Latest Version: 6.0
Question: 1
You are taking vitals on a one month old female and find that her heart rate is 160. Based on your knowledge of pediatric cardiac function, what do you do?
A. Hook the patient up to a 12 lead EKG
B. Immediately call the nurse
C. Call a code blue
D. Document as a normal finding
Explanation:
Answer: D
The normal heart rate of an infant up to 11 months old is between 100 and 170. Therefore, no immediate action is required.
Question: 2
You are called to the scene of a cardiac arrest. On arrival, you find a 55 year old male with a history of hypertension, COPD, and congestive heart failure, pulseless and apneic. His wife tells you that he collapsed about three minutes before your arrival. Your partner begins one rescuer CPR, and another paramedic on scene controls the airway. As you are applying your ECG leads, the patient’s wife tells you that she wants you to let him die in peace.
Which of the following would be most appropriate in this case?
A. Perform rescue breathing only, and contact medical control
B. Cease resuscitation only if the monitor does not indicate the presence of a potentially viable rhythm
C. Continue performing resuscitation efforts, and ask if the patient has a DNR or living will
D. Comply with her request, and cease all resuscitation efforts
Answer: C
Explanation:
The only time it would be considered appropriate to not provide ACLS interventions to a patient who does not have signs and symptoms of imminent death (i.e., rigor mortis, independent lividity) is if the patient or the patient's family has a legal document, such as a DNR or living will, that legally lays out what treatments should be initiated or withheld in the event of cardiac arrest.
Without the inclusion of a DNR or living will, resuscitation should be continued until deemed appropriate to stop. If the patient's family member continues to demand stopping resuscitation, the family member should be attended to by another rescuer or law enforcement can be contacted if needed. If there is any doubt, contact medical control for further direction.
Visit us athttps://www.certschief.com/nremt-paramedic/
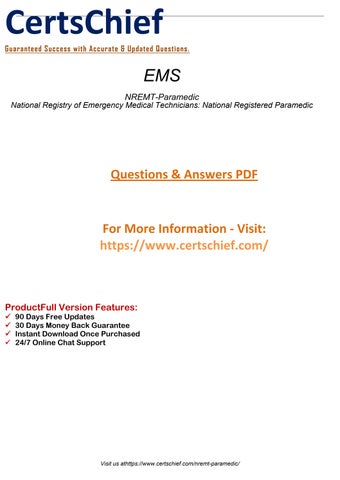
Question: 3
Identify the following artifact.
A. Artifact from defibrillation or cardioversion
B. Artifact from performing CPR
C. Baseline sway
D. 60 cycle interference
Explanation:
Answer: B
The chest compressions during CPR are picked up by the electrodes, resulting in an abnormal rhythm. Artifact from defibrillation/cardioversion, baseline sway, and 60 cycle interference are more irregular and bizarre than CPR artifact.
Question: 4
Which of the following incomplete spinal cord syndromes commonly occurs with hyperextension and/or flexion cervical spine injuries and presents with a greater loss of function in the upper extremities than in the lower extremities?
A. Central spinal cord syndrome
B. Anterior spinal cord syndrome
C. Brown Sequard syndrome
D. Posterior spinal cord syndrome
Explanation:
Answer: A
Visit us athttps://www.certschief.com/nremt-paramedic/
Central spinal cord syndrome presents with some hyperextension and/or flexion injuries of the cervical spine. The syndrome is characterized by greater motor impairment in the upper than lower extremities. The signs and symptoms of central spinal cord syndrome include paralysis of both arms with sacral sparing.
An anterior spinal cord syndrome patient would likely present with complete paralysis and decreased sensation below the area of the injury. There is no such syndrome as posterior spinal cord syndrome. There are only three classifications used: central spinal cord syndrome, anterior spinal cord syndrome, and Brown Sequard syndrome. Brown Sequard syndrome is a hemitransection injury. The classic finding involves weakness or paralysis on one side of the body or the other, depending on the direction of the spinal cord transection.
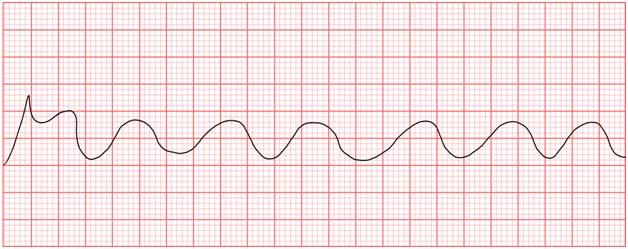
Question: 5
Calculate the heart rate of the rhythm strip.
A. 75 bpm B. 55 bpm C. 105 bpm D. 130 bpm
Explanation:
Answer: A
The heart rate can be calculated by dividing 300 by the number of large squares in between the R waves. The R wave is the highest wave noted on the EKG strip and is part of the QRS complex, which represents ventricular depolarization. On this strip, there are four large squares in between each R wave.
300 / 4 = 75
Question: 6
Sighing is a slow, deep inspiration followed by a prolonged expiration and is thought to be a protective reflex. Which of the following is it thought to prevent?
Visit us athttps://www.certschief.com/nremt-paramedic/
A. Atelectasis
B. Subcutaneous emphysema
C. Aspiration
D. Carbon dioxide retention
Explanation:
Answer: A
Atelectasis is an abnormal condition characterized by the collapse of lung tissue preventing the exchange of oxygen and carbon dioxide at the cellular level. Patients with the potential for this to occur, such as emphysema and rib fracture patients, may sigh to help keep the alveoli open at the end of exhalation.
Sighing does not prevent aspiration. The main preventive measure to protect our airways from aspiration is the epiglottis. Sighing is not considered a preventive measure for carbon dioxide retention. Its primary purpose is to allow a little air to remain in the lower air sacs to prevent alveolar collapse. Subcutaneous emphysema is an abnormal finding in pneumothorax. It occurs when air escapes the injured lung and accumulates in the tissue. It presents with the classic "rice crispy" sound and feeling when the injury is palpated.
Question: 7
You are called to assist a worker at a local fertilizer plant after he began experiencing rapid onset agitation, anxiety, confusion, and dyspne
a. During your assessment, his dyspnea increases with wheezing while his pulse rate decreases. Yet, he is found to be hypertensive without any history of high blood pressure. Which of the following would you suspect in this case?
A. Hydrocarbon exposure
B. Chlorine bleach irritation
C. Ammonia contamination
D. Cyanide exposure
Explanation:
Answer: D
Cyanide exposure, although rare, can occur in the presence of fertilizer and other chemical products used industrially around the U.S. Cyanide is a chemical asphyxiant that can cause a number of pulmonary and local effects when inhaled. These toxic systemic effects prevent the uptake of oxygen by the blood and can interfere with tissue oxygenation.
Ammonia contamination can cause local burns at the contact point, but it only causes local pulmonary problems if inhaled for a period of time. In severe cases of inhalation, bronchospasm may develop rapidly, but bradycardia and hypertension are not normal findings, especially in contact burn situations. Hydrocarbon exposure can happen accidentally, but most emergencies are related to patients purposely inhaling the hydrocarbons in an attempt to become intoxicated. Most hydrocarbon inhalation patients will present with euphoria and pulmonary congestion. They do not normally present with hypertension
Visit us athttps://www.certschief.com/nremt-paramedic/
and bradycardia as seen in cyanide inhalation. Chlorine bleach irritation typically involves the eyes and mucosal membranes. It does not usually cause bradycardia and hypertension.
Question: 8
You are called to the scene of a passenger car train derailment with possible injuries and/or fatalities. Once all services are on scene, who has the ultimate authority for all issues regarding patient care at the scene of the potential mass casualty incident?
A. Incident commander
B. Medical Branch Officer
C. EMS medical director
D. Senior or highest ranking paramedic on scene
Explanation:
Answer: B
For all issues regarding patient care, the EMS medical director has ultimate authority. However, the Medical Branch Officer is responsible for overseeing all emergency care provided at the scene. The EMS medical director is ultimately responsible for all treatments but is not available in most cases on the scene. Therefore, treatment officers make treatment decisions on the scene of a mass casualty incident. The highest ranking paramedic may be asked to be the triage officer, or even the treatment officer, in some situations. The paramedic would only make treatment decisions when he is the recognized treatment officer in the treatment area of the incident. Being the lead paramedic does not make it his right or responsibility. The incident commander leads all collaborations of the various divisions of the mass casualty incident. However, he does not make patient care decisions on scene.
Question: 9
All traditional means of clearing an obstructed airway have been exhausted, and your adult patient is quickly approaching cardiopulmonary arrest. As a last resort effort to save your patient's life, you decide to attempt ventilation through a needle cricothyrotomy. Where do you want to insert the catheter in order to ventilate the patient?
A. At a 90 degree angle in the sternal notch just below the cricothyroid membrane
B. Upward at the bottom edge of the first tracheal ring below the cricothyroid membrane
C. Downward through the tracheal ring just above the cricothyroid membrane
D. Into the midline of the cricothyroid membrane at a 45 degree angle toward the feet
Answer: D
Explanation:
After properly locating the patient's cricothyroid membrane, insert the cricothyrotomy needle into the midline of the cricothyroid membrane in a downward direction toward the carina. Never attempt to cannulate the trachea at any other level than in the midline of the cricothyroid membrane. The sternal notch is not an approved landmark for the procedure. It is not appropriate to
Visit us athttps://www.certschief.com/nremt-paramedic/
insert the needle in an upward direction. It would force any air you were able to get in, straight back toward the upper airway and the mouth, not toward the lungs as needed. Never insert the device into the tracheal rings above or below the cricothyroid membrane to prevent unneeded injury. If a cricothyrotomy kit is not available, a 14 or 16 gauge IV cannula may be used with a 10 mL syringe attached.
Question: 10
You hook a patient up to a 12 lead EKG and see a spike preceding the P wave. Based on your understanding of EKGs, you identify the cause as:
A. Multifocal atrial tachycardia
B. Atrial fibrillation
C. Atrial pacing
D. Wandering atrial pacemaker
Explanation:
Answer: C
A vertical spike preceding a P wave indicates the presence of an atrial pacemaker. The goal of a pacemaker is to maintain sinus rhythm in the patient's heart.
Atrial fibrillation, multifocal atrial tachycardia, and wandering atrial pacemaker are arrhythmias that distort the sinus rhythm
Visit us athttps://www.certschief.com/nremt-paramedic/