AUTISM RATES RISE AGAIN, NOW
AFFECTING 1 IN 31 U.S. CHILDREN
1 IN 5 ADULTS SUFFER FROM MENTAL ILLNESS
What’s behind the seeming surge in mental illness?



AUTISM RATES RISE AGAIN, NOW
AFFECTING 1 IN 31 U.S. CHILDREN
What’s behind the seeming surge in mental illness?
There need to be at least 2.7 children per woman to reliably avoid long-term extinction, according to study
Billionaire and Tesla CEO Elon
Musk has made headlines with dire warnings that declining birth rates are an “existential crisis” for humanity.
The threat might be even more dire than Musk (the father of at least 14) says, a new study argues.
The number of new births needed to maintain human population levels is higher than previously thought, researchers report.
There need to be at least 2.7 children per woman to reliably avoid long-term extinction, according to findings published April 30 in the journal PLOS One.
That’s higher than previous estimates, which held that a fertility rate of 2.1 children per woman would maintain population levels, researchers say.

However, that figure didn’t account for random differences in how many children people have, as well as changes in death rates, sex ratios and the possibility that some adults never have children, researchers said.
“A fertility rate higher than the standard replacement level is necessary to ensure sustainability of our population,” lead researcher Diane Carmeliza Cuaresma, an assistant professor at the University of the Philippines Los Baños, said in a news release.
All G7 countries have fertility rates well below either level, researchers noted — Italy at 1.29, Japan at 1.30, Canada at 1.47, Germany at 1.53, the U.K. 1.57, the U.S. at 1.66 and France at 1.79.
South Korea has the lowest fertility rate, at 0.87, and Japan’s popu-
lation is projected to decline by 31% in every generation if the fertility rate stays below the replacement level, researchers added.
For the new study, researchers calculated population levels accounting for factors like the ratio of females giving birth, the number of women who don’t have children and death rates prior to reproduction.
Results also showed that if more girls are born than boys, that reduces the extinction risk among humans.
That finding jibes with a long-observed evolutionary phenomenon, that more girls than boys tend to be born under severe conditions like war, famine or plague.
Most developed countries don’t need to be immediately concerned about population levels, the study explained.
“Extinction is not an immediate issue owing to the large population size in these countries,” researchers wrote.
However, the results suggest that most family lines will vanish due to a lack of offspring.
“The present results have a profound implication from an individual perspective: The family lineages of almost all individuals are destined to go extinct, whereas very few exceptions may survive for many generations,” researchers wrote.
“Languages also face the risk of extinction, with at least 40% of more than 6,700 spoken languages in the world threatened to disappear within the next 100 years,” researchers added. “The extinction of a language results in the disappearance of a culture, art, music and oral traditions.”




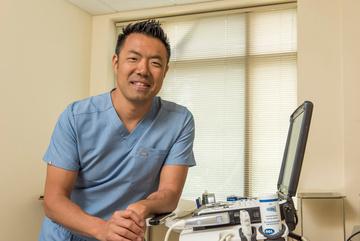
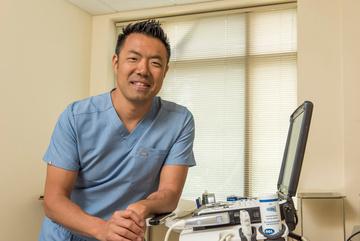
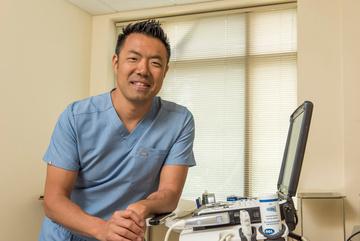
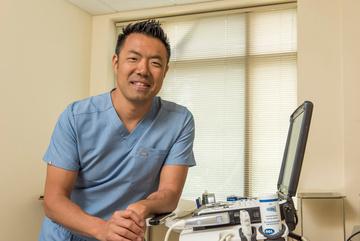
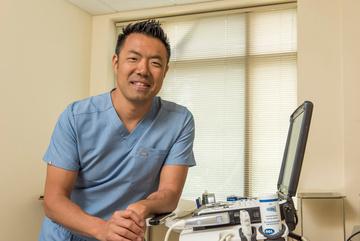
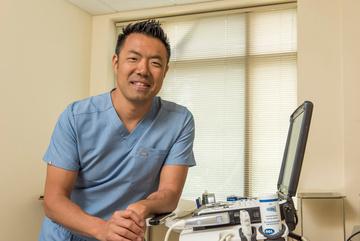
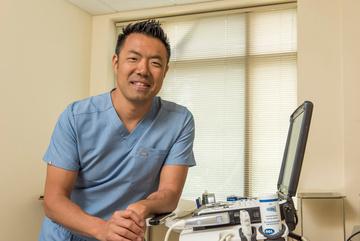
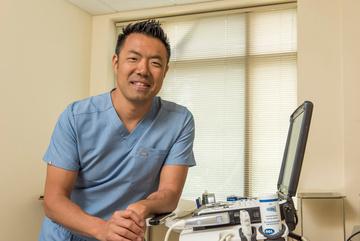
By Chris Motola
Dermatologist with a sub-specialization in pediatric dermatology discusses the delicate balance of treating kids with skin problems
Q: You’re a dermatologist with a sub-specialization in pediatric dermatology. I understand that there aren’t very many of you.
A: Yes, we treat both, adult and pediatric patients. Pediatric is a separate board certification. There are less than 15 fellowship programs for pediatric dermatology and probably 400 or less actively practicing in the U.S.
Q: What’s fundamentally different about treating children’s skin?
A: There are a lot of differences. In a general pediatrics sense, we have a saying that children aren’t just little adults. Because of their age, the management of skin conditions can
be more challenging. Where most adults can take care of their skin on their own, children and particularly infants, can’t do that. So you have to deal with and educate parents on treatment options. Children can participate in the decision-making process, but ultimately the responsibility lies with their parents. That also presents a different set of challenges. Kids are often born with genetic mutations in their skin that are unique to the pediatric population. To give you an idea of how challenging it can be, there have been several studies that have looked at the caregiver burden for children who have eczema, for example. The caregiver burden for that is akin to taking care of a parent with
Alzheimer’s. So the child isn’t the only one with the disease burden but the whole family. Additionally, kids with skin conditions often do worse in school than their peers and have more trouble with social engagement.
Q: Take eczema as an example. For adults it seems like more of a nuisance than debilitating unless it’s an extreme outbreak. Do children get worse flareups?
A: The caregiver burden is one thing, but the other is that it disturbs the child’s sleep. That makes it harder for them to do well in school. The constant itching also sets them up for skin infections whether it be bacterial, viral or fungal. So that presents a little bit of a challenge as well. And as a mentioned before, the treatment usually needs to be initiated by the parent. It is a chronic condition. Some kids are fortunate enough to outgrow it. Some kids carry it into adolescence or adulthood, which can be a challenge. With adults it’s just a lot easier to set up a plan and have them carry it out. It can be more of a challenge for parents, especially working parents.
Q: What got you interested in the sub-specialty?
A: I think having good mentors initially does that. Some people are just drawn to working with kids. I think each age presents different joys. For me the sense of humor of 5- or 6-year-olds or the dry wit of adolescents are just fun. I really enjoy that. It takes a different skill set to engage with a child or teenager and I enjoy that. Some people don’t like working with parents and children at the same time. I think every child presents a unique opportunity to watch them grow and I like participating in that. I think that’s a gift.
Q: You mentioned that children grow out of a lot of skin conditions. What’s going on there, biologically?
A: That’s the other thing that happens. When you’re dealing with a pediatric population you’re dealing with a population that’s continuing to change and grow. And so some things will present themselves in infancy and then as the immune system matures they’ll disappear. Other things, like acne, will show up later in life. It’s unusual to see it before adolescence. Those things come and go because you’re dealing with a more dynamic system. So you can provide parents with some reassurance or at least prepare them for what’s coming down the pipe and what interventions are available at each stage. Most aspects of medicine that concern children are a lot more conservative than they are with adults.
Q: When should a parent bring their child to a specialist like you?
A: I work with a lot of pediatricians in the area. In general, whenever a parent sees anything of concern on a child’s skin, the pediatrician has some concern as well and will make a referral, if needed. The good news is, in general, kids are much less likely to get skin cancers. On the other
‘Kids with skin conditions often do worse in school than their peers and have more trouble with social engagement.’
hand, they can be more vulnerable to chronic conditions that an intervention can fix or ameliorate. We’re pretty flexible in seeing kids.
Q: Shifting to adults, how should they prepare for a skin exam?
A: The first and most important thing is no cosmetics, makeup, moisturizers. Wear clothing that’s easy to change out of. Be aware of your personal and family history, if you’ve had any changes to moles. Let us know if you’ve gone tanning, if you work outside or have had multiple sunburns. We look patients over from head-to-toe, working around underwear. I also look inside the mouth. The most important thing I talk about is that the standard of care is now to use a dermatoscope, which allows us to evaluate patients more closely.
Q: Does being a dermatologist and beekeeper give you any special insight into bee stings?
A: The nice thing is that bees are usually pretty kind. It’s the wasps, yellow jackets and hornets that are the mean guys. I think the more interesting thing with beekeeping is how incredibly organized and structured a colony is. I find that just so fascinating. One female worker will, in her lifetime, generate an eighth of a teaspoon of honey. It takes almost 600 bees to make a pound of honey. Their lifespan from hatching to death is only about a month on average.
Name: I.A. Tangoren, M.D.
Position: Dermatologist and dermatologic surgeon. Owns and operates I. A. Tangoren M.D. P.L.L.C Dermatology ad Dermatologic Surgery in Syracuse
Treatments: He and his team provide comprehensive evaluation and care for all medical, surgical and cosmetic dermatologic conditions to patients of all ages
Hometown: Rockville, Maryland
Education: Perelman School of Medicine at the University of Pennsylvania
Affiliations: Crouse Hospital.
Organizations: American Academy of Dermatology; American Society of Pediatric Dermatology
Family: Wife, two daughters
Hobbies: Beekeeping, gardening



Next time you see your family physician or a hospital doctor, be extra kind and patient — they could be on the verge of burning out, a new study warns.
About 10% of internal medicine doctors in the U.S. report a high level of burnout, researchers reported May 5 in the Annals of Internal Medicine.
Further, doctors in the West are at significantly higher risk for burnout compared to those in other U.S. regions, researchers found.
“Understanding burnout in this population that provides general medical care is particularly relevant given the projected shortage of approximately 40,000 primary care physicians within the next decade,” concluded the research team led by physician Nathan Houchens, a clinical associate professor of internal medicine at the University of Michigan Medical School.
For the new study, researchers surveyed 629 internal medicine docs found through a national database maintained by the American Medical Association. About half of the doctors provide primary care, and the other half work in hospitals.
Researchers found that around 10% of the doctors had the three signs of burnout — emotional exhaustion, a sense of detachment and a feeling that their efforts don’t make a difference.
Sto Back a
Burnout risk was similar among doctors working at community medical centers, veterans affairs facilities and academic hospitals, results show. Similarly, there were no significant differences in burnout risk between primary care or hospital doctors, or between doctors working in inpatient or outpatient settings, researchers found.
and
Stop missing life’s greatest moments Stop planning life around pain
Back Pain should not mean
However, about 15% of doctors in the West suffered from burnout, significantly higher than those in the Northeast (9%), Midwest (9%) or South (7%), researchers found.
“Burnout remains prevalent among internal medicine physicians and does not seem to correlate to spe cific practice contexts,” researchers concluded. “Future research should explore systemic interventions that target common, important burnout drivers for internal medicine physi cians.”
Stop missing life’s greatest moments Stop planning life around pain
Stop missing life’s greatest moments Stop planning life around pain
A monthly newspaper published by Local News, Inc. 33,500 copies distributed throughout more than 1,000 high-traffic locations, including all Wegmans stores.
In Good Health is published 12 times a year by Local News, Inc. © 2025 Local News, Inc. All rights reserved. P.O. Box 276, Oswego, NY 13126
Phone: 315-342-1182 • Fax: 315-342-7776 • Email: editor@cnyhealth.com
Editor & Publisher: Wagner Dotto • Associate Editor: Stefan Yablonski
Writers: Deborah J. Sergeant, Jim Miller, Gwenn Voelckers, Anne Palumbo, Chris Motola, Melissa Stefanec, Eva Briggs (MD), George Chapman, Mary Beth Roach, Norah Machia
Advertising: Amy Gagliano, Pam Roe • Layout & Design: Angel Campos-Toro • Office Manager Trepasso-Ayers
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
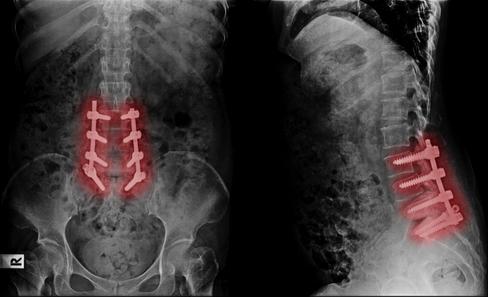
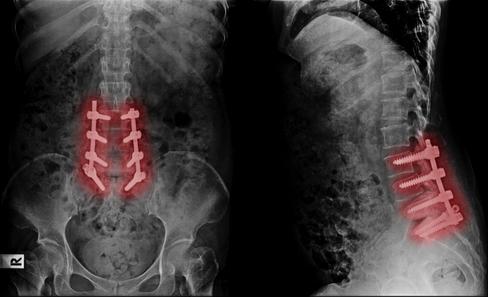
Back Pain should not mean fusion,
Back Pain should not mean fusion, screws, and lengthy recoveries Regenerative Medicine is changing how back pain is solved.
Back Pain should not mean fusion, screws, and lengthy recoveries. Regenerative ng how back pain is solved
Stop missing life’s greatest mome planning life around pain. B k P in should not mean fusio i Regenera g
’s greatest moments. Stop around pain mean fusion, screws, e l d
Back Pain should not mean fusion, screws, d l th eries Regenerative ow back pain is solved. ur last stop ur life!


your last stop Th e your life! Y O U
last stop. ife!







By George W. Chapman
Advantage plan offered by commercial insurers. It is often the only Advantage plan in a market. Unlike traditional Medicare, you are limited to providers within your chosen Advantage plan. When the local hospital system can’t reach an agreement with an Advantage plan, (surprise, usually over reimbursement) you can be left holding the proverbial bag and must scramble to find another Advantage plan accepted by your physician–hospital or give up Advantage plans altogether and revert back to traditional Medicare with which virtually all docs and hospitals participate. Medicare Advantage plans have been paying out more in claims as their senior members age. If they can’t be paid more by CMS they resort to negotiating lower payments to providers. If no agreement is reached, the Advantage plan will exit the market.
This confusion is just another reason to seriously consider universal health.
The American Association of Medical Colleges predicts that, unless things change, the shortage of primary care docs will increase to 45,000 by 2034. A survey produced by MDLinx and administered by M3 Global research of practicing physicians revealed 42% are very concerned about the impact of the shortage on quality, 84% have already seen the quality of care compromised and 34% would not recommend pursuing a career in medicine. Ironically, medical school applications are at an all-time high.
One of the problems is there are not enough residency programs for all the medical school graduates. Medicare determines the number of residency slots per hospital and funds them. Another problem is most medical school grads are faced with tuition debt around $250,000. So the
Once practically eradicated, there have been measles outbreaks in six states (as of early May). Vaccine hesi tancy and fatigue from the COVID-19 pandemic coupled with misinformation and even disinformation have contributed to the outbreaks. Scientific studies show that even a slight uptick in MMR vaccine use can prevent millions of new infections. JAMA recommends the first dose at 12-15 months followed by a second at 4-6 years. If the current rate of vaccination was kept constant, measles could become an epidemic with 850,000 cases over 25 years. If the current rate of vaccination decreased by just 10%, the prediction model estimates 11 million cases of measles over the next 25 years. The expense, let alone the potential deaths, would be cataclysmic. Now, if there was just a 5% increase in the current MMR vaccination rate, the prediction model estimates there would be less than 6,000 cases over 25 years. That is what is called a “tipping point.” If 95% of kids are vaccinated, we reach herd immunity. If parents refuse to vaccinate their kids,
more lucrative specialties are more appealing than primary care specialties like family practice, pediatrics, internal medicine and OB-GYN. Most primary care docs work 50-60 hour weeks. Finally, third party reimbursements have not kept up with inflation so running a financially viable primary care practice is a challenge, to say the least. Without a comprehensive national system to address and correct the impediments to pursuing primary care, it is very likely the 45,000 shortage will happen. Some ideas to make primary care more attractive are: increase and fund the number of residency slots at hospitals but only for primary care; forgive medical school debt for all primary care docs (there is such a program but the physician must work three years in a federally designated manpower shortage area);
could insurance companies deny the expenses associated with treating the disease? Could insurance companies increase the premiums?

The DOJ has filed a complaint against Aetna, Elevance and Humana for allegedly paying insurance brokers or advisers millions to steer relatively healthy prospects to their plans and to steer relatively unhealthy patients to the competition. The needs of the individual patient be damned. So far, there has been no determination of liability. The services of an insurance broker or adviser are free. They are eventually paid by the insurance company selected by the client. These brokers have an ethical and fiduciary responsibility to recommend the coverage that best suits the client’s individual situation.
Former National Institutes of Health director Frank Collins, M.D, Ph.D. (note M.D. and Ph.D.) regrets when you mix politics and science, you get just politics. He observed this became baked in during the politically polarizing COVID-19 epidemic when conspiracy theories and med-
incorporate “lifestyle” medicine into the primary care purview and reimbursement which includes nutrition, diet, exercise, sleep and stress management for chronic diseases. Finally, every year more and more physicians, in all specialties, seek employment with one of the hundreds of hospital-based healthcare systems. The business headaches of medicine are killing private practice. An effective and accessible primary care base is absolutely essential to the clinical and financial success of a large healthcare system. Absent a national fix, it may be up to savvy healthcare systems to provide more lucrative compensation packages and better working conditions for primary care physicians if we are to at least mitigate the predicted shortage.
ical quackery took hold, but probably showed early signs during the Obama administration. Before that, Collins contends, both parties were in sync and relationships between NIH-CDC-CMS-FDA and Congress were cordial and professional. You could not tell what anyone’s party affiliation was as all were interested in defeating Alzheimer’s, cancer and various diseases impacting the nation’s wellbeing.
Research was considered to be not only necessary but vital. It must have been nice back in the day to let scientists do their thing. Hundreds of researchers have been fired by the current secretary of Health.
So what do you do when your phy sician or hospital no longer accepts your insurance? You are often taken by surprise with little notice. Now you have to find a new provider or switch insurance. This dilemma is happening with increasing frequency especially with Medicare Advantage plans. Fifty-four percent of 62 million Medicare eligibles are enrolled in an

You can thank the CFPB (Consum er Fraud Protection Bureau) for keeping medical debt from be ing considered by lenders when it comes to loans or credit cards. But with the fate of the CFPB is now in limbo, consumer advocates fear the rule could be rescinded. The bureau has kept about $49 billion in medical bills from the credit reports of some 15 million people. Despite political pressure to kill the rule, advocates remain cautiously optimistic because the rule has bipartisan support due to the pervasiveness of medical debt (which would not exist with national universal coverage).

As of this writing in early May, there is growing support in Congress not to slash Medicaid by $880 billion over the next 10 years. It would deny coverage for millions and place hospitals in financial jeopardy. But what is most infuriating is the belief that the Medicaid budget should be cut because of supposedly rampant waste, fraud and abuse. So throw the baby out with the wash? Fraud, waste and abuse are already sought, litigated and recovered by the HHS Office of Inspector General. There is an effective police force, so punishing medical providers and legitimate Medicaid recipients to reduce fraud is absurd. The OIG recovered more than $7 billion in 2024. It brought 1,548 criminal and civil enforcement actions including overpayments to providers, enrollees and outright criminals. So no need to slash the Medicaid budget. Increase the budget of the HHS OIG.


George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.
By Gwenn Voelckers
Iremember the first time I hosted a gathering on my own after my divorce. It was a holiday party, and — no surprise — most of my guests were married. I worried I would feel like the proverbial third wheel at my own event.
On top of that, I was afraid my house would be too crowded, my seating too sparce, and the idea of entertaining without someone at my side felt … well, overwhelming.
Who would replenish drinks and the cheese board while I greeted people at the door? What if I ran out of ice or the music stopped or someone spilled wine on the rug?
For too long, I avoided hosting altogether, telling myself I wasn’t the entertaining type. But deep down, I missed bringing friends together in my home like “old times.”
I missed my former life.
Like so many things we learn when adjusting to life alone, solo hosting takes a little courage, a little planning and a willingness to stretch. But the good news is, it gets easier. Actually, it gets to be pretty fun.
Take my friend Sarah. She had been divorced for about a year when she decided to throw her first party alone. Her best friend was turning 60, and instead of meeting at a restaurant, Sarah wanted to do something more personal. “Nothing big,” she said. “Just a few friends, maybe some cake.”
Well, it turned into much more than that.
At first, Sarah was nervous. She worried her condo wasn’t big enough or stylish enough. She was anxious about the food, the music and the fact that she didn’t have a partner to help introduce old friends to new friends.
But once she got going — selecting a fun “Oldies but Goodies” theme, making a playlist, even serving fondue à la 1960s — her energy shifted. And when the sun set? Her patio glowed with string lights while guests let loose to “September” by Earth, Wind, and Fire, including her sister who hadn’t danced in decades.
Sarah was radiant. “I forgot how much I love entertaining,” she told me.
So, if you’re thinking about gathering friends together this summer, I say go for it.
Start small. A potluck picnic is a perfect, low-pressure way to ease into solo hosting. And who doesn’t love a backyard get-together in warm weather with easy food and good company?
Here are 10 tips to help make your solo-hosting picnic smooth, relaxed, and enjoyable:
1. Enlist a Co-Host — Just because you’re hosting solo doesn’t mean you have to do everything alone. Invite a friend to be your co-host. He or she can help greet guests, find serving
utensils and provide moral support if you start to worry whether you made enough guacamole.
2. Choose a Simple Theme — Themes add structure and fun without being fussy. Think “Summer Fiesta,” “Backyard BBQ,” or “Garden Party.” A theme gives guests a jumping-off point when planning what to wear or bring and helps you narrow down decorations and music choices.
3. Create a Guest List and Online Invite — Evite or even a group email will do the trick. Keep it casual, upbeat and clear. Let people know it’s a potluck picnic, the start time, and whether kids are welcome. Be sure to include your theme (if you have one) and any special notes, like “BYO lawn chair.”
4. Coordinate the Potluck — A little planning goes a long way. In your invitation, assign a category (salad, main, side, dessert, drink) and ask guests to reply with what they’re bringing. You can then easily manage any duplications by email. Simple.
5. Set the Scene Without Stressing — You don’t need to turn your backyard into a magazine spread. A few folding tables, some string lights or battery-powered candles, and fresh flowers from Trader Joe’s can transform your space. Launch your playlist, toss a few blankets on the lawn, and call it a day.
6. Keep the Menu Self-Serve — Buffet-style is the way to go. Set up stations: one for food, one for drinks. Stock a cooler with water and nonalcoholic options. Keeps things casual and let guests help themselves.
7. Include Something to Do (Besides Eating) — A game or two can help break the ice and give people a reason to move around. Think lawn games like cornhole or bocce ball. Last summer, I set up a badminton net and went old-school with croquet. Have fun!
8. Be Present, Not Perfect — No one cares if the napkins match or if you forgot to light the citronella candle. Your guests are there to enjoy your company, not critique your tablecloth. Relax and enjoy the moment. A dropped drink or a late arrival keeps things interesting.
9. Leave the Cleanup for Tomorrow — Consider leaving the big cleanup until the next day. Do the basics (like getting food inside and covering anything perishable), then pour yourself a drink and bask in the glow of what you just pulled off.
10. Do It Again — Seriously. Once you realize how doable and fun it is, you’ll want to throw another party. Hosting solo doesn’t have to feel lonely or hard. It can feel liberating, empowering — even thrilling.
So, if you’re on the fence about your first solo hosting experience, wondering whether it’s worth it ... trust me, it is. Not just because you’ll have fun, but because you’ll remind yourself that your life, your home, and your friends are worth celebrating.
Start small. Keep it light. Feel the joy.
This summer, let yourself be the host who says, “I can do this.” Because you can!

Gwenn Voelckers is a certified life coach (CLC), columnist, and author of “Alone and Content,” a collection of inspiring essays for those who live alone. She welcomes your comments, questions, and inquiries at gvoelckers@rochester.rr.com.
Previously, the CDC estimated 1 in 150 kids had autism. That rose to 1 in 44 by 2018, 1 in 36 in 2020, and now 1 in 31
Autism diagnoses are on the rise again, with about 1 in 31 U.S. children affected, according to a new report from the U.S. Centers for Disease Control and Prevention (CDC).
The latest data, from 2022, shows a jump from the 2020 estimate of 1 in 36.
The report looked at health and school records for 8-year-olds in 14 states and Puerto Rico, the Associated Press said.
Rates were higher among boys, and also among children who are Asian/Pacific Islander, Black or
American Indian/Alaska Native, the CDC added.
Autism is a developmental condition linked to differences in the brain. Symptoms vary, but may include delays in learning and speech, trouble with social interactions and a strong need for a routine.
Until the 1990s, autism was considered rare. Back then, only children with severe symptoms were typically diagnosed. But it came to include a range of other mild conditions, known as autism spectrum disorder (ASD), The Associated Press said.
Previously, the CDC estimated 1

in 150 kids had autism. That rose to 1 in 44 by 2018, 1 in 36 in 2020, and now 1 in 31.
Experts say the increase is due to better awareness and improved screening. There’s no blood or lab test for autism; doctors make the diagnosis by observing behavior.
Over the years, research has ruled out childhood vaccines as a cause. Other studies have explored genetics, as well as age of parents, maternal health and exposure to certain chemicals. Some researchers suspect a combination of factors could play a role.
Still, some people still continue to question the science. U.S. Health Secretary Robert F. Kennedy Jr. recently announced plans for a major autism research effort.
He said it would involve hundreds of scientists worldwide and find the cause of autism by September.
Kennedy also claimed the program would help remove those causes. During a recent meeting at the White House, Kennedy and President Donald Trump both referenced the new 1-in-31 stat, The Associated Press said.
Kennedy’s announcement drew much criticism for his decision to hire physician David Geier to lead the research.
Like Kennedy, Geier has long pushed the idea that vaccines cause autism. In 2011, Maryland officials found that Geier practiced medicine without a license.
By Norah Machia
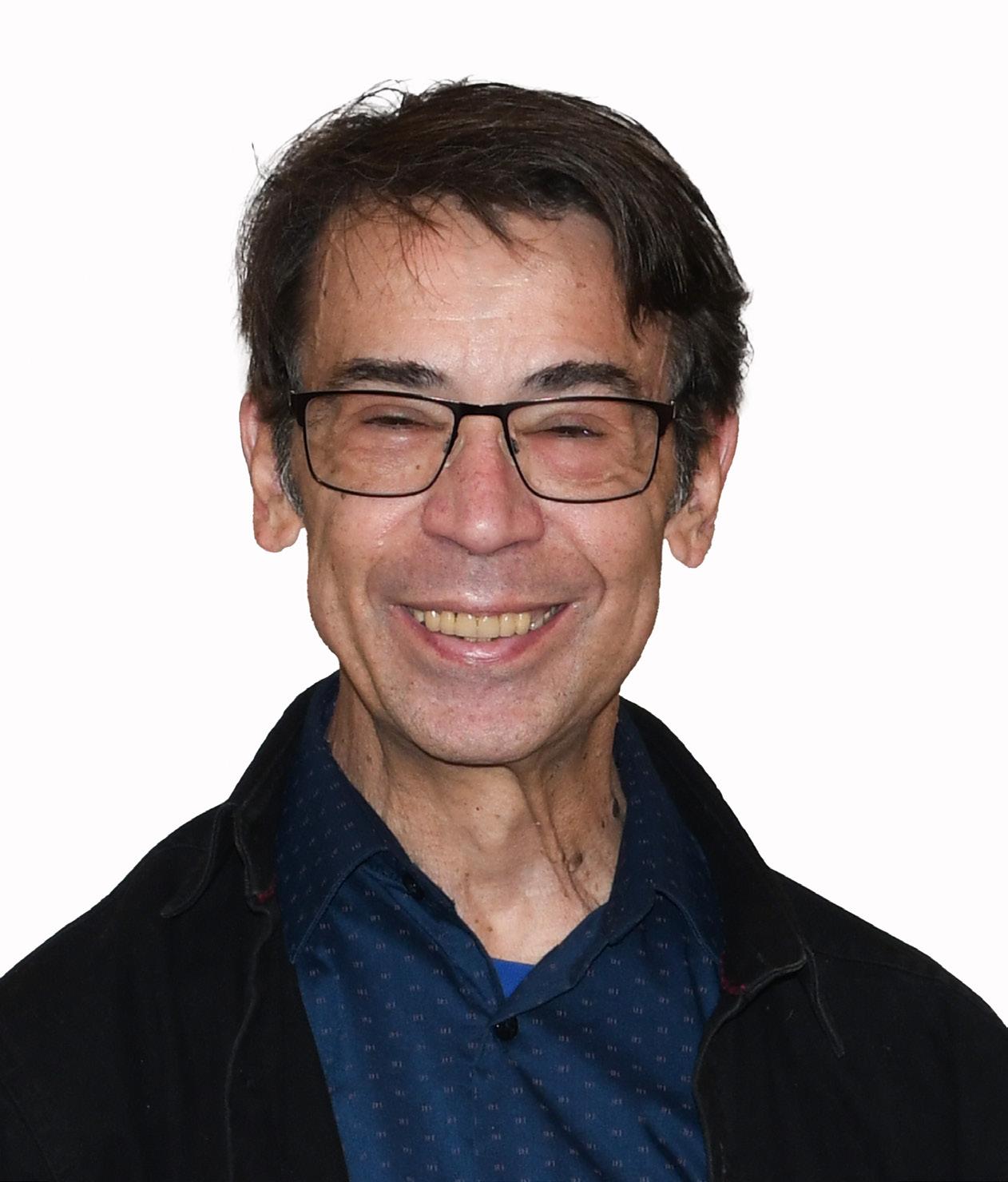
ASyracuse man has written a fictionalized book reflecting on his battle with cystic fibrosis and the double-lung transplant that saved his life 20 years ago.
Dave Murray, 68, a one-time associate editor at the former Syracuse New Times, was inspired to publish the book “A Breath of Fresh Air (A Transplant Tale)” as he reached his lung transplant milestone anniversary in August. In 2004, Murray received his new set of lungs at the Cleveland Clinic in Ohio.
The book chronicles Murray’s challenging life experiences with cystic fibrosis through the fictional character Danny Martini. While many aspects of Murray’s life, such as his family, past employers, friends and relationships, were given fictional references or imagined in another way, the medical information throughout the book represents a true reflection of his health crisis, said Murray.
“I fictionalized it because I’m a private person and in some cases, my memory wasn’t great,” he said. “I took some liberties in telling my story — I wanted the book to be exciting and amusing to engage the reader.”
In his book disclaimer, Murray writes, “Any resemblance to actual persons, living or dead or actual events is purely coincidental.”
But the medical information throughout the book is “98% accurate,” he said.
Although Murray exhibited cystic fibrosis symptoms (such as a chronic cough and weight loss) throughout his childhood and teenage years, he was not officially diagnosed with the condition until age 19.
“My mother had read a newspaper article about cystic fibrosis and told me I should get tested,” he said. “I was floored when I got the diagnosis and at that time, I didn’t have the discipline to take care of myself.”
In the book’s description, Murray wrote about his reaction to the diag nosis through the character of Danny.
“Average CF life expectancy then was just 31 short years. Danny Martini’s world was turned upside down. His optimism was replaced by the seeming certainty of an early death,” Murray wrote. “Danny lived fast and burned through his life as if each night might be the last. A nihilistic lifestyle of drugs, drinking and hard living and the cumulative impact of CF took a heavy toll.”
“He fell in and out of love. He made great and lifelong friends. But by 2004, cystic fibrosis left him emaciated and exhausted, tethered to an oxygen tank,” he added. “His breath and his time grew short. Only a lung transplant could save his life.”
According to the Mayo Clinic, cystic fibrosis is a genetic disease that causes the body to produce thick, sticky mucus. This mucus clogs the lungs and leads to frequent infections. It also blocks the digestive enzymes in the pancreas from reaching the intestines, where they are needed to help digest food. Most cases are diagnosed in childhood, but nearly 10% of CF cases aren’t found until adulthood.
Although cystic fibrosis is progressive and requires daily care, people with the condition are usually able to attend school and work. Today, people diagnosed with the disease typically have a better quality of life than those in previous decades. Many improvements in screening and treatments have enabled CF patients to live longer and better lives.
At the time Murray was born, newborns were not routinely screened for cystic fibrosis as they are today in all 50 states. His symptoms were milder at the beginning, so the doctors who treated his ailments as a youth were skeptical of a CF diagnosis.
During his 20s, Murray experienced bleeding ulcers because of the
time, CF can also damage lung tissue to the point where lung function gradually worsens and eventually becomes life-threatening. That was Murray’s case by the time he reached 48 and became dependent on oxygen to breathe.
“I began coughing up blood, and I was really surprised,” he said. “I was hemorrhaging and I didn’t know that could happen.”
In 2003, he was placed on a waiting list for a lung transplant list after years of medical evaluations.
“They don’t want to give you new lungs too early because they want you to keep your own lungs for as long as possible,” Murray said.
At his last evaluation before being placed on the waiting list, the physicians “realized I had reached the point of no return,” he said.
The first attempt at a lung transplant was unsuccessful. Murray was prepped for surgery and awaiting a new set of lungs when his surgery was abruptly canceled.
“I was just told those donor lungs were unsuitable,” he said.
But the second time was a success.
Throughout the book, Murray tries to make light and add humor to his medical crisis, as only someone who has experienced it firsthand can get away with writing. But his seriousness about the CF also shows through, particularly when he writes about being near death and receiving the lung transplant.
Murray is rigid about taking his medications, about 50 pills daily, including anti-rejection drugs and an assortment of digestive enzymes. He developed diabetes as a result of steroids following surgery, but he manages it well with daily insulin injections and a continuous glucose monitor. Murray said he appreciates a second chance at life and is doing everything possible to prolong it.
Although Murray wrote letters expressing his gratitude to the lung donor’s family (which were delivered through the Cleveland Clinic), the family has not responded to them. But in his book, Murray portrays Danny as writing and eventually meeting the lung donor’s family to show his appreciation for the life-saving donation.
“It made for a better end to the story,” he said. “It was a good emotional tie-up to the book and it was uplifting to imagine what it would be like to meet the family.”
“A Breath of Fresh Air (A Transplant Tale) is available in both paperback and a Kindle version on Amazon or may be purchased through traditional bookstores,” Murray said.
Cover of “A Breath of Fresh Air (A Transplant Tale),” a book written by Dave Murray. He details the struggles growing up with cystic fibrosis and his life after a transplant in 2004.
Dave Murray exhibited cystic fibrosis symptoms throughout his childhood and teenage years, but he was not officially diagnosed with the condition until age 19. In 2004 he received his new set of lungs at the Cleveland Clinic in Ohio.
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126
315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
SPRINGBROOK APARTMENTS
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101
The following services are included in your rent
• Trash Collection • Free Wi-Fi
• Bus for shopping/groceries
• Heat, Electricity & Hot Water
• Snow Removal & Lawn Care
• Planned Activities
• All repairs & maintenance Applications are now being accepted! 62+ No smoking!
Preference given for veterans & spouses of veterans.
Equal Housing Opportunity Supervised by NYS DHCR
Local News Inc. is hiring drivers to distribute copies of In Good Health – CNY Healthcare Newspaper in Madison County. It’s not a regular job. Once or twice a month.
The job consists of getting the monthly publication in Liverpool and distribute it to various locations, mostly at doctor’s offices, hospitals, healthcare centers and other high traffic locations. We provide a list of places. The job needs be performed during the day, roughly from 9 to 5 from Monday through Wednesday. In general, pick up is on the first Monday of the month around 9 a.m. (once a month). A reliable car with a good size trunk is a must.
$15.50 an hour plus mileage allowance (30 cents per mile). It amounts to about $200 per job.
Great for active retirees and for stay-at-home mom who have some free time.
For more information, call (315) 342-1182 and ask for Mary T.
By Deborah Jeanne Sergeant
Kyle Riley, a nurse anesthetist from Upstate University Hospital, discovered his career “by accident,” he said.
When a senior in high school, he was taking a class through BOCES about basic anatomy and also job exploration in health care. Part of it included job shadowing. While shadowing in an operating room, Riley stood against the wall to avoid touching anything.
“A gentleman asked if I would stand with him,” Riley recalled.
He agreed and learned that the gentleman was a nurse anesthetist, who shared his job responsibilities, education and work-life balance. At home, Riley looked up the career online and liked what he saw.
“From that time forward, that’s all I wanted to do,” he said.
He works with the adult population, but nurse anesthetists can specialize in many areas. He works with
anesthesiologists. He checks and prepares equipment to start his day. He talks with patients and compares that with what the surgeon requires. He can prescribe an anesthetic plan and administer it.
As the father of young children, Riley likes that he can work weekdays from 7 a.m. to 3 or 4 p.m.
“The job offers a great amount of flexibility,” he said. “I can pick and choose as to when and where I want to work.”
He advises anyone interested in the career to read up on it and have a good understanding and aptitude for pathophysiology, pharmacology and chemistry.
Shadowing a nurse anesthetist as he did can help people know if this is the right path as well.
“One reason I find it rewarding is we provide anesthesia to people who need to have a surgeon to fix a problem in their lives,” Riley said.
The nurse practitioner field has expanded substantially in the past three decades
By Deborah Jeanne Sergeant
Valerie Meyers, nurse practitioner in adult health at Northern Family Care in Central Square, had been working for a few years as a registered nurse and loved the nursing field. But she “wanted to be able to do a little more to help patients stay healthy,” she said.
That’s when she furthered her education to become a nurse practitioner. This year, she celebrates her 30th year in the profession. Initially, she had begun her education at LeMoyne on a pre-med track.
“I liked the aspect of taking care of the whole person and the handson healing to get people better,” she said. “I had really wanted to take care of people. I love math and science. It all fits together with nursing.”
Working as a nurse practitioner has allowed her to broaden her scope of practice in holistic way, caring for the entire person instead. She views
doctors and nurse practitioners as working together in a complementary way.
The nurse practitioner field has expanded in the past three decades.
“When I started, you were certified in adult or pediatrics,” Meyers said. “Now it has expanded to acute care, geriatrics and so much more. It standardizes the practice more.”
She enjoys working with her patients and building lasting relationships with them, which is less like the hospital setting, where patient care tends to be more acute.
To perform this type of work, “you’ve got to be a person who will put the patient first and care for people based on their perspective, not yours,” she said. “When you’re taking care of someone, it’s all about them. That can be hard for some people to do. It’s a good field. It’s a good part of the team. It takes a team to take care of people.”
“There’s a lot of anxiety. To be able to help them through a difficult point of their lives in such a short amount of time, to me that’s rewarding. They’re relying on you to be their caretaker while unconscious. We help them forget a time they don’t want to remember. I’m so happy I was exposed to this accidentally. I owe that gentleman a large platter of gratitude.”
Nurse anesthetists have additional training beyond the registered nurse designation.
Mark Blazey, nurse anesthetist at Highland Hospital and president of New York State Association of Nurse Anesthetists, said that nurse anesthetists do everything that physician anesthesiologists do, but from a nursing background, as nurse anesthetists must first earn a nursing degree and work as a nurse in a high acuity ICU.
“We go over the patient chart and medical history and talk with the patient about consent, risks and benefits,” he said. “We bring them into the OR, administer anesthesia, communicate with the physician about their needs, make sure they’re asleep and their vital signs are within the parameters we want.”
They also may administer
There’s a broad range of what someone can do with an advanced degree: specializing in a type of patient or scope of care, educating the next generation of nurses and working in an institutional setting such as a hospital or long-term care facility.
Selma Mujezinovic, Rochester Regional Health vice president of advanced practice providers, said that many people who end up working as a nurse practitioner start as RNs and then develop the desire to pursue a master’s and doctorate as a nurse practitioner.
“The root of nursing is caring,” Mujezinovic said. “We deliver nursing care in a medical model.”
Although the master’s degree is the minimum requirement, she added that the trend is to go for the doctorate degree.
“There are various ways to get into advanced practice,” Mujezinovic said. “The vast majority have chosen this as a first career. But it’s not impossible to choose it as a second career.”
Nurse practitioner training focuses on population health across the age span but can specialize in areas such as pulmonology through on-the-job training for many of the niches. They support the other providers in a team-based environ-
Salary
According to the Bureau of Labor Statistics, the annual mean wage for a nurse anesthetist in the Rochester area is $229,850 (information is not available for the CNY area).
anti-nausea medication, check fluid balance and offer post-op pain management.
As part of their work, nurse anesthetists are airway and cardiopulmonary experts.
The age range of Blazey’s patients can vary from newborns to seniors.
“We have a short period of time to develop a rapport with the patient,” he said. “They have to believe ...they can place their lives in your hands.”
He enjoys the technical aspects of his job and that he solves problems while helping patients remain safe and comfortable.
“I like making a difference in their outcome,” he added.
People interested in becoming nurse anesthetists don’t need to worry about career longevity.
“The career is absolutely in high demand,” said Cheryl Spulecki, past president of the New York State Association of Nurse Anesthetists and current professional practice chair, works as a professor at University Buffalo. “There is a shortage of anesthesia providers.”
She said that a strong science background and a penchant for helping others are traits people should have if they’re interested in working as a nurse anesthetist.
“It’s for someone who’s interested in longevity within a profession; it’s a career, not a job,” Spulecki added. “Very few do any providers regret their decision. There’s a lot of flexibility within the profession regarding to finding your ‘happy place’ where you want to work.”
ment, including doctors in hospitals, doctor’s offices and clinics. In some fields such as dermatology, nurse practitioners can perform minor surgical procedures within that area of practice. They can also diagnose acute or chronic conditions, prescribe medication without a supervising physician and perform other therapeutic measures in that area.
Many small practices rely upon nurse practitioners for tasks such as physicals, managing chronic conditions, patient education and counseling and monitoring medication effects.
“If we didn’t have them, we wouldn’t be able to meet the needs of as many patients,” Mujezinovic said. “There would be delays in care. We are able to reach the vast majority of patients with high quality, affordable care.”
Salary
According to the Bureau of Labor Statistics, the annual mean wage for a nurse practitioner in the Syracuse area is $121,660.

It’s vital for those interested in becoming a PA to possess a heavy aptitude for science.
By Deborah Jeanne Sergeant
Ashley L. Volles had known from a young age that she wanted to work in medicine.
Shadowing various medical professionals while in high school led to her current designation as a doctor of medical science, physician assistant (PA) and assistant director of Advanced Practice Services at Upstate University Hospital.
“While I was shadowing with a physician, he introduced me to his physician assistant,” Volles said. “I was able to spend some time with her and she explained her role, scope of practice, and relationship with the care team, and I found it intriguing.”
That encounter caused her to narrow her options to physician and physician assistant. She took all the required college courses for both and took the MCAT, but ultimately decided that becoming a physician assistant aligned more closely with her professional and personal goals.
She also liked the notion that she has so much hands-on care with patients.
“I’m a fixer, and I take great pride in helping patients, my team, and anyone I can,” Volles said. “Being a PA allows me this opportunity and I am so fortunate.
“My role as a PA is fulfilling to me because I come to work every day with the opportunity to advocate for my team, advance our profession on a departmental and institutional level, and hopefully, make everyone’s life just a little bit easier.”
PAs can switch their specialty without major educational pursuits. The position’s on-the-job training helps PAs segue into a different specialty. PAs practice under a supervising physician, but still experience a great deal of autonomy.
Sometimes it’s challenging feeling like someone’s overlooking one’s work as a PA. Over time, PAs and their supervising physicians build a relationship based on trust and the autonomy increases.
Patients asking for “a real doctor” is still a challenge PAs occasionally face, even though they can do nearly everything a physician in primary care can do, including treat and diagnose patients, prescribe medication—even narcotics—and read tests such as X-rays. Practic-
ing independently is one of the few things PAs can’t do.
With the current physician shortage, it’s little wonder that PAs are often call “physician extenders,” along with nurse practitioners.
Selma Mujezinovic, Rochester Regional Health’s vice president of Advanced Practice Providers, sees extenders as a means of helping meet the healthcare provider crisis.
“Physician assistants are trained in a medical model,” Mujezinovic said. “They enter the educational programs straight out of high school, generally as a first career.”
At entry level, PAs have a master’s degree, similar to a nurse practitioner, although trained in a medical model rather than a nursing model.
She believes that the science of medicine and innovation is what draws many to the career, along with the desire to help people.
“There’s passionate care delivered by PAs,” Mujezinovic said. “While they might not be interested in becoming a MD and going through that training, they can contribute to the wellness of their patients.
“They can impact patients’ wellness and healing. It’s a very rewarding job. They can educate their patients and families about how to improve health and aid in pain management. It has a lot of flexibility. They have a lot of flexibility for their hours and whether in person, hybrid or home. It’s a very enticing profession.”
It’s vital for those interested in becoming a PA to possess a heavy aptitude for science. Demonstrating a commitment to academics and volunteering in a healthcare program can also help prospective PAs enter the programs which Mujezinovic said can be as vigorous and competitive as medical schools.




Dr. Tangoren is board certified in dermatology and pediatric dermatology. He and his team provide comprehensive evaluation and care for all medical, surgical, and cosmetic dermatologic conditions to patients of all ages.
2949 Erie Blvd Suite 110 • Syracuse, NY 13224 315-424-1430 • https://drtangoren.com/
June 8, 2025 at 10:00am check-in at 9:00am

According to the Bureau of Labor Statistics, the annual mean wage for a physician assistant in the Syracuse area is $123,850










By Melissa Stefanec MelissaStefanec@yahoo.com
comeback, but weeds are persistent. Perhaps, they are even more persistent than my children’s boredom. If you’ve got time to be bored, you’ve got time to weed. Am I right?
• Response 3: “Let’s be bored together.”
The fact that actions speak louder than words is the bane of parenting. However, if I want to teach my kids that being bored is totally benign, I should offer to be bored with them. Come to think of it, I’m dying for a little boredom. So, why not indulge the concept?
that the world has never heard of or making a dream home out of boxes for our cats. I need to nudge them to create and see what they find.
• Response 7: “Why don’t you cook or bake something you love?” Cooking is a valuable life skill. When I give my kids permission to make whatever food they want, they will usually take the task head-on. So what if it means the oven is on when it’s 85F outside? It beats the heat of whining, complaining and bickering.
• Response 8: “Why don’t you do or make something nice for someone

Upstate's revitalized and growing heart services provide benefits to you.
From six cardiology outpatient sites to the arrival of our new heart surgeons, and more doctors and advanced providers for procedures such as caths and TAVRs, we are here to work with you.
Learn more about what The Upstate Advantage can do for you.
By Anne Palumbo
Idon’t eat a lot of meat these days, but when I do, it’s usually chicken and if it’s chicken, it’s typically thighs. Plump, juicy, flavor-packed thighs that are more affordable and more forgiving when overcooked.
Why chicken over beef, especially now during grilling season when the prospect of a char-grilled burger still makes me salivate?
The more I learn about beef’s negative impact on the environment—much worse than chicken!— the less I’m inclined to eat it.
On top of that, chicken generally has fewer calories, less cholesterol and less fat than beef, especially saturated fat, the unhealthy fat that raises bad cholesterol.
Both chicken breast and thigh are excellent sources of protein, a powerhouse nutrient that plays a crucial role in building and repairing tissues, supporting the immune system and fueling metabolic processes. What happens when we don’t get enough protein? Research shows that, over time, a protein deficit can make you lose muscle mass, slow your metabolism, and also
lead to anemia, all of which makes you weak and tired.
Furthermore, people who are low in protein often find their injuries—from cuts to sprains to broken bones—are slower to heal. Same goes for colds, sore throats, and the flu: a lack of protein can weaken the immune system, contributing to longer recovery times when you do get sick. On the fat and calorie front, chicken generally has fewer calories and less fat than beef, making it a better choice for weight management.
To compare: a 3-oz 80/20 hamburger patty has about 230
Serves 4, Seasoning adapted from Chef Kia Damon; crema adapted from loveandlemons.com
Lime crema ingredients:
1 cup whole milk Greek yogurt or sour cream
2 tablespoons mayonnaise
1 tablespoon fresh lime juice
1 small garlic clove
½ teaspoon salt
¼ teaspoon onion powder
½ cup fresh cilantro
Blackened chicken ingredients:
½ tablespoon kosher salt
1 tablespoon paprika (regular or smoked)
½ tablespoon dried thyme
½ tablespoon dried oregano
½ tablespoon dried garlic powder
½ tablespoon dried onion powder
1 teaspoon mustard powder
¼ teaspoon ground cayenne (optional)
½ tablespoon vegetable oil
4-6 boneless, skinless chicken thighs, trimmed
1. Remove chicken from refrigerator to allow it to come to room temperature.
2. Make the lime crema: In a food
processor, place the yogurt, mayo, lime juice, garlic, salt, and onion powder. Process until creamy.
3. Add the cilantro and pulse until the sauce is smooth but green flecks are still visible. Season to taste. (Can be made ahead and stored in the refrigerator for up to 5 days.)
4. Make the blackening seasoning: In a small bowl, combine all the dried seasonings.
Prepare the chicken: Pat dry, then rub thighs lightly with oil and coat all sides with blackening seasoning. Set aside while you prepare the grill.
5. Place thighs on grill and cook until the seasoning darkens. After 5 minutes, flip the chicken and cook for another 3 minutes.
6. When ready to serve, slice the chicken on a bias into ½-inch pieces or leave whole; serve alongside lime crema.
calories and 15 grams of fat (with nearly 6 of that saturated fat) while the same amount of skinless chicken breast has only 120 calories and 1 gram of fat (with no saturated fat). Skinless chicken thighs have about 150 calories and 7 grams of fat (with 2.5 of that saturated fat).
Chicken is also rich in many B vitamins, particularly niacin, as well as the trace mineral selenium. People who are mildly deficient in niacin, an essential vitamin that helps keep the nervous system, digestive system, and skin healthy, may experience skin rashes, diarrhea, and mental confusion or memory loss. An antioxidant superstar, selenium improves thyroid health, boosts the immune system, and helps prevent cognitive decline.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

Since not all chicken is prepared the same, you should limit or avoid certain types that may be higher in unhealthy fats, carbs, salt and calories, such as fried and breaded chicken, rotisserie chicken, and heavily processed lunchmeat. Choosing poultry raised without antibiotics is an important way to help fight back against antibiotic resistance. Finally, no hormones are ever used in the production of any US chicken.

By Anne Palumbo
We hear a lot about “superfoods” these days — foods that offer high levels of desirable nutrients that are believed to offer simultaneous health benefits beyond their nutritional value.
These foods, as defined in the Merriam-Webster Dictionary, are “rich in compounds (such as antioxidants, fiber or fatty acids) considered to be beneficial to a person’s health.”
But what about “superbadfoods” — foods that offer high levels of undesirable nutrients that clog arteries, add pounds, raise blood pressure, trigger diseases, and shorten lives? Foods that we mindlessly eat or (gasp!) feed to our kids or grandkids? Where’s Merriam’s definition for those disastrous foods?
While there are dozens of unhealthy foods out there, we’ve mentioned some alarming — perhaps surprising — foods that our bodies could regularly do without.
Just how bad are they?
Well, when you compare what these superbadfoods offer up in a single serving against what the experts recommend for an entire day, you may be persuaded to rethink your eating habits.
Average daily recommendations from accredited institutions:
• Sodium: less than 2,300 milligrams per day (equal to about 1 teaspoon of table salt) and no more than 1500 milligrams per day with high blood pressure.
• Sugar: no more than 100 calo ries per day (about 6 teaspoons or 24 grams) for most adult women and no more than 150 calories per day (about 9 teaspoons or 36 grams) for most men.
• Fat: should contribute 20% to 35% of total daily calories (about 4578 grams) with no more than 20 to 30 grams of saturated fat.
ing you never fraternize with another Frito again. Moderation is the key here: daily, devoted, mindful moderation. As the saying goes, “Man and woman cannot live on junk food alone.”
What do years of regularly eating processed meats and health have in common? Cancer.


• Cholesterol: no more than 200 milligrams a day (if risk factors for heart disease present); no more than 300 milligrams a day (if no risk factors).
• Overall calories: Calorie needs vary depending on the person and their personal health goals, but an average starting number is around 2,000 calories per day.
Of course, no one is suggest-
According to the World Health Organization, regular consumption of processed meats — bacon, sausage, hot dogs, ham and cold cuts — has been associated with an increased risk of cancer (especially colon and stomach), as well as heart disease and diabetes. All meat that has been smoked, salted, cured, dried or canned is considered processed. Nitrates and nitrites — whether synthetic or natural (i.e. celery powder) — are the processing agents behind the elevated risk. Chemicals aside, many processed meats are high in calories, fat (especially saturated fat) and sodium. One classic Zweigles hot dog (minus the bun and fixings) has 220 calories, 19
grams total fat (7grams saturated), and 660 milligrams salt. Three slices of bacon have 150 calories, 12 grams total fat (3 grams saturated), and 550 milligrams salt. With early-onset colon cancer rates on the rise for younger adults, it should give all of us pause. Many experts do say, however, that eating a small amount of processed meat occasionally, such as once or twice a month, is unlikely to significantly harm health.
Tips: Check out plant-based alternatives. Swap red-meat processed foods for white-meat processed foods, which generally have less total and saturated fat. Consider canned or pouched tuna or salmon instead of classic lunchmeats like ham, pastrami, roast beef or salami.
Drinking soda is like guzzling liquid candy, no thanks to its high concentration of sugar. Sugary drinks are a major contributor to our country’s obesity epidemic, which
is why many states have actively banned the sale of sodas in high schools. Coke Original, America’s most popular soft drink, has 2-3 times our average daily sugar needs in one serving! Why worry about consuming too much sugar? In the short term, it may contribute to acne, weight gain, tooth decay and fatigue. In the long term, excessive sugar consumption increases the risk of Type 2 diabetes, obesity, heart disease, certain cancers, high blood pressure and depression. Of course, some sugar (which the body converts to glucose) is essential for energy production and proper brain function.
Tips: Gradually replace soda with nutritious alternatives: water infused with fresh fruits and herbs, sparkling water with a splash of fruit juice, homemade iced or herbal tea, reduced-sugar fruit juices and smoothies, and good old plain water.
Oh, how we love our Lay’s, Doritos, Cheetos and Rice Krispies Treats here in America! Indeed, they fly off our supermarket shelves to the tune of $52 billion per year. Despite being convenient and addictive to boot, chips, like most other ultraprocessed snacks, are astoundingly unhealthy (one serving of Lay’s classic: 160 calories, 10 grams of fat, 170 milligrams sodium). What’s more, they defy everything — everything — a snack is supposed to do: give your body a nutrient-dense, long-lasting pick-me-up between meals. Research has shown that because today’s ultraprocessed snacks contain a lot of fat, sugar, salt and carbs, they are better at activating the brain’s reward system. Translation? We can’t stop eating them. The unfortunate consequences? We develop many of the same chronic diseases as those associated with sugar-loaded soft drinks.
Tips: Opt for snacks with protein, fiber, and healthy fats that take longer to digest and help keep you full throughout the day. A few suggestions: nuts, Greek yogurt

with fruit, hard-boiled eggs, cheese with whole-grain crackers, popcorn, homemade trail mix and protein smoothies.
Although soups may be the perfect meal when you’re feeling chilly, under the weather or not particularly hungry, some canned and chain-restaurant soups are not so perfect for your health. From sodium to fats, calories to cholesterol, soups can foil your good intentions in just a few slurps. Are you sitting down?
One cup of Campbell’s Chicken Noodle Soup, their most popular soup, has 1780 milligrams of sodium — a whopping 78% of daily needs knocked off in one bowl (over 100% for those with high blood pressure).
Panera’s popular broccoli cheddar soup has 1560 milligrams of sodium without the bread bowl and a staggering 2140 milligrams with. While sodium is an essential nutrient that controls blood pressure and is needed to make nerves and muscles work properly, too much sodium can lead to high blood pressure, heart disease, kidney strain, and stroke. It can also drain calcium from bone.
Tips: When dining out, choose broth-based soups over cream-based; when buying canned, opt for lower-sodium broth-based soups; and when making soup, go easy on the salt, substitute cream or whole milk with reduced-fat milk, use whole grains versus refined, and up the veggies.
Most of us think salads are automatically healthier foods: low in calories, sodium, and fat; high in vitamins, protein, and fiber. The ones we make at home: perhaps; the ones we order out: perhaps not. For example, Chick-fil-A’s Cobb salad with avocado-lime ranch dressing—high in calories (830), fat (60 grams), and sodium (2220 mg)—is no day at the healthy-diet beach! And building a Chipotle salad with lettuce, chicken, guacamole, corn, cheese, and chipotle-honey vinaigrette, chased with a side of queso blanco and chips, could quickly turn that healthy-sounding lunch into a calorie bomb. Nonetheless, salads are an important part of a healthy diet because they are a year-round source of essential vitamins, nutrients, and beneficial antioxidants that can help reduce the risk of chronic diseases such as heart
disease, diabetes, cancer, and obesity.
Tips: Whether taking out or making at home, assemble salads wisely: forgo caloric toppings (bacon bits, croutons, candied nuts) and baked shell bowls, go for dark greens, add healthy protein sources, bump up the veggies, opt for vinaigrette- or yogurt-style dressings over cream-, cheese-, or mayo-based ones, and request dressing on the side. Oh, and stay away from “crispy” and “crunchy” protein sources, as the description implies “deep-fried.”
From French fries to onion rings, doughnuts to funnel cakes, many of us find fried foods irresistible. Unfortunately, compared to other cooking methods, deep frying adds a lot of calories and fat. For example, one small baked potato contains 120 calories and 0.2 grams of fat, while the same amount of French fries con tains 430 calories and 20 grams of fat. What’s more, fried foods are typical ly high in trans fats, the worst kind of fat you can eat. Unlike other dietary fats, trans fats do a number on cho lesterol: raising “bad” while lowering “good.” Research has shown that a diet laden with trans fats increases the risk of heart disease, the leading killer of adults. But the badness of fried foods doesn’t end there. Regu larly eating fried foods puts you at a greater risk of developing Type 2 diabetes and obesity, two conditions that, over time, can lead to high blood pressure, some cancers, nerve damage, sleep apnea, dementia, heart disease, asthma, and more. Yikes.
Tips: Avoid or severely limit your intake of fried foods. When frying at home, choose safer, more stable oils: coconut, olive, or avocado over canola, corn or sesame oil (to name a few). Consider healthier cooking methods: steaming, roasting, stir- or air-frying.




Read product labels and restaurant menus carefully, from nutritional information to ingredients. Consider how something is prepared: baked versus fried. Think about health in the long run, from yourself to your loved ones to those on the way.
Anne Palumbo writes the column Smart Bites, which is published every month in In Good Health.

What’s behind the seeming surge in mental illness?
By Barbara Pierce
One in 20 of US adults and 1 in 5 Americans aged 6-17 experience a mental health disorder each year, according to the National Alliance on Mental Illness.
It may seem the number is climbing higher than in previous decades. However, data from the New England Journal of Medicine indicates that the rate in 1990 is similar to current times. But is it really a matter of higher recognition rather than an increase in the rate of occurrence?
A rise in diagnoses also points to at least a small increase in openness about mental healthcare.
“Since the pandemic, rates of endorsed mental illness among the general population in the US are exponentially increasing and more of those people are seeking professional services,” said John Ringhisen, board certified psychiatric-mental health nurse practitioner at Upstate Medical University. “There has also been an explosion of awareness on social media that must be approached with caution in the age of misinformation and uninformed opinion being presented as truth.”
Ringhisen directs the Psychiatric Nurse Practitioner Fellowship at Up-
state and the ADHD Clinic as well as serving as an adjunct professor at the Norton School of Medicine at SUNY Upstate Medical University.
During the pandemic, people began to give more attention to mental health problems. With work, travel and leisure activities halting, people had more time to look frankly at their mental health. Plus, people who already had mental health problems typically experienced an increase in severity and some people experienced onset of problems — and that’s still trending. Employment changes, a lack of interest in social interactions and the convenience of delivery services as isolative factors which can contribute to mental health problems. Limiting social interactions isn’t good for mental health.
“COVID-19 pandemic is believed to account for some of this change,” said Monique Winnett, Ph.D. and clinical psychologist at St. Joseph’s Health. “Increased access to global news and worries about society and politics can also contribute. In general, young adults aged 18-25 are most likely to report behavioral health concerns and women are more likely than men to report symptoms.”
By Deborah Jeanne Sergeant
Talking with friends and family can improve mental health. You can share your struggles, receive practical and emotional support and feel encouraged about your life.
But you likely will need help from a professional mental health provider at some point in your life.
Whether an acute or ongoing issue, connecting with a provider can make a big difference in improving your mental health. Finding a provider can seem daunting.
“Despite the need, there remains a disparity between the need for behavioral health services and the availability of providers,” said Monique Winnett, clinical psychologist at St. Joseph’s Health. “Initiating a dialogue with your primary care provider or other healthcare provider can always be a good starting point.”
Healthcare providers have referral lists of mental healthcare providers in the area and also likely have an idea of someone that would make a good fit for your needs.
Winnett said that it’s also import-
ant to call your insurance company to see which therapists are within your network. Out-of-network providers will cost more or could even be entirely out of pocket and those expenses will add up quickly as these issues tend to take time to resolve.
“There is a lot of variability among behavioral health providers training and areas of proficiency,” Winnett added. “It is always recommended that you find someone with experience in treating your specific conditions and that you work to engage with a therapist who uses evidence -based treatments to increase your likelihood of having a remission in your symptoms.”
John Ringhisen, board-certified psychiatric-mental health nurse practitioner at Upstate Medical University, also said that it’s important to figure out the kind of provider and services that are needed.
“Do you want medication? You need a psychiatric provider, such as a nurse practitioner specifically licensed in psychiatry, a psychiatric-mental health nurse practitioner.
Winnett also attributes the increase in mental health issues to greater screening by medical providers, who routinely assess mental health during visits. But Winett added that behavioral health symptoms remain underreported.
Physician Sutanaya Pal, assistant training director and assistant professor in the Department of Psychiatry and Behavioral Sciences and in the psychiatry residency program at Norton College of Medicine at SUNY Upstate Medical University, said that the rate of serious distress or impairment is much lower than 20%.
Some of the mental health issues reported relate to “problems with daily living, which people have reasonable reactions to,” she said. “There is a lot of economic strife and inequality. There’s a very reasonable reaction.”
This may lead to pathologizing a reasonable reaction that can be remedied with a few life changes.
Pal believes that limited access to normal family supports have increased mental health problems. When students attend a school far from home and settle there after graduation, they lose an entire com-
If you only want talk therapy, do you want someone qualified to do testing? You need a clinical psychologist. If testing isn’t important, then someone to work through issues and skills like a licensed clinical social worker may be a better fit.”
Ringhisen directs the psychiatric nurse practitioner fellowship at Upstate and the ADHD Clinic, as well as serving as an adjunct professor at the Norton School of Medicine at SUNY Upstate Medical University.
Any previous diagnoses should also be noted, such as autism, ADHD, borderline personality or substance use.
“These may require more specialized and comprehensive care or multiple providers,” Ringhisen added. “Be persistent and patient. Finding a mental health provider is more personal and may require a few sessions before you can really determine whether it’s a good fit for both you and the provider.”
National Alliance of Mental Illness maintains a site with helpful articles about mental illness, along with a list of crisis lines and providers who can provide scheduled sessions for mental health. The local chapter is NAMI Syracuse (www. namisyracuse.org).
Other resources for finding help include www.betterhelp.com, and the department of health (Onondaga County, http://www.ongov.net/ health; Oswego County, https://
munity of support. The same goes for people who relocate for work or retirees who move out of state.
Pal also said that many young adults and adults are still dealing with issues carried over from adolescence.
“The rate is 50%,” she said. “They’ve grown up without a village. It’s an understandable reaction to a difficult situation.”
She encourages people struggling with mild to moderate, nonacute mental health issues to do things that support them, like interacting with their community, whether through common interest, religion, ethnic community or anything else.
“Find something you can connect with people on and use those to build community,” Pal said. “I am a psychiatrist by training and provide therapy at all ages. The point of therapy is to find out ways in which you can help yourself. Maintain your physical health and connections in any way you can.
“There’s always a role of medications, but that is challenging. They only fix so much. But if the distress is really bad, talk with your doctor about it. Most primary care providers are good at providing support and have a good idea of medications and prescribing. Most of the time, this can be handled on a very basic level. Do common sense things that help you feel well.”
Instead of comparing yourself with others, which can cause anxiety, it helps to focus on gratitude. Instead of ruminating on global stressors, think about what you can control to keep your life going well.
It’s also helpful to regularly engage in self care, reach out to friends or professionals for help as needed. Find fulfillment in helping others, as this helps turn the focus outward. Let go of past mistakes and give yourself grace for things that you cannot change.

health.oswegocounty.com; Cayuga County, https://www.cayugacounty. us/1850/Health-Department).
Therapists understand that you need time to determine if you’re a good fit with that therapist. It’s OK to speak with a few different therapists until you find one that feels right.
By Deborah Jeanne Sergeant
Whether it’s a trait directly related to male gender or a tendency of how men care for their health, men’s health needs can be different from women’s. To safeguard and improve their physical and mental health, men and those who love them should heed these health tips from area experts:
• “Many men grow up thinking they must be strong all the time and keep their emotions inside, often being afraid to let anyone know how they are truly feeling. Here is the truth though. Mental health is just as important as physical health and therefore, we want to ensure that men know that asking for help is not a sign of weakness as it is so often stereotyped.
• “Here’s something serious to think about: men die by suicide nearly four times more often than women, according to the Centers for Disease Control and Prevention. That’s why it’s so important to speak up, support one another and have honest check-ins with men about how they are feeling. While checking in, it is important to know and understand some of the common signs of mental health struggles in men which tend to include but is not limited to the following: feeling sad, angry or hopeless often; sleeping too much or too little; losing interest in things you used to enjoy; trouble focusing or making decisions; feeling tired all the time; using alcohol or drugs more than usual; and thinking about self-harm or suicide. If you or someone you know shows these signs, talk to your doctor or a mental health professional and please under-
stand you are not alone, and help is available.
• “If you find yourself struggling this month, consider also trying some simple ways to increase your mental health and feel better which may include but again is not limited to going for a walk or getting outside; exercise regularly — even 15 minutes helps; talk to a friend or family member try breathing or relaxation exercises; set small goals for your day; get enough sleep and eat well; and limit alcohol and screen time. Some of these steps may seem too simple to work, but they are in fact incredibly useful tools to boost mental health.
• “If you’re in emotional distress or thinking about suicide, call or text 988 anytime to connect with a trained crisis counselor. It’s free, confidential and available 24/7.
• “Mental health affects more people than you think. Remember that asking for help is not a sign of weakness. Providers are working hard to increase support and services to make mental health care more accessible to the community. If you’re struggling, reach out. Getting the help you need may be simpler and more convenient than you realize.
• “If you live in Oswego County and are passionate about or would like to learn more about mental health resources that are available, please don’t hesitate to reach out to the Oswego County Suicide Coalition at preventioncoalitionstaff@gmail. com to learn more and get involved.”
Travis Bulluck, manager at Suicide Prevention Coalition in Oswego.
• “What we do, what we eat, and when we sleep are the key points to physical, mental health.
• “The more you move and remain strong, the better off you are. It doesn’t have to be a complicated gym routine; it can be a 20-minute walk each day.
• “Healthy bodies are built from healthy foods, and it must be in proportion to how much you move. If you don’t know what’s healthy, there are plenty of free or paid apps to help track what and how much you eat and set goals. Some even let you take a picture of your food and AI figures it all out for you.
• “Sleep is when our bodies repair and recover. If you’re not sleeping, it’s like idling your car in the garage overnight. Something is going to break down before you expect it.
• “Men today are more isolated and less social than ever compared to
Men’s Health Month is observed annually during the month of June. It’s a time dedicated to raising awareness about health issues that affect men and boys, and encouraging them to take proactive steps to improve their overall well-being.
Key objectives of Men’s Health Month include:
• Raising Awareness: Highlighting preventable health problems and encouraging early detection and treatment of diseases among men and boys.
• Promoting Healthy Habits: Encouraging men to adopt
any other demographic.
• Mental health flourishes when we have meaningful — not online or virtual — relationships with other people. Find a group, friend or activity that involves talking to people and sharing experiences and ideas. Men need to work harder to find safe places to express emotion and work through feelings without fearing reprisal. It may require talking to a professional if no one else can allow vulnerability without judgment.”
John Ringhisen, board-certified psychiatric-mental health nurse practitioner at Upstate Medical University and director of the Psychiatric Nurse Practitioner Fellowship at Upstate and the ADHD Clinic. Ringhisen also serves as an adjunct professor at the Norton School of Medicine at SUNY Upstate Medical University
healthier lifestyles through diet, exercise, and regular checkups.
• Encouraging Preventive Care: Emphasizing the importance of regular medical screenings and check-ups.
• Supporting Men’s Mental Health: Addressing the stigma surrounding mental health issues and encouraging men to seek support when needed.
• Promoting Family Engagement: Recognizing that men’s health impacts families and encouraging loved ones to support men in their health journeys.

By Eva Briggs, MD
Iremember the first cell phone that I ever saw. It belonged to my nephew, an early adopter.
I recall it being roughly the size and shape of a concrete block. It was a far cry from today’s powerful smart phones that easily fit into a pocket.
Medical technology, too, continues to evolve to become smaller yet more powerful.
I recently read about a tiny absorbable pacemaker that is roughly the size of a grain of rice! It measures 1.8 millimeters wide, 3.6 millimeters long and 1 millimeter thick.
Engineers at Northwestern University developed this technology. They set out to develop a device that could be used in newborn infants with congenital heart disease. These babies sometimes need a temporary pacemaker after heart surgery. Existing temporary pacemakers were just too big. This little pacemaker will also be able to be used for older children — or adults — who need a pacemaker temporarily while their heart recovers following surgery.
The pacemaker is soft, flexible and wireless. It can fit into the tip of a syringe, allowing it to be placed through a blood vessel to reach the heart. No surgery required.
Current temporary pacemakers require the insertion of wires which are later removed. These wires go through the chest wall, potentially allowing infection. Sometimes scar tissue forms around the wires. The scar tissue can tear and bleed during the removal process.
The new device is made from bioabsorbable materials that are safely absorbed by the body in seven to 10 days. This is similar to absorbable sutures. This eliminates the risks and dangers of wires and their removal: infection, dislodgment, tissue damage, bleeding and blood clots.
A skin-mounted patch worn on the body communicates with the device telling it when to send an electrical signal to the heart muscle. When it detects an irregular or slow heartbeat it signals to the pacemaker that the heart needs an electrical pulse. The patch communicates
via infrared light that safely passes through the body to the tiny pacemaker. The power for the pacemaker itself from comes from two different metals inside the device. They form a battery when in contact with bodily fluids.
The tiny size means that doctors could potentially insert several pacemakers into a single patient. This would permit stimulation of different segments of the heart muscle to improve synchronization of the heart muscle contraction.
The technology used to develop the miniature pacemaker may have
future applications to help heal nerve damage and broken bones, to treat wounds and block pain.


New executive director Meals on Wheels Syracuse expects a higher demand for the nonprofit’s services
By Mary Beth Roach
Q: Can you share what the Syracuse Meals on Wheels is and how many people you serve?
A: Our mission is to organize, plan and administer the service of delivering nutritious meals, nutrition education and resource assistance to people living in our community that are unable to do so for themselves. We provide education resources and case management services to our clients. Typically, on a daily basis, we serve around 395 people. A statistic that to me is really significant is 247,000 meals a year.
Q: These meals are not just for senior citizens, is that correct?
A: Eligibility requirements typically start at 60. However, there are circumstances when that requirement is waived, particularly if a client has a disability that creates a lack of mobility or they’re homebound and unable to prepare meals or shop for food.
Q: You come from a background of nonprofit organizations, having worked at Arise and Prevention Network. How do you believe that prepared you for Meals on Wheels?
A: My entire career was primarily in the behavioral health realm. I was the executive director at Prevention Network for eight years and loved nonprofit leadership, loved that organization and really honed my leadership skills. And what I’ve learned over the course of my career is that there’s so much that impacts a person besides physical and mental health. There are eight dimensions of wellness that frame my thinking. What attracted me to Meals on Wheels and leading this organization was the opportunity to intersect the mission of this organization with the “power of a knock,” which is Meals on Wheels America’s tagline. It’s so much more than meals. Sometimes it’s the only socialization for individuals that we serve. I saw an opportunity for building on that, continuing to provide the meals, but also taking this “power of a knock” and really enhancing what we could offer individuals in terms of resources. My
experience helped me become very familiar with the community and other resources.
Q: What are the eight dimensions of wellness?
A: They’re emotional, social, occupational, financial, environmental, physical, intellectual and spiritual. It comes from the Substance Abuse and Mental Health Services Administration.
Q: Do you see the need increasing? And if so, why?
A: Absolutely. I think that there are a number of reasons. The state of affairs in the world right now and continued funding and attention given to human service needs, especially of vulnerable populations, are increasingly concerning. I think with some of the anticipated changes, we’re going to see an increase in folks that are unable to continue doing some of these things for themselves. And unfortunately, I also think that we’re going to see an increase in the number of people that are homebound. The biggest issue is uncertainty for both those we serve and the team here. I see it as part of my responsibility to prepare us for what may come.
Q: What are your goals moving forward?
A: The first goal is to honor the legacy that [former executive director] Mason Kaufman established. There is an amazing staff and almost 500 volunteers. It’s mind-blowing to watch what happens here on a daily basis so that we can serve 400 people every day. Another goal would be in terms of intersecting with the eight dimensions of wellness in any way that we can. And with the unknown that lies in front of us, guiding the team and the organization, to the best of my ability, to continue serving one of our most vulnerable populations. She became executive director of Syracuse Meals on Wheels this spring, replacing Mason Kaufman, who retired after having been at the organization since 1995.

•
Excellus BlueCross BlueShield
“A close friend once told me that I was a people person and should use that ability as a social worker,” Megan Bunce recalls.
That advice, shared more than 15 years ago, led Bunce to a career that has improved hundreds of children’s lives. Bunce, a licensed social worker at Excellus BlueCross BlueShield, works with some of the most vulnerable people in our society.
She began her role in the foster care program in 2023. Each year, this team provides case management to more than 1,000 children. More than that, though, the program provides stability, hope and a chance for a healthier future in a system that includes over 25,000 boys and girls in New York state.
Excellus BCBS may be best known for offering health plan options, but the nonprofit prides itself in its wide-ranging work around access and quality care. That includes children in foster care.
“I remember helping a little girl who had been struggling with her vision for years,” Bunce recalls. “Together with her foster care case manager, we identified a provider, got the coverage approved and lined up the appointment where she was prescribed glasses. This may seem simple to some, but it’s often these types of things people take for granted that make a significant difference in a child’s life.”
The foster care team ensures medications are being used properly, vaccines are completed, and
well-child visits are scheduled. Staff members also address any other gaps in care that may arise.
While the work is rewarding, it can often be difficult, according to Lindsay Rachow, a licensed mental health counselor and manager of the foster care program. “As you can imagine, these young members’ stories can be challenging to read,” she says. “It takes a special person to serve in this role. Bunce’s ability to connect with people is what makes her work so impactful.”
Bunce appreciates that her work is seen and felt. “Never have I looked back and regretted the decision to move forward with this career,” she says.
JeanMarie Armellino, a social worker from the Children’s Home of Wyoming Conference, understands the complexity of these children’s needs. “Our continuous communication with the [Excellus BCBS] foster care team empowers us to respond swiftly to the children’s needs while fostering a more integrated approach to care,” she says.
The partnership with local foster care programs began in 2013, when Excellus BCBS launched an initiative to ensure children in foster care receive necessary services and support.
“Too often, the challenges faced by those aging out of the foster care system can lead to housing instability, unemployment and substance use,” Rachow says. “The need for comprehensive support throughout

their life is critical.”
For example, when the Excellus BCBS foster care team receives a notification that a member in its care has had an emergency department or inpatient hospital visit, staff members take immediate action. They seek to understand the reason for the visit, providing education on urgent care versus emergency visits and ensuring that safety planning, medication changes and follow-up care are in place.
“Teamwork allows us to become a trusted resource for families, filling gaps in care and providing support
Upstate nurse named president of American Pediatric Surgical Nursing Association
Maryellen Sheridan, a pediatric clinical nurse specialist at Upstate Golisano Children’s Hospital, has become president of the 1,000-member American Pediatric Surgical Nurses Association, Inc. (APSNA). She will serve through 2027.
Founded in 1992, the APSNA aims to shape pediatric surgical nursing through advocacy, collaboration, mentorship and leadership, and to transform the treatment of pediatric surgical patients through its research and education. By developing guidelines and sharing evidence-based practices, APSNA promotes consistency and quality in pediatric surgical nursing. This contributes to safer, more effective care for children across diverse healthcare settings.
Sheridan’s leadership and
service to the organization are significant, having served in a variety of roles over the past 10 years, including as president-elect, treasurer and on various committees.
Sheridan has been a member of the nursing team at Upstate since 1995 having worked in pediatric urology; she currently serves as a clinical nurse specialist in pediatric surgery. In 2017, Sheridan spent time in Uganda on a medical mission providing surgical nursing medical care to pediatric patients in the East African nation.
In her current role, Sheridan brings extensive experience in surgical patient care, serving as a vital liaison between physicians, patients, and families. Her work includes developing and implementing educational materials for surgery, trauma, and postoperative care, and providing guidance to families of pediatric surgical patients. Sheridan has helped enhance patient outcomes
through assessment support and service coordination, while also leading initiatives such as resident orientation and hospital discharge follow-up.
Sheridan received both her bachelor’s and master’s degrees in nursing from the Upstate College of Nursing.
She has received numerous awards and accolades for her work, including the APSNA Founders Award for excellence in pediatric surgical nursing; the Upstate President’s Team of the Year Award (for pediatric surgery (2008), Upstate Pediatric Nursing Excellence award (2004, 2009) and Upstate Patient Experience award (2019) and nominee (2024).
Sheridan’s research on such topics as pediatric incontinence and kidney disease has been published in various publications, including the Journal of Urology.
during critical transitions,” Bunce explains.
Children in foster care are twice as likely as other children to have learning disabilities, three times more likely to have ADD or ADHD and seven times more likely to suffer from depression, according to the Journal of American Medical Association (JAMA). These alarming statistics underline the necessity of the services that Excellus BCBS provides.
“Youth in the foster care system often face unique social determinants of health challenges,” Bunce says. “It’s common for them to have higher rates of mental health conditions like anxiety and depression, as well as chronic health issues like obesity to asthma. They’re at a greater risk for a myriad of health problems compared to their peers. Our work is vital.”
Both Bunce and Rachow say their support extends beyond case management. They offer training to foster parents, encouraging them to attend the children’s advisory committee meetings held twice a year, covering topics like substance use and selfcare for caregivers. They also ensure that children’s wishes are considered when making decisions about their medical needs, working closely with caseworkers to respect each child’s voice.
“The work we are doing serves as a powerful reminder that when we come together to support one another, we can create lasting change and brighter futures for those who need it most,” Bunce says. “I have found meaning in being the person families could rely on. When they look back, they can say, ‘Bunce was there for our family’ — those are the moments I will never forget.”
To hear Megan Bunce’s story, go to www.youtube.com/ watch?v=TE2vUYBUPbw
To learn more about the foster care program at Excellus BCBS, visit excellusbcbs.com.

By Jim Miller
Dear Savvy Senior,
What all does Medicare cover when it comes to vision care? I currently have good vision insurance through my employer but will lose it when I retire.
Almost 65
Many soon-to-be retirees are a bit blurry with what Medicare does and doesn’t cover when it comes to vision care.
The good news is that Medicare covers most medical issues like cataract surgery, treatment of eye diseases and medical emergencies. Unfortunately, routine care like eye exams and eyeglasses are usually the beneficiary’s responsibility.
Here’s a breakdown of what is and isn’t covered.
Eye exams and treatments: Medicare does not cover routine eye exams that test for eyeglasses or contact lenses, but they do cover yearly medical eye exams if you have diabetes or are at high risk for glaucoma. They will also pay for exams to test and treat medical eye diseases if you’re having vision problems that indicate a serious eye problem like macular degeneration, dry eye syndrome, glaucoma, eye infections or if you get something in your eye.
Eye surgeries: Medicare will cover most eye surgeries that help repair the eye function, including cataract surgery to remove cataracts and insert standard intraocular lenses to replace your own. Medicare will not, however, pick up the extra cost if you choose a premium multifocal lens that restores full range of vision, thereby reducing your need for glasses after cataract surgery. The extra cost for a premium lens can run $1,500 to $4,000 per eye.
Eye surgeries that are usually not covered by Medicare include refractive (LASIK) surgery and cosmetic eye surgery that are not considered medically necessary.
Eyeglasses and contact lenses: Medicare will not pay for eyeglasses or contact lenses, with one exception: If you have had a conventional intraocular lens inserted during cataract surgery, Medicare will pay for eyeglasses or contact lenses following the operation.
Although original Medicare’s vision coverage is limited to medical issues, there are ways you can save on routine care.
Here are several to check into.
Medicare Advantage plans: Many of
these plans, which are alternatives to original Medicare and sold through private insurance companies, cover routine eye exams and eyeglasses, but coverage is limited so be sure you understand the specifics.
While I don’t recommend enroll ing in an Advantage plan just to get vision coverage, it is an option you should know about. To locate Advantage plans in your area that provide vision coverage, go to Medicare.gov/ plan-compare or call 800-633-4227.

Purchase vision insurance: If you get routine eye exams and purchase new eyeglasses annually, a vision insurance plan may be worth the costs. These policies typically range between $5 and $30 per month. Most plans will also have copays or deductibles you’ll be responsible for.
Check veterans’ benefits: If you’re a veteran and qualify for VA health care benefits, you may be able to get some or all of your routine vision care through VA. Go to VA.gov/ health-care/about-va-health-benefits/vision-care to learn more.
Find cheaper shopping options: Many retailers provide discounts –between 10 and 50 percent – on eye exams and eyeglasses if you belong to a membership group like AARP or AAA.
You can also save by shopping at discount retailers like Costco Optical, Sam’s Club Optical or Target Optical, which are all recommended by Consumer Reports. Or consider buying your glasses online at retailers like ZenniOptical.com, EyeBuyDirect. com or GlassesUSA.com which offer big savings.
To purchase glasses online, you’ll need a valid prescription from an eye doctor (no more than a year old), plus your pupillary distance number, which is the distance, measured in millimeters, between the centers of your pupils in each eye.
Look for assistance
There are also health centers and local clinics that provide free or discounted vision exams and eyeglasses to those in need. To find them put a call into your local Lions Club (see Directory.LionsClubs.org) for referrals.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.


Are you paying too much for your prescriptions?
Do you qualify for Medicaid?
Do you have enough $$$ set aside for your funeral?














Say hello to a convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at nine School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI ACUTE CARE SUITE
MONDAY - FRIDAY 7:00AM - 6:00PM
ACCEPTING NEW PATIENTS AT ALL SCHOOL BASED HEALTH CENTERS! SCAN THE QR CODE FOR ENROLLMENT FORMS!
Central Square (315) 675-9200 Fulton (315) 598-4790 Oswego (315) 342-0880 Pulaski (315) 298-6564 Parish (315) 625-4388 Phoenix (315) 695-4700 Mexico (315) 963-4133