

COLORADO MEDICINE
ADVOCATING EXCELLENCE IN THE PROFESSION OF MEDICINE
ANSWERING THE CALL
WHY PHYSICIAN ENGAGEMENT MATTERS MORE THAN EVER IN THIS ISSUE:
• Photos from the CMS Annual Meeting in Keystone
• Navigating effects of federal policies on Colorado
• A primer on Colorado's prior auth reform law, effective Jan. 1, 2026
• And more

ANSWERING THE CALL: WHY PHYSICIAN ENGAGEMENT MATTERS MORE THAN EVER
Newly installed CMS President Brigitta Robinson, MD, FACS, shares her story of involvement in organized medicine and how it shaped her medical career. She asserts that every challenge physicians face today in health care demands physician leadership, and organized medicine is where you have a voice.

6 EDUCATION MEETS CELEBRATION: PHOTOS FROM THE 2025 CMS ANNUAL MEETING
Physicians from around the state gathered in Keystone for the 2025 CMS Annual Meeting for educational sessions, a hike in the fall colors and a prom-themed President’s Gala.



8 BENEATH THE SURFACE: NAVIGATING EFFECTS OF FEDERAL POLICY IN COLORADO
The federal HR-1 legislation and the ACA Marketplace Integrity Rule are reshaping health care in Colorado. Read what the Colorado Medical Society is doing and what physicians and practices need to do know to prepare for these challenges.
10 PRIOR AUTHORIZATION REFORM: A WIN FOR PATIENTS AND PHYSICIANS
A new Colorado law championed by the Colorado Medical Society takes effect on Jan. 1, 2026, transforming how health insurers manage prior authorization for the benefit of patients and physicians. It is critical to understand your new rights under the law.
12 LIFESAVING PROVEN MEASURES PUT INTO ACTION IN COLORADO SPRINGS
A program in Colorado Springs is saving lives by enabling trained paramedics to administer whole blood transfusions in the field.
14 CELEBRATING THE MESA COUNTY MEDICAL SOCIETY EXECUTIVE DIRECTOR’S CAREER UPON HER RETIREMENT
CMS honors Dolores Bennett for more than 30 years of service as MCMS executive director, celebrating a tenure that shaped the society's growth and success.
15 CELEBRATING MEDICINE IN COLORADO
This fall, several of Colorado’s local component medical societies hosted events to bring together the physician communities in their region.
24 FINAL WORD: COLLABORATION IS COLORADO’S STRONGEST VACCINE SAFEGUARD
In the face of radical changes to federal vaccine policy, Colorado physicians, health departments, policymakers and vaccine advocates are collaborating to ensure every Coloradan has the ability to choose vaccination.
• Advocating for health care reform with an incremental change to Medicare-eligible age
• Until the time is right for reform, remember the great Colorado charities
17 Introspections: The physician’s paradox: Why we prescribe what we don’t practice
18 Reflections: From tech to physician: Holding on to the bedside
19 Reflections: Partners in care
20 Copic Comment: Grant funding for scalable
COLORADO MEDICAL SOCIETY
OFFICERS, BOARD MEMBERS, AMA DELEGATES, and STAFF
2025-2026 OFFICERS
Brigitta Robinson, MD, FACS
President
Sean Pauzauskie, MD
President-elect
Kim Warner, MD
Immediate Past President
Hap Young, MD
Treasurer
Dean Holzkamp
Chief Executive Officer
BOARD OF DIRECTORS
Matthew Belton, MD
Brittany Carver, DO
Elizabeth Cruse, MD, MBA
Kamran Dastoury, MD
Scott Dhupar, MD
Renee Dreher, MSC
Eleanor Jensen, DO
Rachelle M. Klammer, MD
Marc Labovich, MD
Justin McCoy, DO
Michael Moore, MD
Rhonda Parker, DO
Lynn Parry, MD
Darlene Tad-y, MD, MBA
COLORADO MEDICAL SOCIETY STAFF
Dean Holzkamp
Chief Executive Officer
Dean_Holzkamp@cms.org
Kate Alfano
Director of Member Engagement
Kate_Alfano@cms.org
Jen Atchison, BHA, MSDA
Director of Continuing Medical Education and Recognized Accreditor Programs
Jen_Atchison@cms.org
Virginia "Ginny" Castleberry
Executive Director
Denver Medical Society
Virginia_Castleberry@cms.org
Cecilia Comerford-Ames
Executive Director, Colorado Society of Eye Physicians and Surgeons
Communications and Marketing Manager
Cecilia_Comerford@cms.org
Dorcia Dunn
Membership Operations Manager
Dorcia_Dunn@cms.org
Crystal Goodman
Executive Director, Northern Colorado Medical Society
Crystal_Goodman@cms.org
Blake Johnson
Member Engagement Specialist
Blake_Johnson@cms.org
AMA DELEGATION
David Downs, MD, FACP
Amy Duckro, DO, MPH
Carolynn Francavilla, MD
Mark Johnson, MD, MPH
Jan Kief, MD
Rachelle Klammer, MD
A. “Lee” Morgan, MD
Tamaan Osbourne-Roberts, MD
Lynn Parry, MD
Brigitta J. Robinson, MD
Michael Volz, MD
Patricia Weber, MD
AMA PAST PRESIDENT
Jeremy A. Lazarus, MD
Mihal Sabar
Director of Accounting
Mihal_Sabar@cms.org
Chet Seward
Chief Strategy Officer
Chet_Seward@cms.org
Debra Will Director of Business Development
Debra_Will@cms.org
Tim Yanetta
Membership and IT Manager
Tim_Yanetta@cms.org
Holzkamp,
Editor, and Kate Alfano, Managing
Answering the call: Why physician engagement matters more than ever
Brigitta Robinson, MD, FACS
From the moment I entered medical school, I discovered something that would shape my entire career: medicine is not just practiced in exam rooms and hospitals – it is shaped in board rooms, committee meetings, and legislative arenas. As a first-year medical student, I was invited to attend my first meetings of the Indiana State Medical Association and the American Medical Association. I didn’t know much about policy or advocacy, but I saw quickly that if physicians don’t show up, decisions about us – and our patients – will be made without us.

Like many who begin this journey, I started small: attending meetings, writing testimony with friends late into the night, and learning how our voices could shape the future of our profession. Those early experiences taught me two things: policy matters and physicians working together can move mountains.
Through residency, early practice, and now decades into my career in Colorado, I have stayed involved in the Colorado Medical Society and the AMA – not because it was easy, but because it was essential. I have seen firsthand how organized medicine protects patients, advances science, and defends the integrity of our profession. I have testified on issues that affect how we practice. I have watched resolutions turn into real change.
Organized
I have traveled across the country to stand with colleagues who believe, as I do, that advocacy is part of our calling.
Along the way, I was supported and inspired by mentors who opened doors for me and by peers who reminded me that collaboration is our greatest strength. I raised two children during this time, and they grew up attending many medical society meetings. They learned – as I did – that meaningful progress takes commitment, courage, and community.
As I take on the responsibility of CMS President, my journey is not just a personal milestone, it is proof of what happens when physicians stay engaged. Organized medicine gives us a voice, but only if we use it.
medicine gives us a voice, but only if we use it.
Every challenge we face today – workforce strain, administrative burden, threats to the physician-patient relationship – demands physician leadership. That means all of us. Not just the people at the microphones, not just those with titles, but every physician who believes our patients deserve better.
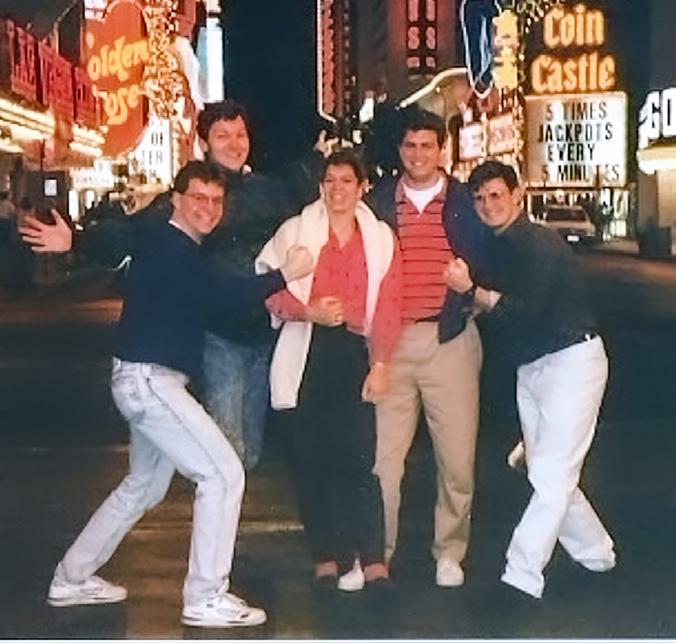
Robinson’s service to organized medicine began as a medical student through the Indiana State Medical Association and the American Medical Association. Pictured with friends from the AMA at the 1990 AMA Interim Meeting in Las Vegas.

I am thrilled to have the role of president of the CMS. I am here because a physician leader once tapped me on the shoulder and said, “Get involved – we need you.” I offer every CMS member the same invitation. Join a committee. Write a resolution. Mentor a medical student. Testify at the Capitol. Stand up for this profession and for the future of medicine in Colorado. Because when physicians show up, patients win. When we lead together, we shape the future of health care.
Our work continues – and this year the Colorado Medical Society is poised for meaningful progress. My focus as president is grounded in three priorities: practice sustainability, physician wellbeing, and greater physician engagement in organized medicine. I’m proud that the new CMS strategic plan, to be rolled out in the coming months, aligns with these pillars.
PRACTICE SUSTAINABILITY IS FUNDAMENTAL.
Across the state, I’ve watched physicians work harder for less reimbursement while malpractice costs and clinical risks stay the same. Too many colleagues are
forced to choose employment over independence or leave medicine entirely. Insurance companies talk about value yet refuse to value physicians. We didn’t choose medicine to get rich – we chose it to serve. But service must also be sustainable. When physicians cannot support their families, or even keep their doors open, patient care suffers. We must restore respect for the physician’s role and secure fair payment for the work we do.
SECOND, WE MUST PROTECT THE MENTAL HEALTH OF PHYSICIANS.
We already provide one-on-one wellbeing “consults” through the Doc2Doc program. We passed legislation last session to remove stigmatizing language from medical license applications. Our new communications strategy, Your Care is at our Core, reminds the public that physicians are human beings with purpose, families, and limits. We can do more. Burnout is a crisis. Medical students graduate under mountains of debt. Behavioral health services remain severely under-resourced and physicians are too often left alone to absorb the emotional toll. As a trauma surgeon,
Because when physicians show up, patients win. When we lead together, we shape the future of health care.
I witness tragedy daily, and I know how deeply it affects all of us. This year, I intend to advocate more strongly for mental health resources, reduce barriers to seeking help, and support psychiatrists and all physicians who care for patients in crisis.
FINALLY, WE MUST GROW AND STRENGTHEN OUR MEMBERSHIP.
Throughout my 34 years in organized medicine, one question has followed me everywhere: how do we increase engagement? The truth is, CMS already delivers value – advocacy, policy leadership, legal protections, education – but too many physicians don’t know what we do for them every day. That’s on us. We must reach physicians where they are, especially those who feel isolated, overworked, or disconnected. I know we can do it, and I believe our membership committee, led by Dr. Omar Mubarak, will open new doors for outreach and participation. But this can’t just be a committee

Robinson pictured with her children, Tristan, left, and Tatiana, right.
effort, it must be a community effort. So, I challenge each of you: bring one new member into CMS before December. If each of us does that, we don’t just grow – we transform.
And yes, let’s have fun doing it! I believe in mixing purpose with joy. If growth requires a little Fabergé Organic Shampoo-style exponential momentum – “and they’ll tell two friends, and so on, and so on” – I’m here for it!
I am honored to serve as your CMS President. Organized medicine has always been my home, and I am grateful to the people who helped me reach this moment. Thank you to the colleagues and mentors who opened doors and built this path. Thank you to the incredible CMS staff, your dedication makes our work possible. To our Colorado delegation and all of the physicians who show up year after year at AMA meetings, your advocacy inspires me. And to my parents and my children –Tristan and Tatiana – thank you for giving me the time and strength to stay involved. This has truly been a journey.
Thank you from the bottom of my heart. The future of medicine in Colorado is bright – and together, we will move forward. ■


reimagining into Central Line.
Speaker of the House.
The future of medicine in Colorado is bright –and together, we will move forward.



Robinson joined many Colorado Medical Society leaders to speak with state legislators at the Capitol advocating for Colorado health care. Pictured in 2006 with her infant son, Tristan, in tow.
The Colorado Delegation to the AMA is proud to serve homegrown wines at the PacWest Wine Reception, held annually at the AMA Annual Meeting. Pictured with Delegation Vice Chair Rachelle Klammer, MD, left, and Delegation Chair Lee Morgan, MD, center.
Left: Robinson’s involvement in organized medicine continues alongside the many peers and colleagues who started with her in medical school, residency and the Young Physicians Section. Pictured at the 2025 AMA Annual Meeting in Chicago with former YPS members and leaders. Right: Robinson was the last Vice Speaker of the Colorado House of Delegates before governance reform sparked the
Pictured with Bob Yakely, MD, who served as the final

Education meets celebration at the 2025 CMS Annual Meeting in Keystone Staff
report
As Dr. Robinson shared in her inaugural speech, “Remember that sometimes you need to have fun when you are working so you can be more productive.”
At the 2025 CMS Annual Meeting in Keystone, attendees learned and attended sessions as well as enjoyed a hike in fall colors and a prom-themed evening with dancing, Family Feud and more!
Save The Date
Save the date for next year's meeting, Sept. 18-19, 2026, to join us for fun, networking and learning! ■







1. Incoming CMS President Brigitta Robinson, MD, after her oath of office. 2. Medical students at the President's Gala. 3. Fall colors hike. 4. Humanitarian Award winner Robert Williams, MD, with Copic Medical Foundation Executive Director Meredith Hintze. 5. From left, Tamaan Osbourne-Roberts, MD, with spouse Camille, and Sarah Anderson, MD, with spouse John. 6. Outgoing CMS President Kim Warner, MD, congratulates incoming CMS President Robinson. 7. From left, President-elect Sean Pauzauskie, MD, Robinson, Warner, and Immediate Past President Omar Mubarak, MD, MBA.








Beneath the surface: Navigating effects of the current policy climate in Colorado
UNPACKING HR-1
Brigitta Robinson, MD, FACS CMS President
The federal HR-1 legislation – alongside the ACA Marketplace Integrity Rule passed earlier this year – is reshaping health care across the country. For Colorado physicians, these sweeping federal changes are already rippling through our state budget, coverage systems, and clinical practice environment. The effects will build over the next several years, and physicians must be ready to adapt and engage.
THE BIG PICTURE: A SYSTEM UNDER PRESSURE
As the saying goes, what’s above the surface is only part of the iceberg. Beneath the visible policy shifts lie deep fiscal and administrative currents that will shape Colorado’s health system for years.
Colorado is already facing a $1.2 billion budget shortfall , compounded by hundreds of millions in additional gaps tied to HR-1’s Medicaid and ACA provisions. Health care makes up nearly 40 percent of the state budget – meaning rising costs and new federal requirements will inevitably strain other priorities like education and transportation.
AMONG HR-1’S MOST IMMEDIATE IMPACTS
• Medicare will receive a temporary +2.5 percent conversion factor update , but the fix expires after one year, creating renewed uncertainty.
• Medical student loan caps could discourage future physicians, especially from underserved areas or underrepresented populations.
• Medicaid work requirements are expected to disenroll as many as 100,000 Coloradans, increasing uncompensated care and administrative costs.
• Enhanced premium tax credits (EPTCs) under the ACA are set to expire – jeopardizing coverage for up to 100,000 individuals and destabilizing the individual insurance market.
COLORADO’S COVERAGE STRATEGY AT RISK
The Health Insurance Affordability Enterprise – built on interconnected programs like reinsurance , the Colorado Option, and OMNI Salud – relies on both state fees and federal waivers. Without continued federal tax credit support, the reinsurance program’s savings drop, slashing federal pass-through funding by an estimated $100 million and threatening market stability.
Hospitals and health plans have already warned that these changes could make participation unsustainable. Simultaneously, new federal mandates will require more frequent eligibility verifications, pushing even more Coloradans off coverage.
WHAT’S COMING NEXT
By 2027, the hospital provider fee –which funds Medicaid expansion and helps reimburse uncompensated care –will begin to phase down from 6 percent to 3.5 percent, draining an estimated $10.4 billion from the system over five years. Additional state costs to administer SNAP and Medicaid could deepen fiscal pressure.
All of this adds up to a system under extraordinary strain. Physicians can expect to see more uninsured patients, delayed care, higher administrative burdens, and increased stress on clinical teams.
WHAT CMS IS DOING NOW
The Colorado Medical Society (CMS) is taking action to help physicians navigate the shifting policy landscape created by HR-1 and related federal and state changes.
• CMS’s advocacy team – supported by physician leaders and policy experts – is closely monitoring state budget developments, Medicaid policy changes, and insurance market impacts tied to HR-1. CMS continues to engage with legislators and regulators to safeguard patient access and preserve a sustainable practice environment.
• Through its communications and advocacy strategy, “Your Care is at Our Core,” CMS is collecting physician and patient stories to demonstrate the real-world consequences of policy shifts and to strengthen the physician voice in public discussions.
• Recognizing that HR-1 could drive higher uncompensated care and administrative costs, CMS is also expanding resources to help members adjust. This includes tools, peer networks, and more.
• CMS encourages physicians like you to participate directly in advocacy – responding to alerts, contributing local data, and sharing patient stories. These efforts ensure policymakers understand how proposed changes affect both physicians and the patients you serve.
In short, CMS is not waiting for the dust to settle. CMS is working now – educating, equipping, and advocating – so that when the effects of these changes reach Colorado practices, physicians are informed, supported, and ready to act.
WHAT PHYSICIANS CAN DO NOW
While the challenges are significant, Colorado physicians are not powerless. The Colorado Medical Society is working to help practices anticipate changes and advocate for solutions. Here are concrete steps physicians can take today to prepare for HR-1’s impact:
• Prepare for more uncompensated care by assessing potential increases and plan for financial resilience.
• Update your bad debt estimates to incorporate projected shifts in payer mix and coverage loss.
• Engage your finance department to review cost-sharing structures for high-impact services and clinics.
• Connect with referral sources by strengthening coordination with partners likely to see similar patient churn.
• Run a payer-mix impact analysis to identify which portions of your patient population are most vulnerable.
• Strengthen eligibility workflows by updating checklists, training staff, and maintaining up-to-date communication contacts with payers to track patients at risk for coverage loss.
• Engage with CMS, the American Medical Association (AMA), and your state specialty society. Join collective advocacy to mitigate the impact of federal and state policy shifts.
• Collecting patient stories and local data for real-world examples from your community are powerful tools for advocacy.
THE PATH FORWARD
The waters ahead may be turbulent, but Colorado physicians have weathered storms before. By staying engaged and working collectively through CMS, we can help shape how these federal shifts play out – protecting patients, preserving access, and sustaining the physician voice in Colorado’s health system.
As a trauma surgeon who works closely with emergency medicine, I am working hard to stay connected, prepare for the changes, and advocate for patients. CMS invites all members to stay connected, stay informed, and take the next right step for Colorado physicians and the patients we serve. ■ HR-1 Timeline: 2025-2026
July 4, 2025
HR-1 passes
SNAP: More work reqs for able-bodied adults without dependents (ABAWDs)
Nov. 5, 2025
Application due for CO Rural Health Transformation Fund
Dec. 31, 2025
ACA: Enhanced premium tax credits (PTCs) expire
Jan. 1, 2026
Medicare:
June 1, 2026
Medicaid: Deadline for fed guidance on work requirements
+2.5% conversion factor increase begins ACA: Lawful permanent residents no longer eligible for PTCs during 5-yr Medicaid waiting period July 1, 2026 Med student loans: Lifetime capped to $200k, ends Grad PLUS loans, changes forgiveness programs
Timeline: 2027-2032
1, 2028
Oct. 1, 2026
Medicaid: Other “qualified aliens”(eg. refugees, asylees, sex tra cking & domestic violence victims) under PRWORA no longer eligible for Medicaid.
SNAP: State’s admin cost sharing increases from 50% to 75%
Nov. 1, 2026
ACA: Annual open enrollment period shortened to Nov. 1-Dec.31
Dec. 31, 2026
Medicare:
+2.5% conversion factor increase ends, no further updates
Medicaid: Work reqs begin. Expansion pop. must renew elig every 6 mos, retroactive elig decrease from 3 to 2 mos, and 1 mos for expansion population
Nov. 7, 2028 -
Nov. 2, 2032Presidential Elections
Prior authorization reform: A win for patients and physicians
New law takes effect January 2026, reducing red tape and improving access to care in Colorado.
Cecilia Comerford, CMS Communications and Marketing Manager
When a patient’s treatment plan gets stuck waiting for insurance approval, the consequences can be serious — missed medications, delayed surgeries, and even preventable hospitalizations. Colorado physicians have long called for change. Now, that change is here.
Beginning Jan. 1, 2026, a new Colorado law — House Bill 24-1149 — will take effect, transforming how health insurers manage prior authorization, and it is critical that Colorado physicians and practices understand your rights under the law. The bipartisan measure, sponsored by Colorado Rep. Shannon Bird, [then Rep., now] Sen. Lisa Frizell, Sen. Barbara Kirkmeyer, and Sen. Dylan Roberts, was championed by the Colorado Medical Society (CMS) and its physician members. It is designed to make the process fairer, faster, and more transparent for patients and physicians alike.
“This law is about restoring common sense and fairness to health care,” said Rep. Bird.
“Too often, patients face unnecessary delays or denials for the care their doctor knows they need. By making the process more transparent and efficient, we’re making it easier for Coloradans to get timely, medically appropriate treatment.”
THE NEW STATUTE MODERNIZES PRIOR AUTHORIZATION IN SEVERAL CRITICAL WAYS, IMPROVING BOTH ACCESS AND ACCOUNTABILITY
• Extends approval durations: Prior authorizations for medical services will now last one year or the full course of treatment. For chronic medications, approvals extend to three years (one year for high-cost drugs).
• Prevents harmful denials during surgery: If an approved surgical procedure requires an additional or related covered service during the operation, insurers cannot deny coverage for that procedure when a delay would risk the patient’s health.
YOUR VOICE MATTERS
• Requires transparency: Health plans must post all prior authorization requirements, clinical criteria, and outcome data — including the number of requests, approvals, and denials — on a public-facing, searchable website.
• Creates exemptions for trusted providers: Insurers must establish alternative programs that reduce or eliminate prior authorization for physicians who consistently provide high-quality, evidence-based care.
• Streamlines electronic submissions: Carriers must comply with federal electronic standards for prior authorization requests and, by 2027, develop APIs that integrate with electronic health records so physicians can check requirements and submit requests directly.
“Physicians see firsthand the stress and harm caused when care is delayed by
Powerful interests are shaping Colorado health care policy every day. Who’s advocating for physicians and patients? WE ARE — BUT WE NEED YOU BESIDE US.
COMPAC (Colorado Medical Political Action Committee) and the CMS Small Donor Committee are the only political funds in Colorado dedicated solely to advancing physician-led advocacy at the state Capitol. These issues are being decided right now. Laws get written by those who show up—and those who are heard. PAC support is how physicians stay in the room.
Together, we elect pro-physician, pro-patient candidates who stand up for:
• Fair physician reimbursement
• Reducing administrative burden
• Physician-led care and scope of practice integrity
• A strong, stable medical liability climate
• Policies that support access to care and improve patient outcomes
TWO WAYS TO STRENGTHEN PHYSICIAN ADVOCACY:
Give to COMPAC Fuel a strong, unified physician voice in state elections and partner with AMPAC at the federal level.
Join the CMS Small Donor Committee
Multiply your impact—small contributions from many physicians create powerful influence in Colorado’s most competitive races.

This is not about politics — it’s about protecting your profession and your patients. Make your contribution when you return your membership invoice or give online: www.cms.org/contributeadvocacy
Every contribution matters. Every voice counts. Stand with us.
Questions? Contact membership@cms.org
Faster Approvals
1-year and 3-year terms

red tape,” said Brigitta Robinson, MD, FACS, President of the Colorado Medical Society. “This law will allow patients start treatment sooner, continue medications without disruption, and spend less time waiting for insurance approval. It’s a win for both patients and providers.”
IMPACT ON SURGICAL CARE
Under the new law, surgeons gain a crucial safeguard: when a medically necessary related procedure is discovered during an approved surgery, insurers can no longer deny coverage because the additional service wasn’t separately pre-approved. This protection ensures that care decisions remain in the hands of physicians and allows them to act in the patient’s best interest — especially in cases where a delay could lead to harm. Practices should ensure documentation of intraoperative findings and timely post-procedure notification to carriers.
IMPACT ON MEDICAL AND PRESCRIPTION CARE
For physicians managing chronic illness and complex treatment plans, the law brings long-overdue relief. Longer approval durations mean less time spent resubmitting identical requests. Carriers
Surgical Care
must also review their prior authorization lists annually and remove requirements that fail to improve quality, equity, or cost savings. For patients managing long-term conditions, the change is significant. Prior authorizations for chronic medications will now be valid for three years, providing stability and reducing treatment interruptions — a change that directly addresses widespread patient frustration and harm.
GREATER ACCOUNTABILITY AND EQUITY

electronic health record systems can support automated prior authorization once APIs become available, and watching for carrier communications on provider exemption programs to ensure eligibility documentation is accurate. CMS will provide additional guidance, templates, and educational materials to help physicians and administrators implement these changes smoothly.
The legislation also tackles inequities in access to care. Studies have shown that prior authorization delays disproportionately affect historically marginalized communities, including patients of color and those with disabilities or lower incomes. By mandating public reporting and requiring insurers to justify and remove unnecessary barriers, HB24-1149 aims to create a more transparent and equitable health system.
WHAT PRACTICES SHOULD DO NOW
While the law takes effect in January 2026, practices can begin preparing by reviewing internal workflows to track one-year and three-year approval periods, identifying chronic medications most affected by the new timelines, confirming
For years, prior authorization has symbolized one of the most frustrating administrative burdens in health care. Colorado’s reform represents a meaningful step toward a better balance — maintaining accountability in coverage decisions while prioritizing patients’ access to timely, medically necessary care.
“I’m proud to support this law because it puts patients first,” said Sen. Kirkmeyer. “By streamlining the approval process and reducing unnecessary hurdles, we are ensuring that Coloradans receive the care their doctors recommend – without delay or confusion.”
The law takes effect Jan. 1, 2026. ■

Lifesaving proven measures put into action in Colorado Springs
Matthew Angelidis, MD
The Whole Blood Program is a groundbreaking initiative in Colorado Springs that enables specially trained paramedics to administer lifesaving whole blood transfusions in the field – before a patient reaches the hospital. Designed for patients over the age of two experiencing significant blood loss due to trauma, internal bleeding, or conditions like obstetric or gastrointestinal hemorrhage, this program helps treat hemorrhagic shock at its earliest and most critical stage. Following state EMS Chapter Waiver Guidelines, the program ensures whole blood is safely administered to patients of all ages and blood types, including children and pregnant women.
The No. 1 cause of death under the age of 46 and the No. 1 cause of preventable death in the United States is hemorrhagic shock (bleeding to death). Forty percent of patients bleed to death in the care of first responders (firefighters or paramedics)
When first responders are empowered to save lives... they save lives.

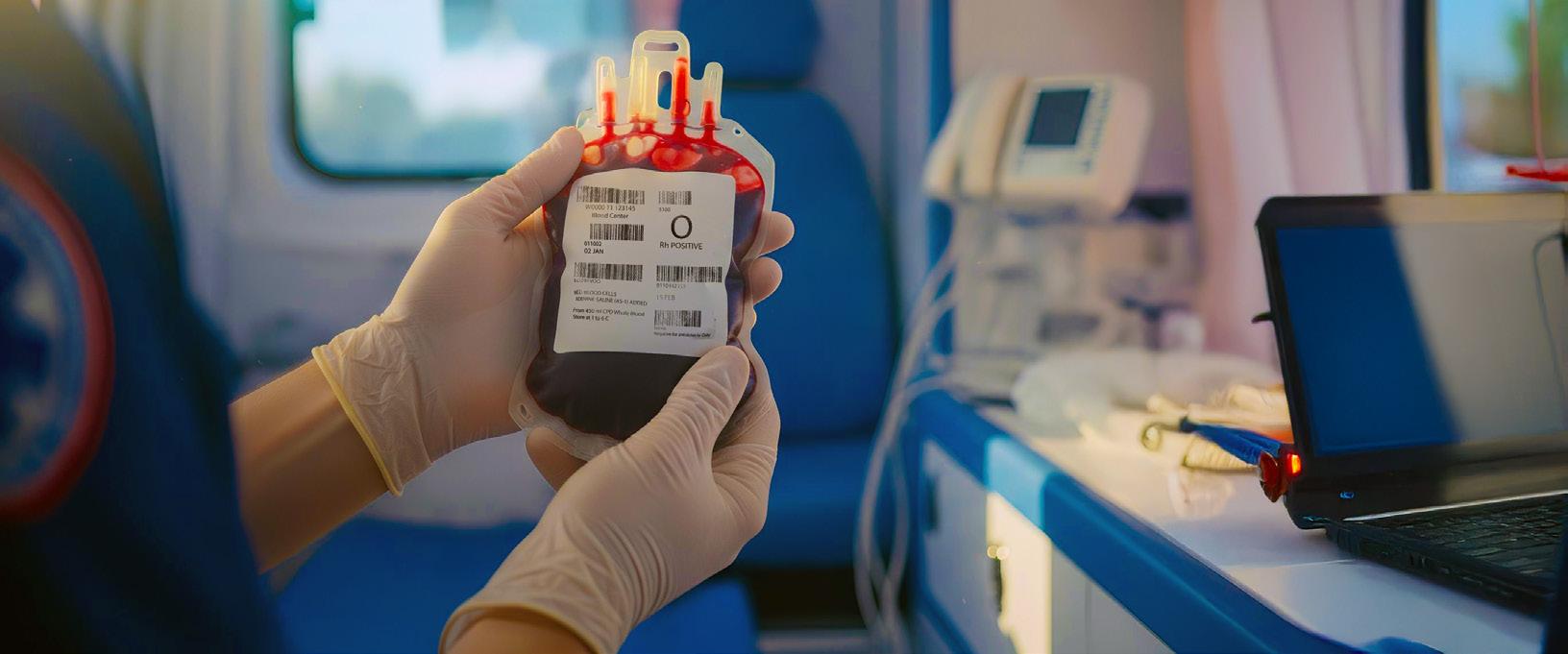
before they can make it to the hospital. In these cases, a blood transfusion is the resuscitation treatment of choice and has been proven to save lives. When first responders are empowered to save lives by storing, transporting, and transfusing low-titer O(+) whole blood to bleeding patients before they die and before they arrive at our hospitals, they save lives.
In the first year of the Colorado Springs Fire Department’s program, our city’s EMS professionals have transfused over 150 units of blood to 100 survivors. One Colorado resident is saved every 72 hours, who would have died without the lifesaving blood transfusion.
Trauma and hemorrhagic shock do not discriminate based on age, sex, gender, or income. If you or your family live, work, or play in Colorado Springs, you are a poten -
tial benefactor of this program. Someone you know or love is going to need a blood transfusion to survive, and you can help ensure they get that transfusion when they need it. While less than 2 percent of EMS teams in the America currently provide blood transfusions to their communities, you can help Colorado Springs Fire Department, Ute Pass Regional Health Services District, and the Memorial Health Foundation sustain our EMS Blood Transfusion Program and ensure our friends and families have access to cutting-edge care.
This is an incredible lifesaving measure; however, EMS blood transfusions are not reimbursed by health insurance companies, so hospitals and EMS agencies are forced to bear the cost of these treatments at a huge loss. One unit of blood costs approximately $700. Additionally, EMS teams that wish to store, transport, and transfuse blood need specialized equipment and specialized training to safely and effectively transfuse blood to patients outside of a hospital.
Billing On the Coast, LLC started in Florida in 2021 with over 20 years’ experience.
We specialize in providing education for billers and/or providers, medical coding & billing, external auditing, consulting and credentialing.
Our team is dedicated to ensuring accurate and timely billing services for healthcare providers. We understand the unique challenges of medical billing and strive to make the process seamless for our clients. Our commitment to excellence and attention to detail set us apart from our competitors. Let us handle your medical billing needs so that you can focus on providing exceptional patient care.
Owner Operator
If you are in El Paso, Teller or Pueblo counties and feel compelled to contribute to this great work, visit this link – uchealthmemorialcares.org/wholeblood – or scan the QR code to donate to the Memorial Health Foundation, our EMS Communities principal partner in funding this innovative cutting-edge lifesaving treatment.
Outside of our area, consider learning if there is a whole blood program in your community and if not, connect with us to learn more. ■
Matthew Angelidis, MD, is the current medical director for UCHealth EMS, co-chief medical director for Colorado Springs Fire Department, co-chief medical director for El Paso County AMR, co-chief medical director for Plains to Peaks RETAC, and clinical assistant professor for UC School of Medicine


A legacy of leadership and heart: Celebrating Dolores Bennett’s remarkable career serving Mesa County physicians
Staff report
When the Mesa County Medical Society gathered to celebrate Dolores Bennett’s remarkable career in Palisade on Aug. 5, 2025, the plaque presented to her captured the sentiment felt by all: “With appreciation and respect for over 30 years of outstanding service, commitment, and dedication to the physicians of Mesa County.”
For more than three decades, Dolores has been the steady heart of the MCMS – a source of knowledge, continuity, and compassion for the physicians she served. Beyond her professionalism, she became a trusted friend to many, sharing in their milestones and offering support through challenges. “Dolores Bennet’s excellent people skills coaxed many fine speakers and arranged great events for
Mesa County Medical Society, a major factor in our County Medical Society’s cohesion,” said Bronwen Magraw, MD, a Mesa County leader.
Dolores was a proud supporter of the work of the former MCMS Alliance, which was active for many years and made a lasting impact through its volunteer initiatives. The group championed causes ranging from domestic violence awareness and vaccine promotion to bringing health education into local classrooms – reaching families and helping shape a healthier future for the region.
Enno Heuscher, MD, shared, “Dolores dedicated a great part of her life to her work as executive of MCMS, and she deserves great credit in keeping physi -

cian participation one of the highest in Colorado. She also helped the physician Alliance in our county survive longer than any other Alliance. As former president of MCMS, I had her full support during my tenure, making my role easier. She also provided superb support in my recent role as Colorado Medical Society board member. Her people skills and physician support were unparalleled in her field, and she will be sorely missed.”
As Dolores enjoys retirement, the Mesa County Medical Society extends its deepest gratitude for her years of exceptional service, her unwavering dedication, and the kindness and care she brought to every part of her work. Her legacy will continue to inspire all who had the privilege of working alongside her. ■
“In 2005, I first met Dolores when I began my career at the Medical Society. During my very first week, I was invited to attend the spring meeting up in Vail. It seemed like an adventurous start, not knowing a soul. However, Dolores immediately came over to me, greeted me warmly, and invited me to sit beside her. Dolores was very kind but unmistakably in charge. I initially wasn’t sure if she was truly this kind or just feeling the need to keep her eye on the new girl, but either way, I felt immediately at ease. Over the next two decades, I experienced Dolores’ hands-on approach with her physicians. She was truly their friend, and I loved seeing how she interacted with them. Her attention to detail was always so admirable. Mesa County Medical Society has always been in such great hands with Dolores. We will miss her terribly as our colleague as she begins her well-deserved retirement; however, Dolores will continue to be our cherished friend.
Andrea Chase
Arapahoe-Douglas-Elbert Medical Society Executive Director, reflecting on her decades of work as a peer of Dolores Bennett
Below: Dolores Bennett, right, pictured at the Mesa County Medical Society Evening at the Winery on Aug. 5, 2025, with incoming MCMS Executive Director Amey Collazo.
Celebrating medicine in Colorado
Staff report
This fall, several of Colorado’s local medical societies hosted events across the state – each one celebrating community and connection in its own unique way.
From annual meeting concerts to interactive cooking demonstrations to the inaugural Doctors and Dogs fashion show, these events brought physicians together for engaging discussions and philanthropy, reflecting the diversity and vitality of Colorado's physician community.
Participating societies include the Boul der County Medical Society, El Paso County Medical Society, Denver Medical Society, Foothills Medical Society, Auro ra-Adams Medical Society, and Arap ahoe-Douglas-Elbert Medical Society. Their programs continue to showcase the many ways physicians come together to learn, collaborate, and strengthen the profession statewide. ■















Letters to the editor
Clifford Watts, MD

One of the least disruptive and simpler solutions is to lower the eligibility age for Medicare by two years every year for 10 years. That would cover the citizens who are 45 years old and older and who consume the majority of medical care. A gradual but effective transition. The next step would be to open Medicare for All, which could eliminate the multiple programs we now fund as taxpayers. Not the faster way but maybe a way to start what is needed.
Sincerely and with thanks for your efforts, Clifford Watts, MD
Joel C. Boulder, MD
In the Summer 2025 issue of Colorado Medicine, Dr. Cagan and his colleagues advocated for universal health care coverage for everyone in Colorado, health care justice and equality. They described it as an urgent need.
This would require an “industrial lift” and one that is very expensive and time-consuming. Their first step would be yet another feasibility study followed by more legislative debate to craft the bill and ultimately a vote of the people to approve the necessary tax increase for the program.
Keep in mind that Amendment 69, which called for similar objectives, was voted down 80 percent to 20 percent in 2016. Our state budget deficit is estimated to
Helping medical professionals solve their mortgage puzzle


be between $7.5 million and $1.2 billion, and Medicaid is the largest line item. As a result, the 1.8 percent Medicaid provider pay increase was cut. It is my understanding that Medicaid accounts for only 20 percent of the patient population, and we can barely afford it now. Suffice it to say that the tax increase necessary to cover everyone would be substantial.
An urgent need should warrant a prompt response. Although there are a multitude of problems with our current system, there are things that we can do right now to improve the situation for many patients. Worthwhile charities are often forgotten.
Doctors Care is just one of the excellent nonprofit organizations in Colorado. We were originally formed in 1988 to serve the working poor and those without insurance. Today we serve thousands of Medicaid, CHP+, and uninsured patients. Please consider supporting these organizations, encouraging others to do so as well. If you are an employed physician, encourage your employer or associate to see at least a small percentage of indigent patients on a sliding scale.
We can’t make everything right, but we can make things better for many in our community, without another study, election or Socialist Revolution.
Thank you,
Joel C. Boulder, MD
Dr. Boulder has been affiliated with Doctors Care since 1988 and previously served as its Volunteer Medical Director. The opinions expressed are his own. ■

The physician’s paradox: Why we prescribe what we don’t practice
Breea Diamond

Breea Diamond is a mountain enthusiast and Colorado native. She attended Colorado State University for her B.S in Biology and the University of Colorado Anschutz for her M.S in Biomedical Science and Biotechnology. She is currently a second-year student at Rocky Vista University in the Digital Health Track. She serves as the president of the Student Osteopathic Medical Association (SOMA) chapter. Additionally, she is a student representative for Denver Osteopathic Foundation (DOF) and Colorado Society of Osteopathic Medicine (CSOM).
Second-year medical students transition from understanding anatomy and physiology to applying it to patient cases. We begin to recognize symptom patterns and integrate diagnostic tools to build a plan for improving patients’ quality of life. In my own life, however, I was blind to the patterns of physical and mental burnout. The reality of medical training – the punishing hours, the emotional weight of patient care – had slowly chipped away at my wellbeing. I was chronically stressed, constantly ill, and desperately close to physical exhaustion. Here I was spending all day learning about how to improve physical health and neglecting my own.
I wasn’t alone. My own father, a psychiatrist, was living perpetually within this paradox. He recently lost his mobility and became wheelchair bound. In his time of transition and trauma, he refused to see a psychiatrist for support. His reasoning was simple and unsettling: he was a psychiatrist himself, and he knew the DSM manual front to back. To him, the idea of seeking help was a professional failure, not a human necessity.
This false idea of professionalism was paralleled by my mother-in-law. She has been a family medicine doctor for over 20 years and has a full schedule of patients. She treats a patient panel riddled with metabolic disorders, like autoimmune disease and diabetes, to whom she preaches the importance of lifestyle modifications. Yet, she sleeps less than three hours a night despite knowing the
evidence that sleep deprivation aggressively worsens metabolic health. She sees her exhaustion and her H1aC levels rising as a badge of honor, a necessary sacrifice for her patients.
These were the models I inherited – one where professional knowledge was a shield against personal need and another where self-care was a betrayal of professional duty. I kept finding myself asking a core question: What is it about the culture of medicine that makes us less likely to seek care or integrate the very lifestyle medicine we champion?
The answer arrived, not in a lecture hall, but during Savasana. After crash landing into second year and getting poor marks and even poorer health outcomes, I decided to try a yoga class. It was only 10 minutes away from my apartment, and I held out hope the movements might address the physical toll the stress was taking. I felt out of place at first; I was convinced twelve o’clock yoga should be reserved for stay-at-home moms and retirees. One day, my yoga instructor abruptly took an urgent call. She apologized and said: “I have to take this patient call; I’ll be right back.” After class, I asked her about her patients. She explained that yoga was her passion, but she was, in fact, a genetic counselor specializing in oncology.
I asked her why she chose to become a yoga instructor if she had such a demanding medical career. She revealed
a hard truth: she discovered yoga not as a recreational pursuit, but as a form of medicine recommended by her osteopathic physician. Her demanding work hours as a counselor had driven her to a state of complete physical and emotional depletion, which coincided with a cancer diagnosis in her late 30s.
What resonated with me was her raw vulnerability. She was not a model of flawless professional endurance; she was a testament to the fact that the system sometimes breaks the people meant to fix others. Her story was the ultimate counter-narrative to the stoicism I had witnessed. Her practice was not about achieving a perfect pose; it was about surviving, and then, thriving. It was about reconnecting with herself when her professional life had disconnected her from her most fundamental human needs.
I’m learning that my medical knowledge isn’t just a tool for treating patients. I now recognize that the same compassion I’m training to extend to others must first be extended to myself. My yoga instructor’s impact has led me to a crucial realization. My own wellbeing is not a personal luxury; it is a professional imperative. Her example has redefined success for me: not as enduring endless exhaustion, but as practicing deliberate, sustainable compassion. I now recognize that being an effective physician means showing up for my patients whole, and this begins with showing up for myself – one breath, one moment, at a time. ■

From tech to physician: Holding on to the bedside
Morgan McCord


Morgan McCord is a fourth-year medical student at the University of Colorado School of Medicine. Originally from Indianapolis, she earned her degree in biochemistry at DePauw University in Greencastle, Ind. Before medical school, she worked in several clinical roles, spending countless hours at the patient bedside. Morgan moved to Colorado in 2020 with her now-fiancé, Charlie, where they share a love for hiking 14ers and skiing every free weekend in the winter. She plans to specialize in anesthesiology and critical care, drawn to the privilege of supporting patients and families through some of medicine’s most vulnerable moments.
ROSE
Before medical school, I worked nights as a certified nursing assistant, or “tech,” on a medical-surgical floor for two years. Rose was my charge nurse, a steady presence who had worked at the hospital for over 15 years. Her superpowers were patience and composure.
She had patience for everyone. For me, a new and nervous tech who had never been at a patient’s bedside, Rose walked the halls with me at 3 a.m., showing me how to gently wake patients to draw their morning labs. For new nurses, she quietly pulled them aside after difficult moments – like guiding one through her first decompensating patient with an active GI bleed. For new interns, she offered gentle reminders to “double check” an order before giving an incorrect medication dose. And most important, she had patience for her patients. Rose taught me that while it might be just another shift for me, it could be the worst night of someone’s life – whether because of post-operative pain, unrelenting nausea, or the realization they’d spend Christmas in the hospital.
Her composure in the face of chaos was just as remarkable. Even on short-staffed nights, when a rapid response was called while two new admissions arrived at once, she maintained the same calm, steady demeanor. Her composure grounded the entire team.
My time with Rose will always be with me – from our hushed (and sometimes not-sohushed) 4 a.m. giggles at the charge desk to the lessons she modeled through her patience and grace. I hope to carry her superpowers with me one day as the physician I aspire to be.
ARIEL
Ariel worked nights with me as a tech while finishing her nursing degree. Before long, we were comparing schedules to make sure we worked every shift together. Ariel’s superpowers were looking out for others and always knowing exactly what a patient needed.
The role of a tech could be overwhelming. We were assigned six to eight patients, and chaos was always just a few call lights away – two patients needing assistance to the restroom, another asking to have dinner warmed up, one wanting to go for a walk, and another vomiting down the hall – all while realizing you’re 30 minutes behind on vital signs. But having Ariel there made all the difference. She defined teamwork in the hospital. She never walked past a call light just because the patient wasn’t in her assignment. Sometimes we’d gather all our supplies to draw morning labs and visit each room together, finding small efficiencies that made the night easier (and a little more fun). She looked out for everyone – other techs, the nursing staff, and even me.
What amazed me was her ability to meet patients exactly where they were, even when each patient needed something different. Ariel intuitively knew what would help – a laugh, a listening ear, or a graham cracker with peanut butter (the most elite hospital snack). And she didn’t care just for patients, she cared for her co-workers. She’d answer my patient’s call light if she saw me trying to squeeze in an MCAT practice question at 2 a.m. Once when I was upset after a patient raised their voice with me, she comforted me in the hallway, and then, with grace and professionalism, went to speak kindly with the patient.
My hundreds of hours spent working alongside Ariel taught me such valuable lessons about teamwork, friendship, and empathy. I know I’ll carry what I learned from Ariel through every step of my medical career. And I’m confident she is now a practicing nurse looking out for her people and teaching others what she taught me.
REFLECTION
What began as a second job to make ends meet became one of the most formative experiences of my career. Working alongside Rose, Ariel, and countless others taught me more than I ever expected. Spending hours at the bedside revealed the humanism braided through medicine – and how much small acts of care can mean. Washing a patient’s hair at 2 a.m. because they needed a moment of comfort and normalcy. Sitting with an altered, combative patient reaching for his new tracheostomy for 12 hours straight. Finding a window view for a patient who loved fireworks on New Year’s Eve.
The transition from clinical staff to medical student – and soon, physician – has been a complex one. I’ve often felt a stronger connection with nurses, techs, and other hospital staff than with my medical school peers. I think of Michael, an environmental services employee who helped me choose my specialty, and of Nat, an anesthesia tech who shared stories of balancing single-parenting while pursuing her education. My years as a tech taught me lessons no textbook could: patience, composure, and the value of teamwork. As I move forward in medicine, I hope to hold tight to the perspective I gained at the bedside. ■
Partners in care
Ellie Golding


Ellie Golding is a fourth-year medical student at the University of Colorado School of Medicine. She is a Colorado native, and enjoys skiing, hiking, and practicing yoga in her free time. Ellie is an aspiring OBGYN and plans to incorporate addiction medicine into her practice.
Medicine cannot heal in a vacuum; it requires connection.
Dr. Rana Awdish, author of In Shock
In medical school we learn not only about genetics, biology, and pharmacology, but also about social determinants of health, patient-centered care, and recognizing and addressing our biases. When I got to the clinical portion of my education, these lessons I had heard in lectures and small groups came to life through harm reduction. Harm reduction is a principle of public health that aims to decrease the negative consequences associated with human behaviors and is often employed in the context of substance use.
I remember a patient admitted to the hospital with her third case of pneumonia within a year. She was unhoused and used IV drugs, and her pneumonia was thought to be from aspiration. She quickly weaned from oxygen and was
medically stable but begged to be able to stay inside one night longer. In preparing for her discharge, I was distressed by not being able to do more for her. I looked for other ways we could help prevent this from happening again, and I suggested we prescribe Narcan and a pneumococcal vaccine. While I couldn’t at that moment provide her the safe housing she deserved, I could honor her story and experiences and provide patient-centered care and an opportunity for risk mitigation. I could also carry her experience forward and look for opportunities for advocacy. At its core, though, the principle of harm reduction honors patient autonomy and lived experience. It helps us become partners in care, rather than arbitrary deciders of right and wrong.
To me, being a doctor is about meeting people where they are (both physically and situationally) and honoring patients’ stories, autonomy, and life circumstances in each encounter. It is about learning not just about diseases and how to treat them, but about people’s lived experiences and how to deploy our medical knowledge to advocate for patient-centered care. As Dr. Awdish so beautifully wrote, Medicine cannot heal in a vacuum; it requires connection. Naloxone, Suboxone, vaccines, and other treatments cannot alone save lives – they require non-judgement, trusting relationships, and empathetic encounters with patients. ■
Reflective writing is an important component of the University of Colorado School of Medicine curriculum. Beginning in the first semester, medical students write essays, stories or poetry that reflect what they have seen, heard and felt. The Reflections column was co-founded by Steven Lowenstein, MD, MPH, and Tess Jones, PhD. It is now co-edited by Dr. Lowenstein and Kathryn Rhine, PhD. It is dedicated to the memory of Henry Claman, MD, Distinguished Immunologist and Professor at the University of Colorado, and founder of the Arts and Humanities in Healthcare Program.
Grant funding: Scalable solutions for fragmentation in health care
Gerald Zarlengo, MD, Chairman & CEO Copic Insurance Company

Grant funding through the Copic Medical Foundation is an essential part of how we invest in the health care community and support people and ideas that are making a difference. Our 2026 funding cycle opens this November, and we’re looking for scalable solutions to fight fragmentation.
Making health care delivery more connected is key to giving patients better care and improving outcomes. When things are fragmented – like when providers aren’t on the same page – it can lead to confusion, higher costs and frustration for everyone involved. And most importantly, it can negatively impact patients.
By working to reduce fragmentation, health care organizations can create a smoother, more effective system. But it’s not always easy. Real-world challenges like poor communication between providers, disjointed services, and patients feeling lost in their own care journey all play a role. On top of that, limited resources and complex regulations can make coordination even tougher.
When organizations find ways to share patient information and close the loop on care, everyone benefits. It helps ensure that all providers are informed and aligned, which leads to better decisions and better care. Ultimately, it’s about building a health care system that puts patients first and makes the most of the resources we have.

Making health care delivery more connected is key to giving patients better care and improving outcomes.
GRANT FUNDING APPLICATON PROCESS
What we fund:
• Programs and initiatives that improve patient safety and quality of care through systems changes and improvements
• Pilot programs designed to reduce medical errors
• Development and implementation of tools to improve care delivery
Minimum criteria to be considered:
• Approach or program demonstrates potential for uptake or replication by the health care community
• Organization is designated as a 501(c) (3) organization or has an identified fiduciary
• We prioritize projects that exemplify sustainability, feasibility, replicability and scalability
Deadlines and applications – Grant applications are due Jan. 16, 2026 by 5 p.m. (Mountain Time). Visit our website at www.copicfoundation.org to review
requirements and submit an application. If you have any questions, please email mhintze@copic.com . Applicants can expect to hear from us regarding potential support in March 2026.
GRANTEE UPDATE
Advancing Safer Care: MSU Denver EMT/Nursing IPE Grant Impact
Copic Medical Foundation’s grant to Metropolitan State University (MSU) Denver in 2023 has sparked lasting change in how future clinicians approach patient safety and teamwork. This initiative directly addresses the challenges of patient handoff and care fragmentation – issues that impact safety, outcomes, and the daily work of clinicians across settings.
Through high-fidelity simulation scenarios, dozens of nursing and EMT students have participated in immersive training focused on the critical transition from prehospital to in-hospital care. Based on data from the initial cohort, the results were striking: 95 percent of students said, “Because of this experience I plan to adjust my approach to improve handoff communication,” and 97 percent agreed that “team-based skills are essential for all health care students to learn.” Approximately 96 percent of students agreed
or strongly agreed that “Debriefing enhanced my learning.” Underscoring the program’s impact on real-world practice, students noted, “I have a better understanding of respectful and effective handoff communication.”
Faculty and facilitators also saw the value. As noted in the report, “Educating the facilitators on current best practices was just as beneficial as educating the students. Facilitators noted the overwhelming success of the grant and the need for more interprofessional education (IPE) events.” The collaboration between MSU Denver and Denver Health has grown stronger, with plans to expand IPE across health programs and address workforce shortages in EMS and nursing. As MSU Denver anticipates a 25 percent increase in nursing students by 2026,
2023
Grant awarded to MSU Denver

and Denver Health EMS education grows, the grant’s impact will continue to shape the region’s health care landscape.
This project aligns with Copic’s commitment to advancing patient safety and supporting clinicians. By fostering a culture of communication, teamwork, and continuous learning, the grant helps ensure that the next generation of health care professionals is prepared to deliver safer, more coordinated care. The Copic Medical Foundation’s support stands as a testament to the power of partnership and innovation in driving positive change for insureds, partners, and the communities they serve.
2026
25% expected increase in nursing students and growth in EMS education
2024–2025
Program expansion and collaboration with Denver Health
May 2026 5th Annual Grantee Summit
Medical Transcription Services
Busy vs. Kinda Sorta Maybe Busy
2026 GRANTEE SUMMIT
In May 2026, the Copic Medical Foundation will convene its fifth annual Grantee Summit, welcoming both past and present grantees alongside valued community partners. This gathering is designed to foster meaningful connections, spark the exchange of insights, and inspire collaborative solutions – all centered on our shared commitment to “reducing fragmentation across care settings.”
We see the Grantee Summit as a cornerstone of our mission to advance health care quality, minimize adverse outcomes, and champion innovation. Our aspiration is for every participant to leave energized – with fresh ideas, new collaborators, and broadened perspectives – empowered to amplify their impact and drive patient safety improvements on a larger scale.
Eligible Colorado Medical Society (CMS) members can receive up to a 10 percent premium discount on Copic policies. Get more information on CMS membership by contacting membership@cms.org. ■
Few can contest physicians and healthcare providers when they say they’re busy. They truly are. They barely have seconds to scarf down vending machine chips for lunch, let alone transcribe their patients’ medical charts. By bringing Ditto Transcripts on board, time’s back on your side to juggle more administrative tasks and care for patients—the work that matters most to you. The way it should be.
For the medical field, Ditto Transcripts delivers:
• Experienced, U.S.-based medical transcriptionists skilled in EHR and EMR systems
• 99% accuracy for all transcription—guaranteed
• Access to speech recognition software editors
• Rapid turnaround and on time for fast access to medical records and reports 24/7
• Electronic file delivery in 24 hours or less
• Speech recognition software editing
• Secure, private, confidential and HIPAA compliant
• Adhere to AHDI/AAMT standards
• Unlimited customer support services
• No long-term contract required
• E-signature/digital signature available
When we say specific, we mean specific. We have deep medical transcription service expertise for cardiology, clinical, dermatology, emergency medicine, hematology/oncology, mental health, neurology, ophthalmology, orthopedic, pathology, podiatry, psychiatry, radiology, urology, among others.
Free Trial
Take us for a test drive. Enjoy 1,000 lines or 60 minutes free. No credit card needed—this trial’s on us. For pricing models and to learn more about our Free Trial, visit us at dittotranscripts.com







Your time back: How AI in your EHR benefits independent practices
For many independent medical providers across Colorado, the day rarely ends when the last patient leaves. Hours are often spent catching up on documentation — a task that eats into personal time and contributes to burnout. Research shows that 89 percent of providers regularly spend over 30 minutes after hours just on charting. This administrative burden is a significant pain point, but technology is making it easier than ever to reduce it.
AI-powered documentation tools built into your Electronic Health Record (EHR) system help independent practices save hours each week. These tools address one of the biggest time drains in your day, allowing you to focus more on patient care and less on administrative work.
RECLAIM YOUR EVENINGS BY REDUCING CHARTING TIME
Repetitive charting is a major source of frustration. Nearly half of all providers spend over a quarter of their workday on documentation alone. This is time that could be better spent building patient relationships or simply recharging. AI-powered note-taking offers a direct path to greater efficiency.
Imagine finishing a patient visit and having a structured, accurate clinical note already generated. AI tools can capture and transcribe your encounters in real time, automatically creating structured SOAP notes. This significantly cuts down on manual data entry and editing. In fact, 48 percent of providers report that AI has already helped them reduce after-hours charting. For independent providers, this reclaimed time is invaluable, supporting better work-life balance and lowering the risk of burnout.
ENHANCE CLINICAL ACCURACY AND PATIENT SAFETY
Beyond saving time, AI-powered documentation also improves the quality of care you deliver. By automating note transcription and organization, these tools help reduce the potential for human error. An integrated EHR with AI capabilities keeps all patient information — history, notes, and data — consolidated in one place.
This single source of truth gives you a complete view of each patient, supporting more confident clinical decision-making. Some advanced systems, like Tebra’s AI Note Assist, can even suggest relevant ICD-10 codes based on your documentation, helping streamline the billing process and improve coding accuracy. This not only promotes patient safety but also ensures your practice is appropriately reimbursed for the care you provide.
A MODERN EHR PUTS THE FOCUS BACK ON PATIENTS
The right EHR should do more than store patient records; it should actively support your workflow. For independent practices, that means simplifying everyday tasks like scheduling, billing, prescribing, and communicating with patients.
When your EHR includes AI-powered tools, you can shift your focus from the computer screen back to the patient in front of you. Ambient AI charting — technology that captures conversations in real time — lets you have natural interactions while ensuring every important detail is recorded accurately. This enhances the patient experience

of providers spend 30+ minutes after hours charting of providers say AI reduced
and strengthens the provider-patient relationship.
Solutions built for private practices, such as Tebra AI Note Assist, automate documentation directly within your existing EHR workflow. They keep you in control while handling the most time-consuming parts of note creation, freeing you up to focus on what matters most: caring for your patients. A smarter EHR doesn’t just improve your documentation — it gives you back your time and helps you build a more efficient, patient-focused practice.
Tebra is proud to be a preferred partner of the Colorado Medical Society, dedicated to empowering independent practices across the state. As a trusted partner of the Colorado Medical Society, Tebra is pleased to offer CMS members an exclusive 10% discount off individual module subscriptions.
Learn more at www.tebra.com ■


PROGRAM HIGHLIGHTS



Collaboration is Colorado’s strongest vaccine safeguard
David Higgins, MD, MPH, FAAP
This year, radical changes to federal vaccine policy and recommendations have fragmented and destabilized the U.S. vaccination ecosystem that has safeguarded generations from life-threatening vaccine-preventable diseases. These changes include the dismantling of the CDC’s Advisory Committee on Immunization Practices, the removal of independent scientific advisors, and the bypassing of long-standing vaccine review and approval processes.
The consequences are visible in exam rooms. Parents and patients are asking whether vaccines are still recommended, covered, or even safe, and clinicians are trying to reconcile conflicting messages. Outside clinics, communities are facing reduced access, and politics, misinformation, and uncertainty are eroding confidence.
Fortunately, Colorado is not standing still in the face of this uncertainty. Physicians, health departments, policymakers, and vaccine advocates are collaborating statewide to protect evidence-based guidance and ensure every Coloradan has the ability to choose vaccination.
Professional societies and community organizations, such as the American Academy of Pediatrics, Immunize Colorado and the Colorado Medical Society, among many others, have long championed vaccines in Colorado and continue to collaborate and coordinate their responses. These groups are building on their past successes and partnering with new initiatives such as the Colorado Chooses Vaccines alliance and regional coalition efforts to sustain a unified, evidence-based approach to vaccination in Colorado.
Colorado lawmakers are also taking decisive action. In June, two landmark bills were signed into law (SB25-196 and HB25-1027) that aim to preserve access to vaccines in the face of federal rollbacks and keep state regulations in line with best practices. Additionally, state leaders recently took steps to ensure the contin -
ued availability of COVID-19 vaccines by authorizing pharmacists to administer them without a prescription. These examples demonstrate the initiative and responsiveness of Colorado’s leaders in countering federal actions that weaken vaccine availability.
However, there is much more work ahead, and no single organization, agency, or profession can do it alone. The disruption of federal vaccine policy leaves gaps in vaccine financing, supply, administration, and communication that span often siloed professionals and communities. The model where professional associations, health organizations, and community coalitions share responsibility for filling gaps in federal guidance is challenging, but community health is a shared responsibility.
Sustaining vaccine access and confidence in the months ahead will require a coordinated effort on several fronts, including protecting access, maintaining confidence, and ensuring vaccines reach every community.
To protect access, Colorado must continue strengthening its vaccine financing systems, ensuring predictable reimbursement and stable supply chains. The Vaccines for Children Program (VFC), which covers nearly half of Colorado’s children, must remain fully supported and insulated from federal uncertainty, as disruptions would immediately cause access gaps. Physicians and health systems also require clarity on the legal framework governing vaccine administration, coverage, and liability to confidently stock and administer vaccines.

Protecting community health is not the work of one profession or organization; it is the shared calling of physicians, nurses, pharmacists, public health officials, educators, and community leaders.
Maintaining confidence requires clear, consistent, and credible communication from national and state vaccination leaders all the way down to the front lines of care. Colorado’s public health and professional leaders must fill the federal void with unified, science-based information that both clinicians and families can trust. This means coordinated public communication and transparent decision-making. Colorado must invest in its communication infrastructure to quickly adapt and deliver accurate information in real-time.
Finally, the ability to choose to vaccinate should not depend on where a person lives, insurance status, or access to community resources. Protecting every Coloradan means ensuring that no community is left behind. Rural and underserved communities, which are most vulnerable to disruptions in vaccine policy, must remain fully included in outreach and policymaking.
Protecting community health is not the work of one profession or organization; it is the shared calling of physicians, nurses, pharmacists, public health officials, educators, and community leaders. By working together across disciplines and communities, Colorado can continue to build trust from the ground up and make sure vaccine policy is rooted in science and centered on better health for all. ■
David Higgins, MD, MPH, FAAP, is a general pediatrician, preventive medicine specialist, and health services researcher who has practiced in urban and rural settings in Colorado and Montana. He strives to improve child and adolescent health through innovative, community-based interventions, with a particular focus on vaccine delivery.

COLORADO PHYSICIAN OR MEDICAL STUDENT CALLS 720-810-9131.
24/7 line answered by a Masters-Level Licensed Clinician (LCSW, LPC) to assess the clinical need of the caller, including life-threatening situations.
CONFIDENTIALITY IS REVIEWED AND PEER SUPPORT SERVICES ARE INITIATED.
Only in circumstances where an individual is a threat to self or others or as outlined in the Medical Practice Act would confidentiality be breached. Doc2Doc Wellbeing Consulting has the same reporting obligation as all licensed Colorado physicians.
PHYSICIAN CALLER RECEIVES WELLBEING SUPPORT FROM A PEER PHYSICIAN.
If Doc2Doc Wellbeing Consulting is the best fit based upon the caller’s presentation, a physician will return the physician’s call for the first of three free peer consultations.
If CPHP traditional comprehensive evaluation services are a best fit based upon caller’s presentation OR if more help is needed at the end of three free Doc2Doc Wellbeing Consulting sessions, CPHP’s process will commence to ensure client has appropriate treatment supports in place.
