Evolving heart & vascular care
2025 Impact report


2025 Impact report

Dear Colleagues, Nationally ranked. High-volume. Experienced. Pioneering. Patient-centered. Heart and vascular at Corewell Health is all this and more, as we join forces to meet the growing needs of our communities.
With expertise and facilities that span the state, a track record of excellent care, and partnerships that promise more breakthroughs to come, we are poised to deliver even better outcomes to patients in Michigan and beyond.
Our efforts are resulting in impressive recognition. In 2024, U.S. News & World Report ranked eight of our hospitals as High Performing in heart and vascular care, with Corewell Health William Beaumont University Hospital ranked No. 25 in the nation, and tied for No. 1 in the state overall. We are one of two health systems in Michigan to be designated a Center of Excellence by the Hypertrophic Cardiomyopathy Association, and the only health system in Michigan to maintain HeartCARE Center Accreditation from the American College of Cardiology.
Our team has notched some noteworthy firsts, from performing the first transcatheter aortic valve replacement procedure in North America in 2005 to becoming the first health system in Michigan to use pulsed field ablation technology for Afib patients in 2024.
Yet for us, even more gratifying than accolades, records or rankings is the chance to change people’s lives for the better. It’s why we implemented our Student Heart Check program, which since 2007 has trained 11,878 students and educators on hands-only CPR, and screened 21,418 students for underlying heart concerns. In 2024 alone, we donated 14 AEDs to schools in Michigan and helped 42 schools become HEARTsafe certified.
It’s also why we’re developing new ambulatory surgery centers with the goal of reducing the cost of care; launching and growing a statewide advanced heart failure program to provide better care for our sickest patients; exploring emerging strategies such as cardioneuroablation; and investing in outreach.
Read on to learn more about how our teams are evolving heart and vascular care—through our continued legacy of discovery and groundbreaking treatments, and a relentless pursuit for excellence.
Corewell Health in Southeast Michigan
Corewell Health in Southwest Michigan
Corewell Health in West Michigan
With state-of-the-art facilities, the latest treatments and combined, statewide expertise, our heart and vascular teams have you covered.
Our goal as one of the nation’s leading integrated health care systems is to continue improving patient care and outcomes in our communities across the state. We’re proud of our hospitals that have earned 2024 recognition from U.S. News & World Report. Learn more.
Corewell Health William Beaumont University Hospital
In Michigan, No. 1 hospital* No. 2 for cardiology and heart surgery
Ranked #25 nationally for heart and vascular care
5 Corewell Health hospitals ranked in the top 8 in the state
Several Corewell Health hospitals recognized as high performing in heart and vascular procedures
10 high performing in COPD
9 high performing in congestive heart failure and stroke
8 high performing in heart attack
4 high performing in
• Transcatheter aortic valve replacement

• Abdominal aortic aneurysm repair
• Aortic valve surgery
• Heart bypass surgery
Largest health system in the state.** 21 hospitals.
300+ ambulatory locations.
12,000+ physicians and advanced practice providers.

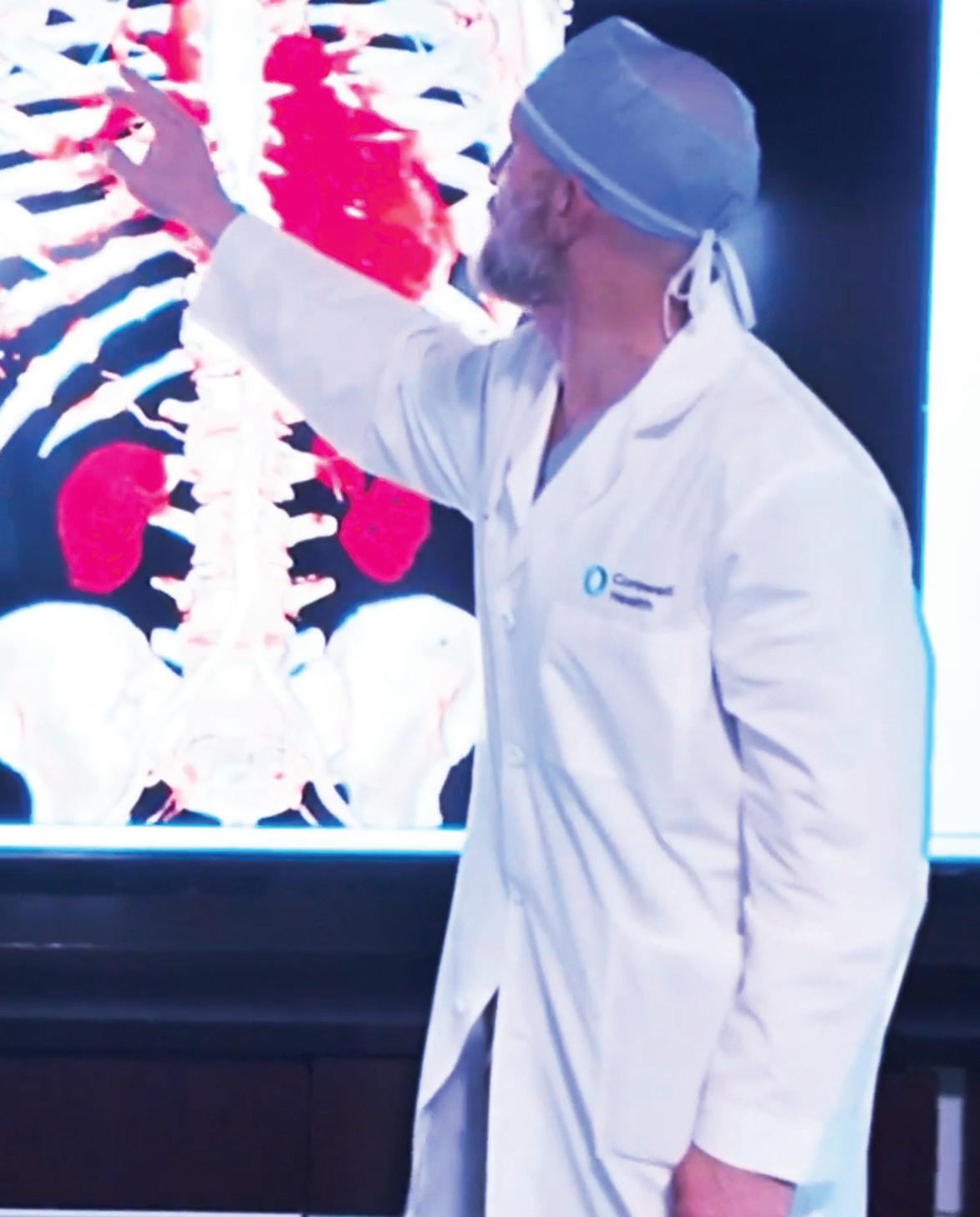
Treating the most severe and life-threatening heart attacks and complex diseases with percutaneous and surgical interventions. 08

Combining expertise across the state.
Advanced
Using state-of-the-art technology to detect and create individualized treatment plans.
Leading-edge techniques combined with promising new approaches.
Valve and structural heart
Pioneering procedures to meet growing community needs.
Expanding screening, surgical interventions and innovative treatments.

Collaborating to enhance prevention, early diagnosis and treatment.

Improving outcomes, reducing length of stay and decreasing readmissions.
Top performing fellowships and residencies, and continuing education.

More than 20.5 million U.S. adults have coronary artery disease, which makes it the most prevalent type of heart disease.1 It claimed more than 680,000 lives in 2023.2
While the stats are staggering, our teams are set up for success, treating the most severe and life-threatening heart attacks and complications of coronary artery disease with percutaneous and surgical approaches. Our accreditations and recognitions shine a light on our continual focus on quality and best practices. And, many of our hospitals have significantly lower mortality rates than similar hospitals at regional and national levels.
Chronic total occlusion
Coronary artery bypass grafting surgery
Coronary artery stenting
Coronary brachytherapy
Intracoronary lithotripsy
Intravascular ultrasound and optical coherence tomography
Corewell Health performs the most coronary artery bypass grafting procedures in the state.
(Source: Michigan Hospital Administration Inpatient Database, CY2023.)
• Routine exclusion of the left atrial appendage at the time of surgery to eliminate the cardioembolic source of stroke.
• One of the highest volume centers in Michigan for coronary brachytherapy.
• One of the highest volume centers in the state for intravascular imaging with percutaneous coronary intervention.
• Several hospitals received the BMC2 PCI 2023 Excellence in Cardiovascular Quality Improvement Award for perfect performance on the Outcomes and Process Composite Goal.
• One of the highest volume centers in Michigan for the treatment of ST-segment elevation myocardial infarction and chronic total occlusion.
We are pioneers in multiple arterial CABG, with a 40–60% utilization rate—far exceeding the 13% national average. This approach significantly extends patient survival, and our team has helped drive its adoption into routine practice.
Near-infrared spectroscopy
Rotational, orbital and laser atherectomy
Temporary mechanical circulatory support devices such as intra-aortic balloon pump, Impella® and extra-corporeal membrane oxygenation
6,200+ CABG procedures performed from 2020 to 2024.
“I am proud of our cardiac surgery team and CABG program. We maintain a focus on our continuous quality improvement while producing impressive outcomes.”
– Charles Willekes, M.D., cardiothoracic surgery
Corewell Health Fred and Lena Meijer Heart Center continues to maintain the highest available top decile 3-star rating from the Society of Thoracic Surgeons for coronary artery bypass grafting procedures.
• At the forefront of clinical studies involving mechanical circulatory support for acute myocardial infarction and cardiogenic shock.
• Fourth highest enrolling center globally in the LeAAPS research study, a randomized blinded study that includes removing the left atrial appendage exclusion for the prevention of ischemic stroke or systemic arterial embolization.
• Presented experience and findings at national and international conferences including the Society of Thoracic Surgeons Coronary Conference, Annual Meeting of the European Association for Cardiothoracic Surgery and the Annual Meeting of the International Coronary Congress.
Below are a just a few of our most recent published findings:
• The Contemporary Use of Intracoronary Brachytherapy for In-Stent Restenosis: A Review Cardiovascular Revascularization Medicine.
• Risk Factors for Percutaneous Left Ventricular Assist Device Explant Complications. Catheterization and Cardiovascular Interventions.
• Drug-Eluting Stent Restenosis: Modern Approach to a Classic Challenge. Current Cardiology Reviews.
• Comprehensive Shielding System Enhances Radiation Protection for Structural Heart Procedures Journal of the Society for Cardiovascular Angiography & Interventions.
• Multiarterial Coronary Artery Bypass Grafting Practice Patterns in the United States: Analysis of the Society of Thoracic Surgeons Adult Cardiac Surgery Database. The Annals of Thoracic Surgery.

We are recognized by the American College of Cardiology with the following accreditations:

• Continuously improving our quality metrics, including reducing the incidence of renal failure and stroke, reducing length of stay and the need for readmissions, and maintaining low mortality rates.
• Adopting minimally invasive and robotic-assisted CABG programs, delivering all the benefits of conventional surgery with less perioperative pain and faster recovery.
• Exploring more procedures that can be performed at outpatient surgery centers, creating more access to inpatient care for those who need it and reducing days in the hospital for those who don’t.
Cardiovascular imaging offers a non-invasive way to assess a wide range of conditions, provide answers and guide patient care. Our expertise in advanced imaging modalities allows us to detect and diagnose conditions early, as well as support lifesaving interventions and surgeries for critically ill patients.
4D intracardiac echocardiography
Cardiac computed tomography, including fractional flow reserve and plaque characterization
Cardiac MRI, including stress testing
Echocardiography, including 3D and strain analysis
Nuclear stress testing (SPECT and PET)
PET imaging for inflammation and viability assessment
Stress and hemodynamic stress echocardiography
Structural echocardiography
Vascular ultrasound (carotid, renal, aortic and peripheral) Corewell Health Heart &
Aortic diseases
Cardiac masses
Congenital heart disease
Congestive heart failure
Coronary artery disease
Hypertrophic and other genetic cardiomyopathies
Ischemic and non-ischemic cardiomyopathies
Inflammatory, infiltrative and arrhythmogenic cardiomyopathies
Pericardial disease
Valvular heart disease
Selected to participate in the Plaque Analysis
Case Evaluation program with HeartFlow, a new technology that more accurately assesses risk for coronary artery disease and guides treatment plans.
• Cardiac MRI capabilities for numerous indications with a wide bore magnet (not a true open magnet).
• Corewell Health William Beaumont University Hospital established one of the first dedicated Advanced Cardiac Imaging fellowships in 2005, delivering cutting-edge training in cardiac CT/FFR-CT, cardiac MRI and interventional echocardiography.
Our cardiac magnetic resonance imaging program is one of the busiest in the state and includes expertise in stress testing. We routinely and safely perform exams on patients with implanted pacemakers and defibrillators with minimal to no artifact.
Our cardiac CT program is one of the largest in the state and a national leader in using CT to triage chest pain in the ED. It continues to grow, adopting the latest ACC guidelines to assess coronary artery disease and guide procedures.
Our cardiac PET program provides non-invasive assessment of coronary artery disease, particularly for patients with higher BMIs, and helps evaluate active cardiac inflammation.
Our team is engaged in pioneering cardiovascular research, including:
• Studying the use of MRI to identify and treat scarring in the heart of patients with arrhythmia.
• Investigating radiation protection for interventional echocardiographers in structural heart procedures.
• Collaborating with Michigan State University College of Human Medicine to develop and test an all-in-one nanoparticle-based platform for plaque measurement, selective immunotherapy delivery and outcomes.
• Researching the use of Cardiac CT Plaque Analysis, an AI-enhanced imaging technology that provides non-invasive assessment of coronary plaque type and severity.
• Studying gated cardiac CT for improved planning of robotic mitral valve repair.
• Exploring artificial intelligence to enhance the quality of our imaging labs.
• Adding plaque analysis to coronary CT exams for better characterization and risk stratification.
• Adding 4D flow to CMR exams for enhancing the evaluation of valvular heart disease.
Advanced cardiac imaging with echo, MRI, CT, PET, MUGA
Advanced echocardiography including 4D imaging
Alcohol septal ablation
Cardiac magnetic resonance imaging
Cardio-obstetrics
Cardiopulmonary stress testing
Endomyocardial biopsy
Patients with advanced heart failure often face the poor median survival rate of less than two years without interventions such as heart transplantation or mechanical circulatory support.3 To us, this signals a need for more education, earlier screenings and healthier lifestyles, and also more treatments and therapies—at every stage.

Heart transplantation
Implantable cardiac pressure sensors
Mechanical circulatory support
Right/left heart catheterization
Septal myectomy for hypertrophic cardiomyopathy
Transesophageal echocardiogram
Ventricular assist device
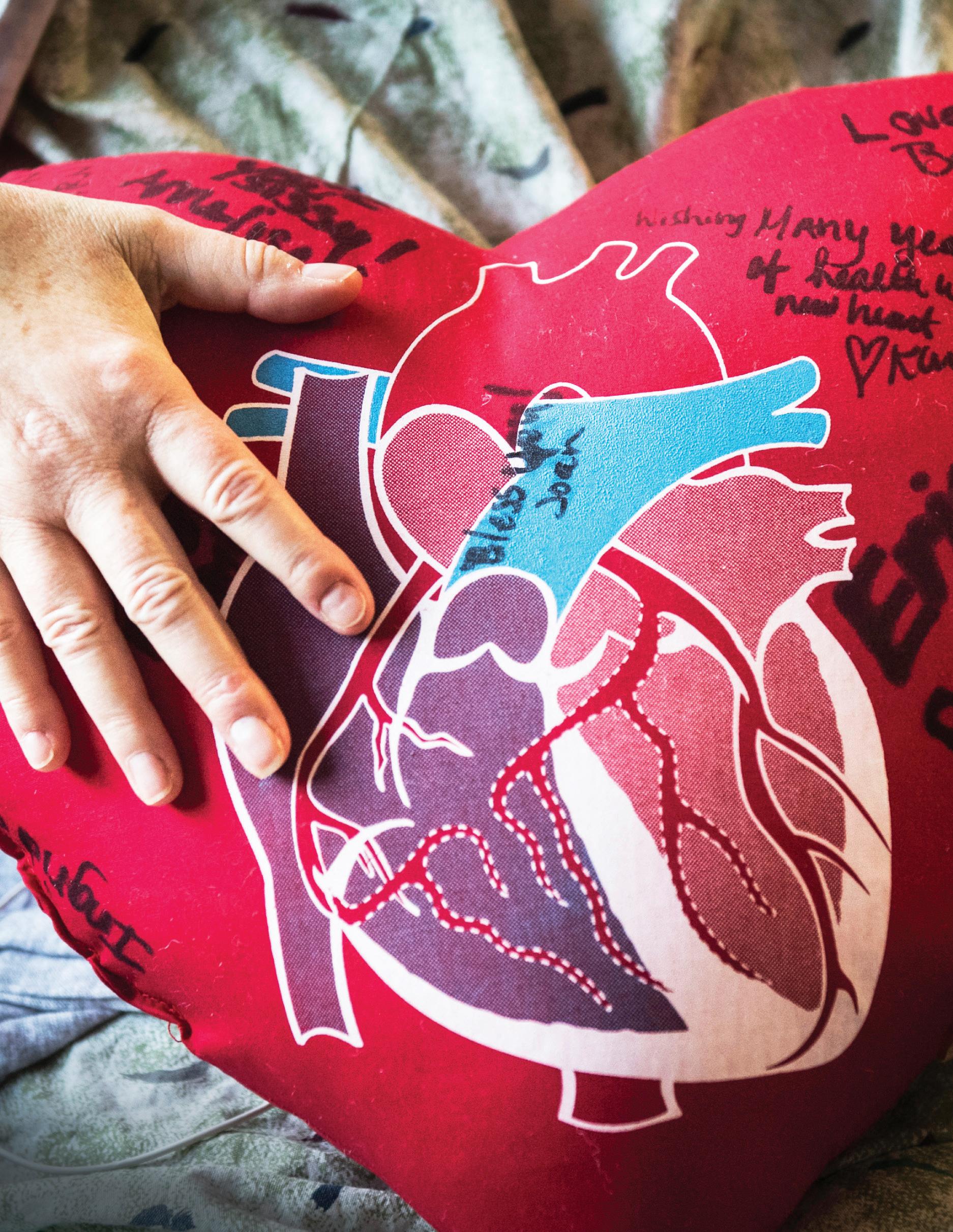
With that in mind, we’re growing our efforts throughout the state, supporting patients with multidisciplinary teams, individualized care plans and programs to improve quality of life. For the most complex and highrisk cases, our transplant center provides hope for those in need of the most advanced treatments. Together, our decorated teams are determined the 21st century will be the one in which heart failure finally meets its match.
Arrhythmogenic right ventricular dysplasia
Cardiac amyloidosis
Cardiac sarcoidosis
Cardiac tumors
Chemotherapy-induced cardiomyopathy
Diastolic heart failure
Genetic cardiomyopathies
Hypertrophic cardiomyopathy
Ischemic cardiomyopathy
Myocarditis
Non-compaction cardiomyopathy
Postpartum cardiomyopathy
Pulmonary hypertension
“The potential to expand access to the full spectrum of heart failure therapies, including heart transplant and left ventricular assist devices, for patients across the entire state of Michigan is extraordinary.”
– Douglas Horstmanshof, M.D., advanced heart failure cardiology

One of 40 health systems in the nation— and one of two in Michigan—designated as Center of Excellence by the Hypertrophic Cardiomyopathy Association.
• Launched support groups for hypertrophic cardiomyopathy patients in West Michigan to connect patients with peer support and education.
• Our multidisciplinary Hypertrophic Cardiomyopathy Clinic provides consultation from heart failure specialists, interventional cardiologists, cardiac surgeons and geneticists, and initiates and maintains patients on mavacamten, a medication that is specifically designed for HCM.
• Our pharmacist-led Guideline-Directed Medical Therapy clinic optimizes key life-sustaining medications for patients with weakened hearts. Over 80% of patients were able to achieve their ideal treatment doses within 12 weeks, which directly results in more days of better life for patients with heart failure.
Corewell Health Butterworth and William Beaumont University hospitals both provide extracorporeal membrane oxygenation for patients with severe cardiac or respiratory conditions. Butterworth Hospital is a Gold Level Center of Excellence, certified by the Extracorporeal Life Support Organization.
We reduced average hospital length of stay from 7 to 3.85 days—and less than 15% of patients were rehospitalized within 30 days. In 2023, this saved our patients 2,295 days in the hospital.
“The average time spent in the hospital for these patients was almost cut in half. Helping people get back to the things that are important to them is also important to us.” –Matt Gonzales, M.D., advanced heart failure cardiology
From 2020-2024, our Advanced Heart Failure program cared for 6,955 individual patients.
Our active research and clinical trials are a testament to our relentless pursuit for better care when it comes to heart failure. Below is a brief sampling of work in progress:
• Participating in the Corcinch-AH trial, the first AccuCinch® Ventricular Restoration System implant in Michigan.
• Studying the biomarkers of cardiovascular complications during pregnancy as a predictor of future cardiovascular risk.
• Participating in Explorer HCM, VALOR-HCM, MavaLTE, Embark clinical trials.
• Developing a statewide, world-class advanced heart failure patient experience.
• Launching a new Regional Referral Amyloid Center. This highly specialized facility will employ clinicians trained in advanced heart failure, clinical cardiology, hematology, neurology, orthopedics, nephrology and gastroenterology.
• Integrating AI technologies into heart failure devices to help detect the onset of heart failure decompensation earlier, maximizing patients’ cardiac function for longer and improving outcomes.
• Exploring the potential for a hypertrophic cardiomyopathy outreach program, with the goal to launch in 2026.
Corewell Health Butterworth Hospital received highest possible marks in the American Heart Association’s Get With the Guidelines® program for heart failure care.

Our heart and lung transplant programs are the largest in the state with excellent outcomes.
Heart
• One- and three-year survival rates better than the national average.*
• Tied for No. 1 in Michigan for one-year survival rate.*
• In 2024, our program performed 45 heart transplants, making it the highest volume center in the state.
• Completed more than 250 heart transplants since program inception.
Ventricular assist device
• One-year survival exceeding 94% with one-, three- and five-year survival better than the national average.**
• Reached our 500th LVAD implant in 2023.
Lung
• No. 1 in the nation for one-year survival rates.*
• Leading the state in outcomes and volumes.*
• No. 4 in the nation for three-year survival rates.*
• Completed 400+ lung transplants.
• Highest volume lung transplant program in Michigan since 2021.
Additionally, our teams offer adult liver and kidney transplants with better than national average outcomes, and pediatric kidney transplants through Corewell Health Helen DeVos Children’s Hospital. With more than 3,300 adult transplants combined (heart, lung, kidney and liver), we’re focused on statewide collaboration and program growth to continue serving the needs of our communities.
Predictors of Early Mortality After Lung Transplantation for Idiopathic Pulmonary Arterial Hypertension. Pulmonary Circulation.
• Starting pediatric heart transplant in 2025.
• Introducing new capabilities including implanting “total artificial hearts.”
• Working with UNOS and HHS on an “expeditious growth taskforce” to increase solid organ transplantation across the nation.
• Starting a “lung procurement at 10 degrees” research trial to evaluate improvement of graft function post-transplantation.
Heart rhythm disorders happen for a variety of reasons— genetic conditions, coronary artery disease, high blood pressure, cardiomyopathy, valve disorders—and sometimes for no apparent reason at all.4 In fact, one out of four people have a lifetime risk of developing atrial fibrillation, which increases the risk of stroke and congestive heart failure.5
Regardless of the exact diagnosis or etiology, our team takes addressing heart rhythm disorders very seriously. Our tailored treatment plans are a result of our leading-edge techniques combined with promising new approaches.
Conditions
Atrial fibrillation
Atrial arrhythmia
Hypervagotonia
Tachycardia
Vasovagal syncope
Ventricular arrhythmia
Ventricular tachycardia
Implanted an Extravascular CardiovertorDefibrillator—a first-of-its kind device, outside of the vascular space, to treat sudden cardiac arrest and abnormal heart rhythms with defibrillation and anti-tachycardia pacing.
• Extensive experience in conduction system pacing, an emerging alternative to biventricular pacing for those who don’t respond to cardiac resynchronization therapy.
We are recognized by the American College of Cardiology with the following accreditations:


• 70% of our patients are able to be discharged from the ED with short-term follow-up in our Atrial Fibrillation Clinic instead of being admitted for work-up.
• Treated 129 (2022 to 2024) patients in our Cardiac Resynchronization Therapy Device Non-responder Clinic designed to troubleshoot care, optimize devices and identify interventions for those who do not respond to CRT.
Atrial fibrillation ablation
Pacemaker implantation, including leadless and conduction system pacing
Cardiac resynchronization therapy
Cardiovertor-defibrillator implantation

Cardioversion
Pulsed field ablation
Stereotactic radiation therapy
Radiofrequency and cryoablation
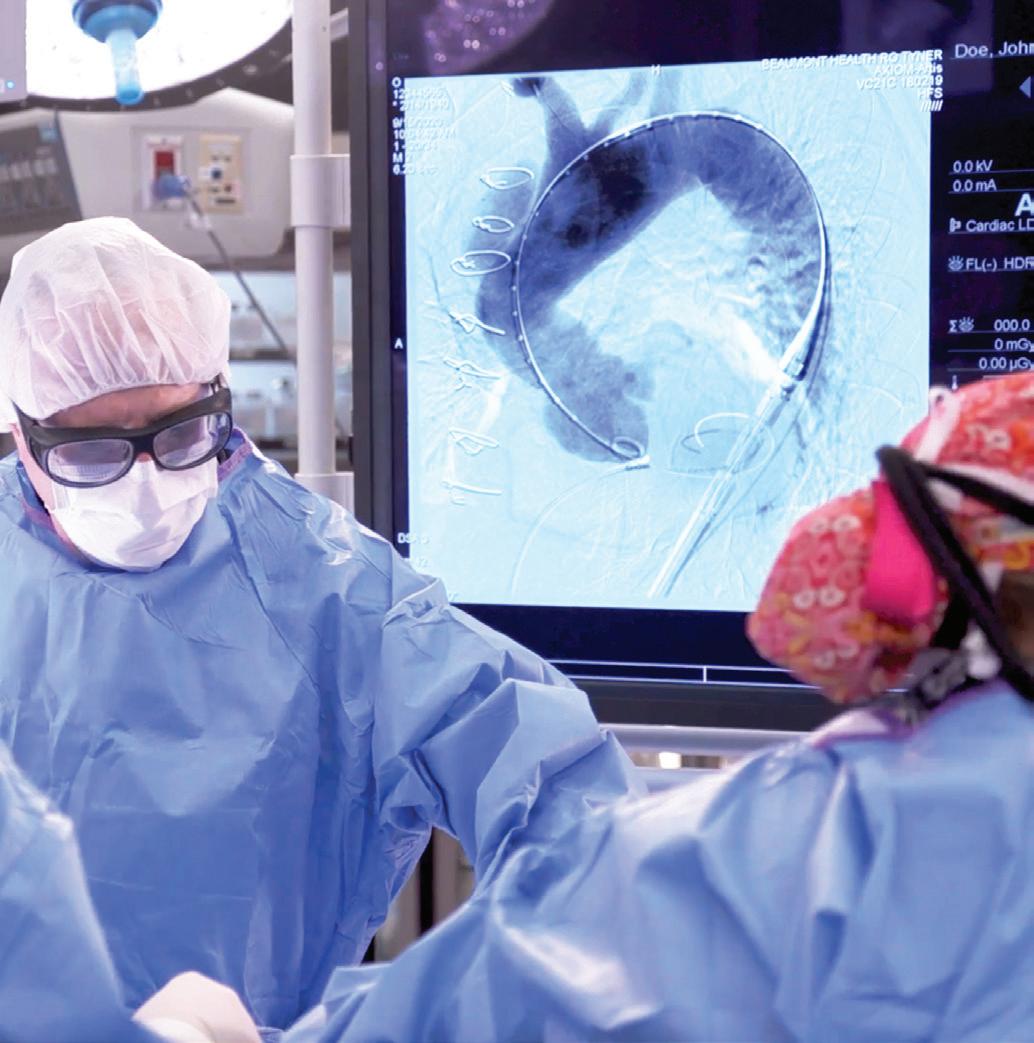
In 2024, Corewell Health became the first health system in Michigan—and fifth in the nation—to use pulsed field ablation technology for atrial fibrillation ablation following FDA approval, with the first cases performed in tandem across the state. From February to July, our teams performed 220 PFA procedures. Results so far are excellent, with no serious adverse events.
William Beaumont University Hospital is the first and only adult IAC accredited electrophysiology lab in Michigan.

Ventricular Late Gadolinium Enhancement by Cardiac MRI as a Predictor of Atrial Fibrillation in Hypertrophic Cardiomyopathy. International Journal of Cardiology.
Four-Year Follow-up of Outcomes of the Hybrid Epicardial-endocardial Ablation: A Single-center experience. Heart Rhythm.
Multidisciplinary Approach to Patent Foramen Ovale Closure for Cryptogenic Stroke: Brain-Heart Board Experience. Neurology.
• Using pulsed field ablation for the treatment of arrhythmias beyond atrial fibrillation.
• Exploring refinements for cardioneuroablation, an emerging strategy in the treatment of hypervagotonia and vasovagal syncope. The procedure locates and modifies specific nerves near the heart and disrupts the neural pathways that cause abnormal regulation of involuntary functions.
• Investigating stereotactic body radiation therapy to treat structural heart disease and recurrent monomorphic or ventricular tachycardia that is refractory or where standard ablation is a contraindication.
“Pulsed field ablation is a safer modality of creating that scar tissue in the appropriate areas of the heart to treat Afib without the need for medications. And it’s a little quicker.”
– Andre Gauri, M.D., electrophysiology

We treat thousands of individuals with various types of valve and structural heart conditions including congenital disorders, cardiomyopathy and heart valve disease—which affect more than 5 million people in the United States.6
Our teams have led the way for decades, pioneering techniques and procedures to meet growing community needs. Our clinicians rank among the nation’s leaders in minimally invasive techniques, robot-assisted surgeries and other advanced treatments.
6 CDC.gov, July 2024.
Alcohol septal ablation
Left atrial appendage occlusion
Minimally invasive and robotic surgical
repair and replacement
Septal myectomy
Transcatheter aortic valve replacement surgery
Transcatheter closure of congenital defects
Aortic valve stenosis
Bioprosthetic valve failure
Left ventricular outflow tract obstruction
Left ventricular pseudoaneurysm
Mitral valve regurgitation
Mitral valve stenosis
Patent ductus arteriosus
Fred and Lena Meijer Heart Center is the only location in Michigan with the distinct American College of Cardiology HeartCARE Center Accreditation for TAVR.
• Our neuro-cardio board is dedicated to identifying the appropriate work-up for patients with embolic stroke and heart rhythm disorders who are not candidates for anticoagulation. Known as “Brain Heart,” this multidisciplinary team of structural heart experts, neurologists and electrophysiologists meets monthly to review medically complex cases and develop appropriate plans of care.
• Our hospitals have 3-star (highest ranking possible) and 2-star rankings within the Society of Thoracic Surgeons and American College of Cardiology Transcatheter Valve Therapy Registry.
Transcatheter closure of prosthetic paravalvular leak
Transcatheter mitral edge-to-edge repair
Transcatheter mitral valve replacement surgery
Transcatheter tricuspid edge-to-edge repair
Transcatheter tricuspid valve replacement
Patent foramen ovale atrial septal defect
Post-infarction ventricular septal
Prosthetic paravalvular leak
Pulmonic valve disease
Ruptured sinus of valsalva aneurysm
Tricuspid valve regurgitation
Ventricular septal defect

In 2024, William Beaumont University Hospital was one of the first sites in the nation to offer transcatheter tricuspid valve replacement therapy after FDA approval in addition to transcatheter tricuspid valve edge-toedge repair. Fred and Lena Meijer Heart Center also offers T-TEER and began TTVR, expanding transcatheter services to patients with tricuspid valve regurgitation across the state.
Butterworth Hospital is one of only 20 centers in the nation to receive the Mitral Valve Repair Reference Center Award from the Mitral Foundation for superior clinical outcomes resulting from evidence-based, guideline-directed degenerative mitral valve repair.

William Beaumont University Hospital is one of two centers of excellence in the U.S. and a physician training center for transcatheter edge-to-edge repair using the PASCAL System.
Corewell Health is a statewide leader in structural heart procedures.
Corewell Health Meijer Heart Center has been providing cardiac robotic surgery with excellent outcomes for over 10 years. Today, 68% of mitral valve surgeries at this center are done robotically. In 2024, Corewell Health William Beaumont University Hospital launched its cardiac robotic surgery program, specializing in world-renowned minimally invasive mitral valve repairs using a port-based surgical approach. Five tiny incisions are made, without cutting into bone and muscle, resulting in less pain, no narcotics, faster recovery and shorter hospital stays.
Learn more at corewellhealth.org/innovators

Our teams are breaking new ground through active research and clinical trial enrollment. Below is sampling of research in progress:
• Exploring early aortic valve replacement for the treatment of moderate aortic stenosis before it becomes severe.
• Participating in novel therapies for tricuspid valve regurgitation.
• Studying the potential for embolic protection devices to filter embolic debris during TAVR procedures, to reduce the occurrence of neurologic events.
• Evaluating the safety and efficacy of the IntrepidTM and AltaValveTM TMVR system for patients with moderate to severe mitral regurgitation who aren’t candidates for TEER or other surgical mitral valve interventions.
Below are a just a few of our most recent published findings:
• Self-Expanding or Balloon-Expandable TAVR in Patients with a Small Aortic Annulus. The New England Journal of Medicine.
• 1-Year Outcomes Following Transfemoral Transseptal Transcatheter Mitral Valve Replacement: Intrepid TMVR Early Feasibility Study Results Journal of the American College of Cardiology Cardiovascular Interventions.
• 3 Year Outcomes from the Evolut Low Risk TAVR Bicuspid Study. Journal of the American College of Cardiology Cardiovascular Interventions.
• Reinterventions After CoveVale/Evolut Transcatheter or Surgical Aortic Valve Replacement for Treatment of Severe Aortic Stenosis. Journal of the American College of Cardiology Cardiovascular Interventions.
• Real-World Outcomes for the Fifth-Generation Balloon Expandable Transcatheter Heart Valve in the United States. Journals of the American College of Cardiology.
• Patient-Prosthesis Mismatch After Surgical Aortic Valve Replacement: Analysis of the PARTNER Trials. The Annals of Thoracic Surgery.
• Is Annular Enlargement in Mini Right Thoracotomy Aortic Valve Replacement Safe and Feasible? ISMICS Annual Scientific Meeting.
• Expanding tricuspid therapies with multiple repair and replacement platforms.
• Exploring and expanding innovative methods to diagnose and treat valvular disease with earlier intervention.
• Researching novel technologies for transcatheter mitral value therapies and expanding current indications for approved valves.


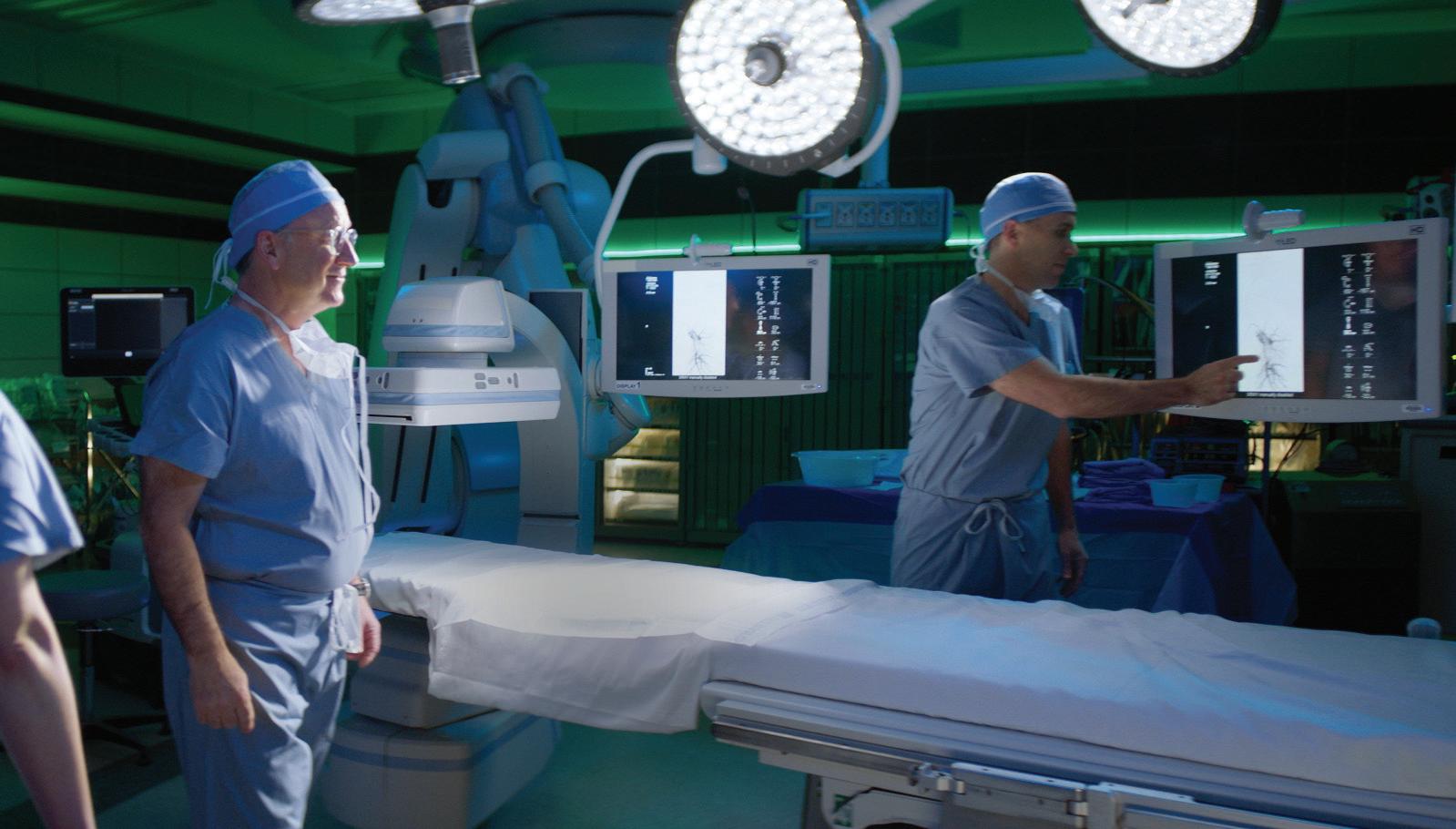
Aortic diseases are, by their nature, very serious. While not as common as some other conditions, their tendency to fly under the radar for years can result in life-threatening emergencies. This inspires us to continue investing in improved screening, genetic counseling, surgical interventions and innovative treatments.
With expertise in open repair of aortic conditions, endovascular therapies and hybrid aortic solutions, our multidisciplinary approach offers patients treatments that not only support physical health but align with their personal goals and preferences.
Endograft design, construction and deployment
Risk assessment for inherited conditions, which includes:
- Genetic evaluation, testing and education
- Prevention options
- Screening options
- Research protocols
Abdominal aortic aneurysm
Aortic aneurysm
Aortic dissection
Arteriosclerosis/atherosclerosis.
Ehlers-Danlos syndrome.
Familial thoracic aortic aneurysm syndrome.
Hypertrophic cardiomyopathy.
Loeys-Dietz syndrome.
Lupus.
Marfan syndrome.
Pararenal aneurysm.
Takayasu’s arteritis.
Thoracic aortic aneurysm.

Surgical interventions:
- Endovascular repair
- Endovascular treatment of the aortic arch
- Fenestrated endografting
- Repair of thoracic aneurysms and emergent dissections
- Thoracic endovascular aortic repair
- Thoracoabdominal aortic aneurysm repair
First Thoracoabdominal Branch
Endoprosthesis procedure in Michigan, a major advancement in the minimally invasive treatment of thoracoabdominal aortic aneurysms.
• Leader in aortic root pathology treatments and preservation of the native aortic valve.
• First in Michigan to use conscious sedation combined with percutaneous approach in TEVAR cases.
To evaluate the safety and effectiveness of new treatments for various aortic conditions, our teams are involved in multiple clinical trials including:
• Serial AAA CT
• IMPROVE-AD
• SOCRATES
• AAA-Shape
Highest-volume aortic center in the state for combined infrarenal AAAs and TEVARs.
Source: Michigan Hospital Administration Inpatient Database, CY2023
Determining the genetic basis of a heart condition can be helpful, particularly for patients with the following:
• Suspected or clinically diagnosed heart condition.
• Known family history of an inherited heart condition.
• Family member(s) who experienced sudden cardiac arrest or death, especially at a young age.
• Family member(s) who experienced an aortic aneurysm or dissection.
• Family member(s) with unexplained abnormal cardiac testing.
• Family member(s) experiencing chronic heart palpitations, fainting or shortness of breath not explained by another health condition.
As part of the Population Precision Health initiative, more than 1,000 adults have been screened over the past two years and diagnosed with multiple inherited cardiovascular conditions, such as hypercholesterolemia and arrhythmia.
Below are some of our most recent presentations and publications:
• Hemiarch Versus Extended Arch Replacement for DeBakey Type I Acute Aortic Dissections. American Association for Thoracic Surgery.
• Aortic Regurgitation, Time to Aortic Valve Reintervention, and Mortality in Degenerated Trifecta Versus Non-Trifecta Bioprosthesis American Journal of Cardiology.
• Expanding Aortic Center of Excellence across the state with referral mechanisms, expanded research efforts and dedicated resources to inpatient and outpatient aortic care.
• Focusing on the endovascular treatment of the aortic arch.
• Insurance credentialing for our genetic counselors, to help remove financial and logistical barriers to genetic counseling for patients at risk of inherited heart conditions.

Peripheral arterial disease is a common condition that often coexists with other cardiovascular diseases. Even though it’s common— affecting 6.5 million Americans age 40 and older—up to 50% of people with PAD don’t experience symptoms or think symptoms are a normal part of aging, which leads to underdiagnosis.7
But, left untreated it can have serious consequences such as heart attack, stroke, limb amputation or even death.8 In fact, PAD is the leading cause of lower limb amputation, with an estimated 185,000 amputations occurring annually in the U.S.
To save people from the pain, complications and disability that comes with PAD, we are collaborating across the state to enhance early diagnosis and treatment, strengthen prevention efforts and salvage limbs of those already affected.
Services and procedures
Advanced vascular imaging
Angioplasty
Atherectomy
Endarterectomy
Gene therapy
Hybrid bypass (open and endovascular)
Lifestyle support
Medication management
Open bypass
Percutaneous transmural arterial bypass (or endovascular bypass)
Stenting
Smoking cessation
Stem cell therapy
Transcatheter arterialization of the deep veins
Wound care
Atherosclerosis
Cardiovascular disease
Critical limb ischemia
Gangrene
Heart attack
Rest pain
Stroke
Tissue damage
Our Lifestyle Support programs come alongside our medical and surgical treatments to improve and proactively manage chronic conditions (like diabetes and high blood pressure), and improve diet, physical activity and substance use.
• Offer free vascular screenings throughout our health system to aid in early diagnosis and treatment of PAD, prevent complications and improve quality of life.
• Our “pre-hab” (rehabilitation prior to surgery) programs promote better surgical outcomes and healing after surgery through improved physical fitness, nutrition, lifestyle and psychological health.
• The Corewell Health Hyperbaric Oxygen Therapy Center in Royal Oak has one of the largest multipatient chambers in the state, as well as the largest mono-place chamber in Southeast Michigan.
The Intersocietal Accreditation Commission (IAC), a national nonprofit that accredits and awards high-quality diagnostic imaging programs throughout the country, has honored vascular ultrasound facilities throughout Corewell Health for 25 years (silver) and 30 years (gold) of continuous accreditation.

Corewell Health is the only health system in Michigan with Undersea & Hyperbaric Medical Society-accredited hyperbaric medicine facilities, located in Grand Rapids and Niles. The Grand Rapids facility is accredited with distinction and is the only emergency hyperbaric chamber in the state.
In 2024, our vascular teams performed:
• 4,214* hospital-based vascular surgery cases systemwide.
• 128,495 ultrasound vascular imaging systemwide.
• 955 limb preservation procedures in West Michigan, including angiograms, lower extremity endo and open stent, and lower extremity bypass.
*annualized
• Exploring the establishment of a limb salvage clinic.
• Researching how stem cell and gene therapies may be used for promoting blood vessel growth.

Pulmonary embolism is one of the most common cardiovascular health issues, affecting up to 900,000 people per year in the United States.9 It’s the third-leading cause of cardiovascular death10 and the leading cause of in-hospital death.11 Yet, it’s lesser known than more common cardiovascular conditions, leaving many patients unaware of their risks—and providers less equipped to address them.
Corewell Health is meeting this challenge through a systemwide pulmonary embolism response team that is prepared to assess and manage both complex and low-risk pulmonary embolism patients. And our efforts are resulting in improved cardiopulmonary outcomes, reduced mortality, reduced length of stay and decreased 30-day readmissions.
CDL EKOS Thrombolex
Embolectomy
MCS ECMO RP Impella
Reperfusion
Systemic tPA
Thrombectomy
Thromboaspiration
Vascular ultrasound (carotid, renal, aortic and peripheral)
Acute congestive heart failure
Acute kidney injury
Acute myocardial infarction
Acute respiratory distress syndrome
Acute respiratory failure
Acute right ventricular failure
Cardiomyopathy
Chronic congestive heart failure
Chronic obstructive pulmonary disorder exacerbation
Coagulopathy
Coronary artery disease
Deep vein thrombosis
End-stage renal disease
Liver disease
Non-sustained ventricular tachycardia
Obesity
Pneumonia
Sepsis
Shock
Ventricular fibrillation
• Our risk-stratification approach to managing patients has demonstrated remarkable outcomes including reducing mortality rates from 14% to less than 1.5% over a span of 10 years.
Multidisciplinary expertise from interventional cardiology, pulmonary medicine, interventional radiology, cardiac surgery, advanced heart failure, advanced imaging and emergency medicine collaborate on the best treatment option for each patient’s unique presentation.
• Pharmacologic and interventional treatments are used to manage high-risk or intermediaterisk pulmonary embolism, including mechanical thrombectomy, thrombolytic strategies and mechanical support.
• Patients identified as low risk with very low likelihood of clinical deterioration are referred to our outpatient low-risk Pulmonary Embolism Transition Clinic, which optimizes treatment and care without the unnecessary hospital stays.
• Our teams have expertise in venoarterial extracorporeal membrane oxygenation, an advanced temporary life support system for the most critical and complex conditions including massive pulmonary embolism with acute right ventricular failure and cardiogenic shock.
Engaging in the creation of the largest allcomers pulmonary embolism database, logging approximately 5,000 cases per year—making Corewell Health the national leader in true, real-world pulmonary embolism data.
Our physicians are members of the Pulmonary Embolism Response Team Consortium, which guides and influences pulmonary embolism care and research across the country, and our eastern region is a PERT Consortium Center of Excellence.
Grand Rapids Hospitals –Butterworth Hospital was named the inaugural National Blood Clot Alliance Center of Excellence in the United States. This new designation combines the excellence in clinical outcomes demonstrated by Corewell Health with the NBCA emphasis on patient education and post-hospitalization patient care for both deep veinthrombosis and pulmonary embolism patients.

4,800 patients treated for pulmonary embolism in 2024.
• 2,200 advanced PE interventions and 1,600+ deep vein thrombosis interventions over last 5 years (since program inception).
• 1,800+ life-saving thrombectomies.
We are one of the largest health systems with thrombectomy experience treating pulmonary embolism in the world, with 1,531 procedures performed from 2020 through 2023.
Our active research and clinical trials are a testament to the energy and passion of our systemwide pulmonary embolism response team, and its commitment to delivering better patient outcomes and a better patient experience across the care continuum. Recent publications include findings on new product development, outcomes, establishing standards of care for PE and partnerships with CMS and FDA.
• Using AI for pulmonary embolism escalation pathways and to support prompt care and coordination across the system.
• Developing a Pulmonary Embolism Transition Clinic.
• Prioritizing new device development to optimize outcomes.
• Standardizing clinical care pathways for pulmonary embolism, including EPIC order sets.
• Improving Mechanical Circulatory Support (MCS) strategy for high-risk patients.


Training the next generation of specialists is a responsibility and privilege we take seriously. Collectively, we train dozens of heart and vascular specialists and subspecialists each year.

Fellows train in our integrated Corewell Health Frederik Meijer Heart & Vascular Institute.
Fellowships
• Cardiovascular Disease
• Interventional Cardiology
• Advanced Heart Failure & Transplant Cardiology
• Thoracic Surgery
• Vascular Surgery
• Advanced Cardiovascular Imaging* Residency
• Integrated Vascular Surgery
*non-ACGME accredited
Join us at the 2025
Corewell Health experts, along with national and state experts, will discuss hot topics in heart and vascular medicine, including cardiovascular care, cardiovascular surgery and vascular surgery. The course will feature debates, business and political landscape, plus multiple keynote presentations.
Friday, June 20 to Sunday, June 22, 2025
Traverse City, Michigan
Learn more at corewellhealth.org/cardiovascular-summit

Fellows train at Corewell Health Dearborn, Farmington Hills or William Beaumont University hospitals.
Fellowships
• Cardiovascular Disease
• Interventional Cardiology
• Electrophysiology
• Vascular Surgery
• Advanced Cardiovascular Imaging*
• Advanced Structural Heart*
Learn more at corewellhealth.org/graduate-medical-education

Explore careers: corewellhealth.org/careers
Download this report: corewellhealth.org/cv-impact
Referrals — Find a heart & vascular specialist: corewellhealth.org/impact25