores the necessity of rigorously enforcing these guidelines. Across the US, most local public entities (86%) lack ADA transition plans to implement accessibility improvements and maintenance for accessible travel pathways.29 As the First State, there is a compelling call for stakeholders within Delaware to lead by example in addressing these regulatory gaps, ensuring compliance with ADAAG standards. Such initiative is crucial for the inclusive and accessible design, construction, and alteration of today’s and tomorrow’s parks and playgrounds.
STRENGTHS AND LIMITATIONS
This research study is characterized by notable strengths that enhance its impact. First, utilizing the CHII Tool, recognized for its validity and reliability, provides a robust framework for evaluating the accessibility of parks and playgrounds. The comprehensive nature of this tool enables a detailed examination of a multitude of critical accessibility factors, ranging from public transit and parking to internal environmental elements. Second, the study’s diverse sampling strategy, featuring ten parks and playgrounds across different zip codes in New Castle County, Delaware, including both urban and suburban areas, significantly broadens the applicability of its findings. Third, the data collection, conducted by university students trained in adapted physical activity and employing standardized measurement tools, along with stringent data quality checks, significantly enhances the study’s reliability and the credibility of its findings. Despite its strengths, the study has several limitations that warrant consideration. First, its geographical focus on New Castle County, Delaware, may constrain the broader relevance of its findings to other areas in the US, as other regions in the US may present varied accessibility and usability challenges. Second, the study may be subject to selection bias due to the convenience-based choice of sites and the exclusion of parks with admission or parking fees. This approach might have restricted the comprehensive accessibility assessment across a broader range of public spaces. Third, a significant limitation of the study is its reliance on observational data, which may not fully capture the intricate experiences and perspectives of people with disabilities utilizing these parks and playgrounds. Gathering firsthand feedback from this group is essential for a complete and nuanced understanding of accessibility and usability issues and their impact on inclusion and PA participation. Such personal insights are vital for a comprehensive assessment of the intricacies that impact the influences of various environmental factors on the functioning and PA participation of people with disabilities within the ICF framework. Fourth, although efforts were made to ensure measurement accuracy, the inherent nature of manual tools and human observation can introduce minor errors or inconsistencies in data collection, potentially affecting the precision of the findings.
81
CONCLUSION
This research study significantly contributes to our understanding of public space accessibility, advocating for equitable access and active participation in recreational and PA environments. It underscores the imperative to develop inclusive public spaces that support active living and contribute to mitigating chronic disease risks among all community members, with a particular emphasis on those with disabilities. The findings represent a crucial call to action for current stakeholders, including policymakers, urban planners, and community organizations, who must unite with community members in their efforts to dismantle these barriers and reimagine public spaces that exceed mere legal compliance, striving instead for environments that are universally welcoming and accommodating to people regardless of disability status. This research underscores the importance of understanding accessibility as a dynamic, multi-faceted concept that goes beyond physical infrastructure. It calls for a more holistic approach to public space design that considers the diverse experiences and needs of people with disabilities and integrates these considerations into our community spaces. By doing so, we can ensure public parks and playgrounds are not just spaces for PA and recreation but also for social inclusion, health promotion, and community well-being.
PUBLIC HEALTH IMPLICATION
This study addresses a critical aspect of public health by evaluating the accessibility and usability of parks and playgrounds in New Castle County, Delaware, for people with disabilities. It highlights the importance of inclusive public spaces in promoting PA and mitigating chronic disease risks. The findings reveal significant barriers to accessibility, underscoring the need for improvements in public transit, parking, and playground design, construction, and maintenance. By advocating for more accessible and inclusive recreational environments, this research contributes to the broader goal of reducing health disparities among people with disabilities and supports the public health vision of creating healthier communities for all. This study’s outcomes are particularly relevant for policymakers, urban planners, and public health professionals, providing them with actionable insights to foster equitable access to PA opportunities and enhance the overall well-being of diverse community populations. Dr. Obrusnikova may be contacted at obrusnik@udel.edu
REFERENCES
1. World Health Organization. (2001). International classification of functioning, disability and health. Geneva.
2. Paul, S., Rogers, S., Bach, S., & Houtenville, A. J. (2023). Annual Disability Statistics Compendium: 2023. Durham, NH: University of New Hampshire, Institute on Disability.
3. Khavjou, O. A., Anderson, W. L., Honeycutt, A. A., Bates, L. G., Hollis, N. D., Grosse, S. D., & Razzaghi, H. (2021). Statelevel health care expenditures associated with disability. Public health reports (Washington, D.C.: 1974), 136(4), 441–450. https://doi.org/10.1177/0033354920979807
4. Froehlich-Grobe, K., Jones, D., Businelle, M. S., Kendzor, D. E., & Balasubramanian, B. A. (2016, October). Impact of disability and chronic conditions on health. Disability and Health Journal, 9(4), 600–608.
https://doi.org/10.1016/j.dhjo.2016.04.007
5. Dixon-Ibarra, A., & Horner-Johnson, W. (2014, January 30). Disability status as an antecedent to chronic conditions: National Health Interview Survey, 2006-2012. Preventing Chronic Disease, 11, 130251.
https://doi.org/10.5888/pcd11.130251
6. Krahn, G. L., Walker, D. K., & Correa-De-Araujo, R. (2015, April). Persons with disabilities as an unrecognized health disparity population. American Journal of Public Health, 105(Suppl 2, Suppl 2), S198–S206.
https://doi.org/10.2105/AJPH.2014.302182
7. Reichard, A., Stolzle, H., & Fox, M. H. (2011, April). Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disability and Health Journal, 4(2), 59–67.
https://doi.org/10.1016/j.dhjo.2010.05.003
8. Delaware Center for Health Statistics. (2021). Delaware vital statistics annual report, 2018. Delaware Health and Social Services, Division of Public Health.
9. Rattay, K. T., Henry, L. M. G., & Killingsworth, R. E. (2017, April 19). Preventing chronic disease: The vision of public health. Delaware Journal of Public Health, 3(2), 52–56.
https://doi.org/10.32481/djph.2017.04.008
10. Frank, H. R., Mulder, H., Sriram, K., Santanam, T. S., Skinner, A. C., Perrin, E. M., Armstrong, S. C., Peterson, E. D., Pencina, M., & Wong, C. A. (2020). The dose-response relationship between physical activity and cardiometabolic health in young adults. The Journal of adolescent health: official publication of the Society for Adolescent Medicine, 67(2), 201–208. https://doi.org/10.1016/j.jadohealth.2020.04.021
11. Physical Activity Guidelines for Americans Committee. (2018). 2018 Physical Activity Guidelines Advisory Committee Scientific Report. In: US Department of Health and Human Services.
12. Carroll, D. D., Courtney-Long, E. A., Stevens, A. C., Sloan, M. L., Lullo, C., Visser, S. N., . . . Dorn, J. M., & the Centers for Disease Control and Prevention (CDC). (2014, May 9). Vital signs: Disability and physical activity—United States, 20092012. MMWR. Morbidity and Mortality Weekly Report, 63(18), 407–413. https://pubmed.ncbi.nlm.nih.gov/24807240
13. Martin Ginis, K. A., van der Ploeg, H. P., Foster, C., Lai, B., McBride, C. B., Ng, K., . . . Heath, G. W. (2021, July 31). Participation of people living with disabilities in physical activity: A global perspective. Lancet, 398(10298), 443–455. https://doi.org/10.1016/S0140-6736(21)01164-8
14. Giles, L. V., Koehle, M. S., Saelens, B. E., Sbihi, H., & Carlsten, C. (2021, June 30). When physical activity meets the physical environment: Precision health insights from the intersection. Environmental Health and Preventive Medicine, 26(1), 68.
https://doi.org/10.1186/s12199-021-00990-w
15. Jerome, G. J., Boyer, W. R., Bustamante, E. E., Kariuki, J., Lopez-Jimenez, F., Paluch, A. E., . . . Barone Gibbs, B., & the American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Peripheral Vascular Disease. (2023, June 20). Increasing equity of physical activity promotion for optimal cardiovascular health in adults: A scientific statement from the American Heart Association. Circulation, 147(25), 1951–1962.
https://doi.org/10.1161/CIR.0000000000001148
82 Delaware Journal of Public Health - March 2024
16. Sallis, J. F., Cerin, E., Kerr, J., Adams, M. A., Sugiyama, T., Christiansen, L. B., . . . Owen, N. (2020, April 2). Built environment, physical activity, and obesity: Findings from the International Physical Activity and Environment Network (IPEN) adult study. Annual Review of Public Health, 41, 119–139. https://doi.org/10.1146/annurev-publhealth-040218-043657
17. Architectural and Transportation Barriers Compliance Board. Americans With Disabilities Act Accessibility Guidelines for Buildings and Facilities; Architectural Barriers Act Accessibility Guidelines; Self-Service Transaction Machines and Self-Service Kiosks [Proposed Rule]. https://www.federalregister.gov/documents/2022/09/21/2022-20470/ americans-with-disabilities-act-accessibility-guidelines-for-buildingsand-facilities-architectural
18. Rimmer, J. H., Riley, B., Wang, E., Rauworth, A., & Jurkowski, J. (2004, June). Physical activity participation among persons with disabilities: Barriers and facilitators. American Journal of Preventive Medicine, 26(5), 419–425. https://doi.org/10.1016/j.amepre.2004.02.002
19. Eisenberg, Y., Vanderbom, K. A., & Vasudevan, V. (2017, February). Does the built environment moderate the relationship between having a disability and lower levels of physical activity? A systematic review. Preventive Medicine, 95, S75–S84. Retrieved from https://doi.org/10.1016/j.ypmed.2016.07.019
20. Saitta, M., Devan, H., Boland, P., & Perry, M. A. (2019, January). Park-based physical activity interventions for persons with disabilities: A mixed-methods systematic review. Disability and Health Journal, 12(1), 11–23. Retrieved from https://doi.org/10.1016/j.dhjo.2018.07.006
21. Smith, M., Hosking, J., Woodward, A., Witten, K., MacMillan, A., Field, A., . . . Mackie, H. (2017, November 16). Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. The International Journal of Behavioral Nutrition and Physical Activity, 14(1), 158.
https://doi.org/10.1186/s12966-017-0613-9
22. Eisenberg, Y., Rimmer, J. H., Mehta, T., & Fox, M. H. (2015, October 13). Development of a community health inclusion index: An evaluation tool for improving inclusion of people with disabilities in community health initiatives. BMC Public Health, 15(1), 1050.
https://doi.org/10.1186/s12889-015-2381-2
23. Bezyak, J. L., Sabella, S. A., & Gattis, R. H. (2017). Public transportation: An investigation of barriers for people with disabilities. Journal of Disability Policy Studies, 28(1), 52–60. https://doi.org/10.1177/1044207317702070
24. Xiao, C., Goryakin, Y., & Cecchini, M. (2019, March). Physical activity levels and new public transit: A systematic review and meta-analysis. American Journal of Preventive Medicine, 56(3), 464–473.
https://doi.org/10.1016/j.amepre.2018.10.022
25. Rosenberg, D. E., Huang, D. L., Simonovich, S. D., & Belza, B. (2013, April). Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. The Gerontologist, 53(2), 268–279.
https://doi.org/10.1093/geront/gns119
26. Bezyak, J. L., Sabella, S., Hammel, J., McDonald, K., Jones, R. A., & Barton, D. (2020, November). Community participation and public transportation barriers experienced by people with disabilities. Disability and Rehabilitation, 42(23), 3275–3283.
https://doi.org/10.1080/09638288.2019.1590469
27. Perry, M. A., Devan, H., Fitzgerald, H., Han, K., Liu, L.-T., & Rouse, J. (2018, April). Accessibility and usability of parks and playgrounds. Disability and Health Journal, 11(2), 221–229.
https://doi.org/10.1016/j.dhjo.2017.08.011
28. Wojnowska-Heciak, M., Suchocka, M., Błaszczyk, M., & Muszyńska, M. (2022, February 11). Urban parks as perceived by city residents with mobility difficulties: A qualitative study with in-depth interviews. International Journal of Environmental Research and Public Health, 19(4), 2018.
https://doi.org/10.3390/ijerph19042018
29. Eisenberg, Y., Heider, A., Gould, R., & Jones, R. (2020). Are communities in the United States planning for pedestrians with disabilities? Findings from a systematic evaluation of local government barrier removal plans. Cities (London, England), 102, 102720.
https://doi.org/10.1016/j.cities.2020.102720
30. Lepoglavec, K., Papeš, O., Lovrić, V., Raspudić, A., & Nevečerel, H. (2023). Accessibility of urban forests and parks for people with disabilities in wheelchairs, considering the surface and longitudinal slope of the trails. Sustainability, 15(10), 7741.
https://doi.org/10.3390/su15107741
31. Gupta, M., Abdolrahmani, A., Edwards, E., Cortez, M., Tumang, A., Majali, Y., . . . Kuber, R. (2020). Towards more universal wayfinding technologies: Navigation preferences across disabilities. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems (CHI ‘20). Association for Computing Machinery, New York, NY, USA, 1–13.
https://doi.org/10.1145/3313831.3376581
32. Tester, J., & Baker, R. (2009, April). Making the playfields even: Evaluating the impact of an environmental intervention on park use and physical activity. Preventive Medicine, 48(4), 316–320.
https://doi.org/10.1016/j.ypmed.2009.01.010
33. Papas, M. A., Stolz, N., Orsega-Smith, E., Sparling, E., & Freedman, B. (2018, March). The importance of inclusion for cardiovascular health promotion programs in Delaware. Health Promotion Practice, 19(2), 256–266.
https://doi.org/10.1177/1524839917704209
34. Kärmeniemi, M., Lankila, T., Ikäheimo, T., KoivumaaHonkanen, H., & Korpelainen, R. (2018, February 17). The built environment as a determinant of physical activity: A systematic review of longitudinal studies and natural experiments. Ann Behav Med, 52(3), 239–251.
https://doi.org/10.1093/abm/kax043
35. Akobirshoev, I., Mitra, M., Li, F. S., Dembo, R., Dooley, D., Mehta, A., & Batra, N. (2020, December). The compounding effect of race/ethnicity and disability status on children’s health and health care by geography in the United States. Medical Care, 58(12), 1059–1068.
https://doi.org/10.1097/MLR.0000000000001428
83

2022 DHSA Research Competition
Call for Abstracts
DHSA is seeking population health research proposals from students, faculty, or staff affiliated with any of DHSA’s member institutions. This is a ‘shark tank’ type event with real -time presentations, judging and awards!
This year, proposals are requested to have a Population Health focus specifically for vulnerable populations. Proposals may address any area of population health including but not limited to social determinants of health, environmental health, behavioral and mental health as related to or impacting vulnerable populations.
Vulnerable populations include but may not be limited to those individuals who experience greater risk factors due to age, gender, geographic location, sexual orientation and preferences, those who are socioeconomically disadvantaged or underinsured
Background
The DHSA Research Competition was established in 2019 to foster collaboration between colleagues at our member institutions. We favor projects in population health, including topical areas of interest such as those outlined above and encourage multidisciplinary collaborations with strong community engagement.
DHSA was established in 2009 with four founding partn ers – ChristianaCare, Nemours/Alfred I. duPont Hospital for Children, Thomas Jefferson University, and the University of Delaware. Since then, additional partners have joined including the Philadelphia College of Osteopathic Medicine, Bayhealth the Delawa re Academy of Medicine/Delaware Public Health Association, Beebe Healthcare, Delaware State University and Delaware Technical Community College.
DHSA aligns resources and efforts to create a unique, broad-based alliance, focused on establishing innovative collaboration among experts in medical practice, health economics and policy, population sciences, public health, biomedical sciences and engineering, research, medical education, and healthcare workforce development.
The alliance enables partner organizations to collaborate and conduct cutting-edge research, to improve the health of Delawareans through access to services in the state and region, and to educate the next generation of health care professionals.
Guide for Researchers
The deadline to submit proposals is 11:59pm Sunday, May 5, 2024
Proposals must include the following:
- Researcher’s Name(s)
Structured Abstract, including the overall research plan, innovat ive aspect of the proposal, budget, and budget justification
o Salary*, fringe, benefits, and indirect expenses are not allowable
▪ *salary unallowable for anyone directly employed by a DHSA member institution regardless of full or part time status, hourly or salary
- Proposed partnership with at least two of DHSA’s partner organizations
o Applicant cannot include only one researcher who spans multiple DHSA organizations, there must be a minimum of two researchers from 2 or more DHSA organizations to ensure collaboration.
o Each DHSA member institution on proposal must have an independent established PI
- A letter of support from each applicant’s Department chair or institutional leaders such as VP of Research or VP of Academic Affairs (or equivalents) is expected. The letter should address the institution’s interest in collaborating across DHSA and in supporting the applicant(s) in their work.
- Proposals must prioritize impact on Delaware populations.
Physical
Mailing
Delaware Health Sciences Alliance
Ogletown Stanton Rd | Suite L10 | Newark DE
|
Address: 4765
19713
www.dhsa.org
Concord Pike | #103 | Wilmington,
Address: 2207
DE 19803
84 Delaware Journal of Public Health - March 2024

Please submit all proposals to Pamela Gardner, DHSA Lead Program Manager, (pgardner@dhsa.o rg) no later than 11:59pm Sunday, May 5, 2024. Proposals submitted after the deadline will not be considered.
Process of Review:
- All proposals will be vetted by a review committee
- The top three scoring proposals will be invited to the final event for presentation and pitch to the DHSA panel in late Spring 2024.
o Date, location, and format of event to be announced.
o Finalists will have fifteen minutes to verbally pitch their proposal and the panel (along with community members) will have time allotted to ask questions.
o It is expected that teams will be present for the entire event.
o A rubric will be utilized by the panel and a numerical score will be given to each proposal.
o The researchers with the highest score will be announced the winner and will receive a $50,000 grant to fund their proposal and work.
In the event initial proposal scores are too close to determine the top three finalists, teams may be requested to give a brief presentation virtually to determine teams advancing to finals.
DHSA reserves the right to evaluate the final project and timeline one year after awarding funds. If funds have not been utilized after 12 months, upon review, DHSA will either grant an extension of time or require unused funds be returned to DHSA.
For any inquiries about the event, please contact Pamela Gardner (pgardner@dhsa.org). We look forward to hearing from you!
Sincerely,
Omar Khan, MD MHS President & CEO, Delaware Health Sciences Alliance okhan@dhsa.org










Delaware Health Sciences Alliance Physical Address: 4765 Ogletown Stanton Rd | Suite L10 | Newark DE 19713 | www.dhsa.org Mailing Address: 2207 Concord Pike | #103 | Wilmington, DE 19803
85
How Interprofessional Community Mobile Healthcare and Service-Learning Work Together to Identify and Address Chronic Health Disparities
Emma Mathias
Graduate Research Assistant, Epidemiology Program, University of Delaware
Peyton Free
Graduate Research Assistant, Partnership for Healthy Communities, University of Delaware
Abby Storm, M.S.
Graduate Research Assistant, Epidemiology Program, University of Delaware
Heather Milea, M.S.N., F.N.P.-B.C., A.G.A.C.N.P.-B.C.
Nurse Practitioner, HEALTH for All Program, University of Delaware
Christine Sowinski, M.S.M.
Project Coordinator, HEALTH for All Program, University of Delaware
Jennifer A. Horney, Ph.D.
Professor and Founding Director, Epidemiology Program, University of Delaware
ABSTRACT
Background: Residents of the State of Delaware experience high levels of health inequities. Service-learning programs provided jointly by universities and community partners can address health disparities through documentation of disparities and service provision that sees patients where they are. Benefits accrue for both students and communities experiencing health inequities. Methods: HEALTH for All (H4A) mobile unit clients can receive a variety of services at sites co-located with community based organizations (CBOs). Between September 2023 and January 2024, H4A clients had their blood pressure assessed by a trained healthcare provider. Demographic and ZIP Code of residence data were collected by a trained graduate student. Data were recorded and analyzed using Microsoft Excel Version 16.5 (Redmond, WA, USA). All documentation was reviewed and approved by the University of Delaware’s Institutional Review Board (IRB #1567044-3). Results: Between September 2023 and January 2024, 152 clients participated. Most participants were female (72.27%; 104 of 143) and identified as White (68.66%; 92 of 134). The largest group of clients were in Stage 1 Hypertension (34.21%; 52 of 152), followed by Elevated (23.68%; 36 of 152), Normal (22.37%; 34 of 152), and Stage 2 Hypertension (19.74%; 30 of 152). Black or African American clients had higher systolic and diastolic blood pressure compared to other racial and ethnic groups. There were also differences in the share of clients with hypertension by ZIP Code of residence.
Conclusions: Interprofessional service-learning in a mobile health context provides students with practical field experience and real-world insights into community perspectives and needs, including addressing health inequities. Academic-community partnerships and mobile health programs should be prioritized in the future to address health inequities and foster the development of socially engaged, community-minded future professionals.
INTRODUCTION
Delaware ranks thirty-first among all states in overall health and in the bottom half of all states for indicators of overall health, including exposure to air pollution, child poverty, physical inactivity, and infant mortality.1 Residents of Delaware experience high levels of health inequities, particularly racial and ethnic minorities living in the cities of Wilmington and New Castle.2 For example, the prevalence of chronic diseases among African Americans is higher than any other racial group in Delaware. More than 28% of African Americans live with chronic diseases such as diabetes, cardiovascular diseases, and asthma, leading to disparities in mortality from diabetes, kidney disease, and hypertension.3 Similarly, persistent disparities in Black infant and maternal mortality are linked to residence in high-risk ZIP Codes in Wilmington and New Castle.4
One approach to addressing health inequities is through academic-community service-learning programs.5 For example, the University of Arizona has service-learning programs that focus on serving populations that face disparities, including undocumented individuals, persons experiencing homelessness, the elderly, and those who identify as lesbian, gay, bisexual, or transgender.6 Asian-American community groups partnered with a midwestern university’s student volunteer program to train students to provide culturally competent preventive care to residents of Chicago’s Chinatown.7 In addition to community benefits, students also benefit from these academic-community service-learning placements. Public health students reported an increased interest in working in governmental public health.8 Nursing students placed in an emergency housing facility reported perceived future career benefits from the opportunity to work in community placement.9
Doi: 10.32481/djph.2024.03.10
86 Delaware Journal of Public Health - March 2024
Another approach to addressing inequities is the use of alternative types of community-based interventions such as mobile healthcare clinics to deliver direct care and services. Among mobile health clinics in the U.S. from 2007 – 2017, 35% of the clients were black and 27% were Latinx or Hispanic.10 Other populations served by mobile health include the uninsured, those living in poverty or experiencing homelessness, and migrant populations. Service-learning in a mobile health context can provide opportunities for university-community partnerships to address health inequities. At the same time, these models give students experience in providing socially engaged community care that may spark an interest in a career in health equity or assist students with building a professional network among those working to address health inequities.11 For example, physician assistants participating in a mobile clinic rotation reported a better understanding of medical needs and the intricacies of treating individuals experiencing homelessness.11 Following participation in the Oral Health on Wheels mobile clinic, dental hygiene students reported increased learning, confidence in skills, and personal growth around working with underserved populations.12
In partnership with the Highmark Blue Cross Blue Shield of Delaware’s BluePrints for the Community Program and more than 20 community-based organizations (CBOs), the University of Delaware’s College of Health Sciences’ Partnership for Healthy Communities established a mobile health service-learning program called Health, Engagement, Access, Learning, Teaching, Humanity for All (HEALTH for All) to address gaps in access to care among underserved populations in Wilmington and New Castle, Delaware. The program placed interprofessional students from clinical and non-clinical programs across the university in a mobile health unit (MHU) with a program manager and a nurse practitioner. In addition to providing care, the program was also designed to offer students hands-on experience to build interprofessional skills related to addressing health equity issues in community settings that may inform the focus of their future careers. This paper reports on a HEALTH for All project designed to assess health inequities around hypertension in New Castle County, Delaware.
METHODS
The MHU visits more than 20 CBO partner sites including community centers, senior centers, libraries, churches, and barber shops on a rotating schedule and provides basic healthcare services (e.g., screening, primary care services, chronic disease monitoring) and referrals for follow-up care when needed. When clients have completed their interactions with the healthcare provider, a trained graduate student approaches them and asks if they are willing to complete a brief demographic and self-rated health perceptions survey. Beginning in September 2023, a separate 5-question survey was administered that included age, gender, race, ZIP Code of residence, and blood pressure. Responses were recorded and analyzed in Microsoft Excel Version 16.5 (Redmond, WA, USA). All surveys and other documents were reviewed and approved by the University of Delaware’s Institutional Review Board (IRB #1567044-3).
RESULTS
One hundred and fifty two HEALTH for All clients completed the 5-question survey between September 2023 and January 2024. The mean age of respondents was 60 years (Range: 19-93). Most participants were female (72.27%; 104 of 143) and identified as White (68.66%; 92 of 134).
Elevated Blood Pressure is defined as a reading between 120 and 129 systolic and <80 diastolic. Stage 1 Hypertension is when the reading is between 130 and 139 systolic or 80 to 89 diastolic while Stage 2 Hypertension is when the reading is ≥140 systolic or ≥90 diastolic. Delaware ranks thirty-ninth out of the fifty U.S. states in terms of the percentage of adults who have been told by a health professional that they have high blood pressure.1 In the U.S. and in Delaware, non-Hispanic blacks have the highest rate of hypertension compared to non-Hispanic Whites and Asians. More than one-third of HEALTH for All clients assessed were in Stage 1 Hypertension (34.21%; 52 of 152), while around a quarter had either Elevated (23.68%; 36 of 152) or Normal (22.37%; 34 of 152) blood pressure. One in five (19.74%; 30 of 152) had Stage 2 Hypertension. Black or African American clients had higher diastolic and systolic blood pressure overall compared to other racial and ethnic groups and clients who reported the residential ZIP Code of 19720 were most likely to have Stage 1 or 2 Hypertension (29 of 38; 76.3%, Figure 1).
CONCLUSIONS
Cardiovascular diseases are the leading cause of death in the U.S. and in Delaware. Racial minorities and those living in areas characterized by poverty have a higher prevalence of unrecognized risk factors for coronary diseases. Public health interventions that target majority-minority communities are essential to addressing cardiovascular disease disparities by race in Delaware and the U.S. To carry out these interventions, current students – who are future professionals – can benefit from seeing how social, economic, and political factors impact health through a health equity lens.4,6 While MHUs can help ensure access to care and document barriers and inequities, longer-term and lasting improvements in health equity in these contexts will require additional investments and interventions to provide evidence of measurable changes in health outcomes.
PUBLIC HEALTH IMPLICATIONS
Delawareans experience high levels of health inequities that may be more effectively addressed through approaches that include evidence-based interventions to reduce health disparities including mobile health and service-learning. This paper describes an example from a University of Delaware mobile health program serving vulnerable populations in New Castle County through community engagement and student experiential learning. More evidence is needed to demonstrate how Social Determinants of Health-driven educational experiences can improve patient health equity through access, care coordination, and training the future public health and healthcare workforce to be actively engaged in addressing these issues.
ACKNOWLEDGMENTS
HEALTH for All is supported by a grant from the Highmark Blue Cross Blue Shield Delaware’s BluePrints for the Community program.
87
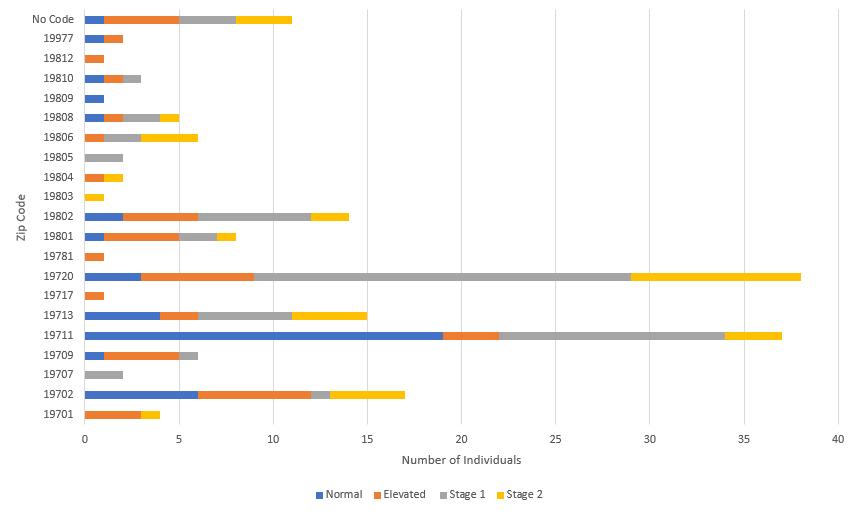
REFERENCES
1. United Health Foundation. America’s Health Rankings. Retrieved August 10, 2023, from: https://www.americashealthrankings.org/explore/annual/state/DE
2. Delaware Health and Social Services, Division of Public Health. Community Health Status Assessment 2012. 2012. Available from: https://dhss.delaware.gov/dhss/dph/files/shipchsa.pdf
3. Delaware Health and Social Services. Delaware Vital Statistics Annual Report. 2016. Available: https://www.dhss.delaware.gov/dhss/dph/hp/files/ar2016_net.pdf
4. Delaware Health and Social Services. Delaware State Health Improvement Plan. 2019. Available from: https://dhss.delaware.gov/dhss/dph/files/ship2019.pdf
5. Gillis, A., & Mac Lellan, M. (2010). Service learning with vulnerable populations: Review of the literature. International Journal of Nursing Education Scholarship, 7, e41. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/21126228/ https://doi.org/10.2202/1548-923X.2041
6. Sabo, S., de Zapien, J., Teufel-Shone, N., Rosales, C., Bergsma, L., & Taren, D. (2015, March). Service learning: A vehicle for building health equity and eliminating health disparities. American Journal of Public Health, 105(S1), S38–S43. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25706014/ https://doi.org/10.2105/AJPH.2014.302364
7. Lee, B. J., Wang, S. K., So, C., Chiu, B. G., Wang, W. Y., Polisetty, R., . . . Liu, H. (2015, November 25). A student-led health education initiative addressing health disparities in a Chinatown community. American Journal of Pharmaceutical Education, 79(9), 132. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4727369/ https://doi.org/10.5688/ajpe799132
8. Horney, J. A., Bamrara, S., Macik, M. L., & Shehane, M. (2016, Jan-Apr). EpiAssist: Service-learning in public health education. Educ Health (Abingdon), 29(1), 30–34 Retrieved from: https://pubmed.ncbi.nlm.nih.gov/26996796/
https://doi.org/10.4103/1357-6283.178925
9. Parry, Y. K., Hill, P., & Horsfall, S. (2018, September). Assessing levels of student nurse learning in community based health placement with vulnerable families: Knowledge development for future clinical practice. Nurse Education in Practice, 32, 14–20. Retrieved from:
https://pubmed.ncbi.nlm.nih.gov/30015302/ https://doi.org/10.1016/j.nepr.2018.06.015
10. Malone, N. C., Williams, M. M., Smith Fawzi, M. C., Bennet, J., Hill, C., Katz, J. N., & Oriol, N. E. (2020, March 20). Mobile health clinics in the United States. International Journal for Equity in Health, 19(1), 40. Retrieved from:
https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-020-1135-7
https://doi.org/10.1186/s12939-020-1135-7
11. Duford, A., & Matvienko, O. (2019, September). Studentled mobile health clinic: Patients served and learning experience. The Journal of Physician Assistant Education : the Official Journal of the Physician Assistant Education Association, 30(3), 149–154. Retrieved from: https://europepmc.org/article/med/31385911
https://doi.org/10.1097/JPA.0000000000000266
12. Flick, H., Barrett, S., & Carter-Hanson, C. (2016, August). Oral health on wheels: A service learning project for dental hygiene students. J Dent Hyg, 90(4), 226–233. Retrieved from:
https://pubmed.ncbi.nlm.nih.gov/27551143/
–
88 Delaware Journal of Public Health - March 2024
Figure 1. Hypertensive Status by ZIP Code, New Castle County, DE, September 2023
January 2024
“I’m asking for 45 more years.”

Ask about a prostate cancer screening, and you’re asking for so much more.
Approximately one in eight men will be diagnosed with prostate cancer during their lifetime, but one simple screening can help detect cancer when it’s most treatable. If you’re 40 or older, or have a family history of prostate cancer, ask your health care provider if and how often you should be screened. Don’t have insurance? You could be eligible for a free screening.
Visit HealthyDelaware.org/Prostate or call 2-1-1 to learn more.

89
A 6-Week Virtual Exercise/Dance Program Impacts Fitness Levels for Adults with Intellectual Disabilities: A DNP Project
Melanie Ayers, D.N.P., R.N., C.N.E. Associate Professor, Wilmington University
ABSTRACT
Adults with intellectual disabilities (ID) experience age-related diseases, such as diabetes, hypertension, cardiovascular disease, and obesity much earlier than their typical peers. Therefore, health promotion is essential in this population.1 This population tends to live sedentary lives; exercise needs to be a focus. Exercise positively impacts survival rates for those with ID.2 Motivation and support are vital factors to successfully incorporate exercise into their lives. Prevalent barriers are a lack of access to health promotion programs, support, and transportation. Creating virtual programming with exercise and support can fill this gap. The implementation of a 6-week virtual exercise/dance program with music as a motivator Doctor of Nursing Practice (DNP) project, enabled adults with ID to participate in physical activity resulting in improved cardiovascular and muscular fitness using Standing Long Jump (SLJ) and 6 Minute Walk Test (6MWT) as measures. No improvement was noted in Body Mass Index measurements.
BACKGROUND
Intellectual disability (ID), according to the American Association on Intellectual and Developmental Disabilities, is defined as a disability that originates before the age of 18, and has significant limitations in both “intellectual functioning and adaptive behavior which covers many everyday social and practical skills” (p. 422).1 Further, there are approximately 6.5 million people in the United States with ID, with ID affecting 0.5% of adults in high-income countries.1,2 Adults with ID experience age-related diseases earlier in life, and higher mortality rates from chronic, non-communicable diseases, such as diabetes, hypertension, cardiovascular disease, and obesity, than the general population.3 This is attributed, in part, to sedentary lifestyles.3,4 Obesity alone is two to three times more prevalent in individuals with ID due to obesogenic medication and sedentary lifestyles.5 Health care costs associated with a lack of physical activity are $117 billion annually.6 Multimorbidity, or having two or more chronic conditions in addition to ID, can significantly impact individuals with ID, putting those who are physically inactive at greater risk.7 Some factors related to sedentary lifestyles for those with ID include lack of motivation, acceptance of a sedentary lifestyle, lack of caregiver support, barriers to transportation, and limited access to appropriate health promotion programs.1,8
Health promotion applies to all people, including those with disabilities.9 Further, health promotion maintains and enhances function and considers the whole person as its foundation. One role of the health care provider is health promoter. This role encourages health-promoting activities, such as increasing physical activity, which may positively impact the fitness and obesity of the person with ID.1 According to the CDC (2021) only 44% of adults with disabilities received recommendations for physical activity during their doctor’s visit.10 However,
if doctors do recommend physical activity to adults with disabilities, they are 82% more likely to comply than if the doctor does not give recommendations. Additionally, the CDC (2021) recognizes 5 steps to address physical activity with adults with disabilities.10 These steps include: remembering everyone should follow the Physical Activity Guidelines; inquiring about the individual’s physical activity; talking about barriers, giving options for physical activity, and referring them to available resources and programs. Further, the CDC (2021) gives examples of programming across the country that targets this population to improve their weight and physical activity.10 The Alabama Hospital Association, Blue Cross Blue Shield Alabama, and the National Center on Health, Physical Activity, and Disability collaborated on a 10-week campaign promoting healthy weight and physical activity. The Michigan Department of Community Health partnered with the Michigan Arthritis Program to increase access with their EnhanceFitness program, which focuses on adults with developmental, cognitive, and mobility disabilities. The South Carolina Research Foundation partners with the South Carolina Department of Disabilities and Special Needs and Able-SC to promote healthy living through its Steps to Your Health program.
Person-centered care can be provided when the provider has time to get to know and understand the individual with ID.10 Providers should learn the individual’s likes, dislikes, and ideas they want for their life. Therefore, by equipping providers with the knowledge to effectively communicate and care for these individuals, fear and frustration regarding health plans can be prevented, and a more positive attitude will prevail to encourage health promotion activities. As a result, this population may experience an enhanced quality of life through physical activity.1,11 Further, community health care providers can significantly reduce the health disparities adults with ID face by helping them overcome
Doi: 10.32481/djph.2024.03.11
90 Delaware Journal of Public Health - March 2024
barriers and access health care programs. Since there is a lack of accessible programming for individuals with ID, states need to recognize the need for creating physical activity opportunities. Through collaboration, entities that understand the needs of this population can develop quality programs to reach more people with disabilities.
Health promotion with support is vital for people with intellectual disabilities (ID). This DNP project aimed to improve BMI, muscular fitness, and cardiovascular fitness in adults with ID using exercise and dance with music as a motivator. Through consistent participation, weight loss could have also been a benefit for some, in addition to developing the healthy habit of incorporating exercise into daily life.
THEORETICAL FRAMEWORK
This DNP project consisted of a virtual exercise/dance program with music as a motivator. Participants were adults with ID and attended two sessions per week over the course of 6 weeks. Both cardiovascular fitness and muscular fitness were addressed using Bollywood dancing and yoga, respectively. Nola Pender’s Health Promotion Model has guided the project. This model supported the idea that behavior change will happen if there is both a positive personal value and a desired outcome for change.9
This model focuses on wellness, self-efficacy, and that the individual’s characteristics and experiences can impact their actions.12 Further, if the individual perceives benefits or barriers to an action, this would influence their ability to change behavior. Additionally, interpersonal influences such as social support and role modeling can impact a person’s desire to change. Likewise, situational influences can directly influence behavior through the individual’s perception of the options available and the aesthetic features of the environment. Further, competing demands and competing preferences also influence the behaviors of the individual. The behavioral outcome is the endpoint in which there is a positive attitude toward the healthpromoting behavior, and there is a commitment to incorporate this behavior into one’s lifestyle.12
This project assisted the participants to begin to take ownership of their health through their commitment to physical activity. First, by holding these exercise sessions virtually, the barrier of transportation was removed. For this population, not being able to physically get to programming is a significant issue, as is the lack of appropriate health promotion programs in the community.1 By holding sessions virtually, a new option for engagement was created and was tailored to the needs of individuals with ID. The program came to them, and this eliminated the barrier of not being able to attend an exercise program.
Additionally, incorporating yoga and Bollywood dancing to upbeat music influenced the environment into one that was fun and engaging. It is important to identify the type of activity that would motivate this population to yield greater adherence and acceptance of physical activity.3 Dancing is a positive stimulus that increases physical activity in people with ID.13 This exercise/ dance program would teach foundational skills in the first week. With this foundation, each week’s activities were to incorporate familiar exercises and dance steps, and then challenged the participants by introducing new steps as the program progressed.
Therefore, varying the program diminishes boredom from doing the same repetitious routine. By monitoring the sessions and giving motivational words and phrases directed at the group and individuals, confidence levels could increase, as could their perception of self-efficacy.
Supporting a healthy lifestyle through physical activity is an important aspect of health promotion, and involving supporters is critical for the ID population.1 Further, involving caregivers, such as parents, in reminding and encouraging the individuals to join the sessions, as well as playing the role of coach is important in motivating these individuals to participate in healthpromoting behaviors.
PHYSICAL ACTIVITY
One key to improved health outcomes is to increase the amount of physical activity for this population. The U.S. Department of Health and Human Services (2018) published its guidelines for physical activities for adults.14 These guidelines include at least 150 minutes of moderate-intensity or 75 minutes of vigorousintensity aerobic physical activity or an equivalent combination of these two intensities ideally spread over a week. Further, muscle-strengthening activities of moderate or greater intensity involving all major muscle groups are also recommended on two or more days per week. Additionally, for adults with disabilities, the same guidelines are in place if the individuals are able. When they cannot meet the guidelines, they should avoid inactivity and engage in physical activity according to their abilities.
Studies support that people with ID can, and should, engage in physical activity. Those with Down syndrome were able to participate successfully in exercise programs, which included interval and aerobic training.15 Another trial compared a 12- to 16-month diet and physical activity health promotion intervention with a wait-list control group with 130 participants.16 There was a positive intervention effect on physical activity. Additionally, carers were involved, and their support likely contributed to significantly improved physical activity levels after the program. In a feasibility study, significant improvement in cardiovascular and muscle fitness, and weight loss, had been documented following participation in programs that incorporated combined training programs that included aerobic and muscle endurance training, particularly Zumba and strength training to music.3 Motivation to complete a challenging task was an important factor, with physical activities being more fun when using music and games to make the activity stimulating and enjoyable.
BARRIERS
Barriers to adequate physical activity are identified as a lack of adapted exercise courses and programs of inclusion, transportation, and independence difficulties.17 Families identified challenges in finding expert instructors and coaches for adapted physical activity, finding gyms that were available to these young people, and the quality of sports activities. Further, paid caregivers and families did not agree on who should be responsible for managing physical activity for those with ID, therefore inactive lifestyles continued.8 The paid caregivers thought the family should be responsible to manage exercise and in contrast, the families thought the paid caregiver should do it.
91
Another significant barrier during the time of this project was the COVID-19 pandemic. The pandemic impacted many populations, including those with disabilities. Once recreation and fitness facilities closed, negative side effects emerged regarding general health, physical activity, social isolation, and overall lifestyle.18 As many options for in-person physical activity were closed during this project, alternate programming needed to be considered. This led to using virtual technology to hold the exercise program sessions.
MATERIALS AND METHODS
From the challenges noted in increasing the activity levels and decreasing health risks of those with ID, the DNP Project Leader wanted to evaluate whether the implementation of an exercise program compared to no exercise program affect physical fitness of those with ID in a six-week period. This DNP project implemented a virtual six-week exercise/dance program, with music as a motivator, for adults with ID. The program consisted of two 1-hour sessions per week. These sessions included yoga for strength training and Bollywood dancing for aerobic exercise. The aim was to compare cardiovascular and muscular fitness measurements before and after the program to determine if an exercise/dance program was effective in improving fitness for adults with ID. The 6-minute Walk Test (6MWT) was used to determine cardiovascular fitness. The Standing Long Jump (SLJ) was used to measure muscular fitness.
The 6MWT is a measurement that has been used in several studies focused on physical activity and people with ID. The study by Guerra-Balic et al. (2015) evaluated the reliability and validity of using the 6MWT on adults and seniors with ID. Validity was evaluated by calculating Pearson’s r correlation between the 6-minute walk distance and the VO2 peak.19 The intraclass correlation coefficient of 0.96 between two out of three tests indicates high reliability.19 Relative VO2 peak, along with the isometric leg strength, contributed to the 6-minute walk distance. Therefore, the findings showed the 6MWT is a valid, inexpensive, and simple way to test mobility and submaximal exercise performance, as well as aerobic endurance and functional ability for many populations, including those with ID.19
The standing long jump (SLJ) is a commonly used test to measure and compare strength and conditioning to determine athletic potential.19 It is a horizontal jumping field test that is uncomplicated and does not require special equipment. Its reliability is well documented.
Participants
Participants were recruited from the clientele of a center for independent living, which serves adults with ID. Clients from two of the three buildings volunteered. Since adults were the target age group for this project, the criteria for inclusion were that clients must be 18 years of age and have an intellectual disability. They had to be ambulatory and be able to follow simple directions, have no physical limitations, health issues, or behaviors preventing them from fully participating in the hour-long exercise sessions, and were not currently enrolled in a formal exercise program. Additionally, their participation was voluntary, and the project was explained to them. Considering this vulnerable population, the DNP Project Leader also contacted the participants’ parents, guardians, and/or caregivers
of those with higher levels of parental/caregiver involvement due to lower cognitive ability. This was completed by telephone to make the parent/caregiver aware of the project in full detail. Other participants were quite independent and had higher cognitive abilities to understand the purpose and activities of the project, which allowed them to make autonomous decisions regarding participation. Finally, the participants needed to attend 80% of the exercise sessions (10 out of 12 sessions) for their participation to be included in this project.
In all, 12 participants were recruited for this project. Participants were placed in the following groups: six participants in Group A (one building at the center), four participants in Group B (a second building at the center), and three participants in Group C (an all-virtual group).
Measurements
The participants met face-to-face with the DNP Project Leader on two occasions for data collection: once before the program implementation and once after the program ended. Demographics and baseline measurements were collected at the first meeting, while post-program measurements were collected at the second meeting. COVID-19 pandemic precautions were maintained per the current recommendations during these meetings.
Baseline Demographics
The DNP project was again fully explained to the participants at the first meeting. Each participant was interviewed to collect baseline demographic data such as age, race, and sex. Their ID diagnosis was identified if it was known. Additionally, health restrictions or behavioral issues were identified, as well as having access to technology, such as a computer/tablet and the internet. Access to technology and demographic data were collected using a questionnaire. If the participants met inclusion criteria, a yoga mat and two colorful dance scarves were given to them to be used during the exercise sessions.
Pre-Program Fitness Levels
In addition to demographic data, baseline fitness data were collected. Height in feet/inches using a stadiometer, and weight in pounds using a beam scale were measured to determine BMI for the pre-exercise program measurement. Additionally, the standing long jump (SLJ) was measured in feet/inches, as well as the distance traveled in the 6 Minute Walk Test (6MWT). The corridors in each of the center for independent living buildings were measured in feet/inches. Measurements for the SLJ and the 6MWT, followed the procedure for these techniques as outlined in the Martinez-Aldao et al. (2019) study.3 For the SLJ, the participants stood behind a horizontal line and then jumped as far as possible, taking off with both feet. The participants were allowed to bend their knees and swing their arms to build momentum. If they fell backward on their hands during or after landing or did not take off and land with both feet, that jump would not count and a second jump was allowed.
For the 6MWT, the corridors in each building were measured. Each participant walked the corridor for six minutes and the distance traveled was measured in feet. For two participants, a staff member stood at one end of the hallway and the DNP Project Leader stood at the other end to cue the participants to turn and continue walking. All participants were given verbal motivation to cheer them on throughout the test. Upbeat music was also played during the 6MWT as a motivator.
92 Delaware Journal of Public Health - March 2024
Before taking the actual measurements, participants were permitted to have a practice run through of each measurement so they would be familiar with the processes. They walked one lap in the corridor and had one practice jump. The DNP Project Leader remained with the participants and gave instructions during the practice session. Participants had a rest break before the actual tests were measured. Throughout all measurements, the participants received verbal motivation to complete the measurements. For this project, the SLJ measurements determined pre-program muscle fitness, and the 6MWT distance determined pre-program cardiovascular fitness. Height and weight determined pre-program BMI.
Post-Program Measurements
During the week following the completion of the program, each participant met at the center’s location that was most convenient for them at a specified appointment time. Pandemic precautions recommended at that time were followed for these face-to-face meetings. Post-program measurements for BMI, SLJ distance, and 6MWT distance were obtained using the same process as the pre-program measurements. From these data, differences in pre-program and post-program measurements were analyzed to determine the effectiveness of this exercise program on the participants’ muscular and cardiovascular fitness, and its effect on BMI. A certificate of completion was distributed to each participant at the post-program measurement appointment. The participants who completed the program were able to keep their yoga mats and dance scarves they used throughout the program.
Since the participants were not currently enrolled in a formal exercise program, and no other lifestyle changes, such as diet, were being implemented, any positive outcomes could be attributed to increased physical activity through this exercise/ dance program. Additionally, upon post-program measurements, an increase in SLJ distance would show improved muscular fitness and an increase in the 6MWT would show improvement in cardiovascular fitness.
The Exercise/Dance Program
This program had adults with ID participate in one-hour exercise/ dance sessions virtually two times a week for six weeks. Text messages and/or Facebook Messenger messages were sent to the participants or their caregivers before the sessions as reminders to join the session. Some participants joined from home, and some participants joined from their respective center locations during their small group programming. Due to the virtual nature of this program, participants were able to join the sessions from home or a location convenient for them via a computer or tablet.
The exercise/dance videos set to Bollywood music were created by a certified yoga instructor who was also a Bollywood dance instructor. One video was shown each week, with each week building on basic moves to include various yoga poses and more complex dance choreography as the program progressed. The one-hour sessions had a warm-up period with yoga, moderatevigorous activity with dancing, and a cool-down period with more yoga. The DNP Project Leader joined in many of the sessions by role modeling the activity, as well as monitoring the participants and giving verbal cues regarding technique. Verbal motivation was given throughout the sessions toward each group as a whole and to each individual.
Group A, which met weekly at one of the center’s buildings for their peer support meeting, participated together at the center on Tuesday evenings. They wore masks and maintained social distancing. At least two supervising adults from the center were present to monitor the group as they participated in the virtual session. The DNP Project Leader attended each of their Tuesday night peer support group meetings and presented the video directly from the YouTube link accessed on her cellular phone, which was then projected onto the large screen television. These participants joined their second session of the week virtually via Zoom from their homes or a convenient location for them. Group B participated in the project together as a small group via Zoom during their regular programming times at the center’s other building, with another participant joining this group from home. The DNP Project Leader interacted with these participants virtually, while the center’s staff accessed the session to view on the large screen television and supervised and motivated the small group in person.
The all-virtual group met over Zoom from their homes or a convenient location for them. Two of the three participants met together at one of their homes as the third joined from her home. This group had either parent or caregiver support to assist them in accessing the sessions and motivating them to participate in the sessions. Two of the three participants’ mothers joined in the sessions to motivate their adult children through role modeling. Participants from each of these groups were offered make-up sessions if they could not attend with their respective groups (i.e. participants had conflicts such as inconsistent work schedules, doctor appointments, or other obligations). These makeup sessions were either individual sessions or completed by having the participant join in via Zoom during another group’s virtual session. The sessions gave each participant approximately 120 minutes, or 80%, of the Centers for Disease Control and Prevention (2020b) recommended 150 minutes of moderate- to vigorous-intensity physical activity each week.
t-Test
Once the pre-program and post-program measurements for BMI, SLJ, and 6MWT were collected, data were analyzed using the IBM SPSS Statistics software. Reports were generated to compare findings between the pre-program and post-program measurements using a two-sample t-test. The Confidence Interval for the mean was 95%. Because of the small number of participants, correlation and significance could not be computed.
RESULTS
After attrition, a total of nine participants completed the program. Of the remaining nine participants, seven completed all 12 sessions, one completed 11 sessions, and one completed 10 sessions. Therefore, all participants who completed the program attended at least 80% of the sessions, which was a requirement for the project.
Of the remaining nine participants who completed the program, three were female (33.3%), and six were male (66.7%). Two of the females were from the all-virtual group. One female was from Group B. Of the six males, one was from the all-virtual group, three from Group A, one from Group B, and one joined from home with the Group B sessions. This yielded three participants from each group. See Table 1 for participants by Group.
93
Demographics according to race revealed all three females identified as Caucasian. Four of the males identified as Caucasian; one identified as African American; and one identified as being mixed race (Hispanic and African American). Their ages ranged from 18 to 41 years old.
There was a mixture of participants’ ID diagnoses noted. Five participants (55.6%) were identified as having Autism Spectrum Disorder (ASD). All five with ASD were male. One female had Down syndrome (11.1%). One female participant’s diagnosis was in the category of “Other” (11.1%), which was identified by the parent as having a communication disability. One male and one female reported their disability was unknown (22.2%).
All Participants BMI
Table 1 indicates all participants’ BMI, SLJ, and 6MWT. A comparison was generated of all the participants’ BMI measurements. The mean pre-program BMI was 30.24, and the mean post-program BMI was 30.44. The standard deviation was 6.96 for pre-program BMI and 7.26 for post-program BMI. The change in BMI means was an increase of 0.2. The change in means showed an increase in score by 0.66%.
SLJ
The SLJ distances were compared for all participants. The mean pre-program SLJ distance was 37.78 inches with a standard deviation of 17.87. The post-program mean was 43.22 with a standard deviation of 17.35. Thus, the change in pre-program and post-program SLJ distance means for all participants increased by 5.44 inches. The change in means showed an increase of 14.40%.
6MWT
The 6MWT distances were compared for all participants. The mean pre-program 6MWT distance was 1468.72 feet with a standard deviation of 200.99. The post-program mean was 1584.61 feet with a standard deviation of 157.97. The change in pre/post SLJ distance means for all participants was an increase of 115.89 feet. The change in means was 7.89%. See Table 2 for all participants for BMI, SLJ, and 6MWT.
DISCUSSION
The adult participants with ID in this DNP project participated in the exercise/dance session without injury or adverse events. This was consistent with what was found in the literature.16,20 Improvement in cardiovascular and muscular fitness was found in most participants, also consistent with the literature.5,14,21 Weight loss was not found in most participants, which aligned with the findings of the systematic review by Bouzas et al. (2019).5 One participant from Group A had negative scores in all three areas. It was not revealed until after the completion of the post-program measurements that the participant had walked over a mile to the center for this appointment. Fatigue may have played a part in this participant’s worsening scores for SLJ and the 6MWT.
Other observations were noted during the project. The participants enjoyed both the yoga and Bollywood dance components. They expressed they had fun and found the music lively. Through the text and Facebook messenger reminders, communication from the participants was positive, and they expressed excitement for the sessions. All participants who completed the program had at least an 80% attendance rate. This is consistent with Bouzas et al. (2019) finding exercise with workout music was effective for improving adherence.5
The participants easily joined the Zoom sessions, either independently or with the assistance of staff or parents. Consistent with Ptomey et al. (2017), using a virtual platform was feasible in delivering the yoga/dance session to the participants.22 This platform eliminated the need for transportation for these participants, which was identified as a barrier.1 Involving supporters, such as parents, paid staff, and the DNP Project Leader, ensured the participants joined the sessions and received encouragement throughout the program. Roll (2018) regarded supporters as a critical role in the attribute of health promotion for people with ID.1 The supporters were effective in motivating the participants to remain focused and active during each of the sessions.
Paired Samples Test Paired Differences Mean Std. Deviation Std. Error 95% Confidence Level Lower Upper Interval of the Difference t dfSig. Pair 1 Pre-program BMIPost-Program BMI -0.20.0455520.15184-0.550140.15014-1.31780.224 Pair 2 Pre-program SLJPost-Program SLJ -5.44446.67762.22587-10.5773-0.31159-2.4468 0.04 Pair 3 Pre-program 6MWTPost-Program 6MWT -115.8987.0290129.00967-182.785-48.9925-3.9958 0.004
Table 1. BMI, SLJ, and 6MWT for All Participants
Table 2 represents the change in the mean by percentage for all participants as described above.
Variable Pre Mean SD Post Mean SD Sig. % Chg BMI 30.24 6.96 30.44 7.26 0.224 0.66% SLJ 37.78 17.87 43.22 17.35 0.040 14.40% 6MWT 1468.72200.99 1584.61 157.97 0.004 7.89% 94 Delaware Journal of Public Health - March 2024
Table 2. Change in Mean by Percentage for All Participants
Roll describes one result of health promotion for those with ID as having an improved quality of life.1 For example, one participant stated he had nothing to do during the pandemic. He was not enrolled in any program, and most activities were closed due to the pandemic restrictions. However, he consistently commented on how much he liked the program, and he did not want to see it end. Bringing a fun exercise program through Zoom allowed him to not only become physically active but allowed him to socialize with the other participants in attendance. Further, when the certificates of completion at the end of the program were distributed, the participants were extremely grateful and proud of their accomplishments, with one participant tearing up with joy. Because of the positive results and participant satisfaction of this project, the DNP Project Leader reported these findings to the center’s Executive Director and Board of Directors. The Project Leader recommended continued physical activity opportunities as a permanent offering of the center. The center’s leadership agreed.
Limitations
This project had some limitations. First, there was a small number of participants from one center for independent living. This impacts the ability to run statistics for correlation and significance. A larger group would have made data analysis more impactful. Additional participants may have been drawn if there was more widespread advertising beyond the convenience of this center’s clients. Next, only younger adults with ID participated in this project. The ages ranged from 18 to 41 years old. Findings might have been different if older adults were factored into the data. In addition, due to the imbalance of the number of females (n 3) compared to males (n 6), the data on gender may not be equitable. Further, the participants needed to be fully ambulatory and able to follow simple directions. Those with more profound cognitive and/or physical disabilities were not included in this project. Therefore, findings may not represent all people with ID. Finally, the Covid-19 pandemic may have impacted the project. Although using a virtual platform was successful for this project, not all people have access to technology or reliable internet service. Holding the sessions virtually may have limited those who were not technologically knowledgeable or had poor internet service as barriers to joining the sessions.
CONCLUSION
Physical activity is vital to the health and well-being of adults with ID. Promoting and supporting physical fitness in this population will improve modifiable risk factors that impact premature chronic illness and mortality. Legislators are recognizing this population’s challenges and are introducing bills to support health equity and transportation for people with disabilities so they can get better access to care. The National Institute on Minority Health and Health Disparities (2023) designated people with disabilities as those with health disparities and supported research for this population.23 It is crucial to promote and assist people with ID to exercise as a preventative measure for health and fitness. Pursuing legislation may be a necessary avenue for advocacy to gain the services and support adults with ID need to maintain their health. Some programs have been implemented, such as the collaboration with the CDC, the National Center on Birth Defects and Developmental Disabilities, the National Association of Chronic Disease Directors, and the National Center on Health Physical Activity and Disability. They have implemented a national pilot called Reaching People with
Disabilities through Healthy Communities.24 Using an Inclusive Healthy Communities Model, the collaborative focuses on policy, systems and environmental changes to promote healthy living for those with disabilities, including physical activity. Examples of these changes include the Inclusivity Policy by the Lerner Center in Syracuse, New York providing inclusive walking routes. In Oregon, the Bergen County Health Department, Corvallis Public Works, and civil engineering graduate students combined efforts to make the downtown area more accessible for those with disabilities using curb cuts, accessible parking spots, and improved crosswalks.25 This would allow them to more easily access the fitness centers and other downtown activities. Gaining support at the state and federal levels for improved accessibility and quality programming tailored to the needs of those with ID will give the opportunity for this population to care for their health.
With support, the participants enjoyed participating in this DNP project. In six short weeks, these participants exhibited positive change in their cardiovascular and muscular fitness with only two exercise/dance sessions per week. This supports the evidence in the literature that those with ID can participate in exercise and gain health benefits from it. Through consistent participation, weight loss could have also been a benefit for some, in addition to developing the healthy habit of incorporating exercise into daily life. This vulnerable population needs assistance and motivation from others to engage in physical activity. More awareness, training, and inclusion are needed to support those with ID and their health needs. With the clients’ interest in this project, exercise using music is being sustained as a permanent part of the center’s programming at least two to three days per week. In addition, walking and yoga programs have been implemented at the center to offer a variety of physical activities. This population needs more programs to provide enjoyable physical activity opportunities for those with ID to improve their fitness levels. Consequently, improving fitness will decrease the modifiable risk factors for chronic disease. Jacob et al. (2023) found physical activity had a moderate to strong positive impact on those with ID.26 In particular, they noted an improvement in sedentary lifestyle, weight loss, and quality of life.
As for health care providers, health care visits to primary care practices are a perfect time to discuss activity levels and interests with people with ID. This lends an opportunity to assess physical fitness needs, educate the patient and caregiver on the benefits of exercise, and recommend programs and activities the person may enjoy. Studies show that people with ID are more apt to participate and complete a task when the environment and activity are enjoyable. Healthcare professionals need to take a person-centered approach when educating and making recommendations for exercise to those with ID and their caregivers. By doing so, individuals with ID can experience improved fitness and quality of life by preventing chronic disease and early morbidity and mortality.
Dr. Ayers may be contacted at melanie.l.ayers@wilmu.edu
REFERENCES
1. Roll, A. E. (2018, March). Health promotion for people with intellectual disabilities - A concept analysis. Scandinavian Journal of Caring Sciences, 32(1), 422–429. https://doi.org/10.1111/scs.12448
95
2. Centers for Disease Control and Prevention. (2019). Addressing gaps in health care for individuals with intellectual disabilities. https://www.cdc.gov/grand-rounds/pp/2019/20191015-intellectualdisabilities.html
3. Martínez-Aldao, D., Martínez-Lemos, I., Bouzas-Rico, S., & Ayán-Pérez, C. (2019, June). Feasibility of a dance and exercise with music programme on adults with intellectual disability. J Intellect Disabil Res, 63(6), 519–527.
https://doi.org/10.1111/jir.12585
4. Melville, C. A., McGarty, A., Harris, L., Hughes-McCormack, L., Baltzer, M., McArthur, L. A., . . . Cooper, S. A. (2018, January). A population-based, cross-sectional study of the prevalence and correlates of sedentary behaviour of adults with intellectual disabilities. J Intellect Disabil Res, 62(1), 60–71.
https://doi.org/10.1111/jir.12454
5. Bouzas, S., Martínez-Lemos, R. I., & Ayán, C. (2019, December). Effects of exercise on the physical fitness level of adults with intellectual disability: A systematic review. Disability and Rehabilitation, 41(26), 3118–3140.
https://doi.org/10.1080/09638288.2018.1491646
6. Centers for Disease Control and Prevention. (2020a). Health and economic costs of chronic diseases.
https://www.cdc.gov/chronicdisease/about/costs/index.htm
7. Tyrer, F., Dunkley, A. J., Singh, J., Kristunas, C., Khunti, K., Bhaumik, S., . . . Gray, L. J. (2019, March). Multimorbidity and lifestyle factors among adults with intellectual disabilities: A cross-sectional analysis of a UK cohort. J Intellect Disabil Res, 63(3), 255–265. https://doi.org/10.1111/jir.12571
8. Cartwright, L., Reid, M., Hammersley, R., & Walley, R. M. (2017). Barriers to increasing the physical activity of people with intellectual disabilities. British Journal of Learning Disabilities, 45, 47–55. https://doi.org/10.1111/bld.12175
9. Huckstadt, A. (2019). Health promotion. In P. D. Larsen (Ed.), Lubkin’s chronic illness: Impact and intervention (10th ed., pp. 365-389). Jones & Bartlett Learning.
10. Desroches, M. (2020, April). Nurses’ attitudes, beliefs, and emotions toward caring for adults with intellectual disabilities: An integrative review. Nursing Forum, 55(2), 211–222. https://doi.org/10.1111/nuf.12418
11. Oppewal, A., & Hilgenkamp, T. I. M. (2019, July). Physical fitness is predictive for 5-year survival in older adults with intellectual disabilities. J Appl Res Intellect Disabil, 32(4), 958–966. https://doi.org/10.1111/jar.12589
12. Shih, C. H., & Chiu, Y. C. (2014, October). Assisting obese students with intellectual disabilities to actively perform the activity of walking in place using a dance pad to control their preferred environmental stimulation. Research in Developmental Disabilities, 35(10), 2394–2402. Retrieved from http://dx.doi.org.mylibrary.wilmu.edu/10.1016/j.ridd.2014.06.011 https://doi.org/10.1016/j.ridd.2014.06.011
13. U. S. Department of Health and Human Services. (2018). Physical activity guidelines for Americans (2nd ed.). https://health.gov/sites/default/files/2019-9/Physical_Activity_ Guidelines_2nd_edition.pdf
14. Boer, P. H., & Moss, S. J. (2016, April). Effect of continuous aerobic vs. interval training on selected anthropometrical, physiological and functional parameters of adults with Down syndrome. J Intellect Disabil Res, 60(4), 322–334. https://doi.org/10.1111/jir.12251
15. Hassan, N. M., Landorf, K. B., Shields, N., & Munteanu, S. E. (2019, February). Effectiveness of interventions to increase physical activity in individuals with intellectual disabilities: A systematic review of randomised controlled trials. J Intellect Disabil Res, 63(2), 168–191. https://doi.org/10.1111/jir.12562
16. Alesi, M., & Pepi, A. (2017, January). Physical activity engagement in young people with Down syndrome: Investigating parental beliefs. J Appl Res Intellect Disabil, 30(1), 71–83. https://doi.org/10.1111/jar.12220
17. Meijer, K., Hoekstra, T., & Brandenbarg, P. (2022). The impact of the COVID-19 pandemic on physical activity and social isolation among adults with physical disabilities living in Canada and The Netherlands. Disabilities, 2, 778–794.
https://doi.org/10.3390/disabilities2040054
18. Guerra-Balic, M., Oviedo, G. R., Javierre, C., Fortuño, J., Barnet-López, S., Niño, O., . . . Fernhall, B. (2015, December). Reliability and validity of the 6-min walk test in adults and seniors with intellectual disabilities. Research in Developmental Disabilities, 47, 144–153.
https://doi.org/10.1016/j.ridd.2015.09.011
19. Makaruk, H. (2021). The effects of attentional focus on testretest reliability of jumping tasks. Measurement in Physical Education and Exercise Science, 25(4), 306–313.
https://doi.org/10.1080/1091367X.2021.1878361
20. Centers for Disease Control and Prevention. (2020b). Walking: Why walk? Why not!
https://www.cdc.gov/physicalactivity/walking/index.htm
21. Shields, N., & Taylor, N. F. (2015). The feasibility of a physical activity program for young adults with Down syndrome: A phase II randomized controlled trial. Journal of Intellectual & Developmental Disability, 40(2), 115–125.
https://doi.org/10.3109/13668250.2015.1014027
22. The National Institute on Minority Health and Health Disparities. (2023). Minority health and health disparities: Definitions and parameter. National Institute of Health.
https://www.nimhd.nih.gov/about/strategic-plan/nih-strategic-plandefinitions-and-parameters.html
23. Centers for Disease Control and Prevention. (2020c). Reaching People with Disabilities through Healthy Communities.
https://www.cdc.gov/ncbddd/disabilityandhealth/reaching-people.html
24. Centers for Disease Control and Prevention. (2020d). Stories about Reaching People with Disabilities through Healthy Communities.
https://www.cdc.gov/ncbddd/disabilityandhealth/reachingpeople/ stories.html#anchor_1521552136756
25. Jacob, U. S., Pillay, J., Johnson, E., Omoya, O. T., & Adedokun, A. P. (2023, June 8). A systematic review of physical activity: Benefits and needs for maintenance of quality of life among adults with intellectual disability. Frontiers in Sports and Active Living, 5, 1184946.
https://doi.org/10.3389/fspor.2023.1184946
26. Hankle, Z. J., Bluestone, D. C., Kramer, J. K., Bassi, P., & Goreczny, A. J. (2022, February 13). What activities individuals with intellectual disabilities do for fun: Exploration into selfcare. International Journal of Developmental Disabilities, 68(5), 712–722. Retrieved from
https://doi.org/10.1080/20473869.2021.1884788
96 Delaware Journal of Public Health - March 2024
IF THIS WAS IN YOUR PAST, A COLON CANCER SCREENING SHOULD BE IN YOUR FUTURE.
If you’re 45 or older, have a family history, or are experiencing symptoms of colon cancer — including bloody stools, cramping, and weight loss— talk to your health care provider about getting screened.
Don’t have a health care provider? A screening nurse navigator can help you schedule a screening at no cost. And if you’re uninsured or underinsured, you could be eligible for a free screening through the Division of Public Health’s Screening for Life program.
To learn more, visit HealthyDelaware.org/Colon or call 2-1-1.


97
Navigating Risk: Understanding Chronic Disease Factors in Delaware’s College Population
Amy Gootee-Ash, Ph.D., M.S.W., M.S.
Director, Bachelor Public Health Program, Public & Allied Health Sciences Department, Delaware State University
Megan Rothermel, Ed.D., M.S.
Professor of Practice/Lecturer II, Public & Allied Health Sciences Department, Delaware State University
Adam Kuperavage, Ph.D.
Associate Professor, Public & Allied Health Sciences Department, Delaware State University
ABSTRACT
This study aimed to assess the prevalence of chronic disease risk factors among college students, particularly within a minority-serving institution in Delaware, to inform targeted prevention efforts. A quantitative cross-sectional research design was employed, administering surveys to 457 students at Delaware State University over a threeyear period. Surveys assessed tobacco use, physical activity, and dietary habits. Descriptive statistics were used to analyze the data. The majority of respondents were people of color (83%) and female (74%). Significant findings included 24.1% reporting trying tobacco cigarettes, 4.9% smoking in the last 30 days, and 37.2% trying e-cigarettes, with 11.8% vaping in the last month. Regarding physical activity, 65.6% reported being active for 120+ minutes per week, while only 5.7% consumed four or more servings of vegetables daily. Behavioral disparities were observed, with more males reporting tobacco use but also higher engagement in physical activity compared to females. Nutritional intake was inadequate for both genders. Convenience sampling may limit generalizability, highlighting the need for larger, randomized studies. Colleges are pivotal settings for promoting healthy behaviors and addressing chronic disease burdens. Integrated approaches involving education, policy changes, and community engagement are crucial. Investing in health promotion programs is essential for cultivating a healthier future population. This study underscores the importance of preventive measures and equitable access to resources for addressing chronic disease risk factors among college students.
INTRODUCTION
In the United States, eight out of the 10 leading causes of death are related to chronic disease.1 Americans are recording at least one chronic health condition, with one in four adults diagnosed with multiple chronic health conditions.1,2 In 2021, Delaware mirrored this United States data with the top two causes of death reported as heart disease and cancer.3 Minority populations, including racial and ethnic minorities, often face disparities in the risk of chronic diseases compared to the general population. For example, Black Delawareans have a higher prevalence of diabetes (17.5%) than white Delawareans (11.8%), with their death rate from diabetes more than twice that of their white counterparts.4 These disparities partly result from a broad range of dimensions, such as the social determinants of health and cultural and behavioral influences. Long-term health conditions that impact quality and quantity of life can be traced back to an abbreviated list of risk factors, including tobacco use, physical inactivity, and poor diet, the last two strongly associated with obesity. Risk factors developing into chronic diseases typically involve a complex interplay of various influences over time. Collegeaged students face many adverse conditions linked to chronic diseases, such as lifestyle, environment, and socioeconomic factors. Peer pressure, social norms, and cultural influences can contribute to unhealthy behaviors such as smoking, sedentary
lifestyles, and poor dietary choices. Research has shown these unhealthy behaviors typically persist into adulthood; therefore, effective programs focusing on chronic disease prevention in young adults are needed.5 Currently, one in three young adults attend college in the U.S., making the college setting an optimal location and opportunity for health promotion during a critical stage of development.6 Behaviors such as smoking provide a significant risk factor for chronic diseases among college students and can have serious long-term health consequences, such as cardiovascular disease, respiratory conditions, and cancer. Physical inactivity, often due to long hours of studying or sitting in classes, increases the risk of obesity, heart disease, and other metabolic disorders. Poor nutrition habits, such as excessive intake of fast food, sugary beverages, and processed snacks, can contribute to chronic diseases like obesity, diabetes, and cardiovascular issues.6,7 Addressing these risk factors to reduce the disease burden requires a comprehensive approach involving education, promoting healthy lifestyles, biometric screening assessments, and creating supportive environments within college communities. We must also consider racial disparities to equitably address the chronic disease burden. This study was designed to understand chronic disease risk factor prevalence within a Delaware minority-serving higher education institution to provide increased prevention focus for these young adults that will develop into the future health of our population.
Doi: 10.32481/djph.2024.03.12
98 Delaware Journal of Public Health - March 2024
METHODS
Population Description
This study was a quantitative cross-sectional research design. Surveys (n 457) were administered in classes, through social media, during campus activities, and through peer-driven campaigns over a three-year mini-grant cycle at Delaware State University (DSU), which assessed approximately 10.2% of the student population (N 4,471). DSU is one of America’s Historically Black Colleges and Universities (HBCUs) located in Dover, Delaware with a 61% African-American enrollment.8
Measures
Ethical procedures for collecting student data included approval from the Institutional Review Board - Human Subjects Protection Committee. An exemption was granted under category three, and information obtained was recorded by the investigator in such a manner that the identity of the human subjects could not readily be ascertained directly or through identifiers linked to the subjects. The survey tool was adapted from the American Lung Association Tobacco Prevention/PANO MiniGrant 2020-2022 participant survey to assess tobacco use, physical activity engagement, and dietary habits. Students in the public health program planning and evaluation course completed the peer-driven survey campaign (n 218) in hard copy, taking these surveys onto main campus for students to complete. At the same time, an online hosting platform, Anthology, was utilized to capture an additional n 239 students through on-campus events and social media campaigns.
Data Analysis
Descriptive statistics were used to provide the prevalence of three leading risk factors of chronic disease by assessing 16 self-report behavioral questions and three demographic questions delineating gender, student classification, and race/ethnic group. Four risk factors associated with chronic disease were chosen to evaluate students’ self-reported behavior regarding tobacco use, physical activity, and consumption of vegetables. The question regarding either the smoking of cigarettes or e-cigarettes (vaping) required a binary response to the questions, “Have you smoked one or more cigarettes in the past 30 days?”and/or “Have you used e-cigarettes (also known as JUULs, vapes or hookah pens) in the past 30 days?” To collect student data regarding physical activity level, students could choose from six responses to the following question, “During the past seven days, on how many days were you physically active for a total of at least 60 minutes per day? (Add up all the time you spent in any kind of physical activity that increased your heart rate and made you breathe hard some of the time).” Responses to this question were coded as binary, collapsing values with 120 minutes and more time of physical activity engagement designated as the factor for meeting physical activity guidelines. A question regarding vegetable consumption was chosen to record a nutritional risk factor, “Not including lettuce salads and potatoes, how often did you eat other vegetables? INCLUDE TOMATOES, GREEN BEANS, CARROTS, CORN, CABBAGE, BEAN SPROUTS, COLLARD GREENS, AND BROCCOLI.
INCLUDE RAW, COOKED, CANNED, OR FROZEN VEGETABLES. DO NOT INCLUDE RICE.” Multiple responses to this question were coded binary, collapsing response values with those meeting dietary guidelines of four or more vegetables consumed daily designated as the factor for meeting nutritional guidelines. The data were analyzed in the R programming language using the Tidyverse suite of packages.9 Counts and percentages by gender were made for the survey questions indicated above. In addition, counts of demographic features of the sample, including gender, race, and class, were calculated. This analysis identified patterns, trends, and relationships within the data, contributing to a comprehensive understanding of the research phenomenon under investigation. Survey sponsors were comprised of the American Lung Association and the Delaware Health and Human Services Physical Activity Nutrition Obesity Prevention Program.
RESULTS
Out of survey respondents (n 457), 83% classified themselves as a person of color (n 380), with 74% identified as female (n 340) and 26% identified as male (n 117). The majority of participants were upperclassmen, with 34% juniors (n 154) and 28% seniors (n 129), followed by 17% sophomores (n 80), 11% freshmen (n 49), and 10% graduate students (n 45). Regarding tobacco use, 24.1% of survey respondents admitted to trying tobacco cigarettes, with 4.9% smoking in the last 30 days. In addition, 37.2% reported having tried e-cigarettes, with 11.8% reporting vaping in the previous 30 days. Vaping habits were used as preliminary data to inform a campus campaign, however data regarding tobacco use was combined into a binary variable that found 4.5% of respondents reported using tobacco in any form over the last 30 days In the latest version of the survey from the academic year 2021-2022, out of 92 respondents, 62.2% of students recorded having tried hookah, with 37.8% having utilized hookah in the last 30 days. A significant number of students, 65.6% (n 300), reported being physically active for 120+ minutes per week in an activity that increased their heart rate and made breathing hard some of the time, while 20.7% (n 96) reported 0 days of physical activity. The majority of students, 54.3% (n 253), described their weight as “about the right weight,” with the second highest participant group representing their weight as “slightly underweight” at 21.9% (n 102). Screen time behaviors outside of computer use for schoolwork were recorded as time spent ‘gaming,’ texting, or on social media. 20% of students reported not using their computer systems outside of schoolwork, with 40.3% recording three hours or more of screen time spent on their computer outside of schoolwork. Vegetable consumption was minimal in the sample, with only 5.7% (n 26) of the participants consuming the recommended four or more servings per day over the last seven days. Students reported 9.2% (n 42) not having consumed vegetables at all within the previous seven days and 22.1% (n 103) only consuming vegetables 1-3 times a week. Characteristics of the sample regarding risk factors discussed in this paper, use of tobacco products, physical activity levels, and consumption of vegetables can be found in Table 1
99
DISCUSSION
Understanding the progression from risk factors to chronic diseases highlights the importance of early detection, prevention strategies, and interventions to mitigate risk factors and reduce the burden of chronic disease. Behavioral disparities were discovered between the genders. A significantly higher number of males (10.3%) reported either smoking cigarettes or vaping in the past month, as opposed to their female counterparts (2.7%). The 2022 American College Health Association - National College Health Assessment (ACHA-NCHA) reported that tobacco or nicotine delivery products (cigarettes, e-cigarettes, Juul or other vape products, water pipe or hookah, chewing tobacco, cigars, etc.) use on campuses was 33.2%, females reporting at 32.2% and males at 35.8% use.10 The ACHA-NCHA respondents averaged much higher than DSU respondents, both data sets were based on use in a 30-day period but the ACHA-NCHA compiled multiple delivery methods of tobacco products into one question, as opposed to the DSU survey which contained a question for each mode. The prevalence of current (30-day) cigarette smoking related to a 1998 study show a significant decline from 27.8% to 13% reported on the DSU campus.11 This tobacco reduction could be based on “Tobacco Free” policies within the campus community, which prohibits tobacco use on campus grounds, in campus buildings, and on any campus property. However, more current tobacco behavior regarding e-cigarettes and Hookah use needs to be collected in youth populations who have been heavily targeted in recent years with the introduction of flavors and misconceptions regarding harmful practice. Questions regarding regarding aerobic health found that more men (76.1%) reported engaging in 120+ minutes of physical activity than women (62.1%) on campus. Within the 2022 ACHA-NCHA 68.7% of students reported meeting the 150 minutes minimal requirement for physical activity, 67.2% females and 74.4% men.10 Although the number of DSU students reporting meeting the physical activity standards are higher than the national average, the DSU survey question followed the ALA/PANO suggested physical activity guidelines of 120 minutes per week. The percentages would exhibit a higher disparity if the question reflected the Department of Health and Human Services Physical Activity Guidelines for Americans 2nd Edition, which recommends 150 minutes of physical activity within a week, which is the same benchmark found within the 2022 ACHA-NCHA survey questions.12 Nutritional intake for both genders was minimal, with only 6.2% of women and 4.3% of men reporting consuming the recommended daily allowance of four or more vegetables. A higher number of college students within the 2022 ACHA-NCHA
survey reported consuming three or more servings of vegetables, averaging 18.1%; females reported at 18.1%, and males reported at 18.2%.10 Disparities may be related to a lower vegetable consumption guidelines within the 2022 ACHA-NCHA, which was three compared with the DSU respondents reporting four or more vegetables per day. Within the ACHA-NCHA questionnaire fruit and vegetable consumption are asked within the same question which may also create unrelatable data when compared to the DSU data. Regarding risk factors discussed in this paper, only 2.5% (n 11) of students sampled did not use any tobacco products and met the physical activity and nutritional guidelines, behaviors known to reduce risk of chronic disease, which creates concern to the future health of this generation.
A better appreciation of today’s students and their challenges can enable policymakers in higher education to develop effective strategies and outreach programs as stewards of our nation’s young adults. Our college student population may reflect disparities found in marginalized groups within our society. There is a concern of heightened risk to this generation of learners for decreased access to basic resources, such as living in food deserts/ swamps, not having safe places to engage in physical activity, and exposure to minority-targeted tobacco campaigns. A larger data set will allow researchers to investigate disparities by ethnicity to identify these gaps that need to be addressed.
Limitations
Data collected regarding risk factors is complex at best to get accurate measures, especially in self-report survey tools. This case was a convenience sample instead of a randomized sample of the student population, which could create results that may not accurately describe the population. Future quantitative studies need to provide a larger, randomized sample of the population, to include Hookah use, an increase in baselines metrics to 150 minutes per week for physical activity, and a broader question set for nutritional habits..
Public Health Implications
University systems are, by virtue, educational. Influential exposure to multiple value systems, including behavioral choices, can be used to introduce new concepts and choices when students are exposed to behavioral diversity. College then becomes a valuable setting that could affect a student’s level of importance assigned to healthy behaviors that can influence chronic disease development and progression. To effectively and equitably address the chronic disease burden, public health and healthcare systems need to deploy integrated approaches that bundle strategies and interventions, address many risk
Gender Did Not Use Any Tobacco Products and Met the Physical Activity and Nutritional Guidelines. Had a Cigarette and/or Vaped in Last 30 Days Engaged in 120+ Min of Physical Activity in Last 7 Days Consumed 4 Vegetables or More Daily Over the Last 7 Days Female n 9 (1.97%) n 9 (2.65%) n 211 (62.06%) n 21 (6.18%) Male n 2 (0.44%) n 12 (10.26%) n 89 (76.07%) n 5 (4.27%) Total Student Responses n 11 (2.41%) n 21 (4.59%) n 300 (65.64%) n 26 (5.68%) 100 Delaware Journal of Public Health - March 2024
Table 1. Population Characteristics of the Sample
factors and conditions simultaneously, create population-wide changes, help the population subgroups most affected, and rely on implementation by many sectors, including public-private partnerships and involvement from all stakeholders. To help meet the chronic disease burden, the US Centers for Disease Control and Prevention (CDC) uses four cross-cutting strategies that our colleges and universities can employ: (1) epidemiology and surveillance to monitor trends and inform programs; (2) environmental approaches that promote health and support healthy behaviors; (3) health system interventions to improve the effective use of clinical and other preventive services; and (4) community resources linked to clinical services that sustain improved management of chronic conditions.7 Institutions can provide significant opportunities to promote change through campus program infrastructure and policy. Investing in health promotion/prevention programming is a must to ensure we are developing an educated generation responsible for their personal health and well-being. Our responsibility in public health is to prevent, promote, and protect the populations we serve; these young adults in our care are the future health of our nation. Dr. Gootee-Ash may be contacted at aash@desu.edu
REFERENCES
1. CDC. (2022, December 21). Mortality in the United States, 2021. https://www.cdc.gov/nchs/products/databriefs/db456.htm
2. World Health Organization. (2014) Global status report on noncommunicable diseases.
http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_ eng.pdf?ua=1
3. Facts, U. S. A. (2023, Aug 7). Health in Delaware: statistics, rankings, and data trends on deaths, spending, life expectancy, and more.
https://usafacts.org/topics/health/state/delaware/#1c799f2d-84db-4e0aaf3f-b95798e68b1b
4. WHYY. (n.d.). Delaware takes aim at health disparities that show higher rates of diabetes. https://whyy.org/articles/delaware-tracking-racial-health-disparitiesonline-dashboard-research-grant-diabetes/
5. Kolodziejczyk, J. K., Norman, G. J., Rock, C. L., Arredondo, E. M., Madanat, H., Roesch, S. C., & Patrick, K. (2014, November). Strategies that predict weight loss among overweight/obese young adults. American Journal of Health Behavior, 38(6), 871–880.
https://doi.org/10.5993/AJHB.38.6.9
6. Ng, R., Sutradhar, R., Yao, Z., Wodchis, W. P., & Rosella, L. C. (2020, February 1). Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic disease. International Journal of Epidemiology, 49(1), 113–130.
https://doi.org/10.1093/ije/dyz078
7. Vainshelboim, B., Bopp, C. M., Wilson, O. W. A., Papalia, Z., & Bopp, M. (2019, August 28). Behavioral and physiological health-related risk factors in college students. American Journal of Lifestyle Medicine, 15(3), 322–329.
https://doi.org/10.1177/1559827619872436
8. Delaware State University. (2024). A proud legacy, a promising future.
https://www.desu.edu/about
9. R Core Team. (2023). R: A Language and Environment for Statistical computing. R Foundation for Statistical Computing. https://www.r-project.org/
10. American College Health Association. (2022). Spring 2022 reference group executive summary.
https://www.acha.org/documents/ncha/NCHA-III_SPRING_2022_ REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf
11. Wechsler, H., Rigotti, N. A., Gledhill-Hoyt, J., & Lee, H. (1998, November 18). Increased levels of cigarette use among college students: A cause for national concern. JAMA, 280(19), 1673–1678.
https://doi.org/10.1001/jama.280.19.1673
12. Physical Activity Guidelines for Americans. 2nd Edition. (2019).
https://health.gov/sites/default/files/2019-09/Physical_Activity_ Guidelines_2nd_edition.pdf
101
Implementing a Successful Influenza and Updated COVID-19 Vaccination Campaign Among Healthcare Workers in a Delaware Healthcare Facility
Lija Gireesh, D.N.P., M.B.A., F.N.P.-B.C., N.E.A.-B.C., C.O.H.N.-S. ChristianaCare
Tabe Mase, F.N.P.-B.C., M.J., C.H.C., C.O.H.N.-S. ChristianaCare
Marci Drees, M.D., M.S., D.T.M.H., F.A.C.P., F.I.D.S.A., F.S.H.E.A. ChristianaCare
ABSTRACT
Although influenza (flu) and COVID-19 vaccines are highly recommended for healthcare workers, it is known that vaccination rates are suboptimal in healthcare settings. There is a need to optimize vaccination rates among healthcare workers as there are direct correlations to increased patient safety and protection of staff from healthcare associated infections. Our health care organization employed some novel strategies to increase the uptake of both flu and COVID-19 vaccinations by identifying and addressing common barriers. Barriers were identified through team meetings, review of previous years’ vaccination trends, and historical information. Strategies to overcome these barriers included dissemination of information through various team meetings; identifying peer vaccination champions among specific groups that had historically low vaccination rates; creating a sense of urgency with weekly announcements regarding vaccinations; and computer screensavers with graphics promoting vaccinations. We believed education was key to success. Our focus was not only on the vaccination rates, but also on compliance which is defined as either getting the vaccine or submitting a declination after completing an education module. These efforts resulted in the organization achieving more than 95% compliance for both vaccinations. Our vaccination uptake rates for influenza were greater than 85% and updated COVID -19 vaccination rates were around 42%. We believe that the grass-root level work initiated for this year’s campaign was one of the drivers for our success and some aspects could be replicated for vaccinating the public as well.
INTRODUCTION
The Centers for Disease Control and Prevention’s (CDC) MMWR weekly report1 describes that implementing workplace strategies demonstrated increased vaccine coverage among healthcare workers for flu and COVID-19, as well as reduced morbidity and mortality among healthcare workers and their patients. Annual influenza vaccination with vaccine strains closely matching the circulating strains is widely recognized as one of the proven strategies for prevention of active cases of influenza. There is evidence supporting that influenza vaccination in healthy adults can prevent at least 64%2 of laboratory confirmed cases of flu and reduce the incidence of influenza like illness (ILI) by 42%.3 Furthermore, there are implications of reducing absenteeism for health care workers by 37% and lessening workdays lost by 0.18 days per person among vaccinated healthcare workers in contrast to a comparison group.2 Although COVID-19 vaccine mandates among hospitals were controversial, our health system adopted a COVID-19 vaccine mandate for all employees for the primary series (which was mainly the first two doses of a 2-dose series or a single dose vaccine) which was later lifted around 2022. Healthcare workers are often the target population when it comes to vaccination uptake as there is a moral obligation to avoid harm to patients
and healthcare workers are often looked upon as role models.4 Vaccinating healthcare workers with both influenza and COVID-19 vaccines can effectively reduce laboratory-confirmed cases of illness and workday absenteeism.
BACKGROUND AND LITERATURE SEARCH
A meta-analysis conducted by Fan et al from 92 studies comprised of 125 vaccination data points from 26 countries concluded that the overall influenza vaccination rates among health care workers was 41.7%.3 The study identified factors that influenced vaccine uptake as age, length of employment, education level, area of work, occupation, coexisting medical conditions, perception of being at risk of infection, participation in vaccine training, and health education and knowledge of vaccine timing.3 Although some members of the public were accepting of the new COVID-19 boosters, healthcare workers also encountered barriers similar to the public, which included mistrust in vaccines, misinformation related to vaccine safety and concerns of safe vaccine use during pregnancy.5 The CDC’s MMWR weekly report1 describes that healthcare workers whose employers’ neither required or recommended the vaccines had the lowest vaccine coverage, although the coverage with COVID-19 primary series vaccination was greater than 80% in all work settings possibly because of the prioritization of vaccination
Doi: 10.32481/djph.2024.03.13
102 Delaware Journal of Public Health - March 2024
among health care workers and the vaccine mandates that existed during the pandemic. There is a lack of high-quality studies that assessed interventions to improve seasonal vaccination rates among healthcare workers. A systematic review and meta-analysis by Gualano et al identified different interventions to increase vaccination rates among healthcare workers which included availability of free vaccines, flexible worksite vaccine delivery, education materials, education sessions, reminders, incentives, dedicated staff, vaccine mandates, and availability of signed declination statements.6 The results from a study conducted by Flanagan et al to determine the effectiveness of interventions to increase vaccine uptake among healthcare workers concluded that a program with multiple targeted interventions increased the vaccination rates.7
VACCINATION CAMPAIGN
This Delaware healthcare facility offers a fall vaccination drive to all employees during the months of October and November. This year’s campaign was conducted between October 2, 2023, and November 30, 2023, and included both influenza and updated COVID-19 vaccines. All employees were encouraged to be vaccinated or complete an education module to submit a declination or claim exemption. Neither vaccination was mandatory for the organization. The goal was for at least 90% of the employees to comply. For those employees who would be considered for a yearly bonus by the company, participation in this program was one of the criterions for eligibility to the bonus program. The campaign kicked off with a two-week mass vaccination blitz at our major locations followed by smaller clinics in the subsequent weeks based on needs.
This was a monumental undertaking, which included around 14,500 employees spread over 100 different locations in four different states. Some barriers that were identified through team meetings included vaccine hesitancy and lack of trust in vaccines. Logistical challenges in implementing two vaccination campaigns at the same timeframe as well as budgetary constraints with the cost of vaccines were also present. Approval from the Food and Drug Administration (FDA) for the updated COVID-19 vaccine was delayed longer than anticipated, which added to the logistical constraints.
We knew that we must implement novel strategies and exhaust every measure to overcome these barriers. Some strategies to enhance vaccine uptake this year included enhanced communications, identification and support from peer champions, and other grass-root level efforts.
COMMUNICATION
There was utilization of local huddles, team huddles, and system wide huddles, as well as communication in company portals and emails to employees. We capitalized on the system-wide operational huddle, which is a venue to escalate any operational concerns, to create awareness regarding the campaign. A representative from Employee Health announced the campaign weekly during our systemwide operations huddle which progressed to daily as we were nearing the campaign dates. This created increased awareness for team leaders who then disseminated the information to local teams. Additionally, all employees received an email communication from the organization’s senior leader encouraging participation in the
vaccination campaign. A new graphic was introduced which depicted two shots, while carrying the implicit message that both influenza and COVID-19 illness coexist, and employees need to adhere to safety measures to prevent the spread. To capture these messages, we created a new name for the campaign: #HitMeWithYour2Shots which was a variation of our existing and familiar influenza vaccine campaign #HitMeWithYourFluShot This tagline and graphic were introduced as a screen saver on all clinical computers at least six weeks before the campaign started. Additionally, peer champions were identified from groups with historically low vaccination rates and were educated on both vaccines to disseminate information to their peers. This education was conducted in-person to rebuild trust. This strategy proved to be the most important driving force in changing the culture and narrative around vaccine uptake in this health system, as we saw an increased vaccine uptake in departments that had a peer champion.
EDUCATION
Education modules were created to provide general information about influenza and COVID-19 vaccines as well as declination statements. Employees were required to complete the education module prior to accessing the declination module. We also utilized the organization’s SharePoint site to create a comprehensive vaccine page that included information about the vaccines, key vaccine clinic dates, etc. To simplify access for any vaccine-related questions or concerns, we created an Information Technology (IT) portal and deployed it to all employees. They were able to submit their confidential question in the IT portal which then got transferred to Employee Health clinicians to answer in real time.
CREATING A SENSE OF URGENCY
The electronic medical record was programmed to send at least eight reminders to employees and their direct leaders reminding them to get the vaccine or complete the education module to access the declination. Reminder communications were sent weekly, which progressed to daily for the last week of the campaign. Additionally, each leader had access to an electronic dashboard displaying compliance status of their employees.
DECENTRALIZED VACCINE ADMINISTRATION WITH CENTRALIZED OPERATIONS
We implemented unit-based vaccination efforts to capture healthcare workers working all shifts. Vaccines were also delivered to all our ambulatory sites which decentralized vaccine administration, but we kept the operations centralized. Vaccinators positioned to vaccinate peers and administrative volunteers who facilitated the events ensured that lines moved quickly and were not a disincentive to get vaccinated. These volunteers also represented the diversity of our employee population at all levels and varied job roles. Candid photos were published daily on the employee portal of those in line getting vaccinated or volunteering for the campaign, providing visibility of how well the campaign was going as well as giving “bragging rights” to many. Additionally, employees were encouraged to get vaccinated at local pharmacies or their doctor’s office and provide us with a proof of vaccination if they were unable to come to any of the vaccination events hosted.
103
Previously compliance rates for flu vaccination hovered close to 90% and data from COVID -19 bivalent booster vaccine administration was not captured as it was administered separate from the fall vaccination project. The goal for this year’s vaccination drive was 90% employee compliance. A combination of the strategies described resulted in more than 95% compliance for both vaccinations. Our vaccination rates for influenza were greater than 85% (global average approximately 40%) and updated COVID-19 vaccination rates were around 42% (global average for those who received at least one dose of booster dose is approximately 32%)
DISCUSSION
In the wake of the COVID-19 pandemic and conspiracies surrounding COVID-19 vaccines, vaccination rates for all vaccines suffered. Similar to the general population, healthcare workers were also affected by all the information and misinformation about the COVID vaccines that has eroded trust for all vaccines.
To improve influenza and COVID-19 vaccine uptake for the 2023/24 season, we tried some novel strategies. The first strategy was to re-build trust. For this we utilized a grass-root level work starting with peer champions. Vaccine education was created in simple language and there was direct access to Employee Health to answer questions. The second strategy was to simplify education and make it accessible. We utilized the organizations’ SharePoint site to create a very comprehensive vaccination page and utilized our learning management system to deploy education and declination statements if needed. Another strategy was to incentivize engagement by tying the program as one of the elements for eligibility for the incentive bonus. We kept the communication simple, fun, and accessible. The lessons learned from this vaccine campaign included that vaccine acceptance behavior is complex and difficult to understand, and a multipronged approach might be more beneficial than a single prong approach to enhance vaccination rates.
CONCLUSION
Vaccine hesitancy is a complex behavior and multifactorial. Considering the influenza and COVID-19 illnesses peaking in the fall, we must resort to novel strategies to improve vaccination rates. There is a gap in evidence of the most appropriate strategy supporting vaccination rates among healthcare workers and most studies indicate the use of a multipronged approach. The strategies used for the fall vaccination campaign at a major healthcare facility in Delaware might include tactics that could help the success of a mass vaccination program that could be replicated at other facilities.
Dr. Gireesh may be contacted at lgireesh@christianacare.org
REFERENCES
1. Razzaghi, H., Srivastav, A., de Perio, M. A., Laney, A. S., & Black, C. L. (2022, October 21). Influenza and COVID-19 vaccination coverage among health care personnel — United States, 2021–22. MMWR. Morbidity and Mortality Weekly Report, 71(42), 1319–1326.
https://doi.org/10.15585/mmwr.mm7142a2
2. Li, T., Qi, X., Li, Q., Tang, W., Su, K., Jia, M., . . . Feng, L. (2021, September 29). A systematic review and meta-analysis of seasonal influenza vaccination of health workers. Vaccines, 9(10), 1104.
https://doi.org/10.3390/vaccines9101104
3. Fan, J., Xu, S., Liu, Y., Ma, X., Cao, J., Fan, C., & Bao, S. (2023, November 6). Influenza vaccination rates among healthcare workers: A systematic review and meta-analysis investigating influencing factors. Frontiers in Public Health, 11, 1295464.
https://doi.org/10.3389/fpubh.2023.1295464
4. Politis, M., Sotiriou, S., Doxani, C., Stefanidis, I., Zintzaras, E., & Rachiotis, G. (2023, April 21). Healthcare workers’ attitudes towards mandatory COVID-19 vaccination: A systematic review and meta-analysis. Vaccines, 11(4), 880.
https://doi.org/10.3390/vaccines11040880
5. Burrowes, S. A. B., Casey, S. M., Dobbins, S., Hall, T., Ma, M., Bano, R., . . . Pierre-Joseph, N. (2022, December 25). Healthcare workers’ perspectives on the COVID-19 vaccine and boosters for themselves, their patients, and their communities: A mixed methods study. Z Gesundh Wiss, 1–14; Advance online publication.
https://doi.org/10.1007/s10389-022-01793-1
6. Gualano, M. R., Corradi, A., Voglino, G., Catozzi, D., Olivero, E., Corezzi, M., . . . Siliquini, R. (2021, February 5). Healthcare Workers’ (HCWs) attitudes towards mandatory influenza vaccination: A systematic review and meta-analysis. Vaccine, 39(6), 901–914.
https://doi.org/10.1016/j.vaccine.2020.12.061
7. Flanagan, P., Dowling, M., Sezgin, D., Mereckiene, J., Murphy, L., Giltenane, M., . . . Gethin, G. (2023, November). The effectiveness of interventions to improve the seasonal influenza vaccination uptake among nurses: A systematic review. Journal of Infection Prevention, 24(6), 268–277.
https://doi.org/10.1177/17571774231208115
104 Delaware Journal of Public Health - March 2024


Fentanyl
is
it’s
Visit FightFentanylDE.com to order them for free. GET NARCAN® AND FENTANYL TEST STRIPS DELIVERED TO YOUR DOOR Free. Anonymous. Lifesaving. FYL FYL FYL FYL FYL FYL 105
a silent killer that’s being mixed into other drugs — and
now the leading cause of overdose deaths in Delaware. Know what you’re taking. Get fentanyl test strips to detect it, and Narcan to reverse an overdose.
Mapping Health Disparities: Leveraging Area-Based Deprivation Indices for Targeted Chronic Disease Intervention
Darrell Dow, M.S.
Corporate Director of Analytics and Digital Solutions, ChristianaCare Health System, Adjunct Instructor, Wilmington University
ABSTRACT
This article addresses the critical link between socioeconomic status and health outcomes in chronic disease patients, emphasizing the need for system-level outcome measurement stratified by socioeconomic status. Despite the acknowledged influence of social determinants, there is a lack of published studies analyzing chronic disease outcomes neighborhood by neighborhood. The importance of mapping as a public health tool, and the significance of analyzing outcomes at the neighborhood level is emphasized. The U.S. Census Bureau’s hierarchy of space definitions Is presented, particularly focusing on census tracts as a unique opportunity for analyzing chronic disease outcomes. Two Area-Based Deprivation Indices (ABDIs) - the Area Deprivation Index (ADI) and the Social Vulnerability Index (SVI) - as tools to measure socioeconomic disadvantage and vulnerability to environmental stressors, respectively are described. A brief survey of the weaknesses of ABDIs and limitations in addressing individual-level factors is addressed followed by a discussion of the challenges in translating patient address data into census block data. The evolving conversation around equity analysis and its impact on chronic disease management is presented. It highlights the willingness of public payers to tie payments to ABDIs, signaling a shift towards a more equitable healthcare system. Private insurers and health systems are urged to invest in geocoding strategies to understand and improve outcomes for the diverse neighborhoods they serve, acknowledging that the path forward involves addressing health disparities at the population level.
BACKGROUND
It is widely recognized that socioeconomic status is a determining factor in health outcomes for patients with chronic diseases. Going back as far as 1987, the Alameda County Study in California found evidence that education and economic disparities directly contribute to poor health-related behaviors and the prevalence of chronic disease.1 More recently, a 2021 Australian study found that the increase in cost and utilization for disadvantaged chronic disease patients was 20% higher than their more privileged counterparts while in-hospital poor outcomes increased by 80% in the disadvantaged population.2 Multiple subsequent studies have confirmed this finding including a survey of populations in the American MidSouth which adds that “education-level disparities were more pronounced in health-related behaviors, whereas incomelevel disparities were more pronounced in [chronic health conditions].”3
Although we can readily acknowledge the influence of social determinates of health on chronic disease outcomes, there remains an alarming lack of system-level outcome measurement stratified by socioeconomic status. In short, published studies from either healthcare payors or providers that speak to the health outcomes of their chronic disease patients by analyzing socioeconomic status at a neighborhood-by-neighborhood level are scarce. This kind of analysis is not easy work, but it is vital to measure whether the care given produces desired results across the socioeconomic spectrum.
DEFINING A NEIGHBORHOOD
The idea of mapping as a public health tool is hardly novel and maps have been used in the fight against disease as early as John Snow’s famous 1856 cholera map.4 A robust background on the topic of general mapping and Geographic Information System (GIS) tools has previously been covered in Highberger and Merriman-Nai’s “The Value (and Nuances) of Mapping as a Public Health Tool” (DOI: 10.32481/djph.2021.07.003)5 and does not need to be reiterated here.
When considering analysis of the effectiveness of social determinates of health on chronic disease outcomes specifically, however, it is critical to choose an appropriate way to segment populations into groups that have common characteristics. In other words, equitable analysis must be done at the neighborhood level. To that end, in the United States, the US Census Bureau (UCB) has created a hierarchy of space definitions from County to Census Tract (see Figure 1) that allow for finer grains of data to be analyzed.
According to the UCB, census tracts have three defining characteristics:
• They have a target size of 4,000 people (although can vary from 1,200 to 8,000);
• They are created with the intention of being maintained over a long period of time for historical comparison;
• They follow “visible and identifiable features” or legal boundaries.6
Doi: 10.32481/djph.2024.03.14
106 Delaware Journal of Public Health - March 2024
Understanding the Relationships Among U.S. Census Bureau Geographic Entities

Although variation can exist within even a small group of people, designating consistently held spaces allows for the tracking of neighborhoods both in comparison to other neighborhoods and to themselves over time. As a result, census tracts provide a unique opportunity to analyze outcomes for patients with chronic conditions.
A TALE OF TWO INDEXES
Once a neighborhood has been defined, the next step in population health analysis is for researchers to systemically define those spaces in terms of socioeconomic factors. To this end, there are two Area-Based Deprivation Indices (ABDIs) that are commonly referenced when attempting to measure social determinates of health in each neighborhood area: the Area Deprivation Index (ADI) and Social Vulnerability Index (SVI).
Area Deprivation Index
The Area Deprivation Index is a statistical tool designed to assess the level of socioeconomic disadvantage within a specific geographic area. Developed by the University of Wisconsin School of Medicine and Public Health, the ADI considers multiple factors such as income, education, employment, and housing conditions to create a composite measure of deprivation. The index utilizes census tract data, allowing for a granular analysis of neighborhoods or communities.
Census tract scores are created on a 1-10 scale at the state level (See Delaware in Figure 2) and 1-100 scale nationally, with higher ADI scores indicate greater levels of deprivation, signaling areas with reduced access to resources, economic opportunities, and social services.8,9 The inherent value of this index has earned it the title of “The Most Scientifically Validated Social Exposome Tool Available For Policies Advancing Health Equity” in recent publication by its proponents.10
Social Vulnerability Index
The Social Vulnerability Index is a measure that evaluates a community’s susceptibility to the impact of environmental and social stressors (Figure 3). Developed by the Agency for Toxic Substances and Disease Registry (ATSDR), the SVI incorporates factors such as socioeconomic status, household composition, and minority status. Census tracts are then ranked on a scale from 0 (Least Vulnerable) to 1 (Most Vulnerable). By considering these variables, the SVI identifies communities that may face challenges in responding to and recovering from disasters, public health emergencies, or other adverse events. Higher SVI scores indicate increased vulnerability and a need for targeted interventions to enhance resilience.
Figure 1. ‘Census Small-Area Geography’ Graphic from the U.S. Census Bureau6
107
Census Small-Area Geography
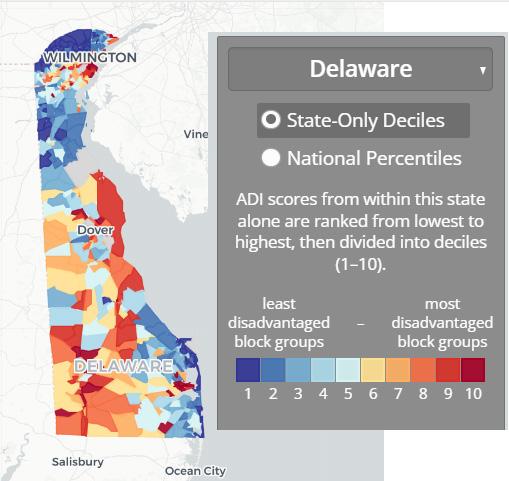
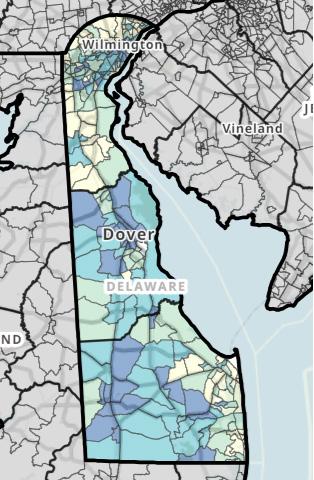
Comparison
Researchers at the University of Michigan who recently performed statistical comparisons of the two indices were very clear in their finding that the “ADI and SVI are not interchangeable measures of socioeconomic deprivation at the tract level.”12 While both the ADI and SVI aim to capture aspects of social and economic disadvantage, they differ in their focus and application. The ADI primarily concentrates on measuring general socioeconomic deprivation within a geographic area, emphasizing factors like income and education. In contrast, the SVI places a specific emphasis on vulnerability to external stressors, including environmental hazards and public health emergencies with indicators related to social vulnerability, including minority status and housing composition.
In summary, the ADI is geared towards assessing overall deprivation, whereas the SVI is tailored to identify communities at higher risk during crises. Depending on the research or policy goals, one or both indices may be employed to gain a comprehensive understanding of the challenges faced by different communities and to target interventions effectively.
Limitations
One notable constraint on the use of both ABDIs is the potential for oversimplification which masks internal variations and nuances. This may obscure the true extent of deprivation experienced by specific populations within a given area. Moreover, ABDIs may not fully consider individual-level factors. No single score can sum up the entire social history or individual needs of a given patient.
The Advisory Board publication recently reported that when the Centers for Medicare & Medicaid Services (CMS) introduced the ADI in 2022 to adjust payment rates and quality incentives in certain healthcare payment models the reception was mixed.13 Some continue to raise concerns that the ADI’s methodology may not accurately represent health disparities, particularly in densely populated urban areas due to factors like average home prices. Stakeholders, including provider organizations, are calling for improvements to the ADI’s methodology, suggesting considerations for community-level barriers, regional adjustments, and incorporation of additional metrics like life expectancy.
THE INSUFFICIENCY OF 5-DIGIT ZIP CODE IN SOCIOECONOMIC ANALYSIS
To understand the variation in neighborhoods that can exist within a single zip code one only needs to look at the most populated ZIP code in Delaware, 19720. According to American Community Survey 2022 5-Year Data this zip code covers a geographic area of about 38.3 square miles in the northwest of the state and contains approximately 60,514 residents.14
If only looking at the ADI ranking for this zip code in aggregate, one can observe that the mean ADI for this zip code is 6.6, the median ADI IS 7, and the mode ADI is 5. However, when a distribution is created (Figure 4) it becomes obvious that aggregating these neighborhoods into a single value would be useless for equity analysis when looking at chronic disease patients.
Figure 2. Area Deprivation Map from the Neighborhood Atlas®7
108 Delaware Journal of Public Health - March 2024
Figure 3. Social Vulnerability Map of Delaware11

Distribution of census blocks within zip code 19720 is based on 2022 Area Deprivation Index data.9 Census blocks marked GQ are suppressed from ranking due to a high group quarters population. Bearing in mind that the higher the ADI ranking the more vulnerable the population, one can note that 2,079 census block groups received a rank between a more privileged 2 to 5 while 3,035 were ranked between a more vulnerable 6 and 10. It becomes clear at this grain of data that there are highly vulnerable neighborhoods (ranks 8 to 10) within this zip code that effectively disappear if analysis is aggregated above the census block level.
MOVING MEDICAL DATA FROM SIMPLE DEMOGRAPHICS TO POPULATION DESCRIPTION
The typical demographic data capture into an electronic medical record includes elements such as age, sex, race, and home address. However, this captured patient address data is often difficult to translate into an Area-Based Deprivation Index for the simple reason that, typically, only five-digit zip codes are captured. By the same token, medical claims files provided by private insurance payers also will only include 5 digits. However, determining a patient’s neighborhood status with either the ADI or SVI requires a 9-digit ZIP code (ZIP+4) to determine the patient’s census block group. One notable exception: CMS does provide 9-digit zip codes as part of its beneficiary information.
This deficit of four digits may not seem on its face to be a great barrier but the process of geocoding every patient’s address into a neighborhood often requires investment in the time of trained staff and expensive software. It is an overhead cost that may have obvious benefits to population health but is often not directly tied to reimbursement.
Individual research and publications use the ADI in studies on chronic conditions to great effect, such as the study which recently found that in Delaware Medicaid recipients between the ages of 8 and 18 “communities with ADI greater than or equal to 50 was associated with 60% greater odds of a hypertension diagnosis.”15 However, at the enterprise level, health systems and insurers alike are slow to take on the cost and effort associated with a comprehensive geocoding strategy that would allow rapid iterations of these kinds of analysis within chronic disease management programs.
THE PATH FORWARD
The conversation around the use of ABDIs in population health and their impact on chronic disease management is only in its nascent stages. Public payers have already shown their willingness to tie payments to the ADI and where CMS leads others in time will inevitably follow. Public policy will ultimately shape the future of ABDIs but in the meantime private insurers and health systems who embrace creating equitable systems of care as one of their core values are faced with a difficult truth: without an investment in geocoding strategies, it is impossible to know if they are truly changing outcomes for the neighborhoods that they serve. Mr. Dow may be contacted at Darrell.c.dow@wilmu.edu
REFERENCES
1.Haan, M., Kaplan, G. A., & Camacho, T. (1987, June). Poverty and health. Prospective evidence from the Alameda County Study. American Journal of Epidemiology, 125(6), 989–998.
https://doi.org/10.1093/oxfordjournals.aje.a114637
2. Yong, J., & Yang, O. (2021, March). Does socioeconomic status affect hospital utilization and health outcomes of chronic disease patients? Eur J Health Econ, 22(2), 329–339.
https://doi.org/10.1007/s10198-020-01255-z
109
Figure 4. 2021 ADI Census Block Group Distribution Within 19720
3. Oates, G. R., Jackson, B. E., Partridge, E. E., Singh, K. P., Fouad, M. N., & Bae, S. (2017). Sociodemographic Patterns of Chronic Disease: How the Mid-South Region Compares to the Rest of the Country. American journal of preventive medicine, 52(1S1), S31–S39.
https://doi.org/10.1016/j.amepre.2016.09.004
4. Snow, J. (1856, January). On the mode of communication of cholera. Edinburgh Medical Journal, 1(7), 668–670. https://pubmed.ncbi.nlm.nih.gov/29647347
5. Highberger, J. P., & Merriman-Nai, S. (2021, July 15). the value (and nuances) of mapping as a public health tool. Delaware Journal of Public Health, 7(3), 6–9. https://doi.org/10.32481/djph.2021.07.003
6. US Census Bureau Staff. (2022, April 11). United States Census Bureau Glossary. Accessed Feb 21, 2024. Census.gov. https://www.census.gov/programs-surveys/geography/about/glossary.html Accessed Feb 21, 2024
7. Neighborhood Atlas. (n.d.). Delaware. Retrieved from https://www.neighborhoodatlas.medicine.wisc.edu/mapping
8. Kind, A. J. H., & Buckingham, W. R. (2018, June 28). Making neighborhood-disadvantage metrics accessible - The Neighborhood Atlas. The New England Journal of Medicine, 378(26), 2456–2458. https://doi.org/10.1056/NEJMp1802313
9. University of Wisconsin School of Medicine and Public Health. (2021). Area Deprivation Index Downloaded from https://www.neighborhoodatlas.medicine.wisc.edu/ Accessed Feb 21,2024
10. Powell, W.R., Sheehy A.M., Kind, Kind J.H. (2023) “The Area Deprivation Index Is The Most Scientifically Validated Social Exposome Tool Available For Policies Advancing Health Equity”, Health Affairs Forefront. DOI:
https://doi.org/10.1377/forefront.20230714.676093
11. Agency for Toxic Substances and Disease Registry. (2020). CDC/ATSDR Social vulnerability index (SVI). Retrieved from https://www.atsdr.cdc.gov/placeandhealth/svi/interactive_map.html
12. Rollings, K. A., Noppert, G. A., Griggs, J. J., Melendez, R. A., & Clarke, P. J. (2023, October 5). Comparison of two area-level socioeconomic deprivation indices: Implications for public health research, practice, and policy. PLoS One, 18(10), e0292281.
https://doi.org/10.1371/journal.pone.0292281
13. Advisory Board Staff. (2023). Exploring the impact of CMS’ ADI tool on underserved communities.
http://www.advisory.com/daily-briefing/2023/06/29/adi-payment-models Accessed Feb, 22, 2024.
14. U.S. Census Bureau. (2022). American Community Survey 5-year estimates. Retrieved from Census Reporter Profile page for 19720
http://censusreporter.org/profiles/86000US19720-19720/
15. Baker-Smith, C. M., Yang, W., McDuffie, M. J., Nescott, E. P., Wolf, B. J., Wu, C. H., . . . Akins, R. E. (2023, March 1). Association of area deprivation with primary hypertension diagnosis among youth Medicaid recipients in Delaware. JAMA Network Open, 6(3), e233012.
https://doi.org/10.1001/jamanetworkopen.2023.3012
110 Delaware Journal of Public Health - March 2024



of 94TH ANNUAL MEETING MAY 1, 2024 | 6 PM- 9 PM HYATT PLACE WILMINGTON RIVERFRONT 760 S. Justison St, Wilmington, DE 19801 111
Review of Pediatric Tracheostomy Training Program for Home Discharge Patients
Katlyn L. Burr, M.S.M., R.R.T.-N.P.S., A.E.-C.
Department of Respiratory Care, Nemours Children’s Hospital
Erin Nilson-Italia, R.R.T.-N.P.S.
Department of Respiratory Care, Nemours Children’s Hospital
Michael Treut, R.R.T.-N.P.S., A.E.-C.
Department of Respiratory Care, Nemours Children’s Hospital
Kimberly McMahon, M.D.
Department of Respiratory Care, Nemours Children’s Hospital
Kelly Massa, B.H.S., R.R.T.-N.P.S.
Department of Respiratory Care, Nemours Children’s Hospital
ABSTRACT
Background. Transitioning long term care of pediatric patients with tracheostomy tubes and ventilator dependence from hospital to home is a comprehensive process that requires intense oversight and management to ensure patient safety. Our pediatric hospital has seen an increase in length of stay post tracheostomy tube placement with and without ventilatory dependency since the COVID-19 pandemic. This change is presumed to be associated with an increase of 22-26 week gestational age premature infants surviving beyond birth. Moreover, within the community, there is a shortage of private duty nursing to care for patients with tracheostomy tube needs which has delayed discharge to home for otherwise medically stable patients. Caregivers were reluctant to accept training if there were limited resources available to them upon discharge. We aimed to evaluate the impact of the pandemic on the inpatient education program to support patients’ transition to home with trained caregivers. Methods. An- IRB approved retrospective review of pediatric patients with tracheostomy placement who elected a path of discharge to home were evaluated from 2010-2022. The home education plan for patients with tracheostomy and ventilator dependence includes 8-13 weeks of intensive inpatient education (Table 1). Our tracheostomy and ventilator training program encompass a multidisciplinary approach including a Respiratory Family Educator, Nursing, Social Work, Case Management, and a Pulmonary APN. Our program occurs over an 8 to 13-week period which is largely dependent on the availability of two caregivers. All caregivers must show competency in tracheostomy changes, managing the artificial airway, CPR, tracheostomy emergency scenarios, as well as all other routine care for a medical complex child. Upon completion of the program, caregivers are required to complete a 24-hour stay within the hospital where they are responsible to perform all aspects of care for their child. Caregivers also are required to participate in a simulation to review tracheostomy emergency using a simulation mannequin. atient timelines were reviewed and evaluated to assess program efficiency and impact of discharge delays on length of stay and education time. Pre-COVID was defined as 2010-2019 and COVID/Post COVID was defined as 2020-2022. Results. During the study period our pediatric hospital provided care, training, and education for 359 patients who required tracheostomy, ventilator support, and training to facilitate home discharge (Figure 1, Table 2). When compared to the pre-COVID period, COVID/post-COVID tracheostomy tube placement increased 13%, time from tracheostomy tube placement to education program start increased by 26%, and time from tracheostomy tube placement to completed education decreased 3.7%, home RN availability related delays increased 442%, and average length of stay increased 2.7%. Conclusion. While both the discharge delay time and length of stay increased in the post COVID period they did not increase at the same rate. There was also an increase in time from tracheostomy tube placement to initial education but a decrease in total time to complete the education program. A collaborative team management approach to tracheostomy tube placement, training track, education and discharge planning was able to overcome delays in discharge related to home nursing availability. Further studies must be done to evaluate the impact of COVID and discharge delays in other populations of technology dependent patients.
Doi: 10.32481/djph.2024.03.15
112 Delaware Journal of Public Health - March 2024
1.
TASK (2 Caregivers required to complete all components) Recommended Timeline View tracheostomy videos Week 1-2 Respiratory anatomy Week 1-2 Assessment of respiratory status Week 1-2 Suctioning the child with a tracheostomy tube Week 2 Manual ventilation (self-inflating bag) Week 2 Care of a tracheostomy site and stoma Week 2 Changing the tracheostomy tube (each caregiver must insert 3) Week 1-6 3 sessions of CPR and trach emergency scenarios Week 3-6 Emergency portability bag Week 3 Nebulizer Week 4 Pulse oximetry Week 4 Nebulizer Week 4 Trach collar/HME/PMV (if applicable) Week 4 Ventilator Week 5 Portability Week 5 Simulation lab scenarios Week 6 Supervised family care (24-hours) Week 6 113
Table
Tasks and Timelines
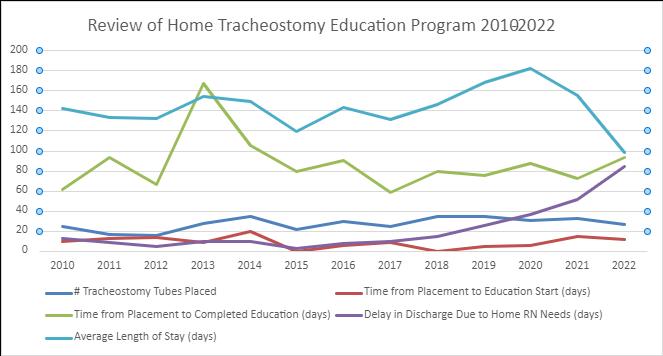
# Tracheostomy Tubes Placed Time from Placement to Education Start (days) Time from Placement to Completed Education (days) Delay in Discharge Due to Home RN Needs (days) Average Length of Stay (days) 2010 25 10 62 13 142 2011 17 13 94 8.5 133 2012 16 14 67 4.8 132 2013 28 9 167 9.9 154 2014 35 20 106 10 149 2015 22 0 80 2.1 119 2016 30 6 91 8 143 2017 25 9 59 9.3 131 2018 35 0 80 14.3 146 2019 35 5 76 25.8 168 2020 31 6 88 36.3 182 2021 33 14.5 73 51.7 155 2022 27 12 94 84.5 99 Average # Tracheostomy Tubes Placed Average Time from Placement to Education Start (days) Average Time from Placement to Completed Education (days) Average Delay in Discharge Due to Home RN Needs (days) Average Length of Stay (days) Pre COVID 26.8 8.6 88.2 10.6 141.7 Post COVID 30.3 10.8 85 57.5 145.3
Table 2. Review of Home Tracheostomy Education Program 2010-2022
114 Delaware Journal of Public Health - March 2024
Figure 1. Review of Home Tracheostomy Education Program 2010-2022
Delaware Mini Medical School Spring 2024 - NORTH
10
24 APR
APR

Rheumatology- Joint Inflammation: Do I have an autoimmune disease?
08
MAY


Thoracic Surgery and Robotic Surgery
Devanshu Verma, MD, MBA Brian Nam, MD
Behavioral Health - Understanding Addiction & Anxiety/Depression
Vishesh Agarwal, MBBS & Matthew Lind, PA-C
Endocrine Disorders (Non-Diabetic Related)
John Donnelly, MD & Resident Elizabeth Klingensmith
Sports Medicine (Dance, Fitness, & Sports Medicine)
Elizabeth Barchi, MD
Skin Cancer
Arvind Sabesan, MD

17
APR
01
MAY

15 MAY
delawareminimed.org
115
Lieutenant Governor’s Challenge: Motivating and Honoring Delawareans to Improve Their Health and Well-Being
Helen Arthur, M.H.A.
Chief, Health Promotion and Disease Prevention Section, Division of Public Health, Delaware Department of Health and Social Services
Lauren Butscher, C.H.E.S.
Program Administrator, Physical Activity, Nutrition and Obesity Prevention Program, Division of Public Health, Delaware Department of Health and Social Services
Lisa Moore, M.P.A.
Chief, Health Promotion Bureau, Division of Public Health, Delaware Department of Health and Social Services
Keith Warren
Chief of Staff, Office of Lieutenant Governor Bethany Hall-Long, State of Delaware
ABSTRACT
The Lieutenant Governor’s Challenge 2.0, Wellness Award Initiative, is an opportunity for everyone to drive change and to elevate the well-being, productivity, and prosperity among communities in Delaware. The 2.0 reference is rooted in the mission of former Lieutenant Governor, and now Governor, John Carney to address physical activity and fitness levels of youth and adults. The Lieutenant Governor’s Challenge 2.0 presents the opportunity to unite the entire state in an ongoing effort to create an overall healthier population. Mobilizing communities to get healthier, promote better health outcomes, and lower health care costs are the goals of this statewide initiative. Community recognition is a powerful tool to applaud and inspire individuals and organizations that implement health promotion and disease prevention programs. To reduce the burden of chronic disease in Delaware, the Lieutenant Governor’s Challenge 2.0 honors individuals, programs, organizations, and institutions who are implementing policy, systems, and environmental change initiatives to improve the health and well-being of their respective communities. This article highlights the Lieutenant Governor’s Challenge Wellness Award Initiative and discusses the importance of policy, systems, and environmental change strategies in chronic disease prevention. This is more than a recognition program for health and wellness. It is a statewide effort to influence, advance, and sustain systemic change in emotional well-being, healthy living, chronic disease management and prevention, and mother and child health. This effort achieves health equity through approaches that center community voice.
BACKGROUND
According to the Centers for Disease Control and Prevention (CDC), chronic and mental health diseases contribute to the leading causes of death and disability in the United States, and to the country’s $4.1 trillion in annual health care spending.1 Common chronic diseases include heart disease and stroke, cancer, diabetes, and obesity.1 Chronic disease can lead to a decreased quality of life and a shortened life expectancy.
Within the Delaware Department of Health and Social Services, Division of Public Health (DPH), Delaware Health Statistics Center indicates that chronic diseases account for three of the top five leading causes of death among Delawareans.2 In 2021, cardiovascular diseases and cancers accounted for 39% of all deaths in Delaware.2 High blood pressure and high cholesterol are major risk factors for cardiovascular diseases.3 In 2021, 36% of Delaware adults reported having high blood pressure and 38% reported having high cholesterol.4
Diabetes is associated with higher risk of heart disease, stroke, and other serious health conditions.5 In 2022, 14% of adults in Delaware reported having been diagnosed with diabetes, and 14% reported having been diagnosed with pre-diabetes.6 As diabetes becomes more prevalent with age, 19% of adults ages 55 to 64 had diabetes, and 24% of adults ages 65 and older had diabetes.6
Obesity and excess weight are associated with an increased risk of developing other chronic diseases and premature death compared to those of normal weight. In 2022, 37.9% of Delaware adults were obese and another 33.9% were overweight.6 In 2021, 18.7% of Delaware adults with obesity and 12.6% of Delaware adults who are overweight had diabetes, compared to 3.5% of Delaware adults of normal weight.4
From 2017-2021, the Black infant mortality rate in Delaware was still more than three times the White infant mortality rate. Delaware’s White infant mortality rate was 3.4 deaths per 1,000 live births, which was lower than the national White infant mortality rate.7 From 2017-2021, the Delaware Black infant mortality rate was 11.0 deaths per 1,000 live births, which was higher than the national Black infant mortality rate of 10.3 deaths per 1,000 live births.7,8 Risk factors such as obesity, preeclampsia, and high blood pressure are on the rise in women of reproductive age.9
Chronic disease can be prevented, delayed, and managed through simple lifestyle changes. Many chronic diseases are caused by common risk behaviors such as tobacco use, unhealthy diet, physical inactivity, and excessive alcohol use.10 Remaining tobacco-free, meeting the recommended levels of physical activity, and maintaining a healthy diet play a large role in preventing obesity and other chronic diseases.
Doi: 10.32481/djph.2024.03.16
116 Delaware Journal of Public Health - March 2024
The factors contributing to chronic disease are complex. Chronic disease and an individual’s ability to make healthy decisions are influenced by distinct factors such as genetics and lifestyles choices, and the social and economic context in which one lives, works, and plays. Differences in social determinants of health can limit a community’s availability and accessibility of opportunities to engage in a healthy lifestyle and contribute to disparities in chronic disease prevalence among racial, ethnic, and socioeconomic groups.11 Policy, systems, and environmental change approaches are used to address health disparities and achieve equitable health outcomes by making healthy choices available and accessible to all.12
Community recognition is a powerful tool to applaud and inspire individuals and organizations implementing health promotion and disease prevention programs.13 Recognizing community champions not only honors and shows appreciation for those doing important work, but also creates an example for other partners to follow. Honoring community partners and programming also provides opportunity to highlight and explain community issues and needs.13
To reduce the burden of chronic disease in Delaware, during his tenure as Lt. Governor (2001-2009), Governor John Carney established The Lieutenant Governor’s Challenge, a wellness award program aimed at inspiring individuals to take the first steps toward leading healthier lifestyles. The program focused on increasing physical activity and fitness levels of Delawareans. In 2018, Lt. Governor Bethany Hall-Long launched the Lt. Governor’s Challenge 2.0, which builds upon the work and achievements of Governor Carney. The Lt. Governor’s Challenge 2.0 expands the focus with a more holistic approach to health and emphasizes the importance of policy, systems, and environmental change initiatives in addressing community health needs.
THE LT. GOVERNOR’S CHALLENGE
The mission of the Lt. Governor’s Challenge is to improve the quality of life of all Delawareans.14 The program honors individuals, organizations, and institutions that inspire others by making healthy choices the easiest choices for their communities, ultimately helping elevate the well-being, productivity, and prosperity of the state of Delaware. The goal is to recognize organizations or individuals who are going above and beyond to advance health and well-being in one of four areas of focus: emotional well-being, healthy living, chronic disease management and prevention, and maternal and child health.14
More than just a recognition program for health and wellness initiatives, the Lt. Governor’s Challenge is an opportunity for applicants to demonstrate that they are drivers of change among family, neighborhoods, workplaces, faith organizations and institutions, communities, or schools. By sharing nominee’s stories and outcomes, they are motivated to continue to grow their initiatives and encourage other Delawareans to do the same.14
The Lt. Governor’s Challenge focuses on the power of community when it comes to encouraging and implementing changes that can improve quality of life for Delawareans. It was designed to mobilize and inspire individuals to act on their health and wellbeing. The program motivates, supports, and recognizes groups, individuals, and communities that work together to make the healthy choice the easiest choice for their members.15
By engaging businesses, local organizations, and individuals to be change-makers for health in their communities, the Lt. Governor’s Challenge spotlights and applauds those implementing solutions to create environments that support and sustain overall good health in the state.16
A PSE APPROACH
The Lt. Governor’s Challenge honors those who go above and beyond in implementing policy, systems, and environmental change (PSE) strategies. An individual’s ability to make healthy choices is heavily influenced by the systems and environment in which one lives, works, and plays. PSE approaches are sustainable changes used to address health disparities and the social determinants of health. PSE changes go beyond health education and programming and seek to enable communities to choose a healthy lifestyle.17 PSE approaches are designed to drive sustainable, multi-level change by making healthy choices available and accessible.18 Rather than focusing on individual health education, PSE changes are strategic and deliberate ways of addressing public health issues to ensure that healthy choices are practical, available, and accessible (Table 1).19
Programming
Often one-time event
Individual level
PSE Change
Ongoing effort
Population and community level
Short term Non-sustainingLong term Sustaining Additive Foundational
Policy, systems, and environmental change strategies in chronic disease prevention can be achieved through many approaches.
Policy
A formal written statement of position, decision, or course of action at the legislative or organizational level such as laws, ordinances, resolutions, mandates, regulations, or guidelines.19 Examples of policy approaches include:
• School or worksite wellness policies
• Legislation mandating physical fitness assessments in schools
• Tax on unhealthy foods
• Establishing smoke-free zones and policies.
Systems
Rules, procedures, and processes of an organization, involving the infrastructure of an organization or institution.19 Systems-level approaches can include:
• Development of a workplace wellness committee
• Updating intake forms and referral systems
• Training school teachers on childhood obesity prevention.
Table 1. Program vs. PSE Change17
117
Environmental Change
Changes made to the physical, social, or economic environment in which people live, work, and play.17,18 Examples of environmental change strategies include:
• Building and maintaining sidewalks and crosswalks to ensure pedestrian and bicycle safety
• Constructing and caring for community gardens
• Stocking vending machines with only healthy food and drink options
• Placing tobacco-free signage in frequented community spaces.
An individual’s ability to make healthy choices is dependent on the availability and accessibility of healthy choices in their everyday environments. PSE strategies create long-term, sustainable change that make the healthy choice the easiest choice.17
NOMINATION PROCESS
Individuals are encouraged to nominate themselves, another individual, or a group that exemplifies the promotion and practice of healthier living. The Challenge looks for nominees who go above and beyond what is regularly expected of them in their efforts to create a healthier state and who drive results through policy, system, and environmental changes in one of four areas of focus14:
Emotional Well-being
Initiatives promote and support emotional health through stress reduction, encouraging positive behaviors, emotional support groups, or similar opportunities.
Healthy Living
Initiatives foster environments for learning and lifestyle behavior changes related to healthier eating and drinking, exercise, weight control or obesity prevention, and avoidance or reduction of unhealthy habits such as tobacco use or excessive use of alcohol.
Chronic Disease Management and Prevention
Initiatives promote and offer access to health screenings, cultivate understanding of chronic diseases and how to live with them, and create an environment to support a higher quality of life for individuals living with a chronic disease.
Maternal and Child Health
Initiatives offer such opportunities as a breastfeeding policy, an environment supportive of breastfeeding mothers, and access to early childcare, which support the formation of a physically and emotionally healthy relationship between a mother and child in the early years of development.
Potential nominators are provided with resources and support as they navigate the nomination process, including step-by-step guidance and educational resources on PSE change, effective prevention strategies, and health and well-being programming.
SELECTION AND AWARDS
To be considered, an initiative must adopt or enhance policies, systems, or the physical environment aimed at improving physical, behavioral, and/or mental health. All initiatives must address short-term and long-term goals that will ultimately impact the health and wellness of Delawareans. In addition, each initiative must perform well in the following criteria categories14:
• Sustainability: The initiative should provide ongoing opportunity for healthier living, instead of being a one-time activity.
• Reach: The initiative should seek to demonstrate improvements in the capacity to address the health needs of a community or a target population.
• Outcome/Impact: The initiative should demonstrate improved access and/or increased opportunities for improving behavioral and physical health in the state.
The review committee is made up of impartial judges from state government, nonprofits, and community leaders who have high expertise in PSE strategies.14
The Lt. Governor’s Challenge honors two categories of awards and both categories of champions exemplify the Challenge’s mission to encourage healthy lifestyles. Recipients of the Delaware Wellness Hero Award show the highest degree and most comprehensive PSE changes to address their specific public health issues, while winners of the Delaware Health Leader Award are applauded for taking significant steps to improve the overall health of their community.16
Winners of the Lt. Governor’s Challenge Wellness Awards are honored at a prestigious award ceremony. At the ceremony, winners accept their awards, network with other community champions, and spend time with the Lieutenant Governor.
HALL OF FAME
Dozens of individuals and organizations have been honored since the inception of the Lt. Governor’s Challenge. Tables 2 and 3 illustrate honorees and their programs from 2023 and 2022, collectively. Table 4 outlines the list of honorees from 2019 to 2021. Honorees have developed, implemented, and evaluated programs that motivate long-term behavioral changes, leading to measurable impact on the well-being of individuals and their communities. For more information on the Lieutenant Governor’s Challenge and Hall of Fame honorees, visit: 2024 Lt. Governor’s Challenge (ltgovernorschallenge.org).
CONCLUSION
The Lieutenant Governor’s Challenge Wellness Award Program leverages community recognition as a tool to honor individuals and organizations who have gone above and beyond to improve the health and well-being of their community, and to inspire others to do the same. Utilizing a PSE approach drives sustainable, long-term behavior change by making healthy choices the easiest choices. The Lt. Governor’s Challenge continues to recognize those who are driving this change, and ultimately helping elevate the well-being, productivity, and prosperity of the state of Delaware.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Shebra Hall (Chronic Disease Bureau Chief) and Stephanie Belinske (Chronic Disease Epidemiologist II), staff members in the Division of Public Health, and contractors Aloysius Butler & Clark and Slice Communications for their support in implementing the Lt. Governor’s Challenge and for their assistance in developing this article.
Ms. Arthur may be contacted at helen.arthur@delaware.gov
118 Delaware Journal of Public Health - March 2024
Erin Ridout, Delaware Coalition Against Domestic Violence
The University of Delaware’s Institute for Excellence in Early Childhood
Providence Creek Academy Charter School
Nemours Children’s Health
The Sussex County Health Coalition
Face the Facts Delaware
Charity Crossing
Kim Blanch
Hope Lutheran Early Education Center
Delaware State University Wesley College of Health and Behavioral Sciences
Kuehne Company
The Eco Team at George S. Welch Elementary School
Community Education Building
Implementing statewide services to address domestic violence as a health issue and to integrate domestic violence and health services.
Creating a health and wellness program supporting family childcare educators that improves mental health and physical wellness, as well as providing social support to reduce stress and lower risk of chronic disease.
Creating a program that provides alternative therapeutic methods, such as art and farm therapy, to students experiencing loss and grief.
Creating the First Oral Feed Initiative for parents of infants with congenital heart defects, which provides education and fosters important early feeding experiences.
Improving physical health by providing grants for libraries to conduct exercise classes, and to provide access to community health workers who offered health and wellness coaching.
Providing resource and support to those who have lost loved ones to overdose or substance use disorder.
Incorporating physical activity into volunteer and community service activities.
Schell Brothers Homebuilders
Erika Cook
Created a program to educate Beebe Healthcare staff on trauma and how it affects physical health over a person’s lifetime.
Created a cooking class for children to broaden their food preferences and to include healthier choices by teaching about foods, why they are healthy, and how to grow the food from seed to harvest.
Developed a survey to screen for food insecurity and mental health impacts within their student population.
Created a “Wellness Wednesdays” program to improve the physical, emotional, and financial health of their staff.
Created an education program to expand on environmental literacy and knowledge, including lessons on recycling and composting as well as more frequent outdoor classes.
Worked with a network of partners to provide a healthy ecosystem for students, children, and families in Delaware.
Improved physical health by sponsoring exercise classes, having an on-site personal trainer, and building a gym for employees and their families.
Developed programs, including life-enrichment classes and wellness screenings, to combat social isolation and depression for residents at Selbyville’s Bayside community.
Table 2. 2023 Winners of the Lt. Governor’s Challenge, Delaware14
Table 3. 2022 Winners of the Lt. Governor’s Challenge, Delaware14
119
Brandywine Counseling & Community Services
Delaware Libraries
Hank’s Hope
Department of Services for Children, Youth and Their Families
Healthy Foods for Healthy Kids Incyte Corporation
Hispanic American Association of Delaware
The Breastfeeding Coalition of Delaware Reach Riverside Development Corporation
Rose Simon
Seaford School District Behavioral Health Team
Newark Charter School
Sexual Offense Support (University of Delaware)
Colonial District 1st Elementary Wellness Center –Eisenberg Elementary School Compassionate Schools Team Bling Vendors Committee: Healthy Vending Initiative
Department of Health and Social Services
Delaware Technical Community College: Mindfulness Summit
Delaware Department of Correction Perdue (Delaware Fit Biz)
ChristianaCare
IMPACT Delaware Tobacco Prevention Coalition
Polytech School District Children in Nature
Delaware Council on Farm and Food Policy Khayree Bey
REFERENCES
1. Centers for Disease Control and Prevention. (2019). Health and economic costs of chronic disease
https://www.cdc.gov/chronicdisease/about/costs/index.htm
2. Delaware Health Statistics Center. Delaware Vital Statistics Annual Report, 2021. Delaware Department of Health and Social Services, Division of Public Health.
3. Centers for Disease Control and Prevention. (2022, February 3). Heart disease and stroke
https://www.cdc.gov/chronicdisease/resources/publications/factsheets/ heart-disease-stroke.htm#high
4. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online]. 2021. https://www.cdc.gov/brfss/brfssprevalence/
5. Centers for Disease Control and Prevention. (2019). Diabetes and prediabetes
https://www.cdc.gov/chronicdisease/resources/publications/factsheets/ diabetes-prediabetes.htm
6. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online]. 2022. https://www.cdc.gov/brfss/brfssprevalence/
7. Delaware Department of Health and Social Services, Division of Public Health, Delaware Health Statistics Center, Vital Records Data, 2010-2019
8. Centers for Disease Control and Prevention. (n.d.). Linked birth / infant deaths. National Center for Health Statistics, National Vital Statistics System. https://wonder.cdc.gov/
9. Thrives, D. E. (n.d). Facts about rising pregnancy-related deaths in Delaware and the U.S. Delaware Healthy Mother & Infant Consortium. https://ddph-materials.s3.us-east-1.amazonaws.com/DEThrives/ dhmic-resouce-center/DDPHIM29285_BlackMaternalHealth_ infographic_04087.pdf
10. Centers for Disease Control and Prevention. (2022). About chronic diseases
https://www.cdc.gov/chronicdisease/about/index.htm
11. Centers for Disease Control and Prevention. (2022, December 20). Equitably addressing social determinants of health and chronic diseases
https://www.cdc.gov/chronicdisease/healthequity/social-determinantsof-health-and-chronic-disease.html
12. Public Health Law Center. (2022, May 31). Level setting on policy, systems, and environmental change. Public Health Law Center.
https://www.publichealthlawcenter.org/sites/default/files/inline-files/ MDH-PSE-Presentation.pdf
13. University of Kansas Center for Community Health and Development. (n.d.) Section 6. Honoring community champions. The University of Kansas.
https://ctb.ku.edu/en/table-of-contents/maintain/rewardaccomplishments/honor-community-champions/main
14. Delaware, Lt. Governor’s Challenge. (2024). Lt. Governor’s Challenge. https://ltgovernorschallenge.org
15. State of Delaware News. (2019, March 18). Lt. Governor Bethany-Hall Long announces the first round of award winners in the inaugural lt. governor’s challenge 2.0. State of Delaware.
https://news.delaware.gov/2019/03/18/lt-governor-bethany-hall-longannounces-the-first-round-of-award-winners-in-the-inaugural-ltgovernors-challenge-2-0/
16. State of Delaware News. (2023, October 12). 2023 lt. governor’s challenge winners announced. State of Delaware.
https://news.delaware.gov/2019/03/18/lt-governor-bethany-hall-longannounces-the-first-round-of-award-winners-in-the-inaugural-ltgovernors-challenge-2-0/
17. The Food Trust. (2012). What is policy, systems and environmental (PSE) change. The Health Trust.
https://healthtrust.org/wp-content/uploads/2013/11/2012-12-28Policy_Systems_and_Environmental_Change.pdf
18. Rural Health Information Hub. (2024). Rural health promotion and disease prevention toolkit. Rural Health Information Hub.
https://www.ruralhealthinfo.org/toolkits/health-promotion/2/strategies/ policy-systems-environmental
19. University of Delaware Cooperative Extension. (n.d.) What is policy, systems and environmental change. University of Delaware.
https://www.udel.edu/content/dam/udelImages/canr/pdfs/extension/ nutrition-wellness/de-fitbiz/What-is-PSE-Change-Flyer-.pdf
Table 4. 2019 -2021 Winners of the Lt. Governor’s Challenge, Delaware14
120 Delaware Journal of Public Health - March 2024
28th Annual Delaware Healthcare Forum
Tuesday, October 29, 2024



Delaware Healthcare
1280 South Governors Avenue, Dover DE 19904
Phone: 302-674-2853 | Fax: 302-734-2731
Web Site: www.deha.org
Primary Forum Contact: Yasmine Chinoy E-Mail: yasmine@deha.org
Sponsorship Opportunities Available!
Joint Providers
Hosted by
Association
121
Advancing Healthy Lifestyles: A Multicomponent Initiative to Reduce the Burden of Obesity In Delaware
Helen Arthur, M.H.A.
Chief, Health Promotion and Disease Prevention Section, Division of Public Health, Delaware Department of Health and Social Services
Lauren Butscher, C.H.E.S.
Program Administrator, Physical Activity, Nutrition, and Obesity Prevention Program, Division of Public Health, Delaware Department of Health and Social Services
Lisa Moore, M.P.A.
Chief, Health Promotion Bureau, Division of Public Health, Delaware Department of Health and Social Services
ABSTRACT
Advancing Healthy Lifestyles: Chronic Disease, Health Equity, & COVID-19 (“Advancing Healthy Lifestyles” or “AHL”) is a statewide initiative launched in January 2021 by the Delaware Department of Health and Social Services, Division of Public Health (DPH). DPH’s Physical Activity, Nutrition and Obesity Prevention Program (PANO) introduced the initiative as Coronavirus 2019 (COVID-19) swept through the state, exacerbating health burdens already faced by many Delawareans. The PANO Program provides administrative staff support to the Delaware Cancer Consortium’s Cancer Risk Reduction Committee (CRRC). In December 2019, the CRRC launched the Healthy Lifestyles Subcommittee (HLSC) in response to Governor John Carney’s request to develop actionable policy recommendations to positively influence healthy lifestyles in Delaware. The HLSC efforts led to the recommendation of 14 policy recommendations for action in three population health strategic focus areas:
1) birth to age 18; 2) employee health and wellness; and 3) community wellness. The AHL initiative builds from the work of the HLSC and promotes the use of policy, systems, and environmental change (PSE) strategies to reduce obesity and other chronic conditions among Delawareans across the lifespan. Ideally, the AHL initiative is categorized into three component strategies: school, community, and workplace. This article highlights both completed and ongoing projects under the AHL Initiative that aim to address the burden of obesity in Delaware.
BACKGROUND
The Coronavirus 2019 (COVID-19) pandemic presented significant health, social, and economic burdens in Delaware and globally. The pandemic took a disproportionate toll on the health and well-being of people of color and other underserved groups.1 Every sector of society is working to identify solutions that address challenges resulting from the pandemic and to advance policies that focus on the health and wellness of Delaware’s most vulnerable populations. DPH, like the rest of the nation, is concerned with the higher prevalence of chronic health conditions among its aging population, communities of color, and those living with complex medical, behavioral health, and social needs. The state quickly learned through its COVID-19 response that communities of color had an increased risk of COVID-19 morbidity and mortality due to their higher prevalence of chronic health conditions. Communities of color were more likely to be exposed to infection while working, due to their overrepresentation in essential jobs in transportation, government, health care and food supply services, and in low wage or temporary jobs that did not allow telework or provide sick leave. It was evident that DPH needed to advance emerging policy, systems, and environmental change (PSE) strategies to improve health outcomes during the pandemic.
Obesity of adults and children is a serious chronic illness associated with the leading causes of death in the United States.2 According to the Centers for Disease Control and Prevention
(CDC), adults with obesity have a higher risk of chronic disease and premature death compared to those of normal weight.3 Children with obesity are at higher risk of developing mental health issues, social problems, and obesity in adulthood.3 Obesity is associated with a greater risk of other severe health conditions such as type 2 diabetes, heart disease, asthma, stroke, and multiple cancers.3
Obesity and many of its associated chronic diseases are complex and caused by several different factors. Obesity is a result of lifestyle choices and health risk behaviors such as poor nutrition and physical inactivity.4 Obesity is also influenced by the Social Determinants of Health (i.e., the conditions in which one lives, works, and plays). Health inequities and differences in Social Determinants of Health lead to disparities in obesity and chronic disease prevalence among racial, ethnic, and socioeconomic groups and among those in different geographical areas and with different physical abilities.5
The Delaware Department of Health and Social Services, Division of Public Health (DPH) launched the AHL initiative for two primary reasons: 1) to advance healthy lifestyles; and 2) to eliminate health disparities. The AHL initiative aims to facilitate the State’s systematic approach to addressing –structural and systemic inequities by strategizing how to work across sectors, address long-term health and social needs of a community, and remove structural barriers to health for socially vulnerable populations.
Doi: 10.32481/djph.2024.03.17
122 Delaware Journal of Public Health - March 2024
DELAWARE DATA HIGHLIGHTS
In Delaware, and nationally, there are high rates of overweight and obese individuals, and the prevalence of obesity in Delaware is trending upward.6 According to the Delaware Behavioral Risk Factor Survey, in 2022, 37.9% of Delaware adults ages 18 years and older were obese, and 33.9% were overweight.6 High levels of obesity are also seen among Delaware youth. The Delaware Youth Risk Behavior Survey shows, in 2021, 32% of high school students were overweight or obese.7
Obesity is preventable and making simple lifestyles changes – such as choosing a healthy diet and achieving the recommended levels of physical activity – contribute to maintaining a healthy weight and preventing obesity. However, in 2019, only 24% of Delaware adults met the weekly recommended levels of both strength and aerobic activity.8 Additionally, 21% of Delaware adults reported eating less than one vegetable a day, and almost 40% report eating fruit less than once per day in 2021.9 In 2022, 23.5% of Delaware adults reported they did not participate in any physical activity or exercise in the last month.6 Data in 2021 show that Delaware youth were also not meeting the daily recommended levels of physical activity. More than half (58.8%) of high school students in Delaware reported not being physically active for at least 60 minutes every day during the past seven days.7
Obesity and an individual’s ability to make healthy choices are influenced by many factors, including individual-level risk factors and genetics and community and systems-level factors such as school environments, the natural and built environment, access
to affordable healthy foods, and safe, convenient, and accessible places to engage in physical activity.10
Many Delaware residents suffer from chronic disease, and 10% have multiple chronic conditions. According to the Delaware Health Statistics Center, in 2020, chronic diseases accounted for seven of the 10 leading causes of death in Delaware, with more than 6,500 Delaware residents dying of chronic diseases (at least 61% of all deaths, Figure 1). Cardiovascular diseases and cancer accounted for 39% of deaths alone.11
Given Delaware’s high prevalence and mortality rate of chronic conditions, the projected increase in the burden of chronic disease nationwide, and the implications for preventing and treating chronic diseases in the wake of COVID-19, it is important for DPH to continue to monitor chronic disease incidence, prevalence, and mortality. A multi-faceted approach addressing individual, community, and system-level factors is vital to promote healthy lifestyles, address health inequities, and reduce the burden of obesity in Delaware. Individuals and organizations from all sectors must come together to promote PSE strategies in multiple environments to reach Delawareans throughout the lifespan.
The PANO Program’s AHL initiative aligns with the goals and objectives of the U.S. Office of Disease Prevention and Health Promotion Healthy People 2030 initiative and follows evidence-based decisions and sound investments on collaborations across communities and sectors to improve the health of Delaware’s population.
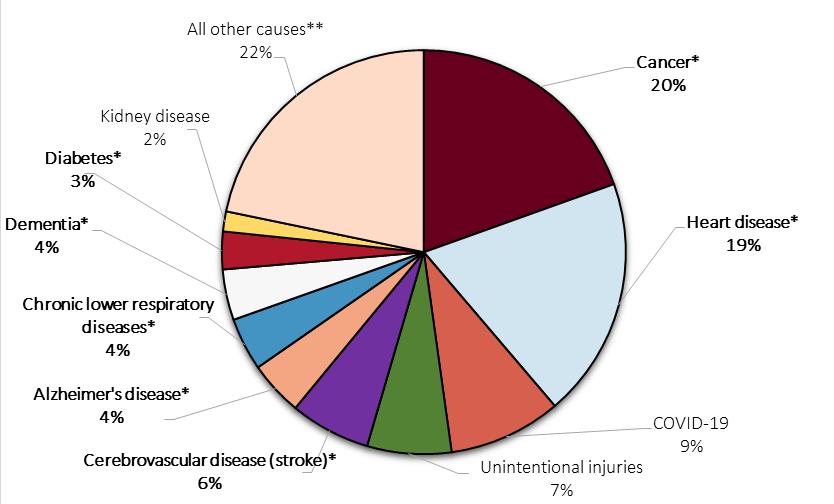 Figure 1. Percentage of Leading Causes of Deaths, by Cause of Death, Delaware, 202011
Figure 1. Percentage of Leading Causes of Deaths, by Cause of Death, Delaware, 202011
123
*Bolded text indicates the cause of death is considered a chronic disease; **This includes all other causes of death not represented in the figure, including but not limited to influenza and pneumonia, chronic liver disease, assault (homicide), and intentional self-harm (suicide).
ADVANCING HEALTHY LIFESTYLES
The Physical Activity, Nutrition, and Obesity Prevention (PANO) Program, within DPH’s Bureau of Health Promotion, uses a public health approach to address the role of physical activity and nutrition in improving health and chronic disease for all Delawareans. PANO’s vision is for all Delawareans to lead healthy lifestyles and its mission is to provide goals and strategies for government, media, communities, health care providers, schools, and worksites to decrease overweight prevalence and obesity in Delaware. The PANO program addresses high rates of obesity, physical inactivity, and poor nutrition through multiple initiatives that build capacity to implement evidence-based programmatic, and PSE strategies.
In January 2021, PANO launched a statewide initiative, Advancing Healthy Lifestyles: Chronic Disease, Health Equity, & COVID-19 (“Advancing Healthy Lifestyles” or “AHL”) in response to the high levels of obesity, chronic disease, physical inactivity, and poor nutrition in Delaware. AHL seeks to reduce obesity and other chronic conditions as part of an effort to achieve long-term health equity throughout Delaware. To accomplish this, AHL promotes the use of PSE strategies in schools, communities, and workplaces to reach Delawareans across the lifespan. The AHL initiative is categorized into three component strategies that are focused on the school, community, and workplace settings (Figure 2).12
ADVANCING HEALTHY LIFESTYLES OUTCOMES
All projects under the AHL Initiative are aligned with the Advancing Healthy Lifestyles outcomes:
• Increase healthy eating and healthy beverage consumption in the state across all settings.
• Increase physical activity in early childcare, schools, and community-based settings.
• Promote the adoption of physical education/physical activity (PE/PA) in schools.
• Promote the adoption of physical activity (PA) in early care and education (ECEs) and worksites.
• Increase population health and wellness programs/ platforms in worksites in state, schools, and community-based settings (e.g., tobacco prevention, wellness challenges, education materials, and online modules focused on wellness and nutrition).
• Adopt strategies to improve community-clinical linkages.
• Increase use of lifestyles intervention programs in community settings for primary prevention of chronic diseases.
• Have policies, processes, and protocols in schools meet the management and care needs of students with chronic conditions (e.g., asthma, diabetes).
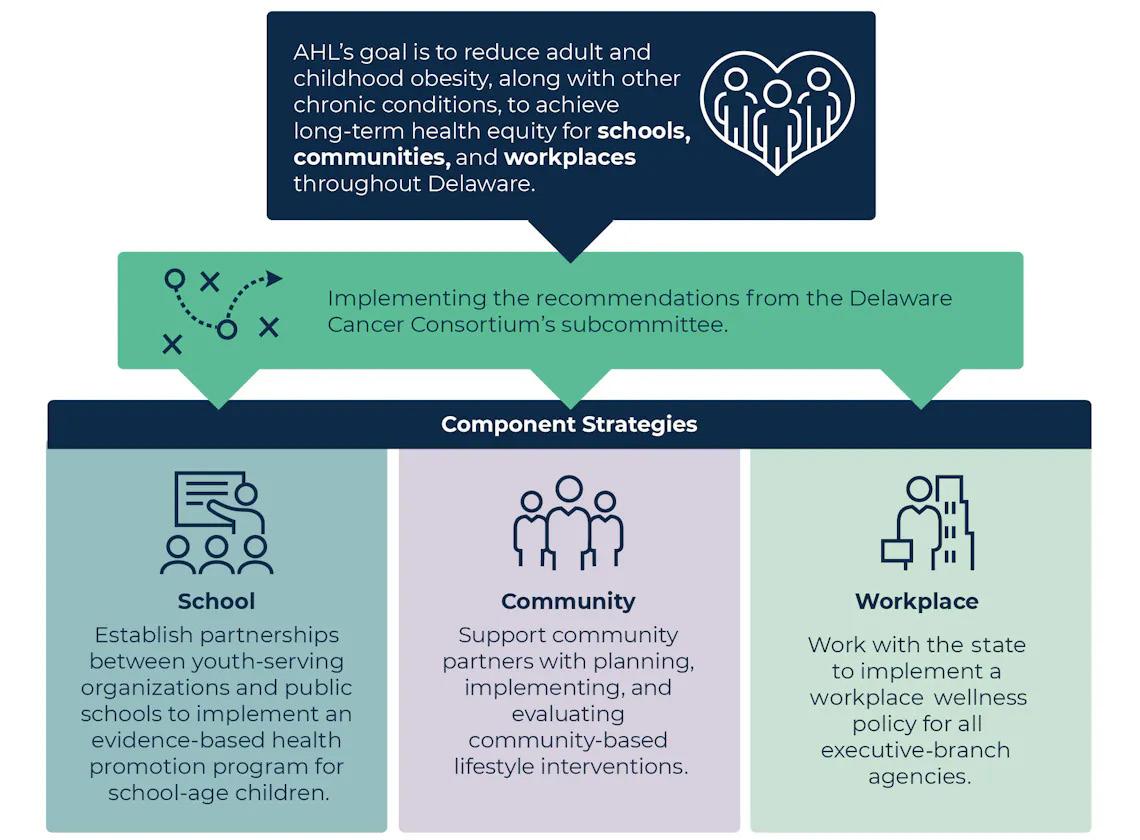
124 Delaware Journal of Public Health - March 2024
Figure 2. Goal and Strategies for the Advancing Healthy Lifestyles Initiative, Delaware, 202112
STATEWIDE ACTION PLAN
In summer 2022, the AHL Initiative produced a statewide action plan, which translates the 2021 Delaware Cancer Consortium’s Healthy Lifestyle Subcommittee (HLSC) policy recommendations into actionable strategies. The 14 HLSC recommendations (Table 1) focus on policy and action in three key areas: 1) early childhood and school-age children (Birth to age 18); 2) workplace wellness (Employee Health); and 3) community interventions (Community Wellness). To develop the action plan, the PANO and the AHL team held discussion groups and interviews with 65 experts, program leaders, and providers from diverse Delaware agencies and organizations. These individuals shared their perspectives and discussed how to advance potential future action for each recommendation. The final action plan summarizes each HLSC recommendation, the recommendation’s potential to advance equity, and whether legislation or funding is needed to implement the recommendation. The action plan also includes factors and challenges that agencies can consider when implementing the recommendations.
AHL LEARNING SERIES
The PANO Program and AHL team facilitated three learning sessions as a part of its Learning Series, with more than 176 people attending all sessions combined between November 2022 and May 2023. The series included webinars on evidencebased approaches to building organizational capacity in key programs related to AHL priorities. The three webinars focused on community-school partnerships, workplace wellness, and nutrition and healthy eating among community partner programs. Table 2 summarizes the learning session topics.
SCHOOL-COMMUNITY PARTNERSHIP DEMONSTRATION PROJECT
To improve the health and wellness of school-age students in Delaware, the AHL Initiative launched an innovative schoolcommunity partnership between youth serving organizations and public schools throughout Delaware. Triple Play is a national Boys and Girls Clubs healthy lifestyles program that
Delaware Cancer Consortiums’ Healthy Lifestyles Subcommittee Policy Recommendations, 2021
1. Endorse a “Health in All Policies” approach to focus on social and environmental justice, human rights, and equity in the development, implementation, and evaluation of all policies to ensure policy-oriented strategies for promoting health equity. (Cross-Cutting)
2. Expand DELACARE regulations (Regulations for Early Care and Education and School-Age Centers) to family childcare homes and strengthen physical activity requirements across settings. (Birth to age 18)
3. Prohibit sugar sweetened beverages (SSBs) in Early Childhood Care and Education Centers. (Birth to age 18)
4. Preserve robust school nutrition standards, as defined in the 2010 U.S. Department of Agriculture(USDA) nutrition guidelines for school lunches and maintain flexible, healthy standards relative toconsumption of sodium, whole grain, and milk. (Birth to age 18)
5. Strengthen the implementation of annual health related fitness assessment, reporting andcompliance standards set forth in Delaware Department of Education Regulation 503 InstructionalProgram Requirements Section 5.0: Physical Education. (Birth to age 18)
6. Develop and implement out-of-school nutrition policies (before-school, after-school, sports). (Birth to age 18)
7. Propose and implement time requirement standards for elementary, middle and high school physicaleducation and physical activity. (Birth to age 18)
8. Strengthen breastfeeding supports in the workplace and other settings, including anti-discriminationprotections; strengthen breastfeeding protections at hospitals. (Employee Health)
9. Create a formal workplace wellness program infrastructure for state employers. Encourage non-stateemployers to adopt workplace wellness program infrastructure. (Employee Health)
10. Strengthen the corner store intervention model via federal food assistance programs to increaseaccess to and consumption of healthier food options to reduce food insecurity and promotenutritious diets in targeted communities. (Community Wellness)
11. Create a financing mechanism to support Healthy Communities Delaware. (Community Wellness)
12. Expand Delaware Supplemental Nutrition Assistance Program Education (SNAP-Ed)-like programming to lowincome Delawareans. (Community Wellness)
13. Explore model policies for reducing consumption of sugar-sweetened beverages (SSBs), includingwarning labels, counter-marketing, SSB taxes, and/or bans on SSB marketing on/near schools. (Community Wellness)
14. Strengthen and enhance Delaware’s Complete Streets policy to support the Delaware Department ofTransportation’s work building active, accessible transportation. (Community Wellness)
Table 1. Fourteen Policy Recommendations of the Delaware Cancer Consortium’s Healthy Lifestyles Subcommittee,13 Delaware, 2021
125
Learning SessionSummary
Community-School Partnerships; Support During After School
November 17, 2022
Workplace and Employee Wellness
March 3, 2023
Advancing Healthy Lifestyles in Delaware Community Partnerships
May 11, 2023
The webinar showcased the Boys & Girls Clubs of Delaware’s work to deliver the Triple Play program to hundreds of school-age youths statewide. The panel reviewed the pilot phase of the project, the basics of the Triple Play curriculum, and problem-solving efforts to deliver programming and collect data while navigating staffing challenges, COVID-19 policies, and competing student priorities.
The webinar focused on benefits to employers and employees, the current state of workplace health in the country, and available tools and resources from the Centers for Disease Control and Prevention (CDC). Panelists reviewed examples of workplace wellness efforts led by Delaware executive branch agencies and the workplace wellness resources from CDC, with DPH serving as a key partner in this effort. This session also addressed Delaware’s work in developing the Department of Human Resources’ (DHR’s) policy and toolkit to help executive branch agencies implement workplace wellness initiatives. The webinar provided an overview of the policy and toolkit.
The webinar discussed the community-based nutrition initiatives of three community partners: the City of Newark; Delaware Breast Cancer Coalition; and University of Delaware Cooperative Extension. The webinar included presentations highlighting their ongoing work in addressing community needs, challenges, and lessons learned.
seeks to improve youths’ knowledge of healthy habits, good nutrition, and physical fitness; increase the time they spend participating in physical activities each day; and strengthen their ability to interact positively with others and engage in healthy relationships.
In partnership with the PANO Program, the Boys and Girls Clubs of Delaware launched the Triple Play Program with elementary school-age youth in 2022 as an after-school program. The Wowzers! Program, a teen workforce initiative in which participants are hired and trained to run programs and lead lessons for younger club members, conduct Triple Play programming with the youth. Triple Play utilizes age-appropriate curricula to implement lessons with students in grades kindergarten through eighth grade. Since Triple Play’s launch in the spring of 2022, more than 1,000 students from schools in New Castle, Kent, and Sussex counties have participated. Lessons within the Triple Play program are written to build the skills, attitudes, knowledge, and behaviors essential to live a healthy lifestyle, and to help students learn to sustain the health of the mind, body, and soul. Three categories of lessons are provided to address the Triple Play program’s goals: daily challenges, healthy habits, and social recreation.15
BUILDING THE CAPACITY OF COMMUNITY PARTNERS
The AHL Initiative supports and strengthens the capacity of four primary community partners: the American Lung Association, University of Delaware Cooperative Extension, and two teams from Delaware State University (DSU). These organizations are launching PSE initiatives focused on accessing healthy food, creating opportunities for physical activity, and finding ways to prevent and manage chronic diseases. The PANO Program provides funding and technical assistance to all four partners, discussing their progress and developing promising solutions to challenges.16
• The American Lung Association is promoting lungfriendly schools and youth-serving environments by providing asthma and tobacco education and training to young people, their caregivers, and school staff.
• University of Delaware Cooperative Extension is improving access to healthy, local foods by connecting food growers and producers with local corner stores.
• DSU is building gross and fine motor skills for children with Autism through play-based activities and swim instruction and improving menu options for caregivers of children with Autism.
• DSU is providing summer and after-school programming for children that increases access to physical activity and healthy eating.
ADVANCING HEALTHY LIFESTYLES MINI-GRANTS
In fall 2022, the AHL Initiative launched a new mini-grant program, through which community partners receive funding and support for their community-based health interventions that promote PSE strategies related to physical activity or healthy eating and nutrition. The annual mini-grant program period is seven months, running from October to May. Mini-grant projects align with the outcomes of the AHL Initiative.
AHL mini-grants are awarded through a formal application and review process. Applicants must detail a proposed project that includes a description of the target population, intended reach, and goals and objectives that are aligned with the outcomes of the AHL Initiative. Mini-grants are funded by the DPH PANO Program through the Delaware Health Fund and can range up to $15,000. Organizations awarded mini-grants are required to submit progress reports throughout the project year to report on activities and project outcomes. Seven organizations were awarded an AHL mini-grant in year one (Table 3) and year two (Table 4) of the mini-grant program.
Table 2. Content summaries, Advancing Healthy Lifestyles Learning Series, Delaware, November 2022-May 202314
126 Delaware Journal of Public Health - March 2024
4-H Cooperative Extension Promote physical activity in schools, the community, and the workplace, including Walk with Ease, Walk Across Delaware, Walking Through the Holidays, and plogging (jogging while picking up litter).
Boys & Girls Clubs of Delaware
City of Newark
Delaware Breast Cancer Coalition
Inner City Cultural League
Worship Christian Center
YMCA of Delaware
Provide educational opportunities on a mini-farm, including food education/ nutrition programs.
Construct a community garden to foster community and a healthy lifestyle.
Support a free, 12-week, open-to-the-public health education program geared toward people at risk for chronic disease, including breast cancer, with the goal of increasing physical activity and nutritional knowledge.
Support a community garden, nutrition education, and physical activity.
Launch a healthy food and nutrition initiative that includes food preparation/nutrition classes and a walking club.
Recruit participants for the Lifelong Essentials for Activity and Nutrition program, which offers education and exercise for those struggling to obtain a healthy weight.
4-H Cooperative Extension Intends to increase chronic disease prevention and population health by continuing physical activity initiatives including walking clubs, plogging, and virtual youth fitness curricula.
Boys & Girls Clubs of Delaware
Delaware State University
Delaware Breast Cancer Coalition
Inner City Cultural League
La Red Health Center
West Side Family Healthcare
Aims to address food access and insecurity, hopes to coordinate community events, establish a produce stand, and enhance youth education in agriculture and nutrition.
Aims to establish and assess programming focused on physical activity and nutrition for DSU students to deliver educational resources that empower students to make informed and healthier lifestyle choices.
Support a free, 12-week, open-to-the-public health education program geared toward people at risk for chronic disease, including breast cancer, with the goal of increasing physical activity and nutritional knowledge.
Aims to continue existing initiative to decrease obesity and chronic diseases which includes conducting physical activity classes, maintaining a community garden, and actively involving participants in education focused on nutrition and agriculture.
Intends to enhance access to healthy food, physical activity, and address food insecurity for prenatal/ pediatric patients and mothers through distributing CSA produce shares and providing pregnancy nutrition classes and martial arts sessions.
Intends to implement an off-road program as an extension of their Feeding Families Initiative. This program assists families in transitioning out of Feeding Families while ensuring access to healthy foods and sustaining their newfound healthy eating habits.
IMPROVING WORKPLACE AND EMPLOYEE HEALTH
The PANO program collaborated with the Delaware Department of Human Resources (DHR)’s Statewide Benefits Office to develop a workplace wellness policy and accompanying toolkit for all executive branch agencies. The PANO and AHL team received input from 18 Delaware state agencies, as well as from an administrator from the CDC’s Workplace Health Program.
DHR released the Workplace Wellness Policy and Procedures and Workplace Wellness Toolkit in June 2022. The policy provided guidance on the foundation and infrastructure for executive branch agencies to establish and maintain workplace wellness initiatives. The toolkit is designed to help agencies implement the workplace wellness policy and offers best practices for employers, tips, and tools. Shareable resources include a standardized liability waiver for participation in workplace fitness activities and a media release form.
Table 3. Mini-grant project activities, Advancing Healthy Lifestyles Initiative, Delaware, October 2022-May 202317
Table 4. Mini-grant project activities, Advancing Healthy Lifestyles Initiative, Delaware, October 2023-May 202417
127
The toolkit describes some benefits that agencies can gain from implementing these initiatives:
• Reduced health risks
• Improved health status and quality
• Improved productivity, morale, and retention
• Lower health care costs and disability
• Fewer workers’ compensation claims
• Reduced absences from illness or injury.
Following the release of the toolkit, the PANO and AHL team worked with select executive branch agencies to assess progress with their workplace wellness initiatives. Collectively, the team interviewed agency leaders from Delaware’s Department of Correction and the Delaware Department of Health and Social Services’ DPH and Division of Social Services to discuss current wellness offerings for the agencies’ employees, as well as facilitators of, and barriers to, the planning of activities and employee participation.
ADVANCING HEALTHY LIFESTYLES CONFERENCE
The Advancing Healthy Lifestyles Conference provides a platform for cross sectional sharing on national, regional, and local best practices, challenges, opportunities, and success stories. The goal of the AHL Conference is to strengthen efforts to reduce obesity and other chronic diseases amongst Delawareans and to serve as an opportunity to close gaps in health inequities, assess progress, and further strengthen the work of community stakeholders. Conference sessions are intended for government legislative and administrative policy makers in public health, nonprofit advocates of health and wellness, educators, medical caregivers and policy experts, and academic and medical researchers who are interested or engaged in health disparities, nutrition, chronic illness, and obesity prevention.18
The inaugural AHL conference was held on May 18, 2023, and focused on improving health through equity. The conference included one keynote speaker and 23 presenters. Of the 309 registrants, 264 attendees participated in a plenary panel session, three breakout panel sessions, and an interactive roundtable plenary session. Local and national subject matter experts presented how to improve health through equity, address systemic bias in health care, and improve health through community collaborations, as well as the trauma of racism and health disparities. There were 10 resource tables on display throughout the conference, with 18 table facilitators providing attendees with resources, education, and information on community services. The discussions led to 69 attendees from New Castle, Kent, and Sussex counties signing up for roundtable follow-up sessions to continue these conversations and begin the strategic planning process and formation of an AHL Coalition. Most conference attendees reported that sessions were “Very Good” or “Good.”
The Advancing Healthy Lifestyles Conference will serve as an annual convening for cross-sector collaboration, further strengthening the knowledge and skillset of Delaware partners to implement effective lifestyle change and obesity prevention initiatives. The second conference is planned for June 6, 2024, on the DSU campus.
ADVANCING HEALTHY LIFESTYLES COALITION
Following the inaugural AHL Conference in the spring of 2023 and follow-up roundtable discussions, the statewide Advancing Healthy Lifestyles Coalition was formed later that year with a collective impact approach to lead community and systems-level change. The vision is to uplift the well-being of all Delawareans and break down barriers to achieve healthy lifestyles. The mission is to bring together coalitions and partners to focus on healthy lifestyles and equity through the PANO lens to leverage and expand resources in the community.19
The AHL Coalition membership is made up of individuals from public and private multi-sector organizations. Coalition membership has representation from local health systems, universities, state agencies, non-profits, faithbased organizations, and youth-serving organizations.
The Coalition supports and promotes strategic planning, implementation, and evaluation of healthy lifestyle and obesity prevention initiatives. All members, projects, and decisions are guided by the Coalition’s four core values: inclusivity, building trust, collaboration, and collective action.19
The AHL Coalition identified five strategic priorities to help form action steps and guide the Coalition’s direction19:
• Collaboration and partnerships. Engage coalitions and key representatives across the health system with a PANO focus to serve as a repository, knowledge sharing, and networking vehicle.
• Community outreach engagement and access. Provide outreach opportunities to increase access to existing programs and services with a PANO focus, regardless of income, race, ethnicity, gender identification, age, ability, citizenship status, or geography.
• Program development linked to PANO. Identify gaps in services and programs that increase access to PANO related services that reduce health disparities, improve outcomes, and affect system or cultural change.
• Marketing and communications. Develop a marketing plan for existing programs linked to PANO and other coalitions that promote equity and help reduce health disparities.
• Policy, systems, and environmental change (PSE). Advocate for PSE strategies with a PANO focus that increase equitable access to health programs and services to increase access and reduce healthy disparities.
The AHL Coalition aims to identify and address current gaps in resources, services, and programs to lead community and systems-level change related to healthy lifestyles, chronic disease, and obesity prevention in Delaware.
128 Delaware Journal of Public Health - March 2024
CONCLUSION
The AHL initiative is an emerging initiative to propel efforts to improve health in Delaware. High rates of physical inactivity, poor nutrition, and obesity leads to the realization that public health efforts in the state to improve health and achieve health equity will require more broad population health approaches that address social, economic, and environmental factors that influence health. In a postpandemic climate, DPH recognizes that it is necessary to take a multi-component approach to address this public health crisis. The PANO Program’s Advancing Healthy Lifestyles Initiative promotes the use of PSE strategies to reach Delawareans across the lifespan. AHL leverages multisector community collaborations to build capacity and utilize collective impact to increase healthy lifestyles and reduce the burden of obesity in Delaware.
As the PANO Program continues to facilitate and support the AHL initiative and the AHL Coalition infrastructure in Delaware, a culture of collaboration and trust is forming. This will undoubtedly lead to development and sustainability of shared goals, strategies, and ownership of lasting social and structural change. DPH foresees this change prompting heightened awareness of factors that focus on social determinants of health, elimination of health disparities, and improvement of overall health outcomes for Delaware residents.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Shebra Hall (Chronic Disease Bureau Chief) and Stephanie Belinske (Chronic Disease Epidemiologist II), staff members in the Division of Public Health, and Mathematica, the contractor supporting the work of the Advancing Healthy Lifestyles Initiative, for their assistance in implementing the Advancing Healthy Lifestyles Initiative and the development of this article.
Ms. Arthur may be contacted at helen.arthur@delaware.gov
REFERENCES
1. Ndugga, N., & Artiga, S. (2023, April 21). Disparities in health and health care: 5 key questions and answers. KFF. https://www.kff.org/racial-equity-and-health-policy/issue-brief/ disparities-in-health-and-health-care-5-key-question-and-answers/
2. Centers for Disease Control and Prevention. (2022, April 7). Common, serious, costly. Centers for Disease Control and Prevention.
https://www.cdc.gov/obesity/basics/index.html
3. Centers for Disease Control and Prevention. (2022, July 15). Consequences of obesity. Centers for Disease Control and Prevention.
https://www.cdc.gov/obesity/basics/consequences.html
4. Centers for Disease Control and Prevention. (2022). About chronic diseases. Centers for Disease Control and Prevention. https://www.cdc.gov/chronicdisease/about/index.htm
5. Centers for Disease Control and Prevention. (2021, August 20). Health equity. Centers for Disease Control and Prevention.
https://www.cdc.gov/nccdphp/dnpao/health-equity/index.html
6. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online]. 2022.
https://www.cdc.gov/brfss/brfssprevalence/
7. Delaware Health & Social Services, Division of Public Health, Youth Risk Behavior Survey (YRBS), 2021
8. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online]. 2019.
https://www.cdc.gov/brfss/brfssprevalence/
9. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online]. 2021.
https://www.cdc.gov/brfss/brfssprevalence/
10. Centers for Disease Control and Prevention. (2021, August 30). Childhood overweight and obesity. Centers for Disease Control and Prevention.
https://www.cdc.gov/obesity/childhood/index.html
11. Delaware Health Statistics Center. (n.d.). Delaware vital statistics annual report, mortality, 2020. Division of Public Health, Delaware Department of Health and Social Services.
https://dhss.Delaware.gov/dhss/dph/hp/2020.html
12. Delaware, H. (2024). Advancing healthy lifestyles. Delaware Cancer Consortium.
https://www.healthydelaware.org/Community-Partners/AdvancingHealthy-Lifestyles#intro
13. Delaware Cancer Consortium, Cancer Risk Reduction Committee. Healthy Lifestyles Subcommittee, 2021.
https://www.healthydelaware.org/Consortium/Committees/CancerRisk-Reduction/Healthy-Lifestyles-Subcommittee#members
14. Delaware, H. (2023). Advancing healthy lifestyles, AHL learning series. Delaware Cancer Consortium.
15. Boys and Girls Clubs of America. (n.d.) Triple Play: A game plan for mind, body and soul. Boys and Girls Clubs of America.
https://www.bgca.org/programs/sports-recreation/triple-play
16. Delaware, H. (2024). Community capacity building. Delaware Cancer Consortium.
https://www.healthydelaware.org/Community-Partners/AdvancingHealthy-Lifestyles/Community-Capacity-Building#intro
17. Delaware, H. (2024). Mini-grant awards. Delaware Cancer Consortium.
https://www.healthydelaware.org/Community-Partners/AdvancingHealthy-Lifestyles/Mini-Grant-Awards#intro
18. Delaware, H. (2024). Advancing healthy lifestyles conference 2024. Delaware Cancer Consortium.
https://www.healthydelaware.org/Consortium/Annual-Retreats-AndSpecial-Events/Advancing-Healthy-Lifestyles-Conference-2024#intro
19. Delaware, H. (2024). Advancing healthy lifestyles coalition. Delaware Cancer Consortium.
https://www.healthydelaware.org/Community-Partners/AdvancingHealthy-Lifestyles/Advancing-Healthy-Lifestyles-Coalition
129




130 Delaware Journal of Public Health - March 2024
The Impact of Diabetes in Delaware, 2023 is prepared for the Delaware General Assembly in accordance with 16 Del. Code, Chapter 1, Subchapter II, §140A The report is a collaboration of the following three agencies:
• Delaware Department of Health and Social Services (DHSS), Division of Public Health (DPH)
• DHSS, Division of Medicaid & Medical Assistance (DMMA)
• Delaware Department of Human Resources (DHR), Statewide Benefits Office (SBO)
DPH oversees diabetes activities and programming statewide DMMA provides medical assistance to Delaware Medicaid members through a variety of programs; most activities related to diabetes are administered through contract ed Medicaid Managed Care Organizations (MCOs). SBO administers health benefits to State Group Health Insurance Plan (GHIP) members and works directly with health plan vendors to provide resources tailored to meet the needs of members with diabetes and tho se at risk for the disease The agencies work together and with partner stakeholders to achieve the four long-term goals outlined in the Delaware Diabetes Plan .
The Impact of Diabetes in Delaware, 2023 provides Delaware legislators with up-to-date information on diabetes prevalence, programming, costs, and progress in the First State.
For more information, contact:
Delaware Department of Health and Social Services
Division of Public Health
Diabetes and Heart Disease Prevention and Control Program (DHDPCP)
Thomas Collins Building, Suite 11 540 S DuPont Highway
Dover, DE 19901 Phone: 302-744-1020
Fax: 302-739-2545
https://www.dhss.delaware.gov/dhss/dph/dpc/diabetes.html
To read the full report, please visit
https://dhss.delaware.gov/dhss/dph/dpc/files/diabetesburdenreports23.pdf.
131
Executive Summary
The Impact of Diabetes in Delaware is published biennially to provide Delaware legislators with up-to-date information on diabetes prevalence, programming, costs, and progress in the First State. The 2023 report is the third iteration of The Impact of Diabetes in Delaware This report includes Delaware diabetes prevalence, programming, and health care utilization data for the 2021-2022 time period.
Diabetes is a chronic disease that affects how your body uses food for energy . Left untreated, diabetes can lead to a host of poor health outcomes including heart disease, stroke, kidney disease, lower limb amputations, blindness, and death . The good news is that diabetes is largely preventable through basic prevention steps like eating a healthy diet, getting regular physical activity, and losing a small amount of extra weight The American Diabetes Association (ADA) recommends at least 150 minutes per week of moderate-intensity physical activity and weight loss of 5%-7% to prevent or delay the onset of diabetes in populations at high risk for the disease [1]. Those who develop diabetes can effectively manage the condition through healthy lifestyle behavio rs and a medication regimen to control blood glucose levels.
Diabetes in Delaware
In 2021, 12.0% of all Delaware adults reported that they had been diagnosed with diabetes [2]. This means that more than 95,000 Delaware adults know they have diabetes. Another 12.6% of Delaware adults report being told they have prediabetes, a condition that places them at greater risk of progressing to diabetes In total, 24.6% of Delaware adults have either diabetes or prediabetes .
In 2021, there was no significant difference in diabetes prevalence between males (12.2%) and females (11.7%) in Delaware [2] While the difference in diabetes prevalence between non-Hispanic Black (15.0%) and non-Hispanic White (11.4%) adults was not statistically significant in 2021 [2], the trend has shown that non-Hispanic Black Delaware adults consistently have a higher diabetes prevalence compare d to non-Hispanic White Delaware adults.
Diabetes becomes more prevalent with age . Among Delawareans ages 45-54, a significantly lower percentage (9.6%) report having diabetes compared to those ages 55-64 (18.2%) and those ages 65 and older (23.4%) [2]. In 2021, diabetes prevalence in Sussex County (13.2%) was higher than in Kent (11.4%) and New Castle (11.6%) counties [2]
The Impact of Diabetes in Delaware, 2023 1 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
132 Delaware Journal of Public Health - March 2024
Diabetes Management
Although diabetes can be effectively managed through healthy lifestyle behaviors and a medication regimen to control blood glucose levels , a high proportion of Delaware adults with the disease do not have their diabetes under control . Only six in 10 Delaware adults with diabetes check their blood glucose level at least once a day [2] Just over half (52.0%) of Medicaid members with diabetes have their diabetes under control, as defined by a Hemoglobin A1C level of less than 8%. High rates of cooccurring conditions, or comorbidities, make it harder for a person with diabetes to achieve diabetes control. In Fiscal Year 2022 (FY22), 78.7% of active employee and early retiree members with diabetes covered by the State Group Health Insurance Plan (GHIP) had at least one of the most frequently diagnosed comorbidities : congestive heart failure, coronary artery disease, chronic obstructive pulmonary disease (COPD), hypertension, osteoarthritis, HIV/AIDS, rheumatoid arthritis, obesity, and low back disorder.
High Risk Populations
The Delaware Department of Health and Social Services, Division of Public Health (DPH), Division of Medicaid & Medical Assistance (DMMA), and the Delaware Department of Human Resources, Statewide Benefits Office (SBO) recognize eight groups of Delaware adults who are at elevated risk for diabetes and diabetes-related complications:
1. Adults ages 55+ (especially males)
2. Black males and females
3. Adults with overweight/obesity
4. Adults in Kent and Sussex counties
5. Adults with prediabetes who have not participated in the National Diabetes Prevention Program (National DPP)
6. Adults with uncontrolled diabetes
7. Adults with diabetes and co-occurring conditions
8. Adults with diabetes who have not participated in Diabetes SelfManagement Education and Support (DSMES) .
Economic Impact
Prediabetes and diabetes cost Delaware $1.1 billion each year [3] – $818 million in direct medical expenses and $293 million in indirect costs On average, medical expenditures for a person with diabetes are 2.3 times higher than for a person without diabetes [3]. Prevention, early diagnosis, and management can prevent and reduce the costly outcomes associated with diabetes
The Impact of Diabetes in Delaware, 2023 2 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
133
In FY22, Delaware Medicaid Managed Care Organizations (MCOs) directly reimbursed providers $49.0 million for diabetes -related care An additional $2.6 million was paid directly to providers via fee-for-service claims for diabetes-related care among Delaware Medicaid clients. Diabetes is the costliest clinical condition by episodes of care among GHIP members The FY22 total allowed amount for diabetes reached $85.3 million –an increase of almost $9 million compared to FY21. In FY22, costs related to diabetes episodes of care represented 5.0% of all GHIP net payments made on behalf of active employees and early retirees.
Delaware Diabetes Plan
DPH, DMMA, and SBO are guided by the Delaware Diabetes Plan, a framework for reducing the burden of diabetes among Delawareans. The Delaware Diabetes Plan aligns with Centers for Disease Control and Prevention (CDC) recommendations and addresses Healthy People 2030 objectives . DPH, DMMA, and SBO represent leading stakeholders within the Plan; the agencies work with each other and partner stakeholders to achieve four long-term goals:
1. Reduce the incidence of diabetes in Delaware
2. Increase the proportion of adults with diabetes who achieve diabetes control
3. Advance health equity among adults with diabetes and those at risk for the disease
4. Improve clinical processes and reduce health care costs.
The Delaware Diabetes Plan is a call to action for all Delawareans to work together to improve health outcomes through diabetes prevention , early diagnosis, and management.
Recommendations
The agencies recommend seven steps to continue reducing the burden of diabetes in Delaware. Recommendations are evidence-based and can be implemented using two parallel approaches: (1) widespread implementation to reach all Delawareans; and (2) targeted implementation to identified high-risk populations.
Recommendation 1: Continue to educate Delawareans about diabetes risk factors while encouraging healthy lifestyle behaviors.
Recommendation 2: Increase referrals to the nationally recognized, evidencebased National Diabetes Prevention Program (National DPP) for Delawareans at high risk for diabetes.
Recommendation 3: Increase referrals to DSMES programs for adults with diabetes.
The Impact of Diabetes in Delaware, 2023 3 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
134 Delaware Journal of Public Health - March 2024
Recommendation 4: Increase medication adherence among Delawareans with high blood pressure and/or high cholesterol
Recommendation 5: Increase the proportion of Delawareans with diabetes who follow the evidence-based CDC Diabetes Care Schedule.
Recommendation 6: Leverage electronic health record (EHR) capabilities to promote the adoption of organizational guidelines for the clinical care of patients with or at risk for diabetes.
Recommendation 7: Enhance care coordination to improve the clinical care of Delawareans with or at risk for diabetes, share resources, and reduce health care costs.
The Impact of Diabetes in Delaware, 2023 4 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
135
Chapter 1: Collaborating Agencies
The Impact of Diabetes in Delaware, 2023 is a collaboration between the Delaware Department of Health and Social Services (DHSS), Division of Public Health (DPH) and Division of Medicaid and Medical Assistance (DMMA), and the Delaware Department of Human Resources, Statewide Benefits Office (SBO)
DPH oversees diabetes activities and programming statewide DMMA provides medical assistance to Delaware Medicaid members through a variety of programs; most activities related to diabetes are administered through contracted Medicaid Managed Care Organizations (MCOs). SBO administers health benefits to State Group Health Insurance Plan (GHIP) members and works directly wit h health plan vendors to provide resources tailored to meet the needs of members with diabetes and those at risk for the disease. The agencies work together and with partner stakeholders to achieve the four long-term goals outlined in the Delaware Diabete s Plan.
Division of Public Health (DPH)
• Target Population: All Delawareans, an estimated 1,013,736 individuals [4]
Diabetes prevention and treatment activities are carried out by the DPH Diabetes and Heart Disease Prevention and Control Program (DHDPCP) DHDPCP is funded by a cooperative agreement with the Centers for Disease Control and Prevention (CDC) with support from the Delaware Health Fund
DHDPCP is tasked with decreasing the emotional, physical, and financial burden of diabetes among all Delawareans DHDPCP programs target Delaware’s most vulnerable populations, including minorities, people of lower socioeconomic status (SES), older adults, people with disabilities, and those with diabetes risk factors Special diabetes resources are in place for those who do not meet health insurance qualifiers and/or whose insurance excludes needed diabetes services and supplies
DHDPCP performs the following duties:
o Collects, analyzes, and publicizes health surveillance data.
o Uses evidence-based strategies to reduce the prevalence of prediabetes, diabetes, and hypertension .
o Promotes health equity among Delawareans.
o Fosters partnerships between clinical and community resources.
o Coordinates public and private joint initiatives related to diabetes and heart disease.
o Supports health information technology (HIT) to improve clinical quality.
The Impact of Diabetes in Delaware, 2023 5 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
136 Delaware Journal of Public Health - March 2024
Division of Medicaid & Medical Assistance (DMMA)
• Target Population: Approximately 300,000 eligible Delawareans whose incomes are insufficient to meet the costs of necessary medical services
The Division of Medicaid & Medical Assistance (DMMA) was established within DHSS in 2005 to improve health outcomes and ensure that Delaware’s most vulnerable populations receive high-quality medical services in a cost-effective manner. DMMA oversees multiple programs under the umbrella category of the Delaware Medical Assistance Plan (DMAP) Medicaid is the largest DMAP program and provides medical assistance to eligible, low-income individuals and families whose incomes are insufficient to meet the costs of necessary medical services Medicaid is jointly funded by states and the federal government . At least 50% of states’ to tal Medicaid funds come from the Federal Medical Assistance Percentages (FMAP) , and states are responsible for generating the remaining funds through a combination of general revenues, taxes, local governments, and other sources .
Approximately 90% of Medicaid clients are enrolled in the Diamond State Health Plan (DSHP), Delaware’s Medicaid MCO DMMA contracts with AmeriHealth Caritas Delaware, Delaware First Health, and Highmark Health Options to provide managed care services to clients covered through the DSHP.1
Statewide Benefits Office (SBO)
• Target Population: More than 129,000 individuals are covered under the State Group Health Insurance Plan (GHIP)
The Statewide Benefits Office (SBO), Department of Human Resources (DHR) is responsible for the strategic planning, daily administration, and financial management of all health and related benefit programs available to members covered by the State Group Health Insurance Plan (GHIP). GHIP members include active employees, retirees and dependents affiliated with state agencies, school districts, charter schools, higher education, and participating non -state groups. SBO staff administer health, prescription, wellness/disease management, vision, dental, and other benefits to more than 129,000 GHIP members.
1 Delaware First Health began providing services to enrolled members in January 2023; data pertaining to this MCO will be included in the 2025 biennial report.
The Impact of Diabetes in Delaware, 2023 6 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
137
Chapter 2: Diabetes in Delaware
What is Diabetes?
Diabetes is a chronic disease that affects how your body uses food for energy . Left untreated, diabetes can lead to a host of poor health outcomes including heart disease, stroke, kidney disease, lower limb amputations, blindness, and death . The good news is that diabetes is largely preventable through basic prevention steps like eating a healthy diet, getting regular physical activity, and losing a small amount of extra weight
The American Diabetes Association (ADA) recommends at least 150 minutes per week of moderate-intensity physical activity and weight loss of 5%-7% to prevent or delay the onset of diabetes in populations at high risk for the disease [1]. Those who develop diabetes can effectively manage the condition through healthy lifestyle behaviors and a medication regimen to control blood glucose levels.
Type 2 diabetes is the most common form of diabetes , accounting for 90-95% of all diabetes diagnoses. Prediabetes, a condition characterized by higher than normal blood sugar levels that do not meet the threshold for type 2 diabetes, is also a recognized medical condition. Type 1 diabetes and gestational diabetes are diagnosed less frequently than type 2 diabetes About 5%-10% of people with diabetes have type 1 diabetes [5]. Gestational diabetes is a type of diabetes that can develop during pregnancy in women who do not already have diabetes Gestational diabetes usually goes away after giving birth but increases the risk for type 2 diabetes later in life [6].
Diabetes Prevalence
In 2021, 12.0% of Delaware adults reported they had been diagnosed with diabetes This means that more than 95,000 Delaware adults know that they have diabetes 2 [7]
Another 12.6% of Delaware adults report being told they have prediabetes, a condition that places them at greater risk for developing diabetes In total, 24.6% of Delaware adults have either prediabetes or diabetes. After increasing throughout the early 2000s and peaking in 2019, Delaware’s diabetes prevalence began declining From 2019 to 2021, Delaware’s diabetes prevalence rate fell from 12.8% to 12.0% (Figure 1).
2 This prevalence does not include gestational diabetes. Although the BRFS survey question does not distinguish between type 1 and type 2 diabetes, the National Diabetes Information Clearinghouse estimates that between 90% to 95% of people with diabetes ha ve type 2.
The Impact of Diabetes in Delaware, 2023 7 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
138 Delaware Journal of Public Health - March 2024

Source: Delaware Department of Health and Social Services, Division of Public Health, Behavioral Risk Factor Survey, 2003-2021
Diabetes prevalence varies among different groups of people . Some differences in diabetes prevalence estimates reach a threshold of statistical significance A statistically significant difference is one that is not attributed to chance . Other differences in diabetes prevalence do not reach the threshold of statistical significance . If a difference is not statistically significant, cha nce cannot be ruled out as an explanatory factor for the difference.3
In 2021, the diabetes prevalence rate among Delaware males (12.2%) was not significantly different than the rate among Delaware females (11.7%) (Table 1) In 2021, 15.0% of non-Hispanic Black adults and 11.4% of non-Hispanic White adults had been diagnosed with diabetes . While the difference in diabetes prevalence between non-Hispanic Black and non-Hispanic White Delaware adults was not statistically significant in 2021, the trend has shown that non-Hispanic Black Delaware adults
3 Significant differences between prevalence estimates were identified by non-overlapping 95% confidence intervals.
The Impact of Diabetes in Delaware, 2023 8 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Figure 1. Adult Diabetes Prevalence as a Percentage of the Total Population Age 18 and Older, Delaware, 2003-2021
139
consistently have a higher diabetes prevalence compared to non -Hispanic White Delaware adults. In some years over the past decade, the difference has been statistically significant, and reaching statistical significance appears to be a factor of sampling.
Diabetes becomes more prevalent with age . Among Delawareans ages 45-54, a significantly lower percentage (9.6%) report having diabetes compared to those ages 55-64 (18.2%) and those ages 65 and older (23.4%). In 2021, diabetes prevalence in Sussex County (13.2%) was higher than in Kent (11.4%) and New Castle (11.6%) counties.
There is no significant difference in diabetes prevalence between males and females.
is no significant difference in diabetes prevalence between Black and White adults.
Diabetes prevalence for adults ages 55-64 and 65+ is significantly higher than for adults ages 18-44 and 4554.
Diabetes prevalence does not differ significantly by educational level.
Diabetes prevalence does not differ significantly by county of residence.
Note: Significant differences between prevalence estimates were identified by non -overlapping 95% confidence intervals. Source: Delaware Behavioral Risk Factor Survey (BRFS), 20 21
The Impact of Diabetes in Delaware, 2023 9 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Prevalence Statistical Significance Total, All Adults 12.0% Sex Male 12.2%
Table 1. Diabetes Prevalence by Demographic Characteristics, Delaware, 2021 Diabetes
Female 11.7% Race White 11.4%
Black 15.0% Age 18-44 3.1%
There
45-54 9.6% 55-64 18.2% 65+ 23.4% Education < High School 16.1%
High School or GED 12.8% Some Post-High School 11.4% College Graduate 10.6% County New Castle County 11.6%
Kent County 11.4% Sussex County 13.2%
140 Delaware Journal of Public Health - March 2024
In FY22, 14,903 Delaware Medicaid clients were living with type 2 diabetes; another 1,878 clients had been diagnosed with prediabetes.4 Among Medicaid clients with diabetes, 68.0% were age 51 or older. Females accounted for 57.4% of Medicaid clients with type 2 diabetes.
In FY22, 13,123 GHIP members had diabetes, reflecting a diabetes prevalence rate of 94.1 per 1,000 members or 9.4% (Table 2).5 Prevalence was highest among the Medicare retiree population, consistent with the fact that diabetes prevalence increases with age An additional 11,246 GHIP members had prediabetes in FY2 2, a prediabetes prevalence rate of 80.6 per 1,000 members or 8.1%.6 Prediabetes prevalence was highest among the active employee population, indicative that prediabetes status fluctuates over time
Note: Member groups overlap due to member movement during the year; frequencies do not sum to totals
Source: Delaware Department of Human Resources, Statewide Benefits Office, 2022
Diabetes Risk Factors
A person’s risk of developing diabetes increases if they have one or more risk factors . Some risk factors are non-modifiable, meaning they cannot be changed. Other risk factors are modifiable and can be reduced or eliminated through lifestyle changes
Table 3 summarizes non-modifiable and modifiable diabetes risk factors recognized by the CDC and the ADA
4 In FY22, 1,459 Delaware Medicaid clients were living with type 1 diabetes and 657 Delaware Medicaid clients had been diagnosed with gestational diabetes.
5 GHIP members were identified as having diabetes if they experienced a diabetes episode during FY22. A diabetes episode is a summary of care (i.e., a claims record) related to a condition or disease that includes inpatient, outpatient, and prescription drug treatment.
6 GHIP members were identified as having prediabetes if they did not have an indication of diabetes, but had been diagnosed with prediabetes, metabolic syndrome, or obesity.
The Impact of Diabetes in Delaware, 2023 10 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Prediabetes
Diabetes, Delaware, Fiscal Year 2022 Prediabetes Diabetes GHIP Member Group Number of Members Rate per 1,000 Members Number of Members Rate per 1,000 Members Active Employee 8,810 89.0 (8.9%) 5,167 52.2 (5.2%) Early Retiree 888 75.9 (7.6%) 1,213 103.7 (10.4%) Medicare Retiree 1,586 55.6 (5.6%) 6,155 215.6 (21.6%) Total 11,246 80.6 (8.1%) 13,123 94.1 (9.4%)
Table 2. Number and Rate (and Percentage) of Group Health Insurance Plan Members with
and
141
NonModifiable Diabetes Risk Factors [8]
Modifiable Diabetes Risk Factors [9]
Diabetes Risk Factor
• Have a parent, brother, or sister with type 2 diabetes
• Are 45 years or older
• Are a Black, Latino, American Indian, or Alaskan Native person Some Pacific Islanders and Asian American people are also at higher risk for diabetes.
• Have ever had gestational diabetes or previously given birth to a baby who weighed over 9 pounds
• Are overweight or obese
• Have prediabetes
• Have hypertension
• Have elevated cholesterol (lipid) levels
• Heavy alcohol intake
• Are a smoker
• Poor dietary intake
• Sedentary lifestyle
• Excessive stress
• Insufficient sleep
Source: Centers for Disease Control and Prevention, 2022; American Diabetes Association, 2021
The Impact of Diabetes in Delaware, 2023 11 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Table 3 Non-Modifiable and Modifiable Diabetes Risk Factors Risk Factor Category
142 Delaware Journal of Public Health - March 2024
Chapter 3: High-Risk Populations
Some groups have a higher diabetes prevalence rate, poorer diabetes control, or are more likely to experience diabetes complications. DPH, DMMA, and SBO identify eight groups of Delawareans at highest risk for diabetes and related complications (Table 4).
The eight high-risk populations are categorized by diabetes status: (a) adults at elevated risk for development of diabetes and (b) adults who have already been diagnosed with diabetes
Diabetes Status
Delaware
Adults at Elevated Risk for Diabetes
Delaware
Adults Already Diagnosed with Diabetes
High-Risk Population
1. Adults ages 55+ (especially males)
2. Black males and females
3. Adults with overweight/obesity
4. Adults in Kent and Sussex counties
5. Adults with prediabetes who have not participated in the National Diabetes Prevention Program (National DPP)
6. Adults with uncontrolled diabetes
7. Adults with diabetes and co-occurring conditions
8. Adults with diabetes who have not participated in Diabetes SelfManagement Education and Support (DSMES)
Source: Delaware Department of Health and Social Services, Division of Public Health and Division of Medicaid & Medical Assistance, and Delaware Department of Human Resources, Statewide Benefits Office , 2023
The eight populations at high risk of diabetes are:
1. Adults Ages 55+ (especially males)
Diabetes becomes more prevalent with age [10] In 2021, 3.1% of Delaware adults ages 18-44 had been diagnosed with diabetes, compared to 9.6% of Delaware adults ages 45-54 and 18.2% of Delaware adults ages 55-64 (Table 5) [2] Nearly one-quarter (23.4%) of Delaware adults ages 65 and older had been diagnosed with diabetes in 2021 [2]
Health surveillance data for active employee and early retiree GHIP members confirms the correlation between age and diabetes (Figure 2) In FY22, diabetes prevalence for active employee and early retiree GHIP members ages 40-49 was more than double the prevalence for those ages 30-39; this trend holds true for men and women Focusing
The Impact of Diabetes in Delaware, 2023 12 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Table 4. Identified Populations at High-Risk for Diabetes, Poor Diabetes Control, or Diabetes-Related Complications by Diabetes Status, Delaware, 2023
143
diabetes prevention and management efforts among adults approaching their 50s is key to reducing the number of Delawareans who develop diabetes or experience complications. Inequities in diabetes prevalence between male and female active employee and early retiree GHIP members suggest that additional outreach to males ages 55 and older may be an effective strategy to reduce their burden of diabetes.
Note: Significant differences between prevalence estimates were identified by non-overlapping 95% confidence intervals Source: Delaware Department of Health and Social Services, Division of Public Health, Behavioral Risk Factor Survey, 2021
The Impact of Diabetes in Delaware, 2023 13 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Age Group Diabetes Prevalence Statistical Significance 18-44 3.1% Diabetes prevalence
45-54 9.6% 55-64 18.2% 65+ 23.4%
Table 5. Adult Diabetes Prevalence by Age Group, Delaware, 2021
for adults ages 55-64 and ages 65+ is significantly higher than for adults ages 45-54.
144 Delaware Journal of Public Health - March 2024
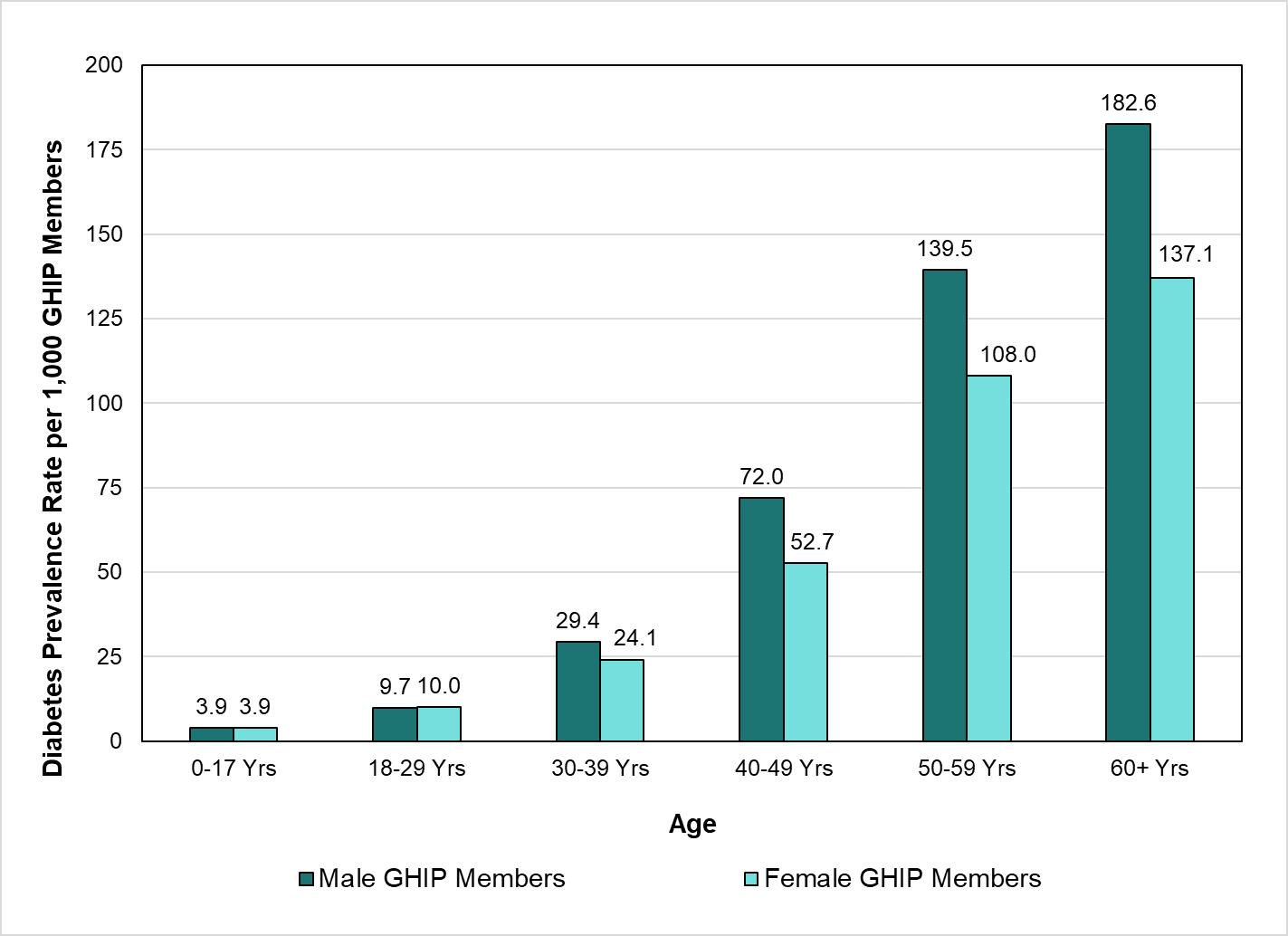
Note: Includes Active Employee and Early Retiree GHIP Members; Medicare retirees exc luded due to incomplete medical and prescription costs and utilization captured through available claims. Source: Delaware Department of Human Resources, Statewide Benefits Office, 20 22
2. Black Males and Females
In Delaware, Black males and females are more likely than White males and females to develop diabetes and die from the disease. While the difference in diabetes prevalence rates between non-Hispanic Black (15.0%) and non-Hispanic White (11.4%) Delaware adults was not statistically significant in 2021 [2], Black adults consistently have a higher diabetes prevalence compared to White adults.
Delaware’s five-year age-adjusted mortality rate (AAMR) for diabetes conveys how many people with diabetes die from the disease over a five-year period. Delaware’s overall diabetes AAMR has declined over time, indicating that a smaller proportion of people with diabetes are dying from the disease today compared to the past. While this is positive news, improvements in the diabetes AAMR have not been equal across all groups. From 2004-2008 to 2016-2020, Delaware’s five-year diabetes AAMR declined 44% for non-Hispanic Black females, 19% for non-Hispanic White females, and 13% for
The Impact of Diabetes in Delaware, 2023 14 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Figure 2. Diabetes Prevalence Rate by Age per 1,000 Active Employees and Early Retirees in the Group Health Insurance Plan (GHIP), State of Delaware, Fiscal Year 2022
145
non-Hispanic White males [11]. In contrast, the diabetes AAMR increased 5% for nonHispanic Black males.
Despite improvements in Delaware’s overall diabetes AAMR, Black males and females continue to die from diabetes at rates higher than White males and females. From 2016-2020, the five-year AAMR for diabetes was 34.5 deaths per 100,000 population for non-Hispanic Black Delawareans – a rate twice that of the AAMR for non-Hispanic White Delawareans (17.2 deaths per 100,000 population) [11]. From 2016-2020, the AAMR for non-Hispanic Black women in Delaware was 22.3 deaths per 100,000 population, a rate 62% higher than the AAMR for non-Hispanic White women in Delaware (13.8 deaths per 100,000 population ) [11]. Similarly, the 2016-2020 diabetes AAMR for non-Hispanic Black males in Delaware was 52.5 deaths per 100,000 population, a rate 144% higher than the diabetes AAMR for non-Hispanic White women in Delaware (21.5 deaths per 100,000 population) [11]
3. Adults with Overweight/Obesity
Overweight and obesity are major diabetes risk factors , and individuals affected by excess weight are more likely to develop diabetes compared to adults with normal weight. In 2021, 18.7% of Delaware adults living with obesity had been diagnosed with diabetes compared to 3.4% of adults who report ed normal weight [7] About 91% of Delaware adults with diagnosed diabetes were overweight or obese in 2021. Not only does obesity increase the likelihood of developing diabetes, but it also increases the likelihood of diabetes-related complications [12] A person who has both obesity and diabetes is at high risk for negative health outcomes like heart disease and stroke .
4. Adults in Kent and Sussex counties
Adults in Delaware’s central and southern counties are at higher risk for diabetes due to higher rates of diabetes risk factors. In Kent County, increased obesity prevalence increases the likelihood that adults will develop the disease. In 2020, 40% of Kent County residents were living with obesity compared to 32.2% of New Castle County residents and 33.3% of Sussex County residents. In Sussex County, the relatively large proportion of older adults increases the number of residents at risk for diabetes. In 2020, 26.4% of Sussex County adults were age 65 or older compared to 16.4% of Kent County adults and 15.9% of New Castle County adults [4]
The Impact of Diabetes in Delaware, 2023 15 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
146 Delaware Journal of Public Health - March 2024
5. Adults with Prediabetes who Have Not Participated in the National Diabetes Prevention Program (National DPP)
The National DPP is a structured, evidence-based lifestyle and health behavior change program developed by the CDC and endorsed by the Centers for Medicare and Medicaid Services (CMS). The National DPP works to prevent or delay type 2 diabetes among at-risk adults. Over the course of a year, National DPP participants work to reduce body weight by 5%-7% and gradually increase physical activity to at least 150 minutes per week.
The National DPP is a cost-effective way to delay or prevent the progression from prediabetes to diabetes Adults who participate in the National DPP have a diabetes incidence rate lower than adults who receive diabetes medication alone [13]. Impressively, the National DPP prevents the onset of diabetes by an average of nearly four years [13]
In Delaware, adults eligible for the National DPP are referred to the program through a health care provider or community-based organization. The National DPP is a covered benefit for Medicaid members and GHIP members at no additional cost Despite evidence that the National DPP is a cost-effective and proven method to prevent or delay diabetes, participation among high-risk Delawareans is low.
6. Adults with Uncontrolled Diabetes
For those diagnosed with the disease, achieving diabetes control is possible with daily effort. The hemoglobin A1C (A1C) blood test is the gold standard for gauging diabetes control. The A1C reflects average blood glucose level for the past two to three months and test results are reported as percentages. A n A1C value below 5.7% is considered normal, whereas A1C values from 5.7%-6.4% indicate prediabetes An A1C value above 8% indicates that a person’s diabetes is uncontrolled , placing them at higher risk for diabetes-related complications [14]
DMMA monitors Healthcare Effectiveness Data and Information Set (HEDIS) measures to learn more about the proportion of Medicaid-enrolled members with diabetes who have achieved diabetes control.7 In FY22, 52.0% of Medicaid members with diabetes had an optimal A1C level of less than 8% Nearly 40% of Medicaid members with diabetes had an A1C greater than 9%.
The Impact of Diabetes in Delaware, 2023 16 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Table 6 summarizes the CDC Diabetes Care Schedule recommended for people who have been diagnosed with diabetes [15]. Adults with diabetes who do not follow
147
7 Healthcare Effectiveness Data and Information Set (HEDIS) measures are used by more than 90% of U.S. health plans to measure clinical care quality and service [26].
recommended Diabetes Care tasks are at greater risk for uncontrolled diabetes and related complications
Care Schedule,
Diabetes Care Task Recommended Frequency
• Check blood glucose levels
• Self-administered foot check
• Proper medication use
• Moderate physical activity
• Healthy eating
• Hemoglobin A1C (A1C) test
• Daily (at least once per day)
• Daily
• Daily
• Daily (at least 150 minutes per week)
• Daily
• Every 3 months for those having trouble achieving blood glucose control goals
• Every 6 months for those meeting blood glucose goals
• Every 3 months for those having trouble achieving blood glucose control goals
• Doctor visit
• Dental exam
• Flu shot
• Kidney function test
• Cholesterol test
• Dilated eye exam
• Complete foot check by a medical professional
• Pneumonia vaccine
• Hepatitis B vaccine
• Mental health screening and support
• Every 6 months for those meeting blood glucose goals
• Every 6 months
• Once a year
• Once a year
• Once a year
• Once a year
• Once a year
• Just once
• Just once
• As needed
Source: Centers for Disease Control and Prevention, 2022.
The Impact of Diabetes in Delaware, 2023 17 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Table 6. Centers for Disease Control and Prevention Diabetes
2022
148 Delaware Journal of Public Health - March 2024
Among Delaware adults with diabetes, compliance with the recommended CDC Diabetes Care Schedule varies by the specific care task (Figure 3) In 2021, 89.9% of Delaware adults with diabetes reported receiving an A1C test at least once during the past year [2]. In 2021, 75.4% of adults with diabetes reported receiving a complete foot check by a health care professional in the past year; 68.2% reported visiting their doctor at least two times in the past year; and 66.6% reported receiving a dilated eye exam in the past year [2]
In 2021, just 60.9% of adults with diabetes reported checking their blood glucose levels at least once a day [2] This finding is particularly concerning because regular blood sugar monitoring is the most important tool for managing diabetes [16]. Daily monitoring allows a person with diabetes to get real-time feedback about what causes their blood glucose numbers to go up and down .

The Impact of Diabetes in Delaware, 2023 18 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Figure 3 Percentage of Self-Reported Compliance with Diabetes Care Schedule Tasks Among Adults with Diabetes, Delaware, 2021
149
Source: Delaware Department of Health and Social Services, Division of Public Health, Behavioral Risk Factor Survey, 2021
7. Adults with Diabetes and Co-Occurring Conditions
Comorbid conditions reduce the likelihood of achieving diabetes control and can complicate diabetes treatment. In FY22, 78.7% of active employee and early retiree GHIP members with diabetes had at least one top comorbidity: congestive heart failure, coronary artery disease, chronic obstructive pulmonary disease (COPD), hypertension, osteoarthritis, HIV/AIDS, rheumatoid arthritis, obesity, and low back disorder (Figure 4)
Hypertension and high cholesterol are independent risk factors for developing diabetes and for experiencing diabetes complications In FY22, 73% of active employee and early retiree GHIP members with diabetes complied with statin medication prescribed to treat high cholesterol, and 67% percent of Medicaid members with diabetes had blood pressure control (defined as less than 140/90 mm Hg). Improving medication management of hypertension and high cholesterol is an important strategy to reduce the number of adults who develop diabetes and experience related complications.

Note: Includes Active Employee and Early Retiree GHIP Members; Medicare retirees excluded due to incomplete medical and prescription costs and utilization captured through available claims. Source: Delaware Department of Human Resources, Statewide Benefits Office, 2022
The Impact of Diabetes in Delaware, 2023 19 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
Figure 4. Number of Top 10 Comorbidities Among Group Health Insurance Plan (GHIP) Members with Diabetes, Fiscal Year 2021
150 Delaware Journal of Public Health - March 2024
8. Adults with Diabetes Who Have Not Participated in Diabetes SelfManagement Education and Support Services
Diabetes Self-Management Education and Support (DSMES) is an evidence-based program to help people with diabetes develop the skills they need to manage their condition. Through DSMES, people with diabetes learn the skills needed to check their blood sugar regularly, eat healthy foods, take medications as prescribed, and build physical activity into their daily routines DSMES is tailored to an individual’s specific needs, goals, and life circumstances. Classes are facilitated by Certified Diabetes Care and Education Specialists (CDCES), and program content incorporates behavioral goal setting, theoretically grounded empowerment models, shared decision -making, and ongoing support [17] Delaware adults who are eligible for DSMES are referred to an outpatient or hospital affiliated DSMES site. Classes are offered in person or virtually to meet participants’ needs.
Despite being a cost-effective strategy to improving diabetes management and outcomes, DSMES participation rates are low compared to other diabetes management recommendations for achieving and maintaining diabetes control . In 2021, half (51%) of all Delaware adults with diabetes had taken a course or class in how to manage the condition [2].
To read the full report, please visit https://dhss.delaware.gov/dhss/dph/dpc/files/diabetesburdenreports23.pdf.
The Impact of Diabetes in Delaware, 2023 20 Delaware Department of Health and Social Services, Division of Public Health, Diabetes and Heart Disease Prevention and Control Program; Division of Medicaid & Medical Assistance; and Delaware Department of Human Resources, Statewide Benefits Office June 2023
151
LEXICON
A Priori
Relating to or denoting reasoning or knowledge which proceeds from theoretical deduction rather than from observation or experience.
Adenotonsillectomy
An operation to remove both the adenoids and the tonsils.
Asthma
A chronic, long term condition that a ects the airways in the lungs, in which a person’s airways can become in amed, narrow, and swell, produce extra mucus, and can lead to di culty breathing.
Body Mass Index (BMI)
A measure of body fat based on weight and height that applies to adult men and women.
Burnout
Physical or mental collapse caused by overwork or stress.
Chronic Illness
A health condition or disease that is persistent, or otherwise long-lasting in its e ects; o en applied when a condition or disease lasts longer than three months.
Compassion Fatigue
Indi erence to charitable appeals on behalf of those who are su ering, experienced as a result of the frequency or number of such appeals.
Craniofacial
Relating to the head, skull, jaws and the face.
Dermatological
Of or relating to the skin.
Diabetes
A disease in which the body’s ability to produce or respond to the hormone insulin is impaired, resulting in abnormal metabolism of carbohydrates and elevated levels of glucose in the blood and urine.
Disparities
Lack of equality or equity; inequality; di erence.
Epidemiology
Epidemiology is the study and analysis of the distribution, patterns and determinants of health and disease conditions in a de ned population.
Hypertension
High blood pressure. A condition in which the force of the blood against the artery walls is too high. Usually hypertension is de ned as blood pressure above 140/90, and is considered severe if the pressure is above 180/120.
Incidence
In epidemiology, incidence is a measure of the probability of occurrence of a given medical condition in a population within a speci ed period of time. Although sometimes loosely expressed simply as the number of new cases during some time period, it is better expressed as a proportion or a rate with a denominator.
Intellectual Disability
A disability that a ects the acquisition of knowledge and skills, in particular any of various neurodevelopmental conditions a ecting intellectual processes, educational attainment, and the acquisition of skills needed for independent living and social functioning.
Mandibular
Relating to the lower jaw.
Malocclusion
Imperfect positioning of the teeth when the jaws are closed.
152 Delaware Journal of Public Health - March 2024
LEXICON
Morbidity
Refers to having a disease or a symptom of disease, or to the amount of disease within a population. Morbidity also refers to medical problems caused by a treatment.
Mortality
Death, especially on a large scale.
Mitigation
e action of reducing the severity, seriousness, or painfulness of something.
Myofunctional Therapy
Myofunctional therapy is an exercise training program for the muscles around your face, mouth, and tongue. ese exercises are designed to improve issues with talking, eating, or breathing.
Neurocognitive
Relating to the neural processes and structures involved in thinking.
Obesity
A disorder that involves having too much body fat, which increases the risk of health problems. A disorder that involves having too much body fat, usually a body mass index of 30 or greater. It increases the risk of serious health problems.
Obstructive Sleep Apnea Syndrome
Intermittent air ow blockage during sleep.
Prevalence
e proportion of a particular population found to be a ected by a medical condition at a speci c time.
Prevention
Interventions aimed at reducing risks or threats to health. Includes primary prevention—intervening before health e ects occur; secondary prevention—screening to identify diseases at the earliest and reduce the impact of the disease or injury; and tertiary prevention—managing the long-term impacts of an ongoing illness or injury with lasting e ects.
Psychotherapy
Also called talk therapy. Refers to a variety of treatments that aim to help a person identify and change troubling emotions, thoughts, and behaviors
Qualitative Research
Qualitative research is a type of research that aims to gather and analyze non-numerical data in order to gain an understanding of individuals’ social reality, including understanding their attitudes, beliefs, and motivation.
Quantitative Research
Quantitative research is a research strategy that focuses on measuring the collection and analysis of data. It is formed from a deductive approach where emphasis is placed on the testing of theory, shaped by empiricist and positivist philosophies.
Retruded
When the lower jaw (mandible) is set further back from the upper jaw.
Risk Factors
Risk factors are characteristics at the biological, psychological, family, community, or cultural level that precede and are associated with a higher likelihood of negative outcomes.
Social Determinants of Health
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that a ect a wide range of health, functioning, and quality-of-life outcomes and risks.
Socioeconomic
e interaction of social and economic factors.
153
RESOURCES
National Resources
American Community Survey:
https://www.census.gov/programs-surveys/acs
American Heart Association: https://heart.org
American Lung Association: https://action.lung.org
American Stroke Association:
https://www.stroke.org
Behavioral Risk Factor Surveillance System:
https://www.cdc.gov/brfss/index.html
Black Mothers in Power:
https://www.blackmothersinpower.org/
Doulas of North America:
https://thechildbirthprofession.com/tag/doulas-of-north-america/
Food Attitudes and Beliefs Survey:
https://cancercontrol.cancer.gov/brp/hbrb/food-attitudes-and-behaviors
Health Information National Trends Survey: https://hints.cancer.gov/
National Center for Chronic Disease Prevention and Health Promotion:
https://www.cdc.gov/chronicdisease/index.htm
National Diabetes Prevention Program:
https://www.cdc.gov/diabetes/prevention/index.html
Physical Activity Guidelines for Americans:
https://health.gov/our-work/nutrition-physical-activity/physical-activity-guidelines
154 Delaware Journal of Public Health - March 2024
RESOURCES
Delaware Resources
Community Health Worker:
https://chwadelaware.org/
Delaware Bureau of Chronic Disease Prevention: https://dhss.delaware.gov/dph/dpc/bcd.html
Delaware Chronic Disease Coalition: https://dechronicdiseasecoalition.org/
Delaware Healthy Mother and Infant Consortium: https://dhss.delaware.gov/dhss/dph/chca/imdhmichome.html
Delaware Physical Activity Nutrition Obesity Prevention Program: https://dhss.delaware.gov/dph/dpc/panohome.html
Healthy Women, Healthy Babies:
https://dethrives.com/programs/healthy-women-healthy-babies
University of Delaware Graduate Programs:
https://www.udel.edu/academics/colleges/grad/prospective-students/programs/
Wilmington University Courses:
https://www.wilmu.edu/programs/index.aspx
155

The Nation's Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 American Public Health Association Start or Advance Your Health Care Career . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 Wilmington University The DPH Bulletin - February 2024 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20 Delaware Division of Public Health Community Health Worker Training Program . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25 chwCORE chwCORE Training Program . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 chwCORE The DPH Bulletin - March 2024 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 Delaware Division of Public Health The Burden of Diabetes in Delaware . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43 American Diabetes Association Field Placements - Public Health Projects . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60 Mid-Atlantic Regional 2022 DHSA Research Competition Call for Abstracts . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 84 Delaware Health Science Alliance DJPH 94th Annual Meeting . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 111 Delaware Journal of Public Health Spring 2024 Delaware Mini Medical School . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 115 Delaware Mini Medical School 28th Annual Delaware Healthcare Forum . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 121 Delaware Healthcare Association We Are All Public Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 157 National Public Health Week Submission Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 158 Delaware Journal of Public Health 156 Delaware Journal of Public Health - March 2024
Index of Advertisers
157
Public Health
Delaware Journal of Submission Guidelines
updated March, 2024
About the Journal
Established in 2015, The Delaware Journal of Public Health is a peer-reviewed electronic publication created by the Delaware Academy of Medicine/Delaware Public Health Association. The publication acts as a repository of news for the medical, dental, and public health communities, and is comprised of upcoming event announcements, past conference synopses, local resources, peer-reviewed content ranging from manuscripts and research papers to opinion editorials and personal interest pieces, relating to the public health sector. Each issue is largely devoted to an overarching theme or current issue in public health.
The content in the DJPH is informed by the interest of our readers and contributors. If you have an event coming up, would like to contribute an Op-Ed, would like to share a job posting, or have a topic in public health you would like to see covered in an upcoming issue, please let us know.
If you are interested in submitting an article to the Delaware Journal of Public Health, or have any additional inquiries regarding the publication, please contact the managing editor at managingeditor@djph.org, or the publisher at ksmith@delamed.org.
Information for Authors
Submission Requirements
The DJPH accepts a wide variety of submission formats, including brief essays, opinion editorials pieces, research articles and findings, analytic essays, news pieces, historical pieces, images, advertisements pertaining to relevant, upcoming public health events, and presentation reviews. Additional types of submission not previously mentioned may be eligible, please contact a staff member for more information.
The initial submission should be clean and complete, without edits or markups, and contain both the title and author(s) full name(s). Submissions should be 1.5 or double spaced with a font size of 12. Once completed, articles should be submitted via the submission page at https://djph.org/submissions/submit-an-article/ Graphics, images, info-graphics, tables, and charts are welcome and encouraged to be included in articles. Please ensure that all pieces
are in their final format, and all edits and track changes have been implemented prior to submission. To view additional information for online submission requirements, please refer to the DJPH website: https://djph.org/submissions/submit-an-article/
Trial registration information is required for all clinical trials and must be included in the final article and/or abstract.
Abstracts
Authors must submit a structured or unstructured abstract along with their article. Abstracts will have a maximum of 200 words, including headings. Structured abstracts should employ 4-5 headings, and may include Objectives, Methods, Results, and Conclusions. A fifth heading, Policy Implications, may be used if relevant to the article. All abstracts should provide the date(s) and location(s) of the study if applicable, as well as any trial registration information.
158 Delaware Journal of Public Health - March 2024
Submission Length
While there is no prescribed word length, full articles will generally be in the 2,500-4,000word range, and editorials or brief reports will be in the 1,500-2,500-word range. If there are any questions regarding the length of a submission or APA guidelines, please contact a staff member.
Copyright
The journal and its content is copyrighted by the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA). The contents are licensed under Creative Commons License – CC BY-NC-ND (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Images are NOT covered under the Creative Commons license and are the property of the original photographer or company who supplied the image.
Opinions expressed by authors of articles summarized, quoted, or published in full within the DJPH represent only the opinions of those authors and do not necessarily reflect the official policy of the Academy/DPHA, the DJPH, or the institution with which the authors are affiliated.
Con icts of Interest
Any conflicts of interest, including political, financial, personal, or academic conflicts, must be declared prior to the submission of the article, or in conjunction with a submission. Conflicts of interest are any competing interests that may leave readers feeling misled or deceived, and/or alter their perception of subject matter. Declared conflicts of interest will be published alongside articles in the final publication.
Nondiscriminatory Language
Use of nondiscriminatory language is required in all DJPH submissions. The DJPH reserves the right to reject any submission found to be using sexist, racist, or heterosexist language, as well as unethical or defamatory statements.

159
e D
of
nonpr
t
d in 1930. Our mission is to enhance the well being of our communit y
h medical e
an
the promotion
medical
and symposia
the 141 st
l
of the American
He alth A ssociation (AHPA) hel d in B oston, MA in November, 2
At this meeting,
D
aware
of
officially on November 5, 2013 by action of the A PH A Governing Council . e Del aware Academy of Me dicine, who’s
“to
well-being of o ur communit y
education and the promotion of public health,” is honored to take on t his responsibility in the First State
Academy of Medicine / DPHA www.dela med.org | www.djph.org Follow Us: P.O. Box 89 Historic New Castle, DE 19720 ISSN 2639-6378
el aware Academy
Medicine is a private ,
ofi
organization founde
throug
ducation
d
of public health. Our educational initiatives span the spect rum f rom consumer health education tocontinuing
education conferences
e Del aware Public Health A ssociation was officially rebor n at
Annua
Meeting
Public
013.
af filiation of the DPH A was t ransferred to the
el
Academy
Medicine
mission statement is
promote the
through
Delaware




 Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
 Katherine Smith, M.D., M.P.H. Publisher, Delaware Journal of Public Health
Katherine Smith, M.D., M.P.H. Publisher, Delaware Journal of Public Health



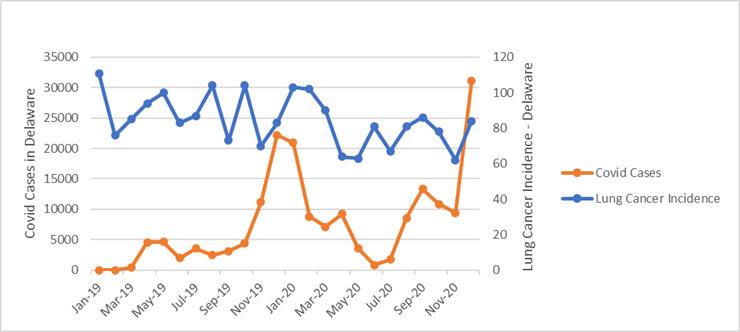

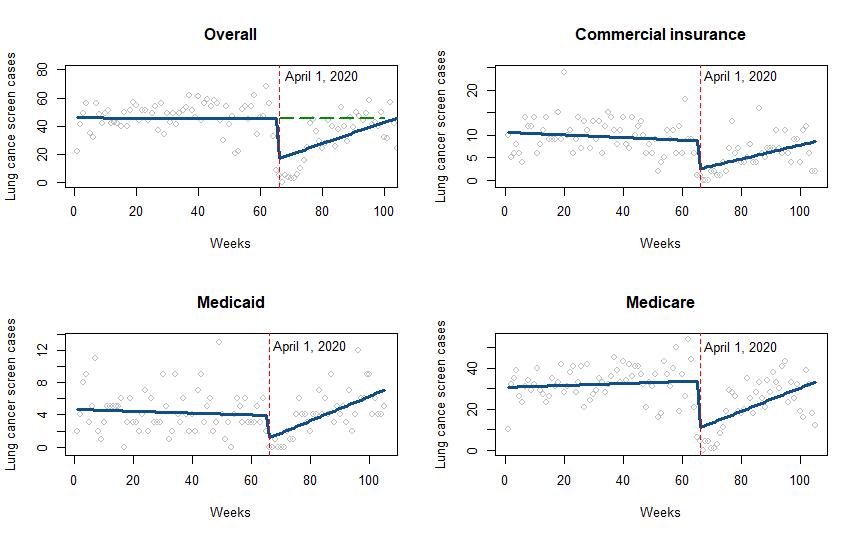
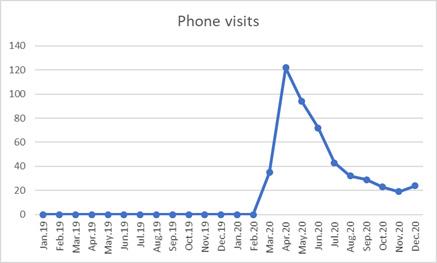
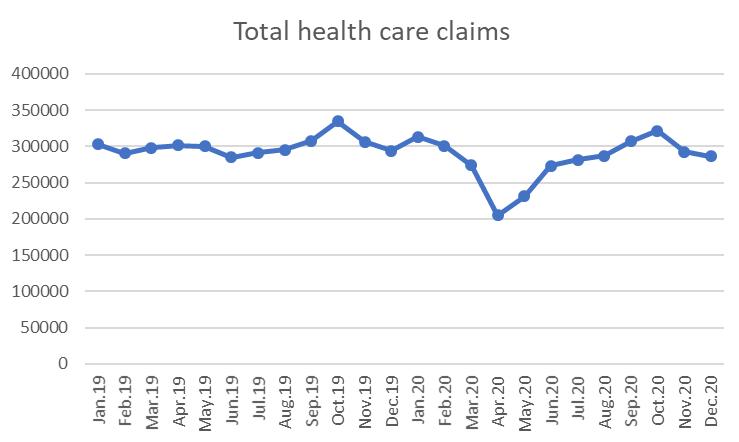

















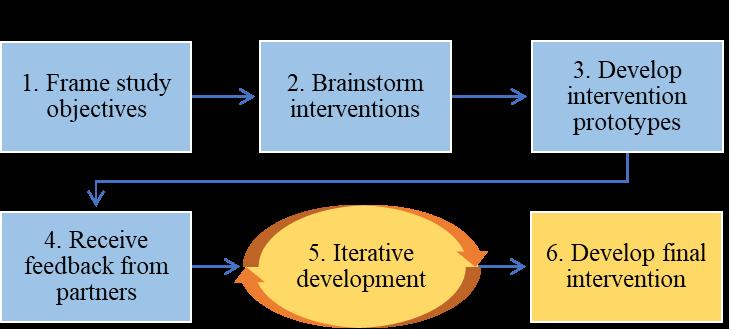













































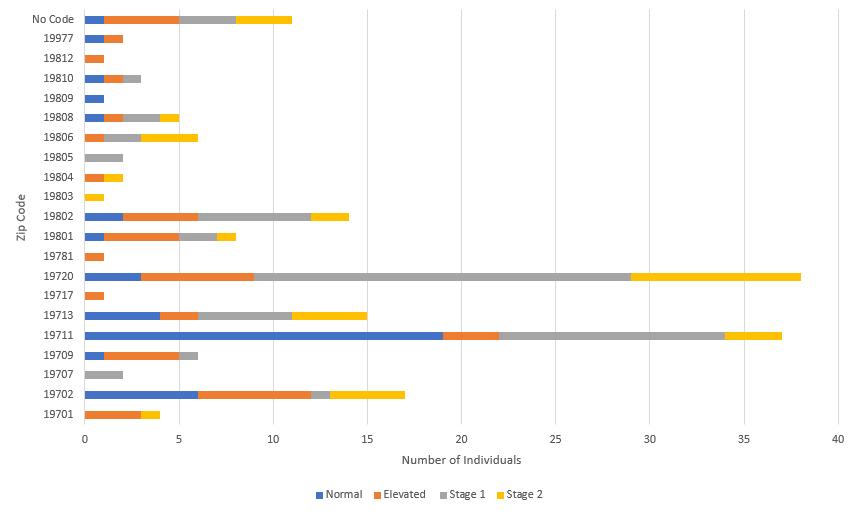







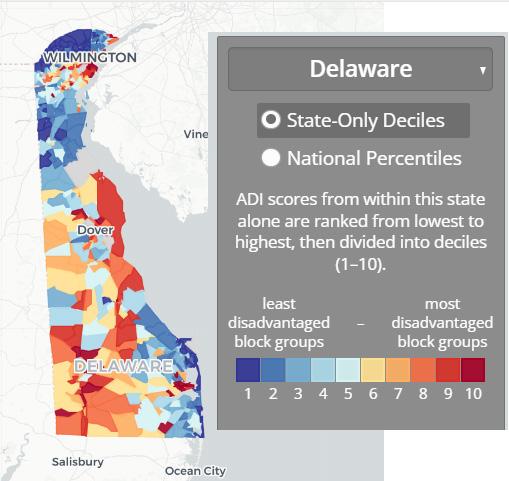
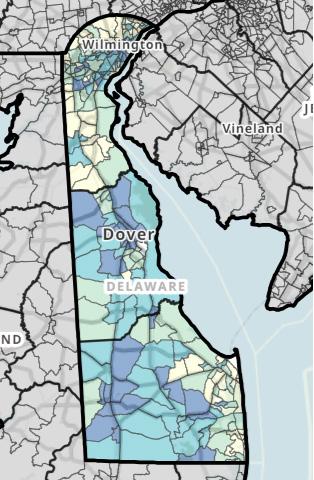




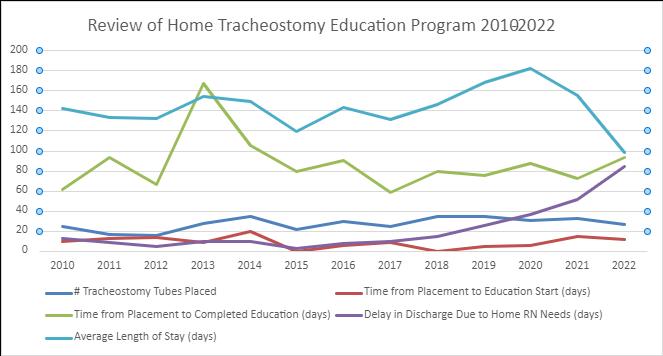








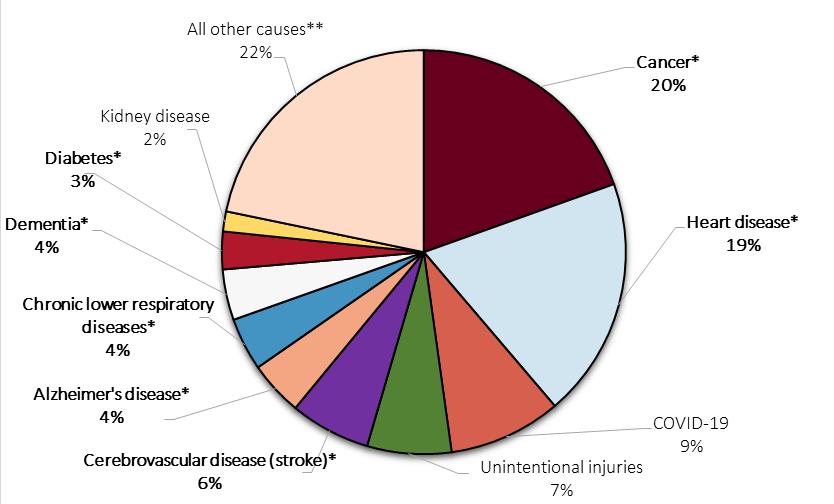 Figure 1. Percentage of Leading Causes of Deaths, by Cause of Death, Delaware, 202011
Figure 1. Percentage of Leading Causes of Deaths, by Cause of Death, Delaware, 202011