cchfnews
encouraging, equipping, and engaging Christians to live out the gospel through health care among the poor
SUMMER
2016
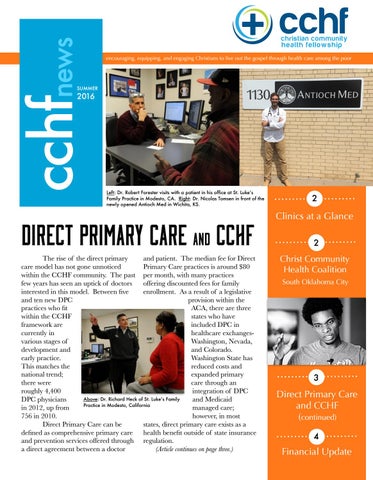
Left: Dr. Robert Forester visits with a patient in his office at St. Luke’s Family Practice in Modesto, CA. Right: Dr. Nicolas Tomsen in front of the newly opened Antioch Med in Wichita, KS.
2
DIRECT PRIMARY Care and CCHF
Clinics at a Glance
The rise of the direct primary and patient. The median fee for Direct care model has not gone unnoticed Primary Care practices is around $80 within the CCHF community. The past per month, with many practices few years has seen an uptick of doctors offering discounted fees for family interested in this model. Between five enrollment. As a result of a legislative and ten new DPC provision within the practices who fit ACA, there are three within the CCHF states who have framework are included DPC in currently in healthcare exchangesvarious stages of Washington, Nevada, development and and Colorado. early practice. Washington State has This matches the reduced costs and national trend; expanded primary there were care through an roughly 4,400 integration of DPC Above: Dr. Richard Heck of St. Luke’s Family DPC physicians and Medicaid Practice in Modesto, California in 2012, up from managed care; 756 in 2010. however, in most Direct Primary Care can be states, direct primary care exists as a defined as comprehensive primary care health benefit outside of state insurance and prevention services offered through regulation. a direct agreement between a doctor (Article continues on page three.)
Christ Community Health Coalition
2
South Oklahoma City
3
Direct Primary Care and CCHF (continued) 4
Financial Update
clinics at a glance Three hundred clinics nationwide are striving to deliver distinctively Christian healthcare to the poor. There’s almost always two or three dozen groups in various stages of development. Here are three clinics who are a valuable part of our community. Please offer them your prayer, counsel and encouragement.
SHAWNEE CHRISTIAN HEALTH CENTER louisville, ky
INNER CITY HEALTH CENTER denver, co
6,700 sq feet in Shawnee’s expanded facility, up from 2,800 sq feet. Plans to increase the number of staff from 20 to 35 and offer expanded services. The new space opened in August 2016.
School based health clinic in Jefferson County was established in the spring of 2016.
rochester, ny
1978 Dr. William Morehouse opened His Branches, one of the original 4 CCHF clinics.
79% of Inner City patients are uninsured. ICHC describes themselves as a “community funded safety net clinic”.
1st
HIS BRANCHES HEALTH SERVICES
2 Locations; the second site opened its doors in 2008. Last year the clinic began the planning process to become an FQHC.
1983 Jan & Bob Williams & Duane Claussen established ICHC in one of the poorest neighborhoods in Denver.
Contact:
Contact:
Contact:
Phyllis Platt
Kraig Burleson
Bill Morehouse
Christ Community Health Coalition About six years ago, seven people began to plant a church on the south side of Oklahoma City. The neighborhood is largely a medically underserved area, and three of the 7 were healthcare professionals. Thus, a vision for a medical home for the uninsured and underinsured was born in January 2015. The Above: Chauncey Shillow is involved with CCHC in OKC; goals are threefold: a medical home here pictured giving a CCHFx talk at Conference 2016. You can watch his poem, “Can You Help Me?” at cchf.org. for the neighborhood, health education & advocacy, and leadership development of indigenous leaders. Right now these goals are primarily accomplished through an after-hours pediatric clinic, a monthly adult clinic, and screenings within apartment complexes and charter schools. Christ Community Health Coalition is beginning their journey towards establishing a flourishing health center in the midst of a medically disadvantaged neighborhood. Please pray for them and offer your support!
Employment Opportunities Jobs are frequently posted on the CCHF website, and through social media. Take a look at some of our most recent postings. Pharmacist at Lawndale Christian Health Center (Chicago, IL) Pediatrician or Family Medicine Doctor at Baptist Community Health Services (New Orleans, LA) Assistant Nurse Manager at Christ Community Health (Augusta, GA) Licensed Vocational Nurse at Los Angeles Christian Health Center (Los Angeles, CA)
DIRECT PRIMARY Care & CCHF (Continued) At a GLANCE Dr. Nicholas Tomsen, a recent graduate of Via Christi Family Medicine Residency, recently cut the ribbon on his new practice, Antioch Med in Wichita, Kansas. Dr. Tomsen and Dr. Alleman co-founded the direct primary care practice with the intention to use medicine as a means for ministry. This new practice is just one example of a growing trend within the larger market. There are currently 7 different CCHF clinics from Seattle, WA to Madison, WI that utilize the DPC model. In addition to the traditional subscription-based “direct access” practices, there are several healthcare centers- such as St. Luke’s Family Practice in Modesto, CA- that offer a model where “benefactors” can subscribe to receive direct access to the physician group, and in turn, the doctors run a daily free clinic as a result of the financial support they receive from their paying patients. As with any novel model, there is no shortage of skepticism regarding direct primary care and its Above: Dr. Nicolas Tomsen with his youngest child at the Direct perceived effectiveness in reaching underserved Care Summit earlier this summer communities with Christ-centered healthcare. In multiple interviews with leaders in the CCHF community, leaders have expressed concerns regarding healthcare access. One prevalent concern is location, as one of the social determinants of health is access to transportation. Placement of practice location within economically disadvantaged neighborhoods eliminates a community barrier to quality healthcare. There are concerns that, because of subscribers’ wishes, practices would be necessarily located near more affluent neighborhoods where there may be more opportunity to gain subscribing patients. Another valid concern is in many states, government legislation prevents Medicare recipients from concurrently opting-in to Medicare and paying a subscription fee. While technically these Medicare patients can still become DPC subscribers, they are not able to submit fees for insurance reimbursement. This functionally eliminates an entire demographic from this model, a major negative as we look at the effectiveness of the DPC model to serve the underserved. Direct Primary Care practitioners are overwhelmingly positive, and even evangelical about the model. They believe that they improve patient outcomes & reduce costs by eliminating third parties. Dr. Farr Curlin of Duke University describes DPC as a “compelling model for people who want to practice good medicine and cultivate mutually respectful relationship with patients, where patients are invested in their own healthcare”. Indeed, the patient investment within the DPC model can be perceived a positive aspect, as patients who invest financially in their own healthcare may be more likely to trend towards proactivity and compliance. In addition, a crucial long-term challenge for the safety net is recruiting and maintaining physicians. The DPC model could be helpful in reducing physician burn-out by eliminating the bureaucracy of the third-party payer. The Direct Primary Care model has been rapidly expanding in the past few years. We need to seriously consider any model which allows the Kingdom of God to advance through healthcare within marginalized communities. As the CCHF community encounters this growing type of model, please offer them your prayers and support. After all, communities are made of diverse people, and the importance of the mission far exceeds any one particular model. Would you like to share your questions or experiences? Send us your comments!
Other pros and cons of Direct Primary Care
PROS: Excellent outcomes at reduced cost, including labs & medication
Providers not tied-down with government & insurance bureaucracy; cut free from meaningful use & QI metrics.
More time for extensive spiritual care & relationship, as providers need not see prolific numbers of patients daily.
CONS:
Excludes patients with government insurance.
Smaller patient panel per healthcare provider, which some argue takes doctors “out of the system” at a time of critical shortage.
There’s not much precedence that the model can offer scalable, sustainable healthcare to the underserved
Core Values -Supremacy of Christ -Prophetic Voice -Holistic Care
31%
34%
16%
-Justice -Reconciliation -Partnership
You are part of a movement of God’s people who, like the Good Samaritan, bind up the wounds of our poorest neighbors. We are an extension of you and the CCHF community, providing support and collective efforts so that this movement can stay strong and continue to grow. It is individual contributions – contributions of ideas, of prayer, of efforts, and of finance - that enable us to serve you and this community. We are grateful, and invite you to help us grow with this growing movement.
20%
Conference Registrations Organizations
Conference Sponsors Individual Donations
Encouraging, equipping, and engaging Christians to live out the gospel through health care among the poor.
cchf
Non-Profit Org
2595 CENTRAL AVENUE MEMPHIS, TN 38104
US Postage PAID Permit No. 534 Memphis, TN