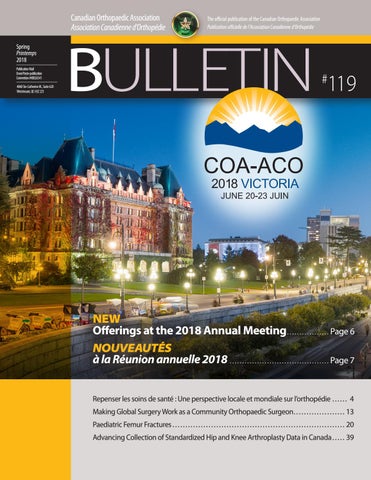
Canadian Orthopaedic Association Association Canadienne d’Orthopédie
Spring Printemps 2018 Publication Mail Envoi Poste-publication Convention #40026541 4060 Ste-Catherine W., Suite 620 Westmount, QC H3Z 2Z3
The official publication of the Canadian Orthopaedic Association Publication officielle de l’Association Canadienne d’Orthopédie
BULLETIN
119
#
NEW Offerings at the 2018 Annual Meeting.................. Page 6 NOUVEAUTÉS à la Réunion annuelle 2018......................................... Page 7 Repenser les soins de santé : Une perspective locale et mondiale sur l’orthopédie � � � � � � 4 Making Global Surgery Work as a Community Orthopaedic Surgeon � � � � � � � � � � � � � � � � � � � � 13 Paediatric Femur Fractures � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 20 .Advancing Collection of Standardized Hip and Knee Arthroplasty Data in Canada � � � � � 39