IMMIGRATION UPDATE
The impact of Government’s latest measures
Substance abuse recovery
The power of communities
Pain management
Unlocking solutions with tech
Resource Finder
CQC compliance

JUNE 2024 www.caremanagementmatters.co.uk






Care Choices Ltd 3, Valley Court Offices, Lower Rd, Croydon, Nr Royston, SG8 0HF (01223) 207770 www.carechoices.co.uk Care Information Search for Care Blog Publications Useful Contacts Contact Us Details Features Care Choices is the reliable place to find the care that’s best for you and the information you need. Whether you’re looking for a care home or ideas on staying independent at home, this website has been designed to make it easy for you. ENHANCE YOUR PROFILE TODAY www.carechoices.co.uk 01223 206967 І paul.ocallaghan@carechoices.co.uk * Minimum booking period is 1 year. Price excludes VAT. For full details of opportunities to promote your service on the website, contact us. Promote your service to care seekers for as little as £5.76 per week*
Social
Care Insights
David Brindle reflects on how the sector has fared over the last decade, since the passing of the 2014 Care Act.
Inside CQC
Mary Cridge updates on the regulator’s new dementia strategy, shares how it’s listening to people receiving care and previews plans to support providers with medicines management.
CMM News
Into Perspective
Two industry leaders discuss how music can enhance wellbeing for people drawing on social care and the benefit to providers of training their workforce to use music in their settings.
Celebrating Excellence
CMM hears from Grant Newton, Head of Day Care at Alzheimer’s Support, who won the Dementia Care Award at the Markel 3rd Sector Care Awards 2024.
Event Review
CMM previews the What Next? 2024 ARCO annual conference, widely recognised as an agenda-setting event for the Integrated Retirement Community (IRC) sector.
What’s On?
Straight Talk
New Association of Directors of Adult Social Services (ADASS)
President, Melanie Williams, outlines her priorities for the year ahead.





Immigration law update: Assessing the impact
Sudipta Dey discusses the key implications for the sector’s workforce following recent changes to the UK’s immigration policy.
Supporting addiction recovery: The power of community
Robert York outlines the challenges facing providers of care services for people with an addiction, highlighting the importance of community engagement and best practice methods for achieving it.
Pain management in people living with dementia: Unlocking solutions
Dr Kreshnik Hoti discusses methods of assessing pain in people living with dementia and describes how one care provider has implemented digital technology to improve quality of life for the people it cares for.
What price a life? A call to raise fee rates
Clive Parry, Director at ARC England, explores the findings of the organisation’s latest Fee Rate Maps and reiterates ARC England’s demand for change.
Resource Finder: CQC compliance
Compliance is core to the successful running of an organisation. In this edition of Resource Finder, a series of expert organisations share how they can help you and share details on the services they offer.
CMM June 2024 3
REGULARS FEATURES 05 07 09 28 42 44 45 46
In this issue
38 30 18 23 30 35 38 18 35 23
EDITORIAL
editor@caremanagementmatters.co.uk
Lead Editor: Henry Thornton
Content Editors: Aislinn Thompson, Melissa Rumbold
PRODUCTION
Designer: Rebecca Mendil
Director: Lisa Werthmann
Studio Manager: Jamie Harvey
ADVERTISING
sales@caremanagementmatters.co.uk 01223 207770
Advertising Manager: Aaron Barber aaron.barber@carechoices.co.uk
Director of Sales: David Werthmann david.werthmann@carechoices.co.uk
SUBSCRIPTIONS
Sign up to receive the latest magazines and news for FREE. info@caremanagementmatters.co.uk 01223 207770
www.caremanagementmatters.co.uk
Care Management Matters is published by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2024 CCL REF NO: CMM 21.4

CMM magazine is officially part of the membership entitlement of:

CONTRIBUTORS

@DavidJ_Brindle
David Brindle Social care commentator and Chair, Ambient Support

Charlotte Miller Director and Founder, Intergenerational Music Making

Grant Newton Head of Day Care, Alzheimer’s Support @AlzheimersSupp

@CQCProf
Mary Cridge Director of Adult Social Care, Care Quality Commission (CQC)


@CQCProf Sudipta Dey Associate (Senior Immigration Advisor) –Employment, RWK Goodman @RWKGoodman

Robert York Director, Swift Management Services Limited
@PainChek @IMMmusicUK @LiveMusicNowUK
Douglas Noble Strategic Director of Adult Social Care and Health, Live Music Now UK

Melanie Williams President, ADASS and Corporate Director of Adult Social Care and Health, Nottinghamshire County Council @1adass

Kreshnik Hoti Senior Research Scientist, PainChek

Clive Parry Director, ARC England @ARCEngDirector
4 CMM June 2024 Are you getting the benefit of the CMM website? Sign up today to start getting more from CMM. It’s FREE for care providers.
www.caremanagementmatters.co.uk
Dr
SOCIAL CARE INSIGHTS
From David Brindle
David Brindle, social care commentator and Chair of Ambient Support, reflects on how the sector has fared over the last decade, since the passing of the 2014 Care Act.
Hard to believe, perhaps, but 10 years ago there was a lot of optimism around social care. The passing of the 2014 Care Act was widely welcomed as a new dawn because of the exemplary way it had been drawn up and agreed, its vision and values and its clear programme of action to address the sector’s challenges. The period since has been ‘a decade of disappointment’ in the words of Melanie Williams, new President of the Association of Directors of Adult Social Services (ADASS).
The brave new world envisaged by the legislation has failed to materialise thanks to relentless cuts in real-terms funding and postponement – perhaps now permanent shelving – of phase two of the Act which included reforms to relieve families of the terror of catastrophic care costs.
Missed opportunity
As we anticipate a general election and, judging by the polls and local election results in May, the likelihood of a change of government, will it be possible to recapture that optimism and even sense of excitement that so many people shared 10 years ago? Let’s recall those days. The Act was the product of careful and inclusive consultation that was widely praised and held up as a textbook model for future law-making.
Its focus on promoting wellbeing and
prevention, its recognition of the vital role of unpaid carers and their own support needs, its acknowledgement of the potential of ‘assetbased’ work in communities, drawing on their strengths, and its placing of adult safeguarding on a statutory footing – these were all seen as hallmarks of a new era in care and support.
The 2014 ADASS President, David (now Sir David) Pearson, who by coincidence was Williams’ predecessor as Director of Adult Social Care and Health for Nottinghamshire, hailed the legislation as ‘fantastic’ and a ‘great platform’ for care and support for the next 20 to 30 years.
Then dismay. There was to be no reversal of the austerity spending cuts made by the 2010 coalition Government in response to the banking crisis two years previously – and certainly not the investment needed to fund the Act’s implementation. The departure of the Liberal Democrats from government in 2015 significantly reduced pressure on the Conservatives to follow through.
By 2019, against a backdrop of £7.7bn savings by adult social care departments in England since 2009 and two postponements of the Act’s phase two, it was becoming painfully clear that the grand vision was not going to be realised. As that year’s ADASS President, Julie Ogley, remarked, ‘The reality of the current situation remains a distant stretch from the one imagined by the legislation.’

Cautiously optimistic
And there, by and large, we remain. Funding constraints continue to be so severe that only 6% of social services directors say they can be fully confident of meeting all their statutory duties under part one of the Act.
As for part two, enshrining a version of the individual spending cap and other reforms recommended by the Dilnot review in 2011, let’s just say there is technically a plan finally to implement it next year. But don’t bet on it.
So, will it be possible for people to start believing again? Labour’s vision of a National Care Service is intended as a rallying cry, but currently lacks detail and colour and would anyway take another 10 years to bring about.
In a new briefing ahead of the general election, the Nuffield Trust thinktank has sought to sketch in some of the particulars and has identified eight essential factors, ranging from parity with the NHS to workforce reform and fair fees for care providers. ‘At its best,’ it says, ‘social care gives people of all ages choice and control over where and how they live, underpinned by principles of wellbeing, prevention and dignity.’
Words and sentiments which could have come straight out of the 2014 Care Act. The tragedy is that for too many people, in too many parts of the country, they remain an aspiration.

CMM June 2024 5 Leeds Kirklees Derbyshire No inghamshire Warwickshire Worcestershire Cambridgeshire Norfolk Suffolk Hertfordshire Essex Buckinghamshire Northamptonshire Southend-on-Sea Bromley Kent Surrey East Sussex Brighton and Hove Bournemouth Christchurch Isle of Wight Poole Dorset Wiltshire Somerset Lincolnshire Blackpool Shropshire Berkshire North Yorkshire Gloucestershire Bedfordshire Luton Stoke-on-Trent Staffordshire Leicester Lancashire Blackburn Darwen Birmingham Cheshire East Oxfordshire Peterborough Bedford Leicestershire Rutland Hampshire Southampton Portsmouth The leading publisher of local authority care and support information Visit our website or call us on 01223 207770 to discuss how you can advertise your business to people looking for care and support in your area. www.carechoices.co.uk
David Brindle is a social care commentator and Chair of Ambient Support. Email: david.brindle@ambient.org.uk : DavidJ_Brindle
FamilyHub
An app for all family engagement needs which allows people to stay connected to their loved ones who are being cared for.
StaffHub

StaffHub provides care staff the ability to enhance operations by having visibility into reports, having live information on resident insights, updating families proactively and spending more meaningful time with residents.

MyHub
MyHub connects residents to the people in their lives that have an impact on their lived experience and daily wellness.

Enhancing your resident and staff experience
ResHub
new resident experience tool! Book a consultation today! personcentredsoftware.com 01483 357 657
with
Person Centred Software’s

Mary Cridge, Director of Adult Social Care at the Care Quality Commission (CQC), updates on the regulator’s new dementia strategy, shares how it’s listening to people receiving care and previews plans to support providers with medicines management.
Earlier this year we announced our intention to develop a cross-sector dementia strategy. In my last column I wrote about the ambition of the strategy and described some of the early conversations we’ve been having.
Our work continues and we’ve been having rich conversations with stakeholders across the health and social care sector. This is helping us to build a clear definition of what ‘good’ looks like when it comes to dementia care.
Capturing experiences
We’ve also been updating and adapting some of our tools, for example, SOFI. SOFI is our short observational framework for inspection tool. It’s used by CQC inspectors to capture the experiences of people who use services but who may not be able to express this for themselves.
We know it’s vital to clearly hear the voices and experiences of people living with dementia and those who care for them. One key element of the work we’re doing involves engaging with public stakeholders to make sure that any engagement we do is co-designed and effective.
I’ve been encouraged by the work we’ve done on this so far and am feeling confident that the ways we are planning to gather information from people will really help us to answer our central question of ‘How can CQC use its role to improve the experience of using health and social care services for people living with dementia and their carers?’
The work has helped us to identify the current state of dementia health and care from the perspective of those who are experiencing it. The team has worked closely with communities of people more likely to experience disadvantage or poorer health outcomes, or from communities whose cultural or language barriers significantly impact
INSIDE CQC
Mary Cridge
the ability of these groups to access dementia care. This helps us understand the current and pressing issues.
There are rapid and exciting developments in dementia research and treatment, and we have an opportunity to bring people, organisations and systems together to great benefit. I see the development of this dementia strategy over the next couple of years as a real opportunity to drive improvement across the whole health and social care sector.
Medicines management
Another area I’ve been focusing on recently is the challenges faced by adult social care providers in getting support for their medicines management. People who are supported by adult social care services often benefit from input from a range of healthcare professionals and providers, such as GPs, hospitals, pharmacies, councils and other providers. We all know that the safe and effective management of medicines is critical but that it can be challenging for care homes to get the support they need from the other agencies involved in a person’s care.
In February, we shared a survey with most of the adult social care providers in England. The survey has informed a study, the aims of which are to understand the support providers are receiving to ensure that medicines are managed safely, both from primary, secondary and other organisations such as ICBs and local authorities.
It also looks at where the gaps are in medicines support, and what impact those gaps are having on the quality of care delivered to people. Thank you to those of you who completed the survey – your insights have been hugely valuable.
We’ll be analysing the data closely and formulating a plan to support providers in the areas identified through this work. Areas like delegation of medicines administration tasks are particularly interesting – what can we do to support care home staff to access training to undertake delegated healthcare tasks and how would that free up capacity in systems?
It’s work like this that underlines for me the importance of working in partnership. Whether it's working closely with the people using your service and those who care for them in terms of making sure that their individual care plans best suit them and their changing needs, or across systems and sectors to create a supportive web of care for entire populations, connected working is key.

What is your experience of partnership working within your organisation? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
CMM June 2024 7
Care Quality Commission (CQC). Email: providerengagement@cqc.org.uk : @CQCProf
Mary
Cridge
is Director of Adult Social Care at the

The informative publication is focused on cost-saving solutions and is essential reading for operational leaders and purchase decision-makers in the social care sector.

In collaboration with @cmm_magazine @CareEngland www.caremanagementmatters.co.uk www.careengland.org.uk
ISSUE 3 Summer 2024
the latest issue Coming soon!
Click here for more information, and to read/download
LGA survey lays bare urgent action needed
Only around two thirds of councils are confident of being able to meet all their legal duties under the Care Act by next year (2025/26) – a decade after the Government introduced the landmark legislation designed to improve access to vital care and support.
This is despite eight in 10 councils forecasting having to cut spending on other community services – such as parks, libraries and leisure – in a bid to try and protect care services, according to a survey of councillors published by the Local Government Association (LGA) to coincide with the 10th anniversary of the Care Act receiving Royal Assent. This follows years of significant underfunding of adult social care services.
"The LGA is calling for immediate investment in adult social care to tackle the urgent issues affecting services, alongside a long-term care workforce plan."
The Act pulled together a patchwork of legislation on adult social care built up since 1948 placing duties on councils, including the need to focus on people’s wellbeing and ensure the provision of preventative services. However, the Act has coincided with a rise in people needing to draw on care and support and cuts to council funding that has left councils under increasing pressure to do more with less.
The LGA's new report – The Care Act 2014: Ten years on from Royal Assent – lays bare that the biggest issues facing adult social care are greater than just severe funding shortages. Responding councillors also pointed to challenges around recruiting and retaining the care workforce, more people with more complex needs and an inability to invest in preventative services to help people live independent lives and avoid the need for more acute care.
The LGA is calling for immediate investment in adult social care to tackle the urgent issues affecting services, alongside a long-term care workforce plan.
Ahead of a General Election, the LGA said all parties need to end the politicisation of adult social care, put the national interest first, and work on a cross-party basis at relevant points to secure the future of care and support so that people can live the life they want to lead.
In response to the findings of the new LGA survey, Cllr David Fothergill, social care spokesperson for the LGA, said, ‘The Care Act was a beacon of hope for those needing care and support, but this hope has faded. A decade on, people are still facing long waiting times for assessments and support, and not getting the full care and support they need.
‘We are at a critical point, for people who draw on care, councils and the sector. Councils are doing all they can to ensure they meet their duties under the Care Act – including cutting spending on other neighbourhood services – but many still fear they will not be able to over the coming years.
‘This simply isn’t good enough. It isn’t good enough for people who draw on care and support and it isn’t good enough for the care workers who work incredibly hard for very little financial reward.
‘Adult social care needs urgent attention. This must be top of the in-tray for any incoming government.’
Professor Martin Green OBE, Chief Executive at Care England, said, ‘LGA’s findings that almost one in three councils are no longer confident they can provide basic adult social care should set alarm bells ringing.
‘The precarious state of the adult social care sector as a result of a persistent workforce crisis and chronic underfunding has yet again been made clear, and still the Government continue to turn a blind eye to the evidence that is staring them in the face.
‘Our sector needs meaningful reform to be able to cope with growing demand. To ignore social care any longer is to ignore the nearly half a million people who receive care and support, and the 1.5 million people who deliver it: Government simply cannot continue to let these people down.’
To read LGA’s new report in full, visit www.local.gov.uk/publications/care-act-2014-tenyears-royal-assent
Achieve Together
Achieve Together, a provider of specialist support in adult social care, has announced two new appointments – Zak Houlahan as Chief Executive Officer and John Ivers as a Non-Executive Director. Zak has 20 years’ senior management experience, the majority of which has been spent providing essential services to the UK local authority network. John is an experienced and recognised health and social care leader, having worked in several executive roles. These include Chief Operating Officer at CareTech, Chief Executive Officer at Nestor Healthcare, Chief Executive Officer at Saga Healthcare and Chief Operating Officer at HC One.
Advance
National housing and support provider, Advance, has welcomed Tracy Lanes as its new Director of Support. Tracy has been appointed the role permanently following her time in an interim role that begun in August 2023. Tracy has already been instrumental in working with Advance colleagues to embed new processes that will further sustain the quality of services the organisation offers.
Langford Park Care Home
Langford Park Care Home, situated just outside Exeter in Devon, has appointed Ed Courtney as its new Home Manager. Ed will be responsible for the day-to-day management of the 35-bed care home as well as overseeing the substantial modernisation and refurbishment project currently underway. Ed has broad experience of all aspects of the care home sector. His first job at 16 was as an Activities Co-Ordinator in a care home, where he realised his passion.
CMM June 2024 9 NEWS
APPOINTMENTS
Cadbury partners with Alzheimer's Research UK
Cadbury has partnered with Alzheimer's Research UK to support the charity’s research for a cure. As part of the partnership, they are releasing ‘Memory Bar Boxes’. Memory Bar Boxes have been created following requests from care homes and dementia support groups to the Cadbury archives for packaging no longer in circulation to support with memory activities and to help in stimulating conversation.
Alongside Alzheimer’s Research UK, the business is working to create a nostalgic experience for those living with dementia, featuring iconic Dairy Milk bars, from as far back as 1915 until the present day.
The ‘Memory Bars’ form part of a wider package in the style of a memory box, which also features a digital download link, where people can find extra content, including classic posters and past packaging from other Cadbury products. The archive material tells the story of an iconic British brand, this year celebrating its 200th anniversary.
Alzheimer's Research UK supporter Layla Andrews, whose mother Karen was
diagnosed with dementia at the age of 64, said, ‘It’s really tough to see the impact dementia has on my mum. Mum struggles with technology, reading and writing and being able to recognise money which is tough given she used to be a bursar at a school. But she is still able to do so much like walking her dog and swimming. We also make time to connect and that is why this campaign from Cadbury is so important, as it gives us and others the opportunity to reflect on our shared memories over the years.’
Samantha Benham-Hermetz, Executive Director of Policy and Communications at Alzheimer’s Research UK, said, ‘We are so excited to be working with Cadbury on these Memory Bar Boxes, as part of our partnership. They are such a special way for people with dementia and their loved ones to reminisce together, and we’re delighted that thousands of people will benefit from them. Our partnership with Cadbury is also helping to put a muchneeded spotlight on dementia and driving forward Alzheimer's Research UK’s work towards a cure.’
Elise Burditt, Senior Marketing Director at Cadbury, said, ‘As Cadbury turns 200 this year, there has been great excitement in celebrating the longstanding relationship between the brand and the British public. 200 years of products that have become part of our culture in life moments big and small. As part of the celebrations, we wanted to answer special requests that had been coming from care homes, dementia support groups and members of the public over the years, for nostalgic Cadbury wrappers and posters, which could provide a sense of comfort and connection to those living with dementia.
‘Earlier this year, we announced our partnership with Alzheimer’s Research UK and released limited-edition Dairy Milk bars featuring iconic designs from 1915 to present day. And now those bars feature within these Memory Bar Boxes, which will be sent around the country to people affected by the condition. We are also donating £200,000 to support Alzheimer’s Research UK’s search for a cure for dementia and their work to drive awareness of the condition.’

10 CMM June 2024 NEWS NHS Transformation Directorate NHS ASSURED SOLUTION EveryLIFE_Technologies_Print Ad_Care Management Matters_186x110mm.indd 1 08/04/2024 11:27
New sustainability initiative
Elmfield Care has announced the implementation of a new sustainability initiative across all three of its facilities, becoming the first care home group in the UK to do so.
This programme eliminates the use of single-use plastic containers for commercial cleaning products used in housekeeping, laundry and kitchens. Previously, each Elmfield Care home generated an estimated 500-600 single-use plastic containers annually. By switching to The Plastic Solution, it is achieving zero single use plastic waste.
The Plastic Solution programme utilises a closed-loop system. Reusable containers with special air-sealed valve caps replace single-use options. Once emptied, these containers are collected and refilled at a dedicated filling plant, minimising plastic waste and
promoting a circular economy.
The staff across the three homes in Chippenham, Salisbury and Lydney are excited to be a part of the programme, recognising its positive environmental impact.
‘The Plastic Solution programme perfectly aligns with Elmfield Care's commitment to sustainability,’ says Sharon Kawonga, spokesperson for Elmfield Care. ‘This programme not only benefits the environment but also offers significant operational advantages.’
Chris Tapp, Co- Founder of the Plastic Solution, said, ‘We are delighted to partner with Elmfield Care, being the first care home group to adopt our unique zero plastic waste programme. Their commitment to driving this unique initiative across their estate is an admirable example to the wider care sector.’
NCA publishes new manifesto
The National Care Association (NCA) has published Our Mission to Level Up Care – A Manifesto for Social Care Reform
The NCA’s new manifesto aims to outline a comprehensive vision and plan for reforming social care in the UK. The manifesto emphasises how the next Government can work towards a sustainable future by tackling major challenges facing the entire care sector, not just services for older people.
‘Our social care system remains fragile with significant unresolved issues around regulatory changes and inconsistencies, workforce shortages, funding gaps, integration with health services and lack of data to drive efficiencies,’ said Nadra Ahmed CBE, Executive Co-Chairman of NCA. ‘We must take bold action to stabilise care and support services which are under
STUDY A MASTERS
Gain skills required for roles within healthcare practice settings, informal support settings, policy or business areas associated with ageing populations or undertake further research
immense strain from spiralling costs and an inadequate level of investment going back several decades.’
Key elements of the NCA's manifesto include:
• Securing £8.4bn in additional funding by 2024/25 to cover the full costs of providing care.
• Implementing regulatory reforms to reduce bureaucracy and enable more integrated care delivery.
• Launching nationwide recruitment and training initiatives to build a robust domestic care workforce.
• Improving data collection and analytics capabilities to increase productivity and quality.
• Greater partnership between the NHS and social care to provide seamless, holistic care.

Study online to gain an MSc Dementia Studies or MSc Gerontology and Global Ageing Our unrivalled expertise in dementia and ageing will help you expand your knowledge, support your professional development and advance your career prospects. • Study online and part time, to fit your studies around your professional or family commitments
We are home to the internationally renowned Dementia Services Development Centre •
•
Find out more: study@stir.ac.uk NEWS CMM June 2024 11
IN DEMENTIA AND AGEING
SC-WRES Improvement Programme open for registrations
The Social Care Workforce Race Equality Standard (SC-WRES) Improvement Programme has opened its registration process for 2024, offering a platform for addressing race inequality within the sector.
Statistics show that while 26% of the adult social care workforce comprised individuals from Black, Asian or minoritised ethnic backgrounds, managerial roles remain predominantly occupied by nonrepresentative demographics. Black, Asian and minoritised ethic staff constitute just 17% of registered manager roles and 17% of
senior management roles.
The SC-WRES serves to support local authorities in addressing race inequalities by asking them to record and submit annual data based on metrics made up of nine indicators, measuring the experiences of people from minoritised ethnic backgrounds.
Skills for Care is encouraging all parties to register by 30 June 2024 to benefit from the practice support sessions throughout July and August. The deadline may be extended until 16 August if interested local authorities need more time. There is no cost for local
authorities to register for programme in 2024.
Fiona Murphy, Skills for Care's Head of Culture and Diversity, said, ‘We're proud to be funding the SC-WRES Improvement Programme for the year ahead. SC-WRES is a powerful tool in achieving meaningful and sustainable organisational change towards race equality and telling the story nationally through the SC-WRES annual report.’
For further information on the SC-WRES Improvement Programme and how to book your place on an information and registration session, visit the SC-WRES webpage.
Local authority announces Caring Communities Commission
An ambitious commission which aims to address the increasing pressures on social care services has been announced by Essex County Council.
Councillor Beverley Egan will be the Chair of the newly created Caring Communities Commission. This will explore local and community-based solutions to social care pressures on public services. The commission will launch in the summer of 2024 and focus on early intervention and prevention to avoid
escalating needs and costs, and how residents could be supported in new ways to enjoy better health and access services in new ways.
Councillor Kevin Bentley, Leader of the Council, said, ‘Data on demographics and demands show us that we need to build on the existing work that we’ve successfully implemented in Essex such as the rollout of caring technologies to support people to live independently, age well and live at home or
Transform Health & Social Care Managment with Platinum6
with their families.
‘I am therefore delighted to announce the formation of our Caring Communities Commission. Instead of looking at how to pay the ever-growing cost of social care, this commission will find radical, community-based solutions to meet care needs in a cost-effective way. It will be informed by the expertise and experiences of frontline staff, care users and their families.’
Platinum6 supports Care Homes, Supported Living, Domiciliary, Disability & Palliative. More than a Care Planning system, built by Health & Social Care professionals, Platinum6 is a single web browser-based program with all you need included.
Free Business Intelligence Views, auto generated Quality Indicator Reporting, eMAR, HR, Education/Competencies, Continuous Improvement, Document Library, Forms/Report Builders, suppliers/stock/assets, nance, sta & resident/client & family Apps represent the form changes you make in real time.









12 CMM June 2024 NEWS DSCR APPROVED Contact us for a free demo: leecare.co.uk T: 07735 294745 | E: Annick.g@leecare.co.uk Follow us: @leecare_solutions
Florence launches agency manager tool
Staffing solutions provider Florence has launched Agency Manager, a tool that helps care providers optimise time and reduce agency spend by managing all their agency shifts in one place.
Florence – whose app connects open shifts directly with temporary staff –launched Agency Manager after customer feedback revealed the challenges of working with multiple agencies at once.
A survey of 37 UK care home managers showed providers currently spend nearly two full days (45 hours) a month filling 27
shifts using agencies, while contacting at least two agencies at a time per shift (all numbers on average).
Providers also commented on the difficulties comparing prices between multiple agencies, managing sometimes hidden extra costs (like staff travel or employers’ National Insurance), adhering to different invoicing schedules and working with staff with varying compliance standards.
Agency Manager matches qualified candidates to open shifts, removing the
Ridouts joins HCR Law
Specialist health and social care lawyers, Ridouts, has joined Top 60 UK law firm HCR Law's healthcare team.
Ridouts is a nationally renowned law firm known for its regulatory expertise. The firm acts for care homes, GP practices, children’s homes, dental practices, domiciliary and home care agencies, supported and independent living services and both private and NHS hospitals.
HCR law believes that Paul Ridout and his
team will complement HCR’s existing national healthcare operation. HCR advises a wide range of clients within the healthcare sector including adult social care, children’s services and a wide array of healthcare professionals.
Commenting on Ridouts joining HCR Law, Paul Ridout said, ‘We’re delighted to join HCR law’s established healthcare team. It’s clear to me that our values of client care and our shared focus on supporting the sector are a
need to reach out manually to multiple agencies. Florence’s compliance team verifies agency credentials to ensure only qualified and legally compliant candidates can be hired.
Dan Blake, Chief Operating Officer and Co-Founder of Florence, said, ‘Our Agency Manager platform has been meticulously designed with input from key customers, ensuring it truly delivers on filling shifts with the right people fast. We're eager to support care providers and panel agencies, enhancing the overall care experience.’
good match […] for healthcare providers who are looking to work with a different type of law firm.’
Rebecca Leask, Head of Healthcare at HCR, said, ‘We’re very much looking forward to […] being able to bolster our offering to existing clients of both HCR and Ridouts. Healthcare providers need access to the full range of legal services, from specialist experts who have a deep understanding of their unique needs.'
ACCREDITED & OUTSTANDING ONLINE SOCIAL CARE TRAINING FOR CARE PROVIDERS ACROSS THE UK DELIVERED BY ALTURA LEARNING


Endorsed by Skills for Care as a Centre of Excellence
• For quality online care courses, flexible delivery with bespoke membership packages, Altura Learning is your first choice.
• Helping our customers for over 20 years to build media rich e-learning training that supports blended learning for Adult Social Care services across the UK and Ireland
• Our unique and innovative approach uses best in class video-based content that reflects real life situations.
• A complete LMS solution that will support your compliance and reporting needs.
EXPLORE OUR COURSES TALK TO OUR EXPERTS

month’s trial when you mention you have seen us in CMM




CMM June 2024 13 NEWS
www.alturalearning.com | 01908 318990 FREE
Older people subject to adaptations delays
Two-thirds of local authorities took longer than the recommended six months to deliver an adaptation through the Disabled Facilities Grant (DFG), with the longest taking more than 24 months.
In a new report, Age UK calls for all local authorities to radically improve the way they deliver adaptations. The charity says an overhaul of the system is required to help older people to live independently for longer and reduce pressure on NHS and care services.
Age UK has published a report which highlights the delays many older and disabled people face waiting for councils to install home aids and adaptations, making it more difficult for them to live independently at home.
The report, A step change: improving delivery of the Disabled Facilities Grant says that increasing the amount of age-friendly, accessible housing and providing quicker access to appropriate aids and adaptations should be central to the UK's vision for the future of older people's housing.
According to Age UK, surveys consistently suggest that older people are keen to remain living independently at home. Accessible housing, aids and adaptations are key to this independence and give people the autonomy and confidence to live a full and active life. They are also important in reducing pressure on the NHS and social care services.
"Sometimes the delay is so pronounced that by the time an older person finally has the opportunity to explain what they want, the adaptation they requested is no longer relevant."
Adaptations such as walk-in showers and stair-lifts help to reduce falls, sustain better health, lessen dependence on others for care and ease hospital discharge.
However, in 2021/22, over two-thirds of local authorities took longer than the six months recommended by the DFG guidance, issued by Government, to install most adaptations through the grant. The longest took more than 24 months. These are average figures and so some individual
cases will have taken even longer. Age UK states there have been further delays since, due to a backlog of cases post-COVID.
There are several reasons for these lengthy delays, according to the charity, but many seem to come down to poor administration and customer service, and a lack of communication between local authority teams. The case studies included in the report set out a catalogue of unreturned calls, incorrect information and delay. Responsibility is often split between multiple busy local authority departments and cases fall between the cracks. Many adaptation teams are working to make their part of the process effective but admit to being severely stretched. Some teams have focused on making their administration of the Grant more efficient and are achieving much better results, proving this is possible, but in too many areas this hasn’t happened.
In April 2023, the Government announced an additional £102m of funding for the DFG. However, to get the most from this funding, the charity says it is crucial to get its local delivery right. The fund is run by local authorities and administration therefore varies from area to area. As Age UK has found, outcomes are very mixed. The budget for 2023/2024 is now £623m, almost triple the £220m budget seen in 2015/2016 and 8.7% up on 2022/2023.
However, with an ageing population and significant unmet need, this budget will have to rise further over the coming years, in the charity’s view. It knows that the number of people over 85 is forecast to almost double between 2020 and 2040, and in 2019/20, 53% of households that required adaptations did not have all the adaptations that they needed.
According to Age UK, many authorities have experienced problems with administering the DFG for some time. The charity also says that lasting improvements need to be made so that the huge potential benefits to older people of these funds are maximised.
Caroline Abrahams, Charity Director at Age UK, said, ‘Our report highlights the horrific delays older people often face when trying to get the adaptations they need through this funding. Sometimes the delay is so pronounced that by the time an older person finally has the opportunity to explain what they want, the adaptation they requested is no longer relevant,
because their health has declined to the point that they can no longer make use of it. In the meantime, while older people endlessly wait, they have to endure discomfort and inconvenience, and they may be at increased risk of falls. This is so frustrating when installing an adaptation could have made all the difference.
‘The Disabled Facilities Grant is one of the few sources of Government funding directed at supporting older people to live in their own homes which has actually significantly increased in recent years, and with public money so tight it’s crucial that we make best use of it. Speedy installation of the right aids and adaptations is not only good for older people, it can also pay back in terms of the savings to the NHS and social care from enabling them to stay fit and well.
‘We know that falls cost the NHS more than £2.3bn per year, with 30% of people aged 65+ and 50% of people aged 80+ falling at least once each year, so you can see how important home adaptations can be. Something as simple as a grab rail or a walk-in shower can make the difference between someone being able to remain at home, living independently, and having to move into a care home, at substantial cost to the taxpayer or to themselves if they have to pay their own fees.
‘We also need to improve the accessibility of our new and existing housing stock so there is less need for expensive adaptations in the first place. There is a massive shortage of accessible housing, and we should be making better use of new build and renovation work to provide more homes that can easily flex to meet our changing needs as we age.
‘Where adaptations are required however, many people will need to continue to rely on the DFG. Its delivery would be transformed if each local authority made a conscious effort to speed up the process, learning from the practice of the best. Better communication within local authorities and between them and older applicants is also essential. The frustration some older people experience when applying for this funding adds insult to injury. At Age UK we fully recognise that local authorities are underfunded and under enormous pressure, but that makes it all the more important that they make the best use of the money they do have.’
14 CMM June 2024 NEWS
Landmark social care data court case
Two Government departments have appeared in a landmark court case to avoid revealing social care data. Government agencies, HM Treasury and the Department for Levelling Up, Housing and Communities (DLUHC), have appeared in court against the Information Commissioner (ICO), with Access Social Care (ASC) as a second respondent, in a landmark court case for England.
"Government’s position is that social care is adequately funded but they are refusing to reveal their maths."
This landmark case happened due to the Government challenging a ruling by the ICO that it must disclose details around the decision-making process which determines funding for adult social care. ASC has stated that this will be a 'landmark court case for Government transparency and accountability in social care, as well as for the many families across the country who rely on adult social care'.
This case began when Freedom of Information requests were made by ASC to reveal data available to and used by policymakers in relation to decision making on social care funding. Both HM Treasury and DLUHC denied the requests.
These decisions to deny the request were then overturned by the ICO in July 2023, who ruled that disclosure was in the public interest and outweighs the arguments made by HM Treasury and DLUHC that it should be exempt as it is live Government policy.
Government then placed an appeal for this ruling, and that is what formed the latest court discussion.
Chief Executive Officer of Access Social Care, Kari Gerstheimer, said, 'The social care sector, including public bodies, charitable and commercial organisations, are all aligned that social care is critically underfunded. Government’s position is that social care is adequately funded but they are refusing to reveal their maths.'
It has been two years in which the two Government bodies in this case have refused to share information regarding how they reach the conclusion that social care is adequately funded, despite agreement from the ICO that it is in the public interest to do so.
ASC is a specialist legal rights charity working in the social care sector. Through its work ensuring people receive the social care they have a legal right to, ASC has seen that older and disabled people are denied that care every day.
According to the Association of Directors of Adult Social Services (ADASS), 434,243 people are still waiting for assessments, care and support, direct payments or reviews. In addition, Age UK estimates that 2.6 million people over the age of 50 in England are living with some unmet need for care.
The aim of this case was to reveal the decision-making that guides social care in this country, and how that process can be improved upon. ASC hopes that it will 'shed light on whether the Government is considering [all] relevant factors'. Keri Gerstheimer argues that, 'this case strikes to the heart of the need for Government transparency to enable good quality public decision making'.
IN FOCUS
Switching to decaf could save NHS £85m per year
WHAT’S THE STORY?
In a first-of-its-kind trial, care home residents were offered decaffeinated hot drinks in a bid to reduce falls experienced rushing to the toilet. A subsequent joint report outlining the findings has published by Care England, Stow Healthcare and University Hospitals of Leicester NHS Trust (UHL). The trial followed a similar initiative by UHL in 2021. Falls are the most common cause of injury-related deaths in people over the age of 75. People living in care homes are three times more likely to fall than those living at home; they are generally more frail, less mobile and have a higher prevalence of incontinence than the general population.
WHAT WERE THE FINDINGS?
Conducted across eight residential care homes over six months, the simple switch resulted in a 35% reduction in toileting-related falls. If scaled across the sector, the results would mean thousands of falls prevented and NHS savings of up to £85m per year.
Roughly 300 residents across Stow Healthcare’s eight care homes were given the chance to blind taste-test caffeinated and decaffeinated drinks. Over 90% of residents chose to take part in the trial after being told about the potential health benefits of making the switch, with the choice of caffeine always
available on request.
Over six months between June – November 2023, falls associated with care home residents going to the toilet dropped by 35%. With fragility fractures in social care estimated to cost the NHS £1.1bn per year, replicating these results across the sector could save £85m per year in prevented falls and hospital admissions.
WHAT DO THE EXPERTS SAY?
Professor Martin Green OBE, Chief Executive at Care England, said, ‘With a huge national focus on reducing pressure on the NHS, this pioneering trial demonstrates that simple solutions can help address enormous challenges. Care England is delighted to have been involved in this project and would encourage care providers across the country to give decaf a go.’
Ruth French, Director at Stow Healthcare, said, ‘The impact of a serious fall can have devastating consequences, and finding simple ways such as decaf drinks that might reduce this risk is groundbreaking. We hope it will inspire everyone in social care to take up the challenge.’
Sarah Coombes, Continence Nurse Specialist at University Hospitals of Leicester NHS Trust, said, ‘I hope that this will inspire other care providers to follow suit and to promote this simple change to improve patients' continence and reduce the risk of falls.’
CMM June 2024 15
NEWS / IN FOCUS
For more information about this trial and its results, read issue 3 of Care England's Savings, Solutions, and Sustainability publication, published in collaboration with CMM.
NEWS FROM ACROSS THE GLOBE
Gibraltar Alzheimer’s and Dementia Society fund workforce training
Health and social care staff across Gibraltar attended an innovative dementia palliative care course, delivered virtually by St Christopher’s Hospice. This course aimed to enhance the quality of care for individuals living with dementia. St Christopher's Hospice provided a bespoke course for Gibraltar which was funded by the Gibraltar Alzheimer's and Dementia Society (GADS).
The course has been designed to provide healthcare professionals with the confidence to support people with advanced dementia and their carers. Drawing upon evidencebased practices and the latest advancements in dementia care, participants have gained insights during the two-day course which included a focus on common symptoms, successful future planning, distressed and adaptive behaviours, emotional labour of
caring and communication.
Daphne Alcantara, GADS Chairperson, said, ‘The Gibraltar Alzheimer’s and Dementia Society is proud to have funded the first dementia palliative care course for health and social care staff in Gibraltar which will greatly benefit the lives of people living with dementia and their families.’
Karen Truman, Dementia Coordinator, said, ‘We are immensely grateful to the Gibraltar Alzheimer's and Dementia Society for their generous support, which has made this course possible. Their dedication to improving dementia care aligns with the Gibraltar National Dementia Strategy (2023-2028), and together, we strive to make a meaningful difference in the lives of those affected by this condition.’
Dr James, Palliative Care Doctor at St

Bernard’s Hospital, said, ‘We are thrilled to have launched this initiative that embodies our commitment to providing holistic care for individuals with dementia. This course represents a collaborative effort between healthcare professionals and community organisations, underscoring the importance of multidisciplinary teamwork in addressing the complex needs of patients and their families.’
Gibraltar Health Authority Director General, Mr Kevin McGee OBE IPFA, said, ‘This dementia palliative care course has been very popular, and demand has exceeded spaces available. This speaks volumes about the dedication of health care and social care professionals in Gibraltar, who deeply value the importance of enhancing the quality of life for individuals with dementia, to be able to provide compassionate and dignified care until the end of life.’
BCU professors help to drive critical care nursing in Zambia
International Nurses Day saw the celebration of two Birmingham City University (BCU) nurses on a mission to improve lives and champion change across the globe.
Professors Chris Carter and Joy Notter, the driving forces behind BCU’s Centre for Global Partnerships for Health, have worked in 12 countries over more than two decades. Their remit has always been to work with local partners to capacity strengthen nursing. Together, they’ve have worked with local partners in Zambia to transform critical care nursing. Over the last decade, the impact of their work in this country has been testament to the power of two people with a shared passion to improve thousands of lives:
• 400 nurses registered or in training by local partners: Two critical care nursing courses launched (advanced diploma and bachelor’s degree) delivered at three colleges, attracting students from Botswana, Zimbabwe and Lesotho.
• 700 nurses trained to safely administer oxygen: 76 ‘super trainers’ from 19
hospitals shared the training with 672 healthcare workers.
• Eight Zambian nurses mentored by UK practitioners: Nurses from five provinces spanning over 500 miles signed up for support, guidance and virtual networking through a mentorship programme with Livingstone University Teaching Hospital, Zambia.
• 1,600 nurses and healthcare workers trained during COVID-19: The UKRI/ Newton COVID-19 project spanned 18 months and supported the COVID-19 response in Zambia.
• 65 international volunteers engaged: Taking part in activities in-country and virtually, including online lectures, mentorship, peer reviewers and clinical assessment.
‘I’ve invested a decade of my life in Zambia,’ said Associate Professor Carter. ‘We’ve been in this together. My aim was always to be replaced. It’s good to take a

step back, it’s for the right reasons, but it’s hard to let go. Seeing 10 years, 20 cohorts of critical care nurses, shape their future is incredible. We’re still here, but we’re in the final chapter. The sustainability and hand over is crucial.’
Through the BCU Centre for Global Partnerships for Health, Chris and Joy manage a range of projects and partnerships across the globe including Vietnam, Romania, Malawi and Zambia.
Professor Notter, who holds a campaign medal for services to health by the Vietnamese Government, added, ‘We never do role substitution; it builds dependence and deskills. Our approach sustains practice. We aim to create something they own. It’s not ours. We give people confidence. We are now becoming mentors and peers, and rightly so. We’re not leading any more, they are.’
In 2023, the pair were awarded a BCU Knowledge Exchange Award for their instrumental work with Kanyama General Hospital in Zambia.
16 CMM June 2024 NEWS NEWS
NEWS


Nominate your laundry hero at washco.co.uk/lovelaundryawards Chat with us about your home’s needs today. 08000 546 546 washco.co.uk When it comes to laundry. We care too. You need reliable service and a provider that listens. You need to trust your equipment. You need WASHCO.

18 CMM June 2024

Sudipta Dey, Associate (Senior Immigration Advisor)
– Employment at RWK Goodman, discusses the key implications for the sector’s workforce following recent changes to the UK’s immigration policy.
The changes in UK immigration policy which were announced by the Home Secretary in December 2023 have now come into force. The aim was to regulate migration by prioritising the local workforce for suitable roles and providing them with necessary training. We have seen similar initiatives in the past, with the introduction of the Immigration Skills Charge, increased visa fees and salary thresholds for Skilled Worker visas, but figures have continued to grow.
The care sector has benefited from reduced rates to compensate for recruitment challenges after Brexit, when freedom of movement came to an end. This has led to record figures in net migration, and in some cases, abuse of the Skilled Worker visa route. The latest measures are designed to address these issues, but their effectiveness remains to be seen.
Some of the most relevant changes include raising the Skilled Worker salary threshold, revising migrants’ eligibility to bring dependants, replacing the Shortage Occupation List (SOL) with an Immigration Salary List (ISL) and raising the minimum income threshold for the family route, amongst others. There will be more changes for family members of British citizens, and fee increases in 2024, with a potential review or cancellation of the Graduate visa route.
What you need to know
Here are the main changes pertaining to the Health and Care Worker visa route:
• Dependants: As of 11th March 2024, migrants applying for Entry Clearance under the Health and Care Worker visa route cannot be accompanied by their dependants. There is an exception for migrants sponsored under SOC 6145 (care workers and home carers or 6146 senior care workers), provided they were sponsored under the previous rules and have continuously held permission as a Skilled Worker; any worker who was granted a Skilled Worker visa before this date and has not switched to a different visa category can still bring dependant family members (partner and children under 18).
• SOC code changes: The Standard Occupational Classification (SOC) has been updated from SOC 6145 to SOC 6135 for care workers and home carers and from SOC 6146 to SOC 6136 for senior care workers. Besides, the SOL has been replaced with the ISL.
• Salary threshold: The salary threshold for Skilled Workers has been raised to £38,700. There is an exception for migrants sponsored under the Health and Care Worker visa with a general minimum salary of £29,000 and for those roles on the ISL, either £23,200 for 37.5 hours or their occupation specific threshold, whichever is higher.
• Sponsor requirements: Sponsors must now hold active registration with the Care Quality Commission (CQC) and be currently undertaking at least one ‘regulated activity’.
• Sponsor Licences: Licences are set to auto-renew from 6th April 2024, although it is advised to monitor the expiry date closely in these early stages of implementation.
The outlined changes will undoubtedly have profound implications for individuals, employers, sponsors and the broader care sector, as well as the general economy. There are additional moral considerations that the Government may not have fully taken account of, particularly concerning the prohibition on care workers bringing dependants to the UK.
Responding to change
Records indicate a scarcity of service providers in the sector, with care workers often experiencing overwork, which can detrimentally affect their health and wellbeing. The contribution of domestically recruited staff in the social care sector is pivotal to the UK's care system, but the demand is higher than the figures the local workforce can supply. These changes, however, mean that qualified, professional care workers may choose not to relocate to the UK if they cannot bring their spouse and minor children, potentially breaching
> CMM June 2024 19
their basic right to family life. This situation could significantly impact care workers’ mental health and wellbeing due to feelings of isolation or family separation.
Current recruitment trends already point at other countries being more favoured by skilled migrants, with better prospects for themselves and their family members. In the past, dependant family members of sponsored migrants, could have been employed in the adult care sector if they were sufficiently qualified and experienced, thereby helping to fill vacancies. Moreover, dependants working in the UK contributed to their household finances, which is particularly important given the comparatively low payment rates in this sector.
These moral considerations highlight the complex interplay between immigration policies, healthcare provisions and individual rights. There must be a nuanced approach that balances national interests and the public perception on immigration, considering ethical imperatives and the wellbeing of both care workers and those they serve.
Unfortunately, the Government has implemented these policies without consulting all stakeholders. We believe a consultation with industry representatives could have provided valuable insights into the potential consequences of the changes.
In addition to the updates in immigration policy, the Government has launched a programme aimed at fostering careers in adult social care. The objective is to train, motivate and recruit in the resident UK workforce to cope with the growing demand in the sector. It is evident that achieving the necessary standards will take time, and the effectiveness of the programme is not certain. In the interim, these positions will effectively be filled by professional care workers recruited from overseas.
An imperfect system
A recent report by the Independent Chief Inspector of Borders and Immigration on the social care sector has revealed the inadequacies of the immigration process and the abuse of this route. It is evident that the Home Office was unprepared for the popularity of the Health and Care Worker visa when first introduced. Numerous Sponsorship Licences have been granted to organisations
in the sector. Some employers are failing in their compliance duties, including instances of underpaying workers and, in more egregious cases, engaging in the sale of Certificates of Sponsorship (COS). These practices not only violate immigration regulations but also exploit vulnerable migrants, placing them in positions where promised employment may not even exist.
Reports of Sponsor Licence abuse have prompted the Home Office to take corrective action. Consequently, Sponsor Licence Applications in general, and in the care sector in particular, are undergoing more thorough scrutiny. Additionally, the increased demand has also resulted in significant delays to the approval process for Defined Certificates of Sponsorship (DCOS). Previously, such requests were typically decided within one to two working days.
However, in recent months, it has taken weeks or even months for the Home Office to reach a decision on these requests. Sponsors must provide additional information and documents to establish the genuineness of the vacancy before approval. Even upon submission of the requested information, it can take weeks for the Home Office to decide, whether approved or rejected.
Those sponsors whose requests were not approved before the changes, and were unable to assign their COS before 4th April, will have to meet the new requirements of the rules. It remains uncertain whether the approval process for DCOS requests will be expedited following the rule changes and updates to internal portals. These delays or rejections in COS allocation have had profound impacts on the service provided by care workers. This has resulted in insufficient staffing levels, employee overwork and sometimes departures to larger sponsors where possible, as well as increased instances of illness and sick leave amongst staff. The increasing demand for care providers cannot be addressed unless the Home Office reverts to its original timeline for deciding COS requests.
No clear solution
The cross-party House of Lords Secondary Legislation Scrutiny Committee has raised concerns about the Government’s plans to restrict Health and Care Worker visas under changes to immigration rules. Despite
this, the Home Office has failed to provide substantial explanation, exacerbating uncertainties within the sector.
Baroness Randerson, Member of the Secondary Legislation Scrutiny Committee, said, ‘We recognise that these changes are intended to address concerns about levels of legal migration. However, there is alarm among social care providers about the impact of these changes: the care sector is already struggling to recruit sufficient workers and is worried these measures could make things worse.
‘The Government says that the dependant ban will not reduce the number of immigrant workers, but it has not provided evidence to back this up. This means it is impossible for Parliament to assess the effects of the changes properly and the sector is also left in the dark.
‘Whenever the Government lays legislation which has the potential to affect the effectiveness of a sector and has real world consequences for the public at large, it must provide information on the impact. This is a principle the Government has accepted but does not always observe in practice and we are writing to the Home Office to ask for further details.’
Currently, the Home Office is collaborating closely with other Government departments, such as HMRC, to track the records of sponsor licence holders. This will ensure that sponsors are adhering to National Minimum Wage (NMW) payments to their employees.
To tackle compliance issues, the Home Office has substantially increased audits and inspections of licence holders. It is imperative for stakeholders to ensure compliance of the immigration rules and other relevant UK laws. By doing so, employers can continue to sponsor their existing migrant workforce and increase it, where necessary. This compliance would address the concerns raised by the Independent Chief Inspector and would also demonstrate the crucial role migrants play in the care sector and the broader economy.
This approach may lead to a more constructive dialogue with policymakers and potentially open the door to changes that benefit migrants rather than penalise them. Highlighting the positive contributions migrants make to addressing workforce shortages, delivering essential services, and driving economic growth can be instrumental in shaping a fairer immigration policy. CMM

How will the changes to UK immigration policy impact your organisation? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
20 CMM June 2024
Sudipta Dey is an Associate (Senior Immigration Advisor) – Employment at RWK Goodman. Email: sudipta.dey@rwkgoodman.com : @RWKGoodman
IMMIGRATION LAW UPDATE: ASSESSING THE IMPACT >
Controlled Drug Disposal

Guard against the misuse of controlled drugs to protect your staff, residents and communities by using drug denaturing kits.
; Suitable for use with tablets, capsules, liquids, aerosols or patches
; Formula contained in a water-soluble sachet to prevent accidental spillage of granules
; Available in volumes 250ml to 20L

Purchase at NHS supply chain: my.supplychain.nhs.uk/catalogue or www.alphalabs.co.uk/safer-denature





CMM June 2024 21 TIME FOR CHANGE! Care Home Insurance due for renewal? For FREE, no obligation quotations call 01273 977221 or visit: www.care-insurance.co.uk Phoenix Specialist Risk Solutions, Office One, 1 Coldbath Square, Farringdon, London, EC1R 5HL PHOENIX SPECIALIST RISK SOLUTIONS
023 8048 3000
Phone:
www.alphalabs.co.uk
Safe, Compliant
07 July 2023 - Care Management Matters - Safer Denature.indd 1 12/07/2023 15:31:11










22 CMM June 2024 A selection of the quality care homes sold by NGA Care Your Business is Our Priority THE CARE HOME BROKERAGE PROFESSIONALS GET IN TOUCH Due to huge demand, we urgently require care homes throughout the country. Contact our Managing Director Nick Greaves in confidence on: 07943 107 887 nick@ngacare.co.uk ngacare.co.uk THE NEXT STEPS IN DIGITISING SOCIAL CARE Sponsored by New episode out now!

Supporting addiction recovery: The power of community
Robert York, Director at Swift Management Services Limited, outlines the challenges facing providers of care services for people with an addiction, highlighting the importance of community engagement and best practice methods for achieving it.
CMM June 2024 23





Staff Rota Planning Carebeans Ltd, Singleton Court, Wonastow Road, Monmouth, Monmouthshire NP25 5JA. www.carebeans.co.uk The all-in-one digital solution designed to simplify and supercharge your workforce management. Get in touch today to book a free system demonstration by calling 01925 386800 or emailing info@carebeans.co.uk SYSTEM INCLUDES Time & Attendance HR Compliance Payroll Staff Training Staff Rostering 00057 CMM 186x110mm June 2024.qxp_Carebeans CMM June 2024 186x110mm 14/05/2024 13:06 Page 1 24 CMM June 2024
As a health and social care consultancy, Swift Management assists companies to establish new care homes, many of which are providers of services caring for people with an addiction. One thing we have frequently discovered is the lack of understanding in the community where the home is to be situated. Nobody wants a care home of this sort on their doorstep.
A beacon of hope
In a world where addiction is often hidden away, care homes stand as a beacon of hope offering sanctuary and support to those grappling with alcohol or drug dependency. These facilities play a vital role in the journey towards recovery, providing a structured environment where individuals can heal, learn and rebuild their lives.
However, the path to sobriety is fraught with challenges, and those who work within these care homes face a unique set of obstacles. From navigating relapses to celebrating triumphs, the journey of providing care for individuals with addiction is both demanding and rewarding.
Addiction is a complex and multifaceted issue that can affect anyone, regardless of age, gender, or socioeconomic status. It doesn’t discriminate. Whether it’s alcohol, prescription drugs or illicit substances, addiction can quickly spiral out of control – leaving individuals trapped in a cycle of dependency. This cycle not only harms the individual but also takes a toll on their relationships, careers and overall wellbeing.
One of the primary challenges in providing care for individuals with addiction is understanding the root cause of their dependency. Addiction often stems from a combination of genetic, environmental and psychological factors. Trauma, stress and underlying mental health issues all contribute to substance abuse. Therefore, effective treatment requires a holistic approach that addresses these underlying issues, while also focusing on breaking the cycle of dependency.
Care homes specialising in addiction treatment provide a structured and supportive environment where individuals can begin their journey to recovery. These facilities offer a range of services, including detoxification, counselling, therapy and life skills training. The goal is not just to help individuals abstain from substance use but also to empower them to lead fulfilling and meaningful lives, free from addiction.
One of the key advantages of care homes is the sense of community they provide. For many individuals struggling with addiction, feelings of isolation and loneliness are common. In a care home setting, residents have the opportunity to connect with others who understand their struggles and offer support without judgement. This sense of camaraderie can be a powerful motivation in the recovery process.
Overcoming challenges
While the rewards of helping individuals overcome addiction are immense, the journey is not without its
challenges. Perhaps one of the most significant hurdles care providers face is the reality of relapse. Addiction is a chronic condition, and setbacks are a natural part of the recovery process.
Witnessing someone relapse after making progress can be disheartening for both the individual and their caregivers. However, it’s essential to view relapse as a learning opportunity rather than a failure. Each setback provides valuable insights that can inform future treatment strategies.
“Witnessing individuals reclaim their lives from the grip of addiction is nothing short of miraculous.”
Another challenge is the stigma surrounding addiction. Despite efforts to raise awareness and promote understanding, there remains a pervasive stigma associated with substance abuse. Care providers often encounter prejudice and discrimination from the local community, wider society and the care system itself.
Overcoming these barriers requires ongoing education and advocacy to change attitudes and promote empathy and compassion. We frequently see when a crime is committed in an area adjacent to a care home providing care to those with an addiction, the first assumption made is often that the crime must have been committed by a resident from the home. This is often far from accurate but damages the morale and resolve of those in care as they feel they will always live with the stigma of addiction no matter how far along the journey they have come.
Community connections
Despite the challenges, working in a care home for individuals with addiction can be incredibly rewarding. Witnessing the transformation that occurs as individuals reclaim their lives from the grip of addiction is nothing short of miraculous. Every small victory is wonderful – whether it’s a resident reaching a sobriety milestone, reconnecting with loved ones or pursuing their hobbies and interests. Every milestone is a cause for celebration.
One of the most rewarding aspects of working in addiction care is the opportunity to build meaningful connections with residents. By providing a safe and nurturing environment, care providers form bonds based on trust, respect and empathy. These relationships play a crucial role in the recovery process, offering support and encouragement during the most challenging moments.
In the battle against addiction, care homes serve as a beacon of hope, offering refuge and support, but in order to do this they often need the support and empathy of the local community and that is >
CMM June 2024 25 SUPPORTING ADDICTION RECOVERY: THE POWER OF COMMUNITY
never easy. Care home providers often need to invest considerable time and energy in managing community resistance when opening a drug and alcohol service and this requires a proactive and transparent approach.
At Swift Management, we believe there are a number of elements to addressing community concerns:
1. Education and awareness: Provide accurate information about addiction and recovery to dispel misconceptions and reduce stigma. Organise community workshops, presentations or open houses to educate residents about the purpose and benefits of drug and alcohol services. Highlight success stories of individuals who have overcome addiction and reintegrated into society.
2. Community engagement: Engage with local community leaders, organisations and residents to understand their concerns and address them openly. Invite community members to participate in the planning process and provide feedback on the services being offered. Foster partnerships with community groups, schools, churches and businesses to build support for the service.
3. Clear communications: Communicate openly and transparently with the community about the plans for the drug and alcohol service. Address concerns regarding safety, security and potential impact on property values. Provide assurances that the service will be well managed and adhere to all relevant regulations and standards.
4. Safety measures: Implement safety measures such as security cameras, controlled access and regular patrols to address concerns about safety and security. Develop protocols for handling emergencies and incidents to ensure the safety of residents and the community.
5. Community involvement: Offer opportunities for community involvement, such as volunteer programmes or community events hosted at the care home. Encourage residents to participate in community clean-up initiatives such as neighbourhood watch programmes, or other community-building activities.
6. Building trust: Build trust with the community by demonstrating a commitment to being good neighbours and responsible stewards of the environment. Be responsive to community feedback and address any issues or complaints in a timely and respectful manner. Maintain open lines of communication and be accessible to address concerns as they arise.
7. Legal compliance: Ensure that the service complies with all relevant laws and regulations, especially the Health and Social Care Act 2008. Obtain necessary permits and licences and adhere to any conditions
imposed by local authorities.
8. Addressing the ‘not in my backyard’ feelings: Acknowledge the concept of ‘not in my backyard’ and its underlying concerns. Emphasise the importance of providing support services for individuals struggling with addiction as a community responsibility. Highlight the positive impact of the drug and alcohol service on the community, such as reducing substance abuse, improving public health and supporting individuals in their recovery.
Addressing the issues of the local community can help to address the wider issues of care in this specialised field.
The community challenges, if not managed well, can impact on residents’ recovery due to:
• Stigma and discrimination: Residents may face discrimination from society due to their addiction history, which can affect their self-esteem and sense of belonging.
• Resistance to change: Some residents may resist the structure and routines of the care home, especially if they are accustomed to a lifestyle of substance use and independence.
• Relapse: This is a common challenge in addiction recovery. Despite efforts to create a supportive environment, some residents may struggle with triggers and cravings, leading to relapse.
• Limited resources: Care homes may face limited resources for providing comprehensive support, including funding for staff training, therapy sessions and recreational activities.
• Staff burnout: Staff working in drug and alcohol care homes may experience burnout due to the emotional intensity of the work and the challenges of supporting residents through their recovery journeys.
• Co-occurring disorders: Many residents may have co-occurring mental health disorders such as depression, anxiety or trauma, which can complicate their recovery process and require specialised care.
• Lack of family support: Some residents may lack family support or have strained relationships, which can hinder their recovery process and sense of belonging in the community.
Whilst addiction services are one of the least discussed areas of social care, the services provided are vital, therefore being able to provide services and advocate for the residents is vital. As consultants, we work with providers to address the issues with local communities to give a new service the best possible start. CMM
What
of
26 CMM June 2024 SUPPORTING ADDICTION RECOVERY: THE POWER OF COMMUNITY
York
Swift Management Services Limited.
Linkedin:
Robert
is Director at
Email: robert.york@swiftmanagement.org.uk
www.linkedin.com/company/swift-management-services-limited
is your experience
engaging your business with the local community? Have you encountered any resistance and if so, how did you overcome it? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
>







CMM June 2024 27 • Life Insurance • Relevant Life Insurance • Shareholder Protection • IHT Planning • Critical Illness • Private Medical Phoenix Specialist Risk Solutions, Office One, 1 Coldbath Square, Farringdon, London, EC1R 5HL PHOENIX SPECIALIST RISK SOLUTIONS Phoenix Specialist Risk Solutions Ltd are authorised and regulated by the Financial Conduct Authority – FRN: 992540. HAVE YOU GOT COVER? Call 01273 977221 or visit: www.phoenixsrs.co.uk SECURE YOUR PLACE NOW In association with @CMM_Magazine #CMMInsight www.caremanagementmatters.co.uk A series of lunchtime webinars FREE to attend

INTO PERSPECTIVE
How can the workforce benefit from training to use music for wellbeing?
This issue, Into Perspective invites two industry leaders to discuss how music can enhance wellbeing for people drawing on social care and the benefit to providers of training their workforce to use music in their settings.
Music has been used therapeutically for centuries, with Greek philosopher and mathematician Pythagoras being one of the first documented professionals to use sound for healing purposes, calling it ‘soul adjustment’. Pythagoras used music (along
References
with sound and chanting) to support people who were experiencing feelings of anger, sadness, worry or frustration.
Today, sound is still used as a form of sensory therapy and music is recognised as a powerful tool to build community and promote feelings of pleasure. Listening to music has been found by researchers to release dopamine at peak moments of enjoyment. According to a study reported in Nature Neuroscience1, ‘intense pleasure in response to music can lead to dopamine release in the striatal system’. Dopamine, often referred to as the ‘feel-good hormone’, is a type of monoamine neurotransmitter produced in the brain that facilitates communication between nerve cells in your brain and your body.
Music therapy is a clinical intervention that uses music to help people with various health
and emotional challenges. According to the British Association for Music Therapy (BAMT), music therapy is ‘a particularly effective clinical intervention for people who have difficulty communicating verbally’.
The BAMT continues, ‘For people affected by disability, illness or injury, working with music therapists can be life changing. Children with autism can develop emotional, social and communication skills. Someone with an acquired brain injury as the result of an accident can be helped to regain their speech. An older person frightened by the isolation and confusion brought on by dementia can, through the powerfully evocative nature of music, connect with these memories again and share these with others.’
Bringing music into social care
According to research into the impact of musical stimuli on human beings2, music creatively blends sounds and silences to craft compositions encompassing elements of melody, timbre, pitch and rhythm. Music ‘serves as a means of human expression and aesthetic communication, offering a profound impact on the emotional, cognitive and physiological aspects of individuals’ experiences’.
It is worth noting, however, that to produce a pleasurable effect the music must be enjoyable to the listener – discernment is the order of the day when it comes to delivering music to the people in your care and observation is necessary to ensure the music being offered is inducing the desired effect in all the participants3.
For providers of care who wish to bring music into their setting or make it part of their provision, there are training options available for your workforce. Live Music Now works with care providers and settings to bring ‘enjoyment, excitement and benefits of live music back into people’s lives’, and Intergenerational Music Making (IMM) looks to create ‘cohesive communities’, aid ‘the improvement of mental and physical wellbeing’ and reduce ‘feelings of loneliness and isolation’.
Here, both Live Music Now and IMM offer their perspective on how the sector can benefit from training its staff to use music for wellbeing and the sense of connection, inclusivity and pleasure music can bring.
1Salimpoor VN et al (2011), Anatomically distinct dopamine release during anticipation and experience of peak emotion to music, Nature Neuroscience, 14: 257-262. 2Gómez-Carballa A et al (2023), Music compensates for altered gene expression in age-related cognitive disorders, Scientific Reports, 13(21259). 3Merrill J et al (2023), Effects of disliked music on psychophysiology, Scientific Reports, 13(20641).
28 CMM June 2024

Music training facilitates interpersonal connections
Charlotte Miller, Director and Founder, Intergenerational Music Making
: @IMMmusicUK
Email: info@imm-music.com
Integrating music into workplace training programmes can equip employees with strategies to harness its therapeutic effects and foster a more positive and productive environment.
Recent research underscores the tangible benefits of incorporating music into daily work routines. Studies, such as one in the Journal of Occupational Health Psychology1, reveal music's ability to reduce stress levels, which enhances mood and overall job satisfaction.
Music sessions can also be used to cultivate a sense of unity and understanding amongst employees of different age groups. By incorporating collaborative music sessions into training initiatives, organisations promote camaraderie among employees which can transcend generational divides.
Music training also facilitates interpersonal connections.
Research in the Journal of Music Therapy2 demonstrates that group music-making activities strengthen social bonds and communication skills within teams.
Beyond individual benefits, music positively impacts
organisational outcomes. For example, a study published in Behavioral Sciences3 suggests that listening to music during work activities could help to create positive organisational practice within the workforce. Investing in music training programmes can lead to lower turnover rates and a more engaged workforce.
However, implementation requires strategic considerations.
Tips for organisations:
1. Tailor music training to align with diverse tastes and preferences.
2. Encourage using music during breaks or meetings.
3. Ensure employees have access to music streaming platforms and quiet spaces.
4. Facilitate group music-making activities to enhance teamwork and creativity.
5. Offer workshops to educate employees on the therapeutic effects of music.
6. Create a culture that values and respects musical diversity.
7. Use metrics like employee surveys to assess the effectiveness of music training programmes and adjust accordingly.

‘It has turned our staff into leaders’
Douglas Noble, Strategic Director of Adult Social Care and Health, Live Music Now UK
: @LiveMusicNowUK
Email: douglas.noble@livemusicnow.org.uk
Our study with the University of Winchester demonstrates how carefully delivered live music contributes to person-centred care and makes care homes happier places to live and work. The study seeded our Live Music in Care model; innovative hands-on workforce development, increasing staff understanding, confidence and skills in the use of music.
Tracey Judd, Lead Lifestyle Co-ordinator at Appleby House Care UK, said, ‘[Care team] confidence has got so great that they will actually stand up in front of the choir and lead them in a song; going from being someone very shy to standing up and leading.’
Care teams work alongside trained professional musicians, delivering participatory music activities working towards a Badge of Excellence in Musical Care. Having a musical care tool kit enhances capacity to lead structured activities. Care workers draw on music in day-to-day care to support people experiencing distress and anxiety, and to ease transitions and intimate care.
A team member at OSJCT Monkscroft Care Centre, said, ‘When Mary first came, she could
not speak. Now when I do her personal care she's talking and telling me to get on with it and there is also real connection with Peter (her husband).’
Bogumil Cwiklak, Manager at OSJCT Monkscroft Care Centre, said, ‘It has turned our staff into leaders. It has allowed the team to come out of themselves and show their strengths.’
A team member at The Beeches care home, said, ‘I love having the musicians. The job is very hard, and the music helps my mental health. It helps me feel more positive and productive.’
Indira Baster, Registered Manager at Params Care Home, said, ‘We get bogged down with cooking and personal care, and making connections can get lost. Doing the music sessions had a huge impact. Not only for the relationships with residents but also as a team as well.’
Developing musical care through the Live Music in Care programme can support workforce development and wellbeing, increase job satisfaction and potentially support retention and recruitment. It impacts positively on the quality of person-centred care.
To view the full list of academic and literary references used to write these comments, visit www.caremanagementmatters.co.uk

CMM June 2024 29
Pain management in people living with dementia: Unlocking solutions

Dr Kreshnik Hoti, Senior Research Scientist at PainChek, discusses methods of assessing pain in people living with dementia and describes how one care provider has implemented digital technology to improve quality of life for the people it cares for.
Chronic and persistent pain in later life is a worldwide problem. Of those people living in care homes, it is estimated that over 50% experience persistent or chronic pain1
People living with dementia or cognitive impairment are particularly vulnerable to pain being poorly managed as they may not always be able to self-report pain effectively, resulting in it going untreated.
Dementia affects around 850,000 people in the UK and was the country’s leading cause of death in 20222. It is estimated that 70% of people in care homes have dementia or severe memory problems3, and it is thought that at least 50% of them regularly experience pain4
The need for best practice pain management also extends to older people living at home with access to home care packages that enable long-term home living. These populations include people living with dementia, suffering with multiple chronic pain conditions, as well as those with sensory, cognitive and mental health impairments and who have difficulties in self-reporting pain.
People living with dementia can experience difficulties in verbally communicating that they are experiencing pain, along with the severity and location of that pain. To compensate, they become more reliant on non-verbal communication, through behaviour, which may include anger, frustration, restlessness, withdrawal and changes in body language, speech and sleep patterns, appetite and facial expressions.
Moreover, with over 90% of people living with dementia
affected by behavioural and psychological symptoms (BPSD)5, pain is often missed and may remain untreated and unrecognised. This can result in inappropriate prescribing of psychotropic medication.
A Department of Health study found that of 180,000 antipsychotic prescriptions, the majority (140,000) were prescribed inappropriately to people living with dementia6. This is particularly concerning as antipsychotic medications can increase the risk of stroke nine-fold and double the risk of death7,8
People living with dementia are susceptible to increased levels of pain compared to others as they have decreased mobility and therefore a high risk of falls, accidents and injury, and like others, may also experience age-related conditions such as osteoarthritis, pressure sores, skin tears, stiffening of joints, muscle rigidity and constipation.
Effective assessment and management of pain are therefore crucial to supporting high-quality care for this patient population.
Benefits of digital pain assessment
The social care sector is rapidly evolving, driven by technological advancements and the overarching digitisation of care. Care providers can harness the power of technology to overcome gaps in care documentation and give them the means to better plan care according to evidence-based practices.
Technology-enabled pain assessment can play a critical
30 CMM June 2024 >


role in facilitating better health outcomes for care home residents. Point-of-care assessment facilitates documentation, hence reducing associated administrative burden.
This has the potential to equip carers with information to better care for residents whilst meeting the requirements of Care Quality Commission regulators regarding auditing and personalising care9. Moreover, the collection of data allows for a broader and more accurate analysis of issues affecting the entire care home population.
Technology in action
Further evidence of the benefits of embedding technology into everyday operations and the care plans of residents living with dementia comes directly from carers on the ground.
A leading care provider, Orchard Care Homes, has been running care homes across the UK for over a decade and has established a strong reputation in the care industry for providing quality care for older people.
To more effectively meet the needs of people living with advanced dementia in Orchard Care Homes’ properties, the provider established a multi-faceted psychosocial intervention programme called ‘Reconnect’. This offered enriched psycho-social care to reduce people’s distress and thus enhance their quality of life and wellbeing. The programme also incorporated the use of a digital pain assessment tool.
A recent study10 published in the peer-reviewed journal Frontiers in Psychiatry, reviewed the impact of this programme on people living with dementia who had not previously responded to support in alternative settings or found previous care ineffective in relieving their distress and reducing risks they posed to themselves or others.
The study identified that the introduction of the Reconnect programme, through its interventions based around meaningful activity engagement, pain management and constipation relief, resulted in significant improvements related to people’s distress, psychotropic use and safeguarding, with a 91.7% reduction (i.e., from 36 to three events) in safeguarding events related to behaviours observed.
Additional analysis recently carried out at Orchard Care Homes’ properties has also linked use of a digital pain assessment tool to a 91% drop in significant injuries and a 20% reduction in falls since it was added to Orchard’s falls prevention policy and post-falls protocol 12 months ago11.
Hannah Miller, Head of Dementia at Orchard Care Homes, said, ‘It is well known that failure to recognise and treat pain effectively is a problem amongst people living with dementia. Pain is a trigger of distress, yet often overlooked as a contributing factor, and the person is not only left to suffer unnecessarily in pain, but also to be prescribed psychotropic agents to manage their behaviours.
‘Integration of a digital pain assessment tool has been a real game changer, enabling our care teams to closely
monitor and assess the pain experience of individuals in their care using a mobile care device, providing staff with a long-term view of when a resident is likely to experience pain.
‘Orchard strives to incorporate technological advances and put them into practice to ensure we are enabling all people living in our care homes to achieve good outcomes and be afforded equitable care regardless of their cognitive ability or ability to self-report health concerns such as pain.
‘Individuals who are not able to effectively verbally communicate pain who were previously disadvantaged are now on an equal footing with those that can communicate effectively.’
Looking to the future
Access to effective pain management is important for everyone and is widely accepted as a human right12, so it is crucially important that those unable to reliably self-report can have their pain accurately identified and assessed, and effectively managed.
With an ageing global population, and 1.7 million people projected to be living with dementia in England and Wales by 204013 – over 40% more than previously forecast – digital technology is becoming an integral strategy for improving care standards for people living with dementia in care homes of all sizes and handling the increasing costs associated14 CMM
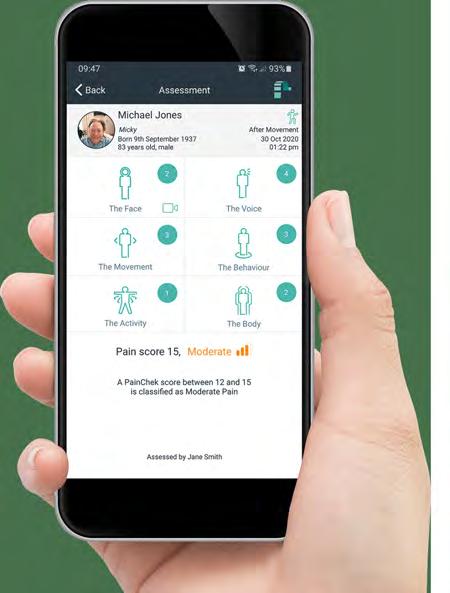

CMM June 2024 33 PAIN MANAGEMENT IN PEOPLE LIVING WITH DEMENTIA: UNLOCKING SOLUTIONS
What is your experience of implementing technology to provide care and support to people living with dementia? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts. Dr
Hoti is Senior Research Scientist at PainChek. : @PainChek Email: info@painchek.com > To view the full list of academic and literary references used to write this feature, visit www.caremanagementmatters.co.uk
Kreshnik
WHAT PRICE A LIFE?
A call to ra ise fee rates

Clive Parry, Director at ARC England, explores the findings of the organisation’s latest Fee Rate Maps and reiterates ARC England’s demand for change.
When we published our first set of Fee Rate Maps in March 2023, we had no idea that the positive response they generated would lead to them becoming an annual project that would play such a central role in guiding the focus of our work.
Our members and the wider learning disability social care sector told us that the maps made a real difference in negotiations with commissioners and that more realistic fee rate uplifts were secured as a result.
So, in December 2023 the ARC England Learning Disability and Autism Research Unit commissioned data visualisation experts Polimapper to begin sending the next round of Freedom of Information requests to all the local authorities in England and
Wales, asking them about the rates they pay for learning disability and autism services.
Following feedback from the first year of the maps, we were able to extend the reach of the questions to local authorities. As well as asking about rates for supported living, residential services, domiciliary care and day services, we also asked about the services local authorities provide themselves, so that we can compare these with externally commissioned services.
We also asked about the time allowed for staff training and added some more detailed questions about day services. The reasons for this were twofold; firstly, day services are purchased differently from other services, and we wanted to ensure that the fee rate data works better for day services providers, and secondly, day services are faring least well in terms of fee uplifts across all learning disability service types.
You can see the results of our Freedom of Information requests in this year’s maps, which again contain data searchable by local authority and by constituency (increasingly useful as we move towards a general election).
Looking at the National Living Wage (NLW) rise over time in
CMM June 2024 35
>
comparison with fee rate uplifts, we now have six years of data mapped in line graphs for each service type. As can be seen from the following graph for residential services, fee rates have failed to keep up with NLW increases and this illustrates the cumulative impact of year after year below inflation increases. This is particularly pertinent in supported living services, where staff wages and salaries can represent upwards of 85% of operating costs.
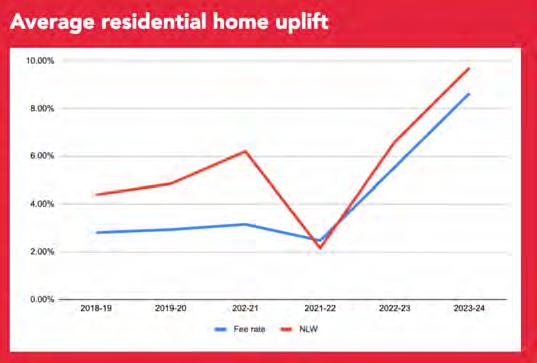
Local authorities need to be paying upwards of £22.95 per hour if providers are to meet their statutory requirement to pay their staff the NLW. For comparison, staff undertaking comparable roles in the NHS at Band 3 are paid, including allowances, an hourly rate of £27.80. The Unfair to Care 2024 report by our member Community Integrated Care has found a 36% pay gap between the average care worker and their equivalent role in the NHS.
Talking to our members and looking across the sector, we think a fee rate uplift for 2024-25 of at least 12% is required. Even this, however, does not begin to address the cumulative funding shortfall that year upon year of fee rate uplifts below inflation has created.
The current picture
If adult social care is invisible, then learning disability and autism service providers are towards the bottom of this hierarchy of invisibility.
CQC’s Market Oversight of adult social care has identified that it is specialist providers that are working under the worst of the financial pressures affecting social care services. This means learning disability and autism services. The urgent need to address this does not appear to have been understood by the Department for Health and Social Care.
We continue to see councils paying different rates for the same or similar services. This creates disparity and unfairness in the system. Our members are telling us that for 2024/25, councils are offering them fee rate uplifts in single figures, well below the 12% we have identified as the minimum required, and at a level which does not allow many of them to fulfil their statutory requirement to pay the NLW.
On top of that, we have even heard that some councils are suggesting to providers that they should use their reserves to continue to operate. Maintaining sensible operating reserves is necessary for an organisation, not only to ensure Charity Commission compliance, but because not doing so would be a dereliction of the duties of trustees and board members.
Clearly, it is inappropriate for a local authority to suggest that they could or should dictate a provider’s reserves policy. Learning disability support providers, whether charities or private sector, need to grow and invest in their staff, in IT and technological developments, and in bringing about the very best person-centred care for the people who draw on their support. To suggest that they should be subsidising their own services that the state has a duty to pay for is simply unacceptable in any sector, let alone one in which the voices of the people who rely on services are largely unheard.
The cumulative effect of fee rate uplifts that have failed to keep pace with inflation and other cost pressures is that providers are handing back unsustainable contracts and declining to accept packages of care that they are well placed to provide. We know that providers who are looking to expand their services are using the Fee Rate Maps to check rates in neighbouring counties to see if this expansion is viable, and we know of at least one occasion where a provider has decided not to offer services to a local authority who is shown to be paying inadequate fees.
It is also interesting to look at the role of day services. If learning disability and autism services are among the lowest in the social care ‘hierarchy of visibility’ then day services are the least visible service type overall. This is despite the fact that day services save local authorities huge amounts of money every year by, for example, enabling supported people to be looked after within their family home. As well as offering opportunities and activities for people who draw on support to live lives of choice and control, day services also provide a small amount of respite for unpaid family carers.
What price a life?
Although the latest LeDeR 2022 report found a drop in the number of avoidable deaths since 2021; 42% of deaths were still deemed ‘avoidable’ for people with a learning disability in 2022 compared to 50% in 2021.
The report also found that appropriate care was associated with reductions in premature death. Taking this into account, Government’s persistent underfunding of this essential care begins to appear as if they are simply turning their backs on the health of the learning disability community and potentially contributing to early deaths. The National Audit Office report, Reforming adult social care in England, backs up our view that the department is operating without a long-term social care plan.
Successful services run by our members improve people’s quality of life and support them to take the necessary steps towards an independent life. Moreover, they improve physical and mental health conditions and therefore alleviate pressure on overstretched NHS services. When we help and support individuals, their families and carers to pursue and achieve their goals in life, we are contributing to social change in our communities.
People with learning disabilities and autistic people are some of the most socially excluded in our society. Employment opportunities are scarce, they rarely live in their own homes or have a choice over who cares for them. However, at ARC England, along with our research partners, members and advocates, we believe that every individual has a right to a life lived with choice and control and in which their strengths and abilities are nurtured and celebrated.
We are therefore calling for Government to act quickly to stabilise the learning disability social care sector and for learning disability and autism services funding to be properly and robustly ring fenced thereafter. CMM

36 CMM June 2024 WHAT PRICE A LIFE? A CALL TO RAISE FEE RATES
Clive Parry is Director at ARC England. Email: clive.parry@arcuk.org.uk : @ARCEngDirector > Is your local authority paying a fair fee rate? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.

10.5 THOUSAND Proud to have supported almost £5.9 MILLION IN GRANTS AND SUPPORT care workers with over Support us to help even more www.thecareworkerscharity.org.uk
RESOURCE FINDER:
CQC COMPLIANCE
Compliance is core to the successful running of an organisation. For all care services, sometimes seeking external help could fill in any gaps when it comes to impressing regulators. Here, a series of expert organisations share how they can help you and share details on the services they offer.
Bettal Quality Consultancy
Tel: 01697 741411
Email: info@bettal.co.uk
Website: www.bettal.co.uk
SECTORS
• Care homes.
• Home care.
• Supported Living.
• Learning disability services.
• Mental health services.
• Home care registration.
SERVICES
• Quality management systems (policies and procedures).
• Support with new registration.


• Home care digital management.
• Audit tools.
LEAD INDIVIDUAL
Albert Cook is a former manager and principal inspector of care services and is responsible for more than 200 adult care services. The company is now recognised as one of the leaders in providing quality management systems (policies and procedures) to the care sector.
As a fellow of the Chartered Quality Institute, Albert is committed to quality in care. He has supported companies and organisations to improve their care services using the Bettal Quality Management System,

Albert Cook
Tel: 01697 741411
Cared 4, in the UK and Europe, including services in England, Scotland, Ireland, Germany and Poland. The Bettal System complies with the requirements of the CQC.
COMPANY INFORMATION
Bettal Quality Consultancy has been promoting quality in the care sector for nearly 30 years. Bettal is a leader in the registration of care services, demonstrating that its documentation complies with the CQC's requirements.
The Bettal Quality Management System is not just a tool but a commitment to excellence. Continually updated to align with best practice and the CQC’s Quality Statements and I Statements, it ensures that Bettal’s customers are always compliant.
The key to Bettal's growing success is the quality of its policies and procedures, which have been developed by experts with knowledge and experience gained from working in the social care sector and backed up by first-class customer support.
Email: albert.cook@bettal.co.uk
38 CMM June 2024
Care Quality Solutions Limited
Tel: 07805 081455


Email: support@carequalitysolutions.co.uk
Website: www.carequalitysolutions.co.uk
SECTORS
• Residential care and nursing homes.
• Domiciliary care services.
• Supported Living services.
• Mental health services.
SERVICES
Please visit our website for more comprehensive details.
• Mock CQC inspections. (Full and targeted.)
• Provider Information Return (PIR) completion support.
• Auditing (health and safety, good governance reviews).
• Enforcement action support. Notice of Proposal (NOP)/ Notices of Decision (NOD).
• Factual accuracy challenges.
• Crisis management and service recovery.
• All aspects of CQC registration/ changes/notifications.
• Providing policies and procedures.
• Root Cause Analysis (RCA) investigations.
• Management solutions and new business start-up services.
• Dedicated operational management (part or full –running your service on your behalf).
• Business appraisals/sector benchmarking.
• Due diligence appraisal pre-acquisition.
• Bespoke packages of support according to business and owner needs.
LEAD INDIVIDUAL
Rob Baillie is the managing director with 36 years’ experience as a qualified nurse (RNMH). He has devoted his career to the development and delivery of social and healthcare services for people with learning disabilities and/or autism, mental ill health
and care services for older adults experiencing dementia.
His work has been within the NHS, private and voluntary sectors and over the years he has gained further education qualifications in business studies, teaching and assessing, autism, clinical research, mentoring and coaching and non-executive directorship.
He has worked in roles as care home owner and operator and has held a number of regional and national operational, strategic, clinical and senior director roles.
His experience spans concept, design, development and service delivery with a strong focus on clinical and care governance, compliance and driving quality and transformation.
Rob has a proven track record of being a critical thinker, being innovative and creative, but most importantly recognition as being a quality-driven person with a strong desire to deliver only the best possible care and support services.
COMPANY INFORMATION
Care Quality Solutions Limited set out on its journey in 2016 with a strong emphasis on developing and driving quality to positively impact on business performance and reputation. The company has a proven track record of turning under-performing care services into high-quality and commercially successful services delivering 'good'-quality care.
Care Quality Solutions Limited works with a number of associates and business partners, each being specialists in their own field. The vitality of having access to a range of specialists ensures that we are able to respond to your precise requirements and avoids a one-size-fits-all approach.
Quality Care Group
Tel: 01273 424904
Email: hello@qcaregroup.co.uk
Website: www.qcaregroup.co.uk
SECTORS
• Residential care and nursing homes.
• Domiciliary care services.
• Supported Living Services.
• Mental health services.
• Children's Homes.
• End of Life Care.
SERVICES
• Insurance cover.
• Mock CQC inspections.
• Fire risk assessments.
• HR & employment law.
• New venture scheme.
• Reinstatement cost assessments.
• Staff training.
• Free compliance phone line.
• Care management consultancy (best practice modelling and roadmap to ‘Outstanding’).
• Health and safety (prevention, resolution and compliance).
• Turnaround programme and excel programme.
• Legal support (CQC support, advice and representation).

LEAD INDIVIDUAL
Simon van Os brings with him over 25 years’ experience in customer success, service delivery and product management across a variety of industries. With a strong passion for customer excellence, relationship building and business growth, Simon has successfully assisted many clients with business improvement, scalable growth initiatives and strategic problem solving.
COMPANY INFORMATION
• Training and development (health and safety/basic training and specialist/clinical training, such as dementia support).

Quality Care Group provides specialist insurance solutions to care homes and domiciliary businesses across the UK. In addition, it also provides wider business solutions and services to the sector, including recruitment for senior hires, risk control, business efficiency and wealth management. In addition, the organisation provides insurance solutions beyond the care sector, from its General Insurance team.

CMM June 2024 39
Simon van Os Francesca Jeffrey Email: simon.van.os@qcaregroup.co.uk Email: francesca.jeffrey@qcaregroup.co.uk Tel:
Tel: 01273
01273 424904
424904
Quality Compliance Systems (QCS)
Tel: 0333 405 3333
Email: info@qcs.co.uk
Website: www.qcs.co.uk
SECTORS
• Care groups.
• Care and nursing homes.
• Domiciliary care.
• Dental.
• General practices.
• Healthcare clinics.
• Supported Living.
SERVICES
QCS Compliance Centre:
• Tracks all regulatory updates and guidance changes.
• Updates and amends your policies for you.
• Automatically pushes all updates to you on desktop and mobile.
QCS Quality Centre:
• Access your online audits and digital mock inspections.
• Establish, maintain and run a comprehensive assessment programme.
• Share audit results with regulators showing continuous improvement.
QCS Dementia Centre:
• QCS Pool Activity Level (PAL) Instrument – a digital assessment of cognitive abilities.
• A library of dementia-relevant resources, including the PAL guides, to create meaningful care plans and support in-house learning and development.
• Evidence your specialism in dementia to regulators, families and commissioners.
LEAD INDIVIDUAL
Nikki Walker leads QCS and is accountable for its ambitious growth targets and enabling



QCS to scale. She is the guardian of QCS’ culture and coach to its amazing talent.
Nikki has had a broad career with over 20 years’ experience across diverse industry sectors. She has operated at board level for market-leading, fast-moving consumer goods (FMCG) and technology companies, overseeing finance, strategy, operations and culture.
Nikki has proven experience of inspiring transformation and growth through Chief Executive Officer mentoring and coaching in large and small businesses including Cisco, Schwarzkopf & Henkel and Coca Cola Schweppes.
COMPANY INFORMATION
QCS (Quality Compliance Systems) is a leading digital provider of compliance management, policies and procedures that are always up to date, enabling over 7,200 care locations to deliver and evidence the highest quality care. At its core, QCS Compliance Centre is your digital hub for quality compliance and knowledge.
QCS makes compliance management easy so you can focus on what matters most – delivering quality care. With a diverse team dedicated to enhancing care services across the UK, each member brings a wealth of knowledge, experience and a shared vision to help you deliver care that’s not just compliant but sets new standards for excellence.
Swift Management Services Ltd

Tel: 0208 087 2072
Email: info@swiftmanagement.org.uk
Website: www.swiftmanagement.org.uk
SECTORS
• Care homes and nursing homes.
• Supported Living and extra care.
• Domiciliary care.
• Independent hospitals and clinics.
• Respite care.
• Local authority and private providers.
SERVICES
• Mock CQC inspections and compliance audits.
• Compliance support.
• Preparation of action plans.
• Enforcement action support.
• Notice of Proposal and Notice of Decision support.
• Factual accuracy responses.
• Training (face to face or virtual).
• Crisis management.
• Registration support.
• Coaching and mentoring.
• Competency assessments of staff.
• Policies, procedures and forms.
LEAD INDIVIDUAL
Christopher Stringer set up Swift Management Services Ltd to provide a comprehensive support service to registered care providers.
Christopher has substantial experience of working in the public and private sector in a variety of roles and is passionate about making a difference. He has worked in healthcare for over 33 years and has held many roles, including Chief Operating Officer for a leading national care charity.
Christopher has worked with
all the regulators in the UK, whilst maintaining his nursing registration. He holds a PGDip in Healthcare Management, as well as many other essential qualifications.
Christopher acts as an expert witness for both civil and criminal cases and can quickly understand the situations and challenges faced by providers on a daily basis. He helps providers by delivering support and guidance. Christopher has supported providers that have been previously rated ‘Inadequate’ to improve their CQC service rating to ‘Good’ or ‘Outstanding’.
COMPANY INFORMATION
Swift Management Services Ltd provides expert support through a network of highly experienced healthcare professionals. The organisation’s innovative action plans have proven especially popular with CQC, because it is easy to evidence progress and improvements through its ‘You said – we did’ information programme.
Swift Management Services Ltd can support your service through a crisis or on an ongoing basis with its retained consultancy service package, providing regular one-to-one coaching and development, quality monitoring reviews, mock key lines of enquiry inspections, unlimited telephone and email support, tailored service improvement plans and access to a dedicated care consultant to work in partnership with you to drive sustainable improvements.
Nikki Walker Christopher Stringer
Tel: 0333 405 3333
Email: info@qcs.co.uk

Tel: 07973 925262
Email: christopher.stringer@swiftmanagement.org.uk
40 CMM June 2024 RESOURCE FINDER: CQC COMPLIANCE
Whether you’re taking your first steps on your digital journey – or looking for the latest news, the Digital Care Hub can help. We provide free advice and support on data protection, cyber security and using technology. And we get you. We are run by social care providers, for social care providers.
www.digitalcarehub.co.uk
Data Security and Protection Toolkit – deadline 30 June
Is your DSPT up to date? If not, you can’t use it as evidence of your data protection arrangements. The deadline for 2023/24 is 30 June 2024. Get free assistance to complete and implement your DSPT from the official support programme –Better Security, Better Care.
www.digitalcarehub.co.uk/dspt
Free elearning for care staff
Use the free elearning course on data protection and cyber security specifically for social care staff.
www.digitalcarehub.co.uk/elearning
How would you cope if you lost data? How would you access information about people’s care needs, or staff rotas and payroll data? Make sure your business continuity plan is up to date. Use our free templates and tools to develop your plan.
www.digitalcarehub.co.uk/business-continuity
Don’t delay Get free support on data protection and cyber security
CELEBRATING EXCELLENCE IN DEMENTIA CARE


In this issue, CMM hears from Grant Newton, Head of Day Care at Alzheimer’s Support, who shares his journey from supporting a friend with an Alzheimer’s diagnosis, to running multiple award-winning dementia day clubs.
To be at the Markel 3rd Sector Care Awards, and in the same room as several hundred of the UK’s most respected social care providers, was a remarkable and humbling experience. For our day clubs to then win the national award for dementia care was wonderful recognition for the hardworking and inspirational teams that run our clubs in Wiltshire.
Taking initiative
My involvement in dementia care, and the driving factors behind our service as it is now, came from assisting a friend with early-onset Alzheimer's disease. At the age of 48 and physically fit, he was offered (and duly refused) a place in a care home which highlighted to me the frustrations of finding appropriate frontline dementia care. Around the same time, I was asked to apply for a two-day a week post to develop a day club for Alzheimer's Support Wiltshire, something I was supremely underqualified for, but it happened.
A lack of experience and a brave, supportive Chief Executive Officer led me into asking a lot of 'why is it like this?' questions and reaching the conclusion that neither my friend, myself or anyone else would want to go to a ‘Dementia day club’. So, the mission
became how do we build a club that no one wants to come to but would enjoy if they did – and that is what we built. I was supported, thankfully, by a very experienced, very patient and forgiving team. A team given full permission to be themselves, given ownership of their space, allowed to follow their hearts and to treat people as they would wish to be treated themselves.
Sixteen years on, that two-day a week club has morphed into four dementia day centres in Wiltshire: Mill Street in Trowbridge, Sidmouth Street in Devizes, Old Silk Works in Warminster and Scots Lane in Salisbury, which together provide 17 days of care each week. We have 45 salaried and part-time staff and 60 highly committed volunteers.
Ethos of choice and empowerment
Anyone visiting our clubs is struck by the genuine friendship between members, staff and volunteers. There are no uniforms or badges. Although the teams are highly experienced in dementia care, they do not dwell on the dementia, other than as part of the fuller understanding of the person’s preferences, character and background. Visitors to the club always remark on the relaxed,

42 CMM June 2024
Markel 3rd Sector Care Awards

informal and uplifting atmosphere, and while they are with us, we treat members as a group of friends coming together.
The clubs are underpinned by our ethos of choice and empowerment, enabling members to pursue interests and retain skills, and creating connections – with each other, between clubs and families and between clubs and their local communities. Inclusivity is also a cornerstone and the team go the extra mile to enable members to remain with us as their dementia progresses.
Each space is carefully chosen close to, or in, a town centre, rented on a long lease and renovated to our own design thanks to successful community fundraising appeals. The buzz we generate around a new club helps local people feel invested and involved even before it opens (great for finding volunteers). The exceptional quality of our interiors was confirmed when our Warminster club, Old Silk Works, won Best Dementia Design at the National Dementia Awards in 2019.
Each club includes a spacious communal area, quiet lounges and indoor or outdoor gardens. All are bright, colourful, well-maintained spaces that reflect the positive experiences of the members attending. We make sure they are filled with art, objects and photographs which reflect members' lives now and in the past.
Fresh meals are cooked daily in the club kitchens and everyone eats together. No one takes a break at lunchtime. Members can assist with cooking and the two newest clubs, Old Silk Works and Scots Lane in Salisbury, have specially designed open plan kitchens with a long, low counter to encourage participation and involvement. No area is out of bounds to members (except cleaning cupboards). Members return home with a detailed diary of their day which gives family carers an idea of what their relative has done and sparks conversations.
Therapy whippets Higby and Dottie, and a carefully selected group of other volunteer dogs, wander free range in the clubs, spreading their own brand of love and helping to build the atmosphere of relaxed normality. Their non-judgemental listening ears provide support to people who may find it hard to integrate initially. And club members whose dementia may have forced them to give up a pet can groom, stroke, talk to and about the dogs, just as any group of animal lovers might do.
Going the extra mile
When new members join, staff take the time to get to know them well, talking to family members as appropriate and sometimes visiting at home. Joining is a gradual process with short visits, or coming in for lunch, to build up familiarity and to find out more about individual preferences. The teams constantly develop new activities in response to members’ interests and accommodate people who wish to 'do their own thing' in the company of others. High staff and volunteer ratios allow us to do this.
As people find it harder to be active in their communities, the clubs bring the communities in. Most club days include visits – from musicians (lots of singing and dancing), artists, poets, choirs, special interest groups, churches, museums and many school children and college and university students. Each club has a long-term connection with local primary and further education and the presence of young people brings real joy to club members.
More widely, the work of the clubs informs the practice of local healthcare professionals. Our doors are always open and we love to share our approach. Social work students on placement, local GPs, NHS care co-ordinators and dementia nurses have all found inspiration in our practice.

Robust support network
Family carers are fully involved in our work. The team understand the pressures on families and make time to talk through issues that may arise at home, offering informal emotional support and advice as needed. Families often tell us how invaluable this is in keeping them going as carers. Husbands, wives, partners, adult children and grandchildren of all ages are welcomed into the life of the club and encouraged to spend time with us if they wish to do so.
Particularly in the early days, it is an effective way to reassure a family carer that their loved one is having a good time. The ‘family’ feel of the club extends to social media where wider families are highly engaged with club news and photographs. Many families form friendships through the day clubs for mutual support.
Doing things differently
Not everyone has 'got' what we do over the years or understood both the bigger picture and also very small elements of care that we pay attention to and insist on. My best compliment came very early on in developing the clubs. A somewhat traditional 'from past times' health professional visited, surveyed the room and exclaimed, ‘I don't know what you are doing – it’s all chaos!' I have quoted that ever since.
We embrace the chaos of life, the laughter, the friendships, the difficulties of being human and the infinitely different characters that come through our doors. And, somehow, we make it a club where people with dementia do want to be. CMM
Grant Newton is Head of Day Care at Alzheimer’s Support.
Email: office@alzheimerswiltshire.org.uk : @AlzheimersSupp

Headline sponsor

CMM June 2024 43
BUILDING TOMORROW: CREATING HOUSING AND CARE OPTIONS FOR
ALL – ARCO’S WHAT NEXT? 2024 CONFERENCE
3rd-4th July 2024
Widely recognised as an agenda-setting event for the Integrated Retirement Community (IRC) sector, join the largest, most prominent Housing with Care operators and sector-leading organisations at the What Next? 2024 ARCO annual conference on 3rd and 4th July in London.

Welcoming up to 450 attendees representing over 170 organisations from across the Housing with Care sector, the conference is known for its fresh content where new, innovative ideas are shared first, and for the abundance of networking opportunities, including the attendance of ministers and senior policymakers.
Opportunities abound
A year on from the launch of the Task Force on Older People’s Housing, and with the country heading for a general election, opportunities abound for sector growth so that Housing with Care and IRCs play a key role in transforming the future of the UK’s social care and housing crisis.
This year’s programme, under the title of Building Tomorrow: Creating Housing and Care Options for All, will focus on the key factors underpinning both sector growth and operational excellence. Topics will include:
• Bridging the gap – What are the key factors in enabling the sector to grow at scale, establishing a vibrant market across the spectrum, but with a particular focus on the mid-market? What are the key unit numbers, density and service charge rates to make IRCs available to all?
• A year in focus – The Older People’s Housing
Taskforce has, over the past year, researched existing offers and also the future landscape of older people’s housing in the UK. What will the key recommendations be and how will Government respond?
• The changing face of filial piety – Around 7% of the UK population currently provide informal, unpaid care – often to family members. However, increasingly common reasons to move to an IRC are customers not wanting to burden their families with caring responsibilities or not having family members to rely on. This session explores whether this is a sign of our increasingly fragmented society or simply a logical consequence of families living further apart, high employment rates and an increasing number of people growing old without having had children.
• Is intergenerational living the key to wellbeing for all? – Since the first series of Channel 4’s Old People’s Home for 4 Year Olds hit our TV screens back in 2017, the benefits of intergenerational connections have been evident. We are now seeing more and more operators of IRCs building this into their village offer from the beginning, whether that is integrating with a local nursery group, dedicated IRC units within a larger general residential offer or living alongside medical students as they train. This session explores the key benefits of
intergenerational activities and hears first-hand from residents, operators and parents/students why this is key to building happy and vibrant communities, while also looking at the challenges that need to be overcome to make this happen.
• Mature market mastery: Lessons from NZ –The New Zealand Retirement Village sector is 20 years ahead of the UK’s and benefits from a thriving mid-market and a better customer awareness of what IRCs offer. Following the return of an ARCO member delegation to visit and learn more about the market and operators in New Zealand, the group will share key observations, lessons and insight on what we might want to consider for the UK.
The conference will run over two days and will be held once again at the IET London, Savoy Place on the London Embankment, with The Knowledge Exchange Workshop Day taking place at the London offices of Trowers & Hamlins LLP.
As it is tradition, the main conference day on 3rd July will conclude with a social gathering and networking opportunities at the ARCO Annual Drinks Reception.
Don’t miss out
Tickets are now on sale. Visit ARCO’s website to book your place.
What recommendations are you hoping to see from the Older People’s Housing Taskforce? Visit GOV.UK for more information.
EVENT PREVIEW
44 CMM June 2024

WHAT’S ON?
Event:
Date/Location:
Contact:
Event:
Date/Location: Contact:
Event:
Date/Location: Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location: Contact:
The Alzheimer’s & Dementia Show 14th-15th June 2024, London https://alzheimersshow.co.uk
NQSW Forum 18th June 2024, Online www.skillsforcare.org.uk (search ‘NQSW Forum’).
Midlands and Eastern individual employer and personal assistant framework network webinar 26th June 2024, Online www.skillsforcare.org.uk/Home.aspx (search ‘Personal assistant framework’).
South East Social Care Alliance (SESCA) Conference 26th June 2024, Wokingham www.eventbrite.co.uk (search ‘South East Social Care Alliance’).
CQC ‘Well Led’ Quality Statements – an analysis webinar 2nd July 2024, Online www.careengland.org.uk/events/cqc-well-ledquality-statements-an-analysis
Finding funds, fixing homes: Innovation in local authority provision of home improvement grants and loans webinar 10th July 2024, Online https://ageing-better.org.uk/events/findingfunds-fixing-homes
Supporting staff bereavement in the workplace webinar 10th July 2024, Online www.socialcareconferences.co.uk/virtual-onlinecourses/staff-bereavement-workplace
CMM EVENTS
Event:
Date/Location: Contact: CMM Insight Webinar 4th July 2024, Online Lisa Werthmann, Director, 01223 207770 lisa.werthmann@carechoices.co.uk www.caremanagementmatters.co.uk/webinar/
Please mention CMM when booking your place. Sign up online to receive discounts to CMM events and for more information on our upcoming events in 2024.
www.caremanagementmatters.co.uk @CMM_Magazine #CMMInsight

CMM June 2024 45
H.W.Pickrell Ltd Gardiners Lane North, Crays Hill, Billericay, Essex, CM11 2XE Mobile: 07860 894 331 • Email: sales@hwpickrell.co.uk Telephone: (01268) 521033 www.hwpickrell.co.uk
STRAIGHT TALK
CMM caught up with the new Association of Directors of Adult Social Services (ADASS) President, Melanie Williams, at the organisation’s annual ADASS Spring Seminar, who spoke about her priorities for the year ahead.

Inclusion and diversity
One thing I’m really committed to is our ability to lead on inclusion and diversity. Not just for our workforce but also for people who draw upon care and support. We know that the care workforce is predominantly female. So, we’re largely women and we also have, more than other sectors, people from other protected characteristics: people with disabilities, carers and people from black and other minority communities. So, it’s really important to me that we have that represented visibly in what we do.
That commitment to equality and diversity, race equality standard and leading with being diverse by design, is crucial. The commitment I have to equality and social justice has driven me through my career and lead me to being President today.
Care closer to home
We also have priorities to articulate to the incoming Government. For example, providing care closer to home is going to be really important. We know that there is growing public awareness of health and social care, but the place to get support is almost always hospital, still.
We hear a lot about ‘Well you can’t get a GP if you try’ or ‘People can’t get packages of care and support’ and not all of that is the reality. So, it’s going to be vital that ADASS continues to raise awareness of and improve access to care closer to home. To achieve this, we can

support people by understanding what they want, rather than people feeling that they’ve got to meet a criteria.
I also think that we currently have a system of care where we’re giving people support in crisis, rather than focussing on prevention. We’ll be working closely with Government in the next year to identify how support can be built into communities and provided early on, to avoid crises.
Support for carers
Carers will continue to be one of my priorities. I’m really driven about the role of carers and they constantly tell us that they want advice and guidance and support when it’s needed. We know that carers often are stuck trying to navigate things at the worst times and the support isn’t always there. In Nottinghamshire, for example, carers tell me that the support is good when they get it, but it takes a while or they don’t know how to get there.
So, one of the things that I’ll be looking to the incoming Government to do, but also ADASS’ membership, because there is a lot we can do ourselves, is to focus on that information, advice, guidance and support offer. We are asking broadly for a whole range of interventions for carers, such as carers’ leave and a focus on carers’ poverty because we know that carers have been really impacted by the cost-of-living increases. Living with a disability, spending more time in the home or having certain needs because
you’re older or more isolated can mean that you’re more likely to use more energy.
Workforce
I don’t think there is really an accurate public narrative about what social care does. Social care is quite amazing; there’s a whole diverse set of interactions, relationships and ways that we support people everyday that I don’t think is really well understood by the public.
People who work in social care, if they’re a care worker, social worker or occupational therapist, often don’t feel there is recognition or support targeted towards managing their wellbeing. All too often, we also hear that there is a lack of public understanding about what the social care workforce does. The public sees social care through the lens of the NHS, or worse, thinks that social care is delivered by the NHS.
So, increasing that pride in our workforce is really important to me. We’re also looking for the long-awaited workforce strategy from Government that Skills for Care is leading for the sector. We want this work to be funded by Government so that we can think about creating robust career pathways and fairer pay terms and conditions, amongst other things.
This is because of what we know about those of us who work in social care: pay is important but it’s one of a bundle of things. It’s not just about pay, it’s about having a full-time contract, having some certainty about work, being valued but importantly, being trained, developed and having some idea of progression within the sector.
46 CMM June 2024
Which areas of the sector would you like ADASS to focus on in the year ahead? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts. Melanie Williams is ADASS President and Corporate Director of Adult Social Care and Health at Nottinghamshire County Council. Email: team@adass.org.uk : @1adass


Education and training for the social care workforce
If you work in adult social care, Macmillan’s Social care community on the Learning Hub is the go-to place for free education and training on cancer care.
There are over 20 on-demand e-learning courses, bitesize resources and virtual classrooms to develop your knowledge and skills in supporting people affected by cancer.
This community is for all staff working in adult social care who want to improve their understanding of cancer and skills in supporting people affected by cancer. This includes staff working in residential care, nursing homes, home care, sheltered accommodation, assisted living and day centres.
In the community you’ll find the following topics:
• Cancer awareness
• Cancer and other conditions
• Communication skills
• Personalised care
• Palliative and end of life care
Scan the QR code to log in or register for an account, then search ‘Social care community’
 Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland.
Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland.

SIGN UP FOR
FREE PROVIDERS
Yes, that’s right. Absolutely free.
Gain CPD points
Access extended features and additional content
Read latest news email alerts
Comment on features and debate on important subjects
Access archived editorial
Receive a digital edition of CMM (10 issues per year)










Sign up at www.caremanagementmatters.co.uk @CMM_Magazine
Designed by Evan Ho buhr












































































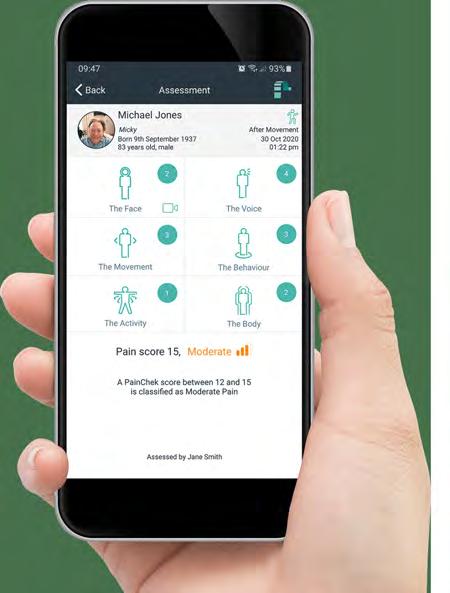

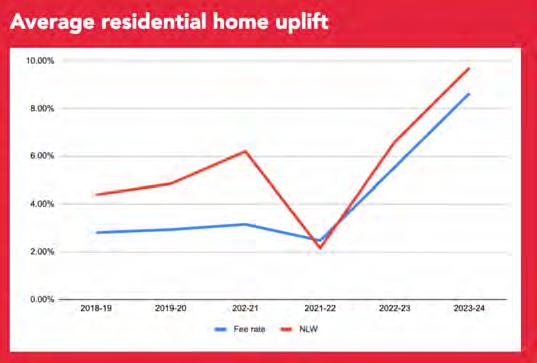

























 Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland.
Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland.





