





Dear Alumni, Friends, and Colleagues, Hard to believe we are almost through this academic year. This issue of BU Medicine celebrates the contributions of our alumni, faculty, and staff, beginning with our cover feature on the joys and challenges our alumni experience when playing vital roles in the lives of rural residents and their communities.
We also highlight the physician assistant (PA) and MD entering classes. These students have started 18 months of combined studies taught in a team-based learning environment that integrates foundational sciences and pathology and mirrors the cooperative approach they will encounter in their careers. We are one of only two schools nationally where PA and MD students attend classes together for an extended period.
You can read about our many outreach programs introducing Boston public high school students in our community to careers in STEM-M (Science, Technology, Engineering, Mathematics, and Medicine) to diversify the biomedical research and healthcare workforce.
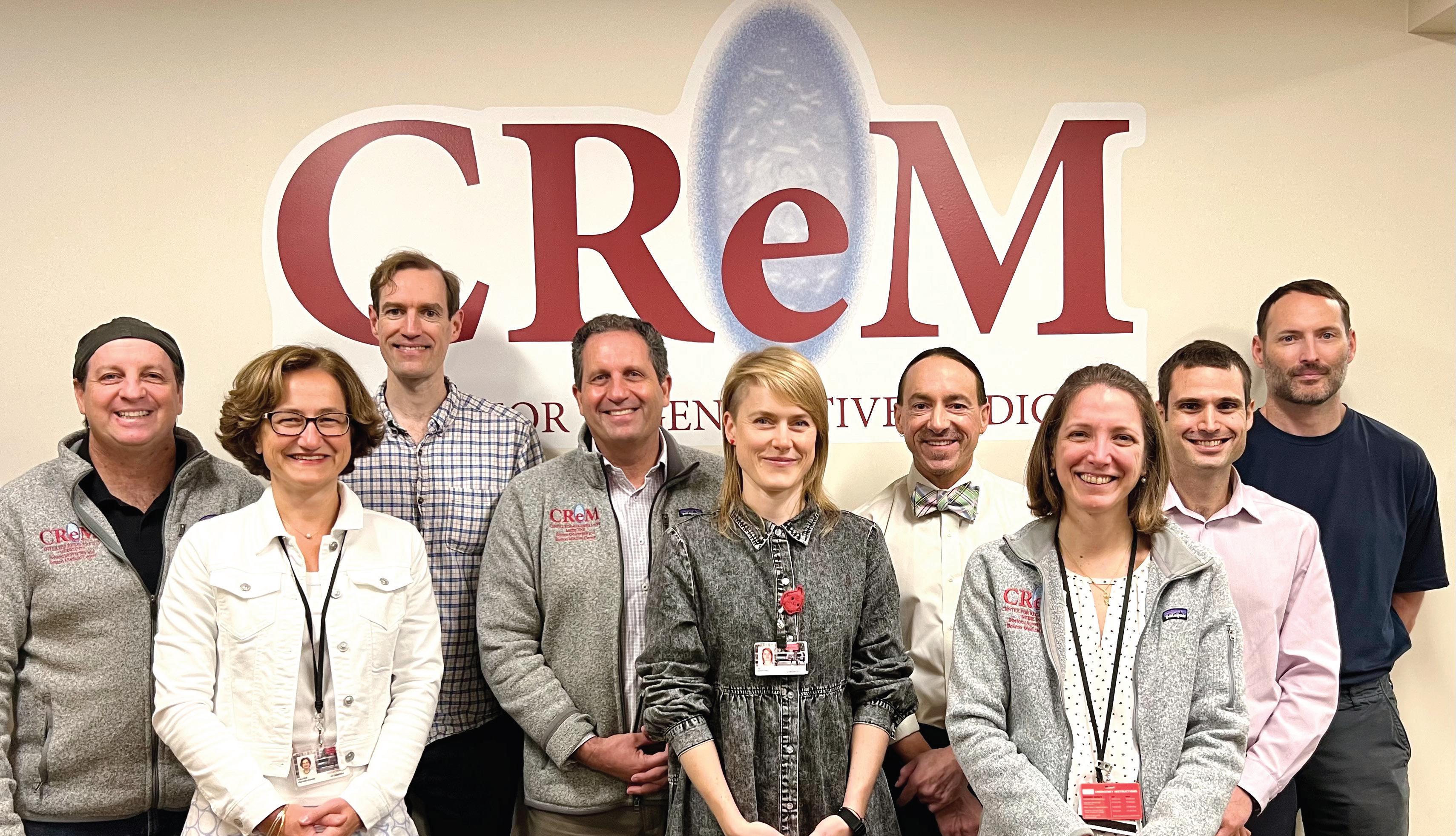
We are proud to celebrate the 10th anniversary of the BU-BMC Center for Regenerative Medicine (page 10). Meet the team that is advancing science to heal the world!
Globally, we write about our unique collaboration with the country of Lesotho, the Lesotho Boston Health Alliance (page 14). Led by the late William Bicknell, MD, professor and director of international health programs in our school’s department of family medicine and chair emeritus of the BU School of Public Health department of global health; and Brian Jack, MD, professor and chair emeritus of family medicine, BU faculty and students have been working closely with Lesotho since 1990.
Boston University Medicine
Boston University Medicine is published by the Chobanian & Avedisian School of Medicine Communications Office.
Maria Ober
Associate Dean, Communications
design & production
Boston University Creative Services
contributing writers
June Bell, Lisa Brown, Gina DiGravio, Doug Fraser, Sarah Rowan
photography
Zoë Farr, David Keough, Sarah Rowan
cover photography
Joshua Corbett
cover story photography
Joshua Corbett, Janelle Lyford, Patrick Strattner, Isabel Vinson
Please direct any questions or comments to:
Maria Ober
Communications Office
Boston University Medical Campus
85 East Newton Street, M810H Boston, MA 02118
P 617-358-7869 | E mpober@bu.edu
Our giving section and donor report (page 31) highlight your generous gifts. We also profile Marvin Hoffman (CAMED’47) and feature stories on grants from the Breast Cancer Research Foundation to Julie Palmer, ScD, and from the American Cancer Society to Deborah Lang, PhD, and Rachel Flynn, PhD; and the Smith Family Foundation Odyssey Award to Mohsan Saeed, PhD, their first BU honoree.
Our alumni section (page 36) celebrates our 2023 Distinguished Alumni Award recipient Reshma Kewalramani (CAS’98, CAMED’98), CEO and president of Vertex Pharmaceuticals, and Drew Weissman (CAMED’87, GRS’87, Hon.’23), who, with Katalin Karikó, won the 2023 Nobel Prize in Physiology or Medicine for their pioneering research in powering the mRNA COVID vaccines.
Thank you to our donors and friends for your continued commitment to our school and your generous support for our outstanding students, faculty, and staff on the front lines of science and medicine.
Best Regards,
Karen Antman, MD Provost, Medical Campus Dean, Chobanian & Avedisian School of Medicine
Boston University Chobanian & Avedisian School of Medicine is one of just two medical schools nationally where physician assistant (PA) students and medical (MD) students attend classes together for an extended period. In the past, BU PAs would take foundational science courses like biochemistry, physiology, and gross anatomy separately from medical students, while joining them for the pathophysiology course.
This year, PA and MD entering classes started simultaneously in August, with 18 months of combined classes taught under a new curriculum launched last year for medical students, a team-based learning technique that integrates foundational sciences and pathology and closely mirrors the cooperative approach they will encounter in their careers.
“Teamwork is foundational to the curriculum, and our physician assistants have a lot of work experience, many of them in healthcare. Some, but not all, of our medical students have that,” says Priya Garg, MD, associate dean for medical education. Garg notes that as more doctors gravitate to specialties, PAs and nurse practitioners are helping to fill the ever-widening shortage of primary care physicians.
Created in the 1960s in response to a physician shortage that continues today, the PA position was initially filled by many post–Vietnam War medical corpsmen. There are now 304 PA education programs in the United States; curriculums also include over 2,000 hours of clinical rotations. There is no residency requirement.
BU’s PA program began in 2013 in part due to the need for more PAs at Boston
Medical Center, says Susan White, MD, assistant professor of obstetrics & gynecology and PA program director.
“There’s more need for the PA profession because it’s a cost-effective way of providing care. Physicians alone can’t keep up with the demand for medical care,” says Aliza Stern, MMS/MMSc, director of didactic education for the PA program.
While other PA programs may have instructors teaching classes outside their specialties, BU can call upon specialists in all fields, including a robust research community, medical school faculty, and physicians at Boston Medical Center.
A 2020 Association of American Medical Colleges report predicted a shortage of between 54,100 and 139,000 primary care physicians by 2033. The Affordable Care Act enacted in 2010 created greater access to health insurance and healthcare, helping to spur demand for the position. There has been a 34% growth in licensed PAs since 2006, and according to the United States Department of Labor, a 38% increase in PA jobs is predicted as necessary over the next decade to meet the need.
The prerequisites for medical school and admission into a PA program are very similar, says White. Initially, there was some concern that PA students would not keep up academically, but their track record on other combined courses has demonstrated their competency.
“We’ve had the PAs in the second-year DRX (Disease and Therapy) course for a long time, and their performance has been pretty equivalent to the MD students,” says Garg.
PAs fall under the supervision and direction of licensed physicians, which has helped create a team philosophy and approach at the clinical level. Medical and PA school administrators hope the new team-based learning approach will further remove barriers and encourage familiarity for PAs and MDs alike.
“Most MDs have very little understanding of what other people in healthcare do until they’re pretty far along in their residency, which is a detriment to being successful in treating patients,” says Garg. “The fact that they’re sitting next to someone who is training in the PA program will help them to understand what a PA is and hopefully undo some of the bias that exists. In clinical practice, it’s much more about teamwork and everyone contributes their expertise.”
PA students go directly from graduation into clinical settings. BU’s program has a lot of appeal to prospective students, says Stern, because of the challenge and academic rigor associated with being taught at a university medical school.
While other PA programs may have instructors teaching classes outside their specialties, BU can call upon specialists in all fields, including a robust research community, medical school faculty, and physicians at Boston Medical Center.
“It is important for PA students to have a really good foundation of medical knowledge,” says White, adding that instead of having two separate programs teaching the same courses, “the right thing to do was to join them.” ●


The stethoscope draped around her neck meant a lot to first-year medical student Rohini Kambhampati as she posed for a photo with classmates at the sixth Annual Lorraine Stanfield, MD, Memorial Doctoring Lecture, held on August 28. The lecture aims to help new students understand the healing role of patient-physician interactions, especially how the physical examination contributes to diagnosing and caring for patients.
“I feel like I’m finally entering the field that I’ve always wanted to enter,” said Kambhampati, whose family emigrated from India. Her father is a Houston-based physician.
It’s become a tradition for first-year medical students to receive the tools of their profession—a stethoscope donated by alumni, a patella hammer, and the tuning forks, an ophthalmoscope and an otoscope—following the Stanfield Lecture.
In the keynote lecture, Stephen Tringale
(CAMED’90), an assistant professor of family medicine, told the 175th entering class that the doctor-patient relationship is one of the most important healing tools they will have.
“When I walk into the [examination] room, I think in my head that I’m shoulder to shoulder with the patient, that I’m on the same side of the table,” said Tringale, who also serves as the Codman Square Health Center medical director for quality and patient safety, performance improvement & research. He is a resident and student preceptor and a family physician.
A key principle guiding his patient interactions is how he can help them. Medicine involves continuous learning, and ideally, a doctor experiences tremendous personal and professional growth during a medical education and throughout a career. The doctor-
Continued from previous page

patient relationship is, at its core, a selfless experience in which knowledge is partnered with the human relationship shared by a doctor and patient.
“We are meeting the patient where they are, not where we are,” Tringale stressed.
“Understand why you want to be a doctor, and this will sustain you through the tests, the down times, and the difficult relationships. It will sustain you through the hardships that you will be present for and bearing witness to. It will be your North Star, your compass,” he said.
Stanfield, who died in 2017 from breast cancer at age 56, spent two decades taking care of medically underserved patients at Dorchester House Health Center (now known as DotHouse Health) as a primary care provider. She was one of the first physicians involved in the Center for Community Health, Education & Research program, which offered medical students longitudinal experience at a community health center, and for 25 years she strove to eliminate racial and ethnic disparities in healthcare through the education of health professionals and by improving services to underserved populations.





Stanfield was intellectually curious and made a point of knowing and understanding her patients in the context of their communities. “Lorraine coached people to listen,” said Michelle Nadow, chief executive officer at DotHouse Health. Nadow urged students to venture beyond the four walls of the hospital or medical practice and into the neighborhoods.
“The qualities that people use to describe Dr. Stanfield are the qualities we want you to take away from your time here and bring into your future practice.”
Molly Cohen-Osher, MD, assistant dean of medical education for curriculum and instructional design and assistant professor of family medicine
Molly Cohen-Osher, MD, assistant dean of medical education for curriculum and instructional design and assistant professor of family medicine, recalled Stanfield ensuring a supportive space for her when she joined BU a decade ago as a junior faculty member and new mother. “She set an example for me of the type of clinician-educator and faculty mentor I wanted to become,” said Cohen-Osher. “The qualities that people use to describe Dr. Stanfield are the qualities we want you to take away from your time here and bring into your future practice.” ●


This year’s Summer Training as Research Scholars (STaRS) cohort culminated their 10-week on-site internships at the Graduate Medical Sciences Summer Undergraduate Research Symposium on August 11.
Held at Hiebert Lounge, the symposium offered STaRS scholars the opportunity to present their independent research projects to Boston University Medical Campus faculty, staff, and students.
The 2023 STaRS scholars:
● Jacqueline Alford
● Jessica Oliveira Bacelar
● Matthew Jacob Byrne
● Jonathan Matthew Carnino
● Malia Magnolia Cole
● Shira Maya Freilich
● Arielle Gilliam
● Stevia Coralie Nanfack Tsakem
● Chioma Okolo
● Elizabeth Myriam Puyo
● Valerie Reyes Ortiz
● Leila Alejandra Rivera Rosario
● Diana Esmeralda Rodriguez
● Mikaili Zoe Senwah
Coming from colleges and universities across the continental US and Puerto Rico, the cohort included six second-year undergraduates, seven third-year undergraduates, three fourth-year undergraduates, and one Boston University medical student.
The faculty mentors for this year’s STaRS cohort:
● Joseph P. Mizgerd, ScD
● Francesca Seta, PhD
● Sarah Mazzilli, PhD
● Andrew Wilson, MD
● Gareth Morgan, PhD
● Joseph Zaia, PhD
● Jeffrey Siracuse, MD, MBA
● Weining Lu, MD
● José Rafael Romero, MD
● Jessica Levi, MD
● Vickery Trinkaus-Randall, PhD
● Suryaram Gummuluru, PhD
● Frederick Ruberg, MD
The symposium was also open to all summer undergraduate students on campus and was attended by one Undergraduate Research Opportunities Program (UROP) scholar and one Summer Program in Neuroscience (SPIN) scholar. This year’s presenting UROP scholar was Sanjana Prudhvi, mentored by Manveen Sethi, PhD, and Joseph Zaia, PhD. The presenting SPIN scholar was Grace Li, mentored by Ella Zeldich, PhD.
Founded in 2010, the STaRS program promotes equitable access to graduate research and education for students historically underrepresented in science and medicine. Every summer, STaRS cohorts participate in faculty-mentored research informed by the scholars’ personal research interests.
Over the course of 10 weeks, scholars execute independent projects, participate in seminars on career development, research competencies and graduate school applications, and receive training on critical scientific communication skills. Ultimately, the program aims to enhance skillsets for application and entry to graduate or MD/PhD programs in biomedical sciences. Scholars receive a certificate recognizing their outstanding academic research achievements.
“Congratulations to this year’s STaRS scholars for a summer of successful research,” said STaRS Program Director Isabel Dominguez, PhD. “Thank you to all participating faculty mentors, personnel, and staff for your commitment and support of the STaRS scholars. It has been a pleasure and a privilege to see the scholars grow their research and communication skills and be empowered to follow a research career path.” ●
Like most high school students entering senior year, Dorchester’s Sabrin Warsame, who attends the John D. O’Bryant School of Mathematics and Science in Roxbury, is contemplating her future.
“I’m still trying to understand what I want to do, but I know I do want to go into medicine and healthcare,” she says.
Warsame, who is considering nursing and biochemistry as career options, was one of six O’Bryant students selected for the Summer Biomedical Research Internship at the Chobanian & Avedisian School of Medicine, a new six-week program implemented by the department of medical sciences & education with funding from the Burroughs Wellcome Fund. Another 24 students from the Boston Public Schools (BPS) are enrolled in the two-week Med-Science Program (MSP) with support from Boston-based Vertex Pharmaceuticals.
High school outreach programs introduce underrepresented youth from Boston and other communities to post-secondary STEM-M (Science, Technology, Engineering, Mathematics, and Medicine) with the overall mission of diversifying the biomedical research and healthcare workforce.
“I can tell you that getting a degree in science is one of the best ways to stay employed going forward,” Chobanian & Avedisian School of Medicine Dean and Medical Campus Provost Karen Antman, MD, told the high school students at a welcoming reception in July, pointing out that growth industries include taking care of patients and doing research that leads to better care.
Burroughs Wellcome originally approached the school with the idea of creating a biomedical research pipeline program for students considered as underrepresented in medicine (URM). Unlike other medical professions, biomedical research lacks high visibility—especially among students who, like Warsame, will be the first in their family to attend college.
“One of the reasons there are very few URM students in biomedical research is that very few know about it,” says Hee-Young Park, PhD, professor and chair of medical sciences & education and associate dean for faculty affairs. “We want to reach out to younger students so that they begin to appreciate and identify themselves as physicians, biomedical researchers, physician assistants, or genetic counselors.”
High school outreach programs introduce underrepresented youth from Boston and other communities to postsecondary STEM-M (Science, Technology, Engineering, Mathematics, and Medicine) with the overall mission of diversifying the biomedical research and healthcare workforce.
According to their interests, research interns are assigned to individual labs in the department of pathology & laboratory medicine. Supervised by a faculty researcher and working alongside graduate students and postdoctoral researchers, they experience the life of a biomedical scientist while also taking classes in professional development, leadership, and the college application process. Every intern completes an independent research project and makes an oral presentation at the end of the program.
Open to all BPS students, MSP is held in person for two weeks in the summer, with virtual programming on Saturday mornings during the school year. Last summer, the sessions were led by medical and graduate students focused on genetic counseling, neuroanatomy, clinical applications of anatomy and pathophysiology, surgery, anesthesiology, and sports medicine.
O’Bryant senior Aleeza Gavin of Roslindale said that while the six weeks she spent as a research intern cut into her summer, “I feel like this pertains more to my future than having a couple of months of fun.”
Recognizing that BPS students frequently must work to help support their families, MSP students receive a $750 stipend. Research interns receive $450 per week. All students are issued free MBTA passes
“The students who come to us are motivated, trying to fit a job and their aspirations for the future into their summer,” says Maura Kelley, MD, an assistant professor in the department of medical sciences & education and director of the high school programs.
This hands-on approach comes at a pivotal moment in a high school student’s educational life, as they are deciding about college and a path that could potentially lead to a career.
“I’m already intrigued by the medical field and just wanted to look at more career options, like surgery, that I feel this [Med-Science] program will help me look into,” says Danial Kahn of Brighton, an O’Bryant junior.
Kelley stresses that most BPS students must depend on their own initiative and skills to navigate the daunting college application process, and that a new pilot program offering mentorship will help these students on that vital next step.
Adds Park, “We are making an investment in the future.” ●


Members of the Physician Assistant (PA) Class of 2026 officially marked their entry into the professional study and practice of medicine at the White Coat Ceremony on August 1.
The cohort’s 20 students make up the 10th class of the Chobanian & Avedisian School of Medicine PA program, which graduated its first students in 2016. Since then, the program has graduated more than 200 students.
During the ceremony, students were addressed by PA Program Director Susan White, MD, and Graduate Medical Sciences Assistant Dean of Master’s Programs Theresa Davies, PhD. Robert Lowe, MD, associate professor of medicine/gastroenterology, delivered the keynote address.
“Congratulations as you receive your white
coats,” Davies said. “It’s amazing, and you should be very proud. Congratulations as well to your parents, who have supported you to this point. You should be so proud as well. You have incredible faculty serving you, and you have bright futures. We will be celebrating you and your program all year.”
Davies encouraged the class to “explore Boston, be a student, grow and learn.”
Lowe described the White Coat Ceremony as the start of a great journey and an invitation to work hard. “Nothing worthwhile is easy,” he said. “The program is tough. When you’re done, it’s still tough. But you’re going to step up and do it.”
Lowe told the students that ultimately, the white coat is a symbol. “You will be the person to help when needed,” he said. “On the days you’re not wearing [the white coat],

you’ll still be the person to step forward.” He pointed out that the new cohort will have the opportunity to work with talented colleagues and “gain a perspective on life that many people don’t have.”
“The things we do are incredible, and an incredible privilege,” he concluded.
Following the keynote speech, PA faculty members coated each student individually. Associate Director of Clinical Education Michael Smith, MS, PA-C, read out every name. Students were coated by Dan Tzizik, MPAA, MPH, PA-C, and Robert O’Brien, MHS, PA-C, associate directors of didactic education for the program.
Once all the students were coated, they recited the Physician Assistant Professional Oath. Led by Class of 2024 President Elise McIntosh, PA-S, the oath summarizes the professional and ethical responsibilities of the physician assistant.
“Congratulations on taking your first step to joining the PA profession,” White said. “You are our 10th class, and this is a wonderful milestone for us. We are very happy to have you here and look forward to getting to know you.” ●

In a tradition marking the entrance of first-year medical students into the medical profession, students, their families, friends, faculty, and staff gathered under a tent on Talbot Green for the annual White Coat Ceremony on August 1.
Kristen Goodell, MD, associate dean for admissions, presented the 146 members of the 175th entering class of the Chobanian & Avedisian School of Medicine.
“You should know that our shared intention is for you to reach your goals so that you can set about making the world a better place,” said Goodell.
Organized by Student Affairs, the White Coat Ceremony is a symbolic rite of passage grounded in the reality of hard work and responsibility. Associate Dean for Student Affairs Angela Jackson, MD, told students that their white coats represented “visible evidence that you are joining this profession, taking your first steps along this path to a demanding, but so rewarding, career in medicine.”
Because passing along knowledge from one generation to the next is at the heart of medical education, the focal point of the ceremony is the actual coating, when the faculty adviser assigned to each student for the next four years helps them into their white coat.
“When you put on your white coat for the first time today, the message is that, as of today, you are now already a part of the profession,” said BUMC Provost and Chobanian & Avedisian School of Medicine Dean Karen Antman, MD
The class was chosen from more than 10,600 applicants from 30 states, representing 65 undergraduate colleges and universities. Ranging in age from 20 to 34 years old, the entering class speaks 22 different languages—with 86% speaking more than one—and 17% are from groups underrepresented in medicine.
“In cultural, social, economic, racial, ethnic, gender identity, educational and linguistic terms, and in your life experiences, you define the pluralism that we so value on this campus and which is so central to our society,” said Goodell.
Putting on the white coat embroidered with his name was an emotional moment for Nnaemeka Nwoke, who wiped away tears as he walked back to his seat.
“I’m still processing that this is a reality,” he said. “To have gone through all the nitty-gritty details and overcome all the challenges and obstacles and persevered, this literally means the world to me.”
Originally from Nigeria, Nwoke wanted to become a physician since age 10. He moved to Tampa, Florida, in 2014 to attend the University of South Florida (USF), graduated in 2018, and worked at USF’s medical school and a private neurology practice before gaining admission to BU
“One of the things that stood out was that BU is truly focused on teaching us how to care for people of all walks of life regardless of race, gender, sexual orientation, or socioeconomic status,” he said.
Guest speaker and Massachusetts Secretary of Health and Human Services Kate Walsh, MPH, the former president and CEO of Boston Medical Center (BMC) Health System, championed that view of health equity.
“We have a mandate to use our privilege to change and improve our healthcare system,” said Walsh. “We need this entire generation of doctors to go beyond the traditional boundaries of medicine to create a healthier, more equitable world.”
Walsh urged the new medical students to do the research that cures disease and alleviates suffering, to engage and eliminate disparities in health outcomes due to race and ethnicity, and to understand and address factors that cause poor health.
Ekta Karkala from Union City, California, was drawn to the school and BMC, its primary teaching affiliate, due to their shared social mission.
“We provide for a lot of underprivileged and underserved communities, and I think that’s a really beautiful mission and I’m really grateful to be a part of it,” she said.
Goodell discussed the varied and often difficult paths students had traveled, especially given the COVID-19 pandemic that shut down research labs and other traditional avenues while making the remaining healthcare opportunities more dangerous.


Andrew Pendergrass graduated from the University of Washington in 2017, then worked as a nursing assistant at a safety-net medical center in Seattle during the pandemic.
“It was a bad time to be in the hospital,” he said. “The fact that I was still getting energy from going to work, getting a lot of fulfillment from doing it, and was enjoying being around patients despite the conditions was something that gave me confidence in moving forward.” ●
Professor of Medicine Gustavo Mostoslavsky, MD, PhD, recalled fellow Argentinian scientist and Nobel Prize winner César Milstein telling him that as a young scientist you are presented with a ball full of knots and that you keep untying them, one knot at a time, and, maybe, 20 years later you might have a major discovery.
In the decade since the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center (BMC) was established by cofounders Mostoslavsky, Professor of Medicine Darrell Kotton, MD, and Associate Professor of Medicine George Murphy, PhD, there has been a lot of untying of knots on some of the world’s most intractable diseases.
“We have a slogan that reflects our mission, ‘Advancing Science to Heal the World,’” says Kotton. “And we’ve tried to pursue that in the most selfless way possible.”
Regenerative medicine uses stem cells and the body’s natural healing process to replace or rebuild damaged tissues and organs. Until Japanese scientist Shinya Yamanaka, MD , PhD, discovered a way to make induced pluripotent stem cells ( iPSCs ) from mouse fibroblasts in 2006 and then from human fibroblasts in 2007 , research had been restricted by political and ethical debates over using pluripotent stem cells from human embryos. iPSCs are cells engineered from adults that are nearly identical to embryonic stem cells ( ESCs ). Once engineered in the laboratory
in the undifferentiated state, like ESCs , iPSCs are pluripotent, meaning they have many potentials. Differentiated iPSCs can be used to build specific tissues and organs, mimicking the embryonic tissue-building process.
“The stem cell field really took off with the discovery of reprogramming; of how to generate these pluripotent stem cells from anyone, especially patients,” says Kotton.
CReM first launched in 2008 as a virtual center with a seminar series and website. Within a few years, Kotton, Mostoslavsky, and Murphy were able to gain the support of Kate Walsh, then president and CEO of BMC, former BU President Robert Brown, medical school Dean Karen Antman, MD, and David Coleman, MD, then chief and chair of the department of medicine and now professor emeritus of medicine. The virtual center was also supported by Katya Ravid, PhD, when the group received the inaugural Affinity Research Collaborative (ARC) award from Ravid’s then-new Evans Center for Interdisciplinary Biomedical Research.
With support from BU and BMC, the CReM
opened its physical doors in 2013. Since then, its lab space has grown from around 7,000 to 16,000 square feet, from one culture room to five, and from 25 researchers in six labs to 66 in nine. The group’s high-impact publications have resulted in yearly accolades from a variety of campus and national organizations and an impressive 300% growth in grant dollars.
Kotton separates the CReM’s progress over the past decade into three phases. In the early years, the center made significant strides in reprogramming cells from patients, making iPSCs that duplicate cells or tissues needed for damage repair. In the middle years, there were remarkable advances in using those stem cells to discover how tissues are encoded and differentiate to become specific organs and other parts of the body. More recently, research advanced the science of engraftment, the transplanting of these engineered cells and organoids into damaged organs in animal models, successfully regenerating a variety of injured tissues.
“The transplanted cells rescue organ function, and they survive, in some cases, for the lifetime of the recipient,” says Kotton.
The next phase is to move testing into larger animals and then into human clinical trials, with the goal of creating gene therapies using stem cells.
“I think anybody around the world would recognize that the CReM has made contributions in those three areas: reprogramming technology to make stem cells; directed differentiation to make really advanced organoids and cell types; and progress towards cell and gene-based therapies,” says Kotton.
As a virtual center, one of the CReM’s first discoveries was publication of a new reprogramming approach led by Mostoslavsky, which earned him the “BU Innovator of the Year” award in 2017 iPSC generation was a time-consuming and expensive process until Mostoslavsky developed a tool called STEMCCA that made it simpler and more efficient. BU patented the tool, which was freely shared and used in over 1,000 labs worldwide.
“In the last 10 years, we have become much, much better at making cells that are closer to what they are supposed to look
like,” says Mostoslavsky, who looks forward to future advancements in cell and tissue manufacturing that will enable them to build whole, functioning organs.
“I think anybody around the world would recognize that the CReM has made contributions in those three areas: reprogramming technology to make stem cells; directed differentiation to make really advanced organoids and cell types; and progress towards cell and gene-based therapies,” says Kotton.
“Many famous centers have big discoveries, but I think, in addition to the scientific discoveries, what is unique about the CReM is the track record of selfless sharing,” says Kotton, who was the inaugural recipient of the AAMC’s National Research Resource Sharing Award (2017) in recognition of the CReM’s record of sharing their stem cells.

Kotton, Mostoslavsky, and Murphy came to BU for its culture of collaborative research. They decided from the outset that the center would follow the opensource sharing model that had emerged in computer code-writing culture. They created biobanks that housed stem cells and organoids and made them freely available upon request. Their efforts resulted in one of the largest repositories of iPSC samples for various diseases in the world.
“It’s 100% that people know us and recognize us as the guys who collaborate and share,”
says Mostoslavsky. This also was something that the world came to realize as an important principle in the desperate race to develop tests and find vaccines to fight the COVID-19 pandemic.
“There was a lot of cultural dogma at the time [CReM was founded] that you have to protect your research until you publish because you are in competition with others and are going to get scooped,” explains Kotton. “The collaborative approach is more efficient and faster, with shared research across the globe. For us, it’s been an even more positive and productive experience than we planned at the beginning.”
Today, the CReM includes nine principal investigators covering different aspects of developmental biology, stem cell biology, and regenerative medicine. Associate Professor of Medicine Andrew Wilson, MD, who was recently named scientific director of the Alpha-1 Foundation, runs both a research program in the CReM and an internationally recognized clinical center at BMC focused on caring for patients affected by alpha-1 antitrypsin deficiency, the most common genetic cause of chronic obstructive pulmonary disease. Assistant Professor of Medicine Finn Hawkins, MBBCh, uses iPSCs to develop new therapies for genetic airway diseases, such as cystic fibrosis.
CReM cofounder Murphy, who originally established studies in the field of sickle cell anemia, is now part of a team studying supercentenarians and understanding aging and extreme longevity. Valerie Gouon-Evans, PhD, MS, PharmD, directs the BU Liver Biology Program focused on developing approaches for liver regeneration. Angie Serrano, PhD, assistant professor of medicine, joined the CReM in 2022, studying iPSCs and how various mutations impact cell fates in a variety of diseases.
The two newest additions, Kim Vanuytsel, PhD, MS, and Kostas Alysandratos, MD, PhD, research treatments for sickle cell disease and interstitial lung diseases, respectively. Along with Mostoslavsky, who works on understanding neurodegeneration, intestinal organoids, and T cells, and Kotton, who studies lung injury and repair, they lead the nine research programs of this multidisciplinary center, advancing the field of stem cell biology and regenerative medicine. ●

Andrew Henderson, PhD, has spent the last 16 years at the Chobanian & Avedisian School of Medicine, during which time he has performed groundbreaking research and been a part of developing two innovative PhD-training pathway programs in Graduate Medical Sciences (GMS).
Henderson, a professor of medicine/infectious diseases and virology, immunology & microbiology, also serves as assistant dean of research for Graduate Medical Sciences.
He completed his PhD training at the University of California, Riverside, before accepting a postdoctoral fellowship at Columbia University, where he embarked on what would eventually become a career in researching human immunodeficiency virus (HIV).
“I was really interested in questions of how genes get expressed in different cell types in the context of the immune response,” he says. “Since HIV targeted the immune system, it became an important question to understand how it was expressed in the different immune cells.”
Following his fellowship at Columbia, Henderson took a position at Penn State, where he remained for 10 years. In 2007, he accepted an associate professorship at Boston University, joining the Medical Campus as an established, mid-career investigator.
Drawing on his background in immunology and his goal of understanding how the immune system develops, Henderson’s lab focuses on several projects related to the cellular mechanisms that regulate HIV replication and transcription.
“One of the nice things about doing research in an academic environment is that you can explore, shift, and do things that sometimes will change the direction of your research interests,” he says.
Eager to combine his research with his role as a GMS educator, Henderson worked with former Associate Provost and GMS Dean Linda Hyman, PhD, to establish the yearlong Post-baccalaureate Research Education Program (BU PREP), now in its fifth year.
Supported by a grant from the National Institute of General Medical Sciences, BU PREP is designed as a pathway for recent bachelor’s degree recipients seeking entry into competitive PhD training programs.
According to Henderson, by facilitating the process, the program inspires recent bachelor’s degree graduates to consider PhD training and other long-term careers in science. It aims to create more diversity in STEM by appealing to research-motivated students who are historically underrepresented in scientific fields.
“We’re closing that gap a little bit, but we need to do a better job in science and attracting underrepresented groups to the STEM fields,” Henderson says.
The program matches each student with a lab at the medical school, where they will work throughout the year on a variety of research projects. Students can also audit courses, join journal clubs, and attend professional development and other seminars featuring prominent STEM professionals.
“There are lots of opportunities where you can be a leader in the field, whether it’s being a professor at an academic institution, leading a group at a biotech company, or directing policy and education,” Henderson says. “So, we try to expose BU PREP students to that as well.”
The program also offers mentorship throughout the PhD application process including assistance with recommendation letters, personal statements, and career development. With the support of the NIH-funded Providence/Boston Center for AIDS Research (CFAR), where Henderson serves as an associate director, participants also network with students at other PREP programs throughout New England.
“Obviously, the lab experiences are super positive and can really transform somebody’s perspective of science and future careers,” Henderson says. “However, I think the mentorship and the engagement with students is something that we do really well.”
Every student who has completed BU PREP is still in science, whether in a PhD program, at a biotech firm, or in the process of graduate or medical school applications.
“I feel like we’ve supported people through this process,” Henderson says. “I would hope everybody comes out of BU PREP feeling like they’ve gained from this experience.”
Supported by a grant from the National Institute of General Medical Sciences, BU PREP is designed as a pathway for recent bachelor’s degree recipients seeking entry into competitive PhD training programs.
Capacity Building and Partnership with the University of Liberia
Henderson’s mentorship roles also include his participation in the Boston University and University of Liberia Emerging and Epidemic Virus Research (BULEEVR) program, which is supported by the NIH Fogarty International Center.
A collaborative effort of BU, the University of Liberia, and several other stakeholders, BULEEVR creates a training program that supports Liberian scholars in their journey to pursue PhD training in biomedical sciences and public health.
Henderson leads the BULEEVR program
alongside BU School of Public Health Chair and Professor of Global Health Patricia Hibberd, MD, PhD; Director of the BU Center for Emerging Infectious Diseases (CEID) and Associate Professor of Medicine Nahid Bhadelia, MD, MA; Refuge Place International President and CEO Mosoka Fallah, PhD, MPH, MA; and Vice President of University of Liberia College of Health Sciences Bernice Dahn, MD, MPH
Now entering its sixth year, the program was founded in the wake of the 2014–2016 Ebola outbreak in West Africa, when Bhadelia and Fallah began to consider programs focused on research, clinical care, and sustainable STEM training in Liberia.
“There was a realization about the need for sustainable research and education programs as well as larger questions around equity, and the need for investment in places such as West Africa, where emerging infectious diseases are having an impact every day,” Henderson says.
The program offers individual mentorship to trainees by building their foundational scientific knowledge, assisting with their research papers and application processes, and guiding them toward competitive PhD programs.
BULEEVR currently has six trainees: four in PhD programs across the United States and two in the epidemiology PhD program at BU School of Public Health. A past trainee recently received his MS from the GMS program in Clinical Research.
Ultimately, according to Henderson, the program’s long-term goals are rooted in sustainable educational programs and research projects. The BULEEVR team actively engages with Liberian stakeholders and aims for program trainees to eventually train the next generation of scientists in-country.
“I would hope that by the end of the next five years, we’re training people in Liberia, doing collaborative research in Liberia, and our trainees are getting PhDs from the University of Liberia,” Henderson says.
Whether in his lab, mentoring traditional PhD students, or working with trainees in the BU PREP and BULEEVR programs, Henderson enjoys seeing the professional maturation process of new scientists who are excited about their work and grow alongside their projects.
“I think sometimes we get kind of rigid in thinking about our careers and our progression and we forget to enjoy and embrace the process,” he says. “Science can be really fun.” ●

In 1948, the first of 15,000 volunteer participants entered the research center of the historic Framingham Heart Study (FHS) to have their vitals taken and other tests performed that would provide scientists with the data they needed to fight heart disease and cardiovascular-related conditions like stroke and Alzheimer’s disease.
The last person in the first cohort of over 5,000 volunteers who signed on in 1948 passed away at the age of 105 last year, but study participation is a tradition that has been passed down through generations of families over time, and many descendants of the original group continue to take part in the study. On Wednesday, October 25, nearly 300 participants and their guests visited the research center, taking tours covering eight distinct research areas. Twenty principal investigators in research teams joined
together to cover common themes like neurology and cardiology.
Over 40 research staff and volunteers were on hand to help as participants conversed both with researchers whose work they’d profoundly influenced and with current and former staff members who had known them for years and in many cases, decades.
Appreciation went both ways.
“My mother, my brother, my aunts, my first cousins,” said Joanne Barber, 74, ticking off the generations of her family that have participated in the study from 1948 to today.
“I’m just honored to be a part of it, with my father, my grandfather, and my seven brothers,” said John Villa, 69, who has lived in Framingham his entire life. “I think it’s great to help to find cures for all our ailments. The big ones. Nice to be a part of giving back to society.”
Continued from previous page
According to George O’Connor, MD, the study’s interim codirector, the generational record of participation for 75 years is unique in medical research. A professor of medicine at the Chobanian & Avedisian School of Medicine, which oversees the study, O’Connor has been a principal investigator at FHS for 31 years. He pointed out that the loyalty of participants over such a long period of time has created unforeseen research options. “It gives you a wealth of opportunities,” he said. “It’s just a remarkable achievement.”
Along with the clinical data on health conditions, researchers also obtain longitudinal measures of pulmonary function, electrocardiograms, blood lipids, genetics, and other data that deepen the understanding of what is going on in the human body over time and generations.
Ruby Bishop and Anita Beckett were among the first Black participants as the study broadened its base from exclusively white European families to include Black, Hispanic, and Asian American families in the 1990s
“I thought it would be a good thing,” said Bishop. “There are little nuances brought on by our genetic makeup and our environment.”
“I really wanted to be in on the celebration,” said Donna Boundy, 73, who drove over three hours from her home in Woodstock, New York, to attend, as she has done every three years for most of her life as a participant. Her mother and father were in the original cohort.
“I have no idea what study they’re using (my information) for,” Boundy said. “I do it because it meant a lot to my father. It meant a lot to them; they were proud of it.”
Researchers also traveled long distances to attend the celebration. Neurologist Sudha Seshadri, MD, a senior FHS investigator and founding director of the University of Texas San Antonio Glenn Biggs Institute for Alzheimer’s & Neurodegenerative Diseases, came from San Antonio with her husband Vasan Ramachandran, MD, the former longtime FHS director and now founding dean of the University of Texas School of Public Health at San Antonio. For most of the day, they explained to participants how their data was being used in research.
“I had to be here. It’s now 30 years since I started working with the heart study,” said Seshadri. “This is my life’s work, just as it is for participants.” ●
Last October, a ribbon-cutting ceremony in Lesotho, a small mountainous country in southern Africa, marked the successful construction of the country’s first postgraduate medical training facility. Located in Leribe, the facility was a collaborative project through an ongoing partnership with the Chobanian & Avedisian School of Medicine and the Lesotho Ministry of Health (MOH) known as the Lesotho Boston Health Alliance (LeBoHA).
As reflected in remarks by Lesotho Minister of Health Selibe Mochoboroane, Deputy Prime Minister Nthomeng Majara, and US Ambassador Maria Brewer, the occasion was also an opportunity to recognize more than 20 years of work by Boston University and the government of Lesotho, highlighted by nearly 200 new doctors returning to their native country to practice medicine and receive internships and specialty training. The country’s first medical school is now a government priority.
“This is not just a physical structure, but a symbol of our shared commitment to the health and well-being of the people of Lesotho,” Brewer said at the ribbon-cutting ceremony.
Recognizing its achievements in strengthening Lesotho’s healthcare system, the United Nations Interagency Task Force/ World Health Organization 2022 Special Programme on Primary Health Care Award was presented to LeBoHA before the UN General Assembly.
With a diverse population of nearly 12,000 international students representing over 145 countries, Boston University has a long history of international involvement and service with over 300 teaching, research, and service activities on all seven continents. BU ran a health program in West Africa in the 1970s and worked with Egypt through the 1980s to develop a medical school and family medicine residency training program. The schools of medicine and public health conduct worldwide service delivery, operations, and policy research programs.


BU has been involved with Lesotho since 1990, particularly through the work of the late William Bicknell, MD, founder and chair emeritus of the BU School of Public Health department of global health and professor and director of international health programs in the department of family medicine at the medical school, and Brian Jack, MD, professor and former chair of family medicine.
The celebration in Leribe was the culmination of a conversation between Bicknell and Jack decades ago.
Bicknell, who passed away in 2012, had traveled to 62 countries over a five-decade career of improving public health. Jack recently recalled the two discussing how the international projects they’d been involved in during their careers often didn’t last beyond the few years they were supported by grants.
“It’s not even a net neutral; it’s often a negative, because nothing sticks,” said Bicknell at the time. The two men talked about taking a new approach—getting to know a country first by talking to the people and government officials, then carrying out the work the locals had identified as sustainable priorities.
Bicknell and other BU faculty had long-standing relationships in the country, and Lesotho certainly needed the help. After South Africa ended the use of foreign workers in their mines, 300,000 men returned to a Lesotho dominated by subsistence farming as its main source of income, with nearly half the population earning below the poverty line. The tuberculosis infection rate was the second highest in the world; the maternal death rate per live births the second highest in the region
and nearly 20 times that of the US. But what really threatened the country’s future was the HIV/AIDS epidemic, with nearly a quarter of the population infected and national life expectancy reduced to 36 years.
This was a country desperately in need of physicians, but in the early 2000s Lesotho’s doctor-to-patient ratio, one physician per 20,000 people, was a third that of Africa’s national average. By comparison, the World Health Organization estimates that 2.5 medical staff—including physicians, nurses, and midwives—per 1,000 people is the minimum needed for adequate healthcare.
At the root of the problem was a “brain drain.” The government paid for 10 to 20 of their brightest students to attend medical school abroad each year, usually in neighboring South Africa. But few of those students returned to their home country, and those who did were generally assigned to remote mountainous areas where they encountered a wide range of medical issues for which they weren’t prepared, with little or nonexistent support systems, poor pay and living conditions, and lack of opportunities for teaching, research, and career growth.
As a result, explained LeBoHA Executive Director Elizabeth Nkholongo, many of her country’s doctors were from the Democratic Republic of the Congo or Cuba, and couldn’t speak English or the primary language of the Basotho people, Sosotho.
“It was just challenging for us. The local people could not easily access healthcare services because they could not communicate with the doctors,” she said.
But the country did have a stable transparent democracy and a healthcare infrastructure with a national hospital, district hospitals, and health centers. And there was a core group of idealistic Basotho physicians who wanted to come home to take care of their country, their villages, their elders, and their communities in this time of crisis.
In 2002, the Minister of Health and Social Welfare indicated the government was interested in working with BU. In 2003, then-BU President John Silber agreed to a long-term institutional commitment to Lesotho.
Over the past two decades, LeBoHA, supported by other funders like the Dreyfus Health Foundation and the W.K. Kellogg Foundation, worked with the government to stop the exodus of young doctors and to build up in-country training, facilities, and support. They formed a medical students association in 2007, initiated Lesotho’s first physician training program in 2008—a fouryear postgraduate specialty training program in family medicine—and created the first competency-based nursing and midwifery in-service training program in 2009.
In 2015, the physician training program was the first in the country’s history to gain accreditation. In 2019, the Ministry of Health required all students finishing medical school abroad to return home for internship training, and because of their successful Family Medicine Specialty Training Program (FMSTP), the MOH looked to LeBoHA to run that program as well.
BU supports the education of those who commit to stay in Lesotho with a $1.5 million endowment from the late BU School of Public Health Professor Rex Fendall and his wife Doreen, who left their estate to support health workers from Lower Middle Income Countries (LMIC) who are committed to returning to their native countries to further their education.
Lesotho physicians who return and graduate from the FMSTP are still assigned to rural districts, but now they have more robust support systems and work together in teams. They also hold management positions and participate in continuing education that includes regular professional meetings, training updates, teaching positions, and opportunities to do research and publish articles. Their advanced training in the clinical conditions facing the country and further
Continued from previous page
training in improving the quality of care, community-oriented care, and district health management give them the skills and confidence crucial to providing needed services in the districts. With these skills, graduates now are in 7 of the 10 districts in Lesotho and, to date, none of the FMSTP postgrads have left the country.
“The people who are actually leading the work on the ground in Lesotho are people who have been trained [in the LeBoHA program],” said Stephen Wilson, MD, MPH, FAAFP, chair of the department of family medicine and chief of family medicine at Boston Medical Center (BMC). Wilson’s department oversees the LeBoHA program.
With funding from the United States Agency for International Development Schools and Hospitals Abroad program, LeBoHA supported the construction of the Postgraduate Medical Campus that now includes an academic center, library, administration building, and student housing. One structure, the Bill Bicknell Academic Center, was built with funds raised by LeBoHA and the nonprofit Global Primary Care.
According to Jack, the success of LeBoHA’s FMSTP offered proof that other medical education programs could sustain themselves beyond grant funding. The government now pays the salaries of the returning doctors and the faculty, plus the cost of the training programs. Jack and Minister of Health Mochoboroane said the country has prioritized building its first medical school, possibly within the next five years.
“We have addressed the brain drain issues to encourage people to come back home,” said Jack. “Our claim to fame now is that there are more doctors in the LeBoHA training programs than there were in the country in 2005.” To date, 24 specialists and 170 interns have returned from abroad for postgraduate training, with 90% staying.
Success breeds success.
“Because this program has been successful at producing good physicians, the government is asking us to help them model specialty training in other areas,” said Wilson, who traveled to Lesotho for the first time in 2023 and attended the ribbon-cutting ceremony. “I would say that’s a significant marker of sustainability, when you start

to build on, and add programs on, to what you’re already doing.”
Over the past decades, BU faculty and students and BMC physicians and residents have made the trip to help in Lesotho.
The LeBoHA program drew Stephen Christiansen, MD, professor and chair of ophthalmology at the school and chief of ophthalmology at BMC, who for years had been trying without success to find a site in Rwanda, Zimbabwe, or another western African country to establish an eye clinic and surgery suite.
In Lesotho, he found a mature program with government support and encountered tremendous need, with just one ophthalmologist in a country where cataract blindness afflicts 30,000 new patients each year.
“Consider the enormous burden it is to have a substantial part of your population blind as a consequence of a preventable blindness,” said Christiansen. His program started an initiative to train district nurses to do both eye exams and surgery. “To be able to train a nurse and put them in a district hospital with equipment and support would be really terrific, and a substantial way of improving cataract blindness.”
While the nurses receive most of their training through a two-year program in Gambia, they’re also trained by specialists from BU and BMC who treat patients in Lesotho, with all involved benefiting from the experience.
“As a chair, I want to open my residents’ and trainees’ eyes to what the needs are in the developing world, to how people can be helped with even modest interventions,” Christiansen said.
David Henderson, MD, professor and
chair of psychiatry and psychiatrist in chief at BMC, has worked in many resource-limited countries evaluating mental health needs and setting up training. When he came to Lesotho a few years ago there were no psychiatrists, so his department sponsored a PhD-level fellow over the past two years to lay the groundwork for a training program.
Henderson stressed that participating in overseas programs makes residents and trainees better physicians. “You have to figure out how to be useful, how you treat this illness without an MRI or fancy tests. How do you treat it with the tools that you have,” he said.
At the Lesotho medical campus last October, Professor of Dermatology Jag Bhawan, MBBS, worked on solutions to a critical shortage of dermatologists and pathologists and was impressed by the energy and commitment of the Basotho (the people of Lesotho) physicians and medical staff he met there.
“They are all local people who have graduated from the program, are now on the faculty, and are absolutely committed to improving healthcare there,” said Bhawan. “I met so many people who are trying very, very hard.”
According to Wilson, the nearly 20-year effort to build a healthcare system in Lesotho by going at the pace set by the people and government of Lesotho has paid off.
“By doing that, and having buy-in along the way, it’s really now cemented into the culture,” he said, recalling how the government officials and the communities interacted with Jack. “They were thanking him, not in a way that showed he was the boss, but in a way where they looked at him as a collaborative partner.” ●

Philipp Mews, PhD, assistant professor of physiology & biophysics, has received the 2023–2024 Peter Paul Career Development Professorship. Working to develop novel therapeutic strategies for treating neuropsychiatric disorders, including PTSD and substance abuse, Mews studies metabolic and epigenetic processes that underlie brain plasticity.
Boston University awards Career Development Professorships annually to talented junior faculty members who are emerging as future leaders in their fields. The Peter Paul Career Development Professorship is made possible by the generous support of University Advisory Board Member Peter Paul (Questrom’71).
Mews received his PhD in cell and molecular biology and a BS in molecular biology from the University of Pennsylvania, and a BS in biology from Freie Universität in Berlin, Germany. He completed his postdoctoral training at the Icahn School of Medicine at Mount Sinai in New York.

Jennifer Luebke, PhD, Waterhouse Professor and chair of anatomy & neurobiology since 2018, has announced
her intention to step down as chair of the department when her successor is named.
Luebke’s many roles at BU have included principal investigator of the Laboratory of Cellular Neurobiology since 1996, vice chair of anatomy & neurobiology, and director of the PhD and Vesalius Master’s Programs in anatomy & neurobiology. She has served as a member of the Executive Committee of the Boston University Faculty Council, including as chair of the Sustainability Committee, and chair of the Supply Chain & Waste Working Group of BU’s Climate Action Plan Taskforce. She also has served on BU’s Council Committee on Graduate Academic Programs and Policies and is currently on the medical school’s Faculty Appointment and Promotions Committee.
Luebke received her doctorate in anatomy & neurobiology from Boston University and completed postdoctoral training in neurophysiology at Harvard Medical School and Tufts University School of Medicine. She joined the faculty as an assistant professor of anatomy & neurobiology in 1996.
Her research focuses on how specific anatomical, physiological, and molecular features of neurons and neuropil in diverse cortical regions enable area-specific functionality, and how distinctive features may be associated with differential vulnerability in normal and pathological aging. Her work, continuously funded for more than 25 years, has identified region and species-specific characteristics of neurons and potential mechanisms underlying vulnerability of neurons in normal aging and in neurodegenerative disease.
During her tenure as chair, Luebke strengthened the department by recruiting outstanding new faculty researchers and educators, enhancing infrastructure, and supporting graduate and medical student training as well as faculty and staff careers, including healthy work environments. She leaves a legacy of collegiality, collaboration, and dedication to the highest standards in education, graduate training, and research.

Ronald Corley, PhD, professor and chair of microbiology since 1994, has announced his intention to step down as chair of virology, immunology & microbiology when his successor is named.
Corley has served in many roles at BU, including director of the National Emerging Infectious Diseases Laboratories (NEIDL) from 2014 to 2022; associate director of the NEIDL from 2007 to 2014; BUMC associate provost for research from 2009 to 2014; and chair ad interim of genetics & genomics from 2007 to 2008.
He worked tirelessly on a University-wide team to open the NEIDL, now an internationally recognized center of excellence for emerging infectious diseases, and the BU microbiology department was ranked 15th nationally in NIH funding among microbiology departments in 2022. Over the years, his dedication to training program development and strengthening important research areas— including RNA viral biology and pathogenesis—proved invaluable to the school.
Corley’s research focuses on the relationship between innate and adaptive immunity, and how components of those two discrete systems interact to generate long-lasting protective immune responses. He earned a BS in zoology and a PhD in microbiology and immunology from Duke University and did his postdoctoral work at the Institute for Immunology, Basel, Switzerland. Prior to joining BU, he served on the faculty at Duke University.
He is a member of many professional societies, including the American Association of Immunologists, the American Society for Microbiology, and the American Society for Microbiology and Immunology Chairs. In 2014, he was elected a
Continued from previous page
fellow of the American Association for the Advancement of Science.
Corley’s expertise and experience in faculty recruitment and team building fostered a deep sense of shared commitment among those he inspired and influenced throughout his years at the NEIDL, the Medical Campus, and the University.

Terence M. Keane, PhD, professor of psychiatry and clinical psychology and assistant dean for VA research at Chobanian & Avedisian School of Medicine, received the Lifetime Achievement Award from the Division of Trauma Psychology at the 2023 American Psychological Association (APA) meetings in August.
Keane was recognized for his contributions and leadership in science, clinical care, education, and advocacy in the field of psychological trauma and posttraumatic stress disorder (PTSD). He is widely credited with opening the field of psychological trauma to scientific inquiry.
Keane, who also serves as associate chief of staff for research and development at VA Boston Healthcare System and director of the National Center for Posttraumatic Stress Disorder’s Behavioral Science Division, is a national leader in the field of psychological trauma, having published more than 400 articles and book chapters on the assessment and treatment of PTSD. His current work revolves around constructing an internet-based treatment program to help war veterans with postdeployment behavioral health problems readjust to life outside of the military. Keane is the current president of the
American Psychological Foundation, a major funder of small grants for early career psychologists and graduate students. He is past president of organizations worldwide including the International Society for Traumatic Stress Studies, the Anxiety and Depression Association of America, the Society of Clinical Psychology, the Association of VA Psychology Leaders, and the Division of Trauma Psychology of the APA.
Keane is a fellow of the APA and the Association for Psychological Science. He has received numerous honors including the Lifetime Achievement Award and the Robert Laufer Award for Outstanding Scientific Achievement from the International Society for Traumatic Stress Studies, the Harold Hildreth Award for Contributions to Public Service from the APA, and two honorary doctorates in recognition of his contributions to the field of psychology.
Keane completed his predoctoral clinical internship at the University of Mississippi Medical Center/VA Jackson Consortium. He received his PhD in psychology from Binghamton University and his bachelor’s degree in psychology from the University of Rochester.
Wilson received his bachelor’s degree from Eastern Nazarene College in Quincy, Mass., and his medical and public health degrees from the University of Pittsburgh. He completed his internship and residency in family medicine and a faculty development fellowship at the University of Pittsburgh Medical Center (UPMC) St. Margaret Hospital in Pittsburgh.
Wilson has published more than 85 peer-reviewed publications and numerous book chapters, handbooks, and letters to the editor. He has served on the US Health Resources and Services Administration’s Advisory Committee on Training in Primary Care Medicine and Dentistry and on the Society of Teachers of Family Medicine in numerous positions, including board of directors’ president. Wilson is a member of the American Academy of Family Physicians, Society of Teachers of Family Medicine, Association of Family Medicine Residency Directors, and the National Medical Association.
Stephen

Stephen A. Wilson, MD, MPH, FAAFP, chair of the department of family medicine at Chobanian & Avedisian School of Medicine, has been elected to the board of directors of the American Board of Family Medicine. Wilson, who also is chief of family medicine at Boston Medical Center, will serve a fiveyear term.

Katya Ravid, DSc, has been elected a fellow of the American Heart Association by the Council on Basic Cardiovascular Sciences, one of the world’s preeminent organizations of cardiovascular and stroke professionals, “for excellence, innovative and sustained contributions in the areas of scholarship, practice and/or education, and volunteer service within the AHA/ASA.”
Ravid is the Barbara E. Corkey Professor of Medicine, a professor of biochemistry, biology, and health sciences at the school,
and a Fulbright Research Scholar. She is the founding and current director of the Evans Center for Interdisciplinary Biomedical Research and the BU Interdisciplinary Biomedical Research office.
Represented in more than 170 publications, Ravid’s research and contributions in the interdisciplinary field of hemato-vascular biology—with a focus on the megakaryocyte/platelet lineage—have been recognized nationally and worldwide. Her honors include an American Heart Association Established Investigator Award and a fellowship in the American Association for the Advancement of Science.

Frederick (Rick) Ruberg, MD, has been named section chief of cardiovascular medicine and Thomas Ryan Professor of Cardiology.
Since joining the faculty in 2005, Ruberg has built an outstanding cardiac imaging program with a focus on cardiac amyloid.
He received a bachelor’s degree in psychology and neuroscience from Haverford College and an MD from University of Pennsylvania School of Medicine, served a residency in internal medicine at Boston’s Brigham & Women’s Hospital, and completed fellowships in cardiovascular disease at Boston Medical Center and cardiovascular magnetic resonance imaging at Beth Israel Deaconess Medical Center in Boston.

Carl Streed, Jr., MD, assistant professor of medicine, has received a 40 Under 40 Public Health Catalyst Award 2023 from the Boston Congress of Public Health.
He is part of the second cohort that represents the next generation of leaders, entrepreneurs, researchers, scientists, activists, intellectual provocateurs, authors, and directors who inspire us all to strive for a more just and equitable world.
Research lead for the GenderCare Center at Boston Medical Center, Streed has chaired the American Medical Association Advisory Committee on LGBTQ Issues and served on the board of GLMA: Health Professionals Advancing LGBTQ Equality. He is currently president-elect of the US Professional Association for Transgender Health.

After more than 20 years of unflagging dedication to the Chobanian & Avedisian School of Medicine and Boston Medical Center community, Aviva Lee-Parritz, MD, has announced her retirement from her position as chair and chief of obstetrics & gynecology effective March 1, 2024.
Lee-Parritz began her career as a nurse with a deep passion to making a positive impact in the
life of every patient placed in her care. She eventually began training as a physician, committing her life to maternal health and reproductive justice. Through myriad clinical and administrative roles of increasing responsibility, she evolved her practice and became a staunch advocate for the right to choose to have a child and to raise families in safety, causes she has carried into her role as chair and chief of the department.
Among Lee-Parritz’s accomplishments was her role in encouraging faculty to implement programs focused on mitigating inequities in health outcomes such as Project Respect, a national model for the care of pregnant persons with substance use disorders; leading Equity in Pregnancy, the first clinical vertical in the Boston Medical Center Health System’s Health Equity Accelerator; and building a robust research portfolio. She also championed faculty-developed programs on eliminating racial inequities in sexual health, family planning, and treatment including for women with fibroids and gynecologic cancers.
In addition to her role as department chair, Lee-Parritz created and serves as inaugural Director of Equity, Vitality & Inclusion for the Boston University Medical Group. Established to integrate and amplify gender equity, racial equity, and professional vitality initiatives, the office has implemented foundational tools for culture transformation that have been recognized with the 2021 Gold Award by the American Medical Association Joy in Medicine Health System Recognition Program.
Lee-Parritz’s leadership style is anchored in a belief that every team member delivers immeasurable value, and she unfailingly encourages clinicians to bring their best to their work and deliver excellent care. She is committed to educating students and trainees, developing leaders, and helping clinicians contribute new and groundbreaking knowledge. Under her leadership, the department has grown significantly and consistently delivers impressive outcomes across clinical care, scholarship, and advocacy.
Going forward, Lee-Parritz will dedicate her time to initiatives that advance reproductive justice, antiracism, and human rights. ●

“
That was some of the excitement, for me, of going into general surgery—that I would be exposed to a breadth of things that I would be able to help treat.”
Dr. Kaitlin Peace
See page 26 for her full story.

for most physicians, the next step following residency is a position at a hospital or private practice in an urban or suburban area, sometimes paired with a career in academia. Only an estimated 11% of all physicians choose to work in rural areas, and as a result, the United States is approaching a crisis point in rural medicine. Many physicians are retiring or moving away, with diminishing replacements and a population whose health is decidedly worse in all the major benchmark diseases than populations in metropolitan areas.
USAF Maj. Kaitlin Peace, MD (CAMED’14), is stationed at a 25-bed military hospital in Anchorage, Alaska.BBoston University Chobanian & Avedisian School of Medicine alumni who serve in rural communities say that too few doctors have experienced the reality of healthcare work in nonmetropolitan settings, and they dispute the characterization of lower pay, longer hours, and a less challenging career path. They are convinced that the benefits of being part of a small community—living among those you serve and being appreciated for making the choice to play a vital role in their lives— outweigh the drawbacks.
“I think a lot of people think a rural practice means I’m living in the middle of nowhere for lower pay,” says Frederick Powell
(CAMED’11 , PhD’11). He points out that his pay as an anesthesiologist at Moultrie, Georgia’s Colquitt Regional Medical Center is better than what was being offered in larger, urban hospitals; the cost of living is lower, the hours are less taxing, and his commute is a relaxing, two-mile drive.
Powell also was pleasantly surprised by the level of community involvement made possible due to his increased free time. “Most of us are so busy in our medical practice that we do medicine, go home, wake up the next morning, and try to recharge,” he says. “But I’m on a variety of boards, and I meet with community leaders. People are appreciative that I choose to spend my time practicing medicine in their town, and they try to do their best to make sure that I recognize that it’s my town, too.”
Not everyone wants the fast pace and busy lifestyle of an urban physician. Alumni say they choose rural locations for a range of reasons, one of the most important being what drew many to BU as medical students in the first place—the sense of purpose that comes with directly addressing the disparities in healthcare for marginalized and medically underserved people.
The benefits of an improved work/life balance, easy access to nature and the outdoors, and sometimes, the financial incentives of better pay and a lower cost of living than what metropolitan practices or hospitals offer are also considerations.
“One of my goals going into medical school was to treat underserved populations,” says David Veltre (CAMED’13), an orthopedic surgeon at Southwestern Vermont Medical Center, a regional 99-bed hospital in Bennington with five operating rooms.
Family considerations weighed heavily when Veltre and his wife Julia Keosaian (SPH’11) decided he would accept his present position and live in the nearby college town of Williamstown in western Massachusetts.
“I took the job because we loved the area,” he says. “Just being in the proximity of the mountains, lakes, and parks, with outdoor activities like skiing and hiking so close by, has been wonderful for our family.”
“People come to rural areas because they want to have a good work/life balance,” he adds. “We all want to work hard, but we also
David Veltre, MD (CAMED’13), is an orthopedic surgeon at a regional 99-bed hospital in Bennington, Vermont.

realize that there are other important things in life.”
Veltre is the only hand surgeon in the lower third of Vermont, from New York State on the west to New Hampshire on the eastern boundary. He knows there is a shortage of primary care physicians and that long waiting periods to become a patient of a primary care practice leave many so discouraged that they stop seeking medical care for health problems that, ultimately, are much worse when treated at the hospital.
All but one of Vermont’s 14 counties have a federally designated Health Professional Shortage Area (HPSA) where there are insufficient providers—MDs, DOs, physician assistants, and advanced-practice RNs—to care for the population. The HPSA designation allows providers working in those areas, as well as Federally Qualified Health Centers and Rural Health Clinics, to access benefits and incentives such as bonus payments for Medicare services, National Health Service Corps (NHSC), the State Loan Repayment Program (SLRP), and the J-1 Visa waiver program.
“One of my goals going into medical school was to treat underserved populations.”
Dr. David Veltre
With fewer people, one would expect scaled-back services, but the difference is starkly disproportionate when it comes to healthcare. According to the Health Resources and Services Administration, there are just 13.1 providers per 10,000 people in nonmetropolitan areas, and 31.23 per 10,000 in metropolitan areas. For specialists, the disparity is much more pronounced, with 30 per 100,000 people in rural communities as compared to 263 per 100,000 people in metropolitan areas.
“I think our hospital does the best they can, but for specialized care, people are travelling long distances,” says Emily Nelson (CAMED’14). Nelson lives with her husband Ben (CAMED’16) and their two children in the woods of Camden in rural midcoastal Maine, “where the mountains meet the sea.” Like Veltre, the Nelsons wanted to find a better work/life balance.
“I’m a little too laid back for the city and academia,” says Emily. “It’s really a wonderful place to raise a family. Very idyllic. The kids spend summers swimming the lakes. The shoulder season we hike; the winter we ski.”
“We are not rural heroes. Thanks to our degrees from Boston University, we are able to
“
You’re at the mercy of who the hospital has been able to hire and what those doctors are comfortable treating.”
Dr. Emily Nelson

live in a spectacular part of the world and have consistent, meaningful work,” she adds.
Even in such an idyllic setting, healthcare challenges exist. The US is still a profoundly rural nation, with nearly 81% of the population living in urban areas that take up only 3% of the country’s land area; the remaining 20% occupies 97% of the land. Nonmetropolitan areas have higher rates of death from cancer, heart disease, and other major causes, yet have one-third the number of physicians per 100,000 compared to metropolitan areas. Coincidentally, nearly 62% of HPSA s in the US are in rural areas.
Emily Nelson is a physical medicine and rehabilitation specialist helping patients with stroke, spinal cord injury, and neurological conditions reach their functional goals at a clinic in Rockport, Maine, a town with a population under 4,000. Primary care in her area is difficult to access, and it’s hard to recruit and retain specialists, nurses, medical technicians, and other staff.
“I’m a one-woman show, really,” she says. “It’s a bit of a struggle to do the things I do. I see things in a much more unmanaged state than you do in Boston.”
Since the availability of specialists varies depending on who the hospital has been able to recruit, Emily occasionally reaches out to the BU alumni network for medical specialty advice.
“You’re at the mercy of who the hospital has been able to hire and what those doctors are
“
There’s less help than in the city, especially with surgical cases that happen in the middle of the night.”
Dr. Ben Nelson
comfortable treating,” she says. Some physicians will take on cases beyond their specialty, read the literature, seek advice from specialists outside their practice, and widen the scope of diseases and injuries they’ll treat. Others just ship them out.”
Ben Nelson is a general surgeon at the 25-bed Waldo County General Hospital, a Critical Access Hospital (CAH ) in Belfast, Maine, a city with around 7,000 residents. A rural hospital designation made by the Centers for Medicare & Medicaid Services (CMS ) in response to the closure of over 400 rural hospitals nationally during the 1980 s and early 1990s, a CAH is designed to reduce the financial vulnerability of rural hospitals and provide higher levels of Medicare reimbursement, flexible staffing, grants, educational resources, and technical help.
Ben is one of three surgeons at the hospital. Lacking a lot of surgical subspecialties, they perform a wide variety of operations—and the locals are grateful they are there.
“Patients don’t want to travel for surgery. They want to stay in their community, and we feel very fortunate to be able to provide many of the services they need,” he says. “A lot of the families up here have been here for generations, and we see a lot of people with the same names by treating generations of one family.”
He finds building relationships within a small rural community to be very rewarding. When patients call the hospital, the surgeons answer the phone. The heartfelt ways their

patients show their appreciation— jars of maple syrup, pickled green beans, apple butter, knitted items for him and his family—are especially touching.
He’s on call more often than he would be in a city rotation, but the daily hours tend to be better, providing opportunities for him to occasionally drive his daughter to school and be home to help with dinner. Still, the job can be stressful.
“There’s less help than in the city, especially with surgical cases that happen in the middle of the night,” he says.
Vardan Papoian, (CAMED’14, SPH’14) lives in Helendale, California, a small highdesert town of around 6,000 whose population center is twin subdivisions of relatively new homes clustered around two small adjoining lakes and surrounded by a brown flat desert landscape ringed by mountains.
But Papoian is not a returning son of the desert, having grown up in decidedly urban Hollywood, California. Following his residency at Georgetown University, he and his wife wanted to move back to California with their four children to be closer to their families in Los Angeles. Establishing a practice in the high desert of San Bernardino County allowed him to care for a medically underserved community.
“[The high desert] had a big population boom over the past 10 years as the [California

coastal home] prices kept going up, but the healthcare infrastructure that supports that population has been slow to catch up,” Papoian says. “We have only a handful of specialists.”
“We have the population, but we don’t have the appeal of a city,” he said. “When you try to get younger, new graduates from their residency to come establish a practice here, it’s not appealing to them because it doesn’t have the nightlife or the extra advantages of a city.”
Others, accustomed to the urban hospitals they trained in with specialists always available for consultation, are put off by the lack of experts they can call on when they encounter a difficult case.
“They think about who’s going to help them out if they run into a complication,” he says.
The only general surgeon for hundreds of miles, Papoian works out of nearby Barstow. Where there were once three specialists working in the city, he’s now the only one. There are just three urologists in the entire high-desert area serving over 300,000 people, and a desperate need for primary care physicians.
He enjoys the challenge of learning new skills and taking on cases that involve research and consultation with other specialists, welcoming the opportunity to return to what a general surgeon used to do. Papoian was one of the few in his class who chose to become a general surgeon, a reflection of that role diminishing in recent years as specialists have assumed many of the operations the general surgeon once performed.
In such a small community, Papoian is widely known and recognized. He recalls standing in line in the local department store in his scrubs—which would hardly draw a glance in Boston—when a father looked his way and told his daughter that if she studied hard and went to college, she could be a doctor. He sees patients at work at the local shop, gas

According to the Health Resources and Services Administration station, and post office. “People see you in the community, going to the store, getting your car washed,” he says. “They have to consult with me about anything surgical because I’m the only one here.”
“There’s definitely more that falls into the wheelhouse of a general surgeon [in rural areas] than elsewhere,” notes Kaitlin Peace (CAMED ’14), a general surgeon in the Air Force who is currently stationed at a 25-bed military hospital in Anchorage, Alaska. “The number of things that you are able to do is going to be minimized in a big city because the referrals go to a subspecialty.”
Peace also is an on-call surgeon at the nearby Alaska Native Medical Center, a large hospital complex that solely serves indigenous Alaskans, many of whom hail from “The Villages,” isolated locations so remote that patients are flown in for treatment. Aside from the endemic problems of obesity, diabetes, and cardiovascular problems, she has seen unusual cases like the 10-year-old child with a large chainsaw wound that required a reconstruction of the chest wall.
“That was some of the excitement, for me, of going into general surgery—that I would be exposed to a breadth of things that I would be able to help treat,” says Peace.
There are 13.1 providers per 10,000 people in nonmetropolitan areas, and 31.23 providers per 10,000 people in metropolitan areas.
For specialists, the disparity is much more pronounced, with 30 per 100,000 people in rural communities as compared to 263 per 100,000 people in metropolitan areas.
Studies have shown that most rural doctors practice in the areas in which they grew up, or similar settings. They appreciate the values, strong sense of community, and natural beauty of such surroundings—and also understand the isolation, poverty, and chronic poor health that comes with decreased access to healthcare.
“It comes as no surprise that one of the best predictors of who’s going to practice in a rural area is that they come from a rural area,” says Joshua Wynne (CAMED’71, CAS’71), since 2010 dean of the University of North Dakota (UND) School of Medicine & Health Sciences and vice president for health affairs at the university.
Wynne is at ground zero for the multitude of issues impacting rural healthcare. Although the school, which sits on the border of Minnesota, is in a city of 59,000, it is surrounded by farmland and a third of the county is a designated HPSA, as are 41 of North Dakota’s 53 counties. About half of the state’s 784,000 residents live in nonmetropolitan areas, including 38 counties that are considered “frontier” with fewer than seven people per square mile.
“There are challenges no matter where you live, but one of the things that’s important [in a career in rural medicine] is a real commitment to, and excitement about, being in rural areas,” says Wynne, who was not born into a rural lifestyle himself. Originally from New York City, he moved to Long Island with his family, attended
BU for six years in a combined undergraduate and medical school program, followed up with a residency in internal medicine and a fellowship in cardiology at Brigham and Women’s Hospital, then joined Harvard as an assistant professor before being named chief of cardiology at Wayne State University in Detroit.
Wynne had spent his entire medical education and career in urban settings when he decided to shake things up in 2004 by accepting an administrative post at UND and ultimately, the university’s medical school deanship.
“This would be a real change,” he recalls thinking. “I liked learning about rural medicine, the challenge of rural healthcare delivery, and what we, as a state-based school, could do.”
Wynne’s goal as an administrator was to remove any roadblocks, particularly financial, that might discourage medical students and residents from taking a rural post. He took the lead in developing a program that required medical students to experience rural healthcare as part of their medical education and created rural residencies that sent surgeons into needy communities as needed. The school also introduced the incentive of 100% forgiveness for medical school tuition debt after five years serving a rural community.
“We want to remove barriers so that someone who has a passion for rural life and practice can actually do it,” he says.

Identifying risk factors for Parkinson’s disease (PD) is essential to early diagnosis. Dating back to the 1920s, Parkinson’s disease and parkinsonism—an umbrella term that refers to motor symptoms found in Parkinson’s disease and other conditions—have long been described in boxers. Repetitive head impacts from tackle football can also have long-term neurological consequences like chronic traumatic encephalopathy (CTE), but research on the association between participation in tackle football and PD is limited.
In the largest study to describe the association between football participation and the odds for having a reported diagnosis of PD, researchers from the BU CTE Center used a large online dataset of people concerned about having PD and found participants with a history of playing organized tackle football had 61% increased odds of having a reported parkinsonism or PD diagnosis.
In this study, published in JAMA Network Open, researchers evaluated 1,875 sport participants: 729 men who played football, predominantly at the amateur level, and 1,146 men who played other sports who served as the control group.
“Notably, we found a link between playing football and increased odds for having a parkinsonism or PD diagnosis even after accounting for known risk factors for PD,” says corresponding author Michael L. Alosco, PhD, associate professor of neurology and codirector of clinical research at the BU CTE Center.
They also found that players who had longer careers and played at higher levels of competition experienced increased odds for having a reported diagnosis of
Researchers from the BU CTE Center used a large online dataset of people concerned about having PD and found participants with a history of playing organized tackle football had 61% increased odds of having a reported parkinsonism or PD diagnosis.
parkinsonism or PD. Football players who played at the college or professional level were at 2.93% increased odds for having a PD diagnosis compared with those who played only at the youth or high school level. Age of first exposure to football was not associated with odds for having a reported parkinsonism or PD diagnosis.
A new BU CTE Center study has found that, among a sample of 152 young athletes exposed to repetitive head impacts (RHI) who were under age 30 at the time of death, 41.4% (63) had neuropathological evidence of chronic traumatic encephalopathy (CTE), a degenerative brain disease caused by RHI. Published in JAMA Neurology, the study includes the first American woman athlete diagnosed with CTE, a 28-year-old collegiate soccer player whose identity remains private.
“This study clearly shows that the pathology of CTE starts early,” says corresponding author Ann McKee, MD, chief of neuropathology at VA Boston Healthcare System and director of the BU CTE Center. “The fact that over 40% of young contact and collision sport athletes in the UNITE brain bank have CTE is remarkable, considering that studies of community brain banks show that fewer than 1% of the general population has CTE.”
There are four stages of CTE, with stage 4 being the most severe. Nearly all the young athletes had mild CTE (stages 1 and 2), while three donors had CTE stage 3. In those with CTE, there was often other evidence of brain injury, including the presence of a cavum septum pellucidum, enlargement of the ventricles, and more perivascular macrophages in the white matter.
Clinical symptoms were common among the athletes, regardless of whether they had CTE. Clinical symptoms

included depression (70.0%); apathy (71.3%); difficulty controlling behaviors (56.8%); and problems with decision making (54.5%). Substance abuse also was frequent, with alcohol abuse present in 42.9% and drug abuse in 38.3% of the athletes.
“The study suggests that some of the symptoms these young athletes are experiencing are not caused by the early tau pathology of CTE,” says McKee. “It is imperative that young athletes who are experiencing neuropsychiatric symptoms seek out care, as it is likely that the symptoms can be reduced with effective management and follow-up.”

The most common neurodegenerative disorder in the world, Alzheimer’s disease (AD) affects individuals of all races and ethnicities; however, most genetic research for AD has been performed on individuals of European ancestry (EA), with a limited number of large-scale genetic studies in other populations.
For many centuries, Ashkenazi Jews lived in communities in Eastern Europe and were genetically isolated from their non-Jewish neighbors. As a result, researchers from the school hypothesized that some AD susceptibility variants are more frequent, and thus more likely to show statistically significant associations, in this group compared to much larger and more genetically heterogeneous EA cohorts.
“Our study illustrates the greatly increased power for detection of genetic associations in communities like Ashkenazi Jews who trace their lineage to a relatively small group of ancestors. In such communities, diseaseassociated variants may be much more frequent
Researchers reviewed data from 142 patients with newly diagnosed stage IIIb AL amyloidosis with advanced cardiac involvement from 2007 to 2022.
compared to samples ascertained from large, mixed populations,” says corresponding author Lindsay A. Farrer, PhD, chief of biomedical genetics.
Farrer and his colleagues conducted a genome-wide association study for AD in a sample of approximately 3,500 individuals whose ancestry was almost exclusively Ashkenazi Jewish, including roughly equal numbers of persons with AD and cognitively normal individuals who were identified in a much larger group of EA participants in national AD genetics studies using an approach that compared genetic signatures with members of an Ashkenazi Jewish reference sample. The researchers identified several genetic risk factors for AD, including some previously known (APOE, TREM2) and several novel ones that are strong biological candidates (RAB3, SMAP2, ZNF890P, SPOCK3, GIPR).
Farrer said this study, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, illustrates the greatly increased power for detection of genetic associations in communities like Ashkenazi Jews who trace their lineage to a relatively small group of ancestors.
According to new research released in Blood Advances, early improvements in cardiac and hematologic parameters may predict better survival outcomes for patients being treated for stage IIIb AL amyloidosis, a deadly disease with a median survival of 4–6 months that is caused by abnormal protein buildup.
Amyloidosis occurs when normal proteins in the body misfold and form amyloid deposits in vital organs and tissues, which can lead to organ dysfunction, failure, and
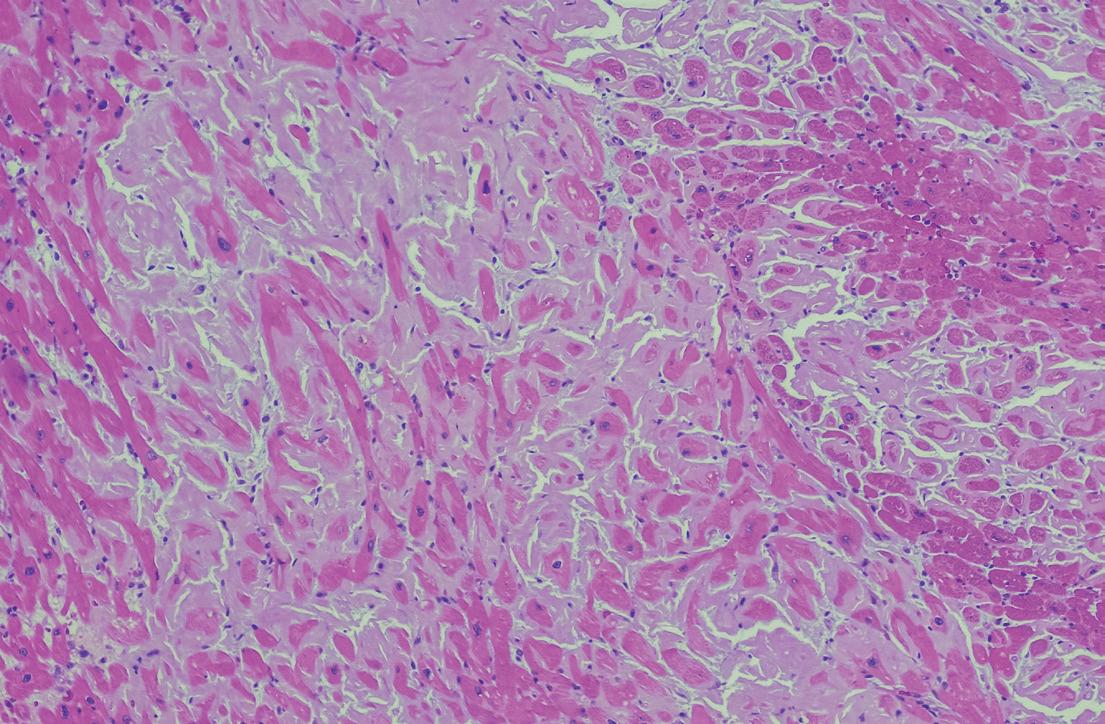
Continued from previous page
death. The prognosis for patients with advanced cardiac amyloidosis is extremely poor, but clinicians have little data to guide treatment regimens. This study reveals how early responses to treatment may predict survival outcomes.
“While AL amyloidosis is a rare condition, symptoms can mimic those of many other more common diseases, like diabetes, hypertension, autoimmune disorders, and connective tissue diseases, making it difficult for clinicians to diagnose it early,” explains senior author Vaishali Sanchorawala, MD, director of the Amyloidosis Center. “By understanding the significance of early treatment responses at one and three months after beginning treatment, we can better guide our approaches to therapy and improve patient outcomes.”
The prognosis for patients with advanced cardiac amyloidosis is extremely poor, but clinicians have little data to guide treatment regimens.
Researchers reviewed data from 142 patients with newly diagnosed stage IIIb AL amyloidosis with advanced cardiac involvement from 2007 to 2022. Patients were included after 2007 when bortezomibbased treatment regimens became available for the treatment of AL amyloidosis, following their success in treating myeloma. After 60 months of follow-up, patients exhibited a median overall survival of nine months. Several baseline factors were predictors of worse survival, including the onset of symptoms to diagnosis of greater than six months; bone marrow plasma cell count of more than 10%; higher troponin I levels (a marker of heart damage); and walking a distance of less than 200 meters in six minutes. Treatment with bortezomib and daratumumab-based regimens led to improved survival.
The COVID-19 pandemic took a toll on the mental health of healthcare workers across the world. Most described increased levels of stress and anxiety early in the pandemic, from constant exposure to patient deaths and later, from increased healthcare demands due to worsening chronic conditions like diabetes. Healthcare workers also reported that their mental health—and that of their family members—deteriorated during the pandemic.
A new study in the Journal of Interprofessional Education & Practice quantified the results of those impacts, finding that healthcare workers in Massachusetts experienced high levels of burnout, with nearly 40% planning to leave healthcare within five years and nearly a third of those under age 35 planning to do so within two years. Nearly 80% felt that lack of workplace support contributed to burnout and cited staffing shortages that left them unable to provide the best care for patients.
“These findings highlight the far-reaching impact of the COVID19 pandemic,” notes corresponding author Rebecca Perkins, MD,
professor of obstetrics & gynecology. “Staffing shortages prevent healthcare workers from taking the best care of their patients, leading to moral injury. Bringing healthcare leadership and frontline workers together is essential if we are to solve this problem.”
The researchers conducted interviews with Massachusetts healthcare workers that focused on their experience with COVID19 vaccines and the impact the pandemic had on their work in healthcare. They also asked healthcare workers to complete a survey on their mental health—including any issues that continued to worsen even as the pandemic eased—and addressed the issue of burnout at work and how to improve support that would reduce the desire to leave healthcare. ●

Scan for a complete list of BUSM’s FY23 donors.
ith great appreciation, the Chobanian & Avedisian School of Medicine recognizes our donors for their contributions this past year. Their generosity supports the vital study and practice of medicine and research, and we deeply value the impact they have made on the school, on our students, and on research.
GIVING LEVELS:
$100,000–$249,999
Bronze members
• Invitation to the spring Chester S. Keefer, MD Society Dinner
• Honorary plaque
• All of the previously listed benefits
• Invitation to and preferred seating, when available, at select BU/CAMED events throughout the year
$250,000–$499,999
Silver members
• All of the previously listed benefits
• Personalized tour of research/ clinical area of your choice at BU Medical Campus
$500,000–$999,999
Gold members
• All of the previously listed benefits
• Direct communication with the recipients of your generosity (students, faculty, researchers)
$1,000,000+
Platinum members
• All of the previously listed benefits
• Private lunch with the Dean and other leadership of the Chobanian & Avedisian School of Medicine
■ 2023 Donor
■ Deceased
■ New Keefer Member
This year, the FY23 (July 1, 2022, to June 30, 2023) Chobanian & Avedisian School of Medicine donor rosters are available online. In this issue, only the Dean’s Advisory Board and the Chester S. Keefer, MD Society are listed. For a complete list of FY23 donors, including all individual and foundation giving, please scan the QR code above or visit our website at bumc.bu.edu/camed/giving/who-gives
Thank you, donors.
The Chester S. Keefer, MD Society
• The Chester S. Keefer, MD Society is named in honor of distinguished physician and scientist Dr. Chester S. Keefer, who served as chairman of the department of medicine, dean of Chobanian & Avedisian School of Medicine, and director of Boston Medical Center. Dr. Keefer was responsible for laying the foundation for the center and as the dean of the school, he established a tradition of cutting-edge research that continues to this day.
The Chester S. Keefer, MD Society recognizes individuals whose personal philanthropy has helped advance the school by supporting the research and educational mission of Chobanian & Avedisian School of Medicine. In memory of Dr. Keefer, we honor the outstanding generosity of donors whose lifetime contributions to the school have reached $50,000 or more.
PLATINUM
Joel J. Alpert ■ and Barbara W. Alpert (SPH’79)
Edward Avedisian (CFA’59,’61, Hon.’22) ■ and Pamela A. Avedisian (Hon.’23) ■
Merwyn Bagan (CAMED’62, SPH’95) and Carol J. Bagan
Jag Bhawan and Pratibha G. Bhawan ■
Nancy L. Bucher ■
Howard D. Buzzee ■
Shamim A. Dahod (CAMED’87, CGS’76, CAS’78) and Ashraf M. Dahod ■
Richard H. Egdahl, MD ■ and Cynthia Taft (GRS’77) ■
Ralph G. Ganick (CAMED’67, CAS’67) and Lois B. Ganick ■
Alan Gerry and Sandra Gerry
Jonathan P. Gertler (Questrom’99) and Jane R. Clark ■
Albert M. Ghassemian ■
Audrey & Martin Gruss Foundation
Lewis Heafitz and Ina B. Heafitz ■
Rod F. Hochman (CAMED’79, CAS’79) and Nancy J. Hochman (Sargent’77,’83) ■
Stephen R. Karp (CAS’63) and Jill E. Karp ■
Sarkis J. Kechejian (CAMED’63) ■
Stanley H. Konefal (CAMED’47) ■ and Catherine M. Konefal ■
Sherry M. Leventhal and Alan M. Leventhal (Hon.’09)
Inez Lopez ■
Frank J. Miselis (CAMED’45) ■ and Theodora T. Miselis ■
Carl A. Olsson (CAMED’63) and Mary D. Olsson ■
Peter T. Paul (Questrom’71) ■
Jerome S. Serchuck ■ and Joan S. Serchuck ■
Richard C. Shipley (Questrom’68,’72, Hon.’22)
Wesley R. Skinner ■ and Charlotte A. Skinner ■
Jack N. Spivack ■
Christine E. Stiefel ■
Helen L. Tarlow ■ and Sherwood J. Tarlow ■
Diane Tauber and Laszlo N. Tauber ■
GOLD
Norman W. Alpert and Jane D. Alpert
Karen H. Antman and Elliott Antman ■
Nancy Baler
Anita B. Barkan (CAS’46) ■ and Donald B. Barkan (CAMED’45) ■
Elizabeth C. Dooling (CAMED’63) ■
George A. Finley III and Phyllis A. Finley
John L. Hall II (CAS’65) and Ann T. Hall
Paul F. Nace, Jr.
Joelyn L. Rohman and Michael Rohman (CAMED’50) ■ ■
Albert Rosenthaler and Debbie Rosenthaler
Paul Rothbaum and Jean Rothbaum ■
Elayne Russek ■
Thomas J. Ryan ■ and Nancy T. Ryan
Lee B. Silver (CAMED’82, CAS’82) and Rachelle L. Silver ■
Sumner Stone (CAMED’58) and Martha Skinner ■
Andrew Yee and Mirta Yee
SILVER
Erika Ebbel Angle (CAMED’12) and Colin Angle
William Y. Au (CAMED’55, CAS’51) and Beverly N. Au ■ ■
Donna R. Barnard (CAMED’65) and Douglas E. Barnard (CAMED’65) ■
Gerald Besson (CAMED’50) ■ and Eleanore S. Besson ■
Mary Ann Blount and James A. Blount, Jr.
Paul C. Burke and Gloria J. Burke ■
Helen L. Burr ■ and George Burr ■
David J. Caron and Susan M. Caron ■
Lin Castre and Abraham D. Gosman ■
Richard J. Cavell (CAMED’61) and Bonnie Cavell
Ann C. Cea (CAMED’67) and Anthony Tedeschi
Aram V. Chobanian (Hon.’06) ■ and Jasmine Chobanian ■ ■
Andrew B. Crummy, Jr. (CAMED’55) and Elsa E. Crummy ■ ■
Jodi Dome Linger and Nicholas T. Linger ■
Idea S. Fiering ■
Frederick L. Fox (CAMED’68) and Gail P. Fox ■
Laurie Girand and Scott McGregor
Burton P. Golub (CAMED’65) and Lee H. Golub ■
Robert C. Green and Sally E. McNagny
Hideo H. Itabashi (CAMED’54, CAS’49) ■ and Yoko O. Itabashi ■
Donald M. Kaplan (CAMED’73) and Edna E. Kaplan (COM’88) ■
Heidi Abdelhady, MD (CAMED’98) ■
Erika Natalie Ebbel Angle, PhD (CAMED’12,’12)
John T. Avellino
Gabriella J. Avellino, MD (CAMED’09,’13)
Deb Boedicker ■
H. Kim Bottomly, PhD ■
Elizabeth R. Brown, MD ■
Richard J. Catrambone, MD, DMD (CAMED’92) ■
Jane R. Clark, MD ■
Suzanne Cutler, PhD (Questrom’61) ■
Shamim A. Dahod, MD (CAMED’87, CGS’76, CAS’78) ■
David R. Edelstein, MD (CAMED’80) ■
Mary Jane R. England, MD (CAMED’64, Hon.’98) ■
Joseph S. Fastow, MD (CAMED’70) ■
Maurice R. Ferré, MD (CAMED’92, CGS’81, SPH’92) ■
Dan R. Fishbein, MD (CAMED’85, CAS’85) ■
Jonathan P. Gertler, MD (Questrom’99) ■
Shahram S. Gholami, MD (CAMED’96) ■
Burton P. Golub, MD (CAMED’65) ■
Rod F. Hochman, MD (CAMED’79, CAS’79) ■
Christine Spitaels Hunter, MD (CAMED’80, CAS’80) ■
Jeffrey Robert Jay, MD (CAMED’83, CAS’83)
Donald Martin Kaplan, MD (CAMED’73) ■
Sarkis J. Kechejian, MD (CAMED’63) ■
Reshma Kewalramani, MD (CAMED’98, CAS’98) ■
Sherry M. Leventhal
Douglas M. Macdonald, PhD (CAMED’98, GRS’92) ■
J. Kenneth Menges, Jr., Esq (Questrom’79) ■
Simon C. Parisier, MD (CAMED’61) ■
Peter T. Paul (Questrom’71) ■
Albert Rosenthaler
Sharon G. Ryan (Sargent’70)
Pedram Salimpour, MD (CAMED’96,’00) ■
Leslie Karen Serchuck, MD (CAMED’90) ■
Emily Wise Shanahan, MD (CAMED’09) ■
Richard C. Shipley (Questrom’68,’72, Hon.’22)
Lee Bryan Silver, MD (CAMED’82, CAS’82) ■
Rachelle L. Silver ■
Louis Wade Sullivan, MD (CAMED’58, Hon.’90) ■
Patricia Janine Williams, MD (CAMED’89, CAS’84) ■
Deborah Whittaker Wilson, PhD (GRS’72) ■
■ FY23 Donor
New DAB Members in Italics
Reshma Kewalramani (CAMED’98, CAS’98) and Abhijit R. Kulkarni (ENG’93,’97) ■
Joseph J. Konefal (CAMED’77) and Karen G. Konefal ■
Lenore Larkin and Harold S. Larkin ■
Patricia M. Leavitt (CAS’54, CAMED’58) ■
Susan E. Leeman
Henry T. Lew (CAMED’62) and Winifred Lew ■ ■
Douglas N. MacInnis (CAMED’46) ■
Barry M. Manuel (CAMED’58, CAS’54) and Patricia D. Manuel (SON’78, Wheelock’86) ■
Rita Z. Mehos
Steven A. Miller (CAMED’70, CAS’70) and Jacqueline H. Miller (CAS’70)
Joseph B. Mizgerd and Ann F. Mizgerd ■
John H. Nichols, Jr. ■
Simon C. Parisier (CAMED’61) and Elaine S. Parisier ■
Tania J. Phillips and Jeffrey S. Dover ■ ■
Peter E. Pochi (CAMED’55) ■
Jeffrey D. Tripp and M. Douglass Poirier (CAMED’76, CAS’73)
Ronald L. Ragland (CAMED’82) ■
Alexander M. Rodger ■
Richard D. Scott and Mary Scott ■
Louis W. Sullivan (CAMED’58, Hon.’90) and E. Ginger Sullivan ■
Mary U. Taylor ■
A. Raymond Tye (Questrom’47) ■
Martin L. Vogel (CAMED’53) and Phyllis M. Vogel ■
Arthur B. Wein (CAMED’39) ■
Madeline Wikler and Joseph M. Wikler ■
Deborah W. Wilson (GRS’72) and John Wilson ■
Amber Wong
Arnold Wong, Jr.
Jeremiah O. Young (CAMED’62) and Beverly A. Young
BRONZE
Anonymous (4) ■
Carmela R. Abraham and Menachem E. Abraham
Winston D. Alt (CAMED’80) and Deborah A. Gribbon ■
Rahul S. Anand (CAMED’01, CAS’97) and Meredith Anand ■
Gerhard R. Andlinger ■ and Jeanne D. Andlinger
Michael L. Apuzzo (CAMED’65) ■
John T. Avellino and R. Ellen Avellino
Ruth M. Batson (Wheelock’76) ■
Robert M. Beazley
Melvin R. Berlin ■ and Randy L. Berlin
David G. Bradley and Katherine B. Bradley
Yvonne K. Brockman and Stanley K. Brockman (CAMED’55) ■ ■
Alan J. Brody
Elizabeth R. Brown ■
Richard J. Catrambone (CAMED’92) and Sophia Catrambone ■
Robert D. Champion and Marjorie Champion
Harold N. Chefitz (COM’55, CGS’53) and Charlotte M. Chefitz ■
Hsi-Pin Chen (CAMED’96,’96, CAS’89, SPH’91) and Kenneth E. Hancock (ENG’92,’01) ■
Yi-Chuan Ching (CAMED’58) and Helen Yu-Ching ■ ■
David J. Chronley (CAMED’74) and Marianne K. Chronley ■
Michael J. Critelli and Joyce M. Critelli
Suzanne Cutler (Questrom’61) ■
Clare L. Dana (CAMED’69)
R. Gordon Darby ■
Paul R. Dooling ■ and Sandra A. Danussi
E. Elaine Erbey (Wheelock’72)
Joseph S. Fastow (CAMED’70) and Ellen K. Fastow ■
Maurice R. Ferré (CAMED’92, CGS’81, SPH’92) and Maria D. Ferré ■
Joseph T. Ferrucci and Brenda Ferrucci
Samuel Finkielsztein and Gala Finkielsztein
Charles N. Freed ■ and Marlene Freed
Patricia L. Freysinger (SON’82)
Ronald S. Gabriel (CAMED’63) and Pamela Hobbs ■
Shahram S. Gholami (CAMED’96) and Neda Gholami ■
Godley Family Foundation
Malcolm Gordon (CAMED’48) ■ and Nan Miller ■
Donald J. Grande (CAMED’73) and Elena M. Grande ■
David T. Greenleaf (CAMED’65) and Katherine O. Greenleaf ■
Jack C. Guden ■
Haynes Family Foundation ■
Lea Highet and Ian Highet
Marvin J. Hoffman (CAMED’47) ■
Michael F. Holick and Sally A. Holick
Thomas R. Insel (CAMED’74, CAS’72, Hon.’20) and Deborah J. Insel (Wheelock’71)
Jeffrey R. Jay (CAMED’83, CAS’83) and Mary Ellen A. Jay
Denise S. Katsaros (Wheelock’69) and Arthur T. Katsaros ■
Earl G. Kendrick, Jr. and Randy Kendrick
The Kessler Family
Nasir A. Khan ■
Elaine B. Kirshenbaum (CAS’71, Wheelock’72, SPH’79) ■ and Howard D. Kirshenbaum ■
Shirley P. Klein (CAMED’68, CAS’68) ■
Rose Ann Kornfeld and Lewis F. Kornfeld, Jr. ■
Lawrence E. Langsam (Questrom’57) and Hannah S. Langsam
Estella I. Leach ■
Richard S. Leghorn ■
Ruth R. Levine ■ and Martin J. Levine ■
Rita E. Loos ■
James H. Lowell II and Susan W. Lowell
The Estate of Lillian A. Luksis
Jules N. Manger (CGS’66) ■ and Janis G. Manger ■
Rocco S. Marino (CAMED’42) ■
Allan P. Markin and Patricia Markin
JoAnn McGrath
Robert B. Melikian (CGS’60, CAS’62) ■
Ruth A. Moorman (CAS’88, Wheelock’89,’09) and Sheldon N. Simon
Charles Mosesian ■
Peter J. Mozden (CAMED’53) ■
Carolann S. Najarian (CAMED’80) and K. George Najarian
John Noble ■ and Ewa Kuligowska
Wilson Nolen and Eliot Nolen
Zein E. Obagi and Samar A. Obagi
Paul I. Ossen (CAMED’43) ■
William Patty and Eliot Patty
Louise E. Penta and P. A. Penta (CAMED’51) ■
Carol C. Pohl (CAMED’67) and Alan L. Pohl ■
Theodore Polos (CAMED’47) and Jean Polos
Allen Questrom (Questrom’64, Hon.’15) and Kelli Questrom (Hon.’15) ■
Martin S. Rifkin (Questrom’82) and Judy A. Rifkin ■
Elihu Rose and Susan W. Rose
Doris M. Russell and Robert F. Russell (CAMED’46) ■ ■
Ralph L. Sacco (CAMED’83) ■ and Scott Dutcher
David J. Salant and Anne Salant ■
Paulette Samowitz ■
The Schulze Family
Charles L. Schwager (Questrom’66) and Evelyn C. Schwager (Questrom’66)
Richard Seeborg
Florence Seldin ■ and Ira L. Seldin ■ ■
Leslie K. Serchuck (CAMED’90) ■
Muriel Shapiro and Arnold Shapiro ■
The Shooshan Family ■
Stuart E. Siegel (CAMED’67, CAS’67) ■
Barry E. Sieger (CAMED’68) and Margarete Sieger ■
John Silber (Hon.’95) ■ and Kathryn U. Silber (Hon.’01) ■
Charles W. Smith and Hazel Smith ■
Gordon L. Snider ■
Edward Spindell (CAMED’53) ■ and Judith K. Spindell
Eliot B. Stewart and John M. Stewart ■
Elliott H. Sweetser (CAMED’43) ■ and Aileen B. Sweetser ■
Nevart Talanian
Gloria P. Talis ■ and George J. Talis (CAMED’50) ■
Alfred I. Tauber and Paula Fredriksen
Gerald Treece and Patricia Treece
Yolande Tsampalieros and Gabriel Tsampalieros ■
Burton White (CAMED’61) ■ and June S. White ■
Marcelle M. Willock (Questrom’89) ■
Henry R. Wolfe (CAMED’45) ■ and Grace A. Wolfe ■
Herbert H. Wotiz ■
Sam S. Wu (CAMED’92, CAS’87, GRS’90, SPH’92) and Patricia C. Tsang (CAMED’92, CAS’92, GRS’92)
Lawrence A. Yannuzzi (CAMED’64) and Julie Yannuzzi ■
Larry C. Young and Sue Young
Lily M. Young (CAMED’65) and John G. Johansson ■
The Family of Alan Ziskind ■ MERCURY
Anonymous (3) ■
Lawrence D. Ackman ■ and Ronnie Ackman
Noubar B. Afeyan and Anna Afeyan
Gerald Ajemian and Lucille Ajemian
Dwight M. Akers (CAMED’53) ■ and Beverly R. Akers ■
Max M. April (CAMED’85, CAS’81) and Pamela T. April (Questrom’83)
Carola A. Arndt (CAMED’78, CAS’78) ■ ■
Amin Ashrafzadeh (CAMED’97, CAS’93) and Christine Ashrafzadeh (Questrom’96, CAS’92) ■ ■
Sonya Nersessian (LAW’85) and Richard K. Babayan ■
Steven Baker ■ and Shirley Baker ■
Gary J. Balady and Rosemary Mehl ■ ■
Elizabeth D. Barnett (CAMED’85) and Suleiman N. Mustafa-Kutana ■
Paul C. Barsam (STH’52) and Joyce L. Barsam
Howard C. Bauchner (CAMED’79) and Christine M. McElroy (GRS’81,’84) ■ ■
Howard C. Beane (CAMED’57) ■ and Shirley T. Beane
John H. Bechtel (CAMED’50) ■ and Shirley F. Bechtel
Franklyn D. Berry (CAMED’41) ■
David W. Bishop (CAMED’46) ■
Elsa C. Bodon (CAMED’41) ■
Deb Boedicker and Mackenzie Boedicker ■ ■
James F. Bopp, Jr. ■
S. Arthur Boruchoff (CAMED’51) ■ and Anna Silverman-Boruchoff (CAMED’49) ■
Robert A. Cameron ■
Robert J. Carey (CAMED’54) ■ and Mary E. Carey (Wheelock’55)
Russell K. Carney and Geraldine Carney
Lisa B. Caruso (SPH’99) ■
David M. Center (CAMED’72, CAS’72) and Patricia Rabbett ■ ■
Edmond E. Charrette (CAMED’62) and Maria T. Charrette ■
Jeremy Chess (CAMED’70, CAS’70)
Frank Citrone, Jr. and Carol Citrone
John P. Cloherty (CAMED’62) ■
John F. Cogan, Jr. ■ and Mary L. Cornille (GRS’87)
Alan S. Cohen (CAMED’52) ■ and Joan P. Cohen
Patricia A. Connolly (CAMED’84) ■
Marian M. Cook
Ronald B. Corley and Janice Corley ■
Sidney Covich ■
Brit D’Arbeloff and Alexander V. D’Arbeloff ■
David P. DiChiara (CAMED’84, CAS’80) and Maria J. DiChiara ■
Paul E. Dixon, Jr. and Rebecca K. Dixon
Thomas J. Dowling, Jr. (CAMED’81, CAS’81) and Rosemary Dowling
Hilda R. Dressler (CAMED’34) ■
Carol A. Dyer and Gene Gordon (CAMED’46) ■
Alan M. Edelstein (Questrom’47, LAW’49)
■ and Sybil Edelstein
David R. Edelstein (CAMED’80) and Eve L. Edelstein ■
Alvin N. Eden (CAMED’52) ■ and Elaine R. Eden ■ ■
Mary Jane R. England (CAMED’64, Hon.’98) ■
Michael J. Esposito (CAMED’49) ■
Geraldine L. Feldman (CAMED’69, CAS’69) ■
Judith N. Feldman
I. Howard Fine (CAMED’66) and Victoria Fine
Bertha Offenbach Fineberg (CAMED’36) ■ and Nathan L. Fineberg (CAMED’30) ■
Nicholas J. Fiumara (CAMED’39) ■
Daphne H. Foster (CAS’79, Questrom’82) and Lawrence Foster
Beverly R. Franklin (CAS’44) ■ and William E. Franklin (CAMED’46) ■
Myrna Franzblau (Wheelock’73) and Carl Franzblau
Monte Friedkin and Skeets Friedkin
Ray A. Garver ■ and Donna L. Garver ■
Marion L. Gendron (PAL’26) ■
George E. Ghareeb (CAMED’62) ■ and Nancy B. Ghareeb
The Ginwala Family ■ ■
Harold M. Ginzburg (CAMED’68, CAS’68) and Jenny Boyer ■ ■
Arnold Goldenberg (CAMED’54) and Gloria Goldenberg ■
Dorothy A. Gottlieb (CAS’76) and Leonard S. Gottlieb ■
Doris Grabosky ■ and Jack Grabosky
Ellen R. Grass ■
Robert E. Griffin and Cathleen Griffin
Morton S. Grossman (MET’42) ■ and Sylvia Grossman ■
Kenneth M. Grundfast and Ruthanne Grundfast
Fritz Grunebaum (Hon.’79) ■
Robert W. Healy (CAMED’67) and Bonnie M. Healy ■
Juan D. Hernandez Batista ■ and Maria A. Tavarez-De Hernandez
Arnold S. Hiatt
George L. Hines (CAMED’69, CAS’69) and Helene A. Hines (Sargent’69) ■
Ann S. Hintlian ■ and Deran Hintlian
Michael G. Hirsh (CAMED’63) ■ and Carol N. Hirsh
Betsy E. Horen ■
Arline Housman ■ and Herbert E. Housman ■
Charles Housman
Edward L. Housman (Questrom’42) ■ and Charlotte Houseman ■
John P. Howe III (CAMED’69, Hon.’19) and Tyrrell E. Flawn ■ ■
James B. Howell (CAMED’65) and Marlene A. Howell
Bernard L. Huang (CAMED’62, CAS’57) ■ and Ann M. Huang
Richard E. Hunter (CAMED’44) ■ and Minta L. Hunter ■
David Ingall (CAMED’57, CAS’52, GRS’53) ■ and Carol Ingall
Patricia K. Issarescu (CAMED’61) ■
Joseph A. Izzi, Sr. and Barbara A. Izzi
Peter F. Jeffries (CAMED’60) ■ and Jeanne F. Arnold (CAMED’61) ■
Clinton W. Josey, Jr. and Betty Josey ■
Lori A. Jurado and Xavier Jurado
Esther B. Kahn (Wheelock’55, Hon.’86) ■
Charlotte A. Kaitz ■ and Louis L. Kaitz ■
Kenneth P. Kato (CAMED’89) and Nancy A. Nagy ■ ■
Damon J. Keith ■
The Kibrick Family
Burton I. Korelitz (CAMED’51) ■ and Ann Z. Korelitz
Conan Kornetsky ■
Bernard E. Kreger ■
Edward E. Krukonis (CAMED’63) ■ and Priscilla J. Krukonis ■
Saul Kurlat ■
Cecelia Lance
Charna C. Larkin and Alan B. Larkin ■
Robert E. Leach and Laurine Leach
Paul M. Leiman (CAMED’74, CAS’72) and Carol R. Leiman ■ ■
Brian Levine and Beth Levine
Brigette Lonner and Joseph J. Lonner ■
Thomas A. MacLean (CAMED’64) and Colleen K. MacLean ■
William I. Malamud (CAMED’54) ■ and Camille C. Malamud ■
William M. Manger and Lynn S. Manger
Richard C. Marcus
Stella C. Martin and Clive R. Martin
Ronald P. McCaffrey and Maureen McCaffrey
John F. McCahan and Kathleen B. McCahan ■ ■
Hubert W. McDonald and Ann S. McDonald ■
Edward J. McDonald, Jr. and Catherine A. McDonald
Jean E. McPhail ■
Robert F. Meenan (CAMED’72, Questrom’89)
Mark S. Michelman (CAMED’67) and Susan F. Michelman ■
Daniel E. Moalli (CAMED’61) and Glenna M. Moalli ■
Jordan Monocandilos
Rodney A. Montag and Sally A. Montag
Sanford R. Montag and Nancy L. Montag
Thomas J. Moore and Mary C. Moore ■
Sunit Mukherjee (CAMED’89, CAS’89) and Sumeeta Mukherjee
Michael F. Mullarkey (CAMED’70) and Dawn Mullarkey (CAS’68)
Praveen V. Mummaneni (CAMED’95, CAS’95) and Valli P. Mummaneni ■ ■
G. Vijaya Naidu
Newton Family Fund
Merel G. Nissenberg
Dawn B. Norcia and David J. Norcia
N. Stephen Ober (CAMED’86, CAS’82)
John F. O’Brien (CAMED’59) ■
Anne W. O’Connor and John F. O’Connor (CAMED’57) ■
Hytho H. Pantazelos (CAMED’63) and Peter G. Pantazelos ■ ■
Dianne M. Parrotte (CAMED’79, CAS’79)
Edward F. Parsons (CAMED’65) ■
Jordan C. Paul and Valerie J. Paul ■
Lita Perkins ■ and John S. Perkins ■
Jona A. Perlmutter and Donna Perlmutter
Astrid O. Peterson (CAMED’77, CAS’74) ■
N. Neal Pike (LAW’37) ■
John I. Polk (CAMED’74, Wheelock’13) and Mary C. Nugent Polk (SON’76,’77)
Helen S. Ratner ■ and Frank Ratner (CAMED’47) ■
Iver S. Ravin (CAMED’40) ■
Nancy E. Rice (CAMED’65) and Millard J. Hyland
Joel A. Roffman (CAMED’75, CAS’72) and Nancy C. Roffman ■
Gerald L. Ross ■
Melanie Rothbaum and David Rothbaum (CAMED’82) ■
Richard A. Rudders ■
Stephen W. Russell (CAMED’55) and Gail D. Russell
Pedram Salimpour (CAMED’96,’00) and Stacy Weiss ■
Hannah E. Sandson and John I. Sandson ■
Francis P. Saunders (CAMED’58) and Lydia M. Saunders
Frank J. Schaberg, Jr. (CAMED’68, CAS’68) and Monica J. Schaberg (CAMED’68, CAS’68) ■
Alan L. Schechter (CAMED’78) and Genevieve Schechter
Harold S. Schell (CAMED’70) and Antoinette M. Schell ■
Rocco Schelzi ■
Herman Selinsky (CAMED’24) ■
Richard J. Shemin (CAMED’74, CAS’72) and Susan H. Shemin
Norton L. Sherman ■ and Claire M. Sherman
Ethan M. Shevach (CAMED’67, CAS’67) and Ruth S. Shevach ■ ■
William F. Shields (CAMED’94, GRS’90) ■
Richard L. Simmons (CAMED’59) ■
Simon L. Strong (ENG’79, Questrom’91) and Sarah A. Strong
Lois N. Talis (PAL’49) ■
Tony Y. Tannoury and Viviane Tannoury
Stephen M. Tringale (CAMED’90, CAS’80, GRS’86) ■
Sanford W. Udis (CAMED’44) ■
Marian A. Vita ■
Franz Waldeck ■
Carl W. Walter ■ and Margaret H. Walter ■
Murray Weinstock (CAMED’65) and Gloria Weinstock ■
Sue Rosenwasser Weiss and Seymour Rosenwasser ■
Anthony Weldon
Judith F. Wellington and Peter S. Wellington ■
Jerrold Wexler and Joan Wexler
Robert H. Wexler ■ and Joanna B. Wexler ■
Alan Winters and Hope Winters
Robert A. Witzburg (CAMED’77) and Lorraine G. Witzburg (Wheelock’06) ■
Peak Woo (CAMED’78, CAS’78)
Earle G. Woodman (CAMED’58) ■
Moshe Yanai and Rachel Yanai
Charles R. Young ■ and Marion L. Young ■
Frances W. Young ■
Barry S. Zuckerman and Pamela A. Zuckerman
HONORARY
Dorothy C. Keefer (PAL’46,’48) ■
Ishebel K. Lyle ■ and Carl Lyle ■
Marvin Hoffman (CAMED’47) owes his medical degree to Boston University—as well as his 60-year career, his marriage, and the golden opportunity he had to see the 1946 American League Champion Boston Red Sox play at Fenway Park.
In gratitude for his education and his livelihood, he has used a charitable IRA rollover to endow the Marvin J. Hoffman and Nancy Yanes Hoffman Scholarship Fund, which will provide tuition support to medical students. Besides being a generous gift to BU, it’s a present to himself for a milestone birthday: Hoffman turned 100 in December.
Hoffman received a scholarship of sorts to attend medical school when the US military paid his tuition; he enrolled in 1943 knowing he would serve in the Army after completing his medical training. “I took my last exam at the University of Rochester, and the next day I went to Buffalo, took a physical, and was given a uniform,” Hoffman recalls. “I went to [Army induction center] Camp Upton in Long Island for 10 days, then to BU in uniform.”
That uniform provided a splendid benefit to its wearer: free admission to Fenway Park. Hoffman, who lived a block away, remembers cheering legendary Red Sox left fielder Ted Williams.
While in medical school, Hoffman was smitten by Nancy Yanes, a Connecticut College of Women student he met at a dance one January. He immediately sent her a Valentine’s Day card and suggested they get together when she came back to Boston. “She said she’d be in town on March 8, we went to dinner, and that was the beginning of the end,” Hoffman says, laughing. The couple wed in 1948 and were married for 68 years. Nancy, an author and longtime English professor at St. John Fisher University in Rochester, passed away in 2016.
After graduating in 1947, Hoffman completed his internship and residency in his hometown of Rochester, New York, beginning his internal medicine practice there in 1951 while teaching at the BU medical school.
Drafted into the Korean War, he served as sole medical officer of the US Army’s 24th Division and became chief of the US Army base hospital in Otsu, Japan. Upon his return, he settled in Rochester, where he and his wife raised their family. Hoffman became the senior medical director at Excellus Blue Cross/Blue Shield of Rochester and helped establish its first HMO, Blue Choice. He retired in 2008 at age 85.
Medical careers run in the family. The Hoffmans’ son, William Hoffman, is a plastic and reconstructive surgeon at University of California San Francisco and three of their eight grandchildren are doctors—including Rachel Hirshorn (CAMED’20), an internist.
Hoffman hopes the BU scholarship fund he endowed will ease the heavy financial burden most medical students carry and urges other alumni to support similar causes.
“The main reason for giving money was that I had money to give,” he says with a chuckle. “Do I have advice for people who want to make a gift to BU? I think it’s a great thing to do, and if you’re able to do it, you should do it. The medical school where you went is as good as any other place, because it’s the one that gave you your life.”
Funding will help reduce breast cancer disparities, improve outcomes among Black women
Julie Palmer, ScD, codirector of the BU-BMC Cancer Center, has been awarded a one-year, $589,000 grant from the Breast Cancer Research Foundation (BCRF) for her research project, “Breast Cancer Drivers in Black Women: Society to Cells.”
The project’s goal is to reduce breast cancer disparities and improve outcomes among Black women by advancing personalized, evidence-based care. Ultimately, over a five-year period, a comprehensive study of the interaction of comorbidities, social determinants of health (SDOH), and breast cancer genetics in Black women will be conducted.
“This grant will support the initial involvement of the Black Women’s Health Study (BWHS) in the BCRF-Estée Lauder Companies Disparities Project and set the stage for future work,” explains Palmer, a founding leader of the BWHS, a prospective cohort study of 59,000 Black women who enrolled in 1995 and have been filling out biennial questionnaires since that time.
A cancer epidemiologist with research projects spanning early detection, etiology, and survivorship, Palmer’s primary focus is on elucidating reasons for the disproportionately high incidence of hormone receptor negative breast cancer in Black women and on understanding and reducing racial disparities in breast cancer mortality.
While the BWHS has a wealth of data on SDOH, comorbidities, and lifestyle factors among Black women who have been diagnosed with breast cancer, as well as data on more than 45,000 Black women without cancer, funding from this grant will add missing data elements to create uniformity across the BWHS and similar large studies. “A comprehensive and contemporary profile of SDOH and a strategic plan for collecting and standardizing data/ SDOH elements will be formulated,” says Palmer, the Karin Grunebaum Professor in Cancer Research and director of BU’s Slone Epidemiology Center.
Among the proposed improvements and additions:
● Link with national databases that provide neighborhood-level information on environmental exposures, poverty, and racial discrimination, and with health system-level data on provider characteristics and facilities.
● Supplemental questionnaires will be sent to BWHS participants who are breast cancer survivors to obtain additional data on treatments, insurance status, comorbidities, psychosocial stressors, and outcomes.
● A novel method of obtaining dried blood spots as a source of identifying circulating RNA for BWHS breast cancer survivors will be used and, as funds permit, will also be used for women who are cancer-free but at a higher baseline risk due to a family history of breast cancer.
The American Cancer Society (ACS) recently awarded the Chobanian & Avedisian School of Medicine $1.26M through three grants that support exploratory research and provide career development activities for students who are pursuing a doctoral degree in a STEM discipline or health profession.
Deborah Lang, PhD, associate professor of dermatology, and Rachel Flynn, PhD, associate professor of pharmacology, physiology & biophysics, each received a $300,000 Discovery Boost Grant.
Lang’s research, “Exploring roles for PAX3 in regulating gene expression on a posttranscriptional level,” will investigate the role of PAX3—a protein that directs melanocytes to maintain stem cells and to lineage-specify—in stems cells and cancer. Cancer subverts these normal PAX3 stem cell maintenance roles to promote melanoma growth and metastasis.
Lang previously discovered several PAX3interacting proteins that play roles in RNA control and degradation. With support from the ACS, she will further investigate the relationship between PAX3 and lineagespecific RNA regulation. She aims to target this pathway to hinder disease progression
or support stem cell multipotency, which will provide an attractive target for therapy.
Through her project, “Defining the replication stress response in the Alternative Lengthening of Telomeres Pathway,” Flynn will investigate the activation of the Alternative Lengthening of Telomeres pathway (ALT). Cancer cells use ALT to promote cellular immortality. This process is active in approximately 10% of all human cancers and approximately 60% of aggressive forms of cancer including osteosarcoma, glioma, and pancreatic neuroendocrine tumors. Flynn will define the molecular mechanisms that regulate ALT activity to identify tractable therapeutic targets in the treatment of ALTpositive cancers.
Flynn also received $660,000 to implement a Diversity in Cancer Research Post-Baccalaureate Fellows Program to expand diversity in the cancer research workforce by increasing the number of underrepresented groups in the biomedical field. The Boston University-Boston Medical Center Cancer Center will provide training in academics, research, and professional development to four fellows over two years. “We hope that after participating in this program, fellows are well positioned to succeed in the cancer research workforce,” Flynn says.
Mohsan Saeed, PhD, assistant professor of biochemistry & cell biology, has received the 2023 Smith Family Foundation Odyssey Award, the first recipient from BU so honored.
Created by the Richard and Susan Smith Family Foundation in 2017 to fuel creativity and innovation in junior investigators in the basic sciences, the Odyssey Award supports the pursuit of high-impact ideas to generate breakthroughs and drive new directions in biomedical research by funding high-risk, high-reward pilot projects solicited from the brightest junior faculty in the region.
As part of the award, Saeed will receive $400,000 to study how mosquito-borne viruses (arboviruses) overcome the immune system of mosquitoes and establish
persistent infection that is then transmitted to humans. He will collaborate on this project with Joseph Zaia, PhD, professor of biochemistry & cell biology, and Fabiana Feitosa-Suntheimer, PhD, a senior research scientist at the National Emerging Infectious Diseases Laboratories (NEIDL).
Mosquito-borne arboviruses claim over one million human lives each year and are considered a global health priority due to their frequent resurgence of activity and unprecedented geographical expansion in recent decades. In the absence of vaccines and targeted treatments, designing strategies to control arboviruses at the mosquito level is imperative.
According to Saeed, his project is based on the premise that an in-depth understanding of mechanisms by which arboviruses establish lifelong infection in mosquitoes can inspire the design of powerful approaches to reduce viral transmission to humans. He will use an advanced technique, which he recently developed, to investigate the molecular details of how arboviruses disarm mosquitoes’ antiviral defense systems and establish persistent infection.
“These studies will open up new lines of investigation into viral persistence and mosquito biology and facilitate the design of transgenic mosquitoes unable to harbor and transmit infections. It will also accelerate a discovery pipeline that can then be extended to other insect-borne pathogens such as plasmodium and borrelia,” says Saeed, who joined BU in 2019 and also is an investigator at the NEIDL, where his lab explores the role of viral and host proteases in disease mechanisms of positive-strand RNA viruses.
When COVID-19 was declared a global pandemic in early 2021, Saeed’s lab pivoted to SARS-CoV-2 research and has since made contributions to the molecular understanding of how SARS-CoV-2 establishes infection in various tissues and interacts with the human innate and adaptive immune systems ●
Greetings, Alumni and Friends,

With fond recollection, I shared that it was my time observing and learning from physicians and those they served in southeast Alaska communities that drew me to medicine and public health. In this issue of Boston University Medicine, we continue our “alumni stories” series with a cover feature about alumni who practice medicine in rural communities. Our alumni describe the profound benefits of providing healthcare in rural areas and the sense of belonging they experience within the community. We are proud to share their compelling and touching stories with you.
We thank those of you who journeyed back to the Medical Campus for Alumni Weekend 2023 to attend events, connect with classmates and students, tour the campus, and reminisce. It was another successful and highly enjoyable alumni weekend, and we are grateful to the many who joined us!
During the weekend, we celebrated many alumni and historical moments, including the 40th anniversary of the Early Medical School Selection Program (EMSSP). Frederick Powell (CAMED’11) was honored with the EMSSP Champion Award for his hard work and steadfast commitment to the students and the program.
Reshma Kewalramani (CAS’98, CAMED’98), the first woman to serve as chief executive officer of a major biotech company, received the 2023 Distinguished Alumni Award for her outstanding career in medicine, unflagging healthcare leadership, and groundbreaking work as a top executive in the biotechnology industry.
We extend heartfelt congratulations to our 2022 Distinguished Alumni Award recipient Drew Weissman (CAMED’87, GRS’87, Hon.’23) and his collaborator Katalin Karikó for winning the 2023 Nobel Prize in Physiology or Medicine for their pioneering work with modified mRNA
technology. The entire Boston University community is tremendously proud of this outstanding achievement and well-deserved recognition.
As we look to future reunion events, we ask that classes celebrating in 2024 save the dates September 26–28 for Alumni Weekend. If you celebrate your 50th or 50th-plus reunion, please join us May 16–17 for unique reunion activities including the opportunity to be present at the Class of 2024 commencement. More details to follow. We are providing opportunities for all reunion classes to virtually reconnect and build enthusiasm for your in-person reunion. We want to make this meaningful for you. If you are interested in helping plan your celebration, please join us for a virtual event or reach out to the Alumni Relations team. We welcome your involvement!
Maintaining strong connections with alumni like all of you fosters a sense of belonging and enhances the opportunities for our community. This year, we visited alumni in Long Island, New York, and Stratham, New Hampshire. Alumni board members Alan Multz (CAS’81, CAMED’85) and Frank McMillan Jr. (CAMED’95) hosted neighborhood events bringing alumni together for casual conversation and catching up. If you are interested in connecting with classmates and hosting a gathering in your area, please reach out to us! We would love to hear from you.
As always, we greatly appreciate you and look forward to staying connected.
Sincerely,
 Heather Miselis, MD, MPH (CAMED’00,’04, SPH’00) Assistant Dean for Alumni Affairs
Heather Miselis, MD, MPH (CAMED’00,’04, SPH’00) Assistant Dean for Alumni Affairs

Physician and scientist Drew Weissman, who earned both an MD and a PhD at Boston University, and his research collaborator Katalin Karikó won the 2023 Nobel Prize in Physiology or Medicine for their pioneering work developing the technology that powers the Pfizer-BioNTech and Moderna COVID-19 vaccines
Those two vaccines are among the most widely distributed coronavirus vaccines worldwide. They are being used in more than 200 countries to help contain the spread of the deadly virus that upended global society in early 2020 and has so far killed nearly 7 million people and infected nearly 770 million.
“The laureates contributed to the unprecedented rate of vaccine development during one of the greatest threats to human health
in modern times,” the Nobel committee said in a statement. The committee praised the scientists for their “groundbreaking findings” that “fundamentally changed our understanding of how mRNA interacts with our immune system.”
“It’s an incredible honor,” says Weissman (CAMED’87, GRS’87, Hon.’23). “We couldn’t have come to the result without both of us being involved.” He adds, “The future is just so incredible. We’ve been thinking for years about everything that we could do with RNA, and now it’s here.”
Moderna and German firm BioNTech used the mRNA technology to research vaccines. Then COVID-19 struck in late 2019, and the rest became Nobel history.
Weissman, 64, who grew up in Lexington, Mass., did his undergraduate work at Brandeis University and his graduate work at BU, focusing on immunology and microbiology. He is a professor of medicine and the Roberts Family Professor in Vaccine Research at the University of Pennsylvania Perelman School of Medicine.
Weissman and Karikó, 68, a biotech executive, researched so-called messenger RNA, or mRNA, a molecule essential in protein production. While Weissman’s research dates to the 1990s, the breakthrough by the two came in 2005, when they discovered
that adding altered mRNA to cells could trigger production of any desired protein—a feat that could revolutionize therapeutics and vaccines to treat and prevent devastating diseases and infections.
To create immunity against the SARSCoV-2 virus responsible for COVID infections, mRNA vaccines instruct cells to make the coronavirus’ hallmark “spike” proteins. Those proteins nestle on the surface of the virus, causing COVID; when a person’s immune system detects the protein on a cell’s surface, it makes antibodies that protect against COVID. The mRNA vaccines trigger the body into producing those spike proteins, and the antibodies necessary to destroy them, thus providing protection against coronavirus without risking the health consequences of having to build immunity by catching the virus itself.
Weissman and Karikó’s paper about their discovery was initially rejected by several scientific publications. When Immunity published it in 2005, few scientists took notice. Finally, Moderna and German firm BioNTech used the mRNA technology to research vaccines. Then COVID-19 struck in late 2019, and the rest became Nobel history.
Speaking to Bostonia in 2021, Weissman reflected on the day when he and Karikó received their own vaccine shots together, in December 2020: “It was an emotional moment. There were a lot of down times, a lot of soul-searching, a lot of figuring out why things weren’t working. But we never lost hope because we both saw the incredible potential that mRNA had.”
The Associated Press contributed to this article ●
Reshma Kewalramani, MD (CAS’98, CAMED’98), CEO and president of Vertex Pharmaceuticals, has received the 2023 Distinguished Alumni Award for her exceptional accomplishments in medicine, healthcare leadership, and as a top executive in the biotechnology industry
Presented to graduates of the Chobanian & Avedisian School of Medicine in recognition of their outstanding achievements, the Distinguished Alumni Award is often awarded to those who exemplify the school’s mission of addressing healthcare inequities and treating traditionally underserved and marginalized populations.
Kewalramani was honored at a luncheon in Hiebert Lounge on September 22 as part of Alumni Weekend. The first female chief executive officer of a major US biotechnology company, Kewalramani told the audience of friends, family, students, faculty, and alumni that making the career change from physician and teacher into biotech was never about becoming a CEO.
“Not because I didn’t think I was capable, but because it wasn’t ever about the title,” she said. “I wanted to make medicines for patients. That’s what interested me.”
Fellow classmate and former Alumni Board President Heidi Abdelhady, MD (CAMED’98), presented the award, followed by a casual Q&A session.
“I [gained confidence] at BU because it was a nurturing environment. It was a challenging environment. It was a place where you could make a real difference and people gave you the opportunity to do so,” said Kewalramani, referencing her work in the labs of Associate Professor of Pharmacology, Physiology & Biophysics Judith Saide, PhD, and Professor of Biochemistry & Cell Biology Vickery Trinkaus-Randall, PhD.
Kewalramani emigrated with her family from Mumbai, India, when she was 11. In an interview last year in the online journal Women Who Win, Kewalramani quipped
there were three generally accepted career choices in her family: engineering, medicine, or the priesthood.
“I chose medicine,” she said. From the start, she intended to become a “triple threat” by conducting research, teaching medical students and residents, and seeing patients.
Following her graduation with honors from BU’s seven-year undergraduate and medical school program, Kewalramani completed an internship and residency in internal medicine at Massachusetts General Hospital (MGH) and a fellowship in nephrology in the combined MGH/Brigham and Women’s Hospital program.
Vertex develops medicines that treat the underlying cause of cystic fibrosis (CF) for up to 90 percent of all people with CF. The company also develops drugs to treat other serious conditions like sickle cell disease, beta thalassemia, type 1 diabetes, and APOL1mediated kidney disease.
Her medical education had fostered her interest in clinical research. Kewalramani realized the instrumental role new medicines played in improving patient lives, and the biotech industry was where the big advances in patient care were happening.
In 2004, Kewalramani left a career as a physician and nephrologist at MGH and Brigham and Women’s Hospital to move to California with her husband and their twin boys. She spent the next dozen years at
Amgen, one of the world’s largest biotech companies, ultimately serving as vice president and head of the US medical organization.
Returning to Boston in 2017 to work at Vertex, Kewalramani became chief medical officer and executive vice president of global medicines development and medical affairs in 2018 before being named to the top job two years later.
Vertex develops medicines that treat the underlying cause of cystic fibrosis (CF) for up to 90 percent of all people with CF. The company also develops drugs to treat other serious conditions like sickle cell disease, beta thalassemia, type 1 diabetes, and APOL1-mediated kidney disease.
“Vertex captured my heart and imagination when I saw the opportunity to help create medicines that have a huge impact on people’s lives,” she told BU Medicine in a 2019 interview.
After a yearlong transition period, Kewalramani began work as CEO and president in April 2020, facing the COVID-19 pandemic head-on while working remotely.
Discussing the monumental changes she has made in her career, Kewalramani advised the audience to be daring. “Take risks. Do things outside of your comfort zone. Try to live a life where you don’t look back and say ’I wish.’”
Kewalramani also champions diversity of gender, race, and ethnicity in the pipeline of students who take Science, Technology, Engineering, and Mathematics (STEM) courses.
Kewalramani has received numerous honors and accolades for her leadership and contributions to science and innovation, including the Harvard Business School Alumni Achievement Award, the International Institute of New England Golden Door Award, the New England Council New Englander of the Year Award, and the Asian American Business Development Center Pinnacle Award. She has been named one of Boston Business Journal’s Power 50, one of Boston magazine’s Most Influential Bostonians, and one of Business Insider’s 10 People Transforming Healthcare.
She is a member of the school’s Dean’s Advisory Board and sits on the MGH board of trustees and Ginkgo Bioworks board of directors. She is also on Year Up’s national board of directors and the board of directors for the Biomedical Science Careers Program ●

Medical school alumni returned to campus September 22–24 for Alumni Weekend 2023 to celebrate alumni awards, class reunions, and the 40th anniversary of the groundbreaking Early Medical School Selection Program (EMSSP).
The weekend began on Friday with a luncheon recognizing the trailblazing career of 2023 Distinguished Alumni Award recipient Reshma Kewalramani, MD (CAS’98, CAMED’98), the first woman to serve as chief executive officer of a major biotech company. Kewalramani’s husband and parents, former classmates and professors, fellow alumni, and current faculty and students gathered in Hiebert Lounge to mark the occasion.
After introducing Kewalramani, former Alumni Board President Heidi Abdelhady (CAMED’98) hosted a Q&A session discussing Kewalramani’s life and career as president and CEO of Boston-based biopharmaceutical company Vertex Pharmaceuticals. Abdelhady also announced the alumni board’s newest president, Demetrios Vavvas (CAMED’99).
On Friday night, the Class of 1973 celebrated their 50th reunion with a dinner in Hiebert Lounge. Assistant Dean for Alumni Affairs Heather Miselis, MD, and Dean Karen Antman, MD, welcomed the class back to campus, and attendees spent the evening reflecting on times past and catching each other up on the present.
Nearby, EMSSP alumni and current students gathered at Doña Habana restaurant in the South End to honor the program’s longtime coordinator, Malissia Evans, who retired in June after 38 years of service. Since 1982, the program has partnered with Historically Black Colleges and Universities, and more recently, schools with large Latinx and Pacific Islands populations, to ease the transition into medical school.
Also Friday evening, a dozen members of the Class of 2003 commandeered a section of the well-known Back Bay hide-
away Clery’s for their own memorable reunion festivities led by Mark Buzzelli, MD (CAMED’99,’03), and Alyson Hedgepeth (CAMED’03). The group returned to campus for a more formal (but equally lively) dinner the following night.
On Saturday, during a coffee-andconversation event with Dean Antman, alumni welcomed the opportunity to ask the dean about the institution as it moves forward. “[Alumni are] looking at the geopolitical environment and bringing it back to our home base,” said Abdelhady. “I think Dr. Antman and the team are doing a terrific job navigating this rough terrain that we’re living in.”
Student and staff-led tours of the campus followed, with highlights including the team-based learning center, Gross Anatomy Lab, and the Alumni Medical Library. Alumni enjoyed learning about the current curriculum, reminiscing, and taking selfies at Bakst Auditorium.
On Saturday evening, the EMSSP celebrated their 40th anniversary with program alumni and current students. Following a welcome from Assistant Dean of Diversity & Inclusion and EMSSP Director Ebonie Woolcock, MD, MPH (CAMED’10, SPH’10), and
Continued from previous page
Dean Antman, the event revisited EMSSP’s history and invited student and alumni panelists to share their experiences in the program and their post-graduation careers. Panelist Dallas Reed (CAMED’10) described the program’s importance to her.
“I really owe my professional career to EMSSP . . . I have lifelong friends, lifelong colleagues from this program. I think it is probably the single most important reason why I’m still involved with the school,” said Reed, chief of genetics, medical geneticist, and an obstetrician/gynecologist at Tufts Medical Center in Boston.
The anniversary celebration culminated with the Class of 2011’s Frederick Powell, MD, PhD, now an anesthesiologist and critical care physician at Colquitt Regional Medical Center in Moultrie, Georgia, being honored with the EMSSP Champion Award recognizing his impressive career achievements. Former EMSSP director Samantha Kaplan, MD, MPH, commented on Powell’s unflagging dedication to the program.
“[Powell] is, and has been, amazingly committed to the program. He understands exactly why it exists and what it can do, but also what it takes to be successful,” said

Kaplan. “And he’s brought all that expertise consistently through the years to the forefront, to make sure the program is successful, and the students are successful.” Powell addressed the attendees virtually from his home in Georgia.
Saturday night’s reception and reunion dinner in Hiebert Lounge gathered alumni from the Classes of 1963, 1968, 1993, 1998,
2003, and 2013 together to enjoy good food, stimulating conversation, and a wonderful cityscape view.
The weekend’s final event was held on Sunday, as EMSSP alumni joined their families and current students for a brunch celebrating the program’s storied history and ongoing success. ●

Jerome Waye of Greenwich, Connecticut, writes, “After graduation, I trained in gastroenterology at Mount Sinai Hospital (MSH) in New York, then went into private practice and was affiliated with MSH for 52 years. I became the world’s best-known colonoscopist, lecturing across the world and writing 7 books and over 200 papers. I have been president of the American Society for Gastrointestinal Endoscopy, the American College of Gastroenterology, and the World Organization of Endoscopy. In 2015 I joined the full-time staff at MSH, now known as the Icahn School of Medicine at Mount Sinai. I retired in 2019 at age 87 and traveled to Ethiopia to set up an endoscopy training program and also went to Uganda, where I began the first remote training of endoscopists via Zoom, which I am continuing.”
Gilles R. G. Monif of Bellevue, Nebraska, writes, “Just completed a new book (third in a series) on Crohn’s disease, The Prevention and Treatment of Crohn’s Disease, which is available on Amazon. This book is the summation of a 20-year collaboration between Infectious Diseases Incorporated and the University of Florida to rescue Crohn’s disease from the quagmire of autoimmunity and the rule of biologic. We now know Crohn’s disease pathogenesis and using it, how to effectively and cost-efficiently treat, prevent, and possibly cure the disease.”
John Hermos
John Hermos of Brookline, Massachusetts, writes, “My wife Rosalie and I remain in our home in Brookline, around the corner from
where I lived with Ted Parsons, Peter Clark, and Milt Pettapiece, Jr., in our third and fourth years at BU. We have three daughters (two MDs one PA) and six grandchildren. Golf, tennis, long walks and now, some Little League coaching keep me active. I am still connected to the Boston VA, where I did research in my postclinical career at the VA Cooperative Studies Program, a very rewarding conclusion to my career. Clinically, I am my sole patient, taking my medications and keeping my appointments—you know that drill. My best wishes to my classmates and other alumni. We will plan another virtual reunion soon.”
Peter Glassman of San Antonio, Texas, writes, “My 19th thriller novel is published on Kindle. Anyone Can Play focuses on the real problem of Mexican cartels kidnapping well-to-do Mexican students attending US colleges. The fictional Charles River Boston Academic is a campus similar to Boston University’s. The problem and solution involve the university, a Mexican and an American family, and collateral US citizens.”
Mark Michelman of Pinellas Park, Florida, writes, “After I graduated in 1967, I did my
internship, medical residency, and hematology fellowship at the Albany Medical Center Hospital in Albany, New York. In the middle of my training, I was called to active duty in the military and served as major in the US Army Medical Corps and as chief of Department of Clinics at Fort Benning, Georgia. After the military, I returned to Albany to complete my training in 1974. We moved to Clearwater, Florida, where I practiced hematology at three hospitals. At my main hospital, a 600-bed facility affiliated with the University of South Florida (USF), I was chief of medicine, president of the medical staff, and a member of the board of trustees.
While in practice, I also was clinical associate professor of medicine at USF College of Medicine, where I ran the hematology clinic for many years, and clinical director of the Florida Quality Improvement Organization. I served as the physician advisor for physician/hospital coding and clinical documentation at the state and national level. After clinical practice, I served as vice president of medical affairs at my main hospital until my retirement. During my career, I was very fortunate to receive several awards, including Favorite Resident during my residency, the Army Commendation Medal for meritorious service, the Excellence in Medicine Award from my main hospital, and the Distinguished Service Award from the Florida Health Information Management Association (I was the first and only physician to receive this honor). I have published several books and articles covering a variety of topics, including appropriate blood management, various roles of the physician advisor, clinical process improvement, physician and hospital coding and appropriate clinical documentation, and reducing inappropriate hospital Medicare admissions.
My wife Susan and I were very fortunate to have all our family and many friends join us in celebrating our 60th wedding anniversary this past June. We have two married children and four lovely grandchildren, ranging in age from 11 to 23. I have certainly enjoyed my career involving so many different areas. Since retirement, I have remained quite active in attending grand rounds and weekly medical webinars. Prior to COVID, I never missed a high school, college, or medical reunion. I hope to revisit my reunions starting again next year. I will never forget my four years at BU. Not

only was it a great education, but the many hospital rotations in various areas prepared me very well for my subsequent career.”
Marc Hirsch of Bowling Green, Kentucky, writes, “I retired from hospitalist work in 2011. My wife and I flew to Vancouver, British Columbia, and took ferries to the little island I lived on, off the coast, for several years in the early 1970s. We visited a former patient and her daughter, whom I’d delivered 40 years ago, and travelled around my old stomping grounds. My fifth book of detective fiction, The Case Of The Little Island In The Pacific, is set on that island and almost ready for publication. My previous books are discounted on my website (marchirsch.com) in e-book, paperback, and audiobook formats. Before I started med school in the mid1960s, I worked in the blue research building at BU under Dr. Sidney Cooperband, trying to develop an immunologic treatment for cancer. I am tickled that immunotherapy is now part of the standard protocol for cancers of many types, and I still attend a weekly tumor board at my local hospital.”
James Brasic of Baltimore, Maryland, writes, “I am busy conducting research, teaching, and providing patient care. I participated in the Ballet Essentials Workshop Weekend taught by the Education Department of the New York City Ballet in August 2023.”
Stephen Joyce of Sun City West, Arizona, writes, “Still enjoying private practice part time.”
Stephen Goldberger of Midlothian, Virginia, writes, “I’m retired in Richmond, Virginia, living near my two daughters and four grandchildren. I play golf a few times a week and recently shot less than my age for the first time. I am single, but have a new significant other who is excited to come to the reunion with me. Looking forward to trying to recognize my classmates after 50 years.”
Alice Rothchild of Seattle, Washington, writes, “Since ‘retirement’ I have been focused on writing about social justice issues. My latest book (published February 2023) is Finding Melody Sullivan, a young
adult novel exploring grief and friendship in the setting of broader political questions raised by realities in Israel/Palestine (alicerothchildbooks.com/finding-melodysullivan). I am writing and lecturing widely, have authored three books on health and human rights in Israel/Palestine, contributed to a number of anthologies and poetry journals, and directed a documentary, Voices Across the Divide.”
Larry Nichter of Newport Beach, California, writes, “Hard to believe how time has accelerated since med school. I continued with several residencies and fellowships, including general surgery at UCLA, plastic surgery at UVA, hand and microsurgery, craniofacial, and burn fellowships (board certified in three specialties), and an MS in surgery (wound healing) at UVA. An award in my name is still presented to the best research graduating medical student.
I helped launch the USC Plastic Surgery Division at Children’s Hospital Los Angeles and USC/LAC Hospital and served as director of research; we quickly grew to 27 faculty. I left in 1993 as a tenured professor and entered private practice in Orange County, with voluntary professorships at USC and UCI. I also was the department of plastic surgery chairman or vice chairman for eight years at Hoag Hospital. Still working full time and enjoy my craft.
Twenty-five years ago, I started Mission Plasticos as a development and capacity building NPO training surgeons worldwide and just returned from Kenya on my 110th volunteer training mission, the reason I cannot make the reunion. We are the only organization I know that also trains in acute burn care starting in Nepal. Through a generous grant we also have begun a domestic program across the US for free breast reconstruction for cancer survivors. I was recently honored to be invited by the Dalai Lama to speak about our organization.
I am most proud to be a dad to my three grown sons Austin, Bryce, and Travis. Finally, I have just become a grandfather, to June Anne. After my wife passed in 2002, I have not remarried. I still surf, snowboard, ski, hike, and bike when time allows. Still crazy after all these years. My best to all.”

Mardia Stone of New York, New York, writes, “On October 24, 2023, the book I coauthored, Collapse and Resiliency, The Inside Story of Liberia’s Unprecedented Ebola Response, was released by Johns Hopkins University Press (JHUP). This book presents a Liberian and African perspective of what actually happened during the response regarding the political climate, the imbalances in international public health, corruption, deception, and the influx of foreign nationals in every category, many of whom knew less about Ebola than the Liberians did. My coauthor, Tolbert Nyenswah, to whom I was senior and technical advisor, served as the incident manager of the response.
In November, the Center for Strategic and International Studies hosted our book launch and reception in Washington, DC. It has been such a joy to hold this book in my hands and finally bring this story to the world after so much time and effort. An interesting and easy read, it is available on the JHUP website, Amazon, Barnes & Noble, and other booksellers. Please support our effort and order a copy. It is worth your investment in time and purchase. Thank you.”
Andrew Wexler of Pacific Palisades, California, writes, “I continue to teach and operate as a global craniofacial surgeon primarily in low-resource countries. Over the last year I have worked in Jordan, Egypt, Rwanda, and Korea, and I’m leading an international team to Malawi in February. I was delighted to have given Surgical Grand Rounds this summer on global surgery—in the same lecture hall we sat in as med students. It’s a lot of years from the back of that room to the podium. I was blessed this spring with two granddaughters, who, along with my grandson, are my stateside focus. I remain married to Geri, the woman I met as a second-year med student.”
Scott Greenbaum of Great Neck, New York, writes, “Published a new technique to treat significant dry eye this year that I started on autoimmune patients called Punctal Plug Informed Punctoplasty.”
I. Michael Leitman of Roslyn, New York, writes, “I am now dean for graduate medical education at the Icahn School of Medicine at Mount Sinai. I am happy to continue participating in medical student education and helping our residents and fellows develop their professional careers in medicine. I was honored to receive a lifetime achievement
award from Mount Sinai’s Faculty Council and most recently, the Jacobi Medallion. I still practice general surgery.”
Stephen Corn of Sharon, Massachusetts, writes, “We are all doing well and our wonderful son is now a junior in college! Time has flown. I served for over 25 years on the faculty of Harvard Medical School and as director of clinical innovation at two of the school’s affiliated teaching hospitals. Enjoying time overseeing companies based on several of my inventions and providing multiaccredited education and the state-required medical marijuana courses for New York, Ohio, Pennsylvania, Utah, and West Virginia, among others, on the endocannabinoid system and medical cannabis through TheAnswerPage.com, the website I founded in 1998. Related to this work, I received the Special Award for Medical Cannabis Education from the International Association of Cannabinoid Medicine.”
Joshua Feder of San Diego, California, writes, “On September 28, 2023, I delivered a speech at a high-level meeting of the United Nations General Assembly in New York launching my new book with the International Networking Group on Peace Building with Young Children. I am cochair of the disaster & trauma issues committee at the American Academy of Child & Adolescent Psychiatry, executive medical director at Positive Development, and editor in chief at the Carlat Child Psychiatry Report.”
James Pomposelli of Cherry Hills Village, Colorado, writes, “Liz Pomfret (CAMED’90, GRS’90) was honored as the Seymour Schwartz visiting Professor of Surgery at the University of Rochester, the department’s highest honor. The last time we visited was during surgical residency interviews.”
Scott Dudak of Park City, Utah, writes, “Marla and I have moved to the Beehive State for some fresh air, seasons, and less traffic. Reach out if passing through Park City.”

Scott Goldstein of Dresher, Pennsylvania, writes, “Still thankful for my time at BU and all that I learned. Still in private practice in Philadelphia and teaching at the University of Pennsylvania. Proud to note that I was named the president of the Pennsylvania Academy of Ophthalmology (2023–2025) and started a second term as treasurer of the American Society of Ophthalmic Plastic & Reconstructive Surgery (2023–2025).”
Sarita Mohanty of Los Angeles, California, writes, “This year, I had the incredible privilege of joining the Forbes third annual 50 Over 50 list among 199 outstanding individuals. The recognition of age as a superpower deeply aligns with the values of the organization I lead, the SCAN Foundation. Through grants and impact investing, we’re dedicated to creating a positive impact of bold and equitable change in how older adults age in home and community.”
Ronda Rockett of Wellesley, Massachusetts, writes, “I continue my efforts to improve lives and prevent disease through nutrition and CrossFit coaching at my gym, CrossFit Launchpad. I am inspired by those who have made a global impact and seek ways to do the most good for others.”

Selene Parekh of Lawrence Township, New Jersey, writes, “Dr. Selene Parekh, a board-certified, fellowship-trained orthopaedic surgeon specializing in the treatment and conditions of the foot and ankle, has joined the Rothman Orthopaedic Institute in their Princeton, New Jersey, and Bucks County, Pennsylvania, practices. He is known for utilizing state-of-the-art implants and techniques that he has designed and developed to provide better support and offer limb salvage. Dr. Parekh also focuses on minimally invasive surgery and is a pioneer in the use of 3D printing techniques,
total ankle replacements, limb salvage, and the treatment of foot and ankle conditions in athletes.”
Daniel Oates of Quincy, Massachusetts, writes, “Looking forward to rejoining the faculty at the BU Chobanian & Avedisian School of Medicine and the geriatrics staff at Boston Medical Center (BMC). I was fortunate to gain extensive experience in the value-based care sector working in private group practices on the South Shore of Massachusetts over the past 10 years, and look forward to bringing this experience back to BMC as the medical director of senior services and partnerships, building out and enhancing the Senior Care Options program for dual eligible (Medicare and Medicaid) seniors.”
Padma Channavajhala of San Jose, California, writes, “Dear 2001 classmates, so happy to communicate with you all after a long time. Career-wise, contributing to oncology (solid tumors) with Ras(on) inhibitors. So proud to work with the company that is targeting this molectle with first-in-class drugs. Also proud to announce I worked on a Ras(off) inhibitor as well as a blockbuster drug.”

Shant Broukian of Marshfield, Massachusetts, writes, “Graduated in 2009 with my MaMS degree and from Drexel University College of Medicine in 2013. I completed an emergency medicine residency at Staten Island University Hospital in New York City in 2016 and have been a practicing emergency physician at Cape Cod Hospital ever since!”
Essence Cohen Fields of Drexel Hill, Pennsylvania, writes, “Essence Cohen Fields, LPC, is a licensed therapist in private practice, owning and operating First Love Yourself Counseling. She authored a children’s book titled That’s Not Okay! focused on preventing sexual abuse through assertiveness, advocacy, and family engagement. She also partners with the School District of Philadelphia providing mental health counseling and clinical consultation.”
Chris Wong of Weymouth, Massachusetts, writes, “I recently opened my own business as an executive coach and consultant working with nonprofits to retain, develop, and engage their high-performing employees. I also recently was interviewed for a feature in Authority Magazine. My training and edu-

cation in the Mental Health Counseling & Behavioral Medicine program have been invaluable in my career.”
TJ Dinsmore of Londonderry, New Hampshire, writes, “I live in southern New Hampshire and own a solo psychotherapy practice. I can’t extend enough gratitude to the faculty and staff of the Mental Health Counseling & Behavioral Medicine program—where I am wouldn’t be possible without their support at the front end of my career. These days I am in the midst of the twists and turns of parenting my young daughters with my wife, Kim. Proud to be connected to the BU community and wish I had more time in life to get involved!”
Stephanie Feldman of New York, New York, writes, “I am excited to share that this summer I started a new position as the director of cardio oncology at New York Presbyterian/ Weill Cornell Medical College.”
2015
Domenic Filingeri of Pittsburgh, Pennsylvania, writes, “Currently completing my pediatric endocrinology fellowship at the Children’s Hospital of Pittsburgh and working on diabetes research using mice under T32 grant-supported research.”
Miriam Segura-Harrison of Brighton, Massachusetts, writes, “This year Josh and I welcomed our third child, Tzemach. He joins big brothers Hiyya, five, and Hasdai, 12. Some of you may remember Hasdai—he was born during my first year and used to come with me to lecture! He’s getting ready for his Bar Mitzva this January. I’m also loving being a full-scope family doctor at Cambridge Health Alliance, delivering babies, watching them grow, and taking care of whole families! It’s the best work.”


Sunny Yoo of College Point, New York, writes, “I am completing my anesthesia residency at SUNY Downstate Brooklyn. Very grateful and happy to be in this field. Boston University and the people I met have helped me so much on this journey.”
Carolina Nvé Díaz San Francisco of Brighton, Massachusetts, writes, “Enrolling in and completing a master’s of science in medical anthropology was an essential chapter in my career path. My thesis was dedicated to studying perceptions of the concept of healing and illness within contexts of migration and transnationalism, representing my interest in medical systems and my experiences as a migrant in the United States. The results of my thesis have helped me design current and future research interests through my current PhD candidacy that explores the relations between culture, medicine, and mental health in the United States and Equatorial Guinea. I have published several research articles, chapters in edited volumes, and a biographical novel about my life in Spain, the United Kingdom, and the
United States. I am an editor of an academic journal and an anthropology faculty adjunct at a university. The best part is that I maintain communication with my former teachers at BU, who continue to support me in mastering the incredible values of good writing, research, publishing, and teaching. Thank you!”
Tyler Robinson of Folsom, California, writes, “In October, after 15 years of school and training, I finally started practice as a general and minimally invasive surgeon in Sacramento, California. My wife Basia and I spend most weekends chasing around our two dirty-but-happy sons, aged four and one. My first children’s book, The Higgily Hospital, was just published on Amazon!”
Maria D’Amico of Newtown, Pennsylvania, writes, “Maria D’Amico and Chase Kahn were married on September 23 in Cape May, New Jersey. They met during medical school orientation in 2016. Maria is currently a fourth-year urology resident and Chase is a fourth-year otolaryngology resident, both at

Thomas Jefferson University in Philadelphia. They were lucky to have numerous former classmates in attendance to help them celebrate their special day!”

Aileen Hickey of Boston, Massachusetts, writes, “I’m happy to share that in March 2023, after working for many years in the Boston Public School system as a school-based outpatient therapist, I have opened my own private practice called Aileen Hickey Therapy! I provide individual outpatient therapy for children, adolescents, and young adults struggling with anxiety, depression, stress, life transitions, PTSD, grief, and learning disabilities, to name a few. It has been amazing and very rewarding!”
Saba Chowdhry of Boston, Massachusetts, writes, “As a COVID-era graduate, I think back to the moment I defended my dissertation over Zoom from my apartment. Those were uncertain times, highlighted by the unusual setting of my defense, and I really didn’t know what was in store for me next.
I left academia to broaden my horizons in industry. In my current position, I lead vascular clinical research at a unicorn startup that brings artificial intelligence-based solutions into healthcare. I curate real-world evidence on the performance and clinical impact of our solutions on hospital workflow efficiency and patient outcomes. I am grateful for my time at BU that sharpened my scientific knowledge and research skills, as they are the foundation I rely on every day in my role. Outside of work, you can find me on the racquetball court, baking something sweet, or trying not to lose at TV trivia. After graduation, I set a goal to travel more. So far in 2023, I’ve visited Norway, Greece, Italy, Mexico, Honduras, and the Bahamas. I hope to travel more in 2024.
I would love the opportunity to meet fellow alumni and grow my network. Please don’t hesitate to connect. Wishing you all success in your endeavors!”
Daniela Toledano of Miami, Florida, writes, “Following my BU journey, I completed my post-graduate clinical hours and am proud to be a licensed mental health counselor in Florida.
My path led me to Rogers Behavioral Health, where I specialized in Obsessive-Compulsive Disorder (OCD), anxiety,
and depression through a partial hospitalization/intensive outpatient program. Today, I’m thrilled to announce my private practice, focusing on exposure and response prevention for OCD and anxiety disorders. Tailoring treatments to individual needs, I employ cognitive and dialectical behavioral therapy approaches with a primary focus on teens and young adults, serving both Spanish and English-speaking clients. I’m passionate about making a positive impact on mental health and look forward to what the future holds.”
Clara Zundel of Detroit, Michigan, writes, “Clara Zundel, PhD, received the prestigious Ruth L. Kirschstein Postdoctoral Individual National Research Service Award from the National Institute of Mental Health to support her training and research into how air pollution exposure impacts brain development and risk for anxiety disorders in youth.” ●

June Jackson Christmas of Manhattan, New York, a trailblazing psychiatrist who served under three New York City mayors and as a Black woman, broke barriers by heading the Department of Mental Health and Retardation Services, died in the Bronx, New York, on New Year’s Eve. She was 99.
Born June Antoinette Jackson in Cambridge, Massachusetts, Christmas received her BS in zoology from Vassar College in 1945, where she was one of the first three Black women to graduate from the college, and her MD from Boston University in 1949, where she was one of only seven women in her class. She completed psychiatric residencies at Bellevue Hospital and Queens General Hospital in New York City.
Christmas was chief of the group therapy program at the Harlem Hospital Center and in 1964 founded the Harlem Hospital Rehabilitation Center, a community organization that trained Harlem residents in how to help psychiatric inpatients transition back into society.
In 1971, Christmas began a storied teaching career at Columbia University as a clinical professor of psychiatry at the College of Physicians and Surgeons. She also was a professor of behavioral science at the City University of New York, where she founded the Urban Issues Group think tank, and resident professor of mental health policy at the Heller Graduate School of Social Welfare at Brandeis University.
In 1972, New York Mayor John Lindsay appointed Christmas commissioner of Mental Health and Retardation Services, and she was subsequently reappointed by Mayors Abraham Beame and Ed Koch. A health advisor to Jimmy Carter’s presidential campaign, she served on his transition team and was a member of New York Governor Mario Cuomo’s Advisory Committee on Black Affairs. In 1980, Christmas became the first Black woman to be appointed president of the American Public Health Association.
Her civil rights activism was rooted in childhood experiences. In a 2017 StoryCorps interview Christmas recalled her father—a postal worker who struggled for two decades to get a promotion despite top civil service test scores—and his campaign to allow Black postal workers to join the union. Her mother also worked to fight segregation in Cambridge and Boston in the ‘40s and ‘50s. Later, Christmas and her husband Walter were involved with the Student Nonviolent Coordinating Committee and opened their New York City home to students from Africa and the United Nations. They also brought a case against the city that resulted in changes to the Fair Housing Act in New York.
Christmas was active at Boston University as well, working with the National Association of Interns and Medical Students to push for national health insurance and the rights of Black doctors to have hospital admitting privileges.
“It seems to me that I’ve often been in places where if you wanted to make life better for yourself, you had to work to make life better for everybody,” she said.
The Christmas-Eastman-Fuller Scholarship at the Chobanian & Avedisian School of Medicine was established in May 2018 by Elizabeth C. Dooling (CAMED’65) in honor of Christmas; Charles Eastman (CAMED1890), one of the first Native American physicians; and Solomon Carter Fuller (CAMED1887), an early pioneer in Alzheimer’s disease widely recognized as the first Black psychiatrist. The scholarship benefits medical students from underrepresented populations.
Christmas leaves her daughter Rachel, her son Gordon, and four grandchildren. Her husband Walter and son Vincent preceded her in death.
Donald Perlman of Swampscott, Massachusetts, on July 20, 2023, passed away peacefully at his home after a long and valiant battle with ALS, with his beloved wife Cynthia and youngest daughter Victoria at his side. Dr. Perlman also leaves his daughter Lisa and her husband Alan, son Timothy and his wife Amy, and grandchildren Isabel, Jacob, and Zachary, as well as his caregivers Carmen, Ramona, Lucy, and Jeimy. He lived an extraordinary life of giving and sacrifice.
Following medical school at Boston University, he trained at Case Western Reserve University Hospital in Cleveland before beginning his surgical career as a captain in the United States Army, stationed at Fort Jay in New York and Fort Devens in Massachusetts. He was a clinical instructor in surgery at Harvard University School of Medicine and on the staff at Massachusetts General Hospital, where he trained a generation of surgical residents from 1962 through 1987. Dr. Perlman truly loved medicine and practiced surgery faithfully in Lynn, Union, Saugus, and Salem hospitals for more than 50 years, until he retired at the age of 84. His patients always came first in his tireless quest to heal them. Dr. Perlman loved his office staff, with whom he worked for the greater part of his career.
He greatly respected his fellow doctors, nurses, and hospital staff, and looked forward to working with them every day. He most delighted in his family, with whom he spent the happiest moments of his life. He will be remembered with deep love and admiration and will be dearly missed.
Richard C. Newell of Bloomfield, Connecticut, Gilford, New Hampshire, and Naples, Florida, on September 22, 2023, peacefully in his sleep at McLean Health Center in Simsbury, Connecticut. He had recently celebrated his 95th birthday with his beloved family. Richard was the loving husband of 66 years to the late Beverly Newell and the son of Albert and Edna (Kidder) Newell.
A devoted son, husband, father, grandfather, brother, and uncle, Richard had a warm personality, a bright smile, a great sense of humor, and a deep sense of humility and service. He was a dedicated physician to multiple generations of patients throughout the area. He represented a traditional family doctor who knew his patients well and made regular house calls, even to remote farms, back in the day.
Richard grew up on New Hampshire’s Lake Winnipesaukee, swimming, boating, water skiing, and fishing on the “Big Lake,” and snow skiing and hiking on nearby mountains. He was the captain of the Laconia High School basketball team, played the piano, and sang in the choir at the Congregational Church of Laconia.
Richard served in the Army during World War II as a surgical technician, invaluable experience to his future in medicine. Following WWII, he attended Boston University as a premed student, where he also rowed on the varsity crew team. After graduation, he worked at Massachusetts Memorial Hospital in Boston before gaining admission to medical school at Boston University. In 1950, he met his future wife in Boston, where she was studying at Wheelock College.
After earning his medical degree in 1956, Richard completed his medical residency and internship at Hartford Hospital in Hartford, Connecticut. In 1960, he opened a private practice in internal medicine in Bloomfield, Connecticut, where he raised a family with his wife and treated patients for nearly 30 years. Board-certified in internal medicine, a member of the senior staff at Hartford Hospital, and a member of the Endocrine Group and Teaching Rounds staff, he also served as medical director at the Bloomfield Convalescent Home for 25 years and as assistant medical director at the Duncaster Retirement Community.
Richard served as president of the Civitan Club of Bloomfield and as a deacon at the First Congregational Church of Bloomfield, where he and Beverly were keenly involved and made lifelong friends.
Upon his retirement, Richard and Beverly spent summers in Gilford, New Hampshire, and winters in Naples, Florida. Finding nonworking life a bit slow-paced, he became a real estate agent in New Hampshire and Florida, embarking on a second career that lasted 17 years. During this time, he also served as an incorporator for the Lakes Region General Hospital and the Taylor Home in Laconia, New Hampshire. An avid golfer and tennis player, he also enjoyed boating, traveling, and cherished time with family and friends.
The couple eventually returned to Connecticut to be closer to their growing family, ultimately residing at McLean in Simsbury,
where they received loving care from the wonderful nurses, aides, and other staff.
Richard is survived by his daughter Jan Newell Spears and her daughter Jasmine; his son Randy Newell, his wife Karen, and their three sons Matthew, Ryan, and Christopher; and his daughter Wendy Newell Hunt, her husband Patrick, and their two children, Lila and Patrick. He was dearly loved and will be greatly missed.

Burton White of Hillsborough, California, on August 7, 2023, at his home in Hillsborough, California, at the age of 87. He was born in Boston and attended Boston Latin School, Harvard College, and Boston University’s medical school. He interned at the LA County Hospital where he met his wife, June. When he was accepted to the Harvard Psychiatric Residency Program, he and June returned to Boston, where they married in 1962. The Vietnam War was ramping up, and after completing his specialty training, Burton was assigned to Clark Air Force Base in the Philippines as a psychiatrist.
After returning to California, Burton worked as the regional chief at the Daly City Mental Health Center before going into private practice in San Mateo with a special interest in senior care and community issues. In the mid-1980s, he was named chief of psychiatry at Peninsula Hospital and became involved in several mental health committees that effected real change. He was honored as a Distinguished Life Fellow by the American Psychiatric Association in 2016 before retiring at age 80.
Music was always one of his passions and he loved traveling with June, with whom he saw the world. Starting in 1987, they spent winters in Cabo San Lucas.
He leaves his wife June, sister Eunice, and nephews Jonathan and Jeffrey, along with grandnieces and nephews Brianne, Hayley, Drew, Lindsay, and Brody

Harry W. Bennert Jr. of Scarborough, Maine, on July 18, 2023, at the Scarborough Veterans’ Home.
He was born in 1936 in Manchester, New Hampshire, the son of Elizabeth Florence McIntire and Harry W. Bennert, MD, and educated in Manchester public schools. He majored in religion at Bates College, graduating in 1958. In 1961, he married Joan Marie Nolet of Auburn in the Bates Chapel; they welcomed
sons Eric and Jeffrey in 1967 and 1969, respectively. After serving as assistant alumni secretary at Bates for two years, he attended medical school at Boston University, graduating in 1965. He did his internship and one year of general surgery at Maine Medical Center in Portland.
As the Vietnam War raged, he joined the Navy as a medical officer and served on the USS Providence-CLG 6 for two years, on the 7th Fleet Flag Ship home-ported in Yokosuka, Japan.
After satisfying the active-duty requirement, Harry moved his family to Massachusetts, where he became a resident in obstetrics and gynecology at the Boston Lying-In Hospital in Boston (now Brigham and Women’s). In 1972, the family relocated to Falmouth, Maine, and Harry began his practice at Maine Medical Center.
During this time, Harry initiated a study to identify high-risk pregnancies in order to improve the outcomes. With the overwhelming cooperation of the actively practicing doctors in Maine providing obstetrical care, the Maine Fetal Risk Project was able to gather information on 12,817 pregnancies. Harry also developed the Maine Diabetes and Pregnancy program, which concentrated on physician education. All of this contributed to the development of a high-risk pregnancy program at Maine Medical Center known as Maternal Fetal Medicine. He continued to maintain an active teaching schedule and practice until he retired from medicine at the age of 67.
Following retirement, he pursued his lifelong dream of becoming a Christian minister in the United Church of Christ, graduating from the Bangor Theological Seminary in 2009. Sadly, his dream was cut short when he was diagnosed with Alzheimer’s disease.
Harry loved the water, boating, and spending summers on Lake Winnipesaukee in New Hampshire, where he met his future wife. After moving to Maine, he became a member of the Portland Yacht Club and was named a commodore.
He was a member of the Foreside Community Church, where he sang in the choir. He is a founding member of two quartets, the Deansmen at Bates and Doc Bennert’s Quartet aboard the USS Providence
He is survived by his wife of 62 years, Joan; his sons Eric “Huck” Bennert and his wife Alex, and Jeffrey Bennert and his fiancée Beth Andrews; and three grandchildren, Jacob Tucker, Katherine Elizabeth, and Thomas Watson.

William
of Taos, New Mexico, on October 8, 2023, peacefully at home. Known for his warmth, humor, and universal kindness, Bill opened his heart to everyone he met. He had a knack for finding a way to connect with people from all walks of life, initiating conversations, listening carefully, and sharing stories freely.
Bill was born in Montreal, Québec, to William R. and Marcelle A. Christmas. The family immigrated to West Springfield, Massachusetts, and subsequently to the greater Boston area, where Bill
attended Rivers preparatory school. After graduating from Bowdoin College, he attended medical school at Boston University, graduating in 1965. He completed his internship at Sinai Hospital of Baltimore and his residency in internal medicine at the University of Vermont, where he was also an NIH Fellow in Infectious Diseases. Bill married Maribeth Hanson in 1962 and started a family; their son Jamie was born in 1965.
The highlight of Bill’s residency training was a two-month practicum taken at the Hospital Albert Schweitzer in Deschapelles, Haiti. The hospital allowed Maribeth, a registered nurse, to serve on staff as well. Caring for patients suffering from starvation and other maladies associated with living under a repressive dictatorship left a deep impression on both.
The family continued to grow as Bill began his career as a physician specializing in internal medicine. He served for three years (1969–1972) on active duty in the Army, working at the US Medical Research Institute of Infectious Diseases in Frederick, Maryland. Daughters Ann (1968) and Gillian (1969) arrived and the family moved to Bennington, Vt., where Bill began a private practice in internal medicine with several other doctors (1972–1977). Bill and his colleagues doggedly built up their practice to the point where expansion was necessary to meet patient demand.
Although Bill had helped build a successful practice and enjoyed clinical work, he and Maribeth decided to leave private practice for the more regular hours promised by a position in college health when son Ira joined the family in 1974. He apprenticed at University of Rochester health services (1977–1981), eventually becoming medical director there, leading to director of student health positions at the University of Vermont (1982–1993) and Duke University (1994–2004). He received a lifetime achievement award from the American College Health Association (ACHA) in 2005, the year he retired.
Sadly, Bill lost Maribeth to cancer in 2001. After mourning her and the plans they had made together, he reconnected with Polly Raye, whom he’d known since junior high school. They married in 2003 and Bill relocated to Taos, New Mexico. Spending time with their blended family, including 10 grandchildren, was the couple’s top priority as they traveled from coast to coast for visits. They also took trips abroad and cherished their rich and gratifying friendships at home. Bill traveled extensively as a consultant reviewing many student health programs for the ACHA and several volunteer health programs for the US Peace Corps, the latter taking him to exotic locales in the South Pacific and Africa.
Bill and Polly enjoyed camping in their RV and cross-country skiing. He loved water, particularly swimming and canoeing, wood fires, baking yeasted breads, and singing (at Bowdoin he sang in both the Glee Club and Chapel Choir, and in later years, brought his beautiful deep bass voice to many a church choir). He was also a voracious and careful reader, especially of history

Marcia F. Katz of Winter Park, Florida, on March 26, 2023, after a three-year battle with pancreatic cancer. She died as she lived, fiercely smiling, wearing her signature blue glasses, surrounded by family, and mouthing the words to James Taylor songs. After graduating at the top of her class from Cranston West in Rhode Island, Marcia earned a bachelor’s in biology at Brown University, where she fostered a joyous community and friendships that will endure beyond her life. She embarked on her medical education at Boston University, completing an internal medicine residency at Boston City Hospital followed by a pulmonary and critical care fellowship at BU’s Pulmonary Center.
Throughout her career, Marcia strove to reach new heights, and at 4’9,” her five-inch heels helped her do so. She served as Baylor College of Medicine’s associate chair of medicine for clinical affairs and medical director in the department of medicine. She also was chief of adult medicine at Texas Children’s Pavilion for Women and spearheaded the development of Baylor’s Lung Institute.
Marcia had a profound impact on the Cystic Fibrosis (CF) community. She was medical director of the Baylor Maconda Brown O’Connor Adult CF Center and sat on the center committee of the CF Foundation, the governing body of CF center accreditation. She also served as coprincipal investigator of the CF Therapeutic Development Center.
In 2016, Marcia left Houston to live among the colorful flora and fauna of Winter Park, Florida, including the peacocks and turtles. After a nationwide search, Marcia was hired as associate dean of clinical affairs at University of Central Florida (UCF) College of Medicine. During her time there, she worked closely with UCF hospitals and the community to build an academic clinical service system that will benefit patients and students for years to come. When Marcia retired in 2020 to spend time with her family and travel the world, she’d earned the title of UCF Professor Emerita.
Dr. Katz’s most treasured accolades came from her patients, who often credited her clinical excellence, boundless encouragement, and unwavering advocacy for helping them live longer and healthier lives, raise families, and achieve their dreams. Since Marcia’s diagnosis, countless patients have reached out to express their gratitude to her for saving their lives. In 2012 she was bestowed with Baylor’s highest honor given to a medical school faculty member, the Ben and Margaret Love Foundation Bobby R. Alford Award for Academic Clinical Professionalism, in recognition of her outstanding humanism.
While working as a full-time physician, Marcia was also a fulltime mom to her two daughters, Becca and Jess. She never missed a weekly Kabbalat Shabbat sing-along or the opportunity to take her girls shopping. On their car rides home, they blasted Shania Twain and Gloria Estefan, belting the words while laughing hysterically. Marcia did everything for her daughters, and loved them unconditionally. As
Marcia faced cancer, Becca and Jess were by her side, laughing at her dark humor and hugging her tightly.
Marcia Katz squeezed life out of every moment. During the last few years, she became an avid gardener and birder, spending many happy days harvesting her tomato plants and watching the cardinals living in her bougainvillea.
Marcia is survived by her daughters Becca and Jess Wolinsky, mother Trudy Katz, twin Debra Katz, sisters Elyse and Michelle Katz, husband Asher Aremband, nephew Sammy Bienenstock, brothersin-law Michael Bienenstock and James Darrish, stepdaughters Lisa Blumenband and Jody Aremband, and grandcat Tushi.

Michael A. Posternak of Greenland, New Hampshire, on July 2, 2023. Michael grew up in Lexington, Massachusetts, the son of Noel and Carlotta (Krohn) Posternak. He attended Phillips Academy Andover and Trinity College in Hartford, Connecticut, where he majored in philosophy, and received an MD from Boston University. He completed his residency in psychiatry and fellowship in mood disorders research at Brown University and spent two years working at the Massachusetts General Hospital Depression Clinical and Research Program before entering private practice in Wellesley, Massachusetts, where he stayed for the remainder of his career.
Believing that veterans gave to our country much more than our country gave back to them, for the past 10 years he volunteered his time to the Give an Hour foundation, which offers free mental health services to veterans in need.
Dr. Posternak published over 50 peer-reviewed articles in psychiatric journals. He served on the editorial board of The Carlat Report for the past 15 years and was a frequent contributor.
Dr. Posternak was very active playing tennis, golf, hockey, and skiing. He loved nature, worked to protect the environment, and was an avid reader of history and science. He leaves behind his children Alysha and Zach, brothers Barry and Daniel, and many nieces and nephews. ●

Giving to Boston University in your will is a simple way to make a real difference.
It’s easy—and rewarding. Take the time now to make sure that your will reflects your intentions to care for your family and the people and causes that matter most to you.
If you include a gift for BU in your estate plans, you will have the satisfaction of knowing that future generations of students will benefit from your generous legacy.
To learn more about how you can make a gift in your will to support BU, contact Boston University Planned Giving at 800-645-2347 or opg@bu.edu, or visit bu.edu/plannedgiving.
Download a complimentary copy of our Estate Planning Guide at bu.edu/estateguide.