DEPARTMENT OF MEDICINE
PHILANTHROPY
Donor’s generosity helps other patients through their healthcare journeys.
RESEARCH
Food as Medicine
Dartmouth Health and Geisel School of Medicine take unique approach to treating obesity

EDUCATION
Researcher finds many factors influence women in choosing cardiology fellowship programs.
Faculty and residents practice managing bias from patients.
Center DEPARTMENT OF MEDICINE
Dartmouth Hitchcock Medical
Fall 2022
PHOTO BY: ROB STRONG
page 6
page
3
page 4
page 8
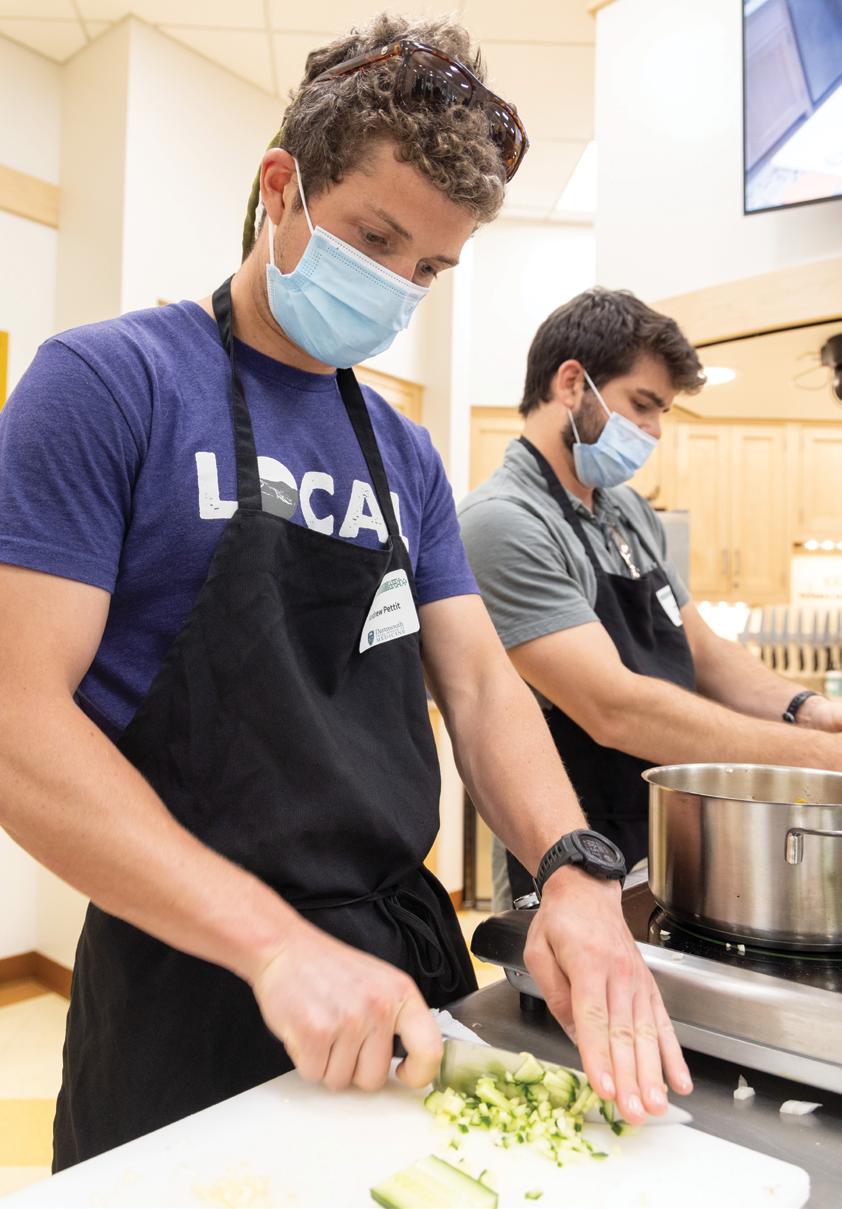
Auden McClure, MD (right), and Rima Itani Al-Nimr, MS, RDN, LD, lead medical students through the preparation of a healthful meal.
A Message from Our Chair
I am again delighted to share our latest newsletter highlighting areas of research, teaching, patient care, and culture in the Department of Medicine. I hope you have enjoyed our previous issues, which are archived at d-h.org/medicine. Each newsletter shares the clinical and scholarly activities of our faculty and trainees and features various endeavors, which, viewed in aggregate, will show you the exciting journey of our department.
In this issue, we show you the multifaceted activities of the Weight and Wellness Center. These include clinical pathways for children and adults, numerous educational offerings from its Culinary Medicine Program (with curricular teaching for patients, families and Geisel medical students), and active research engagement, including working with the national Teaching Kitchen Collaborative. Drs. Auden McClure, Sarah Finn, Jen Meijer and Diane GilbertDiamond, along with Rima Itani Al-Nimr, director of Geisel’s Nutrition in Medical Education Longitudinal Curriculum, illuminate the areas of clinical care, research and education in the important area of obesity medicine.
In a timely piece on uncovering the reasons that women trainees choose particular cardiovascular fellowship training programs, Dr. Kerrilynn Hennessey shares her research on the impact of leadership and of a program’s culture on decision-making at this transitional time for residents.
The work of Drs. Kelly Kieffer and Ellen Eisenberg is detailed in a story on workshops developed for residents and attendings to learn how to appropriately respond to biased patients who create hurtful situations for learners. Advance preparation gives the healthcare team confidence in handling these stressful events to ensure learners have an inclusive environment in which to care for their patients.
The invaluable role of a patient navigator to help individuals move through the complex maze of processes in the healthcare system is highlighted in the story of generous philanthropy that made a new position possible in the Section of Gastroenterology and Hepatology. Section chief Dr. Corey Siegel, patient navigator Tyler Dillehay, and Dorothy
Heinrichs, director of Patient and Family Giving, provide perspectives on this inaugural role and the power of philanthropy to underwrite dreams that improve the lives of others while bringing joy to those making the gift.
In this issue, I also want to announce my decision to step down next summer from the position of chair of our Medicine department as part of my transition to a part-time schedule. I will have completed 40 years of full-time service to our institutions, 12 as chair of Medicine, 15 as section chief of Gastroenterology and Hepatology before that, and so many other rewarding roles that I have been fortunate to have over the years. A national search for my replacement will commence soon. Perhaps you or someone you know may be interested in becoming a candidate for this leadership position. Please let our recruiter, Juliann Hamblin, know of potential candidates. Juli can be reached at Juliann.Hamblin@hitchcock.org or (603) 653-0430. Meanwhile, we have much to finish before the end of my tenure, and I am so proud of the robust scholarship and dedicated clinical care provided by our faculty and staff. Thank you for all you are doing!
We are excited to share our stories with you, and we enjoy hearing your stories as well. Write us at D-H.Alumni.Relations@hitchcock.org . If you are interested in learning more about opportunities to engage with and support our departmental activities, please contact Megan Dodge in the Medical & Healthcare Advancement Office at Megan.Dodge@hitchcock.org
Richard Rothstein, MD, HS’85 Chair, Department of Medicine
2
dartgo.org/deptofmed
Easing the Burden of Disease
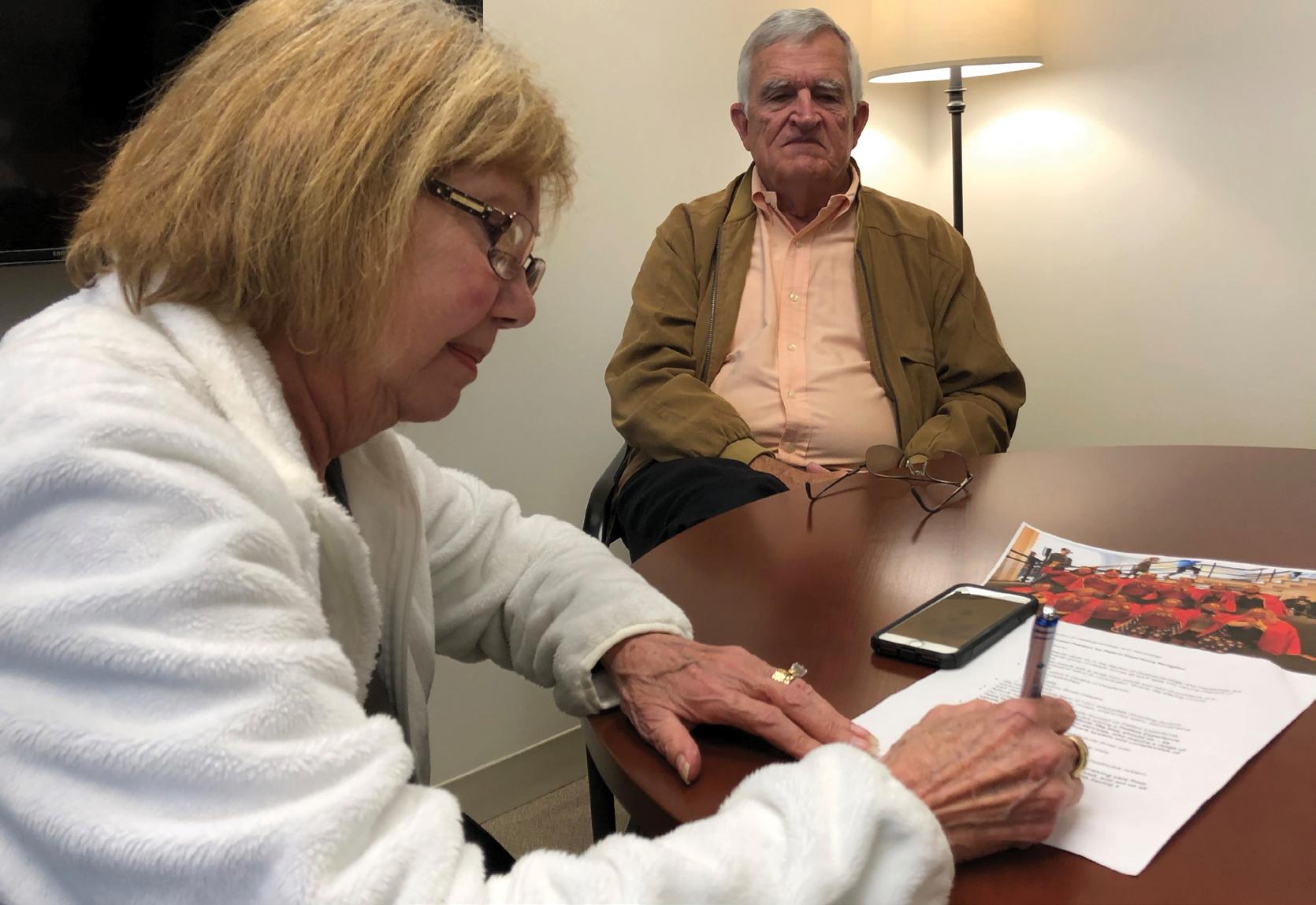
Lynne Carpenter, joined by her husband, Don, signs off on the patient navigator job description. Lynne’s generous gift funded this position and provides personal assistance to other Gastroenterology and Hepatology patients who need help navigating the complex healthcare system.
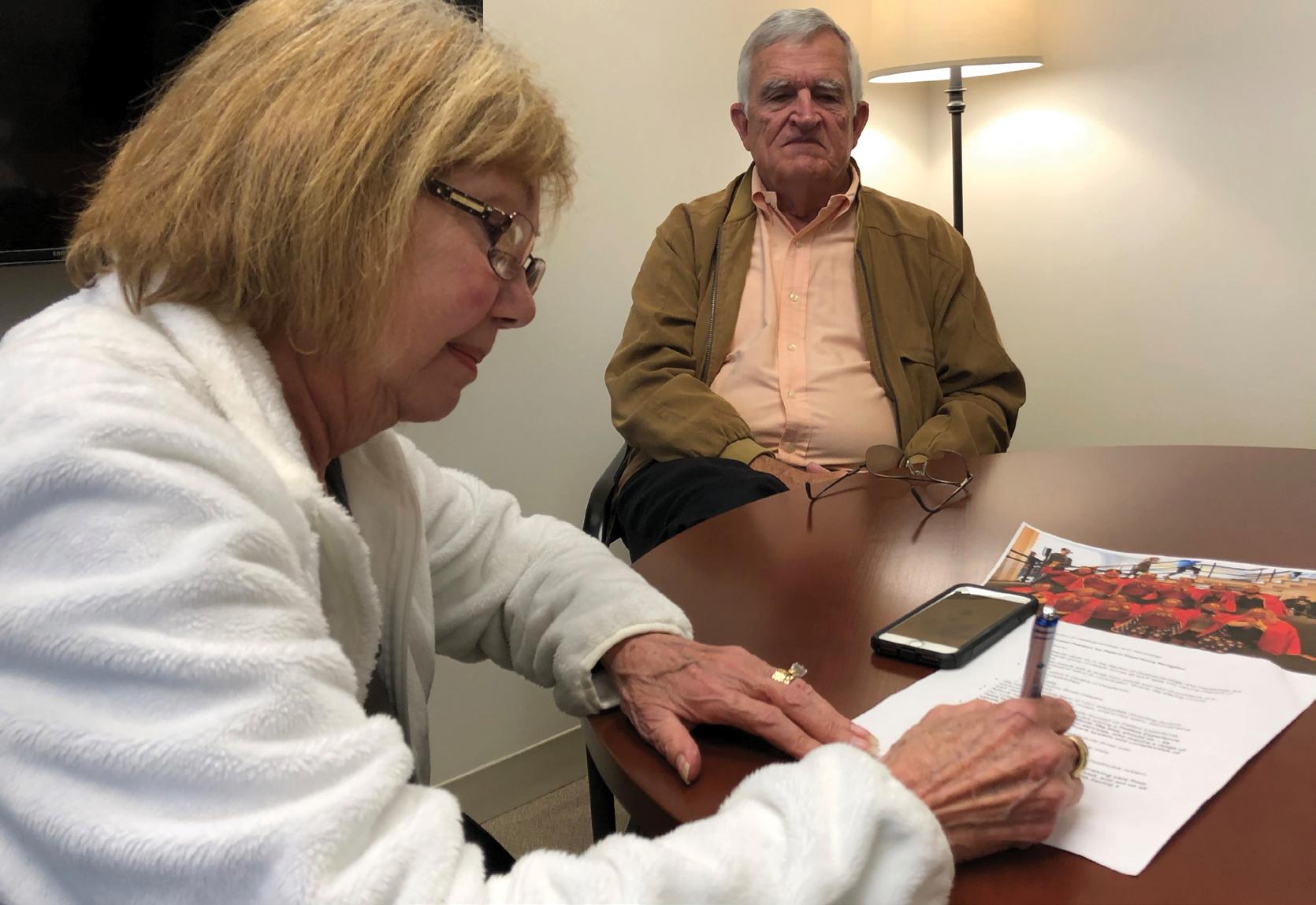
Before she passed away, Lynne Carpenter knew what it was like to have a serious illness. As a nurse manager and educator, she knew the healthcare system well and understood what each step in her treatment would be.
She also knew that not all patients with serious illnesses would have the same understanding. That’s why she made a generous gift of $500,000 to establish a patient navigator program in the Section of Gastroenterology and Hepatology—to make other patients’ health journeys a little bit easier.
As the first GI patient navigator, Tyler Dillehay can attest to how much the program has helped patients by giving them the gift of time—time that physicians simply don’t have the luxury of offering.
“I worked directly with patients and families, calling to make sure they’re set up for their appointments, ar ranging transportation, coaching them on how to follow up with their care. I helped them get to the next step,” Dillehay says. “Having a patient navigator call and check
to see if everything is going okay helps patients feel sup ported and know they aren’t falling through the cracks.”
“The burden of disease on patients goes far beyond just symptoms,” says Corey Siegel, MD, HS’02, HS’05, MS’09, section chief of Gastroenterology and Hepatology. “As healthcare providers, we always want to do more but are limited by time and resources. Because of this gift from Lynne, now we have someone on our team whose sole focus is to look for opportunities to further help our patients.”
Another aspect of the job is to improve the section as a whole, helping to enhance the patient experience. For example, Dillehay rewrote procedure instructions in plain language, making them easier for patients
3Dartmouth Health | Geisel School of Medicine Department of Medicine
Generous gift established a patient navigator program to help patients get the help they need—outside the doctor’s office
Continued on page 11
Kerrilynn Hennessey, MD, a cardiologist at Dartmouth Hitchcock Medical Center, examines a patient with Hannah Bensimhon, MD.
WOMEN in Cardiovascular Medicine
Nearly half of all medical school students for the past two decades have been women, but this representation is not reflected in the practice of cardiology. Kerrilynn Hennessey, MD, is working to find out why.
Her research study, LIFT: Leadership Impacts on Cardiovascular Fellowship Training, aims to determine how cardiovascular leadership impacts where women cardiovascular fellows pursue their training and what these women value most when choosing their training programs.

4 dartgo.org/deptofmed
Researcher finds that factors beyond diversity play a role in attracting women learners to cardiology training programs
“We hypothesized that the proportion of women trainees would be highest in programs with more gender diversity among their leadership,” says Hennessey, a cardiologist at Dartmouth Hitchcock Medical Center (DHMC) and an assistant professor of medicine at Geisel School of Medicine.
While the presence of women as mentors and role models is one of the strongest known factors influencing women to choose cardiology as a career, Hennessey notes that only 15% of cardiovascular attendings are women and that 35% of cardiovascular academic programs have zero women in leadership positions—a significant underrepresentation of the national population, which may also affect patients’ health.
“If some women only feel comfortable talking to women providers, we’re going to miss a group of patients who aren’t being served,” Hennessey says.
She is taking a dual approach to the LIFT study, which seeks to discover whether the underrepresentation of women in cardiology is also reflected among leadership and whether this factor is important to potential trainees choosing a fellowship program in cardiovascular medicine.
Hennessey first had to manually compile the gender of cardiovascular leadership across academic cardiovascular training programs around the country, data that has not been readily accessible in the past. She collected data on the gender of current fellowship program directors using a publically available data set from the Accreditation Council for Graduate Medical Education (ACGME). Then she evaluated the association between women in cardiovascular leadership and the proportion of women trainees in academic programs.
As for the second component of the research, she collected qualitative data to understand what factors are important to women when choosing a cardiovascular fellowship. Hennessey used a structured virtual focus group with women trainees to hear, in their own words, how women in leadership and women role models rank among factors trainees considered when selecting a fellowship program.
Diversity isn’t a prerequisite to inclusion. … While there’s work to be done to recruit women into the field of cardiovascular medicine, this work can be shared by men and women alike.”
Kerrilynn Hennessey, MD cardiologist at Dartmouth Hitchcock Medical Center
The study’s quantitative results did not find a significant association between women in leadership and the proportion of women trainees. Hennessey says it remains unclear whether this result is due to the scarcity of women in leadership or a true lack of association.
The qualitative component of her research, however, has provided valuable insight. These results show that other factors, such as the program’s culture and work-life balance, had more influence on the learners’ decision process than the number of women mentors.
Hennessey says this research, which received a SEAM award from the Department of Medicine, shows that even more important than having women in leadership positions, other ways of improving diversity, equity and inclusion may help increase the number of women in cardiovascular training programs.
“We don’t have to wait until women are better represented in order to get other women to join us, and there’s hope in that message,” Hennessey says. “Diversity, equity and inclusion are important factors when trainees are looking at a program, but diversity isn’t a prerequisite to inclusion. There are behaviors in training programs that can help everyone feel welcome. While there’s work to be done to recruit women into the field of cardiovascular medicine, this work can be shared by men and women alike.”
Dartmouth Health | Geisel School of Medicine Department of Medicine
5
Food as Medicine
Dartmouth
Health and Geisel School
of Medicine take unique approach to treating obesity
As obesity rates rise among adults and children across the U.S., activities underway in the Department of Medicine, at Dartmouth Health’s Weight and Wellness Center, and at Geisel School of Medicine are taking a proactive—and multifaceted— approach to improving the good health of patients, physicians and students, both now and in the future.
Weight and Wellness Center
Patients of any age are welcome at the Weight and Wellness Center, where specialists focus on the management of obesity and metabolic disease. These Dartmouth Health (DH) experts help patients to address not only weight and related comorbidities, but also to set goals and develop healthy lifestyles.
There’s no single cause of obesity, says Auden McClure, MD, MED’99, HS’08, MPH’08, the interim section chief of Obesity Medicine in the Weight and Wellness Center, codirector of the Pediatric Lipid and Weight Management Center, and director of the Culinary Medicine Program. Stress, physical limitations, poor sleep, medications, hormones, genetics—as well as eating habits—can all play a role. Because of this complexity, the Weight and Wellness Center employs a multidisciplinary team to address this chronic disease: health coaches, dietitians, chefs, exercise specialists and psychologists as well as physicians, who work closely with surgical colleagues in bariatric medicine. The Pediatric Lipid and Weight Management Center takes a similar approach for treating children and adolescents with a focus on family-based care and management of metabolic disease and health risk factors.
“Obesity medicine programs often focus primarily on medications and bariatric treatments,” McClure says. “One of the unique things about the Weight and Wellness Center is that we also offer an intensive lifestyle program. We help people eat smarter, move smarter and live smarter as a foundation upon which

to support these other effective approaches, improving sustainable weight loss.”
Even though obesity medication and bariatric surgery are very effective treatment options, stress and lack of sleep are common causes of weight regain, says Sarah Finn, MD, the medical director of DH’s Regional Weight and Wellness Center clinics in Bedford, Manchester, and Nashua, New Hampshire. Individualized treatments and targeted lifestyle changes can help address the underlying issues of sleep and stress. However, many adult patients coming to the center have previously had discouraging healthcare experiences, often encountering bias about their weight, which creates a barrier to getting the right treatment.
“Weight bias causes lack of trust and increased stress for patients. Communicating the disease process to patients helps build trust,” Finn says. “In visits with patients, I tell them I’m their teammate. I’m here to support and guide patients through their treatment. This is a core approach to patient care our entire team embraces and for which we provide specific training.”
Education Programs
Beyond medical management, the Weight and Wellness Center also offers weekly and monthly virtual classes to support patients in ways to improve their health. Topics include reading nutrition labels, nonexercise activity thermogenesis, managing stress and emotional eating, improving sleep, meal planning and preparation, plant-based eating, and more.
6 dartgo.org/deptofmed
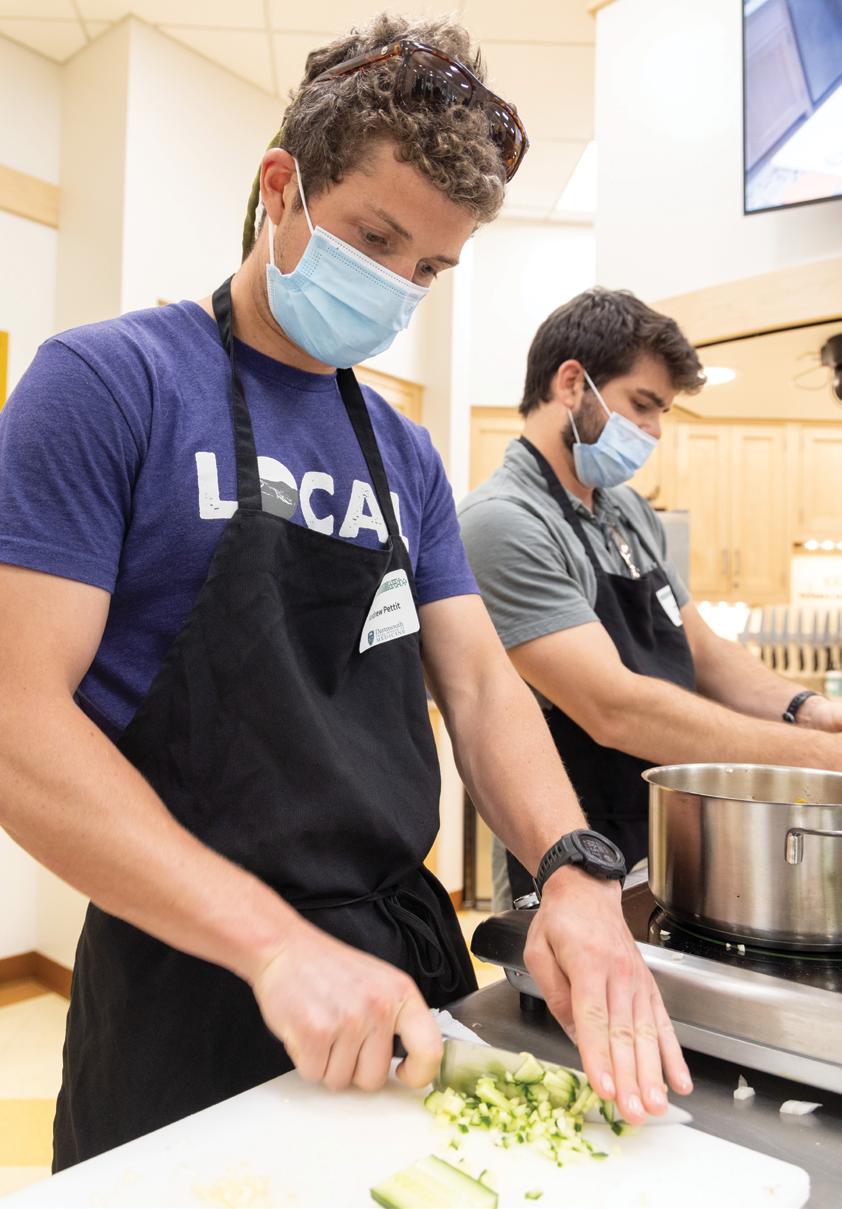
“Some patients need guidance in food prep skills and the ability to plan ahead or adapt recipes, especially when finances are an issue,” says McClure, a trained chef. “A teaching kitchen experience may help them become more engaged in healthy eating through education, culinary-skills acquisition, and peer support. It expands people’s palate and breaks down barriers to trying new things.”
This teaching kitchen is exactly what it sounds like—a kitchen where medical students, physicians and patients take classes to boost their culinary know-how. As a member of the Teaching Kitchen Collaborative (TKC) since its inception in 2016, Dartmouth Health joins a national network of organizations, academic or otherwise, that seek to improve people’s quality of life through food. McClure is working with the TKC to develop and test best practices for teaching kitchen curricula, and the Weight and Wellness Center’s
At left: Medical students Monika Gabriele ’25 (left), Sage Palmedo ’25 (right) and their classmates prepare a meal in the teaching kitchen at the Co-op Culinary Learning Center.

At right: The instructor’s food simmers invitingly while students prepare their own dishes.

culinary team recently completed a 16-week teaching kitchen pilot study aimed at improving lifestyle behaviors and metabolic health. This study will inform a multi-site clinical trial beginning in January.
Curriculum changes also are underway at Geisel, which offers a culinary medicine elective as well as a hands-on culinary medicine session as part of the required first-year medical education curriculum. Rima Itani Al-Nimr, MS, RDN, LD, is the director of Geisel’s Nutrition in Medical Education Longitudinal Curriculum, which integrates evidence-based nutrition education into each year of medical school. She says this will not only help future physicians make healthy choices themselves, but also feel prepared to counsel their patients.
In addition to the curriculum’s lectures and large-panel discussions, hands-on sessions teach students to read nutrition labels, and food models help students understand food combinations and portions. In the culinary medicine session, students cook a complete, healthful meal. Students learn to recognize bias against people with obesity and to offer treatment in a respectful and inclusive manner. They also learn how food insecurity affects health and how to connect patients with healthful food resources.
Research Activities
Dartmouth Health and Geisel are also committed to research into the future of good health as it relates to
7Dartmouth Health | Geisel School of Medicine Department of Medicine
We help people eat smarter, move smarter and live smarter as a foundation upon which to support these other effective approaches, improving sustainable weight loss.”
Continued on page 11
Auden McClure, MD Obesity Medicine interim section chief
PHOTOS BY: ROB STRONG
“When you’re confronted with unexpected and socially unacceptable language, it’s hard to know what to do if you haven’t prepared in advance.”
Kelly Kieffer, MD
MD
Handling Bias from Patients
Workshops help residents and faculty learn what to say when hurtful situations arise
Attendings and residents face a dilemma when confronted with racist, sexist, or other biased remarks from their patients—they must treat a patient’s medical condition and also address the inappropriate remarks.
“It’s a complicated problem because we’re obligated to care for patients regardless of whether we like them, but we also want to provide a safe and inclusive work environment,” says Kelly Kieffer, MD, HS’00, MS’11, an associate professor of medicine at Geisel School of Medicine and vice chair for education in the Department of Medicine at Dartmouth Hitchcock Medical Center (DHMC). “When you’re confronted with unexpected and socially unacceptable language, it’s hard to know what to do if you haven’t prepared in advance.”
As a faculty member at Geisel, Ellen Eisenberg, MD, faced such a confrontation several years ago in a resident clinic. “The patient told one of the interns that she didn’t belong here and that she should go back to the country she came from. She was devastated,” recalled Eisenberg, an assistant professor of medicine and retired associate director for the residency program at DHMC. “That prompted me to think about how we can support our learners when they experience bias from patients and how we can support faculty so they know what to do.”


With that inspiration and a grant from the Department of Medicine, Eisenberg helped create two annual workshops—“Developing an Approach to Responding to Patients with Bias” for residents and “Standing Up for Learners” for faculty—that use simulations and participant discussion to teach skills and strategies to use when they encounter overt bias or microaggressions from patients.
“There’s a spectrum of bias,” says Kieffer, who works with Eisenberg to lead the workshops. “Sometimes it’s a patient calling a woman physician ‘sweetie’ or asking if her husband minds if she works. Maybe it’s not meant to be hurtful, but it’s not reinforcing the resident’s view of themselves as a professional.”
When the workshops began in 2015, volunteers acting as biased patients would accost DHMC residents, who practiced what to do and say in these situations. The scenarios were not too extreme at first, Eisenberg says, but participants urged her to make patients even more aggressive to simulate really challenging situations. Soon, Eisenberg began recording these interactions, and the workshops now present several video vignettes and facilitate discussions afterward to brainstorm ways to address a range of potential confrontations.
8 dartgo.org/deptofmed
Ellen Eisenberg,
In one of the videos, for example, a simulated patient comes to the emergency department with chest pain. A resident and a medical student of color attend to the patient, but the patient won’t allow the student of color to touch him and wants him to leave the room. In this scenario, Eisenberg explains, the most important thing is to treat the patient having a heart attack. “They can’t take time to discuss in depth why the patient feels this way,” Eisenberg says. “Instead, the resident must refocus the conversation on the patient’s health. To support the student, the resident can say, ‘We work as a team, and I have utmost confidence in this student to help me take care of you.’” In a nonemergency situation, a resident or faculty member can refocus on the patient’s health and also explain that such behavior is not acceptable in this room or at this institution.
After the video, workshop participants discuss what they might have done and said, practicing the language they would use to communicate with biased patients and to support learners.
“It’s good to have a mixed group of participants in these workshops because people learn from each other,” Kieffer says. “Some people learn that their colleagues might experience a particular situation differently than they would, and later they can ask how their colleague is feeling. It helps to support inclusivity of the team and to learn to talk openly about bias.”
Kieffer stresses that, ultimately, it’s the faculty member’s responsibility to ensure situations are handled in a way that meets the resident’s needs as a learner and a clinician.
“In situations that are really hurtful, you don’t want to undermine the learner’s authority or leave them stranded to muddle through on their own,” Kieffer says. “You can provide the opportunity for the learner to leave the room if they want to, or you can empower them to speak up for themselves. We talk in the workshop about having a conversation with learners in the beginning to say, ‘Let’s talk about how we’ll handle a demeaning situation. We are here for each other, and I’m here for you.’”
The Department of Medicine continues to have a strong commitment to academic success through research scholarship under the leadership of Chair Richard Rothstein, MD, HS’85; Vice Chair of Research Richard Enelow, MD; and Director of Research Operations Jessica Chevalier, BS, CCRP.
In future newsletter editions, we will continue to highlight areas of active research by our faculty and learners. Below we present our current research portfolio, which includes all academic Department of Medicine faculty activities.
GRANTS
$15.5M ANNUALIZED REVENUE 125
Research in the Department of Medicine
statistics
July
through
2022
ACTIVE
Grant
are from
1, 2021,
June 30,
trials statistics are
July 1, 2021, through June 30, 2022 non-enrolling studies 327enrolling studies 291 618 active studies accruals are on treatment trials 298 NEW PARTICIPANT ACCRUALS 1,092 active treatment trials, out of the 618
studies 369 60% 27% 9
RESEARCH STUDIES Clinical
from
active
Dartmouth Health | Geisel School of Medicine Department of Medicine
The Department of Medicine
Scholarship Enhancement in Academic Medicine (SEAM) Awards Program
The SEAM Awards Program supports academic “dreams.” Successful proposals may include innovations in teaching, discovery/research, publication/presentation, practice improvement, and/or digital scholarly communications, with the ultimate goal of enhanced quality of patient care. The SEAM Awards funding exceeds $1.2 million since 2018.
Academic Year 2021-22 SEAM Awards Round 1: Fall 2021
Modifiable Behaviors Related to Cardiorespiratory Fitness in Children and Adolescents
Project Leader: Jennifer L. LaBarre Meijer, PhD, MPH, RD
Assistant Professor of Medicine Section of Obesity Medicine
Safe and Effective Practice of Food Oral Immunotherapy
Project Leader: Marcus S. Shaker, MD, MS’08, MSc, FAAAAI, FACAAI, FAAP
Professor of Pediatrics and of Medicine Section of Allergy and Clinical Immunology
Project Co-Leader: Sarah W. Hughes, MPAS, PA-C
Instructor in Medicine Section of Allergy and Clinical Immunology
Barriers to Adherence with Immune Modifying Medications in Crohn’s Disease
Project Leader: Michael W. Winter, MD
Assistant Professor of Medicine Section of Gastroenterology and Hepatology
Project Co-Leaders:
Robert E. Brady, PhD
Assistant Professor of Psychiatry
Jessica K. Salwen-Deremer, PhD, DBSM
Assistant Professor of Psychiatry and of Medicine Section of Gastroenterology and Hepatology
Academic Year 2021-22 SEAM Awards
Round 2: Winter 2022
Ventricular Repolarization as a Predictor of Atrial Anti-arrhythmic Efficacy
Project Leaders:
Daniel Feldman, MD, HS’21 Cardiovascular Medicine Fellow Daniel B. Ambrus, MD, MSc Cardiovascular Medicine Fellow
Project Co-Leaders: Kevin F. Kwaku, MD, PhD
Assistant Professor of Medicine Director of Electrophysiology Section of Cardiovascular Medicine Cynthia C. Taub, MD
Professor of Medicine Section Chief, Cardiovascular Medicine Yinong Young-Xu, ScD, MA, MS Assistant Professor of Psychiatry Clinical Epidemiologist
VA Medical Center, White River Junction, Vermont
Caroline Korves, ScD Clinical Epidemiologist VA Medical Center, White River Junction, Vermont Daniel J. O’Rourke, MD, HS’96, MS’97, MEd Associate Professor of Medicine VA Medical Center, White River Junction, Vermont
Deep Learning Assisted Segmentation of Brain Tumors and Organs-at-Risk for Increased Efficiency in Radiation Therapy Treatment Planning Workflows
Project Leaders:
Saeed Hassanpour, PhD
Associate Professor of Biomedical Data Science and of Epidemiology
Brady Hunt, PhD Instructor, Section of Radiation Oncology
10
dartgo.org/deptofmed
Continued from page 7
Food as Medicine
nutrition, metabolism, genetics, and the microbiome. The goal of the research program is to refine clinical programs and to contribute to the larger body of precision medicine for obesity.
One such project aims to determine whether the ability to metabolize a high-fat shake may
predispose certain kids to this disease.
Meijer notes there are thousands of markers to interpret, an impossible task for any clinician. Her research aims to narrow down the most determinant markers, those that may predict children’s risk of type 2 diabetes.
“If we can learn what’s going on in a child’s physiology, we can give good recommendations about how to manage the cards they have been dealt,” Meijer says.
In a separate project, Diane Gilbert-Diamond, ScD, an asso ciate professor of epidemiology, of medicine, and of pediatrics, is working with the Weight and Wellness Center to create a repository of biological samples as a resource for hypothesis-driv en research. Blood and stool samples collected from adults can be used for genetic, protein, and microbiome analyses. This biobank gives other scientists a head-start on their research, providing them immediate access to samples from which to extract the data they need—which can contribute to the advancement of precision medicine.
Continued from page 3
Easing the Burden
to understand. He also scoured patient surveys and planned projects to help patients and families feel better supported. “Since healthcare providers in GI spend much of their time caring for patients, having a patient navigator focus specifically on projects that will improve the patient experience has helped GI to be more prepared to meet the needs of the people we serve.”
“Being ill is confusing enough,” says Dorothy Heinrichs, the director of Patient and Family Giving. “You need someone to sit and say, ‘We’re going to make an appointment for you, and then this will happen, and I will help you.’ Lynne knew how navigation should work and wanted other patients to have that help.”
Heinrichs hopes the GI patient navigator program, which started in 2019, will be a model for other departments and sections to create similar programs. “As ill as Lynne was, she still wanted to take care of others,” she says.
Siegel saw joyful excitement on Lynne’s face when she made her gift, despite the seriousness of her condition.
help identify kids at high risk of type 2 diabetes to prevent disease onset. Jen Meijer, PhD, a registered dietitian in the Weight and Wellness Center and an assistant professor of medicine and of pediatrics at Geisel, is using metabolomics to discover what markers may
“We want to understand whether there are signals to guide doctors to provide better individualized treatment,” Gilbert-Diamond says. “Maybe in the future, patients will have microbiome workups, which, when considered with genomic and demographic information, will inform physi cians of the best treatment for each individual patient.”
“It was eye-opening to see the pleasure patients can get through giving—she had so much passion for making other people’s lives better,” Siegel says. “Seeing how much that meant to her truly inspired me. We were determined to make good use of her gift, and it was very well spent to create this position.”
11Dartmouth Health | Geisel School of Medicine Department of Medicine
Medical students Andrew Pettit ’25 and Jerry Tullo ’25 complete prep work in the Co-op Culinary Learning Center.
PHOTO BY: ROB STRONG
Faculty Promotions & Appointments
Our faculty members are the foundation of the Department of Medicine. Their dedication and commitment to our mission and their work is exemplary. Being recognized for academic achievement is an honor bestowed upon our clinician-scholars by their faculty peers.
We are excited to announce the following faculty promotions and appointments granted November 1, 2021, to July 1, 2022. Congratulations to them all!
Antonia Altomare, DO, HS’13, MPH’13
Associate Professor, Infectious Disease and International Health



Joseph Anderson, MD, MHCDS’14



Professor, Veteran’s Affairs Medical Center, Gastroenterology
Sushela Chaidarun, MD, PhD Professor, Endocrinology





Amelia Cullinan, MD
Associate Professor, Palliative Medicine
Alicia Zbehlik, MD, HS’12, MPH’12
Associate Professor, Rheumatology
* Indicates faculty appointment
David Feller-Kopman, MD Professor, Pulmonary and Critical Care Medicine *
Ugis Gruntmanis, MD Professor, Endocrinology *
Nirav Kapadia, MD, D’03, MS’16
Associate Professor, Radiation Oncology
Robert Simms, MD Professor, Rheumatology *
Benjamin Williams, PhD Professor, Radiation Oncology
Mary G. Turco, EdD, MA’78
Associate Professor, Medicine; Principal for Scholarship Enhancement and Academic Professional Development
One Medical Center Drive, Lebanon,
03766 dartmouth-hitchcock.org
NH
Dartmouth Hitchcock Medical Center DEPARTMENT OF MEDICINE
Photographer: Mark Washburn Writer: Ashley Festa Designer: Linnea Spelman
Keisuke Shirai, MD, MSc Professor, Medical Oncology