

2025

CARING FOR THE WHOLE CHILD Child Life and Integrative Care Services
Kids Rediscover the Magic of Childhood at Summer Camp
Introducing Our Podcast:
“The Lead in Peds”
The wonderful experience in the hospital has left a lasting impression on us.”



2025

Kids Rediscover the Magic of Childhood at Summer Camp
Introducing Our Podcast:
“The Lead in Peds”
The wonderful experience in the hospital has left a lasting impression on us.”

AtOur responsibility to our patients extends far beyond the walls of our hospital and clinic locations.”
― Michelle Riley-Brown
Children’s National Hospital, caring for children means much more than medicine. A certified Child Life specialist may soothe a patient’s anxiety before surgery. A care coordinator may organize a family’s transportation or confirm that they receive the right prescription from the pharmacy. The medical director of our summer camp may phone a loved one with an update about their child’s first sleepaway experience.
Responsibility to our patients extends far beyond the walls of our hospital and clinic locations. Our commitment to kids’ wellbeing as whole children — and to the broader community — shines through all we do. In this issue of Believe, we give you a closer look at how Children’s National brings this commitment to life.
Our cover story highlights the incredible Child Life and Integrative Care Services team (p. 6). They bring comfort and understanding to procedures and hospital stays, embodying the art of healing by providing sciencebacked interventions.
With summer upon us, I encourage you to learn about our partnership with Melwood, a leading advocacy and service provider for people with disabilities and their caregivers (p. 16). Since 2024, we have worked together
to offer Camp Accomplish, where children with medical needs experience the joy, discovery and independence that make summer camp a memorable learning opportunity.
In this issue, we also recognize several talented staff who make our work possible (p. 24), including Pedro Flores Canales, a coordinator in our Cleft and Craniofacial Program. “I try not to see a child as just a patient but as my own kid or the kid down the block,” Flores Canales says about the connections he builds with families. The passion he incorporates into each appointment is an example of what makes care at Children’s National extraordinary.
We hope you enjoy this glimpse into our efforts to bring together expert care, compassion and community so that young patients and their families can thrive.
All my best,
Michelle Riley-Brown, MHA, FACHE President & Chief Executive Officer Children’s National Hospital

Our programs offer opportunities for growth, expression and healing that complement traditional treatments. These interventions bring understanding, comfort and laughter and are life-changing.”
― BobbiJo Pansier, Director, Child Life and Integrative Care Services

EDITORIAL
Jean Bratman
Georganne Coco
Kitson Jazynka
Jennifer Morrison
Katherine Shrader
Margetta Thomas
Dan Wilcock
Maura Zehr
PRODUCTION AND DESIGN
Christina Aycock
Alex Bozoghlian
Jen Littrell
Rachel Phillips
Allison Chess Ruiz
CONTRIBUTORS
Ali Chope
Meagan Davis
Lauren Scheinert
Leslie Schrader
Morgan Worley
COVER STORY PHOTOGRAPHY
Tracey Brown
Children’s National Hospital Foundation works with generous donors to advance the hospital’s mission. Gifts from individuals, corporations, foundations and community organizations fund world-class care and research for kids in the Washington, D.C., region and beyond.

For Believe magazine’s digital experience please visit childrensnational.org/ believe or scan the QR code
ONLINE childrensnational.org/giving FACEBOOK.COM/childrens.national INSTAGRAM.COM/childrensnational LINKEDIN.COM/company/ childrens-hospital-foundation
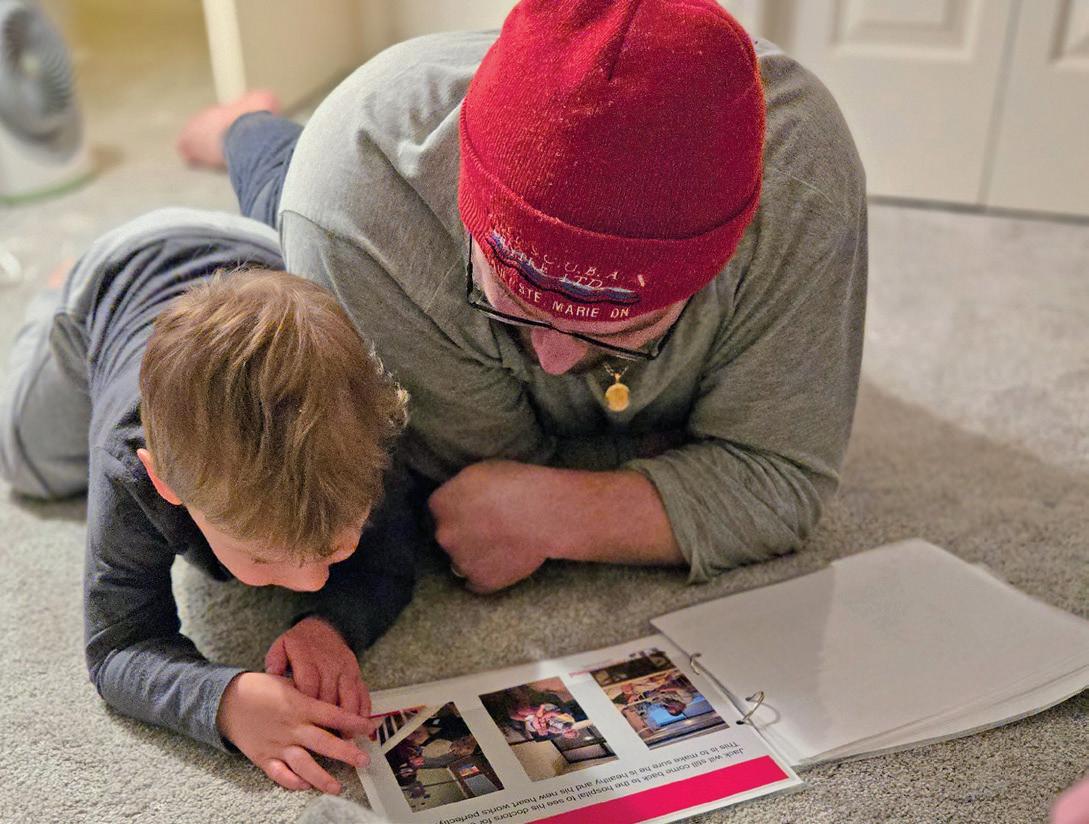
Cover: Jack and Lanie, Child Life
Specialist
Child Life and Integrative Care Services
Families who navigate illness and injury need more than medical treatment to heal. Our Child Life and Integrative Care Services team provides comfort, support and therapeutic interventions for patients and families throughout their journey.


Children with chronic medical conditions and disabilities find joy, confidence and meaningful connections at Camp Accomplish, our new collaboration with Melwood.
Providing exceptional healthcare is everyone’s role at Children’s National. Meet some staff members who go above and beyond to help kids feel better.



Caring for the Senses to Support Children’s Development
Diego Preciado, MD, PhD, chief of Otolaryngology, is an innovator. He is raising the bar for ear, nose and throat care and better outcomes for patients.
Investing in Breakthroughs: An Urgent Need to Support Pediatric Science
The Children’s National Research Institute has more than 2,000 active investigations underway to transform pediatric health. Why critical advances are at risk.
Owen’s Boundless Gratitude
Owen received lifesaving care for a rare form of epilepsy. He and his family find many ways to say thank you, including twice-a-year delivery of lunch and hugs to hospital staff.



The people at Children’s National saved our son’s life, and he is still in ongoing care. We hope to inspire staff to keep fighting hard for all the kids in their care.”
― Karen, Owen’s Mom
36 A Historic Visit
The president of the United Arab Emirates brings joy to patients at Children’s National.
37 Breakthrough Device
Garners Support
Scientists are on a quest to measure and better understand pain through patients’ eyes.
Ramadan Gathering
Muslim families came together at Children’s National for Iftar, an evening meal in observance of the holy month of Ramadan.
38 Children’s Ball
Our annual gala celebrated a bright path forward, raising more than $3.2 million for pediatric care and research at Children’s National.
39 A Day of Victories
Patient Landon takes the field at a Washington Commanders game to celebrate being cancer-free.
40 Introducing Our Podcast: “The Lead in Peds”
Our chief academic officer and director of the Children’s National Research Institute interviews hospital leaders who are transforming healthcare.
41 Experience Ambassadors
Two new faces offer comfort and connection to families in our Emergency Department.
42 A Patient’s Perspective
Twelve-year-old Sumukh shares the special things that helped him complete his leukemia treatments.

I magine a kaleidoscope of play, education and creative therapies that engage patients and their families to promote healing and decrease pain, fear, trauma and grief. These programs, backed by science, create nurturing environments and experiences that reduce the need for pain medication, shorten hospital stays and improve health outcomes. They allow us to care for the whole child — body, mind and spirit.
“Our dedicated Child Life and Integrative Care Services team plays a critical role in supporting families through their medical journeys,” says Director BobbiJo Pansier, MPH, CCLS, CTRS. “Our programs offer opportunities for growth, expression and healing that complement traditional treatments. These interventions bring understanding, comfort and laughter and are life-changing.”
“I see the impact of this care every day,” says Pansier. “Not long ago, a patient who had spent her entire life at Children’s National graduated to another facility. She had never been in a vehicle or experienced the world outside our main campus. Multiple teams came together to ensure her transition would be free of trauma. Her medical care providers, along with a music therapist and Child Life specialists, assisted the transport team. Our team made introductions to staff at the new facility. The patient waved goodbye with a smile.”

Child Life and Integrative Care Services at Children’s National, critical to caring for patients, are nonreimbursable by insurance and rely on philanthropic support.


Nine-month-old Jack, awaiting a heart transplant, was in too much pain to sleep. His heart condition had caused serious, painful gastrointestinal problems. His mom, Rachel, had been up all night trying to soothe him.
Lanie Berk, MS, CCLS, a certified Child Life specialist, offered a familiar, friendly face. She held Jack close. She sang to him and read his favorite books.
“There are so many negative touch experiences in a hospital — needles, countless procedures and tubes hooked up to a child,” says Berk. “It’s so important to give positive stimuli in the form of touch that nurtures and heals.”
Jack fell asleep in Berk’s arms, giving Rachel a much-needed break. “It’s a privilege to be part of their story,” says Berk, who Rachel reports is pretty much her son’s favorite person in the hospital. “For a mom to trust me to hold her baby so she can leave for a little while is a huge honor.”

Jack was in heart failure when he arrived at Children’s National by emergency helicopter transport in February 2024. He was 4 months old. Our cardiologists diagnosed him with dilated cardiomyopathy, a condition that causes the heart’s chambers to thin, stretch and weaken. On Valentine’s Day, Jack’s family learned he would need a heart transplant to survive. “We were shocked and overwhelmed,” Rachel says. She and her husband Brandon began alternating care for their baby in the hospital and their 2-year-old son Nolan at home.
In April, surgeons installed a ventricular assist device to help Jack’s body pump blood while he waited for an
The wonderful experience in the hospital has left a lasting impression on us. Rachel and I are truly thankful for everything the Child Life team has done for Jack and us throughout this journey.”
― Brandon, Jack’s Dad
organ donor. But there were complications. His stomach swelled, and he had two strokes. “We quickly learned that Children’s National is an exceptional place with exceptional people,” Rachel says. “There were moments when we fully wanted to panic. Instead, we learned to breathe deeply and trust the care and our team.”
That trust and human connection, along with clear, thorough communication, helped make the hard times easier, Rachel says. Throughout the family’s long stay in the hospital, they received healing support from members of our Child Life and Integrative Care Services team.
Berk kept the mood light during Jack’s medical procedures — for instance, his first round of vaccines. That day, she played music, sang and danced to keep him smiling. Knowing that socializing could help Jack’s parents feel more comfortable and at home, Berk started a monthly dinner tradition in the Cardiac Intensive Care Unit (ICU) waiting room to help families connect.
She also helped Jack’s parents explain the situation to his brother, Nolan. She created books for Rachel and Brandon to read with him at home. The first one explained Jack’s illness and why he needed a new heart. The second prepared Nolan for a trip to the hospital after his brother’s transplant and included details about the devices supporting Jack and his scar. These books helped Nolan understand and feel a part of the journey.
“This experience makes you feel isolated in so many ways,” Rachel says. The Panda Cares Center of Hope, our Family Resource Center, provided a place for her to relax and connect with parents facing similar challenges. “Reading was the perfect way to distract myself while Jack was sleeping or having a procedure.”
Rachel inspired Berk and Allie Slocum, our patient family library and resource center coordinator, to start a monthly caregiver reading group for Cardiac ICU families. “The group has three important functions,” Berk says. “It encourages parents to be involved with their child’s care, enables them to meet each other, and it helps families connect with their babies through reading, which is great for a baby’s development.”

It’s comforting to know you’re not alone and there are others who understand what you’re going through and will listen and offer guidance.”
― Brandon, Jack’s Dad

Jack’s parents enjoyed a parent support group with art therapist Katherine Pedrick. Brandon made paper cherry blossom branches, and Rachel made a vase. They painted comfort boxes filled with words of encouragement. Art therapy gave them an outlet within the hospital and helped them connect with other families in the Cardiac ICU. “It’s comforting to know you’re not alone and there are others who understand what you’re going through and will listen and offer guidance,” Brandon says.
Children’s National volunteers read to baby Jack on a regular basis. “One particular volunteer came often and really connected with him,” Rachel says. “By the end of her visits, he would be asleep in her arms. The volunteer visits allowed me to take a walk or get something to eat. It meant a lot.” Other volunteers visited Jack to play with developmentally appropriate toys and games.
Rachel enjoyed events at Seacrest Studios, especially inperson appearances by American singer-songwriters Andy Grammer and Phillip Phillips.
The Bunny Mellon Healing Garden served as an oasis Jack’s parents visited often, including with Jack, to breathe fresh air, read, walk and enjoy a change of scenery. “Sunlight can do wonders,” Brandon says. “On the night before Jack’s heart transplant, we sat outside enjoying a perfect summer night underneath a star-filled sky. It was calm and peaceful and just what we needed.”



Rachel says her son always had a great smile; but at the start of his hospitalization, it was subtle, and sometimes he could lift only one cheek. One week post-transplant, Jack’s smile was even. Now, his mom reports that he has a roaring belly laugh. This summer, he is working to sit up and enjoys stroller rides.
“Our team at the hospital taught me to be a little more spontaneous and celebrate the good moments,” Rachel says. “I’m more likely to go outside and play with the boys now, even if there are chores to do. I’m more about thriving in the moment. Children’s National gave Jack the ability to live a life. We’re here to enjoy every minute of it.”
Jack received his new heart when he was 11 months old. He went home a few months after the transplant, just before Christmas.
are highly trained experts in child development who use play as a therapeutic tool with patients to ease the stress of being in the hospital. They advocate for kids, educate and support families, manage crises and provide bereavement support. These experts also conduct research to better understand and improve this kind of care.
Care for 26,000+ patients and families annually
Impact: Less use of sedation and pain medication
Art Therapy
800+ interactions annually
is a mental health intervention that improves cognitive function, fosters self-esteem and cultivates emotional resilience. Sculpting with clay, painting, sketching and tie-dyeing T-shirts allows patients and families to express their thoughts, de-stress and share experiences to process emotions.
· Calms patient heart rates
· Lowers the need for pain medication
· Helps get kids home faster
Music Therapy improves mental and physical outcomes. A therapist may use interventions such as playing the piano to soothe a distressed psychiatric patient, strumming a guitar to help a burn patient endure painful dressing changes or offering a rhythmic tune that helps regulate a baby’s heartbeat.
30+ galleries at 10 hospital locations
Art Galleries support well-being by contributing to a healing environment. Paintings, murals, photography and other creative works foster a sense of connection that transcends language and cultural barriers and decreases stress and anxiety.

9,400+ sessions and 600+ hours of goal-directed therapies by facility dogs annually
provides comfort and joy. The program includes four facility dogs: Company, Hampton, Tux and Montana and about 20 volunteer pet therapy teams. Facility dogs support patients during medical procedures, including IV placements, blood draws and scans.
50+ performances for 2,000+ children and families annually
soothe and entertain. We invite talent from our community to the hospital’s main atrium, the bedside and specific pediatric units. Partners include the National Symphony Orchestra, John F. Kennedy Center for the Performing Arts, Musicians on Call and local schools and theaters.

Philanthropy helps Children’s National provide vital Child Life care to more families. We have one Child Life specialist for every 148 patients. Many peer children’s hospital have more: an average of one per 15 patients.

manages hundreds of individuals in roles such as soothing newborns, passing out water bottles and activity books in the Emergency Department waiting room, crafting with patients in their rooms and academic tutoring.
8,000+
volunteer hours at the hospital annually
1,200+ families served annually
The Panda Cares Center of Hope provides a place to relax, read, connect with others; and engage in fun events, such as book fairs and yoga classes.
1,500+ visitors to the center annually
2,500+ books gifted annually
275+ visitors to the center annually

provide nonclinical therapeutic, diversionary and meaningful programming — and a bit of normalcy and laughter. They may host a birthday party for a child who has been in the hospital for months. Events often take place in the Bunny Mellon Healing Garden and Lavinia Lemon Pitzer Garden Room.
285,000+ individuals hosted annually
emphasizes the transformative power of creativity and community through radio, television and news media. Kids participate in VIP interviews, play games, deejay and create shows. The studio broadcasts to hospital rooms so that all patients can participate.
~20
celebrity visits and 50 patient-created shows annually
246,000
child and family encounters annually



By Lanie Berk, MS, Certified Child Life Specialist
In the Cardiac ICU at Children’s National, every family teaches me something. Jack’s mom, Rachel, taught me about the power of finding something positive to focus on, even on the hardest days. She and Brandon found at least one thing to feel good about each day ― be it a small improvement for Jack or what they did to take care of themselves.

When I first met Jack, he had the best smile I’d ever seen. A huge team focused on his care. I helped to manage his pain and things like making sure he got the rest he needed. I decorated his room to make it cheerful. But my primary focus was on Jack’s family and helping get them through this very difficult time.
I have always loved helping others. When I was 15, my best friend since kindergarten had a complex illness and a lot of hospital stays. Seeing her struggle and become completely dependent on other people and machines made me feel helpless. I thought a lot about what I could do to make her life better. I spent time with her in the hospital. We chatted, looked at magazines and made bracelets to pass the time — anything to help make her feel normal.
Later, as an adult, she told me what a big difference it made in helping her get through those hard times. In college, when I came across the Child Life specialist career path, memories of those times with my friend flooded back. I suddenly knew what I wanted to do with my education and my life. In the Cardiac ICU and all over the hospital, this kind of support truly helps families heal.
Generous philanthropy during the last decade from Gerard Martin, MD, FAAP, FACC, FAHA, and his wife Roberta Martin, and from other donors made psychosocial support from a dedicated certified Child Life specialist in our Cardiac ICU possible. Berk has been in this role since 2023.

Jumping into the pool on a hot day. Canoeing on a clear lake. Roasting marshmallows around the campfire. For many children, camp is the highlight of summer. They make new friends, create memories and build confidence. But too often, summer camp — especially overnight options — are out of reach for kids with chronic medical conditions and disabilities. At Camp Accomplish, every child has a chance to grow and have fun.

This summer, campers ages 5 to 18, with autism, cerebral palsy, congenital heart disease, epilepsy, hydrocephalus, neurofibromatosis, sickle cell anemia, spina bifida, Type 1 diabetes and other conditions will enjoy inclusive experiences tailored to their abilities. Activities include swimming, horseback riding, creative and performing arts, sports, climbing walls, horticulture and science, technology, engineering and mathematics (STEM) projects. Kids can attend day camp or sleepaway camp.
In 2024, Children’s National launched a collaboration with Melwood — a leading area employer, advocate and provider for people with disabilities — to expand Camp Accomplish, located at Melwood Recreation Center in Charles County, Maryland. Melwood has operated the camp for more than 25 years.
Children’s National brings nearly three decades of experience offering summer camps for kids with chronic health conditions, including Brainy Camps. At Camp Accomplish, John Schreiber, MD, a neurologist, serves as medical director, and many additional hospital staff devote their time to helping kids find joy and make memories that will last a lifetime.


363 campers
101 campers attended multiple weeks
85% of campers had a disability or chronic health condition
23 counselors in training
73
Children’s National doctors, nurses, pharmacists and other medical staff
218 scholarships provided to all camper families who requested financial aid

Gerard B. Lambert Foundation President Thomas Lloyd, second from right, with staff at Camp Accomplish in 2024. The Lambert Foundation has supported Children’s National camps and other areas focused on mental health for several years. Thanks to their generosity, approximately 30 campers attended on a full scholarship last summer. The foundation’s gift also funded a portion of Children’s National camp staff salaries.


Growing up with a chronic health condition isn’t easy. When other kids your age are out having fun, you’re stuck at the doctor’s office or in the hospital. You get bullied too. You question your worth, and your selfconfidence takes a hit. I know this because I was that kid. I was born with sickle cell anemia.
I also know the life-changing power of camp. I have attended Brainy Camps of Children’s National and Camp Accomplish for nearly a decade. It’s where I developed leadership skills, and where I gained the confidence needed to pursue my dreams. This fall, I start my sophomore year at Stevenson University where I’m studying healthcare management. I’m going into this field because I want to continue what I started at Camp Accomplish and help people with chronic health conditions and disabilities live their best lives. Camp is where I learned that my sickle cell anemia doesn’t define me. Because of camp, I know my future is bright.


Before last year, I had never been to summer camp. I grew up in Guatemala and was born with spina bifida. It’s a birth defect that causes your spinal cord to not form correctly. I had to have five surgeries. We came to the United States for a better life and so I could get better care for my condition. A Children’s National nurse told me about Camp Super Bifida at Camp Accomplish.
I was nervous about going but made friends quickly and loved the activities,

especially archery, horseback riding and swimming. The other campers were fun to be around, and it was easy to talk to them because they grew up with similar struggles. Camp staff were very encouraging. Next year, I’d like to become a counselor in training so I can help younger kids. If I can be positive and give them the knowledge that they will be OK, it will give them hope for the future.
When you live with a chronic health condition, life can feel limiting and lonely. I know this because I have epilepsy. I started having seizures when I was 2. Today, I still have seizures. I had two brain surgeries to try and stop them and spent countless hours in medical settings and at doctor’s appointments. My activities are limited because we never know what’s going to trigger a seizure. School is challenging too. Other kids see someone who is different, and that means I get made fun of — a lot.
Camp Accomplish is the one place I can go where I know I’ll fit in. I don’t have to sit out while everyone else has fun. I can do things I wouldn’t normally get to do, like climb a ropes course, glide on a zipline and ride a horse.
When I have questions about my condition, I can talk with people at camp who share my experience. Now my goal is to become a counselor in training. I want to pay it forward and help younger campers with epilepsy and other chronic health conditions grow their confidence and know they’re not alone.



Hear, smell, taste. These senses impact and shape children’s everyday lives. Diego Preciado, MD, PhD, chief of Otolaryngology and Joseph E. Robert, Jr. Professor of Pediatric Otolaryngology, aims to set the gold standard for care of a child’s ear, nose and throat (ENT) — pathways to the senses. “We treat the senses that drive an individual’s personality,” he says. “ENT care has seen wonderful advances in the last 30 years, but there is still more work to do. That’s why I entered the field.”
Dr. Preciado is an innovator. His team, at the Sheikh Zayed Institute for Pediatric Surgical Innovation, helped to advance early detection and treatment of otolaryngology disorders, such as hearing loss, the most common sensory impairment in children. Four in every 1,000 infants are born with it.
In the laboratory, the team uncovered fundamental molecular aspects of chronic ear disease. This led to the development of new medications aimed at reducing the need for surgery. The team and collaborators are developing a drug delivery method, using liposomal nanoparticles — spherical vesicles
that are insoluble in water — to carry treatments directly into the ear canal. It could potentially eliminate the need for oral antibiotics and surgery in children with recurrent ear infections. The team also developed an app to guide patients through critical aspects of ENT care. It will help kids with hearing impairments in language development after cochlear implantation.
“At Children’s National,” says Dr. Preciado, “the future is all about helping children get better faster.”
Dr. Preciado’s team works across the hospital and with parent groups in our community to remove barriers to ENT care. “All care is not equal,” he says. “Sadly, families with public or no health insurance typically only receive care at a much later date. This delay often permanently impacts their children’s hearing, speech and social skills.”
Currently in development is a medical and educational intervention model for patients with complex ENT needs. It includes expanding critical wraparound services and creating new care solutions. The focus is precision medicine and personalized therapies. Continuing refinement of our fellowship program to train pediatric otolaryngologists is helping to build a strong workforce for the future.
“Real change can happen only by adopting a team approach to care. An effective leader must be an equal member of the team and lead by example. Children’s National is committed to this approach and ensuring that everyone receives expert care in the same manner.”

At Children’s National, the future is all about helping children get better faster.”
― Dr. Diego Preciado


By Jorgé, Sr. a Children’s National parent
My son Jorgé is a lovely 11-year-old kid. He has many friends and always helps other people. He loves to play basketball and American football. We live in Mexico, about four hours south of El Paso, Texas.
Last summer, Jorgé was visiting a friend’s ranch. The boys went out to explore a remote area on all-terrain vehicles. Jorgé didn’t see a wire fence and drove right into it. The wire caught his neck, and he landed on
the ground. Later, he told me he felt like the world had ended. He couldn’t breathe. His friend carried him back 3 miles on the other vehicle. The drive to the hospital was three hours. All we could do was pray. It was a miracle he held on.
Surgery to repair the serious injury to Jorgé’s neck and trachea saved his life. Months later, however, his life was not the same. Scar tissue in his airway made breathing difficult, and he couldn’t play or run up the stairs without sitting down to rest. Even though he survived the accident, for him, it was like he had lost his life. This was stressful for our whole family.
I researched the best doctors and found Dr. Preciado at Children’s National. During our first video conference, he really seemed to care
about helping Jorgé and invited us to come to Washington, D.C., for an endoscopy and maybe surgery. Jorgé was really scared. But everything about Dr. Preciado made my son feel comfortable, especially his explanations in perfect Spanish. Soon we scheduled a laryngotracheoplasty. This is a complicated upper airway reconstructive procedure for patients with severe airway obstruction.
Dr. Preciado and everyone at the hospital understood that we were far from home and going through a very tough time. We trusted them, and they took the best care of us. Now Jorgé is back to playing basketball and soccer with his friends. Dr. Preciado and his team gave him back a normal life. We will always be grateful.
Children’s National is blessed with an incredible team of pediatric intensivists, nurses, anesthesiologists, speech pathologists and hospitalists. All are essential for this kind of care. To see a child regain the ability to breathe normally without the need for a tracheotomy tube, and gain the trust of their family, is the greatest privilege imaginable.”
― Dr. Diego Preciado



At Children’s National, more than 8,000 dedicated employees provide patients with world-class care and make new discoveries in pediatric medicine. We are proud to introduce you to a few staff members who exemplify our commitment to improve the health and well-being of children and their families.



Children born with cleft lip, cleft palate and other craniofacial anomalies face a complex care journey that begins at birth and can span decades. Many patients undergo surgical treatment before their first birthday, and comprehensive care frequently requires an interdisciplinary approach of more than 11 different medical specialists. This can be overwhelming for families.

I consider myself a personal concierge to alleviate the stress of being a patient and navigating the hospital system.”
― Pedro Flores Canales
Program Coordinator Pedro Flores Canales helps them seamlessly navigate the process. From the moment a child becomes a patient at Children’s National, Flores Canales and Clinical Coordinator Elizabeth Benitez, PA-C, are there to help families understand their child’s needs and answer questions, arrange necessary clinic visits, coordinate surgical care and provide social support.
Flores Canales cares for families as though they are his neighbors. “I try not to view a child as just a patient but as my own kid or the kid down the block,” he says. “I scoot down and speak eye to eye. I consider myself a personal
concierge to alleviate the stress of being a patient and navigating the hospital system. It can be intimidating, especially for a family that speaks Spanish. They’re trying to understand signs, wondering where to go and what to expect. Families say it’s a relief that someone is here to speak with them.”
The daylong cleft clinic is where kids and families feel the extra effort Flores Canales puts into his work. This clinic is critical to integrated care, and it is common for patients to see many specialists in one location. “By the afternoon, I come in with my treasure box, little toys and decompression gadgets they like to play with,” he says. “This gets kids
excited. It also distracts them so that mom or dad can have a productive conversation with the specialist. It feels great to reward patients with a little gift that they’re anticipating after such a long day of medical care.”
This exemplary care coordination and access to specialty services improves patient outcomes and satisfaction. Generous support from the Johnston Family Endowment makes the program coordinator position possible.
“My goal is always to help patients have better days,” says Risi Idiokitas, DAOM, LAc
As a member of our PANDA Palliative Care team, she provides acupuncture, acupressure, massage and other Chinese medicine treatments to patients with serious and life-limiting illnesses. She works with children in several inpatient units, including Oncology. “Whether they have a headache, nausea or just a lot of anxiety, I’m there to help them feel better.”
She also treats patients in our Sickle Cell Integrative Care Clinic. “Acupuncture helps relieve pain in the moment for these children. I teach them selfacupressure and things that they can do at home; the clinic focuses on helping kids help themselves.”
Children in the hospital often face a barrage of procedures they can’t control. The choice to receive this kind of care is an opportunity to make up their own mind. Dr. Idiokitas explains to families that acupuncture heals using tiny needles that don’t hurt. “I’ll say, ‘The worst that can happen is nothing.’ Most are receptive. With treatment, the symptom we’re addressing often gets better, and there can be bonus benefits. For example, sleep may also improve.”
Recently, Dr. Idiokitas treated a patient for the first time for a headache. During the session, the girl and her mother spoke to each other in their native language. The mom appeared skeptical and would ask her daughter questions. Then her daughter would giggle and shrug her shoulders. When the treatment was over, the patient said she didn’t understand what had happened, but her headache was gone. Both she and her mom laughed and asked if Dr. Idiokitas could come back the following week.
Dr. Idiokitas says it’s rewarding to see how meaningful this therapy is for



Acupuncture
provides cumulative healing effects over time for children with chronic pain and other pain-related conditions. It is a safe, natural treatment that activates the body’s self-healing abilities.
patients. “It is such a private time in these families’ lives,” she says. “To be invited in, welcomed, then asked to come back or stay longer is an honor. To know that I have positively contributed to their quality of life, that’s huge.”
I teach them selfacupressure and things that they can do at home; the clinic focuses on helping kids help themselves.”
― Dr. Risi Idiokitas

Building lasting relationships with children and their families, especially those who come to receive treatment every two weeks, is so rewarding.”
― Jullie Rhee

Children with rare, neurogenetic conditions that affect the development and function of their nervous system see Jullie Rhee, MSN, CPNP-AC, throughout their healthcare journey. As nurse practitioner team lead in Neurology, she works across disciplines to deliver specialized care to these patients. All face shortened lifespans and hope for a cure.
“I work closely with many who are unable to speak or advocate for themselves,” says Rhee. “This is due to cognitive impairment or because their condition has progressed so far. Building lasting relationships with children and their families, especially those who come to receive treatment every two weeks, is so rewarding. I get to build
connections with these families and provide continuity of care. Frequent visits allow them to have their own specialized team with nurses and staff who know the child and how to handle specific aspects of their care — from the equipment they need to best positions for their procedures to ensure success.”
Rhee joined Children’s National 18 years ago as a Neonatal Intensive Care Unit (NICU) nurse. Today, in her leadership role, she supports advanced care providers in both clinical and research practice and leads a team of 10.
In our Leukodystrophy and Myelin Disorders Program, also known as the White Matter Clinic, Rhee ensures that every patient receives the care they need with the specialists within the program. She then coordinates after-visit care, helping with forms, letters and phone calls to pediatricians,
local providers, other care team members and schools.
In the operating room and radiology suite, she handles spinal taps to diagnose patients or administer medication for conditions like Spinal Muscular Atrophy. Kids with inherited metabolic disorders like NiemannPick disease and Dravet Syndrome are receiving a new treatment as part of a study in the rapidly evolving field of rare disease research.
“It is challenging work but really rewarding to see how far treatment has come during the last 10 years,” Rhee says. “Children who did not have the opportunity to receive or be considered for treatment can now access it. We might not be able to provide a cure for all, but being involved in this innovative research allows me to be a part of patients’ journeys, and that is special.”
Unfamiliar prescription names. Multiple appointments. Information overload. A family whose child has a sudden diabetes diagnosis often experiences confusion and fear.
Roxy Velasquez, a health coach in our Division of Endocrinology and Diabetes, offers kindness and ongoing support for families in this situation. She helps families cope and keeps patients’ diabetes care on track by serving as a bridge to our multidisciplinary care team.
“Imagine everything is OK one day and suddenly you’re facing a shocking diagnosis,” says Velasquez. “It completely changes a family’s life.” She provides bilingual support in Spanish and English to help families navigate insurance and manage appointments and occasionally transportation. She connects them with mental healthcare and social workers. Sometimes it’s a three-way phone call to a pharmacy to make sure a family gets the right medicine or enough insulin pens.
This support is especially important, says Velasquez, for families without cellphones or those who don’t speak English. Help to manage these details means fewer kids will get so sick that they need emergency care.
“When I speak to a mom or dad, I feel like maybe I’ve given them a little peace of mind,” she says. “It helps them to know they’re not alone. My job is all about making sure they’re OK.”
Velasquez’s position is supported entirely by philanthropy.


When I speak to a mom or dad, I feel like maybe I’ve given them a little peace of mind. It helps them to know they’re not alone. My job is all about making sure they’re OK.”
― Roxy Velasquez
MEET THE MOMENT
Scientists at the Children’s National Research Institute are pioneering breakthroughs to reshape how we care for children. Their work saves and transforms lives. Through collaboration and innovation, with cutting-edge technologies, they are pushing the boundaries of what’s possible in pediatric medicine.
Recent news headlines showcase their remarkable progress. A Children’s National team administered the first commercial gene therapy to a teenager with sickle cell disease, offering hope for a future free from the condition’s painful burden. Another research group is harnessing low-intensity focused ultrasound to treat children with brain tumors. It penetrates the blood-brain barrier, delivering therapies to the diseased cells and providing new options for families facing the unthinkable.
More than 2,000 active research projects are underway at Children’s National, with more than 70% of the funding coming from federal agencies. Critical advances are at risk. Announced funding cuts at the National Institutes of Health (NIH) and other federal grantmaking agencies threaten groundbreaking studies that could improve young lives.
“We are on the cusp of breakthroughs,” says Nathan Kuppermann, MD, MPH, executive vice president, chief academic officer and Fight for Children Distinguished Chair of Academic Medicine. “We must find new ways to support our scientists. We have so many advances within reach and with them, the opportunity to change entire lifetimes.”


Center for Cancer and Immunology Research
Fulfills the promise of cell and gene therapies
Center for Genetic Medicine Research
Advances precision health
Center for Neuroscience Research
Pioneers our understanding of the developing brain
Center for Prenatal, Neonatal & Maternal Health Research
Develops neuromonitoring technologies to target disease at its earliest stages
Center for Translational Research
Bridges the gap between laboratory discoveries and clinical care
Makes pediatric surgery more precise, less invasive and pain-free

The next frontiers in pediatric research will transform the future of children’s health. Personalized medicine is making treatments more precise and tailored to each child’s unique genetic and medical profile. Advances in artificial intelligence are enabling earlier and more accurate detection of life-threatening conditions. Precision cancer therapies are revolutionizing treatment by harnessing the immune system to target and destroy diseased cells. Novel gene therapies address disorders at the molecular level, offering lifelong cures without scars.
Children’s National Research Institute is home to more than 600 scientists and staff across six specialized centers. Many physicians divide their time between clinical work and investigations, ensuring that discoveries rapidly translate into real-world impact.
Our scientists are dedicated to advancing care locally and internationally, with research priorities that cover the spectrum of pediatric health. These include studies to develop neurological and acute care treatments to help children recover faster from traumatic injuries like concussions. Investigators also think globally about generational challenges, including climate change.
“We cannot afford to wait to respond to the health implications of a changing planet,” Dr. Kuppermann says. “We need new strategies to protect children from climate-related conditions, such as asthma, mental health issues and the impact of chemical exposures.”
More than 2,000 active research projects are underway at Children’s National, with more than 70% of the funding coming from federal agencies. Critical advances are at risk.
Children’s National relies on a variety of funding sources, including the federal government, private organizations and generous donors. This funding supports investigations and the experts behind them, including early-career scientists and established researchers who pursue groundbreaking studies.
Pediatric innovation has long been underfunded compared to adult research. Although children make up more than 20% of the U.S. population, pediatric studies receive just 10% of the NIH budget — the primary driver of funding in this field. A widening gap threatens critical discoveries.
“For decades, the federal government has supported everything from state-of-the-art labs to professionals who enroll patients in clinical trials. In this new climate, we must bolster our resources,” says Catherine Bollard, MD, MBChB, chief research officer and director of the Center for Cancer and Immunology Research and the Dr. Robert J. and Florence T. Bosworth Distinguished Professor of Cancer and Transplantation Biology Research. “Philanthropy allows us to turn today’s breakthroughs into tomorrow’s standard of care. With the right investments, science can change lives.”

By Ljubica Caldovic, PhD
Rare diseases cause physical and intellectual disabilities that can devastate the lives of children and their families. With nearly 10,000 rare diseases affecting 10% of the world’s population, these diseases aren’t as rare as they seem. Many have no cure. For 25 years, I have dedicated my career at Children’s National to finding answers through genetic medicine.
Why should we care about genetic medicine research? From a human perspective, it’s about the

desire to help others. From a scientific perspective, these investigations yield important data about rare diseases and also help us understand common health issues.
For example, my research into the urea cycle (how the body eliminates toxic ammonia) and how to protect children’s brains from ammonia toxicity has led to a better understanding of other conditions that cause liver damage and brain injury in children.
Genetic research leads to better interventions and treatments to improve and extend patients’ lives — faster and sooner. Our cells work like a large orchestra. Genes and gene products are instruments; some more
important genes are conductors. If a gene is out of sync or not performing its job well, the “music” doesn’t sound right.
It’s exhilarating when I’m the first to discover something or make an important connection in how genes work. No one else knows yet, and I have good news to share.

This drives my work to advance science, which helps our patients and families feel better.
Dr. Caldovic is interim director of the Center for Genetic Medicine Research.
MACK’S STORY
As a high school freshman, Mack was a standout running back, catching the attention of college football scouts. His coaches praised his “downfield vision”— the ability to push forward and get the ball across the goal line no matter what. This determination would soon help him fight for his life off the field.
At 15, Mack had a bout of mononucleosis that triggered a severe systemic inflammatory syndrome called hemophagocytic lymphohistiocytosis, a rare and often fatal immunodeficiency disorder. It is more common in babies and toddlers than teens. At first, Mack had a fever and fatigue. Soon, he couldn’t get out of bed or eat or drink independently. “I felt lifeless,” Mack says. He later learned this was when his organs had started to fail.
Care providers at a local hospital called the immunology team at Children’s National, where experts diagnosed and treated Mack with a bone marrow transplant. He spent two months recovering at the hospital.
After his transplant, Mack joined a clinical trial at our Center for Cancer and Immunology Research (CCIR) to treat persistent Epstein-Barr virus infection. CCIR investigators pioneered a process for producing and banking healthy T cells to treat severe viral infections after bone marrow transplants. They boost the immune system’s recovery. A single dose of this virusspecific T-cell therapy resolved Mack’s infection.
“Everyone at Children’s National did an incredible job of blending top-notch clinical care with very human care,” says Mack’s

dad, Ben. “Mack was always ready to fight to get to the goal line. He never let the pokes, prods and bone marrow biopsies drilled into his pelvis get in the way. Mack is living proof of the power of research. He wouldn’t be alive if it weren’t for research and immunotherapies at Children’s National.”
Now 20, Mack still loves football. His time at Children’s National inspired a new goal: a nursing degree. He hopes to help others overcome medical challenges with the same skill, kindness and humor that his care team gave to him. In a recent physiology class, Mack was the only student familiar with immunoglobulins, or antibodies.
“After everything I’ve been through,” Mack says. “I could relate.”


Mack is living proof of the power of research. He wouldn’t be alive if it weren’t for research and immunotherapies at Children’s National.”
―Ben, Mack’s Dad

GIVE BACK YOUR OWN WAY
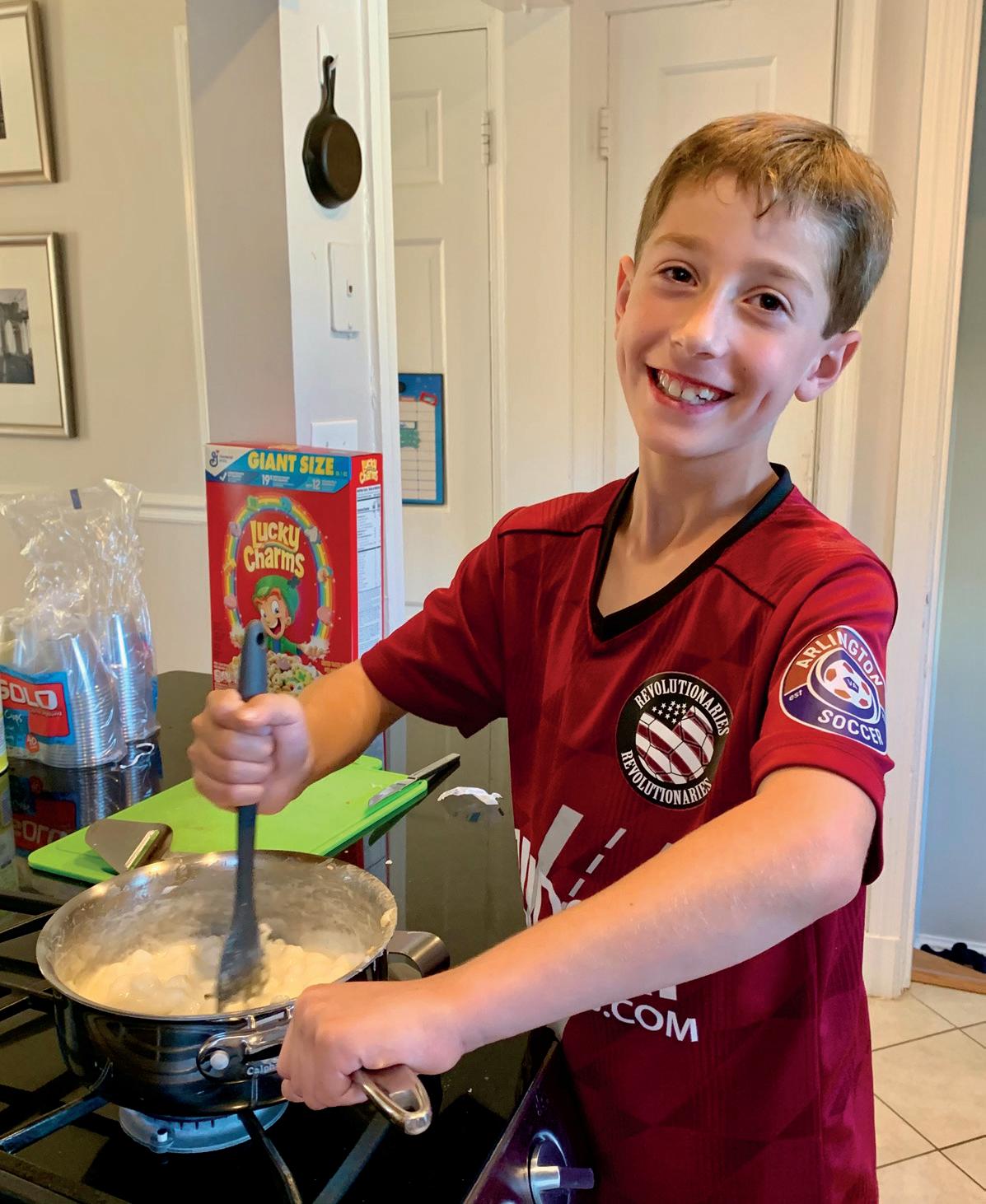
Owen, 9, loves playing soccer, practicing photography and eating pepperoni pizza. He’s also passionate about caring for others. His dad, Craig, says if someone falls on the playing field, Owen is often the first to offer a hand. Twice a year, his family delivers stacks of their
favorite pizza and submarine sandwiches as a gift to staff at Children’s National. “I get lots of hugs when we go,” Owen says. “Everybody is happy to see me and asks what I’ve been up to.”
The lunch deliveries started as a way for Owen’s family to thank staff who cared for him when he was younger and to boost morale. “Staff in the Pediatric Intensive Care Unit (PICU) don’t get a lot of repeat patient visits to see the improvement of a child after hospitalization,” says Owen’s mom, Karen. “We wanted them to see how well he is doing and celebrate what ‘good’ looks like.”
For Owen, the food donations are a way to share his appreciation for something very important to him: how hard care providers work to get kids home. “I know how it feels to be stuck in the hospital,” he says. “I want kids to get back home to their families as fast as possible.”
At age 5, Owen spent more than 100 days at Children’s National, after Elizabeth Wells, MD, senior vice president of Neuroscience and Behavioral
Medicine Center diagnosed him with a rare and sometimes fatal form of epilepsy called Febrile Infection-Related Epilepsy Syndrome (FIRES). He had hundreds of seizures and was in a medically induced coma for more than a month. He spent time in our PICU and recovered in the Neurology acute care unit.
Owen and his family support the hospital in two additional ways. They participate in neighborhood bake sales throughout the year, along with a robust group of their cousins, aunts, uncles, friends, neighbors, classmates, and even Owen’s school principal and teachers. One 2023 bake sale in Arlington, Virginia, raised $3,000 in a single day. Customers bought homemade cookies, brownies and sticky marshmallow cereal bars that Owen and his friends made. “He loves to work as the cashier and his little brother, Ethan, works the crowd,” says Karen.
At bake sales, Owen also asks customers to sign up to support his family’s enthusiastic fundraising effort, as a team named Fighting FIRES With Owen, for our annual Race for Every Child. Karen was Race co-chair in 2024 and will serve again in 2025. In all, the family has raised nearly $250,000 for the hospital for research related to neuroinflammatory diseases. “The people at Children’s National saved our son’s life, and he is still in ongoing care,” Karen says. “We hope to inspire staff to keep fighting hard for all the kids in their care.”


His Highness Sheikh Mohamed bin Zayed Al Nahyan became the first president of the United Arab Emirates (UAE) to visit America since his nation’s founding in 1971. His visit last fall included a stop at Children’s National.
Emirati patients and families welcomed His Highness. “I felt an immense, indescribable happiness,” said Ali, 15, a neurology patient. “His smile is like medicine for me.” More than 100 patients come from the UAE to Children’s National every year for care.
His Highness toured the Board of Visitors Telehealth Command Center, where technologies such as artificial intellligence allow continuous monitoring of heart patients. It enables consultations between doctors around the world. His Highness also learned about innovations at the Sheikh Zayed Institute for Pediatric Surgical Innovation — created through the UAE’s support 15 years ago.
Following the visit, the UAE announced a $35 million donation to Children’s National. This gift will advance breakthroughs in research and care. Focus areas include prenatal, neonatal and maternal health.




One of the biggest challenges in children’s health is measuring pain. Doctors rely on imperfect techniques, such as the pain scale, with its range of smiling to crying faces.
Children’s National researchers aim to improve on this method. They are developing a new device, the AlgometRx Nociometer that is designed to precisely measure pain. It promises to transform care for patients everywhere. In October, the Advanced Research Projects Agency for Health bolstered this work with a two-year $8 million grant award through its Sprint for Women’s Health program.
Julia Finkel, MD, a pediatric anesthesiologist and investigator at our Sheikh Zayed Institute for Pediatric Surgical Innovation, invented the device and leads its development. The portable, noninvasive Nociometer analyzes pupil dilation. Within one minute, it can quantify how the nervous system is processing painful stimuli. This data will allow care providers, in nearly any medical setting, to manage pain better with appropriate medications.
Dr. Finkel will conduct the research sprint during the next two years alongside colleagues from Johns Hopkins University and Medstar Research Institute. “As physicians, we often feel helpless to understand how our patients experience pain and whether treatments are working,” Dr. Finkel says. “The Nociometer will change that.”

Muslim families of Children’s National patients experienced a taste of home at the hospital this spring. They celebrated Ramadan by breaking the fast together, with a traditional evening meal, or Iftar. Ramadan, a holy month of reflection, faith and fasting from dawn to sunset, can be a difficult time for families to be apart.
The Iftar on March 20 brought together families from around the world and featured prayers and traditional Middle Eastern food. Children enjoyed superhero sightings, henna art and face painting. Hospital leaders and UAE Embassy partners joined them in the Geico Cares Atrium of the Sheikh Zayed Campus for Advanced Pediatric Medicine.
“This dinner was a beautiful opportunity to meet new people and share a meal,” says Safiya Ibrahim Alzaabi, a patient’s mother. “It brought back so many memories of home. It truly filled my heart to feel that sense of community again.”
This is the third year that the UAE Embassy sponsored the event.


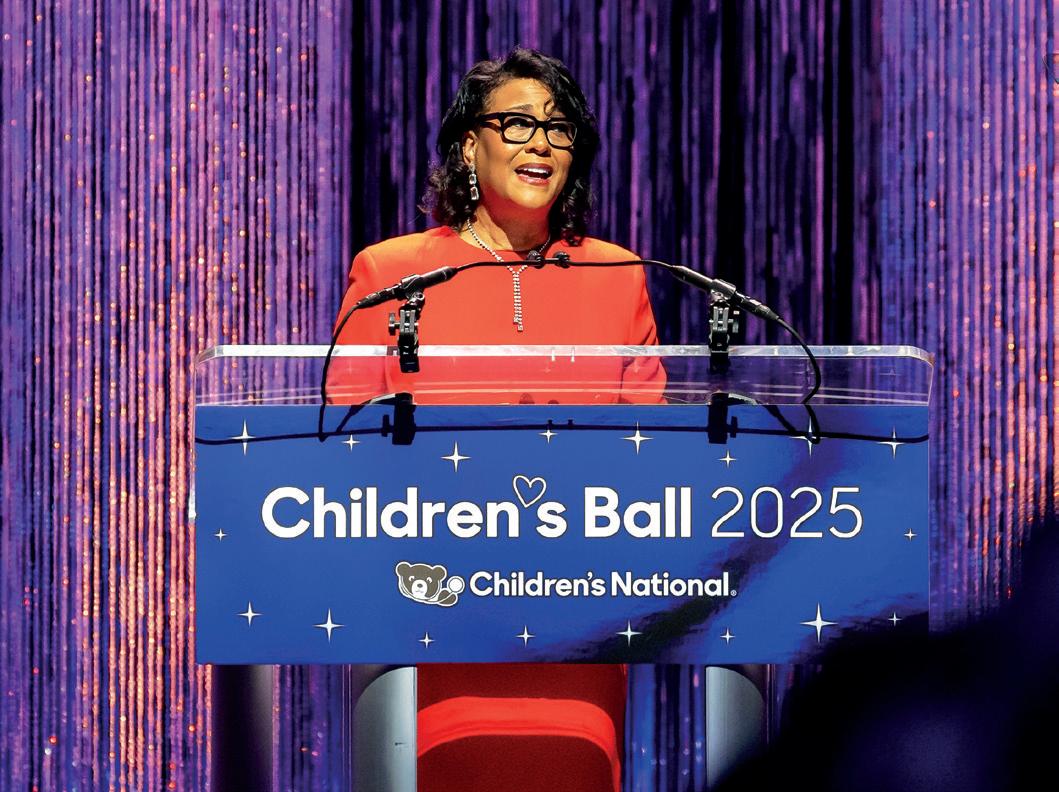
Two patients were the stars of our Children’s Ball on April 26, 2025. Max welcomed 750 guests at The Anthem with an electric smile and guitar work that struck the perfect chord. “I came to Children’s National for cerebral palsy treatment and knew right away that I was in the best place. I’m beyond grateful for the kindness of every person on my care team,” Max said.
Two years ago, Raci, now 7, endured a horrific car crash and required six surgeries. Her mother,



Tia, spoke about Raci’s remarkable path to recovery. “Doctors surrounded us. They said, ‘Kiss your child. We’re about to try to save her life.’ Those words will stick with me forever.”
Children’s National President and CEO Michelle Riley-Brown, MHA, FACHE, shared her vision for the future and noted how she met Raci soon after joining the hospital. “I feel an enduring connection to her,” she said.
The gala raised more than $3.2 million for the Fund for Every Child. Proceeds will support urgent pediatric priorities and expand access to care. Jon and Allison Kling joined Mara Glaser McCahan and Daniel McCahan as Children’s Ball Co-Chairs. Both couples, who generously support the hospital, shared how their sons survived and thrived after cancer diagnoses.
I’m beyond grateful for the kindness of every person on my care team.”
The Gerard B. Lambert Foundation received the Joseph E. Robert, Jr., Prize in Philanthropy. Lambert Foundation President and Hospital Foundation Board member Thomas Lloyd accepted the prize.
The foundation supports care for mental health and ADHD, and our summer camps. It also helped make the Bunny Mellon Healing Garden possible.


A dream came true for Landon on a clear bluesky Sunday in October. Wearing a Washington Commanders jersey, he stepped forward surrounded by cheerleaders in a packed stadium of football fans. He pumped his arms to excite the crowd, then grabbed the rope dangling from a giant golden bell. He rang the bell vigorously. “Let’s go!” he screamed to overwhelming applause.
750 guests attended the Children’s Ball, raising more than $3.2 million for pediatric health.

Landon rang the bell to signify the completion of his cancer treatment. When he was 11, continuous pain led him to multiple doctors and eventually an MRI that revealed abnormal cells and a bone lesion. A biopsy confirmed stage 4 non-Hodgkin lymphoma.
It took six rounds of chemotherapy at Children’s National, and in May 2024, Landon’s doctors told him his treatment was a success. Today, at age 13, he looks forward to 8th grade, playing soccer and thriving.
Children’s National is the proud pediatric partner of the Commanders. The team went on to defeat the Cleveland Browns 34–13 that day after celebrating Landon’s victory.

Hope lives at the Children’s National Research Institute, fueled by groundbreaking science to advance pediatric medicine. Dive into this vital work with our new video podcast, “The Lead in Peds.”
The host is Dr. Nathan Kuppermann, executive vice president, chief academic officer, director of Children’s National Research Institute and the Fight For Children Distinguished Chair of Academic Medicine. With more than 30 years of experience in emergency medicine and federally funded clinical research, he approaches each conversation with a scientist’s curiosity and a pediatrician’s compassion.
“The

“I’m excited to give listeners a behind-the-scenes look at Children’s National — to showcase our exceptional science, how it transforms clinical care and how meaningful this work is to my colleagues. It’s a joy to bring our audience along for the journey.”
In our first season, Dr. Kuppermann explores the latest research in cardiology, addiction medicine, our first-in-the-world growth trial and more. He recently sat down with one of our experts in artificial intelligence to discuss how new technologies will revolutionize pediatric care. Tools to help doctors spot diseases early and choose the right treatments are under development and will extend the reach of our clinicians to small towns and other countries.
“With more than 2,000 active research projects underway, the potential to improve children’s health worldwide is within reach,” Dr. Kuppermann says.

Episode 1 | Beating Strong: The Lifelong Impact of Pediatric Cardiology with Mary Donofrio, MD, and Wayne Franklin, MD
Episode 2 | Hidden Struggles: The Reality of Pediatric Addiction with Sivabalaji Kaliamurthy, MD
Episode 3 | Growing Hope: Advancing Care for Kids with Growth Disorders with Andrew Dauber, MD, MMSc
Episode 4 | Future Ready: AI’s Role in Revolutionizing Pediatric Care with Marius George Linguraru, DPhil, MA, MSc
Learn more, play and subscribe! Scan this QR code.


A bottle of water, an activity kit or just a smile can make a difference to families waiting in the Emergency Department (ED). Our new Experience Ambassadors Jacqlyn Johnson and Andriy Chybisov deliver these comforts during what often is a stressful time. Their presence also frees up clinical staff to focus on critical patient care.
“From consoling a frightened child to wrapping a blanket around a worried parent, we can change the trajectory of the whole experience in our ED,” says Johnson.
The team responds to questions about wait times, fasttracks patients who need a rapid check-in, escorts families, gathers feedback, and manages bed availability and the need to restock supplies. “In our roles, we have a unique vantage point,” says Chybisov. “Seeing things from the patient’s perspective helps us identify both small and systemic improvements.”
The team’s positive impact already is evident in rising ED satisfaction survey scores. “It’s all about making our young visitors and their families feel more comfortable, informed and in control of their visit,” says Chybisov.
One mother recently confirmed to Johnson that it’s working. “You are the reason I did not completely fall apart,” she said. “Thank you for your kindness and patience.”
This effort also improves the ED staff experience. Children’s National is a pioneer in Human Experience, a concept that recognizes the importance of taking care of our care providers. We turned to this approach as the pandemic brought the need into stark relief. A staff that feels supported and engaged can better care for patients.
From consoling a frightened child to wrapping a blanket around a worried parent, we can change the trajectory of the whole experience in our ED.”
— Jacqlyn Johnson


Soon after Sumukh, 12, was diagnosed with leukemia at age 9, his care team dubbed him the “mayor” of our Oncology unit. Sumukh quickly made friends with fellow patients and staff, hosted video game leagues, danced and played bingo. In October 2023, he rang the bell to mark the end of his six months of chemotherapy. So many care team members wanted to cheer him that they rescheduled the celebration to accommodate his community of support. “Sumukh does everything he can to make others feel special,” says his mom, Suchitra. “I’m grateful he received the same with the amazing care and all the love he could get at the hospital.”
How would you describe your experience at Children’s National?
It was awesome! Everyone supported me and talked to me a lot. The nurses were so fun and always came to my room to help distract me, especially with movie nights and Mario Kart challenges. Carl and Evan were the only two nurses who could beat me. My friends at school told me they were jealous of all the cool things I got to do in the hospital.
Tell us about a time someone took special care of you.
The Child Life specialists taught me about my leukemia diagnosis with a lot of kindness and respect. I learned everything I could about my treatments and medicines, and it was a big help to not feel so afraid. And one of the nurses, Ali, made so much time for me. She said she was 50% nurse and 50% my playmate.
What’s your favorite place or thing about the hospital?
I love Seacrest Studios. The deejays, weekly bingo sessions and game shows like “Are You Smarter Than a 5th Grader?” made me happy. Because I finished my treatments, I only need to go back to the hospital for annual scans, but I still want to visit to see the fun things happening around Halloween and other holidays.
What do you do for fun?
I play cricket on a junior league and hope one day to compete in the World Cup. When I was in the hospital, I loved getting to play cricket with my dad in the Healing Garden. I also like to do karate, Bollywood dance and travel. And I really want to become a pilot!

Watch Sumukh ring the bell at his Mario-Kart-themed party.

Children’s National Hospital Executive Leadership
Michelle Riley-Brown, MHA, FACHE
President, Chief Executive Officer
Donna Anthony, MPH
Senior Vice President, Chief Strategy Officer
Nathaniel Beers, MD, MPA, FAAP
Executive Vice President, Community and Population Health
Catherine Bollard, MD, MBChB
Senior Vice President, Chief Research Officer
Denice Cora-Bramble, MD, MBA Professor of Pediatrics
Gina M. Cronin, MHA, FACHE
Senior Vice President, Chief People Officer
Jeffrey Dome, MD, PhD
Senior Vice President, Cancer and Blood Disorders Center
Wayne J. Franklin, MD, FACC
Senior Vice President, Heart Center
Jordan Grossman, JD Vice President, Chief of Staff
Mary Anne Hilliard, Esq., RN, FAAN
Executive Vice President, Chief Legal Officer, General Counsel
Nathan Kuppermann, MD, MPH
Chief Academic Officer, Chair of Pediatrics
Aldwin Lindsay, MBA
Executive Vice President, Chief Financial Officer
Matt MacVey, MBA
Executive Vice President, Chief Information Officer
DeAnn Aston Marshall, MHA
Executive Vice President, Chief External Affairs Officer
President, Children’s National Hospital Foundation
Jessica Menter, MPP
Executive Director, Corporate Governance and Strategic Engagement
Anthony Sandler, MD
Senior Vice President & Surgeon-in-Chief
Joseph E. Robert, Jr., Center for Surgical Care
Director, Sheikh Zayed Institute for Pediatric Surgical Innovation
Linda Talley, MS, RN, NE-BC, FAAN
Senior Vice President, Chief Nursing Officer
Elizabeth Wells, MD, MHS
Senior Vice President, Neuroscience and Behavioral Medicine Center
David Wessel, MD
Executive Vice President, Chief Clinical Officer
Physician-in-Chief
Children’s National Hospital Foundation
Executive Leadership
DeAnn Aston Marshall, MHA
Executive Vice President, Chief External Affairs Officer
President, Children’s National Hospital Foundation
Julie Butler
Vice President
Kerri Yoder Hubbard
Associate Vice President, Major, Principal and Research Gifts
John Loughner Vice President, Systems and Data Integrity
Melanie McCarty
Associate Vice President, Special Events and Stewardship
Tin Pham
Associate Vice President, Finance
Mandy Ranalli
Associate Vice President, Major, Principal and International Gifts
Leslie Schrader Vice President, Chief Marketing and Communications Officer
Elizabeth Treble
Associate Vice President, Corporate and Annual Giving
Children’s National Board of Directors
Horacio Rozanski Chair
Barbara Lopez Kunz Vice Chair
Ramu Potarazu Treasurer
Amy Baier
Jonca Bull, MD
Toni Bush
Amy Freeman
Michael Jones
Jason Levien
Carrie Marriott
Linda Rabbitt
Jimmy Reyes
Mark Rouchard
David Strickland
Caroline Van Vleck, MD
Michael Ward Directors
Michelle Riley-Brown, MHA, FACHE President, Chief Executive Officer
Children’s National Hospital Foundation Board of Directors
Kathie Williams Chair
Fernando Goldsztein, MBA
Paul Grayson
Thomas Lloyd
Timothy Lowery
Mei Xu Directors
Michelle Riley-Brown, MHA, FACHE President, Chief Executive Officer
Horacio Rozanski
Children’s National Board Chair


― Karen Stauffer, Mom of Children’s National Patient Owen and Race Co-chair