Welcome to Volume Four, Issue One of Together: Stories of Collective Impact
This Fall 2025 issue brings forward stories that highlight the power of collaboration, creativity, and connection across health and social care. From innovative interprofessional electives and global partnerships to arts-based learning and systems-focused initiatives, this issue showcases the many ways people are reimagining education and care. You’ll also see the growing global reach of this work through contributions from partners in Singapore, Ethiopia, Indonesia, the United States, and beyond.
Our cover art, “Fragile: Handle With Care” by Kim Neudorf, offers a powerful entry point into this issue’s reflections on teamwork and transition, reminding us how deeply relationships, communication, and trust shape each step of the care journey.
We are also honoured to celebrate Professor Sylvia Langlois and her extraordinary contributions to interprofessional education, patient partnership, and collaborative leadership. Her Retirement Tea story reflects the collaborative community she has cultivated over her decades of leadership.
If you are reading Together for the first time, WELCOME! This magazine exists to share stories that connect us and inspire collective impact. To our returning readers and contributors, thank you for continuing to share your work, reflections, and art. We look forward to your f uture submissions , feedback, and reactions
Thank you for reading, and enjoy this issue.
With Gratitude, Elizabeth (Eli) Cadavid Lead Editor, on behalf of the CACHE Team
CACHE Editorial Team, Fall 2025
Eli Cadavid (Lead Editor); Farah Friesen; Kaitlyn Lau; Stella Ng; Belinda Vilhena
The views, opinions, and content expressed in this magazine do not necessarily reflect the views, opinions, or positions of the Editorial Team, CACHE, the University of Toronto, or the University Health Network. While we aim to provide informative and thought-provoking content, and do review material for relevance, we do not endorse or condone every statement, opinion, or perspective presented in the magazine.

Kim Neudorf BSN, MEd (Patients for Patient Safety Canada, Infection Prevention and Control Canada)
This is a story about safe transitions for a vulnerable population - the frail elderly. This story accompanies a painting. The central themes of the story are accompaniment and a culture of safety. The competencies that made this transition successful were: collaborative leadership, communication, interprofessional collaborative team work towards person-centered care, role identity, risk management, and relationship building on day one of a transition from a hospital to a long-term care facility.
Charlene, my care coordinator, announced that a room was available at the Rosehill care home. Rosehill was my first choice, because it was close to my daughter, and it had lovely rose gardens. Yet, I felt nervous, because I spent the past four months hospitalized. Charlene assured me that she would accompany me every step of the way. A short video, starring me, was prepared for the team at Rosehill. In turn, my daughter and I watched a video that introduced us to Rosehill’s layout, the team, and our responsibilities.
When we arrived at Rosehill, it felt special. At the entrance there were two planters filled with flowering shrubs and trailing ivy. A large blackboard said, “Welcome Lucy and family!” Charlene was there to greet us. She said, “We’re ready. You don’t have to worry about a thing!” As I passed down the hallway, Charlene introduced us to the manager and several residents. My room was spic and span. My clothes were hanging in the closet, and I recognized my furniture and mementos. Charlene assured us that the teams at the two facilities collaborated back and forth to ensure my transition was welcoming, safe, and a priority for the day.
Charlene introduced us to the nurse in charge. The nurse said my medications were in place and that everyone was looking forward to meeting me. She explained the fall alarm on my bed, and the alarm set into the cushion of my wheelchair. She explained how the floor was designed for a soft landing. She told me a volunteer would be at my side all week to help me get to know the place. The cleaner said she would clean my room every day, and fill the dispensers, and that everyone would wash their hands when they gave me personal care, as they were committed to preventing infections. The recreation director said she knew I loved BINGO, and now I can play three times a week. The dietician knew my favourite meal was fried chicken, and she prepared it for my first dinner. They knew everything about me.
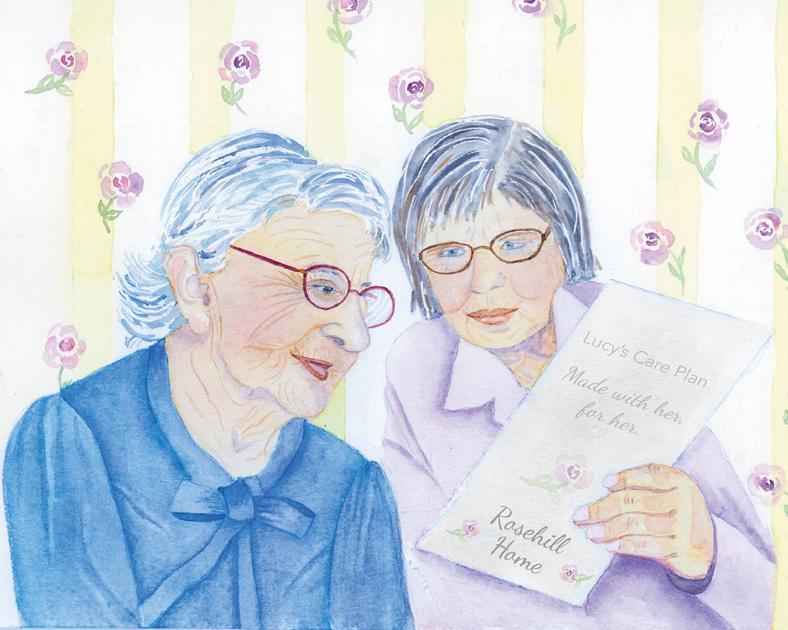
In this painting, I’m reviewing the care plan my team prepared with me. I’m amused because they wrote, “Lucy is 99 years old. She is as fragile as a precious teacup—handle with care.”
Art Piece: Kim: This is a painting of my grandmother (99) and her daughter (my mom).
Volume 1.1 (Fall 2022)

Volume 1.2 (Winter 2023)

Volume 1.3 (Spring 2023)

Volume 1.4 (Summer 2023)
Cover Art for Together’s Vol. 4.2 (Spring 2026)!

Volume 2.1 (Fall 2023)

Volume 2.2 (Spring 2024)
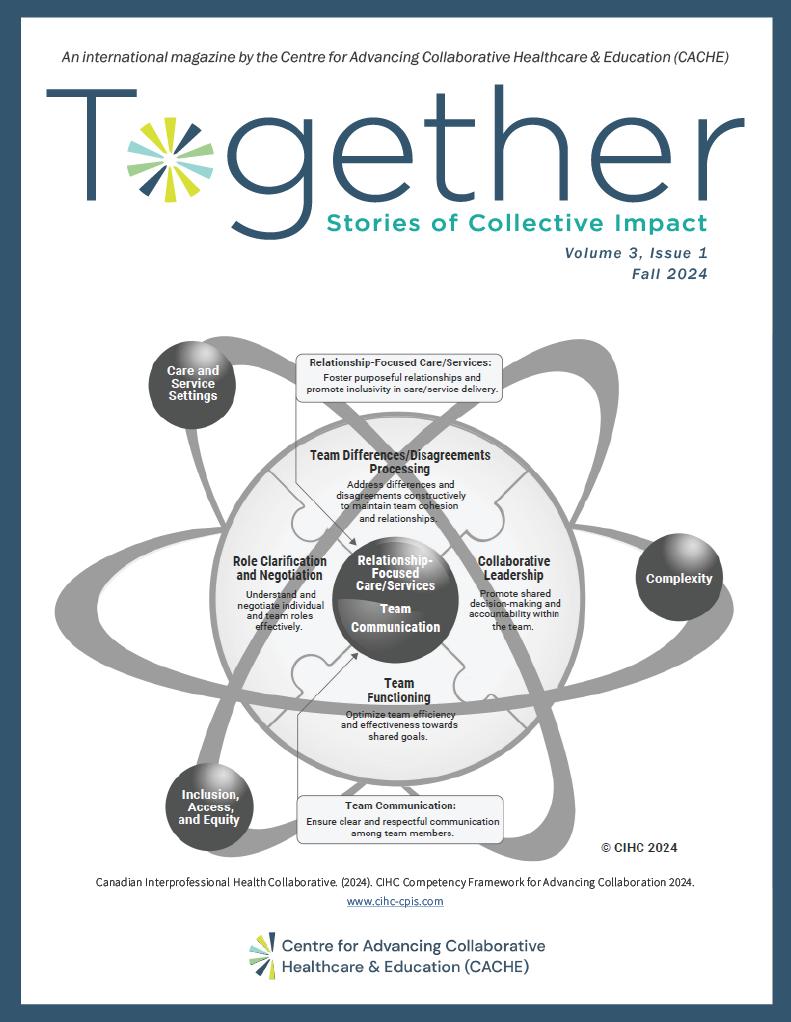
Volume 3.1 (Fall 2024)
Volume 3.2 (Spring 2025)



Welcome Marissa to the CACHE Team
CACHE Editorial Team

Marissa Shaw is the Administrative Assistant at the Centre for Advancing Collaborative Healthcare & Education (CACHE). She brings a strong background in healthcare administration, operations coordination, and scheduling, with a bachelor’s degree in Business Administration from the Universidad Autónoma del Estado de Morelos in Mexico. Over the past six years, she has held administrative roles in long-term care and senior living communities, supporting interdisciplinary teams and contributing to staff training and engagement initiatives.
At CACHE, Marissa supports the Curriculum portfolio, the InterFaculty Curriculum Committee (IFCC), and the Interprofessional Education Leaders (IPEL) Network. She also contributes to the Centre’s overall operations, including team meetings and event planning, ensuring that behind-the-scenes systems run smoothly to advance CACHE’s mission.
Passionate about improving healthcare delivery through thoughtful organization, clear communication, and empathetic support, Marissa is especially interested in how strong administrative foundations can enable more effective health and social care education. Bilingual in English and Spanish, she values connecting with diverse communities and fostering inclusive collaboration.
Outside of work, she enjoys walking, watching movies and series, and relaxing with a good cup of tea.
Join us in welcoming Marissa to CACHE!
CACHE Editorial Team
On July 1, 2025, the University of Toronto (UofT) community marked a monumental milestone: the retirement of Professor Sylvia Langlois, a leader whose vision, dedication, and relational brilliance deeply shaped the field of interprofessional education (IPE) in Canada and around the world.

For nearly three decades, Sylvia’s work advanced collaborative practice, strengthened partnerships across professions and systems, deepened the role of patient, family, and caregiver partners in health professions education, and inspired thousands of learners to see themselves as a team, a system, a community.
Her legacy lives not only in the programs she helped build, but in the people she mentored, the bridges she strengthened, and the values she modeled: authenticity, curiosity, generosity, and unshakeable belief in the power of working together.
In June, the CACHE community gathered for a special Retirement Tea to celebrate Sylvia’s extraordinary contributions. What unfolded was an outpouring of stories of gratitude and respect that reflected the breadth and depth of her impacts as an educator, scholar, colleague, and leader. It was an afternoon filled with laughter, tears, and the kind of collective warmth that only emerges from years of shared purpose.
This article honours both the remarkable career and the remarkable person we have been privileged to learn with, from, and about: Sylvia Langlois, Associate Professor, Emerita, Department of Occupational Science & Occupational Therapy, Temerty Faculty of Medicine, University of Toronto.
Sylvia began her IPE journey 29 years ago, hired as an Academy Associate to support the Faculty of Medicine in responding to accreditation feedback calling for greater emphasis on interprofessional learning, a concept that was hardly recognized at the time. As Sylvia described in her remarks: “We had to kind of figure out what it meant… those early years were very much trench work.”
From those early days, Sylvia became a foundational force in shaping IPE at UofT and beyond. She was instrumental in building structures and systems that endure. Helping evolve IPE from isolated efforts within academies to coordinated, system-wide integrated curricula, supporting the development of the Office of IPE, then the Centre for IPE, and now CACHE chairing the Interfaculty Curriculum Committee (IFCC) for many years, helping align 12 health and social care professions in a shared curriculum.

Elevating Patient, Family, and Caregiver Partnership
Long before patient engagement became a widely recognized pillar of education transformation, Sylvia championed it, embedding patient voices meaningfully in curricular design and learning activities.
Jennifer Boyle, Co-Chair of CACHE’s Patient/ Family/ Caregiver Partner Advisory Committee, captured this beautifully with her S-Y-L-VI-A tribute:
• S for superhero… with an invisible cape.

• V for visionary… and a tireless champion for patient, family, and caregiver partnerships.
• I for impact … on countless people, colleagues, students, and partners.
IPE Across Systems
Through Sylvia’s leadership, UofT became a hub for IPE innovation and collaboration across hospitals, practice environments, national networks such as the Canadian Interprofessional Health Collaborative (CIHC), and international organizations and conferences. Colleagues across the country credit Sylvia with elevating IPE into a recognized, evidenceinformed discipline, work that CIHC founding leader and Chair John Gilbert described as: “Ensuring that the discipline is a more secure, evidence-informed endeavour… Her leadership has been globally significant.”
Scholarship and Global Leadership
At conferences across continents, in peer-reviewed journals, and in collaborative research teams, Sylvia helped shape the global conversation on interprofessional identity, collaborative practice, and systems transformation. As one colleague summarized: “There are some people who are bridges and Sylvia is one of the very special ones.”
A Celebration Filled With Gratitude, Stories, and Love: Highlights from the Retirement Tea On the day of the Retirement Tea, the atmosphere
was filled with warmth, laughter, and affection, an unmistakable reflection of Sylvia’s influence.
CACHE Director Stella Ng opened with joy, “We are so excited to celebrate you… You are a remarkable human being.” She welcomed four generations of Sylvia’s family, acknowledging the personal sacrifices behind a lifetime of leadership. From the IFCC, Keith Adamson and Sharona Kanofsky spoke about witnessing Sylvia navigate the complexity of multifaculty curriculum work with grace, “IPE and IPC are somewhat synonymous with Sylvia Langlois.” Keith noted.
Sharona added, “You create harmony… 90% ‘Mrs. Nice Guy’ and 10% ‘time to make a decision;’ the ideal balance.”
Joining live from British Columbia, John Gilbert offered poetic reflections, quoting T. S. Eliot and Geoffrey Chaucer, recognizing Sylvia’s scholarly contributions and her commitment to learners, “I have been privileged to learn with, from, and about the innumerable aspects she brings as an occupational scientist and occupational therapist.” He left her with an Irish blessing and this gentle warning:“I flunked retirement—the hardest word to learn begins with N and ends with O.”
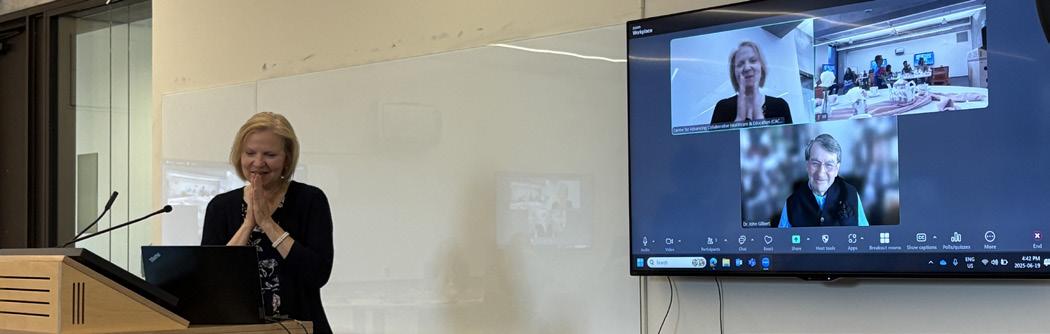
From the Interprofessional Education Leaders (IPEL) Network, Darlene Hubley and Elizabeth McLaney highlighted Sylvia’s ability to bring academic and practice environments into meaningful dialogue. Their personal stories, from tea-related first aid to navigating conference cities by foot, brought the Photo: CAB VI 2017 in Banff — Sylvia and CACHE team members.

room to laughter and tears. At one point, colleagues recalled a planning retreat conducted by flashlight during a power outage, and an office flood where umbrellas doubled as evacuation tools, memories that paint a picture of resilience, camaraderie, and Sylvia’s steady presence through it all.
Sylvia’s son Zach offered a moving tribute to the qualities they see mirrored across her personal and professional life,“She has a standard of excellence that follows her everywhere… And the passion she brings to her work is the same passion she brings as a mom.” Her husband Terrance shared stories of her ongoing commitment to teaching and service, including helping a newcomer learn English weekly for years, “People who love to teach also love to learn, and Sylvia is a lifelong learner.”

In her own words, Sylvia described the celebration as “a eulogy you get to hear yourself,” and thanked colleagues, partners, students, and family with characteristic humility and humour. She shared a new metaphor for retirement, inspired by noticing discarded tire treads on the highway, “Retiring is really retreading, traveling new roads, finding new adventures… soaring, perhaps, with more energy and fewer balls to juggle.”
In a surprise announcement, the CACHE team unveiled the new Sylvia Langlois Patient, Family, and Caregiver Partner Impact Award, honouring patient partners who enrich student learning - an enduring reflection of Sylvia’s life’s work and values.
As the celebration came to a close, it was clear that Sylvia’s contributions will continue to shape CACHE, UofT’s IPE Curriculum, and the wider health and social care community for many years to come.
Her career reminds us what becomes possible when collaboration is built on relationships, when education is grounded in human experience, and when leadership is expressed through humility, curiosity, and courage.
The CACHE Editorial Team is honoured to celebrate Professor Sylvia Langlois, a visionary leader, a beloved colleague, and a lifelong champion of collaborative care and education. As Sylvia steps into this season of “retreading,” we know she will continue to inspire, not with titles or roles, but with the same generosity, curiosity, and dedication that defined her career.
Enjoy some photos from Sylvia’s Retirement Tea.














Every issue of Together captures real stories of collaboration, learning, and change in health and social care. Whether you’re looking for inspiration, practical ideas, or a sense of connection & community, our past volumes are full of insights from across the system.
New to Together? Start with Volume 1.1 (Fall 2022) to see how it all began.
Looking for fresh perspectives? Browse through stories of growth and innovation in our most recent volumes. Click below to dive in:
• Together: Stories of Collective Impact, Volume 1.1 (Fall 2022)
• Volume 1.2 (Winter 2023)
• Volume 1.3 (Spring 2023)
• Volume 1.4 (Summer 2023)
• Volume 2.1 (Fall 2023)
• Volume 2.2 (Spring 2024)
• Volume 3.1 (Fall 2024)
• Volume 3.2 (Spring 2025)
Loved what you read? Please share with your colleagues and networks!
Each year, patient partners join us in governance, curriculum design, facilitation, teaching, and research, shaping the interprofessional education of more than 4,000 learners. Their lived experience brings depth and humanity to learning, and students consistently describe these interactions as some of the most transformative moments in their training.
We are committed to building meaningful partnerships through remuneration, shared leadership, and collaborative processes grounded in trust and respect.
Every donation directly supports patient partner remuneration. Your gift helps ensure that patients, clients, families, and caregivers can participate fully in the work of preparing tomorrow’s healthcare workforce.
Your contribution is more than support, it’s a statement. It affirms that experiential knowledge matters. It helps grow a more inclusive partner community. And it strengthens a system where learning with, from, and about patient partners is core to high-quality care.
Thank you for investing in this collective future. https://ipe.utoronto.ca/giving


Ruby Rajendra Shanker M.B.B.S., M.H.Sc. (Bioethics) (University Health Network’s Department of Clinical & Organizational Ethics, University of Toronto)
At Toronto Rehab, the UHN Department of Clinical & Organizational Ethics offers several novel ethics education opportunities, including Bioethics Rounds on Wards—affectionately known as BROWnies. This adapted model invites interprofessional teams within a unit or program to pause clinical tasks for one hour of reflective dialogue. Participants gather to share ethics cases that linger—those on our minds or those that haunt us. Developed and facilitated by the clinical & organizational ethicist, Ruby Shanker, BROWnies are intentionally designed to be both safe and brave spaces: safe enough to respectfully enquire into difference, and brave enough to share vulnerability and acknowledge collective solidarity. There are no slides, no fixed themes. Instead, conversations are lightly guided to nurture the team’s ability to distinguish and navigate moral, ethical, and legal dimensions of practice.
BROWnies foster all six domains of the CIHC interprofessional collaboration framework, with particular emphasis on reflexivity in communication and role negotiation. Participants are gently nudged to consider ethical obligations
and how these shape—and are shaped by—our evolving professional identities. As seasoned clinicians offer novel responses to familiar ethical tensions, all remain engaged in refining clinical judgment. Grounded in principles of communicative democracy—narrative, relationality, and community building—BROWnies welcome all forms of participation. Whether speaking, listening, or simply being present, each contribution is valued. Conversations unfold through commensality: brownies and seasonal fruit always await a shared table where hierarchy softens and honesty flows more freely.
In a healthcare landscape marked by complexity and constraint, BROWnies offer a rare space for moral repair. They remind us that ethics education is not only about dilemmas and specific decisions, but about who we are becoming—together.
References:
• Arawi, T. (2016). BROWnies: bioethics rounds on the wards. Medical Education, 50(11), 1147-1148. https:// doi.org/10.1111/medu.13194
• Canadian Interprofessional Health Collaborative. (2024). CIHC Competency Framework for Advancing Collaboration 2024. www.cihc-cpis.com
• Young, I. M. (2002). Inclusion and democracy. OUP Oxford.
• Okamoto-Garson, K. H. (2024). In Good Company: Commensality’s Influence on Workplace Well-Being and Productivity (Master’s thesis, California State University, Fresno).
Amanda Beales MAN RD CDE, (University Health Network); Raisa Kassam MScPT (University Health Network); Stella Paterakis RD, CDE (University Health Network); Linda Pugliese PT (University Health Network).
Tackling malnutrition effectively requires a united, interprofessional approach where every team member plays a critical role. At UHN, the interprofessional Malnutrition Taskforce exemplifies this collaboration by bringing together dietitians, physiotherapists, occupational therapists, respiratory therapists, nurses, social workers, and other healthcare professionals to raise awareness and promote coordinated strategies for malnutrition prevention and management.
Earlier this year, the task force launched an interactive session for all newly hired health professions staff as part of UHN’s Corporate Clinical Orientation. This session highlighted the importance of cross-disciplinary teamwork in addressing malnutrition and empowered staff to recognize their unique contributions to improving patient nutrition outcomes. The initiative has since fostered meaningful engagement and strengthened a shared understanding of nutritional care across professions.
Building on this foundation, the task force spearheaded a series of engaging activities during Canadian Malnutrition Awareness Week (October 6–10, 2025) to further promote reflection on interprofessional roles in malnutrition care. Activities included webinar watch parties, a traveling education cart visiting clinical areas, and a contest inviting clinicians from multiple professions to share their personal approaches to malnutrition care. This contest generated a valuable collection of real-world examples to inform future education efforts.
Additionally, over 400 personalized buttons reading “Malnutrition matters to [their name]” were created and worn proudly by team members as a visible commitment to addressing malnutrition. These buttons serve as a lasting reminder that every discipline has a role in improving nutritional care.
Through these collaborative and innovative efforts, the UHN Malnutrition Taskforce is cultivating a culture of accountability and shared expertise. By harnessing the strengths of diverse healthcare professionals, the taskforce is driving measurable improvements in patient outcomes— elevating nutrition as a vital component of holistic care.

Eileen Hoftyzer (University of Toronto)
Open up any social media app and you might come across posts that raise doubts about medications or promote questionable health advice. For many people, this can create confusion and fear when making decisions about their health. The Canadian Medical Association has found that health misinformation has led to more Canadians delaying or avoiding care they need, and feeling uncertain about who to trust. That’s why it’s so important for health professionals to meet people where they are and support informed decision-making in a respectful and inclusive way.
Pharmacists, nurses, and other healthcare professionals inevitably encounter patients who have inaccurate or misinformed beliefs about their health, and they may have to navigate challenging conversations while maintaining trust with these patients. This can be especially common for pharmacists and nurses, who are often the most accessible healthcare providers and have many opportunities for these conversations.
“Sometimes as healthcare providers, we can get a bit on our toes when a patient makes a decision based on misinformation, but these patients are more than just the one decision they make that you don’t agree with,” says Jennifer Lake, assistant professor, teaching stream at the Leslie Dan Faculty of Pharmacy. “Learning to have these difficult conversations while maintaining a good relationship is really important, so that you can keep their trust. Maybe you’ll change their mind, maybe not, but they still deserve your best care.”
Lake recently teamed up with Summer Haddad, assistant professor, teaching stream at the Lawrence Bloomberg Faculty of Nursing, along with Stella Ng, Director & Scientist, CACHE , plus Donald Bettencourt and Ellena Andoniou from The Institute for Education Research (TIER) at University Health Network. Together, they developed a two-part elective course through
the U of T’s Interprofessional Education (IPE) Curriculum to teach students from the U of T’s 12 health profession faculties approaches to addressing mis- and disinformation. The elective, Meeting People Where They’re At: RelationshipCentered and Evidence-Informed Approaches to Addressing Mis/Disinformation, was held for the first time in late spring 2025, with 12 students enrolled, and the next offering in November 2025 with up to 30 students.
Lake and Haddad had heard from students in their respective faculties that they were encountering misinformation more often in their communities. While health profession faculties may include the topic in their own curriculum, Lake and Haddad also wanted to address it in an interprofessional setting.
“Patients will see many different health professionals, and it’s helpful for all of the professions to use the same approach and consistent communication,” says Haddad. “When health providers collaborate, it strengthens our approach and improves the care we provide to our patients.”
Some health professionals and researchers on social media take a ‘mythbusting’ approach to countering misinformation, providing evidence and explaining why the misinformation is wrong, but Lake says this isn’t necessarily the best approach when speaking one-on-one with a vulnerable patient. When designing the elective, she and Haddad wanted to focus on how to engage in difficult conversations while maintaining a trusting relationship with the patient.
The course shared evidence-informed approaches to responding to mis- or disinformation with patients, colleagues, and community members. The learners then worked in teams to devise approaches for responding to misinformation through realistic case studies. “It’s important to provide students with realistic opportunities that
allow them to simulate a difficult conversation in a safe space,” says Lake. “They need the opportunities to practise this skill before they encounter it for the first time with a vulnerable patient.”
Interprofessional Groups Allowed Students to Learn from Each Other Chloé Lavoie (2T6) recalls that her first experience working in pharmacy was several years ago, during the rollout of COVID-19 vaccines, and she didn’t know how to respond to health misinformation that her patients were sharing. So when she saw the course advertised, she enrolled to learn strategies and approaches that would help her in similar situations in her future pharmacy practice.
During the course, Lavoie worked in a small group with students from medicine, social work, and radiation technology. For their case study, they presented a puppet show that allowed them to creatively role-play different approaches each profession could take in addressing vaccine misinformation with a patient.
“Everyone had a different level of expertise on a topic, and so having an interprofessional group, we could learn from each other and contribute in the area where we were knowledgeable,” she says.
“Working on the case study together was a good opportunity for everyone to learn a little bit more about each profession and how we can all work together to educate our patients.”
Lavoie found the course to be a valuable experience, and she says she learned approaches to communicate with empathy and understanding, provide patients with the amount of information that they are ready to hear, and make patients feel heard. For Lake and Haddad, learning to meet patients where they are is a critical part of providing high-quality care.
“If a patient feels unheard by healthcare professionals, they are going to turn elsewhere for health information,” says Haddad. “Trust, communication, and open dialogue are critical to addressing misinformation and disinformation so we can provide the best possible care.”
Reprinted with permission from Eileen Hoftyzer, copyright 2025 by University of Toronto’s Leslie Dan Faculty of Pharmacy. This article was originally published in the August 19, 2025 News & Announcements section of the University of Toronto’s Leslie Dan Faculty of Pharmacy website. Find the original work online at https://www. pharmacy.utoronto.ca/news-announcements/ interprofessional-elective-teaches-skills-counterhealth-misinformation

Elizabeth Cadavid on behalf of the IPE Dying & Death Working Group (Centre for Advancing Collaborative Healthcare & Education)
How do we prepare future health professionals to approach dying, death, and loss with compassion, confidence, and humanity?
At the University of Toronto, the Dying & Death interprofessional education (IPE) elective invites students to engage with one of healthcare’s most profound realities, not only through academic learning, but through reflection, dialogue, and presence.
This elective explores the psychological, physical, and spiritual challenges that arise at the end of life. Students from across the health sciences come together to deepen their understanding of how diversity in faith, culture, and personal and professional values shape experiences of dying. Through case discussions and guided reflection, they learn how to communicate sensitively, support patients and families, and collaborate effectively as interprofessional teams.
Behind the elective is a dedicated working group representing multiple disciplines and perspectives: Vinita Arora (Pharmacy Faculty); Jeffrey Brown (Multi-Faith Centre for Spiritual Study and Practice); Elizabeth (Eli) Cadavid (CACHE Education Coordinator); Bhavini Patel (Family/Caregiver Partner); Aisha Sheikh (Medical Radiation Sciences Faculty); Brian Walsh (Spiritual Care); and Kimberley Widger (Co-Chair, Nursing Faculty).
For over a decade, the group was deeply shaped by the contributions of Dr. Maxxine Rattner, Assistant Professor in the School of Social Work at York University, who joined the group in 2014. Maxxine’s teaching on the emotional and psychological issues of dying and death left an enduring mark on both students and colleagues. She illuminated the spectrum of losses (physical, cognitive, and relational) that individuals and families face, and spoke openly
about the worries, fears, and death anxiety that often accompany the dying process. Her sessions encouraged future healthcare professionals to not only understand these experiences intellectually, but to reflect on their own values, reactions, and sources of resilience. “Self-reflection,” Maxxine often reminded students, “is essential if we hope to accompany others through dying and loss.”
As Maxxine moves on from the working group, CACHE and the Dying & Death team express their deep gratitude for her years of leadership, compassion, and expertise. Her legacy continues to ripple through the elective and the many students she has inspired.
With this transition comes a new opportunity to amplify lived experience within the elective. The working group is pleased to officially welcome Bhavini Patel , a Family and Caregiver Partner who brings her personal journey as a caregiver for her father into her educational and advisory work. Bhavini has been part of the working group since 2023 and will now step into a presenter role, offering students the chance to learn directly from a caregiver’s perspective. Her contributions complement the interprofessional and spiritual dimensions of the elective, creating a richer and more holistic learning experience.
“This elective is about being human together, as patients, families, and health and social care providers,” says Eli Cadavid, Education Coordinator at CACHE. “Bhavini’s voice helps bridge those worlds beautifully, reminding students that compassion and collaboration go hand in hand.”
The Dying & Death elective continues to embody what interprofessional education can achieve at its best: a space for honest conversations, shared learning, and growth, where students practice not just what to do, but how to be with those who are dying and those who grieve.
As the team looks ahead, they carry both gratitude for Maxxine’s lasting influence and excitement for the perspectives Bhavini brings, a reflection of the ongoing evolution of this meaningful elective, and of CACHE’s commitment to advancing compassionate, collaborative healthcare education.
Bhavini Patel EMBA, CCP, PMP (Governance & Advisory Committee Member, Facilitator, Health Mentor, Centre for Advancing Collaborative Healthcare & Education)
This fall, approximately 1400 first-year students from 12 health and social care programs embarked on their academic journey at the University of Toronto (UofT). Through engaging in interprofessional education (IPE) activities, they discovered the power of collaboration in transforming patient care.
By listening to patient experiences, taking time to self-reflect, and contributing to small group discussions, these amazing students dug into how valuable teamwork is to delivering patient care. Various views from diverse health and social care learners generated thoughtful conversations, activated listening skills, and deepened empathy. They worked together effectively in the introductory activity and identified key traits of successful teams such as: leveraging strengths, communicating, team huddles, using tools and checklists, maintaining a suitable tone of voice, and providing constructive feedback.
As a facilitator in the UofT IPE Curriculum, I combine my caregiver/patient partner perspective with my leadership experience to encourage learners to share their thoughts about how collaboration impacts patient experiences. Ultimately, identifying that including patients/ caregivers in the care plan results in an elevated experience for everyone.
The goal of “enhancing healthcare and human services through collaborative, relationshipfocused partnerships to shared decision-making around health and social matters” is embedded in the 2024 Competency Framework for Advancing Collaboration. Launched by the Canadian Interprofessional Health Collaborative (CIHC), this model identifies 6 domains that form the foundation of collaborative care. At the Centre for Advancing Collaborative Healthcare & Education ( CACHE ) this framework informs the IPE activities for our future healthcare professionals. As they continue their journey, the collaborative mindset they are developing will positively influence how care is delivered.

Canadian Interprofessional Health Collaborative. (2024). CIHC Competency Framework for Advancing Collaboration 2024. www.cihc-cpis.com
Daniela D’Annunzio RN, MN (Sr Manager, Nursing and Interprofessional Education); Mandy Kohli MRT (N), BSc (Interprofessional Education Specialist, Department of Diagnostic and Interventional Radiology); Alicia Hayes RN, MPH (Interprofessional Education Specialist, Surgical and Endoscopy Community Partnerships Program); Erin Lawson OT Reg. (Ont.), MPH (Interprofessional Education Specialist, Rehabilitation Services); Jamie Waltman CCLS, MSc (Interprofessional Education Specialist, Emotional Safety); Bonnie Fleming-Carroll RN(EC), MN, FCAN (Associate Chief of Nursing, Nursing and Interprofessional Education); Jingjing Chen MEd, PMP (Program Coordinator, Nursing and Professional Education).
Welcoming newly hired interprofessional staff into SickKids is about more than sharing information–it’s about creating connection, purpose, and belonging.
The Interprofessional Orientation Program (IPO) is a new initiative designed to ground staff in the principles that guide our practice and culture. Developed by the Interprofessional Education Council, the IPO provides foundational education that strengthens collaboration through relationshipcentered partnerships and shared decision-making. Through case studies, patient journey mapping, video debriefs, and interactive discussions, participants explore how teamwork directly impacts patients and families.
This first-of-its-kind program at SickKids, reflects our commitment to supporting allied health professionals as they find their place, build relationships, and thrive as vital contributors to pediatric care. The IPO focuses on:
• Inclusive, respectful communication and professionalism across disciplines
• Trauma-informed, compassionate care as the foundation of trust and safety
• Child and Family-Centered Care, emphasizing respect, partnership, and excellence
• Resources and strategies that promote interprofessional practice and a strong safety culture
Guided by the Canadian Interprofessional Health Collaborative (CIHC) 2024 Competency Framework for Advancing Collaboration , allied health new hires will learn with, from, and about each other. By recognizing each profession’s unique contributions, participants will foster mutual respect, break down silos, and strengthen teamwork that leads to better outcomes.
The pilot session, held September 22, 2025, was described as “informative, engaging, and a clear framework for understanding professional roles” across SickKids. Participants highlighted that the session:
• Fostered collaboration across disciplines
• Clarified care processes
• Demonstrated how diverse professionals work together to deliver high-quality care
Participants also valued meeting colleagues, learning about available services, and building relationships that strengthen our collective ability to provide exceptional care.
The Interprofessional Orientation Program officially launches in early 2026 and is a significant step forward in advancing our culture of collaboration and excellence in pediatric care.

The Interprofessional Education Council is a broad representational group of health care professionals who have educational responsibilities within their role. The Council members provide leadership in promoting a sustainable culture and environment for collaborative practice to promote learning for staff and students across all levels of SickKids to positively influence interprofessional thinking, behaviour, and practice.
Darlene Hubley OT Reg. (Ont.), BScOT, MScCH, IPE Leader (Holland Bloorview Kids Rehabilitation Hospital)
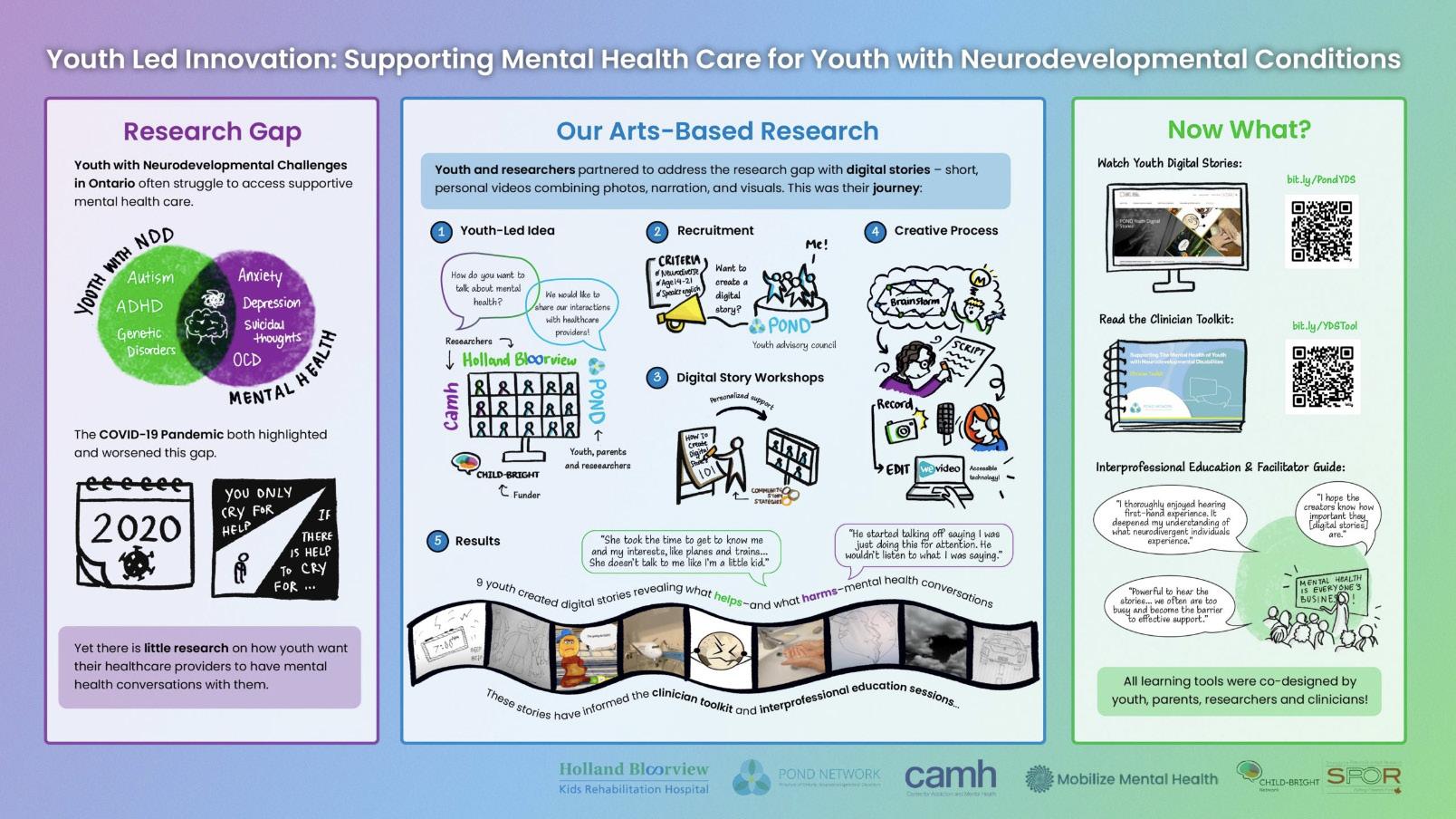
Ateam of researchers, clinicians, education leaders and people with lived experience have co-created an IPE elective learning activity called, “Mental Health is Everyone’s Business!” The IPE elective, now formally part of the IPE Curriculum at the University of Toronto, is an interactive, two-hour, virtual, small group, collaborative learning session. Digital stories authored by youth with neurodevelopmental conditions and mental health needs bring learners closer to the youths’ experiences, are the catalyst for dialogue, and invite learners to deepen their compassion and collaboration in future practice. The team recently presented the IPE session at the AMEE Conference 2025, in Barcelona, Spain. We invite you to explore the digital stories , the clinician toolkit and the IPE facilitator’s guide and offer the IPE session in your context.
The co-creation of the IPE session followed the realization that youth with neurodevelopmental conditions experience high rates of mental health challenges, yet healthcare providers express limited knowledge, lack of experience, and low confidence in delivering care to them. To address this gap in education, youth with neurodevelopmental conditions were supported to author digital stories to share their experiences seeking mental health care. Research and education leaders then invited story authors, their family members, others with lived experience, and community partners to co-design an IPE session. The session design process identified shared hopes for practice change and established
learning objectives for the session, whereby learners will: (i) listen to the expressed needs of neurodivergent youth; (ii) acquire strategies that enhance collaboration and shared decisionmaking; (iii) describe their healthcare provider role; and (iv) identify how interprofessional care can improve wellbeing for neurodivergent youth. The session outline ensures a supportive learning environment, opportunity to view and discuss stories, engage with a panel, share resources, and reflect on learning. A comprehensive facilitator’s guide enables other educators to offer the session in their environments.
To date, Holland Bloorview Kids Rehabilitation Hospital has offered the IPE session four times to over 65 learners from 11 different healthcare provider programs. Program evaluation data highlights that learners appreciate (i) connecting with people with lived experience; (ii) deepening their understanding of the human experience through digital stories, and (iii) exploring collaborative approaches together. As one learner articulated in their evaluation of the session, “I enjoyed hearing from the family perspective to listen to how their lives are impacted by the healthcare system. Their engagement was a good reminder toward collaborative practice by remembering that the parents of a child are a part of the healthcare team as well.”
Laura Banks PhD, MA, R.Kin. (Faculty of Health Sciences, Ontario Tech University & KITE/Toronto Rehabilitation Institute, University Health Network); Adam Dubrowski PhD (Faculty of Health Sciences, Ontario Tech University); Janet McCabe PhD, MEd, RN (Faculty of Health Sciences, Ontario Tech University).
On April 24, 2025, Ontario Tech University’s Faculty of Health Sciences launched the Faculty’s first Interdisciplinary Case Competition – bringing together twelve third and fourth year students from Human Health Sciences, Public Health, Kinesiology, and Nursing to present solutions to a complex case. Students were assigned to four different groups with program representation mixed across all groups. The case, developed in conjunction with leading Faculty experts, presented the story of a complex older adult with a history of chronic illness, integrating social considerations such as cultural and generational needs and differences, transition to long term care, and dementia.

Case-based learning broadly encompasses scientific inquiry, integration of knowledge and practice, clinical reasoning, and critical reflection. At competitive case competitions, teams collaborate and develop a solution to a real-world case study. Case competitions can effectively provide an active learning experience, reinforce fundamental concepts, enable students to connect course concepts to the real world, require critical thinking and analytic skills, and promote a team-based learning approach ( Umble et al., 2008 ). These elements closely align to the
CIHC (2024) Competencies – with a specific focus on Team Communication and Team Functioning rooted in relationship focused care/services.
Teams were asked to design a digital health intervention that addressed challenges faced by the patient, family, and care team. In the two hours that followed, the three teams developed a seven-minute overview of their specific case study solution, which was presented to the judging panel and the in-person audience.

The judging panel had interdisciplinary expertise in health sciences, nursing, and medical laboratory science. Students, mentors, and judges were all very satisfied with the competition and their experiences. Students were at first apprehensive about their readiness for interprofessional collaboration and case presentations, yet they recognized the significant value in this opportunity.
References:
• Canadian Interprofessional Health Collaborative. (2024). CIHC Competency Framework for Advancing Collaboration 2024. www.cihc-cpis.com
• Umble, E. J., Umble, M., & Artz, K. (2008). Enhancing undergraduates’ capabilities through team-based competitions: The Edward Jones Challenge. Decision Sciences Journal of Innovative Education, 6(1), 1–27. https://doi.org/10.1111/j.1540-4609.2007.00164.x
Dr. Joseph P Buhain EdD, MBA, RRT, CMSP, CHSOS, CMSP, FAARC, NREMTB (Director of Interprofessional Simulation and Emerging Technology, Marieb College of Health & Human Services, Florida Gulf Coast University)
Florida Gulf Coast University’s 2024 Disaster Day Interprofessional Simulation engaged over 600 students from Nursing, Social Work, Public Health, Occupational Therapy, Physical Therapy, Physician Assistant, and Performing Arts programs in a large-scale mass-casualty simulation designed to build teamwork, communication, and crisis readiness.
Participants collaborated with first responders, hospitals, and community agencies to manage complex emergency scenarios involving triage, trauma care, mental health counseling, and rehabilitation.
Working alongside first responders, hospital partners, and community agencies, students navigated diverse scenarios such as triage, trauma response, mental health counseling, and rehabilitation. The simulation integrated both the Canadian Interprofessional Health Collaborative (CIHC) competencies and the Interprofessional Education Collaborative (IPEC) Core Competencies to create a comprehensive interprofessional framework. Disaster Day simulation acts as a practical, immersive enactment of these competencies: students from different professions must communicate (Competency 3), understand their roles and others’ (Competency 2), function as a team under pressure (Competency 4), and respect ethical/patient-centered values (Competency 1).
The rationale: Using IPE core competencies within a high-fidelity simulation setting allows students to move beyond theory into “learning about, from and with each other” (definition of IPE from WHO, which the college references) and to experience the interprofessional collaboration required in real crises.
These frameworks guided the event by emphasizing:
• Interprofessional Communication: Real-time decision-making, patient handovers, and clear, respectful dialogue across disciplines.
• Roles and Responsibilities: Clarifying each profession’s scope of practice and contributions within the care team.
• Teams and Teamwork: Building cohesion, mutual trust, and adaptability under pressure.
• Values and Ethics for Interprofessional Practice: Promoting respect, equity, and patient-centered collaboration.
The use of both CIHC and IPEC competencies provided a rationale for global alignment—the CIHC model underscored collaborative leadership and systems-based care, while IPEC’s U.S.-based standards ensured consistency with national interprofessional education benchmarks. Together, they offered a comprehensive, evidenceinformed framework for evaluating and enhancing teamwork performance.
Inclusive, patient-centered scenarios featured diverse populations and individuals with disabilities, while hybrid technologies—including high-fidelity mannequins, telehealth tools, and virtual simulations—enhanced realism and accessibility for all learners.
Post-event evaluations showed marked gains in participants’ confidence, communication, and understanding of professional roles. Overall, FGCU’s Disaster Day remains a national model for experiential interprofessional education, effectively preparing future healthcare professionals to respond with skill and compassion during real-world emergencies.
If interested, please read the complete report by Dr. Buhain, available through the link here: https:// maipdf.com/file/d691e68ba062ca@pdf
Alan Bennett B.A. (Assistant Director of Communications, University of New England)
F rom rising sea levels that threaten coastal livelihoods to aging populations and fragile global supply chains, the world faces mounting challenges to both environmental and human health.
To help address these challenges, the University of New England in Maine, U.S.A., has announced the formation of a new School of Public and Planetary Health . The school will bring together expertise from across the University in interdisciplinary collaboration, highlighting several of UNE’s core strengths in silo-breaking academic leadership.
“We are creating a powerful platform for research and innovation at the intersection of environmental and human health,” said Gwendolyn Mahon, M.Sc., Ph.D., UNE provost and senior vice president of Academic Affairs. “The formation of the School of Public and Planetary Health represents UNE’s growth and leadership across diverse disciplines and highlights UNE’s commitment to preparing workforce-ready students who are equipped to lead change in their communities.”
The new School of Public and Planetary Health will educate students to explore human health challenges holistically and to be collaborative, systems-level thinkers, with faculty drawn from a broad network of experts in public health, medicine, the allied health professions, marine and environmental sciences, political science, and supply chain management.
The school will also establish two new academic centers, the Center for Public Health Practice and the Center for Healthy Aging. UNE’s Michele Polacsek, M.H.S., Ph.D., a nationally recognized public health nutrition expert and leading voice in strategies to improve the health and wellbeing of underserved communities, will serve as the school’s founding director. In this role, Polacsek will work closely with faculty and administrators from UNE’s Westbrook College of Health Professions, under the leadership of John Vitale, PA(ASCP), M.H.S., Ph.D., dean and associate provost for Interprofessional Education.
Additional collaborators include the College of Professional Studies, UNE’s Center for North Atlantic Studies, College of Business, and leaders from the UNE College of Osteopathic Medicine — Maine’s only medical school and one of the country’s top schools for student residency placements using a holistic, interprofessional approach to medical education — on UNE’s Portland Campus for the Health Sciences, the only fully integrated, interprofessional health education campus in New England.
Siti
Rokhmah Projosasmito MD, M.Ed.(L,P&C), FFRI (Department of Medical Education and Bioethics, FMHPN, Universitas Gadjah Mada) ; Noviarina Kurniawati M.Sc (Department of Medical Education and Bioethics, FMHPN, Universitas Gadjah Mada).
Adolescence marks a pivotal chapter in human development—where bodies change, identities form, and reproductive organs mature, often bringing both physical and psychological challenges. Yet, despite its significance, conversations around reproductive health remain scarce among Indonesian teenagers. According to national data, discussions about puberty, menstruation, and personal hygiene are still limited, especially within peer groups and classrooms.

To address this gap, a collaborative project was launched at Pondok Pesantren Abi Ummi, an Islamic boarding school in Central Java. With 530 female students and 120 female teachers and house parents (musyrifah), the school had already introduced reproductive health education grounded in Islamic law. The project aimed to complement this with medical science, creating a holistic and culturally sensitive approach.
The project brought together experts from three academic departments—medical education and bioethics, obstetrics and gynecology, and biostatistics, population health, and epidemiology. Eight students, both undergraduate and postgraduate, with backgrounds in medicine and midwifery, joined the initiative, bringing fresh energy and diverse perspectives.
The program unfolded in two phases. First, female teachers and house parents received training to strengthen their foundational knowledge. While many already understood the basics of teenage reproductive health, they expressed uncertainty in advising students confidently. This insight shaped the second phase: a student-centered training designed to address common myths and misconceptions, particularly around menstruation and personal hygiene.
During these sessions, the students—referred to as santri—were encouraged to ask questions and engage in open dialogue. Medical and midwifery students acted as peer educators, facilitating discussions and gently challenging misinformation. One of the most powerful outcomes was the realization that health beliefs are deeply intertwined with personal values and religious teachings. The presence of students from various religious backgrounds added richness to the conversation, fostering mutual respect and reflection on how diverse beliefs shape health literacy and service delivery.
This initiative not only empowered young women with knowledge but also created a safe space for dialogue—where science and faith could coexist, and where future health professionals learned the importance of cultural sensitivity in education and care.
Short documentation of the project: https://www.instagram.com/reel/ DPyECOuj40p/?igsh=aDNxcGF3ZWRoenJi

Collaboration (IPC) Showcase (2025): Elevating Care Through Purposeful
Sabrina Bartlett M.Ed., B.Ed (Manager, Curriculum & Education Innovation, Centre for Advancing Collaborative Healthcare & Education); Robyn Davies BHScPT, MAppSc, FCAMPT (Collaborative Learning Specialist, Unity Health Toronto); Elizabeth McLaney MEd , BA, BSc (OT), OT Reg. (Ont.) (Senior Director, Clinical Education; Senior Advisor, Centre for Advancing Collaborative Healthcare & Education).
The Interprofessional Collaboration (IPC)
Showcase celebrates excellence in teambased learning, collaborative care and leadership, interprofessional research, and quality improvement across our healthcare system. It was offered jointly on June 4th by Sunnybrook Health Sciences Centre, the Centre for Advancing Collaborative Healthcare & Education, and at the St. Michael’s site of Unity Health Toronto.

This year’s event leveraged a variety of methods to explore the Canadian Interprofessional Health Collaborative’s competency of ‘relationshipcentred care/services.’ The hybrid format attracted over 184 participants who experienced an excellent keynote address by Dr. Kateryna Metersky, Patient Partner, CACHE and Assistant
Professor of Nursing, Daphne Cockwell School of Nursing, Toronto Metropolitan University, entitled Relationships that Heal: Building Stronger Teams and Better Outcomes.
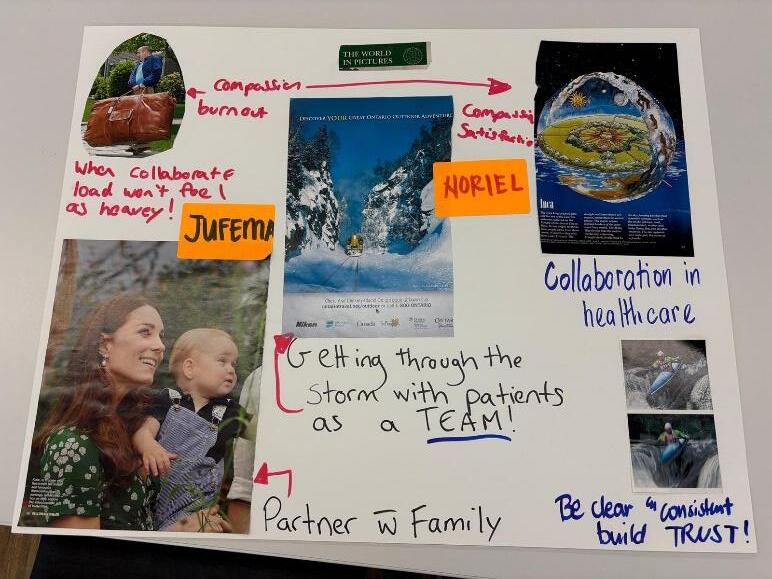
The afternoon included: organizational stories illustrating collaborations between healthcare practice settings and patients/families, a panel discussion highlighting moments of excellence with patients partners in education initiatives, and a collaborative collage-making reflective group activity - all exploring the impact of relationships in healthcare and healthcare education.
Dr. Metersky ended the formal part of the Showcase with a reflective poetry reading . Inperson participants enjoyed a time for networking and some excellent nibbles to round off the event, while online participants used breakout rooms to connect with other attendees. The IPC Showcase stands as a beacon of what’s possible when we invest in people and the relationships that connect them. With the success of this year’s event, the co-chairs are already looking ahead to 2026 - stay tuned and stay inspired!
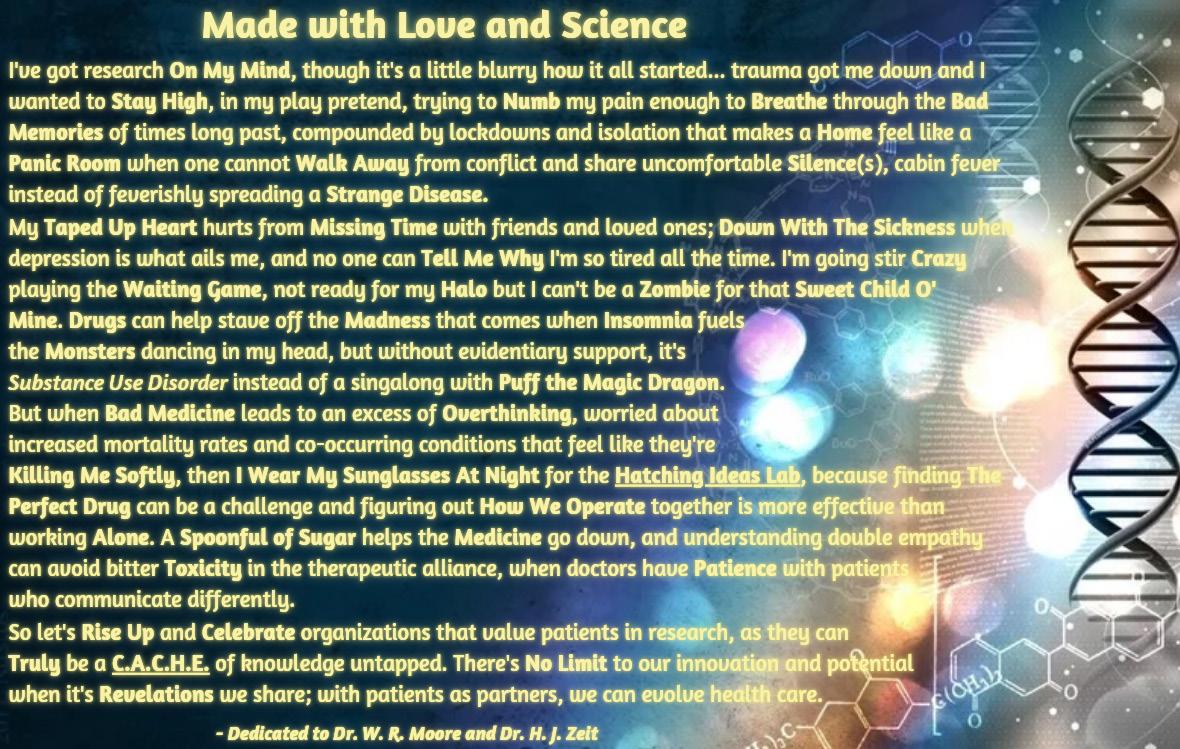
Tracy White, Patient Partner (Centre for Advancing Collaborative Health Education)
First shared as a visual art piece at the 2024 PiPER Conference, this work weaves together themes of patient engagement and lived experience in research. To support accessibility, the text from the original image is reproduced below.
I’ve got research On My Mind , though it’s a little blurry how it all started… trauma got me down and I wanted to Stay High , in my play pretend, trying to Numb my pain enough to Breathe through the Bad Memories of times long past, compounded by lockdowns and isolation that makes a Home feel like a Panic Room when one cannot Walk Away from conflict and share uncomfortable Silence (s), cabin fever instead of feverishly spreading a Strange Disease
My Taped Up Heart hurts from Missing Time with friends and loved ones; Down With The Sickness when depression is what ails me, and no one can Tell Me Why I’m so tired all the time. I’m going stir Crazy playing the Waiting Game , not ready for my Halo but I can’t be a Zombie for that Sweet Child O’ Mine Drugs can help stave off the Madness that comes when Insomnia fuels the Monsters dancing in my head, but without evidentiary support, it’s Substance Use Disorder instead of a singalong with Puff the Magic Dragon
But when Bad Medicine leads to an excess of Overthinking , worried about increased mortality rates and co-occurring conditions that feel like they’re Killing Me Softly, then I Wear My Sunglasses At Night for the Hatching Ideas Lab , because finding The Perfect Drug can be a challenge and figuring out How We Operate together is more effective than working Alone A Spoonful of Sugar helps the Medicine go down, and understanding double empathy can avoid bitter Toxicity in the therapeutic alliance, when doctors have Patience with patients who communicate differently.
So let’s Rise Up and Celebrate organizations that value patients in research, as they can Truly be a C.A.C.H.E. of knowledge untapped. There’s No Limit to our innovation and potential when it’s Revelations we share; with patients as partners, we can evolve health care.
— Dedicated to Dr. W. R. Moore and Dr. H. J. Zeit
Stephanie Fernandes MN-NP (PHC-GH), HBSc, MHA, CHE (Sunnybrook Health Sciences Centre) ; Oliver De Laurentiis RN, MN, CNCC(C) (University Health Network).
The Canadian Interprofessional Health Collaborative (CIHC) framework identifies relationship-focused care as a core competency for effective interprofessional collaboration. This competency emphasizes developing mutual trust, respect, and shared understanding across professions and cultures, values that are especially vital in global health partnerships.

In May 2025, we traveled to Addis Ababa, Ethiopia, as part of the Toronto Addis Ababa Academic Collaboration (TAAAC) Nursing Program, a longstanding partnership between the University of Toronto and Addis Ababa University (AAU). Led by Drs. Vanessa Wright and Jana Lok, the program brings together emergency and critical care nurses and nurse practitioners to co-develop and deliver curriculum for AAU’s Master of Critical Care Nursing.
Twice a year, in May and November, nursing faculty from Toronto partner with AAU counterparts to deliver lectures and interactive skill stations that highlight clinical reasoning, evidence-based practice, and collaborative teamwork. The May 2025 session focused on identifying and managing deteriorating patients, underscoring key principles of emergency and critical care. Our cohort of 5-10 master’s students brought diverse regional experience, making the exchange deeply reciprocal.

The spirit of co-learning was central, reflecting the CIHC competency of relationship-focused care as we shared knowledge while learning from the contextual expertise of our Ethiopian colleagues. Challenges such as limited equipment and differing practice environments prompted creative approaches to case-based teaching, highlighting the value of adaptability and shared purpose.
Daily reflections amongst the faculty helped refine our approach throughout the month. We found that students responded most positively to interactive, scenario-based learning, which evolved as our relationships deepened. In addition, real-time debriefs with the faculty enriched our teaching, while student feedback guided improvements such as simplifying dense lectures and strengthening links between classroom and bedside learning.

This collaboration continues to evolve through mutual learning and respect. It illustrates that relationship-focused care is not built overnight, but grows through long-term, cross-cultural engagement that is grounded in trust and humility. Through this partnership, we witnessed the transformative potential of co-learning and capacity building. As the next team prepares to travel in November 2025, the momentum continues to be sustained by shared purpose and a deep belief in the impact of working together.
Alan MacKenzie, Communications Officer (Rady Faculty of Health Sciences, University of Manitoba)
Since 2017, students across nursing, pharmacy, midwifery and rehabilitation sciences programs at the University of Manitoba’s Rady Faculty of Health Sciences have undertaken several immersive international learning experiences in Ecuador, coordinated by the Office of Interprofessional Collaboration (OIPC).

From harvesting medicinal plants to engaging with the Kichwa healers and midwives, these journeys brought learners into culturally rich, communityled settings.
The experiences have involved spending up to a week in the Amazon rainforest in Amupakin, a birthing centre run by a collective of traditional Kichwa midwives known as “mamas.” Students also took part in hands-on workshops, cultural exchanges, and harvested medicinal plants.
Nicole Martin, a student in the College of Nursing’s midwifery program, has always had an interest in working internationally and saw the trip as a perfect opportunity. She also gained an appreciation for the other health disciplines represented on the trip.
“It was great to learn what respiratory therapists and occupational therapists do. It was a wonderful way to collaborate and build respect for each other’s professions,” Martin said.


Lisa Mendez, occupational therapy instructor and interprofessional practice coordinator with OIPC, facilitates the experiences, which she said are a “natural fit” for the Rady Faculty of Health Sciences, as the community is keen to host future healthcare providers.
She said one of the main objectives is to recognize the importance of cultural safety in providing healthcare within Indigenous communities. The other is for experience in interprofessional education and collaborative practice.
Mendez said the students involved in the initiative also had an opportunity to learn in Manitoba First Nation communities.
“I want to make sure we can link this back to our local context. Learning about traditional ways of knowing and being doesn’t have borders,” said Mendez.
For further reading, three related publications connected to this story are also available:
• https://news.umanitoba.ca/program-sendsrady-students-to-rainforest/
• https://news.umanitoba.ca/pharmacy-studentlearns-about-traditional-medicine/
• https://news.umanitoba.ca/amazonexperience-highlights-holistic-care/
“If you need to master something, teach it.”
- Richard Freyman
Khoo Su Ann MD MRCPCH (UK), MMed (Paediatrics), MMEd (Dundee) (KK Women’s and Children’s Hospital and Centre for InterProfessional Healthcare Education, SingHealth Duke-NUS Academic Medical Centre); Ong Hwee Kuan PT, BSc (Biochemistry), BHSc (Physiotherapy), DClinPT, MSc (Health Education) (Singapore General Hospital and Centre for InterProfessional Healthcare Education, SingHealth Duke-NUS Academic Medical Centre); Catherine Poey Hui Xin RN, MW, BHSc (Nursing), MEd, GDHM (KK Women’s and Children’s Hospital and Centre for InterProfessional Healthcare Education, SingHealth Duke-NUS Academic Medical Centre); Yvonne Goh Huat Keng MBBS, MMed (Emergency Medicine), MRCS Edinburgh (A&E), FAMS, MSc (Changi General Hospital and Centre for InterProfessional Healthcare Education, SingHealth Duke-NUS Academic Medical Centre); Kevin Tan BMedSci, BMBS, MRCP, FAMS, MS-HPEd (National Neuroscience Institute and Centre for InterProfessional Healthcare Education, SingHealth DukeNUS Academic Medical Centre).
This is the story of how we journeyed to grow from learners to facilitators of ehpic™ , with our lovely coaches from CACHE , Canada, from 2023 to recently 2025, in Singapore.


From top to bottom: ehpic™ 2025 cohort; ehpic™ 2025 facilitators.
“A journey of a thousand miles begins with a single step.”- Lao Tzu
In this journey, we discovered elements of ourselves that we never realized we had. We started out as learners in 2023 and then became small group facilitators in 2024. We learned to facilitate a diverse group of learners, often engaged in the questions and conversations of “Why does interprofessional education/ collaboration matter” and “Is it worth the effort”? In 2025, we challenged ourselves to lead and teach the large group theory bursts with coaching from our experienced CACHE facilitators.


From top to bottom: ehpic™ 2024 facilitators; ehpic™ 2024 cohort.
Our key learnings from this journey in becoming IP facilitators:
1. Observing and reflecting as teachers from CACHE kept the class intrigued and engaged
• The coaches had never treated us as ”just learners”. They role-modelled humility, steadfastness, and collaborative leadership throughout the years.
2. Never be afraid to seek feedback from peers and coaches
• As we stepped up to become facilitators, we sought and were given constant, in-themoment feedback, and gathered constantly to debrief. We were also each other’s biggest cheerleaders!
3. Learning to step out of our comfort zone and taking up space
• We were constantly nudged to step up and speak out to build our confidence. We were weary, stumbled, or filled with doubts, yet our coaches would say “We have your backs.” It was the most comforting phrase throughout the journey.
4. The importance of continued learning, unlearning, and relearning
• As healthcare professionals, we were our own harshest critics. This journey highlighted the importance of agility, forgiveness, and moving forward.
5. A community that focused on relationships, with shared purpose – a family
• Through ehpic™ yearly, we renewed our fire and passion for disseminating and rolemodelling interprofessional education and collaboration, the seed that our coaches first planted within us.

Ivy, Lynne, Dean, and Belinda started out as our teachers. They then became our teammates and coaches. We are proud to regard them as an integral part of our community and family.
We would like to dedicate this article and express our heartfelt gratitude to our coaches and friends from CACHE: Ivy Oandasan, Lynne Synclair, Dean Lising, and Belinda Vilhena.



Invent 2030.
Abegail D. Huevos RN; Ahmed Nasef MD; Annie Hoang RD; Claudia Wong, RN; Jennifer Lovering RN; Lauren Cosolo RN; Lisa Di Prospero MRT(T); Mylene Im RN; Romina Marchesano RPh; Tracey DasGupta RN. (All authors are affiliated with Interprofessional Practice, Practice-Based Research & Innovation, and Education, Sunnybrook Health Sciences Centre).
At the heart of healthcare transformation lies one powerful truth: we achieve more together. A Sunnybrook interprofessional team of health professionals, educators, and researchers joined leaders from across the globe to explore how AI, equity-driven leadership, and interprofessional collaboration can accelerate system change at THInC 2025 *, the Healthcare Innovation Conference, in Calgary. Throughout every session, common themes surfaced—communication that connects, reflection that refines, and shared decision-making that empowers. From using the “5 Whys” to uncover root causes, to embracing the “innovation dip” as part of growth, the team experienced how psychological safety fuels creativity and courage. Curiosity was ignited as we participated in design thinking that focused on how AI can enhance—not replace—clinical reasoning. This experiential learning strengthened our shared commitment to building digital confidence and collaborative competence across professions. What are we bringing back to our teams? Sunnybrook is charging forward to embed innovation into everyday interprofessional practice. We are launching dedicated innovation sprints, piloting AI-enabled learning tools, and creating spaces for joint reflection where all voices are valued—from bedside to
boardroom. Guided by our Core Competencies for Interprofessional Collaboration—communication, shared decision-making, role clarity, conflict resolution, reflection, and values & ethics—we are turning insights into action.

There is more ahead. A new interprofessional team has come together to Invent 2030 – calling ourselves innovation ambassadors. Our commitment is to foster a future where collaboration drives every breakthrough. This group will shape the next generation of practice, education, and research, ensuring innovation remains grounded in teamwork, equity, and patient-centered care. Starting with Nursing Council initiatives and interprofessional scope-of-practice dialogues, we will translate THInC lessons into tangible improvements: stronger teamwork in pressure injury prevention, more inclusive patient education, and empowered front-line innovation.
Together, we are proving that when teams collaborate with purpose, transformation is not just possible—it is unstoppable.
* For more on interprofessional nursing innovation and global collaboration, visit Sonsiel – The Society of Nurse Scientists, Innovators, Entrepreneurs & Leaders: https://www.sonsiel.org/
Dr. Alice Kam MD, MScCH (HPTE), FRCPC (Affiliate Scientist, KITE Research Institute, University Health Network; Scholar, The Wilson Center, Temerty Faculty of Medicine, University of Toronto)

Patients and caregivers (P/C) remain marginal in interprofessional education (IPE). Traditionally, P/C are involved as standardized patients to provide communication feedback. While valuable, this approach overlooks their practical knowledge.
To address this gap, our CIHR-funded project brought together physicians (generalists and specialists), allied health professionals, and P/C to co-design compassionate care rubrics. These rubrics establish relational care standards that recognize both care providers and recipients as equally essential to IPE.
Co-designing standards is an innovative pathway for IPE collaboration practice. Our collaborative process revealed contradictions—such as system standardization—that, rather than hindering collaboration, strive for innovative and flexible adaptations of compassionate care practices.
By embedding P/Cs as active partners, this assessment co-design directly support several CIHC Competencies:
• Team differences processing through balancing equal partnership in defining compassionate care.
• Collaborative leadership by valuing P/C knowledge alongside professional expertise.
• Teamwork functioning through shared language for relational standards of care.
This work demonstrates that balancing care provider and recipient perspectives is not only possible but essential for preparing learners to deliver high-quality compassionate care. Our collaborative co-design approach offers a practical, replicable model for embedding equity and compassion into IPE. For further information, please see our website: www. compassionatehealthcare.ca
References:
• CIHC Competency Framework for Advancing Collaboration (2024). Website: https://cihccpis.com/wp-content/uploads/2024/06/CIHCCompetency-Framework.pdf . Date of access: October 1, 2025
• Vygotsky, L. S. (1980). Mind in Society. Harvard University Press. https://www.hup.harvard. edu/books/9780674576292
• Tehranineshat, B., Rakhshan, M., Torabizadeh, C., & Fararouei, M. (2019). Compassionate care in healthcare systems: A systematic review. *Journal of the National Medical Association, 111*(5), 546–554. https://doi.org/10.1016/j. jnma.2019.04.002
• Engeström Y, Pyörälä E. Using activity theory to transform medical work and learning. Medical Teacher. 2021;43(1):7-13. doi:10.1080/01 42159X.2020.1795105
• Braak, M. van, Groot, E. de, Veen, M., Welink, L., & Giroldi, E. (2018). Eliciting tacit knowledge: The potential of reflective approach to videostimulated interviewing. *Perspectives on Medical Education, 7*(6), 386–393. https://doi. org/10.1007/s40037-018-0487-9
Ghada Faddoul MSc. BSc. MRT (R)(MR) (Michener Institute of Education at University Health Network)
Background:
Patient involvement is now common across medicine, nursing, and allied health education. A 2024 review (Palmaria, Bolderson, & Fawcett) highlighted benefits for patients, students, and programs. Educational strategies have included patient storytelling, workshops, role-playing, simulation, patient interviews, and public speaking, all of which contribute to enhanced empathy, communication, and clinical readiness.
Historically, Magnetic Resonance Imaging (MRI) was exclusively a second-entry profession for Medical Radiation Imaging Technologists (MRITs) transitioning from other imaging modalities. Rising health human resource (HHR) demands and shortages have led to new MRI pathways for learners without prior healthcare experience.
The Michener Institute of Education at University Health Network (UHN) has long been a leader in MRI education, offering a part-time, online program for MRITs. To address Ontario’s evolving HHR needs, Michener launched the MRI First Discipline Program in January 2024—a two-year, full-time, hybrid program designed for learners without previous healthcare experience.

To support the development of patient-centered competencies, the MRI First Discipline Program introduced new curricular activities involving patient partners. These activities aimed to cultivate patient advocacy, empathy, stewardship, and clinical readiness during the final didactic semester prior to clinical training. This initiative was made possible through Michener’s collaborative partnership with CACHE.
Pedagogical approaches have been documented in other health professions, but the literature is lacking in MRI education. It is essential to incorporate patient stories that reflect the unique experiences of MRI patients into the curriculum to enhance care delivery and help shape the next generation of MRI technologists.
Methodology:
In collaboration with CACHE, the MRI program invited patient partners to share their MRI experiences. The invitation email clearly outlined the activity’s goals, emphasized the importance of diverse patient experiences, and offered an honorarium. Participants could choose between a video-recorded interview or a written narrative.
Participation: Six patients responded. One submitted a written narrative; five chose video interviews. Of these, one later provided written responses after a virtual meeting, while four completed video interviews (via Teams or Zoom) facilitated by the MRI Program Academic Chair.
Learning Activity: Students engaged with the patient narratives (written or video) as part of their coursework. Each student selected one case for deeper reflection and submitted a written paper connecting the patient’s experience to course content and professional practice.
Evaluation:
Students completed pre- and post-intervention surveys to measure changes in knowledge, empathy, and application of patient-centered care. This approach aimed to foster reflective practice and reinforce the role of patient experiences in MRI care.
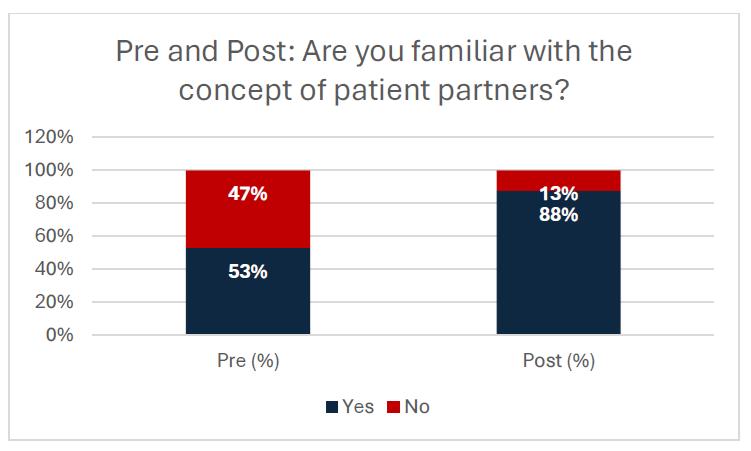
Results:
Sixty-nine percent of students reported they had not previously encountered patient partner stories. After the activity, 88% indicated they were familiar with the concept, reflective of the progression of familiarity from the activity. All students recognized, both before and after the intervention, that patient perspectives are
essential in MRI care. Nearly all students felt comfortable advocating for patients at both time points. Importantly, 96% of students reported being satisfied with the patient partner learning activity. These results indicate that patient partner engagement was both impactful for students and feasible within the curriculum. Additionally, some students reflected on their role towards impacting systemic change by speaking up and advocating for patients not just within the MRI department but within the larger health care spectrum.
Discussion and Conclusion:
Overall, our collaboration with CACHE resulted in positive patient partner engagement. While assessing and determining competence in patient advocacy proved challenging, students consistently reflected on the valuable skills they gained by listening to patient stories. Many emphasized the importance of empathy, compassion, kindness, and active listening in their future practice. They also recognized the significance of putting themselves in the patient’s shoes, treating others as they would want to be treated, ensuring patients feel heard and welcomed, going above and beyond to provide patient-centered care, and building trust to foster a positive MRI experience.
This initiative also identified several opportunities to expand the patient partner program at Michener. Key considerations include establishing clear criteria for selecting patient partners, ensuring diversity within the panel, and providing comprehensive orientation for patient partners.
Reflecting on the process, in the future, we plan to provide more in-depth preparation for patient partners prior to recordings.

The development of this new curriculum underscored the value of partnering with CACHE to support the integration of patient partners into curricular activities at Michener. As the only institution in Canada dedicated exclusively to health professions education, Michener is uniquely positioned to benefit from ongoing collaboration with CACHE. Strengthening this partnership will support multiple health professions and promote a culture of patient-centered care.
References:
• Palmaria, C., Bolderston, A. & Fawcett, S. (2024). A scoping review of patients as partners in undergraduate allied health curriculum: How are they involved? Journal of Medical Imaging and Radiation Sciences: 55 (4). https://doi. org/10.1016/j.jmir.2024.101724
Ali Kasim Rawji BSc (University of Toronto) ; Charlie Steele (Advocate, Concussion and Brain Injury Survivor).

One section of our Knowledge Translation for Disability & Rehabilitation Research (KTDRR) Conference presentation was titled “From Patients to Leaders: How Patient-Centered Partnerships Can Build the Future of Healthcare.” This section grew out of an interprofessional team that brought together perspectives from patients, caregivers, healthcare professionals, and learners. After open conversations between physician Dr. Alice Kam, patient Charlie Steele, and medical student Ali Kasim Rawji, our team developed a model to help define what “good care” really means. The model has three steps: patient–provider partnerships at the base, leading to leadership that drives health impact, and ultimately mentoring the next
generation to embody the same principles. At the conference, we presented together to demonstrate what collaboration across roles can look like in action. The presentation became more of a dialogue between Ali Kasim and Charlie, rather than a lecture. Charlie told stories that grounded our model in real experience. He described moments when a physician paused, made eye contact, and spoke slowly so he could follow along. Those small, intentional actions made him feel not just supported, but like an active leader in his own care. He also reflected on how these moments shaped his trust in the healthcare team and his confidence in participating in decision-making. By sharing these concrete examples, we were able to show how attention to communication, respect, and patient engagement can influence outcomes, strengthen partnerships, and create a more meaningful care experience for patients. Charlie’s reflections also sparked discussion with the audience, prompting them to share similar experiences from their own practice and observations. Through these exchanges, we were able to demonstrate that collaborative care is not just an ideal, but a tangible practice that can shape outcomes, enhance trust, and foster stronger connections between patients and providers.
At its core, our project emphasized collaboration— working across roles and experiences and advocating for patient–provider partnerships that make healthcare more compassionate and equitable.


Sabrina Bartlett M.Ed., B.Ed. (Manager, Curriculum & Education Innovation, CACHE); Maria Tassone MSc, BScPT (Health Systems & Policy Advisor, CACHE); Belinda Vilhena M.Ed., B.Sc. (Director of Operations & Business Development, CACHE); Jill Shaver RD, MBA, MSOD (Independent Consultant); Kathryn Parker PhD (Associate Director, Transformative Change & Evaluation, CACHE); Sacha Agrawal MD MSc FRCPC (Inclusion & Co-Production Advisor, CACHE)
On May 7, 2025, the Collaborative Change Leadership (CCL) Alumni community came together for an Inaugural Alumni Event. This day was an opportunity for the CCL Alumni to connect and reconnect, reflect, and explore the evolving practice of collaborative change leadership.
The day began with participants reconnecting with peers and sharing stories of impact in their environments and systems. The morning’s highlight was the keynote session with Dr. Haesun Moon, titled “Words that Change Worlds: Curating Better Conversations with Coaching”. Dr. Moon’s engaging talk resonated deeply, inviting participants to consider how language and coaching can shape meaningful change. Her curiosity, warmth, and energy sparked rich dialogue, and participants noted how her ideas aligned with the spirit of the CCL model.
The afternoon continued with making ‘old and new’ connections, as well as exploring how alumni are applying collaborative change leadership concepts in their diverse settings. Conversations revealed both pride and humility as many alumni surfaced the
breadth and depth of their individual and collective impact in healthcare and health professions education.
“Amazing to see everyone! Networking was great! Met some new people...all kindred spirits:) Keeping the common language and worldview of CCL alive!”

The energy in the room was undeniable, and alumni left feeling inspired, committed, and eager to continue building a stronger, more connected CCL community. We look forward to sharing what’s coming next with and for our alumni community!
“The energy in the room, the openness and vulnerability during small group discussion exercises. As always, the CCL team formats the day with a beautiful cadence of activities that keep the group engaged all day long.”

Marianne Ng RRT, BSc, MHSM (University Health Network)
Prompted by the Ontario Health Home First directive, UHN embarked on a strategic planning journey to transform discharge practices across its acute and post-acute sites. The directive emphasizes:
• Initiating early discharge planning discussion with patients and families
• Supporting patient-centered transitions
• Ensuring all community supports are explored before considering long-term care (LTC)
In December 2024, UHN launched strategic planning for Home First with a leadership retreat that brought together more than 80 leaders from acute care, post-acute care, and community partner organizations. This retreat as the foundation for collaborative engagement— designed to seek feedback, brainstorm ideas, share learnings, and co-create the Home First pathway. It ensured all voices were heard and set the tone for inclusive, interprofessional practice.
A steering committee was formed, followed by seven task forces with more than 100 participants
representing diverse disciplines, care settings, and patient partners. These structures were grounded in the CIHC Competency Framework:
• Collaborative Leadership: Shared accountability and co-ownership of strategy and implementation
• Team Communication: Retreats and discussions fostered open, respectful dialogue
• Role Clarification and Negotiation: Clear alignment of responsibilities across professions and care settings
• Relationship-Focused Care: Patient partners co-developed resources like tip sheets and posters
Two additional retreats followed, each deepening engagement and supporting the co-design of tools, workflows, and discharge communication strategies.
In Summer 2025, UHN transitioned to implementation, forming committees focused on education and communication to support staff across UHN in adopting the Home First philosophy.
The UHN Home First Pathway go-live in September 2025 marks a milestone in collaborative change— driven by provincial direction and powered by interprofessional teamwork.

Isabella Cheng MSc, OT Reg.(Ont); Liane Chornobay; Tracey DasGupta RN, MN; Chris FanLun BScPhm, ACPR, BCGP; Lois Fillion R.N., BScN, MHSc; Lina Gagliardi MSW, RSW; Amber Hall M.Ed., BA (TR) Hons, R/TRO; Megan Hamilton MHSc; Annie Hoang MEd, RD; Dr. Barbara Liu MD, FRCPC; Sonia Nobleza RN, BScN, MN, GNC(c); Theepana Singarajah RN, BScN, APN; Kaili Walters PT, MScPT; Julie Waspe RN, BScN, MN, BASc; Erica Wong MSc, AuD. Reg. CASLPO; Jennifer Wong MHSc, S-LP (C). Reg. CASLPO (All authors are affiliated with the Specialized Geriatric Services at the Peter Cipriano Centre for Seniors Health, Sunnybrook Health Sciences Centre).
Sunnybrook Health Sciences Centre is proud to introduce a bold new vision for Specialized Geriatric Services at the Peter Cipriano Centre for Seniors Health. The Cipriano Centre is a custombuilt 13,000-square-foot senior-friendly space, home to integrated, research-inspired, patientfirst care. It brings together a full spectrum of outpatient services to improve care accessibility, coordination, and outcomes for older adults. The Cipriano Centre model of care emphasizes:
• Seamless access to specialized care and community resources
• Interprofessional collaboration
• Patient journey modeling, co-designed with patient partners and staff
• Efficient and effective care coordination with community partners

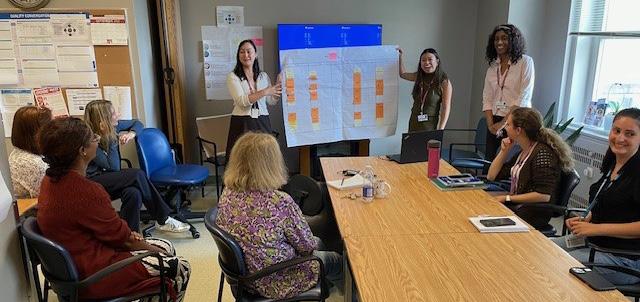
In partnership with Quality and Patient Safety, Interprofessional Practice, Clinical Informatics, and Strategy teams, we held cocreation workshops with patient partners and frontline staff to define team-based workflows and interprofessional role clarity, and realign daily practices with a commitment to transform integrated care as One Team to support older adults to remain independent at home. Our interprofessional team—including a dietitian, nurses, occupational and physical therapists and assistant, pharmacist, recreation therapist, social workers and a speech language pathologist—is redefining comprehensive geriatric services. By piloting and refining our team-based approaches, we build on collective strengths to focus on what is most important to each patient. Older adults benefit from personalized care plans developed through coordinated consultation with geriatricians and health professionals. “Onestop” access to audiology and optometry services enhances continuity with primary care. Outpatient rehabilitation programs include Day Hospital, Falls Prevention, and Learning the Ropes. Our expanded outreach pathway offers rapid access after emergency department visits and home-based assessments for those needing in-home services. As Canada’s first hospital with Level 2 AgeFriendly Health System designation, Sunnybrook is excited to lead this transformation. More than a welcoming space, the Cipriano Centre is a movement advancing compassionate, connected, and person-centred care.
Amber Hall BA Therapeutic Recreation, M.Ed, (Sunnybrook Health Sciences Centre); Christina Pachete MHSc SLP(C) Reg. CASLPO (Sunnybrook Health Sciences Centre); Debbi Leith BA, MA (Sunnybrook Health Sciences Centre); Kathryn Rochette RD; BASc., ADRS, M.Ed (Sunnybrook Health Sciences Centre); Mackenzie Conn BSN RN (Sunnybrook Health Sciences Centre).
Eating in isolation, during hospitalization, can have a profound negative impact on patients, particularly those with cognitive impairments, depression, or who require assistance with meals. Patients with cognitive impairments may miss social cues while eating, while those experiencing depression may have reduced appetite and oral intake. Additionally, patients in need of tray set-up or supervision frequently receive limited assistance in their rooms due to staffing constraints. These factors contribute to hospital-acquired malnutrition, which adversely impacts recovery, prolongs hospital stays, and increases healthcare costs (Correia & Waitzberg, 2003; Wright et al., 2006).
To address these issues, Sunnybrook’s Holland Centre Campus developed a communal dining program that transforms an activity lounge into a two-table dining space accommodating eight wheelchair/seated patients. This initiative is an interprofessional effort involving dietitians, speech-language pathologists, physiotherapists, nutrition technicians, nursing, occupational therapists, personal support workers, recreation therapists, and volunteers.

Patients are invited to eat their hospital meals together, fostering social interaction that encourages better oral intake. A list is provided to volunteers identifying suitable patients for the program, along with patient-centred conversation starters and activities for mealtime.
The volunteers escort patients to the dining space, assist with tray set-up, and help open food containers, with nursing staff present to ensure safety. This set-
up also allows healthcare professionals to monitor intake, preferences, diet texture tolerance, and use of safe swallowing strategies.

The communal dining program addresses common barriers to food intake identified in Canadian hospitals, such as poor positioning, difficulty accessing trays, and limited self-feeding ability (Keller et al., 2015). Patients benefit from improved positioning, reducing risks related to dysphagia (Shune & Linville, 2019), and engage in social cues that increase consumption of energy, protein, and fluids (McLaren-Hedwards et al., 2022).
Overall, this collaborative, patient-centred program supports nutrition, mealtime safety, and rehabilitation outcomes, and can reduce hospital length of stay and associated costs.
References:
• Correia, M. I. T. D., & Waitzberg, D. L. (2003). The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clinical Nutrition, 22(3), 235–239. https://doi.org/10.1016/ S0261-5614(02)00215-7
• Keller, H., Allard, J., Vesnaver, E., Laporte, M., Gramlich, L., Bernier, P., Davidson, B., Duerksen, D., Jeejeebhoy, K., & Payette, H. (2015). Barriers to food intake in acute care hospitals: a report of the Canadian Malnutrition Task Force. Journal of Human Nutrition and Dietetics, 28(6), 546–557. https://doi.org/10.1111/JHN.12314
• McLaren-Hedwards, T., D’cunha, K., Elder-Robinson, E., Smith, C., Jennings, C., Marsh, A., & Young, A. (2022). Effect of communal dining and dining room enhancement interventions on nutritional, clinical and functional outcomes of patients in acute and sub-acute hospital, rehabilitation and aged-care settings: A systematic review. Nutrition & Dietetics, 79(1), 140–168. https://doi.org/10.1111/1747-0080.12650
• Shune, S. E., & Linville, D. (2019). Understanding the dining experience of individuals with dysphagia living in care facilities: A grounded theory analysis. International Journal of Nursing Studies, 92, 144–153. https://doi.org/10.1016/J. IJNURSTU.2019.01.017
• Wright, L., Hickson, M., & Frost, G. (2006). Eating together is important: Using a dining room in an acute elderly medical ward increases energy intake. Journal of Human Nutrition and Dietetics, 19(1), 23–26. https://doi.org/10.1111/J.1365277X.2006.00658.X


Partnering with People with Lived Experience to Enable PersonCentered Integrated Care
Tuesday December 9, 2025 | 12:00-1:30PM ET | Virtual
Across Canada, people with lived experience are leading transformative work in integrated care. From national networks to research partnerships, this leadership is creating the infrastructure needed for genuine co-design and shared decision-making. Healthcare systems increasingly recognize the importance of involving people with lived experience, and many are doing more of this work than ever before. What’s emerging now is the shift from involvement to authentic partnership where power is genuinely shared.
Moving from consultation to authentic partnership requires systems to change how they operate, not just how they engage. It means confronting power dynamics, investing time in building trust and relationships, and creating conditions where people can participate fully as co-leaders, not just advisors.
This session brings together people with lived experience, researchers, and system leaders to explore what authentic partnership looks like in practice, what it takes to sustain it, and how to build on the transformative leadership already happening across the country. Join us to learn and unlearn together, connecting with others working toward integrated care that’s genuinely shaped by the people it serves.
To learn more about this session or to register visit the website: https://integratedcarefoundation.org/events/people-with-lived-experience-webinar

Teaching for Transformation Co-Facilitation Certificate January 12 – 19, 2026 | Virtual & In Person
The Teaching for Transformation (TforT) Co-Facilitation Certificate Program is an interactive and immersive learning experience designed for individuals interested in co-facilitating interprofessional educational initiatives informed by humanistic and transformative education practices.
When we say co-facilitation, we mean collaborative facilitation by a patient/family/caregiver partner in partnership with a faculty member, learner, or practitioner. Participants will engage in hands-on practice, receive feedback, and build essential skills for leading and facilitating interprofessional education.
This certificate program provides a unique opportunity to grow as a leader, educator, and collaborator in health professions education. By participating, you will:
• Build Leadership Capacity – Strengthen your confidence in co-facilitating learning with diverse groups.
• Enhance Your Educational Practice – Learn facilitation strategies that center equity, collaboration, and partnership, while gaining direct experience in interprofessional teaching.
• Shape the Future of Healthcare – Contribute your perspective as a patient/family/caregiver or practitioner in shaping how over 1,000 UofT health and social care students learn about partnership.
• Gain Transferable Skills – Hone communication, teamwork, and critical reflection skills that apply across professional, community, and leadership contexts.
• Join the U of T Community – Join a network of faculty, students, and partners engaged in collaborative, interprofessional education.
Visit the website to learn more about the program components and/or to register: https://teachingfortransformation.com/certificate-in-co-facilitation/
For anyone who may not be able to attend the workshop (Jan. 12), but can co-facilitate on January 19th, please email eli.cadavid@uhn.ca directly, we would love to get you involved.
Teaching for Transformation (TforT) is jointly offered by Centre for Faculty Development and Centre for Advancing Collaborative Healthcare & Education

Bird Discount Deadline: January 12, 2026
March 9-11, 2026 | 9:00AM – 4:00PM ET |Virtual or In-person
TforT:C is a three-day immersion in the education paradigms and practices needed for today’s health care work. TforT:C involves invited speakers/facilitators and submitted abstracts.
In health professions education, trust is more than a principle. It’s a practice that must be embodied across teaching, science, and care. At the 2026 Teaching for Transformation: Conference , we explore how trustworthiness in our roles requires not just evidence and ethics, but connection: to one another, to our patients, and to the diverse communities we come from. Ironically, the journey into professional identity can sometimes create distance from those very communities. Transformative education invites us to bridge that gap. This year’s TforT:C will explore what trust means, share educational approaches that can strengthen community, and propose innovative models for caring and connection. Join us and bring your voice to the conversation as we work together toward trust-building, trustworthy transformative education for health and social care.
This conference is relevant to health and social care providers, educators, researchers, health/education policy and decision makers, patients/family partners, caregivers, students, and all individuals who share an interest in advancing the theories and practices of humanistic and transformative education and critical pedagogies and practices.
Registration: The 2026 Teaching for Transformation: Conference will be offered as a hybrid conference. Please note that you can select only ONE conference delivery option. For example, if you choose to attend in-person, you cannot attend online and vice-versa.
Visit the website to register: https://teachingfortransformation.com/conference/
Teaching for Transformation (TforT) is jointly offered by Centre for Faculty Development and Centre for Advancing Collaborative Healthcare & Education

Meet JCIPE in Philadelphia, Pennsylvania for its 9th Biennial Conference!
April 17-18, 2026 | Dorrance Hamilton Building, Philadelphia, PA, USA
The Jefferson Center for Interprofessional Practice & Education (JCIPE) will host its 9th biennial conference, Interprofessional Care for the 21st Century, in Philadelphia, PA this Spring 2026. This conference showcases scholarly work and work in progress related to interprofessional education, practice, research, and advocacy. The conference provides the opportunity to connect and collaborate with interprofessional colleagues and highlights innovative interprofessional competency development, program implementation, evaluation strategies, and best practices to advance the field. Educators, clinicians, practitioners, health system leaders, policymakers, patients, students, and other stakeholders interested in teamwork throughout the health and social services fields are invited to attend.
Conference Contact: Catherine Mills, jcipe@jefferson.edu
Visit the website to learn more and/or to register: https://web.cvent.com/event/fd648808-40b7-49b7-8000-aa1546465478/ summary?environment=P2

May 13th, 2026 | 9:30-12:00pm ET | In Person - Toronto, ON
Unlock your teams full potential with BOOST! — a dynamic, skill-building workshop designed to elevate communication, collaboration, and performance across both virtual and in-person environments.
By the end of the session, you’ll be able to:
• Apply the Canadian Interprofessional Health Collaborative (CIHC) Competencies to enhance collaborative, relationship-focused care
• Explore strategies and tools to optimize team communication, clarify roles, negotiate responsibilities, resolve disagreements, and lead collaboratively
• Examine current team processes and identify opportunities to boost team success
Whether you work in a remote, in-person, or hybrid team, BOOST! will give you the tools to thrive. For additional information contact the Program Manager Sabrina Bartlett, Sabrina.bartlett@uhn.ca
Visit the website to learn more and/or to register: https://ipe.utoronto.ca/boost-workshops

Each page of Together is shaped by real people who believe in the power of collaboration.
Take a moment to reflect:
• What does collaboration look like in your work or learning?
• Where have you seen interprofessional care make a difference?
• How can creativity, conversation, or community shape better systems?