

16th Annual ACDIS Conference
Poster Presentations

Eventhoughtheyarenotusedfor finalcoding,inpatientradiologyrecords provideimportantclinicalindicatorsforCDI specialiststoformqueries. Radiologydocumentscanbetediousto review,andtheirduplicativenatureincreasesfalse positivesinevidence,decreasesaccuracy,and overwhelmsendusers.

Demographics


detailsRadiologicabout procedure










ThereisincreasedCDIinterestinusing radiologyevidenceasclinicalvalidationforquerieswhen radiologydocumentationisnotaddressedbythetreating provider.
Howdoweunderstandandutilizeradiology documentsefficientlyandoptimally?
Weidentifiedkeypointswithinradiology reportsthatarerelevanttoCDIandallowmeaningfuldata extractionandstreamlinedqueries.

Observations ofbody systemsfrom study



Interpretation of observations incontextof indication



Suggestions forfurther medical treatment




hundredsofclinicalrecords.Contents variedbyorganizationandexamtype,but comparisonrevealedageneralstructureand sectioning.
whichsectionsneededtobe includedandexcludedforclinicalvalidationwithin CDIqueries.
radiologicsectionconstraints withinournaturallanguageunderstanding(NLU) logictoensurealldatapresentedisapplicable.



Constrainingsectionsincreasesefficiencytothe CDIprogrambyallowingfortargetedreview

Understandinghowtooptimizesupplemental documentationiscritical
Increaseddemandinradiologyservices=large potentialforfutureCDIimpact
NLP vs NLU: Augmentation to the CDI Workflow
Josh Amrhein, MHASovlentum Health Information Systems Murray, Utah
Natural Language Processing
• Data science technology where “engines” are designed to “read” narrative text to identify and tag specific words with coded values
Introduction
Artificial Intelligence (AI) has been known to assist in the Clinical Documentation Integrity (CDI) workflow(s).
Natural Language Understanding (NLU) is a subset of Natural Language Processing (NLP) which can be found to be used in the CDI workflow(s). Many misconceptions are made between the difference of NLU vs NLP. While both bring benefit(s) to the CDI specialists, such as increased productivity, there is a difference in how the two function. NLU capture can be through explicit documentation, clinical evidence or both whereas NLP capture is text, but doesn’t build on the “clinical” evidence within the encounter like NLU.
Bringing AI to Success
Such challenges to overcome include the following:
• A lack of understanding about what a particular type of AI technology can or cannot do;
• A lack of clear strategies for integrating different AI technologies into the existing care systems to effectively solve the most pressing challenges that health organizations currently face;
• A shortage of a well-trained workforce for AI implementation;
• The incompatibility of AI technologies with legacy infrastructure; and
• A lack of access to good and diverse medical data for training Machine Learning (ML) algorithms/models.
Example:
• Used to convert a blob on text into computer understandable structured data
• NLP engines are built for specific purposes, are not widely adaptable –changes to the encoding logic require reprogramming
• Real-world examples include Computer Assisted Coding (CAC), online chatbots, and auto-generated keyword tabs
Natural Language Understanding
• NLU = NLP + Clinical Reasoning
• Designed to provide machine reading comprehension, wider adaptability
• Extend NLP codes with semantic meaning
• After NLP code markup, NLU engines apply reasoning and comprehension based on clinical concept rules, tested against robust gold standards data sets
The patient is a 60-year-old male with heart failure and shortness of breath. BNP is 600pg/ml. Echocardiogram shows EF 20%.
Conclusion:
NLP captures the text of “heart failure” whereas NLU uses the documentation of “shortness of breath, BNP result, and EF, to be able to produce the opportunity for further clarification of heart failure. The use of NLU in the CDI workflow has been proven to aide in increased productivity of CDI specialists. NLU technology is meant to augment the CDI workflow, but not replace necessary critical thinking of a CDI specialist.

THE WINGS OF TRANSFORMATION TO CDI EXCELLENCE TRANSFORMATIONAL CDI
BACKGROUND

“Embrace the whispers of change for they hold the secrets of tranfsformation.” Anonymous
RECOGNITION RECOGNITION/ENGAGEMENT

LEARNING GAMES: Trivia*Jeopardy*Kahoot*Slido*contests

Poster Presenter-2022, 2023,2024
ACDIS Virtual Conference Speaker-2024
ACDIS/MAHIMA/NYHIMA Speaker-2023
ACDIS

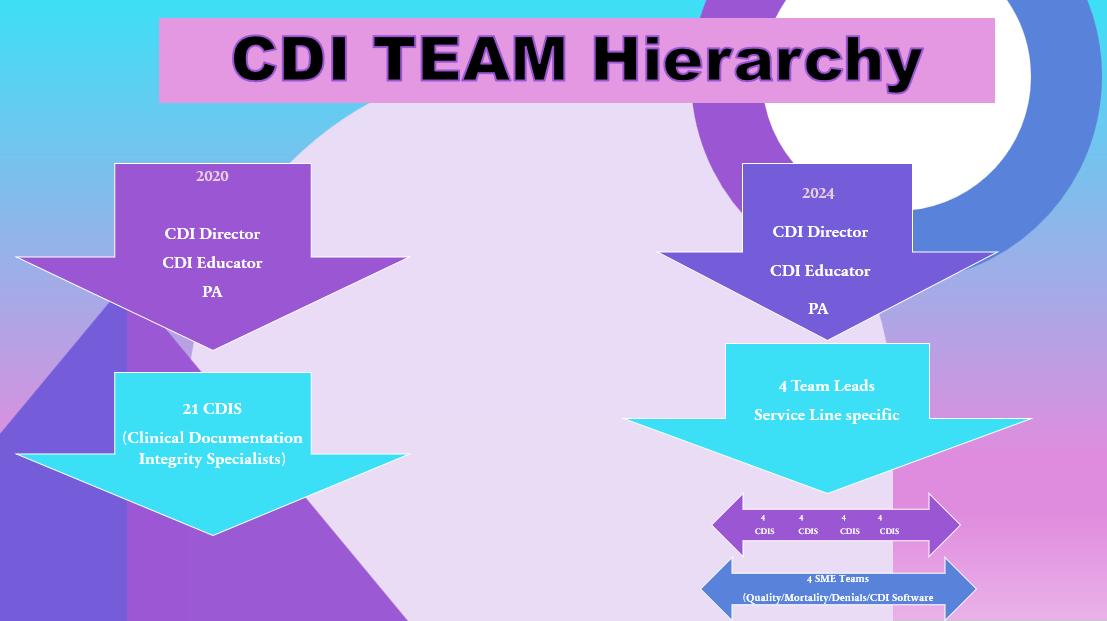
BIDMC began an RN, Pipeline Program-2017-2020 21 RN’s-Interviewed, Entrance Exam and went through a rigorous CDI training program, in multiple phases. All of the nurses went through internal CCDS training (following 2 years in the CDS role) and received their certification (CCDS).
Over the years, the CDI Team has been educated in CDI & Coding service line specialties, and training in SME teams included; Mortality, Quality, Denials and IT/CDI software.
The CDI Team has transformed from Novice to Expert, through advanced education, internally, as well, as external consultants, with multiple innovative strategies and process improvement initiatives through structural and functional changes.
“We delight in the beauty of the butterfly but rarely admit the changes it has gone through.” Maya Angelo

FOR GROWTH & TRANSFORMATION












CDI and Quality Team up to Impact PSIs
Clinical Documentation Integrity teams up with Quality for Patient Safety Indicator Case Reviews
INTRODUCTION
It was determined that a collaborative approach to PSI identification, reporting and review would be beneficial.
PSI Team includes: Quality, CDI, Coding, Wound Care and Physician Advisors. Ad Hoc members: Nursing Services
PSIs being monitored: PSI 90
• PSI 03 Pressure Ulcer Rate
• PSI 06 Iatrogenic Pneumothorax Rate
• PSI 08 In Hospital Fall-Associated Fracture Rate
• PSI 09 Postoperative Hemorrhage or Hematoma Rate
PROCESS
Development of PSI Team
Requested one team member from each facility to become a resource person
Educated the resource team member on PSI definitions, software identification and exclusions.
Utilized resource team members in the education process for the entire CDI team.
Education included:


• PSI 10 Postoperative Acute Kidney Injury Requiring Dialysis Rate
• PSI 11 Postoperative Respiratory Failure Rate
• PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate
• PSI 13 Postoperative Sepsis Rate
• PSI 14 Postoperative Wound Dehiscence Rate
• PSI 15 Abdominopelvic Accidental Puncture or Laceration Rate
Developed a concurrent and retrospective chart review process.
Meet weekly to review PSI cases and outcomes
• PSIs/identification/resources/notification process
• Increased staff awareness of PSI
• Utilize technology in our CDI tool for PSI identification
• Reporting/notification process
• Working with other departments on documentation
PSIs flagged in our data system are reported to the CDI Lead Analyst for a second look review.
RESULTS
PSI 3: Wound care has been part of the committee since the beginning. Pressure ulcer reviews involve the Director of Wound Care on all PSI 3 or potential PSI 3 cases. Wound Care nurses are responsible for documenting stages.
PSI 9 has been the most avoided due to the anticoagulant contributing to bleeding query. D68.32 code addition. Confirmed with AHRQ that coagulopathy does NOT need to be POA.
PSI 11 post op respiratory was greatly affected by developing a network wide definition of respiratory failure, query clarification and physician education. Improvement in our O/E ratio in all facilities and service lines.

This process includes consistent focused provider education from both CDI and Quality regarding PSI and clinical documentation. Resulting in increased capture and reporting accuracy of all PSIs being monitored.
RESULTS


All cases are reviewed by CDI, Quality and Coding as needed to ensure that no opportunities are missed.
Feedback is utilized to provide ongoing education to all departments.
Utilize our technology reports to confirm all identified PSIs are reviewed concurrently.
Placed a hard stop on all final coded cases with identified PSIs for retrospective review, to ensure a 100% review rate.
Notifications: the # of PSIs flagged in our data system and reviewed.
Avoided: PSI which were appropriately excluded from our PSI metrics through our combined chart review process, query clarifications and coding validation reviews.
With improved documentation integrity the result is improved quality metrics, case management, patient outcomes and appropriate revenue support.



Optimized DRGs by Length of Stays- Collaboration between CDI and Case Management
Lourdes A. Cacanindin, MD-FMG, CCDS Sutter Delta Medical CenterIntroduction
Length of Stay [LOS] became a critical priority and continues to be one as the need for optimization of the DRGs Length of Stay key for health care organization. Incorrectly placed patients end up at the wrong level of care and /or being treated by clinical staff who do not specialize in their condition that can lead to slower recovery times and even clinical complications. Getting the right patient to the right bed at the right time can reduce LOS and CDI Specialist can help maximize and optimized the DRG’s length of Stay by helping case management in identifying comorbid conditions which can impact DRG assignments at the time of admission up to the time of discharge.
1. To be able to show how the collaboration between Case Managers and CDI Specialist impacted the Length of Stay- AMLOS and the GMLOS from the time of admission to the time of discharge.
2. To identify the Operators involved and their respective roles in this collaboration
a. Clinical Documentation Specialists
b. Case Managers
c. CDI Physician Advisor and Hospitalist
d. CDI Director/ Supervisor / Lead
3. To be familiar with all the tools used to identify the Length of Stay- AMLOS and the GMLOS
a. EPIC
b. Clintegrity
c. Optum CAC Computer Assisted Coding
4. To have further discussion and collaboration with the case management department regarding LOS by ensuring proper patient placement and with the hospitalist’s identification of the proper diagnosis that necessitated a hospital bed.
5. To educate Case Managers regarding the CDI perspective on the importance of accurate interpretation of AMLOS and GMLOS (Show the impact of identifying the appropriate Principal Diagnosis, the Principal Procedures, and other comorbid conditions such as homelessness, type of depression, drug dependence, alcohol withdrawal.)
6. CDI can provide quick educational resources to Case Management using Coding Clinics / Coding Guidelines and the use of our Sutter Health KDS [know, Do, Share] of certain diagnosis.
7. To show the harmonious collaboration of the CDI Specialist with the Senior Case Managers.
8. To finally show some sample of the cases that has Optimized DRGs by Length of Stay Impacted by the CDI Specialist
1. All CDI Specialists and Case Managers/ Coordinators who want to collaborate with CDI Specialist on this regard.
2. All CDI Managers and Case Manager Supervisors who actively engage in such Collaboration
3. All Providers who want to improve their proper documentation to enhance the impact of the DRG’s Length of Stays
The Top 12 Optimized DRGs by Length of Stay as Impacted by the CDI Specialist Reviews and CDI queries done were identified in this chart within the month of October 2023 as an example to show the parameters used as follows:
1. Total Days added to the GM- LOS
2. Number of Accounts Impacted
3. Average Days added per Account

COLLABORATION BETWEEN THE CASE MANAGERS, OUR PROVIDERS AND THE CDI SPECIALIST IMPACT THE APPROPRIATE REDUCTION OF THE LENGTH OF STAY OF INPATIENTS

Manager
• Helps determine the correct Level of Care and communicates with the CDI Specialist the possible initial condition that necessitates the case admission.
• Helps determine the correct placement of patients and monitors the assigned LOS that corresponds to the possible DRG assignment by the CDI specialist reviews done up until possible discharge dates.


CDI Specialist
• Helps in Optimization of the DRG’s Length of Stay by assigning Initial DRG upon admission which is communicated to the Case Managers thru EPIC
Continuously work on the Possible DRG assignment with corresponding Length of Stays by identifying all the appropriate comorbid conditions noted until the time of Discharge


Providers
• Gives the appropriate specialized care to the patients for all the identified comorbid conditions upon admission and throughout the inpatient stay
Promotes faster recovery times without clinical complications cognizant of the Length of Stay assigned to the case.






Conclusion
In conclusion, “Getting the right patient to the right bed at the right time” with the collaboration of the
Evaluation
Give the audience a quick 3 question survey to access their knowledge and their awareness of their own facilities’ Average Length of Stay / Hand them some quick tips on how to perform an effective and efficient collaboration/ Engage audience with one-on-one conversation regarding the approach to this collaboration between CDI Specialist, Providers and Case Management Department

Addressing CDI Challenges: A Guide on How to Handle The Problem List
AHIMA
“Well-designed problem lists provide important information for patient care and support meaningful use requirements and health information exchange. While there are many approaches to a well-designed problem list, the key is to define clear policies and procedures that support your organization's objectives in using the information in a problem list.”1
• Is editing permissible by roles other than independent licensed professionals?
• Are the roles specified?
• Is it clearly stated in the institution’s privileging policy?
• What is the authorship?
The CDI Goal as it Pertains to the Policy
• Problem list accuracy
• Revenue protection of OIG/RADV targeted diagnoses
• Maximizing efficiencies in the BPA for 2024 RAF capture of re-certified conditions
• Identify education opportunities
The Policy
Problem List Policy Additions
I. Documentation in the provider encounter note:
• Encounter HPI, A&P, PE (amputations)
• Status code of amputation, stomas, GT in PE, in ROS
• Specificity in provider encounter, in the provider’s own words, within the body of the note
• Specialist note (on staff at institution), in the provider's own words, within the body of the note (i.e. secondary cancer, resolved cancer, diagnosis specificity, etc.)
II. ICD-10 Guidelines:
• DM ‘with’ where both conditions in same DOS but not billed with a combination code
• Old MI (>4 weeks)
• BMI measurement
• Status codes (i.e., AKA, GT, etc.)
Real-Time Examples ADDED as a Result of the Policy:
• Dementia
• Morbid obesity
• AAA
• Skin ulcers
• Morbid obesity
• History of breast/ prostate cancer
• CKD III, CKD IV
• Secondary cancer
• Dementia
• CVA with hemiparesis
• DM2 with CKD, with neuropathy, with PVD, etc.
3 Month Outcome with 13 Providers
Problem List Policy Deletions
I. Duplication
• Same diagnosis multiple times
III. Documentation in the provider encounter note negating an active event:
• I.e., ‘history breast cancer s/p lumpectomy in 2008, Anastrozole completed 2013’
II. ICD-10 Guidelines:
• AMI
• CVA
IV. Acute conditions moved in history:
• Fractures
• Sepsis
• AKI
• PNA
V. Unsupported diagnoses:
• Morbid obesity
• BMI
• Stage of CKD
Real-Time Example DELETED as a Result of the Policy:
• AMI, STEMI, NSTEMI
• Thrombocytopenia
• Acute Respiratory Failure
• Morbid Obesity


• PNA
• CVA
• Cancer
• Sepsis
• Fractures
• Morbid obesity
• DM2 with CKD, with neuropathy, with PVD, etc.


The Best of Both Worlds
Two Healthcare Systems Unite and One Best-in-Class CDI Program Emerges
Grand Rapids/Southfield, Michigan
 Elaine Koetje, BS, BSN, RN, CCDS, CRCR, CHC Manager, Clinical Assurance Program
Elaine Koetje, BS, BSN, RN, CCDS, CRCR, CHC Manager, Clinical Assurance Program
INTRODUCTION
Corewell Health is the success of Beaumont Health and Spectrum Health joining together to create a $15 billion organization with nearly 65,000 team members. Corewell Health’s CDI program has flourished during this integration by utilizing shared expertise across the East and West regions of lower Michigan. 2023 was especially successful as our legacy CDI programs joined forces to produce standardized query templates and developed processes and protocols to support system alignment.

INITIATIVES

 Jeanette Lyons, RN, BGS, CCDS, CRCR Director, Clinical Documentation Integrity and Coding Quality
Jeanette Lyons, RN, BGS, CCDS, CRCR Director, Clinical Documentation Integrity and Coding Quality
• Implemented a unified AI CDI Software tool
• Modified daily workflow processes
• Created system-wide Provider Query Policy
• Standardized query templates
• Streamlined Mortality workflow processes
• Expanded collaborative PSI process
• Broadened CDI educational offerings
• Annual CDI pocket guides distribution
• Aligned CDS productivity/query dashboard
• Enhanced CDI quarterly quality reviews
• Established Query Focus Group
Successful Outcomes






STRATEGY
All 98 CDI team members contribute to the success of our program. CDI successfully established cohesive partnerships while strengthening relationships across the healthcare system. Collaboration and engagement with other healthcare teams prevailed. CDI’s journey to bestin-class system metrics included: Coding, Coding Quality, Physician Advisors, Quality Safety & Experience, HIM, Compliance, Managed Care Contracting, Patient Financial Services, Senior Leadership, and Provider Leadership.





















Team Achievements










Optimizing Neuroscience Mortality Index: A Collaborative Approach
Yasmin Aghajan MD, Cheryl Codner MPH, BSN, Patricia Martin RN, BSN, Sandhya Prakash RN, BSN, Ronald Mendoza RN, BSN, Deborah L. Jones MSN, RN, Bradley J. Molyneaux MD, PhD
Background
Quality of care delivered Department
Why does mortality matter?
Mortality Index O:E
% Observed mortality
% Expected mortality
Gaps in documentation→ falsely low expected mortality and high mortality index
A. Expected mortality pre- and post- review

Aim & Hypothesis
Physician collaboration with CDI can identify commonly missed documentation opportunities and serve as basis for ongoing improvement in documentation practices, improving accuracy of neuroscience expected mortality
Methods
Neurologist Neuroscience CDI specialist
B. Expected mortality pre- and post-review by quarter
Results

D. Mean number of additional diagnoses captured per patient

Review neuroscience mortality charts for additional undocumented diagnoses present on admission that impact Vizient risk-adjusted expected mortality*
Additional queries Track expected mortality calculation pre- and post- review*
*Vizient
C. Most common additional documentation opportunities Mean expected

E. Mean number of additional diagnoses identified by physician reviewer

Conclusions
# Diagnoses affecting riskadjusted mortality increased from 4.3 to 7.8 per patient
Significant decrease in Vizient mortality index
F. Monthly Vizient Neurology & Neurosurgery expected mortality pre- and post-intervention
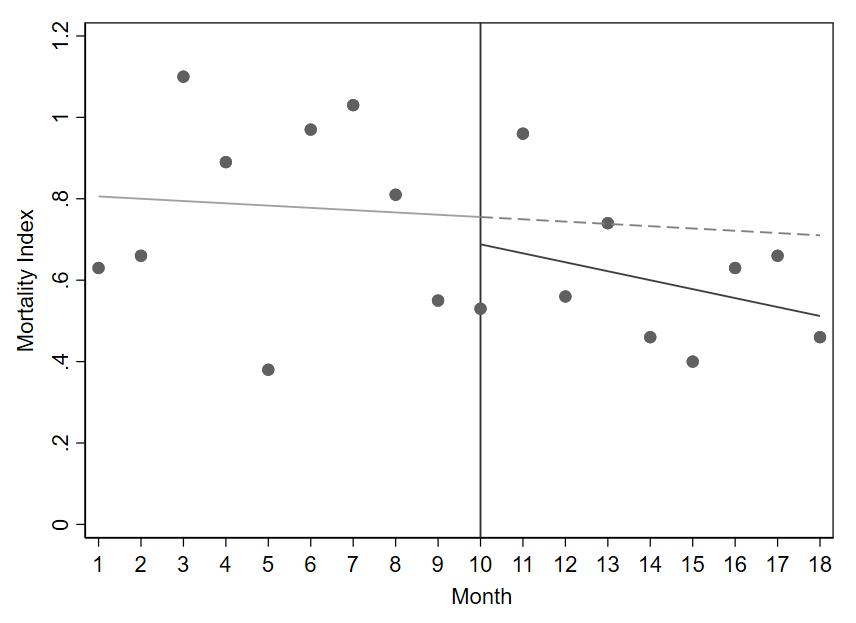
Collaboration between neurologists and Clinical Documentation Integrity (CDI) specialists to review documentation improves specialty-specific capture in neuroscience and increases the accuracy of neuroscience expected mortality.
Interrupted times series analysis demonstrates a significant decrease in neurology and neurosurgery service-line mortality index after the implementation of the intervention at month 10 (absolute decrease of 0.067; p<0.0001) with a continued decrease over time (slope change of 0.016 relative to preintervention slope; p<0.0001
References



THE ADVANTAGE of TECHNOLOGY


THE CDI STRATEGISTS

CMS’s Risk Adjustment model needs accurate patient data to predict statistics and reimbursement for health systems. The model uses diagnoses identified in Hierarchical Condition Categories (HCCs), and there must be evidence that these conditions are evaluated and managed by providers each year. In the busy ambulatory setting where encounters can easily number in the thousands annually, this information can be difficult to track, especially using antiquated systems, such as spreadsheets and different file folders. This sort of basic electronic data capture might be slightly better than paper charts, but still can be cumbersome and inefficient. CaroMont Medical Group implemented utilized technology in the following ways to assist with workflow:
OPTIMIZING A RISK ADJUSTMENT PROGRAM

Does your data currently reflect accurate HCC risk scores based on reported diagnoses for your patient population?
• Are all chronic conditions documented in the medical record at least once per calendar year?
• Do you capture HCC diagnoses in all care settings?
A Risk Score in the context of Medicare is a numerical value meant to denote the patient’s expected costs solely based on demographics and HCCs.
A risk score of 1.0 is the average expected Medicare patient’s score.



Workflow

Moving the metrics: I

• Identify High Risk Areas





Aggregates claims by patient for the past 2 years. Displays all ICD 10-CMs codes that went out on claims. Filters all codes previously billed in past years but not yet billed for current year. Uses technology such as Natural Language Understanding (NLU) to find evidence for diagnoses not yet sent out on a current claim, and displays to the user. Alerts CDI Specialists on gaps in clinical documentation. Allows the user to filter out most relevant diagnoses based on documentation. Shows gaps in risk scores remaining for the current year.
• Quality Data • Complete Documentation • Accurate Coding



& Patient Encounters
Functionality that allows for notifying providers Sends auto notifications to providers based on NLU output. Allows CDI specialists to request clarification from providers for certain diagnoses before a visit takes place. Nudges providers during note creation to improve the quality of documentation.
With the implementation of technological support to CaroMont Medical Group’s workflow, we were able to increase our benchmark risk scores by 6% overall, a notoriously difficult metric to move. Analysis IMPROVE RAF SCORE






• Data Analytics & Reporting
• Reduce Denials
• Increase Patient Safety Organization Goals
• Improve Reimbursement & Quality Metrics
An organization’s success with risk-adjustment depends on the ability to ensure accurate and complete documentation and coding. CDI programs are key touchpoints for closing the gaps in care by capturing compliant and accurate hierarchical condition categories (HCCs) and risk adjustment factor (RAF) scores to reflect the patient true and accurate clinical picture. Technology provides a process to improve risk adjusted documentation and coding through patient prioritization and real time physician nudges at the point of care. Solutions like this, along with a prioritized worklist that allows for filtering patients by risk scores, risk scores gaps, visits and diagnoses, can help provider organizations track their population from year to year.



Uses NLU to suggest ICD 10 CM codes based on completed documentation for particular visits, allowing medical coding staff to accept, modify or reject the output. Shows the HCC categories the ICD 10s are a part of.











Results By The Numbers

Increase in the number of
Viral Pneumonitis in Pediatric Patients: Is it Actually Pneumonia?
Pneumonia or Pneumonitis?
Children will present to the hospital with increased work of breathing, some critically ill, needing respiratory support. Chest x-rays show no evidence of pneumonia. No antibiotics are administered, just respiratory support. The physician’s diagnosis is viral pneumonitis. There is a growing debate among coders, auditors and clinical documentation specialists. RAC auditors are denying claims coded as viral pneumonia.
As of FY 2024, the ICD-10-CM Alphabetic Index made a simple, but significant change concerning pneumonitis.
Does this impact code selection?
Pediatric Viral Pneumonitis: What is it?
Inflammation of lung tissue
Occurs when irritant enters the lungs
Typically not contagious
Can affect breathing efficiency
Causes
Bacteria
Bird feathers/feces exposure
Certain antibiotics
• High doses of aspirin
Molds
• Certain anti-arrhythmia medications
Radiation therapy
Can be self-limiting
Pediatric Viral Pneumonitis Symptoms
• Shortness of breath
Decreased appetite
• Dry cough
Fatigue
• Unintentional weight loss
Children often present in respiratory distress with
RA saturations in the 80s, requiring NIPPV for support. Patients are usually weaned to HFNC then room air. No treatment with antibiotics is needed
Physician Documentation
Discharge Summary
Reason for Hospitalization
Noah is a previously healthy 4-year-old M admitted due to WARI and presumed viral
albuterol treatments. At time of discharge, illness more consistent with asthma
Please refer to H+P note for complete details of presenting illness.
Next steps for PCP
-Hospital follow up visit, repeat respiratory exam
-Ensure medications at home. Flovent (or Asthmanex) and albuterol
Pending Studies (Results not Final) (Last 100 days)
01/02/24 1119 Hold Tube Green Top – UCH MN Routine Ordered by an
Unspecified provider in process
Hospital
Do the official guidelines and/or coding conventions offer any direction?
Clinical Indicators and Imaging: Pneumonia vs. Pneumonitis
Pediatric Pneumonia
Infection of the lungs
• Wheezing
• Fever/chills
• Productive cough
• Difficulty/rapid breathing
Pediatric Pneumonitis
Inflammation of the lungs
• Dry cough
• Decreased appetite
• Fatigue
• Shortness of breath
• Unintentional weight loss


Physician Query & Response
Hi CDIS - My discharge summary note never mentioned “pneumonia” or implies bacterial pneumonia. I can’t control what the other notes from other providers say. This patient had an asthma exacerbation triggered most likely by a virus. The “pneumonitis” in my note means nonspecific inflammation of the lung. I don’t usually have to answer this type of compliance question for an asthma patient.
-----Message------
Subject: Coding Clarification
Dear Dr. Attending,
Pulmonology was consulted, recommended to start Flovent BID, continue albuterol PRN And follow up in Pulmonology clinic. Benefited from airway clearance with IS and flutter
-Completed 7 days of steroids
-Asthma education (asthma action plan) and inhaler teaching completed
-Prior to discharge, pt active and playful, appears comfortable, afebrile and eating/drinking well -Parents counseled on return precautions and understood to follow up closely with PCP
X-RAY CHEST 2 VIEW
CLINICAL HISTORY: Worsening respiratory status; And concern for developing pneumonia
Radiology Report
<LCI> COMPARISON: 1/2/2024 </LCI> FINDINGS There is increased perihilar, peribronchial thickening and interstitial prominence. No confluent airspace consolidation, pleural fluid, or pneumothorax. Heart size is within normal limits. test results are released to you at the same time they are released to your healthcare team. This means you may see these results before your healthcare provider has seen them. Your healthcare provider will review all of your results. If you have not heard from them or you have questions, please contact your healthcare team through MyChart or call your healthcare provider’s office during normal business hours.
IMPRESSION: Peribronchial thickening has increased without focal consolidation.
How is Pediatric Viral Pneumonitis Coded?
Alphabetic
Index FY 2023
Alphabetic Index FY 2024
Coding Conventions
A review of the medical record has identified a need for documentation clarification in order to meet compliance, accuracy of coding and severity of illness standards.
In the H&P and discharge summary, pneumo nia is documented. After study was completed, could you please clarify the type of the Noah’s pneumonia to the highest specificity known?:
- Aspiration pneumonia (please specify aspiration content, if known)
- Viral pneumonia (please specify virus, if known)
- Bacterial pneumonia (please specify bacterial agent, if known)
- Pneumonia, unspecified
- Other (please specify)
- Unable to determine
source: https://www.cms.gov/files/document/fy-2024-icd-10-cm-coding-guidelines-updated-02/01/2024.pdf

It Takes Two to Make a Thing go Wrong PSI 15 Abdominopelvic Accidental
Puncture or Laceration Rate v2023
LaKisha B. Richardson BSN, RN, CCDS, CCS, CRCR

V2022- The Old Numerator
✓ Any secondary ICD-10-CM diagnosis code for accidental puncture or laceration during an abdominopelvic procedure (TECHNI15D*)
✓ AND a second abdominopelvic procedure (ABDOMI15P* ) follows one or more days after an index abdominopelvic procedure (ABDOMI15P*)
Denominator
✓ Surgical (Appendix E: SURGI2R) or medical discharges (Appendix C: MEDIC2R ), for patients ages 18 years and older,
✓ with any ICD-10-PCS procedure code for an abdominopelvic procedure (ABDOMI15P*)
v2023- The New Numerator
✓ Any secondary ICD-10-CM diagnosis code for accidental puncture or laceration of a specific organ or structure during an abdominopelvic procedure (~15D *)
✓ AND a potentially related procedure for evaluation or treatment (~15P *)
✓ Performed, one to 30 days after the index abdominopelvic procedure (ABDOMI15P *), on an organ or structure related to where the reported accidental puncture or laceration (~15D *) occurred
✓ AND without a principal ICD-10-CM diagnosis code (or secondary diagnosis present on admission) for accidental puncture or laceration of a specific organ or structure (~15D*) that matches the organ or structure of the potentially related subsequent procedure (~15P*) described above
Denominator
✓ Surgical (Appendix E: SURGI2R) or medical discharges (Appendix C: MEDIC2R), for patients ages 18 years and older,
✓ with any ICD-10-PCS procedure code for an abdominopelvic procedure (ABDOMI15P*)



New Inclusion Criteria
✓ Requires specific organ or site of accidental puncture or laceration diagnosis code
✓ AND a requires a RELATED procedure code to evaluate or treat that specific site.
Example:
If code J9572 Accidental puncture and laceration of a respiratory system organ or structure during other procedure is coded, a RELATED procedure code within the DIAPHR15P * code set, such as 0BQR4ZZ Repair right diaphragm percutaneous endoscopic approach, would be required to qualify for a PSI 15.
New Time Frame
✓ Time frame now limited to "one to 30 days" rather than "one or more days" after the index abdominopelvic procedure
Examples:
Qualifying index procedure occurs on 12/01/23 and an accidental puncture and laceration code is also captured for K9171 Accidental puncture and laceration of a digestive system organ or structure during a digestive system procedure is coded. On 12/03/2023 a subsequent procedure, 0DQ73ZZ Repair stomach, takes place to treat the A&P. This will qualify as a PSI.
Same scenario, but with second procedure date of 01/04/24 changes the outcome. This will no longer qualify as a PSI 15 since > 30 days from index procedure.
What is the Impact?
✓ Fewer erroneous PSI 15s reported due to mismatching accidental puncture codes with unrelated second procedures not directed towards the treatment of an accidental puncture or laceration.
✓ Fewer erroneous PSI 15s on patients with long stay admissions.



Enter
Enter





Discovering opportunities to improve care team documentation through the expansion of computer assisted physician documentation tooling to other healthcare disciplines.
Megan Schneider MSN, RN, CCDS, CCDS-O, TaraJo Vaught MSN, RN, CCDS Solventum Health Information Systems, Murray, UT USAIntroduction
• Accurate documentation is crucial in all disciplines of healthcare to record and track patient information.
• Providers rely on accurate documentation from the care team when reviewing the record, placing orders, and determining the plan of care.
• Accurate records assist in data collection, tracking diagnosis patterns, quality outcomes, and risk management.
• Computer-assisted physician documentation (CAPD), an artificial intelligence (AI) tool, assists providers to accurately document diagnoses.
• Natural language understanding (NLU) allows technology to find meanings in different sentences
Conclusion
Real-Time analysis and monitoring
Proactive in-workflow notifications based on clinical context
Across the patient encounter
Identifies relationships and meaning between concepts
Detects gaps in documentation
Surfaces evidence for CAPD to send notification
REGISTERED NURSES
• Wound Type
• Wound Stage
• Wound Location
• Wound POA

• Intubation/Extubation time
• BMI
• COMA Scale
• Infusion times

SOCIAL WORKERS
• Social Determinants of Health
• Homelessness
• Social environment
• Psychosocial circumstances

REGISTERED DIETITIANS
• ASPEN Criteria
• Provider documentation of malnutrition
• Nutritional risk factors documented
Healthcare is an ever-changing system where technology and AI are at the forefront of countless vital advances, especially clinical documentation integrity (CDI). A focus point in CDI is complete and accurate documentation, thereby expanding the use case of current technology to include additional healthcare disciplines would achieve a most complete patient record. While ongoing research evaluates the use cases with CAPD technology, CDI specialists understand the importance of documentation within a multidisciplinary team that is invaluable to patient care.
KarenVakkas,MA,RN,CCDS,CCRN,AliciaWhite-House,BSN,RN,CCDS
INTRODUCTION
Likemanynon-clinicaldepartments,theClinicalDocumentationSpecialistsonour teamtransitionedfromhospital-basedworktoremoteworkinMarchof2020. Duringtheinitial18monthsofthistransition,therewasanaverageannual turnoverrateof24%.
Higher-than-usualturnovercauseddissatisfactionprimarilyduetoincreased individualproductivityquotas,continuousneedforpreceptorstoorientnew specialists,anddecreasedrevenuewhilenewteammembersweretrained.Exit interviewsexposedisolationfrompeersandperceivedlackofteamsupportas majorfactorsinfluencingthedecisiontopursuenewemployment.
Anexhaustiveliteraturestudyrevealedmentors,separatefromorientation preceptors,canhaveasignificantpositiveimpactonretentionrates.Using anonymoussurveys,specialistshiredafterthetransitiontoremoteworkwhodid notseeknewemploymentwereaskedtosharehowtheyfeltabouttheir orientationprocess.Answerssupportedthehypothesisthatembodyingasenseof teamworkthoughmentorshipwouldpositivelyimpacttheexperienceofboththe newhiresandtheexistingteam.
OBJECTIVES
Overallobjective:
Decreaseturnoverandincreaseoveralljobsatisfactionthroughexpansionofthe orientationprocesswithimplementationofamentorshipprogram.
Secondaryobjective:
SurveyCDIteaminordertoobtainabaselineanddetermineafocusfor interventionsandchanges.
Surveyquestionsincluded:
Isthereanythingthatshouldbechangedoraddedtotheorientationprocessthat wouldpositivelycontributetoanewhire’sexperience?
Respondentsanswered:
“Offermoreshadowingexperiences,specificallywhentheorienteeiscompleting thebootcampmodules,havetheorienteecompletethecardiacmoduleinthe morningthenpairtheorienteetoshadowaCDItoreviewacardiacchartonthe sameday.”
“Findopportunitiesfornewstafftointeractwithavarietyofstaff.Work relationshipsthatarepreviouslyestablishedcanbedifficulttonavigatefornew staff,especiallyduringinformalstaffgatherings,lookforopportunitiestobuild relationshipswithnewerstaff.Mentor(s)fornewstaffandensurestaffawarenessof whotheycancontactforquestions/concernsifmentorisout.”
“ItwouldhavebeenhelpfultoobserveexperiencedCDIsreviewseveralcharts forseveraldaystobetterunderstandtheirworkflowandthoughtprocesses regardingqueries.”
“Apeerpreceptor/mentorroletosupportnewstaffwouldbeinvaluable.This shouldbealeaderrecognizedrolewithtrainingonpreceptingandeducating adultsandfilledbysomeonewhoisoutgoing,supportivebynatureandwantingto beapreceptor.”
Duringthefirstfewmonths,howsupporteddidyoufeelwhenyouwantedorneeded helpfromothers?
Respondentsanswered: Verysupported–33% Somewhatsupported–50% Notverysupported–17%
Inthefirstfewweeksonthejob,didyouhavetheresourcesyouneededtoperform yourresponsibilitiestoyoursatisfaction?
Respondentsanswered:
“Ididn’tknowhowtousetheresourcesorwhentousethem.”
“Overallyes,butattimeswouldfeelunsurehowtoproceedwhenmeetingswere onlyscheduledoncedaily;feltalittleoverwhelmingtotrytoensureallquestions wereaddressed.”
“Iwasprovidedtoomanywrittenresources,itwaslikedrinkingoutofafirehose. Theywerenotprovidedorbrokendowninamannerandtimelinethatwas manageabletolearntheconceptsneededtoperformthejob.”
“Moreresourcesbecameaccessiblewiththerematchofthementor,which includedthesupportforthetransitiontotheremotenatureofthework.”
Ifhadmoresupportforquestions,Iwouldhavefeltmorepositivelyaboutmy orientationexperience.
Respondentsanswered:
Agree–71%
Disagree–29% Itwaseasytobuildrelationshipswithmynewcolleagues.
Respondentsanswered:
Onaverage,howquicklyareyouabletogetananswertoaquestionyouhave?
Respondentsanswered:
Itiseasytofigureouttheanswertoquestionshaveonmyown.
Respondentsanswered:
METHODS
Priortodevelopmentofthementorshipprogram:
Theorientationprocesswascompleteattheendofapproximately6weeks,and wasstructuredasfollows:
Weeks1-2:
ACDISBootCamp(online)todefinetheroleofCDIspecialistandprovide comprehensivetrainingontheirresponsibilities.
Uponcompletion,theCDISshouldunderstand:
•CodingandreportingrequirementsrelatedtoCOVID-19anditsmanifestations
TheICD-10-CMOfficialGuidelinesforCodingandReporting,asseenfroma CDIperspective
Diagnosesfrequentlyinneedofadditionaldocumentationtosupportaccurate codeassignmentacrossallmajorbodysystems
•Thevalueofcompliantproviderquerypracticeandbestpracticesassociated withthequeryprocess
•CoreprovidereducationconceptssuchasIPPSreimbursement, documentationintegrity,andqualitymetrics
•IPPSmethodologybasedonMS-DRGassignmentandtheimpactofdiagnosis assignmentandsequencingonhospitalreimbursement
•CDIbenchmarkingbasics,compliancerisks,andprofessionalethics
*InconcurrencewiththeACDISBootCamp,weeklymeetingswiththeCDI Educatoralsooccur.
Week3:
DailyMicrosoftTeammeetingswithvideo(60minute)withtheCDIDirectorto reviewcontentoftheICD-10Monitor“EssentialsforClinicalDocumentation Integrity:Acompleteresourcefordocumentationandcodingtomakechart revieweasy”.Meetingsalsoincludecasestudyreview.
Weeks4-6:
DailyMicrosoftTeammeetingswithvideo(60minute)withtheCDIDirectorto reviewcasesthatwerecodedbytheCDIspecialist.
*Dailymeetingsmayextendpast6weeksdependingonthequalityofthechart reviewand/orcomfortlevelofthenewCDIspecialist.
Uponcompletionoforientation,newemployeesbeginindependentchart review,withCDIDirectorsupportforquestionsastheyariseandforverificationof thequality,accuracyandcomplianceofqueries.
Additionally,theCDIDirector,CDIEducatorandCDISpecialistmeetjointlyat30, 60,and90daystoensureorientationbenchmarksarebeingmet.
Currentprocess:
Thementorshipprogramisimplementedaftercompletionoftheinitialorientation period.
Mentorselectionmethod:
Thenewemployeepartnerswithamentorafterdeterminingthetwowhomost closelyalignaccordingtotheirpersonalitystyleandclinicalbackground (*detailedbelow).
Thementorshipprogramisstructuredasfollows:
Weeks7-10:
DailyMicrosoftTeammeetingswithvideo(30-45minute)forthefirst2weeks.After theinitialtwo-weektimeframe,partnersmeettodiscussthefrequencyand durationofthemeetingsfortheupcomingtwoweeks,withoptionstodecrease toeveryotherdayorcontinuewithdailymeetings.Primaryconsiderationisgiven tothepreferencesofthenewemployee,basedonhisorhercomfortlevelwith independentchartreview.Theoptiontoextendthisprocessformoretimeisalso consideredpriortomovingontostep2.
Weeks11-14:
Beginsattheconclusionofthedaily/everyotherdayscheduledmeetingperiod): Touch-basemeetings,onaweeklybasisminimally,withon-demandaccessto mentorforquestionsviaTeamstextingfeature.Theoptiontoextendtheweekly meetingprocessformoretimeisalsoconsideredpriortomovingontostep3.
Week15andforward: On-demandTeamscallsortextingfeatureforquestionsastheyarise.
*Determiningpersonalitystyle: PersonalitystylewasdeterminedbyhavingallexistingstaffcompletetheDISC assessmenttool.Thistool,basedonpsychologistWilliamMoultonMarston'sDISC emotionalandbehavioraltheory,determineshowanindividualranksintermsof fourpersonalitystyles:Dominance,Influence,Conscientiousness,andSteadiness.

Determiningclinicalbackground:
Clinicalbackgroundwasdeterminedbypredominantpastworkexperience; medicalvs.surgical.
RESULTS
Inthetimeperiodafterinitiationofthementorshipprogram(September2022February2024),theturnoverrateinourdepartmentwasreducedfrom24%to 0%.
Thesurveyusedtoassesshownewemployeeswhodidnothaveamentor feltabouttheirorientationprocesswasalsogiventonewemployeeswho hadamentortoassesseffectivenessoftheprogram.
Surveyresultsbeforeandaftertheprogramwasinitiated: Howsupporteddidyoufeelasanewemployee?
CONCLUSIONSANDNEXTSTEPS
Conclusions:
OurmentorshipprogramwasdevelopedandinitiatedinSeptember,2022. Sinceimplementationofthementorshipprogram,ourdepartmenthasadded sixnewteammembersandhashadnoturnover.
Surveyresponsesbeforeandafterimplementationofthementorshipprogram validateditspositiveimpactonnewemployeesinthefollowingareas:
Teamsupport
Experienceasanewemployee
Easeinbuildingrelationships
Timetoresponseforquestions
Independentproblem-solving
Limitations:
InAugust,2022,hospitalhierarchywasrestructured.Duetothechange,our CDIDepartmenttransitionedfromreportingthroughtheQualityDepartment toreportingtotheRevenueDepartment.
Additionally,thistransitioncombinedCDIspecialistsfromfourdifferentteams undersingularleadership.
Potentialimpacttoemployeeturnoverduetothischangeispossible.
Ifhadhadmoresupportforquestions,wouldhavefeltmorepositively aboutmyexperienceasanewemployee.
Itwaseasytobuildrelationshipswithmynewcolleagues.
Onaverage,howquicklyareyouabletogetananswertoaquestionyou have?
AnewCDIDirectorwasappointedinOctober2022.
Potentialimpacttoemployeeturnoverandretentionbeforeandafter transitiontonewleadershipispossible.
Modifications:
Intheinitialphaseofourprogram,mentorscouldbechosenorcould volunteerfortheprogram.
Incomparisonwithmentorswhovolunteeredfortheprogram,thosewho werechosenreportedlesssatisfactionwiththeprocess.Further,new employeespairedwithmentorswhodidnotvolunteerreportedlesspositive impactontheirorientation.
Subsequently,onlymentorswhovolunteertoparticipateintheprogramare consideredforselection.
REFERENCES
Andersen,T.,&Watkins,K.(2018).Thevalueofpeermentorshipasan educationalstrategyinnursing.JournalofNursingEducation,57(4), 217-224.
Chen,C.M.,&Lou,M.F.(2014).Theeffectivenessandapplicationof mentorshipprogrammesforrecentlyregisterednurses:Asystematicreview. JournalofNursingManagement22(4),433-442.
Fox,KathyC,R.N.,M.S.N.(2010).Mentorprogramboostsnewnurses’ satisfactionandlowersturnoverrate.TheJournalofContinuingEducation inNursing,41(7),311-316.
MarshallM.&GordonF.(2010)Exploringtheroleoftheinterprofessional mentor.JournalofInterprofessionalCare,24(4),362–374.
Persaud,D.(2008).Mentoringthenewgraduateperioperativenurse:A valuableretentionstrategy.AORNjournal87(6),1173-1179. Raymond,J.M.,&Sheppard,K.(2018).Effectsofpeermentoringonnursing students’perceivedstress,senseofbelonging,self-efficacyand loneliness.JournalofnursingEducationandPractice,8(1),16-23. Slowikowski,M.K.(2005),UsingtheDISCBehavioralInstrumenttoGuide LeadershipandCommunication.AORNJournal,82,835-843.
CONTACTINFORMATION
KarenVakkas,MA,RN,CCDS,CCRN
CDISpecialist,ClinicalDocumentationIntegrity
Itiseasytofigureouttheanswertoquestionshaveonmyown.
PennStateHealth kvakkas@pennstatehealth.psu.edu
AliciaWhite-House,BSN,RN,CCDS
CDIEducator,ClinicalDocumentationIntegrity PennStateHealth awhitehouse@pennstatehealth.psu.edu

