Living at the height of wellness Winter 2017 | VOLUME 5, ISSUE 1
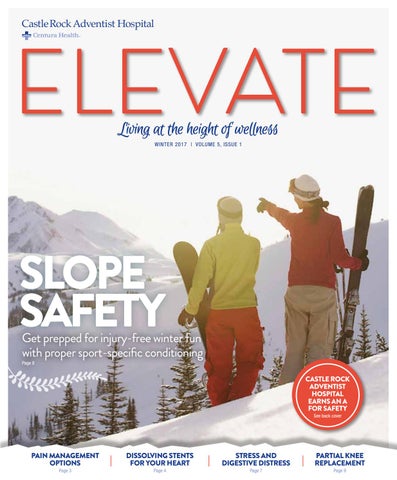
Slope Safety
Get prepped for injury-free winter fun with proper sport-specific conditioning Page 8
Castle Rock Adventist Hospital Earns an A for Safety See back cover
Pain Management Options Page 3
Dissolving stents for your heart Page 4
stress AND digestive distress Page 7
Partial knee replacement Page 9