TOP DOCTORS
OVER 100 PROVIDERS ACROSS 30+ SPECIALTIES ELECTED BY THEIR PEERS in the Greater Chattanooga Area

ER Doctors: Care During Crisis
Meet Five Dedicated Emergency Room
Doctors
LIFE FORCE Air Medical Service in the Skies
Answering the Call
Graduate Students Pursuing a Passion for Healthcare
Women’s Venous Disease Is Real— And Often Misdiagnosed
Women’s Venous Disease Is Real— And Often Misdiagnosed


Pelvic Congestion Syndrome (PCS), May-Thurner Syndr ome, and Chronic Venous Insufficiency are common yet underdiagnosed conditions that disproportionately affect women—especially those wh o’ve had children.
Pelvic Congestion Syndrome (PCS), May-Thurner Syndr ome, and Chronic Venous Insufficiency are common yet underdiagnosed conditions that disproportionately affect women—especially those wh o’ve had children.
Symptoms may include:
Symptoms may include:
• Chronic pelvic or groin pain
• Chronic pelvic or groin pain
• Visible veins in the pelvic area or upper thighs
• Leg heaviness, aching, or swelling
• Visible veins in the pelvic area or upper thighs
• Leg heaviness, aching, or swelling
• Pain that worsens with standing, menstruation, or at the end of the day
• Pain that worsens with standing, menstruation, or at the end of the day
At the Vascular Institute of Chattanooga, we’re the only regional center offering comprehensive, accredited vein care for both superficial and deep venous disorders. Our non-surgical, image-guided treatments—like pelvic vein embolization and venous stenting—can help you get your life back. With advanced imaging, minimally invasive treatments, and a women-centered approach, the VIC team delivers vascular care that’s a priority, not an afterthought.
At the Vascular Institute of Chattanooga, we’re the only regional center offering comprehensive, accredited vein care for both superficial and deep venous disorders. Our non-surgical, image-guided treatments—like pelvic vein embolization and venous stenting—can help you get your life back. With advanced imaging, minimally invasive treatments, and a women-centered approach, the VIC team delivers vascular care that’s a priority, not an afterthought.
Take control of your health care.
• No referral needed
Take control of your health care.
• Appointments within one week
• No referral needed
• 6 convenient locations.
• Appointments within one week
• 6 convenient locations.
423.602.2750
423.602.2750


Treat


Provider




Since 1930. Trusted for Generations.

Cailey Mullinix Easterly CO-PUBLISHER
Celebrating 36 Years! HealthScopeMag.com
Follow HealthScope® and CityScope® magazines and Choose Chattanooga®Chattanooga Resource & Relocation Guide® on social media!
“The best way to find yourself is to lose yourself in service to others.” - Mahatma Gandhi
Although we never wish for it, it’s inevitable that at some point in our lives a loved one or even ourselves will need the expertise of a medical professional. In these times, we are fortunate to live in an area that is burgeoning with outstanding, compassionate medical providers. These individuals have studied, researched, and dedicated their lives to providing the highest level of care to their patients.
To honor these incredibly skilled professionals, this issue of HealthScope® magazine recognizes several of our area’s most trusted and respected physicians and showcases people and practices that are making a difference in our communities.
To start, the article “Care During Crisis” profiles five local ER doctors who provide critical care and comfort when it matters most. Next up, a feature on LIFE FORCE Air Medical provides insight into this crucial organization and spotlights individuals who provide life-saving care. Lastly, in “Answering the Call,” four of our region’s most dedicated nursing and medical students share what drives their path and passion towards a career in healthcare.
Not to be missed is the special section “Top Doctors.” This brand-new annual section presents many of our region’s most exemplary physicians, as selected by their peers and thoroughly vetted by Castle Connolly, the leading physician research firm.
More special sections and health insights await. In “Meet Our Caregivers,” you will meet six local caregivers who have dedicated their careers to serving others, while the annual “Advancements in Medicine” section features seven medical advancements that local providers offer for the highest level of care.
Last but certainly not least, topics ranging from styling scrubs, avoiding burnout at work, and a local guided workout are just a few pages away.
We hope you enjoy this issue of HealthScope® magazine and that you join us in a moment of gratitude for the individuals who have dedicated their schooling, careers, and lives to caring for our community.
Happy reading,

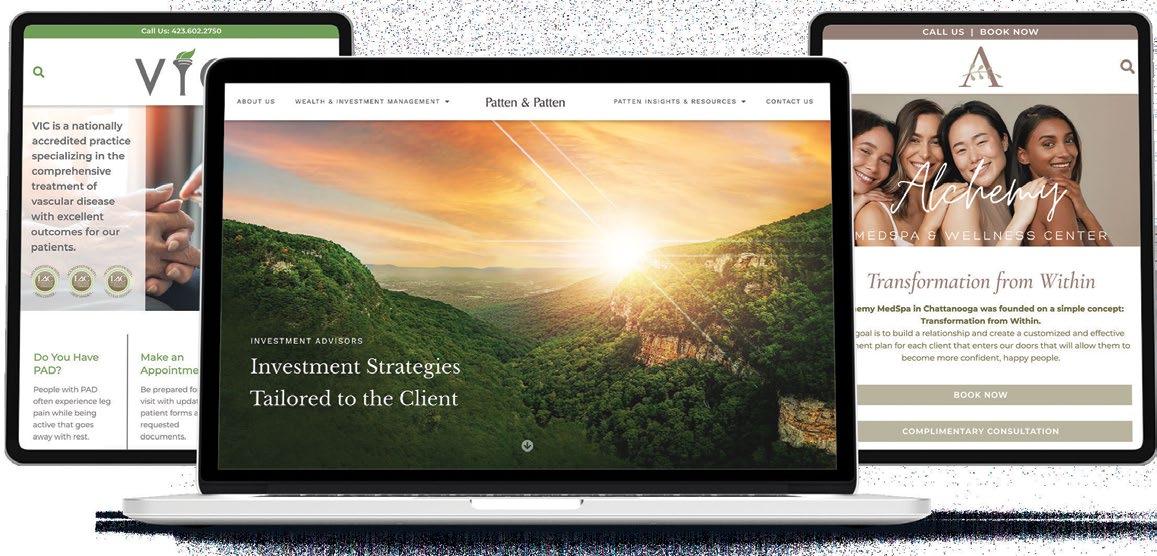
We’ve assembled a team of well-established and highly experienced financial professionals. It has given us the ability to address every aspect of our clients’ financial needs. And by limiting the number of clients we serve, it allows us to offer an uncommon level of service and maintain our unwavering focus on helping to create quality financial solutions.
This is what we bring to the table – and what will ultimately bring you to us. If you are an individual seeking seasoned financial guidance and the comfort of working with an experienced group of advisors who call Chattanooga home, we welcome the opportunity to sit down together. Main Office: 1200 Premier Drive, Suite 100 • Chattanooga, TN 37421 Downtown Office, by appointment only: Warehouse Row • 1110 Market Street, Suite 210 • Chattanooga, TN 37402 www.RoundTableAdvisors.com • 877-770-0009 • 423-510-8889





Burnout Blues Breaking Down Occupational Burnout
Together The Importance of Support Systems
&
Skincare for Healthcare Professionals Four Products to Amplify Your Routine
Styling Scrubs Practical, Professional Ways to Express Your Personality
Guide to Trauma-Informed Design Creating Spaces With Care
Beyond the 9 to 5 Keeping Relationships Strong With an Unconventional Schedule








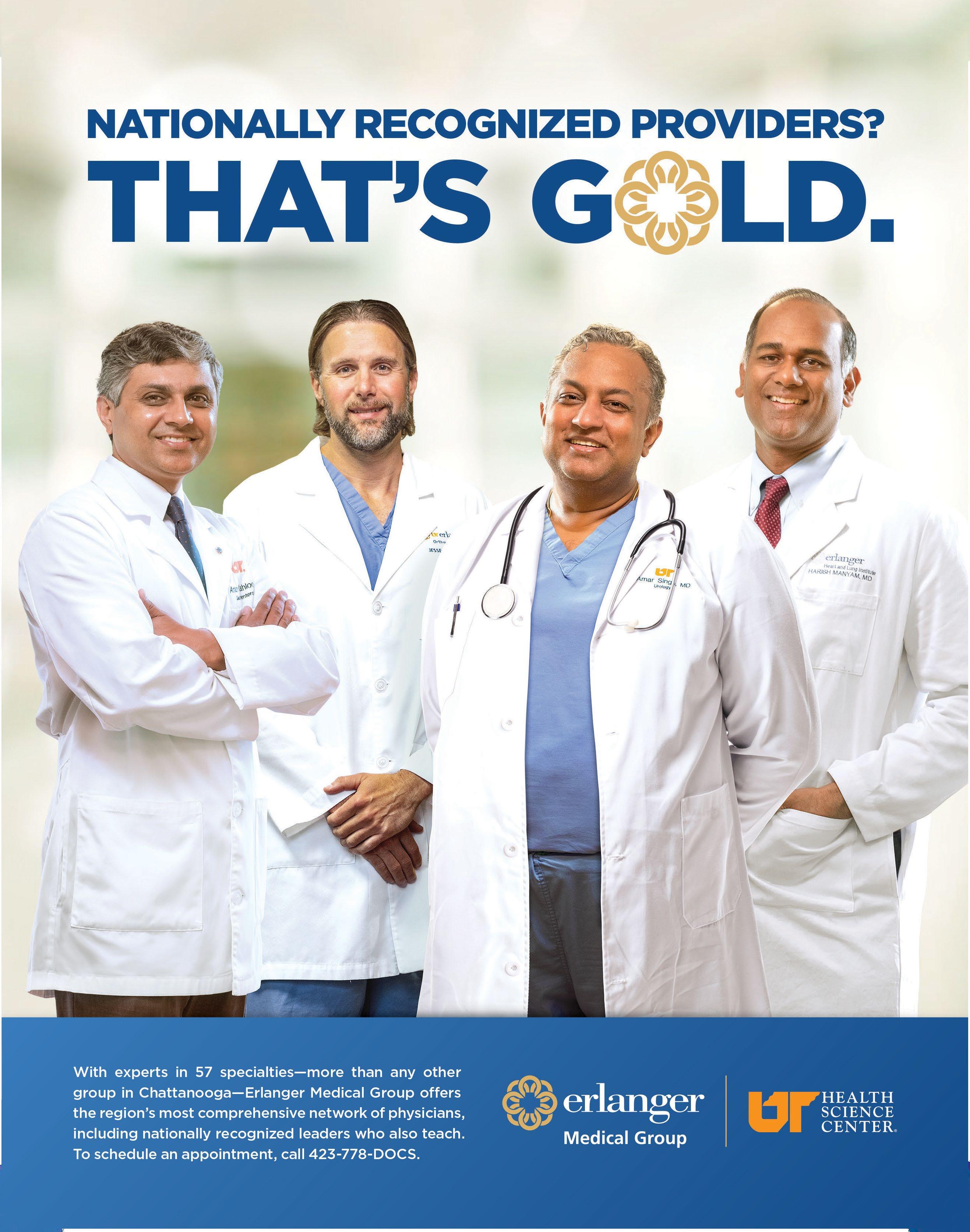
Vitruvian Health is more than a new name it’s the next chapter in trusted care for northwest Georgia and southeast Tennessee. W ith the combined strength of Hamilton Medical Center, Bradley Medical Center, and a team of over 200 physicians across 30+ specialties, Vitruvian Health brings nationally recognized care to your neighborhood. We’re proud to celebrate all our physicians, 2025
This is Vitruvian Health.
Schedule your appointment today!

HealthScope® magazine’s firstever Top Doctors Issue recognizes many of the greater Chattanooga area’s dedicated providers across 30+ specialties and celebrates the outstanding medical care available in our community.
Publisher George Mullinix
Co-Publisher Cailey Mullinix Easterly
Sales & Business
Development Amanda Worley
Sales & New Business
Development Meredith McNeeley
Design Lead,
Sr. Graphic Designer Lauren Robinson
Sr. Graphic Designer Tamara Slocum
Managing Editor Rachel Studebaker
Editors Kristen Dee Tory Irmeger
Editors/Digital Content Specialists Lindsey Clute Ali Lemmons
Digital Marketing Manager Houston McLain
Digital Marketing Intern Joshua Underwood
Marketing, Events, & Operations Laci Lanier Jackson
Photographers Hacker Medias Kristina Armstrong Rich Smith
Subscribe to CityScope® or HealthScope® magazines: Call 423.266.3440 or visit cityscopemag.com or health scopemag.com and click “Subscribe.” A one-year subscription for CityScope® or HealthScope® magazine costs $18.
To receive advertising information, change your mailing address, or share your views on editorial: Call 423.266.3440 or visit cityscopemag.com or healthscopemag.com and click “Contact.”
CityScope® and HealthScope® magazines and Choose Chattanooga® – Chattanooga Resource & Relocation Guide® (the magazines) are published by CMC Publications, LLC, a Chattanooga, Tennessee company. Reproduction in whole or in part without written permission is strictly prohibited. Views expressed herein are those of the authors or those interviewed and not necessarily those of the publisher, editors, or advertisers. The publisher, editors, and advertisers disclaim any responsibility or liability for such material. All content associated with and included in advertisements (ads, advertorial, and special promotional sections) placed in the magazines are the responsibility of the respective advertiser. CMC Publications, LLC, cannot and does not assume responsibility for any material contained within or associated with any advertisement.
CityScope® magazine
Copyright, CMC Publications, LLC, 1993
CityScope® magazine is a registered trademark owned by CMC Publications, LLC.
HealthScope® magazine
Copyright, CMC Publications, LLC, 1989
HealthScope® magazine is a registered trademark owned by CMC Publications, LLC.
Choose Chattanooga® – Chattanooga Resource & Relocation Guide®
Copyright, CMC Publications, LLC, 2011
Choose Chattanooga® and Chattanooga Resource & Relocation Guide® are registered trademarks owned by CMC Publications, LLC. Choose Chatt™ and Chatt Choices™ are trademarks claimed by CMC Publications, LLC.
CityScope® magazine Southern Gentleman® is a registered trademark owned by CMC Publications, LLC.


health in a minute
QI’m caring for my mother and starting to feel easily irritated and withdrawn while helping with end-of-life care – is this a sign of compassion fatigue, and what coping strategies can help?
A. Yes, feeling irritable and withdrawn while providing end-of-life care can be signs of compassion fatigue. This can develop when caregivers prioritize others’ needs over their own, especially during intense caregiving periods. It’s important to recognize these signs early and know you’re not alone. At Alexian PACE, we understand that caring for a loved one is both meaningful and demanding –that’s why we make it a priority to support our caregivers. We offer counseling and a team of professionals to support you, along with a supportive adult day center to give both caregivers and participants the care and respite they need.
Coping strategies like setting boundaries, taking breaks, and connecting with others can make a big difference. Caring for yourself is essential to continue showing up with compassion for those you love.
Lorna Birch, MD

Q. What are some early signs of codependency in romantic relationships, and what approaches are commonly used to help couples navigate it?
A. Codependency in relationships involves both internal and relational dysfunction, often rooted in low self-worth and insecure attachment styles. It can stem from childhood experiences, generational or cultural patterns, abuse, neglect, dysfunctional family systems, or trauma. Common symptoms include: over-functioning while a partner under-functions (common in addiction dynamics), difficulty setting healthy boundaries, fear of abandonment, people-pleasing, control issues, low self-trust, resentment, trouble receiving,
a strong need for external validation, and manipulation to get needs met – often without realizing it. Many also struggle to even identify their own needs. Codependency is something people can heal and grow out of with deliberate healing and work. This is a very common dynamic I work with in my practice, and I more than welcome those reading to reach out if you may be interested in learning more about how to overcome codependency in your own story.
Karisa
Kaye, LMFT, CST
Q. My husband recently had minimally invasive thyroid surgery and his voice is very hoarse. When can he expect his voice to return to normal?
A. In any approach to thyroidectomy, some degree of postoperative voice change is fairly common, and the extent of change ranges from minor alterations of voice pitch or tone to profound hoarseness or difficulty controlling air escape and voice fatigue. Both mild and severe symptoms can be the result of intubation-related trauma, local inflammation about the nerves that control voice (superior laryngeal nerve and recurrent laryngeal nerve), traction or compression trauma to the nerves, or direct injury to one of the nerves. Most often, voice changes begin to improve or totally subside within a few weeks. Less frequently, symptoms may remain significant to the patient (and the surgeon) for several months and gradually resolve. Rarely, voice changes or impairment fail to improve or are life-altering and may need to be addressed. Noninvasive vocal training can be beneficial, and interventions including surgery to improve voice are available in some centers. Michael Roe, MD, FACS

Lorna Birch, MD Medical Director, Ascension Living Alexian PACE ascensionliving.org/alexianpace

Karisa Kaye, LMFT, CST Licensed Marriage and Family Therapist, I Love Us Relationship & Intimacy Counseling iloveusintimacy.com
Q. What can be done to help with teeth grinding and clenching related to TMJ?
A. TMJ pain is often the result of overuse. During the day, the muscles that move the jaw are active while eating, talking, etc. If you also use them excessively by clenching during the day, and/or grinding your teeth at night, the muscles become overworked and sore. During the day, you can consciously try to keep your teeth apart or unclenched. In fact, teeth should only touch when you swallow. If you wake up with sore jaw muscles, you may be grinding your teeth in your sleep. Ask your dentist about getting a night guard that keeps the teeth apart at night and breaks the muscle feedback loop that allows grinding.
Bill Childress, DDS, MD
Q. I’m already using a retinoid at night – can I combine it with a hyaluronic acid serum, or should I alternate them?
A. Retinoids and hyaluronic acid serum are both great skincare product choices for anti-aging. Retinoids work by helping the skin turn over more quickly, which unclogs pores and helps reduce sun damage. Retinoids also stimulate collagen production, which helps reduce fine lines and acne scarring. Retinoids, however, can cause irritation and dryness of the skin, especially with first use. Hyaluronic acid serum acts as a humectant by drawing water into the skin for a plumping effect. I like to apply my hyaluronic acid serum after using my nightly retinoid cream to help reduce dryness and irritation. They work perfectly together and make a great combo for amazing looking skin. Laura Cleary, MD, FAAD

Michael Roe, MD, FACS General/Endocrine Surgeon, University Surgical Associates universitysurgical.com

Bill Childress, DDS, MD Oral Surgeon, Implants & Oral Surgery of Chattanooga ioschattanooga.com

Laura Cleary, MD, FAAD Dermatologist, Four Bridges Dermatology & Cosmetics 4bridgesderm.com
staff spotlight

HAMILTON MEDICAL CENTER
Madison Mills, MHA, BSN, RN, CNOR
Hamilton Medical Center’s Surgical Services director, Madison Mills, recently received the DAISY Leader Award for Extraordinary Nurse Leaders. The DAISY Leader Award recognizes exemplary nursing leadership excellence. The nominations commended Mills for her kindness, patient-centered approach, mentoring skills, support, compassion, and passion for her work.

HAMILTON MEDICAL CENTER
Alison Caraway, RN
Alison Caraway, a member of Hamilton Medical Center’s cardiovascular intensive care unit, recently received the Heart Hero Award, through Abiomed, for her actions that led to a positive patient outcome. The Heart Hero Award recognizes nurses who demonstrate exceptional knowledge, compassion, and leadership. The goal of the program is to create a supportive community of healthcare professionals and celebrate the strength and influence it provides.

MORNING POINTE SENIOR LIVING
Shellie Muncie, CNA
The Lantern at Morning Pointe Alzheimer’s Center of Excellence, Chattanooga congratulates Shellie Muncie, a certified nursing assistant who recently passed her boards to become a certified medication aide. Muncie is also currently in school to become a registered nurse and hopes to eventually be a hospice nurse.

ERLANGER
Erika Morales
Erlanger Neurology recognizes Erika Morales, a clinical staff leader, as a Stroke Nurse Champion recipient. Stroke Nurse Champions are considered team players and experts in stroke nursing care, and serve as a resource for other nurses. Morales is known for her attention to detail, leadership, and hard work during every shift, ensuring stroke patients receive the best care.

CEMPA COMMUNITY CARE
Shannon Burger, DSc
Dr. Shannon Burger, CEO of Cempa Community Care, recently received a Silver Stevie Award in the Thought Leadership category of the 23rd Annual American Business Awards. This award recognized Dr. Burger primarily for her work leading and growing Cempa as CEO over the past decade, as well as for her statewide and national advocacy work.

CENTER FOR SPORTS MEDICINE & ORTHOPAEDICS
Andrew Carlone, MD
Center for Sports Medicine & Orthopaedics welcomes Dr. Andrew Carlone, a fellowship-trained hip and knee specialist to its team. Dr. Carlone completed his undergraduate education at Emory University, majoring in neuroscience and chemistry. He earned his medical degree at Mercer University School of Medicine and completed his five-year orthopedic surgery residency at the University of Kentucky before pursuing a fellowship at Indiana University.

ERLANGER
Patrice Batchelor
Erlanger announced that Patrice Batchelor has been named chief marketing and communications officer. Batchelor brings more than 25 years of experience in healthcare marketing and communications. She holds a bachelor’s degree in corporate journalism and a master’s degree in marketing from Auburn University.

GALEN MEDICAL GROUP
Del Ashcraft, MD, FACOG
Galen OB/GYN Ridgeside welcomes Dr. Del Ashcraft to its team. With more than 28 years of experience in OB/GYN care in the Chattanooga region, Dr. Ashcraft brings exceptional skill and a genuine commitment to patient-centered care. He offers comprehensive services including wellness, obstetrics, menopause management, and minimally invasive surgery for pelvic conditions.


numbers to know
Nature’s Medicine
According to the American Heart Association, spending 120 minutes a week in nature can improve your overall health and well-being by decreasing feelings of depression, stress, and anxiety. Time spent in nature can include going on a daily walk, trying out a new hiking trail, or biking around your neighborhood.
Step to It
According to the National Institutes of Health, a study published in 2020 showed that higher daily step counts were associated with lower mortality risk. In fact, 8,000 steps per day, regardless of step intensity, was associated with a 51% lower risk of death from all causes compared to 4,000 steps per day.
PreventingPeanutAllergies
Take a Breather
Used by the United States Navy SEALs, box breathing is a simple but powerful breathing technique used to lower stress and ease anxiety. Try this technique:
Infants at the highest risk for developing a peanut allergy – such as those with severe eczema or an egg allergy – should be introduced to peanuts between 4 to 6 months of age to reduce the risk of developing an allergy, according to guidelines from the American Academy of Pediatrics. For children who aren’t at an increased risk, peanuts can be introduced into their diets according to family preferences.











Improving Health. Inspiring Change.

We believe in providing high-quality, affordable care to everyone in our community. Whether you are seeking routine check-ups, managing chronic conditions, or simply need a trusted medical provider that understands you, our compassionate team of integrated healthcare providers are here to help you take control of your health.
To learn more, visit us at cempa.org
health & wellness calendar

August
9
Bingo for the Grove
Get ready for an elegant evening of cocktails, dinner, a silent auction, and – you guessed it – bingo! This year’s theme, “Mamma Mia: Here We Go Again,” invites guests to dress up in their best Greek disco outfits and come out to the Hunter Museum of American Art to support the Orange Grove Center. The event starts with a cocktail hour at 6 p.m., followed by an after party with a DJ and dancing. bingoforthegrove.org
23 StarNight
Tickets and tables are still available for StarNight, Siskin Children Institute’s largest fundraiser! This year’s event marks the organization’s 75-year diamond milestone, honoring the children who inspire with their strength, resilience, and joy. Held at the Chattanooga Convention Center, this widely anticipated premier gala includes a cocktail reception, elegant dinner, silent and live auctions, high
energy entertainment, and more. All proceeds help raise awareness and funds to ensure Siskin’s life-changing services continue. siskin.org/ starnight
September
8
CHI Memorial Foundation
Annual Golf Invitational
Join fellow golfers on Monday, September 8, for the 34th annual CHI Memorial Foundation Golf Invitational tournament – Chattanooga’s premier golf event. CHI Memorial remains at the forefront of caring for our community. All funds raised will specifically impact cardiac and cardiovascular care, ensuring the latest technology is available right here at home and the highest level of care is provided. supportmemorialfoundation. org/chi-memorial-foundationgolf-invitational-
8
Kidney Kup
Join the Kidney Foundation for the 8th Annual Kidney
Kup golf tournament on September 8 at the Ooltewah Club! Participants will enjoy a full day of golf, complete with lunch, dinner, drinks, snacks, and exciting giveaways. Hosted in memory of Charles “Pete” Webster, the Kidney Kup supports a meaningful cause – all proceeds directly benefit kidney patients throughout the Chattanooga and North Georgia communities. kidneyfoundation.com/ kidney-kup
20 Celebration of Life and Hope
Get your tickets for the Austin Hatcher Foundation’s 18th annual Celebration of Life and Hope! This gala-style event features family stories and celebrations, complete with live and silent auctions, live music, an open bar, specialty cocktails, food, and entertainment – all in support of families affected by childhood cancer. This year’s event is presented by Material Handling Inc. (MHI) and Textile & Rubber Chemical Company (TRCC). celebrationlh.com
20 RMHC Run4Kids and Fun Fest
In memory of Karen Lawrence, the Ronald McDonald House Charities of Greater Chattanooga will host its 6th annual Run4Kids 5K Run and Fun Fest. The event will take place at the Tennessee Riverwalk, Hubert Fry Center at 9 a.m. on September 20. For 40 years, the Lawrence family has hosted the Karen Lawrence Run in memory of Karen, who battled acute lymphocytic leukemia. Since the opening of RMHC in 1990, the Lawrences have helped other families stay close to their sick children, offering the comforts of home, and RMHC continues to honor her legacy. rmhchattanooga.com/events
26
Kickin’
It for Kids With Cancer
For 18 years, the Austin Hatcher Foundation for Pediatric Cancer and the Lee University women’s soccer team have teamed up to host Kickin’ It for Kids with Cancer, an annual fundraiser supporting local families impacted by pediatric cancer. Held at the Lee University Ray Conn Sports Complex, the event combines a night of soccer, food, and fun with meaningful fundraising efforts. hatcherfoundation.org/events/ playing-for-purpose
28 IRONMAN Chattanooga Chattanooga’s biggest annual triathlon returns on September 28! Get ready for a plunge into the Tennessee River for multiple time Athletes’ Choice Award Winning 2.4-mile swim, a bike ride across a scenic course, and a race through the downtown streets for a final push to the finish line as spectators cheer you on. In total, participants can expect 140.6 miles of heartpumping physical activity for an unforgettable experience. iron man.com/races/im-chattanooga
October
9
Friends of Special Children’s 20th Annual All aBout Children (ABC) Event
Join Friends of Special Children in celebrating the 20th Annual ABC Event in support of Signal Centers! The excitement begins with an online silent auction beginning September 21 at biddingowl.com, and culminates with a dinner and live auction on October 9. This year’s theme, Empowering Our Children’s Future, supports sustainable funding to ensure children at Signal Centers have continued access to assistive technology, inclusive learning tools, scholarships, and professionally trained staff. friendsof specialchildren.org
19 7 Bridges Marathon
This year marks the 15th Annual 7 Bridges Marathon event weekend with over 4,000 registrants expected this fall. Chattanooga’s oldest and biggest marathon event includes five different races: The 7 Bridges Marathon, 4 Bridges Half Marathon, 4 Bridges 10K, Family Fun Run, and the 2 Bridges 5K. Featuring a live DJ, event shirts, custom medals, and a donut truck, each course will begin and end near the Chattanooga Theatre on Tremont Avenue. All finishers will receive a medal and age group awards will be awarded at the awards tent. sevenbridgesmarathon.com
20 RMHC Golf Classic
Join the Ronald McDonald House of Charities of Greater Chattanooga for its annual Golf Classic on October 20 at Black Creek. The RMHC Golf Classic has been ongoing since 1999 and has supported the Ronald McDonald House to provide families the opportunity to stay close to their loved ones during difficult times. Contests are held throughout the tournament with awards for each flight – plus the best
overall team for the day will be awarded the RMHC Kaylor Cup! Golfers may register as a team of four, and each player will receive a sleeve of Pro V1 golf balls, one mulligan, and a $150 gift card to the Black Creek Golf Course Pro Shop. rmhchattanooga.com/ rmhc-golf-classic
24 Casino Royale: Jaw Bones & Saw Bones Chattanooga-Hamilton County Medical Society and the Chattanooga Bar Association are excited to partner together for a premier evening of philanthropy and fun at Casino Royale: Jaw Bones & Saw Bones. This year’s event will be held on Friday, October 24 from 7 to 9:30 p.m. at The Walden Club. Set against the elegant backdrop of downtown Chattanooga, this black-tie-optional evening will feature lively casino games, cocktails, and a gathering of some of the region’s most dedicated medical and legal professionals. chattmd.org/event/ casino-night
25
Dare to Dance
Celebrating 18 years, Dare to Dance, the Chattanooga Kidney Foundation’s largest annual fundraising event, will be held at the Chattanooga Convention Center. Based off the popular TV show “Dancing With the Stars,” the event will feature 12 Chattanooga celebrities taking the dance floor with a professional dance partner to entertain the audience and raise funds for local kidney patients. Guests will enjoy a full dinner, drinks, take home souvenir items, photo opportunities, and more. daretodancechatt.com

LOVE,CARE, & S ERVINGOTHERS
Meet Our Caregivers

There is a lot to know about the loving and caring medical therapists, technicians, nurses, and other professional caregivers who have dedicated much of their lives to serving others.
What follows are local professionals who are providing the utmost in quality care.
ESTABLISHING TRUST
No matter how fast life gets, nurse practitioner Mark Cloutier is dedicated to slowing down and delivering quality patient care. “I was first drawn to nursing because I felt comfortable caring for people during vulnerable moments,” he shares. “When I had the opportunity to work in orthopedics after earning my master’s degree, I was excited because it’s such a practical, hands-on field where you often get to see people heal.” In addition to nine years working with Erlanger Orthopaedics, Cloutier enjoys applying his expertise to keep student athletes healthy, saying, “It’s a great way to give back and stay connected with the community.”
The good news is that most musculoskeletal pain is manageable and often temporary, and with the right understanding and care, most people recover and get back to doing what they love.”
1
MARK CLOUTIER, NP-C
ERLANGER ORTHOPAEDICS
WALK-IN CLINIC
What does your day-to-day look like?
I work as a nurse practitioner in a busy orthopedic walk-in clinic that provides same-day care for injuries and painful musculoskeletal conditions. We treat everything from acute sports injuries to chronic joint pain, with on-site x-rays and a range of procedures and resources. It’s a fast-paced environment, but we do our best to keep care timely yet personal.
2 What do you love most about your profession?
It’s incredibly gratifying to be a resource the community can assess, diagnose, and often begin treatment the same day, which can bring immediate relief and reduce a lot of fear and anxiety. And if more specialized care is needed, I have access to an incredible team here at Erlanger Orthopaedics with top-tier surgeons, non-operative specialists, therapists, and trainers to get patients exactly what they need.
3 What’s the key to making a great first impression?
It’s about connecting with people on a human level. Early in my career, a mentor told me that if you don’t enjoy your time with patients, then you might as well quit, because a truly fulfilling medical practice comes from enjoying time spent with patients and being there to serve them. That advice has stayed with me, and I still try to carry it with every patient encounter.
4 What would you consider to be your main strengths?
One of my main strengths is consistency – showing up every day with dedication. Consistently providing a thoughtful, thorough exam and treatment plan, even when the clinic is busy and I may start to feel the need to hurry. Understanding that is what every patient deserves because they have also sacrificed a lot to be there.
5
What is your philosophy when it comes to the care of your patients?
My philosophy of care is inspired by the old-time country doctors you see in shows like “Little House on the Prairie” or “The Waltons.” They weren’t just medical providers, they were trusted members of the community, showing up with compassion, practicality, and service. I try to carry that same spirit into my practice every day.

A SENSE OF PURPOSE
ALYSSA SANDERS, CNA
THE LANTERN AT MORNING POINTE ALZHEIMER’S CENTER OF EXCELLENCE, EAST HAMILTON
As a resident assistant, Alyssa Sanders knows firsthand the importance of meaningful connection in late stages of life. “My mother and grandmother influenced my career,” she explains. “Watching my mother take care of her mother so lovingly sparked a fire in me to take care of people who needed that same attention.” After eight years with the company, Sanders has stepped into her current role at the Lantern at Morning Pointe of East Hamilton, where she delivers thoughtful care to residents.
1
2
What is one of your happiest professional moments?
Helping and explaining to the family that we value their loved ones and we are a team. It takes a family, and we are here to help not only their loved ones but them as well.
What would you consider to be your main strengths?
As the greatest generation would say, “the gift of gab,” and being loving and understanding.
3
4
What is your best advice for residents?
It is okay not to feel okay. Let’s pray and talk it through. I’m here, and you are not alone.
What’s the key to making a great first impression?
Always be yourself – honest and understanding. I think people connect most with authenticity. A smile, a good attitude, and just being kind can go a long way. I try to make others feel welcomed and comfortable from the start.
I can give my residents a sense of importance and purpose when they feel lost and confused in the hardest times of their lives.”
5
What is your philosophy when it comes to care of your residents?
Whatever you do when caring for a resident, show respect and do it from the heart. Love them as they are your own family.

TRANSFORMATIVE CARE
It came as no surprise that Rachel Newmyer stepped into the healthcare profession. “My mother is an RN and her mother was an RN,” she explains. “I specifically have dedicated my career to bariatric surgery and nonsurgical approaches to weight loss.” When it comes to patient care, Newmyer’s approach is grounded in empowering and educating individuals in need of transformative care. “My job has given me an opportunity to partner with patients to help them achieve lifelong goals that can change the trajectory of their whole medical future,” she says. “This isn’t just about weight loss – it’s about living a longer, healthier, happier life.”
1
RACHEL NEWMYER, RN, CBN
ERLANGER METABOLIC CENTER
What I love about my job role is that I am in a career that sees patient improvement –not just the management of a disease, but a 360-degree transformation of life.”
2
What does your day-to-day look like?
My day-to-day pathway includes a very hands-on clinical role of educating and rounding on pre- and post-surgery patients, and an administrative role leading the hospital through accreditation and upholding the standards outlined by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, so that Erlanger will continue to be the region’s leader in care for an obese patient.
What influenced you to pursue your career?
For my career in bariatric surgery, the credit would have to go to the great and late Dr. Jack F. Rutledge. He talked me into being his surgical nurse 18 years ago and taught me everything I know, from scrubbing surgical cases to being an advocate for the bariatric patient. He was a huge advocate for the disease of obesity, and he would be so excited to see where obesity medicine is heading. I think he would be proud of where my career has led me.
3
What is one of your happiest professional moments?
One of my most treasured parts of my job is seeing what we call “non-scale victories.” These are the beautiful stories that I hear daily from patients who have lost weight and are living their best life: getting down on the floor and being able to play with their kids, wearing that dress that has been hanging in the closet for years, or riding on the roller coaster for the first time because they can fit.
4
5
What is your best advice for patients?
Be your own advocate. The more you understand about your body and why it functions the way that it does, the more in tune you will be to your medical changes. Obesity is not just a misstep in lifestyle – it is a disease, and it deserves to be treated.
What would you consider to be your main strengths?
Humility, confidence, and gumption. I will be the first to take the blame if I’m at fault. I know and trust my ability in who I am and what I am doing, but if I face a job that I don’t know how to tackle, I won’t give up until the job is done or until I have figured out a way to solve it.

erlanger.org/bariatrics
CONNECTING WITH COMMUNITY
With a passion for holistic care and a background in dance, Beth Herring knows that movement is medicine. “I couldn’t decide between attending medical school or pursuing dance,” she shares. “Physical therapy combined my interest in medicine and my love for movement!” Stepping into her new role as executive director, Herring aims to educate others about the services provided through the Program of All-Inclusive Care for the Elderly (PACE). “Currently, Alexian PACE is the only PACE organization in the state of Tennessee,” she says. “It is a blessing to work here and serve our community.”
I love our mission of keeping our participants at home with family instead of in a nursing facility. Because we not only offer medical care, but also all of our wrap-around services, we help participants to remain in the community.”
1
BETH HERRING
ASCENSION LIVING ALEXIAN PACE
2
What does your day-to-day look like?
Our participants can receive in-home personal care from an aide, be transported by our drivers and brought to the day center. We provide breakfast, lunch, and snacks! While at the day center they can see their doctor, have their rehab sessions, and socialize with friends! We take trips to the Lookouts baseball games and Chattanooga Zoo, and we have entertainers perform for us.
What is your best advice for participants?
Be active in your medical care! Let your family and physician know your wishes so they can be honored.
3
4
What would you consider to be your main strengths?
Perseverance and hard work have never let me down! Also, listening to and accepting help from others. I feel blessed to have mentors who continually support my career path, and I aspire to offer that same help to others.
What is one of your happiest professional moments?
One of my happiest professional moments was when Alexian PACE installed a ramp at a participant’s home, enabling him to remain in his own home. Despite being unable to walk or shower himself, with our assistance, he can live at home and has avoided placement at a nursing home.
5
Do you believe in miracles?
Absolutely! I see miracles happen in daily interactions with others when a kind word or deed evokes unexpected joy, or when an elderly participant shares a poem or a story from their past with others. These seemingly small things can alter your outlook and provide a deeper understanding of the human condition.

HELPING PATIENTS THRIVE
For 30 years, Kevin Shrum has been providing lifesaving care at Erlanger. “I help ensure that any respiratory needs that a child may need in all areas of the hospital are available and provided in a timely manner,” he says. His passion for his profession is rooted in helping children thrive through difficult circumstances. “After serving in the military and seeing some of the world’s most impoverished children in a warzone somehow finding ways to survive, I knew I wanted to work with children in some way,” Shrum shares. “I am blessed to work with the best caregivers in the world, providing outstanding care to the region’s sickest children.”
KEVIN SHRUM, RN, RRT
CHILDREN’S HOSPITAL AT ERLANGER
1
What is your philosophy when it comes to the care of your patients?
Always treat them as they are a member of your family and you can’t go wrong.
2
3
What do you love most about your profession?
Although it can definitely be challenging at times dealing with loss working at a children’s hospital, the determination and fight these children have absolutely amazes me. I love working with children and witnessing their amazing journey from neonate fighting for their life until discharge.
What is one of your happiest professional moments?
I got to witness a former patient who was born at 24 weeks graduate from high school. She returned to the hospital with her mother, who had the names of all her caregivers on the night she was born. That was special.
4
I try to always have a positive attitude and always put the patient first. I love to see new employees succeed and learn a new skill.”
5
What’s the key to making a great first impression?
Always smile and introduce yourself. One of the first questions to ask should be, “How may I help you?” Always include the parents in the care of their child.
Do you believe in miracles?
I absolutely believe in miracles. One cannot work at a children’s hospital and not believe in miracles, because we see them every day.

EDUCATING & EMPOWERING
Madison Thomason chose the perfect career path to unite her intellectual and relational passions. “The genetics chapter in high school biology ignited my interest in this field,” she shares. “I knew I wanted to work directly with patients, and genetic counseling turned out to be the perfect combination of science and people.” She brings 14 years of experience to her current role, where she counsels individuals and families through complicated conversations. “When a patient enters my office, noticeably fearful, anxious, angry, or hopeless, and then walks out of my office with an exhale of peace, hope, comprehension, and motivation, it is one of the most rewarding things in the world,” she says.
I love being able to come alongside families to support them throughout the genetic testing process. Genetics can be a complex subject, and if I can help to make it more understandable and less intimidating, that’s a win!”
1
MADISON THOMASON, MS, CGC
ERLANGER WOMEN’S ONCOLOGY
2
What does your day-to-day look like?
As a cancer genetic counselor, I meet with patients to determine if their personal history and/or family history of cancer might be due to an underlying inherited genetic cause. I help them understand what their genetic test results mean, educating them about their cancer risks, options for medical care, and potential risks to their family members. Providing emotional support along the way is an important aspect of the care I give.
What is your best advice for patients?
Don’t be afraid to ask questions. Be inquisitive. Ask your relatives about your family history. Ask your healthcare providers about your diagnosis, test results, and treatment options. Ask about anything you don’t understand. Knowledge leads to wisdom and good judgment. We are all lifelong learners.
3
What is your philosophy when it comes to the care of your patients?
Take a genuine interest in getting to know them as a whole person. Find out their grandkids’ names or what new trick their dog is doing. Learn what makes their face light up and what is their greatest worry. Then build off of those things as I educate and empower them to navigate their medical journey well.
4
5
What’s the key to making a great first impression?
Acknowledge people by name with a sincere smile and undivided attention. Make them feel like they matter more than anything else in the world at that moment.
What would you consider to be your main strengths?
From the “science” perspective, attention to detail comes naturally to me and is of great importance when interpreting complex genetic test results. From the “people” perspective, I deeply care for my patients and their families and consider it an honor to come alongside them in their cancer journeys.



ER DOCTO R S: CARE DURING CRISIS
While finding yourself or a loved one in the emergency room can be stressful, it’s comforting knowing you are in good hands. Here, we highlight five local ER doctors who provide critical care and comfort when it matters most.


DEANN CHAMPION, MD, FACEP
EMERGENCY ROOM MEDICAL DIRECTOR, CHI MEMORIAL
What got you interested in medicine?
My mom was a medical technologist when I was growing up. She took many overtime calls, and I would go to the hospital with her. I felt like I grew up in a hospital, and it was a comfortable place for me.
Why did you decide to pursue emergency medicine over other specialties?
I really enjoy the variety of patients. I enjoy having a breadth of knowledge across all medical specialties. I enjoy how “scheduled” the work is, which makes it easier to plan time outside for family life. I also enjoy that it is a procedure-heavy specialty.
How long have you worked in your current role?
I have been at CHI Memorial for 25 years. I have spent my entire career at one facility, which is unusual for emergency medicine doctors. I recently stepped into more of an assistant medical director role so I could enjoy more time with my family.
Can you share any special stories related to ER work?
A patient went into cardiac arrest multiple times. We would shock his heart, and he would become conscious again. We figured out it was his birthday, and I told him, “You’re not allowed to die on your birthday.” I am glad he listened to me. He successfully made it to the cath lab and then the ICU, where I was able to visit him. He told me that he heard me loud and clear that he wasn’t allowed to die on his birthday.
Anything else you’d like to add?
I really enjoy my job and all of the different patients that I get to interact with. It brings me a lot of satisfaction when I take good care of a patient and they improve. I wouldn’t say I enjoy giving bad news, but when I have to, it is my privilege to do it with kindness, and then, if appropriate, to pray with the patient. I am grateful to have spent my career in a faith-based facility where I can freely do that.



RON BUCHHEIT, MD
MEDICAL DIRECTOR, ERLANGER PRE-HOSPITAL AND DISASTER MEDICINE
Do you have a specialty within emergency medicine?
I specialize in emergency medical services (pre-hospital medicine). I serve as medical director for multiple ambulance services, fire first responders, special operations teams, Hamilton County SWAT, and the Hamilton County 911 Emergency Communications District. I’m passionate about bridging the gap between the field and the hospital to ensure seamless, high-quality care.
What does a strong ER team look like to you?
A strong ER team is made up of people who are caring, open to learning, and willing to keep fighting even when the odds are stacked against us, resources are stretched, and the department is overflowing. We often talk about the “chain of survival,” which begins with the 911 telecommunicators, followed by police officers who are frequently first on scene, then our fire departments and EMS medics who provide early, life-saving interventions. Once patients arrive at the hospital, our techs, nurses, paramedics, and physicians continue that chain. It’s one coordinated effort across multiple disciplines, all working together to save lives and reduce suffering.
What does a “day in the life” look like for you?
Because our emergency departments operate 24/7, we work in rotating shifts to provide constant coverage. When I come on shift, I typically receive a handoff from the outgoing physician and check in with patients already being treated to ensure they’re doing well and understand their care plan. Then, I start seeing new patients, listening to their concerns, performing physical exams, and ordering medications, lab work, or imaging to pinpoint the cause of their symptoms. That steady rhythm is often interrupted by critical cases requiring immediate attention. No two shifts are the same.
What is your proudest moment as an ER doctor?
I work with new doctors in residency training as well as new and experienced paramedics. One of the most rewarding parts of my job is providing education and watching them grow, develop their skills, and become more confident in patient care. Seeing them succeed reminds me that we’re not just saving lives, we’re shaping the future of emergency medicine and making a real difference in our community.

DANIEL A. POOR, MD, FACEP
REGIONAL MEDICAL DIRECTOR, PARKRIDGE EMERGENCY DEPARTMENTS
What is your favorite thing about working in emergency medicine?
Everything. I appreciate knowing that every day and in every encounter I have the opportunity to dramatically improve and/or save a person’s life. I am grateful to be part of the Chattanooga community; my family loves it here. We are blessed to be here, and I am honored to serve.
Why did you decide to pursue emergency medicine over other specialties?
One of the joys of emergency medicine is, and I say this to every group of medical students that I teach, that we are the only specialty that does it all. I am trained to treat you from your first breath to your last, and all the things in between. I find aspects of all specialties interesting – cardiology, surgery, internal medicine, pulmonology, etc. That said, I did not fall in love with a specific one. What I did fall in love with is the pace, the acuity, and the rapid decision-making that can determine, in minutes, if we can save a life.
What is the most challenging aspect of your job?
I want to make sure what I do is right for the patient in front of me and ensure they have appropriate follow up once they leave to go home from the ER. We face many challenges with insurance and access to medical care. I always fear, though I have done everything I can, that patients will not get what they need once they leave.
What does a strong ER team look like?
Our departments are only as strong as our nursing colleagues; without them we cannot do our job or take care of patients in our community. Our nursing staff and leadership from the chief nursing officers down are extraordinary. I am blessed to have the team I have at Parkridge.
What is one piece of medical advice you think everyone should know?
Never lie to your doctor. I am not here to judge you, I am here to care for you, and to do that you need to be honest with me.



JEFF ATHERTON, MD
EMERGENCY MEDICINE PHYSICIAN, HAMILTON MEDICAL CENTER
What is your favorite thing about working in emergency medicine?
I cherish the personal connections that emergency medicine fosters. Whether listening to veterans share their war stories or discussing unique cases with my nurses and colleagues, I thrive on the sense of community in the ER. These shared experiences are very rewarding.
What is your proudest moment as an ER doctor?
When I was a resident physician, I had a patient involved in a football related accident, and to the naked eye he didn’t have any apparent injuries. I felt something wasn’t right though, so rather than proceeding with discharge, I performed a screening bedside ultrasound. To my surprise, I found evidence of internal bleeding. It turns out that he had recently been ill with mononucleosis, which causes the spleen to swell. When he took a hard tackle playing football it had caused an injury to his spleen. This could have turned into a life-threatening situation had I not trusted my clinical gestalt and pursued deeper investigation.
What does a strong ER team look like?
ER nurses are the heartbeat of the emergency department. My nurses bring strength to the team with quick thinking, compassion, and the ability to juggle high-pressure tasks seamlessly. Their sharp instincts catch subtle changes in patients’ conditions, and their empathy provides a lifeline to those in crisis. ER nurses typically have great stories as well!
What is one piece of medical advice you think everyone should know?
Learn the signs of a heart attack and stroke and act fast if you or someone else experiences them. Heart attack signs include chest pain or pressure (may radiate to the arm, jaw, or back), shortness of breath, sweating, nausea, or lightheadedness. Stroke signs include sudden numbness or weakness (especially on one side), confusion, trouble speaking, vision problems, dizziness, or severe headache (use the FAST acronym: Face drooping, Arm weakness, Speech difficulty, Time to call 911). Delays in seeking care for these emergencies can lead to worse outcomes. This knowledge empowers you to act decisively, whether for yourself or others.


TOREY KILLOM, DO
MEDICAL DIRECTOR OF EMERGENCY SERVICES, BRADLEY MEDICAL CENTER
What got you interested in medicine?
From a young age, I was always fascinated with science and the physiology of the body. I also have always enjoyed helping others. I was raised around medicine. My stepfather was an emergency medicine physician, as well as the medical director of his facility. Now I have two younger siblings that are also ER doctors, so it runs in the family.
What is your favorite thing about working in emergency medicine?
It is impossible to get bored in the ER. Every day there is something new or slightly different. I also truly enjoy knowing that I can make a huge change in my patients’ lives. Although visually it seems chaotic in the ER, every single provider is doing their best to provide care for you, and we all generally want the best for our patients and their families. We do care so very much.
What is your proudest moment as an ER doctor?
There are many, but I think the most impactful moments for myself have been when a patient stops me before they are discharged and lets me know that I am exactly in the role that I’m supposed to be in life, and that they truly appreciate me and what I’ve done for them and their family. I love knowing that I have made a difference for the better in my patients’ lives, even if that is just showing them kindness and compassion.
What is the most challenging aspect of your job?
The most challenging aspect of the job is time management, and knowing that no matter how hard you try, you’re not going to be able to save everyone. You just go into each shift telling yourself that you will do your best no matter what.








LIFE FORCE AIR MEDICAL Service in the Skies
By

In life’s scariest moments, we call upon reliable and timely care. For over 35 years, Erlanger’s LIFE FORCE Air Medical has taken to the skies to deliver life-saving care to patients in need. Here, we take a behind-the-scenes look at the acclaimed air ambulance service.
Expanding Emergency Services
Recognizing a need for critical transport services in the Chattanooga region, Erlanger established LIFE FORCE Air Medical in 1988. Ambulance services provide essential care in the wake of an injury or critical illness – but mountainous terrain, hard-to-reach places, and specialized medical conditions make it difficult for certain populations to access emergency care. Air ambulances like LIFE FORCE help bridge this gap.
LIFE FORCE initially serviced the Chattanooga community with a Bell 412 aircraft, a helicopter that could hold two patients, two flight crew members, and a pilot. Since its inception, LIFE FORCE has expanded service to surrounding rural communities, encompassing East Tennessee, North Georgia, Northeast Alabama, and Western North Carolina. With six bases serving over 50,000 square miles in the Southeast, every second counts.

“Time is an enemy of a traumatic insult or medical disease process,” says flight paramedic Richard Medley. “Currently, LIFE FORCE has strategically placed six bases in rural areas with services provided in four states, enabling rapid transport to facilities with a higher level of care. This gives patients in those communities a greater chance of surviving their injury or illness.”
Whether in urban or rural environments, access to timely healthcare can be the difference between life or death. The first 60 minutes following an injury are referred to as “the golden hour,” a crucial period that determines a patient’s outcome. With the help of air transport, critical-care patients can reach a Level 1 Trauma Center like Erlanger, or be taken to Nashville or other cities with specialized healthcare facilities. What could be a two-hour drive via ground transportation is drastically reduced by air ambulance services.
“There’s no doubt that helicopters save lives,” says Eric Breedlove, flight nurse. “Every single flight our team is making a positive difference. I believe we as a team all share the same mindset and are here to make a positive impact and help others during their most vulnerable times.”
The Highest Standard of Care
For lead A&P mechanic Leon Gerardi, quality patient care begins with a reliable and safe helicopter. “As a maintenance tech, all the thousands of flights that my helicopters and team members have completed over the years are so meaningful to me,” he says. “It gives me such great satisfaction knowing that the helicopter that I maintain is carrying my crew safely so that they can do the job that they do.”
From aircraft to medical equipment, top-notch technology helps maximize the medical attention a patient can receive inflight. In 2008, LIFE FORCE partnered with Med-Trans Corporation, who took over administration of helicopters, mechanics, and pilots so Erlanger could focus on patient care. Additionally, the program retired the initial Bell 412 and now operates a fleet of six aircraft. The pilots of these aircraft go through intensive training to prepare for any situation.
Pilot and base aviation manager Jacob May knew he was destined for this profession from a young age. “When I was a kid riding my bicycle in my neighborhood, I saw an EMS helicopter land and take a critically injured patient from a car accident,” he recalls. “Since that day I’ve always wanted to be an EMS helicopter pilot. I thoroughly enjoy working with some of the best clinicians on the planet, and the teamwork involved in making LIFE FORCE work so well is inspiring to me.”
From mechanics and pilots to medical and communications personnel, the LIFE FORCE team is built on trust. “Most of our providers come from a critical care background prior to coming to LIFE FORCE and have years of experience in the critical care setting, including emergency departments, intensive care units, critical care ground EMS, and high volume 911 EMS services,” says Breedlove. “A strong team consists of great communication skills, diversity in medical background and knowledge among crewmembers, and the ability to trust each other and have accountability.”


What makes for a strong crew? “Each team member has an important role, and we all support each other. We all know that without each of us doing our part, there would be no LIFE FORCE.”
–Leon Gerardi, Lead A&P Mechanic

LIFE FORCE AIR MEDICAL REGIONS
LIFE FORCE 1 Cleveland, TN
LIFE FORCE 2 Sparta, TN
LIFE FORCE 3 Calhoun, GA
LIFE FORCE 4 Blue Ridge, GA
LIFE FORCE 5 Winchester, TN
LIFE FORCE 6 Murphy/Andrews, NC

What can patients and their families expect from an experience with LIFE FORCE?
“The highest professional care possible in the field and their best chance of a positive outcome on what could be one of their worst days.” –Jacob May, Pilot & Base Aviation Manager
One of LIFE FORCE’s most notable milestones, Medley says, is the program’s track record of safe flights for over 35 years of operation. “Our daily operations demand respect for safety to allow us to go home to our own families,” he says. “LIFE FORCE has been vigilant with maintaining safety standards that keeps all involved safe.”
Ready at a Moment’s Notice
The day for the crew begins before dawn. The team has briefings, checks all equipment, and performs any necessary maintenance in preparation for a flight. For the pilots, this includes looking at the weather and gauging flying conditions. “All this generally takes 30 minutes,” says May, “During this window we are capable of taking a flight immediately, provided the pilot determines the flight is both legal and safe. We then conduct administrative duties while waiting for a flight request to come in, but are at all times ready to fly as soon as possible. This requires pilots to always know what the weather is and what it will do for their shift.”
While the pilots are keeping their eyes on the skies, the medical crew makes good use of any down time. “Once complete and ready for flight, we wait until a flight request is initiated by our flight communications center,” says Breedlove. “In the meantime, medical crew members are usually training on advanced skills, reviewing protocols, and completing continuing education.”
The medical team’s association with Erlanger ensures access to ongoing medical advancements and training. “Medicine is constantly evolving,” Medley says. “Our affiliation with Erlanger, a teaching facility, has kept our program up-to-date with the latest evidence-based medicine to ensure the best possible care for our patients.”
In addition to staying current with treatment modalities, LIFE FORCE offers ongoing educational programs with regional hospital staff members and rural EMS services. All in all, LIFE FORCE’s dedication to safety, education, patient care, and community health earned the accolade “Flight Program of the Year” by the Association of Air Medical Services in 2024.

Sensible Investing: What’s Most Important to You?
Investing isn’t just about creating wealth. It’s about making your money work for you so you can live your life on your terms. Our single focus is helping you achieve what’s most important to you. Your financial goals are unique. Together, we’ll help identify and define them. We’ll walk through our established process to build your personalized strategies and help you stay on track for the long term.
Downtown
Contact an Edward Jones Trusted Financial Advisor Near You
Becki T Anderson, CFP®, CEPA®, CRPS™
423-541-0303
David J Oesch, CFP® 423-267-8433
Hixson
Derrick C Anderson, CFP®, AAMS™
423-843-4994
Heather W Edmondson, CFP®, AAMS™ 423-843-5034
Ian M Early, CFP®, AAMS™ 423-875-0508
Marty Cabe, CFP®, AAMS™ 423-842-3071
Cari E Weaver 423-843-4994
Soddy-Daisy
Lee H Prichard, CFP®, AAMS™
423-332-3006

Red
Bank
Gretchen Wynn 423-954-7751
Joshua D Schweiger, ABFP™, AAMS™, CRPC™ 423-954-7751
North Georgia
Jonathan G VanderHart 706-858-9676
Paras Sharma, CEPA®, AAMS™ 706-229-8791
Rob Looney, CFP®, AAMS™ 706-375-4727
Ty M Willeford, AAMS™ 706-638-6673
Keith Ware 706-657-2477
Athens
Joseph Ladner, CFP®, ChFC®, CEPA®, SE-AWMA™ 423-746-5975
East Brainerd
Beth Lofgren, CFP®, CEPA®, RICP® 423-499-4144
Stan Russell, CFP®, AAMS™ 423-894-0058
Adam Cline, AAMS™ 423-541-0012
John Attardo 423-899-0792
Geo Mejia, AAMS™ 423-305-0268
David Keith, AAMS™ 423-892-1449
Ooltewah
Corey Madding, CFP®, AAMS™ 423-238-0184
John Nething II, CEPA®, AAMS™ 423-910-1982
Jay Sparks, AAMS™ 423-910-4009
Cleveland
Ron Markel
423-473-2215
Bradley A Hudson, CFP®, AAMS™ 423-476-3320
Ben Payne 423-339-2885
Kelly L Browand, CFP®, AAMS™ 423-476-3320
Bobby Ludwig, AAMS™ 423-473-2215
David B Browand 423-641-4755
Shannon B Ritzhaupt 423-476-0162
Chris Robinson 423-476-4325
Vonore
Tolita Freeman, AAMS™ 423-376-1778
A Lasting Impact
When asked about their most memorable flight, LIFE FORCE crew members say it’s hard to choose just one. “I think the most meaningful flight experiences are the ones that you’re able to follow and see the positive progression of the patient,” says Breedlove. “There have been many flights where the collaboration between ground EMS and LIFE FORCE has ultimately saved a patient.”
LIFE FORCE is able to transport patients of all ages, from infants to geriatrics. The crew’s investment in ongoing training and education pays off each time a patient benefits from treatment. “One common experience that is meaningful is the patients that respond to evidence-based
training – whether it’s a medication given or a procedure performed – and the condition of the patient goes from unstable to stable,” says Medley, who also works as a base educator in the program. “If I had to pick one thing, it would be the administration of blood, which has the most dramatic change in a traumatic patient’s condition when needed. It truly is a gift of life that a trauma patient receives.”
Making a positive difference in the lives of patients is what drives the personnel in LIFE FORCE, day in and day out. May recalls an interaction at a car dealership with a man who had been a LIFE FORCE patient: “He found out who I worked for and began to tell me that he was flown, that some of our crews saved his life, and how grateful
he was to be alive. Even though it wasn’t me who flew him as a pilot (we don’t have the opportunity to interact with patients like the crewmembers do) it made me realize the impact of what we do every day for our community.”
Since its beginnings, LIFE FORCE has completed over 50,000 patient transports. The passion of the crewmembers is evident as they look to the future of continually delivering quality critical care to the Southeast. “I have been part of this LIFE FORCE family for 30 years, and I think that speaks volumes,” says Gerardi. “I have enjoyed working with the best of the best and my crews are exactly that. Their professionalism is beyond belief. It takes all of us to be LIFE FORCE, and that’s what makes it so great!”

What drives your passion for this profession? “First and foremost, every shift when I clock in, I know 100% in my heart and mind that I am here making a positive difference in peoples’ lives and doing my small part to help people in their time of need.”
–Eric Breedlove, RN, CFRN, Flight Nurse & Base Educator






LIFE FORCE AIR MEDICAL TIMELINE
1988 Erlanger launches LIFE FORCE Air Medical flying one Bell 412 aircraft
1994 LIFE FORCE equips a receiver certified to fly Global Positioning System (GPS) approaches, the first helicopter program in the nation to do so
1995 LIFE FORCE 2 begins service based in Sparta, Tennessee
2006 LIFE FORCE 3 begins service based in Calhoun, Georgia
2008 Erlanger partners with Med-Trans Corporation to assist in management of helicopters, mechanics, and pilots
2010 LIFE FORCE 4 begins service to rural areas of Northeast Georgia and North Carolina
2015 LIFE FORCE 5 begins service based in Winchester, Tennessee
2016 LIFE FORCE 1 permanently relocates from downtown Chattanooga to new hangar in Cleveland, Tennessee
2017 LIFE FORCE 6 begins service in Andrews, North Carolina
2024 LIFE FORCE Air Medical named “Flight Program of the Year” by the Association of Air Medical Services (AAMS)
2025 LIFE FORCE becomes the first EMS agency in Tennessee equipped and trained to transport injured or critically ill working K-9s

What is something you’d like to share about the LIFE FORCE crew? “Long hours and extra days worked keeps them from their families … so if you see one of these people, a simple word of appreciation goes a long way and will keep them going on their worst day at work.” –Richard Medley, Flight Paramedic & Base Educator



For those recovering from a stroke, injury or illness, regaining your best quality of life begins with your ability to choose. Choose Encompass Health for exceptional results. Regaining your quality of life begins when you CHOOSE exceptional results in rehabilitation.
encompasshealth.com/chattanoogarehab
Answering the Call
GRADUATE STUDENTS PURSUING A PASSION FOR HEALTHCARE
Acareer in healthcare requires perseverance, compassion, and a commitment to serving others. From the long hours of nursing and medical school to the high-stakes responsibilities of patient care, every step requires more than just knowledge – it requires heart. Behind every future nurse or doctor is a story of resilience and a deep-rooted passion for making a difference. We sat down with four of our region’s most driven nursing and medical students to uncover what fuels their journey, the obstacles they’ve overcome, the support systems that helped them rise, and the unwavering sense of purpose guiding their paths.
By Lindsey Clute and Rachel Studebaker

Travis Wright
UNIVERSITY OF TENNESSEE AT CHATTANOOGA
Doctor of Nursing Practice –Adult-Gerontology Acute Care (AG-ACNP)
With a passion for science and a drive to help people achieve their goals, Travis Wright decided to take his nursing career to the next level by pursuing a Doctor of Nursing Practice in AdultGerontology Acute Care. Now in his third year at the University of Tennessee at Chattanooga, he’s found purpose and inspiration at every step, thanks in large part to the mentors who helped shape him along the way.
“I have been able to learn from some of the smartest, most knowledgeable practitioners,” Wright says. “Our instructors are passionate about what they do, and I hope to carry that passion with me into my practice. Additionally, our program director, Dr. Denton, is one of the most knowledgeable people I know and someone I would trust with my life. She is the practitioner I aspire to be.”
But Wright’s path to medicine didn’t begin in a classroom or clinic. Before ever donning scrubs, he spent 10 years working as a motorcycle mechanic, a career that, unexpectedly, held important parallels to the medical field. “It taught me a lot about thinking through problems to get to the root issue,” Wright shares, “but more importantly, it taught me that whatever you’re working on is part of a larger system. You have to approach things holistically and treat the entire machine if you want it to run well.”
As a full-time student, husband, and father, Wright’s journey hasn’t been straightforward. However, a desire to serve others at their most vulnerable ultimately solidified his pursuit. “I love critical care. It’s fast-paced, challenging, and is essentially a continuous stream of controlled chaos. It’s often not easy, but helping people go from being critically ill to being able to go back to their lives and hobbies is incredibly rewarding.”
For Wright, caring for patients goes far beyond the immediate bedside. It’s also about empowering people to take ownership of their health and finding ways to continually improve the care he provides. “Adding new tools to my toolbox and using the latest evidence to improve my care is exciting to me,” he says. “I want to continue to grow for as long as I’m practicing.”

John P. Smith
SOUTHERN ADVENTIST UNIVERSITY
Doctor of Nursing Practice –Psychiatric-Mental Health (PMHNP-DNP)
From growing up on a farm to serving as captain and company commander of his high school’s ROTC program, John Smith learned the value of discipline, empathy, leadership, and work ethic from an early age. Now a third-year Doctor of Nursing Practice student at Southern Adventist University, Smith brings that same foundation into his work as an aspiring psychiatricmental health nurse practitioner.
“Early on, I recognized that health is deeply intertwined with a person’s environment, resources, and mental well-being, not just their physical symptoms,” he shares. “This led me to the field of psychiatric-mental health nursing, where I felt I could genuinely make a difference by listening, advocating, and walking alongside individuals during their most vulnerable moments.”
That passion for people, especially those often underserved or overlooked, became the heartbeat of Smith’s career goals. But his journey hasn’t been without hardship. After losing his mother to stomach cancer, Smith was left to navigate grief while juggling academic demands. Still, he persevered. “Despite the struggles, or maybe because of them, I’ve become more committed than ever to this path,” he says. “I know what it means to endure loss, carry on, and still choose to care – and that, I believe, is at the heart of nursing.”
Smith now channels that resilience into his vision for the future: one where healing goes far beyond symptom management. “I want to create safe, nonjudgmental spaces where patients feel seen, heard, and empowered,” he explains. “Healing happens in relationships through empathy, education, and empowerment.”
He’s also passionate about supporting those behind the scenes – his fellow healthcare providers. “Mental health among providers is too often neglected,” he says. “Through initiatives like workshops and burnout prevention, I hope to create healthier systems that support both patients and professionals.”
Whether he’s mentoring future nurses, advocating for equitable care, or offering hope to someone in crisis, Smith is driven by the core belief that every person deserves to feel they matter. “If I can be a steady presence in someone’s journey toward healing,” he says, “then I’ll know I’ve done something meaningful.”

M ASTER’S DEGREE

Enjoy the confidence, respect, and career oppor tunities that come with an advanced degree.
Your life
Classes meet one day each week , so you can manage work and responsibilities on your time.
You choose.
Full- and par t-time options allow for a customized study plan that works for you. We also offer accelerated RN-to-MSN programs, post-master ’s cer tificates, and a dual MSN/MBA degree
You succeed.
MSN graduates from Southern Adventist University have 100 percent job placement in their chosen field.
Master of Science in Nursing
• Acute Care – Adult /Gerontology Nurse Practitioner
• Primary Care – Adult /Gerontology Nurse Practitioner
• Primary Care – Family Nurse Practitioner
• Primary Care – Psychiatric Mental Health Nurse Practitioner (online )
• Nurse Educator (online )
• MSN/MBA (online )
Call or visit online to find out how you can get star ted.






Alia Parker
LEE UNIVERSITY
Doctor of Nursing Practice –Family Nurse Practitioner (DNP-FNP)
For Alia Parker, a career in nursing is about providing hope and holistic healing to her patients. She has had plenty of experience doing just that in her healthcare career, holding positions from an EKG tech and patient care technician to working in the ER, ICU, and travel nursing. Currently pursuing a Doctor of Nursing Practice at Lee University, Parker is eager to put her degree and broad experience to use as a new nurse practitioner.
Parker describes the knowledge that she and other practitioners gain from their studies as a “toolbox,” adding, “From it, we can draw many different resources to help our patients achieve better health and reach their personal goals.” She plans to put her toolbox to use in the field of functional and integrative health, looking at the mental and spiritual, as well as physical, components of well-being.
However, acquiring these tools doesn’t come without hard work. “Entering graduate school is very much like committing to a long-term relationship – one that requires loyalty, sacrifice, and endurance,” describes Parker. Despite the challenges of juggling graduate studies with daily demands and raising three sons, Parker has persevered in pursuit of her passion and says the support from her husband has been invaluable.
To those entering graduate school, Parker says to take it day by day. “This journey is a marathon, not a sprint,” she advises. “Pace yourself, and adopt a mindset rooted in hope – knowing that you will reach the finish line by taking it one mile at a time.”
“I have always been deeply grateful for becoming a nurse,” concludes Parker. “I am especially thankful to my family, who has supported me every step of the way as I’ve grown into the person I believe God created me to be.
I’m also incredibly grateful to Lee University and the professors there for providing such an excellent environment to learn, grow, and be shaped both professionally and personally … I truly believe it has made me a better person, a better leader, a better nurse, and a better provider.”
Empowering Nurse Leaders to Transform Patient Care
Advance Your Nursing Practice with Lee University’s DNP Program

3 specialty tracks: Family Nurse Practitioner, Transformational Executive Nursing Leadership, Post-APN
• Flexible entry points: enroll with a BSN or MSN
• Hybrid learning with minimal on-campus commitment
• Options for part-time or full-time study
• Engaged and supportive faculty
• Dedicated practicum coordinators
For more information, email dnp@leeuniversity.edu or call 423-614-8526


Alvaro Cortez
DALTON STATE COLLEGE
Doctor of Medicine (MD) and Master of Public Health (MPH)
Equipped with a bachelor’s degree in biology from Dalton State College, Alvaro Cortez is taking the knowledge and lessons he learned as an undergraduate with him into the Doctor of Medicine and Master of Public Health dual-degree program at the Medical College of Georgia. Fueled by a longstanding dream and steadfast passion for family medicine, Cortez is nearing the finish line of a path he’s walked with heart and grit.
“I love the ability to form long-term relationships with patients and address broad needs,” explains Cortez. “Having a good primary care doctor keeps the community healthy and ensures that patients receive comprehensive care.”
For Cortez, the choice to enter the medical field stemmed from a deeply personal place. “I was inspired to pursue a career in medicine when my sister was born with trisomy 18, also known as Edwards’ Syndrome,” says Cortez. “Watching my Mexican immigrant parents navigate my sister’s health needs showed me that the Hispanic/ Latino population faces many barriers to healthcare. I realized that there is a great need for Hispanic/Latino physicians, which has ultimately shaped my career aspirations.”
His adversity didn’t stop there. As a first-generation college and medical student, Cortez has had to push boundaries, relying on resilience and determination. “I’ve had to navigate many aspects of this journey without a roadmap,” he says. “That challenge has made me more resourceful, disciplined, and empathetic. It’s also deepened my commitment to mentoring others who are walking similar paths and may be facing similar doubts or barriers.”
Although he faced many challenges, he never endured them alone. His parents have been his greatest role models, instilling in him a deep respect for education and diligence. Through their example, he is inspired to encourage others from similar backgrounds to pursue their dreams.
“Don’t be afraid of being uncomfortable,” Cortez says, offering a message of hope to those beginning their medical journey. “There will be moments when you feel unprepared, overwhelmed, or unsure of yourself. That’s okay. Lean into those moments and trust that they are shaping you into the physician your patients need. You are more capable than you know, and every challenge is an opportunity to grow into the doctor you’ve always dreamed of becoming.”



















ANNUAL SPE C IAL SECTION
Advancements in Medicine
From minimally invasive surgical technologies to innovative appproaches to rehabiliation and beyond, new research in the medical field is optimizing care for patients and doctors alike. Read on to discover the latest in revolutionary treatment options.
By Rachel Studebaker

An Expert Weighs In
“Advancements in the management of DVT have revolutionized therapy and restored hope for those with what was once a debilitating condition. Gone are the days of placing someone on blood thinners and wishing them ‘good luck’ that they did not develop ulcers or lifestyle-limiting swelling in their legs. With modern devices like those from Inari and Penumbra we can quickly remove the clot, often in an outpatient setting, thereby restoring normal venous flow. This significantly decreases the chances of post-thrombotic syndrome and leg ulceration in the long term and helps people quickly return to normal, healthy states.”

William B. Harris, DO, FACS, RPVI Vascular Surgeon, Vascular Institute of Chattanooga
Advancements in Deep Vein Thrombosis Treatment
Clot-removal procedures and tools can quickly and effectively treat venous issues.
Understanding Deep Vein Thrombosis
Unexplained sudden leg swelling, pain, and heaviness aren’t always due to poor circulation or aging – they can be signs of deep vein thrombosis (DVT), a dangerous condition where a blood clot forms in the deep veins, most often in the leg or pelvis. Left untreated, DVT can cause long-term complications or become life-threatening if the clot travels to the lungs, resulting in a pulmonary embolism.
New Solutions
Traditional treatment involves blood thinners to prevent clot growth, but this approach doesn’t remove the existing clot. In patients with large or symptomatic clots, percutaneous venous thrombectomy has emerged as the new gold standard. This minimally invasive procedure allows surgeons to physically remove the clot from the vein using advanced catheter-based devices. It’s performed through a small incision, typically under ultrasound or fluoroscopic guidance, and can immediately restore blood flow.
Among the latest systems used during thrombectomy are:
• Inari FlowTriever and ClotTriever. These systems use mechanical aspiration to remove clots, particularly in patients with newer-onset symptoms, and can effectively treat small and hard-to-reach areas.
• Penumbra Indigo System. This device is designed for large clots in the pulmonary and deep venous systems and works without the need for clot-dissolving drugs, making it ideal for patients at a higher bleeding risk.
Benefits to Patients
Thrombectomies using advanced clot-removal tools can treat DVT quickly and effectively. Potential benefits include faster symptom relief, preserved vein function, and reduced risk of post-thrombotic syndrome and other serious complications.
The best outcomes happen when treatment is started early – ideally within 14 days of symptom onset. If you or a loved one is experiencing sudden leg swelling or pain, schedule a screening. A simple vascular ultrasound could uncover a hidden threat and allow a life-saving solution.


An Expert Weighs In
“The use of orthobiologic treatments continues to evolve and advance as a helpful adjunct to traditional orthopedic care. We’ve been very encouraged by positive results for the majority of individuals choosing to explore these cutting-edge options. Many patients who decide they are not physically or mentally ready for joint replacement or other surgery have been successfully treated with inoffice orthobiologic injections to manage symptoms and preserve function. We’ve also seen great success using orthobiologics as an augmentation to traditional orthopedic surgical procedures to enhance healing and optimize recovery.”

Chad Smalley, MD Shoulder & Knee Specialist, Center for Sports Medicine & Orthopaedics
Advancements in Orthobiologics
These advancements include a variety of cuttingedge treatments that harness the biologic healing powers of human cells to treat orthopedic conditions.
Understanding Orthobiologics
Orthobiologics, also known as orthopedic regenerative medicine, is a rapidly advancing field of medicine that uses natural, tissue-derived compounds to treat acute injuries and chronic or degenerative conditions affecting the muscles, bones, joints, and soft tissues. These treatments can reduce inflammation; relieve pain; promote healing after injury or surgery; and improve joint function. Orthobiologics can be administered on their own, or, more commonly, used in conjunction with physical therapy, pain management techniques, or during surgery.
How It Works
Orthobiologics work by extracting healthy platelets and/or bone marrow that contain growth factors – naturally occurring proteins that stimulate growth and healing – and other anti-inflammatory agents from a patient’s body and injecting them into the affected area. These procedures are minimally invasive and patients typically experience results within 4-6 weeks of treatment.
Common Orthobiologic Procedures
Platelet Rich Plasma (PRP). The patient’s peripheral blood is drawn and then spun in a centrifuge to separate it into layers. The PRP layer that is rich with growth factors and platelets is extracted and reintroduced into the joint.
Bone Marrow Aspirate. Bone marrow fluid, called aspirate, is extracted from a healthy bone in the patient’s body and placed in a centrifuge to generate a concentration of powerful cells. These are then reintroduced into the joint to stimulate regeneration and encourage healing.






















Advancements in Treating Teenage Acne
Multiple treatment options are available to help teenagers clear up acne.

Understanding Teenage Acne
Acne is a very common skin condition that, according to the American Academy of Pediatrics, affects approximately 85% of teenagers. It occurs when the skin’s pores become clogged with dead skin cells and excess oil and cause bacteria to multiply. Hormonal changes during puberty can increase oil production, leading to acne.
Acne can appear as blackheads, whiteheads, pimples, or nodules and cysts, and may be accompanied by redness or tenderness. While acne most commonly appears on the face, it can also affect other areas of the body, such as the neck, back, and chest.
Treatment Options
Advancements in medicine have produced many options for treating acne:
Benzoyl peroxide can be found in over-the-counter products, with a
4% concentration used for the face and 10% mainly used for body acne. Benzoyl peroxide kills bacteria without causing bacterial resistance and reduces oil production. Another over-the-counter option is adapalene cream or gel. This helps with whiteheads and blackheads if used nightly after gentle cleansing. It also helps prepare the skin for stronger retinoids commonly prescribed as part of an acne topical regimen. Retinoids promote skin cell turnover, reducing inflammation and preventing clogged pores.
Topical or oral antibiotics are prescribed to kill skin bacteria and reduce redness. Hormonal component of acne is addressed differently with several safe and effective topical and oral options, such as Winlevi and spironolactone.
Accutane is an oral medicine used to treat severe cystic acne that hasn’t responded to other treatments.
An Expert Weighs In
“Consistency is key when treating acne, with results typically beginning to appear within two months. To aid treatment, teenagers should wash their face morning and night with a gentle cleanser such as Cerave, Cetaphil, or Vanicream, and avoid picking at their skin. A dermatologist can help advise which products to use and create a personalized treatment plan to restore clear skin.”

Markiza Cooper, MD, FAAD Board-Certified Dermatologist, Uderm








Advancements in Functional Electrical Stimulation
This therapeutic method can help patients experiencing paralysis exercise their muscles.
Understanding Functional Electrical Stimulation
Functional electrical stimulation (FES) is a rehabilitative treatment that uses small electrical currents to activate specific nerves and muscles and restore lost function. FES is often used to treat patients with neurological disorders such as spinal cord injury, multiple sclerosis, cerebral palsy, traumatic brain injury (TBI), and stroke. It can also be utilized by patients experiencing weakness following surgery.
How It Works
The brain controls the body’s movement by sending electrical signals through the nerves to the muscles. If the brain or nerves are damaged, these signals become interrupted, causing muscle weakness or paralysis. FES works by replacing these lost signals with electrical currents delivered by electrodes into the body. These make the muscle contract, allowing the patient to perform movements such as lifting their leg or arm, and strengthen muscles that cannot move on their own.
New Solutions
FES devices can provide an alternative to traditional exercise equipment for patients with muscle paralysis. Advanced stationary bikes, for example, are being implemented into rehabilitation plans. Known as FES cycling, these bikes target arm and leg muscles in a pattern that allows the patient to pedal the bike and exercise.
Benefits to Patients
FES makes it possible for patients to strengthen muscles and regain functions that better their quality of life. Its benefits include:
• Preventing muscle atrophy
• Increasing blood circulation
• Maintaining or increasing range of motion
• Relaxing muscle spasms
• Reeducating muscles
FES may also help restore the ability to stand, step, and walk short distances; sit upright; and grasp objects and can improve bladder and bowel control, breathing, and swallowing.
An Expert Weighs In
“The FES cycle is great because it provides electrical stimulation to all the major muscle groups in the affected arm at once while the patient is mentally focused on performing active movement with both arms in an identical, alternating pattern. The activity is intense, intentional, and repetitive, which is ideal for the neuro-reeducation process. Patients also enjoy the FES cycle because it provides immediate feedback that can be tracked to show progression.”

Laura Hampton, OTR/L, CSRS Inpatient Therapist, Siskin Hospital for Physical Rehabilitation


An Expert Weighs In
“It is best to remove wisdom teeth between the ages of 15 and 26 to prevent an increased rate of complications and difficulty in treatment associated with the surgery as you age. As a general rule, it is much easier on the patient, doctor, and surgical team to surgically remove wisdom teeth in the younger population due to the overall health and flexibility of their bone.”

Ricky Johnson, DDS, MD Oral Surgeon, Implants & Oral Surgery of Chattanooga
Advancements in Wisdom Teeth Removal
Improved imaging and medications make this common surgery a safer and more comfortable experience.
Understanding Wisdom Teeth
Wisdom teeth refers to the third molars, which are located at the back of the mouth and are the last teeth to emerge. When wisdom teeth become impacted, or overcrowded, they put pressure on the neighboring molars and can lead to problems including pain, cavities, bone loss, cysts, tumors, and infections. Surgical removal can help prevent these problems and is recommended between the ages of 15 and 26 to reduce the risk of complications.
New Solutions
Wisdom teeth removal surgery is a very common procedure, and advancements in imaging and medications have made strides in improving the patient experience. Imaging technology is used to view wisdom teeth placement and inform plans for the procedure. Conebeam CT scans are an innovative imaging option that can produce detailed, three-dimensional images of the teeth and mouth, as well as the nerves and vessels.
Anesthesia is administered during the procedure to aid a pain-free experience. Advancements in medicine have produced a variety of options, which include local anesthesia, nitrous oxide, conscious oral or IV sedation, and general anesthesia.
Pain medication can assist the healing process. Prescriptions may include narcotics for acute episodes of pain, and non-opioid options are available for use throughout recovery.
Benefits to Patients
Detailed imaging allows for precise planning that reduces the risk of complications, while anesthesia and pain medication have improved patient comfort during and after removal. Knowing these advancements are available to prevent complications and ease discomfort can be a great relief to any anxieties patients may have about this procedure.



An Expert Weighs In
“CatarActive3® was designed to improve compliance with post-surgery regimens. Dr. Robin Brady asked for help after 20 years of seeing patients struggle with three separate eye drops. He wanted to simplify healing, knowing recovery is critical. I created this solution to serve all cataract patients. My greatest joy is delivering a bottle to someone in Haiti - where blindness can last years before surgery. Restoring sight is a blessing. The good Lord provides to all His children.”

Randy Davis, DPh President & Owner, Designer Drugs
Advancements in PostCataract Surgery Care
Compounded eye drops are making care convenient following cataract surgery.
Understanding Cataracts
Cataracts refer to the clouding of the eye’s lens and resulting blurry vision. This condition can be remedied through cataract surgery, a common procedure that removes the clouded lens and replaces it with an artificial one to restore clear eyesight. Following cataract surgery, or any type of eye procedure, patients are instructed to follow an eyecare regimen to aid comfort and ensure proper healing. This traditionally involves three individual eye drops, however a new solution has emerged to make postoperative care more convenient.
New Solutions
CatarActive3® is an innovative option that combines these three components – an antibiotic, steroid, and anti-inflammatory – into a one-drop solution. The compounded eye drop is comprised of moxifloxacin (fluroquinolone antibiotic), dexamethasone (steroid), and bromfenac (nonsteroidal anti-inflammatory). Patients simply use one bottle of CatarActive3® four times daily until the bottle is empty for each eye.
Benefits to Patients
By combining care into a single bottle, CatarActive3® streamlines the postoperative care process for patients and providers alike. Patients don’t have to worry about juggling three eye drops, which often require different doses and are taken at different times of the day. Instead, CatarActive3® is easy to use, with straightforward instructions that prevent confusion and the need for calls to providers with questions. It also cuts down on costs by requiring only one prescription and payment instead of three. With this advanced solution, patients can complete their postoperative regimen with confidence.

THIS LOOKS FAKE.

Advancements in Prenatal Care
Personalized options are helping improve care during pregnancy.

Understanding Prenatal Care
Prenatal care is one of the most common preventative services in the United States and plays a crucial role in the well-being of pregnant women and their children. Early and regular checkups can ensure both the patient and her baby are healthy, prevent and treat any problems, and provide education on what to expect before, during, and after birth.
New Solutions
The American College of Obstetricians and Gynecologists recently released a clinical consensus titled “Tailored Prenatal Care Delivery for Pregnant Individuals,” which details ways that providers can improve upon the prenatal patient experience and personalize care. These advancements include:
Virtual offerings. Providers can combine in-person and virtual appointments, or telemedicine, according to their patient’s needs and stage of pregnancy,
allowing women to conveniently receive care from the comfort of home. Shared decision-making. During initial visits, providers can learn their patient’s preferences and encourage patients to participate in creating a personalized care plan informed by a comprehensive prenatal assessment.
Personalized visits. Tailoring visit frequency and appointment lengths can ensure patients have time to ask questions and leave feeling confident in their care plan. To further improve the patient experience, practices can assign a designated member of the care team to work with each patient and guide her on what to expect at each appointment.
Comprehensive care. In addition to a full range of OB/GYN services, providers can take an approach that looks at all aspects of well-being, such as sleep, stress, diet, and exercise. These offerings can include mental health care, diet and nutrition counseling, health coaching, classes for continued education, and more.
An Expert Weighs In
“Diana Health offers a wholehealth approach to maternity care that is compassionate, individualized, accessible, and empowers each patient to be in the driver’s seat of her care experience.”

Jack Rowland, MD Physician and Medical Director, Diana Health Chattanooga






Maternity Care Where...



















Robert L. Huang, MD
The Chattanooga Heart Institute Interventional Cardiology

Brian H. Negus, MD
The Chattanooga Heart Institute Interventional and Vascular Cardiology

John M. Craig, MD
The Chattanooga Heart Institute Cardiothoracic Surgery

Henry G. Cheng, MD
The Chattanooga Heart Institute Cardiovascular Disease


Krish Bhadra, MD
CHI Memorial Interventional Pulmonology Interventional Pulmonologist

John C. House, MD
CHI Memorial Urology Associates Urologist

Aaron R. Soufer, MD
The Chattanooga Heart Institute Cardiovascular Disease
L. Richard Sprouse, II, MD
CHI Memorial Vascular Surgery Specialists Vascular Surgeon
TOP DOCTORS
For many, one of the greatest challenges when a loved one falls ill, or needs care, is discerning where to go. You want to know that the doctor you are seeing is top-tier, trusted, and has you and your loved one’s best interests at heart.
Luckily, for residents living in Southeast Tennessee and North Georgia, our area is burgeoning with leading physicians who
have dedicated their lives to providing the highest level of care for patients and their families. However, with so many options, it can be even more difficult to choose where to seek care.
To help alleviate the challenges that can come with choosing a healthcare provider, HealthScope® magazine partnered with Castle Connolly, the leading physician research firm, to
compile a list of our area’s most outstanding physicians. What follows are many of our region’s most exemplary physicians, as selected by their peers and thoroughly vetted by Castle Connolly. While this peer-nominated and highly vetted list provides an incredible resource, it is not a finite list. Rather, it provides a strong foundation as you look after your health and that of your loved ones.
ALLERGY & IMMUNOLOGY
Marc Cromie, MD
Chattanooga
Allergy Clinic
423.899.0431
Todd Levin, MD
Chattanooga
Allergy Clinic
423.899.0431
Jennifer Patel, MD
Chattanooga
Allergy Clinic
423.899.0431
Lee M. Perry, MD
Chattanooga
Allergy Clinic
423.899.0431
Jessica Van Mason, MD
Chattanooga
Allergy Clinic
423.899.0431
BARIATRIC SURGERY
Jaime Ponce, MD
Weight Loss Center of Chattanooga
423.362.5673
CARDIAC ELECTROPHYSIOLOGY
Michael C. Allan, MD
Centennial Heart at Parkridge
423.508.6733
Anand S. Kenia, MD
Vitruvian HealthHeart & Vascular
706.226.3434
CARDIOVASCULAR DISEASE
Alison L. Bailey, MD
Centennial Heart at Parkridge
423.508.6733
Henry G. Cheng, MD
The Chattanooga Heart Institute
423.697.2000
Hugh Coke, MD
Vitruvian HealthHeart & Vascular
706.226.3434
Aaron R. Soufer, MD
The Chattanooga Heart Institute
423.697.2000
COLON & RECTAL SURGERY
Alan Hyde, MD
University Surgical Associates
423.267.0466
Eric C. Nelson, MD
University Surgical Associates
423.267.0466
J. Daniel Stanley, MD
University Surgical Associates
423.267.0466
DERMATOLOGY
Deanna G. Brown, MD
Four Bridges Dermatology & Cosmetics
423.521.4232
Laura Cleary, MD
Four Bridges Dermatology & Cosmetics
423.521.4232
Cara F. Hennings, MD
Four Bridges Dermatology & Cosmetics
423.521.4232
DEVELOPMENTALBEHAVIORAL PEDIATRICS
Lorena Ferreira, MD
Siskin Children’s Institute
423.490.7710
Jenesis Yanez, MD
Siskin Children’s Institute
423.490.7710
ENDOCRINOLOGY, DIABETES & METABOLISM
Carlos Peñaherrera, MD
Hamilton Diabetes and Endocrinology
706.278.1622
FACIAL PLASTIC SURGERY/ OTOLARYNGOLOGY
James R. Shire, MD
Shire Facial Plastic Surgery
423.888.0385
FAMILY MEDICINE
Suzannah L. Bozzone, MD
True Health Journey
423.521.8783
FAMILY MEDICINE (CONT.)
Hannah Bujak, MD
Galen Mountain View Medicine
423.551.3562
Oliver Bujak, MD
Galen Mountain View Medicine
423.551.3562
John “Chip” Harris, MD
Erlanger Primary CareSouth 706.937.9292
Julie H. Haun, MD
Galen North Internal Medicine
423.870.2450
James W. Haynes, MD
Erlanger Family Medicine
423.778.8837
GASTROENTEROLOGY
Sergio F. Quijano, MD
Hamilton Physician Group – Gastroenterology
706.272.4127
INTERNAL MEDICINE
Bradley Keel, DO
Southeast Medical GroupRestore Health and Wellness
423.888.5930
INTERVENTIONAL CARDIOLOGY
Selwin J. Abraham, MD Vitruvian Health –Heart & Vascular
423.476.4466
Robert L. Huang, MD The Chattanooga Heart Institute 423.697.2000
Brian H. Negus, MD
The Chattanooga Heart Institute
423.697.2000
Ateet B. Patel, MD Vitruvian HealthHeart & Vascular
706.226.3434
NEPHROLOGY
Kenneth Kokko, MD Nephrology Associates
423.826.8000
NEUROLOGICAL SURGERY
Peter Boehm Jr., MD Erlanger Neurosurgery and Spine
423.778.2233
Daniel Kueter, MD Erlanger Neurosurgery and Spine 423.778.2233
NEUROLOGY
Joshua Alpers, MD
Erlanger Neuroscience Institute
423.778.9001
OBSTETRICS & GYNECOLOGY
Patricia K. McLelland, MD
Galen OB/GYN East
423.899.9133
OPHTHALMOLOGY
John R. Bierly, MD
SouthEast Eye Specialists
423.508.7337

OPHTHALMOLOGY (CONT.)
Sophie Cai, MD
Southeastern Retina Associates 423.756.1002
Francis C. DeCroos, MD Southeastern Retina Associates 423.756.1002
Devon H. Ghodasra, MD
Southeastern Retina Associates 423.756.1002
Asghar “Abbas” Haider, MD
Southeastern Retina Associates 423.756.1002
Joshua F. Hendrix, MD Professional Eye Associates
706.226.2020
Brian Kim, MD Professional Eye Associates
706.226.2020
Robert E. Levy, MD Chattanooga Eye Institute 423.892.3937
Elizabeth D. Mabry, MD Mabry Eye Center 423.385.2020
Timothy E. O’Boyle, MD Professional Eye Associates
706.226.2020
Edward A. Peterson, MD SouthEast Eye Specialists
423.508.7337
ORTHOPAEDIC SURGERY
W. Timothy Ballard, MD Center for Sports Medicine & Orthopaedics
423.624.2696
Todd Bell, MD Center for Sports Medicine & Orthopaedics
423.624.2696
Brandon Cincere, MD Erlanger Sports Medicine
423.778.3390
John A. “Jad” Dorizas, MD Erlanger Sports Medicine
423.778.3390
Jesse Doty, MD Erlanger OrthopaedicsFoot and Ankle 423.778.6784
Benjamin Geddes, MD Center for Sports Medicine & Orthopaedics
423.624.2696
Joshua A. Lawson, MD Center for Sports Medicine & Orthopaedics
423.624.2696
John Nash, MD Center for Sports Medicine & Orthopaedics
423.624.2696

ORTHOPAEDIC SURGERY (CONT.)
Jason M. Rogers, MD
Center for Sports Medicine & Orthopaedics
423.624.2696
PEDIATRIC SURGERY
S. Dave Bhattacharya, MD University Surgical Associates
423.267.0466
Curtis S. Koontz, MD
University Surgical Associates
423.267.0466
PEDIATRIC UROLOGY
Israel Franco, MD
Erlanger Children’s Urology
423.778.5910
PEDIATRICS
Tonia R. Cox, MD
Pediatric Diagnostic Associates
423.698.2229
Delia A. Wessels, MD
Allied Pediatrics
423.602.9545
PLASTIC SURGERY
Mark A. Brzezienski, MD
Erlanger Plastic and Reconstructive Surgery
423.778.9224
Christopher W. Chase, MD Associates in Plastic Surgery
423.624.0021
Larry A. Sargent, MD
Sargent Plastic Surgery
423.305.7274
Todd E. Thurston, MD
Erlanger Plastic and Reconstructive Surgery
423.778.9224
PULMONARY DISEASE
Krish Bhadra, MD
CHI Memorial Interventional Pulmonology
423.531.6104
RADIATION ONCOLOGY
Ryan K. Cleary, MD
Erlanger Radiation Oncology
423.778.9506
John Fortney, MD
Tennessee Oncology
877.836.6662
Patrick Williams, MD
Tennessee Oncology
877.836.6662
REPRODUCTIVE ENDOCRINOLOGY/ INFERTILITY
Rink Murray, MD
Tennessee Reproductive Medicine
423.509.8094
Jessica Scotchie, MD
Tennessee Reproductive Medicine
423.509.8094
RHEUMATOLOGY
Richard W. Brackett, MD
Scenic City Rheumatology
423.893.6890


RHEUMATOLOGY (CONT.)
Michael Brit, MD University Rheumatology Associates
423.778.4396
Jayne Crowe, MD University Rheumatology Associates
423.778.4396
Lizeth Romero, MD University Rheumatology Associates
423.778.4396
Elizabeth Turner, MD University Rheumatology Associates
423.778.4396
SPORTS MEDICINE
Bradford Mitchell, MD Center for Sports Medicine & Orthopaedics
423.624.2696
L. Shay Richardson, MD Center for Sports Medicine & Orthopaedics
423.624.2696
Jason Robertson, MD Center for Sports Medicine & Orthopaedics
423.624.2696
SURGERY
Christopher Bell, MD University Surgical Associates
423.267.0466
R. Phillip Burns, MD University Surgical Associates
423.267.0466
W. Todd Cockerham, MD University Surgical Associates
423.267.0466
Benjamin W. Dart IV, MD University Surgical Associates
423.267.0466
W. Heath Giles, MD University Surgical Associates
423.267.0466
Stephen Greer, MD University Surgical Associates
423.267.0466
John Huggins, MD University Surgical Associates
423.267.0466
Darren J. Hunt, MD University Surgical Associates
423.267.0466
Robert J. Jean, MD University Surgical Associates
423.267.0466
Neelima Katragunta, MD University Surgical Associates
423.267.0466
Benjamin E. Kellogg, MD University Surgical Associates
423.267.0466
We’re proud to celebrate our Galen doctors named Top Doctors by their peers – a testament to their unwavering commitment to delivering the very best in patient care.
When you need care – choose Galen.

Dr. Hannah Bujak Family Medicine
Galen Mountain View Medicine

Dr. Elizabeth Mabry
Ophthalmology
Mabry Eye Center

Dr. Oliver Bujak Family Medicine
Galen Mountain View Medicine

Dr. Julie Haun Internal Medicine
Galen North Internal Medicine

Dr. Patricia McLelland
Obstetrics & Gynecology
Galen OB/GYN
The Allergy Asthma Group of Galen Center for Diabetes & Endocrinology
Galen Dermatology
Galen Digestive Health
Galen East Internal Medicine & Pediatrics
Galen Hepatology
Galen Mountain View Medicine
Galen North Internal Medicine
Galen North Pediatrics
Galen OBGYN - East
Galen OBGYN - Ridgeside
Galen Primary Care - North Georgia
Galen Primary Care - Southside
Galen Research
Galen Surgery - Vascular
Mabry Eye Center
galenmedical.com
SURGERY (CONT.)
Alan J. Koffron, MD University Surgical Associates
423.267.0466
Julie A. Koffron, MD University Surgical Associates
423.267.0466
Vicente A. Mejia, MD University Surgical Associates
423.267.0466
S. Michael Roe, MD University Surgical Associates
423.267.0466
Lisa A. Smith, MD University Surgical Associates
423.267.0466
Beth Snell, MD University Surgical Associates
423.267.0466
With over 30 years’ experience researching, reviewing, and selecting Top Doctors, Castle Connolly is a trusted and credible healthcare research and information company. Its mission is to help people find the best healthcare by connecting patients with best-in-class healthcare providers.
Castle Connolly’s physician-led team of researchers follows a rigorous screening process to select top doctors on both the national and regional levels. Its online nomination process is open to all licensed physicians in America who are able to nominate physicians in any medical specialty and in any part of the country, as well as indicate whether the nominated physician(s) is, in their opinion, among the best in their region in their medical specialty or among the best in the nation
SURGICAL ONCOLOGY
Alvaro A. Valle, MD University Surgical Associates
423.267.0466
THORACIC & CARDIAC SURGERY
John M. Craig, MD
The Chattanooga Heart InstituteCardiothoracic Surgery
423.624.5200
UROLOGY
John C. House, MD CHI Memorial Urology Associates
423.756.7860
Anand Shridharani, MD
Erlanger Urology
423.778.5910
VASCULAR SURGERY
Eugene D. Eddlemon, MD
University Surgical Associates
423.267.0466
Michael S. Greer, MD University Surgical Associates
423.267.0466
Charles Joels, MD University Surgical Associates
423.267.0466
Christopher LeSar, MD Vascular Institute of Chattanooga
423.602.2750
L. Richard Sprouse II, MD CHI Memorial Vascular Surgery Specialists
423.654.7670
in their medical specialty. Then, Castle Connolly’s research team thoroughly vets each physician’s professional qualifications, education, hospital and faculty appointments, research leadership, professional reputation, disciplinary history and if available, outcomes data. Additionally, a physician’s interpersonal skills such as listening and communicating effectively, demonstrating empathy, and instilling trust and confidence, are also considered in the review process. The Castle Connolly Doctor Directory is the largest network of peer-nominated physicians in the nation.
Physicians selected for inclusion in HealthScope® magazine’s “Top Doctors” feature may also appear online at www.castleconnolly.com, or in in conjunction with other Castle Connolly
Top Doctors databases online and/or in print.
Castle Connolly is part of Everyday Health Group, a recognized leader in patient and provider education, attracting an engaged audience of over 74 million health consumers and over 890,000 U.S. practicing physicians and clinicians to its premier health and wellness digital properties. Its mission is to drive better clinical and health outcomes through decision-making informed by highly relevant information, data, and analytics. The organization empowers healthcare providers and consumers with trusted content and services delivered through Everyday Health Group’s world-class brands. For more information, please visit Castle Connolly or Everyday Health Group.





















D R . M A R C C R O M I E
Dr. Cromie is a double board-certified pediatric and adult allergy and asthma specialist, licensed in Tennessee and Georgia. He earned his medical degree and completed an Allergy/Immunology fellowship at the Medical College of Georgia. He has practiced at Chattanooga Allergy Clinic since 2000 and currently serves as a clinical instructor at T.C. Thompson Children’s Hospital and the UT College of Medicine. Active in the community, he has held leadership roles in several medical and nonprofit organizations. Dr. Cromie is a lifelong sports fan and enjoys time with his wife and five children. His personal affliction with childhood asthma and allergies allows him to relate to patients of all ages.
D R T O D D L E V I N
Dr. Levin is a double board-certified pediatric and adult allergy and asthma specialist, licensed in Tennessee and Georgia. He earned his medical degree from the Medical College of Georgia in 2001, where he was inducted into the Alpha Omega Alpha Honor Society. After completing his Allergy/Immunology fellowship, he joined Chattanooga Allergy Clinic in 2006. Dr. Levin is a Fellow of both the AAAAI and ACAAI and serves as a clinical instructor at T.C. Thompson Children’s Hospital. He has held leadership roles in various medical and community organizations. Dr. Levin enjoys sports, cooking, and time with his wife Rebecca and their two children.
D R . L E E P E R R Y
Dr. Perry is a double board-certified pediatric and adult allergy and asthma specialist, licensed in Tennessee and Georgia. He earned his medical degree in 2004 and completed both his pediatric residency and Allergy/Immunology fellowship at the Medical College of Georgia. He joined Chattanooga Allergy Clinic in 2009 and is a Fellow of the AAAAI and ACAAI. Dr. Perry serves on staff at Erlanger Medical Center and is active with the American Lung Association. As a father of children with severe allergies and asthma, he brings personal insight to patient care. He enjoys sports and spending time with his wife Leanne and their six children.
D R . J E N N I F E R PAT E L
Dr. Jennifer Patel is double board-certified in allergy and immunology as well as internal medicine. She completed her medical degree, residency, and fellowship at the University of Tennessee, giving her firsthand insight into the allergy challenges faced by Tennesseans. She holds a biology degree and is an active member of the AAAAI and ACAAI. Dr. Patel treats both pediatric and adult patients, with a special interest in the treatment of food allergies. Outside of work, she enjoys the outdoors and spending time with her family.
D R . J E S S I C A VA N M A S O N
Dr. Van Mason is a double board-certified allergy and immunology specialist, trained to treat both children and adults. She completed her medical degree, pediatric residency, and fellowship in Kansas City and moved to Chattanooga in 2020. Her research has focused on social determinants of health and home environmental impacts on allergic disease and asthma. She has published articles on accelerated immunotherapy as well as the primary prevention of asthma. She serves as a Clinical Assistant Professor of Pediatrics at the University of Tennessee College of Medicine Chattanooga. Outside of medicine, she enjoys photography, yoga, cookies, football, and spending time outdoors with her family.


Burnout Blues
BREAKING DOWN OCCUPATIONAL BURNOUT
Whenburnout strikes, it can feel unbeatable. High stress levels, exhaustion, cynicism, and falling behind on tasks are only a few signs that work might be taking a toll on your well-being. The World Health Organization defines occupational burnout as “resulting from chronic workplace stress that has not been successfully managed.” That means those suffering from burnout may feel like a weekend or vacation isn’t enough to reset and refresh them for the new workweek.
Hope is not lost, however. Understanding the factors that lead to burnout can determine what steps are necessary for recovery. To learn more, we chatted with burnout and holistic career coach Lydia Fogo Johnson, founder of ThriveCulture Coaching.
SOS! I am experiencing all the signs of burnout from work, and I don’t know what to do. How do I get unstuck?
LFJ: Let’s back up – did you know there are at least four distinct types of burnout? So, the first step to getting unstuck is identifying the kind of burnout you’re suffering from and then taking steps specific to your burnout profile.
Wow, I had no idea. What are the different types of burnout?
LFJ: Overload burnout is when you have too much to do and not enough time to do it. You may be working long hours, at an unsustainable pace, or without adequate breaks. You probably do need better work/life balance if you’re suffering from this type of burnout!
Under-challenge burnout is when your job feels boring, uninteresting, or unchallenging. Check in with yourself: When did you last learn something new related to your job? If you’re stuck in a lackof-growth rut, look into opportunities to hone your skills, get new training, or take on a stretch project. You’d be surprised at how much you can tweak your tasks to be a better fit – this is called job crafting.
Neglect burnout is when you feel “neglected” due to a lack of support and resources. You may be struggling with feeling helpless or incompetent. Try to get to the root of your challenge by listing the specific areas you’re struggling with and why this has been so difficult. Then, ask yourself the question: What could change in order for me to feel confident and supported in this task/situation?
Lack of purpose burnout is when your role no longer feels meaningful or important. Look for the “why” behind your job. What’s the big picture here? How are you helping others with your work? Imagine a world where your job doesn’t exist – no one on earth is doing what you do. How would we be worse off?
How is burnout different from compassion fatigue?
LFJ: Traditional burnout stems from chronic stress, but compassion fatigue arises from the emotional labor of caring for others, especially in high-stakes or trauma-exposed environments.
While burnout can affect anyone, compassion fatigue is particularly relevant in professions where emotional investment is part of the job. Recognizing and addressing these challenges is a vital part of maintaining long-term well-being in high-impact fields.
What are a few strategies to avoid burnout in the first place?
LFJ: Know your warning signs that stress is rising. The first step to burnout prevention is noticing when your chronic stress levels are starting to creep out of control. For example, my red flags are when my creativity disappears and my mind feels like it’s constantly racing.
Protect your recovery time. Your off-hours aren’t optional – they’re how your brain and body reset. Prioritize restorative and restful activities that refuel your cup and protect your mental health: sleep, movement, time with people you love, and activities that give you energy. Word of warning: although screen time is tempting when you’re drained, it does little to refuel you!
Detach mentally after work. If your mind keeps spinning about work when you’re off, you’re not in recovery mode. If you struggle to mentally detach from work worries, try an end-of-work transition ritual (like a walk or music) to shift gears, or use mindfulness practices to come back to the present.
There are definitely some changes I want to make for a more balanced workload –should I broach the topic with my team?
LFJ: Research consistently shows that incorporating diverse perspectives leads to better decision-making. You can gain fresh insights and approaches to address your challenges effectively by seeking input from others.
Ask for help early – don’t wait until you’re underwater. Even though it can feel vulnerable, it’s best to let your manager know when you’re overloaded so you can reprioritize together.

Lydia Fogo Johnson, MS, ACC Holistic Career Coach & Founder, ThriveCulture Coaching @thriveculture.coach
Better Together
The Importance of Support Systems
By Ali Lemmons












































Having people you can rely on – whether it’s for a helping hand or just a listening ear – can make all the difference for your mental and physical well-being. That’s why it’s essential to have a support system: a network of friends, family, or loved ones who can offer emotional and practical assistance during life’s highs and lows. Here, we explore the benefits of a support system, how to build one, and how it can affect your long-term health.
The Benefits of a Support System
A support system includes the people in your life who offer encouragement, listen without judgment, and help you navigate challenges –whether emotional, practical, or both. Research shows that relationships like these can have a positive impact on your mental health. Friends and other close relationships can boost your sense of purpose, increase feelings of happiness, and lower feelings of stress.
According to the Mayo Clinic, having close friends can also play a role in your physical well-being. Research shows that adults with strong social connections have a lower risk of depression, high blood pressure, and unhealthy weight levels, and some studies have found that adults with strong support systems are more likely to live longer than those who don’t.
How to Build and Maintain a Support Network
Building a strong support system takes time and commitment. Your support system can
include family, friends, coworkers, mentors, and more. When looking to grow your social circle, it may be necessary to step outside of your comfort zone. Joining a new club, volunteering in your community, and signing up for workout or educational classes can help you meet new people and develop like-minded connections. Once you’ve established a close circle of supporters, it’s important to nurture those relationships. Remember, support is a two-way street. Keep your circle up to date about your life, accept and extend invitations to social events, and offer your own advice and practical help when someone in your life needs it.
Support Makes a Difference
From everyday challenges to life-changing events, having people to lean on in times of stress can make tough times all the more manageable. Whether it’s a trusted family member, friend, or coworker, having a reliable support system helps you stay grounded, resilient, and mentally strong – no matter what comes your way.






Skincare for Healthcare Professionals
Four Products to Amplify Your Routine
A busy schedule can sometimes mean your skincare routine falls to the wayside. Protect, heal, and moisturize your skin with these four easy-to-use, nourishing products. While washing your hands frequently is critical to killing germs and stopping the spread of disease, antibacterial soaps can disrupt the skin barrier, leading to dry and cracked hands. For those in the healthcare industry, caring for your hands helps ensure they stay moisturized and comfortable. Gloves In A Bottle Hand Shielding Lotion is specially formulated to act as an invisible barrier against water and soaps, allowing you to have clean hands while still maintaining moisture. It’s fragrance free, tested by dermatologists, and safe to use in hospital settings.
By Kristen Dee




While antibacterial agents like alcohol can strip the skin, hypochlorous acid is less drying and eases inflammation associated with acne, eczema, and other skin conditions. When used in spray form, it can help fight bacteria on the surface of the skin while soothing irritation. A popular option is the Tower 28 SOS Daily Rescue Spray, which comes in a large bottle or smaller travel size and is perfect for at-home or on-the-go use. The spray has acceptance seals from the National Eczema Association and the National Rosacea Society, making it a great option for sensitive skin.
Nothing feels better than washing your face after a long day at work. Cerave Acne Foaming Cream Face Cleanser will leave your skin squeaky clean while helping to fight acne and hydrate the skin. It’s formulated with benzoyl peroxide to help clear and prevent acne, and hyaluronic acid, niacinamide, and ceramides to help soothe and hydrate. Follow it up with your favorite serum or moisturizer to lock in hydration and further protect your skin barrier.
Lips can easily become dry and chapped from mask wearing or navigating a busy patient schedule. Keep lips nourished all day with Paula’s Choice Pro-Collagen Peptide Gloss Balm lip treatment. Described as a balm that “packs the power of a lip treatment, the sheen of a gloss, and the deep hydration of a balm into one,” this formula soothes chapped lips and keeps them moisturized for hours.








PURE Face Care is a leading medical spa offering a unique blend of medical esthetics and traditional spa therapies. Our personalized “East Meets West” approach ensures you receive the highest quality skincare treatments, tailored to your specific needs. From rejuvenating facials to advanced procedures like laser resurfacing and injectables, we're committed to helping you achieve your skincare goals. Our focus on transparency, honesty, and exceptional customer service sets us apart.




Styling Scrubs
Many healthcare professionals spend their workday in scrubs – comfortable, sanitary clothing worn in clinical and surgical settings. While it’s important to keep things simple and safe on the job, adding practical, professional accessories can add a pop of personality and help you feel fashionable when in uniform. Here, Misty Craig and Vicky Villanueva with Medical Outfitters share the many ways scrubs can be styled and personalized from head to toe.
Photography by Kristina Armstrong Scrubs modeled by Ainsley Craig
“Accessorizing medical scrubs can add personality and style while still keeping things professional and functional.”


Misty Craig Owner, Medical Outfitters
Functional Accessories
These items can combine both practicality and personality.
• Badge reels or holders – choose a creative retractable reel (think monograms, glitter, or character designs)
• Compression socks – available in tons of fun patterns, these support your legs during long shifts
• Utility belts or fanny packs – especially for nurses or techs, these can hold essentials like scissors, pens, and alcohol wipes
• Penlights or clipboards – select sleek designs or colors to match your personality
Jewelry
Stick to small, non-dangling items that won’t get in the way.
• Stud earrings – simple and safe for a clinical setting
• Silicone rings – comfortable and safe alternatives to metal bands
Footwear
Your shoes can be supportive and comfortable without sacrificing style.
• Sneakers or clogs with colorful designs
• Shoe charms or lace clips – small, cute additions that make your shoes pop
Hair Accessories
If you wear your hair up, these accessories can add a personalized touch.
• Patterned or sparkly headbands
• Colorful scrunchies or clips
• Surgical caps in fun patterns or seasonal prints
Embroidery
Custom embroidery can make your scrubs one-of-a-kind.
• Single letter or initials monograms
• Name with credentials
Vicky Villanueva Owner, Medical Outfitters
• Logos
• Appliqués
• Custom designs


Guide to Trauma-Informed Design
By Tory Irmeger
Have you ever walked into a building and felt out of place? Odds are, it’s not just you. Physical spaces – whether it’s our homes, workplaces, schools, health facilities, or places of worship – can impact our emotions and behaviors in both positive and negative ways. Trauma-informed Design (TiD) explores this, promoting personal and communal spaces that promote wellness, healing, and safety for all.
What is Trauma-Informed Design?
According to the Trauma-informed Design Society, TiD is based on trauma-informed care, integrating those principles into physical spaces. Trauma-informed care, established by the Substance Abuse and Mental Health Services Administration (SAMHSA), is an approach that actively avoids re-traumatization for patients and staff while integrating knowledge about trauma into policies, procedures, and practices.
Why consider trauma when designing spaces? Without meaning to, it’s possible to perpetuate trauma with design elements that trigger individuals with traumatic histories. Common triggers, such as buzzing noises, fluorescent lights, or dark stairwells, can cause psychological distress and make an individual feel as though they’re in danger. TiD is an opportunity to remove these triggers and opt for more inclusive, balanced spaces that cultivate safety and connection.
Core Principles of Trauma-Informed Care
Safety - Both physical and psychological safety is promoted for patients and staff.
Trustworthiness + TransparencyDecisions regarding care are made with transparency with the goal of building trust.
Peer Support - Individuals with shared experiences are viewed as integral to service delivery.
Collaboration - Power differences are leveled to support shared decision-making.
Empowerment - Patient and staff strengths are recognized, built on, and validated, fostering resilience and healing.
Humility + Responsiveness - Historical trauma, biases, and stereotypes (based on race, ethnicity, sexual orientation, age, or geography) are recognized and addressed.
Applying Care to Design
When applying trauma-informed care to design, choices typically promote a sense of safety, respect, community, and dignity for the individuals who will be using the space. This can be applied to living areas, classrooms, offices, care facilities, and other communally used spaces. While there is no one-size-fits-all approach to TiD, there are some key findings to consider:
Prioritize a connection to nature. Views of greenery, trees, and gardens promote wellbeing, healing, and reflection. Maximize natural daylight as much as possible.
Quality design materials Show care for guests by choosing durable materials and maintaining clean, well-ventilated spaces. Artful décor can foster connection among guests while offering a positive distraction from any negative feelings.
Easy access and wayfinding. Guests may feel more comfortable if interiors are predictable and navigable. Make sure entrances are easy to locate and appropriate signage directs individuals between spaces.
Provide clear circulation paths. Accessible pathways allow guests to choose how they move through the space. Avoid obstructing sightlines, such as in corridors or stairwells, and instead, ensure these areas are well-lit and visually clear.
Offer a variety of adaptable spaces. The option to adjust one’s surroundings gives a sense of comfort and empowerment. Lightweight, movable furniture offers guests the choice to customize their space, as do features like adjustable thermostats, partitions, and lighting. Design for privacy and safety. Guests may feel safer if there are visual security measures, such as locked storage space for personal items. Invest in walls or adjustable partitions that promote acoustical privacy, which can mitigate loud noises and create a quiet place to retreat.
Like trauma-informed care, TiD is centered on building meaningful, trusting relationships and promoting community and beauty. By recognizing the emotional power of physical spaces, we can take the first step in designing a more hospitable world.
Beyond the 9 to 5
Keeping Relationships Strong With an Unconventional Schedule
By Lindsey Clute
In today’s fast-paced work culture, where more adults than ever are clocking in for at least 40 hours each week, balancing work and relationships can be a challenge. At the forefront of this struggle are those working nontraditional shifts – overnights, weekends, or split schedules – making maintaining meaningful relationships more difficult. These off-hour demands don’t just disrupt sleep, they can disrupt connection, routine, and intimacy. When your schedule doesn’t match the rest of the world’s, staying connected to the people who matter most takes intentional effort.
Work-Relationship Balance
In 2018, the Bureau of Labor Statistics reported that over 30 million Americans (16% of all wage and salary workers) work irregular hours. Balancing work and relationships under these conditions can be tricky, but not impossible. Whether you’re trying to be more present with your family as a thirdshift worker, invest in a romantic relationship while working weekends, or maintain a social calendar while juggling an unpredictable schedule, it often starts with assessing how you spend your downtime to create small, meaningful moments that strengthen your relationships – even when time is limited.
Staying Connected as a Couple
Differing schedules can put strain on a relationship, resulting in missed meals or solo weekends. While finding large stretches of time to spend together may not always be easy, building a work-relationship balance that caters to both you and your partner is possible with intentional habits.
DO:
• Prioritize quality over quantity. Even short interactions like a catch-up before bed or a quick phone call during a break can build closeness.
• Plan recurring rituals or dates, like a Saturday morning walk after a night shift or Sunday night takeout. Predictability, even in small ways, can anchor you both.
• Communicate often and clearly. Let your partner know what you need emotionally and practically. Transparency can prevent misunderstandings and conflict.
DON’T:
• Assume your partner isn’t trying. Fatigue and burnout are common with shift workers, and it can impact their ability to connect. Offer grace and listen without judgment.
• Overbook the little time you have together. Leave room for flexibility, rest, and simply being present together, even without a specific activity planned.
Being a Present Parent
Wanting to be present with your children when you have completely opposite schedules is a common challenge – the U.S. Census Bureau reports that 43% of kids have a parent whose work schedule would be considered nontraditional. While you may sometimes miss bedtime routines or school events, there are still plenty of ways to stay involved.
DO:
• Build a consistent routine that fits your availability. For example, if you can’t make dinner, have a dedicated breakfast ritual before school.
• Make time visible. Use calendars, countdowns, or visual reminders so your child knows when they’ll see you next. This builds anticipation and emotional security.
• Stay engaged even when you’re apart. Quick video chats, notes in lunchboxes, or voice recordings can help your child feel connected throughout the day.
DON’T:
• Compare yourself to parents with traditional schedules. Your family dynamic is unique, and comparing only adds pressure.
• Assume missed time equals missed connection. Children value consistency, not necessarily the clock. It’s the quality of your presence that matters most.
Maintaining Friendships
Lastly, trying to keep up with friends as a night-shift or weekend worker can feel exhausting without proper planning. You may find yourself turning down invitations or losing touch with friends simply because your free time never matches theirs. However, social connection is essential to well-being, and learning how to nurture friendships while navigating an unconventional schedule is easier than it may seem.
DO:
• Be upfront about your availability. Let your friends know what windows work for you (even if it’s Tuesday mornings instead of Friday nights).
• Initiate one-on-one hangouts during your “weekend,” even if it falls midweek – and make the effort to plan ahead.
• Find creative ways to stay connected: daily checkins, shared playlists and memes, or quick voice messages can go a long way.
DON’T:
• Disappear entirely and assume friends will understand why. A little communication can make a big difference.
• Say yes out of guilt. Protect your rest and recovery. Real friends will understand your boundaries and appreciate your effort, even in small doses.

Foods to Fuel Your Day
Everything you eat is converted into energy, however the type of food you choose can make all the difference in feeling energized versus exhausted throughout the day. Read on to learn what to eat to enjoy lasting energy and wave goodbye to lethargy.
By Rachel Studebaker
Eat to Energize
To prevent fatigue, these two food groups are key:
COMPLEX CARBOHYDRATES
Carbohydrates are the main source of energy for your body. Complex carbohydrates in particular are high in fiber and take longer for the body to break down, providing a steady energy supply throughout the day. They include whole grains like oats, brown rice,
and quinoa; legumes like beans and lentils; starchy vegetables like potatoes and corn; and fruits like apples, bananas, and berries.
LEAN PROTEINS
Similarly, proteins provide sustained energy. To deter drowsiness, opt for lean proteins, such as fish, poultry, eggs, legumes, nuts and seeds, and plain yogurt.
Avoid the Afternoon Slump
If you find yourself feeling sluggish in the middle of the day, these may be the culprit:
SIMPLE CARBOHYDRATES AND SUGARS
Foods high in simple carbs and sugars – such as white bread, pasta, and products with added sugars – are quickly broken down by the body, leading to a spike in blood sugar levels followed by a plummet that saps energy.
CAFFEINE
While caffeine is commonly reached for to curb fatigue, consuming too much can actually make
you more fatigued and disrupt sleep. The Food & Drug Administration recommends limiting caffeine intake to below 400 milligrams a day – the equivalent of two to three 12-ounce cups of coffee.
Practice Portion Control
After a large meal, it’s common to experience a “food coma,” or a state of intense lethargy. This is because the body is busy using energy to digest. Eating smaller portions throughout the day and incorporating energizing snacks can help prevent a post-meal crash.
Don’t Forget to Hydrate
In addition to eating energizing foods, it’s essential to stay hydrated. Studies show that even mild dehydration can lower energy levels and hinder the brain’s ability to concentrate. Drink fluids throughout the day, and try incorporating fruits and veggies with high water content into your diet, such as melons, strawberries, cucumbers, and tomatoes.
Sleep, stress, and lifestyle also play an important role in energy levels. To help you feel your best, combine a balanced diet with regular exercise and seven to nine hours of sleep every night.

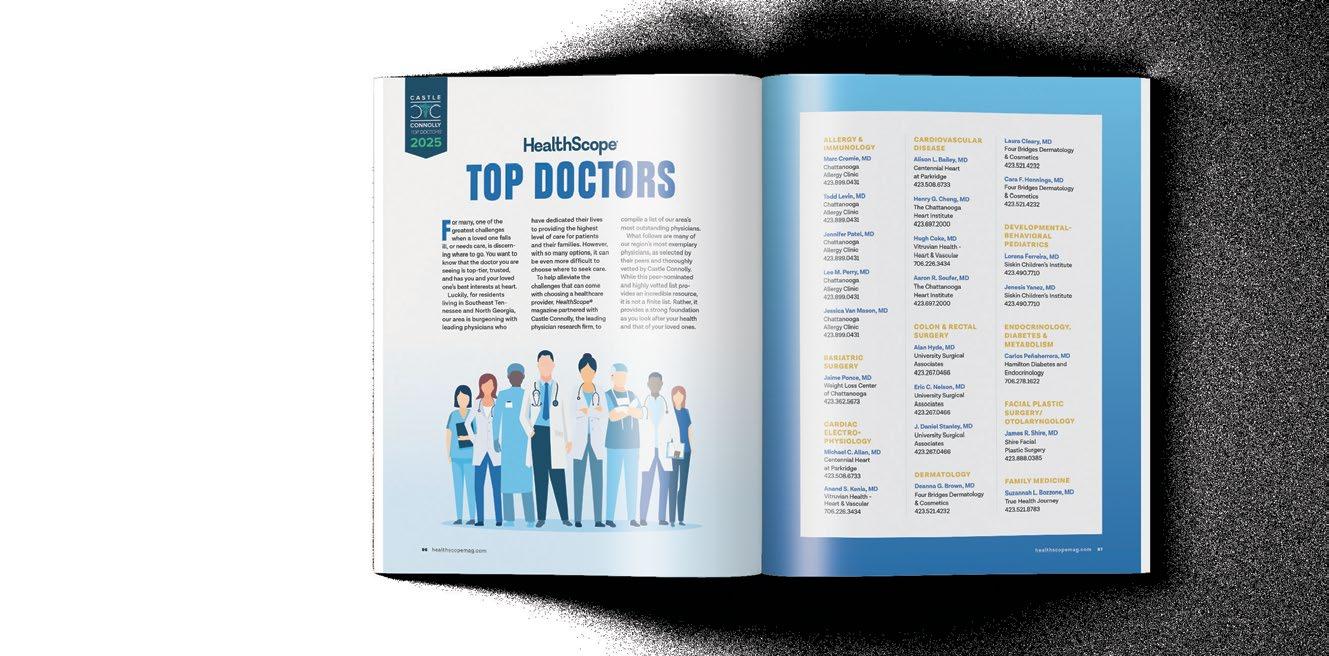





Breakfast
On the Go
Thisone’s for the busy parent, the commuter trying to beat the traffic, and the serial snoozer who wanted 10 more minutes in bed. We’ve all been there – rushing out the door with coffee in one hand, keys in the other, and no time for a proper meal. If your mornings feel like a mad dash, it may be time to rethink your breakfast routine. With a little prep the night before, you can say goodbye to morning chaos and hello to breakfast that moves with you. Set your day up for success with these quick, easy, and healthy on-the-go breakfasts!
“For this nutrient-rich, on-the-go breakfast smoothie, avocado is the key ingredient for the proper texture. It may seem odd to add to a smoothie, but don’t worry – you can’t taste it at all! My kids love the avocado, and I make this smoothie for them (without the AG1 powder) and replace the milk with chocolate milk. I often substitute bananas with whatever fruit I have on hand. If desired, add protein powder or another supplement of choice, and you’re ready for the day!”
– Kirby Yost


Kirby Yost’s Glow Getter Smoothie
SERVES 1
Ingredients
• 8 oz. milk of choice or water (I use 4 oz. heavy cream and 4 oz. water)
• Handful of ice
• 1/2 large banana
• 1/2 ripe avocado
• 1 Tbsp. organic, all-natural, sugar-free peanut butter
• 1 scoop AG1 Next Gen powder
• 1 scoop ARMRA Colostrum powder
Directions
Add all ingredients to a blender, and blend until smooth and creamy. Pour into a to-go cup and head out the door!

Mean Mug’s Savory Keto Egg Bites
SERVES 6
Ingredients
• 1 cup cooked bacon, chopped
• 10 eggs
• 1 cup heavy cream
• 1 tsp. dried oregano leaves
• 1/2 tsp. pepper
• 1 cup shredded mozzarella or cheddar cheese
• 4 cups fresh spinach, chopped and sautéed
“These savory keto egg bites make it easy to stay both sa tiated and in ketosis. I love them because I always want breakfast, but I don’t want to load up on carbs and sugar. They are also easy to eat on the go and are per fectly seasoned, so you feel like you are being treated instead of feeling like you are dieting or sacrificing.”
– Matt Lewis, Mean Mug
Directions
Preheat conventional oven to 350° or gas convection oven to 275°. Add 0.5 ounces of bacon to each muffin cup or silicone muffin pan. Whisk the eggs, heavy cream, oregano, and pepper until combined. Fold in cheese and sautéed spinach to the egg mixture and stir until fully combined. Pour mixture into muffin cups evenly (each will likely be around ¾ full). Bake for 15-18 minutes until egg is puffed up like a muffin and slightly browned.

Charis Todd’s Simple & Effective Circuit
“I really enjoy this workout because it’s simple, efficient, and empowering. Each movement has purpose – you’re not just burning calories, you’re building real strength and functional fitness that carries over into everyday life. The variety keeps things engaging without being boring! The balance of lower and upper body exercises creates a satisfying full-body challenge that can be done in a short amount of time, which is perfect for a busy schedule. Plus, there’s something really motivating about feeling your glutes fire in a hip thrust or powering through a set of pushups. You’ll leave this workout feeling energized, capable, and proud of what your body can do.”
Charis Todd, Fire Fitness @firefitnesstn




Standing Single Arm Dumbbell Rows
Place one hand on a bench and form a stable stance with both feet on the floor. Pull your ribs down and brace your core. Allow your shoulder blade to move freely and your lat to fully stretch as you reach your arm down and forward slightly in an arc-like movement. From here, drive your elbow back and up toward your hip using your lat and upper back. Squeeze hard at the top then lower with control until you return to the fully stretched position. Aim to minimize momentum by avoiding swinging your torso or jolting the weight up. Fight against the rotational forces using your core. Exhale at the top of each rep and inhale as you lower. Repeat for three sets of eight to 12 reps.
Romanian Deadlifts (RDLs)
Hold a dumbbell in each hand in front of your thighs, palms facing you. With a soft bend in your knees, hinge at your hips while pushing them back as you lower the weights along your legs. Keep your back flat and core tight, pulling your ribs to your hips. Stop just below your knees as you feel a stretch in your hamstrings, then return to standing. Repeat for three sets of 10 to 12 reps.




Goblet Squats
Hold a dumbbell or kettlebell close to your chest. Stand with your feet shoulder-width apart. Inhale as you lower into a squat by pushing your hips back and pressing your knees out, and bend at your knees. Keep your chest up and back straight. Exhale as you drive through your heels to return to standing. Repeat for three sets of eight to 12 reps.


Push-Ups
Start in a plank position with hands slightly angled out and just wider than shoulder width apart. Pull your ribs and hips together as you lower your body until your chest touches the ground. Keep your core tight as you push back up, powering up through the palms of your hands to the starting position. Repeat for three sets of five to 10 reps.


Hip Thrusts
Sit on the ground with your upper back against a bench. Roll a barbell or place a dumbbell across your hips. Bend your knees with your feet flat on the floor. Drive through your heels to lift your hips until your body forms a straight line from shoulders to knees. Squeeze your glutes at the top, then lower down. Repeat for three sets of 12 to 15 reps.

When a Jet Ski accident left 13-year-old Jada Defoor with a compressed spinal cord, her life changed in an instant. The severity of her injury led to emergency spinal fusion surgery, but her journey was far from over. After three years of struggling and a second extensive surgery, Jada was admitted to Siskin Hospital. With compassionate, personalized care and a trusted therapy team by her side, she found more than just healing – she found hope. Her gait improved, her con dence grew, and with continued support from Siskin Outpatient Therapy, Jada made incredible progress. Now a recent high school graduate, Jada is preparing for her next great adventure: working in the mission eld. Having experienced rsthand the di erence hope can make, she is thrilled to share it with others.


Leading the way in vascular care.






At CHI Memorial, we offer complete vascular care, from diagnosis to treatment, all in one place. Our vascular specialists use the latest treatments for conditions like aortic aneurysm, carotid disease, dialysis care, DVT, peripheral artery disease and varicose veins. Trust our team to put your health first every step of the way.
To learn more, visit memorial.org or scan the QR code below.