











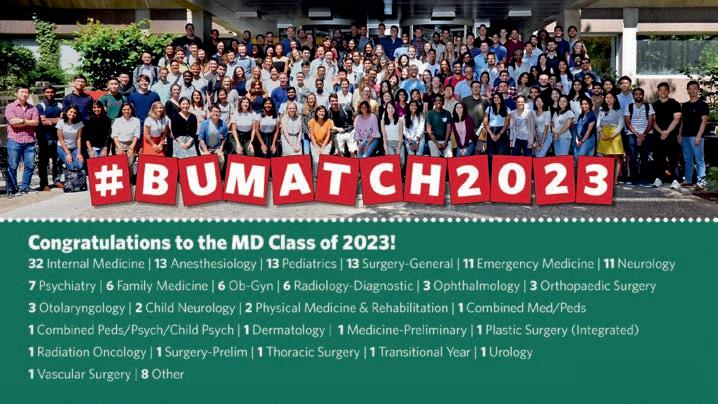
Fourth-year medical student Kenya Homsley felt nervous as she stood in front of the rows of long white envelopes laid out on banquet tables. In a 71-year-old ritual known as Match Day, at noon on the third Friday of March, thousands of medical school students nationwide open envelopes to discover where they will spend the next four to seven years training in a hospital or other medical setting.
“Deep down, even with all the nerves, I do feel like I’m ready. There’s so much more to learn, but I’m right where I’m supposed to be,” said Homsley. A native of Charlotte,
North Carolina, Homsley matched with her first choice, obstetrics and gynecology at Kaiser Permanente Oakland Medical Center in California.
Matches are based on an algorithm that pairs students with medical facility residency programs based on preference lists developed by both the students and the schools through rigorous application and interview processes. Under supervision, residents diagnose, manage care, and treat patients in their specialty, with increased responsibility over time.
“You will now be at the front lines. You will be the doctor that the patient will trust,” said Priya Garg, MD, associate dean for medical educa-
tion, urging students to remember the social mission that drew many of them to the school when they become residents and physicians.
“Many of you came in here loving social justice, equity. That was your journey to us, and that’s been your journey with us,” Garg said. “Do not forget your role in changing the way medicine will be forever. Use your voices and the power you have as a doctor.”
“On behalf of the faculty, I am delighted to congratulate you on reaching your Match Day,” said Dean Karen Antman, MD. “Most of you arrived at medical school in August 2019. You had a conventional medical education for the first semester and a half, through Feb-
ruary 2020, anyway. Then, COVID upended your education, starting with studying for and taking the Step 1 exam. Your clerkships were a totally unique experience.
“In addition to medicine, you learned flexibility and creativity—important skills in medicine—as well as disaster management, up close and personal,” Antman continued. “I’m pretty sure your generation of physicians will be distinctive.”
Originally from Ohio, Jyla Hicks graduated from North Carolina Central University and came to the school to work with underrepresented and marginalized patient populations. She was pleased to match in internal medicine with BU’s primary teaching affiliate Boston Medical Center (BMC).
“Just to have the privilege to continue to serve those systematically marginalized populations is my goal,” Hicks said. “I know, especially with the minority populations, it’s really important for patients to see providers who look like them, so I love that I’m adding diversity to the already diverse BMC staff.”
There was a point in his medical school education when Madhav Sambhu thought he may not have what it takes to be a doctor. But he took an extra year, switched his focus to neurology, and through mentors and family support, stayed motivated and hopeful. On Match Day, his efforts paid off as he matched at Emory University Hospital in his hometown of Atlanta.
“I struggled a lot, and I think there was a point at which I didn’t know if I was going to be a doctor. Today, I realized it was possible— that I’m going to do this,” he said.
Carolyn Wilson of Long Island, New York, who studied at Boston University for seven years as an undergraduate and medical student, matched in internal medicine with New York University Grossman School of Medicine and looks forward to working in a city hospital with similar clientele to BMC. “During that hour waiting to open up your envelope, your nervousness peaks,” she said. “I’m excited to be going back home after such a long time.”
Following graduation, 37 medical students will stay in Massachusetts, including 18 at
BMC, five at Beth Israel Deaconess Medical Center, four at Massachusetts General Hospital, two each at Brigham & Women’s Hospital, Children’s Hospital Boston, UMass Chan Medical School, and Tufts Medical Center, and one each at Cambridge Health Alliance and St. Elizabeth’s Medical Center.
New York (22), California (17), and Connecticut (10) were the next most popular matched states. The class matched in a range of programs, with internal medicine (32), anesthesiology, pediatrics, and general surgery (13 each), and emergency medicine and neurology (11 each) as the top specialties. ●

2023
Match by State and Specialty
“Do not forget your role in changing the way medicine will be forever. Use your voices and the power you have as a doctor.”
PRIYA GARG, MD, ASSOCIATE DEAN FOR MEDICAL EDUCATION
As the school celebrates its 175th anniversary, the Class of 2023 is the first class to graduate from the newly renamed Chobanian & Avedisian School of Medicine.
Medical Campus Provost and Dean Karen Antman, MD, addressed students, family, and friends gathered at the BU Track & Tennis Center for the Chobanian & Avedisian School of Medicine convocation ceremony on May 18.

Describing the 2023 MD and PhD graduating class as “creative, flexible, and resilient,” Antman spoke of the global pandemic that upended their lives and graduate education while also revealing disparities within the healthcare system. She cited wars and tensions around the world that have escalated and refugee numbers that have increased, “with many in our own patient populations.”
“In addition to science and medicine, you learned flexibility, adaptability, and creativity—important skills in both science and medicine, as well as in disaster manage-
ment—up-close and personal,” Antman said.
The school conferred 29 PhDs, 149 MDs, nine MD/PhDs, three MD/MPHs, and three MD/MBAs. Graduates ranking at the top of their class included 16 cum laude, five magna cum laude, and two summa cum laude graduates, Joshua Gustine and Flaminio Pavesi.
C. James McKnight, PhD, associate provost and dean of Graduate Medical Sciences, advised graduates to “continue to make a difference in the world, in your families, and in your communities. Be involved, take care of the world, be engaged, and speak out with your opinions. Your hard work here has prepared you, and we are confident that you have the necessary will, the courage, and the tools to make a difference in all our futures.”
One of many medical students who stepped up to help during the pandemic, graduating MD student speaker Divya Satish-
chandra and her peers started a call center for Boston Medical Center (BMC) patients to connect them with community resources.
Satishchandra aspires to a career in cardiology and will complete her residency at BMC.
“There will always be more to do, more to learn, more to innovate, more to fix. The field of medicine is ever-expanding and infinite,” she said.
She spoke of experiences like holding a human heart in anatomy class, the awe and existential dread of the learning process, and the tests that could open or close a door on a future career, all giving way by year three to the intangibles of patient care.
“We quickly learned that although multiple choice questions have one answer, real patient care involves multiple answers, or sometimes no answers. I think we’ve all learned that to be a physician is to embody qualities that may never be truly captured by a number, or any single outcome,” she said.
PhD student speaker Michael Breen noted that despite the array of degrees being awarded and the diverse careers represented,



“We are all bound by a common cause: the health and well-being of humankind.”
“The world, potentially now more than ever, needs caring and compassionate doctors and researchers,” said Breen, who received his PhD in microbiology with a focus on immunology and infectious diseases.



“During the pandemic, we all came together…in incredible ways. Selflessly, and before vaccinations were available, we all were on the forefront of the mass testing program, helping patients in any way we could and researching new treatments and diagnostics.”
Advising graduates to also credit themselves as they thank those who helped them along the way, Breen said, “There is no being here without your hard work, tenacity, and sacrifices.”
“There will always be more to do, more to learn, more to innovate, more to fix. The field of medicine is ever-expanding and infinite.”
STUDENT SPEAKER DIVYA SATISHCHANDRAAlissa Frame, MD/ PhD’23, gets hooded by Dr. Richard Wainford. Faculty Marshal David Greer, MD, chair and chief of neurology, leads the faculty into the MD and PhD convocation ceremony, followed by Dean Karen Antman and speaker Rochelle Walensky. Graduating MD students listen to remarks during the convocation ceremony.
General Hospital and studied vaccine delivery and strategies to reach underserved communities, spoke of the need to heed those who go largely unheard.
“Barriers may stand in the way of those we work with and care for, like poverty, poor housing, and unsafe or unhealthy environments, as well as lack of access to good jobs, quality education, and comprehensive, high-quality healthcare,” Walensky said.
“With your newly minted degrees, you have knowledge, you have wisdom, you have stature, and you have privilege,” Walensky continued. “And, I would argue, you now have a responsibility to not just use your voice for your own advocacy, but to use it for those who cannot otherwise advocate for themselves.”
She pointed out that the choice to listen and speak up requires the sacrifice of one of a physician or scientist’s most precious commodities: time.
“It will mean that when someone conveys an uncomfortable professional interaction that is so easy to gloss over, you will instead ask to hear more, unpack the details, sit with your colleague through their tears—even when you are overbooked with experiments and meetings,” she said.
Walensky advised graduates to be intentional about how they use their time and voice, and to use them for a purpose and for good.
“I ask you to use your voice to end the practice of marginalizing people, clinically and professionally, based on their identity,” she said. “I ask you to use your voice to eliminate the structural barriers to opportunity for everyone in this country. And I ask you to use your voice and the power of your research and your data to drive equity in policy change.
“Never in our history have our voices been so mightily important. You and I are so fortunate to be living in such an exciting time where great work and meaningful change for people of all communities and all backgrounds can happen not by accident, but because of your devotion; because you used your voice, and it rings clear.
“Keep your voice strong. Consistent. Compassionate. Be courageous and never give up.” ●
Centers for Disease Control & Prevention (CDC) Director Rochelle Walensky, MD, MPH, addressed MD/PhD graduates and their guests at the Convocation Ceremony on Thursday, May 18. Here, Walensky answers questions from students and faculty about her journey, women in leadership roles, lessons learned from the pandemic, and other issues facing our nation today.
Q. Please share with us how you got to where you are today.
A. My passion for public health became clear in 1991 during the AIDS crisis when the disease ravaged inner-city Baltimore, where I was completing my medical training. I remember admitting countless patients and feeling hopeless because we had little to offer clinically and therapeutically in the early day of the AIDS endemic. Challenging and touching conversations with patients ignited my call to service and fight against disparities. I would routinely call on those moments as a professor at Harvard Medical School, chair of the NIH’s AIDS Research Advisory Council, chief of infectious diseases at Massachusetts General Hospital, and even today as the CDC director. My passion for disease prevention and treatment has remained steadfast, and I’m grateful to the mentors and collaborators who have helped me help others.
How do you feel about women in leadership roles?
Women in leadership are integral to producing fresh perspectives and new ideas. We must continue to offer opportunities, and support women in fields where they are underrepresented. Inclusivity throughout our public health workforce is
how we can create the best outcomes. This is why it is important that our workforce be as diverse as the communities we serve.
What are your biggest lessons learned during the pandemic or knowing what you know now, what would you have had the CDC do differently with regard to the COVID pandemic response?
I know the word is overused at this point, but the pandemic was truly unprecedented. Never in the CDC’s 76-year
history has the agency been forced to make decisions so quickly with limited and changing science. Before COVID-19, public health was somewhat unknown and chronically under-resourced. In addition, traditional scientific and communication processes in the context of a frail public health infrastructure left us woefully unprepared for the size and scope of COVID-19. At CDC, we are building on the lessons learned from COVID-19 to improve how we deliver our science and programs. These include:
“Women in leadership are integral to producing fresh perspectives and new ideas. We must continue to offer opportunities, and support women in fields where they are underrepresented.”
Sharing scientific findings and data faster: Release scientific findings and data more quickly in response to the need for information and action, as well as being transparent about the agency’s current level of understanding.
Translating science into practical, easy-to-understand policy: Enact a standardized policy development process for implementing guidance documents and other public health communications.
Prioritizing public health communications: Prioritize and enhance public-facing health communication practices and staff expertise.
Promoting results-based partnerships: Work more effectively with our public health partners to accomplish result-oriented goals and address the limitations of a siloed approach to solving major public health problems.
Developing a workforce prepared for future emergencies: Focus on diversity, equity, inclusion, accessibility, and belonging to strengthen the CDC workforce’s response to infectious and noninfectious public health emergencies, including new skills, training, capabilities, and aligning incentives for commitment to these efforts.
How has the COVID-19 pandemic changed your thinking about how to handle emerging infectious diseases?
The COVID-19 pandemic highlighted CDC’s role as a response agency. CDC is an exceptional science-based agency; traditionally, the agency has taken a more academic approach to our work. However, during the COVID-19 response, we learned that we must be a response-based agency, too, that can quickly respond to any emerging public health threat. I made this a priority for the agency to critically reflect on and implement lessons learned so that we can better prepare for future health threats. Through the initial implementation of my Moving Forward initiative, CDC is now disseminating science faster, communicating more efficiently, and becoming more of a response-based agency.
Given the gravity of the opioid epidemic and overdose-related deaths, how might it
be possible to create a national dashboard for reporting opioid-related deaths in as timely and detailed a method as we were able to achieve for COVID deaths?
CDC uses multiple sources to track the drug overdose epidemic. Examples of these systems include the Drug Overdose Surveillance and Epidemiology System and the Unintentional Drug Overdose Reporting System. CDC’s National Center for Health Statistics also provides monthly provisional drug overdose death counts.
CDC’s Overdose Data to Action initiative supports collecting and using this data to inform prevention and response efforts like prescription drug monitoring programs, community-level interventions, empowering individuals, and developing partnerships with public safety experts.
states becomes complicated and limits what we can provide in a timely manner concerning the national picture of overdose-related health outcomes.
What can be done to bolster faith in the CDC amongst groups that have turned away from science during the COVID-19 pandemic?
So much about trust is really about accountability. To bolster faith, we are acknowledging past mistakes and showing how we are working to do better in the future. This is a key focus in the CDC Moving Forward initiative I launched in August 2022. The priorities of Moving Forward include sharing data and decisions quickly, communicating uncertainty and developments, and sharing science and guidelines directly.
CDC has already started to put these priorities into action in response to recent public health threats. During the mpox response, CDC prioritized making timely data publicly available through web postings of key data finding including results of the American Men’s Internet Survey on behavior change and an early look at vaccine performance data. In both cases data were posted online even before they were packaged for publication. Similarly, CDC has continued to make timely and transparent data available on avian influenza through multiple and ongoing updates to our Avian Influenza Technical Report.
CDC is committed to building on trust through good science, good recommendations, and a good relationship with the public.
While CDC can get a national picture of overdose deaths from the National Vital Statistics System, this data can take time to collect and finalize. The additional data dashboards fill in some gaps, but the agency does not have the authority to require states to report specific, standardized data on overdose outcomes. As it does for most of its data, CDC relies on different surveillance systems, voluntary data sharing, or individual data use agreements to gather information from states and jurisdictions. Without standardized reporting, sharing and comparing this data across jurisdictions, cities, and
At CDC, our recommendations and public health decisions are based on science and protecting people. We must also recognize that public health policy impacts everyone and consider multiple perspectives. Coordinating across the government is critical when implementing our science-based policies.
As CDC director, I prioritized one-on-one conversations with legislators of all political parties so that they understand where we are coming from and what our science is
“I know the word is overused at this point, but the pandemic was truly unprecedented. Never in the CDC’s 76-year history has the agency been forced to make decisions so quickly with limited and changing science.”
telling us. I emphasize the significance of public health, the role of CDC, and the need for government support to protect our country’s health and security. Public health is a critical component of policy making, and it is important that CDC has a seat at the table and a voice in key decisions impacting the nation’s health.
Science has become politicized with results frequently cast as true or untrue. How can scientists communicate their level of uncertainty about their research…is there a way to cultivate an educated consumer base that understands how science works? Do you have any examples of scientists who are doing that now?
I have learned about the importance of communicating limitations and uncertainty

throughout the pandemic and during my time as CDC director. Ambiguity is a normal part of science and a fact of life; people deserve to know when they can expect changes. Part of CDC Moving Forward is communicating directly with the public using plain language and understandable resources. COVID-19 and mpox showed us that partnering with a diverse group of trusted messengers is critical in sharing our science and recommendations. To cultivate an educated public, we must earn and sustain their trust, prioritize diversity and accessibility, and be honest and thorough when uncertainty arises.
We should approach firearm injuries and deaths as a public health issue to accurately capture the complexity, urgency, and need for solutions. It must be understood that there is no single cause or solution to gun violence and that circumstances and needs vary across the country. Furthermore, it is important to recognize that, like many other public health issues, gun violence is often the result of poverty, racism, gender inequality, and other underlying social determinants. When we have this conversation in the context of a comprehensive public health framework, evidence-based solutions that protect individuals, families, and their communities become more conceivable.
Implementing safer public health policies is a team effort, requiring support from various partners. Looking through a public health lens, we recognize that we need to engage everyone on this topic, from gun owners to law enforcement. At CDC we have invested in research in this area spanning from firearm suicide prevention to safe storage of firearms in the home.
We all share the same goal of preventing adverse outcomes; let’s find areas where we agree and promote safe practices and interventions that can save lives.
What role can the CDC play in addressing the physician and healthcare worker shortages in rural areas?
A robust public health infrastructure requires a diverse workforce representing the communities they serve regardless of zip code. We are establishing the Office of Rural Health to build on our existing rural health work and provide a home for focused action and leadership. The goal is to integrate the best science and solutions to ensure that rural health needs are reflected in public health programs. We plan to make the most of this opportunity by developing a strategic plan, establishing federal leadership, integrating rural health into our major programs, and collecting better data to propose better solutions. A well-resourced environment and healthcare system are essential in attracting and retaining physicians and healthcare workers in rural areas. ●
The annual commencement ceremony celebrates a joyous passage in academic life, Medical Campus Provost and Chobanian & Avedisian School of Medicine
Dean Karen Antman, MD, told the Graduate Medical Sciences (GMS) Master’s Class of 2023 as graduating students, their families, friends, and faculty assembled for the convocation ceremony at the BU Track & Tennis Center on May 18.

“The diploma you get today is the credential that grants you entry to the next stage of your life,” said Antman. Forty Master of Arts and 467 Master of Science degrees were awarded.
Antman noted that this academic achievement occurred in challenging times
for both education and personal lives, with loved ones, friends, and colleagues lost to a global pandemic that exposed the “health disparities that we in medicine knew existed but are now clear to everyone.”
“The faculty hope you have acquired the habit of continued, disciplined inquiry and that you are committed to contributing to the advancement of science,” said Antman. “We hope you will be the leaders in solving these problems.”
C. James McKnight, PhD, associate provost and GMS dean, urged graduates to use their education and training to effect positive change in the world.
“Your hard work has prepared you, and we are confident that you have the will, the cour-
age, and the tools that are necessary to make a difference to all of our futures,” he said.
Student speaker Darilyn Mahoney spoke of her plan to combine two passions—working with children and genetics—as a pediatric genetic counselor at Children’s National Hospital in Washington, D.C.
Mahoney described moving to Boston from her Maryland home two years ago as her first time being truly alone.
“No friends, no family, no familiarity, no community,” she recalled.
She found friends, mentors, and community, and successfully completed her master’s degree in genetic counseling, becoming the first African American to earn a degree in that program. She noted that her experi-
ence showed her that achievements come with challenges.
“From me to you, I say embrace discomfort, push for progress, and strive to support those whose voices need uplifting,” she said.
It was a long road to the speaker’s podium for Eaba Beyene, who was born in Ethiopia, moved to Canada when he was seven, and ultimately enrolled at Boston University to pursue an MS in Oral Health Sciences. He has been accepted into BU’s Henry M. Goldman School of Dental Medicine.

Like Mahoney, Beyene urged classmates to show courage, take risks, and be unafraid of failure.
“Get out of your comfort zones and don’t let past negative experiences taint your capabilities,” he said. Beyene spoke of a goldfish that grows to the size of its watery environs, trading the safe confines of the fishbowl for the dangers of the pond.
“Even though the goldfish is in danger of becoming prey, growth was a product of a riskier environment,” he said. “I warn you
that there is no fun in a life that is risk-free and boring.”
Erika Minetti, who traveled from her home in Milan, Italy, to attend BU as an undergraduate before earning her MS in the Medical Sciences Program, reminded her fellow graduates that their journey is far from complete.
“Today, we are crossing the finish line, but it doesn’t end here. As individuals aspiring to become leaders in medicine and in the medical sciences, the marathon has just begun,” she said. “I have no doubt in my mind when I say that we will use everything we learned to fuel our future, no matter where we will be or who we will become.” ●

“Today, we are crossing the finish line, but it doesn’t end here. As individuals aspiring to become leaders in medicine and in the medical sciences, the marathon has just begun.”
STUDENT SPEAKER ERIKA MINETTI

Each year we receive questions about what are known as “legacy” admissions at Chobanian & Avedisian School of Medicine, so BU Medicine sat down with Associate Dean for Admissions Kristen Goodell, MD, to discuss the topic.
How do you decide who is considered a legacy applicant?
Rather than “legacy,” we use the term “special-interest” applicant, which includes any applicant who has a particularly strong family or personal connection to the school. There is a place on the medical school application to note such a relationship, and applicants can use free text to describe their specific connection. We ask applicants to provide the name and graduation year or years of employment of their relative who has an affiliation with the school.
Generally, applicants whose parents or grandparents graduated from the school are considered special-interest applicants. We treat the children of current or former faculty and employees of the medical school the same way. We typically do not consider as special-interest applicants those whose parents or other relatives graduated from other schools or colleges at BU, or who completed a residency or fellowship at Boston Medical Center but did not graduate from the school. Occasionally, other relationships or connections with the school may merit special consideration, such as a sibling or a spouse of a current student.
What procedures does BU Chobanian & Avedisian SOM follow when a specialinterest applicant applies?
All applicants, regardless of their connection to the school, must meet our standards for admission. In other words, they must be competitive within our pool of applicants. We
use holistic application review, which means that we consider the applicant’s entire academic record and lived experiences. Accordingly, demonstrating a close connection to our school, understanding us well, and genuinely wanting to be part of this institution adds favorably to our overall assessment of the application.
If a special-interest applicant is not selected for interview, or if they are rejected after they are interviewed, they are offered follow-up counseling/application feedback by the associate or an assistant dean of admission.
How does carefully considering a specialinterest candidate benefit the school?
We want students who want to be at our school and share our commitment to the community served by Boston Medical Center, New England’s largest safety-net hospital. Medical school will be a better and happier place if the students in attendance feel positively about the school. In our experience, this positive association is often magnified if a student has a deep understanding of our mission; is dedicated to it and inspired by it. We have learned that students who have a parent
or grandparent who attended the school are more likely to better understand the school’s culture and to feel connected to the school from early on in their medical education.
Are there any challenges to considering special-interest candidates?
Each admissions cycle presents challenges because the number of applications from qualified candidates that we receive far exceeds the number of spaces we have available. In addition, special-interest applicants are more likely to have parents and grandparents who have college and graduate degrees and therefore, financial stability. However, we know that a diverse student population is better at solving complicated problems and that all students will develop a better and more nuanced understanding of the foundational principles of medicine if they are learning alongside classmates who are equally accomplished but have different experiences, expectations, and ideas. In our view, a more diverse physician workforce ultimately benefits patients. Our holistic review values these other experiences and obstacles overcome in our admissions process. ●
“All applicants, regardless of their connection to the school, must meet our standards for admission.”
Ateam of medical students made the Final Four of Innovate@BU’s BU Refugee Challenge with a proposal aimed at relieving social isolation and meeting the nutritional needs of 200 postpartum or pregnant newly arrived Haitian migrants.
In a field of 30 teams representing 16 of Boston University’s 17 colleges, one medical school student proposal, “Community Connection Through Cooking,” advanced to the finals, and a second team reached the semifinal round with a presentation called “Recipes for Refugees” about an interactive nutrition website.
“We were trying to develop creative ways to best incorporate systems we know are successful for increasing social support in a way that matches the specific needs of this population,” said Community Connection team member Leah Hollander (CAMED’23, SPH’23).
The Community Connection team included medical students Hollander, Hassan Beesley (CAMED’23), Heejoo Kang (CAS’20, CAMED’26), and Alyssa Quinn (CAMED’22, ‘26), and graduate student Gwendolyn Strickland (CAMED’25, SPH’25). The proposal— cooking classes focused on the affordability, cultural relevance, and dietary recommendations for pregnant people using Haitian recipes and ingredients, and adapting them to microwave cooking, a common cooking method in temporary housing—was a collaboration between the Chobanian & Avedisian School of Medicine Refugee Wellness Student Group, Boston Medical Center’s Refugee Women’s Health Clinic, and the Teaching Kitchen.
The Recipes for Refugees team included first-year medical students Jessica Barmine, Monica Abou-Ezzi, and Emily Getzoff.
“We’d been incubating this idea of doing group nutrition classes as part of prenatal care,” said Sarah Kimball, MD, assistant professor of internal medicine and codirector
of BMC’s Immigrant Refugee Health Center (IRHC), which oversees and connects clients to programs like the Women’s Health Clinic.
Hollander and Beesley discovered that the biggest impediment to implementing their program was transportation cost, with more than $10,000 of a $13,000 budget earmarked for rideshare and other services.
“It’s a great lesson to learn that there are a lot of steps in between having an idea and operationalizing it,” said Beesley. “But I don’t think that should be a barrier to anyone trying to achieve an idea.”
“All of the pitches were incredible,” said Innovate@BU Program Director for Social Entrepreneurship Katie Quigley-Mellor, who oversaw this year’s challenge and expressed admiration for the medical students who put tremendous time and effort into the project
while maintaining rigorous academic and clinical schedules.
Managing the demands of a dual degree, Hollander, in short order, delivered her master’s thesis in public health, participated in Match Day—where she matched in a family medicine residency at University of North Carolina Hospitals—and prepped for the Refugee Challenge.
The Community Connection team worked in the Refugee Women’s Health Clinic at the IRHC.
“They have real, tangible experience, and that is the point of a cross-campus initiative—to get students from different colleges talking to each other, learning about different initiatives, and sharing skill sets and ideas,” said Quigley-Mellor.
Maria Gorskikh (Questrom’23) took the $10,000 top prize with Dream Venture Labs, a proposal that creates a place for refugees and migrants to develop their business ideas with the help of student volunteers from Boston-area universities.
The Innovate@BU Changemaker Challenge launched in the spring of 2019 with the Global Impact Challenge. They are sponsored through the BUild Lab IDG Capital Student Innovation Center that helps all BU students and recent alumni translate ideas into reality by developing innovation and entrepreneurial skills with the goal of strengthening communities.
Utilizing the “challenge” format allows for educational opportunities within a compressed time frame that includes a two-day retreat focused on taking an entrepreneurial approach to solving social issues; coaching; and connecting with local nonprofits and policy makers.
All semifinalists received $500 toward their proposal. Quigley-Mellor’s office encouraged semifinalists and finalists to take advantage of coaching and additional funding at the BUild Lab to continue working on their projects. ●
“All of the pitches were incredible,” said Innovate@BU Program Director for Social Entrepreneurship Katie Quigley-Mellor, who oversaw this year’s challenge and expressed admiration for the medical students who put tremendous time and effort into the project while maintaining rigorous academic and clinical schedules.
This year marks the 40th anniversary of two landmark programs, the Modular Medical/ Dental Integrated Curriculum (MMEDIC) and the Early Medical School Selection Program (EMSSP), which have created unique admission pathways to Boston University’s medical and dental schools.
For four decades, MMEDIC has served high-achieving BU undergrads who want to remain at the University for their medical degrees. Four years ago, the dental track was added, which provides a similar pathway for students to enter the dental school.

“MMEDIC is good for the medical school because we get great students, and it is good for the students because it takes some of the pressure off the medical school admissions process,” says Kristen Goodell, MD, associate dean for admissions.
Goodell says that 10 to 12 BU sophomores enter MMEDIC each year and commit to continuing their postgraduate medical education at the Chobanian & Avedisian School of Medicine.
In contrast to most medical school admissions processes, which are normally time-consuming and expensive, the MMEDIC pathway has candidates—all excellent students who have focused on medical school throughout their academic years—fill out one application in their sophomore year and do on-campus interviews before being accepted into the program. Provided they meet certain academic metrics, they are then guaranteed entrance into the medical school upon graduation, which, Goodell says, allows them to follow their intellectual curiosity when choosing other courses.
Once in the program, their undergraduate course selection is done in consultation with the MMEDIC director and must include four choices from a list of graduate-level courses chosen to augment a typical premed student curriculum and offering the opportunity to
study subjects such as medical ethics, public health, and medical anthropology.
“This helps them to develop into the kind of physician who solves really complicated problems where you have to pull knowledge from different fields and specialties to address what is going on with a patient,” Goodell says.
EMSSP is focused on recruiting underserved and underrepresented medical students from a consortium of historically
Black, Latinx, and Pacific Islands colleges and universities. Each year, 12 to 18 students are admitted to the program.
“These students have the native talent,” says Goodell. “What we’re trying to do is address the external obstacles that often keep people out of medical school.”
An incredibly competitive process, getting into medical school can include deciding factors such as participation in research, clinical experience, and volunteer or paid work, all of which are often much more difficult to achieve in lower-resource settings, especially without the aid of family and friends. An undergraduate college or university with the resources and experience to keep students on track and prepared is invaluable.
EMSSP students enroll in six weeks of summer courses at BU prior to their junior year and eight weeks of BU coursework— including an MCAT preparatory course— prior to their senior year, which they spend at BU taking both undergraduate- and
“These students have the native talent,” says Goodell. “What we’re trying to do is address the external obstacles that often keep people out of medical school.”Samantha Kaplan, MD, celebrates with EMSSP graduate Jyla Hicks at the 2023 MD and PhD convocation ceremony.
graduate-level classes to prepare them for the intensive medical school curriculum.
Giving students the opportunity to spend senior year at an institution other than their undergraduate university sets BU’s EMSSP apart from similar programs at other medical schools, says EMSSP Director Ebonie Woolcock, MD, who also praises the built-in support system.
“There are a lot of programs that recruit people of color, or people from underserved backgrounds, but the support isn’t there after they arrive,” she says. “We give a much more personal approach to easing their transition into medical school and supporting them while they’re here.”
A Boston native, Woolcock was an EMSSP student while attending the Chobanian & Avedisian School of Medicine. In her first summer in the program, her father was deported to Jamaica and her mother died of cancer. Suddenly, at 19, she was the primary caregiver for her two sisters, ages 12 and 15. She says that Program Director Kenneth Edelin, MD, along with her fellow EMSSP students, helped her through that tough time.
“He shared that he had lost his mom when he was 14 and what his path was, and from then on, he had my back,” says Woolcock, who speaks with the EMSSP students after every exam. She stresses that the program helps with nonacademic, but important, aspects of the educational process, like navigating the culture of the medical profession.
Approximately half of the school’s Black medical students, and a quarter of the Latinx students, are EMSSP participants.
“We’re recruiting from places like Tougaloo, Mississippi, and El Paso, Texas, where students are coming from neighborhoods that are [medically] underserved,” says Woolcock. “That’s the beauty of the program, that we graduate people who go back home and work in underserved communities.”
Woolcock believes that EMSSP benefits everyone, not just those taking part in it.
“There are students who have never talked to a Black student before, and it’s an introduction to someone who is going to help them bridge the gap with their future patients because we are from the same background,” she says.
Please see the Alumni Stories series beginning on page 46 for profiles on six EMSSP alumni. ●

On February 21 and 22, more than 100 artworks created by Medical Campus students, faculty, and staff were on display in Hiebert Lounge during the two-day celebration known as Art Days

Keith Tornheim, PhD, an associate professor of biochemistry, is very pleased—and unsurprised—by the creative output he’s overseen as Art Days faculty advisor over the past 20 years. “The medical field, the health field, they have this other side, this creative side, in abundance,” he said.
A 33-year-old Medical Campus tradition, Art Days showcases a wide variety of art and artistic inspiration. This year, some works were drawn directly from work and study, such as the snakelike intertwining of embroidered hemoglobin, the glass and polyvinyl installation that resembled blood platelets draped over an IV line and bag, and a photograph of vegetables and fruits assembled as an exposed ribcage and heart. Others were fanciful, including a celestial migration of whales and Van Gogh’s Starry Night over BU’s new data sciences building.

Bhavana Ganduri, a physician trained in India and a graduate student at the School of Public Health, admired a painting of three dancers—an explosion of pink resembling the windblown petals of a chrysanthemum—by Ashley Davidoff, MD, a clinical professor of radiology.
“It’s beautiful,” Ganduri said. “These people are already great at their jobs, but I came to see how good they are at art—and, wow—I don’t know if artwork makes a person more complete, but I think it makes them more interesting.”
Second-year dental student Nathan Faynzilbergim mused that fellow dental student Han Chaoshi’s intricate miniature sculptures
of a pair of fantasy creatures fit his friend’s personality and professional choice.
“You can just see the immaculate detail he put into them, the steady hand it takes, and it makes sense since he is in dental school,” said Faynzilbergim.
LaKedra Pam, MD, likes to focus on things other people overlook, “or maybe don’t necessarily think are the prettiest, and make them look awesome.” An assistant professor in obstetrics and gynecology, Pam said architectural details grab her attention. One of her two photos mounted on woodblocks at the show showed the lines of a building rising into clouds and a brilliant blue sky.
“I think creative thinking is a big part of obstetrics,” she said. “And anything you do that engages another part of your brain helps.”
According to Kristen Segars, a fourth-year MD/PhD candidate, if you’ve got a creative side, it’s best to let it out. “You can try not to do creative things, try not to focus on art, but in the end, you’ll always find yourself doodling in your notebook,” Segars said, standing in front of the polychromatic dress she knit for the event. She noted that doing art can ease stress as well. “It kind of keeps everything in perspective, especially when there’s so much emphasis on the grind and always working.”
Second-year medical student Alexis Fearing said that her whirling mosaic maelstrom of jagged tiles arose from both a time of emotional turmoil and a love of meteorology.
“Art is a source of inspiration, and it’s important to seek out sources of inspiration because that’s how we have growth, how we make changes,” she said. ●
The names of the school’s basic science departments have historically represented the disciplines taught in medical school almost a century ago. New scientific disciplines—including structural biology, cell and tissue imaging, and data science—have evolved. After a comprehensive review beginning in June 2021, faculty and departmental leadership requested the names of some of our basic science departments be changed to more accurately describe the actual research done in their departments.
On March 8, 2023, the University approved the new names. Now, the school will need to update areas including department, faculty, and lab websites; the University Bulletin; course descriptions; campus and other signage; CVs, and publication submissions.
Diplomas and transcripts will change as of September 1, 2023. Students graduating in May and August 2023 will retain the former department names.
Speaking at a February 8 virtual symposium celebrating Rebecca Lee Crumpler, MD, four distinguished alumni reflected on their medical careers, their experiences at the school, and the personal impact of Crumpler’s legacy. More than 190 viewers registered for the event, sponsored by the school’s Diversity & Inclusion and Development offices.
Graduating from New England Female Medical College in 1864 (which merged with Boston University in 1873 to become Boston University School of Medicine), Crumpler was the first Black female physician in the United States. In A Book of Medical Discourses in Two Parts, she wrote that she was driven to pursue “every opportunity to relieve the sufferings of others” and chose to provide treatment—particularly to women and children—regardless of their ability to pay.
Crumpler faced racism and sexism as pharmacists refused to fill her prescriptions, fellow physicians shunned her, and she was denied admitting privileges at hospitals.
“The fact that the School of Medicine was originally a female medical college . . . speaks volumes to the emphasis placed on the importance of women in medicine. And then, to have a Black woman . . . at the end of the Civil War who actually graduated (with a medical degree) and was the first in the US . . . it just reemphasizes the school’s mission . . . in terms of understanding the importance of women, and women of color, in medicine,” said Patricia Williams (CAS’84, CAMED’89), former vice president of safety surveillance and risk management for Pfizer Pharmaceuticals.
Williams said the premed competitiveness during undergraduate years shifted to a supportive environment once she started at
medical school, which featured a fair amount of “tough love” but also staff, faculty, and students pulling together to help everyone.
As a medical student, Nancy Roberson Jasper (CAMED’84), a former assistant professor of obstetrics and gynecology at Columbia University Medical Center, was impressed by the school’s emphasis on community outreach. She recalled an incident where medical students went to the home of a man suffering from prostate cancer who was experiencing elder abuse and brought him back to the hospital.
“I thought that was so courageous, and how unique that was, that we had done that for this individual,” said Jasper.
The idea of serving the community locally and globally permeated her career, including a mission to the impoverished and war-torn West African country of Sierra Leone to investigate women’s health issues and infant mortality. She recently decided to leave Columbia University and a private practice in midtown Manhattan for a position as an OB/ GYN at the James J. Peters Veterans Affairs Medical Center in the Bronx.
said her BU education “sparked her curiosity and made me look at medical problems . . . with a much more global view.”
She chose cardiology following the loss of her grandfather due to a heart attack. As a cardiologist, she was “intrigued by the heart and how the heart worked” and was drawn to consider the larger issues. A third-year rotation with attending cardiologist
Alice Jacobs, recently retired professor of medicine and vice chair for clinical affairs in the department of medicine at the school, showed her that women could succeed in what continues to be a male-dominated field. Her subsequent research work pushed her to investigate root problems—such as why women with heart issues were diagnosed so much later than men—and to help write American Heart Association guidelines on how to use diagnostic technology on women.
The coauthor of five books and coproducer of four documentaries including the Emmy-nominated A Woman’s Heart, Mieres lauded Crumpler’s book for making medicine understandable to the average person.
“I was inspired by my patients to translate all of the science into actionable steps,” she said. “So, I think, like Rebecca Lee Crumpler, with the intellectual curiosity and the solution-minded mindset that started at Boston University, I was able to join forces with colleagues to really help patients and people become empowered to be partners in their health.”
bit different, and the support for me might be a little bit different, was really, really important,” said Woolcock.
The larger social and medical issues behind teen pregnancy helped draw her into women’s health and to ultimately become an OB/GYN. Mentored by the late Kenneth Edelin, MD, while in medical school, Woolcock found that she was particularly interested in the surgical delivery of babies by Cesarean delivery (C-section).

Woolcock recounted a difficult C-section with a medical student observing. “I said to him, ‘so that’s not normal, that’s not what we normally do.’ But his eyes were so big, and I remember having that same moment when I saw my first C-section,” she said. “My eyes [were] so big, like, this is amazing. We went in the room with one-and-a-half patients, then came out with two.” The earlier experience had helped her connect the direct ways in which physicians help people, regardless of their life circumstances.
“For me, it was this whole idea of intervention and public health and [that] this is really a space where I, as a Black woman, can make a difference and use my hands, and within two minutes, I can actually make a difference in someone’s life,” she said.
Woolcock saw a life lesson in Crumpler’s solitary drive, and she constantly reminds her students of the importance of self-affirmation.
“I’m going to go back to where I really feel my roots are . . . to get back to the community for [whom] I had gone into medicine, to take care of women who had not had the opportunities that I had . . . who I knew couldn’t come and see me in my own practice because they didn’t have insurance,” said Jasper.
Jennifer H. Mieres (CAMED’86), dean for faculty affairs and professor of cardiology at Hofstra University’s Zucker School of Medicine,



Born and raised in Boston, Ebonie Woolcock (CAMED’10, SPH’10), assistant professor of obstetrics & gynecology, assistant dean for diversity & inclusion, and director of the Early Medical School Selection Program (EMSSP), was the first in three generations of her family to break the cycle of teen pregnancy and the first college graduate. Her background differs from the typical applicant admitted to medical school.
“Having deans and faculty who recognized that my path to the school might be a little
“In those moments, I remind myself that, ‘I’m the bomb. Do you know how hard I had to fight to get here? Do you know how smart I had to be to get here? Do you know whose shoulders I stand on? Dr. Rebecca Lee Crumpler did it, so can I,’” she said.
Jasper advised medical students not to be afraid of change, as she and most of the other panelists had made career moves that were often dictated by life circumstances.
“Be fearless,” she said. “There are going to be times when things are not going to go the way you expect them to, but then, there are going to be times when you’re going to have riches beyond your belief.” ●
“In those moments, I remind myself that, ‘I’m the bomb. Do you know how hard I had to fight to get here? Do you know how smart I had to be to get here? Do you know whose shoulders I stand on?
Dr. Rebecca Lee Crumpler did it, so can I.”
EBONIE WOOLCOCK
Graduate Medical Sciences (GMS) is pleased to present three high-achieving graduating students with Outstanding Student Achievement Awards in the categories of Outstanding Research and Community Service.
These students have made exceptional contributions to their departments and communities during their time at GMS. Meet each awardee:
PhD in Molecular & Translational Medicine, Program in Biomedical Sciences
Outstanding Student Achievement Award: PhD Research Category
Claire Burgess matriculated into the PhD Program in Biomedical Sciences (PiBS) in 2017 and currently works in the lab of Darrell Kotton, MD, director of the Center for Regenerative Medicine (CReM) and David C. Seldin Professor of Medicine at Chobanian & Avedisian School of Medicine.
During her time in the Kotton Lab, Burgess has discovered two different methods for generating human alveolar epithelial type I cells (AT1s) from pluripotent stem cells (iPSCs). These cells, which form most of the gas exchange surface of the lung, had no previous human in vitro culture model and are difficult to access from primary tissue.
These difficulties limited scientific understanding of lung epithelial diseases like acute respiratory distress syndrome (ARDS), idiopathic pulmonary fibrosis (IPF), and chronic obstructive pulmonary disease (COPD).
“AT1s have the largest surface area and are one of the most topologically complex cells, as well as one of the thinnest,” Burgess says. “They’re difficult to isolate because they get
shredded in the process. There weren’t any good culture model systems for these cells, and so we didn’t know a lot about them.”
Her research contributed to the Kotton Lab ultimately discovering how to grow iAT1s from different genetic backgrounds in 3D organoids, as well as in 2D air-liquid interface cultures. The lab has completed a provisional patent application for these lentiviral and media-based methods.


“Being able to generate [iAT1s] from iPSCs, not only have we managed to make a model for these cells, so that we can understand how they’re affected by smoke exposure or viral infections […], but we’ve also been able to understand a little bit more about their development and the signals that are involved in differentiation, and how that might be perturbed in different disease states like IPF and COPD,” Burgess says.
Burgess and the Kotton Lab also have demonstrated the role of nuclear YAP/TAZ signaling in the differentiation of human type I cells. She has generated a reporter iPSC line to track and purify these iAT1s, which she has shared with academic and industry-based labs across the country, like the Chobanian & Avedisian SOM Varelas Lab and labs on the University’s Charles River Campus, Massachusetts General Hospital, Massachusetts Institute of Technology, and Novartis.
In 2021, Burgess was awarded an F31
National Research Service Award through the National Heart, Lung, and Blood Institute of the National Institutes of Health for her research. The project, “Generation of Human Alveolar Epithelial Type I Cells from Pluripotent Stem Cells,” is posted on the preprint server for biological sciences, bioRxiv. Burgess successfully defended her dissertation on February 9, 2023.
Burgess is very grateful for her Outstanding Student Achievement Award.
“I’ve been doing this research for five years, so the successes come spaced out with as many if not more failures,” she says. “When you condense all the successes into a single paragraph [for the award application], it suddenly seems very impressive. It’s funny to be able to look at that paragraph and think, ‘Wow, I really have done a lot.’”
Master’s in Medical Sciences (MAMS) Program Outstanding Student Achievement Award: Master’s Research Category
Born and raised in Milan, Italy, Erika Minetti moved to Boston in 2015 to pursue a BA in biochemistry & molecular biology with a minor in music performance at Boston University.
Following graduation, Minetti spent a year as a research technician in the lab of Reiko Matsui, MD, assistant professor of medicine at the Chobanian & Avedisian School of Medicine, then another as a clinical research coordinator in a translational setting with Naomi Hamburg, MD, the Joseph A. Vita Professor of Medicine and chief of the vascular biology section.
When it came time for Minetti to apply to graduate programs, MAMS stood out as an excellent option.
“I’ve been doing this research for five years, so the successes come spaced out with as many if not more failures.”
CLAIRE BURGESS
“I’ve been doing research from 2017, since I was an undergrad,” Minetti said. “I have a lot of important mentors here from my research experience, in addition to all the professors that I’ve met and who have also guided me through my master’s. That’s also why I picked the MAMS program specifically.”
Minetti returned to the Hamburg Lab to write her MAMS master’s thesis, “Cardiometabolic Proteomics and Vascular Endothelial Health in Type 2 Diabetes.”
“What we found is that there are associations between abnormal vascular endothelial phenotype and serum biomarkers in T2DM,” Minetti said. “That was our main finding, and that was really exciting to write about and to understand.”
The Outstanding Student Achievement Award is well-deserved recognition of Minetti’s research and education before and throughout her time in the MAMS program.
Minetti dedicated her award to all of the mentors she had at BU, especially Hamburg and Matsui, as well as Robert Weisbrod, her senior lab manager, and Gwynneth Offner, PhD, director of the MAMS program and an associate professor of medicine.
“The great thing about all my mentors is that they helped me not only in my academics and in my research, but they also take the time to mentor me through the challenges I face in my life,” she said. “I’m incredibly grateful, and I don’t think I could have made as much progress without them.”
Physician Assistant Program
Jean Jacques describes her own experience as a refugee in the United States as an important part of her journey that ultimately led her to BU and to the service project that earned her the Outstanding Student Achievement Award.
The project, “A Warm Welcome for Babies & Families Winter Essentials Fundraiser & Drive,” came from her experience in her OB-GYN rotation at Boston Medical Center (BMC) in October and November 2022.
During that time, Jean Jacques spoke with many refugee patients in the labor and delivery unit. Hearing their stories, she learned that many of these mothers and their families were adjusting to the cold Boston winter weather for the first time.
People with type 2 diabetes are more vulnerable to developing cardiovascular disease, and endothelial dysfunction is one of the early indicators of cardiovascular disease. Vascular endothelial cells make up the innermost layer of blood vessels.
To better understand what drives endothelial dysfunction in patients with type 2 diabetes, Minetti and her team obtained serum from people who have type 2 diabetes and nondiabetic controls.
The serum was used to assess levels of cardiometabolic markers using two O-Link panels. The biomarkers of which levels were significantly different in the two groups are involved in metabolism, immune function, apoptosis, vascular effects, and fluid homeostasis, but some of these biomarkers have many different cellular and physiological functions.
The lab also collected endothelial cells from both groups, stimulated them ex vivo with insulin, and measured the fold change in levels of phosphorylated endothelial nitric oxide synthase (p-eNOS), an enzyme in the pathway that produces the potent vasodilator nitric oxide (NO). Then, they correlated the biomarker findings with p-eNOS levels.
Outstanding Student Achievement Award: Master’s Community Service Category Born and raised in Portau-Prince, Haiti, RhodeArmelle Jean Jacques and her mother sought refuge in Miami, Florida, due to ongoing political instability in their home country.
Jean Jacques completed high school and her undergraduate degree in Miami, graduating from the University of Miami in 2016 with a bachelor’s degree in biology and a minor in chemistry.

She also obtained an MPH from George Washington University in 2020 before starting the Boston University Physician Assistant (PA) Program in 2021.
Completing BU’s PA Program has given Jean Jacques several opportunities to serve her community, as the Greater Boston metropolitan area is home to the third-largest Haitian population in the United States.
“Haiti has a special place in my heart because it’s home,” Jean Jacques said. “The fact that I’m able to practice medicine and do what I do and be able to give back to my community is very special to me.”
“There really is a need here to have [these patients] be able to make an easier transition and then to get them the help that they need,” Jean Jacques said.
Jean Jacques spearheaded the project and partnered the Physician Assistant Program with BMC midwives to collect supplies and raise funds for frequently needed items, such as portable cribs, car seats, diapers, and clothing. The fund also collected donations of new and gently used winter coats and accessories to help keep families and their new babies warm.
To facilitate this project, Jean Jacques worked alongside BMC Director of Childbirth Education Cesylee Nguyen, CNM, MSN, RN, as well as PA Program Director Susan White, MD, and her classmates.
Jean Jacques recommends that all students try to step away from their studies from time to time and volunteer.
“There’s so little time, but a little thing can just make such a huge difference in someone’s life,” she said. “Even if it’s volunteering somewhere just for a few hours, whenever you have the chance, I think you’ll get a lot more from that than you think that you’re losing time-wise.” ●
“The great thing about all my mentors is that they helped me not only in my academics and in my research, but they also take the time to mentor me through the challenges I face in my life.”
ERIKA MINETTI
“There’s so little time, but a little thing can just make such a huge difference in someone’s life.”
RHODE-ARMELLE JEAN JACQUES
On April 21, Graduate Medical Sciences held the 29th Annual Henry I. Russek Student Achievement Day in the Hiebert Lounge with 98 students—the most in “Russek Day” history— registered to present their research.

Shelley Russek, PhD, organizes the event each year in honor of her late parents—Henry I. Russek, MD, a prolific physician scientist in cardiology, and philanthropist Elayne Russek— and to celebrate the ongoing achievements of the graduate student body at Boston University Chobanian & Avedisian School of Medicine.
According to Russek, a professor of pharmacology and experimental therapeu-
tics, director of the graduate program for neuroscience, and president of The Russek Foundation, the mission of Russek Day goes above and beyond academic research by incorporating how students balance their research with service to their departments, their programs, and their communities.
“Each person getting an award today is giving something back to the community in balance with their outstanding research mission,” Russek said. “That’s behind a lot of what my family believes in and why we started this endowment 29 years ago.”
Associate Provost and Dean of Graduate Medical Sciences C. James McKnight, PhD, applauded the presenting students on the caliber of their research at GMS.
“My job is to make sure that all you students get the best experience you can have while you’re on campus learning science,” McKnight said. “Hopefully, we’re imparting the joy of science. That’s our goal.”
David Housman, PhD, a Virginia and D.K. Ludwig Professor for Cancer Research at the Koch Institute for Integrative Cancer Research at Massachusetts Institute of Technology and a cofounder of Genzyme, was the keynote speaker. Housman is renowned for his contribution to discovering the HTT gene, which causes Huntington’s disease, the role of p53 in cancer, and WT1 in Wilms Tumor.
The Housman Lab uses genetic approaches to identify the molecular bases of human disease pathology—specifically
in cases like Huntington’s, cancer, and cardiovascular disease—and works to develop effective intervention strategies for fighting trinucleotide repeat disorders.
Shoumita Dasgupta, PhD, assistant dean for diversity & inclusion at Chobanian & Avedisian SOM, professor of medicine/biomedical genetics, founding director of the Genetics and Genomics Graduate Program, and former Housman lab member, introduced Housman to the audience, describing her time as an MIT undergraduate in his lab as her “origin story in genetics.”
Housman drew from his expertise in genetics and human disease and his team’s lab work to present “Treating Multiple Sclerosis: An MD/PhD Student Teaches Us.”
Students then introduced their research during a luncheon and poster presentation
● Devin Kenney, Department of Virology, Immunology & Microbiology
● Gian Sepulveda, Program in Genetics & Genomics
● Beverly Setzer, Graduate Program for Neuroscience

● Ioanna Yiannakou, Nutrition & Metabolism Program
Russek presented winners with certificates onstage, including 11 first prizes of $1,500, eight second prizes of $500, and five third prizes of $350.

The ongoing success of Russek Day stems
from the research accomplishments of GMS students and their dedication to their projects, their peers, and their departments, as well as the Russek family and Russek Foundation’s unwavering support of these student research and service endeavors.
GMS administrative coordinator James Mazarakis; Chobanian & Avedisian SOM student Alison Tipton; Pharmacology, Physiology & Biophysics Administrator Sara Johnson, and several other GMS staff members and students contributed to this year’s event. ●
In April, Ellen DiFiore, assistant dean and registrar for the MD Program, announced her plans to retire effective June 2, 2023.
DiFiore worked at BU in various roles since 1989, serving as a research assistant in pediatric infectious diseases, an administrative manager of the Primary Care Training Program in the department of medicine, and a project manager for the Robert Wood Johnson Generalist Physician Initiative. She was appointed the MD Program registrar in 2000.
access to their schedules, grades, and many services, and developed an online add/drop system for fourth-year scheduling. And when the school transitioned to remote operation during the pandemic, the service level remained exceptional.
session. Prior to the event, departments had selected the award winners, who proudly displayed stickers on their posters and nametags.
In the afternoon, 11 first-prize recipients delivered oral presentations of their research:
● Guillermo Arroyo Ataz, Department of Pathology & Laboratory Medicine
● Anne Billot, Behavioral Neuroscience Program
● Morgane Butler, Department of Anatomy & Neurobiology
● Andrew Chang, Department of Pharmacology, Physiology & Biophysics
● Jenna Libera, Department of Pharmacology, Physiology & Biophysics
● Liang (Martin) Ma, Graduate Program in Molecular & Translational Medicine
● Adeline Matschulat, Department of Biochemistry & Cell Biology
She received the University’s John S. Perkins Distinguished Service Award and the school’s Student Committee on Medical School Affairs Annual Service Award. She also served on the Association of American Medical College’s Group on Student Affairs (GSA) Committee on Student Records and was the secretary/treasurer for the GSA Northeast Region.
Under her leadership, the registrar’s office has provided outstanding service to students and graduates, implementing many changes over the years—including some suggested by the students themselves—in order to give them access to the information they need for success in medical school and beyond.
Among the changes, the office transitioned from paper and forms to electronic records, giving students 24/7
“It has been an honor to have played a small part in the success of the 3,800 graduates awarded the MD degree during my tenure. I have shared in their triumphs and disappointments and am proud of their accomplishments.”
“It has been an honor to have played a small part in the success of the 3,800 graduates awarded the MD degree during my tenure,” DiFiore said. “I have shared in their triumphs and disappointments and am proud of their accomplishments. The school has been my home and the students, faculty, and staff my family. I will miss them all greatly.”
The school thanks Ellen DiFiore for her many contributions to our community and wishes her all the best in the years ahead. ●
Nancy Sullivan, ScD, director of the National Emerging Infectious Diseases Laboratories (NEIDL), and Venetia Zachariou, PhD, chair of pharmacology, physiology & biophysics, have been installed as the inaugural recipients of the Edward Avedisian Professorships. The endowed chairs were funded out of the historic $100 million gift the late Edward Avedisian gave to the school.
“I believe they are most worthy inaugural Edward Avedisian Professors, and congratulate them,” Avedisian’s wife Pamela told a hybrid audience at the ceremony held in Hiebert Lounge that included faculty, students, friends, and members of the Sullivan and Zachariou families.
A longtime musician with the Boston Pops and Boston Ballet Orchestra, Edward Avedisian (CFA’59,’61, Hon.’22) was also a highly successful investor who quietly amassed a fortune. He made donations to educational programs and buildings in his ancestral country of Armenia as well as throughout Rhode Island and at the University, which renamed the medical school the Aram V. Chobanian & Edward Avedisian School of Medicine in honor of Avedisian and his childhood friend Aram Chobanian, MD (Hon.’06). Medical school dean emeritus and BU president emeritus, Chobanian attended the ceremony online.
Twenty-five percent of the gift is dedicated to funding endowed professorships.
A professor of microbiology and biology, Sullivan came to BU from the National Insti-
tutes of Health, where she was chief of the Biodefense Research Section at the Vaccine Research Center, National Institute of Allergy and Infectious Disease (NIAID). An international leader in filovirus vaccines and hemorrhagic fever virus immunology, her team was first to demonstrate Ebola vaccine protection in primates and later developed Marburg and Sudan vaccines that are currently in Phase 2 human trials, in addition to a monoclonal antibody for Ebola that resulted in a nearly 90 percent survival rate.
Sullivan thanked family, friends, and mentors, noting that like SARS CoV-2, there are new viruses, still unknown and unstudied, that exist in animal reservoirs around the world.
Projecting a slide showing researchers in “space suits” that are worn while studying highly infectious emerging diseases in the highest-level containment labs at the NEIDL, Sullivan said, “We need to do that so that we can, ahead of time, develop therapies and vaccines for these viruses that we know are coming.”
Joseph Mizgerd, ScD, professor of medicine and the inaugural Jerome S. Brody, MD, Professor of Pulmonary Medicine, said he has been both friend and fan of Sullivan since the 1990s, when they were both pursuing their doctorates at Harvard T.H. Chan School of Public Health.
“I learned so much from her,” said Mizgerd. “I’m so glad to welcome Nancy to BU and congratulate her on this wonderful professorship.”
Zachariou joined BU in November 2022 from the Icahn School of Medicine at Mount Sinai in New York, where she was professor of neuroscience and pharmacological sciences.

Karen Antman, MD, Medical Campus provost and dean of the medical school, introduced Zachariou, citing her work investigating chronic pain states and addiction at

the cellular level and her efforts in developing novel therapeutics for the management of chronic pain by targeting novel genes and intracellular pathways.
“Twenty percent of the American population suffers from very severe chronic pain conditions such as peripheral neuropathy, fibromyalgia, chronic migraines, or chronic fatigue syndrome,” said Zachariou. “It’s important to develop novel approaches to break this vicious cycle of chronic pain, instead of simply suppressing symptoms.”
Given the ravages of a national opioid epidemic, one of her research goals is to develop alternatives to opioids as pain relievers.
“I’ve been extremely lucky to be surrounded by amazing trainees and colleagues. We’ve discovered new treatment targets. But more importantly, we connected with other scientists all over the world,” said Zachariou.
Alex Serafini, a postdoc in BU’s pharmacology, physiology & biophysics department who studied under her at the Icahn School of Medicine as an MD/PhD student, told the audience that Zachariou was an outstanding mentor.
“She forces people to become the best scientist they can be,” Serafini said.
Five Boston University Chobanian & Avedisian School of Medicine faculty have been honored as 2023 Educators of the Year by the school’s Awards Committee. The annual awards recognize Chobanian & Avedisian School of Medicine educators who demonstrate excellence in teaching and mentoring.
Nominated by students and faculty, this year’s recipients are Ricardo Cruz, MD, MPH, Educator of the Year, Preclerkship; Julia Bartolomeo, MD, Educator of the Year, Clerkship; Lillian Sosa, MS, CGC, Educator of the Year, MA/MS Programs; Douglas Rosene, PhD, Educator of the Year, PhD Programs; and Jia Jeannie Xu, MD, Resident Educator of the Year.
“I believe they are most worthy inaugural Edward Avedisian Professors, and congratulate them.”
PAMELA AVEDISIAN (HON.’23)Nancy Sullivan Venetia Zachariou
Ricardo Cruz is an assistant professor of medicine and a board-certified primary care physician in internal medicine. He has clinical expertise in addiction medicine and treats patients with substance use disorders at Boston Medical Center’s (BMC) Faster Path low-barrier bridge clinic and the Office Based Addiction Treatment clinic, where addiction treatment is integrated into primary care services.
He also works with individuals who have a history of incarceration, striving to mitigate reentry risk by reengaging them in primary care and behavioral services with a focus on the treatment of substance use disorders. As a member of the Academy of Medical Educators at the school, Cruz serves as the core advisor to a cohort of medical students for the duration of their studies and core educator for the doctoring courses, where students learn communication and clinical reasoning skills and knowledge.
According to his nominators, Cruz “has repeatedly demonstrated a passion for teaching first- and second-year medical students as they lay the foundation for becoming doctors in the Intro to Clinical Reasoning course. He loves engaging the students and encourages a deeper understanding of what can be learned through the physical exam. He provides ongoing support through mentorship and professional coaching to ensure Underrepresented in Medicine residents are retained and achieve success in the residency program.”

Julia Bartolomeo is an assistant professor of family medicine who sees patients at East Boston Neighborhood Health Center (NHC) and rounds on the inpatient Family Medicine service at Boston Medical Center (BMC) with residents and fourth-year students.


As associate director of the Family Medicine clerkship, she teaches third-year
students and serves as site director for those rotating at East Boston NHC. She was accepted into the inaugural Academy of Medical Educators in 2019, where she is an educator and advisor for first- and second-year students in the doctoring courses. She has been a field-specific advisor for many students applying to Family Medicine and served as faculty advisor for the Family Medicine Interest Group.
Bartolomeo’s nominators said, “Her leadership and commitment to the Family Medicine Interest Group (FMIG) during COVID was essential. As events were often cancelled or provided via Zoom during our first year, we did not have any experience planning in-person events when we became student leaders. She encouraged us to develop our own ideas, which allowed us to explore our interests in family medicine, including collaborating with the Geriatrics Interest Group to establish a joint event on the intersection of geriatrics and family medicine. She helped FMIG achieve its goal of increasing awareness and interest in family medicine in the preclerkship years.”
Lillian Sosa is a licensed genetic counselor practicing in the department of obstetrics & gynecology. The assistant program director of the genetic counseling master’s program, her primary responsibilities include overseeing and coordinating the fieldwork and clinical education curriculum. Sosa also manages students and faculty education for clinical supervisors in her region.
A nominator said, “Lillian is a deeply valued core member of our faculty who continues to elevate the quality of teaching for our program in the classroom and the clinic for
our students. She is consistently rated highly by students on her knowledge, experience, professionalism, mentorship, and teaching ability.” According to a student, “She has always gone above and beyond in providing in-depth feedback and tailors each day of the rotation to fulfill skills that I needed improvement on. I appreciate how open she is in receiving feedback and am always confident in being able to have a conversation with her.”
Douglas Rosene is a professor of anatomy & neurobiology and a world expert on the anatomy of the temporal lobe limbic system, an area in which he has published extensively. He is also recognized for his work in the neurobiology of cognitive aging and for 15 years served as program director of a long-standing NIH program project studying the neural bases of cognitive decline using an experimental model of normal human aging. He is the principal investigator or coinvestigator on several other NIH grants studying various aspects of aging and age-related disease in experimental models.

A nominator said, “He epitomizes the mission of the award in that he certainly goes above and beyond expectations for our teaching mission. He challenges students to acquire skills critical to their development as scientists and delivers exceptional education to our students, as his commitment to their learning is unrivaled.” Another colleague cited Rosene’s exceptional mentoring of young PhD candidate neuroscientists. “He provides unending patience, support, guidance, and wisdom to his students, postdoctoral fellows, and faculty colleagues who, themselves, mentor PhD students.”
Jia Jeannie Xu is a graduate of the BU combined seven-year program and an ophthalmology resident at BMC. Following an
internal medicine internship year at Beth Israel Deaconess Hospital, she returned to the University to fulfill her residency at BMC.
According to a colleague’s recommendation, “Jeannie is an exceptional resident educator because she prioritizes medical student education and fervently encourages student involvement in attending clinics and the operating room. She is also a superior educator because she carves out time for teaching, even during busy clinic days.
“As chief resident, Jeannie is clearly committed to diversity, equity, and inclusion. As a patient advocate, she always made sure that all the medical students knew how to get an interpreter for the different languages that our patients speak at BMC, so that they could comfortably communicate in their preferred language.”
Two faculty members, Samantha Kaplan, MD, assistant professor of obstetrics & gynecology, and Elizabeth Klings, MD, professor of medicine, and Peter Flynn, tech lead for Boston University Medical Campus IT Application Services, have each received the Diversity, Equity, Inclusion & Accessibility (DEIA) of the Year Award. The annual award recognizes faculty and staff who have done extraordinary work addressing and improving diversity and a culture of inclusion, equity, and accessibility throughout the school community.
Kaplan has served as assistant director of the obstetrics & gynecology clerkship, assistant dean of diversity & inclusion, and former director of the Early Medical School

Selection Program. Her academic interests focus on workforce diversity as a path to achieving health equity; how race and gender manifest in academic recruitment, retention, and advancement; and increasing awareness of how racism and bias impact medical education and patient care.

According to a nominator, Kaplan has devoted her career to fighting for diversity, equity, and inclusion in every realm of her work. “Through her work as both a family planning physician and obstetrician, Dr. Kaplan ensures her diverse patient population has the invaluable access to the resources and care they need to have the families and reproductive lives they desire.”
As a researcher, she has contributed to critical conversations regarding the relationship between diversity and academic medicine. “Her published scholarship includes topics such as recruitment, retention, and compensation of women faculty and faculty of color; the impact of race and ethnicity on success in academic medicine; colorism; and deconstructing racism and power in medical education,” read a colleague’s recommendation letter.

Klings’ diversity, equity, and inclusion work goes back to her years as a medical student. She has cochaired the Pulmonary, Critical Care, and Allergy Faculty Recruitment Diversity Committee since 2019, and chaired the Pulmonary Racial Equity Committee since 2021.
“Liz is a champion of DEIA. In the Pulmonary Center, she chairs two different committees designed to help us make our community more diverse by enhancing equity, inclusion, and accessibility. She has been chair of our Racial Equity Committee since its inception. With her leadership, this committee provides a monthly equity and inclusion educational program involving readings, seminars, and interactive workshops.
“Liz’s fervent dedication to the Sickle Cell Disease (SCD) community is further evidence of her DEIA passion. SCD predominantly affects persons of color, and this disease traditionally is terribly underserved by the medical and research communities due to multiple factors including systemic racism. Liz works passionately to change that,” a colleague wrote in recommendation.
Flynn joined the University in 2005 as a programmer in the Data Coordinating Center (which later became the Biostatistics and Epidemiology Data Analytics Center) at the School of Public Health and rose to assistant director of Database Applications in 2008. In 2009, he moved to the BUMC Application Services unit within BUMC Information Services & Technology as a senior developer and was promoted to technical lead in 2016.

“Peter has led an array of projects to promulgate and support a culture of inclusion, equity, and accessibility for the school and BU at large,” said a colleague. He added a feature to BU Profiles allowing users the option of designating and displaying their preferred pronouns and a public-facing diversity statement.
He also took the lead in creating Hear My Name, which allows people to record their name in their own voice and let others know their preference, such as a nickname. “Name pronunciation is often taken for granted, but names are closely tied with identity. Mispronunciation can be embarrassing, dehumanizing, and even affect a person’s mental health,” another colleague noted.
Chobanian & Avedisian School of Medicine’s highest teaching honor, the Stanley L. Robbins Award for Excellence in Teaching.
“Dr. Ananthakrishnan’s achievements as a teacher, mentor, program developer, innovator, scholar, and leader in medical education make her an outstanding candidate for this award,” a colleague said in recommendation. “She identified the need to improve the quantity and quality of feedback, building a local and national reputation around the educational initiative of improving feedback exchanges across all levels of training in the department of medicine.
“As a clerkship director, she addressed the need for more high-quality assessment by creating the Observed Clinical Reasoning Assessments (OCRA). The OCRA has successfully integrated into the internal medicine clerkship and this style of examination has been adopted by several other clerkships—including neurology and pediatrics— and even in the preclinical curriculum.”
all educators, having excelled in every educational domain including direct teaching, assessment, curriculum development, and scholarship.”

Laura Wung, MD, has received the 2023 Leonard Tow Humanism in Medicine Award from the Arnold P. Gold Foundation. This award is presented to faculty who best demonstrate the foundation’s ideals of clinical excellence as well as outstanding compassion in the delivery of care and respect for patients, their families, and healthcare colleagues.
mentor, but she is cherished by colleagues and other primary care staff.
“It has been a pleasure to be under her mentorship these past three years.”

Alcy R. Torres, MD, FAAP, associate professor of pediatrics and neurology, has been selected Physician of the Year for Scientific Achievements by the Ecuadorian Physicians College. Torres has an extensive research background and was recognized for his work in treating folate deficiency in the central nervous system of infants.
Ananthakrishnan has championed diversity, equity, inclusion, and belonging on the Medical Campus.
Ananthakrishnan has championed diversity, equity, inclusion, and belonging on the Medical Campus and helped originate the Lights On, Intent vs Impact, Full Stop, Teach (LIFT) training for bystanders addressing micro-aggressions as part of the Mid-Career Faculty Leadership Program in 2020. The LIFT training program has been widely disseminated across campus in part due to her work facilitating more than a dozen sessions for students, faculty, and hospital leadership.
Ananthakrishnan has been active in medical student and resident education at the school since 2009, mentoring hundreds of medical students as they travel through the residency application process. According to another colleague, “She is a role model for

An assistant professor of medicine who has served on the faculty since 2002, Wung is a primary care physician at Boston Medical Center (BMC). Her passion for working with traditionally underserved patient populations started during her medical school rotations in New York’s Bellevue Hospital and increased during her primary care residency at BMC.
According to a colleague, “Dr. Wung is well respected by her colleagues for her outstanding clinical role in primary care and is consistently described as being singularly focused on the care and welfare of her patients.”
Another said, “Though deeply respected by trainees, staff, and fellow faculty, Laura is humble and giving—almost to a fault. I would trust my family and closest friends to her care and consider her one of my most valued friends and colleagues families.”
Wung’s students look up to her as an exemplary physician and cite her bedside manner as a model for interns and residents. Said one resident, “She is compassionate, caring, patient, and respectful of all patients. As trainees, we strive to model her behavior as the gold standard. It is clear that her patients trust her and feel safe with their care under her guidance. Not only is she a trusted
Born in Ecuador, Torres received his medical degree at Universidad Central del Ecuador in 1990. He completed his pediatric and neonatology residencies at Carlos Andrade Marin Hospital in Quito, Ecuador, a residency in pediatrics at the Nicklaus Children’s Hospital in Miami, and a pediatric neurology residency at Boston Children’s Hospital, Harvard Medical School, where he remained on-staff for 13 years. He is the founding director of the Pediatric Brain Injury Program at Boston Medical Center and serves as director of the global health and bilingual programs, division of pediatric neurology.
Torres has received multiple awards for teaching and mentoring early career clinicians and investigators. He also founded and has volunteered for the Association of Ecuadorians in New England since 2005, raising more than $1.5 million to support 25+ projects for children with neurodevelopmental disabilities.
Aliza Stern, MMSc, PA-C, director of didactic education for the school’s Physician Assistant Program, has been selected to serve on the Reconsideration Panel of the Accredita-
tion Review Commission on Education for the Physician Assistant (ARC-PA). The panel, a voluntary national service to the PA profession, reviews programs that wish to appeal adverse accreditation actions.
Stern joined the BU community in 2016, serves as chair of the didactic curriculum committee and is a member of the program’s clinical, executive, and data committees as well as an assistant professor of dermatology, providing care at Boston Medical Center to patients with a wide variety of dermatologic needs.

She received her undergraduate degree from Lehigh University and her MMSc from Yale University School of Medicine.
Elijah Paintsil, MD, has been named chief and chair of pediatrics at Boston Medical Center (BMC) and Chobanian & Avedisian School of Medicine, beginning in late August 2023.
Paintsil joins BU/BMC after 18 years at Yale School of Medicine, where he assumed progressive leadership responsibilities and most recently, served as section chief of pediatric infectious diseases and global health and a professor in pediatrics and pharmacology. He also was a professor of epidemiology at Yale University School of Public Health and the Yale School of Management.
As a leading physician-scientist and an NIH-funded investigator, Paintsil has focused his research on antiretroviral therapy induced mitochondrial dysfunction; transmission of hepatitis C among injection drug users; and pediatric HIV treatment outcomes in resource-limited countries.

He is a member of the American Academy of Pediatrics, Society for Pediatric Research, Academic Pediatric Society, and the Pediatric Infectious Diseases Society Board; a scholar of the Pediatric Leadership Development Program sponsored by the Association of Medical School Pediatric Department Chairs; and a consultant to Africa CDC in their continent-wide COVID19 mitigation efforts in Africa.
Paintsil began his career in his native country of Ghana, completing his medical degree at the University of Ghana and clinical positions at Korle-Bu teaching hospital, Accra, and Battor Catholic Hospital. He moved to the US to do a pediatric residency training at Lincoln Hospital in New York City before joining Yale School of Medicine through a fellowship in pediatric infectious diseases.
Deeply committed to advancing pediatric care training and research and achieving health equity for the communities served by BU and BMC, Paintsil brings strong strategic leadership to the Department of Pediatrics and the Medical Campus community.
He succeeds Bob Vinci, MD, who announced his plans to step down as chief/ chair last April after making countless and lasting contributions to the hospital, school, and broader community.
Bob Vinci, MD, has been appointed an assistant dean for student affairs.

A member of our community for more than 40 years, Vinci is stepping down from
his role as chief and chair of pediatrics effective August 2023. He began his career as a pediatric resident at what was then Boston City Hospital (now Boston Medical Center/BMC) in 1980, going on to hold various leadership positions at BMC and the school before being named chief and chair of pediatrics and the Joel and Barbara Alpert Professor of Pediatrics in 2013.
From his earliest days on the Medical Campus, Vinci demonstrated unmatched collaborative spirit as a partner to his clinical colleagues, students, and patients. He has made significant contributions to the Medical Campus community over the years, such as the creation of the Division of Pediatric Emergency Medicine and establishment of the Boston Combined Residency Program, among many others. ●
Deeply committed to advancing pediatric care training and research and achieving health equity for the communities served by BU and BMC, Paintsil brings strong strategic leadership to the Department of Pediatrics.
ON FRIDAY, MARCH 3, with his wife Miriam at his side, Professor of Anatomy & Neurobiology Ronald Killiany, PhD, peacefully passed away at home following a long illness.
A member of the department for more than 30 years, Killiany held secondary appointments in the departments of neurology and radiology, as well as in environmental health at the School of Public Health.
After earning his PhD in psychology from Northeastern University in 1991, Killiany joined BU, where he did three years of postdoctoral training in neuroanatomy in the department of anatomy & neurobiology that formed the basis of his extensive teaching and research expertise. He was a broadly experienced and innovative leader on many modalities of neuroimaging, neuroanatomical studies, and the cognitive assessment of human and nonhuman primates.

A key investigator and leader for the Alzheimer’s Disease Research Center and the Alzheimer’s Disease Neuroimaging Initiative, Killiany published extensively on the basic and clinical anatomical sciences, neuroimaging, and alterations to the brain during normal and pathological aging. With the late Rahul Desikan, his PhD student, Killiany published a highly influential MRI automated parcellation system that is used worldwide in studies of the human cerebral cortex and has been cited more than 10,000 times.
For more than a decade, until 2020 Killiany served as director of the Center for Biomedical Imaging on the Medical Campus (BUMC), a key role in which he facilitated imaging studies by BUMC and affiliated scientists.
In the three departments with which he was affiliated, Ronald Killiany was a cherished colleague to faculty members, many of whom
fondly recall long, interesting discussions with him about novel research avenues. He was also a caring and concerned primary mentor to countless PhD and master’s students and served on the research advisory and dissertation defense committees of many departments. His door was always open, and he was always willing to share his wise and thoughtful counsel.
Our heartfelt condolences to Ron’s cherished wife Miriam and all his friends and colleagues. He will be deeply missed. ●

At far left, medical students sit on the steps of a neighborhood brownstone in 1885. One hundred and fifteen years later, medical students gather in 2000 to recreate the photo.

In1848, the Boston University Chobanian & Avedisian School of Medicine began as New-England Female Medical College, the first medical school to accept women. Twenty-five years later, Boston University took over the financially troubled school and became the first co-educational medical school in the US, admitting African Americans, Native Americans, and people of Asian descent, even as other schools restricted their access to medical education.
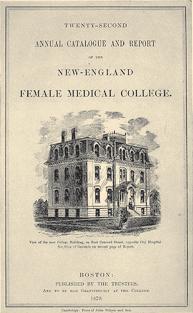

In September 2022 the school celebrated a new name in honor of former medical school dean and Boston University president Aram Chobanian, MD, and his childhood friend Edward Avedisian, a professional clarinetist and successful investor. The renaming came with a $100 million transformative gift that includes $50 million for need-based student scholarships, $25 million for endowed professorships, and $25 million for research and teaching.
Today, Boston University Chobanian & Avedisian School of Medicine is a large, highly ranked institution of health sciences education and research committed to inclusive excellence as we celebrate 175 years of teaching, learning, and discovery on the front lines of our missions of health sciences, education, and research.
The school currently enrolls 650 medical students who continue to experience the traditional educational components important

to generations of BU medical students, including the geriatrics Home Care Program, in which participating medical students are accompanied by faculty to help care for homebound seniors. The innovative program was established in 1875. The traditional firstyear anatomy course continues cadaver dissections, now through simultaneous radiology imaging instruction with CT scans and ultrasound examinations of cadavers in the newly renovated anatomy lab featuring surgical lighting, virtual anatomy enhancements, and more efficient HVAC.
The MD program curriculum constantly evolves to meet the needs of the medical profession of the future, using evidencebased pedagogy rooted in research findings of effective adult education. The curriculum was modified last year to minimize lectures and facilitate more active, team-based learning and collaboration. Students in teams of eight are presented with problem-based learning in the new learning center surrounded by monitors, with several instructors roaming between tables.
The curriculum also recognizes the increasing emphasis on medical student research experiences by competitive residency programs. The school added curriculum components on research principles, opportunities for four-year longitudinal research experiences, and an assistant dean for medical student research. Students are encouraged to seek mentors with peer-reviewed research funding in basic, translational, clinical
Medical education constantly evolves to serve the medical profession of the future. At left, an archival photo of students learning in a research lab setting. At right, students in the new team-based learning center, which facilitates more active learning, problem-solving, and collaboration.

CHOBANIAN & AVEDISIAN SCHOOL OF MEDICINE By The Numbers
FY22 BUDGET
$595M
STUDENTS
649
1,129
MD Master’s/PhD FACULTY
1,487 ALUMNI
12,745
public health, or health services research and are drawn to programs like the Homeless Health Immersion Experience, in which they conduct full clinical interviews and examinations of people experiencing homelessness and explore socioeconomic determinants of healthcare.
There is a wide selection of clinical experiences available to medical students at any of 25 affiliated hospitals and medical centers, including Boston Medical Center (BMC), the primary teaching affiliate and New England’s largest safety-net hospital; St. Elizabeth’s Medical Center; three VA Healthcare System hospitals in Massachusetts and Maine; Kaiser Permanente in Northern California; and 12 affiliated community health centers.
There are 261 PhD students, including 21 MD/PhD in PhD phase and 24 MD/PhD in MD phase, and 721 master’s students enrolled in 33 PhD, MD/PhD, MA/MS degree programs spanning the health sciences, behavioral medicine, clinical research,
and other disciplines in Graduate Medical Sciences (GMS). Certificates also are available in several areas of study.
GMS students can tailor their studies toward their unique career interests. Some of its most established programs include the MS in Medical Sciences (MAMS) program, which has helped more than 3,000 students gain admission to medical school since its founding in 1985. The Physician Assistant Program, fully accredited by the Accredited Review Commission on Education for the Physician Assistant (ARCPA), has enjoyed a 100% pass rate since 2016 on the National Commission on Certification of Physician Assistants Physician Assistant National Certification Exam. Other popular degrees include the forensics programs, the well-known Anatomy Vesalius Program, and Mental Counseling & Behavioral Medicine, the only accredited program of its kind at a medical school.
The broad and interdisciplinary PhD programs teach trainees transferable skills for wide-ranging careers. The
THE SCHOOL FOSTERS scholarship and faculty development in a variety of ways, including endowed professorships and funding opportunities such as assistant professorships and pilot grants.
The highest academic award bestowed on a faculty member and a key tool in attracting and retaining top-flight faculty, endowed professorships offer both prestige and a steady source of additional funding to be used for salaries, research programs, or both, depending on how the use of the money is structured. They are managed so that the principal remains largely intact, and funding can continue in perpetuity. Each year, the University determines what percentage of the endowment to distribute to recipients.
In 2008 Shamim Dahod (CGS’76, CAS’78, CAMED’87) and her husband Ashraf gave $10.5 million to the school to establish the Shamim and Ashraf Dahod Breast Cancer Research Center. The gift also endows an assistant professor and international scholar positions and provides several pilot grants each year.
In 2013 Jack Spivack established the annual Spivack Neuroscience awards to support faculty conducting either clinical or basic research in Parkinson’s, Alzheimer’s,
Chronic Traumatic Encephalopathy, and other neurological disorders.
In 2016 BU Trustee emeritus Richard C. Shipley (Questrom’68,’72, Hon.’22) made a gift to the school through the Shipley Foundation to create a prostate cancer research center, a website with information about treatment options, and an endowed professorship at any rank.
Former Chair of Medicine David Coleman, MD, created 11 endowed professorships through the Evans Foundation endowment during his tenure that are supported by $26 million in endowments: David Seldin, MD, Professor of Medicine (held by Darrell Kotton, MD); Norman G. Levinsky, MD, Professor of Nephrology (Sushrut Walker, MD); Franz J. Ingelfinger, MD, Professor of Gastroenterology (currently vacant); John Noble, MD, Professor of General Internal Medicine (Jeffrey H. Samet, MD, MA, MPH); Joseph A. Vita, MD, Professor of Cardiovascular Medicine (Naomi M. Hamburg, MD, MS); Barbara E. Corkey, PhD, Professor of Medicine (Katya Ravid, DSc); Jerome Brody, Professor of Pulmonology (Jay Mizgerd, ScD); Louis W. Sullivan, MD, Professor of Medicine (Sabrina Assoumou, MD, MPH); David J. Salant, MD, Professor of Nephrology (Laurence H. Beck, MD, PhD); Alan S. Cohen Professor of Rheumatology with $2.5M from
an existing endowed professorship (Tuhina Neogi, MD); and the Gitta and Saul Kurlat Professor in Hematology/Oncology with a $2.5M gift from the Kurlat estate (Mathew Kurlat, MD).
In addition, there are the Skinner Professor of Amyloidosis Research (Vaishali Sanchorowala, MD); M. Stuart Strong and Charles W. Vaughan Professor of Otolaryngology (Gregory Grillone, MD); and the Dr. G. Robert Baler Junior Faculty Professor (Debjani Sahni, MD).
The school awards pilot grants supported by the Sexual Medicine Research Fund; Wing Tat Lee, funded to establish cooperative research programs between the school and Chinese universities (with a preference for Hong Kong); and the Toffler Scholar Program, established by the Karen Toffler Charitable Trust to support researchers, physicians, and scientists working on early-stage, futurefocused brain science.
BU’s Clinical & Translational Science Institute provides pilot funding to help investigators address major challenges in translational science—especially those concerning the special health problems of urban communities—by developing new tools, methods, and processes to expedite clinical and translational research and discovery. ●
umbrella Program in Biomedical Sciences offers first-year students the opportunity to explore a variety of research areas along with a core curriculum to determine the focus of their PhD. The Graduate Program for Neuroscience unites graduate training faculty on the Charles River and Medical campuses, while the Anatomy & Neurobiology, Behavioral Neuroscience, and Biomolecular Pharmacology degrees provide students with the expertise they need to be leaders in their fields.
We’ve also invested in our research mission, including the National Emerging Infectious Diseases Laboratories (NEIDL), the Framingham Heart Study, the Black Women’s Health Study, and the Alzheimer’s Disease, Chronic Traumatic Encephalopathy, Cancer, and Regenerative Medicine centers. A unique research facility, the NEIDL opened in 2017, one of only two university-affiliated biosafety level 4 National Biocontainment Laboratories constructed in the US. The infrastructure is funded by a National Institute of Allergy and Infectious Diseases grant to safely study the most infectious and deadly diseases.


To accomplish our education and research missions , we are committed to recruitment and development of outstanding faculty and to state-of-the-art education and research facilities.Tyler Capen, a Gross Anatomy Lab research assistant, demonstrates the new VH Dissector that displays 3D and cross-sectional views of anatomical structures. The National Emerging Infectious Diseases Laboratories.
During the pandemic, the NEIDL and many other research labs and clinical departments focused on SARS-COV-2, studying how the immune system is alerted to fight (and eventually clear) the virus, as well as on the virus’s clinical complications and treatments.
The role of science in informing the public and policy makers led to the creation of the Center for Emerging Infectious Diseases Policy & Research (CEID), which pairs expertise in diseases—such as COVID-19, Zika, and Ebola—with policy research to advise governments, communities, and academic institutions on how to prepare for and respond to epidemics and pandemics.
To accomplish our education and research missions, we are committed to recruitment and development of outstanding faculty and to state-of-the-art education and research facilities.
OVER THE YEARS, the school has transformed and expanded its physical footprint. Key projects include the 2012 opening of the on-campus Medical Student Residence, the addition of the Godley Digital Media Studio, renovations to the Alumni Medical Library and Gross Anatomy Lab, and the new Learning Center on the fourth floor of the Instructional Building.
The $33 million, nine-story, 86,000-square-foot building offers below-market rents subsidized by more than $13 million in gifts from members of the Dean’s Advisory Board.

A vibrant hub within our community, the property contains 104 two-bedroom suites for 208 students, each with a full bath and kitchenette. All units include utilities, furnishings, appliances, cable, and Wi-Fi. The first floor features a large common space to facilitate group study and amenities that foster a sense of community, including a baby grand piano, laundry facilities, and a large kitchen. A large green space with seating and a community garden is adjacent to the building.
Thanks to a gift from the Godley Family Foundation, the 2016–2017 academic year began with a state-of-the-art resource: the Godley Digital Media Studio, which propelled the BU Medical Campus into full and productive use of technology in teaching and learning.
The school continues to foster scholarship and faculty development through a variety of professorships and funding opportunities including core facilities, pilot grants, assistant professorships, and multiple faculty development programs (see sidebar).
Over the years, the school has transformed and expanded its physical footprint (see sidebar). Key projects include the 2012 opening of a $40 million on-campus Medical Student Residence, the addition of the Godley Digital Media Studio, recent renovations to the Alumni Medical Library, Gross Anatomy Lab, and the new Learning Center on the fourth floor of the Instructional Building.
“We are positioning the Boston University Chobanian & Avedisian School of Medicine to become the place students and faculty want to be. The best place to learn, teach, and discover,” Dean Antman said. “We celebrate the contributions of our faculty, staff, students, alumni, parents, and friends as we celebrate this 175-year milestone and build for the future.” ●
Located on the third floor of the Instructional Building, the studio is equipped with a faculty workstation to create and edit recordings, a video production studio with a full editing suite, and a ReadyCam that simplifies live television appearances,
“ We are positioning the Boston University Chobanian & Avedisian School of Medicine to become the place students and faculty want to be. The best place to learn, teach, and discover.”
DEAN ANTMANMedical Student Residence
that enable researchers to conduct interviews with national media outlets without leaving the Medical Campus.
The media studio allows for enhanced computer-based training and improves distance learning opportunities. The studio revolutionized hybrid digital learning on campus before it became mandatory during the COVID-19 pandemic.
The 2014 renovation of the 11th floor of the Alumni Medical Library created a 220-seat testing center to facilitate exam administration while enhancing the quality of study space for all students on the Medical Campus.
A 2019 renovation expanded options for individual and small group study, including carrels, individual study pods, group study rooms, and spaces for one-on-one tutoring.
An anonymous gift allowed for a $1 miilion renovation to the Gross Anatomy Lab that began in 2020 and recently was completed. The upgrade recognizes that there are multiple pathways to learning and is in step with the new curriculum changes implemented this year for the Class of 2026 that incorporate self-directed learning and early exposure to clinical concepts.
New windows flood the 10th-floor lab with sunlight, including the area where dozens of donor bodies lie in bright blue body bags on portable dissection tables.
The renovation improved communications for instructors with an enhanced sound system and monitors linked to iPads, as well as updated lighting, heating, air conditioning, and ventilation. New technology includes ultrasound units and an Anatomage virtual dissection table. The communication upgrades allow images from the VH Dissector, which displays 3D and cross-sectional views of more than 2,000 anatomical structures shown on monitors throughout the lab.
The new technologies also lend color and a realistic look to organs and other structures that can be relatively colorless and physically flattened in donor bodies due to the embalming process. Newly acquired technologies like the VH Dissector and the Anatomage also help students interpret the images from similar instruments like ultrasound, Magnetic Resonance Imaging and Computed Tomography scans that students will see in their clinical rotations and throughout their careers as physicians.

Construction was completed in summer 2022 on a $5.5 million learning center that can accommodate up to 200 students divided into teams of eight and seated at round tables.

The new facility is central to the expanded use of the “flipped classroom,” a collaborative team-based approach that is more in line with how students, who have unprecedented access to information on the internet, study today.
Students are given example cases with questions and provided with materials to learn about them outside of the classroom while self-testing to find their knowledge gaps. Upon returning to the classroom, they undergo both individual and team assessments. Then, teams tackle an hours-long investigation, assisted by faculty and content experts working together from across disciplines who visit the various tables with technology that links to screens around the room.
“We wanted to create an open classroom where everyone was on one level, the faculty were walking around, and students really felt like they were connecting with them and learning from them, asking questions and having a dialogue rather than a lecture,” said Associate Dean for Medical Education Priya Garg, MD. ●
Gross Anatomy LabRESEARCHERS LAUD THE DEDICATION OF 15,000 PARTICIPANTS OVER THREE GENERATIONS
Much of what we’ve come to accept as fact about heart disease comes from studying the more than 15,000 volunteers in the Framingham Heart Study (FHS), now celebrating its 75th anniversary.
“Without the participants, there is no science,” says Maureen Valentino, who has worked at the FHS research center for a quarter-century recruiting new participants and looking after volunteers in the nation’s longest-running human observational study.
“You will not find a researcher or scientist on the face of the earth who is not amazed at the dedication of these people. They come from literally all over the world to do the study and they do it faithfully.”
Doug Stein, a 52-year-old tax attorney from an Atlanta, Georgia, suburb and a third-generation FHS participant, embodies that altruism, dedication, and enthusiasm for research.
“You’re really providing information for the betterment of society— but not just our society, for the whole world,” says Stein, whose grandparents were in the first cohort of participants in 1948. Stein’s parents were in the second-generation study and his children are already asking when they will be included.
“I look at it as a gift to my kids. It’s a unique opportunity for them to participate in something much greater than they are; likely greater than they could ever realistically become,” says Stein.
Often referred to as the “jewel of cardiology,” the Framingham Heart Study’s research center fits into the modest footprint of a dozen wood-paneled examination rooms. On most weekdays, a half-dozen participants arrive at the facility for a five-to-six-hour examination that some of them liken to a supercharged physical.
“Honestly, I really enjoy the tests. There hasn’t been anything they’ve asked me to do that I’ve said no,” says Samira Brown, MD, a pediatrician who grew up in Framingham and now lives in Georgia.
Participants volunteer expecting no tangible reward, rarely miss an appointment over a lifetime of testing, and pass along that responsibility to their children and grandchildren. Researchers like Joanne Murabito, MD, FHS research center director and principal investigator, are both proud of and in awe of their dedication.
“This study is their study, and we could not have accomplished
all that we’ve learned about the risk factors for heart disease, the occurrence of heart disease, all of the genetic and molecular factors related to heart disease, without their willingness to come in for the testing and be forward-thinking about all of these new areas of research,” says Murabito, who has worked at the research center for more than 30 years.
It was the death of popular US president Franklin Delano Roosevelt from a cerebral hemorrhage due to runaway hypertension that shone a light on the knowledge deficit around heart disease, the nation’s number one killer.
Renowned epidemiological cardiologist and longtime director of the heart study William Kannel, MD, first coined the term “risk factors,” largely preventable lifestyle choices like smoking, obesity, and high cholesterol that could bring on heart disease. Incredibly, Kannel and other top researchers were initially as unaware as the public was about them.
Kannel’s daughter Linda Isaacson, a second-generation participant, recalls cigarette, cigar, and pipe smoke hanging in the air of her family’s living room at the informal meetings of physicians and researchers affiliated with the study, even as they debated the possible causes and treatments of heart disease.
“When they’d get together, they all used to smoke and when they found out it wasn’t good for them, they stopped,” she says.
In 1948 President Harry Truman signed the National Heart Act, creating the National Heart Institute and dedicating $500,000 to a 20-year epidemiological study focused on cardiovascular disease that became the FHS. Almost right from the start, FHS research drove the science and public health policy surrounding heart disease and strokes, establishing links to smoking, obesity, hypertension, high cholesterol, and atrial fibrillation.
At the close of a world war, with mobilization and volunteerism for the common good still in the public consciousness, half the adult population of Framingham—5,209 people—signed up for the first round of the study. Doug Stein’s paternal grandparents, who immigrated from Russia and Poland around 1943 to escape the horrors of WWII, immediately agreed when asked to participate in the initial phase of the study.
“They felt that being immigrants, they owed the country something
At the close of a world war, with mobilization and volunteerism for the common good still in the public consciousness, half the adult population of Framingham—5,209 people—signed up for the first round of the study.
and this was payback; this was a way for them to help the country. It was a heartfelt emotion,” says Arthur, Doug Stein’s father and a second-generation FHS participant for nearly 50 years.


Succeeding rounds of funding extended the study’s life span, with 5,124 children of the original group of volunteers and some spouses recruited in 1971, followed by 4,095 third-generation children in 2002 and 103 of their spouses in 2003. Until the 1990s, recruitment had been generational through families and 100 percent white European Americans.

To reflect an increasingly diverse town and nation, the study established two new groups referred to as the Omni cohorts, comprising African Americans, Hispanic Americans, Asian Americans, among others, with 507 participants recruited in the 1990s and an additional 410 of their children from 2003 to 2005.
Samira Brown’s mother Cheryl said she and her husband initially had reservations about participating given how Black people had historically been treated in other medical studies. Her husband Leonard Brown, an associate professor of music at Northeastern University, decided against it.
“I don’t think he distrusted the Framingham Heart Study, but he said, ‘On principle, I’m not going to participate.’ But my position was,
I want to do everything I can to have an impact on the health of future generations—my own, my children’s, my grandchildren’s,” says Cheryl Brown.

In her medical residency program when the invitation came, Samira Brown decided that the FHS was open, transparent, and important—and signed up. She convinced her brother to join, too. “It is very empowering for me to be able to do something as a participant and as a Black physician. As we battle these health disparities, [diversity and inclusiveness] really are important and I think the Framingham Heart Study is a great model,” she says.
One of the reasons for the study’s longevity is its personal approach with participants, notes Christine Hess, the research center manager.
“I think the culture of the place exudes appreciation,” says Brown. Framers of the research made two critical decisions early on that have helped it endure. They incorporated women, which was rarely done in longitudinal studies at the time, and they decided they’d recruit within families, hoping that familial pressure would help ensure cooperation and provide new sources of study participants. This also inadvertently created a generational database that the thenundeveloped science of genetics could use to look at links that might predispose someone to heart disease, even without other risk factors.
“When I was interviewing third-generation participants—the grandchildren of the original participants—they said, ‘I’m here because my grandmother told me to come in.’ So, there is a real family commitment to giving back, and to participating in the science. I heard that a lot,” says Murabito.
Like his parents before him, Arthur Stein didn’t talk much about his participation. Since the 1970s, whenever his exam date came up he’d tell his employer and family that he had a medical appointment, then travel to Framingham from Schenectady, New York, where he worked as a nuclear engineer, and then from Sharon, Massachusetts, after the family moved there.
While he doesn’t have the cross-country commute of his brother in Washington State, Doug Stein still needs two or three days off to fly in from Atlanta, Georgia, which he views as time to tune out of his hectic life and focus on himself. Like the Browns, Isaacsons, and Stein families, he has never missed an appointment.
“Even when I go on vacation, I’m always on the cell phone, always emailing,” he says. “When I go to the Framingham Heart Study, my phone’s off. You can call me, but I’m not going to answer.”
While the core exam is funded for six-year intervals, the 60 to 70 FHS-affiliated researchers use grant money to pay for ancillary studies. Cheryl Brown says she’s volunteered for many over the years, including cognitive research that has her traveling back to Framingham from her Bethesda, Maryland, home every few months.
Circulatory system and heart health affect many other organs and, almost right from the start, additional tests have been added to the core exam. Murabito points out that a particularly big shift took place a little more than five years ago when the primary funder, the National Heart, Lung, and Blood Institute, expanded testing to incorporate other organs and systems impacted by the circulatory system including pulmonary, brain, bone, and cognitive function.
The FHS had always employed cutting-edge tools, and testing grew to incorporate technologies like electrocardiogram, magnetic resonance imaging, computed tomography, bone density scanning, and echocardiogram. With miniaturization, testing has expanded to wearable devices like EKGs and a blood glucose monitor that participants take home for 10 days.

Ancillary tests are approved by a panel for safety and efficacy, says FHS Recruitment Manager Valentino. Participation is strictly voluntary, but many do so because they trust the staff and want to help.
“If it’s associated with the heart study, then yes, I’ll sign up,” says Max Chang, an energy consultant from Sudbury, Massachusetts, who’s been a participant, including in many ancillary studies, for the past two decades. “I’ve done everything. I’m a willing participant.”
Murabito says that longitudinal studies typically don’t last 20 years, and she doesn’t know of any that have even come close to the FHS’s 75. It’s the loyalty and dedication of participants that has allowed the study to continue and allowed researchers to see risk factors play out over a lifetime, something known in genetic medicine research as deep phenotyping.
Soon to span four generations, the FHS database offers researchers a window into the biology and biologic pathways linking the gene to the disease, which could help identify new medications and treatments.
“When we have an association with the gene and a biologic pathway, you can then target for medication treatments to prevent cardiovascular disease or other diseases of interest and really understand what is causing the risk for those diseases,” says Murabito.
FHS research has helped produce new treatments like blood pressure medications and has changed the conversation from heart disease being an inevitable consequence of aging to smoking cessation and healthier diets.
According to the National Institutes of Health, deaths from heart disease dropped from a peak of nearly 750,000 in 1968 to 365,000 in 2014, with half of that decline attributable to reducing the impact of those risk factors through lifestyle and diet changes.
Arthur Stein looks back on his 40 years as a participant and his family’s involvement over the entire 75 years of the study with a sense of mission and pride.
“The Framingham Heart Study, at least from my perspective, was on the forefront of technical and medical research to prolong people’s lives,” says Stein. “I feel proud I was a part of that.”●
“When I was interviewing third-generation participants—the grandchildren of the original participants— they said, ‘I’m here because my grandmother told me to come in.’ So, there is a real family commitment to giving back.”
JOANNE MURABITO, MD, FHS RESEARCH CENTER DIRECTORTesting has expanded to wearable devices.

Self-reported interpersonal racism in employment, housing, and interactions with the police was associated with a 26% higher risk of coronary heart disease among Black women, according to preliminary research presented at the American Heart Association’s Epidemiology, Prevention, Lifestyle & Cardiometabolic Health Scientific Sessions 2023.
“Many Black adults in the US are already at higher risk of developing heart disease due to high blood pressure or type 2 diabetes,” said study lead author Shanshan Sheehy, MD, MSc, ScD, an investigator at BU’s Slone Epidemiology Center and assistant professor of medicine. “Current evidence shows that racism may act as a chronic stressor in the human body and chronic stress may lead to high blood pressure, which increases the risk of heart attack and stroke.”
Researchers evaluated data for approximately 48,000 individuals enrolled in the Black Women’s Health Study, the largest follow-up study on the health of Black women in the country. They reviewed data gathered from 1997—two years after the study began—through 2019 to investigate whether self-perceived interpersonal racism was associated with an increased risk of coronary heart disease. In 1997, participants answered five questions about their experiences related to interpersonal racism in their everyday activities, such as “How often do people act as if they think you are dishonest?” and three questions that asked “Have you ever been treated unfairly due to your race in any of the following circumstances?” The circumstances included employment (hiring, promotion, firing); housing (renting, buying, mortgage); and interactions with police (being stopped, searched, threatened).
Researchers calculated a perceived interpersonal racism score for the three questions on interactions that involved jobs, housing, and police. Their analysis found that women who reported experiencing racism in all three categories
Researchers evaluated data for approximately 48,000 individuals enrolled in the Black Women’s Health Study, the largest follow-up study on the health of Black women in the country.
had an estimated 26% higher risk of heart disease relative to those who answered no to all three questions.
Sepsis occurs in approximately 1.7 million hospitalizations in the US, with more than a third of hospitalizations resulting in death. Patients with septic shock benefit from steroid medications (corticosteroids) to reduce shock duration and potentially decrease the chance of dying. However, it is unclear if one of the two most frequently used steroid regimens (hydrocortisone alone versus hydrocortisone and fludrocortisone together) is better than the other.
A new study in JAMA Internal Medicine by school researchers shows that patients receiving a combination of hydrocortisone and fludrocortisone had lower death rates and discharge to hospice compared to those who received only hydrocortisone.
Sepsis occurs in approximately 1.7 million hospitalizations in the US, with more than a third of hospitalizations resulting in death.
To compare the effectiveness of both treatment regimens, the researchers used a large multicenter database made up of approximately 25% of US hospitalizations and an observational study design that was intended to mimic a randomized clinical trial to compare the outcome of death or discharge to hospice between patients who received the regimen of hydrocortisone and fludrocortisone to those who received hydrocortisone alone.
They found that the regimen of hydrocortisone and fludrocortisone together was superior to hydrocortisone alone. On average, patients who received hydrocortisone and fludrocortisone died or were discharged to hospice approximately 4% less compared to patients who received hydrocortisone alone.
According to the researchers, these findings may change clinical practice. “It is possible that guideline recommendations, which currently suggest starting hydrocortisone alone, will change as a result of this study,” said researcher Nicholas A. Bosch, MD, MSc, who also is a pulmonologist at Boston Medical Center.
The immune system plays a pivotal role in our health, which depends on the approximately 30 trillion cells that make up the human body properly interacting with and supporting each other. One defining characteristic of aging is a decline in the proper functioning of that system. Centenarians, rare individuals who reach 100 years or
more, experience delays in aging-related disease and mortality, suggesting that their immune systems function into extreme old age.
Led by school researchers, a new study finds centenarians harbor distinct immune cell type composition and activity and possess highly functional immune systems that have successfully adapted to a history of sickness, allowing for exceptional longevity. These immune cells may help identify important mechanisms to recover from disease and promote longevity.
“We assembled and analyzed what is, to our knowledge, the largest single-cell dataset of centenarian subjects that allowed us to define unique features of this population that support the identification of molecular and lifestyle factors contributing to their longevity,” explained senior author Stefano Monti, PhD, associate professor of medicine.
Their analysis confirms observations made in previous studies of aging and identifies novel cell type-specific compositional and transcriptional changes that are unique to centenarians and reflect normal immune response.
The researchers believe these findings provide a foundation to investigate mechanisms of immune resilience likely contributing to extreme longevity as a target for healthy aging therapeutics.

Long careers in American football are linked to less white matter in the brain and are associated with impulsive behavior and thinking, according to a new study from the Boston University CTE Center. This finding is independent of whether football players had chronic traumatic encephalopathy (CTE).
This new study suggests that a separate type of brain damage, which can appear earlier than CTE, may underlie some of these symptoms.
“Damage to the white matter may help explain why football players appear more likely to develop cognitive and behavioral problems later in life, even in the absence of CTE,” said corresponding author Thor Stein, MD, PhD, a neuropathologist at VA Boston Healthcare System and assistant professor of pathology & laboratory medicine.
The researchers studied the brains—donated to the Veterans Affairs-Boston University-Concussion Legacy Foundation Brain Bank—of 205 deceased American football players and measured levels of myelin, a component of white matter that covers, protects, and speeds up connections in the brain. They then interviewed
The researchers believe these findings provide a foundation to investigate mechanisms of immune resilience likely contributing to extreme longevity as a target for healthy aging therapeutics.
family members on measures of cognition and impulsivity, comparing how career length and age upon starting to play tackle football related to levels of myelin, and how myelin levels related to cognition and impulsivity. In addition to more years of football played, the researchers found that starting tackle football at a younger age was also related to more white matter loss, independent of career length.
While most women (86%) felt informed after receiving personal breast density information, some felt anxious (15%) or confused (11%), with women of color and those with low literacy more likely to report feeling anxious or confused and less likely to feel informed.
A new study among a diverse group of women published online in Women’s Health Issues has found that reactions to breast density information vary significantly by sociodemographics: non-Hispanic Black, Asian, and Hispanic women, and women with low literacy, were nearly two to three times more likely to report anxiety after learning about the implications of dense breasts than nonHispanic white women.
“Understanding how different groups of women respond to breast density information is essential in ensuring that its provision does not inadvertently exacerbate inequities in breast cancer outcomes by deterring some from undergoing future mammographic screening,” said corresponding author Nancy Kressin, PhD, professor of medicine.
Researchers surveyed a large, diverse sample of American women about their reactions to receiving breast density information and their plans for future mammographic screens, examining how these reactions related to women’s race/ethnicity and literacy levels.
While most women (86%) felt informed after receiving personal breast density information, some felt anxious (15%) or confused (11%), with women of color and those with low literacy more likely to report feeling anxiety and confusion and less likely to feel informed. Specifically, non-Hispanic Black and Asian women were nearly twice as likely to report that knowing their breast density made them more likely to have future mammograms. ●
On April 27, members of the BU Chobanian & Avedisian School of Medicine’s Chester S. Keefer, MD, Society, which recognizes donors who have supported the school with lifetime gifts totaling $50,000 or more, gathered at the Hotel Commonwealth for the society’s 28th annual dinner.

After a cocktail reception, Keefer members and their guests heard welcoming remarks from BUMC Provost and Chobanian & Avedisian SOM Dean Karen Antman, MD, Donald M. Kaplan, MD (CAMED’73), chair of the Dean’s Advisory Board, and medical students Amos Mwaura (CAS’22, CAMED’26), Sarah Schroter (CAMED’26), and Andrew Girgis (CAS’21, CAMED’26).
Dean Antman then introduced the Keefer Society Class of 2023:
Silver Members
● Tania J. Phillips, MD, and Jeffrey S. Dover, MD
Mercury Members
● Carol A.S. Arndt, MD (CAMED’78)
● Amin Ashrafzadeh, MD (CAMED’97) and Christine Ashrafzadeh (CAS’92, Questrom’96)
● Gary J. Balady, MD and Rosemary Mehl, MD
● Howard C. Bauchner, MD (CAMED’79) and Christine M. McElroy, PhD
● Mackenzie M. Boedicker and Deborah D. Boedicker
● David M. Center, MD (CAMED’72) and Patricia Rabbett
● The Ginwala Family
● Harold M. Ginzburg, MD (CAMED’68) and Jenny Boyer
● John P. Howe III, MD (CAMED’69, Hon.’19) and Tyrell E. Flawn
● Kenneth P. Kato, MD (CAMED’89) and Nancy A. Nagy
● Paul M. Leiman, MD (CAMED’74) and Carol R. Leiman
● Praveen V. Mummanemi, MD (Questrom’95) and Valli P. Mummanemi, MD
● Ethan Shevach, MD (CAMED’67) and Ruth S. Shevach
The estate of Marcelle Willock, MD, professor emerita of anesthesiology and chair of the department from 1982 to 1998, has made a $1.2M gift to the Violeta Martinez and Rafael Ortega Anesthesiology Research Fund at the Chobanian & Avedisian School of Medicine. Willock passed away on October 12, 2022.

The fund name honors the parents of Chair and Chief of Anesthesiology Rafael Ortega, Willock’s mentee and longtime friend.
Established with a gift from Willock in June 2021, the fund will support a Department of Anesthesiology postdoctoral associate or junior faculty member in department research while helping them pilot their individual work under the mentorship of senior faculty, ultimately building a pipeline of future anesthesiology researchers.
“Of the many admirable personal qualities Dr. Willock possessed, generosity tops the list. We will use this research fund to continue refining the department of anesthesiology as a bastion of educational and academic excellence,” said Ortega. ●
The department created a space honoring Marcelle Willock with historical medicine books donated by her estate. The rocking chair, presented to her when she retired, is now a seat of honor reserved for those who have made significant contributions to BMC, BU, and society at large.
On April 28, the Dean’s Advisory Board held its annual spring meeting in a hybrid format.
Board members heard updates from Dean Karen Antman, MD, and Associate Dean for Development Suzanne Maselli, and presentations on graduate medical sciences from Associate Provost and Dean Jamie McKnight, PhD, and a fourth-year MD student panel moderated by Associate Dean for Student Affairs Angela Jackson, MD.
In-person attendees also toured the new Team-Based Learning Center and watched a technology demonstration by David King, the instructional technology team lead.
The day concluded with Associate Dean for Admissions Kristen Goodell, MD, discussing the Supreme Court decision regarding the consideration of race in higher education admissions
Rachel Fearns, PhD, and Elke Mühlberger, PhD, professors of microbiology and investigators at the National Emerging Infectious Diseases Laboratories (NEIDL), have each been awarded three-year grants from the Bill & Melinda Gates Foundation to study henipaviruses, bat-borne viruses that cause severe and often fatal illness in humans and could potentially emerge as a pandemic threat.
Fearns, who received $2.26 million, will work with collaborators from Harvard and the University of Massachusetts/Amherst to characterize the structures and functional properties of a henipavirus polymerase, which is essential for the virus to propagate and a good target for antiviral drug development. By characterizing the polymerase in different functional states, the team plans to identify features that are essential for it to make the movements necessary to perform its functions. This research will open the door to developing antiviral treatments against the virus.
Fearns focuses on the transcriptional and genome replication mechanisms of a variety of non-segmented, negative-strand RNA viruses, the virus group that includes henipaviruses. This group contains several significant human pathogens—such as respiratory syncytial virus, human metapneumovirus, measles, mumps, and parainfluenza viruses—and emerging highly pathogenic viruses such as Nipah, Marburg, and Ebola. Her goal is to understand the processes of transcription and genome replication, both at a molecular level and within the context of the cellular environment, to identify targets for drug development.
Mühlberger received $3 million for a highly collaborative project that focuses on using human-relevant infection models to study henipavirus pathogenesis. The BU team combines expertise in studying BSL-4 viruses (Mühlberger); generating human iPSC-derived cells and organoids (Darrell Kotton, MD, David C. Seldin Professor of Medicine, and Gustavo Mostoslavsky, MD, PhD, professor
of medicine & microbiology); using humanized mouse models to study viral infections (Florian Douam, PhD, assistant professor of microbiology); and cutting-edge histopathology approaches (Nicholas Crossland, DVM, DACVP, assistant professor of pathology & laboratory medicine). Stefan Wuchty, PhD, associate professor at the University of Miami’s Miller School of Medicine, will provide expertise in computational modeling. The team will collect and analyze transcriptional data from the various infection models to identify biomarkers and potential drug targets against henipavirus infections in the specific tissues and cell types.
members, paving the way for investigators to complete innovative new projects and pursue novel ideas that will provide preliminary data for future grant applications to other agencies and programs. Awardees also will have access to excellent mentorship resources and the opportunity to build cross-disciplinary collaborations.
To achieve the ACS goal of increasing diversity in cancer research, one pilot award per year will support an investigator from an underrepresented group in biomedical research.
Each have each been awarded three-year grants from the Bill & Melinda Gates Foundation to study henipaviruses, bat-borne viruses that cause severe and often fatal illness in humans and could potentially emerge as a pandemic threat.
Mühlberger has long been interested in studying highly pathogenic viruses that cause severe disease in humans with high case-fatality rates—including Ebola and other viruses that must be handled at the highest biosafety level—and explores different aspects of the viral infection cycle, focusing on identifying determinants of virulence.
Julie Palmer, ScD, codirector of the Boston University-Boston Medical Center (BU-BMC) Cancer Center, has been awarded a $480,000 Institutional Research Grant from the American Cancer Society (ACS) for a three-year period. Through this program that supports newly independent investigators initiating cancer research programs, the ACS aims to invigorate problem-solving, drive innovation, and accelerate cancer research.
The BU-BMC Cancer Center will annually award pilot grants to four early career faculty
“The ACS Institutional Research Grant program has played a critical role in launching the careers of promising newly independent faculty across the many schools and departments at Boston University,” said Palmer, who also is the Karin Grunebaum Cancer Research Professor and director of the Slone Epidemiology Center. “We are excited to have this opportunity to continue supporting outstanding cancer research.”
The Vertex Foundation has donated approximately $305,000 for two diversity initiatives at the school. For the third consecutive year, the foundation’s commitment will expand opportunities for students pursuing education in medicine and STEM fields.
Vertex Foundation funding will support the Early Medical School Selection Program (EMSSP) as well as BEAMS (Boston Education, Advising & Mentoring in STEM).
Established in 1982, EMSSP is a partnership with Historically Black Colleges and Universities as well as schools serving largely Latinx and Pacific Island populations. Students from partner schools are accepted to Boston University during junior year; programming is designed to support their successful application and matriculation to medical school. Similarly, BEAMS aims to engage, develop, and retain underrepresented youth from Boston Public High Schools in healthcare and STEM curricula. Both programs offer
important support, networking opportunities, and mentoring to enhance educational success, a sense of belonging, and diversity in the healthcare and biomedical research workforce.
“I am immensely grateful,” said Angelique Harris, PhD, associate dean for diversity & inclusion. “These grants are helping us to build a culture of inclusion and belonging for structurally marginalized students, many of whom faced multiple educational barriers. Our long-term goal is to diversify STEM fields, leading to more impactful healthcare and innovative biomedical research.”
“The Vertex Foundation seeks to improve the lives of people with serious diseases and contribute to our communities through education, innovation, and health,” said Eustacia McNaught, vice president for community affairs.
“We are proud to continue our support of the EMSSP and BEAMS program, both of which are focused on expanding opportunities for students who have been traditionally underrepresented in STEM.”
“Our partnership with the Vertex Foundation has been enormously instrumental in advancing our shared commitment to diversifying science education and the STEM workforce,” said Karen Antman, MD, BUMC provost and dean of the Chobanian & Avedisian School of Medicine.
In addition to its multiyear commitment to the medical school, the Vertex Foundation has generously supported the University’s Center for Antiracist Research as its first corporate foundation partner.
Xiaodan Qin, PhD, a research scientist in the Feng Lab in the Department of Pharmacology, Physiology & Biophysics, has been awarded a $400,000 Warren Alpert Distinguished Scholar Award from The Warren Alpert Foundation.
The Warren Alpert Distinguished Scholars program supports postdoctoral researchers who advance to full-time faculty by helping them develop a laboratory program that will lead to independent funding. With this award, Qin will study neuroblastoma, a common extracranial solid tumor responsible for approximately 15% of cancer-related deaths in children. Specifically, she will use the zebrafish model to identify the molecular underpinnings promoting tumor immunosuppression and to evaluate their suitability as novel therapeutic targets.
Qin hopes to test currently available antibodies as more effective treatments containing fewer toxicities for children with neuroblastoma, and potentially other types of neuronal cancers as well. Her long-term research goals focus on the elucidation of molecular mechanisms through which tumor cells escape immunosurveillance, and the development of an effective immunotherapeutic for cancer treatment. ●
Both programs offer important support, networking opportunities, and mentoring to enhance educational success, a sense of belonging, and diversity in the healthcare and biomedical research workforce.
THIS YEAR, BOSTON UNIVERSITY CHOBANIAN & AVEDISIAN SCHOOL OF MEDICINE IS CELEBRATING SOME EXCITING HISTORICAL EVENTS: the 175th anniversary of our institution’s inception and the 40th anniversaries of two of our pathway programs, the Early Medical School Selection Program (EMSSP) and the Modular Medical/ Dental Integrated Curriculum Program (MMEDIC). Please see those stories on page 14.
As we celebrate our school’s long and distinguished history, we look to the future and the amazing work we seek to accomplish.
In the spirit of continuing our mission, we had a successful Giving Day on April 11, with 168 unique donors contributing to our school. Their gifts will assist need-based scholarships, provide funding for future health research discoveries, and support student participation in community-based programs. With your generosity, we continue to strive forward, pushing the boundaries of scientific and medical knowledge, as we have these past 175 years.
Our Alumni Stories series continues in this issue with profiles of six of our EMSSP alumni: Chantale Branson, Ebonee Carter, Joshua Joseph, Toya Kelley, Frederick Powell, and Shawn Smith. This early assurance program provides a supportive environment for talented medical students to thrive in their medical careers, as our extraordinary alums have shared.
We have returned to in-person alumni events and at Wine Down After Rounds students, alumni, and faculty appreciated the social interaction and opportunity to exchange ideas and talk about professional careers during this always enjoyable event.
We look forward to Alumni Weekend September 22 to 24, which coincides with the EMSSP 40th Anniversary Homecoming Weekend. To learn more about the schedule of events, scan the QR code at the bottom of this page.

We strive to provide our alumni with meaningful programmed events that connect former classmates, other graduates, and current students. If you would like to sponsor an event, please share your thoughts with us so we can work together to create impactful memories for our community. The Alumni Association welcomes your feedback!
As always, we deeply appreciate your insights and your connection to our school.
Chobanian & Avedisian School of Medicine Alumni Association announces the 2023 Distinguished Alumni Award recipient
Heather Miselis, MD, MPH (CAMED’00,04, SPH’00) Assistant Dean for Alumni Affairs
Kewalramani, MD (CAS’98, CAMED’98)
President & CEO, Vertex Pharmaceuticals
For her outstanding career in nephrology, healthcare leadership, and the biotechnology industry
Dr. Kewalramani will be recognized at an in-person ceremony and luncheon on Friday, September 22, as part of Alumni Weekend events. Congratulations!

Her mother felt differently.
“She was so excited for me. She started literally screaming, and that made me excited about the possibility, the prospects,” Branson recalls. The friendships she made with other EMSSP students and the experience of bonding with others during the summer program eased the transition.
Chantale Branson knows exactly when she first expressed her interest in medicine: in elementary school, as the principal circulated among the students in the auditorium and asked what they wanted to be when they grew up.
“I mispronounced the word, but I distinctly remember saying I wanted to be a pediatrician,” says Branson, a movement disorders/sleep specialist and assistant professor of neurology at Morehouse School of Medicine in Atlanta.
She clung to that desire while attending performing arts elementary and high schools with the goal of becoming a dancer. Her enthusiasm for medicine resurfaced when she attended Clark Atlanta University in Atlanta, graduating with high honors as a biology major. Her undergraduate dean urged her to apply to Boston University’s Early Medical School Selection Program (EMSSP). Intended to increase diversity in the physician workforce, the program provides support in both the admissions and academic processes and draws from Historically Black Colleges and Universities, and now includes schools with large Pacific Island and Latino populations.
Branson had her doubts. Born and raised in Georgia, she did not feel like a minority attending a Black college, but she knew Boston had a history of segregation and racism.
“I remember thinking I didn’t want to go to Boston; that I wouldn’t feel comfortable,” she says.
In her third year of medical school, Branson found her specialty while on a neurology rotation at the VA Boston Healthcare System’s Jamaica Plain VA Medical Center.

“It just clicked. I just really enjoyed the questions, the science behind it, being able to make a diagnosis based on the physical examination, not relying so heavily on other technology,” says Branson.
Parkinson’s disease in underrepresented and underserved minority populations.
“We’re trying to figure out what type of studies would be best to understand how to eradicate [these disparities in diagnosis and treatment],” says Branson.
Ebonee Carter has always had the feeling that she should be doing more and living up to what she sees as her potential.
After nine years of service, Carter recently left the US Army as a major. Now, as a civilian, she is chief of breast imaging services and a staff radiologist at Fort Belvoir Community Hospital, a military hospital in Virginia, and a radiologist at Howard University Hospital in Washington, D.C.

While on that rotation, she received a call from her father informing her that her paternal grandmother had Parkinson’s disease. The warning signs—including a serious car accident and slowed movement—had been there for years, Branson says, but her family and physician attributed them to aging. A neurologist recognized the signs of Parkinson’s in her grandmother as soon as she walked into the examination room.
That experience, combined with her interest in neurology and the urging of mentor Anna Hohler, MD, adjunct professor of neurology, informed Branson’s choice of career.
“It really shaped the decision I made to pursue neurology. And not just neurology, but movement disorders as a specialty,” says Branson, whose research includes racial disparities in the diagnoses and treatment of
While on active duty, Carter held leadership roles as section chief of computed tomography at Fort Belvoir and radiology chief at Winn Army Community Hospital at Fort Stewart in Georgia. She’s served on nearly a dozen hospital committees and received an army commendation medal and a Meritorious Service Medal.
But there was a point during her first year of medical school when it looked like her life goals were fading into dreams that would never be fulfilled.
Adding to the pressure of parenting— Carter arrived in Boston with her 3-year-old son—was her concern over the debt she was accruing and the unprecedented intellectual rigor of medical school.
Carter failed five courses that first semester and had to petition to retake all five.
Her enthusiasm for medicine resurfaced when she attended Clark Atlanta University in Atlanta, graduating with high honors as a biology major.
“I think in those really challenging times, where you don’t see a path forward, you need mentorship,” she says. Jonathan Woodson, MD, then a professor of surgery and now president of the Uniformed Services University of the Health Sciences, was one of her mentors.
“Dr. Woodson could see that potential in me and say, ‘Okay, she may have failed five classes, but let’s put the supports in place to see that she has child care, so that she’s not carrying her son to class every day, studying in the library with him, and trying to feed him from the hospital cafeteria. Then let’s see what
ty’s Early Medical School Selection Program (EMSSP), which was founded in 1982 to increase diversity in the physician workforce by mentoring selective undergraduates from a dozen Historically Black Colleges and Universities as well as other underrepresented and underserved populations.
At Woodson’s suggestion, Carter joined the Army to help finance her four-year residency and yearlong internship.
“I would say the difference in military medicine from private practice is the access to more treatment options, which are more attainable because it is one collective universal payment program,” says Carter.
says Joseph, assistant professor of endocrinology, diabetes, and metabolism at The Ohio State University and attending physician at The Ohio State University Wexner Medical Center.
As a child, Joseph frequently saw his grandmother self-administering insulin shots. She ultimately suffered two heart attacks, the second one fatal. He later learned that the hospital to which his grandmother was taken didn’t have the advanced cardiac procedures available in other Columbus, Ohio, hospitals.
she can do,’” Carter recalls. “In three weeks, I passed five makeup exams, and people were saying, ‘Oh, we get it, she’s really intelligent.’”
Those were dark days, but she’d been challenged before.
Carter grew up in a single parent household in Des Moines, Iowa. At times, the family lived in subsidized housing and she helped her mother by taking care of her siblings and working to supplement family finances, including summers as a licensed practical nurse. As a result, her schoolwork suffered and she graduated in the bottom half of her high school class, not exactly premed material.
But perseverance and talent run in the family. Carter’s mother is now an assistant teaching professor and graduate student lecturer at Iowa State University.
“I guess that is the whole point of my life, that nothing on paper reflects my potential,” says Carter. “It didn’t change my intelligence. It didn’t change my potential. It didn’t change my tenacity. It didn’t change my ability to defer gratification, to commit to something.”
When given a chance, she prospered. Carter did well at Clark Atlanta University and gained admission into Boston Universi-
Carter supports the EMSSP and affirmative action programs that help level the playing field for minority students whose life challenges outside the classroom can inhibit their academic progress. She believes her classroom, clinical, and personal experience at BU help her understand patients from underserved populations who face obstacles in their daily lives that affect their health and treatment.
“I know I’m going to be effective in a way that other people cannot be, and it’s not just based on color, it’s based on experiences, challenges,” she says. “It’s about having the desire, the presence, the life experience, to be able to do it.”
“I loved her dearly and that really informed my path in so many ways,” says Joseph. “I’m trying to not only improve diabetes and cardiovascular disease, but also the important components of health equity.”
Joshua Joseph’s grandmother was a schoolteacher from Louisiana who came to live with his family in Ohio when he was a child.
“She taught me my ABCs and my 1,2,3s,”
Joseph came to BU from Morehouse College through the Early Medical School Selection Program (EMSSP), which provides students from Historically Black Colleges and Universities early exposure to graduate-level coursework and study skills to enhance their transition into the medical school curriculum. He was named a Martin Luther King, Jr., fellow and was president of BU’s Student National Medical Association, which supports underrepresented minority medical students and underserved communities.
“There was a conglomeration of factors that led me to Boston University, and I was truly blessed by my time there, not only from a medical and scientific standpoint, but also from a social justice and student activism standpoint,” says Joseph, citing the influence of the late EMSSP director,

Joshua J. Joseph
(CAMED’09)
“I guess that is the whole point of my life, that nothing on paper reflects my potential.”
Joseph believes healthcare needs to get out into communities and treat patients within the context of how and where they live.
Kenneth Edelin, MD, a staunch supporter of diversity in medical education and women’s reproductive rights.
By his second year of medical school, Joseph found he wanted more science.
“I was enjoying medicine, I was enjoying medical school, but I had bigger questions,” he recalls. “How do we impact a multitude of people—populations? How do we move forward [on cardiovascular health] and diabetes, not only on the individual level but on a population level?”
With the encouragement of faculty like Neil Ruderman, MD, PhD, professor emeritus of medicine in endocrinology, and Joseph Loscalzo, MD, PhD, the former director of the Whitaker Cardiovascular Institute, Joseph pursued research, extending his medical education with two years in a clinical research fellowship at the National Heart, Lung, and Blood Institute. Following his graduation from medical school, he completed his residency at Yale New Haven Hospital, where he founded and directed the Yale Primary Care Center Weight Management and Wellness Clinic. In 2013, he was named the Christopher D. Saudek, MD, fellow in Diabetes Research at Johns Hopkins University School of Medicine.
“In that [Johns Hopkins] fellowship, I really transitioned, taking all the knowledge from basic molecular pathways and applying it to populations,” says Joseph.
Joseph’s NIH, AHRQ, US Department of Defense, and Robert Wood Johnson Foundation–funded research focuses on advancing equity in diabetes and cardiovascular disease through studying adrenal stress hormones, healthcare system to community interventions, and community-based participatory research in partnership with community-based organizations like the African American Male Wellness Agency, Health Impact Ohio, and the Mid-Ohio Food Collective. As a physician, he employs a team-based, patient-centered approach to living with type 2 diabetes that incorporates lifestyle changes with medical therapeutics.
Joseph believes healthcare needs to get out into communities and treat patients within the context of how and where they
live, which he calls community interventions, or partnering with community groups “to engage people where they are.”
Joseph is back where he started in Columbus, Ohio, and says the opportunities he’s had inspire him to eliminate healthcare inequities that exist in central Ohio and the nation. His grandmother’s struggle with diabetes and heart disease is still on his mind as he pursues his research.
“I love what I do, and being able to have an impact for all those grandmothers, grandfathers, aunts, uncles, parents, and siblings out there really means something to me,” he says. “It inspires me and keeps me working hard every day.”
structural brain anomalies in Gulf War veterans and he found himself drawn to anesthesiology, a choice that also provided a better work-life balance.
Growing up in Durham, North Carolina, Powell did well in school science classes.
“I started to become more and more interested in different fields within science,
Frederick Powell sat in front of his cellphone for this online interview still clad in surgical scrubs. An anesthesiologist and critical care physician at the 100-bed Colquitt Regional Medical Center in Moultrie, Georgia, he loves the operating room.
“I was very, very interested in the operating room,” Powell says of making his career choice when entering his third year of medical school and his fifth in the combined MD/ PhD program. “I had to be very selfish with myself and pick a career that fit well with my PhD. Because this is going to be the rest of your life, you need to make sure that it complements [your interests] and provides you with opportunities to do other things.”
He wasn’t interested in surgery. His doctoral studies were focused on looking at
which led me to be interested in medicine as a career,” he says. He attended North Carolina Central University, one of the Historically Black Colleges and Universities that participate in Boston University’s Early Medical School Selection Program (EMSSP), founded in 1982 to increase diversity in the physician workforce.

Powell spent summers and his senior year at BU before entering the medical school, where a fourth-year EMSSP med student also from North Carolina Central University guided him.
“One of the differences between Boston University and North Carolina Central is, obviously, the level of research. Boston University has very robust research programs,” he says. The physiology involved in anesthesiology attracted him to become a critical care physician.
“I always took pride in and wanted to be one of the people taking care of the sickest people in the hospital,” he says. Also known as an intensivist, the critical care physician is trained to coordinate care of the most critically ill patients.
Powell recalls that when the pandemic hit, Colquitt Regional Medical Center—a rural hospital with a 10-bed intensive care unit—
Frederick Powell (CAMED’11,’11)
“I always took pride in and wanted to be one of the people taking care of the sickest people in the hospital.”
was quickly overwhelmed as larger hospitals stopped taking patients.
With even basic protective and medical supplies limited and no proven COVID-19 treatment, the pandemic had an emotional impact on physicians. “[It was] the toll of seeing so many people pass away that you absolutely could not help,” he says.
Powell was struck by the fact that the vast majority of those who died were unvaccinated. There seemed to be a disconnect; a failure to educate the public. So, he volunteered to participate in an advertising campaign urging vaccination.
“A lot of times as a physician you have to step out on a limb and do things you might not be comfortable with,” Powell says. “But you need your community to follow you because you know that it is the right thing for the greater good of that community.”
them that I knew that I wanted my career to be with children.”
Now an assistant professor of pediatrics at Northwestern University Feinberg School of Medicine, Smith also works as a pediatric hospitalist in one of the two Neonatal Intensive Care Units (NICU) at the Ann & Robert H. Lurie Children’s Hospital of Chicago, serves as director of health equity learning and development, and leads a health equity and advocacy course at Feinberg. Smith earned her undergraduate degree at Clark Atlanta University in Atlanta, Georgia, where she initially focused on child psychology but switched to premed to pursue a career in child psychiatry. In her sophomore year, Smith learned about BU’s Early Medical
“They were a nice, built-in support system, even the [EMSSP] students who were years ahead of me, or who had started residency kept in touch and gave us pointers,” she says.
Her decision to choose hospital-based medicine and work in neonatal intensive care was the result of a pediatric residency rotation in a NICU and a stint shadowing a classmate who was working in the NICU at Lurie Children’s Hospital.
Even in a bustling NICU, Smith enjoys the opportunities to teach.
“When you are working . . . it’s busy, it’s moving. That is the best time, where you get to teach others,” she said. “I want the medical students and trainees I work with to feel really comfortable and confident at the head of the bed, taking care of those infants.”
Smith is a member of the American Academy of Pediatrics (AAP) Advancing Equity in Subspecialties and the AAP Illinois Chapter Equity Diversity and Inclusion.

Shawn Smith traces her interest in medicine to the seventh-grade science classes she loved and the example of an older cousin, a pharmacist who helped her win first place in the school science fair for “Penicillin, The Great Discovery.”
“She really helped me with that,” Smith says. “There were petri dishes all around our house.”
Her mother was an elementary school teacher. “Occasionally, I’d go to work with her, if I had a day off from school,” Smith recalls. “Her students were inquisitive and curious and funny, and I had such a good time with
School Selection Program (EMSSP) developed in 1982 with a consortium of Historically Black Colleges and Universities to increase diversity in the physician workforce.
“I said, ‘Okay, this is my chance,’” she says. “I don’t think I even realized how difficult it was to get into medical school, but that was a wonderful program.”
There’s still a shortage of Black, Latino, and indigenous American physicians, and Smith believes it should remain a priority to introduce students from underrepresented populations to science and medical careers throughout their education.
Though she views medical school as the most challenging experience of her life, Smith fondly recalls the companionship and support of the EMSSP students who became her friends during her time at BU.
Her medical school experience at BU informed her approach to teaching and relating to students as an assistant professor and clinical instructor. “I’m really able to be empathetic and listen to them,” she says. She also applies her previous training to her role as director of health equity learning and development: “I help to make sure our trainees and faculty are aware of the implicit bias we as physicians hold and may take into our patient encounters.”
Smith is currently working on several projects to assess maternal and infant mortality. She is a member of the Northwestern IL-PQC Birth Equity team and the Community Advisory Board for Family Connects, which pairs community health workers in Chicago with expectant birthing people to help them ask the right questions and to ensure good communication between physicians and patients. That support continues through the child’s first year of life.
She believes that physicians need to be out in the community, speaking up for change.
“It is very important for physicians . . . to advocate outside of the patient’s room,” she says.
Shawn Smith (CAMED’03)
“I want the medical students and trainees I work with to feel really comfortable and confident at the head of the bed, taking care of those infants.”
mary education and college, but wasn’t the best test-taker.”
“It had built-in mentorship, and that was important for me,” says Kelley. She enjoyed the collegiality and support of her fellow EMSSP students and faculty.
Kelley respected and admired the late Kenneth Edelin, MD, the EMSSP director during her time at BU.
As a child, Toya Kelley frequently accompanied her mother to her job as a public health nurse at the Fulton County, Georgia, health department.
“I loved what she did, and I just knew I was going to go into a field where I was going to help people,” says Kelley, now a lieutenant commander in the US Public Health Service (USPHS).
Currently stationed in Hawaii, Kelley is the acting deputy chief of the Medical Education and Development Unit for the US Immigration and Customs Enforcement Health Service Corps, overseeing medical education for 1,700 employees who take care of detained noncitizens in 21 facilities nationwide. Prior to this posting, she was the clinical director of a medium-security federal prison and medical director of a White House clinic that served generals, admirals, White House staff, US representatives, senators, and Supreme Court Justices.
Her parents nurtured her childhood dream of becoming a doctor, placing her in science and healthcare camps. She took a purposeful approach when applying to college, choosing Morgan State University in Maryland because it participated in BU’s Early Medical School Selection Program (EMSSP), created in 1982 to increase diversity in the physician workforce.
“That really took it to the top of the list of places I wanted to go,” says Kelley. “That program meant so much to me as an individual who really had excelled through pri-
“He was an amazing physician, and I knew I could learn a lot from him. He was straightforward and told you what you needed to hear,” she says.
While at BU, Kelley bonded with a medical student from New Orleans who had fled
BU, but she was motivated to accept the position after hearing the story of a friend who had received poor healthcare while incarcerated.
“He was genuinely a good person . . . and I hated seeing the care he was receiving,” she says.
The story also caused her to reflect on the many disparities of wealth, power, race, and circumstance in healthcare.
“I thought, this is my opportunity to give that same VIP healthcare to a seemingly undeserving population,” she continues. “Yes, they have done wrong things, but they are constitutionally mandated to receive healthcare and they deserve good healthcare.”
Kelley worked in correctional medicine for three and a half years, then moved into detention healthcare for the next four, working mainly in an administrative role. During that time, she addressed health disparities that affect this population by focusing on reentry and educational programs to improve their healthcare.

the devastation of Hurricane Katrina and lived with her while completing a semester at the school.
“I realized that this is what’s important, this humanitarian response, and I wanted to be that physician who could help no matter what,” she says. “I wanted to be out on the street and if someone needed medical attention, I knew I could listen, I could see, hear, feel, and treat that person.”
She points out that’s what the USPHS does: help the public after natural disasters and pandemics like COVID-19 and provide protection against threats from abroad like Ebola and Zika.
Her first duty station at a men’s mediumsecurity federal prison in South Carolina was an adjustment from the family medicine she’d practiced after graduating from
After she implemented a Stanford University chronic disease self-management program called “Better Choices, Better Health” into the prison system, the quality of life of those who completed the program improved to the point where emergency room visits dropped by 100%.
Kelley believes patient education and personal responsibility are underrated and important healthcare strategies, whether employed in institutional settings or in the general population, and people can learn to manage or even avoid illness.
“The disparities are there. One of the best things we can do is to educate,” she says. “If I can teach one person, then they could teach someone else, who could teach someone else. And then, teaching could be contagious.”
Kelley will spend the next year addressing healthcare inequities and disparities through legislation as a congressional fellow through Georgetown University’s Government Affairs Institute. ●
“The disparities are there. One of the best things we can do is to educate.
If I can teach one person, then they could teach someone else, who could teach someone else.”
John Cloherty of Westwood, Massachusetts, writes, “Just published the 9th edition of Cloherty and Starks’s Manual of Neonatal Care.”
Joel Potash of Syracuse, New York, writes, “A good year at 86. In 2022 I received the annual Dorothy Reister Award from Stone Quarry Hill Art Park in Cazenovia, New York. I also was named area Board Member of the Year in the Arts by Le Moyne College in Syracuse. I am a Master Gardener through Cornell Cooperative extension. I just renewed my medical registration, as I sometimes served at a free clinic, and have escaped COVID so far.”
them. I’m fortunate to be able to have a great work-life balance, and Christine and I have just celebrated our 45th wedding anniversary. We continue our passion for travel, having spent two weeks in Egypt last month. We are planning an adventure to Thailand, Cambodia, Laos, and Vietnam later this year.
“I am most proud, however, to be serving on my 23rd pediatric reconstructive mission to Colombia, where I lead a team from Healing the Children, Northeast. Over the last 22 years we have operated on 1,200 children with a variety of congenital, traumatic, and disease-related deformities. I continue to follow my rock and roll fantasy as the drummer for my band, The Regressions, and for a group of talented plastic surgeons/musicians, the Plastic Surgery Jam Band.
“Thank you for accepting me back in 1969 and giving me the opportunity to follow a wonderful career in medical practice. Rock On!”
William Frishman of Ardsley, New York, writes, “After 25 years as chairman of medicine at New York Medical College and director of medicine at Westchester Medical Center and its Health System, I am now in emeritus rank but still active in clinical and academic work. George Hines and I edit a medical journal together, Cardiology in Review. I also serve as an editor of The American Journal of Medicine.”
Robert Gilman of Ann Arbor, Michigan, writes, “I am still working as full-time faculty in plastic surgery at the University of Michigan, where I am director of aesthetic surgery. I love the privilege of working with our residents, teaching them, and, at the same time, learning from
Patricia Donahue of Milton, Massachusetts, writes, “Kevin, my husband, and I cannot make this reunion. We think of our BU time as an incredible experience. I am still practicing radiology, although part time. Kevin graduated from BU School of Public Health in 1979. Our son Kevin graduated from the medical school in 2006; his wife Erin graduated in 2004. Our son John graduated Boston University School of Law for his LLM master’s in law and taxation. His wife Margaret attended Boston University and graduated from Mass College of Pharmacy. So, we are a BU family! We have eight lovely grandchildren ranging in age from 3 to 13 and enjoy every moment. Who knows, there may be some more Boston University graduates in the future from the family.”
Mardia Stone of New York, New York, writes, “I’m excited to share class notes on my most recent achievements. I’ve coauthored a book, Collapse and Resilience: The Inside Story of Liberia’s Unprecedented Ebola Response (2014–2016), with Tolbert Nyenswah, who was the incident manager. Scheduled release date is October 24, 2023. Johns Hopkins University
Press is our publisher. Ellen Johnson Sirleaf, the former president of Liberia, did the foreword.
On December 9, 2022, African Economic Development Solutions of Minnesota honored me with a lifetime leadership award for significant contributions to the African diaspora community in the US and Africa in general. The award ceremony was held during the third National African Leadership Conference in Minneapolis. I was delighted to receive the award from Professor PLO Lumumba, a renowned Kenyan lawyer and Pan African activist who was also the keynote speaker.
Thank you for your service and dedication to alumni. Looking forward to seeing you at our 45th class reunion on June 10.”
Ziv Haskal of Charlottesville, Virginia, writes, “This year the Society of Interventional Radiology awarded me its Gold Medal, making me the only member to have received that and its Innovator Award, give the Dotter Lecture, and serve as (two-term) editor in chief. Another book released in July 2022, and I am launching two global research trials. Early planning for a video interview talk show we’ll shoot in the fall. Happy that we are all traveling again!”
Sanjay Lalla of West Orange, New Jersey, writes, “Saw classmates Jane and David Cohen during a recent visit to Miami Beach for a plastic surgery conference.”

writes, “Just wanted to share a reunion of sorts in April 2023. Five of us who started in the BA/MD program in 1985 met up in New York City when David Druckman was visiting from Minnesota. From left to right, Suneet Mittal, Charnjit (CJ) Singh, Ben Tsoi, Rohit Bhalla, and David Druckman. It was a wonderful evening sharing memories of our time at BU and where we are now after 30-plus years. It was wonderful to hear about the ways folks are making big contributions to medicine and the lives of their patients.”

Horace Wu of Irving, Texas, writes, “Cannot believe it has been over 30 years since graduating! It was wonderful seeing old friends and meeting new ones during the reunion in Boston last September. I have been in a private pathology practice in Dallas for almost two decades. My wife is also a private practice physician and medical director of an in-patient acute care rehab hospital here in DFW. We will finally be empty-nesters this summer. Our daughter is currently in her third year of the accelerated Six-Year BA/ MD Program at the University of Missouri-Kansas City. My son also will be attending the same medical program at UMKC, starting as a freshman in August. Looking forward to having two more doctors joining the family!”
Karen Splansky Farbman of Needham, Massachusetts, writes, “I served as an attending in pediatric emergency medicine, assistant professor of pediatrics, Harvard Medical

School. I was forced into retirement when I suffered a stroke in September 2017. I miss clinical work, but I still find ways to stay involved behind the scenes, volunteering on medical committees. I miss our days together, dear classmates. My daughter is following in my footsteps, embarking on residency in pediatrics starting this summer.”
Elizabeth Winfield of Breckenridge, Colorado, writes, “First year empty-nesting, our son is premed at UCLA while we play and travel from home in Breckenridge, Colorado. Busy with family medicine at Summit Medical Center. We love riding our bicycles and enjoying the outside in our beautiful community.”
Michael Leddy of Alexandria, Louisiana, writes, “Louisiana orthopaedic surgeon and sports medicine specialist Michael J. Leddy III, MD, FAAOS was elected secretary of the Board of Councilors (BOC) of the American Academy of Orthopaedic Surgeons (AAOS), assuming the new role following the recent AAOS 2023 annual meeting in Las Vegas. As BOC secretary, Dr. Leddy also serves on the AAOS Board of Directors. He will assume the
role of BOC chair at the close of the AAOS 2025 annual meeting in San Diego.
“Dr. Leddy has served as member of the Louisiana Orthopaedic Association Board of Directors for the past 12 years, serving as president in 2020–2021. He has also been an active volunteer for the AAOS, as well as

the American Orthopaedic Society of Sports Medicine, Arthroscopy Association of North America, and National Athletic Trainers’ Association.
“Dr. Leddy is a senior partner of the Midstate Orthopaedic and Sports Medicine Center of Alexandria, Louisiana, serving as president and managing partner. He is also a team physician for numerous high schools and collegiate teams. Dr. Leddy resides in Alexandria with his wife Andree and daughters Anna Clare and Mary Caitlin.”
Joshua Levine of Charlotte, North Carolina, writes, “Elissa (‘98) and I are well in Charlotte, North Carolina. Both still in private practice, Elissa pediatrics and myself ENT and sleep medicine. We have two daughters, 17 and 19, busy in high school and college, so we are soon to be empty-nesters. We enjoy hiking, adventure travel, gardening, and backyard chickens.”
Albert Chang of Seal Beach, California, writes, “When I started my path to med school so many years ago, NEVER would I have imag-

ined that I would end up on the side of a BUS! My life is now complete!”
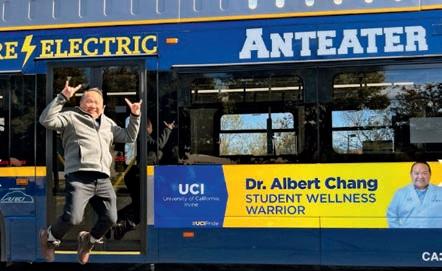
Demetrios Vavvas of Roslindale, Massachusetts, writes, “BU was the reason I came to Boston, and I have been here now for over 30 years! I love the city, the people, and the education I got. I still work at Mass Eye and Ear; I love its people and culture and what it does for the patients! I miss my classmates, and I hope I find more time to reconnect!”
Robert Kiley of Colorado Springs, Colorado, writes, “Got married last September and loving Colorado!”

Bernadatte Gilbert of Harrisburg, Pennsylvania, writes, “Hello! In September 2022 I was

Nikki Appel of Glen Head, New York, writes, “This past September, a love story that began at the medical school in the graduate medical sciences programs reached the milestone of marriage. Nikki Appel was in the forensic anthropology master’s program while George Farah was in the anatomy & neurobiology master’s program. They met in the fall of their first year and as fate would have it, ended up working on their theses in the same histology lab. The trials and tribulations of graduate school never got the best of them, and they supported each other through it all. They got married on September 17, 2022, on Cape Cod, Massachusetts, with friends and family by their side. Currently, Nikki is a PhD student at the University of New Mexico focusing on her degree in evolutionary anthropology while also working on NIJ-funded research and as a forensic anthropologist for the state of New Mexico. George is working as the director of business operations for a start-up artificial

intelligence company in New York City. He transitioned from science to business after graduation but continues to use his science knowledge in the world of AI.” ●

Alvin Eden of New York, New York, on December 9, 2022, passed away peacefully at home at the age of 96. Born in 1926, Dr. Eden lived in Brooklyn throughout his childhood and adolescent years. He obtained his bachelor’s degree from Columbia College in 1948, following two years of service in the US Navy during World War II. He was a lefty pitcher for Columbia College, hoping to become a professional baseball player until a scout for the New York Yankees watched him play and advised him to “gain 30 pounds and grow six inches,” cementing his decision to become a doctor
After receiving a medical degree from Boston University in 1952, he completed his internship at Bellevue Hospital in New York City and pediatric residency at University Hospital (now Tisch Hospital and part of NYU). Since 1955 and until last year, Dr. Eden had been a private pediatric practitioner in Forest Hills, New York. During the seven decades of his professional experience, he was associate clinical professor at NYU Medical School, clinical professor at Weill Cornell Medical School, lecturer at SUNY-Downstate, and former president of both the New York and Queens County Pediatric societies. He was chair of pediatrics at Wyckoff Heights Medical Center in Brooklyn for nearly 50 years and clinical chair of pediatrics at the American University of Antigua Medical School since 2008, in which capacities he taught, supervised, and mentored hundreds of students on clinical rotations as well as residents in training. He also received the Marquis Who’s Who Lifetime Achievement Award.
Dr. Eden will be remembered as a doctor’s doctor par excellence. He was so popular with patients that a friend joked at his last birthday party that he was the only pediatrician in New York who took Medicare. Dr. Eden published eight books, mainly related to childhood obesity, nutrition, exercise, and iron deficiency anemia. He also published nearly 35 scholarly articles on obesity prevention, positive parenting, and raising healthy children for new parents. At 95, he wrote his memoirs, A Look Back.
Dr. Eden was a devoted husband to his wife Elaine for 70 years, a loving father to his two children, Robert and Elizabeth, and a proud grandfather to six.
James F. Tierney Jr., of Mattapoisett, Massachusetts, on June 11, 2023, passed away peacefully at home, surrounded by his loving family. He was born and raised in Boston, the son of Dr. James F. Tierney, Sr., and Margaret (Crowley) Tierney.
After graduating from Boston College, he attended medical
school at Boston University, completing a residency at what is now Boston Medical Center, temporarily interrupted when he left to serve as a lieutenant in the Navy Medical Corps on the aircraft carrier USS Kearsage. After completing his residency, he relocated to New Bedford, Massachusetts, to be closer to his sister, Mary. He practiced medicine at St. Luke’s Hospital for more than 50 years until his retirement in 2013. During his career, he also served as Bristol County Medical Examiner and clinical instructor at Tufts Medical Center.
Jim was best known for his bedside manner, sharp wit, dry sense of humor, timeless dance moves, and fashionable sweaters. Aside from his love of medicine, he also loved golf and baseball and followed the Boston Red Sox closely. He was an avid reader, often finishing his children’s required summer reading books in one evening (much to their amazement).
He was married to Jean (Galligan) Tierney for more than 59 years. In addition to his wife, he is survived by three children and six grandchildren. He was predeceased by his son Ian Tierney; sister, Mary Claire Burns, and her husband, William Burns; and his brother, the Honorable John A. Tierney, and his wife, former New Bedford Mayor Rosemary Tierney.
1966
Jens N. F. Touborg of Sherborn, Massachusetts, passed away peacefully on January 10, 2023. Beloved husband, father, grandfather, friend, and physician, Jens was born and raised in Tecumseh, Michigan, and spent his adult life in the Boston suburbs and southern Maine. Valedictorian of Tecumseh High School Class of 1957, Jens maintained lifelong friendships with his classmates, attending reunions and corresponding faithfully. At Amherst College, Jens deepened his love of literature by majoring in English. During his senior year, Jens had what he described as an epiphany, realizing that he wanted to become a doctor.
After graduating from Amherst in 1961, Jens married Margaret “Margo” Bowers and completed premed studies before enrolling in medical school at BU. Upon graduation, he was proud to serve as chief resident at the Deaconess Hospital in Boston and later launched a private practice. As an “old school” primary care physician in Wellesley Hills, “Dr. T” took time with each patient, getting to know their circumstances and stories. He followed up with personalized letters and phone calls, earning trust and improving lives. The Touborgs settled in Lincoln, where they raised their four children and subsequently divorced.
In 1990, Jens married Marilyn “Merry” Duffy after a whirlwind courtship. Together, they built a log cabin on Great East
Lake in Acton, Maine, which quickly became a family base camp. Jens applied his woodworking skills to carve a sign that grew with the family to include the names of spouses and grandchildren. In 2005, Jens and Merry relocated to Sherborn, where they ultimately enjoyed a retirement full of family, friends, and service. Predeceased by Merry in 2022, Jens is survived and lovingly remembered by six children and stepchildren and 12 grandchildren.
Edmund C. Tramont of Rockville, Maryland, on March 5, 2023, died peacefully after a brief illness. He was born August 5, 1939, and raised in Wallingford, Connecticut. He developed a keen interest in microbiology as a student at Rutgers University and received his MD from BU in 1966. Ed entered the Army Medical Corps in 1968 and became the first Army-trained infectious disease specialist.


Emerging as a leader in military infectious diseases, he established research programs at both the Walter Reed Army Medical Center and the Walter Reed Army Institute of Research. Through these organizations, he helped develop vaccines for a myriad of diseases that impact the armed forces and society in general. He also authored the Army’s first policies on managing HIV and AIDS, protecting both patients and force readiness. Concurrently, he treated patients of all ranks, up to President Dwight D. Eisenhower.
After 23 years of service, “Colonel Ed” retired from the Army in 1991 and was awarded the Army Distinguished Service Medal. He joined the University of Maryland Baltimore staff, where he restructured the Medical Biotechnology Center and established the Institute of Human Virology. In 2001 Ed became director of the AIDS Division of the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health, where he helped lay the groundwork for NIH/US Army collaboration in infectious disease prevention and vaccine development. More recently, Ed served as an associate director for special projects in the NIAID’s Clinical Research Division, where he advised researchers throughout the world, focusing on emerging diseases that include SARS and COVID. In 2012 he received the Distinguished Civilian Service Award from the army chief of staff.
Predeceased by his wife of 47 years, Mary, Ed leaves a son, two daughters, seven grandchildren, and three siblings.
David A. Bailen of Newton Center, Massachusetts, passed away peacefully on April 21, 2023. Born in Boston on July 27, 1941, to Marion and Edward Bailen, he was raised in Brookline and Newton,
attending the Driscoll Elementary School in Brookline and Weeks Junior High School in Newton. After graduating from Newton High School in 1959 and Brown University in 1963, he received his MD from Boston University in 1967, where he was an Alpha Omega Alpha Honor Society graduate.
David was chief resident in medicine at University Hospital (Boston Medical Center/ BMC), and subsequently completed a fellowship in rheumatology. He went on to develop a thriving primary care practice at BMC, spending his 40-year career there. He loved internal medicine and the relationships he formed with his patients, and was known as a superior diagnostician and an intelligent, dedicated, and—above all—kind individual and physician.
As an assistant clinical professor of medicine at BU and instructor of medicine at Tufts University School of Medicine, David taught students and medical residents at BMC and Faulkner Hospital for many years. He was president of BMC’s medical/ dental staff and president of the medical staff at the former Jewish Memorial Hospital in Roxbury. He also served as chair of the patient care and other BMC committees, and as president of the school’s alumni association. Devoted to his synagogue, Temple Israel of Boston, he regularly attended weekly Torah study, Shabbat services, and many educational and musical programs, chairing the music committee. He was a voracious reader, constantly curious, loved making connections with everyone he encountered, and enjoyed teaching, especially his children and grandchildren. He was an eternal optimist and loved life.
David was a devoted husband to Helene Bailen for 57 years and a loving father to Laurence Bailen, MD, and his wife, Jennifer Weber, and Mark Bailen and his wife, Jessica Rosenworcel
Steven L. Berk, of Lubbock, Texas, on May 26, 2023, passed away peacefully in his home from presumed heart complications. He was 74 years old and a dedicated physician, esteemed educator, and visionary leader. The loss of this exceptional individual leaves a void in the medical community and in the hearts of all who had the privilege of knowing him.
Born on March 12, 1949, in New York City, NY, Steven was the beloved son of Sidney and Freida “Fritzie” (Blank) Berk. He grew up in a loving home in Bloomfield, New Jersey. On October 10, 1981, he married his life partner and forever-supporter Shirley Anne Holtsclaw.
Steven is survived by his devoted wife Shirley, his sons Jeremy
Boston University Medicine is published by the Chobanian & Avedisian School of Medicine Communications Office.
Maria Ober
Associate Dean, Communications
design & production
Boston University Creative Services
contributing writers
Lisa Brown, Gina DiGravio, Doug Fraser, Sarah Rowan
photography
Paula C. Augustin, Zoë Farr, David Keough, Sarah Rowan, School of Medicine Archival Photos
Please direct any questions or comments to:
Maria Ober
Communications Office
Boston University Medical Campus
85 East Newton Street, M810H Boston, MA 02118
P 617-358-7869 | E mpober@bu.edu
0923
Another academic year has begun! Our third- and fourth-year medical students are on their clinical rotations. The second years arrived back after taking Step 1 of their boards just after July 4. We welcomed our new MD and PA classes on August 1, and our graduate students resumed classes on September 5. The faculty enjoy watching the campus progressively come alive after the short July pause.
Our cover story focuses on the school’s 175-year history on the front lines of medicine and science and how the school has continuously evolved to address important research questions and educate the next generation of physicians and scientists.
We celebrate the 75th anniversary of the historic Framingham Heart Study (FHS) and its significant contributions to science and medicine, only one example of the right research at the right time. FHS participants continue to come from all over the world to remain part of the study that defined the risk factors for cardiovascular diseases and now also studies Alzheimer’s, osteoporosis, and many other diseases. We are pleased to be the home of this iconic study.
In Campus News, commencement stories celebrate the accomplishments of the Class of 2023. Rochelle Walensky, MD, former director of the CDC, addressed the graduates and their guests at the MD and PhD convocation ceremony, and we share a student conversation with her (see story, page 7).
We also mark the 40th anniversaries of two landmark admission programs, the Modular Medical Integrated Curriculum (MMEDIC) and the Early Medical School Selection Program (EMSSP), that have created unique pathways to the medical school.
We celebrate the 28th annual Henry I. Russek Student Achievement Day (see story, page 20) highlighting master’s and PhD student research, and the 2023 Graduate Medical Sciences Outstanding Student Achievement awardees (see story, page 18).
Other items of interest include profiles of our long-standing Assistant Dean and Registrar Ellen DiFiore, who retired at the end of the academic year, and the annual faculty award winners.
Our Giving section features articles on research support from the Vertex Foundation, Bill & Melinda Gates Foundation, and the American Cancer Society.
Finally, our Alumni Stories series continues with profiles on EMSSP graduates Chantale Branson (’12), Ebonee Carter (’12), Joshua Joseph (’09), Frederick Powell (’11), Shawn Smith (’03), and Toya Kelley (’07).
I hope you enjoy this content-rich issue of BU Medicine
Best Regards,
Karen Antman, MD Provost, Medical Campus Dean, Chobanian & Avedisian School of Medicine
Berk (Jen) and Dr. Justin Berk (Natalie) and his cherished granddaughters Maya and Maggie. He is also survived by his brother Dr. Marc Berk (Helene). Steven was preceded in death by his parents.
Steven graduated from Brandeis University in 1971, BU’s medical school in 1975, and completed his medical and infectious disease training at Boston City Hospital.
In 1979, Steven joined East Tennessee State University in Johnson City to help establish the Quillen College of Medicine, dedicating himself to working with students, residents, and fellows. Steven earned a respected reputation as a skilled clinician and educator, became a prominent authority in HIV/AIDS care, and was appointed chair of the Department of Internal Medicine in 1988.
In 1999, he left the Tennessee mountains to join the faculty of Texas Tech University Health Sciences Center and immediately started wearing cowboy boots. He served as the regional dean for the Amarillo campus, became dean of the School of Medicine in 2006 in Lubbock, and executive vice president and provost in 2010. He “died with his boots on,” giving his final graduation speech as dean one week before his death.
Throughout his career, Steven made valuable contributions to the medical community including more than 150 publications, four textbooks, three board certifications, and several active society memberships (including Phi Beta Kappa, Gold Humanism, and Alpha Omega Alpha). His numerous accolades and teaching awards were a testament to his unwavering dedication to educating future generations of physicians, a role that brought him immense pride and satisfaction.
Dr. Berk’s literary endeavors were equally noteworthy. He published his memoir, Anatomy of a Kidnapping, recounting his 2012 abduction. Recently, he authored a historical fiction novel, In Search of the Animalcule, exploring the story of the discovery of bacteria.
Dr. Berk was a revered figure in the community, known for his visionary leadership and lasting contributions at the medical school. He created the Family Medicine Accelerated Track program to address primary care shortages and proudly supported the Barbershop Hypertension Program, a student-run free clinic, among other organizations. For decades, he served as councilor for the Student National Medical Association.
His legacy extends far beyond his professional achievements as a compassionate and caring mentor. Dr. Berk’s unwavering support and guidance inspired the lives of countless aspiring physicians, leaving an indelible mark on their journeys.
Ralph L. Sacco of Miami Beach, Florida, on January 17, 2023, passed away from a brain tumor at his home on Long Island, New York. He was 65.
Ralph was born and raised in Margate City, New Jersey. He graduated with honors from Holy Spirit High School and Cornell University before earning his MD at BU. He completed his medical training at Columbia Presbyterian Hospital in New York City, where he later founded the Northern Manhattan Stroke Study, becoming a pioneering expert in stroke research.
In 2007 he was appointed Olemberg Family Chair in Neurological Disorders and professor of neurology, public health sciences, human genetics and neurosurgery at the University of Miami Miller School of Medicine.
Ralph’s accomplishments included his selection as the first neurologist to serve as president of the American Heart Association and the only neurologist to also serve as the president of the American Academy of Neurology. He also assumed myriad leadership roles, including executive director of the Evelyn McKnight Brain Institute, chief of neurology service at Jackson Memorial Hospital, worldwide stroke lecturer, and editor in chief of the journal Stroke. Over the course of his extraordinary career, Ralph published more than 1,000 articles on stroke research. In 2019 he was honored with the school’s Distinguished Alumni Award.
Ralph leaves his husband of 22 years, Scott Dutcher; his father, and four siblings. His genuine, unassuming nature touched the lives of everyone he met. His legacy will live on in the medical field and in the hearts of his loved ones, who were blessed to share so many beautiful memories with him, even throughout the past difficult year ●

