5 minute read
Alumni Healthcare Heroes
Over the course of these past six-plus months, the world has witnessed a new kind of superhero emerge—one who doesn’t wear a cape. Instead, these champions have treated the sick and the injured on the frontlines during a once-in-a-century pandemic. They’re our healthcare heroes, and we are proud to feature the stories of two alumni, Anthony Oddo ’07 and Katherine Vendley Lynch ’09, who have been working in their respective medical fields throughout the COVID-19 crisis. Read on to learn, in their own words, about their experiences.
Anthony Oddo ’07 earned his degrees in Anthropology and Chemistry at Emory University in 2011. Subsequently, he worked two years as a high school science teacher on the TexasMexico border as a Corps Member with Teach For America. In 2017, he attained his MD at Wright State University’s Boonshoft School of Medicine in Dayton, Ohio, where he met his wife, Betsy, who is also a pediatrician. Dr. Oddo completed his general pediatrics residency at the University of Tennessee Health Science Center in Memphis before moving to Charleston, SC this summer, where he will practice at Mt. Pleasant Pediatrics.
During the pandemic outbreak, I was a resident physician in general pediatrics and my assignment for the month of March was to be a night shift supervising doctor. As such, I supervised general admissions to the hospital overnight, and furthermore, I was assigned to be the sole provider to evaluate and take care of all of the COVID-19 patients who were admitted to the hospital overnight. At that time, with so little evidence-based information about the virus, it was both an exciting and intimidating experience. I embraced my role as a valuable opportunity to reinforce our safety protocols and to be flexible as new guidelines were released by the CDC and our state department of health throughout those weeks.
I was later assigned to the emergency department, where new safety measures were in place to best help protect our patients and providers. Employees and families alike were asked multiple screening questions and had temperatures taken. It was an adjustment to these new measures, but it also acted as a great time to reflect and to analyze our current practices in order to create safer ways to practice medicine. I helped take care of multiple patients who were undergoing COVID work ups, and it was a unique experience to be the first physician to encounter some of these patients.
This summer, I have since completed my residency training and have relocated to Charleston, SC, where I will join a pediatrics private practice. Already amidst the anticipated challenges of working independently for the first time, working in a new job, and working in a new city, I am also faced with the responsibility of being knowledgeable about the latest national and local recommendations in taking care of my personal patient population. As I prepare to start in August, I am doing my best to stay up to date and to educate myself as much as possible to make informed recommendations to my patients and families.
Overall, fortunately, the pediatric population has had a much lower rate of COVID-19 diagnoses and related-illnesses, such as the multi-system inflammatory disease. Similar to the adult patients, we have children who are at known increased risk
due to pre-existing comorbidities, who we work hard to help protect. My main message that I would like to share is that I am thankful for the measures that individuals have taken to be as healthy and safe as possible. I encourage everyone to keep creating new ways for us to interact remotely and

I was fortunate enough to have my son the week prior to COVID-19 hitting Sumter, South Carolina. Therefore, I was on maternity leave during the initial scary times (thank goodness)! But since being back to work, Sumter has turned into one of the “hotspots” in South Carolina. Our hospital is currently full. The ICU is full of COVID patients again. Therefore, we have to cancel all surgeries that require the patient to stay in the hospital for an extended period of time. (Hip/knee replacements, hysterectomies, carotid endarterectomies, to name a few.)
We have had COVID positive patients in the OR. Just last week, there was a patient who needed a colonoscopy (due to bleeding) and they were COVID positive. That was quite a scare for me. The scary part about a colonoscopy is this patient does not have a breathing tube. It is one thing to intubate a patient and have ten seconds of heart-throbbing fear placing the tube, but a colonoscopy can be 30-45 minutes of the nurse anesthetist being right near the patient’s airway keeping them asleep, yet still breathing! In the OR, we have to remove everything that can’t be wiped down. This includes syringes, tape, gauze, EKG leads, AMBU bags, ETT tubes, to keep social distancing appropriately, including wearing masks and limiting trips outside of the home. And if you are debating about going to a social gathering or doing something else, I ask that you err on the side of safety when possible.
Katherine Vendley Lynch ’09 graduated from Clemson University with her nursing degree in 2013. She worked as a RN in the NeuroTrauma ICU in Greenville, SC for two years, then went back to nurse anesthesia school in 2016 at the University of South Carolina. She received her masters in nurse anesthesia and became a Certified Registered Nurse Anesthetist (CRNA) in May 2018. Katherine married her college sweetheart in March 2019, had her first son, Christopher Jr. in March, and is currently working as a CRNA at Prisma Health Tuomey in Sumter, SC.
and oxygen masks. So when we have a COVID-positive patient or a pending test (we treat them as positive until the results come back), I have to truly think through what I need, or what I will potentially need with me. The room feels so empty. It’s also scary that when we need something, we usually need it fast, and not having our supplies right there with us can make the job even more stressful! We still do paper charting, and so we can’t even bring the chart in the room or else we will have to throw it away. We have another CRNA outside the room charting for us.
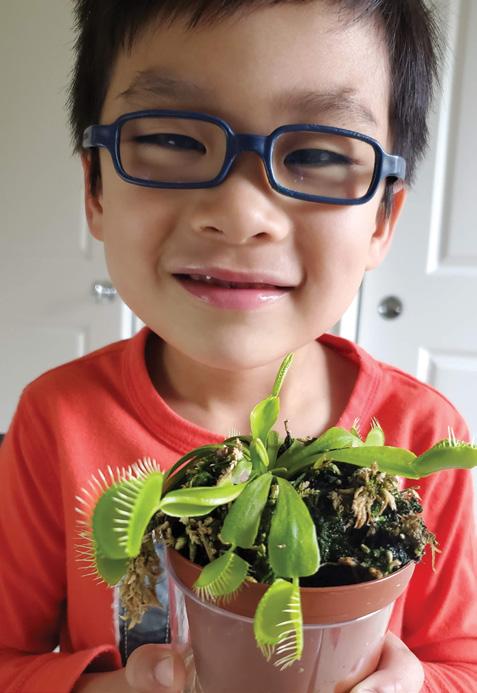
It has also been extra scary having a young child at home. I was always very diligent about having “OR shoes” that I leave at the hospital. But now I am ten times more cautious of what I could potentially bring home to my son.
That being said, I love my job. I wouldn’t change it for anything. A lot of times people are more scared of the anesthesia than the actual surgery. I’m the last person people see before they put their lives in my hands. I try and always take the extra time to make my patients feel comforted, knowing I am going to take the best care of them.