FY23 Nursing Annual Report

“
Through the compassion and skill of CommonSpirit Health nurses, we’ve implemented new programs and practices to enhance patient outcomes, improve efficiencies, and foster a culture of continuous learning and professional growth.
– Kathleen D.
DBA, RN, FACHE, FAAN, CommonSpirit Health EVP and Chief Nursing Officer
Sanford,

A Tribute to Unique Contributions
First and foremost, I would like to express my heartfelt gratitude to each and every one of you for your unwavering commitment to our profession and your invaluable contributions to our ministry. Your dedication, compassion and expertise have touched countless lives and transformed health care experiences for patients, families and communities.
Kathleen D. Sanford
 DBA, RN, FACHE, FAAN, CommonSpirit Health EVP and Chief Nursing Officer
DBA, RN, FACHE, FAAN, CommonSpirit Health EVP and Chief Nursing Officer
As Chief Nursing Officer, I am pleased to welcome you to the third CommonSpirit Health Nursing Annual Report. On the pages to follow, we celebrate the remarkable achievements of the past year and look forward to the strategic priorities and supporting tactics to guide us in the year ahead.
In FY23, we achieved extraordinary milestones that have elevated the nursing profession in our organization as well as our position as a national leader in innovation. Through the compassion and skill of CommonSpirit nurses, we’ve implemented new programs and practices to enhance patient outcomes, improve efficiencies and foster a culture of continuous learning and professional growth.
Looking forward, we are excited to unveil our strategies and tactics for FY24. We will continue to prioritize patient-centered care, promote collaboration and embrace new ways of enhancing patient outcomes. We are also committed to finding solutions to current industry challenges so our nurses can thrive in their profession.
2 CommonSpirit Health Nursing
Once again, I extend my deepest appreciation to every CommonSpirit nurse and nursing care team member whose dedication to delivering exceptional care is the driving force behind our collective success. I am honored to work alongside such dedicated professionals. I believe that by continuing to work together, we will shape the future of health care and create a legacy to inspire generations to come.
Among the many nursing divisions within our ministry, we have three unique groups I would like to acknowledge for their steadfast commitment to excellence within their respective areas:

Faith Community Nurses
By addressing the spiritual dimension of care, Faith Community Nurses, or FCNs, promote a holistic approach to the physical, emotional and spiritual needs of their patients. For so many, this approach provides solace, comfort and a source of strength during challenging times. Thank you to our FCNs for helping individuals navigate through their health-related journeys, cope with stress and find meaning and hope in their circumstances.
Rural Nurses
Rural nurses are often presented with unique circumstances requiring a diverse skill set and the ability to be resourceful, adaptable and innovative in delivering care. These nurses play a crucial role in advocating for the health care needs of their communities. Thank you to all our rural nurses for their mastery in so many areas of our profession.
Once a Nurse, Always a Nurse
At CommonSpirit, nursing is a career of a lifetime. Nurses embody a set of attributes such as empathy, compassion, and a commitment to advocating for and serving others. These values are deeply ingrained, regardless of an individual’s role or career path. Our ministry is blessed to include nurses who have transitioned from traditional nursing roles and are now making a tremendous difference for our patients and communities by serving as attorneys, IT leaders, hospital presidents and more. Your colleagues know that once a nurse, always a nurse, and are grateful for the gifts you bring. Thank you to those nurses who have taken their intellect and love into a variety of areas where they can continue to serve with their head, heart and hands.
Sincerely,
FY23 Annual Report 3
SCAN OR CLICK FOR DR. KATHLEEN D. SANFORD’S VIDEO
4 CommonSpirit Health Nursing 42 National Nursing Teams Advanced Practice Providers, Behavioral Health 43 Clinical Informatics Team, Clinical Command Centers ............ 44 Patient Experience Team, Care Coordination ...............................45 Nurse Triage Department, Virtually Integrated Care (VIC) 46 Patient Care Services 47 36 Business Lines Senior Living ..........................................38 Health at Home ................................... 40 16 Divisions Northern California ............................. 18 Southern California 20 Pacific Northwest ................................. 22 Midwest .................................................... 24 Texas .......................................................... 26 Southwest 28 Southeast ............................................... 30 Centura Health ..................................... 32 Contents 06 Vision and Future Nursing by the Numbers ................. 06 CommonSpirit Health Nursing Vision and Goal.................................... 08 A Shared Purpose 09 Strategic Nursing Priorities.............. 10 The Communities We Serve (Map) ......................................14

Nursing by the Numbers
Nurses are essential health care professionals. At CommonSpirit, we recognize the quality care that nurses provide as well as their important role as patient advocates. This infographic details who our nurses are.
Totals
1,385 Nurse Practitioner
1,570 LVN/LPN
Age
34%
Nurses Comprise Nearly of CommonSpirit’s Workforce
42,533 Total Nurses
39,578 RN
Please note that this does not include registered nurses who are practicing their profession outside of a patient care department. Data effective May 1, 2022.
6 CommonSpirit Health Nursing NURSING NUMBERS
78+
Old <23 Years Old 39–60 Years Old 0.84% 48.84% 0.04% 23–39
Old 60–78
Old 39.75% 10.53%
Years
Years
Years
Forging Pathways With Academic Partnerships
As part of CommonSpirit Health’s efforts to address the ongoing nursing shortage, we have established meaningful partnerships with universities that serve multiple purposes.
First, we aim to raise awareness about the rewarding careers in nursing among young individuals. By doing so, we hope to inspire a new generation of nurses who are passionate about making a difference.
Moreover, we are focused on increasing the number of nursing graduates and fostering diversity within our profession,
recognizing how diverse perspectives fundamentally contribute to more inclusive and culturally sensitive health care.
In FY23, we established strong relationships with two esteemed institutions: the Mervyn M. Dymally College of Nursing at Charles R. Drew University (CDU) in Los Angeles, U.S.; and the Lorma College of Nursing in the Philippines.
We are excited about investing in our future nursing workforce and look forward to sharing more updates as plans unfold throughout FY24. •
2–3 Ethnicity 21.38% 11.01% 5.14% Asian 58.04% White Hispanic or Latino Black or African American 2.35% 1.06% 0.50% Unknown 0.52% Two or More Races Native Hawaiian or Other Pacific Islander American Indian or Alaskan 15+ 10–15 5–10 3–5 1–2 0–1 16.70% 11.83% 10.56% 20.37% 21.48% 11.84% 7.22% Tenure Years at CommonSpirit FY23 Annual Report 7
CommonSpirit Health Nursing Vision and Goal
The journey toward creating one, unifying nursing vision began in 2019*, when our CommonSpirit Health nurse executives across the country took time to collaborate and envision this possibility. We formed a subcommittee and launched several focus groups and surveys to gather feedback about our new nursing vision statement. In total, nearly 16,000 CommonSpirit nurses shared their thoughts about our nursing vision statement.
Today and every day, we will work together with humankindness for all to advance the science and art of nursing.
This means we will…
Be stronger together, achieving excellence in all we do, collaborating across the field and growing our collective knowledge.
Let humankindness guide us as we treat every person with holistic, personalized care for the body, mind and spirit.
Advance the science and art of nursing as innovative leaders who demonstrate the power of evidence-based, compassionate care.
Our goal is for CommonSpirit Health to be the employer of choice for nurses and their teams in a system that is widely known for outstanding patient care.
*Summer 2019: The concept of a nursing vision is born. Fall 2019: All CommonSpirit Chief Nurses invited to provide feedback about the proposed nursing vision. Spring 2020: A formal nursing vision subcommittee launches.
Summer 2020: Nursing vision focus groups begin. Fall 2020: Nearly 8,000 nurses share feedback about the proposed nursing vision statement. Spring 2021: Another 8,000 nurses share final feedback. Fall 2021 to Spring 2022: The first three Nursing Strategic Priorities are defined and implemented.
8 CommonSpirit Health Nursing VISION AND
FUTURE
A Shared Purpose
Fostering alignment and driving collaboration across all levels of the organization
When our goals and mission align with those of the overall organization, something magical happens. It creates a sense of togetherness and a shared purpose that fuels collaboration at every level. It is this spirit of unity that propels us toward success, allowing us to make a meaningful impact on the lives we touch.
In FY21, our ministry embarked on a five-year transformative journey called CommonSpirit 2026, This plan is rooted in faith, driven by innovation and fueled by our unwavering commitment to humanity.
In alignment with CommonSpirit 2026, we developed the CommonSpirit Nursing Vision and a list of tactics to help us meet that vision. Then, multiple nurses took part in focus groups to prioritize these tactics. This ambitious plan focuses on excellence and empowerment of our nurses. We believe that by providing an environment where nurses can work at the pinnacle of their capabilities, we enable them to deliver the highest quality of care to those we serve.
The CommonSpirit Nursing Vision encompasses priorities that harmonize with our ministry-wide plan and ensure we achieve our nursing goals. We aspire to be recognized as the preferred employer for nurses and their teams, renowned for the exceptional patient care we provide. We are committed to giving our nurses a voice, while offering them genuine appreciation for their tireless efforts. Furthermore, we are determined to empower them to make valuable contributions, paving the way for a lasting legacy of excellence that will endure for generations.
The nurses who contributed to our vision were passionate about standing together as a unified force dedicated to serving our mission. Our journey is guided by compassion, innovation and the dedication to the health of our communities. With this shared vision, we will continue to transform lives, create a brighter future and forge a path of healing and hope for all who seek our care. •

FY23 Annual Report 9
Year One Priorities in Action
Strategic Nursing Priorities: Powering progress with a focus on excellence and empowerment of our nurses
To carry out the CommonSpirit Health Nursing Vision, our priorities must ensure CommonSpirit nurses:
With a steadfast focus on these priorities, we made remarkable strides toward our goals in FY23.
Nurse Residency Program
Have a voice.
Know they are appreciated.
Are supported during their professional journey.
With the help of many of our nurses within subcommittees, focus groups and feedback sessions, we chose three distinct priorities and supporting tactics for Year One:
Develop a comprehensive, ministry-wide Nurse Residency Program.
We designed our Nurse Residency Program to help new nurses gain connections, professional development, coaching, mentorship and consistent feedback as they transition from academia to practice. As we end FY23, we are in the process of implementing this program across the system, and all new graduates will be expected to spend a whole year in this program.
To monitor the program’s success, we have created a dashboard to gauge how residents are progressing in their early professional journey. So far, we are hearing great things!
Expand our Virtual Nursing Program.
We are off to an excellent start with cohorts in our Texas, Arizona and California markets and recently started a new cohort in Northern California. Our goal is to have a residency in every hospital within 12 months. That means in one year, all of our nurses will have a Nurse Residency Program in their market.
Create our own Internal CommonSpirit Nurse Staffing Agency.
10 CommonSpirit Health Nursing VISION AND FUTURE
SCAN OR CLICK FOR NURSING RESIDENCY PROGRAM VIDEO
SCAN OR CLICK FOR

Virtual Nursing Program
We’re so proud of our patented Virtual Nursing Program, which CommonSpirit launched over 10 years ago. In 2008, the CHI Board of Stewardship Trustees approved virtual nursing as part of its long-term vision to address an impending shortage of nurses. We quickly recognized Virtually Integrated CareSM as a model for the future and rolled out pilot programs in the Midwest, Kentucky and Denver. In 2018, the U.S. Patent™ Office granted CHI the very first Virtually Integrated Care (VICSM) patent.
Virtual nurses partner with on-site nurses and other team members to lighten the workload on bedside care teams and reduce their operational challenges. Also, virtual nurses give patients additional reassurance that an entire team is contributing to their well-being. Early results show nurses and patients like this new model, and this new way
of caring is already helping reduce lengths of stay and improve the quality of care. We intend to roll out virtual nursing soon in the Pacific Northwest, Midwest and Texas. Our goal is to have VIC programs available across the entire ministry by the end of FY24.
Internal Staffing Agency
We launched our own Internal CommonSpirit Nurse Staffing Agency in FY23. With about 40 nurses on board, we are on our way to achieving our goal of 200 internal agency nurses in our markets by the end of CY24.
This program allows CommonSpirit nurses to pursue travel opportunities while retaining their seniority and health benefits. It also adds flexibility to CommonSpirit nursing careers and a more consistent patient experience from nurses already familiar with CommonSpirit Nursing’s values, policies and procedures. •

FY23 Annual Report 11
SCAN OR CLICK FOR INTERNAL STAFFING AGENCY VIDEO
VIRTUAL NURSING PROGRAM VIDEO
Year Two Priorities: Coming Into Focus
Planning for the future by nurturing personal growth, collaborative governance and workplace well-being
Because we believe strongly that nurses must have a voice in planning the future for CommonSpirit Health Nursing, we held focus groups with frontline nurses to guide the creation of our FY24 priorities and tactics. Based on feedback from those sessions, we are ready to start working on these Year Two priorities.
Shared Governance
Our first priority is shared governance across the ministry. This aligns with our vision of ensuring our nurses have a voice but takes that notion a step further by ensuring our nurses have a hand in decision-making processes. Shared governance will also empower our nurses to contribute to patient care improvements and overall organizational effectiveness.
This is our top priority for Year Two since it will guide the other three priorities. We intend to hold another
round of focus groups led by Connie Clemmons-Brown, DNP, RN, MBA, CENP, System SVP, Patient Care Services, to find out specifically what our nurses mean by shared governance and what the tactics should be within this priority.
Individual Career Growth
Our second priority is to provide our nursing care team members with mobility in their profession. Examples include transitioning to another specialty (including the specialty of nursing management), becoming a travel nurse or choosing to transition to a non-traditional nursing role.
We have ideas on what the tactics within this priority might entail, but again, we want to ensure our nurses have a voice. So, we’ll be holding additional focus groups to shape this priority further.

12 CommonSpirit Health Nursing VISION AND FUTURE
Looking at Productivity in New Nursing Models
As we move into the future, there will be opportunities to utilize our CommonSpirit nurses’ skills along with new technology. CommonSpirit nurses have expressed the desire to reexamine productivity measures based on these new models. Our goal is to ensure we can deliver outstanding patient care efficiently and effectively. As such, we’ll be taking a closer look at productivity across our ministry and, with the help of our nurses, will devise tactics around this priority for FY24.
Resilience and Well-Being
All of us at CommonSpirit recognize that nursing can be a demanding profession, both physically and emotionally. We will continue to emphasize the importance of workplace well-being to ensure our nurses are emotionally and physically resilient.
We are committed to keeping a pulse on the needs of nurses and their teams, as these may change over time. We will do this by continuing to ask nurses: What can make our nursing jobs better? How can we ensure our nurses find joy in their jobs? What makes them feel safe? What makes them happy and fulfilled in their jobs every day? The answers to these questions will be added to our tactics as we pursue a future where our nursing vision becomes a reality.
These FY24 priority tactics will take shape in the weeks and months ahead as we all work together toward our goal to make CommonSpirit the employer of choice for nurses and their teams in a system that is widely known for outstanding patient care. •

FY23 Annual Report 13
Communities We Serve
The map below is reflective of CommonSpirit Health’s FY23 footprint. In FY24, the map will be updated to reflect our ministry’s expansion into new regions and the division consolidations that went into effect in the new fiscal year.
14 CommonSpirit Health Nursing
Northern California
Pacific Northwest
Southwest
Southern California
DIVISIONS • MAP
FY23 Annual Report 15 Southeast
Texas Midwest
Centura Health
Divisions
Elevating the nursing profession while implementing the CommonSpirit Health Nursing Vision in countless geographies across the U.S.*
*The data and information in the Divisions section reflects the structure of CommonSpirit Health in FY23.

16 CommonSpirit Health Nursing

FY23 Annual Report 17
Excellence Amid Change
Coming together to find extraordinary solutions to enhance patient outcomes

The DAISY Award: Revitalizing Recognition

Following the pandemic, many hospitals paused The DAISY Award program, a recognition program that expresses gratitude to nurses everywhere. This past year, the Chief Nursing Officers in the Northern California Division came together to standardize The DAISY Award program across the division. The teams also worked with The DAISY Foundation to revitalize programs that have existed for many years and start new ones.
National Nurse Residency Program
The Northern California Division established the National Nurse Residency Program in April with its first cohort of 20 graduates from Dignity Health Mercy General Hospital. The team is phasing in program adoption by facility readiness. Dignity Health Mercy San Juan Medical Center and Dignity Health Mercy Medical Center Redding started cohorts in June. The Northern California Division will have the opportunity to improve the experience of new graduates, allowing them to be confident and competent after one year in the program.
18 CommonSpirit Health Nursing
Above, left to right: Michelle Hoang, DAISY winner; Northern California Division 2022 Retreat; hospital workers at Dignity Health in Rancho Cordova, California.
DIVISIONS • NORTHERN CALIFORNIA
“Over the past year, our nurses have proven their resilience and excellence again and again in this ever-changing world of health care.”
Noteworthy Numbers
Northern California Division
16,185 Employees
6,692 Total Nurses
Staffing Strategy Task Force
Establishing a Staffing Strategy Task Force for the Northern California Division has been vital to helping address the nursing staff shortage as well as many other clinical staff shortages. The team saw success with numerous tactics, including the Traveler Conversion Bonus and Surgical Tech Tiered Competency job descriptions. In addition, the task force has been communicating with leaders from new nursing programs and improved its website to help attract potential employees.
2,901 Total Beds
“Despite challenges in 2022, our teams have united to find solutions. Leaders and caregivers need to continue coming together to keep patient safety the center of our decisions.”

99,089 Inpatient Admissions
1.2M Outpatient Admissions
Numbers are approximate.
— Karen L. Buckley
Division Fact
First-year nurse retention is at 76.4 percent, and overall first-year employee retention is at 78.1 percent, which ranks the Northern California Division as the highest in these categories within CommonSpirit Health. •

FY23 Annual Report 19
— Karen L. Buckley, RN, BSN, MHA, CENP, Chief Nurse Executive Officer, Northern California Division
An Eye On Innovation
Answering the call with a desire to make a meaningful difference in the lives of others
Impressive New Graduate Numbers
The Southern California Division is immensely proud of its new graduate recruitment strategy and FY23 results, having hired 724 new graduates. The division accomplished this impressive feat through collaborative partnerships with dozens of universities, colleges and professional nursing organizations.

Outreach Workgroup
The Southern California Division has successfully strengthened its community relations by establishing a work group to enhance its outreach efforts. Its Nursing, Talent Acquisition and Communications teams have partnered to raise public awareness of its nursing opportunities,


20 CommonSpirit Health Nursing
Above, top to bottom: Dr. Ron Yolo, center, with Gloria Carter, CNO, St. Mary Medical Center - Long Beach (left) and Erin Keefe, CNO, St. Bernardine Medical Center (right) at the Annual American Organization for Nursing Leadership (AONL) Conference in Anaheim, California; Dr. Ron Yolo presenting to new grad students at Charles R. Drew University’s School of Nursing as part of CommonSpirit Health’s new grad nurse recruitment efforts.
DIVISIONS • SOUTHERN CALIFORNIA
“Thank you for your dedication, your passion and your unwavering commitment to our patients, communities and organization. You are appreciated!”
— Ron Yolo, DNP, MBA, MSN, RN, Chief Nurse Executive Officer, Southern California Division
programs and resources. The Southern California Division proudly represents CommonSpirit Health Nursing at events throughout the year for the Association of California Nursing Leaders; the American Organization for Nursing Leadership; and CommonSpirit Health’s academic partner, Charles R. Drew University.
Innovative Division Nursing Recruiter

In FY23, the Southern California Division piloted an Innovative Division Nursing Recruiter role that specializes in screening, interviewing and hiring nurses. Kim Flanders, MSN, CNM, a retired Chief Nursing Officer with extensive experience, has filled this position. The addition of this role has already resulted in expediting the hiring process while streamlining onboarding for new nurses, which has resulted in increased satisfaction among department managers and nursing leaders. •
“Nursing is a philosophical calling. It involves a deep commitment to caring for others, a profound understanding of human nature and a strong ethical foundation.”
— Dr. Ron Yolo
Noteworthy Numbers
Southern California Division
23,768 Employees
10,643
Total Nurses
4,382 Total Beds
199,929 Inpatient Admissions
2.2M Outpatient Admissions
Numbers are approximate.
FY23 Annual Report 21
Shaping the Future of Health
Initiatives and strategies driving transformation for a promising future
Enhanced Collaborative Care Program
In support of the Year One priority for CommonSpirit Health’s Virtually Integrated CareSM program, Virginia Mason Franciscan Health (VMFH) launched a virtually integrated model at CHI St. Anthony Hospital in Gig Harbor, Washington, known as the Enhanced Collaborative Care Program. The model integrates a virtual team of nurses as members of the inpatient team who can connect to patient rooms with the touch of a screen. The Enhanced Care registered nurse (RN), as part of the care team, supports workflows that drive the plan of care, admissions, discharges, transfers and care team communication. VMFH
Enhanced Care RNs are experts who assist in unburdening the bedside care team by taking on tasks that interrupt or delay clinical care and were previously handled by frontline nurses only.
New Float Pool Program
To assist with staff vacancies while managing costs, VMFH launched a new regional float pool strategy, allowing travel nurses to float within the division.
Noteworthy Numbers
Pacific Northwest Division
17,051 Employees
4,862 Total Nurses
1,656 Total Beds
400,252 Inpatient Admissions
1.7M Outpatient Admissions
Numbers are approximate.
22 CommonSpirit Health Nursing
DIVISIONS • PACIFIC NORTHWEST
The team is also using a regional approach to fill scheduling gaps based on the immediate needs of each hospital. The goal is to provide regional travel nurses across the division with equitable assignments, leadership support, fair pay and eventually, an incentive to join VMFH as a full-time nurse at the hospital of their choice.



Nurse Residency Program
As part of the Year One priority to start a National Nurse Residency Program, VMFH is investing in its talent pipeline and will launch its new nurse residency program in FY24.

“Nurse residency programs are the gold standard for new nurses, and I am honored to help launch our new program. I look forward to our success on this journey together.”
During the 12-month program, nurses will gain more experience through an evidence-based curriculum delivered through carefully crafted, state-of-the-art learning technology and instructional design. •
FY23 Annual Report 23
— Julie Gardner, MSN, RN, PCCN-K, NPD-BC, PNW Division Director, Nurse Residency Program
“Nursing is the heart of health care, and our nurses will continue to play a critical role in shaping the future of medicine.”
FY23 Annual Report 23
— Dianne Aroh, RN, NEA-BC, FACHE, PNW Division SVP & Chief Nursing Officer, Virginia Mason Franciscan Health
Clockwise from left: Members of VMFH at the Tacoma-Pierce County Economic Development Board Annual Meeting; volunteers at community event; nursing residents from St. Michael Medical Center.
Harnessing Change to Enrich Patient Lives
Resilient hearts, saving lives: navigating nursing through challenging times
Triage Nursing Improvements
In FY23, the nursing leadership team at CHI St. Alexius Dickinson worked to revise and implement requirements for staffing a triage nurse in its Emergency Department. They have also developed a new competency for training triage nurses along with additional training that has been rolled out for the rest of the team.
CHI St. Alexius Dickinson has seen positive results from this work and has reduced the rate of early departures to less than one percent. They have also significantly reduced door-to-doctor times, which has resulted in more positive feedback from patients.
With the recent release of the fifth edition of the Emergency Nurses Association’s Emergency Severity Index (ESI) Handbook, the core team intends to develop and provide ESI training to all staff.
Safety First
The Midwest Division is using this challenging time as an opportunity to make changes to improve the lives of its patients and make care delivery more efficient for nurses. The team has a few initiatives in development,
Noteworthy Numbers
Midwest Division
13,000
Employees
3,246
Total Nurses
2,833
Total Beds
67,000 Inpatient Admissions
1.5M Outpatient Admissions
Numbers are approximate.
24 CommonSpirit Health Nursing
DIVISIONS • MIDWEST
including exploring new care models and using technological innovations. However, it is important for everyone to remember the basics. Over time, the Midwest has developed safety guardrails and checklists designed to provide a consistent, safe experience for not only patients but also nurses. The Midwest Division has realized long-term success with the hourly rounding and ISHAPED (I = Introduce, S = Story, H = History, A = Assessment, P = Plan, E = Error Prevention and D = Dialogue) bedside report as a key safety measure. The effectiveness of this safety measure is shown in the increase in patient experience scores that show a 90 percent effectiveness rate for ISHAPED bedside reports.

Virtual Nursing Program
In conjunction with the Year One priority to expand CommonSpirit Health’s Virtually Integrated CareSM (VICSM) program, CHI Health Lakeside recently kicked off a VIC nursing program that will expand to CHI Health Creighton University Medical Center - Bergan Mercy and CHI Health Immanuel in the first quarter of FY24. •


FY23 Annual Report 25
“From a safety perspective, following scripts and checklists every single time is essential as we navigate this tumultuous time in nursing.”
FY23 Annual Report 25
— Tim Plante, RN, MSN, MHA, SVP, Chief Nursing Officer, Midwest Division
Above, top to bottom: Volunteers at a Pink Out event for Creighton University; groundbreaking of the IMC Clinic in Omaha, Nebraska.
Paving the Way for the Future of Health Care

Delivering compassion and kindness during life’s most precious moments
Inaugural Residency Program Cohort
Texas Division education specialists launched the inaugural cohort of CommonSpirit Health’s National Nurse Residency Program (NNRP) and Preceptor Development Program in spring 2023. Both programs were largely influenced by training developed in the Texas Division. Following the NNRP implementation, all Texas markets will seek accreditation in 2024. Heather Wallace Ph.D.(c), RN, NPD-BC, who was recently promoted to Division Director, NNRP, will lead the project with Division SVP and Chief Nurse Executive Officer Dr. Veronica Martin.

Simulation Center
Mastering nursing skills to develop confident, efficient nurses requires hands-on training, and the Simulation Center at Baylor St. Luke’s Medical Center — funded in part by Friends of Nursing — provides a low-risk, handson forum that allows graduate nurses to perfect their skills. It also serves as a crucial training tool for experienced nurses and clinical staff looking to master more advanced skills to improve patient outcomes and enhance the patient experience. Educational staff use the Simulation Center to facilitate learning activities on new equipment
26 CommonSpirit Health Nursing
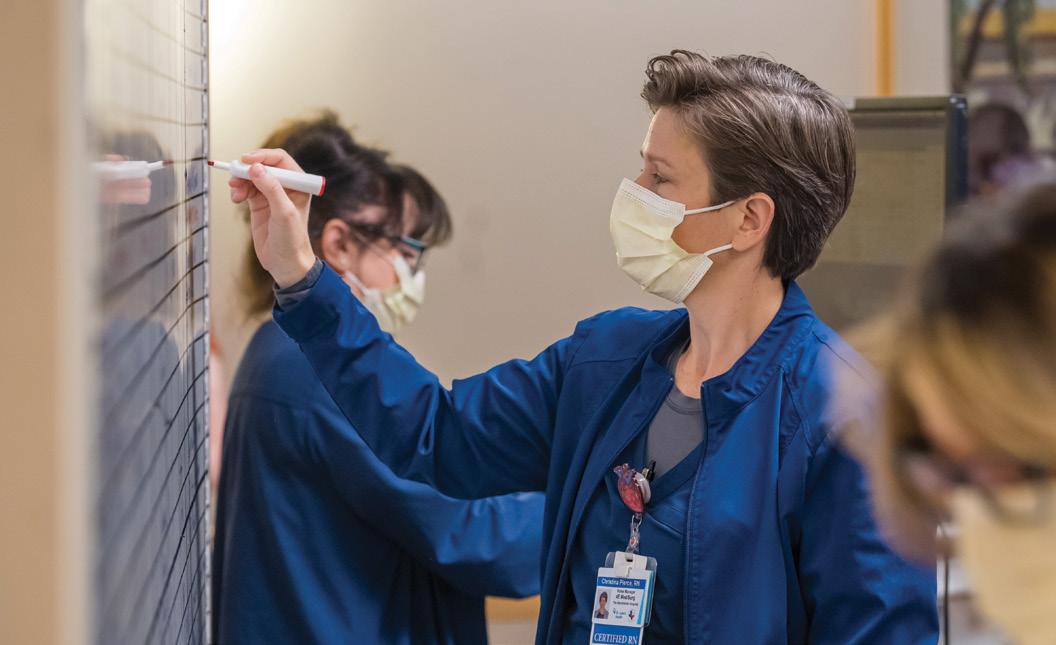
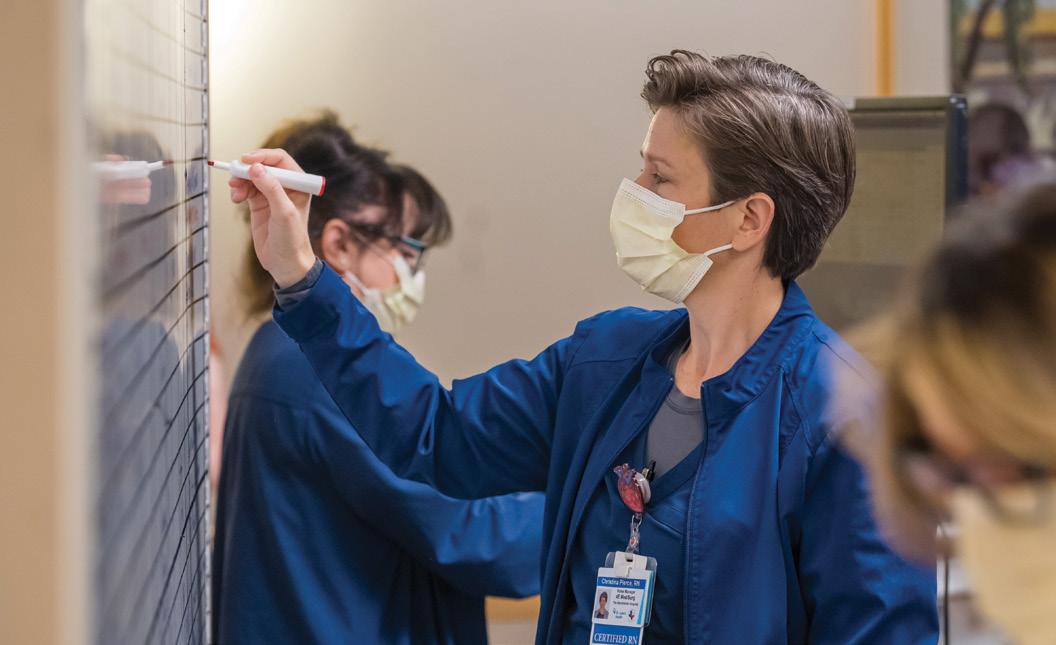
Above, left to right: Deena Khalil, RN, and Dr. Nabil Khoury, from The Vintage Hospital; The Vintage Hospital staff, (Left to Right) Rose Guzman, RN, Linda McCrosky, Dr. Risheng Xu, Mario Garner, Grace Gulapa, RN, Lisa Hansel, RN, Makia Bundu, RN, and Keitha Vanhorn; Christina Pierce, RN, from The Woodlands Hospital.
DIVISIONS • TEXAS
Noteworthy Numbers
Texas Division
11,576 Employees
4,466
Total Nurses
2,606
Total Beds 63,943 Inpatient Admissions
778,519 Outpatient Admissions
Numbers are approximate.
and training for disciplines such as respiratory care and advanced practice care.
Including 12 rooms used for task trainers, virtual reality resources, simulator devices, consumable equipment storage and three high-fidelity simulators, this technologically advanced simulation center allows educators to share active learning scenarios, resources and tips among all facilities across the division. Monitors display scheduled classes, locations and directions to each activity. In 2022, the Simulation Center facilitated 2,564 hours of clinical education.
Nursing Research and EvidenceBased Practice

The St. Luke’s Health nurse collaborative lives and breathes an inclusive nursing vision that supports the communities it serves. These nurses promote and champion a spirit of inquisitiveness while striving for the highest degree of excellence in service to patients and each other. •
FY23 Annual Report 27
“Nursing demands unwavering mental and physical toughness tempered with compassion and patience to care, to reassure, to celebrate and to comfort.”
— Veronica Martin, DNP, RN, NEA-BC, Division SVP and Chief Nurse Executive Officer, Texas Division
Pioneering New Frontiers
Displaying
Record-Breaking Emergency Visits
The 50-bed Dignity Health Arizona General Hospital Mesa, 16-bed Arizona General Hospital Laveen and 12 freestanding Arizona General Emergency Departments (EDs) kept up their record-breaking pace and are on track to post more than 200,000 ED visits. Adapting to the pressure, nurses developed and implemented a Fast Track Triage process that reduced left-without-being-seen patients by 40 percent. Teams also developed and implemented a successful ED Tele-Triage pilot, set to expand in FY24.
Nurse Apprentice Program

The Dignity Health St. Rose Dominican Hospitals in Henderson and Las Vegas, Nevada, strengthened their workforce pipelines by resurrecting their Nurse Apprentice Program.

“Our nurses continue to trailblaze, collaborate and innovate to advance nursing with humankindness as a potent differentiator in our markets.”

28 CommonSpirit Health Nursing
— Robin Shepherd, DNP, MSN, BSN, RN, CENP, Former Division VP and Chief Nurse Executive Southwest Division
Clockwise, from top: Dignity Health AHA trainers volunteer at an event; hospital staff at St. Joseph’s Hospital and Medical Center in Phoenix, Arizona; Malia Keliinoi, Adrienne Braccalarghe and Ariadne Jensen celebrate graduation from the St. Rose Nurse Apprentice Program.
DIVISIONS • SOUTHWEST
honor, teamwork and a culture of excellence as we align under One CommonSpirit
This helped the team quickly respond to a call to action by the governor of Nevada in support of the nursing workforce, along with the specialty Nurse Internship Programs for nurses wishing to become ED, Intermediate Care or Labor and Delivery nurses.
Program Pioneers
Dignity Health Yavapai Regional Medical Centers were the first in the Southwest Division to launch CommonSpirit Health’s National Nurse Residency Program and CommonSpirit Health’s Virtually Integrated CareSM program. Yavapai Regional Medical Center East and Yavapai Regional Medical Center West are the only hospitals in a 150mile radius in rural Yavapai County. The nurses at these facilities continue to model the pioneering spirit of the founding Sisters of Mercy, who opened the first hospital in Prescott, Arizona, in 1896 that would later become Yavapai Regional Medical Center.
Division Fact
At Dignity Health Chandler Regional Medical Center and Mercy Gilbert Medical Center, nurses participated in the development of “Excellence Every Day, Every Way,” a dual-campus methodology for inspirational improvement in quality, safety, experience and stewardship.
With a mission to serve their community, St. Rose Dominican Hospitals’ nurses took the initiative to become American Heart Association trainers for blood pressure self-monitoring and held events to train new community facilitators. •

Noteworthy Numbers
Southwest Division
17,192 Employees
6,410
Total Nurses
1,918
Total Beds
118,965 Inpatient Admissions
1.8M Outpatient Admissions
Numbers are approximate.
FY23 Annual Report 29
Valued Partners in Quality Care
Improving and innovating while adjusting to the new normal
Virtual Nursing
This past winter, CHI Saint Joseph Hospital in Lexington, Kentucky, was the first to implement the Virtually Integrated CareSM (VICSM) program in support of CommonSpirit Health’s Year One priority.
The VIC program is a team model that enhances patient care using in-room technology. On-site staff members receive support from virtual nurses who use CommonSpirit Health’s proprietary Virtual Care Delivery Platform to connect with audio and video to patient rooms. The virtual nurses are integral team members working with the bedside care team to deliver enhanced care to patients.
Partnering with the CommonSpirit command centers, the Southeast Division has also implemented remote virtual patient sitters, added patient discharge workflow support for virtual registered nurses in two facilities and connected one facility’s cardiac telemetry to the command center central monitoring unit.
International Nurse/Academia Partnerships
In FY23, the Southeast Division recruited 350 experienced international nurses, with 70 new nurses already serving at CHI St. Vincent in Arkansas.
Noteworthy Numbers
Southeast Division
14,449 Employees
4,947 Total Nurses
2,817
Total Beds
83,100 Inpatient Admissions
1.6M Outpatient Admissions
Numbers are approximate.
30 CommonSpirit Health Nursing
DIVISIONS • SOUTHEAST
Market leaders across the division partnered with colleges and universities, providing funding for teaching positions as well as scholarships for nursing students. By strengthening partnerships with historically Black colleges and universities (HBCUs) in Arkansas, Kentucky and Tennessee, the team is helping to increase the diversity of caregivers for the greater good of its communities.
A Commitment to Lifelong Education
The CHI Memorial Hospital in Chattanooga, Tennessee, hosted the American Board of Cardiovascular Medicine to teach the Cardiovascular
“This team is focused on transformational leadership, evidence-based practice and innovative workflows to achieve excellent outcomes. I am grateful to be part of such a highperforming team.”

Nurse Board Certification review course on-site over a weekend in January. Thirty-two CHI Memorial Hospital nurses completed the certification with a 100 percent pass rate, demonstrating their commitment to lifelong learning. •


FY23 Annual Report 31
— Melissa Roden
“As we emerge from the pandemic, we celebrate our nurses who continue to provide excellent care to those they serve.”
FY23 Annual Report 31
— Melissa Roden, RN, BS, CPHQ, Chief Nurse Executive and Chief Quality Officer, Southeast Division
Top to bottom: Arkansas international nurses and executive team; RNs pose in a hospital hallway.
Showcasing Excellence in Action
Initiatives aimed at responding to the feedback and priorities of frontline nurses
Enhanced Decision-Making Through Shared Governance
In July 2022, Centura launched Quest, an enterprise nursing professional shared governance model. Through this model, each facility sends two frontline registered nurses and one nurse leader to represent their respective areas at the Quest Nursing Professional Shared Governance Assembly meeting. Each month, Assembly members review upcoming decisions such as policies, practice and workflow changes. Since implementation, members have approved more than 115 decisions to enhance nursing practice, the practice environment and patient care outcomes.
Virtual Sitter Program
There are times when patients who could be monitored as part of a group are assigned a one-to-one approach, putting a strain on nurse resources. To alleviate this strain, provide support and enhance the work environment, Centura Health has expanded its virtual sitter program. As a result, the team has been able to support a safer care environment for patients while freeing up local resources to work more broadly with their teams.
Noteworthy Numbers
Centura Health Division
21,000 Employees
6,000
Total Nurses
2,592
Total Beds
Numbers are approximate.
32 CommonSpirit Health Nursing DIVISIONS • CENTURA HEALTH
Opposite, top to bottom: A hospital staff member speaks at Clinical RN event; Clinical RN Assembly Kickoff.
RN Clinical Ladder Implementation
Centura Health implemented a new, enterprise-wide RN Clinical Ladder program in January 2022. This program is offered twice a year and is focused on recruiting and retaining bedside nurses while supporting their professional development.

In January 2023, over 700 nurses from the program’s first year submitted their portfolios. These demonstrated their involvement in ongoing education, community activities, professional organizations, councils and committees that help to improve the practice environment and patient outcomes.


Telemetry Monitoring
This year, Centura Health focused on the centralization of the Telemetry Monitoring team as well as the Virtual Sitter team. The goal is to ensure patient safety while effectively and efficiently allocating resources. By centralizing the work of these two teams, Centura Health was able to increase patient coverage and reduce the use of inperson sitters at the facility level.
Centura Transition
Centura has a long history of serving patients and communities through a joint operating agreement with another system. In FY24 we will welcome the CommonSpirit Health–owned entities as part of a new division that will include additional facilities located in Utah. The exceptional nursing programs initiated by Centura complement the CommonSpirit nursing strategy as well as FY24 priorities. •
FY23 Annual Report 33
“Centura is dedicated to enhancing the practice environment, increasing the frontline voice in decisionmaking and supporting safety through several initiatives this year.”
FY23 Annual Report 33
— Brenda Simpson, DNP, RN, CENP, SVP and Chief Nursing Officer, Centura Health





34 CommonSpirit Health Nursing
Nurses are the backbone of our organization. Their dedication to the profession is inspiring. Their intelligence and talents are astounding.







FY23 Annual Report 35
Business Lines
Pioneering innovation while meeting patient needs with unwavering compassion and humankindness

36 CommonSpirit Health Nursing

FY23 Annual Report 37
The More You Know, the More You Grow
Providing safe, nurturing care to aging individuals

CommonSpirit Senior Living
(also known as CHI Living Communities by prospective families, residents and the public) offers independent living, assisted living, skilled nursing, rehabilitation and memory care services on 13 campuses in eight states. The mission-minded team members within Senior Living care for more than 2,200 residents daily.
In FY23, CommonSpirit Senior Living continued its pursuit of excellence in providing safe, nurturing senior care services for its residents. Its accomplishments include:

Reduced Pressure Injuries
For aging adults, pressure injuries are not only painful but can also lead to serious infections and debilitating effects. These injuries also increase costs for our ministry. CommonSpirit Senior Living made pressure injury prevention a central clinical focus in FY23, resulting in a decrease in resident pressure injuries. Pressure injuries dropped from 7.5 percent to six percent, as compared to the national average of 8.2 percent. Although the team is pleased with this accomplishment, they remain dedicated to reducing this percentage further in FY24.
38 CommonSpirit Health Nursing BUSINESS LINES • SENIOR LIVING
Above, left to right: Joan Zidor (left), STNA, at St. Leonard near Dayton, Ohio, thoroughly enjoys caring for Nilah L., one of her assisted living residents; Regional Clinical Director Paula Keller, RN, at a Senior Living’s West Region campus; Dr. Ja’Nay Crippen-Derry (center), VP of Clinical Operations, with a few of her nursing leaders at CommonSpirit Senior Living’s annual Leadership Meeting in July 2022.
Noteworthy
Noteworthy Numbers
1,650 Employees
289
Total Nurses
2,237 Number of Residents:
1,227 Short-Term Rehab Residents
Numbers are approximate.
Increased Overall Quality Score
The Centers for Medicare & Medicaid Services (CMS) use a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health plan and health care system. It is referred to as the Star Rating Program, and the national average is 3.7 out of five.

CommonSpirit Senior Living’s overall CMS star rating greatly improved in FY23, surpassing the national average by almost half a point. Specifically, the team scored a 4.1 out of five for overall quality. The team attributes this improvement to regular meetings with nursing leaders where Dr. Ja’Nay Crippen-Derry, VP of Clinical Operations, emphasizes stringent quality standards. She also guides nurses on how to perform a deep dive into any areas they can improve upon so the team can identify and resolve obstacles.
Professional Development Growth
The CommonSpirit Senior Living team believes the more you know, the more you grow. That’s why this past year, they focused their efforts on developing additional professional growth opportunities. As a result, the team is piloting a state-tested nursing assistant ladder as well as a nurse ladder so caregivers can continue advancing their skills. Senior Living nurses also have the opportunity to participate in Duke University’s Leadership certificate program through Dignity Health Global Education, and many were proud to successfully complete this work in FY23. •

FY23 Annual Report 39
“I encourage nurses to search fearlessly for positive outcomes, check paths to resistance and break down barriers in their quest for gratitude and humility.”
— Ja’Nay Crippen-Derry, DHA, MSN, RN, Vice President of Clinical Operations, CommonSpirit Senior Living
Together, We Are Better
Listening and learning to cultivate new best practices
CommonSpirit Health at Home provides care to patients in home health, home hospice and inpatient hospice settings. With 1,492 nurses working across 49 home care and 26 hospice locations, the team provided care to 85,151 patients in FY23.

In FY23, CommonSpirit Health at Home was faced with challenges exacerbated by the COVID-19 pandemic, such as stress and burnout, which created a crisis that threatened the health of workers, patients and communities. It also provided the team with an urgent opportunity to find solutions to properly care for those who care for others.

During the year, Health at Home sought to address these challenges by hosting strategic listening sessions and feedback reviews to encourage nurses to share their voice and be heard — making it a priority to stop and really listen to what nurses were saying. How did they feel? What did they need? What did they want?
Clockwise, from top: Melinda Mills, RN, reads with a home care patient; an RN visits patient at their home; a home care RN checks patient’s blood pressure.

40 CommonSpirit Health Nursing BUSINESS LINES • HEALTH AT HOME
“We are blessed to work with such a diverse, dynamic group of nurses where we can positively impact health care, together!”
— Andrea Callahan, RN, Director of Clinical Optimization, CommonSpirit Health at Home
To help balance nurses’ workload and to extend the humankindness delivered to patients every day by the team, the Health at Home team captured thoughts and ideas and promptly delivered on the actionable items. Some of these included:
• Forming a Change Request team to capture thoughts and ideas generated by frontline staff and others across CommonSpirit Health at Home.
• Creating an Onboarding Task Force charged with leveraging technology and innovation to design a streamlined, comprehensive program to support new nurses and all new employees.

• Removing redundancy and duplication across clinical documentation processes, thereby reducing the burden on team members.
• Integrating partners to support safer medication management as well as providing after-hours patient triage services and remote visit capabilities.
Designed to increase satisfaction and strengthen retention, this work allowed nurses to spend more time providing quality care to patients. By leveraging technology and aligning resources, CommonSpirit Health at Home was also able to provide extra layers of support where it is needed most. With the nursing shortage still at hand, the team is committed to continue finding innovative ways to help nurses balance their day-to-day work, so there is less of a burden on their personal lives while continuing to provide excellent, high-quality patient care.
Noteworthy Numbers
4,509 Employees
1,492 Total Nurses
85,151 Outpatient Visits
Numbers are approximate.
FY23 Annual Report 41
National Nursing Teams
Leading the charge to promote healthy populations and enhance care and outcomes for patients, families and communities

TEAMS
NATIONAL NURSING
Promoting Healthy Communities
Unleashing the power of excellence
The National Office of Advanced Practice ensures the effective and strategic utilization of Advanced Practice Providers (APPs) across the care continuum and all geographies. As a diverse group of strategic, clinical and operational experts, the team promotes economically sustainable, interprofessional, patient-centered care delivery models to promote healthy populations. In FY23:
• In partnership with physician enterprise (PE), the National Office of Advanced Practice launched the Physician and APP Mentoring Program to support newly hired physicians and APPs.
Nurturing Hearts and Minds
Embracing holistic approaches
The Behavioral Health Clinical Council evaluates, develops and executes strategies to ensure a holistic approach to behavioral health care. The team prides itself on being a national and regional leader and a community advocate. In FY23, the team:
• The National Office of Advanced Practice and the Midwest Division Advanced Practice Leadership and Hospital Medicine Leadership teams launched the Hospital Medicine APP Bootcamp and Fellowship Program to support newly graduated APPs and ensure their competence to serve patients.
• The team launched the Advanced Practice Provider Strategic Workforce Planning and Performance Portfolio in partnership with PE Transformation and Innovation. •
“Thank you for your leadership, passion and diligence in building strong care teams to serve our communities and fulfill our mission.”
— Barbara Martin, PHD, ACNP-BC, MPH, System SVP, Advanced Practice

• Developed an internal well-being initiative that includes appropriate mental health support. The team also has plans for an internal Peer Ambassador program in FY24, patterned after other successful peer support models.
• Piloted a placement platform in Sacramento, California, to significantly improve the process of placing behavioral health patients from Emergency Departments into appropriate psychiatric services.
• Partnered with the American Hospital Association (AHA) and other hospitals and health systems to identify and disseminate best practices for suicide prevention. The Behavioral Health Clinical Council team has also developed an action plan for the AHA suicide-prevention initiative, a monumental feat for a system of CommonSpirit Health’s size. •

FY23 Annual Report 43
“I am proud to work with an organization that lives its mission, especially concerning mental health, to truly make a difference.”
— Paul Rains, RN, MSN, System SVP of Behavioral Health and President of St. Joseph’s Behavioral Health Center
Empowering Care Through Data
Driving health care delivery excellence
The Clinical Informatics (CI) team is a collaborative group of nursing professionals, physicians and informatics professionals who oversee data to advance health care delivery. The CI team continues to develop streamlined processes to optimize the electronic health record (EHR) and realize efficiencies in patient care and outcomes. In FY23:
• The CI team was on the ground during CommonSpirit Health’s cybersecurity event, partnering with operational leaders to facilitate recovery and support downtime processes.
Revolutionizing Health Care Delivery
Bridging distances with remote support
Clinical Command Centers enable divisions to advance unified clinical standards, offer enhanced services and manage resources more efficiently across larger geographies. The Command Centers provide communication, coordination and clinical services. In FY23, the team:
• Throughout Kentucky, seven EHRs were converted to one instance of EPIC. The entire team supported its end users on the go-live date and provided just-in-time training while collaborating with the Information Technology team to resolve issues.
• The annual KLAS Research survey included a section on nursing for the first time in FY23, which provided valuable insights into nurses’ perception of EHRs. •
“The end goal is to improve the relationship with the informatics systems that support the work of assuring improved patient care.”
— Linda Goodwin, MSN, MBA, FACHE, System SVP, Nursing Transformation, Virtual Care Innovation and Nursing Informatics


• Operationalized two central command centers for California/Nevada and Arizona.
• Monitored more than 13,000 patients and more than 22,000 adverse events through enhanced virtual companion monitoring.
• Led, optimized and operationalized services for virtual registered nurses and virtual technology for the Admission/Discharge Transfer System (a system that allows patient information to be shared with other health care facilities and systems) using existing resources from three command centers.
• Extended virtual patient care in six states, decreased length of stay, increased patient experience, decreased readmission and closed quality gaps. •
44 CommonSpirit Health Nursing
“Our future is the ability to see and hear heartbeats from 2,000 miles away with our team of nurses and specialists.”
— Gail Daly, RN, MSN, System SVP, Clinical Operations, Integration Optimization
Elevating Experience Across the System
Transforming the patient experience
The National Patient Experience team is responsible for setting the yearly and five-year strategy for patient experience goals, analytics and operations as well as all improvement resources and standardized efforts across CommonSpirit Health. In FY23:
• In alignment with the CommonSpirit 2026 strategic plan, the team developed a new five-year strategy to transform the patient experience. A central tactic is to utilize the net promoter score to enable CommonSpirit to determine how likely a consumer is to recommend the organization to others.
Fulfilling the Mission to Serve
Devoted to making a difference
Care Coordination refers to the process of organizing and coordinating health care services to ensure patients receive the appropriate level of care. In FY23, the team:
• Developed Care Coordination Academy, Fellowship and Residency programs in partnership with Dignity Health Global Education. These programs are designed to address internal staffing challenges and control costs.
• Moved from a Utilization Management Hub dyad model to a triad model. The change consolidates positions into one role with various levels of expertise. Each role will have time
“I am inspired by nurses and nurse leaders who consistently demonstrate humankindness while elevating the patient experience.”
Experience
• The national team partnered with frontline teams to implement and hardwire evidence-based practices. Additionally, the team built the capabilities for Hello humankindness operations, patient experience leader orientation and evidence-based practice resource guides in support of their experience improvement efforts.
• The nursing teams across CommonSpirit significantly impacted the patient experience. With their commitment and focus, CommonSpirit has achieved its annual enterprise goals. •
to focus on specialized functions that will decrease competing priorities as well as employee frustration.
• Created the EPIC Care Coordination Module to standardize the way employees document information within the EHR. The module optimizes the quality, efficiency and effectiveness of the team’s documentation and provides a consistent workflow while allowing leadership to create reports and audit processes for quality control. •
“Each team member is unique and brings their experience and knowledge to serve patients, hospitals and our ministry.”
— Dana S. Farley, RN, MBA, CCM, RN & SW Care Coordination Academy, Social Worker Fellowship for MSWs and Social Worker Residency for BSWs


FY23 Annual Report 45
— Camille Haycock, SVP, Patient
Empowering Virtual RNs Revolutionizing continuity of care
The Nurse Triage Department, a vital part of the Physician Enterprise Patient Connection Center, supports over 800 providers in five states. This talented team of RNs handles calls from patients who are experiencing both acute and chronic symptoms and/or need medical advice and home support.
“I am humbled by our teams’ dedication to defining the future of nursing by guiding patients virtually through challenging situations!”
— Shawna Sharp, RN, Director of Triage Services
Breaking Boundaries in Health Care
Embracing the era of virtual nursing
In alignment with the nursing strategic plan, the Virtually Integrated CareSM (VICSM) team is leading the expansion of a transformational care model to address the significant nursing shortage. This model utilizes an experienced virtual nurse seamlessly integrated into the patient care team to provide pivotal support to the bedside team. In FY23:
• In markets integrating VIC, the team experienced increased staff engagement and improvements in patient experience and patient safety outcomes.
• The Pacific Northwest Division has successfully highlighted the ability
The nurses use their skills to virtually assess patients, triage symptoms and advise on the safest disposition, documenting directly into the electronic health record and practice management systems. As a virtual extension of the clinics, this growing team of RNs enhances continuity of care, improves patient care and helps decrease the overall cost of care. In FY23:
• The Connection Center increased its footprint to support clinics not only in California, Nevada and Arizona but also in Kentucky and Texas.
• Six RNs on the team obtained their Virtual Triage Nursing Certification as part of their growth in the specialty of virtual nursing. •
“In markets integrating VIC, success is evident with increased staff engagement and experience and safety improvements.”
—Linda Goodwin, MSN, MBA, FACHE, System SVP, Nursing Transformation, Virtual Care Innovation and Nursing Informatics


to convert traveling nurses to core staff and the return of nurses who previously left the organization.
• The Southeast Division has also noted the conversion of international traveling nurses to full-time nurse positions along with improved patient experience and less nurse turnover.
The VIC team will continue to expand the program in the current divisions and further expand its footprint across the ministry. •
46 CommonSpirit Health Nursing
Transforming Health Care Across Our Nation
Elevating the quality of care
Patient Care Services (PCS) provides enterprise-level leadership for the practice of nursing and clinical patient care delivery across CommonSpirit Health. PCS supports and facilitates an interdisciplinary and multi-professional approach to the overall delivery of care to patients, families and communities, with a focus on quality, safety, innovation, and alignment to professional standards and evidence-based practices. In FY23:
• In collaboration with nurses and nurse leaders across CommonSpirit Health, the team created and disseminated Standards of Practice for the Medical/Surgical/Telemetry Nursing, Perioperative Nursing, Critical Care
Nursing Leadership Across CommonSpirit: Nurse Executive Council
The Chief Nursing Officer of each division, along with the nurse leaders from Home Health, Senior Services and Physician Enterprise, are part of the national Nurse Executive Council (NEC). The NEC, which also includes system nurse leaders, meets regularly to address issues important to nursing and is chaired by Kathy Sanford, CommonSpirit Health System Chief Nursing Officer.

Nursing and Maternal Health Nursing teams. The team is also developing Standards of Practice for Emergency Nursing and Behavioral Health Nursing.
• The PCS team secured a multiyear, multimillion-dollar Department of Justice federal grant related to human trafficking.
• In collaboration with the Operations Performance Group, the team created and implemented a new productivity standard for operating rooms across CommonSpirit Health. •
“We have a responsibility to embrace our gift to care for people with love and humankindness when they need us most”

— Connie A. Clemmons-Brown, DNP, MBA, RN, CENP, System SVP, Patient Care Services

“
You are the hands of healing, the face of comfort and compassion, the ultimate professional, the special presence that makes the difference to our patients.
– Sister Barbara Hagedorn, SC, Member of the CommonSpirit Health Board of Stewardship Trustees



 DBA, RN, FACHE, FAAN, CommonSpirit Health EVP and Chief Nursing Officer
DBA, RN, FACHE, FAAN, CommonSpirit Health EVP and Chief Nursing Officer