
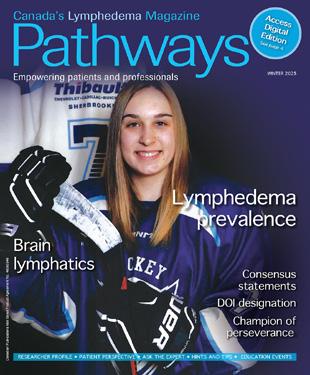
Empowering patients and professionals




































Spring brings opportunities for renewal. It is also a time to raise the profile of lymphedema. On March 6, lymphedema advocates around the globe will unite to participate in World Lymphedema Day by honouring the many people living with lymphedema. Many educational and awareness activities will be hosted throughout the month of March.
The advocacy work of two organizations is highlighted. Anne-Marie Joncas (Quebec) shares practical tips for building advocacy efforts. Christine Chandler and her advocacy team recently submitted a proposal to extend compression garment coverage to a broader set of eligible recipients in British Columbia. We welcome others to share their success stories for inclusion in future articles.
The Canadian Lymphedema Framework and its eight provincial partners swiftly mobilized a national response to the recently proposed trade tariffs that threatened access to essential medical compression garments for Canadians living with lymphedema. While the situation continues to evolve, advocacy efforts—including a petition and letter-writing campaign—remain ongoing. Learn more and add your voice on page 30.
Wounds Canada recently added a new chapter dedicated to lymphedema to the
latest version of their comprehensive Best Practice Recommendations for Skin Health and Wound Management resource. We thank Dr. David Keast and Janet Kuhnke for providing an update and highlighting the Wound Prevention and Management Cycle tool for clinicians.
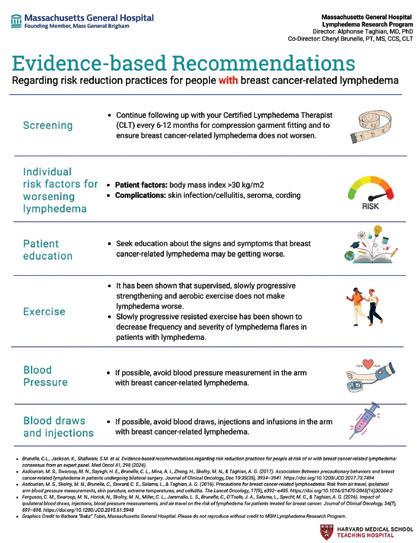
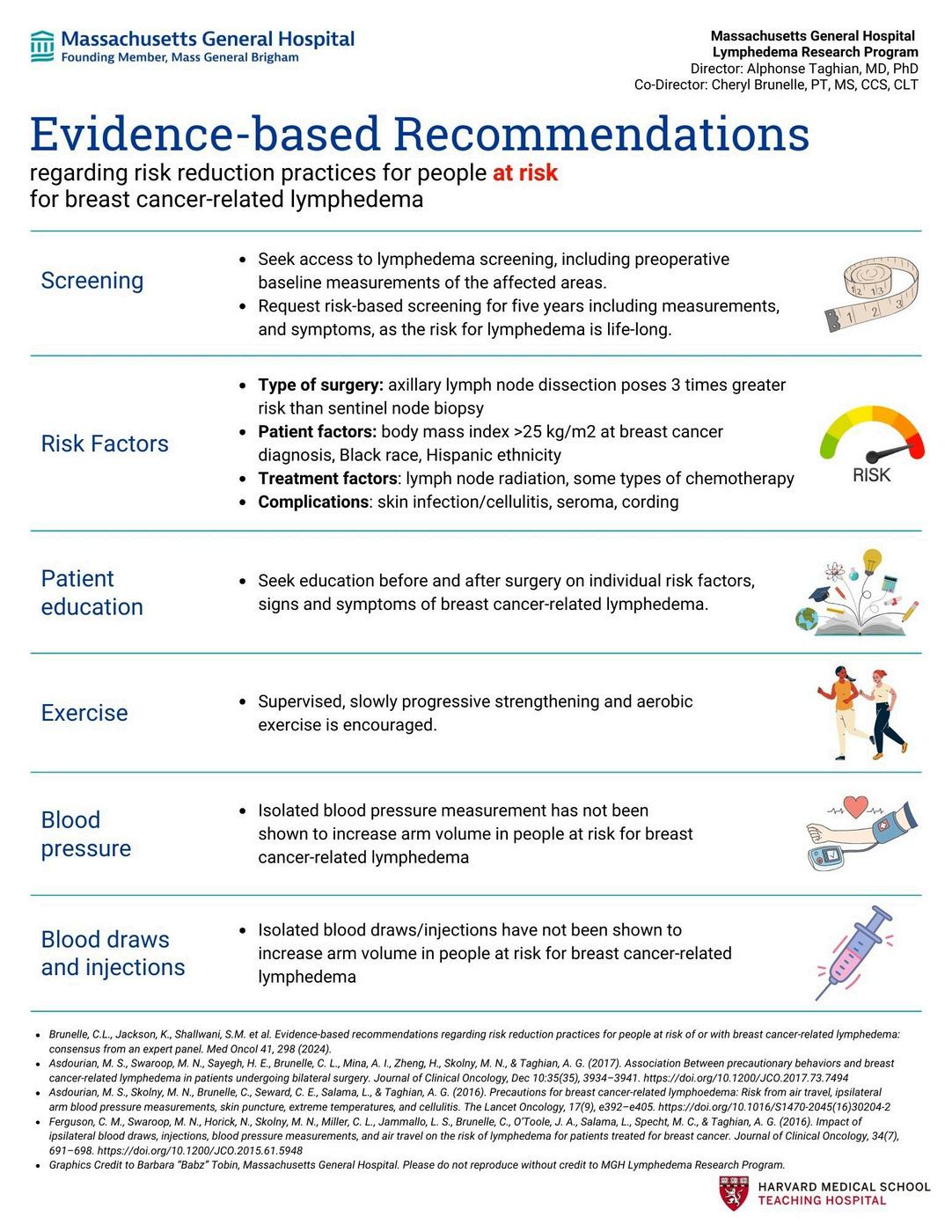
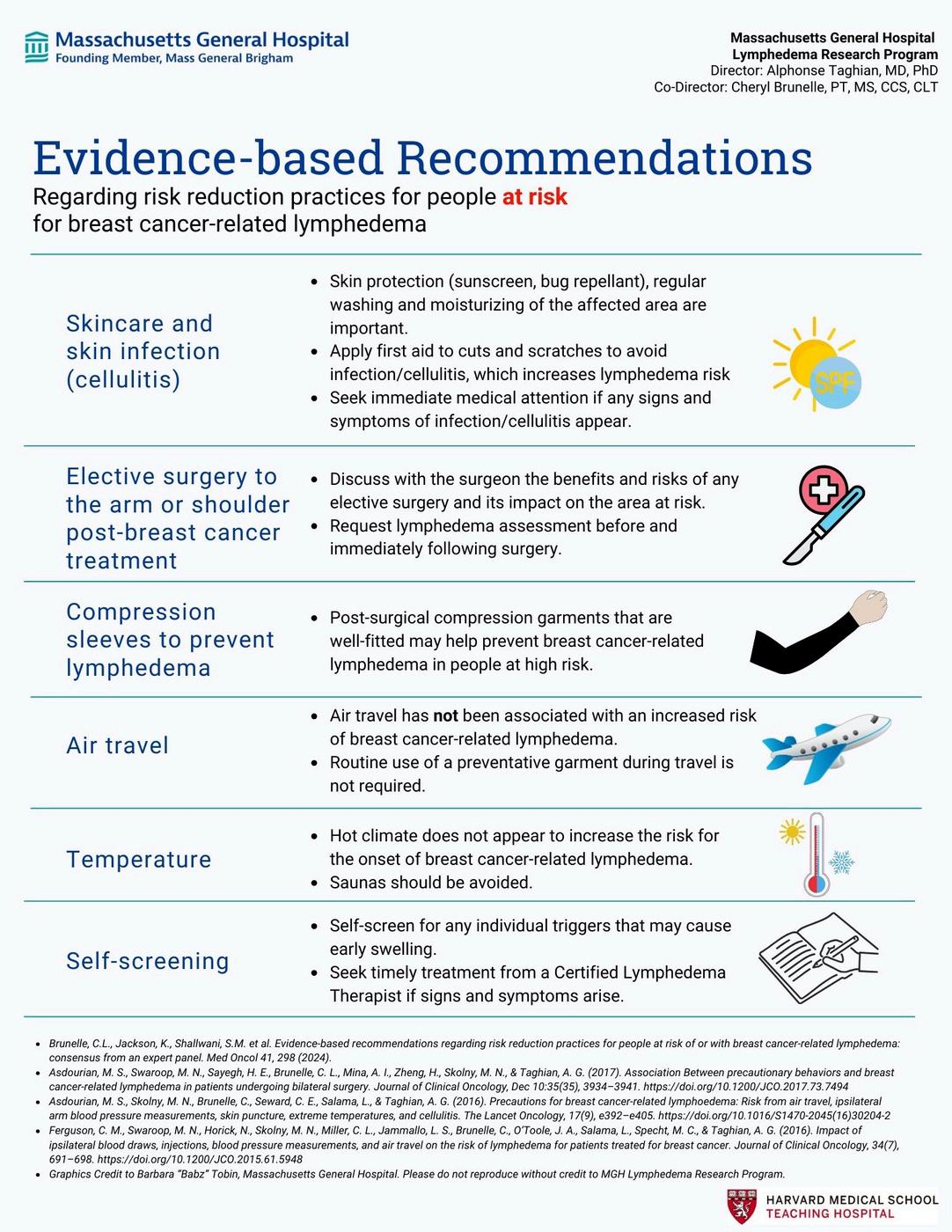
The Winter issue of Pathways featured 15 abstracts of newly published research papers and consensus statements. Risk reduction recommendations is the topic we are focusing on for this issue. An interview with Cheryl Brunelle and Julie Hunley, two key authors, highlights the tremendous work that went into this research and suggests how we might translate this new knowledge into clinical practice. We encourage all hospitals, clinics, and patient organizations to align their current information with these new recommendations.
Mei Fu has provided a synopsis of her team’s research review on the effects of daily living risks on breast cancer related lymphedema. The skin care strategies outlined are prudent to follow for the entire population.
We applaud the efforts of Sonja Redden, a lymphedema therapist, who spearheaded an educational accredited event in Western

Canada, which resulted in 14 physicians among the attendees. We hope the momentum of this event will help move lymphedema care forward in her region.
Patient stories resonate with many of our readers. Doreen Henriksen waited 49 years for a proper diagnosis of primary lymphedema. In the meantime, she was already following strict compliance with three crucial management steps: proper skin care, lymphatic drainage, and compression.
On a sad note, the lymphedema world mourns another hero. Dianne Kipnes passed away in late December. She and her husband provided tremendous financial support to the lymphedema community. Their donation financed the first Endowed Chair in Lymphatic Disorders in Canada and helped research scientists Spencer Gibson (University of Alberta), Pierre von de Wied, and Shan Liao (University of Calgary) and their teams. You can find a tribute to Dianne on page 23. LP

Anna Kennedy

Spring 2025 n Volume 14 Issue 2
Publisher
Pathways is published four times per year by BCS Communications Ltd. on behalf of the Canadian Lymphedema Framework.
Editorial Board
Mei Fu PhD RN FAAN
David Keast MD FCFP
Lori Radke PT CLT
Margie McNeely PhD PT Anna Towers MD FCFP
Editor-in-Chief Anna Kennedy
Executive Director Bonnie Baker
Marketing Manager Grace Neumayer
Advertising and Submissions
We welcome your ideas, contributions, letters and ad copy. While all material is subject to Editorial Board approval, inclusion does not constitute an endorsement or reflection of the views and opinions of the CLF and its Editorial Board. Contents may not be reproduced without written permission of the Canadian Lymphedema Framework.
Subscription Rates (1 year) Canada - $30. United States - $60. International - $75. Single copies and back issues - $8.
Subscriptions/return mail to Canadian Lymphedema Framework 4800 Dundas Street West, Suite 204 Toronto, Ontario M9A 1B1 Telephone: 647-693-1083
Email: pathways@canadalymph.ca www.canadalymph.ca
Photos:
C.Chandler, D.Henriksen, S.Redden, University of Alberta, D.Keast, Wounds Canada
All stock images are CanStock Canadian Publications Mail Agreement 40065546
ISSN 1929-1418 (Print) • Printed in Canada ISSN 2818-5714 (Online)
We acknowledge the financial support of the Government of Canada.
New best practice recommendations For the prevention and management of wounds related to lower limb lymphedema.
Advocating for lymphedema: Awareness, action, and access. A provincial advocacy story.
..........................................
Evidence based risk reduction recommendations for people at risk or with breast cancer related lymphedema.


Managing my lymphedema
Dedicated daily compliance.

A tribute to Dianne Kipnes
A visionary leader and philanthropist.
................................
Inter-professionalism teamwork
The first ever lymphedema conference in the Northern Health Region of British Columbia. ....................................................
A Synopsis:
Infection and skin trauma incrementally increase the risk of breast cancer-related lymphedema.
5 10 15 20 24 27 23



REQUEST ACCESS ONLINE OR BY EMAIL www tinyURL com/yes-digital pathways@canadalymph.ca
The Editorial Board is pleased to announce our newest board member. Margaret (Margie) McNeely is a Professor in the Departments of Physical Therapy and Oncology at the University of Alberta, in a jointly funded position with Cancer Care Alberta. She is the Director of the Cancer Rehabilitation Research Clinic at the University of Alberta. Her primary research interests involve examining physical therapy and exercise interventions for cancer-related impairments including shoulder dysfunction, peripheral nerve injuries, and lymphedema.

By David Keast and Janet Kuhnke

Abstract
Wounds Canada is pleased to present new Best Practice Recommendations for the Prevention and Management of Wounds Related to Lower Limb Lymphedema. The Best Practice Recommendations For Skin Health And Wound Management
2025 is the latest version of Wounds Canada’s most popular resource, used by frontline clinicians, students and policy makers to inform their practice.1 These best practice recommendations are focused on the care of adults and the related wounds of the lower limb.
Why understanding lymphedema is critical in wound management
is defined as chronic edema. All chronic edema involves lymphatic dysfunction and is appropriately classified as lymphedema (LE).
Lymphedema, often termed a hidden disease, is generally under-assessed and underappreciated by health-care providers.2,3 Edema that persists for more than three months and is minimally responsive to limb elevation and/or diuretics


Lymphedema affects more than 200 million people worldwide.4 In the United States, it is estimated that 35 million individuals have the condition.5,6 The prevalence of LE in Canada is approximately 1.25 million (based on 41.5 million population), but the condition is underdiagnosed and undertreated.7 LE is associated with obesity, the rates of which are increasing in Canada.8,9 Because of these factors it is important that patients receive timely assessment, diagnosis and referrals for activation of treatment, with an important focus on skin health and the prevention and management of wounds related to LE.
This is crucial, as wound care is a costly concern to the healthcare system and more research is needed
David Keast MD is the Medical Director of the Outpatient Chronic Wound Management Clinic at the Parkwood Institute (London) and Clinical Adjunct Professor of Family Medicine, Schulich School of Medicine and Dentistry and Associate Scientist in the Parkwood Research Institute. He is Chair: Canadian Lymphedema Framework.
Janet Kuhnke RN, BA, BScN, MS, NSWOC, FCN, DrPsychology is an Associate Professor at the School of Nursing at Cape Breton University (Nova Scotia). She is the research and evaluation lead for Wounds Canada.
Health-care professionals must be mindful of the many tools that can be used in the assessment of LE and corresponding wounds, while tailoring care to the unique needs and goals of the patients they encounter.
to fully appreciate the impact of LE on this issue.10,11 Figure 1 (see page 6) presents information on potential prevalence of LE and its associations with other health conditions. It is important to recognize that these factors often coexist. While chronic venous stasis disease is the greatest risk factor, it does coexist with multiple factors.
What is the relationship between wounds and lymphedema?
Lymphedema, whether congenital or secondary, is a serious, debilitating and progressive condition that develops when protein-rich fluid accumulates because the ability of the lymphatic system is inadequate to transport the excessive interstitial fluid. The fluid accumulation is most commonly seen in the extremities.5,11 This is particularly problematic in the lower extremity due to increased gravitational factors related to dependency, high filtration rates related to venous insufficiency and
Lymphedema and Chronic Edema
Potential Prevalence, Canada 20247

volume overload conditions such as congestive heart failure or renal failure. A review of LIMPRINT data revealed that the prevalence of wounds associated with lymphedema ranged from 2.0 to 73.6 % depending on the population studied.2 Roughly two-thirds of those with lower extremity lymphedema had concomitant wounds.
The condition may range from mild to serious and affect patients of all ages, impacting quality of life, employment/ employability, mobility and social and emotional wellness. Individuals who develop LE live with chronic, progressive swelling, skin changes, risk of infection, emotional distress and pain. Therefore, a holistic approach to lifelong care is required, including multiple referrals and reports from an interprofessional team whose members may represent lymphology, rheumatology, dermatology, endocrinology (diabetes mellitus), orthopedics and internal medicine (e.g., renal, cardiac, respiratory, bariatric) to determine causality.
Early diagnosis of LE is critical, as the disease is progressive. In the past, chronic leg edema (over three months) was not identified as LE. Recently, international
experts have determined that though the pathology of chronic edema and LE may differ, the disorder is to be considered similar, as the overload or impairment of the lymphatics is the constant factor.12
Patients diagnosed with lower limb LE often live with other co-occurring diseases/disorders such as obesity.2
To understand the state of LE in Canada, Wang and Keast (2016) reviewed 326 LE patients and found an average of 7.3 comorbid conditions that were potentially related to the development of chronic edema; hence the term complex lower extremity edema.12 Of importance is that they reported that 45% of patients were found to be morbidly obese. They
state, “it is conservatively estimated that over half those with a BMI ≥ 40 will have lymphedema and if BMI ≥ 50 the risk may approach 100%.”7
The wound prevention and management cycle
In these new Best Practice Recommendations (BPR) the promotion of early assessment and diagnosis is emphasized. This document is part of a series published by Wounds Canada and follows a standard approach to wound assessment and management.
The Wound Prevention and Management Cycle (WPMC) leads the clinician through assessment strategies, setting goals of care, establishing a team, developing







Research is needed to develop
assessment tools that integrate aspects of both lymphatic health and wound care in order to optimize the wellbeing of patients living with complex, combined presentation of lymphedema and wounds.
a care plan which includes removal of non-viable tissue, therapeutic cleansing, managing infection and exudate, and approaches for assessing outcomes. These documents are not Clinical Practice Guidelines but rather a distillation of the best evidence available compiled by an
interprofessional team.1 This document includes distinguishing lipedema from lymphedema. Alongside the patient, the interprofessional team needs to be in partnership with the patient and care partners. We emphasize the importance of and promotion of daily skin health routines. Also, the team emphasized the importance of wearing and managing life-long compression (see Figure 2: Wound Prevention and Management Cycle on page 6).
Outcome evaluation is a stepwise process that engages the patient and care team across several aspects of the health continuum. Health-care professionals must be mindful of the many tools that can be used in the assessment of LE and corresponding wounds, while tailoring
care to the unique needs and goals of the patients they encounter.
Research is needed to develop assessment tools that integrate aspects of both lymphatic health and wound care in order to optimize the wellbeing of patients living with complex, combined presentation of lymphedema and wounds. LP
References can be found at https://canadalymph.ca/ pathways-references
For a copy of the new Best Practice Recommendation: Prevention and Management of Wounds Related to Lower Limb Lymphedema see https://www.woundscanada.ca/ news/752-bpr-new
How to cite: Keast D, Kuhnke J. New best practice recommendations for the prevention of wounds related to lower limb lymphedema. Pathways. 2025;14(2): 5-8. doi: https://doi.org/10.70472/MSVT5658






























3M™ Coban™ 2 Two-Layer Compression System and 3M™ Coban™ 2 Lite Two-Layer Compression System





Coban 2 Compression System has advanced the science of compression therapy by designing materials engineered with Intelligent Compression Dynamics. These materials, which comprise the Coban 2 Compression System and Coban 2 Lite Compression System, create a conformable, inelastic sleeve that supports the patient’s muscle movements for e ective venous return and reduction of edema.


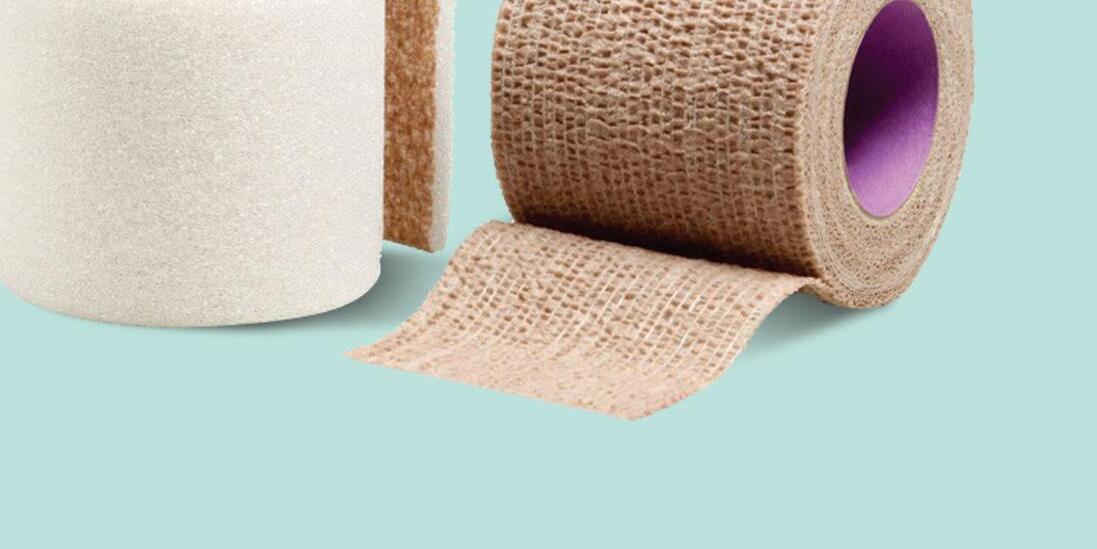

3M Health Care is now Solventum
At Solventum, we enable better, smarter, safer healthcare to improve lives. We’re a new company with a long legacy of creating breakthrough solutions for our customers’ toughest challenges. Because at Solventum, we never stop solving for you.
By Anne-Marie Joncas

Lymphedema, a chronic condition resulting from lymphatic fluid buildup, affects countless individuals worldwide. Despite its prevalence, awareness of the condition and access to structured care remain limited. This article explores actionable strategies for raising awareness and advocating for systemic change, empowering individuals and organizations to champion lymphedema care at local, provincial, and national levels.
Public awareness is foundational to advocacy. It not only educates people about lymphedema but also fosters early diagnosis, which can significantly improve patient outcomes. Moreover, heightened awareness helps to break down societal stigmas associated with the condition, encouraging a more inclusive and supportive environment for individuals living with lymphedema.
Crafting an effective message
To capture public attention, the messaging must be clear, relatable, and impactful.
• “Persistent swelling in your legs, arms, or other areas could be lymphedema. Talk to your doctor today!”
A high-impact message would be: “Swelling? It could be lymphedema. Talk to your doctor.”
• “Lymphedema is a chronic condition caused by lymph fluid buildup, leading to swelling, discomfort, and potential complications if untreated.”
Utilizing diverse media platforms
• Social media: Platforms like Instagram, Facebook, and TikTok can amplify visibility through videos, infographics, and patient testimonials. Use hashtags such as #KnowLymphedema and #FightTheSwelling to create momentum.

• Traditional advertising: Place billboards and public transport ads in high-traffic areas, showcasing visuals of early and advanced stages of lymphedema.
• Television and radio: Create concise advertisements that highlight symptoms and encourage consultations with healthcare professionals.
• Online hubs: English and French-speaking lymphedema communities should work together for a comprehensive resource, offering symptom checkers, directories of certified therapists, and FAQs.
Targeting healthcare professionals
To reach physicians and other prescribers of compression therapy, consider:
• Continuing medical education events: Host informational sessions or workshops for healthcare providers focusing on lymphedema management and the importance of early diagnosis.
• Direct mail campaigns: Send targeted mailings to local physicians, clinics, and healthcare facilities containing educational materials on lymphedema.
• Professional conferences: Attend and present at medical conferences providing resources and information on lymphedema care.
• Referral networks: Establish connections with physiotherapists, occupational therapists, and other allied health professionals who can refer patients for compression therapy.
Engaging communities directly
Organize educational seminars, and awareness walks to engage communities. Partnerships with healthcare providers for collaborative events can enhance credibility and outreach. Specifically, connect with nurses who specialize in wound care, chronic venous insufficiency, and elder care in senior residences to ensure targeted engagement with at-risk groups.
Securing systemic support requires targeted advocacy with policymakers and healthcare authorities. Effective systemic support can lead to structured care pathways, increased funding, and policies that prioritize early diagnosis and treatment, significantly improving outcomes for individuals with lymphedema. Success hinges on building relationships, presenting evidence, and being persistent.
Collaborate with national healthfocused foundations such as the Canadian Cancer Society and Wounds Canada. A full list of suggested organizations can be found as Box 1 in the online references.
Identifying stakeholders
Effective advocacy begins with knowing who to engage. Target key decision-makers such as provincial health ministers, healthcare executives in regional health authorities, members of parliamentary health committees and professional associations representing physicians and allied health professionals.

Make sure to include the Canadian Lymphedema Framework in your approach, as it is the ally with the highest national lymphedema profile and plays a vital role by providing resources and advocacy for lymphedema care.
Presenting a compelling case Craft a message that emphasizes both the economic and human impacts of lymphedema.
• Core argument: “Structured lymphedema care reduces long-term healthcare costs and improves quality of life. Neglecting this issue burdens both patients and the healthcare system.”
• Evidence: Present prevalence data, economic impact analyses, and patient testimonials to highlight the urgency of action. Consider the impact on wounds, chronic insufficiency, obesity, the elderly, and the increased visits to the ER for cellulitis.
Preparing effective advocacy materials
Support your case with well-prepared documents, including a lymphedema care algorithm outlining diagnostic and treatment steps, cost-benefit analyses demonstrating the savings from early intervention and proposals for pilot programs to test the feasibility and impact.
Engaging through meetings and collaboration
Organize meetings with decision-makers to present your case. Prepare concise, impactful presentations, supplemented by handouts and digital materials. Foster coalitions with other provincial associations, the Canadian Lymphedema Framework and organizations in the USA.
Grassroots initiatives bring advocacy to the community level, fostering sustained engagement and localized impact.
Equip volunteers with talking points, educational materials, and training sessions to confidently discuss lymphedema with healthcare professionals, policymakers, and the public.
Encourage patients and caregivers to share their stories through letter-writing campaigns addressed to their provincial representatives. Personal narratives are powerful tools for humanizing the issue and influencing policy.
Funding is critical for sustaining advocacy and awareness initiatives. Successful examples of funding campaigns illustrate how resourcefulness and strategic partnerships can significantly enhance these efforts. For example, a lymphedema awareness charity walk can garner local sponsorship from healthcare providers and businesses, raising thousands of dollars while fostering community engagement. By exploring diverse funding sources, advocates can ensure the longevity and effectiveness of their initiatives.
• Government grants: Apply for grants from federal and provincial health ministries, as well as programs by Health Canada aimed at chronic disease prevention and community health improvement.
• Corporate partnerships: Seek sponsorships from companies producing compression therapy products, pharmaceutical firms, and local businesses interested in community engagement.
• Charitable foundations and fundraising: Collaborate with national health-focused foundations such as the Canadian Cancer Society and Wounds Canada. Organize charity events, galas, and crowdfunding campaigns to gather community support.
• Academic collaborations and in-kind contributions: Partner with universities for research funding and involve students in advocacy projects. Request in-kind contributions, such as advertising space, printing services, and volunteer hours, to minimize costs.
Regular evaluation helps refine strategies and demonstrate progress. These metrics also align with the broader goals of
advocacy by providing clear indicators of awareness, engagement, and systemic change, ensuring that efforts remain focused and impactful. Key metrics include:
• Website traffic and social media engagement to gauge public awareness
• Participation rates in healthcare professional training and subsequent diagnostic improvements
• Policy changes and pilot program outcomes to measure systemic impact
Advocating for lymphedema awareness and care requires a multifaceted approach combining public education, professional training, and engagement with decisionmakers. By uniting individuals, communities, and organizations, we can improve the quality of life for those living with lymphedema and build a future where comprehensive care is accessible to all. LP
References and more suggested resources can be found at https://canadalymph.ca/ pathways-references
Editor’s Note:
Healthcare in Canada is federally funded and guided by the provisions of the Canada Health Act (CHA) of 1984. The CHA requires that “medically necessary” or “medically required” hospital, physician or surgical-dental services be insured by the provincial or territorial plan. As a result, some health services that many Canadians view as essential to maintaining good health – such as prescription drugs and lymphedema compression garments – are not required by the CHA to be insured by the provinces and territories. The result is that the basket of publicly insured health services various among Canada’s provinces and territories.
For a list of the 13 provincial and territorial agencies to initiate conversations about lymphedema care in your province, along with a full set of reference tools, visit https://www.canadalymph.ca/ pathways-references/
Do you know about our lipedema product?
Ideal for active, sporty patients.

Indications
• Primary and secondary stage 1 and 2 lymphedema
• Lipedema
• Scar treatment
• Postoperative and postraumatic edema
Cosy features
• Comfortable all day wear
• Flexible longitudinal knit for easy donning
• Special anatomical foot shape
• Durable knit on the sole and heel


“After attending two CLF conferences and meeting other Provincial Association presidents, I was finally ready to launch an advocacy initiative in British Columbia. Thanks to Anne-Marie Joncas (Quebec) for providing lots of ideas and Diane Martin for sharing the Alberta advocacy experience in achieving two government-funded lymphedema clinics.” - Christine Chandler
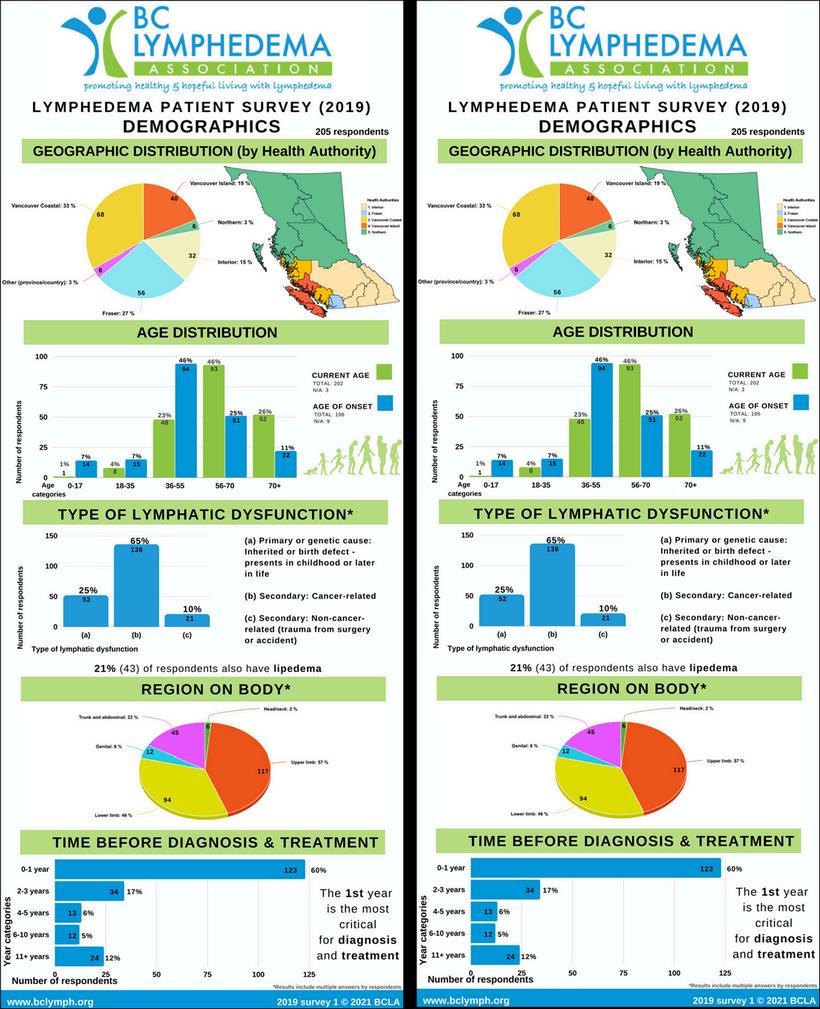
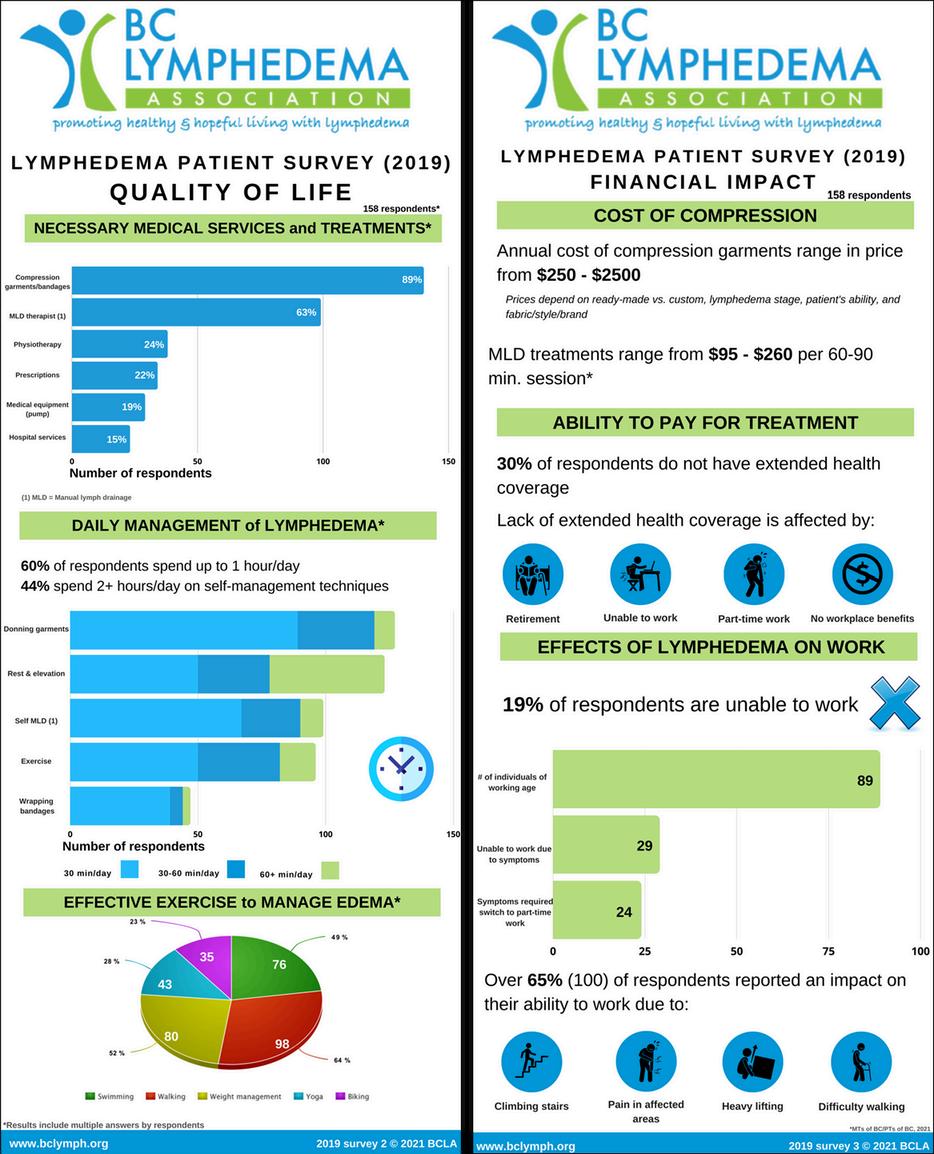
The British Columbia Lymphedema Association (BCLA) developed a patient survey to engage the province wide community. We had a 30% response rate to the 600 surveys distributed through BCLA members, contacts, patients of lymphedema therapists and doctors. With the help of two pre-med student volunteers, data was condensed into a series of Infographics depicting: demographics, health region, length of time before diagnosis, costs involved and effect on quality of life.
We established a patient committee to determine priorities, using an advocacy primer to structure our discussions. The main priority was determined to be funding of compression garments for all lymphedema cancer patients, not just those who had undergone surgery for mastectomy or lumpectomy.
required in an application for financial coverage for assistive devices.
By this time our advocacy committee included an experienced therapist, an industry representative, two BCLA representatives, and two new patients who had the skill sets for researching, organizing and editing the application.
Government Executive Committee. The initial request is for approval of funding for compression garments for all primary and all post cancer patients. Eligibility will be based on a financial means test.
The advocacy committee has continued work on identifying the most effective ways to achieve early diagnosis. This included conducting a survey of BC Wound Care Clinics where many undiagnosed lymphedema patients are identified.

We secured a meeting with the B.C. Ministry of Health, where we shared a patient story plus the survey infographics and outlined the need for financial coverage of compression garments for all lymphedema patients. This led to an introduction to the appropriate B.C. Pharmacare Department Manager, who provided specific details

We began writing at the end of March and in June 2021 we hand delivered the 75-page fully referenced application to the Ministry office. Since submitting the application, we have experienced several delays due to COVID, transition to new Pharmacare contacts, government research processes and finally, in late 2024, a provincial election. However, our application has now reached the final stage with the Pharmacare review team preparing a report to present to the
Christine Chandler lived with lymphedema for 20 years without any support or guidance. Finding out about the BCLA changed everything for her. She served as secretary and then President from 2017-2023 and now chairs their Advocacy Committee.
Our focus has been on writing proposals for Post Cancer Care for those at risk of developing lymphedema. Several physiotherapists within the BC cancer network have taken Vodder training and are in the early stages of implementing some aspects of our proposal. A second proposal is for establishing regional lymphedema clinics which would offer early diagnosis, initial treatment and education on self-management. Throughout the process
BCLA has focused on building public awareness: through March 6th events, reaching out to MLA’s, offering education days and regional workshops, member articles in local papers plus two submissions to the B.C. Budget Advisory committee. We have maintained communications with “key stakeholders” including health care practitioners in all the B.C. health authorities, lymphedema experts, government and political contacts in the BC Legislature. LP
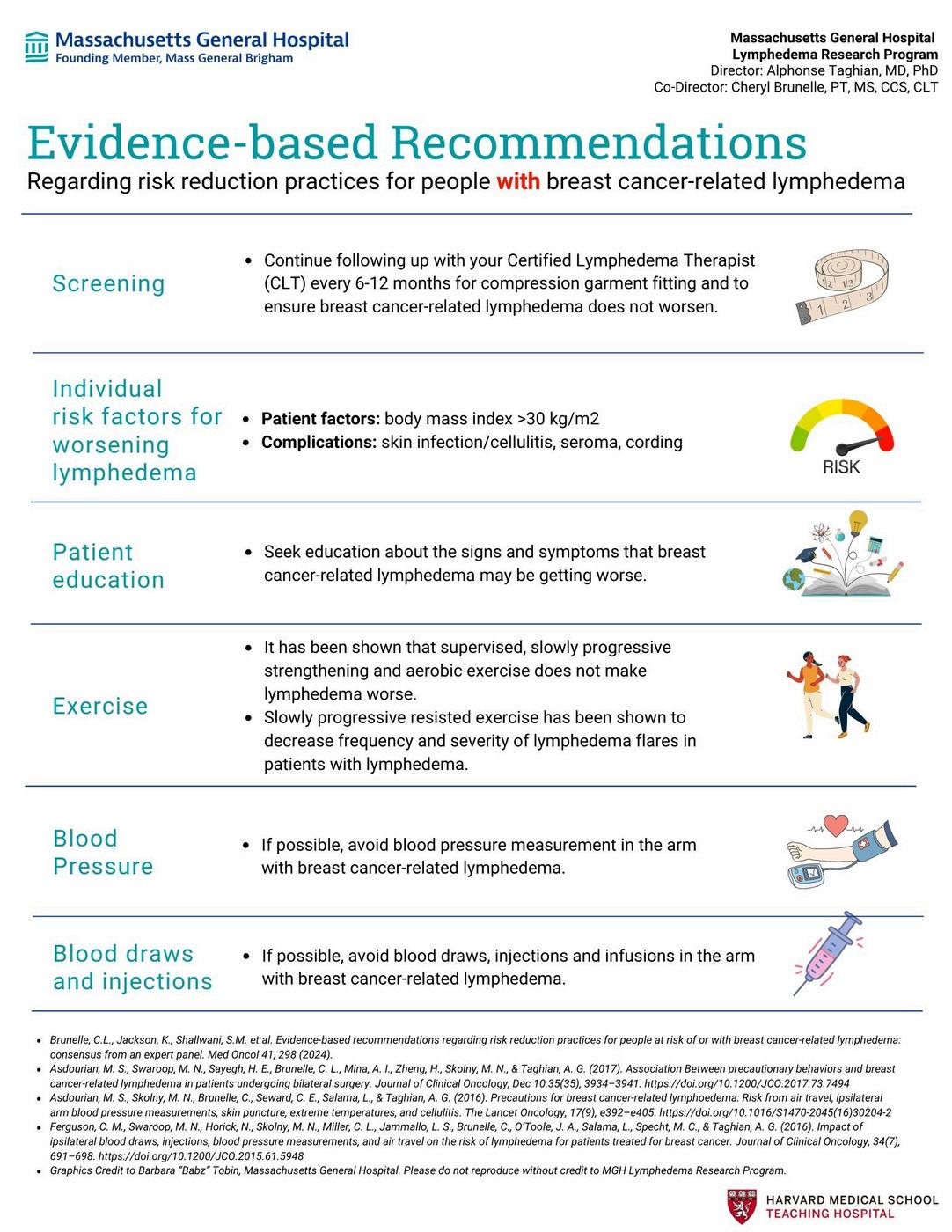
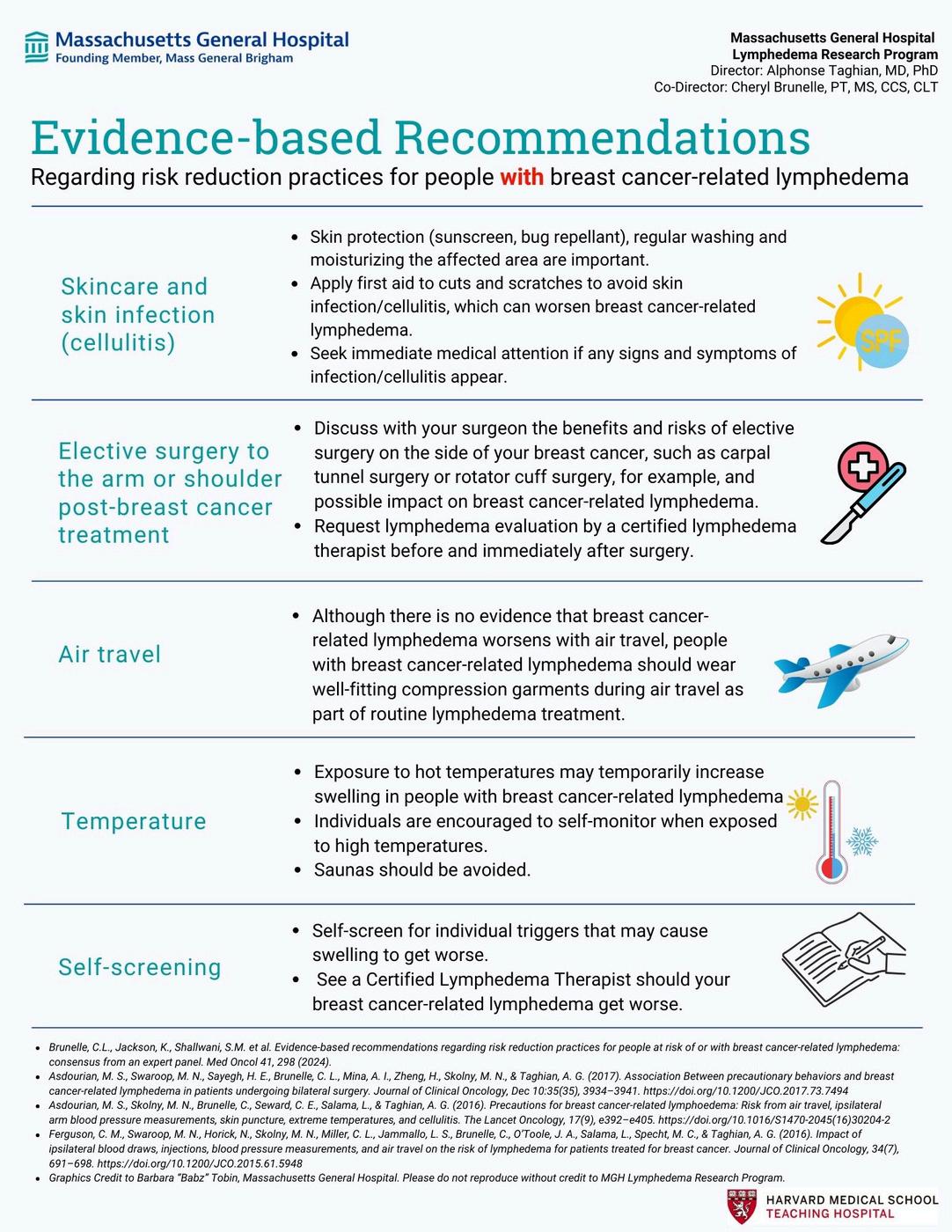
The Pathways Editorial Board is pleased to promote recently published research from the LANA Summit along various themes. This is the first of a series of interviews with some of the authors who were involved, discussing the process, but more importantly, soliciting their ideas of how to translate this new knowledge into clinical practice.


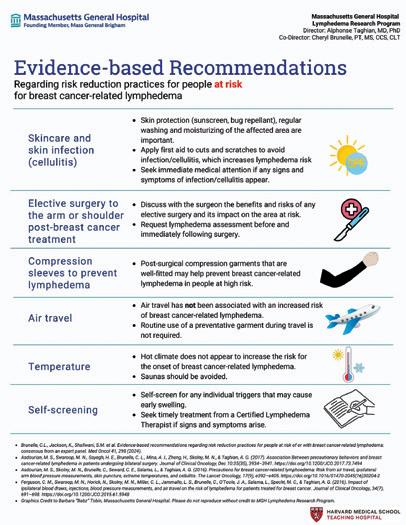
Copyright: Massachusetts General Hospital; Lymphedema Research Program
A transcribed interview by Anna Kennedy with two of the authors (Julie Hunley and Cheryl Brunelle) of the corresponding papers (Bottom of page 18).
Research methodology
AK - What was the decision process for the research methodology used both for the research paper and consensus statement for this new set of recommendations? How did the team choose which areas to include, because so many were not included?
JH - The team consulted the available evidence and the American Cancer Society and determined that a systematic evidence map methodology would meet the study purpose of determining whether current evidence supported or refuted breast cancer-related



lymphedema precautions for women at risk for developing or with lymphedema. We anticipated that there would be gaps in the evidence, so believed that evidence mapping techniques would illustrate risks for each group (at risk or with breast cancer-related lymphedema).
We needed to develop a search strategy that captured evidence related to risks included on the prior precaution list. Some areas were more challenging than others but we’re satisfied that we captured all of the relevant literature to inform the new risk reduction guidelines.
CB - Our group was very meticulous about only including recommendations for which there was an evidence base. If there was no evidence base and the recommendation would really be as a result of consensus opinion only, we did not include it. If we felt the evidence base was sufficient enough to support a recommendation, then we did. There were a lot of different topics within risk reduction that could be addressed, as in the traditional and lengthy “dos and don’ts” list. We had to go into the literature and determine how to categorize those items in ways that we could meaningfully search databases and find evidence related to them.
Cheryl Brunelle PT, MS, CCS, CLT is an APTA Board Certified clinical specialist in physical therapy and the associate director of the Massachusetts General Hospital Breast Cancer-Related Lymphedema Research Program. Julie H. Hunley PhD, OT is Professor of Occupational Therapy at Mount Mary University. She also sits on the LANA Board of Directors and is Chairperson of the Research and Publications Committee.
AK - Why are there different tips for people with lymphedema and those at-risk?
CB - The entire panel felt this was a very important distinction that we needed to make clearly, both in the recommendations and also in the pocket card. Because clinically, these are two very different populations as the evidence base is different. For example, something like blood pressure or injections in an arm at risk of lymphedema – that’s been studied; we have good data to understand what risk, if any, blood pressure measurements and injections impart in a woman at risk. We do NOT have any studies that look at what risk is imparted by blood pressure or injections in an arm WITH lymphedema. So, the recommendation for women with lymphedema would be to avoid these behaviours, simply because we can’t say whether or not there is a risk for those behaviours. If we had evidence, then we would make the recommendations differently. If the recommendations are the same (for both
those at risk and those with lymphedema) –it’s because the evidence is the same.
AK - I can anticipate people reacting to the BCRL risk reduction recommendations and assuming they can be translated to any type of lymphedema. What is your concern with that?
CB - Most, close to all of the research done in this area, is lymphedema related to breast cancer, rather than lymphedema in other etiologies. We simply didn’t have enough evidence outside of BCRL to make conclusions outside of this scope.
AK - The pocket card addresses several audiences (Figure 1). The wording isn’t so clinical that a patient can’t understand, and I don’t think health professionals would be offended. We spent hours as a committee going over what the

words should say, what they should mean and who they’re directed to. It is appropriate for an organization to adopt and put it on their website as patient education material.
CB - Originally I felt the card would be best geared to patients and lymphedema therapists. It’s a set of recommendations summarized into a readable and practical, concise pocket card. Clinicians can put the card in their lab coats, and anyone can access the card electronically through the QR code. But also, for doctors, the card is a succinct part of the publication, as we spent a lot of time to ensure consistency with the larger publication. If doctors really want to see the evidence they can go online to read the full publication. Although the card is fine for a patient to pick up and understand, ideally, a further step would be for it to go through a patient focus group – to make sure it’s truly readable for patients.







Source:

• 135-hours of lymphedema education
75-hr engaging online home study module
60-hr (6 1/2 day) classroom education
• Time-tested, effective and evidence-based curriculum
• Learn from the most experienced instructors in the field
• Fewer days away from home and work
• Greater flexibility to fit your personal schedule
• Exclusive post-graduate resources
• Special pricing for Canadian Therapists
• Breast Cancer Rehabilitation with Jodi Winicour, PT, CLT
• Strength After Breast Cancer with Katie Schmitz, PhD, MPH, FACSM
• Wound Management for CLTs with Jan Weiss, PT, DHS, CLT
• Head & Neck Lymphedema with Heidi Miranda-Walsh, OTR/L, CLT
• Elastic Taping for Lymphedema with Ruth Coopee, OTR/L, CLT
• Add’l courses at klosetraining.com
JH - The card hits the middle of the road in terms of audience. Patients have the capacity to read, at a more detailed level than maybe what we gave them credit for, 20 or 30 years ago. A big change is that people are expecting to drive their own healthcare instead of being passive patients. Advocacy for their own unique set of risk factors is possible for a lot of people.
AK - What are your suggestions in translating the published documents into clinical practice?
CB - There has been a lot of misinformation historically, which will continue to perpetuate until we disseminate this new information as widely as we can. Opportunities like this article in Pathways, public marketing and encouraging as many people as possible to read the full publication. We need to present the work at conferences with lymphedema therapists and encourage lymphedema organizations to

promote the recommendations. We need to focus on getting this new knowledge out to oncologists and to primary care physicians/ GPs because they see these individuals with some frequency and can also introduce and reiterate this education.
I think we can only translate this into clinical practice if the other organizations that also need to update guidelines do so and align with these recommendations. We can’t afford to misalign. We can no longer sit with the status quo and leave things that we know to be incorrect.
AK - How can we help organizations align their patient education with this new research and body of evidence?
JH - I believe that’s a big challenge. I started doing this work in the mid 1990s when we were just fighting to get medical professionals to take ordinary caution with patients who would be at risk or already have lymphedema. I don’t think that all of that was bad. For example, being cautious during medical procedures and rehabilitation was based on the best application of limited evidence and sound clinical reasoning. Current evidence suggests that we can be more nuanced with precautionary guidance. It took so long for those alert bracelets to come out and for warnings to be posted about blood pressure measurements and blood draws. So how do we now make that transition and say, “it depends”. Some healthcare workers are very procedurally trained and may or may not review the chart for patient-specific risk factors. So, I suspect that change will come slowly, and I would imagine it’s going to be by treatment, and by treatment group. That’s why your help in disseminating these articles is so important.
AK - The corporate world is not that much different in some ways than the medical community. At American Express, my team’s responsibility was training 6,000 travel agents across Canada. They had
been trained in certain methods that were tried and true for many years. By tweaking our approach, would we get better training result and increased productivity and sales results? Trying to change one or two procedures and have that accepted and adopted by all the employees in the field was quite a challenge and a very slow process.
JH - I don’t think that this is going to be a whole lot different. I do think it will be an organic process just like it was before. With evidence-based practice, the evidence has a life of its own. It will grow and flourish in some areas. Using a plant metaphor: clipping back a plant so that the strongest parts keep on growing. I think that in some hospital systems or some clinics, they’re going to say, no, we’re going to stick with these, and so it’s not going to grow there. There’s going to be other more progressive places, places that have practices probably more based in evidence, like the larger teaching hospitals. I suspect in this case it’s going to be a little bit like that plant metaphor.
CB - We need to help your readers understand that there was tremendous due process taken coming up with these recommendations. You can’t have more due process that we LANA did. This effort represents a multi-year process in which invited experts were brought together that included an exhaustive review of the literature. There were patients, clinicians, researchers, academics and all types of stakeholders in the room. An exhaustive review of the literature, collaboration with post it notes on those walls where we suggested and analyzed with careful consideration of each word in each sentence until we were happy with the document. It was really like a Delphi process. The Summit was followed by many meetings to write the paper and review and rewrite before submittal for publication.
JH - I agree with Cheryl. This project was much more than just a 2.5-day Summit. For our literature review paper, Betsy, David and
I worked consistently for over a year – taking longer than any other paper I’ve been part of. It was surely a significant effort. As we’re approaching patient education, we don’t have a common day-to-day language or knowledge about lymphedema and the risk factors. Therefore, the need for explicit training is greater. Prospective monitoring is also essential, even though we didn’t include that in our mapping review. However, I’m really glad that it made it onto the editorial as well as onto the other paper. Whether we’re talking about lymphedema or any number of other health risk factors, there’s 1) a segment of the population that is capable and well aware of trying to control their risk; 2) there are other people who have very little awareness, and 3) there are some people who have awareness and are making a choice that they just don’t want to actively work towards reducing their risk. We shouldn’t pass judgment about that. They learn themselves about consequences.
AK - And we have to respect that choice. But we do need to encourage all organizations to align their information with the new evidence-based recommendations so that people can make informed choices.
Editor’s Note:
We encourage our readers (both health professionals and patients) to read beyond the abstracts by clicking on the links and reading the entire research papers and consensus documents below.
The team at the Massachusetts General Hospital (Boston, MA) has adapted and formatted the original pocket card for use in their clinical practice (Pictured on page 15). With their permission, we are distributing them online among our Pathways readers.

Research Paper: Current Evidence on Patient Precautions for Reducing Breast Cancer-Related Lymphedema Manifestation and Progression Risks
https://rdcu.be/d97io Julie Hunley · David Doubblestein · Elizabeth Campione
Consensus Statement: Evidence-based recommendations regarding risk reduction practices for people at risk of or with breast cancer-related lymphedema: consensus from an expert panel https://rdcu.be/d97iy Cheryl L. Brunelle · Katherine Jackson · Shirin M.Shallwani · Julie H. Hunley · Anna Kennedy · Sarah Fench · Alendra Hill · Electra D. Paskett · Katrina Rush · Saskia R.J. Thiadens · Joan White · Paula Stewart

By Doreen Henriksen (as introduced and
transcribed by her daughter, Lynda
Henriksen)
Despite being outside her comfort zone, Doreen was encouraged to share her experience by her certified lymphedema therapist. She was also inspired by fellow lymphedema patient stories. Doreen’s motivation is simple yet profound: she believes people with lymphedema should be seen, heard, and understood. By opening up about her personal journey with this chronic condition, she aims to raise awareness and increase understanding of the challenges faced by those affected by lymphedema. Doreen is grateful to the Pathways Editorial Board for this opportunity. It is our hope that Doreen’s story will resonate with you and your loved ones, fostering empathy and support for the lymphedema community… Lynda Henriksen
How I became “Mrs. Compliant”
My lymphedema journey started in 1965. It was an eventful year when I married the love of my life and we started a family. During my pregnancy, I was diagnosed with toxemia and best rest was ordered. The swelling in my ankles didn’t subside post-delivery. As the years marched on, the swelling progressed into both of my legs. It took 49 years for me to receive an official lymphedema diagnosis!

In 2014, internal medicine specialist, Dr. Rajender Hanmiah confirmed primary lymphedema. He recommended three crucial management steps: moisturizer with the appropriate pH, certified lymphatic drainage massages, and compression stockings. Having already implemented these strategies because I had pretty much figured out for myself that I had lymphedema, I remember replying back to him “check, check and check”! It felt validating to finally have a

diagnosis, but also frustrating to know that I had been right for so long and yet went through decades of feeling like no one was listening, or understood the pain, discomfort and frustration when the swelling prevented me from wearing my shoes or being able to do the things I loved, like dancing with my husband. Worst of all was the feeling that it was somehow my fault. I’m sure many can relate to hearing from doctors and friends alike, “You may have had a lot of salt recently or you need to reduce your sodium intake.”
Today, managing lymphedema is like a full-time job, requiring daily moisturizing, compression stockings, and lymphatic massages. My routine begins with leg and ankle exercises

and includes 30 minutes on my circulation machine before donning custom compression stockings. Due to scoliosis surgery, fusions in my back limit my ability to bend down. The tall butler and rubber gloves that I use are very helpful donning tools. I also appreciate my husband’s kind support, especially at night when it’s time to remove my custom day stockings, do 30 minutes on my circulation machine and then don my night stockings. I’m so dedicated to this daily routine that my husband jokingly started calling me Mrs. Compliant.

Doreen Henriksen, a devoted wife, loving Nana, and soon-to-be great-grandmother, lives in Brant County, Ontario. Married to her gold-hearted (and Kenny Rogers look alike!) husband, Wayne, for 60 years, Doreen recently celebrated her 78th birthday.
Recognizing the importance of the other things I do to manage lymphedema also helps me to live my life to my fullest capacity each day. I’ve enjoyed learning Tai Chi with a friend and making use of the private pool in our retirement community for swimming and water exercises. My walking poles are put to good use in warmer weather, helping me with balance and endurance, even if it’s for a short distance. In the summer I enjoy gardening and flower tending.



• Decreases edema post-mastectomy
• Decreasing graduated compression from wrist to shoulder
• Revolutionary 3-dimensional fabric. Exceptional softness and elasticity


• Manages lipedema, DVT, varicosis, lymphedema
• Graduated compression 15-21 mmHg
• 3-dimensional fabric stimulates microcirculation. Helps eliminate excess fluid
• Available in “Pro” open-toe format. Avoids chafing at the ankles

I also stay hydrated, eat nutritiously, rest my legs, and engage in creative activities like crocheting and reading. Managing lymphedema has become my mission, and I hope that sharing my story will raise awareness and understanding.
Embracing compliance has allowed me to maintain my mobility and quality of life, enabling me to enjoy simple but meaningful pleasures like driving and spending time
with my grandchildren, running errands, and supporting friends and my community.
Over the years, I’ve been fortunate to travel extensively, creating cherished memories with my husband. We have been across Cuba, Arizona, California, and Alaska. We experienced an RV adventure last summer through Nova Scotia and Newfoundland to visit family and spend weeks exploring with my daughter and son-in-law. It was the trip of a lifetime.
My care team, including my experienced lymphedema therapist Pamela Renneberg Monarch, my certified garment fitter, family doctor, and loving family and friends, have been invaluable in my lymphedema journey. However, retirement funds are limited for treatments, and the Ontario Assisted Device Program only partially covers the cost of my compression stockings. As someone living with lymphedema, I firmly believe that everyone facing this chronic condition deserves access to optimal care. Together, we must urge our government to provide more comprehensive

support, including coverage for lymphedema treatments, assistive devices, resources, and better healthcare professional training. I urge you to join me in advocating for the millions of individuals affected by lymphedema. Together, we can create a future where everyone has access to the care and support they need to live their lives to the fullest. LP




The University of Alberta (UofA) community is mourning the loss of visionary leader and philanthropist Dianne Kipnes, who passed away on Dec. 26, 2024, at the age of 81.
Dianne’s passion for medical research was driven in part by her own experience as a cervical cancer patient. Five years after undergoing surgery and treatment in 2004, she developed severe lymphedema in her legs. The condition leads to debilitating swelling and pain and affects more than a million Canadians.
She found there were few treatments available aside from massage and compression therapy, and little research being done into the condition. So, she and Irving set out to change that. They established the Dianne and Irving Kipnes Chair in Lymphatic Disorders—the first position of its kind in Canada—with an initial $5-million donation in 2018, naming scientist Spencer Gibson as the inaugural chair. An additional
$1 million was matched by the University Hospital Foundation for a total of $7 million to establish the research lab, which now includes six graduate students, a research associate and a clinical co-ordinator along with Gibson.
“Lymphedema destroys quality of life,” says Gibson. “A lot of these patients feel abandoned by the medical field. They’re sent off to a rehab clinic where they get compression therapy and that’s it. They’re kind of left to their own devices. And Dianne actually experienced this.”
The goal of Gibson’s research is to reveal the causes of lymphedema and other lymphatic disorders, understand why some people are affected while others are not, and propose new, more effective treatments to improve the lives of patients. He is looking to establish a registry of lymphedema patients in Alberta, and advocates for better care through the Alberta Lymphedema Association and the Canadian Lymphedema Framework

“Dianne was a very practical, handson person,” says Gibson. “She didn’t just give money and walk away. She wanted to be involved every step along the way in terms of understanding what we were doing, where we were going, and whether there was anything she could do to help. That’s her legacy. “I’ve never met anybody else like her.”
Dianne also served on the boards of the Alberta Cancer Foundation, TELUS Edmonton Community Foundation, Capital Care Foundation, Edmonton Opera, the National Arts Centre and Fielding Graduate University
Dianne was truly a pillar of the U of A community, and her memory lives on through the many lives she has touched and will continue to touch through her generosity and vision.
Source: Condensed (abridged) with permission from University of Alberta News.



4 WEEKS of intensive lymphological decongestive therapy includes:
• Specialist medical care by experienced MD‘s
• Daily decongestive therapy by our specialised lymphedema therapists (expert manual lymph drainage and bandaging) and many different decongestive movement therapies as part of group therapy
• Wound treatment if necessary by our certified wound experts and
• Accommodation and meals at the Foeldi Clinic psychological support if necessary by our psychotherapists
By Sonja Redden
The first ever lymphedema conference in the Northern Health Region of British Columbia was hosted in Prince George in the fall of 2024. It consisted of an interdisciplinary “Lymphedema Education Day” (LED) for physicians and health care professionals on November 22, and a half day “Lymphedema Workshop Day” (LWD) for health care professionals on November 23.
The LED was organized by a planning committee1 consisting of dedicated volunteers, physicians, and Northern Health employees. Over 100 health care professionals and physicians attended either in person or online. The event was accredited for continuing medical education for physicians. We are incredibly thankful for the support we received from Northern Health, BC Rural Continuing Medical Education, the Spirit of the North Healthcare Foundation, and the BC Lymphedema Association. The LWD was made possible by generous industry support and provided an opportunity for health care professionals to learn practical skills as well as learning about the availability of products used to treat lymphedema.
The objectives of this conference were to learn about best practice lymphedema management and to discuss accessibility and affordability issues, and strategies to improve access to care for patients in Northern Health’s various Health Service delivery areas.
As in many other areas across Canada,


lymphedema in B.C. is underdiagnosed, undertreated, and underfunded. It is not hard to imagine how challenges in lymphedema care are compounded by our vast geography (600 square km) in the many rural and remote communities in our

Northern health Region. The development and distribution of lymphedema related resources and practice tools for physicians and health care professionals were identified as important components in developing first steps to improved care.
Sonja Redden, BScPT, CLT has focused her work on treating patients with lymphedema ever since becoming a certified lymphedema therapist (Vodder) in 2005. She is the owner of Healing Rivers Physiotherapy (Prince George, B.C.), and has volunteered for the Canadian Lymphedema Framework since 2013.
Themes and values
Inter-professionalism, teamwork, and client centered care were overarching themes throughout these education days and are key to successful lymphedema management.
The main presenter at the LED was Dr. David Keast, Chair of the Canadian Lymphedema Framework (CLF).
Dr. Keast talked about lymphedema as an under-recognized and under-treated condition. He reported on the new prevalence study (published in the Winter 2024/2025 issue of Pathways), concluding that about 1.25 million Canadians suffer from chronic edema/ lymphedema.
Dr. Keast covered best practice treatment of lymphedema, including skin hygiene and exercise, the effectiveness of various compression, and the roles of manual lymphatic drainage, current surgical approaches and lifestyle changes. He elaborated on challenges of lymphedema care and concluded with several case studies. In the afternoon, Dr. Keast spoke about cellulitis infections and wound management in lymphedema.
1. Planning Committee members: Dr. Dick Raymond, Dr. Khalid Bashir, Dr. Brian Hillhouse, Sonja Redden PT, Lila Reynolds, Jayleen Emery, Santaya Garnot, Diane Sarmiento, and Natalie Allan.
2. Source: https://www.bcbudget.gov.bc.ca/annual_reports/2005_2006/hlth/appendix_1.htm

We are thankful for Dr. Keast’s invaluable knowledge which has set us on a trajectory of ongoing improvement in health care for people living with lymphedema in Northern BC.
Other speakers included Dr. Paul Winwood, Associate Vice President, Division of Medical Sciences, University of Northern BC, who provided a warm introduction to the event and contributed to the panel session. Jenna LaFleche, RMT, a member of the board of directors of the BC Lymphedema Association, spoke on compression modalities and her experience in cancer-related lymphedema care. Sonja Redden, PT, a past member of the Education Working Group of the CLF, spoke on the challenges of compression therapy in non-cancer related lymphedema care.
The presentations of two people living with lymphedema reminded us of the human aspect of medicine. These patients were grateful to be able to share their stories about
the impacts of the disease on everyday life, ongoing management challenges, and the fear of recurring, life-threatening cellulitis infections.
An overview of resources available included a directory of therapists and garment fitters, services provided through the BC Lymphedema Association, and information about a regional lymphedema garment fund housed within the Spirit of the North Healthcare Foundation.
assessment skills and discuss treatment planning using a case-based learning approach. Attendees were also able to practice multi-layer bandaging and learn about the application of Velcro Reduction Kits, provided by our industry partners.


Lastly, a panel session provided an opportunity to ask questions to spark discussions on how to move lymphedema care forward in our vast health region.

The Lymphedema Workshop Day gave health care providers the opportunity to apply
This event was a great success. It not only provided new insights but also stimulated increased interest in lymphedema. Many attendees who work in public practice confirmed the need to have coordinated lymphedema services provided through the public health care system. We plan to carry this momentum forward in the hopes that lymphedema will be recognized and treated not just as a symptom of some other disease, but as a chronic disease in its own right. Lymphedema deserves its own continuum of care model, from prevention to long-term management, which needs to be publicly funded. LP


By Dr. Mei Rosemary Fu
Conventionally, breast cancer survivors are instructed to avoid certain daily-living activities or incidents to reduce the risk of breast cancerrelated lymphedema (BCLE).1-2 These activities or incidents include using the affected arm and hand to lift objects, carrying shoulder bags, and avoiding infection, sunburn, cutting cuticles, oil splashes and steam burn.1-2
A recent published study3-5 in Annals of Surgical Oncology provided much-needed evidence regarding the daily-living risks of lymphedema and offers insights into targeted strategies to reduce the risk of lymphedema. This article is available online (https://doi.org/10.1245/s10434-02415946-x) or as a PDF https://link.springer.com/content/pdf/10.1245/ s10434-024-15946-x.pdf. (See synopsis of the study on the right).
This larger cross-sectional and observational study of 567 breast cancer survivors examined the effects of daily-living risks on BCLE. As presented in the published Visual Abstract,5 significant odds of BCLE were associated with infection (OR = 2.58, 95% CI = 1.95-3.42), cuts/scratches (OR = 2.65, 95% CI = 1.97-3.56), sunburn (OR = 1.89, 95% CI = 1.39-3.56), oil splash or steam burns (OR = 2.08, 95% CI = 1.53-3.83), insect bites (OR = 1.59, 95% CI = 1.18-2.13). The daily-living risks were clustered into factors related to skin trauma and carrying objects. Skin trauma risk was significantly associated with BCLE (B = 0.539, z = 3.926, OR = 1.714, 95% CI = 1.312-2.250, p < 0.001). Having 3, 4, or 5 skin trauma risks significantly increased the odds of BCLE to 4.31, 5.14, and 6.94 times. No significant associations between daily-living risks of carrying or lifting heavy objects, carrying groceries, and lifting weights. Carrying a shoulder bag on the affected arm was significantly associated with BCLE, with odds of 0.55, indicating that carrying a shoulder bag may have a protective effect on BCLE.
As complete avoidance of daily-living risks is challenging,3 it is critical for patients to be trained for self-care skills for daily skin care, preventing and managing skin trauma (Box 1).3 More prospective and longitudinal research is vital to further validate daily-living risks for BCLE. LP
References
The Effects of Daily-Living Risks on Breast Cancer-Related Lymphedema (BCLE)















Strategies to Minimize Daily-Living Risks of Breast Cancer-Related Lymphedema18, 22-25
What should I do to prevent trauma/injuries in my affected hand and arm?
4 Wear protective gloves while gardening or doing household chores (washing dishes, cleaning, or cooking).
4 Wear oven mitts when taking hot pots or casseroles out of the oven.
4 Apply sunscreen (SPF 30 or more) or wear long-sleeve clothes to prevent sunburn.
4 Apply insect repellant or wear an insect-repellant band to prevent insect bites.
4 Cuticles should be pushed back and kept moist; Manicure tools should be sterilized
What should I do for daily skin care?
4 Keep skin clean and dry.
4 Use water-based lotions that help skin to absorb readily and low-pH lotions that provide an active barrier against infection.
What should I do when I have cuts or scratches on my affected arm or hand?
4 Wash the area with soap and water.
4 Apply an antibiotic cream or ointment.
4 Cover with a clean and dry dressing as needed.
4 If the area becomes worse, call your doctor.
What should I do when I have mosquito or insect bites?
4 For itching, apply hydrocortisone ointment.
4 If the area is red and slightly inflamed, apply an antibiotic ointment.
4 If the area becomes worse, call your doctor.
What should I do if I notice any changes in my affected arm or hand?
4 Do not ignore any changes in your affected arm or hand.
4 If you notice a rash, blisters, redness, increased warmth/heat in the arm and/or pain, please contact your doctor right away.
1. Shen A, Lu Q, Fu X, et al. Risk factors of unilateral breast cancer-related lymphedema: an updated systematic review and meta-analysis of 84 cohort studies. Support Care Cancer. 2022;31(1):18. Published 2022 Dec 14. doi:10.1007/s00520-022-07508-2
2. Cemal Y, Pusic A, Mehrara BJ. Preventative measures for lymphedema: separating fact from fiction. J Am Coll Surg. Oct 2011; 213(4):543-51.
3. Fu MR, Liu B, Qiu JM, et al. The Effects of Daily-Living Risks on Breast Cancer-Related Lymphedema. Ann Surg Oncol. 2024;31(12):8076-8085. doi:10.1245/s10434-024-15946-x.
4. Fu MR, Liu B, Qiu JM, et al. ASO Author Reflections: Infection and Skin Trauma Incrementally Increase the Risk of Breast Cancer-Related Lymphedema. Ann Surg Oncol. 2024;31(12):8110-8111. doi:10.1245/s10434-024-16078-y
5. Fu, M.R., Liu, B., Qiu, J.M. Sun, Y., Axelrod, D., Guth, A., Korth, S., Kremer, H.L., Wang, Y. (2024). ASO Visual Abstract: The Effects of Daily-Living Risks on Breast CancerRelated Lymphedema. Ann Surg Oncol (2024).

Dr. Mei Rosemary Fu, PhD, RN, FAAN, is The Dorothy and Dale Thompson Missouri Endowed Professor in Nursing and Associate Dean for Research at University of Missouri-Kansas City School of Nursing and Health Studies. Email: mei.fu@umkc.edu or mf67@nyu.edu
Disclosures: No conflicts of interest.






















In the past, individuals with lymphedema were advised to protect the limb with lymphedema in an effort to avoid worsening the swelling.1 “Old school” thinking was that the increased blood flow to the limb from exercise would further compromise the lymphatic system’s ability to drain fluid. We now know that individuals with lymphedema can safely perform and benefit from properly prescribed exercise to help them self-manage their lymphedema, improve their health and quality of life.2

































of movement is helpful to your lymphatic system. Moving frequently during the day, even for short periods of time is helpful!
Exercises initially prescribed for your lymphedema may include gentle stretches, range of motion exercises, resistance (strength training) exercise, and lowimpact exercises such as walking, swimming or Tai Chi.

help drain fluid from the swollen limb or region. This is done by exercising the larger muscles closest to the center of your body first, followed by exercises for the muscles at the top of your limb working down to your fingers (upper limb lymphedema) or your toes (lower limb lymphedema), and then reversing the exercises back to the start.


















































Following the decongestive exercise sequence that is part of Complete Decongestive Therapy is a good place The exercise sequence aims to first stimulate the lymphatic system and clear the fluid centrally and takes advantage of the muscle pump effect to




































If you are unsure of what to do, or are struggling with lymphedema symptoms, we recommend that you talk to your lymphedema therapist. LP
Source and references can be found at https:// canadalymph.ca/pathways-references






















Objective: This study aims to construct and evaluate an individualized nomogram for predicting the risk of lower limb lymphedema after cervical cancer surgery. Healthcare professionals can utilize line chart models to predict the probability of postoperative lower limb lymphedema in different patients, allowing for the early identification of high-risk patients and facilitating early prevention and treatment. Methods: A retrospective study was conducted among 411 cervical cancer patients treated at our hospital from May 2021 to December 2023. The patients were randomly divided into a modeling group (313 cases) and a validation group (98 cases) according to an approximate 3:1 ratio. The modeling group was further divided into a lower limb lymphedema group (61 cases) and a non-lower limb lymphedema group (252 cases) based on the presence of postoperative lower limb lymphedema. Multiple factors Logistic regression was used to identify risk factors, and a nomogram was constructed using R software version 4.0.2, with internal and external validation performed. Results: Risk factors for lower limb lymphedema following cervical cancer surgery include age 60 years or older, a Body Mass Index (BMI) of 24 kg/m² or higher, hypertension, the removal of 30 or more lymph nodes, adjuvant radiotherapy and chemotherapy, and prolonged standing for


six hours or more (P < 0.05). Internal and external validation results demonstrated that the calibration curve closely aligned with the ideal curve. The Area Under Curve(AUC) of the Receiver Operating Characteristic(ROC) curve was 0.890 (95% CI: 0.844 ∼ 0.936) and 0.876 (95% CI: 0.821 ∼ 0.930), indicating high model calibration and discrimination. Decision Curve Analysis (DCA) curve revealed that the Logistic model had good net returns and high clinical practicality when the probability range of the high-risk threshold was 0.11 ∼ 0.98. Conclusion: The nomogram developed using factors such as age, BMI, hypertension, number of lymph nodes dissected, adjuvant radiotherapy and chemotherapy, and duration of standing, has strong predictive value and offers significant clinical benefits, making it a valuable tool for clinical decision-making.
Source:
Primary lymphedema: systemic lymphatic
Background: Primary lymphedema, a condition characterized by impaired lymphatic function, has long remained underexplored. Current diagnostic approaches rely on clinical history and genetic testing, yet the genetic underpinnings remain elusive in many cases. Traditional thinking suggests that primary lymphedema is confined to specific anatomical regions, but our experience


challenges this notion. We hypothesize that primary lymphedema is systemic lymphatic dysfunction. Methods: All patients with clinical diagnosis of primary lymphedema from January 2020 to April 2022 were included in our study. Demographic data, medical and surgical history, and indocyanine green (ICG) lymphographic findings were collected. Results: A total of 152 patients met our inclusion criteria. We observed a predominance of female patients (75%) and a mean age of 43.9 years. The onset of swelling varied, with most patients (82.3%) experiencing it in their lower extremities. Notably, ICG lymphography revealed abnormal lymphatic findings in all symptomatic limbs, affecting multiple extremities in 97.4% of patients. Importantly, even among patients initially presenting with limited symptoms, asymptomatic extremities exhibited lymphatic defects. In addition, the extent of lymphatic disease, assessed through ICG lymphography, surpassed clinical symptoms in 80% of cases, underscoring the systemic nature of primary lymphedema. Conclusions: Our study suggests that primary lymphedema is a systemic lymphatic insufficiency, affecting the entire lymphatic system. This underscores the importance of comprehensive assessments, even with limited symptoms, to facilitate earlier diagnosis and more effective treatment approaches.
Source: Primary Lymphedema: Anatomically isolated or a pervasive systemic disorder? Plast Reconstr Surg Glob Open. 2024 Dec 20. PMC11661748







Mar 6, 2025
Worldwide
Apr 12-15, 2025
Las Vegas, NV
Jun - Nov, 2025
USA
May 16-18, 2025
Fremantle, Australia
Jun 12-14, 2025
Chicago, IL
Oct 6-8, 2025
Chester, UK
Oct 15-19, 2025
Antalya, Turkey
Oct 23-24, 2025
Niagara Falls, Canada
World Lymphedema Day (WLD) is an annual celebratory event to educate the world about lymphatic diseases. Visit the following links to read about advocate-driven world events or contact your provincial association to learn about local events. n www.canadalymph.ca/WLD/ n https://lymphaticnetwork.org/wld/
Power Lymphatics 2025 n https://thepowersymposium.com/power-lymphatics/
NLN 2025 Conference Series: Four events in various cities. n https://lymphnet.org/2025-conferences
Australasian Lymphology Association Symposium 2025 n https://www.lymphoedema.org.au/education-&-resources
LE&RN: Lymphatic Forum 2025 n https://lymphaticnetwork.org
The #BLS2025 Conference n https://www.theblsconference.com/
30th ISL World Congress of Lymphology n https://2025lymphology.org/
12th International Lymphoedema Framework Conference, with Canadian Lymphedema Framework and International Lipoedema Association. Building Bridges: Connecting Global Perspectives. n Register: www.ILF2025.com

Subscription information at www.canadalymph.ca/subscriptions

This is a collaborative petition by the Canadian Lymphedema Framework together with:









The Canadian Lymphedema Framework (CLF) wishes to thank these partners for their support in making this magazine a reality.




The CLF is an academic and patient collaboration, working to improve lymphedema management for lymphedema and related disorders in Canada.









Compreflex®, the innovative inelastic compression wrap designed to optimize the management of venous and lymphatic conditions.
Tailored for those who require effective edema control and enhanced venous support, Compreflex® offers a customizable solution to not only meet diverse clinical needs, but enhancequalityof life.


REFERENCES • SUPPORTING DOCUMENTS • OUTSERTS

A full set of references can be found at:
https://www.canadalymph.ca/pathways-references/


New best practice recommendations
For the prevention and management of wounds related to lower limb lymphedema
By David Keast and Janet Kuhnke
1. Kuhnke JL, Burrows C, Evans R, Botros M, Hoover J, Corks I. Best Practice Recommendation Updates 2024: Methodology for developing foundations of best practice for skin and wound management 2023;21(2): 62-65 DOI: 10 56885/BEGL1924
2 Keast DH, Burian EA, Moffatt CJ, Nørregaard S, Karlsmark T The dilemma of wounds in chronic oedema/lymphoedema J Wound Care 2021 Dec 1;30(Sup12b):7-17 DOI: 10 12968/jowc 2021 30 Sup12b 7
3 Carroll BJ, Singhal D Advances in lymphedema: an under-recognized disease with a hopeful future for patients. Vasc Med. 2024 Feb;29(1):70-84. DOI: 10.1177/1358863X231215329
4. Torgbenu E, Luckett T, Buhagiar M, Phillips JL. Practice points for lymphoedema care in low- and middle- income countries developed by nominal group technique BMC Health Serv Res 2023 Jul 8;23(1):740 DOI: 10 1186/s12913-023-09786-w
5 Borman P Lymphedema diagnosis, treatment, and follow-up from the view point of physical medicine and rehabilitation specialists. Turk J Phys Med Rehabil. 2018 Sep 3;64(3):179-197. DOI: 10.5606/tftrd.2018.3539
6. O'Donnell TF Jr, Allison GM, Iafrati MD. A systematic review of guidelines for lymphedema and the need for contemporary intersocietal guidelines for the management of lymphedema J Vasc Surg Venous Lymphat Disord 2020 Jul;8(4):676-684. DOI: 10.1016/j.jvsv.2020.03.006
7 Letellier M, Keast DH, Towers A, Damji A The prevalence of lymphedema in Canada: an update. 2024 winter. Available from : https://issuu.com/canadianlymphedemaframework/docs/winter pathways 2024-25 volu me 14 issue 1 refer
8 Keast DH Obesity: The Canadian perspective Lymphedema Pathways 2020 Summer:14-15 Available from: https://issuu.com/canadianlymphedemaframework/docs/obesity. canadian per-spective lymphedema related
9. Statistics Canada. An overview of weight and height measurements on World Obesity Day. 2024 Mar 24. Available from: https://www statcan gc ca/o1/en/plus/5742-overview-weight-and-height-measurements-w orld-obesity-day
Keast D, Towers A The rising prevalence of lymphedema in Canada: a continuing dialogue Canadian Lymphedema Magazine. 2017(Spring):5-8. Available from: https://canadalymph.ca/wp-content/uploads/2015/04/PATHWAYS-Spring-2017-The-risin gprevalence-of-lymphedema-in-Canada pdf
11 Keast DH, Kuhnke JL, Hettrick H Lymphedema: issues and interventions Wound Care Canada 2019;17(2):10-22 Available from: https://www.woundscanada.ca/docman/public/wound-care-canada-magazine/2019-vol-1 7-no-2/1474-lymphedema/file
By Anne-Marie Joncas
BOX 1
National foundations to approach
Health Canada
Potential alignment: Funding and support for initiatives that improve healthcare delivery for chronic conditions like lymphedema
Canadian Cancer Society
Potential alignment: Lymphedema related to cancer treatments, such as breast cancer surgery
Heart & Stroke Foundation
Potential alignment: Shared concerns around circulatory health and swelling
The Kidney Foundation of Canada
Potential alignment: Potential overlaps in chronic illness management and patient education.
Canadian Diabetes Association (Diabetes Canada) + provincial divisions
Potential alignment: Collaboration on wounds, swelling and circulation issues common in diabetes patients
Canadian Institute of Health Research (CIHR)
Focus: Health research funding across various fields, including chronic disease and community care
Mental Health Foundation of Canada
Potential alignment: Addressing the psychological impact of living with a chronic condition like lymphedema
Lymphatic Education & Research Network (LE&RN) - Canada Chapter Direct alignment: Advocacy, awareness, and funding for lymphedema-specific initiatives
Canadian Society for Vascular Surgery (CSVS)
Alignment: Advocates multidisciplinary management of chronic vascular conditions
Fondation de l'Institut de Cardiologie de Montréal
Alignment: Although focused on the heart, it also funds projects related to vascular health, including venous insufficiency.
Obesity Canada
Potential alignment: Lymphedema often intersects with obesity issues.
Wounds Canada
Potential alignment: Overlaps in treatment of chronic wounds and swelling
Public Health Agency of Canada (PHAC)
While not a foundation, PHAC funds public health initiatives and could support lymphedema advocacy campaigns.
Canadian Foundation for Healthcare Improvement (CFHI)
Potential alignment: Structuring care pathways for lymphedema patients
Patients for Patient Safety Canada (PPSC)
Potential alignment: Reducing risks associated with untreated lymphedema
By Christine Chandler
The British Columbia Lymphedema Association (BCLA) developed a patient survey to engage the province-wide community. We had a 30% response rate to the 600 surveys distributed through BCLA members, contacts, patients of lymphedema therapists and doctors With the help of two pre-med student volunteers, data was condensed into a series of Infographics depicting: demographics, health region, length of time before diagnosis, costs involved and effect on quality of life.
INFOGRAPHICS - not included in the article
See Infographics on the following pages.
The Pathways Editorial Board is pleased to promote recently published research from the LANA Summit along various themes This is the first of a series of interviews with some of the authors who were involved, discussing the process, but more importantly, soliciting their ideas of how to translate this new knowledge into clinical practice

PAPER: Current Evidence on Patient Precautions for Reducing Breast Cancer-Related Lymphedema Manifestation and Progression Risks:
https://pubmed.ncbi.nlm.nih.gov/39417905/ Julie Hunley, David Doubblestein, Elizabeth Campione
CONSENSUS STATEMENT: Evidence-based recommendations regarding risk reduction practices for people at risk of or with breast cancer-related lymphedema: consensus https://pubmed.ncbi.nlm.nih.gov/39438352/
from an expert panel:
Cheryl L Brunelle, Katherine Jackson, Shirin M Shallwani, Julie H Hunley, Anna Kennedy, Sarah French, Alexandra Hill, Electra D Paskett, Katrina Rush, Saskia R J Thiadens, Joan White, and Paula Stewart
A transcribed interview by Anna Kennedy with two of the authors (Julie Hunley and Cheryl Brunelle) of the corresponding papers

Scan the QR code or visit the link: www tinyurl com/RiskCardBCRL to access the adapted pocket card from Massachusetts Hospital

By Mei Rosemary Fu
A recent published study 3-5 in Annals of Surgical Oncology provided much-needed evidence regarding the daily-living risks of lymphedema and offers insights into targeted strategies to reduce the risk of lymphedema.This published article is available online (https://doi.org/10.1245/s10434-024-15946-x) or as a PDF https://link springer com/content/pdf/10 1245/s10434-024-15946-x pdf The synopsis of the study is in Spring Pathways
1 Shen A, Lu Q, Fu X, et al Risk factors of unilateral breast cancer-related lymphedema: an updated systematic review and meta-analysis of 84 cohort studies Support Care Cancer. 2022;31(1):18. Published 2022 Dec 14. doi:10.1007/s00520-022-07508-2
2. Cemal Y, Pusic A, Mehrara BJ. Preventative measures for lymphedema: separating fact from fiction. J Am Coll Surg. Oct 2011; 213(4):543-51.
3 Fu MR, Liu B, Qiu JM, et al The Effects of Daily-Living Risks on Breast Cancer-Related Lymphedema Ann Surg Oncol 2024;31(12):8076-8085 doi:10 1245/s10434-024-15946-x
4 Fu MR, Liu B, Qiu JM, et al ASO Author Reflections: Infection and Skin Trauma Incrementally Increase the Risk of Breast Cancer-Related Lymphedema. Ann Surg Oncol 2024;31(12):8110-8111 doi:10 1245/s10434-024-16078-y
5. Fu, M.R., Liu, B., Qiu, J.M. Sun, Y., Axelrod, D., Guth, A., Korth, S., Kremer, H.L., Wang, Y (2024) ASO Visual Abstract: The Effects of Daily-Living Risks on Breast Cancer-Related Lymphedema Ann Surg Oncol (2024)
Exercise for your lymphedema In the past, individuals with lymphedema were advised to protect the limb with lymphedema in an effort to avoid worsening the swelling 1 “Old school” thinking was that the increased blood flow to the limb from exercise would further compromise the lymphatic system’s ability to drain fluid. We now know that individuals with lymphedema can safely perform and benefit from properly prescribed exercise to help them self-manage their lymphedema, improve their health and quality of life 2
REFERENCES
1 Johansson, K , and S Hayes "A Historical Account of the Role of Exercise in the Prevention and Treatment of Cancer-Related Lymphedema " Lymphology 53, no 2 (2020): 55-62.
2 Schmitz, K H "Balancing Lymphedema Risk: Exercise Versus Deconditioning for Breast Cancer Survivors."Exerc Sport Sci Rev 38, no. 1 (2010): 17-24.
3. Rockson, S. G., V. Keeley, S. Kilbreath, A. Szuba, and A. Towers. "Cancer-Associated Secondary Lymphoedema " Nat Rev Dis Primers 5, no 1 (2019): 22

A progressive, chronic inflammatory condition that can affect any area of the body, most commonly the limbs. Early diagnosis and adequate management are important.
PRIMARY
Hereditary
SECONDARY
Obesity, immobility
Congenital Venous Disease
Many cancers and their treatments (lymph node dissection, radiation)
Surgical interventions
Trauma, infection
Recurrent bacterial cellulitis in the affected limb, risk of septicemia
Skin and tissue changes, e.g., papillomata, thickened skin (pachydermia), dermatitis
Chronic wounds, lymphorrhea, lymph cysts
Reduced function, work disability
Negative psychological/body image/social impact
Edema (pitting or non-pitting)
Stemmer sign
Rule out deep venous thrombosis, cancer, cardiac, renal, liver disease and hypoproteinemia
Identify causes of co-existing pain
Treatment
Skin
Cleansing
Moisturizing
Avoiding trauma
physical activity
eating Compression garments and devices
Surgical treatments for lymphedema are being piloted and investigated in Canada.
No current, effective drug treatments
Diuretics
Access the digital card at: tinyurl.com/Lymphedema-Info
For more information on treating lymphedema and resources for your patients please contact:

Visit www.canadalymph.ca for comprehensive information on lymphedema, assessment, and educational tools for health professionals. You can subscribe to Pathways magazine, and enroll in the online microcourse co-developed by the CLF and the University of Alberta on lymphedema management. Visit: uab.ca/pd
Prevalence in Canada
1.25 million for 41.5 million population
Canadian Lymphedema Framework 2024
Chronic Edema Related to Venous Disease (Prevalence Undetermined)
Cancer-Related 350,000
Disabilities/Chair-Bound 113,000
Surgeries, Non-Cancer 83,000
Visit the International Lymphoedema Framework (www.lympho.org) to access International Best Practice Guidelines, Focus and Position Documents on topics such as Lymphedema for Palliative Care, Compression Therapy, Care of Children, Surgical Interventions, etc.

Primary Lymphedema 21,000 Mean incidence of cancer-related lymphedema from systematic reviews
Cervical, Vulvar, Ovarian
Prostate, Bladder, Penile Sarcoma: 30% Head and Neck: 60%
Reference: Letellier et al 2024 Learn more: tinyURL.com/LE-Prevalence
The CLF proudly partners with eight provincial lymphedema associations across Canada.
Contact your provincial association for information on local resources including certified lymphedema therapists, compression garment fitters and patient support groups. Visit: www. canadalymph.ca/provinces
