Continuing Education program



- June Modules
Jan
2023
Continuing Education Program 2023 STUDY GUIDE

The Continuing Education Program 2023 Study Guide relates to the following National Safety and Quality Health Service Standards:

Every effort has been made to trace and acknowledge copyright material. Should any infringement have occurred accidentally the authors and publishers tender their apologies.
Copying
Except as permitted under the Act (for example a fair dealing for the purpose of study, research, criticism or review) no part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means without prior written permission. All enquiries should be made to the publisher at the address below.
Chief Executive Officer
SA Ambulance Service
GPO Box 3
Adelaide SA 5001
Published by: Clinical Education, SA Ambulance Service
OFFICIAL OFFICIAL 2
Continuing Education Program 2023 - Jan 2023
Version 1.0 221031
Contents
Introduction 6
What Modules Must be Completed From January-June 2023 6
Reaccreditation 6
CEP Record Keeping 6
Scope of Clinical Practice 7
Providing Clinical Care When Off Duty 7
Delirium 8 Learning Outcomes 8
Introduction 8 Delirium 9 Causes of Delirium 10
Delirium Risk Factors 10 Recognising Delirium 11 Management of Delirium 12
Summary 12
Infection Prevention and Control 13
Introduction 13 Learning Outcomes 13
Infectious Disease 13
Infection Prevention and Control 19
Standard Precautions 19
Routine and Scheduled Cleaning 27
Safe Handling and Disposal of Waste 33
Transmission-Based Precautions 34
Immunisation 36
Managing Occupational Risk and Exposure 36

Out of Hospital Cardiac Arrest (OHCA) Reaccreditation 39
Learning objectives 39 Introduction 39 Covid-19 39
Does Training Influence Patient Outcomes? 40
Cardiac Arrest: The Theory 41 Why Have They Arrested? 41
What About Cardiac Rhythms During Cardiac Arrest? 45
High-Performance CPR 48
Physiology Of CPR 48
Defibrillation 52
Special Circumstances 54
Approach To Airway And Ventilation Management 55
Continuing Education Program 2023 - Jan 2023
Continuing Education Program 2023 STUDY GUIDE OFFICIAL OFFICIAL 3
Cardiac Arrest Choreography - Pit Crew CPR 57
Mobile CPR 61
Post-Rosc Care 63
What’s Documentation Got To Do With Cardiac Arrest Management? 65
Reconciliation Action Plan: Asking the Question 70
Learning Outcomes 70
The Question 70
How to Ask the Question: 71
Tips for Asking the Question: 72
Exceptions on When to Ask the Patient 72
Strategies If Not Well Received: 72
Prepared Answers 72
Research on Why Patients Should Be Asked 73
Cultural Reason Why Patient’s Should Be Asked 76
Asking the Question, and Recording the Answer 76
Summary On Why It’s Important to Ask Every Patient 77
Glossary 78

Continuing Education Program 2023 STUDY GUIDE OFFICIAL OFFICIAL 4 Continuing Education
Program 2023 - Jan 2023
eBook Symbol Key



Click on this icon to play a Video
Click on the orange text to be taken to the Glossary definition for that word. Click on the word in the glossary to return to its reference.

Click on this icon to be taken to a page in a related eBook/learning materials






Click on this icon to view a Clinical Practice Protocol on the web version of the SAAS Clinical App.




SAASNET Links

Click on the following icon to open resource found on SAASnet.
Click on this icon to play Audio
Click to return to the Contents page
Click to open a link to an external website
Click on this icon to be taken to related SAAS eLearning courses. You will need to login to view the course

Please ensure you are logged into the intranet prior to clicking on the icon.
Relevant Clinical Practice Procedure documents
Opens relevant Information Notices
Opens relevant Procedures
Opens relevant intranet pages and resources.
Opens relevant Policies
Opens relevant Safety Alerts
Opens relevant SA Health Guidelines and Directives
Continuing
Continuing Education Program 2023 STUDY GUIDE OFFICIAL OFFICIAL 5
Education Program 2023 - Jan 2023
Introduction
What Modules Must be Completed From January-June 2023
All modules must be completed as outlined in the table below. Other SAAS or SA Health modules may be deemed necessary based on work location/role. For any additional information please discuss this with your Regional Team Leader (RTL).
Semester 1 Modules
BLS
Ambulance Assist Ambulance Responder Ambulance Officer
Each module below has been designed as an educational resource for operational volunteers at an Ambulance Assist (AA), Ambulance Responder (AR) or Ambulance Officer (AO) level.
When completing each module operational volunteers should remember to safely perform any set task or skill demonstration to the level within their scope of practice, to follow their specific Clinical Practice Protocols (CPPs) and comply with SAAS procedures.
This hard copy study guide is provided to assist volunteers with poor internet access or who desire a hard copy of information in addition to the eLearning modules. The online material is more comprehensive with the added advantage of embedded skills and real-life case videos, files and web links. Certain modules have short quizzes that must be completed online. Discuss with your RTL if this poses an issue for you. RTLs will be able to guide you on how to complete these on your own personal computer, SAAS station computer or SAAS issued iPad.
Reaccreditation
This is an annual process of completing skill and competency assessments, skills demonstrations, and declara- tions; to ensure all members retain full awareness and competency in the tasks and requirements of their assigned level of accreditation, and to prove their ability to perform work safely to the level of their accreditation. An opera- tional volunteer can only re-accredit at a level in which they have gained an initial accreditation. Re-accreditation contributes to the member’s efficiency status. If an operational volunteer is unable to complete the requirements of this Continuing Education Program (CEP), discuss your options with your RTL as this may result in restriction or removal of your Scope of Clinical Practice.
CEP Record Keeping
All volunteers should keep a copy of each individual modules certificate of completion, ideally, the Regional Team Leader (RTL) should keep a portfolio for each volunteer.
Note: Module completion certificates and any skill demonstrations/consolidations completed as part of face-to-face sessions do not need to be sent in, volunteers should keep them as a record of the training. Your RTL will complete a ‘Declaration of Evidence’ checklist on SAAS eLearning as each 2022 CEP topic has been completed.
Note: Volunteers and Regional Team Leaders should ensure that copies of the module completion certificates are kept.
6 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Continuing Education Program 2023 STUDY GUIDE
Reaccreditation YES YES YES Delirium OPTIONAL OPTIONAL YES
Infection Prevention and Control YES YES YES Mask Fit Check YES YES YES
OHCA Reaccreditation YES YES YES
Reconciliation Action Plan: Asking the Question YES YES YES
Scope of Clinical Practice
On completion of your relevant training program (qualification), SAAS will issue you with a Scope of Clinical Practice. There are multiple levels of credentialing within SAAS volunteer operations, these include:
• Ambulance Assist (AA)
• Ambulance Responder (AR)
• Ambulance Officer (AO)

• Ambulance Officer (Advanced Skills – Pain Management)

• Ambulance Officer (Extended Practice for Registered Health Professionals)
Each level within SAAS has a defined scope of practice. This scope of practice is defined through clinical documents such as policies, clinical practice protocols, clinical practice procedures and clinical communications. These documents are available on the SAAS Policy and Information Centre (SAASnet). A description of key relevant documents is provided below.
• SA Health Clinical Directives and Guidelines: Clinical policy directives and guidelines establish best practices across SA Health and assist practitioners and patients to determine appropriate health care for specific clinical circumstances. Clinical policy directives are mandatory requirements that are implemented across SA Health as ongoing operational practice, whether it is a short-term or permanent direction, and must be complied with. There is no scope to deviate from the specifications within clinical policy directives.
• SAAS Clinical Practice Protocols: These are documents that dictate the course of action that will be followed in a clinical situation. They set out a minimum level of treatment which ensures that th e majority of cases are handled in a standard manner.
• SAAS Clinical Practice Procedures: These documents provide guidance in the implementation of clinical skills including the application of clinical devices, use of equipment and approaches to clinical care. They are intended to demonstrate and promote best practices.
• SAAS Clinical Communications: Clinical Communications are issued when there is information or clarification that needs to be brought to the attention of the country and me tropolitan operations staff regarding a clinical practice issue.
Your clinical practice must be conducted within your scope of practice in accordance with established SAAS policies, procedures, pathways and protocols, using approved equipment and medications. SAAS staff are not permitted to conduct clinical practice outside their defined scope of practice unless specifically authorised to do so, this must only be done in consultation with a SA Ambulance Service Medical Officer. Where any variation to clinical practice has occurred, the case must be highlighted to your clinical supervisor, usually your Regional Team Leader (RTL), for review.
Providing Clinical Care When Off Duty
Off duty, SAAS staff are authorised to provide clinical care to their approved scope of clinical practice providing that they make their presence known to the ambulance service at the time (usually during the 000 calls). This must occur if intending to apply clinical judgement which may consist of advice and/or treatment. SAAS provides indemnity once notification occurs, staff are then covered as if they were on shift or duty within the jurisdictions of the service.
Examples of this situation include:
• Chancing across a vehicle crash while driving to work
• Assisting an injured player while watching your children’s sports team play
If notification is delayed it should be made as soon as possible to the State Duty Manager. Do not delay emergency treatment to initiate notification. Notification can be made by informing the EOC of your presence during the 000 calls or contacting the State Duty Manager directly.
This coverage and authorisation do not apply when the SAAS volunteer is acting in an official capacity for instance working or volunteering for another ambulance or medical provider (e.g. PTS, event or industrial company). In these circumstances, your practice and insurance are determined by the provider you are working for.these circumstances, your practice and insurance are determined by the provider you are working for.
Policy - Credentialling and Defining the Scope of Clinical Practice
7
OFFICIAL OFFICIAL Continuing Education Program 2023 STUDY GUIDE
Continuing Education Program 2023 - Jan 2023
Delirium
Learning Outcomes
• Recognising delirium
• Understanding the causes of delirium and risk factors
• Having an awareness of the paramedic/ICP 4AT Tool
Introduction
Delirium is a common and serious problem among acutely unwell persons. Delirium is linked to higher rates of mortality, institutionalisation and dementia and is generally underdiagnosed. While detection and management of delirium is traditionally a hospital-based entity, there may be a benefit in recognising delirium in an out-of-hospital environment and communicating this risk during the transfer of care.
Most delirium lasts a few days, but in some cases (around 20%) it lasts longer and can take weeks or even months to resolve. In some patients, there is only partial recovery and they do not return to their pre-delirium state.

People with delirium can present in different ways. The primary abnormality is inattention, ranging from being barely responsive to voice (severely reduced level of arousal), to being unable to engage in simple conversation and follow simple commands, to more subtle difficulties in maintaining focus over periods of 10-15 seconds.

8 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL <Section/Chapter Heading>
DELIRIUMCEP 2023
Delirium
People who can communicate when affected by delirium are usually confused and often show an impaired understanding of what is happening to them. They are often distressed and anxious. They may also believe that they are at personal risk, for example feeling that they have been imprisoned or that people who are offering assistance are trying to harm them. Visual hallucinations are also common and can be very frightening.
Some people with delirium can appear very restless and hyperactive. This is often a consequence of fear in that they feel unsafe and want to leave to reach a place of safety or to be with family.
During a period of delirium, the features can come and go (fluctuate). For example, a patient may be confused, disorientated and fearful at one point overnight but appear calmer and less confused hours later.

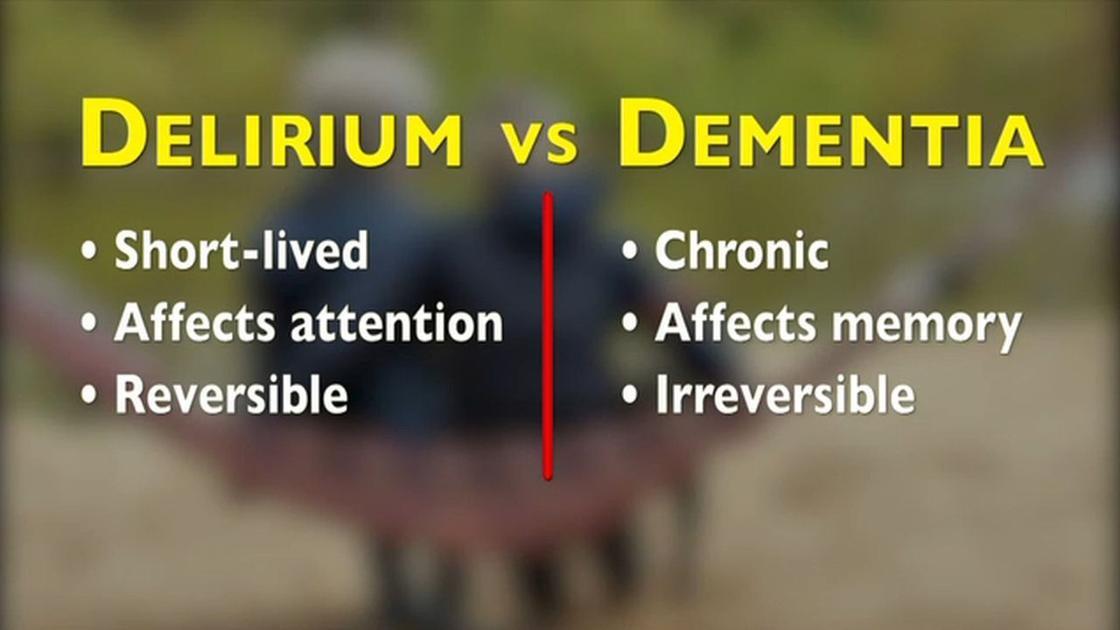
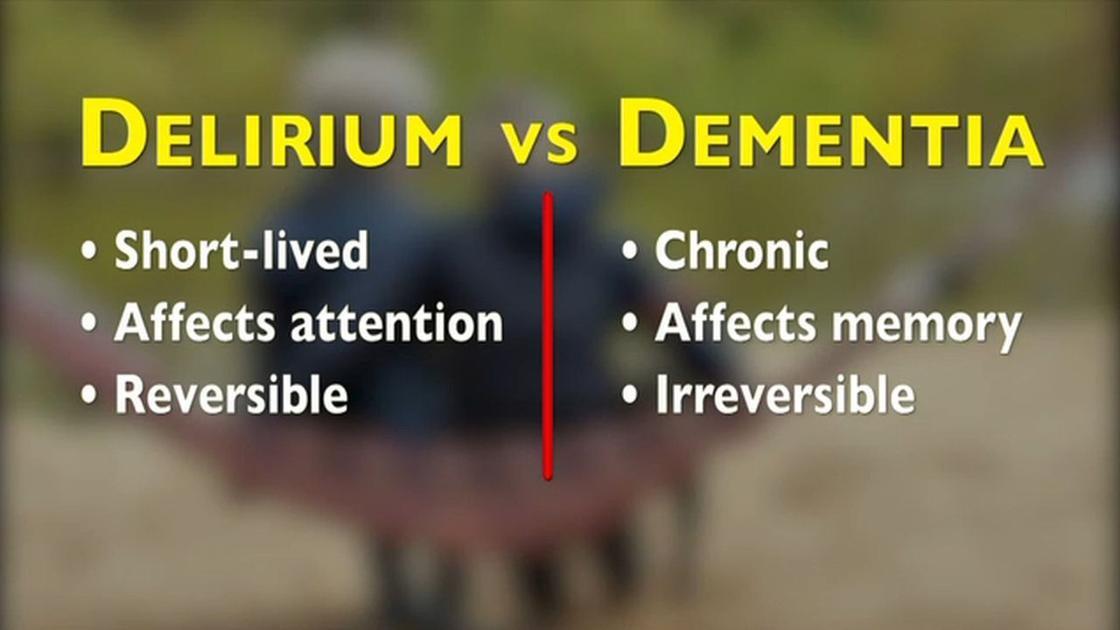
People with dementia have a higher risk of developing delirium. Dementia is different to delirium as it is typically caused by anatomical changes in the brain.

The differences between delirium and dementia are that dementia is a gradual onset, affects memory and is not reversible and usually progresses over time. In contrast, delirium develops rapidly, profoundly affects attention and is potentially reversible.

9 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL DELIRIUM - CEP 2023
Causes of Delirium
Delirium is caused by anything that can rapidly disrupt brain functioning. There is a long list of potential acute medical causes, including infections, trauma, surgery, constipation, drug side effects (e.g. opioids or benzodiazepines), and sudden drug withdrawal (e.g. antidepressants).

Physiological and metabolic changes happening simultaneously as acute illnesses such as hypoxia, hypercapnia, hypoglycaemia, high or low sodium, or high calcium can also directly cause delirium. Acute psychological stress caused by changes in environment, pain, discomfort, disorientation, fear, isolation, and sleep disruption, can also trigger delirium, particularly in patients with dementia.

Delirium - causes, symptoms, diagnosis, treatment & pathology [7:38 mins] https://www.youtube.com/watch?v=qmMYsVaZ0zo
Delirium Risk Factors
Although delirium can occur in any person, increasing age, dementia, frailty, multiple co-morbidities, and sensory impairments all increase the risk of delirium.
Delirium can occur as a result of predisposing risk factors such as severe medical illness or precipitating factors such as changes in the environment that can trigger the onset.
Predisposing Risk Factors:
• Age >65 (>45 for Aboriginal and or Torres Strait Islander people)
• Pre-existing dementia
• Severe medical Illness
• History of previous delirium
• Visual and hearing impairment
• Depression
• Abnormal sodium, potassium and glucose
• Polypharmacy
• Alcohol/ Benzodiazepine use
Precipitating Risk Factors
• Use of physical restraint
• Use of an indwelling catheter
• Altered or multiple medications

• Change in environment
• Pain
• Surgery
• Anaesthesia and hypoxia
• Malnutrition and dehydration
10 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL DELIRIUM - CEP 2023
Recognising Delirium
Signs and symptoms of delirium usually begin over a few hours or a few days. They often fluctuate throughout the day, and there may be periods of no symptoms. Symptoms can worsen during the night when it’s dark and things look less familiar.
Gathering a history from the patient’s family or carers who know the person is essential and should confirm that there is an acute change from the person’s usual mental state and behaviour.
Early identification and notification at the handover of patients at risk are important so that effective interventions can be put in place. Prompt diagnosis and timely treatment of underlying causes are important for reducing the severity and duration of delirium, and the risk of complications that arise from it(2).
A variety of screening tools are used in Emergency Departments and out-of-hospital settings to assist in the early detection and recognition of delirium
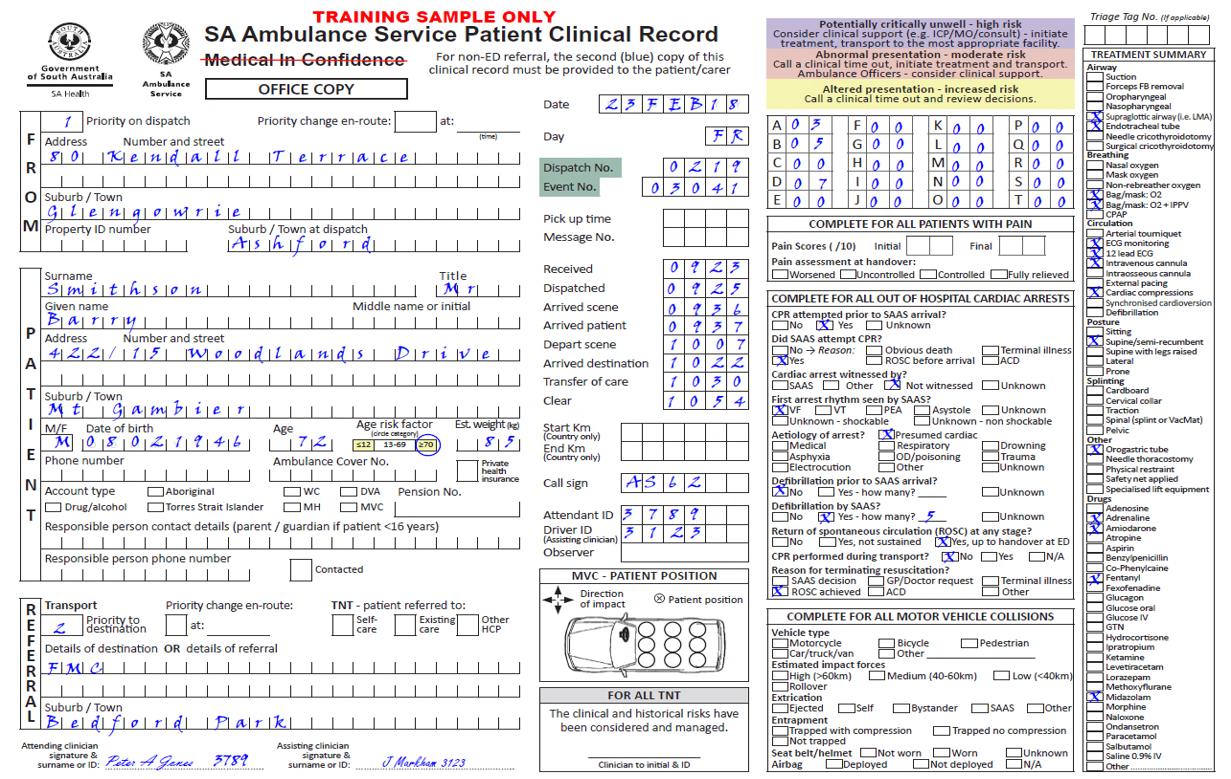
SAAS paramedics and ICPs will be implementing the use of the 4AT Rapid Clinical Test for Delirium in patients who are presenting with or at risk of developing delirium.
Ambulance Officers are not required to use this tool however it is good to have an overview of the assessment process that is undertaken. Below are the 4AT charts paramedics and ICPs use to assess the patient. The chart is available for use by paramedics and ICPs in the SAAS clinical app.


11 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL DELIRIUM - CEP 2023
Management of Delirium
If you suspect delirium during an episode of care several management options should be considered:
• Correct any underlying contributors or causes of delirium such as pain or hypoglycaemia.
• Ensure communication with the patient is suitable to their circumstance. Simple and direct questioning, explanation and instructions may be required.
• Ensure you have introduced yourself, talk slowly and calmly and ensure respectful non-threatening behaviours.
• People with delirium are often distressed. Look for signs of distress, ask if the patient has specific concerns and take opportunities to reduce distress.
• Reduce noise and environmental stimuli where possible.
• Ensure they have their glasses and hearing aids.
• Keep the patient informed, offer reassurance and involve family and carers in decisions and care where possible.
Summary
Delirium is often associated with poor patient outcomes and it is likely that the more severe and longer the episode of delirium, the poorer the outcome. It can have drastic short and long-term consequences for the person such as falls, a decline in their physical strength and function, early admission into residential care, increased healthcare utilisation and costs, and increased risk of death. Some people who have had delirium may never return to their former cognitive or functional capacity.
Traditionally delirium detection and management exist in a hospital-based environment. Recognising symptoms of delirium in a pre-hospital environment and communicating the information to the receiving hospital during the transfer of care may improve patient outcomes.

12 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL DELIRIUM - CEP 2023
Infection Prevention and Control
Introduction
Infection prevention and control (IPC) is a practical, evidence-based approach to preventing patients and health workers from being harmed by avoidable infections.
Effective IPC requires constant action at all levels of the health system, including policymakers, facility managers, health workers and those who access health services.
IPC is unique in the field of patient safety and quality of care, as it is universally relevant to every health worker and patient, at every health care interaction. Inadequate IPC practices can lead to serious adverse events for patients and sometimes death. Without effective IPC it is impossible to achieve quality health care delivery.
Learning Outcomes
By the end of this topic you will be able to:
• Follow standard and additional precautions for infection prevention and control
• Identify infection hazards and assess risks
• Follow procedures for managing risks associated with specific hazards
• Demonstrate an understanding of infection prevention and control policies and procedures
• Demonstrate correct hand hygiene processes
• Demonstrate the correct use of PPE supplied by SAAS for infection prevention and control
Infectious Disease
Infectious diseases are illnesses caused by an infectious agent. Infectious agents are microorganisms that cause communicable diseases. Most commonly these are bacteria, viruses, fungi, parasites, and prions.
Not all microorganisms cause disease or illness, many of them are beneficial (e.g. the bacteria found in the digestive system). A microorganism that causes disease is called a pathogen.
Some infectious diseases can be passed from person to person, some are transmitted by an insect to other animals, and you may get others by consuming contaminated food or water or being exposed to organisms in the environment.
Signs and symptoms vary depending on the organism causing the disease but often include fever and fatigue. Mild infections may respond to rest and over the counter medications from the pharmacy, while some life-threatening infections may need hospitalisation.
Chain of Infection

What will I learn about the Chain of Infection?
• Identify the process for the transmission of disease
• Have an understanding of the significance of microbes and the role they play in causing infection
• Describe the means by which the transmission of disease can be prevented
• Identify potential sources of infection and the appropriate measures to prevent the spread of infection
Certain conditions must be met in order for an infectious agent to be spread from person to person. This process, called the Chain of Infection, can only occur when all six links in the chain remain intact.
The Chain of Infection describes the process of infection which begins when an infectious agent leaves its reservoir through a portal of exit and is transmitted by a mode of transmission, entering through a portal of entry, to infect a susceptible host.
13
OFFICIAL OFFICIAL <Section/Chapter Heading> Infection Prevention and ControlCEP 2023
Continuing Education Program 2023 - Jan 2023
Your role is to know when to use the precautions described in this course to interrupt the chain and limit the spread of infection.
Infectious agent
There are different types of microorganisms. These microorganisms may be harmless, harmful or beneficial to their hosts. Harmful ones are also called pathogenic microorganisms. These microorganisms may cause kinds of communicable diseases by competing for metabolic resources, destroying cells or tissues, or secreting toxins.

Bacteria
Bacteria are single-celled microorganisms that can exist either as independent (free-living) organisms or as parasites (dependent on another organism for life). Bacteria reproduce rapidly by dividing themselves into two cells. Bacteria are found in every habitat including soil, rock and oceans. However, very few bacteria are pathogenic and cause disease, some contribute to normal body function like bacteria found within the digestive system.
The following are some examples of bacterial infections:


• Whooping cough
• Salmonella
• Tuberculosis

• Meningococcal disease

• Methicillin-resistant Staphylococcus aureus (MRSA)

• Vancomycin-Resistant Enterococci (VRE).
Fungi
Fungi are a wide variety of microorganisms that include mushrooms, moulds, yeasts and mildews. Fungi reproduce by releasing tiny spores into the air. Fungi can be found in soil, water, plants and in the human body.

Some common fungal infections include:
• Tinea (athletes foot)
• Ringworm
• Candidiasis (thrush).
Viruses
A virus is a microorganism that can only reproduce inside the cells of a host organism. Viruses cause disease by taking over and altering normal cell functions in the host. The type of cell the virus infects will determine the symptoms and the severity of the disease.

14 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Some common viral diseases are:
• Measles
• Chickenpox
• Human Immunodeficiency Virus
• Influenza
• Common cold
• Novel Respiratory Pathogens e.g. SARS, MERS
Parasites
Parasites are microorganisms that live (grow, feed, shelter) on another species known as the host. Parasites usually enter the body through the mouth by way of contaminated food or water and some live on the skin and hair.
Some common parasitic infections include:
• Threadworm
• Scabies
• Head lice

• Giardia lamblia Reservoir


The reservoir (source) is a host which allows the pathogen to live and multiply. Humans, animals and the environment can all be reservoirs for microorganisms.
Humans
There are two types of human reservoirs:

• Cases (persons with a symptomatic illness)
• Carriers
Carriers can be further defined as:
• Asymptomatic: An infected individual that shows no symptoms. Although unaffected they can transmit the disease to others.
• Symptomatic: This state may occur during the incubation period, convalescence and post-convalescence of an individual with a clinically recognised disease (e.g. influenza). An example of a human reservoir is a person with a common cold.
Animals
Animals can also be reservoirs; they can be carriers of diseases that can be passed on to humans. An example of an animal reservoir is a dog or monkey with rabies.
Environment
Reservoirs in the natural environment are contaminated water, soil or plants. This also includes food that has been contaminated.
Man-made reservoirs include objects and surfaces which have been contaminated.
Examples of an environmental reservoir are standing water infected with Legionnaire’s disease or soil contaminated with tetanus spores.
15 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Portal of exit
Portal of exit is the path by which a pathogen leaves its host. The portal of exit usually corresponds to the site where the pathogen is localized. For an organism to be transmitted from one person to another it must exit the reservoir (this applies only to human or animal reservoirs). The key portals of exit include:
• Respiratory tract (infected phlegm expelled through coughing)

• Gastro-intestinal tract (infected vomit or faeces)
• Skin lesions (infected blood or pus)
• Mucous membrane (nasal discharge)
Modes of transmission
The mode of transmission is the mechanism of transfer of an infectious agent from a reservoir to a susceptible host. The major modes of transmission include:
• Contact Direct Indirect
• Droplet and airborne
• Common vehicle
• Vector Contact transmission
Contact is the most common mode of transmission and usually involves transmission by touch or via contact with blood or body substances. Contact may be direct or indirect.
Direct contact transmission

Direct transmission occurs when infectious agents are transferred from one person to another, for example:
• Contact with infected body fluids (e.g. saliva, urine, faeces or blood), via cuts/abrasions or through mucous membranes of the mouth or eyes.
• Penetrating injuries, such as needle stick injuries.
• Contact with soil, vegetation or water that has been contaminated with an infectious agent.
Indirect contact
Indirect transmission involves the transfer of an infectious agent through a contaminated intermediate object or person, for example:
• A healthcare worker’s hands transmitting infectious agents after touching an infected body site on one patient and not performing proper hand hygiene before touching another patient, or
• A healthcare worker using fomites/equipment (e.g. BP cuff, stretchers, monitoring equipment) that has not been adequately cleaned and then used on another patient.
Droplet transmission
Droplet transmission can occur when an infected person coughs, sneezes or talks, and during certain procedures. Droplets are infectious particles larger than 5 microns in size
Respiratory droplets transmit infection when they travel directly from the respiratory tract of the infected person to susceptible mucosal surfaces (nasal, conjunctival or oral) of another person, generally over short distances. The droplet distribution is limited by the force of expulsion and gravity, it is usually no more than 1 metre.
Examples of infectious agents that are transmitted via droplets include influenza virus and Neisseria meningitidis (meningococcal infection), Pertussis (whooping cough).
16 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
2023
Infection Prevention and Control - CEP
Airborne transmission
Airborne transmission may occur via particles containing infectious agents that remain infective over time and distance. Small-particle aerosols (often smaller than 5 microns) are created during breathing, talking, coughing or sneezing and secondarily by evaporation of larger droplets in conditions of low humidity. Aerosols containing infectious agents can be dispersed over long distances by air currents (e.g. ventilation or air-conditioning systems) and inhaled by susceptible individuals who have not had any contact with the infectious person.
These small particles can transmit infection into the small airways of the respiratory tract. An example of infectious agents, primarily transmitted via the airborne route, are M. tuberculosis, chickenpox, and measles.
Common vehicles
Vehicles that may indirectly transmit an infectious agent include food, water, biological products (blood), and fomites (inanimate objects such as handkerchiefs, bedding, or surgical scalpels).
A vehicle may passively carry a pathogen:
• Food or water may carry the hepatitis A virus. Alternatively, the vehicle may provide an environment in which the agent grows, multiplies, or produces toxins.
• Improperly canned foods provide an environment that supports the production of botulinum toxin by Clostridium botulinum.
Vector transmission

Vector transmission occurs when an infectious agent is carried from a reservoir to a susceptible host by a living intermediary for example insects such as:
• Mosquitoes – malaria, Ross River, Dengue Fever, chikungunya fever, Zika virus fever, yellow fever, West Nile fever, Japanese encephalitis
• Tick – tick-borne encephalitis
Diseases transmitted by vectors are usually not directly transmitted between humans
Portal of entry
An agent enters a susceptible host through a portal of entry. The portal of entry provides a site for the agent to multiply or for a toxin to act.
Infectious agents can enter the body through:
• Inhalation (e.g. breathing in contaminated particles)
• Ingestion (e.g. eating contaminated food)
• Absorption (e.g. contaminated particles coming into contact with conjunctiva or eyes)
• Break in the skin (e.g. needle stick injury)
• Introduction by medical procedures (e.g. catheters, surgery)
Incubation
The incubation period is the time between the exposure to the pathogen, to the onset of signs or symptoms of the infectious disease. The length of the incubation period depends on:
• The portal of entry
• The rate of growth of the organism in the host
• The dosage of the infectious agent
• The host’s resistance
Some examples of incubation periods:
• Chickenpox: 10-21 days
• COVID-19: 1-14 days
• Tuberculosis: 4-12 weeks
• Salmonella: 6-72 hours
Continuing Education Program 2023 - Jan 2023
17
OFFICIAL OFFICIAL
Control - CEP 2023
Infection Prevention and
Colonisation, infection, and disease
Not all infectious agents cause infection or disease, they exist naturally everywhere in the environment.
For example, there is ‘good’ bacteria present in the body’s normal flora
Parasites, prions and several classes of microorganisms, including bacteria, viruses, fungi and protozoa, can be involved in either colonisation or infection, depending on the susceptibility of the host.
• With colonisation, there is a sustained presence of replicating infectious agents on or in the body, without caus ing infection or disease.
• With infection, invasion of infectious agents into the body results in an immune response, with or without the symptomatic disease.
Susceptible host
A susceptible host is required for a pathogen to cause an infection. A person lacking effective resistance to a particular pathogen is susceptible to those organisms. This ineffective immune system leaves people vulnerable to infectious agents. Characteristics that influence susceptibility and the severity of the infection include:
• Gender
• Ethnicity
• Socioeconomic status
• Marital status
• Medications (e.g. immunosuppressants taken after an organ transplant)
• Trauma
• Antibodies (active and passive immunity)
• Medical conditions (e.g. comorbid conditions)
• Heredity
• Occupation
• Balance of the body’s normal flora
• Natural barriers (e.g. people with open wounds)
Healthcare-Associated Infections (HAIs)
Healthcare-associated infections (HAIs) are those infections that are acquired as a direct or indirect result of healthcare. Healthcare-associated infections are one of the most common complications affecting patients in the hospital. As well as causing unnecessary pain and suffering for patients and their families, an HAI can prolong a patient’s hospital stay and add considerably to the cost of delivering health care.
An HAI can occur in any healthcare setting: hospitals, office-based practices (e.g. general practice clinics, dental clinics, community health facilities), the setting in which paramedics work and long-term care facilities. This means that any person working in or entering a healthcare facility is at risk of an HAI.
The good news is that HAIs ARE potentially preventable.
It is possible to significantly reduce the number of HAIs by:
• Putting in place appropriate infection prevention and control measures to prevent people from getting an HAI, and
• Undertaking HAI surveillance to identify what can be done to improve clinical practice to reduce the risk of HAI acquisition.
Breaking the chain of infection
Breaking just one link in the chain of infection means that communicable diseases cannot be passed on to another individual. Transmission may be interrupted when:
• The infectious agent is eliminated, inactivated or cannot exit the reservoir.
18 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Infection Prevention and Control - CEP 2023
• The portals of exit are contained through safe infection control practices.
• The transmission between objects or people does not occur due to barriers and safe infection control practices.
• The portals or entry are protected.
Infection Prevention and Control
Infection prevention and control is achieved by following the principles and processes of the SAAS infection control program, which covers the following:
• Standard precautions
• Transmission-based precautions
• Immunisations
• Management of occupational risk and exposure
Standard Precautions
All people potentially harbour infectious agents. Standard precautions refer to those work practices that are applied to everyone, regardless of their perceived or confirmed infectious status and ensures a basic level of infection prevention and control.
Implementing standard precautions as a first-line approach to infection prevention and control in the healthcare environment minimises the risk of transmission of infectious agents from person to person, even in high-risk situations.

If these precautions are not followed, patients are at an increased risk of acquiring an infection.
Standard Precautions include:
• Hand hygiene and care
• Respiratory hygiene and cough etiquette
• Using personal protective equipment (PPE)

• Environmental controls e.g. routine and scheduled cleaning, spills management
• Aseptic technique
• Reprocessing of reusable equipment and instruments
• Safe handling and disposal of sharps
• Appropriate handling of waste and linen
If these precautions are not followed, patients are at an increased risk of acquiring an infection.
Hand Hygiene
Effective hand hygiene is the single most important strategy in preventing healthcare-associated infections (HAIs). Ease of access to hand washing facilities (soap and water) and alcohol-based hand rubs can influence the transmission of HAIs. Washing hands with soap and water is required if hands are visibly soiled while either product can be used if hands are visibly clean.
Microorganisms present on the hands most of the time are known as resident flora. Microorganisms that are picked up on hands during activities involved in providing healthcare are known as transient flora. Transient flora are usually associated with HAIs, they are easily picked up and easily transferred to others. They are often involved in outbreaks of multi-resistant organisms e.g. MRSA, VRE. They are easily removed with hand hygiene.
19 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
- CEP 2023
Infection Prevention and Control
As it is possible that you may be washing your hands multiple times in a day it is possible that this can cause dry and chapped skin. An appropriate lotion should be used to replace natural oils.
It is important to also inspect your hands regularly for signs of cuts, infections or dermatitis. Persistent skin problems and suspected latex allergies should be reported to a medical practitioner.
5 Moments Hand Hygiene

The ‘5 moments for hand hygiene’ was developed by the World Health Organization and has been adopted by Hand Hygiene Australia and then taken on by National Hand Hygiene Imitative, it:
• Protects patients against acquiring infectious agents from the hands of the healthcare worker
• Helps to protect patients from infectious agents (including their own) entering their bodies during procedures
• Protects healthcare workers and the healthcare surroundings from acquiring patients’ infectious agents.
Moment 1: BEFORE touching the patient in any way.

On entering the patient zone/house/environment, immediately before touching the patient e.g. before the non invasive examination, assisting to move, applying monitoring equipment.
Moment 2: Immediately BEFORE an invasive high-risk procedure.
Once hand hygiene (HH) has been performed, nothing else in the patient zone should be touched e.g. insertion of a needle into a patient’s skin, preparing and administering medications via invasive devices, any assessment, treatment and patient care where contact is made with non-intact skin.
Moment 3: AFTER a procedure or Body Fluid Exposure.
Even if you have gloves on, you should remove gloves and perform HH after invasive procedures (see Moment 2) e.g. contact with urine bottle, sputum via tissues, contact with blood, saliva, mucous, urine, faeces etc.
Moment 4: AFTER touching the patient.
Perform hand hygiene before moving from patient zone to work from a clean HCW zone e.g. after touching a patient in an ambulance you need to perform hand hygiene to access equipment drawers and cupboards, or to drive the vehicle. When pushing a stretcher into a hospital, as soon as you leave the patient you need to perform hand hygiene before touching anything else.
Moment 5: AFTER touching the patient’s surroundings (home, office, hospital).
Immediately after touching the patient surroundings even if you didn’t touch the patient, e.g. after entering the patient’s house and touching anything in the house.
Hand Washing
Hand washing refers to the appropriate use of non-antimicrobial soap and water on the surface of the hands. Plain soaps act by the mechanical removal of microorganisms and have no antimicrobial activity. They are sufficient for general social contact and for cleansing of visibly soiled hands. They are also used for the mechanical removal of certain organisms such as C. difficile and norovirus. Hands need to be dried thoroughly. This should be accomplished using a good quality paper towel or air hand driers. The use of cloth or fabric towels can also be a source for cross-contamination.
20 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Other times to perform hand hygiene starting and leaving work, before eating or handling food, after going to the toilet.
How to wash your hands
The following hand washing steps for both soap/water and alcohol hand gels will ensure that your hands are as clean as possible.


Alcohol-based Hand Rub (ABHR)

Research has demonstrated that alcohol-based ABHR is better than traditional soap and water because they:
• Result in a significantly greater reduction in bacterial numbers than soap and water in many clinical situations, (see Figure 3.2 below).
• Require less time than hand washing.
• Are gentler on the skin and cause less skin irritation and dryness than frequent soap and water washes, since all hand rubs contain skin emollients (moisturisers).
• Can be made readily accessible to healthcare workers e.g. emergency vehicles with no access to soap and water.
• Are more cost-effective.
Soap and water wash is required if hands are visibly soiled, and either product can be used if hands are visibly clean. Neutral hand-wipe products may be considered in instances where hygienic access to soap and water is not readily available, such as in community care settings, patient homes.
There is no maximum number of times that ABHR can be used before hands need to be washed with soap and water.
How to apply Alcohol-Based Hand Rub
Apply enough ABHR to your hands to cover all surfaces, 1-2 pumps of a dispenser similar to a 10 - 20 cent piece. Rub hands together covering all surfaces for 20 seconds or until the ABHR has evaporated.
21 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Surgical hand wash
The process of eliminating transient and reducing resident flora prior to surgery. This comprises removal of hand jewellery, performing hand hygiene with liquid soap if hands are visibly soiled, removing debris from underneath fingernails and scrubbing hands and forearms using a suitable antimicrobial formulation.
At SAAS surgical hand scrubs are performed by Extended Care Paramedics (ECPs) and Retrieval, Rescue and Aviation Services (RRAS), prior to insertion of invasive devices.




Principles of effective hand hygiene
Hand hygiene consists of more than just hand washing, it also includes the following:
• Removing all hand and arm jewellery as they can harbour organisms and spread disease, scratch the client or pierce the gloves.
• Cover all cuts, abrasions and lesions with waterproof tape or spray on dressings which act as a barrier to spreading organisms from the health care worker to the client and vice versa.
• When washing hands, avoid splashing water on your clothing. Keep your hands and uniform away from the surface of the sink and do not lean against the sink.
Procedures – Hand Hygiene [PRO-045]
Respiratory hygiene and cough etiquette
Respiratory hygiene and cough etiquette must be applied as a standard infection control precaution at all times.
Covering sneezes and coughs prevents infected persons from dispersing respiratory secretions into the air. Good respiratory hygiene can help prevent the spread of infections such as colds and influenza.
Covering your sneezes and coughs prevents infectious people from dispersing respiratory droplets into the air.
Key things staff should do:
1. Put a surgical mask on the patient (if tolerated).
2. Cover your mouth and nose with disposable tissues when coughing sneezing, wiping and blowing noses.
3. If no tissues are available cough into your elbow.

4. Dispose of used tissue in the nearest bin.
Healthcare workers with viral respiratory tract infections should remain at home until their symptoms have resolved.
Procedure – Respiratory Hygiene and Cough Etiquette [PRO-250]
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) refers to a variety of barriers, used alone or in combination, to protect mucous membranes, airways, skin and clothing from contact with infectious agents. PPE may include aprons, gowns, gloves, surgical masks, protective eyewear and face shields or a combination of several of these items.
22 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
The selection of PPE must be based on an assessment of the risk of transmission of infectious agents to the patient or HCW and the risk of contamination of the clothing or skin of healthcare workers or other staff by patients’ blood, body substances, secretions or excretions.
SA Health Policy Guideline - Personal Protective Equipment (PPE) Selection
The following roles and responsibilities are specific to PPE, all SAAS workers will take reasonable care to:
• Ensure their own health, safety and well-being in the workplace
• Wear and maintain PPE provided when undertaking exposure-prone procedures
• Attend PPE training including donning and doffing
• Comply with any reasonable instruction, training and safe work procedure when required to use PPE within the workplace
• Use PPE in accordance with policies, procedures and guidelines
• Do not intentionally misuse or damage PPE
• Maintain and clean (where required) PPE in accordance with manufacturer’s instructions and local procedures
• Report all incidents of PPE failure and breaches on the Safety Learning System (SLS)
• Notify line managers if PPE is found to be unsuitable for use e.g. does not fit correctly or you have an adverse reaction using it
• Report any faults, difficulties, damage, defect or need to clean or decontaminate associated with the PPE
Gloves
When used appropriately, gloves can protect both patients and healthcare workers from exposure to potentially infectious microorganisms. They do not need to be worn for most routine patient care of non-infectious patients, and they never replace the need for hand hygiene.
It is recommended that:
• Gloves must be worn as a single-use item for each invasive procedure, contact with non-intact skin, mucous membranes or sterile sites and if the activity has been assessed as being an exposure risk to blood and bodily fluids.
• Gloves must be removed, and hand hygiene performed before leaving a patient’s room or area.
• Single-use disposable gloves must not be reused i.e. washed or alcohol-based hand rub applied for subsequent reuse.
• Single-use disposable gloves must be changed: Between episodes of care for different patients.
Between each episode of clinical care on the same patient to prevent cross-contamination of body sites (e.g. mouth care followed by wound care).

When the integrity of the glove has been compromised e.g. ripped or torn.
• Single-use disposable sterile gloves must be worn during contact with sterile sites:
Procedures requiring aseptic technique where key parts and/or sites are touched directly (e.g. when a non-touch technique cannot be achieved).
• Care should be taken when removing and disposing of gloves to not contaminate the hands after gloves are removed and hand hygiene is performed in accordance with SA Health Hand Hygiene Policy Directive.
• Gloves should be discarded into a designated container for waste to contain the contamination.
Continuing Education Program 2023 - Jan 2023

23
OFFICIAL OFFICIAL
- CEP 2023
Infection Prevention and Control
Safe glove removal
Gloves should be removed, and hand hygiene performed:
• Prior to use of any electronic equipment (i.e. computer keyboard) or non-disposable items (e.g. pens, paperwork, folders).

• Prior to entering a hospital or facility. This is to reduce the spread of organisms between the patient’s environment, the ambulance and the receiving hospital. If required, a new set of gloves can be put on once inside the hospital.
Sterile gloves
Sterile gloves should be worn when there is contact with normally sterile sites or clinical devices where sterile or aseptic conditions must be maintained e.g. urinary catheterisation, complex dressings, central venous catheter insertion.

Single-use disposable sterile gloves must be worn during contact with sterile sites:
• Procedures requiring aseptic technique where key parts and/or sites are touched directly (e.g. when a non-touch technique cannot be achieved).
Refer to the Personal Protective Equipment procedure for donning and doffing gloves technique.
Procedure – Personal Protective Equipment [PRO-249]
Aprons and gowns for infection prevention
Protective clothing (aprons or gowns) are recommended to be worn by all workers when:
• There is a risk of exposure to blood, body substances, secretions or excretions (excluding sweat).
• There is anticipated close contact with the patient, materials or equipment which may lead to contamination of the skin, uniforms or clothing with infectious microorganisms.
• To protect the patient from contact with potentially contaminated uniforms or clothing (e.g. immunosuppressed patients).

SAAS provides a variety of Level 3 isolation gowns that provide protection against moderate fluid exposures e.g. arterial blood splatter, trauma and aerosol generating procedures. Long sleeve isolation gowns should:
• Fully cover the torso and neck to knees,
• Fully cover the arms to the end of the wrist and
• Wrap around the back
24 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Control - CEP 2023
Infection Prevention and
Masks
Surgical masks
Single use face masks are not classified as respiratory protective equipment, but do provide a barrier to splashes and droplets impacting the wearer’s nose, mouth and respiratory tract. Wearing a correctly fitted surgical mask for cough etiquette (source control) reduces the number of droplets and aerosolised particles dispersed into the air.

A surgical mask and protective eyewear or face shield must be worn if:
• There is the potential for the generation of splashes or sprays of blood and body substances into the face and eyes.
• The patient is known or suspected to be infected with microorganisms transmitted by respiratory droplets e.g. influenza, meningococcal.
Particulate Filtration Respirator (PFR)
Particulate Filtration Respirator (PFR) e.g. N95, D95 or P2 are used as respiratory protection to prevent inhalation and contact with:
• Infectious pathogens transmissible by the airborne route
• When performing aerosol-generating procedures, or
• For pathogens where the transmission route is uncertain e.g. novel respirator pathogens
Particulate filter respirators (PFR) are designed to be tight-fitting. Staff must be fit tested to a PFR mask before they can start wearing them. If air leaks around the PFR edges the wearer will not achieve the level of protection needed to protect their health.
Facial hair and facial piercings must not interfere with the safe use of a PFR. Workers who have facial hair (including a 1–2 day beard growth/stubble) must be aware that an adequate seal cannot be guaranteed between the respirator and the wearer’s face.

A correctly fitted P2/N95 respirator must be used when:
• Attending to patients with confirmed or suspected serious diseases transmitted by the airborne route (e.g. measles, chickenpox or active pulmonary tuberculosis).
• When performing high-risk aerosol-generating procedures such as CPR, intubation on patients with a confirmed airborne disease or whose infectious status is unknown or unconfirmed.
• Novel respiratory pathogens where the route of transmission is unknown.
Guidelines for mask wearing
When wearing a mask the following should be considered:
• For a surgical masks ensure, the ties are secured and the mask fits comfortably.
• Ensure they are secured over the mouth, nose and chin.
• Perform a fit check if using a PFR.
• Do not touch the outer surface of the mask when removing it, use the straps.
• Once the mask has been removed and disposed of, wash hands thoroughly.
Continuing Education Program 2023 - Jan 2023
25
OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Eye and face protection (safety glasses and face shields)


Goggles and safety glasses prevent injury to the eyes. Face shields and visors prevent injury to eyes, nose and mouth from hazards including dust, flying particles, chemicals, and potentially infectious blood or body fluids.
Normal prescription glasses DO NOT provide adequate protection. Workers requiring reading glasses should seek additional eye protection which does not interfere with the worker’s vision yet provides an appropriate barrier to hazards.
Workers must wear protective eyewear for any procedure when they may be exposed to hazards or hazardous situations, or where stated in the safe work procedure.
Protective eyewear should be worn when there is the potential for splashing, splattering or spraying of blood and other body fluids. Protective safety glasses should also be worn during cleaning procedures.
Glasses should provide clear vision and be distortion and fog-free. They should be close fitting and shielded at the sides. Safety glasses should be removed by the arms.
Sequence for putting on and removing PPE
To reduce the risk of transmission of infectious agents, PPE must be used appropriately. The following poster outlines sequences and procedures for putting on and removing PPE.

26 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
Routine and Scheduled Cleaning
Infectious agents can be widely found in pre-hospital setting. Transmission of infectious agents from the environment to patients may occur through direct contact with contaminated equipment, or indirectly, for example, via hands that are in contact with contaminated equipment or the environment and then touch a patient.
Cleaning is a process which intends to remove foreign material (e.g. dust, soil, blood, secretions, excretions and micro-organisms) from a surface or an object using water, detergent and mechanical action/ friction. Although cleaning is known to successfully reduce the microbial load on surfaces there are some circumstances where disinfection is also required to be performed.
Disinfection is a process that eliminates many or all micro-organisms except bacterial spores. Disinfection is necessary when body fluids are spilled, when a multi-resistant organisms (MRO) is present or there is an outbreak of an infection. Cleaning of ambulance interiors, ambulance equipment, office environments or stations should be done routinely and anytime they become soiled with dirt or debris. It is an essential part of the standard precautions in infection control.
Therefore keeping the ambulance clean is an important part of infection prevention and should be done in accordance with the Routine Cleaning and the Scheduled Cleaning procedures.
Procedure – Scheduled Cleaning [PRO-252]
Procedure – Routine cleaning [PRO-118]
Ambulance interior and equipment
High-touch areas in ambulances and shared patient equipment are considered high risk and should have a high frequency of clean. This is the responsibility of operational staff after each patient, refer to the Routine Cleaning Procedure.
Low-touch surfaces such as floor, walls, steering wheel, locker doors, etc., in ambulances and light fleet, are considered a moderate risk and should have a frequent scheduled clean. This is the responsibility of operational staff using the vehicles and should occur once per shift whenever operationally possible.
Spot cleaning of surfaces that are visibly soiled should be completed as required by staff using the vehicles.
Fleet Cleaning and Stock Expiry Register





27 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention
Control - CEP 2023
Infection
and
Level 1 clean – standard precaution (after every patient)

Cleaning of all high touch surfaces, all equipment which has had a direct or indirect patient or clinician contact or any surface/item that is visibly soiled must occur after each patient attended.
High touch surfaces and equipment includes ambulance grab rails, handles, drawers, stretcher mattress, belts, handles and rails, response kits, ECG monitor, ECG leads, pulse oximetry probe, BP cuff.
Use appropriate standard precaution PPE as required:
• Detergent and water are adequate for a level 1 routine clean:
Use buckets and mops designated for ambulance cleaning.
With clean disposable cloths, mop and the detergent solution (diluted to the manufacturer’s instructions, wipe/ mop over surfaces and equipment:
○ Empty buckets after use, rinse with a fresh detergent solution and store upside down to allow for draining and drying.
○ Dispose of cloths after use.
○
Rinse mop after use and store upside down to allow for draining and drying. Mop heads should be replaced regularly and when visibly soiled.
• Where this is not practical, all-in-one detergent/disinfectant wipes (e.g. Clinell® wipes) are a suitable alternative:
Use more than one wipe for larger surface areas; sufficient to ensure the whole surface is wet (e.g. 4 to 6 wipes may be required to clean a stretcher).
Allow the surfaces to air dry.
• Alcohol based wipes (e.g. Isowipes®) can be used for cleaning electronic equipment and screens.
Disinfectant wipes (e.g. Clinell®) and alcohol wipes (e.g. Isowipes®) should be available at all ambulance stations and in all ambulances.
Use detergent and water with disposable cloths and bucket and/or mop and bucket (as described in section 3.1 of the Routine Cleaning Procedure) for grossly soiled surfaces that are too large to be managed with detergent/disinfectant wipes, such as the ambulance floor.
For re-usable ambulance items that are grossly soiled or require specialised cleaning, refer to the following procedure.
Procedure – Reprocessing of Used or Soiled Ambulance Equipment [PRO-112]

28 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
Level 2 decontamination – after a patient with transmission-based precautions (contact or droplet)
In addition to a level 1 clean, all surfaces and equipment that have been in contact with a patient requiring transmission-based precautions or indirectly via the clinician must be cleaned with a disinfectant.
A disinfectant is a chemical agent that rapidly kills or inactivates most infectious agents. Disinfectants are not to be used as general cleaning agents, unless combined with a detergent, as a combination cleaning agent (detergent disinfectant).
Where a 2 in 1 detergent and disinfectant has been used, (e.g. Actichlor Plus or Clinell wipes in the level 1 clean), there is no need to repeat, as the decontamination step has already been completed. Use appropriate transmission based precaution PPE as required.
Procedure - COVID-19 Clean using Actichlor Plus Actichlor Plus solution must be prepared with a ratio of 1 tablet to 1 litre of cool water to ensure 1000ppm concentration.
Product Type of Product Dilution Concentration

Actichlor Plus Neutral Detergent AND TGA approved disinfectant

1 tablet (1.7g) dissolved 1 litre water cool/cold water 1000 ppm
Ensure any exposed linen not stored in the overhead locker is disposed of in a linen skip.
Remove any rubbish and empty rubbish bins.
Clean all vehicle surfaces and equipment with the following:
• USE Clinell wipes for equipment (ECG cable, BP cuffs, stethoscopes, etc.)
• USE Actichlor Plus on all other surfaces and larger equipment (stretcher, walls, floor, ceiling and driver/ passenger foot well etc.)
• USE 70% Isopropyl Alcohol wipes for sensitive medical equipment (ECG electrode, MDT/Monitor screens).
Allow all surfaces to dry or, dry electronic equipment with a clean dry cloth, if required.
Empty bucket(s) after use, rinse with clean water or solution and store upside down to allow draining and drying. Dispose of cloth(s) and/or mop head after use.
Spills of Actichlor Plus or bleach
Contain any bleach solution spills with disposable cloths. If unprotected skin or eyes become contaminated, wash with copious amounts of water and seek assistance.
For reusable ambulance items that are grossly soiled or require specialised cleaning, refer to the following procedure.

Procedure – Reprocessing of Used or Soiled Ambulance Equipment [PRO-112]
Level 3 air – after a patient with transmission-based precautions (airborne)
In addition to a level 1 and level 2 clean, air the ambulance and equipment by leaving all doors open and equipment exposed to air for 10 minutes.
Scheduled cleaning of ambulance vehicles
Scheduled three monthly cleaning of metropolitan ambulances (stretcher carrying vehicles) and stretchers is managed by SAAS Fleet Services. Scheduled cleaning of country ambulances will occur as per local arrangements.
Continuing Education Program 2023 - Jan 2023
29
OFFICIAL OFFICIAL
CEP 2023
Infection Prevention and Control -
Ambulance Stations

Ambulance station sluice rooms or equipment reprocessing areas are considered moderate risk and should have a frequent clean. All other areas of ambulance stations are considered low risk and should have a regular scheduled clean.
Routine cleaning
Staff on shift/on station are responsible for:
• Maintaining all station areas free from clutter to not inhibit any external providers from performing contracted cleaning.
• Ensure refrigerators, freezers, kitchens, storage rooms, and personal areas such as lockers, drawers, and cupboards are maintained in a manner that does not put the health and safety of others at risk.
• Wiping benches, storage containers and spaces in clinical areas (clinical storerooms and sluice rooms) and mop floors with detergent and water.
Scheduled cleaning
Scheduled cleaning of ambulance stations is managed by SAAS Building Services, who will inform the relevant workgroup or worksite regional Operations Manager when and what type of cleaning is scheduled.
• Managers should ensure any staff who have known allergies or reactions to scheduled cleaning are accommodated at an alternative worksite for an appropriate pre-determined exclusion period.
Spot cleaning of surfaces that are visibly soiled should be completed as required by staff using the area.
All staff will be required to ensure the station area is tidy and free from obstruction in time to allow access for any scheduled cleaning to occur.
It is the responsibility of staff to ensure any outside facilities e.g. sheds or alfresco common areas are maintained in a manner that does not present a risk of health or safety to others.
Office Environments
SAAS office/administration areas are considered low risk as there is minimal patient contact or indirect patient contact. There is still a risk that infectious agents causing common illnesses can spread easily in a workplace if routine cleaning is not done.
Routine cleaning
Staff are responsible for:
• Regular hand hygiene, particularly after a break away from their workstation.
• Cleaning their workstations, particular attention needs to be paid to ‘hot desks’, which should be cleaned prior to and after each use using all-in-one detergent/disinfectant wipes.
• Cleaning of electronic equipment, with particular attention to telephones and computer keyboards and mice using alcohol wipes at the start of every day/shift.
• Maintaining the office area free from clutter so as to not inhibit any external providers from performing contractual cleaning.
• Ensuring refrigerators, freezers, kitchen, storage rooms, and personal areas such as lockers, drawers and cupboards are maintained in a manner that does not put the health and safety of others at risk.
Scheduled cleaning
Scheduled cleaning of office environments is managed by SAAS Building Services, who will inform the relevant workgroup when and what type of cleaning is scheduled.
Managing a blood or body fluid spill
For all body fluid spills the following process must be followed:
• Don appropriate PPE including eye protection and gowns.
• Contain the fluid using hand towels or blankets.
30 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
• As soon as practicable soak up as much of the fluid as possible using absorbent disposable material and dispose of in a medical waste bin.
• Clean the area with detergent and warm water.
• Remove all visible signs of the spill. This may require more than one attempt, changing the water and cleaning material often.
• Wipe a large spill with bleach after cleaning and drying using 25ml of bleach per 1 Litre of water or Actichlor Plus.
Cleaning equipment
Most cleaning procedures require the use of some equipment including spray bottles, cloths, sponges, mops and buckets.
The following guidelines should be followed when using cleaning equipment:
• Cleaning cloths should be disposable.
• Mops and buckets must be cleaned with detergent and warm water after use and then stored upside down to dry.
• Refillable spray bottles must be cleaned and dried thoroughly before re-use. Bleach solutions should NOT be put in spray bottles.
Cleaning equipment should always be stored in a manner that ensures a safe work environment and should be put away in a way that minimises the risk of injury.
Re-processing of equipment
All ambulance equipment can be sorted into three categories relating to the level of risk it poses. The categories are:

• Critical items which enter or penetrate into tissue, a body cavity or the bloodstream.
• Semi-critical items which have contact with intact mucous membranes or non-intact skin.
• Non-critical items are those which have contact with intact skin only.
In SAAS, all critical and semi-critical items, are single patient use only. They are marked with the following symbol or the words ‘single-use only’ printed on them. These must be disposed of in an appropriate receptacle after single use or single patient use. The reuse of single-use items is not approved by SAAS and is regulated by the Therapeutic Goods Administration (TGA).


The level of reprocessing required for non-critical items depends on the item, its intended use, manufacturer’s instructions and SAAS procedures. After use on a patient, any reusable medical equipment must not be used for the care of another patient until it has been cleaned and reprocessed appropriately.
Cleaning reusable items is the first step and should occur as soon as practicable. This should be done in accordance with the ‘Level 1 Clean’ as detailed in the Routine Cleaning Procedure.
If the equipment has been exposed to a known or suspected multi-resistant organism (MRO) or other infectious agents requiring contact, droplet or airborne transmission based precautions, the cleaning step should be followed by a disinfection step. This should be completed in accordance with the ‘Level 2 Decontamination’ steps in the Routine Cleaning Procedure.
Items that have been heavily soiled may require specialised cleaning (e.g. Posey Restraint Net). This should be done in accordance with the Reprocessing of Used or Soiled Ambulance Equipment Procedure.Uniforms, stretchers and ambulance interiors which are grossly soiled should be managed according to the Reprocessing of Used Soiled Ambulance Equipment Procedure.
Procedure – Reprocessing of Used or Soiled Ambulance Equipment [PRO-112]
Procedure – Soiled and/or Broken Ambulance Stretchers [PRO-258]
Continuing Education Program 2023 - Jan 2023
31
OFFICIAL OFFICIAL
Control - CEP 2023
Infection Prevention and
Safe handling and disposal of sharps waste and linen
The safe handling of sharps, waste and linen is essential to protect you, your work colleagues and patients. This procedure outlines safe work practices for the handling and disposal of sharps, waste and linen.
Safe handling and disposal of sharps

It is important that all staff are aware of the inherent risk of injury associated with the use of sharps such as needles, scalpels and lancets. When handling sharps the following principles apply:
• The person using the sharp is responsible for its safe disposal
• Dispose of the sharp immediately following its use and at the point of care
• Dispose of all sharps in designated puncture resistant containers that conform to relevant Australian Standards (AS/NZS 4261:1994 reusable; AS 4031:1992 non-reusable)
• Dispose of sharps disposal containers when they are ¾ full or reach the specified fill line, seal appropriately and place in the clinical waste stream
• Never pass sharps by hand between health care workers
• Never recap used needles unless an approved recapping device is used
• Never bend, break or otherwise manipulate by hand a needle from a syringe
Linen management
The correct handling of linen is vital, it can be contaminated with blood and any other body fluids as well as through improper handling and storage.
Clean linen does not need to be sterile (free from all microbes), but correct handling will prevent the growth of micro organisms that can develop under poor conditions.
Clean linen
Clean linen must be stored in a clean dry place that prevents contamination by aerosols, dust, moisture and vermin. It should be transported and stored separately from soiled lined. Clean linen should only be handled by staff who have used proper hand hygiene procedures.
Clean linen in Ambulances should be re-stocked with supplies at metropolitan public emergency departments and most ambulance stations, or as per local arrangements.
Soiled linen
All used linen should be handled with care to avoid dispersal of microorganisms into the environment and to avoid contact with staff clothing. The following principles apply for linen used by all patients regardless of their infectious status:
• All used linen is considered contaminated therefore minimal handling is recommended
• Appropriate PPE must be worn during the handling of soiled linen to prevent skin and mucous membrane exposure to blood and body fluids
• Dispose of all linen into an appropriate linen container at the point of care
• Linen which is heavily contaminated with blood and/or other body fluids which could leak must be contained by a leak-proof bag and secured prior to transport
• Hand hygiene must be performed following the handling of all used linen.
• Placed in linen bags which are no more then three-quarters full. Once a linen bag is three-quarters full the top should be tied.
• Collected by a contractor or taken to a contractor and laundered as per SA Health standards.

Hand hygiene must be performed following the handling of any used linen.
Linen is not to be rinsed or sorted by SAAS staff once used and must NOT to be washed in a domestic washing machine.
32 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Safe Handling and Disposal of Waste
General Waste
• General waste is waste which is not recycled or reused and does not pose a threat or risk to public health or safety and meets landfill acceptance criteria. This may include PPE or other items that have been risk assessed as not visibly contaminated by gross amounts of blood and/or body fluids. Materials that are only stained can be disposed of in general waste.
• When the bin is three quarters full, it should be “tied-off” to prevent spillage of the contents for collection and disposal. This waste should NOT go into the recycling bin.
• Hand hygiene must be performed after handling or transporting waste bags or bins (regardless of glove use).
• If in doubt when assessing the level of contamination and/or the required waste stream, default to the medical (clinical) waste streams.
Medical (Clinical) Waste
• Medical waste is defined as waste consisting of all sharps, human tissue including bone, any liquid body fluid, and laboratory specimens. This may include personal protective equipment (PPE) that is grossly visibly contaminated with blood and/or body fluids.
• Medical (clinical) waste is categorised by the colour yellow in South Australia and is incinerated and cannot be disposed of into the general waste or recycling waste streams.
• Yellow biohazard bags should be tied off at the point of use and disposed of into an approved clinical waste bin e.g. yellow 2-wheeled mobile garbage bin (MGB) with a lockable lid.





• Sharps must be disposed of into a sharps container, preferably at the point of care or point of use. Sharps containers must not be overfilled and must be sealed when three quarters full (or at designated fill line). Sharps containers are then to be placed into an approved medical (clinical) waste bin.
• Any waste receptacle, bin or MGB must not be overfilled. When sharps containers and/or medical (clinical) waste bins are ¾ full, the lid should be secured/locked while awaiting collection from the secure location. Waste bags within medical (clinical) bins should not be pushed down or moved to create more room in the receptacle as this may increase risk of aerosol contamination exposure to blood and/or body fluids.
Sharps must be disposed of into a sharps container, preferably at the point of care or point of use. Sharps containers must not be overfilled and must be sealed when three quarters full (or at designated fill line). Sharps containers are then to be placed into an approved medical (clinical) waste bin.
The following materials are not usually regarded as medical waste unless they fall into the medical waste definition:
• Dressings and bandages.
• Materials stained with or having had contact with body substances.
• Containers no longer containing body substances.
• Disposable nappies and incontinence pads.
• Sanitary napkins.
Clinical waste bins are collected by operators licensed by the Environmental Protection Agency (EPA) to transport clinical waste and are then incinerated.
There are other types of waste not regularly used with in SAAS. Clients may receive treatment at home and the appropriate waste receptacles organized or provided by the health provider.
33
OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
Continuing Education Program 2023 - Jan 2023
Cytotoxic waste
This waste includes any residual cytotoxic drug following a patient’s treatment and the materials or equipment associated with the preparation, transport or administration of the drugs. Cytotoxic waste is hazardous to human health and the environment and is subject to the requirements of the South Australian Environmental Protection Act 1993.
All cytotoxic waste should be placed into compliant bags or containers that are appropriately labelled and identified including:

• Containers and bags must be purple/lilac.
• The container must be marked with the ‘cell in late telophase’ symbol in white
• The words CYTOTOXIC WASTE’ must be clearly displayed.
Transmission-Based Precautions
Standard precautions must be applied when caring for any patient regardless of their infectious disease status.
Transmission-based precautions are applied to patients suspected or confirmed to be infected with agents transmitted by the contact, droplet or airborne routes.
Transmission-based precautions are applied in addition to standard precautions and include the following.
Contact precautions
• Transmission occurs by either direct or indirect contact
• Direct: involves close contact with a colonised/infected patient with transfer of the organism to the susceptible host, usually during patient care activities e.g. turning a patient.
• Indirect: occurs if an infectious agent is transferred via a contaminated intermediate object (fomite) or person e.g. when contaminated patient-care devices are shared between patients without cleaning and/or disinfection between patients.
Droplet precautions
• Transmission occurs through large (i.e. >5 microns in size) respiratory droplets that are generated by an infected person who is coughing, sneezing or talking. The droplets do not remain suspended in the air and are propelled a short distance from the source (approximately 1 metre). There is also the potential for indirect contact transmission as the droplets settle on environmental surfaces.
Airborne precautions
• Transmission occurs when small (i.e. <5 microns) respiratory droplets which are carried through the air. The droplets can remain suspended in the air for long periods and can be dispersed by air currents.
Applying standard and transmission-based precautions
When a disease is unknown, applying standard and transmission-based precautions using risk based principles will reduce the risk of transmission to the health care worker, and to other patients. Refer to the examples below:
Symptom Management
Vomiting and/or diarrhoea
• Contact precautions - gloves, gown, fluid resistant surgical mask and eye protection
• Inform healthcare facility patient has potentially infection vomiting and diarrhoea symptoms and will require transmission-based precautions
Fever, cough, sore throat, croup, respiratory symptoms
• Droplet precautions - surgical mask and eye protection
• Surgical mask for patient if tolerated
• Gown and gloves if potential exposure to body fluids
• Inform healthcare facility patient has potentially infection vomiting and diarrhoea symptoms and will require transmission-based precautions
34 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Prevention and Control - CEP 2023
Infection
Suspected or confirmed infectious patients
Transmission based precautions are recommended for suspected or confirmed infectious patients where standard precautions will not provide adequate protection. Refer to the Standard and Transmission Based Precautions Procedure for more information and SA Health Infection Control Management of Infectious diseases summary table below.
Type of precaution Examples of infectious agents Gloves Gown Mask Eye protection Equipment
Standard Standard precautions apply for all work practices to prevent the transmission of infection (PPR should be selected according to patient symptoms and degree of contact)
Gloves, gown and eye protection should be worn if there is the potential for direct or indirect contact with blood or body substances.
Contact MROs, C difficile, intestinal tract pathogens (e.g. norovirus), highly contagious skin infections (e.g. scabies)


Surgical mask if in sputum

If potential for direct or indirect contact with blood or body substances (as per standard precaution)
When there is potential for exposure of splashes or sprays of blood or body substances
Single use, otherwise, ensure reprocessing before next patient use.
P2 (N95)
In the pre-hospital environment, patients with a known or suspected infectious agent requiring additional transmission-based precautions may also require additional cleaning, refer to the SAAS Infection Control Precautions and Cleaning sticker for requirements for specific infectious diseases or SA Health Infection Control Management of Infectious diseases summary table. Clinical Tool – SAAS Infection Control Precautions and Cleaning [CTL-014] SA Health Infection Control Management of Infectious diseases summary table

35 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
Droplet Influenza, PSV, norovirus, pertussis (whooping cough), meningococcus
Surgical Airborne Pulmonary TB, chickenpox (varicella), measles (rubeola), SARS, pandemic influenzas
Immunisation
Most people use the terms vaccination and immunisation interchangeably, but their meanings are not the same. Vaccination means being injected with a vaccine, while immunisation means both receiving a vaccine and becoming immune to a disease as a result of being vaccinated.
Benefits of Immunisation
All diseases we vaccinate against can cause serious ongoing health conditions, and sometimes death.

The World Health Organizaton (WHO) considers immunisation to be the most effective medical intervention we have to prevent deaths and reduce disease in our communities. Immunisation programs prevent about 2.5 million deaths globally every year.

Immunisation protects you from a specific infectious disease and its immediate complications. Immunisation can also provide protection against long term complications from infections such as human papilloma virus which can lead to cancers and infection from the chickenpox virus, which can result in shingles later in life.
Herd immunity

Herd immunity, or community immunity, means there are enough people immunised in the community to slow or stop the spread of disease. If enough people in the community get immunised against a disease, the infection can no longer spread from person to person. The disease can die out altogether.
Herd immunity helps protect people who are more at risk of getting the disease. This includes people who are too young or too sick to get vaccinated. We need high immunisation rates, at about 95%, to achieve herd immunity for many infectious diseases.
Vaccine preventable diseases
Due to the nature of the work, those who work in the health care sector are at a significantly higher risk of encountering infectious diseases. SAAS currently provides vaccination against a number of vaccine preventable diseases.
For more information on immunisation and vaccines available through SAAS visit the immunisation SAASnet page.
Many diseases are preventable through the use of a vaccine, and some can provide life-long protection. Below is a list of some vaccine preventable diseases:
Cholera Japanese encephalitis
Rotavirus gastroenteritis
Covid-19 Malaria Rubella
Diphtheria Measles Shingles (Herpes Zoster)
Haemophilus influenzae type b Meningococcal disease Tetanus
Hepatitis A Mumps
Hepatitis B Pneumococcal disease
Tick-borne encephalitis
Tuberculosis
Hepatitis E Pertussis Typhoid fever
Human papillomavirus infection Poliomyelitis
Varicella
Influenza Rabies Yellow fever
Managing Occupational Risk and Exposure
Employers have the responsibility to provide employees with a safe workplace. It is also an employee’s responsibility to follow workplace policies and procedures and to take adequate precautions to protect yourself from injury and infection.
36 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Infection Prevention and Control - CEP 2023
Hazard Reporting
A hazard is anything with the potential to cause harm to you, patients, co-workers or visitors to the workplace. These hazards can include but are not limited to:
• Sharps injury
• Human waste and human tissues
• Inhalation of aerosols
• Contact with blood and other substances
• Personal contact with infectious materials, substances or people
• Stock (including food) which has passed ‘used by’ dates

• Animals, insects and vermin
All incidents and injuries that occur in the workplace must be reported and investigated immediately. This will ensure that the risk is minimised, controlled and contained and that a safe workplace is maintained for patients and co workers.
Blood and Body Fluid Exposure reporting enables the Team Leader and Staff Health to immediately perform assessment, management and follow-up of individuals who have had exposure, or suspected exposure, to blood borne viruses (BBV). Both the source and the exposed person need to be managed. The person whose blood or body fluids are the source of an exposure should be evaluated when required and if possible.
Procedure – Hazard Reporting [PRO-157]


Exposure to body fluids
Sometimes our PPE and procedures fail. This can lead to an exposure to body fluids. This includes events such as:
• Needle stick injury

• Laceration of the skin by bloody objects
• Fluid / blood splashes to areas including:
Mucous membranes (i.e. eyes or mouth)
Open wounds or scratches.
The risk of acquiring an infectious disease upon exposure to body fluid or blood can be quite low and varies in accordance with different diseases.
In the event you get blood or body fluids on your uniform, you should follow the Ambulance Officer Uniforms Soiled with Blood and Body Fluids procedure.
Procedure – Blood and Body Fluid Exposure Management [PRO-242]
Placement of signage
Signs are a useful way to convey special requirements and can be an added precaution when controlling the risks associated with workplace hazards.
They can be used to explain procedures for special situations and to give information about hazardous substances. All signs must convey messages clearly, be easily read and be displayed in appropriate places.
Signs can include notices informing staff of a potential gastroenteritis outbreak, signage identifying waste categories, signage indicating a trip hazard or signs indicating cleaning in progress.
37 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Control - CEP 2023
Infection Prevention and
Infection Prevention and Control - CEP 2023
Procedure – Immunisation Against Vaccine Preventable Diseases [PRO-246]
Procedure – Standard and Transmission Based Precautions [PRO-120]
Immunisation Intranet Page
Clean and contaminated zones
Contamination can be limited if all staff follow hand hygiene and infection control procedures, and all work areas are kept clean. A way to limit contamination is to ensure there are well designated clean and contaminated zones.
A ‘contaminated’ area should be a specifically designated area for placement of items such as any used equipment that can be reprocessed. This should be separate from the clean area where new or cleaned equipment is stored. Records and materials should be kept in a clean zone.




It is important that both clean and contaminated zones are clearly indicated with signs.
Procedure – Reprocessing of Used or Soiled Ambulance Equipment [PRO-112]
38 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Out of Hospital Cardiac Arrest (OHCA) Reaccreditation
Learning objectives
• Review the theory of High-Performance CPR (HP-CPR)
• Consolidate Ambulance Officers with measurable components of HP-CPR
• Reinforce the Importance of quality documentation of cardiac arrest cases
• Consolidate the standard SAAS scene choreography (Pit Crew CPR), metronomes and standardised instructions/language during a resuscitation
• Refamiliarise scene leadership during resuscitation and the use of an aide-memoire for patient safety
• Review the differences between Adult and Paediatric resuscitation practices
• Airway and ventilation review
• Consolidate the SAAS method of mobile HP-CPR (CPR while moving to the ambulance and mobilising to hospital)
• Demonstrate an understanding of HP-CPR theory by completing a practical assessment.
Introduction
As highlighted in CEP 2022 Out-of-hospital cardiac arrest is a leading cause of death, with an estimated 30,000+ people suffering a cardiac arrest in Australia each year. The prognosis for many of these arrests remains poor despite advances in ambulance service care and technology.
Quality CPR is a means to improve survival from cardiac arrest. Scientific studies demonstrate when CPR is performed according to guidelines, the chances of successful resuscitation increases substantially. Minimal breaks in chest compressions, full chest recoil, adequate compression depth, and adequate compression rate are all components of CPR that can increase survival from cardiac arrest.
Interstate and overseas ambulance services have demonstrated quality CPR and a coordinated approach to the way we prepare, equip and respond as teams to cardiac arrest cases can see a dramatic increase in return of spontaneous circulation (ROSC) and survival from hospital neurologically intact.
Together, all these components combine to create high-performance CPR (HP CPR). This eLearning module will provide you with resources to support your face-to-face training on this topic and guide you to achieve HP CPR in the field.
This module is required to be completed as part of your 2023 Ambulance Officer reaccreditation. For this module, we will be referring to Ambulance Assist/Ambulance Responder/Ambulance Officer practice as Basic Life Support (BLS) CPR and ICP/Paramedic practice as Advanced Life Support (ALS) CPR. We do acknowledge our Ambulance Officers do perform certain ALS skills such as the use of a monitor defibrillator and Supraglottic Airways.
Ideally, you should review the module information and videos before a face-to-face session with your RTL/CTL/ CSO. This will ensure your face-to-face training can be more practical orientated. During the face-to-face session, you need to demonstrate safe and effective practice before the module is complete.
Covid-19
During the Covid-19 pandemic SAAS reviewed its clinical practice to minimise the chance of cross infection between patients, clinicians and the general public. Covid-19 CPG-54 AA/AR/AO changes have been incorporated into this package.
The COVID-19 (Novel Coronavirus, SARS-CoV-2 or 2019-nCoV) pandemic is an evolving situation with rapid virus spread and disease progression. Coviod-19 CPP-54 provides current knowledge and guidance relevant during COVID-19 community transmission. Staff must only initiate treatment within their scope of practice and request clinical support or consult as per normal practice.

COVID-19 transmission occurs via respiratory droplets, aerosols, direct physical contact with infected individual regardless of symptoms, and indirectly through contaminated objects and surfaces. Reduction of virus spread
Continuing Education Program 2023 - Jan 2023
39
OFFICIAL OFFICIAL <Section/Chapter Heading> OHCA ReaccreditationCEP 2023
requires adherence to PPE precautions as per SAAS PRO-313. Focus on early identification of COVID-19 risk factors will maximise the safety of staff and patients.
PPE requirements in AGP/AGB along with modifications to practice are required to reduce transmission risk. Clear communication to all people on scene and where possible moving to a well ventilated space is recommended when performing any AGPs. Refer to COVN-026 PPE Matrix.
AGPs include:
• Intermittent Positive Pressure Ventilation via BVM or i-gel1
• Airway Suctioning
• Nebulised medication
• Endotracheal intubation (ICP only skill)
• Laryngoscopy (Paramedic/ICP only skill)
• CPAP (ICP only skill)
AGBs include:
• Shouting
• Singing
• Coughing
• Crying
• Spitting
Modifications to practice
Current SAAS CPP’s remain best practice for patient management throughout the COVID-19 pandemic. Transmission risk during AGPs and AGBs are influenced by several factors, including symptom and disease severity, forced air over respiratory mucosa, distance from the respiratory emissions, and duration of exposure. To minimise transmission risk while maintaining optimal patient management. Modifications to practice are recommended for Airway Management including i-Gel insertion, BVM and Suctioning. For Cardiac Arrest a pause in compressions, the introduction of mechanical CPR device and the use of a surgical mask over oxygen face masks and nasal specs for the delivery of supplementary oxygen therapy.
Does Training Influence Patient Outcomes?

There has been some excellent research from Victoria that has explored this with interesting results. The main findings are:
• Paramedic exposure to cardiac arrest is rare and declining (in Victoria)
• On average, individual paramedics were exposed to 2 Out of Hospital Cardiac Arrests (OHCA) resuscitations a year, and 1 in 10 had no exposures in the 7 years!
• As many as 42% of paramedics attended less than 1 OHCA per year, so we know exposure alone is not enough to maintain our skills.
• The average paramedic will only see one Paediatric OHCA per 12.5 years’ service, and 1 traumatic OHCA per 9.5 years, so the specific skills for such rare scenarios are even harder to maintain.
40 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
OHCA Reaccreditation - CEP 2023
The study results indicate that resuscitation skills decay and that Paramedics and Ambulance Officers need exposure or training to prevent skill decay and thus improve patient survival. This suggests that 6-month exposure to either real OHCA cases or resuscitation training might be required to prevent skill deterioration and to maximize patient survival.
This research resulted in more than one media headline. It also prompted Ambulance Victoria to dedicate more annual training time. In the hospital setting, simulation has been shown to improve practitioner skill performance, and there is some indication that it may improve patient survival. This fundamentally highlights why the training that you will receive in OHCA treatments during 2018/19 is important; it CAN influence patient outcomes.
As we examined in previous AO CEP training: excellent quality CPR is a critical component of cardiac arrest management. Improving your understanding and application of the components involved with high-performance CPR (HP-CPR) will result in an improved likelihood of cardiac arrest survivability. International literature from pre-hospital services and cardiac arrest reviews (including Australia, America, Japan, Canada) indicate the quality of Emergency Medical Services (Ambulance Services) provided CPR is highly varied, with most services demonstrating room for improvement. The Resuscitation Academy (Seattle) have labelled HP-CPR as one of the four ‘low hanging fruit’ to improve cardiac arrest survivability. It is a simple concept with low complexities.
What do we propose? The dawning of a new era in cardiac arrest management for ALL SAAS clinicians. An era where every patient found in VF/VT survives. An era where Return of Spontaneous Circulation (ROSC) and Signs of Life is expected and not considered a miracle.
The challenge? To become the best-performing state in Australia. There is no reason we cannot achieve this.
WE NEED YOU TO BECOME CARDIAC ARREST CHAMPIONS IN YOUR TEAMS AND COMMUNITY.
VF Arrest - Prolonged Resuscitation [09:06 minutes] https://player.vimeo.com/video/307190312
Cardiac Arrest: The Theory
Cardiac arrest is not a diagnosis. A cardiac arrest is a loss of function of the myocardium to a point that there is no measurable cardiac output. Cardiac arrest can be attributed to a supply issue or a pump issue. Lack of supply of oxygen or blood to the heart, or failure of the mechanical beating of the heart as a pump.


The heart needs a constant supply of oxygen and glucose due to its high metabolic demand, and inability to store sufficient oxygen or glucose. Therefore, a heart in cardiac arrest quickly becomes ischaemic and aerobic metabolism converts to anaerobic metabolism, which we know produces lactic acid and nitric oxide.
Ischaemic myocardial cells also have reduced electrical and muscular function.

Why Have They Arrested?
So why is our patient in Cardiac Arrest? Remembering Cardiac Arrest is NOT a diagnosis.
• Think critically about potential causes and treatment when poss ible
• Identify potential causes to help achieve ROSC.
• Call early for back up e.g. Paramedic/ICP, RERN (a local medical officer with emergency skills), they may be able to address some of the reversible causes.
Continuing Education Program 2023 - Jan 2023
41
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
• Call for extra help - another AO crew, other emergency services etc. just for an extra set of hands, especially if we are considering mobilising under CPR because there is a potentially reversible cause.
We shouldn’t just be going through the motions, but rather (when feasible), we need to think critically about the cause of the cardiac arrest, and if/how it can be reversed. The sooner we can identify and reverse the cause (including early clinical backup or possible transportation to clinical support), the more likely we are to achieve ROSC.
• Think critically about the cause and treat it when possible. If as Ambulance Officers you can’t treat potential causes, we need to consider getting help or getting to help (mobilise under CPR)
• Consider aggressive and prolonged resuscitation efforts if the cause is potentially reversible and/or transport under CPR when appropriate
• Maybe more than one reversible cause
• Consider the H’s and T’s.
Hypoxia
We can do something about this! Oxygenation and ventilation.
Could our patient’s cardiac arrest be a result of hypoxia? From something as basic as airway obstruction or did they have asthma or anaphylaxis before and leading to the cardiac arrest?
Adequate oxygenation requires high flow oxygen, an open airway, correct posturing, ventilation of the lungs, and perfusion. Any interruption in these could lead to hypoxic arrest, the list is endless. As discussed, the heart needs a constant supply of oxygen.
Hypovolaemia
Is there a chance our patient arrested as a result of hypovolaemia? Trauma is the most classic, stand-alone, cause of hypovolaemic arrest.
There are also non-traumatic causes of hypovolaemia including an aneurysm, anaphylaxis, dehydration, sepsis or neurogenic shock (which can cross over a few reversible causes). Don’t forget, if we see signs of considerable blood loss, we should consider hypovolaemia as the cause of cardiac arrest.

What are we going to do about it? Firstly, stop bleeding (if we can) as soon as possible, because we know that survival depends on circulating blood volume to provide adequate cardiac output.
AA/AR/AO treatment can include (concurrently to quality CPR occurring also):
• Direct pressure dressings to wounds
• Use of SOF Tactical Tourniquets
• Use of SAM Pelvic Splint/Binder
• Use of CT-6 Femoral Traction Splint/s.
Paramedics and ICPs can commence intravenous (IV) fluid resuscitation. In a rural area, other providers who can commence IV fluids may include RERN Medical Officers and Ambulance Officers with Extended Practice. Get early SAAS MedSTAR retrieval. Consult with the EOC Clinician for advice..
42 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
CEP 2023
OHCA Reaccreditation -
If the arrest can be reversible on the scene, then this should be simultaneously addressed and the ongoing requirement for fluid resuscitation re-assessed.
Clinical Practice Procedure - Arterial Tourniquet Application [CPPRO-004]
Hyperkalaemia
There is a perfectly balanced harmony between electrolytes in our bodies. Any disruption of electrolytes can lead to cardiac arrest. Immediate treatment of high or low levels is required to ensure the return of homeostasis. Electrolyte abnormalities are among the most common causes of cardiac arrhythmia. Close attention to patient history may help identify the chances of an electrolyte disturbance being the cause of cardiac arrest.
Hyperkalaemia is the most common electrolyte disturbance and can occur rapidly. Suspect hyperkalaemia for patients with severe diabetic problems, Addison’s disease, if they’re taking medications for acute renal failure or are on dialysis. A patient with a relatively prolonged history of fluid loss, including vomiting and or diarrhoea, is likely to have electrolyte imbalances. Particularly loss of potassium and sodium. Hypokalaemia could also be suspected in patients on diuretic medication (e.g. Lasix), or those with chronic kidney disease.

Hypothermia

A quick temperature check (only if able to do so when enough resources are on the scene during good quality BLS) if history or suspicion of temperature extremes is present can help give you an idea if the cause of the arrest is hypo/hyperthermia.
Could our patient be hyper/hypothermic? Is it the end of a heat wave or the middle of winter? It’s 0500 in the morning, the patient has been lying on the bathroom floor for 6 hours or lying in the back garden for 2 hours on a 40-degree summer day, all clues to prompt investigation.
Hypothermia is an unusual cause of cardiac arrest and is often precipitated by another event. It is affecting virtually all organ systems. In terms of cardiac arrest, hypothermia progressively depressed the central nervous systems and makes heart cells more irritable which can lead to lethal arrhythmias.
In hypothermic cardiac arrest patients, it is important to prevent further heat loss and focus on gentle manual handling. Dry them if needed and insulate them with a blanket as best possible to enable treatment. Clinical treatments may not be effective until the patient has been rewarmed, and hence transport should always be a consideration.
The hypothermic heart may be unresponsive to drugs and defibrillation and hence they fit into the special considerations group. Refer to your relevant hypothermia clinical practice protocol regarding care and defibrillation for this subgroup of patients. Early consult with EOC Clinician for advice.
Clinical Practice Protocol - Hypothermia (Severe and Unresponsive) - Ambulance Officer [CPP-019-AO]




Clinical Practice Protocol - Hypothermia (Severe and Unresponsive) - Ambulance Responder [CPP-032-AR]
Clinical Practice Protocol - Exposure to Cold - Ambulance Assist [CPP-044-AA]
Note: The current SAAS thermometers appropriate to guide management in severely hypothermic cardiac arrests? Tympanic thermometers based on infrared technique do not seal the ear canal and therefore are not designed for low core temperature readings. The Braun Thermoscan is the infrared tympanic thermometer currently used by SAAS. According to the Braun Thermoscan product information booklet, the thermometer displays a temperature range of 20-42.2°C. The accuracy for displayed temperature range with a probe cover is ±0.2°C (35.0 - 42°C), and ±0.3°C (outside of this temperature range). Whilst recognising the current thermometers are not optimal for altering management decisions in hypothermic cardiac arrest, they indicate the severity of the hypothermia.
Use of Welch Allyn Braun ThermoScan tempatic thermometer [04:30 minutes] https://www.youtube.com/embed/70dA8B8u6Bw
43
OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Continuing Education Program 2023 - Jan 2023
Diabetes
Hypoglycaemia is a rare cause of cardiac arrest and we do not recommend prioritising a BGL check over BLS in cardiac arrest (you may be able to do a BGL once enough resources are on scene and all other care in BLS has been provided). Consult with EOC Clinician if hypoglycaemia is noted during resuscitation or post-ROSC.
Thrombosis
Potential thrombosis causes can include myocardial infarction and pulmonary embolism.
A sudden collapse is likely the result of a Myocardial Infarction, one of the most common causes of cardiac arrest. This is the one we are most familiar with.
A cardiac arrest occurs when the myocardium is deprived of blood flow beyond the obstructing thrombus, as mentioned the heart needs a constant supply of oxygen and glucose. The muscle quickly becomes ischaemic and contraction of the myocardium is no longer efficient to achieve flow. It is reversible, but the clot needs to be removed and the artery re-perfused within the hospital environment. Consider transport under CPR when appropriate.

Tension Pneumothorax
Is there a possibility that our patient has a tension pneumothorax as a result of a motor vehicle crash or other trauma mechanisms? Other causes include asthma, COPD and barotrauma (e.g. scuba diving incident).
Tension pneumothorax can be associated with an open chest wound but can occur with no obvious evidence of chest trauma (blunt trauma).
Tension pneumothorax compresses major structures in the chest, impairing both ventilation and perfusion.

What do we do? CPR first and foremost. The patient will require decompression of the chest (so get Paramedics / ICP / RERN on the way or if not available consider getting to help e.g. Doctor/Hospital while mobilising under CPR).
Tamponade
If blood or fluid accumulates in the pericardium, the heart will quickly lose its ability to pump and ventricular filling is reduced. It’s very difficult to diagnose. History of chest trauma (blunt and penetrating) will make us suspicious of tamponade. Hypotension or signs of poor perfusion is possible.
We should consider transport under CPR to the hospital, as this is a reversible condition.
44 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Cardiac Tamponade (and cardiac arrest save) - post stabbing - Kings Cross Sydney [43:00 minutes]
https://vimeo.com/66143304/5659471d06
WARNING GRAPHIC CONTENT. Demonstrates the ambulance crew’s decision the patient was time-critical, rapid transportation with BLS care while in transit to the hospital. Ultimately allowing for successful resuscitation.
Toxins
History taking is vital to identify toxins. Treatment limited to us in SAAS depends on the toxin.
A detailed history is the most likely way to determine if the cardiac arrest is due to a toxin. Management will depend on the toxin, and in addition to supportive care may include administering a reversing agent. Consider all potential toxins, medications (legal and recreational), poisons, bites and stings, chemical exposure etc.


Note: When responding to a HAZMAT incident, SAFETY remains the priority - DO NOT compromise your safety, that of your colleagues or the community.

Procedure - HAZMAT Incident Management [PRO-089]

VT is an abnormal and often life-threatening ECG where the electrical impulse originates in the ventricles. Whilst there is still some order to the conduction, there are no obvious P waves and there is a consistent pattern of QRS complexes that are wide, bizarre-looking and fast (greater than 120 per minute).
Continuing Education Program 2023 - Jan 2023

45
OFFICIAL OFFICIAL
- CEP 2023
OHCA Reaccreditation
What
Ventricular
What About Cardiac Rhythms During Cardiac Arrest?
is
Tachycardia (VT)?
VT originates in the ventricles and is most caused by a single re-entry circuit, which explains why it presents as a regular (showing little or no variation in the pattern on the ECG).


The rapid rate of these arrhythmias reduces ventricular filling time and coronary artery perfusion pressure. Cardiac output drops due to the dissociation of atrial and ventricular activity.
Treatment must be initiated as soon as possible; this rhythm is ventricular fibrillation quickly. Defibrillation can successfully revert this rhythm and VT should be more responsive to defibrillation.
Key Points:
• VT originates in ventricles

• Regular “saw tooth” pattern
• Rapid rate reduces ventricular filling. Cardiac output drops due to dissociation of atrial and ventricular activity

• VT can degenerate to VF quickly
• Treatment is early defibrillation and HP-CPR if the patient shows no signs of life.
Note: A patient can be conscious and in VT. Therefore, use extreme caution if operating a monitor Defibrillator in “AED” mode with defibrillation pads in use on a conscious patient. The AED analysis can’t tell if the patient is conscious/with signs of life or not and may charge up and advise a shock. Treat the patient not the monitor/defibrillator.

What is Ventricular Fibrillation (VF)?
46 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
CEP 2023
OHCA Reaccreditation -
VF is when the electrical impulse originates from multiple pacemaker sites in the ventricles and as a result, there is no order to the impulse generation or conduction. There will be no P waves, no obvious QRS complexes and no T-waves present in the ECG. While there is electrical activity present, it is chaotic and there is no discernible pattern to it (has the appearance of an erratic wiggly line)
Key Points:
• Ventricular Fibrillation (VF) is the very fast, uncoordinated, rhythm that does not produce sufficient output to sustain life
• It is believed that VF is maintained by multiple irritated pacemaker cells that generate numerous re-entry circuits across the ventricular myocardium
• We know coarse VF is more responsive to defibrillation
• Time to defibrillation is important.
What is Asystole?
Asystole occurs when there is no electrical activity present in the heart, therefore the heart is unable to pump at all. As a result, there will also be no heart muscle contraction and therefore no signs of life. It presents as a straight and flat line on the ECG. As there is no electrical activity, defibrillation is not indicated for this rhythm and therefore chest compressions should be started as soon as possible.
Key Points:
• AED’s will not advise to ‘shock’ asystole.


• Rarely a true flat line but often described as a wandering flat line. Sometimes occasional small waves may also be seen
• HP-CPR is the treatment for this presenting cardiac rhythm until ALS support is available.
What is Pulseless Electrical Activity (PEA)?
Sometimes the electrical system of the heart is still active but there is a problem with the mechanical action of the pump or hypovolemia (insufficient blood in the circulatory system to be pumped by the heart). Therefore, the muscle is not contracting when it is supposed to or as well as it should or has nothing to pump. This type of fault (mechanical or hypovolemia) may not be seen on an ECG, hence why it is important to assess the patient, not just their ECG (e.g. look for signs of life).
In these situations, the ECG can appear normal with P waves, QRS complexes and T waves. However, the heart muscle does not contract, and a pulse will not be detectable.
Key Points:
• In PEA, there is organised or semi-organised electrical activity in the heart as opposed to asystole (flatline) or the disorganised electrical activity of either ventricular fibrillation or ventricular tachycardia
• As the issue is not the electrical system, defibrillation is not indicated
• HP-CPR should be started as soon as possible until ALS support is available.
Continuing Education Program 2023 - Jan 2023
47
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
High-Performance CPR
Let’s talk about BLS and what actually saves lives in most cardiac arrests. This is high quality, early, continuous chest compressions and early defibrillation and ventilation.
But have you thought about how this actually works?
A review of current literature indicates the prognosis following an out of hospital cardiac arrest has not dramatically improved over the last 20 years. We are, as pre-hospital emergency clinicians, a crucial link in the ‘chain of survival’ and have a responsibility to ensure our link in this chain is as robust as possible. While the literature supports the fact that there is no ‘magic bullet’ in improving cardiac arrest survivability, early defibrillation and HP-CPR are, without question, essential components of surviving a cardiac arrest.
The steps involved to achieve high-performance CPR are:
• Minimal ’hands-off” time and breaks in compressions
• Full chest recoil
• Adequate compression depth
• Adequate compression rate
• Change compression operators every 2 minutes or when fatigued.
CPR is a basic skill, but a skill that requires precise delivery. High-performance CPR can significantly alter the patient’s clinical course; quite literally being the difference between life and death. The concept of HP-CPR will be analysed and discussed throughout this package. Upon completion, the Ambulance Officer will have a better understanding of what HP-CPR is and why it is a critical component of ambulance practice.
Physiology Of CPR
To succeed in improving survivability from cardiac arrest we must first understand the physiology of CPR; in other words, we need to know what we are doing to do it better! CPR comprises two key phases: compression and decompression.
Phase 1 - Compression Phase
With each chest compression, the volume of the chest cavity is decreased and subsequently increases the intrathoracic pressure and the heart is squeezed between the chest wall and the patient’s spine. Each effective compression causes increased pressure in the heart and aorta, resulting in a projection of blood from the heart to the brain and the rest of the body. This occurs due to the presence of one-way valves within the heart and pressure differences between the thorax and the rest of the body.


Phase 2 - Decompression Phase
The phase following chest compression is the decompression phase or the recoil phase. During recoil, the removal of the hands increases the volume of the chest cavity and subsequently reduces the intrathoracic pressure. The reduction in intrathoracic pressure allows for venous return and passive refill of the heart, resulting in the next compression ejecting more blood from the heart and continuing the forward movement of blood (with the aid of valves) to vital or gans. Recoil is not an active motion and therefore the full recoil of the chest wall mustn’t be impeded. Recoil or return of baseline pressure also causes a subsequent decrease in ICP in the same reversed mechanism as explained in chest compression.
48 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Minimising Interruption to Compressions
In understanding the physiology of CPR, it seems obvious that minimising “hands-off chest time” is beneficial for the patient. Compression interruptions are sometimes not obvious; not compressing while charging, changing compressors mid cycle, rhythm checks, poor positioning, poor coordination of shock cycles, and miscommunication with compressor changes all contribute to unnecessary pauses in compressions.
Any pause in compressions reduces coronary and cerebral perfusion pressures. Research has found that once compressions have stopped it can take up to a minute of high-quality compressions to regain adequate perfusion pressures. This means that for every pause it can take half of the subsequent shock cycle to return to optimal perfusion pressures.

Illustration of the drop in perfusion associated with a pause in compression
Scene preparation, leadership and communication are variables that can have a significant impact on minimising interruption to compressions. Ensuring early 360° access to the patient can have a big impact in allowing clinicians to operate effectively. Counting compressions out loud for the last 5 pre ventilation to ensure the ventilator is ready, pre-charging the monitor (ALS providers in manual defibrillation mode) or anticipating the function and timings of the AED (BLS providers in AED defibrillation mode) and rapidly returning to compressions post no shock advised or defibrillation, are examples of how we can effectively work as a team to ensure we bring ‘hands off’ time to an absolute minimum.
Rate
The likelihood of ROSC increases significantly with a higher mean chest compression rate to a point. In a hospital study, 75% of patients achieved ROSC with 90 or more chest compressions/minute compared to only 42% with 72 or fewer chest compressions/minute. Compression rate efficiency decreases at rates above 120 compressions/min.

ANZCOR recommends compressions should be delivered at a rate for all ages of between 100 and 120 per minute. Each compression should be of equal duration to ensure good flow and rhythm. Compression rates of less than 100 and greater than 140 have been associated with lower rates of survival. Compression rates above the recommended rate of 120 have been shown to reduce heart fill time and volume and therefore reducing the amount of circulated blood. Audio visual tools such as metronomes (a feature on the Corpuls monitor/defibrillator) are recommended for monitoring and measuring rates.
The SAAS ideal chest compression rate is 110 compressions per minute
Metronome
The use of metronomes is associated with a greater ability to r emain at an optimal rate of compression. This was proven in a study of 155 medical personnel. The study compared compression rates both when using a metronome and without. Results showed that when a metronome was utilised, compressions were conducted at the optimal rate more often, with an accuracy of the rate jumping from 50% to 72%. Most clinicians in this study, who were not in the desired range, were found to be compressing too quickly.
Metronomes provide auditory feedback for compression performance. The auditory tone of the metronome relays a precise indication of recommended compression rate which allows the clinician to rectify a rate error immediately.
Most new ECG monitors/defibrillators have built-in metronomes, such is the perceived benefit of these devices. The current Corpuls Monitor Defibrillator has this feature which can be either set as a continuous audible beep or set at 30:2 Compression ration which has 30 beeps followed by 2 breath sounds.
Continuing Education Program 2023 - Jan 2023
49
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
Depth
A paper published in 2014 - “Optimal Chest Compression Depth During Out of Hospital Cardiac Arrest Resuscitation of Adults”, demonstrated the probability of survival directly correlated to chest compression depth. Data showed that the survival of patients peaked at a depth of 45.6 mm with the highest survival rates between 40.3mm and 55.3mm. Linking depth of compression data and rate of compressions it was also found that in cases where the rate of compression was higher than the recommended 120 compressions per minute, the depth of compression was adversely affected by 53%.

Depth of compression is recommended at 40 mm in most infants and 40-50 mm in most children. Adolescents should be regarded as adults in terms of depth, with a depth of 50-60 mm, but not exceeding 60 mm. 1/3 the anteroposterior (AP) diameter of the chest can be a useful guide in compressing Paediatric chests.
Recoil
The recoil of the chest during CPR is the return of the chest wall to normal anatomy and height. Full recoil cannot be reached if there remains pressure on the chest during the decompression phase. To achieve full recoil, the sternum must return to normal height briefly after each compression. One way to obtain full recoil is on an upward stroke of compression to ensure your hands are removed slightly but not completely from the chest wall. Avoid ‘leaning’ on the chest by setting up with a good posture before starting CPR.
If decompression is incomplete, the next compression is not as effective due to inadequate blood volume return in the heart and lungs. Inadequate decompression (recoil) compromises both coronary artery and cerebral blood flow. Even limited periods of incomplete decompression can have a lingering effect on coronary and cerebral perfusion pressures, which may remain low even after this deficiency in CPR has been corrected.

Positioning
Adequate positioning of the hands for CPR is of great importance. Chest compression aims to not only compress the heart in between the sternum and the spine but also increase intrathoracic pressure. The compressor must place their hand in the centre of the chest over the lower aspect of the sternum. Too low, and compression of the xiphoid process can cause trauma to other organs including the liver, spleen and stomach (dependent on patient age, size and anatomy). Too high, and compression effectiveness decreases.
50
OFFICIAL OFFICIAL
Continuing Education Program 2023 - Jan 2023
OHCA Reaccreditation - CEP 2023
The compressor’s chest should be directly over their hands, enabling them to use their upper body weight to compress the patient’s chest instead of relying on just arm strength; this will aid in minimizing fatigue. Adequate positioning is also imperative in reducing the compressor’s risk of injury. Locking arms, good alignments and keeping the patient close to you can ensure that you are not in an awkward position and at risk of injury.

Continual reassessment of positioning should be made throughout the resuscitation. With each compression cycle, re-evaluation of position and posture should be made to maximise compression efficiency. Assessing and providing feedback on each other’s position and posture is important; changing culture to allow for providing and receiving constructive, live feedback is critical in ensuring HP-CPR is being delivered at all times.
Fatigue and Rotation of Compressors
Compressor fatigue can impact all aspects of CPR including positioning, rate, depth and recoil. Timely rotation of compressors is vital in ensuring all aspects of CPR are effective and the patient always receives high-quality compressions. ANZCOR explain that often, compression quality can decrease within the first minute of the first cycle, yet it can take 5 minutes for the compressor to report feeling fatigued. ANZCOR suggest a rotation of compressors every two minutes to minimise the effects of fatigue
Any signs of fatigue during compressions need to be addressed immediately; ideally, by self-identification, but also by other clinicians participating in the resuscitation. Colleagues should address suboptimal compressing by coaching as soon as possible. If after coaching, the compressor is still unable to perform adequate CPR, then it is reasonable to swap out a compressor mid-cycle. Fatigue is a real issue that affects us all; we must always put the patient’s best interest before egos. The development of fatigue does not give any indication of effort or competency either. Resuscitations are a team-based performance; no individual should be made to feel targeted and no individual should be scrutinised for acknowledging they require assistance from their team.
If we are using a non-SAAS person to perform CPR compressions it is our responsibility to monitor their CPR compression performance. We should provide encouragement and feedback which should address suboptimal compressing by coaching as soon as possible. If after coaching, the compressor is still unable to perform adequate CPR, then it is reasonable to remove them from the resuscitation team.
Summary
HP-CPR is the application of high-quality CPR, with special care taken to ensure skills are performed in a standardised manner following current best practices:
• Hand positioning on the lower half of the sternum
• Compression depth of 40mm in infants, 40-50mm in children and 50-60mm in adults.
• Ensure chest recoil after each compression
• Compressions performed at a rate of 100-120 with the use of a metronome were achievable set at a rate of 110


A compression to ventilation ratio of 30:2 before and after an advanced airway insertion with a short pause for ventilations. Uninterrupted compressions after insertion of i-Gel® in adults; has been superseded by Covid-19 CPP-54 which states Pause compressions during ventilation with BVM or i-gel. ensuring patients are not hyperventilated. After insertion of an advanced airway for a child, a short pause of compressions for the ventilations is still required.
Continuing Education Program 2023 - Jan 2023
51
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
As an ambulance service, we should be industry leaders in the quality of CPR we deliver to our patients. HP-CPR is the ‘new’ way of thinking about CPR, going back to basics and focusing on delivering excellent quality basic life support (BLS) with elements of advanced life support (ALS) introduced where required.
Be prepared for lots of practical sessions in your upcoming practical sessions!
The Quest to Reverse Sudden Death - History of CPR and Defibrillation [42:00 minutes] (Requires login to YouTube)
A great reminder of how far we have come in terms of both in-hospital and pre-hospital resuscitation.
Defibrillation
Defibrillation is the delivery of lifesaving electrical energy t o the heart of the unresponsive patient who is in a VT or VF rhythm.
SAAS Volunteers were one of the Australian pioneers in the use of Automated External Defibrillators (AED). SAAS introduced AEDs to the AO level in 1994.
What was once considered an advanced care skill is now taught to all SAAS AAs/ARs/AOs at basic recruit training. Modern-day devices are now much cheaper to purchase and simpler to maintain and use, allowing for workplace first aiders and members of the public to access and use.
AED electrodes/pads placed on the patient’s chest to serve as the conduit for delivering a measured electrical shock to the heart to restore natural rhythm.

AEDs are small computerized devices that analyse heart rhythms and provide the shock needed for defibrillation. Through adhesive pads placed on a patient’s chest, a processor inside the AED analyses the victim’s heart. The machine will not shock unless it is necessary; AEDs are designed to shock only when VF or VT, common causes of cardiac arrest, is detected.
After the processor analyses the heart rhythm and determines a shock is required, an electric current is delivered to the heart through the patient’s chest wall through the adhesive electrode pads. The shock delivered by a cardiac defibrillator aims to interrupt the chaotic rhythm and allows it to return to normal.
Defibrillation pad placement is VITAL to successful defibrillation.
We know EARLY defibrillation saves lives. Every minute delay = 10% reduction in survival from VF rhythm. If our pads aren’t in the right place or the current is impeded by anything, we may delay effective defibrillation.
Studies suggest, for defibrillation to be successful, 75-90% of the myocardium mass needs to be defibrillated at the same time. Hence pad placement is vital to successful defibrillation.
We practice often on manikins with training leads that connect directly to the manikin, so it is important to remind ourselves of the patient preparation and actual defibrillation pad/electrode application.

Standard Adult defibrillator pad placement
Essentially, we want to “sandwich” the heart between the two pads as the current runs between them. According to ANZCOR guidelines, pads need to be placed on the exposed chest; one pad slightly below the collarbone on the right chest and one pad on the person’s left side below the armpit (lateral to left breast in large-breasted individuals). In large-breasted patients, if defibrillator pads are placed over the breast tissue this may increase impedance and decrease defibrillation efficacy.
An alternative adult pad placement the EOC Clinician may advise is Anterior/Posterior, which is the upper back between shoulder blades and front of the chest and slightly to the left (ANZCOR guideline 7). Refer to the actual pads and pad packaging for pad placement guidance.
52 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
Adult Defibrillator - Alternative pad placement - Anterior/Posterior
For paediatric and infant patients <8 years, the adult defibrillator pads are uses in SAAS but are placed in the Anterior/Posterior placement.


Keep ‘defib’ pads at least 8cm away from visible ICD and pacemaker devices, due to possible interference (ANZCOR guideline 11.4). Do not place defib pads over medication patches that may be on the patient’s chest.

Typically shocks ranging from 150 joules to 360 joules (varied between brands/manufacturers) are necessary for successful defibrillation when pads are placed on the body surface. However, only 4-20% of the delivered current ever reaches the myocardium. The method outlined in the ANZCOR guidelines allows for optimal joules to be delivered to the greatest area of the myocardium.

Successful pad placement will ensure good contact with the pad on the patient’s bare skin. Hair, moisture, breast tissue, bone can all reduce the effectiveness of the shock and are essential to avoid as much as possible. These things will all create an impedance of the electrical current getting to the myocardium. Make sure your vehicle’s defibrillator has a razor and either a small hand towel or combine dressing. In the unit’s soft pack. Use the razor if the chest is excessively hairy and dry chest with a towel or combine dressing, otherwise, defibrillation pad connection will not be optimal.

If you aren’t getting anywhere with your shocks after multiple attempts, we need to reassess. It may be appropriate to apply new pads or reassess their position. Taking the time to dry and shave the chest should occur when needed.
At the ten-minute mark when you consult with the EOC Clinician, discuss the possibility of changing pad position from standard to anterior/posterior positioning with a new set of pads.
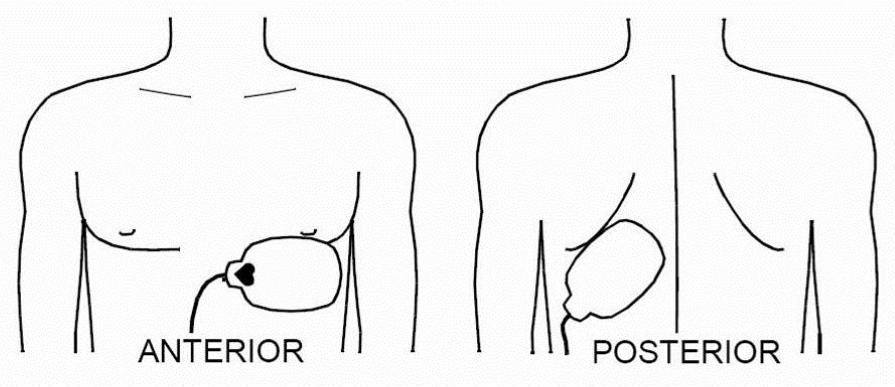
53
Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Continuing
Special Circumstances
Pregnancy and Cardiac Arrest
The patient position has emerged as an important strategy to improve the quality of CPR. After approximately 20 weeks gestation, the pregnant patient’s uterus can compress the inferior vena cava (IVC) and the aorta, impeding venous return, thereby reducing stroke volume, cardiac output and uterine perfusion. IVC compression limits the effectiveness of chest compressions.
Pregnant patients in cardiac arrest with a known or suspected gestation >20 weeks should be resuscitated with a 15°-30° tilt of the patient to the left to raise their right hip if it is feasible and doesn’t interfere with high-performance CPR.

Early consult with the MedSTAR Medical Retrieval Consultant (MRC) via the EOC Clinician should occur to discuss management options.
Bariatric Patients
Morbid obesity can provide challenges during the resuscitation attempt and extra resources should be considered early. In essence, we know that performing chest compressions on these patients may be more difficult and physically exhausting. To maintain sufficient rate and depth of chest compressions, the compressor may need to change more frequently than the standard 2-minute intervals.
Ventilating these patients can also be challenging, and you may require greater inspiratory pressures due to thoracic mass compression, increased intrabdominal pressure and changes to lung physiology. This can result in excessive leaks with ventilation through an i-Gel® during uninterrupted compressions. Consider pausing for ventilation even when an i-Gel® is insitu. The increased intraabdominal pressure and higher inspiratory pressures also increase the risk of aspiration. Have your suction set up and readily available.
If transport under CPR is being considered, there is a need to liaise early with EOC for the potential use of bariatric ambulance or regional bariatric resources
Asthma
For the asthmatic patient in cardiac arrest, we need to be careful of ventilation rates and volumes if the patient is very difficult to ventilate.
We have to stop and think about what we are doing, ensuring that we allow enough time for the patient to completely exhale before delivering the next ventilation.
54 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Approach To Airway And Ventilation Management
Airway soiling
For gross soiling, it is often better to use gravity. Turn patients on their side and remove excess fluid, water, blood and vomit.
The Yankeur suction catheter is good for fluid and blood but will often get obstructed with vomit / blood clots.



The soft Y-Suction catheters are good for thin fluids, can suction down OPA, NPA, and down both the airway and gastric ports of i-Gel®.
Ventilation
ARC guidelines state “ventilation volume should not exceed any more than visible chest rise and fall.” The Resuscitation Academy suggests that during practice using the 3-finger squeeze technique is an effective way to achieve adequate ventilation volume. Lower tidal volumes during resuscitation do not appear to significantly affect the arterial partial pressure of oxygen (PaO2). Excessive ventilation volumes have proven negative effects of reducing cardiac output and increasing the risk of gastric insufflation.
The infant Bag-Valve-Mask (BVM) resuscitator in the maternity kit is designed for children <6 months old. The adult BVM is used for all patients from 6> months of age to adult. Take care when ventilating infants and children with the adult BVM.
Ventilation and Airway Adjuncts
In adults, evidence suggests that in the very first period following a cardiac arrest (apart from a hypoxic arrest secondary to a respiratory or obstructive cause) passive ventilation (gas exchange through the mechanics of chest compression) is acceptable while commencement of CPR is undertaken, and an airway is secured. It is during this phase that we place greater emphasis on the value of compressions over ventilations. It would be reasonable to expect an AED analysis, defibrillation and a 2-minute cycle all commence while an i-Gel® is inserted for adult patients. The i-Gel® SGA has a recorded average of 11 seconds to insert and a 90% first-time insertion success rate.
Because of the quick and easy nature of the i-Gel®, and the fact that it can be inserted while compressions continue, it is reasonable to insert this adjunct in cardiac arrest in the first instance (instead of an OPA or NPA) unless no one qualified to insert an i-Gel® is on site.

i-Gel®

A majority of SAAS volunteer respondents to the post i-Gel® use survey reported successfully insertion on the first attempt. Quick insertion can be achieved especially by those AOs who frequently practice the technique on airway manikins.
The i-Gel® device ensures all ventilations are performed through an advanced airway (reducing the risk of gastric insufflation). Once secured the i-gel can reduce the cognitive load of the clinician ventilating. Remember in paediatrics, ventilate ASAP due to the likelihood of hypoxia being a reversible cause. This will be discussed further in Adult vs. Child resuscitation choreography later in this module.

55 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Covid-19 CPP 54 indicates best practice is to place the HME filter on the i- Gel® and cover the Gastric port with tape prior to insertion to reduce the chance airborne particle from the respiratory tract entering the environment. When possible, placing the patient’s head in the “sniffing the morning air” position increases the chance of successful insertion. The device must be adequately lubricated on all sides to ensure a greater chance of successful insertion. While transpore tape can be used to secure the device, if the patient has soiling on the face (e.g. vomit, blood) or has facial hair, using a traditional cotton tie may provide better securing of the device. The i-Gel® Clinical Practice Procedure has been updated to reflect that ICPs and Paramedics are now using the device.
Note: While AR/AOs may suction via the ventilation and gastric channels of the i-Gel® device using a standard soft Y suction catheter, ONLY ICP/Paramedics may use the longer orogastric tube and 50ml syringe. Likewise only ICP/Paramedics are authorised to attach the end-tidal (ETC02) device to the i-Gel®.

i-Gel® Training Video [08:00 minutes]

https://player.vimeo.com/video/216935522
Note This video includes a “simulated” cardiac arrest scenario using a live actor patient. During a real cardiac arrest, quality chest compressions expected of SAAS crews would be of the correct depth (1/3 of chest depth), rate (110 per minute) and recoil (complete release of the chest between each compression)


Both the airway channel and gastric channel can be suctioned as required. Size 10FG soft Y suction catheter is the most common one to use. Remember to lubricate the y-suction catheter before insertion into the gastric channel then suction as required.


The suction catheter can remain insitu. If airway soiling is significant remove the i-Gel® to clear the airway.
Clinical Practice Procedure - i-Gel® Supraglottic Airway [CPPRO-020]
Adult
Paediatric
During adult BLS CPR - Ventilate initially with Bag-Valve-Mask (BVM) using two-person BVM technique without an OPA/NPA. As soon as possible (any time after first AED analysis and shock/no-shock advice) insert an i-Gel® SGA airway. Don’t delay by inserting an OPA/NPA first. If the i-Gel® cannot be inserted after 2 attempts use an OPA/NPA.
During Paediatric BLS CPR - Ventilate with Bag-Valve-Mask (BVM) using two-person BVM technique with an OPA or NPA. The insertion of the i-Gel® SGA airway is delayed until further resources (beyond the initial primary 2-person crew) become available on site to assist (e.g. another SAAS responder/crew, other emergency services or suitable first aider capable of assisting with high-performance CPR). This ensures quality compressions and ventilations can occur during the preparation and insertion attempt of the i-Gel®.

56 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
2 Rescuer BVM/CPR technique


The 2 rescuer BVM technique in cardiac arrest is greatly encouraged before an advanced airway being inserted (i-Gel® or ETT) for both adult and paediatric patients.
Advantages:
• Two hands to jaw lift and hold the mask on, reducing the risk of leaks

• Decreases the risk of air in the stomach
• With the compressor bagging over or under ventilation is addressed (both over and under ventilating can significantly reduce survival)
• The compressor does not lean on the patient’s chest during ventila tions addressing any risk of recoil when ventilating
• The quality of CPR is improved = Increases rate of survival.
NOTE: In cardiac arrest, the 2 rescuer BVM technique is used primarily as the initial ventilation technique, as a rescue strategy when i-Gel® is not achievable or in paediatric arrest where hypoxia is the likely cause and insufficient resources are on scene to allow for i-Gel® preparation and insertion without interrupting compression/ventilation.
The single-rescuer BVM ventilation technique is now reserved for solo/single responder cardiac arrest management only.
When using the Bag-Valve-Mask (BVM) Resuscitator - ensure oxygen is connected, a flow rate of 15 litres per minute is set and the BVM reservoir bag inflates.


Two Rescuer BVM/CPR Technique [00:11 minutes]
https://player.vimeo.com/video/293885057
Cardiac Arrest Choreography - Pit Crew CPR
What was best practice 20 years ago, 5 years ago or even 1 year ago has and will change. We need to stay “on top of the game”.
• We are here to improve cardiac arrest outcomes in South Australia.
• For inspiration, to improve cardiac arrest survival we look at Seattle (USA). Seattle is often considered the benchmark for cardiac arrest survival.

• Using the Utstein criteria (the international research method which examines the statistics of bystander witnessed cardiac arrest and a presenting shockable rhythm (VF or VT), Seattle achieved 62% cardiac arrest survival. We currently sit around 35%, almost half of that. Don’t get too hooked up on numbers, just know we can do better than we are now.
F1 Pit Stops Old versus New [01:16 minutes]
https://player.vimeo.com/video/294701506
57
OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Continuing Education Program 2023 - Jan 2023
Why is their survival rates nearly double ours?
• They have widespread public access AEDs and an extremely robust system for ensuring everyone knows CPR (starting in 1974, more than half the population have been trained in CPR). There is that saying – “don’t fall asleep on a park bench in Seattle because someone will start CPR on you!”
• They have a high performing ambulance (EMS) service.
What do these high performing ambulance services have in common?
• Focus on HP-CPR.
• Using Pit Crew Models (that forms the structure of their approach).
• Robust Post ROSC (return of spontaneous circulation) management models. Salt Lake City – USA

Look kind of familiar?
The population of 1.1 million, street layouts based on a grid pattern. City/Metro area, flat urban area with nearby hills and a vast countryside also. Very similar to Adelaide?
They rolled out a pit crew model approach to cardiac arrest management and HP-CPR training in 2011. Then they looked at patient outcomes following this implementation and compared it to pre-implementation data and published their research.
In September 2011, Salt Lake City Fire Department EMS providers underwent a system-wide restructuring of care for OHCA patients that focused on the adoption of high-quality CPR with minimal interruptions and a pit crew model.

Am Heart Assoc. 2016 Jan 11;5(1). pii: e002892. doi: 10.1161/JAHA.115.002892 https://www.ncbi.nlm.nih.gov/pubmed/26755555
Their survival rates with neurological intact patients (no disability/brain injury on successful resuscitation) outcomes doubled from 8% to 16%!

58 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
OHCA Reaccreditation - CEP 2023
So, what will the SAAS Pit Crew model look like?
Ambulance Officer’s focus for 2018 was on high-quality CPR, the introduction of the i-Gel® supraglottic airway and the role of the community in CPR and AED use. We did look at some basics of scene logistics and how other services were using the pit crew model. We have since refined what SAAS pit crew CPR will look like. The key points are:

• Early recognition of cardiac arrest patient
• 360° Access
• Kit Dump
• Swift i-Gel® insertion (adults)


• Ventilation efficacy checked
• i-Gel® checked and secured
• CPR uninterrupted with advanced airway
• Metronome used

• Standardised language
• Use of the SAAS cardiac arrest aide memoire
Procedure - Moving an Unconscious Patient to the Floor [PRO-290]
Early recognition of cardiac arrest
Ambulance Officers routinely don’t check for a pulse during cardiac arrest.
We rely on no signs of life: absence of normal breathing (remember agonal ‘gasping” breaths are not compatible with life), no purposeful movements and unconscious/unresponsive to determine a patient is in cardiac arrest.
360° Access and Kit Dump
Reflecting on the Formula 1 (F1) pit crew:
• Is a controlled and well-rehearsed environment
• Everyone knows their job and does it
• They have 360-degree access to the race car
• There is a pit crew team leader.
It is beneficial to rapidly move the patient to a clear area in which 360-degree access can be achieved before commencing CPR if possible.
When we attend a vehicle crash rescue scene, we get to witness how our MFS/CFS/SES rescue colleagues set up “equipment dumps”. All rescue equipment is placed strategically on tarps. Everything has a place and everyone in the team knows where the equipment is. Regards of the vehicle crash location or type, the rescue dump is the same each time.
59 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
SAAS equipment should be placed strategically the same way regardless of the resuscitation that occurs in Rundle Mall, a workplace in Prospect, a residence in Kapunda or the Tumby Bay football oval.
The SAAS standardised equipment layout “kit dump” by the first arriving crew
SAAS community responders and PTS ambulance crews will place their green first response backpack where the blue airway kit is pictured, otherwise, the equipment positioning is the same.
Standardised Language

Just like a standardised kit dump, there will be standardised l anguage and instructions used in SAAS cardiac arrest management.
Putting it all together at the BLS level
The following short video shows the SAAS Pit Crew model in action. During your face-to-face workshop, you will practice these many times. Starting in a 2 person BLS team and progressing to a 4 person BLS team.
An example of a BLS HP-CPR situation. Note flexibility is required in terms of positioning based on the patient’s position, the skill level of crew members and the arrival of ALS providers who may attend. The key points areEarly identification of cardiac arrest, immediate chest compressions, early application of AED, call for clinical support, early i-Gel® insertion for adults, use of SAAS cardiac arrest aide-memoire and call to EOC Clinician.
Pit Crew CPR with BLS Providers (Ambulance Responder and Ambulance Officer) [06:36 minutes] https://player.vimeo.com/video/405713609
SAAS Cardiac Arrest Aide-Memoire and Team Leader

The initial pit crew starts with the first responder or first arriving 2-person ambulance crew, who will move in a pendulum manner switching between airway and compressions. Ideally, the pit crew model is at least 4 people, one who is the cardiac arrest leader.
A crew of 4 in country SA? - Is it possible?

It may not be 4 SAAS Ambulance Officers but it could be other people who can assist with quality CPR e.g. SAPOL, CFS, SES, Nurse, Surf Life Saving, St John First Responders at an event or first aid trained bystanders. You need to provide clear instructions and directions as well as feedback and coaching on their quality of CPR including rate, depth, recoil, etc.
ALWAYS ask for clinical support or another resource during a resuscitation. You just never know who is passing through your area who may be able to assist. Don’t assume you are alone.
60 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Resus Team Leader - Why?
‘There should be a team leader who is responsible for directing and co-ordinating the resuscitation’ (ANZCOR 2014).
‘Key leadership skills in resuscitation include critical decision-making and clear communication, especially with regard to task allocation and planning (Clarke et al. 2015).
‘The role of the team leader during CPR is known to be pivotal’. A randomised controlled study that involved crisis resource management (CRM) leader training found ‘emphasis on team leader behaviour appears to be beneficial in resuscitation.’ (Castelao et al., 2015).
Aide-Memoire
The use of an aide-memoire (stored in the defibrillator case) will allow the resuscitation team leader to check and progress through skills and tasks of care. As we see so few actual resuscitation cases compared to all other case types, the aide-memoire will reduce our cognitive load and stress during these low frequency-high risk and high emotion cases. The cards are 2-sided, one side for the cardiac arrest patient and the other side for use if/when ROSC is achieved. The cards are split into BLS, ALS and special circumstances. Ambulance Officers should follow the BLS checks and review the special circumstances. If ALS providers attend the case, the ALS sections can then be utilised.


Mobile CPR
As we review SAAS resuscitation practices it has become clear:
1. We need to continue resuscitative efforts much longer than we previously have in many cases.
2. There is a particular set of cardiac arrest patients who would benefit from transport to a health facility.
Ambulance Officers (in the absence of ALS providers) need to consult with the EOC Clinician during an adult cardiac arrest at the 10-minute mark to discuss the case and treatment plan. For paediatric cardiac arrest, an EOC Clinician consult should occur ASAP. Discuss with the EOC Clinician regarding mobilising to local health services vs. continuing resuscitation on-site and waiting for clinical support options.


Refer to the relevant Clinical Practice Protocols (access via SAASnet/Office 365 or SAAS Clinical App):
Clinical Practice Protocol - Cardiac Arrest (Adult) - Ambulance Officer [CPP-002-AO]
Clinical Practice Protocol - Cardiac Arrest (Paediatric) - Ambulance Officer [CPP-043-AO]
Continuing Education Program 2023 - Jan 2023
61
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
Ambulance Responders and Ambulance Assist working in the absence of an Ambulance Officer (or ALS provider) should refer to their relevant resuscitation Clinical Practice Protocols.
Clinical Practice Protocol - Cardiac Arrest (Adult) - Ambulance Responder [CPP-028-AR]
Clinical Practice Protocol - Cardiac Arrest (Paediatric) - Ambulance Responder [CPP-043-AR]
Clinical Practice Protocol - Cardiac Arrest (Adult) - Ambulance Assist [CPP-002-AA]
Clinical Practice Protocol - Cardiac Arrest (Paediatric) - Ambulance Assist [CPP-043-AA]
As a rule, for Ambulance Officers dealing with cardiac arrest patients should “Get Help” or consider “Getting to Help”. Clinical Support can come in the form of:
• Paramedic or ICP ambulance crews
• Paramedic or ICP solo responders including RTL, CTL, CSO, other managers and staff travelling through your area
• RERN Medical Officers
• Remote Area Nurses in some locations
• Ambulance Officers with Extended Practice credentialing (who can perform certain ALS skills under protocol/consult).
If the decision is made to mobilise to a health facility with the patient under CPR, the following needs to be considered:
• Any patient movement e.g. extrication from the house, movement to the stretcher, movement of the stretcher to the ambulance and transport in the ambulance to the health facility needs to be planned and safe
• Chest compressions ideally should not be stopped for any longer than 10 seconds. This means patient movement is not necessarily going to be rapid. HP-CPR shouldn’t be compromised during movement
• Mobile CPR will be particularly difficult without an i-Gel® in place
• You will need adequate help to make this happen. This may be other SAAS crews, emergency services or bystanders




• Ideally, the pit crew team leader should be in place and directing the movement and resuscitation
• Crew and patient safety.
Some key points:
• Slow, controlled movement: “slow down, we are in a hurry”.
• Chest compressions continue while moving the Stryker stretcher. The Stryker allows us to have the correct height to perform quality CPR. Effective compressions are possible on the Stryker mattress.
• All moves are pre-planned. Ideally no more than 10 seconds “hands of chest time”. However, you should note with the Stryker powerload system, hands-off chest time when loading in the ambulance will be approximately 13-15 seconds. You cannot do compressions while using the powerload system.
• Once in the back of the ambulance, everyone wears a seat belt except the clinician providing chest compressions.
• The pit crew resuscitation team leader sits in the front passenger seat and directs the resuscitation from this position. Documentation, ongoing communication with the EOC Clinician and notification to receiving health facility are their responsibility.
62 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
• The 2 clinicians in the rear patient cabin swap compressor/ventilation roles every 2 minutes (when the AED analyses), however, they do not swap positions. The BVM connected to the i-Gel® is moved to allow access to clinicians providing ventilations. Once a swap has occurred, the ventilator will secure themself with a seat belt.
• The driver of the ambulance needs to drive to road conditions, being aware that active CPR is being performed and one officer is unrestrained.
• The driver communicates with the clinicians about road surfaces, corners, railway crossings, etc.
• Although mobilising to the health facility under P2 emergency driving conditions, speed may not be beneficial. In fact, in many cases, the ambulance speed will be much slower than normal posted speed limits.
The following video shows a typical ambulance mobile CPR situation (from NSW Ambulance). Note the height of their stretcher, the uncoordinated movement of staff in the back of the ambulance, hands-off chest time, trip hazards of defibrillator cables, oxygen tubing and manual task issues. Immediately following we will show the proposed SAAS movement while under CPR (stretcher to the ambulance) and mobile to hospital.
Note: this video shows SAAS paramedics using the defibrillator in manual mode, however, the principles are identical for Ambulance Officers using an AED that will prompt you to stand clear are analyses every 2 minutes.

Mobile CPR Includes a comparison between a real case from NSW Ambulance and SAAS choreography [06:04 minutes] https://player.vimeo.com/video/286835107
Post-Rosc Care

Return of Spontaneous Circulation (ROSC)

Ambulance Officers will recognise ROSC when the patient:
• Starts breathing normally (not absent or agonal/gasping)

• Shows other signs of life such as purposeful movement
• Shows an increase in consciousness level (AVPU/GCS).
Note that even though a patient may start breathing normally, they may remain unconscious despite a ROSC being achieved. When such above signs of ROSC have been achieved, it is reasonable to then check a carotid pulse.
If there is any doubt that a ROSC has been achieved, continue CPR.
Immediate actions
• Stop chest compressions, leave the defibrillator turned on and keep defibrillation pads in place
• Be prepared the patient may re-arrest again. If this occurs res tart CPR and Defibrillation as per Clinical Practice Protocol
Continuing Education Program 2023 - Jan 2023
63
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
• Request clinical support if this has not already been done. Even in remote areas request as visiting SAAS clinicians/managers may be in the area or other HCPs such as RERN Doctors may be able to respond to assist. Don’t assume you are alone.
• Consider another SAAS crew of any clinical level or other emergency services i.e. SAPOL, CFS, MFS, SES to assist with extrication.
• Consult with the EOC Clinician if this has not already occurred. Their advice will be invaluable.
• When mobilising to a health facility early notification is required to ensure adequate staffing and in rural areas on-call medical and nursing staff can mobilise to the hospital ASAP.
On the reverse side of the aide-memoire is a Post-ROSC Management checklist. Refer to the BLS sections.

Airway
Depending on the patient’s conscious state, the inserted airway e.g. OPA, NPA, SGA (i-Gel®) may remain in place. However, if the patient is showing signs of a returning gag reflex and cannot tolerate the airway, it must be removed as soon as possible. NPAs are usually tolerated well with patients, even those with altered GCS. Suctioning of fluid, vomitus or blood from the oral and nasal cavity may be required. Any gross soiling of the airway may require you to posture the patient (head turned or rolled on their side) and be manually removed by the Ambulance Officer. Vomiting post-ROSC is common.
Breathing
Avoid hypoxia in a patient where ROSC has been achieved. Once ROSC has been achieved, oxygen saturation can be monitored by pulse oximetry.
Provide oxygen either via:
• Bag/valve/mask resuscitation with 15lpm of oxygen (BVM may remain connected to an SGA or used with a resuscitation mask). If actively ventilating or supporting respirations with the BVM, do not hyperventilate the patient (monitor your ventilation rate and volume).
64 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation
CEP 2023
-
• If the patient is breathing spontaneously and an SGA is not insitu deliver high flow oxygen via a non-rebreather oxygen mask (NRB) with 15 litres per minute of oxygen.
As a rule, if the patient remains unconscious and requires airway care and supportive ventilation, use the BVM resuscitator. If the patient is conscious and does not need ventilation support or an airway device, use the NRB or medium concentration mask.
Circulation

With a return of pulse, wound sites and lacerations may start to bleed again. Consider external bleeding control measures may be required. For potential pelvic fractures, consider the SAM Pelvic splint/binder. For long bone fracture e.g. femur, consider the use of the CT-6 traction splint.
Disability and or exposure
• Consider if sufficient resources are available to conduct a secondary survey (including exposure and checking of the whole body). This is very important if the patient has a trauma mechanism.
• Consider if manual spinal immobilisation, a cervical collar or a vacuum mattress is required. This is very important if the patient has a trauma mechanism.
• Take and record a blood glucose level (BGL). If the patient is hypoglycemic consult with EOC Clinician.
• Record other vital signs e.g. blood pressure (palpatory method as a minimum), pulse, respiration rate, pupil response to light and temperature (use tympanic thermometer stored in the Defibrillator case).

• If trained, record ECG - Lead I, II, III with monitor (print 10-second strip of each).
• Do not over warm the patient.
It is not uncommon for patients post ROSC to be combative and agitated. This is normally due to the period of hypoxia during cardiac arrest. Continue with high flow oxygenation.
At all times, be prepared for the patient’s condition to change and cardiac arrest to occur again. If the patient is unresponsive, stops breathing normally and shows no other signs of life, recommence cardiac arrest clinical practice protocol again (CPR and defibrillation). Do not rely on the presenting ECG on the monitor. Constantly reassess for signs of life.
Real-life resuscitation ROSC and care - London Ambulance [04:30 minutes] https://player.vimeo.com/video/295086583
What’s Documentation Got To Do With Cardiac Arrest Management?
It’s our ‘missing piece’.

Cardiac Arrest PCRs can be complex, with a lot of information to record, including treatment, reasoning, timings, mandatory data or declarations, and more. Trying to make sense of a PCR at a later time can sometimes feel like working on a jigsaw puzzle, and then finding you don’t have everything you need to complete the picture.
How do we measure our outcomes and modify our equipment, training and care if we don’t have an accurate picture of how we are performing?
The information that’s written on a Patient Care Record is used to:
• Identify trends
• Change practice
• Drive research
• Improve cardiac arrest survival.
There is a diverse range of completion standards for cardiac arrest PCRs. While it is fair to recognise that there will be variations in structure or writing styles between clinicians, there is a clear need to set a standard and highlight common omissions.
Continuing Education Program 2023 - Jan 2023
65
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
While how you write your PCR will be up to you, some things are not negotiable and are required by policies, procedures, guidelines or legislation, or otherwise prevent meaningful review or invalidate research if left out.

Correct Patient Identification
National Safety and Quality Health Service Standards V2
Australian Commission on Safety and Quality in Health Care – NSQHS Standards – Communicating for Safety Standard – Correct identification and procedure matching – Action 6.05 https://www.safetyandquality.gov.au/standards/nsqhs-standards/communicating-safety-standard/ correct-identification-and-procedure-matching/action-605

Correct patient identification is important not only for standards compliance and record-keeping, but has significant implications when applying Advance Care Directives, or to aid in establishing relevant history, e.g. information that might lead to identifying a reversible cause. Make sure you provide as much patient identification information as possible.
Patient identification is an important part of clinical care. It is confirmation that clinical information on the case card matches the patient and that you have attended the right person. Best practice requires at least 3 approved patient identifiers – because we transfer care to other facilities/HCPs, we will strive for 4 approved patient identifiers.
The approved patient identifiers we use in SAAS are:

1. Patient name (family and given name)
2. Date of birth
3. Gender
4. Address (including postcode).
If unable to identify the patient – write ‘unknown’ in the name/address/dob fields. In these situations, as much detail as possible should be recorded on the PCR. Useful information for this is:

• The location that the person was picked up from (recorded in the ‘from’ section).
• The time the person was picked up (recorded in the ‘arrived scene/patient’ time).
• The SAAS dispatch/event number, day and date.
• Physical description of the person (in the clinical documentation section).
Proper recording of patient identifiers is a requirement of NSQHS Standard 6 Communicating for SafetyAction 6.5
66 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
What has been missing or incomplete?
Some of the key areas on the front of the PCR are often missed or incomplete.
1. ID/Patient Information - Be sure to complete this every time. While you’re here – always record patient weight (known or estimated). It’s not only a statistical tool but helpful for case reviews where weight-based drug doses are used – remember your PCR needs to a useful, reviewable document.
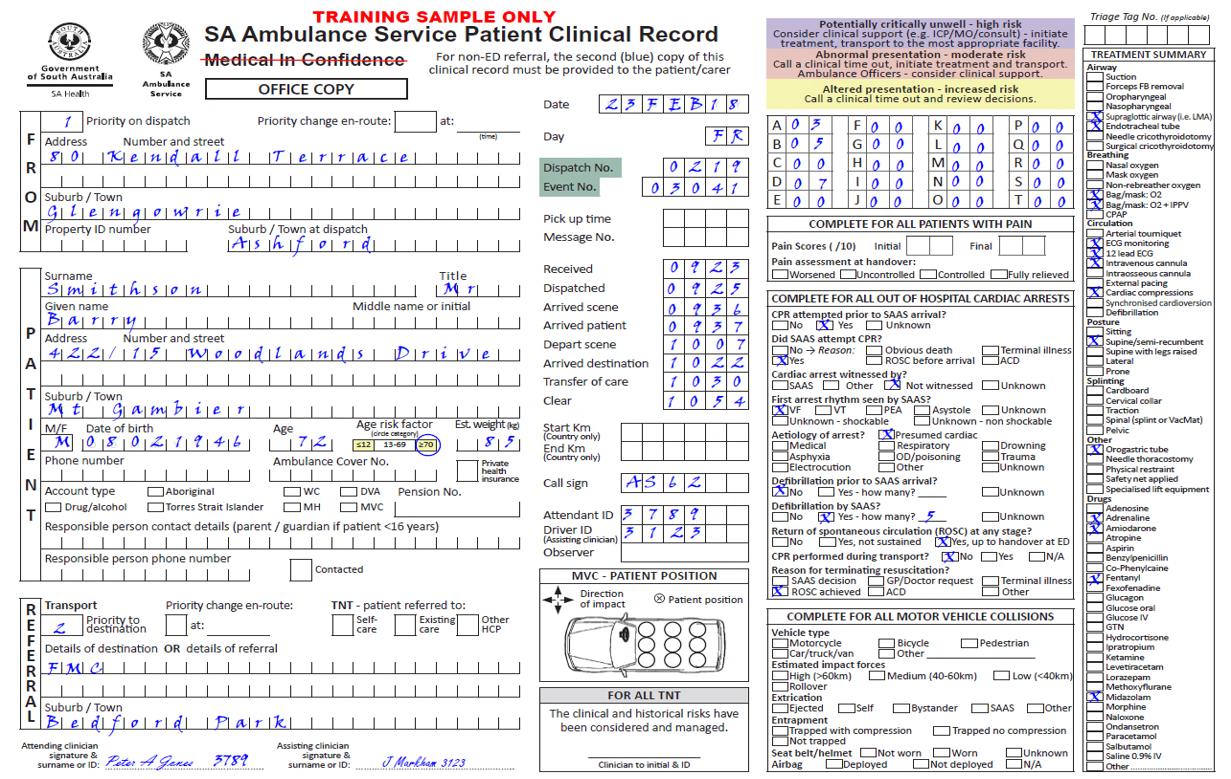
2. Event Number - Last 5 digits of the “1” number (underlined on MDT dispatch information); easy to search through EPAS system for patient management and follow up. This is in addition to the Dispatch “D” number.

3. Codes - The preferred option is to mark all codes with either a number or ‘00’. What is it used for?
o The first code (A) determines the type of bill a patient gets / if they get a bill.
o The remaining codes, while time-consuming is important for any clinical auditing. A number or ‘00’ (not applicable) should be entered for all active codes rather than left blank. Non-active codes can be left blank or crossed out.
- Examples of why these codes are useful:
o If we think we need a new cardiac drug, the audit team will review all cardiac D coded cases (01-12) –it is currently the most effective way to ‘search’.
o If SA Health wants to know how much violence and aggression SAAS operational staff encounter, the search will be for all K codes (01-04).
o If we want to review the safety and suitability of doing trauma bypass, perhaps with the view of expanding the scope of practice (hypothetical example only), then the H code needs to be completed. No data = no evidence to support change in clinical practice.
4. Treatment Summary - Completing these makes the review of cases much easier when looking for trends or instances of drug administration or other treatment e.g. the easiest way to see if a patient required suction, or was given adrenaline, without needing to read PCR.
5. Cardiac Arrest box – Lack of compliance makes data collected less useful. If Bystander CPR or AED occurred before SAAS arrival, be sure to complete the relevant section.
Continuing Education Program 2023 - Jan 2023
67
OFFICIAL OFFICIAL
Reaccreditation - CEP 2023
OHCA
Declaration of Life Extinct - We always plan for ROSC but sometimes we can’t always beat death and resuscitation will be terminated on site. A Declaration of Life Extinct may be added to the PCR by a Paramedic or ICP.

If no ALS staff are onsite and you are instructed to terminate CPR by the EOC Clinician, you should document “CPR ceased at (insert time) as per instruction of EOC Clinician (insert name)”. You are however not declaring life extinct.
The declaration must be personally completed and signed by the clinician making the declaration e.g. the Paramedic/ICP who does the examination, writes the declaration and sign it themselves.
“…Declaration of life extinct is a significant legal responsibility and can only be completed and signed by a clinician who is present with the deceased and authorised to do so following their CPGs. This task cannot be delegated to a clinician who does not hold this authority. The EOC Clinician, State Duty Manager or Medical Officers are not able to “authorise” this by telephone consult or at the scene…”
Clinical Communications –Scope of practice and consult authorization [CLC-17-023]
Readability
Tell the whole story and make it legible. During cardiac arrest case reviews, PCR standards have varied enormously. It’s often hard to understand what was done, and why. They may as well have been written in another language. Some are very brief; some are long and detailed. Many are missing important details and because they are missing, make the PCR difficult or impossible to review in a meaningful way. Sometimes the missing information is annoying, or frustrating, other times it creates an impression of clinical error or omission. Some missing information makes statistical reporting impossible. Some of the information recorded on PCRs is required for medico-legal reasons, including a declaration of life extinct, controlled substance recording or coronial and court cases.
Who writes the PCR?
You’ve just worked as a team to manage a complex case, now who writes the paperwork? The PCR is a collaborative document but is much easier to understand or review if only one person writes it. Ideally, the senior or experienced clinical person involved in the case should write the notes, in consultation with others present. Regardless of who writes the PCR, the senior or most experienced clinician is always responsible for the overall management of the case, so should sign the PCR anyway.

It is preferred that two signatures appear on the PCR; it helps to demonstrate collaboration and agreement. Be thorough, check you have included all relevant information and completed all of the relevant sections. This is another reason to have someone else check or read your PCR.
If you fill up all 6 places on the RDR observation chart, use a second PCR, NOT a Clinical Notes Supplement. This allows continued monitoring of trends as well as ensuring compliance with Policy and Procedures. If you have performed a complex skill, or a significant event has occurred, document it thoroughly. Ensure to number PCR “1/2, 2/2” etc. ensuring others know there are multiple PCRs for the case.
Be sure to attach your ECG code summary to all copies of the PCR and mark it with the patient identifiers, date and dispatch number. This is what makes it possible to review and understand your PCR at a later time. A reviewa ble document can be used to discover trends and develop improved systems.
If you need more room, use Clinical Notes Supplements. If you record more than 6 sets of observations, you MUST use another PCR to allow them to be recorded on the RDR chart.
• If you considered something, write it down.
• If you did something, write it down.
• If you did or did not get a result, write it down.
• If you have made a decision, write it down and state why you made it.
68 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
CEP 2023
OHCA Reaccreditation -
We got a ROSC!!!!
Record the time you notice ROSC on your PCR


• Either within your free text
Or
• In the Drugs or Intervention section
This data is being gathered and at this stage, there is no specific place to record it. We only ask that you write it somewhere. This means that if you have correctly filled out the Cardiac Arrest research box, and ROSC is ticked, the time will be looked for on review of the PCR.
Take away points
• Quality documentation can help to identify trends to improve practice and patient care
• Your PCR is the only record of what you did, will it make sense years from now?
• Remember to comply with policies, procedures and legal requirements
• If it isn’t recorded, it didn’t happen
All PCRs from cardiac arrest cases are returned in the orange cardiac arrest DX postage bag.
69
2023
2023 OFFICIAL OFFICIAL OHCA Reaccreditation - CEP 2023
Continuing Education Program
- Jan
Reconciliation Action Plan: Asking the Question
Learning Outcomes
• Ability to ask the standard question “Are you of Aboriginal or Torres Strait Islander origin?” correctly, for every patient



• Understanding why it is important to collect and record this information consistently for all patients, and how to do so
• Ability to clearly explain to patients the reason for collecting this information
• Understanding that providing an answer is voluntary, and can be changed by the patient at any time

• Enhanced capacity to handle a poor response to the question
South Australia is the fourth largest of Australia’s states and territories, covering more than 983,000 square kilometres. SA Ambulance Service provides out-of-hospital emergency patient care and transport as well as a non-emergency patient transport service, for our population of more than 1.7 million people, living in metropolitan, country and rural and remote communities across this vast state
Aboriginal and Torres Strait Islander people are the Traditional Owners of country throughout South Australia. They have one of the oldest and richest histories in the world and we acknowledge their spirituality, culture and their deep connection to the land that we live and work on.
Evidence shows us that many Aboriginal and Torres Strait Islander people are at greater risk of some health problems - as frontline health providers, we can bring these people to the services they may need sooner. That’s why identifying Aboriginal and Torres Strait Islander people at the point of care is so important. The aim of this module is to provide you with information that will help you do that confidently, so you can support Aboriginal and Torres Strait Islander patients in accessing and achieving improved health outcomes.
Welcome to this module SAAS CEO Mr Rob Elliot (00:48 minutes) https://vimeo.com/764350558
70 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
CEP
Reconciliation Action Plan: Asking the Question -
2023
The Question
Before we begin, how does the idea of asking “Are you of Aboriginal or Torres Strait Islander origin?” make you feel?
Research suggests that the common reasons, difficulties or concerns healthcare workers have in asking the question include:
• Fear of provoking aggressive responses (from both Aboriginal and non-Aboriginal people)
• Data is used to justify bureaucracy (i.e. funding)
• Response may have a bearing on the standard of treatment the patient receives (better or worse)
• Might offend the patient
In reading these statements, which ones resonate with you?
How to Ask the Question:
When it comes to asking the patient, it is important to use the standard phrase consistently, each and every time you treat a patient.
The standard way to ask is ‘are you of Aboriginal or Torres Strait Islander origin?’


Ask the question consistently and uniformly of all patients – do not modify. Changing the wording, even slightly, has the potential to alter the meaning of the question and may influence the patient’s response
The timing of when to ask the question is up to you and may differ with each episode of care. As a guide, aim to ask as soon as practical during patient assessment (for example, when asking other standard questions or when observations are being taken)
If you feel a pre-amble is necessary, say ‘the following information will assist in the planning and provision of appropriate and improved health care services’.
71 Continuing Education Program 2023 - Jan 2023
OFFICIAL
- CEP 2023
OFFICIAL
Reconciliation Action Plan: Asking the Question
Tips for Asking the Question:
• Ask in a respectful manner without anticipating or making assumptions
• Don’t make assumptions about the patient’s identity or about how the patient is likely to react
• Regard the question as no more or less sensitive, or problematic than other items of personal data routinely collected
Did you know that all patients have the right to self-report their status, then have it assumed?
Did you know that refraining from asking is in fact an act of discrimination? Why? Because not asking infringes on the patient’s right to respond to the question themselves
Exceptions on When to Ask the Patient
All patients should be given the opportunity to respond to the question but there will be occasions when you may need to decide whether to ask or not to ask
Situations like this might be if:
• The patient is too ill to be questioned or is unable to respond to questions
• If the patient does not speak or read English
• If the patient is a child under the age of 15
• In situations like this, it is appropriate to ask the parent or caregiver
Strategies If Not Well Received:
• The patient has the right to decline to answer
• Tell the patient their level of care and access to services will not be affected if they choose not to answer the question.
• While we have a duty of care to collect information as correctly as possible, staff are not obliged to convince disgruntled, upset, or unwilling patients to respond to the question.
• If queried by a patient as to why the question is being asked, staff are not obliged to justify the use of standard question
• Staff are not expected to tolerate or engage with aggressive patients in the interest of eliciting a response to asking the question. If the question elicits an aggressive response do not pursue the question anymore.
Prepared Answers
What if the patient wants to know why they have been asked?

It is normal for people being asked any question to want to understand why they are being asked, asking someone if they are of Aboriginal or Torres Strait Islander origin is no exception.
While we don’t need to justify while we have asked, some of these prepared answers may help the patient to understand why and therefore feel more at ease.

72 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
the Question - CEP 2023
Reconciliation Action Plan: Asking
QUESTION 1:
Q1: Why are you asking me this question when I don’t look Aboriginal or Torres Strait Islander?
A1: South Australia is a multicultural place and there are many differences in appearance between Aboriginal and Torres Strait Islander communities as well as the broad range of other ethnic communities we provide services to –it’s not possible to tell from appearance and the only way to know is to ask.

QUESTION 2:
Q2: Why do you need that information? Will I get treated differently?
A2: The statistics are important for improving Aboriginal and Torres Strait Islander health
QUESTION 3:
Q3: Why should they (Aboriginal and Torres Strait Islander people) get special treatment?
A3: The information we collect allows health planners to find out why the health of Aboriginal and Torres Strait Islander people is not as good as the health of the general population.

QUESTION 4:
Q4: Does answering this question change the way I will be treated?
A4: No, it won’t change the way you are treated by health staff. However, complete and accurate records will ensure timely access to your clinical information and improve the quality of your care.
QUESTION 5:
Q5: Who is going to use this information?
A5: Only healthcare workers and those involved in the management of the health system will have authorised access to the information. Individuals will not be identified if the data is used outside of the health service.
Research on Why Patients Should Be Asked
The Australian Institute of Health and Welfare has reported chronic diseases such as cardiovascular disease, diabetes, mental disorders and chronic lung disease occur more often and at a much younger age amongst Aboriginal Australians compared with non-Aboriginal Australians.
National data taken from years of research and studies show that there is a clear 20-year health gap between aboriginal and non-Aboriginal Australians.
73
Education
2023
Jan 2023 OFFICIAL OFFICIAL
the
- CEP 2023
Continuing
Program
-
Reconciliation Action Plan: Asking
Question
This graph shows around four years of clinical risk mapping data relating to SAAS events per age range.
The Y axis represents patient age ranges in four-year groups. The higher we travel up the Y axis, the younger the age range of the patient event.
The X-axis represents the percentage or volume of cases attended within each age range.


The orange section on the left-hand side of the graph represents non-Aboriginal patient data and the blue section on the right-hand side represents Aboriginal patient data there are a few key points we’re about to highlight about this graph.


It should be recognized that whilst these key points are lined with known national data, there are assumptions or extrapolations made about SAAS data and correlating national information.
The first key point is the accuracy of the SAAS-specific information collected is relying on us asking the question, are you of Aboriginal or Torres Strait Islander origin?
The second key point is the peak age range for ambulance attendance for non-Aboriginal patients is around 65 to 89 years.
74 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
CEP
Reconciliation Action Plan: Asking the Question -
2023
Reconciliation Action Plan: Asking the Question
In comparison, the peak age range for ambulance attendance for Aboriginal patients is around 25 to 59 years. While several reasons could account for the significant difference in peak age range is one of the considerations must be the well-defined 20-year health gap between aboriginal and non-Aboriginal Australians.
The final key point is the significant decline in ambulance attendance for Aboriginal patients, most noticeable after the age of 75. This points to a shorter lifespan of Aboriginal and Torres Strait Islander people and needs to be considered.
So what can we do with this information?

As a clinician, there are specific circumstances where consideration of a 20-year health gap is very relevant. These may include age-related comorbidities in the clinical picture or risk of any assessed patient or when referring to the RDR chart for consideration of patient risk.
Knowing if a patient is of Aboriginal or Torres Strait Islander origin is important for referrals to another health stream. For example, non-Aboriginal patients over 65 years are eligible for My Aged Care, whereas Aboriginal or Torres Strait Islander patients are eligible if over the age of 50.
Always keep the 20-year age gap in mind as certain clinical assessments or standards may also apply at an earlier age for Aboriginal or Torres Strait Islander patients. An example of this is the 4AT assessment for delirium, which is routinely applied at 65 years but is applied at 45 years for Aboriginal or Torres Strait Islander patients.
INEQUITY IN HEALTH
Research suggests there is an inequity between the health of Aboriginal and non-Aboriginal patients. “20-year health age gap”
UNDER IDENTIFICATION
Under identification creates difficulties in measuring the gap in health outcomes and understanding Aboriginal people’s preferences in the health services they access, and need, to achieve the best healthcare outcomes.
WE CARE
Evidence shows many Aboriginal people are at greater risk of some health problems and we want to reduce these risks. Therefore, we want to encourage Aboriginal patients to access specific services that will help reduce the health risk for the patient.
COMPLEX NEEDS
Some Aboriginal and Torres Strait Islander patients have complex needs, or certain health conditions, and may need different choices of information.
THE DATA IS IMPORTANT
The collection of data helps us to better understand and assess the health issues of Aboriginal patients so we can improve services and the well-being of all our patients
IT’S THE RIGHT THING TO DO
We cannot guess or make assumptions about a patient’s origin. Therefore, providing the patient with an opportunity to identify themselves and their origin is the right thing to do.
Continuing Education Program 2023 - Jan 2023

75
OFFICIAL OFFICIAL
- CEP 2023
Cultural Reason Why Patient’s Should Be Asked
Lived Experience with Sharon Meagher Adnyamathanha (05:50 minutes) https://vimeo.com/764345905/dbc0b9cc1a
Asking the Question, and Recording the Answer
The patient care record reflects that all patients must be provided with the opportunity to self-report if they are of Aboriginal or Torres Strait Islander origin. Recording the patients answer consistently is important for the data to be recorded accurately.
If the answer is no, or you are unable to get an answer, such as the patient refusing to answer or the answer can’t be obtained, that’s OK. In these instances, leave the Aboriginal and Torres Strait Islander boxes blank.





If the patient responds yes to being asked if they are of Aboriginal or Torres Strait Islander origin, tick or shade, the box is shown. Record the answers the patient gives you, even if you know the patient’s status and their answer contradicts this knowledge. You must not make your own assumptions, and you must not document your own views in any way.

The patient may choose to change their original response. This is OK and should be received without comment because the patient is not required to provide a reason for why they’re changing their status.
If they answered yes and they have changed their response to know, simply strike out the box that has been ticked or shaded and right ‘N’ to the right.
If they answered no, and they’ve changed their response to yes, tick or shade the box.
76 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL
Asking the Question - CEP 2023
Reconciliation Action Plan:
Summary On Why It’s Important to Ask Every Patient
Asking “Are you of Aboriginal or Torres Strait Islander origin?” correctly and consistently is important because doing so:
• Provides an opportunity for the patient to self-report their identity and origin
• May help to identify more suitable health pathways for best patient health care outcomes

• Reminds us about inequity in health - consider the 20-year age gap when using the RDR chart for Aboriginal or Torres Strait Islander patients
Continuing Education Program 2023 - Jan 2023

77
OFFICIAL
OFFICIAL
CEP 2023
Reconciliation Action Plan: Asking the Question -
It is the right thing to do
Glossary
Term Definition
Chickenpox
An infectious disease causing a mild fever and a rash of itchy inflamed pimples which turn to blisters which then from scabs. It is caused by the varicella zoster virus and mainly affects children
Common cold A common infection in which the mucous membrane of the nose and throat becomes inflamed, typically causing running of the nose, sneezing and a sore throat.
Comorbid Relating to a medical condition that co-occurs with another.
Disinfectant A disinfectant is a chemical agent that rapidly kills or inactivates most infectious agents.
Gastroenteritis Inflammation of the stomach and intestines, typically resulting from bacterial toxins or viral infection and causing vomiting and diarrhoea.
Giardia lamblia A parasite responsible for a contagious form of diarrhoea and is most commonly transmitted through direct contact with infected faeces or by eating food or drinking water contaminated by faeces. It is one of the most common intestinal parasites in the world.
Haemophilus influenza Type of bacteria that occurs in the human respiratory tract and causes acute respiratory infections, acute conjunctivitis and meningitis.
Head lice Lice which infests the hair of the human head and that feeds on blood from the scalp. It is especially common amongst schoolchildren.
Hepatitis A Inflammation of the liver caused by a virus. It varies in severity, generally starts within 2 to 6 weeks after contact with the virus, and lasts no more than 2 to 3 months.
Hepatitis B Potentially serious form of liver inflammation due to infection by a virus. Some people who develop hepatitis do not develop symptoms. In its chronic form, the infection may destroy the liver through scarring and may lead to cancer in the liver. In the acute setting, most patients will recover within three months.
Human immunodeficiency virus (HIV)
A virus that attacks the immune system.
Influenza A highly contagious viral infection of the respiratory passages causing fever, severe aching, and catarrh and often occurs in epidemics.
Malaria An intermittent and remittent fever caused by a protozoan parasite which invades the red blood cells and is transmitted by mosquitoes in many tropical and sub-tropical regions.
Measles
Meningitis
An acute, contagious viral disease, usually occurring in childhood and characterised by the eruption of red spots on the skin and fever.
A serious disease in which there is inflammation of the meninges, the thin membrane covering the brain and spinal cord, it is most commonly caused by infection.
Meningococcal disease Can refer to any illness that is caused by the type of bacteria called meningococcus. These illnesses are often severe and include infections of the lining of the brain and spinal cord (meningitis) and bloodstream infections (septicaemia).
Methicillin Resistant Staphylococcus Aureus (MRSA)
Microbes
Causes infection the becomes resistant to antibiotics commonly used to treat ordinary staph infection.
A microorganism, especially a bacteria causing disease or fermentation.
Microorganism A microscopic organism, especially bacterium, virus or fungus.
Mildew
A superficial coating or discolouration of organic material, such as cloth, paper or leather caused by fungi, especially under damp conditions.
78 Continuing Education Program 2023 - Jan 2023 OFFICIAL OFFICIAL Continuing Education Program 2023 STUDY GUIDE
Term Definition
Mould
Multi-resistant organism (MRO)
Normal flora
Protozoan
Ringworm
Salmonella
Scabies
Telophase
Tetanus
A growth of minute fungi forming on vegetable or animal matter, commonly a downy or furry coating and associated with decay or dampness.
MROs are bacteria that have become resistant to the antibiotics normally used in their treatment. MROs are often linked to treatment in hospitals or other healthcare facilities but can also affect people in the community
Microorganisms that live on another living organism (human or animal) without causing disease.
Single celled microscopic organism that is capable of movement that ingests food.
A contagious itching skin disease occurring in small circular patches, caused by any number of fungi affecting chiefly the scalp or the feet.
Any of several rod-shaped bacteria that enter the digestive tract in contaminated food causing food poisoning.
A contagious skin disease caused by a parasitic mite and characterised by intense itching and small raised red spots.
The final phase of cell division.
An acute, often fatal bacterial disease

79
Education
2023 - Jan 2023 OFFICIAL OFFICIAL Continuing Education Program 2023 STUDY GUIDE
Continuing
Program


For more information SA Ambulance Service GPO Box 3 Adelaide SA 5001 Telephone: 1300 13 62 72 www.saambulance.com.au © SA Ambulance Service. All rights reserved. Version 1.0 221031