Pathways Access Digital Edition Seepage4 Canada’s Lymphedema Magazine Empowering patients and professionals CLINICAL PERSPECTIVES • RESEARCH ADVANCES • HINTS AND TIPS • EDUCATIONAL EVENTS SUMMER 2023 Canadian Publications Mail Sales Product Agreement No. 40065546 Melanoma and lymphedema Compression garment fitting Implementation Science Melanoma Risk factors and sun safety
Effective compression.
Sustained, therapeutic compression for up to seven days, with less slippage and increased comfort means more time worn. Clinically proven to be more effective at managing edema.1

Focus on living life.
The thin, lightweight materials create a breathable sleeve, allowing patients to wear their own shoes and clothing. The increased comfort helps mobility leading to more effective treatment.
Designed with comfort in mind.
72% of patients prefer two-layer compression over alternative options.¹ Treatment is more effective when their comfort is prioritized.
Engineered for comfort. Designed for real life. 3M™ Coban™ 2 Two-Layer Compression System Learn more at www.3M.ca/lymphedema
Trust the 3M ™ Coban™ 2 Two-Layer Compression System to get life back on track.
1. Moffat C et al (2012) ‘A preliminary randomized controlled study to determine the application frequency of a new lymphoedema bandaging system.’ British Journal of Dermatology 166.3: 624-632. 3M, 3M Science. Applied to Life., and Coban are trademarks of 3M. Used under license in Canada. Please recycle. © 2021, 3M. All rights reserved. 2107-21114-E This material is intended for healthcare professionals. Please refer to the full product instructions and indications for use and for a full list of contraindications, general considerations and warnings, cautions and notices. If applicable, refer also to your facility policy for detailed information and recommendations. 3M Deutschland GmbH Health Care Business Carl-Schurz-Str. 1 41453 Neuss Germany Available in Canada from: Medical Solutions Divison 3M Canada 300 Tartan Drive London, Ontario N5V 4M9 Canada 1-800-364-3577 3M.ca/Medical
Sunshine is the best medicine (or is it?)
Summertimeis here and most readers are eager to get outside and enjoy the warmer weather. Sunshine certainly can lift our spirits and make everything look brighter. However, what we might have been told as youngsters still holds true. Careful consideration is required to be in the sun safely.


Melanoma Canada is one of the Canadian Lymphedema Framework’s partner organizations. We are pleased to have them contribute to our magazine. It was alarming for me to read that melanoma is the fastest growing cancer in Canada and tends to strike a younger population. Abigail Wiggin’s sun care safety tips will prepare us for the warm summer days ahead. We encourage you to visit the Melanoma Canada website (www.melanomacanada.ca) to learn more about how you can minimize your risks for this serious cancer.
Of all cancer-related lymphedema, melanoma is the third most common after breast and gynecological cancers. We had a chance to chat with the multidisciplinary team at the McGill University Hospital Lymphedema Program about their clinical experiences with melanoma and lymphedema. We are grateful to Dr. Anna Towers, Marize Ibrahim, Marie-Eve Letellier and Angela Yung for sharing their insights.
Darek Mikita is a man living with lymphedema as a result of melanoma. He shares his experiences and promotes the importance of early detection, treatment options and staying active. Some minor adjustments to his lifestyle and sports activities allow him to still participate in the sports he loves and continue an active lifestyle.
An important component of the treatment protocol Darek follows is ensuring he wears the right compression garment. Getting properly fitted and having a good relationship with your fitter is essential. Two experienced garment fitters who contributed to this issue are Yasmin Ejbick and Alla Hardoon. They share some strategies for selecting appropriate compression for clients to control their swelling and to fit their lifestyles. Look for additional authors and articles on compression fitting (with some case studies) in our Fall issue.
The Canadian Lymphedema Framework is also planning a special session on garment fitting at the National Lymphedema Conference this fall. We hope you have saved the date on your calendar and will register soon for this event, taking place in Toronto on Nov 3-4, 2023. The theme of the conference is ‘Moving Forward Together.’ Both health professionals and patients will learn from experts and hear about new research in the field of lymphedema and lipedema.



How new evidence-based research gets translated into everyday practice is the focus of the article by Liz Dylke. Her overview of the emerging Implementation Science opens up our understanding of significant barriers to implementing research findings, including practitioners having insufficient knowledge, skills or resources to deliver the practices in their clinical environment. Attending conferences is one way for lymphedema practitioners to stay up to date on new developments to incorporate into their practice. We hope you have secured your spot at the CLF National Lymphedema Conference.
Hope to see you in Toronto this November! LP

https://www.canadalymph.ca/conference/


Editor’s Message Moving Forward Together November 3-4, 2023 Toronto Airport Marriott Hotel 901 Dixon Road, Toronto ON Toronto, ON Canada Register | Submit an Abstract Sponsor/Exhibit | Learn More canadalymph.ca/conference
Summer 2023 www.lymphedemapathways.ca 3
Anna Kennedy
Melanoma
The dark side of the sun.
Summer 2023 n Volume 12 Issue 3
Publisher
Pathways is published four times per year by BCS Communications Ltd. on behalf of the Canadian Lymphedema Framework.
Editorial Board
Mei Fu PhD RN FAAN

David Keast MD FCFP
Lori Radke PT CLT
Anna Towers MD FCFP
Editor
Anna Kennedy
Executive Director
Bonnie Baker
Editorial Assistant
Nicole Boulet
Advertising and Submissions
We welcome your ideas, contributions, letters and ad copy. While all material is subject to Editorial Board approval, inclusion does not constitute an endorsement or reflection of the views and opinions of the CLF and its Editorial Board. Contents may not be reproduced without written permission of the Canadian Lymphedema Framework.

Subscription Rates (1 year)
Canada - $30.
United States - $60. International - $75.
Single copies and back issues - $8.
Subscriptions/return mail to Canadian Lymphedema Framework 4800 Dundas Street West, Suite 204 Toronto, Ontario M9A 1B1

Telephone: 647-693-1083
Email: pathways@canadalymph.ca www.canadalymph.ca
Photos: D. Mikita, Melanoma Canada, lymphedivas.com, lymphedemablog.com, www.medi.de
All stock images are CanStock. Canadian Publications Mail Agreement 40065546

ISSN 1929-1418 • Printed in Canada

We acknowledge the financial support of the Government of Canada.
Melanoma and lymphedema

A clinical roundtable discussion.
The right fit is key Interviewing compression garment fitters.
The new “science” of Implementation Science Incorporating evidence-based research

https://www.canadalymph.ca/workwithus/

4 www.lymphedemapathways.ca Summer 2023 Contents
CANADIAN
Financé par le gouvernement du Canada Funded by the Government of Canada
LYMPHEDEMA FRAMEWORK PARTENARIAT CANADIEN DU LYMPHOEDÈME
.............................................
............................................
Partner profile Melanoma Canada.
............................................
......................................................................
into everyday practice. ...................................................................... How to live better with lymphedema: Meet the experts Book review. ..................................................... Living with lymphedema successfully The importance of early diagnosis, treatment and staying active. ..................................................... DEPARTMENTS: Hints and Tips 24 Did you Know? 25 Letters to the Editor 26 Canadian and International Events 26 Your print subscriptio complimentary digita FOR PATHWAYS SUBSCRIBERS REQUEST ACCESS ONLINE OR BY EMAIL www.tinyURL.com/yes-digital pathways@canadalymph ca W O U L D Y O U L I K E T O W O R K W I T H U S ? Support special projects or events Help with day-to-day operations. E X P L O R E V O L U N T E E R O P P O R T U N I T I E S c a n a d a l y m p h . c a / w o r k w i t h u s Write for us Tell us your story Share your clinical experience Join a committee or our Board 5 8 10 15 18 21 22
Melanoma The dark side of the sun
By Abigail Wiggin
Asthe days get longer and warmer, the first thought many Canadians have after a tough winter is about hitting the beach or pool and soaking up some sun. Unfortunately, that bright sun has a very dark side and is responsible for causing up to 85% of all melanoma cases.
Melanoma is a potentially deadly form of skin cancer that develops when the melanocyte cells of the skin grow rapidly and divide uncontrollably, eventually causing a cancerous growth or tumour. Melanoma is one of the most common cancers diagnosed in Canadians aged 15 to 59. It is also one of the few cancers with rapidly rising rates of diagnoses and incidence rates have been climbing for the past 25 years.
Overexposure to the sun and artificial sources of ultraviolet radiation is one of the most significant and preventable causes of melanoma. The impact of high amounts of UV radiation on the skin is so severe that just one blistering sunburn before the age of 20 significantly increases the chance of a melanoma diagnosis. Tanning bed usage even further increases these odds, and among those who first used a tanning bed before the age of 35, the risk of a melanoma diagnosis increased by 59%.
The bright side is that melanoma is very preventable, often easily detectable, and simple lifestyle changes and daily habits can have a huge and lasting impact. A sunburn may seem temporary, but the impacts of sun damage on the skin are long lasting. Let’s start summer 2023 on the right foot by implementing safe summer skin care now.
Protect yourself like a pro
Sun safety is essential for preventing melanoma or other forms of skin cancer from occurring. Sunlight is made up of both UVA and UVB rays, both of which penetrate the skin and cause damage. UV rays can also go through clouds, windows, fog, haze, car windshields, and lightweight clothing. To protect yourself from the sun and UV rays you can:
1 Limit the time you spend in UV rays

• Avoid outdoor activities when the sun is strongest, between 11 a.m. and 3 p.m. If you are outdoors during these times, stay in the shade as much as possible.
• Protect yourself from sunlight reflected by water, ice, snow, sand and pavement. If you’re sitting on a dock this summer, remember that UV rays reflected off water increases your UV exposure by 25%.

2 Wear protective clothing
• Clothes made of tightly woven fabrics that cover your arms and legs (for example, see-through materials are not tightly woven)
• Special sun protective clothes with ultraviolet protection factor (UPF) 50 or more.
• A hat with a wide brim that shades your face, neck, and ears.
• Sunglasses with 100% UVA and UVB protection.
Abbie Wiggin is the Manager, Community Programs and Resources at Melanoma Canada where she connects with melanoma and skin cancer patients and caregivers, providing counselling services, healthcare navigation, and advocacy. She also facilitates support services such as the Cancer Coaching program, Peer-to-Peer program, and monthly support groups.

Overexposure to the sun and artificial sources of ultraviolet radiation is one of the most significant and preventable causes of melanoma. The impact of high amounts of UV radiation on the skin is so severe that just one blistering sunburn before the age of 20 significantly increases the chance of a melanoma diagnosis.


3 Use sunscreen the right way
• Apply a broad-spectrum, water-resistant sunscreen with a minimum SPF of 30, ideally SPF 50, 30 minutes before sun exposure.
• Reapply every two hours, or more often after sweating or swimming.
4 Remember, there is no such thing as a safe tan
• There is no such thing as a healthy or safe tan and any tan or change in skin colour is a sign of skin damage.
• The concept of a “base tan” (the idea that a light tan will prevent burning) is a myth and a “base tan” provides little to no protection against sunburn or sun damage.
• Tanning is not a safe source of vitamin D, which is best achieved through maintaining a healthy, vitamin D-rich diet, and taking vitamin D supplements.
ABCDE: 5 letters that can save your life
Survival rates for melanoma are high when it is detected early and unlike other cancers, melanoma is often clearly visible to the naked eye on the skin. Because about 75% of melanomas are detected by patients themselves, we recommend monthly skin self-examinations using the ABCDE’s of
Summer 2023 www.lymphedemapathways.ca 5
Clinical Perspective
ABCDE: 5 letters that can save your life
A – Asymmetry The two halves of the mole have different shapes.
B – Border The edge of the mole is irregular. It may look blurred, ragged, or notched. Pigment may spread into the skin around the mole.

C – Colour The colour of the mole is uneven. The mole may have different shades of tan, brown, and black, sometimes with blue, gray, red, pink, or white.
D – Diameter
While melanomas are usually greater than 6 mm (the size of a pencil eraser) when diagnosed, they can be smaller.
E – Evolving
Example:
The mole has changed in the past few weeks or months. It may be itchy, scaling or bleeding.
Source: American Academy of Dermatology aad.org
https://www.aad.org/
melanoma. If you detect any changes to your moles or skin, contact your doctor for a referral to a dermatologist as soon as possible.

Sign up for our skin check reminders
Scan the QR codes or visit: melanoma network.ca/3ways


Warning signs of melanoma
Normal moles tend to have an even colour and can be pink, tan or brown. They are mostly round or oval and smooth. They also tend to be smaller than the width of a pencil eraser. The first signs of melanoma can be:

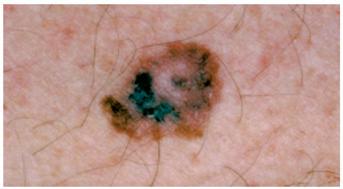
• A change in a mole you already have, such as a change in its shape, colour, size, surface, or texture.
• A new mole that appears.
• In some cases, the first sign of a problem is a swollen lymph node.
The odd ones out
Some forms of cutaneous (skin) melanoma, such as acral lentiginous melanoma, mucosal melanoma, and subungual melanoma, are often found on areas of the body that are not typically exposed to sunlight/high UV radiation, such as the soles of the feet, in between toes, nasal passages, or even genital and anal areas. Because melanoma is a cancer of melanocytes, which are found within skin cells, melanoma can potentially form anywhere on the body. These forms of melanoma are relatively rare and are not known to be caused by UV radiation, but monitoring and checking your body, including those areas that are less exposed to the sun, is still essential in potentially detecting any abnormalities or growths.
Other important factors
Melanomas can look very different from each other:
• Some melanomas may have all the ABCDE signs, others may only have one or two.

• Some forms of melanoma do not follow the ABCDE rule at all (for example, nodular melanoma follows the EFC rule: elevated, firm, and growing).
• Acral lentiginous melanoma can present as dark spots or bruises on the palms of the hands or soles of the feet that do not go away or won’t heal.
• Subungual melanoma can present as a dark vertical stripe on the fingernails or toenails.
Advanced melanomas may have changes in their texture or feel, and may:
• Become hard or bumpy.
• Look scraped or raw, and it may ooze or bleed.
• Be itchy, sore, or even painful.
Since not all melanomas fit the ABCDE pattern, always keep a look out for the “ugly duckling”—a mole or lesion that does not look like the others that you have. If it is changing, itching, bleeding, or scabbing, visit your doctor for a referral to a dermatologist.
Watch our guided skin self-exam video
Skin cancer can be a big deal. Checking for it isn’t. Scan the QR code for a guided skin exam.
Melanoma risk factors
• UV radiation exposure is the most significant risk factor for developing melanoma.
• 85% of skin cancers are caused by UV radiation and overexposure is the number one preventable risk factor for melanoma.
• Even just one severe sunburn with blistering raises the risk of developing melanoma.
• Sustaining just five sunburns as a teenager can make an adult 80 percent more likely to develop melanoma during their lifetime.
• The total amount of sun exposure in your lifetime is a risk factor, especially if it is high.
• People who habitually tan during adolescence and young adulthood have a higher risk of developing melanoma skin cancer later in life.
• Even people who tan without burning have a higher chance of melanoma due to high overall and prolonged exposure to the sun.
6 www.lymphedemapathways.ca Summer 2023
Nighttime
maintenance for e ective treatment of lymphedema Introducing Juzo Night


The wait is over!
Foam channels




Removable fasteners
Easy to put on and take o
Thumb guard

Keeps edema from shifting
Follow lymphatic pathways, promoting lymphatic drainage
Prevents bunching and skin irritation, protects pressure points
Cooling material
Wicks moisture, reduces sweating

https://www.juzo.ca/ emailto:support@juzo.ca
Juzo introduces Juzo Night, a lightweight, comfortable garment that helps prevent edema from rebounding during sleep or rest. Call or email us to learn more 1-844-229-4999 • support@juzo.ca • Juzo.ca • Juzo Canada Ltd.
Anatomical angle
Canadian Melanoma Statistics
87,000 Canadians were diagnosed with melanoma in 2021 (an 8.5% increase from 2020).
1 in 41 males
1 in 51 females Based on annual trends from the past 40 years, melanoma rates have increased 2.2% each year in men, and 1.4% each year for females.
Canadian Cancer Society (https://cancer.ca/en/research/cancer-statistics/canadian-cancer-statistics)
• Tanning beds and sun lamps produce artificial UV light and therefore increase the risk of melanoma.
A personal or family history of melanoma is also a risk factor.
• People who have had a past melanoma have a higher chance of developing another.
• Having at least two close relatives with melanoma is also a risk factor, as it can run in families.
Partner Profile
Certain physical features are also risk factors for melanoma including:
• People with pale skin, who burn easily, have a higher chance of melanoma. These people may have blonde or red hair, blue or gray eyes, or many freckles.
• Having many (or more than 50) moles raises the chance of skin cancer.
• Atypical moles (or dysplastic nevi) often run in families. A dysplastic nevus
has a greater chance of turning into melanoma than a normal mole, but the risk is relatively low.
• Dysplastic nevus syndrome (also called familial atypical multiple mole melanoma syndrome, or FAMMM) is an inherited condition where someone has many dysplastic nevi and usually a close relative who has had melanoma. People with this condition have a very high risk of melanoma.
Melanoma Canada


Melanoma
Canada is a national organization dedicated to advocating for and supporting Canadians who are living with or have been impacted by melanoma and skin cancer. We focus on providing helpful resources for patients and the public, crucial sun safety education and melanoma awareness, and psychosocial support programming to patients and their loved ones. Melanoma Canada was founded in 2009 by three-time melanoma survivor, Annette Cyr, to respond to the need for Canadian melanoma and skin cancer patients to have an organization that was focused on coordinating education and prevention efforts. Additionally, Melanoma Canada was created to provide a strong voice for advocacy in targeting funding for melanoma research and improved access to care and treatment options.
Our mission as an organization is to:
4 Support our community through current and coordinated information and services.
4 Educate Canadians on prevention, detection, and available treatment options.
4 And to advocate for timely diagnoses, improved access to care across the country, and for the best and most effective treatment options to be widely available.
We value above all:
4 Being supportive to every person affected by melanoma and skin cancer at every stage of disease or journey.
4 Being passionate about access to credible information and effective treatment.
4 Being trusted as a reliable resource for the public and our industry partners.

Lifetime probability of developing melanoma by gender in Canada: 1 in 41 males, 1 in 51 females. Contact
https://www.melanomanetwork.ca/
Our support programs include:
4 Cancer coaching
4 Phone and e-mail support
4 Peer to peer support
4 Monthly support groups
4 Private Facebook groups
4 Private online chat
4 Patient information sessions
4 Patient guides and publications
4 Clinical trial finder
Melanoma Canada’s ultimate goal is to live in a world with zero melanoma and skin cancer related deaths. LP
8 www.lymphedemapathways.ca Summer 2023
confidential.
us: Available Monday to Friday, 9 a.m. – 5 p.m ET. We aim to respond to all inquiries within 48 hours. All calls and emails and are
1.877.560.8035 x112 support@melanomanetwork.ca • melanomacanada.ca
Other risk factors that can increase your risk of melanoma are:
• Age - About half of melanomas develop in people older than 50 years.
• Medicine - Some medicines, like antibiotics, hormones, or antidepressants, increase sensitivity to the sun and as a result can raise the chance of melanoma.
• Lowered immune system - The immune system fights infection and removes damaged cells. Some diseases and some medicines weaken the immune system. This can raise the chance of melanoma.

Melanoma does not discriminate Melanoma can occur in anyone, regardless of age, gender, or race. Whilst people of colour are less likely to be diagnosed with melanoma than individuals with light skin, they are four times more likely to be diagnosed at an advanced stage, and often face far worse health outcomes because of delayed diagnoses. Additionally, if diagnosed with
melanoma, people of colour are most often affected by acral lentiginous melanoma (ALM) or subungual melanoma (SM). This summer (and year-round!) it is important to remember that having darker skin, or skin with more melanin, does not provide sufficient protection from UV radiation, and individuals with darker skin tones are still recommended to practice the previously mentioned sun safe habits.
ALM and SM present differently than more common forms of melanoma and are often mistaken and misdiagnosed as bruises on the feet, toes, or fingernails. For more information on detecting these forms of melanoma, please watch our Melanoma Does Not Discriminate video and visit: https:// www.melanomanetwork.ca/skin-of-colour/
Safe summer skin
There is no denying the impact of the sun on our skin and the risk it poses for developing melanoma. Environmental
changes in climate and ozone layer depletion also play a role in increasing our vulnerability to the damaging effects of UV radiation. As we enter spring and summer, don’t forget to practice sun safe habits, monitor your skin, and visit your doctor if needed. A fun summer is one you won’t regret down the line. After all, the skin is your largest organ, so show it some love. LP Watch
Summer 2023 www.lymphedemapathways.ca 9
the Melanoma Does Not Discriminate video: https://www.melanomanetwork.ca/skin-of-colour/
This summer (and year-round!) it is important to remember that having darker skin, or skin with more melanin, does not provide sufficient protection from UV radiation, and individuals with darker skin tones are still recommended to practice the previously mentioned sun safe habits.
Melanoma and lymphedema A clinical roundtable discussion
 By Marize Ibrahim, Angela Yung, Marie-Eve Letellier and Anna Towers (in discussion with Anna Kennedy)
By Marize Ibrahim, Angela Yung, Marie-Eve Letellier and Anna Towers (in discussion with Anna Kennedy)
Pathways had the opportunity to host an online roundtable discussion with the team at McGill University Health Centre Lymphedema Program, regarding melanoma and lymphedema. Their clinical insights are captured in this article, along with the facts, statistics and references they kindly sourced and provided.
What is the prevalence of melanomarelated lymphedema in Canada?


Statistics are currently very difficult to find. The new international review being carried out later this year (see callout ) may shed some light. However, assuming the incidence of lymphedema after melanoma treatment is 20%, we will have 1800 new melanomarelated lymphedema cases per year in Canada. Assuming these persons, who tend to be younger, survive 25 years, the prevalence would be 45,000 persons in Canada living with lymphedema due to melanoma, or about 14% of all cancer-related lymphedema cases (using the 2018 estimate of total prevalence of 330,000 from The Canadian Lymphedema Framework).1 Most of these cases are undiagnosed and untreated. Canadian health care providers are more aware of breast cancerrelated lymphedema, and much less so of lymphedema related to other cancers.
A new review on the prevalence of lymphedema is being carried out this year in an international collaboration, spearheaded by the Lymphology Association of North America (LANA), in which the McGill group is participating. The results are scheduled to be published in early 2024 and are expected to shed some light on the prevalence of melanoma-related (among many other secondary cancerrelated) lymphedema in North America and abroad. Funding is being provided by the American Cancer Society.
Is there a difference between upper and lower extremity lymphedema incidence rates?

The development rate of lower extremity lymphedema in melanoma related lymphedema has a wide range.2
Lower extremity
7.6% to 35.1% after SLNB
48.8% to 82.5% after ILND
Upper extremity
4.4% to 14.6% after ALND
Marize Ibrahim PT, Angela Yung PT, Marie-Eve Letellier PhD and Anna Towers MD, work together in the McGill University Hospital Centre Lymphedema Program (Montreal, Quebec). All of them are recognized authors and presenters on lymphedema and regular contributors to Pathways magazine. They are involved in various research projects to develop novel treatment, assessment and imaging methods for lymphedema. In 2021, this group and their network were recognized as Canada’s first LE&RN Centre of Excellence—to date the only Centre to be so designated in Canada.
What are the risk factors?
Chronic lymphedema after axillary lymph node (LN) dissection is approximately 10%, whereas it can be up to 35% after inguinal LN dissection. The type of lymphadenectomy, whether sentinel lymph node biopsy (SLNB), axillary lymph node dissection (ALND) or inguinal lymph node dissection (ILND) also impacts risk, with a greater risk associated with ILND than ALND and a greater risk for ALND than SLNB. Studies have also concluded that groin dissection, diabetes, high body mass index (BMI) and peripheral vascular disease increase the risk of lymphedema for melanoma patients.3
Why is there more lower limb lymphedema (LLL) after melanoma compared to pelvic cancers?

The rate of development in LLL is strikingly high (48.8%), compared to pelvic cancers, such as gynecological and prostrate cancer, because it involves the inguinal rather than the deep nodes.2 LLL following melanoma treatment has a different physiopathology

10 www.lymphedemapathways.ca Summer 2023
Clinical Perspective






https://www.woundscanada.ca/
All institutions designated as a Center of Excellence have been evaluated by international leaders in an extensive review process. https://lymphaticnetwork.org/centers-of-excellence.
from the LLL secondary to lymphadenectomy for pelvic cancer. American and European guidelines recommend pelvic lymphadenectomy and para-aortic lymphadenectomy in advanced gynecological and prostatic cancer.4 However, the difference is that these lymphadenectomies preserve the superficial limb lymph nodes, whereas they are removed during the ILND for melanoma. This is the cause of the higher rate of LLL in melanoma.
Does a melanoma lymphedema patient present later, rather than earlier, compared to the typical lympedema patient?
In general, lymphedema related to melanoma is underrecognized and so our concern is that they are not being diagnosed at all. The majority of melanoma sufferers are male (56% male vs. 44% female)5 who tend to be less concerned about body image issues and less likely to ask for help. Melanoma patients are also typically younger than other cancer patients.6 For many it’s a busy stage in their lives of juggling work and the demands of young families that make it difficult to find the time to come for assessment and treatment.


Lymphedema following melanoma treatment will usually start as mild painless swelling at first, as happens following breast cancer.
Why do you think these patients might not be referred appropriately and how might this be different than other secondary lymphedema patients? Because melanoma prevalence is not as high (7th most commonly diagnosed cancer in Canada) compared to breast cancer (1 in 8 women in Canada), lymphedema in these patients doesn’t get the same level of attention. Although there are prospective surveillance established programs for breast cancer, they have not yet been developed for many other types of cancer, including melanoma.
What can be done to increase awareness and knowledge among health care providers?
This article is a good first step, as is the new collaborative partnership between the Canadian Lymphedema Framework and Melanoma Network of Canada. We are doing well in the area of breast cancer, in that all major cancer centres across Canada, have at least one physiotherapist trained in lymphedema. Most are designated to work exclusively with breast cancer patients as these centres may not have the resources to expand beyond that. We are always competing with other priorities that these therapists might have. However, staffing with just one lymphedema-trained professional in a major cancer centre is not enough. You need more therapists to deal with all lymphedema patients. The problem is funding. As an example, to date, the McGill Lymphedema program at MUHC has had therapists for 15 years now and 90 percent of our funding has come from a breast cancer foundation. We are still charitably funded and not yet integrated into the health care system.
Is the treatment plan for melanomarelated lymphedema any different than for other types of lymphedema?
Following diagnosis, the treatment plan for this cohort of patients is similar to that of other lymphedema patients:
1—Decongestive therapy to reduce the swelling.
2—Compression therapy (bandaging and garments) to maintain the reduction in limb volume.
3—Exercise therapy and
4—Skin care.
These patients must be even more diligent in their skin care regime (like wearing higher SPF and covered clothing) because of the increased risk that sun exposure will further damage their skin.
How is compression more difficult to address in these patients?
Melanoma patients present uniquely in many ways. Depending on how much of the cancerous area required a wide local excision of the melanoma site, the circumference of the limb above or below the surgical site can be much less and may form an uneven limb shape. There could also be anatomical variations, including concave areas that can create a tourniquet, if not treated properly. Some patients may also have double limb lymphedema, where multiple melanoma locations were treated and/or skin grafts were taken from the contra-lateral limb. An experienced therapist requires creative solutions to ensure bandaging is done correctly, with swell spots and other customized tools so that a tourniquet is prevented and compression garments are fitted properly for the comfort of the patient. Unique compression challenges need to be addressed adequately, with the therapist being aware that in this population, many patients are still working and aesthetics may be more of a concern for them. Also, the patient population is younger compared to other cancers. It is one of the commonest cancers in young adults.
Why do these typically younger patients have more difficulty with adherence?
The challenge of working with younger patients is that their challenges are very different. This particular patient population ranges from young adults, who are busy with school and university, to young parents, who are at a stage in their lives when busy work schedules and looking after young children don’t allow much time for themselves. After their challenging diagnosis and cancer treatment is completed, they want to forget about their ordeal and are eager to get

12 www.lymphedemapathways.ca Summer 2023
The Centre of Excellence designation indicates that the MUHC Lymphedema Program is an institution that sets the highest standard for best practice multidisciplinary care in the management and care of lymphatic diseases.
back to living a normal life. It is much more than just the compliance of donning a compression garment every day. Active participation in their care requires the time-consuming phase of getting monitored and assessed, numerous appointments for decongestive therapy, getting fitted for garments and learning how to actively participate in skin care and exercise. All of this seems too onerous for many of them.
A closing message for therapists
Unfortunately, most of the resources for publicly funded lymphedema treatment centres are supported by grant funding and donations related to breast cancer foundations.
If your physiotherapy facility (whether hospital-based or private clinic) doesn’t currently have an outreach program for melanoma patients, we encourage you to consider this and advocate for the resources. These patients need the same level of follow-up and prospective surveillance
as patients suffering from other better-known cancers. Everyone that has melanoma in the lower limbs needs to be educated and followed up, as the risk they have in developing lymphedema is extremely high. Although therapists might be more familiar and comfortable treating breast cancer and gynecological related lymphedema, don’t be afraid to reach out to other populations, who also need your support. The treatment principles and pillars of care for melanoma related lymphedema are the same, except for some adaptations to maintain proper compression gradients. You also have a community of fellow lymphedema therapists to reach out to for support.
A closing message for patients
Prioritize your health and take the time to get assessed by a qualified lymphedema therapist. Take time early on after your
Prioritize your health and take the time to get assessed by a qualified lymphedema therapist. Take time early on after your melanoma treatment to get properly diagnosed and continue getting monitored for lymphedema, as you are at a lifetime risk. Early diagnosis always leads to better treatment outcomes.



melanoma treatment to get properly diagnosed and continue getting monitored for lymphedema, as you are at a lifetime risk. Early diagnosis always leads to better treatment outcomes. LP
A full set of references can be found at https://www.canadalymph.ca/pathwaysreferences/
Summer 2023 www.lymphedemapathways.ca 13
Melanoma and lymphedema facts on page 14
Lymphedema, or the presence of chronic edema due to decreased lymph transport, is one of the more significant complications that can occur after a lymph node dissection of the axillary or inguinofemoral lymph nodes. Typically, these lymph node dissection procedures are performed in the setting of nodepositive breast cancer and melanoma. Incidence
n For axillary dissection in this setting, lymphedema rates of 6% to 15% have been reported
n For inguinal dissection rates can be even higher at 29% to 41%
Risk factors for lymphedema
n Although risk factors for lymphedema in breast cancer patients having axillary dissections have been described in the literature, these risk factors in melanoma patients, especially in patients having inguinal dissections, have not been well studied.


n A large portion of melanoma ALNDs are in men.

n Lower limb lymphedema (LLL) is the one of the most frequent complications of both SLNB and inguinal lymph node dissection (ILND) in melanoma. Reported rates of LLL secondary to inguinal SLNB are from 7.6% to 35.1% and from 48.8% to 82.5% after
ILND. These rates are higher than the LLL rates reported after surgical treatment of advanced pelvic cancers (studies report a range of 36.9% and 61%).
n Upper limb lymphedema (ULL) rates after ALND for melanoma range from 4.4% to 14.6% in the reports and from 4.1% to 21.4% after ALND for breast cancer. These two rates are similar probably because the ALND is the same for both cancers. LP
14 www.lymphedemapathways.ca Summer 2023 mail to: info@klosetraining.com https://klosetraining.com/ Enhancing patient outcomes LYMPHEDEMA THERAPY CERTIFICATION TheKloseTrainingAdvantage: • 135-hours of lymphedema education 75-hr engaging online home study module 60-hr (6 1/2) day classroom education • Exclusive post-graduate resources • Special pricing for Canadian Therapists; contact us for more information ONLINE COURSES: • Breast Cancer Rehabilitation • Strength After Breast Cancer • Wound Management for Lymphedema Therapists • Head & Neck Lymphedema Management • Add’l courses at klosetraining.com For more information 1-303-245-0333 info@klosetraining.com klosetraining.com updated in 2023 updated in 2023
Background
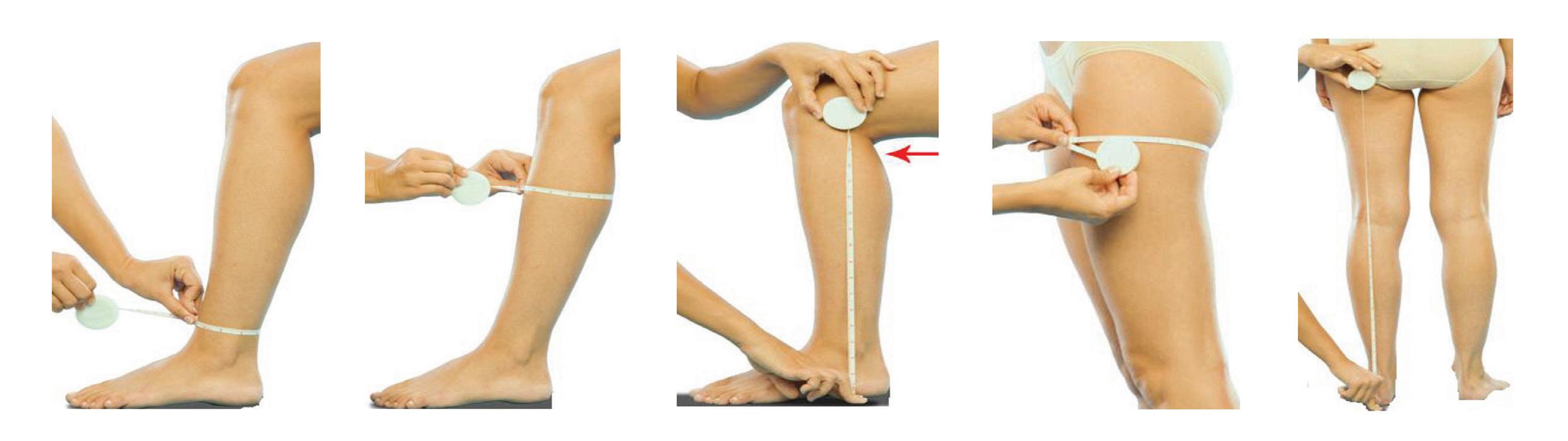
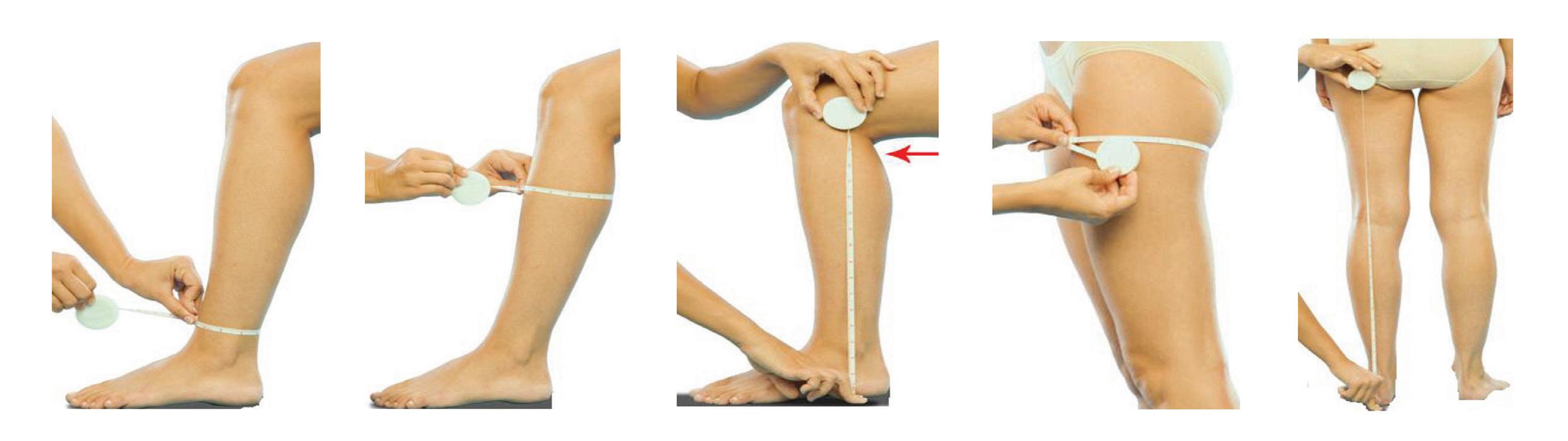
The right fit is key Learning from experienced compression garment fitters

How did you assess clients’ needs?
I would learn about their experiences so far with lymphedema. Was their diagnosis new or had they been wearing garments for a long time? If they were wearing compression; what was the state of their garments, what did they know about them? I tried to understand their attitude by asking questions; How were they feeling? Were they upset by the lymphedema diagnosis? Had they come to terms with it?
What was a common mistake clients made when choosing a garment?
It is important to feel good in what you’re wearing, and appearance is important, but sometimes clients would be shortchanging themselves by choosing fashion over function. They would want off-the-shelf versus custom, or knee-length stockings, rather than the required full pantyhose. Many people were also not aware of their eligibility through provincial health coverage. I would remind them of the number of garments they were entitled to each
year and that their garments should still fit properly and be in good shape. Daily washing is important for hygiene, but also to return the garment back to its original shape for optimum compression.
How do you encourage clients to wear their garment?
If the garment is comfortable, they are more likely to wear it. Although some people will never feel entirely comfortable in a garment, by making it better for them they will see the positive effects, and become more motivated. There are people who just won’t wear compression, even if they really need to and that’s sad. Unfortunately, sometimes it took a bad medical situation for them to finally start realizing that compression is necessary to keep their lymphedema from getting worse.
What suggestions would you give new garment fitters?
For a long time I felt that I should have all the answers but you can’t. Don’t be afraid to
It can’t always be perfect. I would often say to clients, “Custom fit doesn’t mean perfect. It’s going to take a while for us to get to a place where it’s going to be good.”
tell clients, “I don’t know the answer but I’m going to find out for you.” Especially in custom-wear, there’s always a company representative expert who is eager to help. Attending seminars is also good because you pick up information from sharing experiences among other fitters. Finding a balance between what’s a realistic fitting and “how perfect can it be?” is the hard part. It can’t always be perfect. I would often say to clients, “Custom fit doesn’t mean perfect. It’s going to take a while for us to get to a place where it’s going to be good.” Occasionally that never happened.
Summer 2023 www.lymphedemapathways.ca 15 Compression Garments
Images: lymphedivas.com. lymphedemablog.com. www.medi.de
Yasmin Ejbick supported the lymphedema community for more than 33 years with compression garment fitting before recently retiring. She shared her experiences with Anna Kennedy for the benefit of our readers.
Do you have any tips on creative measuring around problem areas?
I remember learning at a seminar how to measure in increments of millimeters; to be so careful and measure right between these exact two lines. But that’s just not realistic, because in minutes, that measurement may be different because it’s hot outside, for example. So you have to learn where to add a little bit or take away after you get to know the person. If I was adjusting a measurement, I preferred to make it consistent all the way up or down the limb, as opposed to just problem areas because you don’t want to cause pockets of compression and create an obstacle for lymphatic flow. Keeping a record of what their actual measurements were along with where and how much you increased it is really important. Custom garments offer many more creative options to make problem areas more comfortable, like soft spots, new weaves at the elbow, knee or ankle area and anatomical feet, etc.
How would you measure someone who is very large or obese?
Wrapping the person’s limb in Saran Wrap is recommended (especially for lower extremity). This firms up the area so you can measure it easier. I would also get a sense of how fleshy the limb was and how firm or soft their tissue was. Picking the right style for someone who is large is extremely important.
What would have been one of your most challenging clients?
One client experienced pain and discomfort, even though she wore a very light compression garment. She needed stronger compression, but couldn’t tolerate that, as she was extremely sensitive to the compression itself. We required many tiny tweaks and changes to make her comfortable. Remake after remake became really frustrating. Luckily, she had a positive outlook, a good sense of humor and was very understanding. However she was also realistic and understood that we couldn’t get it exactly perfect every time.
Are there creative options for people who have trouble donning their garments?
Rubber donning gloves are a must. There’s also a silicone gel that you put on your heel, to make it easier to slip the stocking over your foot. This gel is good for blisters as well. One company has a “slippy aid” for sleeves that includes a loop to hang around a doorknob— making it easy to pull your arm away from it.
Some people have no choice but to wrap (bandage) themselves, as they can’t pull any compression garments on. There are good Velcro-type garments for daytime use that people like because they are so easy to put on, without any help. It’s so important to be realistic to ensure sustainability for people to wear compression for the rest of their lives. Compression for most people is not just “ until I get better.” It’s a commitment for life.
You recently retired after more than 33 years. What did you love most and least about your job?
Watching somebody transition from, “This is something I don’t want to be dealing with, it’s too hard for me” to seeing them smile and feel better once they put on their new garment. That was probably what I loved the most. As for what I liked least; dealing with the bureaucratic paperwork and government health programs! LP
Yasmin Ejbick was a certified compression garment fitter, who also measured and fit off-the-shelf braces and assisted customers with home healthcare purchases. She lives in Toronto with her husband and is enjoying her new retirement.

Anna Kennedy–
“From a selfish perspective, I am very sad to hear of your retirement. You have helped me tremendously with my fittings for over 15 years. Thank you. I will miss you.”
What are your assessment strategies?
My techniques for garment fitting differ from other fitters due to my medical background. I take into account age-related mobility, social status, and what people do for a living.
For example, if the client is a young woman recovering from breast cancer surgery who has had radiation and/or lymph nodes removed and needs to return to work, I must consider her condition and her daily and social life. This can lead to a difficult conversation about what needs to happen for her arm to improve, stabilize and be appropriately managed long term.
Mobility is a significant factor, along with a client’s lifestyle, mental and physical conditions (including the state of their skin and anatomy). My choice for the appropriate garment is very precise, depending on the situation. They could be in one brand initially to preserve the size of their limb and/or decongest further and then move to a different brand to adapt to their social life, as it’s much more comfortable and flexible. For some people, the shape of their limb (arm or leg) is very unique and requires a specific brand. Others may initially be fibrotic and require more rigidity in the garment to reduce swelling before moving on to more flexible and comfortable options.
The stage of their lymphedema and other underlying issues, such as lipedema or other co-morbidities is also essential to consider. People with lipo-lymphedema can experience pain. Although they may require a heavy and sturdy garment, it is a waste if they cannot tolerate it due to discomfort. We have to be careful to not aggravate any pain for any client.
Encouraging garment wear
Understanding the client’s lifestyle, aches and pains, and underlying conditions allows us to accommodate their needs and make the garment work. I approach it as a medical professional and take extensive notes for the
16 www.lymphedemapathways.ca Summer 2023
It’s so important to be realistic to ensure sustainability for people to wear compression for the rest of their lives. Compression for most people is not just “until I get better.” It’s a commitment for life.
Alla Hardoon was introduced to Anna Kennedy as her new garment fitter after Yasmin Ejbeck retired. Alla has kindly provided her expertise in garment fitting, as discussed with Anna.
client’s chart. I want the garment to work for them from a humane point of view, but also that of a business owner, in order to get the best outcome for my clients.
We are fortunate that garment brands support us so graciously with warranties that cover refittings. If the order needs to be corrected, they will remake a garment once we send them new measurements.
I ensure that my clients are contacted for followup and asked proper questions. I warn them that if the garment folds in a particular area of their body, it is not fitting correctly due to a decrease in size. While this decrease is a reason to celebrate, the garment will not be comfortable, and we need to know about it.
Addressing problem areas
Knowledge of the body’s anatomy is essential. As fitters, we are taught the standard measuring points. However, a particular measurement point may need to be corrected for some people. For example, the recommended measuring point on the arm is exactly the halfway point between the elbow and the top of the sleeve because that is the anchoring point. But if that happens to be the thinnest point of the client’s arm (with no muscle there), we will only hurt the person and create a tourniquet, resulting in a “muffin top” and the sleeve not staying up. It’s the reason I always feel
the entire arm or leg to assess the person’s musculature and determine where the garment needs to sit perfectly.
Lack of information
Misinformation or insufficient information can lead clients to make the wrong decision. My initial appointment with every person takes 45 minutes (20 minutes to measure and 25 for education). I cover why they’re getting what they’re getting, what lymphedema is, where it is, and what the garment will do. I make sure I understand what they want from a garment. Some clients are new to lymphedema, while others have worn a garment for the last ten years but were never in the right one. It can be life changing when we put them in the correct garment.
Challenging fittings
The most challenging fitting is not the garment measurement but considering the client’s specific characteristics and life circumstances that dictate their flexibility for compression choices. A person may psychologically understand and be emotionally willing to wear the best garment, but they are not able to due to limited mobility. Often they don’t have a caregiver who can help them, or they are themselves are a caregiver. My preference for bigger legs that have never been fitted in an elastic garment is to start with Velcro wraps to decongest, before we move them to elastic garments, if it fits their lifestyle.
Donning aids
Donning frames for arms and legs make it much easier to put the stocking on the frame and pull the frame to finish it up. Of course we don’t let anyone walk away without giving them a pair of special rubber gloves because we don’t want garments returned because the client can’t get the garment on, or its been damaged with a nail, for example.
Insurance coverage
Insurance companies have become stricter. Some companies now ask for measuring charts, proof of manufacturing invoices, and an updated doctor’s letter with the lymphedema diagnosis and compression level.

We recently had a client who switched to a new insurance company that asked for a letter explaining why a particular garment was necessary. The therapist wrote a letter explaining why the irreversible lymphedema required a custom garment. I provided them with the measurements and packing slip to validate the expense, and everything turned out fine.


Insurance companies have guidelines with charts and may question why more expensive compression garments are chosen over other options. Naturally, they would prefer to cover the cheapest option. They will also question people who want to purchase additional garments over and above what might be covered by their provincial health plan. I suggest spacing out the purchase of extra garments. This makes it self-explanatory to the insurance company that additional garments are needed in-between because the garments are worn so much.
Collaboration with therapists
Communication is key. The best outcomes result from a collaborative approach between the fitter and the therapist. Constant contact involves sending each other emails and pictures and discussing different options that the patient will wear. We can prescribe the best aid in the world, but it’s a waste if they don’t use it and doesn’t fit their lifestyle. We must be open-minded and recommend what best meets their needs and lifestyle. LP
Alla Hardoon RN, is the Founder and Medical Director of Care-Med Ltd, a Toronto-based healthcare company specializing in orthopedic products, compression garment fitting, and post-mastectomy care. She recently also became an American Board-Certified Functional Nutritionist.

Summer 2023 www.lymphedemapathways.ca 17
We can prescribe the best aid in the world, but it’s a waste if they don’t use it and doesn’t fit their lifestyle. We must be open-minded and recommend what best meets their needs and lifestyle.
Leg and arm donning frames.
According to PubMed, there are over 1,000 papers per year published on lymphedema. This volume of research is both impossible to read and engage with in its entirety, nor will the vast majority of findings be brought into clinical practice. It has been widely reported that it takes, on average, 17 years for evidence-based practice to make its way from first suggestion into routine practice.1 Even more depressingly, the majority of good evidence-based practices never make it into widespread clinical use. This represents a waste of good research and potentially missed opportunities for patients. There are many factors that lead to this, but importantly, major barriers to implementing findings include practitioners having insufficient knowledge, skills or resources to deliver the practices in their clinical environment. Even more frequently though, the research undertaken doesn’t align with priorities of healthcare systems and practitioners working in them. Acknowledging this misalignment, a field of research, implementation science, has developed.
Implementation Science has been defined as the ‘scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine care, and, hence, to improve the quality and effectiveness of health services and care’.2 This is fundamentally different to clinical research, such as a typical randomized
The new “science” of Implementation Science

Incorporating evidence-based research into everyday practice
By Liz Dylke
Implementation

control trial or cohort study, as the outcomes analyzed in an implementation study are more often around the use of a practice, including the barriers and facilitators as well as costs of implementing a practice or model of care, rather than just its effectiveness. Implementation studies will also apply strategies to overcome the challenges that are identified.3 This developing form of research is therefore an exciting and critical look into how to bring proven assessments, treatments and models of care into a real clinical workplace. But it’s also quite a different approach to research from traditional clinical research as it approaches the research question and hypothesis with some different assumptions that need to guide the development of the study protocols.4
1 Behaviour change is critical to bringing in research findings to practice, as well as policy.
2 Wide stakeholder engagement is necessary to identify all barriers and facilitators to bring the research findings into practice.
Liz Dylke PhD is Associate Professor, Head of Discipline: Physiotherapy/ Faculty of Medicine and Health at the University of Sydney. She is currently the President of the Australasian Lymphology Association. Dr. Dylke has a passion for demystifying the scientific process for those who are new to research.
3 Flexibility, or a non-linear approach, is often necessary in order to examine how a practice will work within the real world.
Unlike other types of research, clear guidelines on how to interpret implementation sciencefocused studies have not yet been developed. However, when reading an implementation science study, there are some areas to consider most closely to determine if you believe the practice they have evaluated may be applicable in your clinical environment:
1 What is the outcome gap that they were looking to address and is this a practice or outcome gap that you experience? An outcome gap can be defined as the difference between the current health outcomes and what would be expected if the recommended practice were utilized.
2 What is the performance gap that they were looking to address and is it relevant in your clinical setting? A performance gap is the difference between current clinical practice and what would be considered ideal practice. This may focus on providers or systems, and may look at capability, motivation or opportunity of either the provider or the system to undertake the practice.
18 www.lymphedemapathways.ca Summer 2023 Research Perspective
Science has been defined as the ‘scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine care, and, hence, to improve the quality and effectiveness of health services and care.’2
Night garment for lymphoedema management
Vêtement
Compressive Compressif
Helps maintain achieved reduction
Aide à maintenir la réduction ciblée
Creates massaging effect
Crée un effet de massage
Cooling effect
Reduces the temperature at the surface of the skin
Réduit la température à la surface de la peau
Allows the oversleeve to stay in place
Permet de maintenir le couvre manchon en place
Allows adjustable and effortless donning

Facilite l’enfilage de la jambière
https://www.medicanada.ca/ medi. I feel better.
Info :
www.medicanada.ca
Engineered Foam Mousse brevetée
Effet rafraîchissant
Anchor System Systèmed’encrage
EZ-On Tabs LanguetteEZ-On
de nuit pour la gestion du lymphœdème
If you do not experience the same performance or outcome gaps that are identified in setting up the study, the findings of the barriers and facilitators may not apply to your practice. If the gaps do, however, it is worthwhile to then consider how the researchers evaluated their implementation study, to learn about the processes they used and implemented, what they modified or targeted to improve outcomes and how they determined if the practice was adopted or not, and if not, why not.
If you are considering undertaking an implementation-focused study yourself, the most critical thing is planning. A clear idea of the health gap, discussion with all key stakeholders, an understanding of the practice gap and awareness of the system’s or practice’s readiness for change are all necessary to properly develop an implementation study that will provide useful outcomes for the system that you are working within and beyond. Find your local implementation science experts and read the literature widely. There are some great websites out there as well to get you started. An increased focus on the study of how to implement findings into real-world clinical practice will continue to grow, expanding the
field of Implementation Science. While a totally different way to approach research, supporting good evidence-based practice brought into clinical arenas—as well as understanding what clinical practice is interested to bring in and support—is critical for delivering quality care to our patients. LP
This article was first published in LYMPH EXCHANGE, November 2022 and reprinted with permission from the Australasian Lymphology Association.

A full set of references can be found at https://www.canadalymph.ca/pathwaysreferences/
















Implementation Science website resources:










Sydney Health Partners: https://implementationscience.com.au


















National Centre of Implementation Science: https://ncois.org.au/


Global Alliance for Chronic Disease: https://www.gacd.org/about/what-we-do/implementation-science

















■







20 www.lymphedemapathways.ca Summer 2023
‘Even more frequently though, the research undertaken doesn’t align with priorities of healthcare systems and practitioners working in them. Acknowledging this misalignment, a field of research, implementation science, has developed.’
https://www.lymphologyskincare.com * now serving * www.Lohmann-Rauscher.ca Tribute® Wrap Head & Neck NEW Self-care reimagined. ■ Designed for evening, night, and low activity
Fully adjustable
One size fits most Tribute Wrap Head & Neck Adjustable foam compression wrap Adaptives Kompressionssystem aus Schaumstoff ﻞﻳﺪﻌﺘﻠﻟﻞﺑﺎﻗمﻮﻓﻂﻏﺎﺿطﺎﺑر Tribute® Wrap Head & Neck Adjustable foam compression wrap Adaptives Kompressionssystem aus Schaumstoff 2730
■
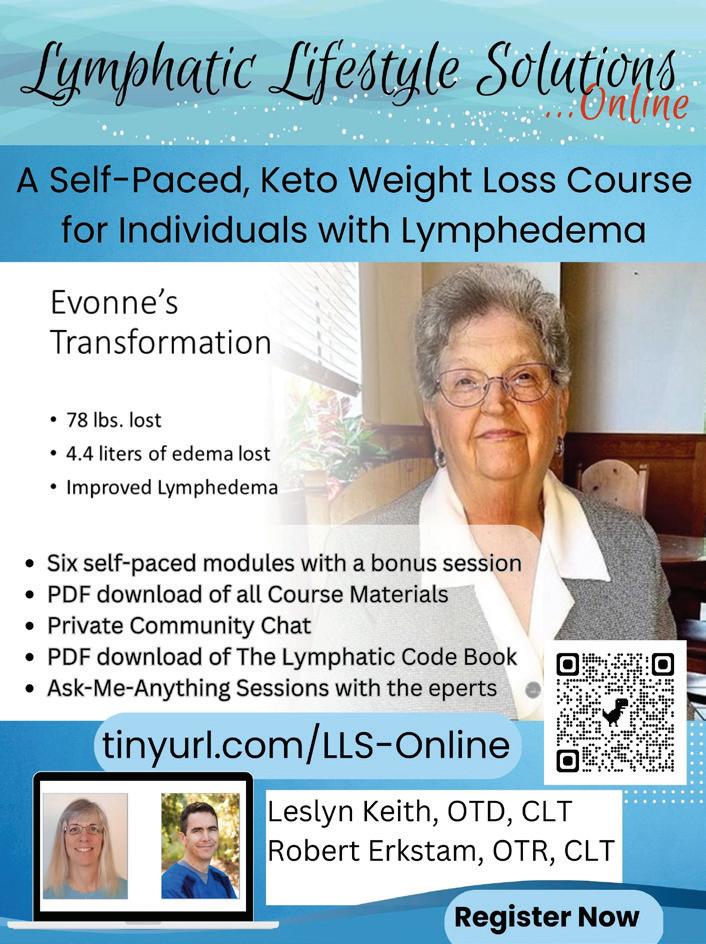
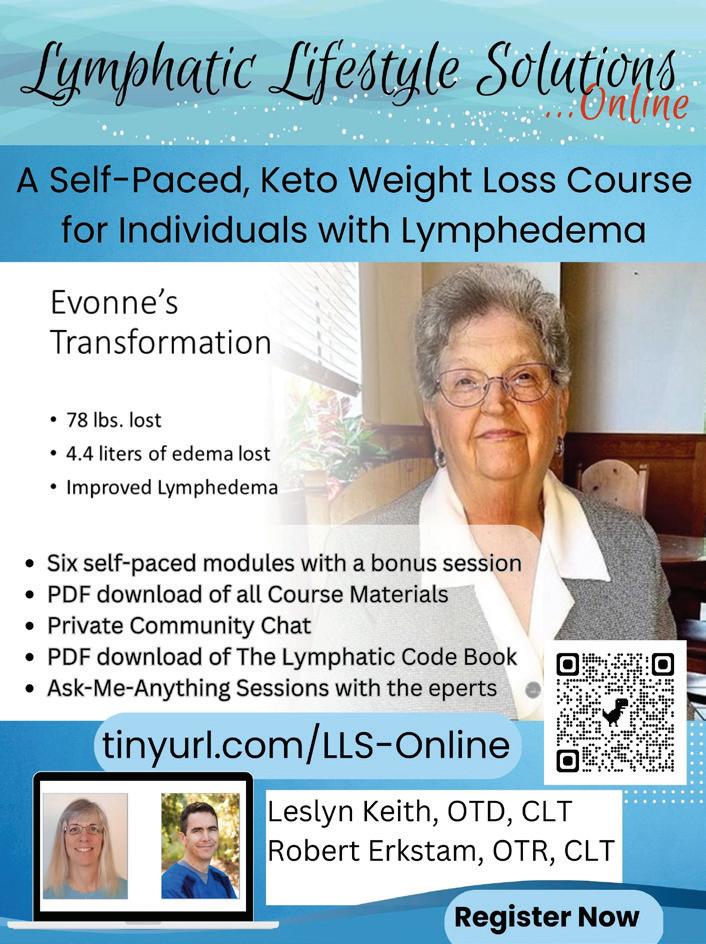
How to live better with lymphedema



Meet the experts
Review by Anna Kennedy. Book written by Matt Hazledine and guests
Introduction
On a recent search through the Amazon website, I discovered more than a handful of new books about lymphedema, all published within the last 18 months. Many of the books are authored by patients and seem to be primarily focused on diet, recipes and what to eat if you have lymphedema.
Assessing credibility
Caution is advised when reading any resource on lymphedema. The reader should carefully review the author’s credentials, whether their sources are rooted in evidencebased research in addition to identifying any possible conflicts of interest. Any book that includes statements or claims such as “no more”, “get rid of” or “reverse” a chronic and life-long disease like lymphedema, should raise a red flag.

Guest co-authors
However, a recent book that stands out is “How to live better with lymphoedema; meet the experts.” The author is Matt Hazledine, an expert patient, who in searching for answers, solicited trusted guidance from over 20 well-known guest lymphedema experts within the international lymphedema community. Some of those experts are affiliated with the International Lymphoedema Framework and include Peter Mortimer, Christine Moffatt, Vaughan Keeley and Kristiana Gordon. Their contributions to the book are in their own words as direct quotes. Although all of these guests live and work in the United Kingdom (as does the author), most of the information is relevant to people living with lymphedema in other countries as well.
Perhaps only some of the local resources referring to therapists, specialists, support groups and some clothes/shoes, are applicable to the UK population exclusively.
Personal experience
Matt is an activist living with lymphedema as a result of non-cancer related lymphedema. Although his frustrations at the beginning of his diagnosis mirror that of most people faced with lymphedema, he moved beyond those frustrations to deliver this book as a message of positivity and hope. His biography states that he has worn every appropriate type of compression garment, tested almost every product, experienced all therapies known to him and had two different types of surgeries. He shares his own trials and tribulations over the past 10 years of his lymphedema journey with honesty, humour and humility. The practical information that he has learned along the way is sprinkled throughout the book as 40 tips, and also neatly summarized in the Appendix.
Book structure
The guest experts cover the traditional four cornerstones of lymphedema management focusing on the physical components, but also cover the psychological and social aspects. The book is divided into 30 chapters,
each devoted to a single subject addressing various questions and aspects of living with lymphedema. Of note, there is an interesting sub-chapter dedicated to the discussion of whether lymphedema should be referred to as a condition vs. a disease.
Sources
The book can be purchased through Amazon as a printed copy or as a Kindle option for the digital version. The author has dedicated 25% of the pretax profits to the Lymphedema Research Fund at St. George’s Hospital in London, England. You can also check out the website of the charity that the author has founded. www.lymphoedemaunited.com
In case you missed it
There was a previous article in Pathways (Winter 2021-22) entitled “Don’t judge a book by its cover” that provided guidance on assessing resources and books for lymphedema. You can access the archived article at tinyurl.com/LEBookRev. LP
Summer 2023 www.lymphedemapathways.ca 21
Book Review
canadianabilities.org/nomination Nominations close November 30, 2023
One
Wish Awards of up to $10,000 Recognition awards are also available to support amazing caregivers!
To
nominate a family caregiver or find out more about the Canada Cares Awards.
Living with lymphedema successfully
The importance of early diagnosis, treatment and staying active
By Darek Mikita
Diagnosis
Darek Mikita was diagnosed with cancer in May 2005 at the age of 47. A malignant melanoma on his back had already spread to the front of his chest and to lymph nodes. The treatment protocol included chemotherapy, radiation and the removal of 39 lymph nodes. At the end of the treatment, Darek noticed that his left arm was different from the right one. During an oncology visit, a nurse recognized the need for lymphedema treatment and referred him to a certified lymphedema therapist in Winnipeg.
Lymphedema treatment
The therapist introduced him to manual lymphatic drainage (MLD) and compression garments. These were able to keep the lymphedema swelling in his arm minimal. Darek now wears a custom compression sleeve all day, and uses a white sports sleeve during sports activities. Although the lymphedema was being managed, the chemotherapy and radiation treatment had


caused him to become weak, as he had lost a substantial amount of weight and muscle. Even walking was a challenge, but the athlete in him knew that he needed a plan to progress. With the continuous support of his wife, Darek slowly built up his cardio by creating a fitness ladder, walking 20 metres to start, and gradually moving to longer and longer laps. Eventually over the next 4-5 years he was able to enjoy biking, running, and jogging again.

Infections
One serious complication for people living with lymphedema is a bacterial infection called cellulitis. Darek continues to battle with these infections as the years go on. His notes that first episode of cellulitis was “selfinflicted” shortly after his lymphedema diagnosis. During a soccer game as a goalie, the ball hit his arm repeatedly while
Darek Mikita, a Professional Engineer lives with his wife Alicia in Headingley, Manitoba. He is an accomplished International Table Tennis Umpire and represented Canada in Para Olympics and Olympics Games. Darek wants to connect with other men living with lymphedema. Darek can be reached at darekm@mymts.net.

This article was adapted from an original interview published in LAM: Swelling with Emotion (Spring 2022).
defending the goal. This may have caused further damage to his lymphatic system. His arm quickly became red and painful. Ten days of antibiotics resolved the infection. It was shortly after this that he was introduced to another certified lymphedema therapist (Edith Mulhall), whom he describes as the “godmother” of lymphedema therapy. He recalls realizing that he should have sought focused treatment sooner and notes that this was where his true journey with managing lymphedema started.
Edith taught him how injuries to his left arm could be detrimental for lymphedema. He learned the importance of protecting his arm, as injuries from cuts, burns or blunt trauma could have a serious impact on his health. She also taught him specific exercises that improved his flexibility and reach; these being extremely important to Darek inorder to participate in sports again.
Darek’s second infection began after painting his deck. He had been supporting himself with his left arm, which prevented the arm from draining properly. COVID-19 lock-down restrictions prevented him from receiving his lymphatic drainage treatments and most likely put him at risk for yet another infection. Darek explains, “I was watching TV and I began to get shivers and started yawning. I felt like I was getting a fever at the speed of sound, while my lymphedema arm was becoming red. I knew I needed to get to the emergency department
22 www.lymphedemapathways.ca Summer 2023 Personal Perspective
for IV antibiotics. I was so tired. I received my medical treatment about 10 hours later, which was not good.” A strong dose of IV antibiotic treatment this time helped resolved the cellulitis within a few weeks, followed by very gentle drainage which helped a lot. The guidance of an experienced therapist is very important when someone is recovering from cellulitis.
Active living with lymphedema


Prior to his cancer diagnosis Darek was very athletic and enjoyed activities like triathlons, soccer, tennis and table tennis. However, the lymphedema in his arm made him nervous about his future participation in these activities. Sports were a priority for Darek to improve his quality of life and he did just that. Today he is back to being an active athlete and he is also an international table tennis umpire. He made modifications that allowed him to play, while minimizing his risks. Playing soccer as a forward rather than goalie is just one example of these modifications. He also wears an arm sports compression sleeve. He has increasingly learned to read his body but does not live in fear of potential infections or what could happen.

Support
Darek has been supported by several therapists over the years. He acknowledges the encouragement and information they provided, that allowed him to use his affected arm normally. Each therapist offered a new and different perspective. Nancy Rosewell, his current therapist, is working with him on specific weight bearing exercises to strengthen his triceps. This is improving the flexibility in his arm and is working on the trouble areas in his elbow. Lymphedema education and awareness have come a long way since beginning his
lymphedema diagnosis. However, Darek believes there are many people living with lymphedema who may not realize it or have the knowledge they need. He is advocating for more information and hopes his story can help others on their journey with lymphedema management.
“The sooner that people start with therapy the better, is a lesson I learned. I would advise people to educate themselves, get proper treatment and coaching as soon as possible, in order to be able to smile and move again, like me.” LP
Summer 2023 www.lymphedemapathways.ca 23
Amoena is a registered trademark of Amoena Medizin-Orthopädie-Technik GmbH. © 2023 All rights reserved Amoena Canada Inc. amoena.ca Linda CuraLymph Comfort Bra Medical Device Classification according to MDR 2017/745: Class 1 New Lymph Care by amoena the global leader in post breast cancer care solutions Now available for stage 1 to 3 truncal lymphedema
Darek has been supported by several therapists over the years. He acknowledges the encouragement and information they provided, that allowed him to use his affected arm normally. Each therapist offered a new and different perspective.
Hints and Tips



















































































Finding a therapist
































If diagnosed with lymphedema, get a referral to a qualified therapist as soon as possible. To find your nearest qualified therapist, contact your local lymphedema support group or organization.
Mental well-being and support groups
Write a letter of gratitude list of three things that you are grateful for every day. Say them to yourself in the mirror every morning. Go on, give it a try, nothing to lose, right?
• Get some fresh air, go for a walk and appreciate your natural surroundings. Nature is calming and therapeutic.
• Connect with other people who have lymphedema by joining online support groups. Also, try to meet other people at local support group meetings. Ask your therapist for information.
• Visit patient-based websites and join local organizations as a member for newsletters and magazines.

Healthy lifestyles
Set an alarm every 30 minutes throughout the day as a reminder to get up and move about. Alternatively, invest in a fitness monitor (or application) which monitors your movement automatically.
• Ask your lymphedema therapist for information on the types of movement or exercise that are particularly suitable


for your personal circumstances.
• Produce a line graph in Excel and record your weight every month. It’s an instant visual guide on weight loss and gain.

• Identify your weak spots; certain times of day or triggers when you are more likely to eat unhealthy snacks or foods and change the routine. Fill that time with another distraction or swap the snack for something that is less bad for you.

• When watching TV, stand up and do some stretches during commercials, or if you find it difficult to stand, stretch out your legs and rotate your ankles in both directions. LP

Source: Appendix I from the book “How to live better with lymphoedema: meet the experts” by Matt Hazledine. https://lymphoedemaunited.com/book/
Calgary
Halifax
London
Montreal
Ottawa
Saskatoon
Toronto
Vancouver
Winnipeg





















24 www.lymphedemapathways.ca https://www.wearease.com/en-ca https://www.vodderschool.com/ MADE IN USA COMPRESSION BRA 15 SIZES LATEX FREE ADJUSTABLE EASY TO FIT 866.251.0076 wearease.com Dr. Vodder SchoolTM INTERNATIONAL Member of Dr. Vodder Academy International Train in Canada with certified instructors www.vodderschool.com info@vodderschool.com | 800-522-9862 PROFESSIONAL TRAINING IN MANUAL LYMPH DRAINAGE AND COMBINED DECONGESTIVE THERAPY Lymphedema management ONLINE Level 1 Theory Available ~ Evidence-based ~ Easy learning modules with small class sizes ~ Interactive, live classroom instruction with physicians ~ Learn precise manual skills with expert, accredited instructors ~ ISO 29990: 2010 certified training ~ CE credit available Visit our website for classes:
Helpful Suggestions
Did You Know?
Impact of severe obesity


With obesity rates increasing worldwide we compared lymphedema (LE) patients with and without concomitant diagnosis of severe obesity (SO), in regard to their baseline demographics, health-related characteristics, treatment plans and patient outcomes. Design: Retrospective observational cohort. Methods: The IBM MarketScan Database was examined (2013–2019) for patients with a new diagnosis of LE. Of 60,284 LE patients identified 6,588 had severe obesity defined by a BMI> 40 kg/m2. The demographics and other characteristics of SO were compared to patients with LE without SO. Results: SO and LE diagnosis increased two-fold from 2013-2019. LE SO+ patients were younger (57.8 vs 60.8 years, having more men (37.7% vs. 24.9%, than the LE SO- patients. More comorbidities were observed in LE SO+ compared to LE SO-, (diabetes 46.0% vs. 24.9 %, heart failure 18.3% vs. 7.4%, hypertension 75.0% vs. 47.6%, renal disease 24.8% vs. 11.9%. Use of diuretics in the LE SO+ group was greater 57.6% vs. 38.0%. LE SO+ patients had higher risk of cellulitis 34.5% vs. 13.5%. Specific LE treatment was given more often to LED SO- 66.3% vs. 64.3%. This was significant for manual lymphatic drainage 46.6% vs. 40.0% and physical therapy 55.4% vs. 51.6%, but not for compression garments 18.2% vs. 17.7%. However, more LE SO+ patients received pneumatic compression device treatment 20.9% vs. 13.7%. Conclusion: There was an increase in SO associated LE. LE SO+ patients have over a two and half-fold increase in cellulitis incidence, with significant increase in medical resource utilization and cost. Despite this, LE SO patients receive less specific therapy such as compression, which has proven to reduce cellulitis incidence.
Source: Clinical impact of severe obesity in lymphedema. Eur J Vas Endovasc Surg. 2022 Nov 17: S1078-5884(22)00759-6. Doi: 10.1016

Telehealth for education and monitoring

Purpose: The primary aim of this study was to compare the attendance rates at a group lymphedema education and same-day individual surveillance appointment between telehealth (TH) and in-person (IP) care for participants following breast cancer (BC) surgery. Secondary aims included evaluating participant satisfaction and costs between the two service models. Methods: Participants following axillary lymph node dissection surgery attended a group lymphedema education and same-day 1:1 monitoring session via their preferred mode (TH or IP). Attendance rates, satisfaction and costs were recorded for both cohorts, and technical disruption and clinician satisfaction for the TH cohort.
Results: Fifty-five individuals participated; all 28 participants who nominated the IP intervention attended, while 22/27 who nominated the TH intervention attended an appointment. Overall reported participant experience was positive with no significant differences between cohorts. Clinicians reported high satisfaction for delivery of education (median = 4[IQR 4-5]) and individual assessment (median = 4[IQR 3-4]) via TH. Median attendance costs per participant were Australian $39.68 (Q1-Q3 $28.52$68.64) for TH and Australian $154.26 (Q1-Q3 $81.89-$251.48) for the IP cohort. Conclusion: Telehealth-delivered lymphedema education and assessment for individuals following BC surgery was associated with favourable satisfaction, cost savings and minimal technical issues despite lower attendance than IP care. This study contributes to the growing evidence for TH and its potential applicability to other populations where risk for cancer-related lymphedema exists.
Source: Evaluating telehealth for the education and monitoring of lymphoedema and shoulder dysfunction after breast cancer surgery. Support Care Cancer. 2023 Mar 28;31(4):239. doi: 10.1007/s00520-023-07693-8.
Seasonal variations
Breast cancer-related lymphedema (BCRL) is a common complication of breast cancer treatment. Anecdotal and qualitative research suggests that heat and hot weather cause an exacerbation of BCRL; however, there is little quantitative evidence to support this. This article investigated the relationship between seasonal climate variation and limb size, volume, fluid distribution, and diagnosis in women following BC treatment.

Methods/Results: 25 women aged between 38-82 years were recruited. Participants completed anthropometric, circumferential, and bioimpedance measures and a survey on three occasions: November (spring), February (summer), and June (winter). Diagnostic criteria of >2 cm and >200 mL difference between the affected and unaffected arm, and a positive bioimpedance ratio of >1.139 for a dominant arm and >1.066 for nondominant arm was applied across the three measurement occasions found. Conclusion: There was no statistically significant variation in limb size, volume, or fluid distribution in this population across spring, summer, and winter, although there were linked trends in these values. The diagnosis of lymphedema, however, varied between individual participants throughout the year. This has important implications for the implementation/commencement of treatment and management. Further research with a larger population in different climates is required to explore the status of women with respect to BCRL. The use of common clinical diagnostic criteria did not result in consistent diagnostic classification of BCRL for the women involved in this study.
Source: Seasonal variations in upper limb size, volume, fluid distribution, and lymphedema diagnosis, following breast cancer treatment PMID:36812466 | DOI:10.1089/lrb.2022.0017 Lymphat Res Biol. 2023 Feb 22.
Summer 2023 www.lymphedemapathways.ca 25
Research Advances
Canadian and International Events



June 13-15, 2023


The 11th International Lymphoedema Nottingham, UK Framework (ILF) Conference. In collaboration with the Lymphoedema Network Wales. n https://www.lympho.org/conferences/
June 13-17, 2023
LE&RN and NAVBO. Lymphatic Forum 2023. Banff, AB n http://lymphaticforum.org/

July 2023

Camp Watchme 2023. Brylan’s Feat Foundation. (various sessions) The first and only summer camp in North America Snow Mountain Ranch, for children with lymphedema. CO, USA n https://www.brylansfeat.org/campwatchme
I have enjoyed your publication for over two years. It is excellent! There is nothing like this in the United States. Thank you for your time.
I received the print copy of the latest Pathways magazine and am so excited to see my article in it. I look forward to feedback regarding the information, and if people find it helpful.







Sep 11-15, 2023
International Society of Lymphology (ISL) Genova, Italy 29th World Congress of Lymphology. n https://www.isl2023lymphology.com/





Lesli Bell Winooski, Vermont
Oct 3-8, 2023
National Lymphedema Network Lymphological Philadelphia, PA Investigations and Exploration. USA n https://lymphnet.org



Nov 3-4, 2023
Canadian Lymphedema Framework –Toronto, ON National Conference. Moving Forward Together. An educational event for both health professionals and patients. n www.canadalymph.ca/conference
26 www.lymphedemapathways.ca Summer 2023 ENROLL NOW: FALL COURSE BEGINS OCTOBER 16 Lymphedema and Chronic Edema Management Microcredential eClass - Learn Online www.tinyURL.com/CLF-CE-Info 35 education hours certificate Learn with leading experts Self-paced, 6-weeks 4 modules
Education Education
Letters to the Editor... The CLF is an academic and patient collaboration, working to improve lymphedema management for lymphedema and related disorders in Canada
magazine
reality ABOUT THE CLF: Charitable Registration 85160 1260 RR0001 Subscription information at www canadalymph ca/subscriptions _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ Pathwaysissuch afabulouspublication. Thankyouforusing theplatformto encourageadvocacy! Heather
Lymphedema
Group _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________
The
Canadian Lymphedema Framework (CLF) wishes to thank these partners for their support in making this
a
Ferguson, Founder & Executive Director
Advocacy
OldPamelaHarveyFort,NorthCarolina _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________ _____________________________________________________
_______________ ______________ ____________ ___________ ________________________ ________ __________________________ ________ _____________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ issueSendingthanksforthelatest NaomiofPathways.DolgoyandDaxEdmonton,(yournewestreader!!) Alberta
Compression where you need it with JOBST®
JOBST JoViPak in combination with the JOBST JoViJacket is designed for lymphedema compression therapy during the night. The 4 blend foam mix and stitched channels are designed to create multiple pressure points and stimulate lymphatic drainage. These garments for edema management come in various styles and, with the addition of specialized pads, are designed to provide comfort and control from head to toe.
JOBST® JoViPak®. Full body solutions for reliable lymphedema management during night-time

jobstcanada.com
1-877-978-5526
https://www.essity.com/ brands/?country=ca
Compression for night-time lymphedema management
HELLO LIFE!
LIVING CAREFREE WITH EDEMA
THANKS TO VENOTRAIN CURAFLOW

Bauerfeind’s flat-knit Curaflow garments are custom-made and perfectly adapted to the lymphedema or lipedema of the patient. Curaflow garments relieve pain and maintain consistant pressure all with exceptional wearing comfort!


BAUERFEIND.CA




























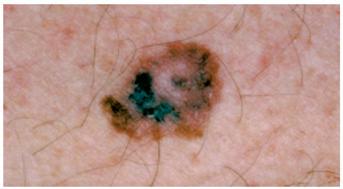













 By Marize Ibrahim, Angela Yung, Marie-Eve Letellier and Anna Towers (in discussion with Anna Kennedy)
By Marize Ibrahim, Angela Yung, Marie-Eve Letellier and Anna Towers (in discussion with Anna Kennedy)