Nursing Columbia
Fall-Winter 2025

Fall-Winter 2025

The Magazine of Columbia University School of Nursing
NEW HYBRID MDE AND PART-TIME DNP OFFER STUDENTS A CUSTOMIZED PACE
STUDY: AI CAN HELP EDIT BIAS OUT OF PATIENT RECORDS
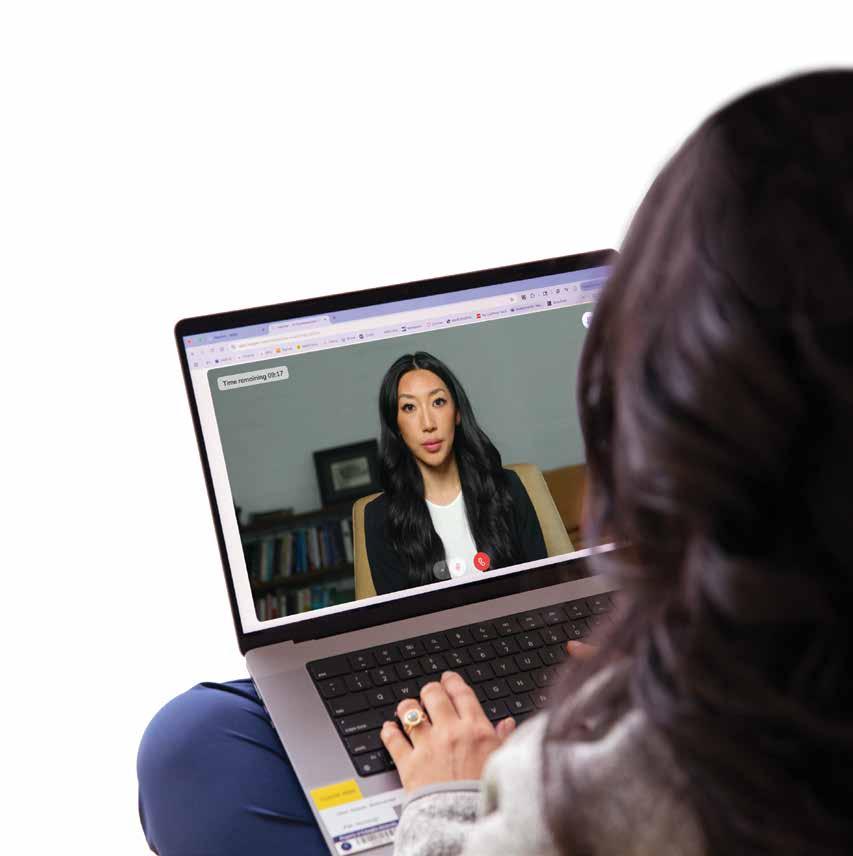
Columbia Nursing is embracing AI avatars as instructors.
Faculty find them effective, students find them compassionate.


Every day, the world seems to spin faster. Time shrinks. Work multiplies. Technology burgeons. Stress mounts. At Columbia Nursing, we prioritize keeping up with our ever-evolving world—without losing the human touch.
That concept is evident in this issue’s features. The students in our Masters Direct Entry (MDE) and Doctor of Nursing Practice (DNP) programs, for example, often juggle studies with jobs, family, and other responsibilities. So—as detailed in the feature on page 14—we’ve created a way for them to customize our demanding curriculum with hybrid MDE and part-time DNP programs that offer the same content as our regular programs, but run slightly longer and include some remote coursework. They perfectly exemplify our commitment to balance: we’re meeting students’ needs while upholding our profession’s standards.
And the cover feature—which starts on page 8 and describes the use of artificial intelligence (AI) avatars as instructors—of course exemplifies our embrace of technology: we’re one of the few schools nationwide using this cutting-edge approach to nursing education. With avatars available 24/7, students can study at their convenience. AI instructors quiz them on clinical topics, push them to think critically, and offer supportive feedback—encouraging students who feel overwhelmed to keep going.

But as much as students appreciate the avatars’ attributes, they acknowledge that they’re an adjunct to, not a substitute for, human instructors. The human touch remains at the core of high-tech nursing education, especially at Columbia.
The power of that point is represented by no one more than a beloved member of our faculty who recently passed away. Mary Moran, MS ’08, died on October 7, at home, with her husband at her side. She was a clinician at NewYork-Presbyterian–Cornell Medical Center for over four decades and a member of our faculty for over 25 years. In that time, her unwavering positivity, compassion, and mentorship sustained her patients, motivated her colleagues, and inspired her students. And Mary was an innovator as well as a humanitarian— embodying the balance Columbia Nursing is committed to striking.
My sense of connection with Mary verged into the personal, too, for she and I share deep Irish roots. Mary spent most of her life in the U.S. but retained an Irish soul—she was steadfast in faith, warm in welcome, and generous in spirit. Her wit, courage, storytelling skill, and embrace of everyone: all these reflected her Irish heritage.
She also held a deep love for Africa. She met her husband, Gebremedhin, in an Ethiopian refugee camp in Sudan in the 1980s and returned to the continent frequently in the ensuing decades, often in times of crisis. In 2009, she founded a nonprofit called Girls2Woman, which provides young Ethiopian women with reusable menstrual supplies, enabling them to stay in school. The effort reflected Mary’s profound belief in education as a path to independence, equity, and dignity.
The word “beloved” doesn’t even begin to express how our community felt about Mary. When students learned of her death, they thronged to the seventh floor to grieve her loss and celebrate her impact.
No matter how fast the world spins, we intend to keep people like Mary as our North Star.
LORRAINE FRAZIER, PhD, RN, FAAN Dean, Columbia University School of Nursing
Mary O’Neil Mundinger Professor of Nursing Senior Vice President, Columbia University Irving Medical Center
Lorraine Frazier, PhD, RN, FAAN
Dean, Columbia University School of Nursing
Mary O’Neil Mundinger Professor of Nursing
Senior Vice President, Columbia University Irving Medical Center
ALUMNI NEWS EDITORS:
Ashaki Charles
Associate Dean, Development and Alumni Relations
Janine Handfus
Associate Director, Annual Fund
Sharon Sobel
Assistant Director, Alumni Relations
Laura Ardizzone, DNP ’10
Director of Nurse Anesthesia Services, Memorial Sloan Kettering Cancer Center New York, NY
Felesia Bowen, PhD ’10
Professor and Associate Dean for Access and Engagement, University of Alabama at Birmingham Birmingham, AL
Brenda Barrowclough Brodie, BS ’65 Durham, NC
Kevin Browne, MS ’92
Associate Executive Director, Chief Nurse, Northwell Health Lenox Hill Hospital; Manhattan Eye, Ear, and Throat Hospital; and Lenox Health Greenwich Village New York, NY
Paul Coyne, DNP ’16
President and Co-Founder, Inspiren; Senior Vice President and Chief Nurse Executive, Hospital for Special Surgery New York, NY
Delphine Mendez de Leon, BS ’78 Chief Strategy Officer, University Hospital of Brooklyn New York, NY
Angela Clarke Duff, BS ’70 Forest Hills, NY
Marjorie Harrison Fleming, BS ’69 Chair Emerita, Board of Advisors Seabrook Island, SC
Susan Fox, BS ’84 President and CEO, White Plains Hospital White Plains, NY
Karen Hein, MD
Adjunct Professor, Department of Family and Community Medicine, Dartmouth Medical School Jacksonville, VT
Columbia Nursing is the magazine of the Columbia University School of Nursing and is published twice a year
Produced by the Office of Strategic Communications and Marketing
Linda Muskat Rim, Editor-in-Chief
Senior Associate Dean, Strategic Communications and Marketing
DESIGN AND ART DIRECTION: Eson Chan
CONTRIBUTING WRITERS:
Anne Harding
Andrea Kott, MPH Kenneth Miller
4
· Columbia Nursing Study Shows AI Can Help Remove Bias from Patient Records
· Barcelona Awarded $2.9M for ID-STIGMA Study
· New Intervention May Improve Quality of Life for Adolescents with Sickle Cell Disease
· CUIMC Honors Outstanding Nurses at Excellence Awards
· Students Present Award-Winning Research at ENRS
Bernadette Khan, DNP
Group Vice President and Chief Nursing Officer, Columbia University Irving Medical Center Plainview, NY
Mary Turner Henderson, BS ’64 San Francisco, CA
Richard I. Levin, MD Professor Emeritus, McGill and New York Universities; President, Optimal Health Advising, LLC New York, NY
Janet Ready, BS ’81, Chair Chief Operating Officer, Premier Medical Group Poughkeepsie, NY
Patricia Riley, BS ’76 Captain (Retired), U.S. Public Health Service Atlanta, GA
Susan Salka, MBA Retired Chief Executive Officer and President, AMN Healthcare Services, Inc. San Diego, CA
Sara Shipley Stone, BS ’69 Brooksville, ME
Edwidge J. Thomas, DNP ’05
Vice President of Clinical Solutions, Northwell Holdings and Ventures New York, NY
Jasmine Travers Altizer, PhD ’16
Assistant Professor, New York University
Rory Meyers College of Nursing New York, NY
20
· Columbia Nursing Inducts 117 into Sigma Honor Society
· Middle Schoolers Dive into a Day in the Life of a CRNA
· A Glimpse of Alumni Events Throughout the Year
· Selected Faculty Publications
· Funding for Research and Training
Please address all correspondence to: press_nursing@cumc.columbia.edu
Alumni are invited to update their contact information by emailing sonalumni@columbia.edu or calling 212-305-5999
Subscribe to our monthly e-newsletter: nursing.columbia.edu
Like us on Facebook: @ColumbiaNursing

Follow us on Instagram: @columbianursing
Follow us on Twitter: @ColumbiaNursing
Follow us on LinkedIn: Columbia University School of Nursing
Subscribe to us on YouTube: Columbia University School of Nursing

By Andrea Kott, MPH
Columbia Nursing is embracing AI avatars as instructors. Faculty find them effective, students find them compassionate.


By Kenneth Miller
Columbia Nursing’s new hybrid MDE and part-time DNP programs let students tailor their schedules to fit their lives.

ords matter, especially in health care, where the language written in patient charts influences how people are treated and how they feel about their care. Imagine reading your medical records and finding yourself described as “noncompliant” or “drug-seeking” or seeing that you “claim” to have pain. For millions of patients who now have digital access to their health records, encountering such language can damage trust and even lead them to disengage from care.

A Columbia University School of Nursing study led by Zhihong Zhang, PhD, a postdoctoral researcher, explores whether ChatGPT could help identify and rewrite such biased language in medical records.
“Previous research shows stigmatizing language in charts can lead to less aggressive pain management and more diagnostic errors,” says Zhang. “With the 21st Century Cures Act giving patients full access to their records, addressing this isn’t just about better care— it’s about preserving the patient-provider relationship.”
The study, “Toward Equitable Documentation: Evaluating ChatGPT’s Role in Identifying and Rephrasing Stigmatizing Language
in Electronic Health Records,” was published on June 5, 2025, in Nursing Outlook.
In their analysis of 140 notes from two major urban hospitals, the research team found while ChatGPT did not catch every instance of stigmatizing language, it was strong (scoring a nearly perfect 2.73.0 out of 3) at rewriting terms to be respectful while preserving medical accuracy. Researchers found an average of two instances of stigmatizing language per note. The model struggled with automatic detection, catching only about half of the problematic language overall, though it performed well in specific categories like doubt markers.
While more work is needed before artificial intelligence can be fully integrated into health care settings, the study is particularly timely as health systems grapple with implementing equitable care practices while navigating the reality that patients can now access and read everything clinicians write about them. The researchers of this study envision ChatGPT being integrated into electronic health record systems to flag potentially stigmatizing phrases in real time and suggest alternatives.
Assistant Professor Veronica Barcelona, PhD, has received a $2.9 million grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to investigate the association between perinatal outcomes and stigmatizing language in clinical documentation.
In the five-year ID-STIGMA study, Barcelona and her colleagues will review records for about 35,000 pregnant women admitted to two hospitals in 2020-2024. They will refine and develop an existing natural language processing system to identify pat-
terns in clinical documentation and determine if these patterns are associated with patient demographics and perinatal morbidity, with the goal of informing future interventions to improve documentation and the quality of patient care.
Barcelona recently completed a three-year Betty Irene Moore Fellowship for Nurse Leaders and Innovators. The new study extends her work on the fellowship project to include community and clinician perspectives on stigmatizing language use, additional maternal morbidity outcomes, and adverse neonatal outcomes.
Anovel intervention aimed at helping adolescents with sickle cell disease maintain their hydroxyurea treatment plans shows promising results at improving their quality of life, a Columbia University School of Nursing study has found. The study, “HABIT Efficacy Trial Intervention Improves Elements of General and Disease-Specific Quality of Life in Youth with Sickle Cell Disease,” was published August 26, 2025, in Pediatric Blood and Cancer.
Sickle cell disease affects approximately 100,000 individuals in the United States; 40% of those affected are children. Adolescents with severe forms of sickle cell disease are advised to take a medication called hydroxyurea daily, a disease-modifying therapy.
“When an adolescent begins treatment with hydroxyurea, there are many benefits,” says Arlene Smaldone, PhD, a professor emerita at Columbia Nursing who co-led the study with Nancy Green, MD,


a professor and pediatric hematologist at Columbia University Irving Medical Center. “There’s less organ damage, their pain is reduced, and they have less hospitalization. Treatment may also improve their quality of life by improving their physical and mental health and their ability to keep up with friends, school, and other obligations. However, because the disease can be physically and mentally draining, adolescents often struggle to take hydroxyurea consistently.”
To explore a method that effectively increases hydroxyurea uptake and improves quality of life for adolescents with sickle cell disease, Smaldone and her colleagues developed the Hydroxyurea Adherence for Personal Best in Sickle Cell Treatment (HABIT) efficacy trial. Fifty English- and Spanish-speaking adolescents from 10 to 18 years old who had been diagnosed with sickle cell disease participated in this 12-month trial, carried out at four pediatric programs within academic medical centers.
Community health workers (CHWs) made five visits to each adolescent’s home, where they reviewed educational handouts with the participant and their caregiver. They also helped identify an existing daily habit that taking hydroxyurea could fit into. This was followed by three months of daily tailored text message reminders to take hydroxyurea based on the identified habit. CHWs also supported caregivers by attending a clinical visit. Each participant completed electronic surveys during the initial, fourth, ninth, and 12th months, with their caregivers.
Findings suggest that the HABIT intervention improved participants’ quality of life in select ways, such as their mental health, at the nine-month mark. However, these effects were not maintained at the end of the trial. Although promising, these results indicate that further research is needed to identify additional methods for effectively inducing and sustaining behavior change.
The second annual Division of Nursing Practice Nursing Excellence Awards were held May 8, 2025, during National Nurses Week, to celebrate extraordinary nurses and nurse practitioners at Columbia University Irving Medical Center (CUIMC).
Out of 40 stellar nominees, six nurses were chosen to receive awards that demonstrate their commitment to excellence and dedication to furthering CUIMC’s mission of improving lives through exceptional medical care. Each awardee also received a $1,000 scholarship for professional development.
Rae Vagg, chief operating officer at ColumbiaDoctors, presented the Nurse of the Year award to Raf Aguiar, RN, quality assurance nurse manager in the department of radiology, and Maison Amori Nasser, RN, a registered nurse in the Division of Hematology and Oncology.
Professor Suzanne Bakken, PhD, presented the Nurse Practitioner of the Year in Research award to Jennie McAllister, DNP ’20, a pediatric ventricular assist device nurse practitioner in the Pediatric Advanced Cardiac Care and Transplantation program.
Professor Mary Hickey, EdD, and Mary Moran, MS ’08, a clinical nursing instructor, presented the Nurse Practitioner of the Year award to Elena Abascal Asimow, MS ’25, a psychiatric nurse practitioner in the Division of Child and Adolescent Psychiatry; Patty Finnegan, MS ’97, lead nurse practitioner in the Division of Gynecologic Oncology; and Diana McDonnell, DNP ’20, a nurse practitioner in the Division of Melanoma and Solid Oncology. (Sadly, beloved faculty member Mary Moran died just a few


months after the awards ceremony. See page 1 for a reflection on this great loss to Columbia Nursing and its students.)
“I feel very grateful to have received this award and be surrounded by colleagues who advocate for better standards of care and inspire me to do my best. I chose this field because I was interested in science that has a human touch,” awardee Nasser said.
McDonnell also expressed her gratitude: “I feel honored. I am an alumna who now works at CUIMC. I love working with the other nurses who constantly inspire me.”
The Division of Nursing Practice is a collaboration among Columbia Nursing, CUIMC, and ColumbiaDoctors, designed to foster nursing careers in service to excellent patient care.
Two Columbia Nursing doctoral students were honored for their research at the Eastern Nursing Research Society’s annual conference, held earlier this year in Philadelphia.
Doctor of Nursing Practice (DNP) student Noor Begum’s poster presentation, “A Narrative Literature Review of the Barriers to Postpartum Depression Screening for Pediatric Providers,” received second place for a school-selected DNP poster.
PhD student Jiaojiao Wright’s podium presentation, “Communication Cards for Enhanced Patient Experience among Chinese-Speaking Patients in the Emergency Room,” was awarded third place for a PhD paper.
Several other Columbia Nursing students also presented their research at the conference, whose theme was “Freedom to Advance Health and Well-Being Through Revolutionary Nursing Research Partnerships.”
ENRS was established in 1988 as the research arm of the Mid-Atlantic Regional Nursing Association and the New England Organization for Nursing, with the mission of creating a community of nurses interested in promoting research.
Columbia University School of Nursing held its annual induction ceremony for the Alpha Zeta Chapter of Sigma Theta Tau International Honor Society of Nursing (Sigma) on May 19, 2025. This year’s event brought 117 students and leaders together to join the diverse and global organization known for supporting and recognizing professionals who are leaders in the nursing profession.
Inductees heard from a range of speakers, including Joan Halpern, DNP, vice president and chief nursing officer at NewYorkPresbyterian/Weill Cornell Medical Center, the event’s keynote speaker. She emphasized the power of nursing and how nurses can use advocacy to help shape health systems:
“Advocacy is one of the most powerful tools we have. As nurses, we are on the front lines of care. We know what our staff need, what our patients need, and what our health care systems lack. As a chief nursing officer, I value and prioritize the voice of nursing in every strategic decision. And I bring the voice of nursing into the rooms where decisions are made. Because when nurses speak, people listen. When nurses lead, change happens. I urge you to use your voice to advocate for safety, for equity, for your patients, your peers, and yourselves. Nursing is just not about responding to systems, it’s about shaping them.”

Inductees also recited the Sigma pledge, signed their name in the chapter’s membership book, and received an honorary cord. After the ceremony, inductees gathered with friends and family at a reception celebrating this impressive accomplishment.
Twenty students from the South Bronx Academy for Applied Media got a hands-on introduction to the certified registered nurse anesthetist (CRNA) profession on April 4, 2025, in an event organized and presented by Doctor of Nursing Practice in Nurse Anesthesia Program residents.
CRNA doctoral student Kadesha Bryan spearheaded the students’ visit, inspired by a similar event her classmate Andrew Fernandez organized last year with his alma mater, a private high school in Queens.
“We thought this year would be a unique opportunity for us to reach out to an underserved school within the community,” Bryan explains.

Teachers and administrators at the Bronx school “were excited at the initiative, to have their students immersed in finding out what is an RN and what is a CRNA,” continues Bryan.
She and her fellow residents began the event by introducing their guests to a day in the life of an RN and a CRNA, explaining the education and experience required for each. CRNAs don’t just provide medication to put patients to sleep before surgery and help them wake afterwards, they explained; they also treat anxiety and pain and ensure patients have no memory of the surgery.
Next, the CRNA doctoral students demonstrated nursing skills, including performing cardiopulmonary resuscitation (CPR), using a stethoscope to listen to the heart and lungs, and taking a pulse on specialized mannequins. Students could also practice administering intravenous medication and placing an endotracheal tube in a simulated surgical patient.
The day concluded with lunch and the presentation of special certificates to each student and the two teachers who accompanied them.
“It was really fun, very interesting,” said sixth-grader Ainara Rodriguez, who especially enjoyed learning CPR and practicing intubation. Her classmate Bella Beltran said she hadn’t known that nurses could become anesthetists and came away from the day very interested in exploring the profession further.

Columbia Nursing is embracing AI avatars as instructors. Faculty find them effective, students find them compassionate.
By Andrea Kott, MPH

ho is Dr. Chen?” Columbia Nursing student Kerrick Dougherty wondered to himself when he opened an email introducing the “professor” who would be working with him on a pre-simulation assignment in the Masters Direct Entry (MDE) program. “I thought I knew all of the MDE faculty at Columbia Nursing,” he remembers thinking. Then he clicked on the link and saw an artificial intelligence (AI)-powered avatar smiling at him.
At age 30, Dougherty is no stranger to AI platforms like ChatGPT. Still, he felt hesitant about engaging with a virtual nurse-professor. “I was a little nervous,” he says. “Being face-to-face with patients was the reason I got into nursing. I didn’t want to dehumanize my profession.” Yet as the avatar guided him through the material, asking questions and providing real-time, compassionate feedback, his comfort with the process grew. “Dr. Chen is definitely a good launching pad for learning,” Dougherty says.
Educational innovation has long made Columbia Nursing one of the most renowned schools of nursing in the country. Now, the institution is bringing learning to the next level with human-like, interactive nurse avatars that engage students in one-on-one conversations to help prepare them for assignments and clinical experiences that they’ll encounter in the simulation center, explains Natalya Pasklinsky, DNP, an associate professor and the assistant dean of the Helene Fuld Health Trust Simulation Center.
“We are one of the few schools nationwide beginning to use AI in this new way, embedding it into education,” she says. In addition to helping students
“We are one of the few schools nationwide beginning to use AI in this new way.”
Associate Professor Natalya Pasklinsky
complete written assignments, the avatar quizzes them orally on clinical topics, such as disease presentations and how to know whether certain interventions are working, pushing them to think critically and on their feet—skills that are essential to delivering superior nursing care. “In using avatars, we are not looking for correct answers but the frame of thought that reveals students’ understanding, interpretation, or lack of knowledge,” Pasklinsky says. “We want to get down to the root of students’ thinking, not just what went through their mind but the thoughts behind their actions.”
Simulation Technology Manager Juan Gonzalez is the talent behind Dr. Chen, Dr. Pedro Bennett, and other avatars that he has developed to represent professors, patients, and even pediatric patients’ parents for MDE students. Creating these avatars, some of whom he modeled after actual faculty members, entailed working closely with content expert Kristy Deyeso, DNP, who provided Gonzalez with all the subject material in the pre-simulation course, such as techniques for inserting a Foley catheter, changing a central line dressing, managing a chest tube, and recognizing signs of a stroke.
During students’ ob-gyn rotation, for example, avatars cover clinical issues like recognizing and treating preeclampsia, as well as social determinants of health like assessing how nutritiously a pregnant woman is eating; ensuring that she doesn’t miss her prenatal care appointments; and supporting her during labor, delivery, and the postpartum period. During their pediatric rotation, avatars teach students how to assess patients with abdominal pain for appendicitis, recognize signs and symptoms of an asthma attack, and treat a child who is seizing or going into anaphylaxis. “We want students to be prepared when they get into the sim lab to put into hands-on practice what the avatar has taught them,” Deyeso says.
To ensure that avatars dispense only accurate information, Gonzalez creates “guardrails” around specific topics by adding relevant policies from health agencies like the Centers for Disease Control and Prevention. “I receive all the information from Kristy and do a little of my own research,” he says. “When I see the avatar can have a fluid conversation, allowing me to speak with it and ask questions, then I send it to the instructor and make sure it performs properly.”
For the pre-simulation assignment, Gonzalez programmed Dr. Chen to conduct a pre-brief, an explanation of the assignment’s content and focus; a question-and-answer period, designed to reinforce students’ knowledge by quizzing them on the simulationrelated material they should have studied (asking, for example, “What’s the first thing you do when you step into a patient’s room?”); and a debrief, during which Dr. Chen or another nurse avatar engages students in a reflective discussion about their performance, clinical reasoning, and communication during the simulation. “The nurse avatar provides personalized feedback, reinforces key learning objectives, and encourages critical thinking to improve future clinical practice,” Gonzalez says. Following the debrief, students write
a 300- to 500-word reflection paper, analyzing their performance, identifying what they have learned, as well as their strengths and areas for improvement, and connecting their experience—along with two of their biggest takeaways—to real-world clinical practice.
“This written assignment promotes self-awareness and deeper learning and must be submitted to Canvas for instructor review,” Gonzalez says.
One of the features that makes the avatars so human-like is their ability to respond in the moment.
“These avatars adapt in real time, responding differently based on what you ask,” Pasklinsky says. If a student omits steps in inserting a Foley catheter, for example, the avatar will offer a gentle reminder to get them back on track. As one student wrote, “One thing I took away from the simulation was the correct order of donning and doffing PPE [personal protective equipment]. [Dr.] Chen helped to clarify the importance of each step and explained that improper use of PPE can lead to contamination.”
Another human-like feature of the avatars is their ability to respond to different tones of voice. They can detect if students are rushing, aggressive, unsure of themselves, or off topic. For example, another student wrote that “the avatar actually listened to my questions and responded in ways that reflected my tone and wording. It felt like a genuine conversation, which made the experience both engaging and educational.”
Such real-time, back and forth interaction fosters learning more effectively and immediately than rote writing exercises that students may not receive feedback on for several days. Moreover, since the avatars are generative, they learn and evolve with every use. “The more you interact, the more they grow and learn to answer differently, so no two students have the same experience,” Gonzalez says.
MDE student Jennifer Skor is not a shy person. But when it comes to asking questions in group settings, she gets nervous. “I get intimidated, even with standardized patients,” Skor admits, referring to the professional actors Columbia occasionally hires to role-play patient-provider interactions with students. But, with avatars, Skor says, “There were no nerves.” She attributes this in part to the avatars’ 24/7 availability, which allowed her to work with them in the privacy of her home, whenever and as frequently as she liked. “There was no time limit,

and there were no other students around, so I didn’t feel judged,” says the 50-year-old mother of two. “I like to ask a lot of questions to make sure I really understand material, and with an avatar I could ask as many questions as I wanted and not feel like I was talking over my classmates.” The avatars’ oneon-one mentorship created a space that felt safer than a classroom, preparing her better for the simulation lab than participating among peers, she says. Dougherty sometimes feels intimidated when asking questions in class, too. Overlooking some of the steps in preventing a central line infection made him especially self-conscious. To his surprise, Chen commended the knowledge he did display and in a kindly way named the steps he omitted. “It was nice to have a friendly reminder in a nonjudgmental environment,” Dougherty says. “No matter my level of experience, Dr. Chen provided a safe place to land.”
In partnership with Deyeso, Gonzalez programmed the avatars to be mentors who are compassionate and encouraging, giving students the freedom they
need to make mistakes. “We didn’t want students to walk away feeling like they were being scolded, we wanted to create a safe space for them to learn and engage,” Deyeso says.
Indeed, the patience, encouragement, and compassion that the avatars extended made Dougherty feel safe. In addition to encyclopedic capacity for clinical knowledge and real-time responsiveness, they are equipped with voice activation technology that enables them to detect a student’s hesitation when answering a question. In response to an uncertain tone, an avatar may say, “I noticed you were hesitant” or “I noticed you took longer to respond to that question,” and then invite the student to request help understanding the material.
Having chosen nursing as a career change, Dougherty needed a good deal of help with most

of the information he encountered. “Whenever Dr. Chen asked a question that I couldn’t answer, she created a safe space for me to work through my uncertainty,” he says. “This reminded me that asking a question is far better than pretending to know something out of fear of being perceived as incompetent. After all, one question can save a life!”
Notes Deyeso, “One of the things I really like about the avatars is that if a student gets something wrong, they keep teaching in a compassionate way, so the student wants to keep going.”
Such supportiveness helped Dougherty gain comfort with unfamiliar scenarios while strengthening his mastery of the content he was learning.
“Dr. Chen’s feedback reassured me that I was truly retaining material, which has been both inspiring and motivating in my learning journey,” he says.
“Whether I entered a simulation with Dr. Chen well-prepared on the topic or uncertain, I have found that another perspective always contributes to well-rounded care.”
The wide array of avatars that Gonzalez has created allows students to practice communicating with the many people, including patients and parents, whom they’ll encounter in various health care settings. “Every student has a different experience, which is important because every patient they meet is going to be different,” says Assistant Professor Kathleen Mullen, DNP. “As a nurse, you have to adapt to every situation.” In this way, she adds, “the avatar gives students a much more rounded education that’s not rote and stuck in the same pattern.”
For example, the avatars enable students to practice explaining to patients why they’re in the hospital or why their child needs surgery. They also ready them for one of the most difficult aspects of nursing—breaking bad news to a patient’s family. “Therapeutic communication is a skill that all nurses have to develop,” Mullen says. “Avatars provide feedback about the nuances of conversation between nurses and patients that students can use to understand when they’re coming across well and where they have to make changes.” As one student reflected, “This simulation reminded me that effective communication isn’t something that happens automatically. It’s a skill that requires intentional effort, practice, and feedback.”
For Skor, working with the avatars also helped her learn “nursing lingo,” which she found to be especially important in giving reports. “They helped
me switch from speaking in lay terms to using the correct clinical language,” she says.
Avatars can even prepare students who want to enter nursing administration for the challenging conversations that they will likely have when proposing programmatic changes, says Mullen, who teaches a course about quality improvement in the school’s Masters in Advanced Clinical Management and Leadership program. Geared toward nurses aspiring to advance from middle to higher management, the course requires students to develop a quality improvement project. For one project, Mullen asked Gonzalez to create an avatar in the form of a correctional facility administrator who opposed a prison-wide flu vaccination program. Students assumed the role of public health nurses who had to persuade the administrator of the program’s importance. “The administrator, who was very resistant to change, was not at all interested in the program,” Mullen says.
Meeting such resistance is exactly the type of experience students need as they prepare for a career that involves implementing change to improve quality, Mullen explains. “Whenever you propose or institute change, there are going to be people who question or say they don’t like it,” she says. “You have to communicate and work with people to get change accepted, despite the barriers.” Furthermore, she adds, “the avatar evaluated students’ responses to the administrator and let them know if they came across as objective, and if there were opportunities where they could have pushed a little harder or achieved more in conversation.”
Pasklinsky found the prison administrator to be so realistic, she almost forgot that she was interacting with an avatar. “I really felt like I had a stake in his allowing me to vaccinate inmates. As the case went on, I felt more empowered and thought, ‘I’m going to convince this guy.’ As an experienced practitioner, I was sweating,” she says.
Years ago, assignments in the MDE program consisted largely of writing answers to questions. Back then, search engines and AI platforms like ChatGPT made it possible for students to quickly search for, copy, and paste their answers, Deyeso says. Avatars eliminate such shortcuts. “Now students have to have a conversation out loud,” she says. The process reinforces their learning and assures professors that they are absorbing the material. “With an avatar, I know students are talking through scenarios
because they are coming better prepared to simulation sessions,” observes Deyeso. Not surprisingly, avatars resonate especially well with younger students, who came of age playing video games or enjoying other high-tech visual experiences that make didactic learning dreary by comparison. “When you’re looking at a static picture, you’re not as engaged as when you’re looking at something dynamic and moving,” Mullen says. The avatar draws students in and makes them feel like the work they’re doing is not just another routine assignment. “It engages students in a way they’re used to engaging, moving and talking, while giving them the kind of feedback about their communication that helps them learn going forward,” she says.
But as advanced as they are, Columbia’s avatars still need some smoothing out, faculty and students agree. For instance, they’re highly sensitive to background noise, so they can easily mistake audio from a television or radio for a student’s voice. Dougherty observed a related shortcoming. “If I paused,” he says, “the avatar would think I was finished speaking when I wasn’t and move on to the next thing.” Skor learned to sidestep glitches of this kind, which
“With an avatar, I know students are talking through scenarios because they are coming better prepared to simulation sessions.”
—— Content Expert Kristy Deyeso
occurred when her husband was watching TV, by typing her questions and awaiting the avatar’s spoken response.
“We’re still in the baby stages,” Pasklinsky says. “This technology will grow in leaps and bounds and exceed everything we’ve expected.” That said, she cautions students against relying on avatars for all their learning. “This is not to say you should 100% rely on avatars, but they do help the human mind explore different ways of thinking,” she says. Indeed, it is with some relief that students notice avatars’ limitations. “Avatars are never going to replace our professors,” Skor says. “They’re a good pre-learning activity, but you need in-person instruction to learn physical skills. For that reason, avatars will never replace human beings. They’re just a good supplementation.”

COLUMBIA NURSING’S NEW HYBRID MDE AND PART-TIME DNP PROGRAMS LET STUDENTS TAILOR THEIR SCHEDULES TO FIT THEIR LIVES.

When it comes to life’s biggest choices, timing can be everything. Take the decision to pursue an advanced degree—let’s say, for the sake of argument, whether to apply for the master’s direct entry (MDE) or doctor of nursing practice (DNP) program at Columbia University School of Nursing.
Both have long been among the top-rated programs of their kind in the country, and both have traditionally operated at a fast pace, requiring participants to put other commitments—work, family, relationships—on the back burner. So what if a would-be student has the talent and drive necessary to succeed in such a pursuit, but feels it isn’t the right moment to set competing responsibilities aside? Until recently, the only options for such aspirants were to look for less intensive programs elsewhere or to put off their ambitions indefinitely.
BY KENNETH MILLER
BY
JÖRG MEYER
This fall, however, the school launched two initiatives designed to overcome that dilemma: a hybrid MDE program and (in two specialties to start with) a part-time DNP program. “Over the years, we’ve seen so many candidates who want a Columbia Nursing education and have excellent qualifications, but for whom an accelerated program is not a fit,” says Dean Lorraine Frazier, PhD. “We realized that if we tweak things just a little bit, they can have their dream.”
The school’s leadership designed these programs partly in response to changing demographics. “Our applicant pool looks different than it did a decade ago,” explains Mary Hickey, EdD, the vice dean of education and a professor of nursing. “Often, students are juggling multiple responsibilities and may be interested in maintaining employment while in school,” she explains. “Offering different program options allows us to attract students with broader life and work experience, who will then bring those perspectives to the health system along with their Columbia training. That’s good for all of us.”
THE HYBRID MDE PROGRAM offers a curriculum similar to that of the traditional program, along with the same superb academic and clinical resources, but the content is disseminated differently. For now, courses begin in the fall rather than the summer (though that’s slated to change in the 2026-27 academic year). More importantly, coursework is decelerated during the first year, with just nine credits per semester instead of 12 to 24, and all classes
THE SCHOOL’S LEADERSHIP DESIGNED THESE PROGRAMS PARTLY IN RESPONSE TO CHANGING DEMOGRAPHICS.
“OUR APPLICANT POOL LOOKS DIFFERENT THAN IT DID A DECADE AGO,” EXPLAINS MARY HICKEY, EdD.
are held virtually during that period. Due to these adjustments, earning a master’s degree takes a bit longer—24 months rather than the traditional program’s 15 months.
Although participants in the hybrid program ultimately come away with the same rigorous nursing education as those taking the traditional path, the less strenuous beginning is designed to ease the transition for those whose current circumstances make it difficult to go all-in. “In the traditional model, students have to deal with pathology and med-surg and peds and OB as soon as they get here,” notes
Heidi Hahn-Schroeder, DNP, the assistant dean of academic affairs and director of the MDE program. “They’re in class from 8 a.m. to 5 p.m. and studying in the evenings, which isn’t adaptable to everyone’s learning style or lifestyle.” In the hybrid program, by contrast, students start with pathology and take on other demanding didactic subjects later in the course cycle. And because classes are online in the fall and spring semesters, those who aren’t ready to relocate to New York can wait to come to campus until the summer term, when the MDE’s clinical studies begin.
Over 30 students have enrolled in the hybrid program’s inaugural cohort, compared to about 200 taking the traditional route. “We consider that number an excellent start,” Hahn-Schroeder says, “and we expect it to grow robustly as word of this option spreads.” Eventually, she predicts, the hybrid program could account for up to 50% of each year’s entering class.
That optimism is based, in part, on a precursor’s success. The new program grew out of a more limited one (still available to those who need it), in which MDE students facing major personal challenges can switch to part-time studies and take some classes remotely. “Going hybrid was a lifesaver for me,” says Nicole Ugorji, MS ’25, who exercised that option. “I encourage anyone who might benefit not to be afraid to try it.”
Ugorji emigrated with her family from Nigeria to Los Angeles as a teenager. Although she majored in English literature at UCLA, she’d always dreamed of a career in health care; the only question was in what capacity. After graduating at the height of the COVID pandemic, she found a job with the California Department of Health Care Services managing a team that provided basic medical services to homeless people. “The hospitals were so packed that the nurses in our group had to become providers,” she recalls. “When I saw the synergy that happened when they were allowed to practice full-scope, I thought, ‘Wow—that’s what I want to do.’”
Ugorji enrolled at Columbia Nursing in June 2023, drawn by the school’s global initiatives and its stellar nurse-midwifery DNP program, which she hoped to join after completing her master’s degree. During her first semester, however, several converging crises threatened to scuttle her dreams. First, a close relative experienced some serious health setbacks. “I was getting calls from family members at 4 a.m., and I had to be up for clinical at 6 a.m.,” she recalls. The stress took a toll on her

own health, leading to an emergency room visit for a life-threatening condition on the day of her final exam. Meanwhile, she lost her lease, became homeless, and found herself struggling to keep up with her studies while couch-surfing with friends.
When school administrators learned of Ugorji’s troubles, they invited her to enter the modified MDE program. She cut back on her didactic courses, participated in the remaining ones remotely, and put off her clinicals until her second year. (To maintain the skills she’d already developed, such as placing Foley catheters and IVs, she’d practice in the simulation lab whenever she had a chance.) “Making those changes allowed me to be there for my family and for myself,” she says. She helped her relative obtain the care he needed, recovered her health, found a new apartment, and rescued her gradepoint average.
Decelerating, Ugorji found, had other upsides as well. Replaying online lectures enabled her to absorb them more deeply. Being less busy gave her time to get involved in professional associations, including the National Student Nurses’ Association, as well as apply for scholarships and join a field research project. By the time she started her clinical rotations, her confidence and enthusiasm were fully
restored. She enjoyed her psych rotation so much that she tweaked her specialization plan; in addition to midwifery, she decided to focus on caring for patients with postpartum depression. Alongside her studies, she found the energy to also serve as a teaching assistant in the skills lab, a student mentor, and an outreach ambassador for the school.
Ugorji completed the MDE program successfully and is now studying for her DNP. “The hybrid approach helped me sharpen my nursing skills, my community skills, and my vision of what I want to do,” she says. “There’s strength in a slower pace.”
UGORJI IS NOW at a point in her life where the traditional DNP program works well for her. As with the hybrid MDE, however, a less intensive approach to a doctorate can be a boon for some students. Columbia Nursing’s part-time DNP program is designed for working registered nurses who want to advance to the highest level of clinical practice while maintaining their professional and personal commitments. It offers a hybrid curriculum that blends online and in-person coursework, allowing students to progress through courses in advanced practice, leadership, and evidence-based practice at a flexible and sustainable tempo. Earning a degree
will typically take about 3.5 years, compared to 2.5 for the traditional program.
“The idea for the part-time option came from listening to our nursing community,” says Susan DoyleLindrud, DNP ’08, the assistant dean of academic affairs and director of the DNP program. “In recent years, we’ve consistently heard from nurses who were passionate about advancing their practice and taking on leadership roles but felt constrained by the traditional full-time doctoral program format.” Such input came from both early- and mid-career professionals with family and financial obligations that made it difficult to stop working for an extended period.
Besides allowing nurses to continue drawing a salary and benefits while earning their DNP, the new program enables them to tap into employer tuition reimbursement programs, when they’re available— especially important now that federal grad PLUS loans have been eliminated for new borrowers.
“The part-time DNP program aligns with the school’s mission of expanding access to advanced nursing education and improving patient outcomes across our community,” Doyle-Lindrud says. “By enabling experienced nurses to maintain their clinical positions while expanding their skills, it ensures that patients continue to benefit from their expertise throughout the educational journey.”
For health systems, another potential advantage is the ability to retain existing employees and move them into roles that require a DNP instead of onboarding and training external hires. “By promoting from within, employers get someone who already knows the policies, the procedures, and the medical record system,” says Vice Dean Hickey. “That improves efficiency and saves money.”
The program is starting on a pilot basis with a small cohort of students working toward being credentialed either as a family nurse practitioner (FNP)

or an adult-gerontology acute care nurse practitioner (AG-ACNP). There are plans to expand the enrollment next year. “We were amazed by the response when we sent out brochures describing the program,” Doyle-Lindrud says. “The enthusiasm from nurses across different practice areas and career stages validated our belief that we’re addressing an unmet need.”
One of those nurses was Katherine Sobá, MS ’20. Raised by immigrant parents in the Bronx, Sobá attended the University of Virginia on a full-ride merit scholarship, earning a BS in kinesiology. During her senior year, she participated in a qualitative research project with nurses and NPs in rural South Africa, studying palliative care practices in end-of-life breast cancer patients. “I’ve always had an interest in the transitional phases of life, those very human moments when someone gives birth or passes away,” she says. “When I saw the impact these nurses had on patients’ health and well-being, and on the well-being of their caregivers, it drew me to the profession.”
Sobá chose Columbia Nursing for its academic rigor, its global initiatives, and its commitment to serving the community where she grew up. When the pandemic hit during her spring semester as an MDE student, she joined the army of nursing students who helped the city weather the crisis, working as a part-time patient-care technician in the ICU at NewYork-Presbyterian’s Allen Pavilion. After graduating in September 2020, she switched to a full-time position in the Division of Hematology and Oncology at Columbia University Irving Medical Center (CUIMC).
As an outpatient clinical coordinator on the leukemia service, Sobá was caring for patients with lifethreatening cancers, following in the footsteps of the South African nurses who first inspired her. She was also steadily expanding her clinical skills, learning from the multidisciplinary team of physicians, physician associates, nurse practitioners, and RNs with whom she worked. Still, as the years passed, she began to feel driven to do more. “I started thinking about a DNP because it’s the highest practice degree a nurse can get,” Sobá says. “I wanted to be as educated as I could be to ensure that my patients got the best care I could provide for them.”
What held her back was a reluctance to stop working. Although the loss of income was a consideration, other factors were equally important. “I felt that leaving would be a disservice to my education,” she explains. “This is one of the best leuke-
mia services in New York, and I’m learning things here that you can’t learn anywhere else. In addition to being our patients’ oncology team, we also serve as their de facto primary care providers. I wanted to continue that aspect of my training, and to be able to apply whatever I learned in class right away, instead of waiting until I finished my studies.”
The part-time DNP program offered a unique solution, with didactic classes that meet once or twice a week, and skills training scheduled according to each student’s needs. Sobá chose the FNP track, aiming to maximize her ability to provide advanced palliative care and other care for cancer patients of all ages. Now in her first semester, she continues to work at CUIMC while taking courses on epidemiology, environmental health, synthesis of evidence, and other topics.
Studying part-time also enables Sobá to oversee care for elderly members of her extended family and to keep up a brisk schedule of volunteer work. She’s active with the Catholic nonprofit Community of Sant’Egidio, helping to provide meals, emotional support, and other aid to homeless people throughout New York City. Under the organization’s aegis, she also leads weekly visits to nursing home residents and helps run a children’s mentorship program in the Bronx. “It gives me energy to
THE PART-TIME DNP PROGRAM OFFERS DIDACTIC CLASSES THAT MEET ONCE OR TWICE A WEEK, AND SKILLS TRAINING SCHEDULED ACCORDING TO EACH STUDENT’S NEEDS.
make sure that people in my community are well taken care of,” she says.
Eventually, Sobá envisions becoming a nurse educator herself. “Being on a university faculty would be amazing,” she muses. “The most effective way to promote crucial values, like evidence-based practice and cultural competence, is to instill them in others.” She hopes to conduct research that will advance the field and also envisions starting a primary care clinic for the unhoused and uninsured. Earning a DNP offers a pathway toward those dreams in the future. But a part-time approach leaves room for tending to the present moment as well. For Sobá, both goals are equally important. “At Columbia Nursing, we learn to look at the big picture,” she says. “We do everything we do because we’re hoping to make a better New York and a better world.”




1: Class of 1970 celebrating their 55th milestone reunion at the annual Dean’s Dinner in April 2025.
2: Tka Edwards, DNP’23, Daniel Billings, DNP’18, and Sergine Delma, MS’25, at the annual Dean’s Dinner in April 2025.
3: Recent graduates and Columbia Nursing friends at the Alumni Happy Hour in Midtown in April 2025.
4: Recent graduates at the Alumni Happy Hour in Midtown in April 2025.
5: Brenda Brodie, BS’65, Yoohee Joun, MS’95, and Dianne Brittain Goodrich, BS’65, at Alumni Reunion 2025.
6: Melissa Beauchemin, PhD’19, Kasey Jackman, PhD’17, and Laurie Ray, MS’11, with Dean Lorraine Frazier, receiving their Alumni Awards at the annual Dean’s Dinner in April 2025.

7: Ann-Margaret Navarra, PhD’11, Maureen Murphy-Ruocco, MS’80, Laura Ardizzone, DNP’10, and Olivia Velez, PhD’11, at the annual Dean’s Dinner in April 2025.
8: Ian West, DNP’24, and Ronald Shpata, MS’23, at the Alumni Happy Hour in Midtown in April 2025.
9: Current students and recent alumni who presented in the student poster session at Alumni Reunion 2025.
10: Alumni participating in simulation demonstrations at Alumni Reunion 2025.
11: Grace Ross, BS’60, Jean Kelly, BS’60, Peggy McEvoy, BS’60, Paula Mosher, BS’60, and Rachel Neville, BS’60, celebrating their 65th milestone reunion at Alumni Reunion 2025.
12: Marie Castronovo, MS’15, and Jessica Mukherjee, MS’15, at Alumni Reunion 2025.










Our faculty’s research continues to create new knowledge that advances health care. Listed are selected articles published by leading peer-reviewed journals.
Gregory Alexander and Maxim Topaz were among the authors of “Understanding Daily Care Experience Preferences Across the Lifespan of Older Adults: Application of Natural Language Processing,” published in Western Journal of Nursing Research, and “Understanding Gender-Specific Daily Care Preferences: Topic Modeling Study,” published in Journal of Medical Internet Research.
Suzanne Bakken was among the authors of “Trajectories of mHealth-Tracked Mental Health and Their Predictors in Female Chronic Pelvic Pain Disorders,” published in medRxiv.
Veronica Barcelona was among the authors of “Concordance of Self-Reported Obstetric Outcomes with Electronic Health Record Documentation: A Secondary Analysis of the Nulliparous Pregnancy Outcomes Study
Monitoring Mothers-to-Be,” published in Birth, and “National Academies of Science, Engineering, and Medicine Recommendations for Transformative Change in Women’s Health Research at the National Institutes of Health,” published in Nursing Research.
Veronica Barcelona and Yihong Zhao were among the authors of “Epigenomic Pathways from Racism to Preterm Birth: Secondary Analysis of the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMom2b) Cohort Study in the USA to Examine How DNA Methylation Mediates the Relationship Between Multilevel Racism and Preterm Birth in Black Women: A Study Protocol,” published in BMJ Open.
Melissa Beauchemin, PhD ’19, was among the authors of “Baseline Characteristics of Parents Enrolled in Children’s Oncology Group
Study ACCL20N1CD: Financial Toxicity
During Treatment for Pediatric Acute Lymphoblastic Leukemia in the United States,” published in Pediatric Blood and Cancer; “Care Pathway- and Guideline-Consistent Care in Pediatric Cancer Symptom Management,” published in JCO Oncology Practice; “Navigating B-ALL in the Era of Blinatumomab,” published in American Society of Clinical Oncology Educational Book; “Prevention and Management of Infectious Complications in Pediatric Patients with Cancer: A Survey Assessment of Current Practices Across Children’s Oncology Group Institutions,” published in Pediatric Blood and Cancer; “Transcreating BMT4me: A Protocol for Adapting a Mobile Health Medication Adherence App for Spanish-Speaking Caregivers in Pediatric Hematopoietic Stem Cell Transplant,” published in Digital Health; and “Use of Food Restrictions to Prevent Infections in Paediatric Patients with Cancer and Haematopoietic Cell Transplantation Recipients: A Systematic Review and Clinical Practice Guideline,” published in eClinical Medicine.
Melissa Beauchemin, PhD ’19, and Rhea Khurana were among the authors of “Insights from Diverse Perspectives on Social Media Messages to Inform Young Adults with Cancer About Clinical Trials: Focus Group Study,” published in JMR Formative Research, and “Prevention and Management of Infectious Complications in Pediatric Patients with Cancer: A Survey Assessment of Current Practices Across Children’s Oncology Group Institutions,” published in Pediatric Blood and Cancer.
Natalie Benda was among the authors of “How Difference Tasks Are Affected by Probability Format, Part 1: A Making Numbers Meaningful Systematic Review”; “How Point (Single-Probability) Tasks Are Affected by Probability Format, Part 1: A Making Numbers Meaningful Systematic Review”; “How Point (Single-Probability) Tasks Are Affected by Probability Format, Part 2: A Making Numbers Meaningful Systematic Review”; “How Synthesis Tasks Are Affected by Probability Format: A
Making Numbers Meaningful Systematic Review”; “How Time-Trend Tasks Are Affected by Probability Format: A Making Numbers Meaningful Systematic Review”; and “Scope, Methods, and Overview Findings for Making Numbers Meaningful Evidence Review of Communicating Probabilities in Health: A Systematic Review,” all published in Medical Decision Making Policy and Practice.
Natalie Benda and Meghan Reading Turchioe, PhD ’18, were the authors of “We Need a Healthcare System That Supports Patients and Health Professionals in Using AI (If They Choose),” published in Journal of General Internal Medicine.
Lauren Bochicchio and Tonda Hughes were among the authors of “Sexual Minority Women’s Perceptions of Sober Curiosity: Lessons Learned from a US Pilot Study,” published in Drug and Alcohol Review.
Lauren Bochicchio, Tonda Hughes, Elizabeth Chadbourne, and Corina Lelutiu-Weinberger were among the authors of “Toward an Understanding of Sexual Minority Women’s Social Stressors and Health in Post-Communist Countries in Europe: A Scoping Review,” published in BMC Public Health.
Maeve Brin, Stephen Ferrara, and Rebecca Schnall, PhD ’09, were among the authors of “Pre-Exposure Prophylaxis Providers in Birmingham, Alabama, and New York City, New York, Identify Critical Barriers to Newer Pre-Exposure Prophylaxis Strategies: A Mixed Methods Study,” published in Journal of the Association of Nurses in AIDS Care.
Maeve Brin, Claudia Michaels, and Rebecca Schnall, PhD ’09, were among the authors of “Acceptability and Perceived Usefulness of the CHAMPS Intervention for Improving Medication Adherence Among People with HIV in Alabama and New York,” published in International Journal of Medical Informatics.
Maeve Brin and Rebecca Schnall, PhD ’09, were among the authors of “Validating the Information Technology (IT) Implementa-
tion Framework to Implement mHealth Technology for Consumers: A Case Study of the Sense2Quit App for Smoking Cessation,” published in International Journal of Medical Informatics.
Jean-Marie Bruzzese was a co-author of “Editorial: Asthma and Mental Health: Novel Insights to the Experience, Etiology, Longitudinal Course, and Management of Mental Health in Asthma and Allergy,” published in Frontiers in Allergy.
Jean-Marie Bruzzese and Yihong Zhao were among the authors of “Barriers to Seeing a Healthcare Provider Among Rural Adolescents with Poorly Controlled Asthma,” published in Annals of Allergy, Asthma, and Immunology.
Penelope Buschman, Mary Tresgallo, and Marlene McHugh were among the authors of “Highlighting the Importance of Nurse Practitioner Fellowships in Palliative Care: A Model at the Columbia University School of Nursing,” published in Journal of Hospice and Palliative Nursing.
Billy Caceres was a co-author of “Altering Adverse Social Determinants of Cardiovascular Health in Sexual Minorities,” published in Journal of the American College of Cardiology.
Billy Caceres, Jacquelyn Taylor, and Tonda Hughes were among the authors of “Examining the Associations of Family-Related Factors with Hypertension in Sexual Minority Women,” published in LGBT Health.
Maya Castiblanco, Joseph Belloir, PhD ’23, Billy Caceres, Jean-Marie Bruzzese, and Kasey Jackman, PhD ’17, were among the authors of “Sleep Health Among Sexual and Gender Minority People in the United States: A Scoping Review,” published in Sleep Medicine.
Christina Congdon, Donald Boyd, and Gregory Alexander were the authors of “Contributing Factors and Associated Outcomes in Burnout Among Certified Registered Nurse Anesthetists: An Integrative Review,” pub-
lished in AANA [American Association of Nurse Anesthetists] Journal.
Suzanne Courtwright, Kathleen Flandrick, Madeline Pollifrone, and Lusine Poghosyan were among the authors of “A Scoping Review of Empirical Evidence on the Nurse Practitioner Workforce in Thailand,” published in International Nursing Review.
Ruth Masterson Creber was among the authors of “Association Between Myocardial Infarction and Quality of Life in the ISCHEMIA Trial,” published in Journal of the American College of Cardiology: Cardiovascular Interventions.
Brittany Daniel, Jianfang Liu, Jean-Marie Bruzzese, and Kasey Jackman, PhD ’17, were among the authors of “Disordered Eating in Early Adolescence: Disparities Among Minoritised Youth,” published in Journal of Advanced Nursing.
Christine DeForge, PhD ’23, was among the authors of “Lower Perceived Social Support During Hospitalization by Close Family Members May Have Significant Associations with Psychological Distress One Month After Cardiac Arrest,” published in Neurocritical Care.
Christina DeForge, PhD ’23, Andrew Dick, and Patricia Stone were among the authors of “Sociodemographic Disparities in the Use of Hospice by U.S. Nursing Home Residents: A Systematic Review,” published in American Journal of Hospice and Palliative Medicine.
Fabiana Cristina Dos Santos, Haomiao Jia, and Rebecca Schnall, PhD ’09, were among the authors of “The Effect of a Combined mHealth and Community Health Worker Intervention on HIV Self-Management,” published in Journal of the American Medical Informatics Association.
Fabiana Cristina Dos Santos and Rebecca Schnall, PhD ’09, were among the authors of “Evaluating the Effectiveness of a Mobile Health Intervention on Enhancing HIV Knowledge in Sexual and Gender Minor-
ity Men,” published in Journal of Acquired Immune Deficiency Syndromes, and “Evaluating the Usability of a Mobile Health Technology to Enhance Medication Adherence in People with HIV,” published in Studies in Health Technology and Informatics.
Safa Elkefi and Phoenix Matthews were the authors of “Factors Impacting Breast Cancer Survivors’ Performance of Annual Follow-up Mammograms: A Nationally Representative Study,” published in Patient Education and Counseling.
Student Alexandria Hahn and Rebecca Schnall, PhD ’09, were among the authors of “‘What I Wish I Would’ve Known Before My HIV Diagnosis’: Qualitative Insights from Women Living with HIV to Inform HIV Prevention Strategies,” published in AIDS Patient Care and STDs.
Student Sarah Harkins and Maxim Topaz were among the authors of “Symptom Burden: A Concept Analysis,” published in Nursing Science Quarterly.
Student Madison Horton, student Justinna Dixon, Rachel Paikoff, and Lusine Poghosyan were among the authors of “Advanced Practice Nurses in Primary Care and Their Impact on Health Service Utilisation, Costs, and Access Globally: A Scoping Review,” published in Journal of Clinical Nursing.
Tonda Hughes was among the authors of “Experiences Of and Recommendations For LGBTQ+-Affirming Substance Use Services: An Exploratory Qualitative Descriptive Study with LGBTQ+ People Who Use Opioids and Other Drugs,” published in Substance Abuse Treatment, Prevention, and Policy; “‘Moderation Is the Holy Grail’: The Acceptability of ‘Sober Curious’ Tools for Alcohol Reduction Among Midlife Women,” published in Drug and Alcohol Review; “Randomised Controlled Trial of LGBTQ-Affirmative Cognitive-Behavioural Therapy for Sexual Minority Women’s Minority Stress, Mental Health, and Hazardous Drinking: Project EQulP Protocol,” published in BMJ Open; “Reducing Heavy Drinking Through the
‘Sober Curious’ Movement in Australia: Protocol for a Mixed-Methods Study,” published in JMIR Research Protocols; and “Resilience Through Social Support: An Intersectional Analysis of Sexual Minority Women’s Social Resources for Wellbeing,” published in Journal of Homosexuality.
Tonda Hughes and Lauren Bochicchio were among the authors of “Using a Sober Curious Framework to Explore Barriers and Facilitators to Helping Sexual Minority Women Reduce Alcohol-Related Harms: Protocol for a Descriptive Study,” published in JMIR Research Protocols.
Tonda Hughes, Jianfang Liu, and Rebecca Schnall, PhD ’09, were among the authors of “Updating an HIV Knowledge Questionnaire with Pre-Exposure Prophylaxis Through Expert Opinions in the United States Using Delphi Methodology: A Qualitative Study,” published in Journal of the Association of Nurses in AIDS Care.
Ismael Ibrahim Hulchafo, student Sarah Harkins, Maxim Topaz, and Veronica Barcelona were among the authors of “Stigmatizing and Positive Language in Birth Clinical Notes Associated with Race and Ethnicity,” published in JAMA Network Open.
Kasey Jackman, PhD ’17, was among the authors of “‘I Don’t Think I Have Been Out of Fight or Flight. Ever.’ Transgender People’s Experiences in Inpatient Psychiatric Treatment,” published in International Journal of Nursing Studies, and was a co-author of “Pediatric Medical Traumatic Stress: What Psychiatric Nurses Need to Know,” published in Journal of Child and Adolescent Psychiatric Nursing.
Kasey Jackman, PhD ’17, and Walter Bockting were among the authors of “Prevalence and Correlates of Nonsuicidal Self-Injury Among Transgender People: Results from a U.S. Probability Sample,” published in Psychology of Sexual Orientation and Gender Diversity.
Jung Kang, Ashley Chastain, Jingjing Shang, and Patricia Stone were among the authors of
“Urban and Rural Disparities in COVID-19 Outcomes in the United States: A Systematic Review,” published in Medical Care Research and Review.
Elaine Larson was among the authors of “Development of the Initial Leapfrog Group’s Hand Hygiene Standard,” published in American Journal of Infection Control.
Ji Won Lee, Christine DeForge, PhD ’23, Bridget Morse-Karzen, Patricia Stone, Andrew Dick, Ashley Chastain, and Jingjing Shang were among the authors of “Racial and Ethnic Disparities in Post-Acute Care Service Utilization After Stroke,” published in Geriatric Nursing.
Rachel Lee and Sarah Rossetti, PhD ’09, were among the authors of “Generative AI Demonstrated Difficulty Reasoning on Nursing Flowsheet Data,” published in AMIA [American Medical Informatics Association] Annual Symposium Proceedings.
Jianfang Liu, Sophia McInerney, Trinity Casimir, and Rebecca Schnall, PhD ’09, were among the authors of “A Remote Intervention Based on mHealth and Community Health Workers for Antiretroviral Therapy Adherence in People with HIV: Pilot Randomized Controlled Trial,” published in JMIR Formative Research.
Phoenix Matthews was among the authors of “Effectiveness of Non-Pharmacological School-Based Therapies for Cigarette Smoking Cessation Among Adolescents in South and Southeast Asian Countries: A Systematic Review and Meta-Analysis,” published in Osong Public Health and Research Perspectives; “Feasibility of Remote Intensive Monitoring: A Novel Approach to Reduce Black Postpartum Maternal Cardiovascular Complications,” published in Journal of Midwifery and Women’s Health; “Navigating Challenges: Insights into Nurses’ Experiences of Caring for Patients During the COVID-19 Pandemic,” published in BMC Nursing; and “Neighborhood Violence, Hair Cortisol, and Perceived Stress Among Black Men Living in a Large Urban City,” published in Psychoneuroendocrinology.
Student Simon Paul Navarro was the author of “Exploring the Implications of the ‘Filipino Mafia’ in the Nursing Professions,” published in American Journal of Nursing.
Stephanie Niño de Rivera and Ruth Masterson Creber were among the authors of “Integrating Community-Based Participatory Research into Cardiac Clinical Trials: Lessons from REVASCHOICE,” published in Journal of the American College of Cardiology: Advances.
Stephanie Niño de Rivera, Yihong Zhao, Sarah Eslami, Natalie Benda, Meghan Reading Turchioe, PhD ’18, and Ruth Masterson Creber were among the authors of “Integrating Public Preferences to Overcome Racial Disparities in Research: Findings from a US Survey on Enhancing Trust in Research Data-Sharing Practices,” published in Journal of the American Medical Informatics Association: Open.
Monica O’Reilly-Jacob was among the authors of “The Quality of Home-Based Primary Care Delivered by Nurse Practitioners: A National Medicare Claims Analysis,” published in Journal of the American Geriatrics Society.
Rebecca Owens was among the authors of “A Mindfulness-Based Intervention: Effects on Psychiatric Nurses Well-Being and Burnout,” published in Journal of the American Psychiatric Nurses Association.
Lusine Poghosyan, Maura Dougherty, Kyle Featherston, and Monica O’Reilly Jacob were among the authors of “Dementia Care Management in Primary Care Practices: A Descriptive Study Among Nurse Practitioners,” published in BMC Primary Care.
Lusine Poghosyan, Jianfang Liu, Kathleen Flandrick, Marcia Robinson, DNP ’10, Maureen George, and Monica O’Reilly-Jacob were among the authors of “Racial and Ethnic Disparities in Emergency Department Use Among Older Adults with Asthma and Primary Care Nurse Practitioner Work Environments,” published in Nursing Research.
Stephanie Potts-Thompson, Laura Prescott, and Jacquelyn Taylor were among the authors of “Neighborhood Deprivation, Trauma Profiles, Coping, and Stress Prospectively Predict Depressive Symptoms Among Young African American Mothers in the InterGEN Study: A Latent Class Analysis,” published in Journal of Racial and Ethnic Health Disparities
Laura Prescott, Stephanie Potts-Thompson, and Jacquelyn Taylor were among the authors of “The Effectiveness of a Race-Based Stress Reduction Intervention on Improving Stress-Related Symptoms and Inflammation in African American Women at Risk for Cardiometabolic Disease: Protocol for Recruitment and Intervention for a Randomised Controlled Trial,” published in JMIR Research Protocols.
Sarah Rossetti, PhD ’09, was among the authors of “Clinician Perceptions of Generative Artificial Intelligence Tools and Clinical Workflows: Potential Uses, Motivations for Adoption, and Sentiments on Impact,” published in AMIA [American Medical Informatics Association] Annual Symposium Proceedings”; “Relationship Between Additional Required Nursing Documentation and Patient Outcomes: A Scoping Review,” published in Applied Clinical Informatics; and “Toward Identifying New Risk Aversions and Subsequent Limitations and Biases When Making De-Identified Structured Data Sets Openly Available in a Post-LLM World,” published in AMIA [American Medical Informatics Association] Annual Symposium Proceedings.
Sarah Rossetti, PhD ’09, and Haomiao Jia were among the authors of “EHR Documentation Frequency Changes Across the COVID-19 Pandemic,” and “Influence of the CONCERN Early Warning System on Unanticipated ICU Transfers, In-Hospital Mortality, and Length of Stay: Results from a Multi-Site Pragmatic Randomized Controlled Clinical Trial,” published in AMIA [American Medical Informatics Association] Annual Symposium Proceedings.
Sarah Rossetti, PhD ’09, Haomiao Jia, and Suzanne Bakken were among the authors of “Real-Time Surveillance System for Patient Deterioration: A Pragmatic ClusterRandomized Controlled Trial,” published in Nature Medicine.
Rebecca Schnall, PhD ’09, was among the authors of “Bridge Nodes Linking Depression and Medication Taking Self-Efficacy Dimensions Among Persons with HIV: A Secondary Data Analysis,” and “Different Classes of HIV-Preventive Behavioral Intention Among Youths Vulnerable to HIV Acquisition,” both published in AIDS and Behavior.
Rebecca Schnall, PhD ’09, Tonda Hughes, and Jianfang Liu were among the authors of “Protocol: The American Women: Assessing Risk Epidemiologically (AWARE) Cohort Study,” published in BMC Public Health.
Rebecca Schnall, PhD ’09, and Jianfang Liu were among the authors of “Feasibility and Acceptability of the Sense2Quit App for Improving Smoking Cessation in PWH,” published in AIDS and Behavior.
Jingjing Shang, Ashley Chastain, U Gayani E. Perera, and Patricia Stone were among the authors of “Policies for Infection Prevention and Control in Home Health Care, 2019 vs 2023,” published in JAMA Network Open.
Jingjing Shang, Uduwanage Gayani E. Perera, Jianfang Liu, and Ashley Chastain were among the authors of “Disparities in Infection Risk Among Home Health Care Patients: A Study Using Area Deprivation Index,” published in Journal of the American Medical Directors Association.
Jingjing Shang, Patricia Stone, and Maxim Topaz were among the authors of “The Paradox of Choice in Palliative Care Decision-Making in Managed Long-Term Care: A Qualitative Study,” published in Home Health Care Management and Practice.
Aluem Tark, PhD ’19, was among the authors of “Leveraging Artificial Intelligence/ Machine Learning Models to Identify
Potential Palliative Care Beneficiaries: A Systematic Review,” published in Journal of Gerontological Nursing, and a co-author of “Pursuing Work-Life Balance: Practical Strategies for Today’s Nurse Practitioners,” published in Journal of Nurse Practitioners.
Jacquelyn Taylor was among the authors of “Changes in DNA Methylation Associated with Psychobehavioral Interventions: A Scoping Literature Review,” published in Biological Research for Nursing.
Maxim Topaz was among the authors of “Artificial Intelligence in Nursing: Catalyzing Change Across Clinical, Educational, and Administrative Domains,” published in Journal of Nursing Scholarship; “Cancers Missed, Women Dismissed Yet Persist: Natural Language Processing of Online Forums,” published in Breast Cancer Research; “Comparing the Influence of Social Risk Factors on Machine Learning Model Performance Across Racial and Ethnic Groups in Home Healthcare,” published in Nursing Outlook; and “Nonlinear Relationship Between Vital Signs and Hospitalization/Emergency Department Visits Among Older Home Healthcare Patients and Critical Vital Sign Cutoff for Adverse Outcomes: Application of Generalized Additive Model,” published in Clinical Nursing Research.
Maxim Topaz, Sarah Rossetti, PhD ’09, and Zhihong Zhang were among the authors of “Building a Time-Series Model to Predict Hospitalization Risks in Home Health Care: Insights into Development, Accuracy, and Fairness,” published in Journal of the American Medical Directors Association.
Meghan Reading Turchioe, PhD ’18, was among the authors of “Opportunities and Challenges for Digital Health and Artificial Intelligence to Support Nurses: Results of a Survey of Nursing Informaticists,” published in Computers, Informatics, Nursing.
Meghan Reading Turchioe, PhD ’18, and Ruth Masterson Creber were among the authors of “Geriatric Vulnerabilities Among Adults with Heart Failure with Preserved Ejection
Fraction: A Cross-Continent Evaluation,” published in Journal of the American College of Cardiology: Advances.
Student David Lopez Veneros and Billy Caceres were among the authors of “Influence of Experiences of Discrimination and Anticipated Discrimination on Cardiovascular Health Outcomes,” published in Current Cardiology Reports.
Student Victoria Wingora, Christine DeForge, PhD ’23, Kimberlee Grier, and Patricia Stone were the authors of “Live Hospice Discharge of Individuals with Cognitive Disabilities: A Systematic Review,” published in Journal of the American Medical Directors Association.
Fengdi Xiao, Tonda Hughes, Jianfang Liu, and Rebecca Schnall, PhD ’09, were among the authors of “A Review of Provider Sexually Transmitted Infection Reporting Requirements Across the US: Identification of the Need for Standardization,” published in AIDS Patient Care and STDs.
Kiera Yamada was among the authors of “The Evolution of a Quality Improvement Curriculum in a Family Nurse Practitioner Residency Program,” published in Journal of the American Association of Nurse Practitioners.
Yihong Zhao was among the authors of “Examining Measurement Discrepancies in Adolescent Screen Media Activity with Insights from the ABCD Study,” published in Npj Mental Health Research.
Yihong Zhao and Jean-Marie Bruzzese were among the authors of “The Association of Mental Health, Asthma Control, and Acute Care Visits Among Rural Adolescents with Poorly Controlled Asthma,” published in Journal of School Nursing.
Yihong Zhao, Billy Caceres, Morgan Morrison, Laura Prescott, Stephanie Potts-Thompson, Erica Matute-Arcos, and Jacquelyn Taylor were among the authors of “Discrimination, Coping, and DNAm Accelerated Aging Among African American Mothers of the InterGEN Study,” published in Epigenomes.

Principal Investigator: Gregory Alexander, PhD
Project Title: Reducing Avoidable Nursing Home-to-Hospital Transfers of Residents with ADRD: An Analysis of Interdisciplinary Team Communication Using Text Messages R01AG078281
Program Funding Source: NIH-NIA (University of Missouri Subcontract)
Total Budget: $135,270
Project Dates: 8/15/2022–5/31/2025
Principal Investigator: Gregory Alexander, PhD
Project Title: Impact of Nursing Home Leadership Care Environments and Health Information Technology on Outcomes of Residents with Alzheimer’s Disease and Related Dementias (ADRD), (Multiple PI: Lusine Poghosyan) R01AG080517
Program Funding Source: NIH-NIA
Total Budget: $3,929,440
Project Dates: 2/15/2023–11/30/2027
Principal Investigator: Gregory Alexander, PhD
Project Title: A Roadmap for Research: The International Summit on Innovation and Technology in Care of Older People (IS-ITCOP) R13HS030051
Program Funding Source: AHRQ
Total Budget: $49,943
Project Dates: 4/1/2024–3/31/2025
Principal Investigator: Veronica Barcelona, PhD
Project Title: Epigenomic Pathways from Racism to Preterm Birth R01HD110429
Program Funding Source: NIH-NICHD
Total Budget: $2,143,751
Project Dates: 3/14/2023–2/29/2028
Principal Investigator: Veronica Barcelona, PhD
Project Title: Using Machine Learning to Measure Racial/Ethnic Bias in Obstetric Settings UCD A20-2994-S021
Program Funding Source: Betty Irene Moore Fellowship Program for Nurse Leaders and
Innovators (University of California Davis)
Total Budget: $500,000
Project Dates: 7/1/2022–6/30/2025
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Symptom Screening Linked to Care Pathways for Children with Cancer: A Cluster Randomized Trial R01CA251112
Program Funding Source: NIH-NCI (Hospital for Sick Children Subcontract)
Total Budget: $67,863
Project Dates: 8/1/2020–4/30/2025
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Children’s Oncology
Group NCI Community Oncology Research Program (NCORP) Research UG1CA189955
Program Funding Source: NIH-NCI (Public Health Institute Subcontract)
Total Budget: $42,450
Project Dates: 8/1/2023–7/31/2025
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Center for SOcial CApital (SOCA): Promoting Multigenerational Health U54 CA280808
Program Funding Source: NIH-NCI (Weill Cornell Medical College Subcontract)
Total Budget: $141,266
Project Dates: 5/1/2023–4/30/2025
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Feasibility and Usability of a Spanish-Transcreated Pediatric PostTransplant R21MD019075
Program Funding Source: NIH-NIMHD (Nationwide Children’s Subcontract)
Total Budget: $125,011
Project Dates: 9/1/2023–3/31/2026
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Navigating Financial and Health-Related Social Needs in Adolescent and Young Adult Cancer Survivors (AYA-NAV): A Digital Intervention Pilot Study R21NR021310
Program Funding Source: NIH-NINR
Total Budget: $461,093
Project Dates: 8/5/2024–7/31/2026
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Unpacking Sperm Banking Insurance Coverage Among Newly Diagnosed AYA Cancer Patients
CNRI30008578
Program Funding Source: Rally Foundation for Childhood Cancer via Children’s National Hospital
Total Budget: $23,749
Project Dates: 7/1/2024–06/30/2025
Principal Investigator: Melissa Beauchemin, PhD
Project Title: Columbia-Cornell-Einstein EQUIP+ Center for Learning Health System Science 5P30HS029763-02
Program Funding Source: AHRQ (Pilot Project)
Total Budget: $199,799
Project Dates: 10/1/2024–09/30/2026
Principal Investigator: Natalie Benda, PhD
Project Title: Maternal Outcome Monitoring and Support (MOMS)—An mHealth Symptom Self-Monitoring and Decision
Support System to Reduce Racial and Ethnic Disparities in Postpartum Outcomes
R00MD015781
Program Funding Source: NIH-NIMHD
Total Budget: $732,428
Project Dates: 2/1/2023–1/31/2026
Principal Investigator: Natalie Benda, PhD
Project Title: Telemedicine for Patients with Limited English Proficiency: A MixedMethods Approach to Identifying and Addressing Disparities R03HS029047
Program Funding Source: AHRQ
Total Budget: $69,138
Project Dates: 2/1/2023–12/31/2024
Principal Investigator: Lauren Bochicchio, PhD
Project Title: Understanding the Individual and Combined Impact of Childhood Sexual Abuse and Minority Stress on Hazardous Drinking Among Sexual Minority Women: Is Emotion Dysregulation a Key Factor?
F32AA029957
Program Funding Source: NIH-NIAAA
Total Budget: $218,118
Project Dates: 8/1/2022–7/31/2025
Principal Investigator: Walter Bockting, PhD
Project Title: Gender Affirmation, Quality of Life, and Access to Care: A MixedMethod Longitudinal Investigation
R01NR019315
Program Funding Source: NIH-NINR (Visiting Nurse Service of New York Subcontract)
Total Budget: $1,271,390
Project Dates: 7/1/2021–4/30/2026
Principal Investigator: Walter Bockting, PhD
Project Title: Social Stress, Social Connectedness, and Health R01MD017085
Program Funding Source: NIH-NIMHD
Total Budget: $3,338,769
Project Dates: 7/15/2023–12/31/2027
Principal Investigator: Ulf Bronas, PhD
Project Title: A Dynamic Environmental Exposure Approach to Study Behaviors in Mid-Life R01AG062180
Program Funding Source: NIH-NIA (University of Illinois Subcontract)
Total Budget: $180,453
Project Dates: 6/1/2023–7/31/2027
Principal Investigator: Ulf Bronas, PhD
Project Title: Accelerated Age-related Cognitive Decline: Impact of Exercise on Executive Function and Neuroplasticity (EXEC-study) R01AG076456
Program Funding Source: NIH-NIA
Total Budget: $1,638,606
Project Dates: 5/1/2024–4/30/2028
Principal Investigator: Ulf Bronas, PhD
Project Title: Midwest Roybal Center for Health Promotion and Translation 2P30AG022849-21
Program Funding Source: NIH-NIA (University of Illinois Subcontract)
Total Budget: $81,074
Project Dates: 8/15/2024–5/31/2029
Principal Investigator: Jean-Marie Bruzzese, PhD
Project Title: Translating an Evidence-Based Urban Asthma Program for Rural Adolescents: Testing Effectiveness and Cost-Effectiveness and Understanding Factors Associated with Implementation R01HL136753
Program Funding Source: NIH-NHLBI
Total Budget: $3,620,591
Project Dates: 7/5/2017–12/31/2024
Principal Investigator: Jean-Marie Bruzzese, PhD
Project Title: The Efficacy of CAMP Air, a Web-based Asthma Intervention, Among Urban Adolescents with Uncontrolled Asthma R33HL151958
Program Funding Source: NIH-NHLBI
Total Budget: $3,165,885
Project Dates: 8/10/2022–6/30/2026
Principal Investigator: Billy Caceres, PhD
Project Title: A Daily Diary Examination of the Influence of Intersectional Stigma on Blood Pressure R56HL168489
Program Funding Source: NIH-NHLBI
Total Budget: $815,009
Project Dates: 9/1/2023–8/31/2024
Principal Investigator: Billy Caceres, PhD
Project Title: A Daily Diary Examination of the Influence of Intersectional Stigma on Blood Pressure R01HL168489
Program Funding Source: NIH-NHLBI
Project Dates: Total Budget: $3,166,090
Project Dates: 9/1/2024–5/31/2028
Principal Investigator: Christina Congdon, MS
Project Title: Anesthesia Care Delivery in Rural America: The Impact of Organizational Climate on Burnout, Job Satisfaction, and Intention to Leave Among Certified Registered Nurse Anesthetists R36HS030178
Program Funding Source: AHRQ
Total Budget: $43,483
Project Dates: 9/1/2024–8/31/2025
Principal Investigator: Christina Congdon, MS
Project Title: Anesthesia Care Delivery in Rural America: The Impact of Organizational Climate on Burnout, Job Satisfaction, and Intention to Leave among Certified Registered Nurse Anesthetists AANA2024-F-1
Program Funding Source: American Association of Nurse Anesthetists Foundation
Total Budget: $6,495
Project Dates: 7/15/2024–6/30/2025
Principal Investigator: Elizabeth Corwin, PhD
Project Title: The Impact of a Culturally Based Live Music Intervention on the Metabolites and Metabolic Pathways Associated with Chronic Stress and the Risk of Preterm Birth in Black Women R01MD016899 (Multiple PI: Joanne Loewy)
Program Funding Source: NIH-NIMHD
Total Budget: $3,446,646
Project Dates: 4/16/2023-11/30/2027
Principal Investigator: Stephen Ferrara, DNP
Project Title: HRSA Advanced Nursing Education Nurse Practitioner Residency (ANE-NPR) Program T59HP49629
Program Funding Source: HRSA (Bassett Subcontract)
Total Budget: $120,000
Project Dates: 8/1/2023–7/31/2027
Principal Investigator: Stephen Ferrara, DNP
Project Title: Advanced Nursing Education — Nurse Practitioner Residency Fellowship Program T5949629
Program Funding Source: HRSA (Community Healthcare Network Subcontract)
Total Budget: $283,292
Project Dates: 8/1/2023–7/31/2027
Principal Investigator: Lorraine Frazier, PhD
Project Title: Ladies Christian Union (LCU)
Fund for Women’s Education LCUCU22-1579
Program Funding Source: Ladies Christian Union (LCU)
Total Budget: $100,000
Project Dates: 7/1/2024–6/30/2025
Principal Investigator: Lorraine Frazier, PhD
Project Title: Pathways to Leadership and Advancement in Nursing (PLAN) Program HEARSTCU24-1468
Program Funding Source: Hearst Foundations
Total Budget: $300,000
Project Dates: 1/1/2025–12/31/2026
Principal Investigator: Tyler Gaedecke, BSN
Project Title: Personal Healthcare Networks of Transgender and Gender-Diverse Adults After GenderAffirming Surgery
Program Funding Source: Sigma Foundation for Nursing
Total Budget: $5,000
Project Dates: 6/1/2024–5/31/2025
Principal Investigator: Tyler Gaedecke, BSN
Project Title: Personal Healthcare Networks of Transgender and GenderDiverse Adults After Gender-Affirming Surgery F31NR021239
Program Funding Source: NIH-NINR
Total Budget: $91,915
Project Dates: 7/1/2024–3/31/2026
Principal Investigator: Maureen George, PhD
Project Title: BREATHE: An EfficacyImplementation Trial of a Brief Shared Decision-Making Intervention Among Black Adults with Uncontrolled Asthma in Federally Qualified Health Centers (FQHC) R01NR019275
Program Funding Source: NIH-NINR
Total Budget: $2,447,470
Project Dates: 5/6/2020–2/28/2026
Principal Investigator: Alexandra Hahn, MS
Project Title: The Role of Social Determinants in Reproductive Coercion: Understanding Health Information and Support Need F31NR021330
Program Funding Source: NIH-NINR
Total Budget: $103,948
Project Dates: 9/1/2024–8/31/2026
Principal Investigator: Amanda Hessels, PhD
Project Title: Simulation to Improve Infection Prevention and Patient Safety: The SIPPS Trial R18HS026418
Program Funding Source: AHRQ
Total Budget: $1,860,798
Project Dates: 3/1/2019–2/29/2025
Principal Investigator: Tonda Hughes, PhD
Project Title: Stress, Hazardous Drinking, and Intimate Partner Aggression in a Diverse Sample of Women and Their Partners R01AA027252
Program Funding Source: NIH-NIAAA
Total Budget: $2,750,690
Project Dates: 9/10/2019–6/30/2025
Principal Investigator: Tonda Hughes, PhD
Project Title: A Unified Protocol to Address Sexual Minority Women’s Minority Stress, Mental Health, and Hazardous Drinking R01AA029088
Program Funding Source: NIH-NIAAA (Yale University Subcontract)
Total Budget: $426,550
Project Dates: 9/12/2022–8/31/2027
Principal Investigator: Haomiao Jia, PhD
Project Title: Mental Health Burden on the U.S. Population, Including Workers in the Wake of the COVID-19 Pandemic 20IPA2014150-M01
Program Funding Source: DHHS-CDCNIOSH-SSTRB
Total Budget: $150,000
Project Dates: 9/1/2020–8/31/2024
Principal Investigator: Jung “Chloe” Kang, PhD
Project Title: Center to Improve Chronic disease Outcomes through Multi-level and Multi-generational approaches Unifying Novel Interventions and Training for health EquitY (The COMMUNITY Center)
P50MD017341 Pilot Project
Program Funding Source: NIH-NIMHD
Total Budget: $50,000
Project Dates: 7/1/2024–6/30/2026
Principal Investigator: Ana Kelly, PhD
Project Title: Effect of Race on Cultural Humility Following Simulation Telehealth Case Scenarios Among Second Degree Nursing Students: RCT
Program Funding Source: National League for Nursing
Total Budget: $29,523
Project Dates: 9/1/2023–08/31/2025
Principal Investigator: Corina LelutiuWeinberger, PhD
Project Title: Ending the HIV Epidemic With Equity: An All-Facility Intervention for and Healthcare Staff Wellbeing R01NR020583
Program Funding Source: NIH-NINR
Total Budget: $4,016,361
Project Dates: 7/1/2022–4/30/2028
Principal Investigator: Corina LelutiuWeinberger, PhD
Project Title: Preparing for Pre-Exposure Prophylaxis Implementation in Central-Eastern European Countries with Low Access to Biomedical Prevention R33TW011752
Program Funding Source: Fogarty International Center
Total Budget: $981,844
Project Dates: 9/9/2020–6/30/2025
Principal Investigator: Corina LelutiuWeinberger, PhD
Project Title: Building Mobile HIV Prevention and Mental Health Support in Low-Resource Settings R01MH116829
Program Funding Source: NIH-NIMH
Total Budget: $3,880,940
Project Dates: 9/5/2018–6/30/2025
Principal Investigator: Corina LelutiuWeinberger, PhD
Project Title: Examining a Multicomponent Intervention to Improve HIV Health among Black Men in Southern Ending the HIV Epidemic in the U.S. Jurisdictions R01MH134265
Program Funding Source: NIH-NIMHD (Rutgers University Subcontract)
Total Budget: $103,268
Project Dates: 8/1/2023–5/31/2028
Principal Investigator: Corina LelutiuWeinberger, PhD
Project Title: Feasibility, Acceptability, and Preliminary Efficacy of an Adapted Group-Based and Online HIV Prevention
Intervention for Immigrant Sexual Minority Men in the US R34MH134603
Program Funding Source: NIH-NIMH (University of Illinois Subcontract)
Total Budget: $60,997
Project Dates: 9/11/2024–03/21/2025
Principal Investigator: David Lopez Veneros, MA
Project Title: Health Policy Research Scholars Cohort Seven–2023
Program Funding Source: Robert Wood Johnson Foundation
Total Budget: $124,000
Project Dates: 9/1/2023–8/31/2027
Principal Investigator: Maribeth Massie, PhD
Project Title: Nurse Anesthetist Traineeships A2233098
Program Funding Source: HRSA
Total Budget: $84,142
Project Dates: 7/1/2023–6/30/2027
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Improve the Meaning of Patient-Reported Outcomes to Evaluate Effectiveness for Cardiac Care (IMPROVE-Cardiac Care) R01HL161458
Program Funding Source: NIH-NHLBI
Total Budget: $2,557,678
Project Dates: 7/23/2022–6/30/2026
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Randomized Comparison of the Clinical Outcome of Single Versus Multiple Arterial Grafts: Cognition (ROMA:Cog) R01NS123639
Program Funding Source: NIH-NINDS
Total Budget: $3,652,136
Project Dates: 7/1/2022–6/30/2026
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Strengthening Healthcare and Research Engagement Through Data Sharing: SHARE 3R01NS123639-04S1
Program Funding Source: NIH-NINDS
Total Budget: $157,869
Project Dates: 7/1/2024–6/30/2025
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: mHealth and Mobile Ultrasound for Mothers R21HD103053
Program Funding Source: NIH-NICHD
Project Dates: Total Budget: $287,260
Project Dates: 9/3/2022–2/28/2026
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Randomized Comparison of the Clinical Outcome of Single Versus Multiple Arterial Grafts: Quality of Life (ROMA: QOL) R01HL152021
Program Funding Source: NIH-NHLBI (Weill Medical College of Cornell University Subcontract)
Total Budget: $554,610
Project Dates: 7/1/2022–3/31/2026
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Using Mobile Integrated Health and Telehealth to Support Transitions of Care Among Heart Failure Patients IHS-2019C2-17373-IC
Program Funding Source: Patient-Centered Outcomes Research Institute (PCORI)
Total Budget: $2,900,722
Project Dates: 7/1/2022–7/31/2026
Principal Investigator: Ruth Masterson Creber, PhD
Project Title: Revascularization Choices Among Under-Represented Groups Evaluation: The RECHARGE Program PCORI #30048
Program Funding Source: Patient-Centered Outcomes Research Institute (PCORI)–Weill Cornell Medicine Subcontract
Total Budget: $1,640,517
Project Dates: 11/1/2023–5/1/2030
Principal Investigator: Phoenix Matthews, PhD
Project Title: Mi QUIT CARE (Mile Square QUIT Community-Access-ReferralExpansion) UH3HL151302
Program Funding Source: NIH-NHLBI (University of Illinois at Chicago Subcontract)
Total Budget: $1,174,188
Project Dates: 9/1/2023–8/31/2027
Principal Investigator: Phoenix Matthews, PhD
Project Title: Reducing Racial Disparities in Lung Cancer Outcomes by Decoding Neighborhood Contextual Environment
R01MD014839
Program Funding Source: NIH-NIMHD (University of Illinois at Chicago Subcontract)
Total Budget: $55,310 Project Dates: 10/01/2022–1/31/2026
Principal Investigator: Phoenix Matthews, PhD
Project Title: A Randomized Control Trial to Improve Metabolic Outcomes in African American Pregnant Women R01MD015724
Program Funding Source: NIH-NIMHD (University of Illinois at Chicago Subcontract)
Total Budget: $80,546 Project Dates: 8/16/2022–4/30/2023
Principal Investigator: Phoenix Matthews, PhD
Project Title: Center for SOcial CApital (SOCA): Promoting Multigenerational Health (Multiple PIs: Rulla Tamimi [contact], Erica Phillips, and Mary Beth Terry) U54CA280808
Program Funding Source: NIH-NCI (Weill Medical College of Cornell University Subcontract)
Total Budget: $901,991 Project Dates: 5/31/2023–4/30/2028
Principal Investigator: Phoenix Matthews, PhD
Project Title: Smoking and Cancer-Related Health Disparities Among Sexual and Gender Minority Adults R01CA276500
Program Funding Source: NIH-NCI (University of Michigan Subcontract)
Total Budget: $338,350
Project Dates: 12/15/2023–11/30/2028
Principal Investigator: Allison Norful, PhD
Project Title: Physiologic Stress and Epigenetic Mechanisms That Precipitate Risk for Suicidal Behavior in Nurses K08MH130652
Program Funding Source: NIH-NIMH
Total Budget: $960,458
Project Dates: 6/15/2023–5/31/2028
Principal Investigator: Monica O’ReillyJacob, PhD
Project Title: Reducing Barriers to
Value-based Care Payments in Nurse Practitioner-led Primary Care
Program Funding Source: American Nurses Foundation
Total Budget: $655,050
Project Dates: 1/1/2024–06/30/2026
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Social Networks in Medical Homes and Impact on Patient Care and Outcomes R01HS025937
Program Funding Source: AHRQ
Total Budget: $2,123,805
Project Dates: 2/1/2019–1/31/2025
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Care for Persons with Dementia in Nurse Practitioner Practices and Racial and Ethnic Health Disparities R01AG069143
Program Funding Source: NIH-NIA
Total Budget: $3,616,936
Project Dates: 9/15/2020–5/31/2026
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Home Based Primary Care for Persons Living with Dementia: Nurse Practitioner Teams and Outcomes (Multiple PI: Zainab Osakwe)
R21AG077384
Program Funding Source: NIH-NIA
Total Budget: $474,360
Project Dates: 8/1/2022–7/31/2025
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Effects of Integration of Advanced Practice Providers into Surgical Group Practice R01HS028975
Program Funding Source: AHRQ (University of Michigan Subcontract)
Total Budget: $51,910
Project Dates: 3/1/2023–12/31/2027
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Enhancing Nurse Practitioner Primary Care Delivery to Address Social Determinants of Health and Reduce Health Disparities: A Mixed-Methods National Study R01NR021007
Program Funding Source: NIH-NINR
Total Budget: $3,124,761
Project Dates: 4/7/2023–1/31/2027
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Social Networks in Nurse Practitioner Teams Caring for Patients with Dementia and Impact on Racial and Ethnic Disparities
R01AG085479
Program Funding Source: NIH-NIA
Total Budget: $3,473,008
Project Dates: 5/15/2024–1/31/2029
Principal Investigator: Lusine Poghosyan, PhD
Project Title: Systems Science and Comparative and Cost-Effectiveness
Research Training for Nurse Scientists (S2CER2) T32NR014205 (Multiple PI: Patricia Stone)
Program Funding Source: NIH-NINR
Total Budget: $2,445,840
Project Dates: 7/1/2023–6/30/2028
Principal Investigator: Rebekah Ruppe, DNP
Project Title: Project ACCESS (Abortion Care Clinical Expansion and Early Pregnancy Loss Support Series) New York State Medication Abortion/Early Pregnancy Loss Workgroup
Program Funding Source: Reproductive Health Access Project (RHAP) and Primary Care Development Corporation (PCDC)
Total Budget: $5,000
Project Dates: 5/8/2023–8/31/2024
Principal Investigator: Rebecca Schnall, PhD
Project Title: Dissemination of the WiseApp for Improving Health Outcomes Across Settings R18HS028523
Program Funding Source: AHRQ
Total Budget: $1,932,705
Project Dates: 9/30/2021–8/31/2026
Principal Investigator: Rebecca Schnall, PhD
Project Title: mChoice: Improving PrEP Uptake and Adherence Among Minority MSM Through Tailored Provider Training and Adherence Assistance in Two HighPriority Settings U01PS005229
Program Funding Source: CDC
Total Budget: $5,192,621
Project Dates: 9/30/2021–9/29/2026
Principal Investigator: Rebecca Schnall, PhD
Project Title: Development and Pilot
Testing of a Just-in-Time Mobile Smoking Cessation Intervention for Persons Living with HIV R21CA265961 (Multiple PI: Ming-Chun Huang)
Program Funding Source: NIH-NCI
Total Budget: $438,936
Project Dates: 9/1/2021–8/31/2024
Principal Investigator: Rebecca Schnall, PhD
Project Title: Development and Testing of MyPEEPS Mobile for Young Transgender Men R34MH128163 (Multiple PI: Robert Garofalo)
Program Funding Source: NIH-NIMH
Total Budget: $733,466
Project Dates: 1/1/2022–11/30/2025
Principal Investigator: Rebecca Schnall, PhD
Project Title: CHAMPS: A Randomized Trial of a Community Health Worker Intervention for Persons Living with HIV in Two High-Priority Settings R01NR019758 (Multiple PI: D. Scott Batey)
Program Funding Source: NIH-NINR
Total Budget: $2,877,282
Project Dates: 9/25/2020–6/30/2025
Principal Investigator: Rebecca Schnall, PhD
Project Title: mLab App for Improving Uptake of Rapid HIV Self-Testing and Linking Youth to Care R01MH118151 (Multiple PI: Robert Garofalo)
Program Funding Source: NIH-NIMHD
Total Budget: $4,090,639
Project Dates: 8/3/2018–5/31/2024
Principal Investigator: Rebecca Schnall, PhD
Project Title: Reducing Health Disparities Through Informatics (RHeaDI)
T32NR007969 (Multiple PI: Suzanne Bakken)
Program Funding Source: NIH-NINR
Total Budget: $3,224,793
Project Dates: 7/1/2022–6/30/2027
Principal Investigator: Rebecca Schnall, PhD
Project Title: American Women: Assessing Risk Epidemiologically (AWARE-RFA) R01AI172469 (Multiple PIs: Amy Johnson and Mirjam-Colette Kempf)
Program Funding Source: NIH-NIAID
Total Budget: $15,149,718
Project Dates: 8/18/2022–7/31/2028
Principal Investigator: Rebecca Schnall, PhD
Project Title: MyPEEPS Mobile LITE: Limited Interaction Efficacy Trial of MyPEEPS
Mobile to Reduce HIV Incidence and Better Understand the Epidemiology of HIV Among YMSM UH3AI169658 (Multiple PIs: Dustin Duncan and Robert Garofalo)
Program Funding Source: NIH-NIAID
Total Budget: $7,420,722
Project Dates: 9/1/2022–7/31/2027
Principal Investigator: Rebecca Schnall, PhD
Project Title: Promoting Viral Suppression Through the CHAMPS+ Intervention in the Deep South R01MD019184 (Multiple PI: D. Scott Batey)
Program Funding Source: NIH-NIMHD
Total Budget: $5,335,905
Project Dates: 9/21/2023–3/31/2028
Principal Investigator: Rebecca Schnall, PhD
Project Title: MyPEEPS Mobile Plus: A Multi-Level HIV Prevention Intervention for Young MSM R01MD019181 (Multiple PI: Robert Garofalo)
Program Funding Source: NIH-NIMHD
Total Budget: $5,158,684
Project Dates: 9/21/2023–3/31/2028
Principal Investigator: Rebecca Schnall, PhD
Project Title: Drive To Zero: Developing a Digital Cohort to Understand the Drivers of Non-Sustained Viral Suppression in the Deep South UG3AI176566
Program Funding Source: NIH-NIAID (University of Alabama Birmingham Subcontract)
Total Budget: $497,510
Project Dates: 8/1/2023–2/28/2026
Principal Investigator: Rebecca Schnall, PhD
Project Title: Project PrOVIDE: PrEP Optimization Via Implementation, Dissemination, and Evaluation U01PS005270
Program Funding Source: CDC (Lurie Children’s Hospital Subcontract)
Total Budget: $124,318
Project Dates: 9/30/2023–9/29/2025
Principal Investigator: Rebecca Schnall, PhD
Project Title: Implementation of Screen, Treat, and Triage for Women Living with HIV in La Romana (iSTAR) U01CA275110
Program Funding Source: NIH-NCI
Total Budget: $2,992,618
Project Dates: 9/1/2024–8/31/2029
Principal Investigator: Jingjing Shang, PhD
Project Title: Infection Prevention in Home Health Care (InHOME) R01NR016865 (Multiple PI: Patricia Stone)
Program Funding Source: NIH-NINR
Total Budget: $3,378,520
Project Dates: 4/18/2022–1/31/2026
Principal Investigator: Jingjing Shang, PhD
Project Title: Disparities in Infection in Home Health and Patients/Caregivers’ Perceptions (Dis-Infection in HHC) R01HS028637
Program Funding Source: AHRQ
Total Budget: $2,443,775
Project Dates: 9/3/2021–8/31/2026
Principal Investigator: Jingjing Shang, PhD
Project Title: Impact of COVID-19 on Care Transitions and Post-Acute Care of Vulnerable Populations (ACROSS-CARE) R01AG074492 (Multiple PI: Patricia Stone)
Program Funding Source: NIH-NIA
Total Budget: $3,334,303
Project Dates: 9/1/2021–4/30/2025
Principal Investigator: Jingjing Shang, PhD
Project Title: Effectiveness of Strategies to Improve Outcomes After Hospitalization for Acute Myocardial Infarction in Older Adults R01HL160822
Program Funding Source: NIH-NHLBI (Yale University Subcontract)
Total Budget: $115,512
Project Dates: 3/01/2022–2/28/2025
Principal Investigator: Patricia Stone, PhD
Project Title: Center for Improving Palliative Care for Vulnerable Adults with MCC (CIPC) P20NR018072 (Multiple PI: Jingjing Shang)
Program Funding Source: NIH-NINR
Total Budget: $2,039,992
Project Dates: 8/8/2018–12/31/2024
Principal Investigator: Patricia Stone, PhD
Project Title: Hospice Use, Hospice Quality, and Related End-of-Life Outcomes in Nursing Homes R01NR020601 (Multiple PIs: Andrew Dick and Lara Dhingra)
Program Funding Source: NIH-NINR
Total Budget: $2,218,515 Project Dates: 8/23/2023–6/30/2027
Principal Investigator: Jacquelyn Taylor, PhD
Project Title: Research Education in Cardiovascular Conditions (RECV) NYUF1416-01S (R25HL145323)
Program Funding Source: NIH-NHLBI (New York University Subcontract)
Total Budget: $12,500 Project Dates: 4/17/2020–4/01/2023
Principal Investigator: Jacquelyn Taylor, PhD
Project Title: The Impact of a Race-Based Stress Reduction Intervention on WellBeing, Inflammation, and DNA Methylation in Older African American Women at Risk for Cardiometabolic Disease (Multiple PI: Karen Saban [contact]) R01AG081251
Program Funding Source: NIH-NIA (Loyola University of Chicago Subcontract)
Total Budget: $1,408,790
Project Dates: 4/1/2023–1/31/2028
Principal Investigator: Maxim Topaz, PhD
Project Title: Improving Patient Prioritization During Hospital-Homecare Transition: A Mixed-Methods Study of a Clinical Decision Support Tool R01NR018831
Program Funding Source: NIH-NINR Total Budget: $2,019,591 Project Dates: 9/25/2019–4/30/2024
Principal Investigator: Maxim Topaz, PhD Project Title: Using Automated Speech Processing to Improve Identification of Risk for Hospitalizations and Emergency Department Visits in Home Healthcare R01AG081928 (Multiple PIs: Julia Hirschberg and Zoran Kostic)
Program Funding Source: NIH-NIA
Total Budget: $2,462,830
Project Dates: 6/15/2023–2/28/2027
Principal Investigator: Maxim Topaz, PhD
Project Title: Optimizing Clinical Documentation Quality to Reduce Health Disparities in Home Healthcare: The ENGAGE Study R01MD018028 (Multiple PIs: Jacquelyn Taylor and Scott Sittig)
Program Funding Source: NIH-NIMHD
Total Budget: $2,676,243
Project Dates: 9/24/2023–4/30/2027
Principal Investigator: Maxim Topaz, PhD
Project Title: NurseAssist-AI: Leveraging AI to Minimize Documentation and Maximize Decision Support in Home Healthcare
Program Funding Source: American Nurses Foundation
Total Budget: $466,590
Project Dates: 6/1/2025–5/31/2027
Principal Investigator: Meghan Turchioe, PhD
Project Title: Data-Driven Shared DecisionMaking to Reduce Symptom Burden in Atrial Fibrillation R00NR019124
Program Funding Source: NIH-NINR
Total Budget: $732,338
Project Dates: 8/1/2022–10/31/2025
Principal Investigator: Meghan Turchioe, PhD
Project Title: Usability Evaluation of a HeartLogic Mobile Application Prototype
Program Funding Source: Boston
Scientific Corporation
Total Budget: $67,347
Project Dates: 3/1/2023–12/31/2024
Principal Investigator: Zidu “Miranda” Xu, MMed
Project Title: 2024 Marilyn D. Harris
Research Grant
Program Funding Source: International Home Care Nurses Organization
Total Budget: $2,000
Project Dates: 1/1/2024–12/31/2024
Principal Investigator: Zidu “Miranda” Xu, MMed
Project Title: MMed MERID-EQ: Multimodal Early Risk Identification for Home Healthcare Equity in Infection Risks
Program Funding Source: Sigma Foundation for Nursing
Total Budget: $5,000
Project Dates: 6/1/2024–5/31/2025
Principal Investigator: Zidu “Miranda” Xu, MMed
Project Title: Employing Explainable Artificial Intelligence (XAI) for Home Healthcare
Infection Risk Prediction Equity and Clarity: A Mixed-Method Study
Program Funding Source: Research Institute for Home Care
Total Budget: $10,000
Project Dates: 7/31/2024–06/30/2025
Principal Investigator: Yihong Zhao, PhD
Project Title: Use of Advanced Analytics to Understand Brain-Behavior Screen
Media Activity Relationship in ABCD Data RF1MH128614
Program Funding Source: NIH-NIMH (Yale University Subcontract)
Total Budget: $577,824
Project Dates: 9/10/2021–9/9/2025
Principal Investigator: Yihong Zhao, PhD
Project Title: Cortical Subcortical Reorganization and Risk Behaviors of Early Alcohol Use Initiation R01AA029611
Program Funding Source: NIH-NIAAA (Yale University Subcontract)
Total Budget: $859,991
Project Dates: 9/25/2021–7/31/2026
Principal Investigator: Maryam Zolnoori, PhD
Project Title: Development of a Screening Algorithm for Timely Identification of Patients with Mild Cognitive Impairment and Early Dementia in Home Healthcare K99AG076808
Program Funding Source: NIH-NIA
Total Budget: $230,278
Project Dates: 12/15/2022–8/31/2024
Principal Investigator: Maryam Zolnoori, PhD
Project Title: Development of a Screening Algorithm for Timely Identification of Patients with Mild Cognitive Impairment and Early Dementia in Home Healthcare R00AG076808
Program Funding Source: NIH-NIA
Total Budget: $741,962
Project Dates: 9/1/2024–6/30/2027
Principal Investigator: Maryam Zolnoori, PhD
Project Title: Columbia Center for Interdisciplinary Research on Alzheimer’s Disease Disparities (CIRAD) P30AG059303 Pilot Project
Program Funding Source: NIH-NIA
Total Budget: $35,000
Project Dates: 7/1/2024–6/30/2025

560 West 168th Street, MC 6
New York, NY 10032
“As a nurse research scientist, my work focuses on designing health technology that improves lives. I believe that digital tools should meet people where they are—culturally, in their preferred language, and with sensitivity to the emotional and psychological realities they face. When a Spanish-speaking HIV patient tells me that a mobile app helped them take their meds on time for the first time in months—that’s when I know I have made a difference.”
— Rebecca Schnall, PhD ’09, MPH, RN-BC, FAAN
Mary Dickey Lindsay Professor of Disease Prevention and Health Promotion; Associate Dean of Faculty Development
YOUR SUPPORT OF THE NURSING RESEARCH FUND FUELS HEALTH INNOVATIONS that make it easier for patients—no matter their language or background— to manage the care they need.
For more information about giving to Columbia Nursing, visit nursing.columbia.edu/giving or contact Ashaki Charles, associate dean, Development and Alumni Relations, at 646-866-9342 or ac2759@cumc.columbia.edu.
