Rebecca
Berberi
Senior Thesis | 2025

Investigating the Impact of Various Opioid Use Disorder Rehabilitation Services on Treatment Completion for Individuals with Mental and Substance Use Disorders
Rebecca Berberi
Introduction:
Opioid Use Disorder (OUD) remains a widespread public health crisis in the United States, affecting millions of individuals across diverse demographic groups. Among those seeking treatment for OUD, a significant proportion also experience co-occurring mental and substance use disorders, complicating the recovery process and influencing treatment outcomes. In 2019, 1.6 million people in the U.S. were diagnosed with Opioid Use Disorder. Of these people diagnosed with Opioid Use Disorder, 39.0% were also reported to suffer from a mental illness.1 This issue makes improvement in intervention and policies crucial. Thus, it is necessary to explore the effectiveness of various rehabilitation services to better cater to these marginalized individuals.
This study aims to evaluate the relative effectiveness of different rehabilitation services in facilitating treatment completion for individuals with OUD and co-occurring mental and substance use disorders. Using data from the Substance Abuse and Mental Health Services Administration’s Treatment Episode Data Set: Discharges (TEDS-D), this research applies statistical matching techniques and machine learning methods to compare treatment completion rates across eight distinct rehabilitation services. Through the use of logistic regression, feature selection techniques, and the calculation of the Average Treatment Effect (ATE), this study seeks to identify which rehabilitation service provides the most beneficial impact on an individual's ability to complete all components of rehabilitation treatment.
Through a data-driven approach, this research contributes to the literature on evidence-based addiction treatment strategies. By isolating the effects of specific rehabilitation services, this study provides valuable insights into which treatment modalities offer the highest likelihood of success for individuals facing the dual challenges of OUD and co-occurring disorders. The findings of this study have the potential to aid treatment providers, policymakers,
and healthcare professionals in optimizing rehabilitation programs to enhance patient outcomes.
Background
Individuals suffering from OUD face heightened risks of overdose-related mortality and other adverse health outcomes. Efforts to combat this epidemic have focused on medication for opioid use disorder (MOUD) a treatment strategy that utilizes buprenorphine, methadone, and naltrexone. MOUD is widely regarded as the standard in OUD treatment due to its effectiveness in reducing opioid use and associated mortality. However, adherence and retention rates remain suboptimal, with only 30-50% of patients completing treatment. In recent years, there has been an increasing development in research exploring factors influencing treatment adherence and completion, highlighting the critical role of psychosocial interventions.
A 2024 study by Sahil Shikalgar, et al., studies one of these factors by focusing on the use of self-help groups in the rehabilitation process and its effects on treatment retention.2 Selfhelp groups, such as Narcotics Anonymous (NA) and Alcoholics Anonymous (AA), have demonstrated potential in improving treatment outcomes for substance use disorders. Combining MOUD with participation in a self-help group has proven to have benefits, including reduced opioid use and enhanced quality of life. Nonetheless, limited empirical evidence exists to establish a causal relationship between self-help group participation and MOUD treatment completion rates. Existing studies often focus on specific subpopulations, such as residential or outpatient specialty care patients, leading to findings that may not accurately reflect the general population with Opioid Use Disorder. Furthermore, while research has acknowledged the presence of a correlation between self-help groups and treatment use, the impact on treatment completion a critical metric for evaluating MOUD success remains underexplored. This gap in information highlights the need
to investigate the potential effects of MOUD and self-help groups on treatment adherence and completion. In response to this gap, the Shikalgar study aims to assess the impact of self-help group participation on MOUD treatment completion using data from the Substance Abuse and Mental Health Services Administration’s (SAMHSA) Treatment Episode Data Set: Discharges (TEDS-D) for 2015–2019. The Shikalgar study uses a similar method demonstrated in this work by leveraging advanced machine learning (ML) methods and causal inference techniques.3 By doing so, the study sought to provide robust evidence for the role of self-help groups in improving treatment outcomes.
The Shikalgar study used a nationally representative dataset encompassing 157,885 treatment episodes for individuals receiving MOUD for OUD. The key variables of this dataset included demographic information, substance use history, treatment modality, and discharge status. MOUD was defined as the use of methadone, buprenorphine, or naltrexone as part of the patient’s treatment plan, self-help group participation referred to attendance at programs such as Narcotics Anonymous or Alcoholics Anonymous within 30 days prior to discharge. Treatment completion was defined as fulfilling all the components of the prescribed treatment plan, while excluding cases of dropout or termination. Patients receiving MOUD were categorized into two groups: those who participated in self-help groups as well as completed treatments, and those who did not participate in self-help groups or did not complete treatment. This participation proved to causally influence MOUD treatment completion rates.
The study used a two-step Machine Learning-assisted causal inference framework to address challenges inherent in observational data. First, machine learning models, including Lasso Regression, Decision Trees, Random Forest, and XGBoost, were employed to identify variables significantly associated with treatment completion and self-help group participation. These models demonstrated high specificity, with Random Forest emerging as the
best-performing model for predicting treatment completion. To estimate causal effects, the study utilized Outcome Adaptive Elastic Net (OAENet) to select confounders and outcome predictors, ensuring minimal bias and variance in treatment effect estimates. Propensity score matching with the nearest neighbor method was employed to balance covariates between treated (self-help group participants) and control (non-participants) groups. The Average Treatment Effect on Treated (ATT) was calculated, revealing a 26.0% improvement in treatment completion rates for self-help group participants. Robust McNemar’s test further confirmed the statistical significance of this causal relationship (p < 0.0001).
The study’s findings emphasize the significant positive impact of self-help group participation on MOUD treatment completion. Among the 157,885 treatment episodes analyzed, 29% of patients completed treatment. However, the completion rate was markedly higher (51%) for those participating in self-help groups compared to non-participants (19%). This effect was consistent across various demographics and treatment-related factors. One determinant that proved to be especially critical was education level. It was found that individuals with 16 or more years of education demonstrated the highest rate of treatment completion. Also, the mode by which the patients were referred to the rehabilitation service also proved to play a significant role. Patients referred through the court/criminal justice system had a significantly higher completion rate (48%) than those who were self-referred (23%). Additionally, demographics also produced a disparity in treatment completion rates, with non-Hispanic White patients achieving higher completion rates than Hispanic/Latino and Black patients. The results highlight the potential for self-help groups to complement MOUD by addressing psychosocial and behavioral dimensions of recovery. These groups provide social support, foster accountability, and promote shifts in beliefs and behaviors that facilitate sustained recovery. Despite their demonstrated benefits, self-help group participation remains underutilized, with various
regions favoring the use of self-help groups more than others. For instance, New England reported the highest participation rate (40%), while Puerto Rico reported the lowest (4%). Barriers to participation may come from stigmatization of MOUD within certain self-help group communities, where medications like methadone or buprenorphine are not universally accepted as part of sobriety.
The findings highlight the need for policy interventions to integrate self-help groups more effectively into MOUD treatment programs. National fellowships such as NA and AA should adopt inclusive policies that recognize MOUD as a valid pathway to recovery. It is also important to prioritize the destigmatization of the use of MOUD within these communities, as it can enhance participation and improve treatment outcomes. Local treatment centers should also emphasize the role of self-help groups in treatment plans, providing patients with information and resources to access these programs. Policymakers should prioritize funding and initiatives that facilitate collaboration between MOUD providers and self-help groups, ensuring these complementary modalities are accessible to all patients.
This study provides evidence of the beneficial role of selfhelp groups in improving MOUD treatment completion rates. By using rigorous ML-assisted causal inference methods, the research addresses significant gaps in understanding the relationship between psychosocial support and MOUD outcomes. The findings advocate for a holistic approach to OUD treatment that combines pharmacological and psychosocial interventions, ultimately enhancing the likelihood of successful recovery. By integrating these insights into policy and practice, the effectiveness of OUD treatment can be improved, contributing to the mitigation of the ongoing opioid crisis.
Methods:
The data for this research was taken from the Substance Abuse and Mental Health Services Administration’s Treatment Episode Data Set: Discharges, or TEDS-D.4 This data includes the records of individuals admitted for Opioid Use Disorder treatment, aged 12 and older, who have been discharged. Each data point is separated by demographics and features of these individuals. However, this study specifically focused on the individuals with a co-occurring mental and substance use disorder, the type of treatment upon admission, and whether all parts of the treatment were completed upon their discharge.
Once the different categories in the TEDS-D were determined, matching techniques were applied.5 The process of matching made the appearance of pairs within the data visible. These pairs were determined by their similarity to one another based on certain characteristics, in order to make them comparable. In this case, the specific characteristic that was targeted was the various treatment services.6 This process required the separation of individuals into two groups: the treatment group and the control group. The treatment groups contained the individuals who participated in the service that were specifically being chosen to be focused on. Whereas, the control group contained the remaining individuals that were not placed into the specific selected service. Comparing the treatment and control groups allows for an estimation of what degree of the outcome is due to the treatment service rather than other factors.7 In this case, the outcome that was investigated is whether the individual has completed the treatment program.
Eight treatment services were targeted in this study.
These services include:
● Service 1: Detox, 24-hour, hospital inpatient
● Service 2: Detox, 24-hour, free-standing residential
● Service 3: Rehab/residential, hospital (non-detox)
● Service 4: Rehab/residential, short term (30 days or fewer)
● Service 5: Rehab/residential, long term (more than 30 days)
● Service 6: Ambulatory, intensive outpatient
● Service 7: Ambulatory, non-intensive outpatient
● Service 8: Ambulatory, detoxification.
Each time this process was attempted, it focused on one specific service. For example, if “Service 1: Detox, 24-hour, hospital inpatient” was chosen for one of the trials, all the individuals who completed Service 1 would be a part of the treatment group and the individuals who participated in one of the other seven services or participated in but did not complete Service 1, would be part of the control group. Thus, this experiment required the process to be applied eight separate times. Through each of these processes, the goal was to find which rehabilitation service was the most effective upon completion, specifically for individuals with cooccurring mental and substance use disorders.
Once our data was obtained from the Treatment Episode Data Set, it was then imported into Python. Once imported, the data was cleaned to remove unnecessary information and allow for more efficient processing. This was done by removing any missing or unknown data that was not specified in the data set. Specifically, categories that focused on age, demographic, gender, etc., that were missing a sum of information that would have skewed this study's analysis was removed. If a category was missing less than 20% of data then those individuals from that feature were removed, rather than removing that category altogether. But, if the category was
missing more than 20%, then it became completely invalid and removed entirely. Then, once a more refined data set was obtained, it was dummied. Dummying allows for the data to be converted from categorical data into data that the machine learning model can understand. Specifically, new variables were created for variables that had between 3 and 5 values. This process allowed for the categorical data to be converted into binary, creating a more accurate comparison between each category to our reference category.
Once the data set was cleaned, it was selected for specific features to further refine and target specific variables. Feature selection is the process of choosing the most relevant features from the dataset to improve the model's performance and efficiency. It involves analyzing the importance of each feature and removing those that are irrelevant, redundant, or add noise. This is similar to what was done when originally cleaning the data. Feature selection is initiated through logistic regression, which is a machine learning algorithm used in binary classification. Because of the data cleaning and matching that was previously performed, logistic regression was employed to compare the control and the treatment groups.9 Using logistic regression, feature selection determines which features most influence the treatment outcome. Features with a larger weight played a more significant role. This process required splitting the data into training and testing sets. 70% of the data was used for training and the remaining 30% was used for testing. The model was then fitted to the training data, to analyze the relationships between variables. This analysis then informed accurate predictions of the test data. After evaluating the model, it was found that all models had an accuracy of over 99.7%.
Besides logistic regression, two other methods for feature selection were performed: Least Absolute Shrinkage and Selection Operator (LASSO) and Adaptive Elastic Net. LASSO uses an L1 penalty to shrink the coefficients of less important features to zero, effectively removing them from the model. By further refining the data set, it aided in simplifying the model and prevented overfitting.
Adaptive Elastic Net, on the other hand, combines L1 and L2 penalties. Both of these penalties are regularization techniques that assisted in minimizing the effect that the not-targeted features have on the learning model. These penalties assisted in preventing overfitting by simplifying the model. This study more heavily utilized the Adaptive Elastic Net method because it offered greater flexibility by adapting to highly correlated features, and allowed a better selection process by which to target the most relevant features.
After refining the data set, a Chi-Squared Test was used to process the features that remained after using logistic regression and AdaptiveElasticNet. To run the Chi-Squared Test, a null and alternative hypotheses were first determined. The null hypothesis, H0, stated that the type of rehabilitation service is independent of treatment completion. The alternative hypothesis, H1, stated that the type of rehabilitation service is not independent of treatment completion. Once the two hypotheses were determined, a contingency table was created to observe the frequencies of the outcomes across different services. These values were then processed through the Chi-Squared Distribution. After inputting these frequencies into the Chi-Squared Test, Chi-Squared statistic was produced and employed to determine whether there was a significant association between those features and treatment completion status. With this test, this study, specifically, necessitated an association between the features and the outcome, and if there was not a strong association, then that feature would be removed from the dataset, further refining the dataset. Then, using that chi-squared statistic, again, the chi-squared distribution was compared to find the likelihood of the null hypothesis occurring. This observation was determined by the P-value, or the probability.
The degree of the P-value determined whether the probability was statistically significant. A significance in the values infers a relationship between the two variables being tested, other than chance. In the case of this study, the variables that were being
compared were the probability of treatment completion per each remaining feature of each service from the data. Thus, the P-value determined the likelihood of completing treatment for each feature of the service. To determine the significance of the P-value, the ChiSquared Test produced a statistic. If this statistic was greater than or equal to 0.05, then the relationship between the features and treatment completion was insignificant, implying weak evidence against the null hypothesis and supporting the null hypothesis. If the produced statistic was less than 0.05, then the correlation between treatment completion and each feature would be significant, thus the null hypothesis would be rejected, implying evidence in favor of the alternative hypothesis. Since there are multiple features for each service with the ability to complete a treatment and each having a different association, the overall association for each service was generalized.
Once the association and use of null hypothesis was determined, the Average Treatment Effect (ATE) is then calculated. The Average Treatment Effect quantifies and compares the outcomes of the treated and untreated groups or the treatment and control groups. In the case of this study, the two variables being compared are individuals who participated and completed one particular rehabilitation service, and individuals who participated and completed one of the other seven. The ATE was calculated using a propensity score that was run through the logistic regression. The propensity score is a statistical measure that quantifies the probability that an individual is assigned to the targeted treatment group, based on their observed characteristics. This propensity is also used in the aforementioned matching process to determine whether individuals should be placed in the treatment or control group based on their score.5 This process ensures that the groups are not randomly assigned, and are instead grouped by similarity to create a balanced comparison group. With the production of the propensity score, the ATE was determined to quantify the difference in the outcome of the two matched groups. This was done by
subtracting the average outcome of the control group from the average outcome of the treatment group.
In the case of this study, the ATE was utilized to quantify the effect of the rehabilitation services on treatment completion. By quantifying the effect, the ATE was then used to determine whether the effect was positive, negative, or close to zero. A positive ATE means that the treatment was beneficial and improved the outcome on average. A negative ATE means that the treatment has a harmful effect and worsens the outcome on average. An ATE that is close to zero means that the treatment has zero to no effect and that there was no advantage or disadvantage on completion from participating in the treatment. With the calculation of the ATE, it is important to note that even with a positive ATE, for example, the overall experience of the group can still be negative. This is because the ATE is a generalization of the effect across the entire population. The same can be said for when the Average Treatment Effect is negative or close to zero.
Once the Average Treatment Effect is determined to be positive, negative, or close to zero, the data is converted into a bar graph (see Figure 2) to visualize the differences in the effects of the eight different services. From this, it is made visible which treatment services provide the greatest beneficial effect, which treatments provide the most harmful effects, and which treatments provide no difference in outcome.
Results:
This study aims to determine the most effective rehabilitation services for individuals with co-occurring mental and substance use disorders in completing treatment for Opioid Use Disorder. Using data from the Treatment Episode Data Set: Discharges (TEDS-D), matching techniques and statistical analyses were applied to compare treatment completion rates across eight distinct rehabilitation services. The results provide insight into the relative effectiveness of each service by assessing treatment completion as the primary outcome.
Through the processes described in the Methods section, the most effective service treatment was determined through the Average Treatment Effect. However, prior to the production of the Average Treatment Effect results, it is necessary to determine the association between each service and whether the null hypothesis will be rejected. For Service 1: Detox, 24-hour, hospital inpatient; Service 2: Detox, 24-hour, free-standing residential; Service 3: Rehab/residential, hospital (non-detox); and Service 8: Ambulatory, detoxification all of the selected features for each service had a Pvalue of less than 0.05 (see Figure 1). This P-value infers that there is a strong association between the features and the treatment service and that the null hypothesis should be rejected, implying evidence in favor of the alternative hypothesis. This conclusion asserts that treatment completion rates are dependent on Services 1, 2, 3, and 8. Therefore, Services 1, 2, 3, and 8 will see the greatest difference in treatment completion rates across the Services.
For Service 4: Rehab/residential, short term (30 days or fewer); Service 5: Rehab/residential, short term (30 days or fewer); Service 6: Ambulatory, intensive outpatient; and Service 7: Ambulatory, non-intensive outpatient most of the selected features had a strong association. It is important to note that not all of the selected features had a strong association; this implies that there are feature characteristics of individuals of the service that are independent of treatment completion rates and will not affect the
individual's ability to complete the specific service treatment (See Figure 1). However, as most of the features have a p-value that is less than 0.05, those features are strongly associated, which implies that rehabilitation service is not independent of treatment completion rates.
After determining the general association of each service and the individual's ability to complete the treatment, the association is then used to establish the degree in which they are associated, which allows for a conclusion of which service is most effective, or the Average Treatment Effect (see Figure 2).
It is discovered that:
● Service 1: Detoxification, 24-hour service, hospital inpatient has an ATE value of 7.126
● Service 2: Detoxification, 24-hour service, free-standing residential has an ATE value -0.750
● Service 3: Rehabilitation/Residential – hospital (other than detoxification) has an ATE value of 0.248
● Service 4: Rehabilitation/Residential – short term (30 days or fewer) has an ATE value of -0.135
● Service 5: Rehabilitation/Residential – long term (more than 30 days) has an ATE value of -0.164
● Service 6: Ambulatory - intensive outpatient has an ATE value of -0.164
● Service 7: Ambulatory - non-intensive outpatient has an ATE value of -7.529
● Service 8: Ambulatory - detoxification has ATE value of 0.118
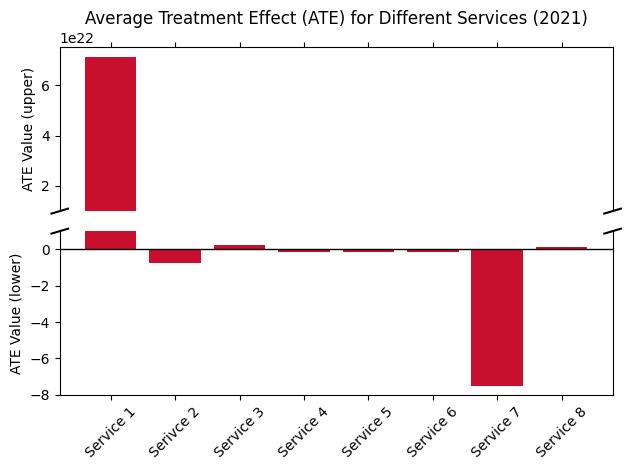
Figure 2. The Average Treatment Effect for each of the eight rehabilitation services.
The ATE scores demonstrate that Service 2, 3, 4, 5, 6, and 8 had an Average Treatment Effect that was close to zero, and therefore it is not possible to infer a causal relationship between these services and treatment completion. Thus, Services 2, 3, 4, 5, 6, and 8 will have little to no effect on an individual's ability to complete their treatment. Moreover, Service 7 had a significantly negative Average Treatment Effect which allows for an inference of a causal relationship between this service and treatment completion, albeit a negative relationship. Due to the negative ATE score, this treatment will have a harmful effect on the individuals' ability to complete treatment. Finally, Service 1 had the most significantly positive Average Treatment Effect and therefore can be used to imply a causal relationship between this service and treatment completion. Due to Service 1’s extreme positive ATE score, it is
concluded that Service 1 will have the most beneficial effect on an individual's ability to complete treatment.
Discussion:
The findings of this study demonstrate significant variations in the effectiveness of different rehabilitation services for individuals with co-occurring mental and substance use disorders seeking treatment for Opioid Use Disorder (OUD). This study found that Service 1: Detoxification, 24-hour, hospital inpatient was the most effective rehabilitation service. This suggests that individuals who undergo inpatient detoxification in a hospital for 24 hours will have the highest likelihood of completing all parts of their treatment, likely due to this service's specific medical supervision, intensive support, and structure of the hospital setting. This service also minimizes external pressures and triggers, as well as withdrawalrelated complications that could hinder the treatment process leading to an increased likelihood of treatment adherence. Additionally, rehabilitation treatment with inpatient care allows for individuals with severe OUD alongside co-occurring mental and substance use disorders to receive treatment in all areas in which they may require rehabilitation instead of only OUD treatment. Inpatient care is especially helpful in aiding in mental and substance use disorders.
This study found that Service 7: Ambulatory, non-intensive outpatient treatment had the most harmful effect on treatment completion and was the least beneficial rehabilitation service. A possible explanation for this negative outcome is that the ambulatory care does not provide the rigid structure of the inpatient treatment and allows for external triggers to interfere with the treatment process. The outpatient care makes it easier for patients with OUD to discontinue their treatment prematurely.8
Finally, the remaining services had little to no effect on treatment completion, indicating that their impact was neither negative nor positive. This suggests that although some people
might benefit or be harmed by one of these services on the individual level, the services do not have a universal impact on the likelihood of treatment completion.
The findings of this study align with existing research as well as the aforementioned Shikalgar study that focused primarily on treatment through self-help groups.2 It is sustained through this study that structured treatment environments are most beneficial for individuals with severe substance use disorders.9 These results provide an important implication for addiction treatment, in both OUD rehabilitation and other substance abuse disorders. These findings also stand to inform future policy decisions and bring significant impacts to the healthcare community. Given the strong positive impact of 24-hour hospital inpatient detoxification, this finding can lead to resources being directed to increase access to this service on a wider scale in order to improve the overall treatment success rates. Policymakers and healthcare providers should prioritize funding and resources for inpatient detoxification programs, which will directly benefit individuals with severe OUD and co-occurring disorders.
Additionally, the strong negative impact of the ambulatory, non-intensive outpatient treatment emphasizes a need for modifications and changes in how this service is structured and delivered. This service can be enhanced through the advancement of additional support programs, such as peer counseling, medication assisted treatment, and case management, to improve the likelihood of treatment completion and retention.10 Modifications in this service could also take the form of individualized treatment planning that matches patients to the most appropriate level of care based on their needs, which may mean a more intensive approach. Through these approaches and changes in policies, the likelihood of recovery and treatment completion can be significantly improved. While this study provides valuable insights that can impact the way that OUD is treated, there still remain limitations to this study. One of these limitations includes the Treatment Episode Data
Set (TEDS-D), which has the potential to overlook relevant patient characteristics and factors that could influence treatment completion, such as socioeconomic status, social support, or personal motivation. There may have also been some confounders that have gone unmeasured and overlooked when the propensity score was used to balance the treatment and control groups. Additionally, this study does not account for the fact that treatment completion does not necessitate long-term success.
Future research should aim to examine additional factors that contribute to treatment success beyond treatment completion. By conducting studies that track individuals post-treatment completion, healthcare providers can produce valuable data on factors that may trigger relapse or sustain recovery.11 In addition, future studies should investigate the role of personalized treatment approaches, such as integrating mental health services into substance use treatment, to refine rehabilitation strategies. Moreover, studies should also examine the impact of social determinants on accessibility to healthcare that may interfere with the completion of treatment, such as housing stability, employment, and familial support. By developing a wider understanding of each individual's needs, healthcare providers can implement more effective rehabilitation services and increase the rate of recovery for individuals with OUD and co-occurring disorders.
Conclusion:
This work analyzed the efficiency of various rehabilitation services for people with Opioid Use Disorder, alongside cooccurring mental and substance use disorders, through the use of statistical techniques, such as logistic regression, feature selection, and the Average Treatment Effect (ATE). The results demonstrate that 24-hour, inpatient detoxification in hospitals is the most effective service and produces the most significant treatment completion, whereas non-intensive outpatient programs have the lowest success rates. These findings emphasize the importance of intensive medically-supervised and specialized services in aiding individuals during their recovery. In light of the current opioid crisis, it is essential for policymakers and healthcare providers to focus on increasing access to effective services and improving outpatient programs through added support systems. By enhancing rehabilitation methods, the healthcare system can more effectively assist individuals battling OUD alongside a co-occurring mental or substance use disorder and sustain a lasting recovery.
References:
1. Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug and Alcohol Dependence. 2019 Apr;197:7882.
2. Shikalgar, S., Weiner, S. G., Young, G. J., & Noor-EAlam, M. (2024). Self-help groups and opioid use disorder treatment: An investigation using a machine learningassisted robust causal inference framework. Addictive Behaviors, 148, Article 107193.
3. Noor-E-Alam, M. and Rudin, C., "Robust Testing for Causal Inference in Observational Studies", working paper.
4. Substance Abuse and Mental Health Services Administration. (2023). Treatment Episode Data Set Discharges (TEDS-D) 2021: Public Use File (PUF) Codebook. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/.
5. Stuart, E. A. (2010). Matching methods for causal inference: A review and a look forward. Statistical Science, 25(1). https://doi.org/10.1214/09-sts313
6. Islam, M. S., Morshed, M. S., & Noor-E-Alam, M. (2024). A computational framework for solving nonlinear binary optimization problems in robust causal inference. Department of Mechanical and Industrial Engineering, Northeastern University, Boston, MA 02115, USA.
7. Greifer, N., & Stuart, E. A. (2021). Matching methods for confounder adjustment: An addition to the epidemiologist’s Toolbox. Epidemiologic Reviews, 43(1), 118–129. https://doi.org/10.1093/epirev/mxab003
8. Hasan, M. M., Young, G. J., Patel, M. R., Modestino, A. S., Sanchez, L. D., & Noor-E-Alam, Md. (2021). A machine learning framework to predict the risk of opioid use
disorder. Machine Learning with Applications, 6, 100144. https://doi.org/10.1016/j.mlwa.2021.100144
9. Wen H, Druss BG, Saloner B. Self-Help Groups And Medication Use In Opioid Addiction Treatment: A National Analysis. Health Aff (Millwood). 2020 May;39(5):740-746.
10. Hasan, M.M., Young, G.J., Shi, J. et al. A machine learning based two-stage clinical decision support system for predicting patients’ discontinuation from opioid use disorder treatment: retrospective observational study. BMC Med Inform Decis Mak 21, 331 (2021). https://doi.org/10.1186/s12911-021-01692-7
11. Hasan, M. M., Noor-E-Alam, Md., Shi, J., Young, L. D., & Young, G. J. (2022). Long-term patient outcomes following buprenorphine/naloxone treatment for opioid use disorder: a retrospective analysis in a commercially insured population. The American Journal of Drug and Alcohol Abuse, 48(4), 481–491.