St. Joseph’s Health in New Jersey trains ED staff to spot trafficking victims
‘It disproportionately affects the population we see: the underserved, potentially homeless patients’
By KATHLEEN NELSON
St. Joseph’s Health in Paterson, New Jersey, has formed a partnership with the U.S. Department of Homeland Security to identify victims of human trafficking and protect exploited persons.
With inspiration and support from the department’s Blue Campaign and other sources, St. Joseph’s will train more than 400 emergency clinicians and staff before expanding to other areas of the hospital that are likely to interact with victims of human trafficking.

“It’s a wonderful project,” says Dr. Marjory Langer, chief of emergency services at St. Joseph’s Wayne campus. “Every day we wonder how many of these people we can help that come through our doors that we haven’t recognized.”
The scope of trafficking
Human trafficking involves the use of force or fraud to obtain some type of labor or commercial sex act. Polaris, which connects victims and survivors of human trafficking to support and services in North America, estimates that 28 million people were victims of human trafficking worldwide in 2022 and that about 68% have contact with emergency departments.
“So, statistically, we’ve all had contact with patients who have been victims,” says Brian Dolan, director of the emergency departments at St. Joseph’s in Paterson and Wayne, both in northern New Jersey.
DHS told St. Joseph’s that victims in southern New Jersey report more sex trafficking, while victims in northern New Jersey report more labor trafficking. The first
Continued on 6
‘A chance to breathe again’ 2
Mercy’s AI-driven chemo care model bears name of co-creator who died of cancer
By KARI WILLIAMS
A researcher at Chesterfield, Missouri-based Mercy who helped develop an AI-driven program to serve at-risk chemotherapy patients received her own cancer diagnosis while working on the project.
Jiajing Chen, the biostatistician assigned to the topic, had peripheral T-cell lymphoma. She died last year. After her death, the platform was named in her honor.
“She was so instrumental that it never would have happened without her,” Dr. Jay Carlson, Mercy Cancer Care Performance
Continued on 5



CommonSpirit
hospitals
send cafeterias’ surplus to community
By NANCY FOWLER
A pilot initiative to tackle food insecurity while also reducing landfill waste is underway at St. Joseph Medical Center in Tacoma, Washington.
The medical center’s system, Virginia Mason Franciscan Health, launched the edible food recovery effort in July. The project sends surplus food from St. Joseph’s cafeteria to people who need it. The pilot program is an alliance between the hospital and three local partners, St. Leo’s Food Connection, the Tacoma Rescue Mission and the Oasis Youth Center, that offer free hot meals.

“This is good food that would otherwise go to waste,” says Doug BaxterJenkins, division director of community health at Virginia Mason Franciscan Health. “But the program gets the food to those who can use it right away.”
Virginia Mason Franciscan Health is expanding the initiative to another hospital
Continued on 4
Rural hospitals are at a tipping point. Rural hospitals are closing services and some hospitals are closing altogether. More than half of rural hospitals do not offer labor and delivery service, said Jamie Orlikoff, an author, consultant and the national adviser on governance and leadership to the American Hospital Assocation. Orlikoff encourages facilities to use technology and artificial intelligence to increase productivity and reduce burnout, and to recruit strong, aggressive board members from outside the community.
Continued on 8
out chaplaincy services
Contracting
3 Executive changes 7
PERIODICAL RATE PUBLICATION MARCH 2024 VOLUME 40, NUMBER 3
Mercy researcher Jiajing Chen, pictured with her husband, Andy Greenwood, and children, lost her battle with cancer last year.
David Clarke, a cook at St. Joseph Medical Center in Tacoma, Washington, readies packaged surplus food that will be shared with community partners in the hospital’s edible food recovery effort.
The American Hospital Association recently hosted the Rural Health Care Leadership Conference in Orlando, Florida. Catholic Health World Associate Editor Valerie Schremp Hahn attended and shares some key takeaways. How to help rural hospitals? Ten takeaways from AHA conference 1
Langer
Baxter-Jenkins

SSM Health partnership
SSM Health and research organization Circuit Clinical announce a partnership that will “significantly expand” access to clinical trials and treatments for patients with cancer.
Hawaiian’s
long journey to Houston gives him ‘another chance to breathe again’
By VALERIE SCHREMP HAHN
When Dr. Gabriel Loor and other doctors at Baylor St. Luke’s Medical Center in Houston heard about a man from Honolulu who couldn’t get the double lung transplant he needed, they figured out how to help.

A health care team in Hawaii had been unable to find a hospital willing to take 54-year-old Benjamin Calimbas, mostly due to insurance issues and his dire condition.
When Calimbas was strong enough for the trip, Baylor St. Luke’s arranged to transport him 4,000 miles to Texas on a medical flight. During the eight-hour flight, he was attached to an ECMO machine, which provided support to his heart and lungs.
“For somebody traveling so far, on a device where anything could happen during that transportation, was absolutely crazy,” said Loor, who performed the surgery on Calimbas. “For them to put all of their trust in our system, to take that risk, was remarkable.”
Loor is surgical director of lung transplantation at Baylor St. Luke’s, where about 70 lung transplants take place every year. The hospital is part of St. Luke’s Health System, a subsidiary of CommonSpirit Health. Most of the patients who get transplants are from Texas or contiguous states, he said.
Healthy, then suddenly frail
Calimbas had been a healthy father of two when he began having breathing problems in February 2023. He developed pneumonia, which progressed to respiratory failure that severely damaged both lungs. Before long, he could no longer breathe on his own. His care team at Queen’s Medical Center in Honolulu intubated him and then put him on ECMO. They determined he needed a double lung transplant.
In addition to respiratory failure, Calimbas was suffering from kidney failure, infection, gastrointestinal bleeding, and physical deconditioning, Loor said. The longer he stayed on the ECMO device, the more risk he had of stroke, bleeding, and more complications.
The doctors at Baylor St. Luke’s heard about the case through an intensivist who knew a thoracic surgeon at the hospital in Hawaii. They started informal talks and eventually determined they could treat him. He flew to Houston in April.
Calimbas spent the first month or so in

$25 million gift
Mercy Housing gets a $25 million gift from the Yield Giving Foundation, headed by philanthropist MacKenzie Scott. The affordable housing provider’s CEO said the gift will help the nonprofit bring about "a healthier, more equitable society.”

Slow and Simple
CHA’s 14-week series of reflective images and meditations offers meaningful ways to journey through Lent and Easter. The resources are designed for both individual and group reflection.

Houston in late spring 2023 rebuilding his strength.
“Our physical therapy teams were working around the clock on the weekends, trying to get him strong enough to be able to tolerate any kind of surgery,” Loor said. “Once we had the confidence that we thought he could get through, we went ahead and presented him to the committee, and he was approved for a bilateral lung transplant.”
The committee is the multidisciplinary transplant review board that reviews the status of patients on waiting lists and determines whether matches are appropriate.
Immediate turnaround
Loor said the surgery, which took place June 20, was challenging because of inflammation and scar tissue from the pneumonia, but the transplant otherwise went smoothly. The surgery itself took about six hours, with eight hours total in the operating room. It involved a large team including an operative assistant, trainee, nurses, perfusionists and anesthesiologists.
Loor said the new lungs made a dramatic difference for Calimbas. “It was almost like changing a battery,” the surgeon said. “Once he had that, he was up, he was sitting

CHA to offer pre-assembly session on Catholic vision for U.S. health care
In the lead-up to this year’s Catholic Health Assembly, CHA is hosting a series of discussions on the Catholic vision for health care.
The series is called “Catholic Health Care and American Culture: Legal, Societal and Theological Implications.” It will delve into the intersection of Catholic health care and American culture. Discussion topics will include the goals of the Catholic health ministry as compared to those of U.S. health care generally; public policy implications; and perspectives on diversity, equity and inclusion, from a Catholic standpoint.
The series also will cover the relationship between church officials, religious sponsors and lay leaders.
The series will start with asynchronous learning through podcast episodes and curated articles the week of April 1. During the first four Thursdays in May, CHA staff will lead virtual dialogue sessions.
Series participants can take part in an in-person panel discussion at the assembly. The assembly will be June 9-11 in San Diego.
Visit chausa.org/assembly-2024 for more information, a list of the series’ faculty and a registration link. Details of the assembly are also available here:
in a chair, then walking.”
Within a couple weeks, Calimbas was in a room on a regular floor, rehabilitating and getting ready to go home. He was discharged from the hospital to rehab in late July, and eventually flew home and is doing well, his family reports.
His son, Russell, had been shocked by his father’s dramatic downturn and was elated by his father’s recovery.
“I work as a nurse in the ER back home at Queen’s Medical and I am used to seeing sick people every day but when it came to seeing my own dad in such a vegetative state, it really affected me,” he said in an interview with Baylor St. Luke’s. “Now that he is out of the hospital, I’m really happy that we can go back to the way life was. My dad really missed home, especially his dog, Louie.”
‘A calculated risk’
Loor said that even though Calimbas was very sick, he was very motivated, as were his family members, who stayed by his bedside. Calimbas and his family also were compliant and positive, doing what was asked by the medical team, said Loor. “Family support is so important for this to be successful,” he said.
He’s happy the hospital decided to take on the case.
“At the end of the day, it was our willingness to take the risk,” he said. “And that’s a calculated risk. There are patients that we have turned down and other people have done the case and successfully, so it’s not like we’re the be-all end-all. But in this case, it was really just our willingness to take the risk, and the risk meaning that it could be a bad outcome.
“I had the privilege to be on call that night and do it, so that was awesome,” he said.
Calimbas is grateful for the second chance.
“I can barely remember how I got to Houston,” he told the hospital. “I am very thankful to Baylor St. Luke’s Medical Center for accepting me as their patient and giving me another chance to breathe again.” vhahn@chausa.org
Catholic Health World (ISSN 87564068) is published monthly and copyrighted © by the Catholic Health Association of the United States.
POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29.
Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Vice President Communications and Marketing Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org 314-253-3437
Associate Editor Julie Minda jminda@chausa.org 314-253-3412
Associate Editor Valerie Schremp Hahn vhahn@chausa.org 314-253-3410
Graphic Design
Norma Klingsick Advertising ads@chausa.org 314-253-3477
We Will Empower Bold Change to Elevate Human Flourishing. SM
Catholic Health Association of the United States, March 2024
©
FIND
ONLINE
MORE CHA RESOURCES
chausa.org
Benjamin Calimbas of Honolulu is surrounded by his care team at Baylor St. Luke’s Medical Center in Houston, where he underwent a double lung transplant in June.
Loor
Calimbas, seen here in a post-surgery photo, is doing well, his family reports.
2 CATHOLIC HEALTH WORLD March 2024
St. Mary’s in West Virginia contracts out chaplain services to community organizations
By JULIE MINDA
When a group of Huntington, West Virginia, community organizations collaborated in 2018 to create a substance use treatment center, they quickly determined that they wanted the center to offer not just drug and alcohol treatment and counseling. They also wanted the center to offer clients spiritual care.
Rather than have the PROACT center hire a chaplain on its own, the group determined the best source of chaplain expertise was St. Mary’s Medical Center, one of the founding organizations. Since St. Mary’s pastoral care department did not have the capacity to spare a chaplain to work full time at PROACT, the hospital and its partners in PROACT came up with a solution: St. Mary’s added a chaplain for PROACT to its own staff of chaplains, and PROACT contracts with St. Mary’s for the chaplain’s time.
The arrangement was so successful that a second organization requested the same model. St. Mary’s has been contracting out chaplain services to the Cabell–Huntington Health Department of West Virginia since 2022. St. Mary’s is open to engaging with other organizations as well.

Rev. Greg Creasy, director of the department of spiritual care and mission at Huntington’s St. Mary’s, says PROACT and the health department “reached out to us because they know we have strong chaplaincy services, and they said, ‘Why would we try to do this ourselves, when St. Mary’s is already doing this locally?’”
He says spiritual care “is an investment they are making.”
Opioid crisis cripples state
Sr
The pastoral care department of the 393-

bed St. Mary’s has six full-time chaplains, including the chaplain assigned full-time to PROACT and one who splits time between the health department and St. Mary’s. The hospital’s chaplain team is ecumenical — one chaplain is a priest, one a Presbyterian minister, one a Quaker, one a Mennonite, one a Baptist and one from the Church of God.
Rev. Creasy, who oversees the department, was part of the team that represented St. Mary’s when the hospital joined with numerous partner organizations to create PROACT, which stands for Provider Response Organization for Addiction Care & Treatment.
The group formed — and help to fund — the nonprofit PROACT because of their concerns about the substance abuse epidemic that has been crippling West Virginia, and Cabell and Wayne counties in particular. West Virginia has had the high-
est rate of opioid-related overdose deaths in the country every year since about 2015, according to the Centers for Disease Control and Prevention.
Fully embedded
Established to bridge a gap in services for people using opioids and other substances, PROACT provides outpatient medical and mental health assessment, medicine-assisted treatment and group and individual addiction therapy as well as help finding jobs.
Rev. Rodney Adkins is the chaplain who has staffed PROACT since 2018. While he is part of the St. Mary’s pastoral care department and attends meetings and other activities at that hospital, his office is at PROACT, and that is where he spends most of his time. “I’m very much a part of the culture here at PROACT,” he says. “I’m fully embedded.”
Rev. Adkins tries to meet every one of the hundreds of patients who seek treatment at PROACT each week to make them aware of the spiritual services he can provide. PROACT staff will refer patients who express a desire for spiritual services to him. And he attends group therapy sessions at the center and offers his services to those group members.
He says he spends lots of time “wandering the halls” of the center on the lookout for new faces. He works on relationshipbuilding in hopes that clients will feel com-
fortable accessing spiritual care from him.
Rev. Adkins offers individualized spiritual care. He talks with his clients about their spiritual history, where they stand spiritually and where they want to head. He can connect them with local religious leaders and spiritual resources.
He says research shows that the type of spiritual care he is offering his clients leads to better outcomes for substance use therapy.
Employee retention
Rev. Creasy says while the chaplain arrangement serves mainly clients at PROACT, it is a different situation for the health department contract.
That contract came about because health department leaders had recognized that amid the COVID pandemic, health department staff were under extreme strain. Additionally, some staffers suffered from their own health issues, which compounded their stress. Leadership wanted to offer employees access to spiritual care in addition to the assistance already available, such as counseling.
The health department contracted to have a St. Mary’s chaplain on-site on an ongoing, part-time basis. Rev. Creasy says health department leadership has been very pleased with the results.
“It’s about resiliency and accessing the spiritual resources needed to be a healthy employee. It’s a total look at the individual as a whole person,” explains Rev. Creasy. “And, when we offer that, we see there’s better employee retention.”
He says employees also feel more engaged with their workplace when their spiritual needs are met.
International recruits
Rev. Creasy is unaware of any other hospital in his region contracting out its spiritual care services as St. Mary’s is doing. He says St. Mary’s provides the services at cost. “We’re not trying to make money — this is part of our ministry to the community,” Rev. Creasy says. “We care about and understand the importance of whole-person care — it’s the strength of chaplaincy.”
He says that despite a nationwide shortage of chaplains, St. Mary’s has been able to fully staff its chaplain positions plus hire these additional chaplains to contract out to other organizations. He says the department has been able to find well-matched applicants on an ongoing basis in large part because of its in-house clinical pastoral education program. His department has hired numerous chaplains who served at St. Mary’s through that program.
He notes that St. Mary’s has had much success in recent years recruiting for its clinical pastoral education residents from overseas. Several such recruits have come from Tanzania, one from South Africa and one is a Pallottine Missionary Sister from Poland. Pallottine is the congregation that founded St. Mary’s.
Present to struggling people
Referring to the contracted chaplaincy work, Rev. Creasy says it takes intentionality for organizations to see to the spiritual care of their clients and employees. “It’s about being present to those who are struggling,” he adds.
St. Mary’s pastoral care team is so convinced of the value of their services that they have been offering their expertise to others to give back to the community, says Rev. Creasy. For instance, they helped the local police department develop a chaplaincy program.
He says St. Mary’s has been “thrilled by the opportunities” that have been arising to extend spiritual care more into the community. He says “the chaplains have made a huge impact in the lives of the people they serve.”
Webinar — What Counts as Community Benefit and Accounting for Community Benefit April 23 | 1 – 2:30 p.m. ET Assembly 2024 June 9 –11 Faith Community Nurses Networking Call July 9 | 1 – 2 p.m. ET Upcoming Events from The Catholic Health Association chausa.org/calendar
1 2/14/24 11:29 AM
Mary 4.875x8 ad_Layout
Page 1
Rev. Rodney Adkins speaks with Yvette Rearden, a family navigator, regarding support they can offer to a patient at the Provider Response Organization for Addiction Care & Treatment in Huntington, West Virginia. Rev. Adkins is a chaplain with Huntington’s St. Mary’s Medical Center. He serves the PROACT substance abuse center under a contract between the hospital and treatment center.
jminda@chausa.org
March 2024 CATHOLIC HEALTH WORLD 3
Rev. Creasy
St. Paul Elder Services facility in Wisconsin hosts meal-prepping event for caregivers
Serving as a caregiver for a person with dementia or other impairment can be extremely taxing. To alleviate a bit of the burden, the St. Paul Elder Services campus in Kaukauna, Wisconsin, recently hosted an event to give caregivers ideas for using meal-prepping to free up their time. St. Paul gave the 32 attendees a slow cooker and multiple meals they could take home and prepare.

“Our goal is to provide some relief from the dayto-day stressors of caregiving by providing resources and ideas for easy meal preparation,” said Peyton Ford, a student at the University of Wisconsin — Eau Claire who is an administrative intern at St. Paul. Ford set up the event as one of several projects she has been completing as part of her internship.
“Cooking for Caregivers,” which took place at St. Paul Jan. 25, was open not only to caregivers of people receiving services at St. Paul but also to any caregivers in the community. The event included a presentation from a dietitian about how to do meal prep and how to ensure the meals are
Edible food recovery
From page 1
with plans to grow it more widely over the next year. Meanwhile, the system’s parent, CommonSpirit Health, has a similar separate initiative underway at hospitals in San Francisco.
Virginia Mason Franciscan Health contracts with Goodr, a food waste solutions company. The company sends food containers and labels to the hospital, which packages the day’s excess food. Main dishes range from chicken parmesan to spaghetti and meat sauce to beef pot roast along with side dishes and rolls. Every Monday, Wednesday and Friday, couriers pick up the filled containers and deliver them to partner organizations where the food is heated and served.
“So it’s kind of like a DoorDash, really,” Baxter-Jenkins says.
‘An obligation and a privilege’
The two-year edible food recovery pilot is funded by a grant from CommonSpirit Health’s Mission and Ministry Fund. It costs $576 a month for containers, labels, and 12 pickups and deliveries.
Goodr keeps track of the list of food destinations and contacts the locations to see which ones have the greatest need on a given day.
The initiative doesn’t require an undue amount of effort on the part of the hospital, according to Justin Lee, production manager of the St. Joseph dietary department. In addition to packaging the food, a hospital

nutritious. After that presentation, attendees could taste test the seven meals that they could assemble as ready meals to take home. Next, they visited seven stations staffed by volunteers with a different meal available at each one.
Volunteers helped attendees scoop ingredients into freezer bags. At the end of the two hours, caregivers left with seven
“
The more we can impact food insecurity, the more we improve the health and resiliency of our community members.”
— Stephanie Christensen
cafeteria employee uses an online system to keep track of how much and what kind will be picked up.
“Over a week, the job takes about three or four hours,” Lee says.
The biggest challenge has been keeping enough containers and labels on hand. In October, delivery and receiving issues caused the cafeteria to run out of these essentials, prompting St. Joseph to pause the program. The hospital is still working out an optimal ordering schedule for these materials.
“If we don’t have the labels, we just have to make our own, which takes a little bit longer,” Lee says. “But if we don’t have the containers, then we can’t prepare the food for pickup.”
Lee chalks up the difficulty to the growing pains of a new program. “It’s nice to know the food is going where it’s needed and not just being thrown away,” he says.
In the first six months of the edible food recovery effort, St. Joseph provided 895 meals, while diverting 1,074 pounds of
bags containing at least one meal per bag. All they had to do at home was to reheat the contents.
Some of the choices were Mongolian beef and a healthy version of macaroni and cheese, with or without meat.
St. Paul used a grant from the Thrivent financial services company to fund the event. In addition to the free slow cooker
waste from landfills, according to Stephanie Christensen, a community engagement professional with Virginia Mason Franciscan Health.

Christensen
Christensen is proud the program is making a difference in Pierce County, Washington, where St. Joseph is located, and where nearly one-third of the population experiences food insecurity.
“We’re one of the major employers in Pierce County,” Christensen says. “We have an obligation and a privilege to do this work, and to reduce the food waste in our community and address the environmental impact of food waste.”
Program expansion
Edible food recovery is part of a larger Virginia Mason Franciscan Health strategy to increase food security. The system is also working to boost enrollment in the Supplemental Nutrition Assistance Program for low-income families, improve the appeal of food banks and pantries, and deliver medically appropriate meals to heart patients every month.
“The more we can impact food insecurity, the more we improve the health and resiliency of our community members,” Christensen says.
In January, Virginia Mason Franciscan Health launched a second edible food recovery program at St. Michael Medical Center in Silverdale, Washington. Plans are underway to expand to five more hospitals.
At the same time, Baxter-Jenkins says CommonSpirit Health is piloting another edible food recovery program in its San Francisco hospitals using a vendor called Replate. A California law requires that by 2025, institutions that produce food waste divert at least 20% of their excess edible food to places that will make it available for human consumption.
Eventually, CommonSpirit could divert surplus food away from landfills to people on a much larger scale, according to Baxter-Jenkins.
“CommonSpirit has hospitals in over 21 states,” Baxter-Jenkins says. “There’s no reason why we can’t expand this partnership to more CommonSpirit hospitals that want to replicate it, or to provide technical assistance to other hospitals that are looking to set up their own programs.”
Baxter-Jenkins points out that a side benefit of the edible food recovery program is better recordkeeping in hospital cafeterias.
“I think, ultimately, our food and nutrition leaders will be able to look at this data
and recipes, attendees got a gift bag with T-shirts, freezer bags, cutting boards, pens, notebooks and other tchotchkes.
Ford is studying to become a nursing home administrator. She was inspired to pursue this career path because she witnessed what her own grandparents went through as her grandmother had dementia and her grandfather cared for her.
“I understand the emotional and physical toll this takes on families, and I have a passion to be there for families,” Ford said.
As part of her 12-month internship at St. Paul, she’s worked in every unit on campus. Her administrative internship special projects have included helping to reopen units closed during the pandemic and learning to use certain pain-management machines in the therapy unit.
Ford said attendees gave the meal-prep event high marks on a survey. They appreciated the chance to gather with other caregivers and to get advice and ideas not just about meal-prep but also about caregiving in general. Ford said St. Paul may offer such programming again.
St. Paul is part of Franciscan Sisters of Christian Charity Sponsored Ministries.
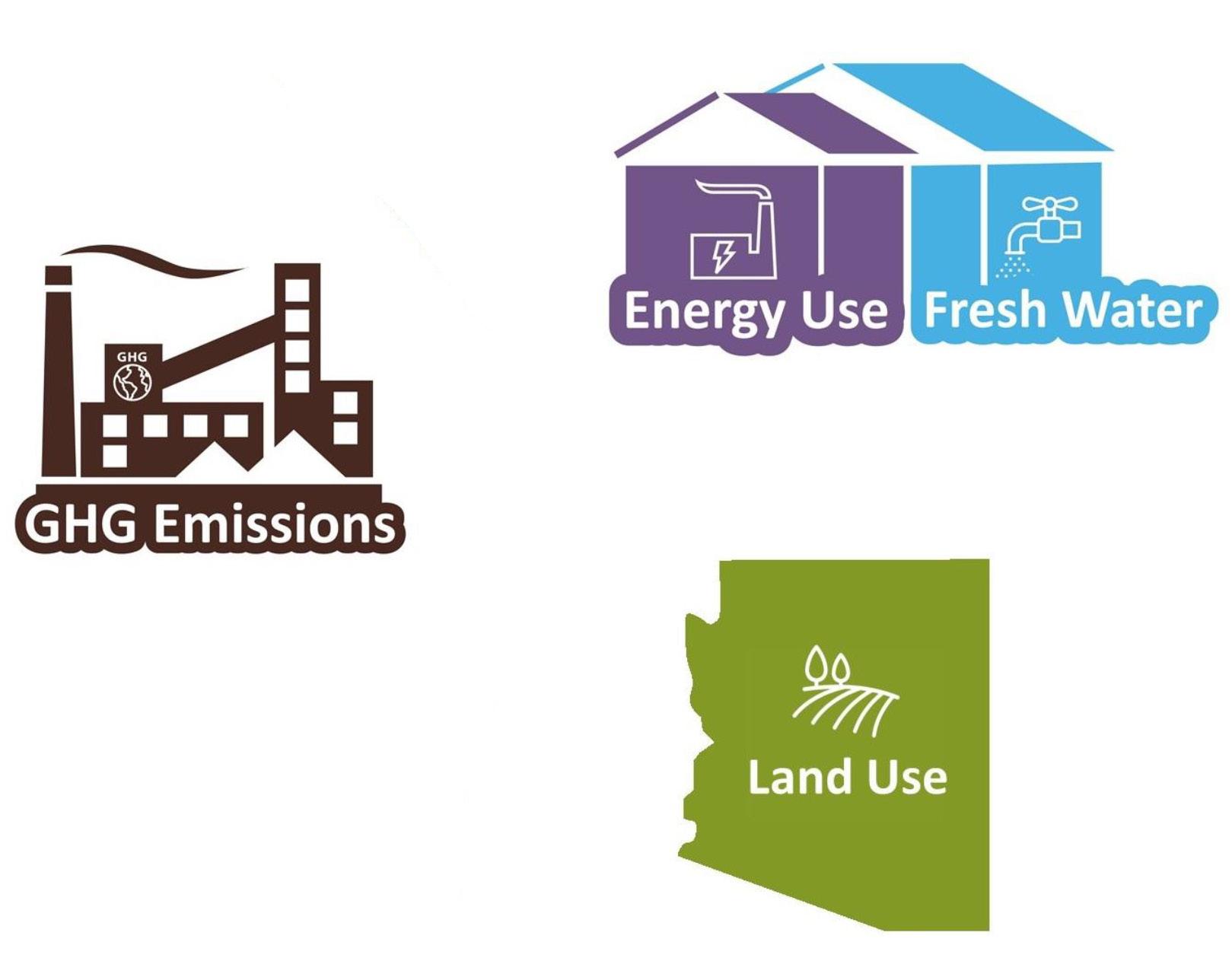
In 2010 food loss and waste at the retail and consumer levels was 31% of the food supply, equaling
133 BILLION POUNDS and almost $162 BILLION
Food is the single largest category of material placed in municipal landfills, where it emits methane, a powerful greenhouse gas.
The U.S. Department of Agriculture and the Environmental Protection Agency have a goal to cut the nation’s food waste by 50% by the year 2030. To reach that goal, the estimated 218.9 POUNDS OF FOOD WASTE
and adjust purchasing to lower our costs,” he says.
But a chief goal of the program remains feeding people who need it, long a tradition among Catholic hospitals.
“One of the sisters on our board, Sister Jude, said that back in the 1970s, she and the other sisters would go to the loading dock every evening and give food to community members,” Baxter-Jenkins says. “And now, we’re doing the same thing but in a more modern way.”
Savings from reducing U.S. food loss and waste by half* *Excludes impacts of waste management, such as landfill emissions. Source: U.S. Environmental Protection Agency GHG emissions equal to 23 coal-fired power plants Enough water and energy to supply more than 20 million homes An area of agricultural land as large as Arizona
PER PERSON sent for disposal per year would have to drop to 109.4 pounds.
U.S. Department of Agriculture
Source:
Ford
4 CATHOLIC HEALTH WORLD March 2024
Event volunteers and participants work together to assemble freezer bags of ready-to-reheat meals at St. Paul Elder Services in Kaukauna, Wisconsin.
AI-driven program
From page 1
Acceleration medical director, said of the Chen Chemotherapy Model.

Chen held a Ph.D. in health outcomes research and a master’s degree in biostatistics and epidemiology, both from Saint Louis University.
Andy Greenwood, Chen’s husband, said she wanted to be a doctor from a young age and completed three years of medical school in China before her family moved to the U.S. She didn’t want to start medical school over again in the states, but still had a love for medicine and public health. That led her to her public health career. “I think she found her talents were best utilized there,” Greenwood said.
“She had such a keen attention to detail and also she never took shortcuts or would sacrifice anything in terms of the work that she did,” he added.
In August 2020, Chen’s project won an Innovation of the Year award at the Association of Community Cancer Centers National Oncology Conference for the original algorithm version of the Chen Chemotherapy Model. The model was recently
updated to include the smart text program.
Identifying risks
Earlier that year, the Centers for Medicare & Medicaid Services had announced its outpatient quality initiative called OP-35. The initiative involved monitoring inpatients and outpatients within 30 days of chemotherapy treatment, said Carlson. The initiative focused on nonleukemia chemotherapy patients 18 years and older.
Using 12 years of medical record data, Chen and Carlson reviewed 42,000 “chemo encounters.” From that information, they developed an algorithm that predicted who is at risk for an emergency room visit after chemotherapy.
Through their research, they identified 18 risk factors that could be associated with an ER visit or inpatient admission, said Carlson, who is also medical director of the oncology service line at Mercy.
In the project’s next phase, Carlson and Chen focused on the reasons chemotherapy patients visit the ER that could be managed in an outpatient setting. That’s when they developed the smart text platform.
Patients who opt into the platform receive a daily text for seven days after undergoing chemotherapy, except weekends and holidays. The text includes a list of symptoms including diarrhea, pain, fever, fatigue, nausea/vomiting or no symptoms.

When patients select a symptom, they are prompted to rate it. Symptoms deemed severe based on
internal criteria in the platform are escalated to the patient’s triage team, Carlson said. Nurses then conduct a further assessment and determine if there’s an opportunity to proactively manage the patient.
The model, according to Carlson, has increased the standard of care. Previously, Mercy care providers wouldn’t know if a patient had a problem until the patient called his or her provider or was in the ER.
“Patients have found it very easy to answer the text,” Carlson said. “Clinics found it to be a very positive option. They’re able to prioritize their day and affect that patient journey in a positive way.”
AI assistance
The assembly main stage will feature thought leaders in health care policy, the future of technology, financial reform, industry innovation and Catholic identity.
Breakout sessions and peer conversations will provide rich opportunities for dialogue and engagement around the pressing issues of our time, including artificial intelligence, health care reform and the unique role of Catholic health care in fostering unity.
Pre-assembly learning modules will explore the nuances of where the Catholic vision of health care fits with American health care.
A specialist in public finance and health economics, Amy Finkelstein, PhD, is the John & Jennie S. MacDonald Professor of Economics at the Massachusetts Institute of Technology. She has been awarded multiple honors and fellowships for her research, including a MacArthur Foundation Fellowship and the John Bates Clark Medal.
One of the health care industry’s leading digital futurists, Tom Koulopoulos is the author of 13 books and founder of Delphi Group, a Boston-based think tank which provides strategic advice to Global 2000 organizations. Drawing on more than 30 years of experience in his field, Tom’s insights have been described as thought-provoking, content rich and inspirational.
The Chen Chemotherapy Model is one of several AI-related products Mercy’s team has developed to assist providers, according to Kerry Bommarito, Mercy vice president of enterprise data science. The intent of AI in a medical setting is to assist patients, she said, “not to be the one thing that makes the decision or determines any sort of treatment or care.”

The texting platform is “enabling patients to respond to questions about their symptoms in the easiest way possible,” Bommarito said. “It’s not intrusive.”
Bommarito said that after Chen’s diagnosis, the chemotherapy model project became “so much more real” to her.
“It was really important to her that once she returned from her medical leave she still had that opportunity to work on it,” Bommarito said. “And after she had passed, it was important to us that we name it after her, because of how important it was to her.”
Chen, with her data science and statistics research background, “really dug into the data” and determined which factors were important, Bommarito said.
Mercy does not plan to market the algorithm, but it does plan to submit the concept and the related workflow for publication in a medical journal so other health systems could potentially make use of a similar analysis within their electronic medical record.
Power of mission
For Greenwood, it’s gratifying that the work Chen was involved with will make a difference and save lives.
“That makes me very proud as her husband, to know I married someone very brilliant,” he said. “It kind of warms my heart to see that come to fruition.”
In addition to her intellect, Greenwood said Chen was a warm person with a happy spirit.
“She loved being around family and friends, helping others and brought great joy, really,” he said. “The thing that was said over and over again at her funeral is that people remember her for her smile. Her smile really did give people a glimpse into who she was and into that spirit.”
Greenwood said his wife fought her illness “with every inch of strength” she had, but the cancer proved very aggressive. “Every day counts, and it was hard for me just to watch someone go through that much suffering,” he said.
Having the model being named after Chen is special for her children, aged 1 and 4, according to Greenwood.
“It gives me something to share with them as they get older,” he said. “Our daughter was in the hospital a lot visiting. She saw everything unfold. So she will carry those memories, I think, forever. And knowing that (my wife) was trying to help cancer patients will, in some ways, potentially help with our personal healing journey through time.”
Chen loved serving others.
“She really felt that power of mission at Mercy through her journey,” Greenwood said. “It’s incredibly meaningful to us that Mercy and the Catholic communities here have been so supportive of us and our families.”
Carlson
Bommarito
March 2024 CATHOLIC HEALTH WORLD 5
A platform created as part of the Chen Chemotherapy Model developed by Jiajing Chen and colleagues at Mercy sends questions to chemotherapy patients after treatments via text. Their answers help care providers determine how to manage their treatment.
Human trafficking
From page 1
challenge is identifying victims or getting them to report abuse.

“We really can’t estimate the number we see because it’s been so underreported and it’s such a sensitive issue,” says Dr. Nilesh Patel, chair of St. Joseph’s emergency services in Wayne and Paterson. “We know that it disproportionately affects the population we see: the underserved, potentially homeless patients. So we’re in a ripe area to identify victims.”
Grassroots impetus
St. Joseph’s Blue Dot program gives patients discrete means to seek help
St. Joseph’s Health in Paterson, New Jersey, has embraced the Blue Campaign wholeheartedly, adding its own twist on recognizing victims of human trafficking — the Blue Dot program.
Brochure offers tips
A brochure produced by the Department of Homeland Security as part of its anti-human trafficking Blue Campaign offers tips on indicators that someone is being trafficked. The brochure is among the library of materials available for download at dhs.gov/blue-campaign.
St. Joseph’s gathered a wealth of state and national resources, thanks to a grassroots effort of nurses in the emergency department at Wayne. In June, nurses Veronica O’Dell and Dawn Simard started research into human trafficking as part of St. Joseph’s RN STARS Program, which promotes professional development for direct care nurses.
Because every patient in the emergency departments at the Wayne and Paterson campuses is required to submit a urine sample, the nurses have filled the designated bathroom with signage and other information about human trafficking in English, Spanish, Arabic and Hindu. Next to the sample cups is a pack of blue circular stickers.

“I think part of the success is that this is a nurse-driven protocol with a lot of support,” Simard says. “It emulates the Magnet aspect of the hospitals that we work for and shows that nurses are held in a high regard and want to be the change.” Magnet recognition is an honor given to nurses who show a commitment to excellence.
O’Dell and Simard gathered resources — including data and material from the Blue Campaign and Polaris — and received training from the New Jersey Coalition Against Human Trafficking. The Blue Campaign is designed to raise public awareness about human trafficking by working with organizations and making awarenessraising resources available to educate the public.
Through their research, O’Dell and Simard developed a three-step program: a survey for all emergency department workers to gauge their knowledge of human trafficking, a training session to identify trafficking victims and a post-training survey/ assessment.
“The signage breaks it down: If you feel unsafe or if someone is trafficking you, we provide a hotline number and instructions to put the blue dot on the bottom of the urine cup,” says Veronica O’Dell, one of the two nurses who initiated the program at Wayne.
ED staff at St. Joseph’s have been trained to check the bottom of the cup, then alert attending physicians, residents and staff to use an assessment tool. “We started it because it’s a simple yet effective intervention,” says Dawn Simard, the project’s other creator.
Since launching in late summer, however, the staff has yet to see a blue dot on a sample. “For now, the most important aspect is that they realize they are safe here in the emergency department,” Simard says.
The benefit for now is learning, using and trusting the process.
“It’s an inspirational project that the nurses have started,” says Dr. Marjory Langer, chief of emergency services at St. Joseph’s Wayne campus. “It’s really helped with the teamwork and the positive attitude in the department. If we can identify one person and help them, it makes the project worth it.”
— KATHLEEN NELSON
“The training they receive from us is what to look for when you triage, what to look for when you go through someone’s chart, the red flags we’re looking for and what our safety protocols are after that,” O’Dell says.
Dolan says that the entire emergency department staff at Wayne has been trained and that O’Dell and Simard trained some of their fellow RNs at Paterson.

“Even after handing out the pre-assessments, we already had staff wanting more information,” says Carlin Keil, one of the nurses training her colleagues at Paterson. “It’s sparking interest even before education.”
Following the emergency departments, St. Joseph’s will train staff in outpatient surgery and labor and delivery.
“Ultimately our plan is to have everyone in the institution knowledgeable about human trafficking, since victims are not likely to have a primary doctor,” Simard says. “Then it will spread through the organization. We want everyone to be able to assess and every corner of our facility to be a place where a patient can feel safe and get information about human trafficking. So, ultimately, that will include everybody.”
In the meantime, St. Joseph’s has leaned heavily on the resources from the Blue Campaign, all provided free. The hospital ordered handouts, posters and pamphlets in English and Spanish. All include the national hotline number, 1-888-3737888. St. Joseph’s also has handed out first responder identifier cards and key tag cards

Physical:
Does the person ...
Show signs of physical and/or sexual abuse, physical restraint, confinement or torture?
Appear to be deprived of food, water, sleep, medical care or other necessities?
Lack personal possessions?
Social:
Does the person ...
Work excessively long and/or unusual hours?
Show sudden or dramatic changes in behavior?
Act fearful, anxious, depressed, submissive, tense or nervous/paranoid?
Defer to another person to speak for him or her?
Appear to be coached on what to say?
Appear disconnected from family, friends, community organizations or place of worship?
Not have the ability to freely leave where they live?
for staff that list signs of human trafficking and how to report it.
Brandi Bynum, section chief of the Blue Campaign, praised St. Joseph’s as “one of the first hospital systems to join the campaign and work with our local office to train hospital staff on how to recognize and respond to potential victims of human trafficking.”
A waiting game
Despite the wealth of resources, St. Joseph’s Blue Campaign is a leap of faith. Whether the information effectively reaches those who need it most or causes them to take action is tough to measure because of the nature of human trafficking.

Cramer
“One of the biggest challenges is that many victims don’t know they are victims,” says Melissa Cramer, ED day shift manager at Wayne. “They are brought into trafficking by coercion. It could be a family member, significant other or sponsor. They think these are people who care about them and want to help them. Even if they do acknowledge being trafficked, it’s hard to ask for help. They don’t know how to get out, or maybe their families are being threatened. So, the number of people who know they are being trafficked and ask for help is really low.”
“
The biggest thing is to get the awareness out there, that patients know that they are safe and they have the ability to get help regardless of where they are.”
— Brian Dolan
With few measurable outcomes to gauge success, Dolan says, “The biggest thing is to get the awareness out there, that patients know that they are safe and they have the ability to get help regardless of where they
are.”
He adds: “We want to make everyone aware, not just at St. Joseph’s but in health care in general. Whether you’re following what we’re doing here at St. Joseph’s or any other program, the idea is just to provide a feeling of safety for the patient to declare themselves a victim, whatever time or whatever facility.”


Contact Madeline Hantak at mhantak@chausa.org for information about underwriting. ApolloMD Aquinas Institute of Theology Health Trust Performance Group Huron Institute of Reproductive Grief Care Key Green Solutions Loyola University Chicago Bioethics Institute ShiftMed
Patel Simard
Dolan
Human trafficking In 2021, there were 10,359 trafficking situations reported to the Polaris-operated National Human Trafficking Hotline. In those situations, 16,554 likely victims of trafficking were identified. TOP TYPES OF TRAFFICKING Escort services 10% Pornography 8% Illicit massage, health and beauty 6% TOP RECRUITER TYPES Family member/caregiver 33% Intimate partner 28% Employer 22% TOP RECRUITMENT LOCATIONS Dating site 13% Street 11% Facebook 10% TOP RISK FACTORS/VULNERABILITIES Recent migration/relocation 54% Mental or physical health concern 10% Substance use concern 9% Unstable housing 8%
6 CATHOLIC HEALTH WORLD March 2024
Sisters of Bon Secours celebrate congregation’s bicentennial
Throughout this year, the Congregation of the Sisters of Bon Secours and many of the sisters’ ministries are marking the bicentennial of the congregation’s founding in Paris, France.
The Sisters of Bon Secours, USA, which is headquartered in Marriottsville, Maryland, has planned multiple events, including a Palm Sunday concert at the sisters’ retreat center this month and a celebratory Mass at the Baltimore Basilica in May. Baltimore Archbishop William Lori will preside over that Mass.
Facilities within the Bon Secours Mercy Health system also are marking the occasion, including with chaplain-led prayers in staff meetings at some locations. The system’s Richmond, Virginia, market held a service in January to formally recommit to its values. That market also is incorporating anniversary themes into this year’s physician and associate recognition events and its hospital week and nurses’ week commemorations. Also in that market, Richmond Bishop Barry Knestout will celebrate a Mass in honor of the sisters’ anniversary at Richmond’s Cathedral of the Sacred Heart.
In the Greenville, South Carolina, and Hampton Roads, Virginia, markets, Bon Secours facilities held in-person prayer services, distributed prayer cards and handed out desserts, including eclairs at Hampton Roads. Some Hampton Roads sites also provided French-themed meals.
A group of a dozen women founded the Congregation of the Sisters of Bon Secours in Paris in 1824 amid the devastation that followed the French Revolution. “Bon Secours” means “Good Help” in French. The sisters took what at that time was a bold approach: They left the security of their cloister to nurse sick and dying people at home. Their message that there is a God who loves all people was the same then and now, says the website of the congregation’s
KEEPING UP





PRESIDENTS/CEOS
James T. Kennelly to president and CEO of SMP Health of Fargo, North Dakota, from vice president of mission and formation. He succeeds Aaron K. Alton, who retired in December after 29 years as president and CEO.
Karl Keeler to chief executive of the Providence LA-Valley service area. He also will retain his position as chief executive of Providence Saint Joseph Medical Center in Burbank, California. Under the role expansion, he now has oversight of Providence Cedars-Sinai Tarzana, in partnership with Cedars-Sinai, and Providence Holy Cross medical centers. Holy Cross is in Mission Hills.
Dr. Jim McGovern to chief hospital executive of the PeaceHealth Oregon network, from interim chief executive and chief medical officer. As hospital executive, he leads hospital operations including at PeaceHealth Sacred Heart Medical Center at RiverBend, PeaceHealth Cottage Grove Community Medical Center and PeaceHealth Peace Harbor Medical Center in Florence.
Theresa Rutherford plans to retire

The early Sisters of Bon Secours did something that was unheard of at the time, traveling outside of the convent to minister to the sick and dying. That practice has continued wherever they are needed. Here, in 1956 in Paris, Sisters of Bon Secours use scooters to travel around their community to minister to the sick.
U.S. province.
In 1881, Cardinal James Gibbons of the Archdiocese of Baltimore invited the sisters to establish a health care ministry in that archdiocese. The women immigrated to the U.S. and established their first hospital in Baltimore in 1919. Over time they built up a network of health care facilities, primarily on the east coast. The sisters’ U.S. hospitals consolidated as Bon Secours Health System in 1983. In 2018, that system merged with Cincinnati-based Mercy to form Bon Secours Mercy Health, which today includes 49 hospitals. Bon Secours Mercy has a presence in seven states as well as in Ireland.
Worldwide, the sisters have health care, housing, education and other ministries in six countries: the U.S., France, Great Britain,






as president and CEO of HSHS St. Mary’s Hospital in Decatur, Illinois, effective April 1. Hospital Sisters Health System is conducting a search to identify her successor.
Tom Hathaway to president of Holy Cross Medical Group, a multispecialty physician group connected with Holy Cross Health of Fort Lauderdale, Florida. Holy Cross is part of Trinity Health. Hathaway was vice president of operations.
ADMINISTRATIVE CHANGES
Trinity Health of Livonia, Michigan, and its subsidiaries have made these changes:
At Saint Agnes Medical Center of Fresno, California: Dr. John C. Evanko to chief medical officer, Sara K. Frauenheim to chief development officer, Jennifer L. Misajet to interim chief nursing officer, William Evo to vice president of operations and Casey Fares to director of marketing and communications.
At Holy Cross Health of Silver Spring, Maryland, Dr. Salim Saiyed to vice president/chief health informatics officer for the region.
Jeremiah Dodrill to chief financial
Ireland, Peru, and the Democratic Republic of the Congo. Laypeople can join the congregation through an associate program.
The sisters have been innovators throughout their history, says the USA sisters’ website, which notes that the congregation established the world’s first formal home health care service, the first day care in the U.S. and the first Catholic facility for disabled children.
The congregation has one request for everyone who wishes to honor the sisters during this milestone year: “We are asking people to think of and pray for the Sisters of Bon Secours when they are doing any type of service work for others,” says Liz O’Neill, the communications director of the Sisters of Bon Secours, USA.
IN BRIEF
Mercy Hospital Oklahoma City opens emergency department expansion
Mercy Hospital Oklahoma City’s emergency department has expanded.
The $2.6 million project was fully funded by local philanthropists Herman and LaDonna Meinders. The addition includes a new CT scanner to serve patients experiencing emergencies like strokes, trauma, abdominal pain, chest pain and other neurological conditions.
More than 50,000 patients seek care at the Mercy Hospital Oklahoma City ER annually, and nearly half of them require at least one CT. Before the expansion, patients were transported to a different floor in the hospital to get the imaging needed for a diagnosis.
In addition to fully funding the ER project, the Meinders donated $7.5 million in August to build the Kathryn Ann Meinders Digestive Health Institute at Mercy.
Avera expands access to inpatient behavioral health care
Avera Health is expanding access to inpatient behavioral health care in Sioux Falls and Aberdeen, South Dakota.
In Sioux Falls, Avera Behavioral Health will finish shell space in the new Helmsley Behavioral Health Center, adding 16 beds for adult care. The project will bring Avera Behavioral Health Hospital to 162 beds, making it the fourth largest hospital in the state.
In Aberdeen, Avera will create a new 18-bed unit for adults and seniors, and crisis stabilization for adolescents in vacant space on the fourth floor of Avera St. Luke’s Hospital. The hospital now has 10 beds for inpatient behavioral health.
Both projects are making use of state and federal funds.
officer of Pittsburgh Mercy.
GRANTS
Holy Cross Health of Fort Lauderdale, Florida, received a $2 million gift from a Fort Lauderdale couple to support the hospital’s outpatient rehabilitation center. Holy Cross has named the facility the Jon and Helaine Ayers Rehabilitation Institute in their honor. The center provides specialized outpatient care for people with neurological, oncologic, vestibular and complex orthopedic conditions. The Ayers’ gift will fund a facility renovation and the addition of advanced rehabilitation equipment. Jon Ayers, who recently joined the Holy Cross Health Board of Directors, was chair and CEO of the IDEXX veterinary diagnostics and software technology. Holy Cross is part of Trinity Health.
St. Mary’s Healthcare of Amsterdam, New York, has received $1.1 million from the New York Department of Health to provide free cancer screenings to eligible New Yorkers through 2028. The health department’s Cancer Services Program funded the grant. That program ensures access to no-cost screenings for breast, cervical and colorectal cancers for uninsured and underinsured New Yorkers. St. Mary’s has led the Cancer Services Program in three counties since 2008, with grants renewed every five years.
PeaceHealth Southwest Medical Center Foundation in Vancouver, Washington, received a $1 million dollar grant from the Cowlitz Indian Tribe through the Cowlitz Tribal Foundation Clark County Fund. The funds will support the medical center’s emergency department expansion project. When completed in the summer, PeaceHealth Southwest Medical Center’s emergency department expansion will double the size of the facility to better meet the needs of the rapidly growing region.
E.J. Kuiper named president
and CEO of FMOLHS
E.J. Kuiper will become president and CEO of Franciscan Missionaries of Our Lady Health System May 1. He succeeds Dr. Richard R. Vath, who is retiring.
Kuiper is now CEO of CommonSpirit Health’s Midwest division.

In that role, he leads 28 hospitals spanning four states.
Previously, Kuiper was CEO of the Illinois division of Hospital Sisters Health System. Before that he was president and CEO of OSF Saint Anthony’s Health Center in Alton, Illinois. Originally from the Netherlands, Kuiper joined Hospital Corporation of America in 1991 to work as a physical therapist at a hospital in Florida. He worked in progressive leadership roles, ultimately becoming chief operating officer of an HCA facility.
Kuiper received a doctor of physical therapy from the University of St. Augustine in Florida and a master’s in health science and health services administration from Florida Gulf Coast University in Fort Myers.
Sr. Laura Wolf, OSF, is chair of Franciscan Calais Ministries, which is the sponsor of FMOLHS. She said in a release, “E.J. is a man of deep faith. He is an advocate for Catholic health care and the unique opportunities we have throughout our entire ministry to be the face of Christ to each person, especially those most in need. We are confident that he will bring the vision and strength of service to this role that are essential for the longterm stability and growth of our ministry.”
Based in Baton Rouge, Louisiana, FMOLHS has eight hospital campuses in Louisiana and one in Mississippi.
Kennelly
Frauenheim
Rutherford
Fares
Alton
Misajet
Hathaway
Saiyed
Keeler
Evo
Evanko
Dodrill
March 1, 2022 CATHOLIC HEALTH WORLD 7 March 2024
Kuiper
Sculpture from Bon Secours and partner honors school’s racial integration
Bon Secours Richmond and a partner unveiled a public art installation at a January gathering in Richmond, Virginia. The piece, called “Strides,” commemorates a racial integration milestone at Richmond’s Westhampton Junior High School.
In September 1961, then-12-year-old Daisy Jane Cooper was the first Black child to integrate into that middle school. Her mother had pursued three years of litigation so that the girl could attend the allwhite school in her neighborhood rather than the school 5 miles away where minority children were bused. NAACP lawyers represented the family in the case.
Other families had filed alongside Cooper but had withdrawn their cases. So, Daisy Jane was alone in breaking the color barrier that day. A year later, she was the first Black student to integrate into Richmond’s Thomas Jefferson High School.

Rural health care takeaways
From page 1
2
Health care facilities, no matter how small, are not immune to cyberattacks. Ransomware attacks are up 278% since 2020, according to the Department of Health and Human Services’ Office for Civil Rights, and health care is the most attacked sector, according to the FBI. Only 8% of stolen health care information comes from electronic medical records, the rest comes from networks and third-party providers. When hospitals contract with third-party providers, they should make sure those providers have cybersecurity guards in place. “You’re not immune from it,” said Chris Logan, vice president of cybersecurity software company Censinet. “You’re gonna get hit.” How much hospitals are prepared and how they respond will help their situation, he said.

3
Big businesses in rural communities can become health partners. Mohamed Diab, CEO of CVS pharmacy’s Accountable Care, explained how his company partners with more than 200 health systems and 60,000 clinicians in value-based care contracts that cover more than 1 million patients on Medicare. Albert Wu is the chief medical officer of Dollar General, which operates 10 times as many stores as there are rural hospitals. He said the company plans to have fresh produce in half of its stores within the next few years and has added more shelf-stable items like canned proteins and frozen fruit and vegetables. The stores also have opened up their parking lots for use as vaccination sites and are looking for other partners to serve the health needs of their customers.

4
Rural hospitals and patients are just as vulnerable if not more to the effects of climate change. Challenges in rural health care include deferred maintenance to buildings and aging infrastructure. These facilities can access incentives like tax credits and grants for environmentally friendly upgrades. Rural hospitals should work to reduce waste, particularly in areas where resources are limited. The efforts can help save money and the planet: the health care sector, including rural hospitals, is responsible for an estimated 8.5% of greenhouse gas emissions.

5
Lack of housing is a concern for staff and communities. Saint Alphonsus Health System, part of Trinity Health, serves southwestern Idaho and southeastern Oregon. Housing was a top priority in its community health needs assessments, since housing prices had skyrocketed and rentals had become short-term options for recreational use. The health system contributed seed money to help fund housing developments and brought partners together to convert an assisted-living facility to affordable housing. “There’s a number of ways hospitals can be involved in community investing,” said Rebecca Lemmons, regional director of community health and well-being for Saint Alphonsus. “You can be a convener; you can use your social capital and your name ... and you can be an advocate.”

6
Virtual space can be used to share ideas and provide support. AHA President Rick Pollack encouraged hospitals to harness technology like telehealth to reach patients who might otherwise have to drive hours for care. Technology can be used for training, too. In Dartmouth, New Hampshire, the Dartmouth Health Behavioral Health Workforce Development team got a grant from the Health Resources and Services Administration to provide ongoing virtual training to help community-based leaders identify at-risk students, respond to students in distress, and understand the resources available to those who need it.
7
Creative ideas are needed to address staffing and scheduling. During a panel discussion on building a more flexible and sustainable workforce, five rural hospital leaders shared how they’ve addressed challenges. Some offered sign-on bonuses, education benefits, and nurse residency programs. One started an apprenticeship program for medical assistants, lab techs and respiratory therapists. One started a high school “Scrubs Camp” to expose students to health care careers. A medical school clinical rotation program at one hospital prompted some of those doctors to stay.
8
Mothers need support before they have their babies. St. James Healthcare, part of Intermountain Health, is improving the lives of women and
Bon Secours Richmond and Thalhimer Realty Partners commissioned the installation. The sculpture is made up of two metal forms that are 4 feet apart. The negative space between them forms a plus sign, symbolizing integration. When people walk between the two parts of Strides, they can sense the tension from the close proximity of those parts, according to a release. This is meant to challenge them to consider the tension Daisy Jane must have felt the first day of school.
Bon Secours St. Mary’s Hospital is adjacent to the historic site where the Westhampton school stood. When St. Mary’s Hospital opened in 1966, it was the first racially integrated hospital in Richmond. Bon Secours is part of Bon Secours Mercy Health.
Daisy Jane, now Jane Cooper Johnson, took part in a ceremony to bless the sculpture.

their newborns in rural southwestern Montana with its First 1,000 days program. The program follows a woman through her pregnancy, or 270 days, and for the first two years of her child’s life, or 730 days. Mothers are screened to connect them to services, treatment and other resources to ensure they can be healthy mothers to healthy babies. The program has meant fewer infants being born with a positive neonatal drug screen, more women receiving adequate prenatal care, and fewer newborns being removed by child protective services.
To assess needs, reaching out to communities and talking to the people helps. Bryan Slaba, CEO of Wagner Community Memorial Hospital in South Dakota, affiliated with Avera Health, told how his hospital struggled to reach people to gather information for a community health needs assessment. About 50% of its patients are Native American. The hospital was unsuccessful with town hall meetings or by approaching people coming out of the grocery store with questions. It found success in gathering members of local law enforcement, tribal law enforcement, and school leaders. It also put an ad in a local newspaper telling people their names would get put in a drawing for a $250 grocery store gift card if they filled out a survey, which drew 500 responses. The CHNA led to several actions, including hiring two full-time counselors for people with addiction and mental health issues, whereas before there was one counselor who worked a half day a week. “Did I have to put up some money for it?” Slaba said. “Yes. But that’s what I had to do to get people to come to the table.”

promoting a culture of openness and accountability.
9
10
Bon Secours Richmond and a partner together commissioned this public art installation called “Strides” to inspire people to reflect on the importance of racial integration. To see more pictures from the ceremony, visit chausa.org/chw.
8 CATHOLIC HEALTH WORLD March 2024
Nimble leaders succeed. Art delaCruz is a retired U.S. Navy instructor who taught at the Navy Fighter Weapons School, popularly known as Top Gun, and the chief operating officer of Team Rubicon, a nonprofit that uses military veterans to respond to disasters. He shared some key points about leadership, namely that effective leaders have a mindset of success and focus on controlling what they can, while discarding what doesn’t matter. He said that leaders should be willing to admit when they don’t have all the answers. They also should share their mistakes to prevent future failures,