DreamLite® flowcharts for use in practice







Myopia? Myopia correction?
Myopia management?
DreamLite® MC night lenses
Check on a regular basis and discuss the risk profile*
• S -0.75 D up to -5.00 D
• Astigmatism up to -2.50 D
• Optical zone diameter: 5.50 mm and 5.00 mm
• S -0.75 D up to -5.00 D
• Astigmatism up to -2.50 D
• Optical zone diameter: 6.00 mm
Presbyopia?
DreamLite® Zoom night lenses
DreamLite® night lenses
• S -0.75 D up to -5.00 D
• Astigmatism up to -2.50 D
• Optical zone diameter: 6.00 mm
• A multifocal correction with a maximum of +1.50 D
Medical history1
Refraction. Spherical -0.75 D up to -5.00 D. Cylinder up to -2.50 D
Slit lamp examination
Determine corneal diameter (Ruler, WTW, topographer)2 Make good topography images 3
Insert the lenses, check the visual acuity1
Measure refraction over the lenses2
Assess the lens diameter.3 Abnormalities?
Assess (initial) topography, recreate if necessary and evaluate corneal diameter
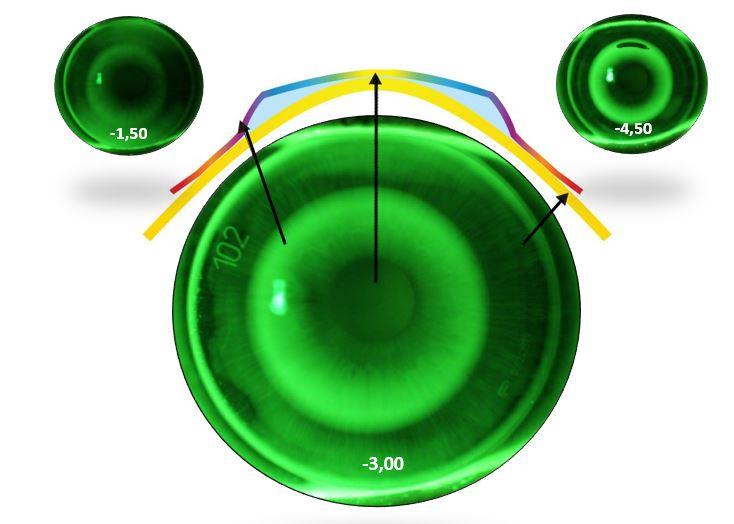
Check with fluorescein and take pictures.4 Assess the ortho-k pattern. Abnormalities?
Give instructions, start by taking out the lenses and then reinserting. Discuss care system and compliance
Export topography to VISAVY® and enter refraction data. The residual refraction is calculated
VISAVY® calculates TRX at higher toricity. Choose TRX in case of limbus to limbus astigmatism. Assess topography: pay attention to symmetry, (ir)regularity and k-values4

Adjust the lenses and/or request support from Professional Services
Sign DreamLite® agreement. Please provide available protocols. Schedule follow-up checks5
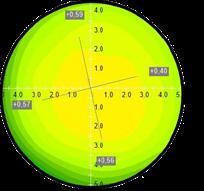
Highest success rate with k-values: 7.40 - 8.40
Discuss expectations: habituation, visual acuity, halos5
Order DreamLite®
1: Also ask about ocular history (e.g. refractive surgery)
2: When measuring the corneal Ø via the topographer, pay close attention to the position of the measuring points at the limbus and adjust them, if necessary
3: Think about palpebral fissure (vertical distance), head position, fixation and good tear film
4: Large differences between OD/OS are usually uncommon at comparable refractive values. Also rule out contraindications
5: Halo complaints can last up to 3 months. The brain needs time to filter this out
1: With the lenses in, one expects a visual acuity similar to that of the initial refraction
2: Large deviations (>0.50 dpt) can indicate a miscalculation of the lens
3: The lens should cover approximately 90% of the cornea
4: If you do not have a slit lamp camera, you can also use a smartphone
5: Schedule for follow-up checks:
After 1st night wear
After 3rd night of wear
After 10th night of wear
Do not dispense the lenses in case of large deviations
Check preferably in the morning. Have the customer come in with the lenses at the first check-up. The customer should not wear the lenses at other checks, but should have them with him/her
Discuss experience: comfort, handling, compliance
Check after 3rd night
Check after
Assess the movement of the lenses. Is it good?
Remove the lenses
Visual acuity + refraction.1 Make topography
Slit lamp evaluation with fluorescein, staining?2 Capture fluorescein images
Extra check of staining at the end of the day. Staining gone?
Cease lens wear. Adjust the lenses and/or request support from Professional Services
Check again on the following day and repeat if necessary
Upload data into VISAVY® Schedule next check-up3
Determine the visual acuity s.c., overrefraction and make topography
Slit lamp evaluation with fluorescein. Staining? Capture fluorescein images
Extra check of staining at the end of the day. Evaluate (use of) care system and compliance. Staining gone?
Staining2 central: cease lens wear, increase sagittal depth and/or request support from Professional Services
Determine the visual acuity s.c., overrefraction4 and make topography
Slit lamp evaluation with fluorescein
Evaluate staining2 and/or residual power. Abnormalities?
Adjust lenses and/ or request support from Professional Services
Upload data into VISAVY® Schedule check-up after 3 months
1: Approximately 60% of the power is corrected after the 1st night
Upload data into VISAVY® Schedule next check-up
2: Dimple veiling is more common at higher powers (>-3dpt) at the level of the reverse curve. This should be gone after the start-up phase
3: If required, provide the customer with soft (daily disposable) lenses for the first days
4: The result should now be good. For higher initial powers, check again after 3 days, if necessary, before adjusting the lens
Upload data into VISAVY®. Schedule next check-up after 3 months
DreamLite® periodic check-up
Check preferably in the morning. Customer brings the lenses along, not wearing them
Evaluation: comfort, handling, compliance
Determine the visual acuity s.c. and overrefraction
Slit lamp evaluation with fluorescein
Rule out lens damage and/or contamination. Clean lenses if necessary and re-assess2 Is there any influence from damage and/or pollution?
Check preferably in the morning. Customer brings the lenses along, not wearing them
Evaluation: comfort, handling, compliance
Determine the visual acuity s.c. and overrefraction
Complaints objectively and subjectively acceptable
Evaluate refraction and topography. Adjust the lenses and/or ask for Professional Services support and evaluate after 2 weeks
1: If staining occurs, check again at the end of the day. Is the staining not gone yet? Cease lens wear & contact Professional Services
2: Improve compliance and/or care system, if necessary
Order lenses with the same parameters and re-evaluate at follow-up after 2 weeks
Order the same lenses again
Slit lamp evaluation with fluorescein
Make topography Make topography Visual acuity and/or comfort complaints Visual acuity and/or comfort complaints
addition higher
2.00
DreamLite® MC periodic check-up Check other myopia management options (like MiSight® 1 day)
• Use the 20-20-2 rule: after 20 minutes of looking at near distance, take a 20-second break to look in the distance and go outside for at least 2 hours a day.1
• Spend at least 15 hours a week outdoors 2
• Limit nearby activities (smartphone, tablet, etc.) 3
Axial length in myopes will increase on average 0.35-0.50 mm per year.4
Is the axial length progression more than 0.2 mm per 6 months or 1.00 D per year? Change the chosen myopia management strategy.
Expected degree of progression per year, per age with- or without lenses for myopia management.5
(using myopia management optical intervention)
The numbers above are averages. Some patients can deviate from the average progression. Myopia management is always an individual therapy.
When there is no progression, it is our advice to keep monitoring until the age of 25 years old.
1 Klaver CCW, & Polling JR; Erasmus Myopia Research Group. Myopia management in the Netherlands. Ophthalmic Physiol Opt 2020; 40 230_240.
2 Enthoven et al; The impact of computer use on myopia development in childhood The Generation R study; Preventive Medicine 132 (2020) 105988.
3 Rose KA, Morgan IG, Ip J, et al. Outdoor Activity Reduces the Prevalence of Myopia in Children. Ophtalmology 2008.
4 Tideman JWL, Polling JR, et a. Axial length growth and the risk of developing myopia in European children. 2018 May;96(3):301-309.
5 Gifford, K. Myopia management message part 1 - expectations. June, 2018.