23 minute read
Pathological Changes in Soft Tissues Associated with Radiographically Normal Impacted Teeth
Pathological Changes in Soft Tissues Associated with Radiographically Normal Impacted Teeth
A Critical Update and Meta-analysis
Adesh S. Manchanda, M.D.S.; Ramandeep S. Narang, M.D.S.; Komaldeep Kaur Sandhu, B.D.S.
ABSTRACT
Aim. The purpose of the study was to conduct a retrospective analysis of histopathological diagnosis of all pericoronal tissues associated with impacted teeth and to correlate it with a hypothetical classification of pericoronal follicular space to improve our clinical management of treating impacted teeth.
Materials and Method. The study was carried out in the Department of Oral and Maxillofacial Pathology at Sri Guru Ram Das Institute of Dental Sciences, Amritsar. Data revealed that during a 12-year period, 1,268 patients reported with a pericoronal follicular space associated with the crown of an unerupted tooth, which was subsequently submitted for histopathological evaluation. Panoramic and periapical radiographs were available in all cases. The study group comprised 593 subjects having a pericoronal radiolucency < 7 mm associated with at least one impacted tooth. In order to establish comparisons, PFs were arbitrarily divided into three groups according to pericoronal space width: Group A ≤ 1.5mm; Group B> 1.5 mm to 4 mm; and Group C> 4 mm to 7 mm. Patients’ ages ranged from 12 to 63 years. A Pubmed, Medline meta-analysis was also searched for previous such work and was tabulated.
Results. In the present study, 56.49% of the specimens, that is 335 out of 593 follicular samples, with radiolucency <7mm had undergone various pathological changes. Histologic diagnosis of the pathological changes associated with the impacted teeth showed a strong distribution of dentigerous cyst (n=287), followed by odontogenic keratocyst (n=27) and ameloblastoma (n=15), respectively. Lesions such as odontogenic myxoma, odontogenic fibroma and calcifying odontogenic cyst were also sparsely documented. Dentigerous cyst was frequently diagnosed in the 18- 30-year age group, with the mean age of 23.1 years. Other cysts and tumors diagnosed had a mean age of 30.6 years.
Conclusion. Cystic changes may develop in both clinically and radiographically asymptomatic impacted teeth. The data from this study cannot justify the complement removal of all asymptomatic impacted teeth but suggests that there is a risk of pathologic changes, particularly in the second to third decade of life.
The primitive dental sac/dental follicle (DF) and dental papilla derived from neural crest cells are the immature tissues that compose the ectomesenchymal portion of the tooth germ.[1] These develop into periodontal ligament and attachments, and dentin and pulp tissue, respectively.[1-3] Once the tooth has fully developed inside the jaw, the coronal part of the follicle is termed pericoronal sac or follicle (PF) and occasionally persists adjacent to the crown of unerupted or impacted teeth.[1,2] It is composed of fibrous connective tissue with variable amount of lining epithelium, including enamel (columnar), cuboidal, squamous and, rarely, respiratory epithelium, and frequently contains epithelial residues of odontogenesis, which could be the starting point of pathology.[2,4-7]
Radiographically, dental follicles are normal developmental structures that characteristically appear as thin, semicircular radiolucencies around unerupted or impacted teeth.[3] Such pericoronal radiolucencies, which represent a normal or enlarged dental follicle, require no intervention; alternatively, they may represent a pathological entity that requires appropriate management and histopathological interpretation.[8]
These PF, radiographically, appear as a thin pericoronal radiolucency, considered normal by some authors when it is less than 3 mm thick[3,9] and by others when it is no thicker than 2.5 mm.[10] However, scientific evidence supporting this assumption is limited, and there is no internationally accepted consensus on the clinical criteria to differentiate between normal and pathological conditions based on radiographic features.[11] Recent studies have reported pathological changes in PF of up to 2.5 mm,[4,7,12-15] with frequency varying from 23%[13] to 58.5%,[15] particularly associated with the third lower molar.
Many reports in literature have discussed the prevalence of cyst and tumor development associated with impacted teeth, with dentigerous cyst (DC) being the most common one.[16] The overall consensus seems to be that pericoronal cyst and tumor development is rare.[5,17] Some reviews have used this information to support the rationale for no treatment of asymptomatic impacted teeth. The fact that not all pericoronal cysts and tumors are symptomatic or that radiographic evidence of their presence may be subtle or nonexistent masquerades the actual statistical presence of cysts and tumors.
Radiological and histopathological criteria for distinguishing between a normal or slightly enlarged DF and a DC are controversial. Radiographical signs of DC include a pericoronal width of at least 3 mm to 4 mm and an asymmetric appearance of the radiolucency.[3,18] Histopathological diagnosis of DC is mainly based on the presence of a continuous lining of stratified squamous epithelium or cuboidal cells, which may exhibit occasional mucous cells, ciliated cells and, rarely, sebaceous cells.[16]
According to Saravana,[14] the presence of squamous epithelium in the lining of a tissue sac that invests the crown of an unerupted or impacted tooth defines progression from DF to DC. These lesions may enlarge considerably if allowed to develop unchecked and have the potential for pathological transformation into tumors and malignancies. Because surgical therapy for such pathologies is usually more extensive than that required for removal of asymptomatic unerupted teeth and their associated follicles and papillas, their prophylactic removal is debatable but worth considering.[19] The resolution of this perplexity among dental professionals in dealing with asymptomatic and radiographically normal impacted teeth can help formulate evidence-based policies in management of impactions to deliver long-term benefit to the patients and improve our knowledge about the epidemiology of associated diseases.
The purpose of the study presented here was to conduct a retrospective analysis of histopathological diagnosis of all pericoronal tissues associated with impacted teeth and to correlate it with a hypothetical classification of pericoronal follicular space to improve our clinical management of treating impacted teeth.
Materials and Methods
The study was carried out in the Department of Oral and Maxillofacial Pathology at Sri Guru Ram Das Institute of Dental Sciences, Amritsar, Punjab, India, after obtaining institutional ethical clearance. All specimens described by the contributor as being pericoronal tissues associated with the crowns of unerupted tooth were retrieved from the archives. Data revealed that during a 12-year period, 1,268 patients reported with a pericoronal follicular space associated with the crown of an unerupted tooth; these were subsequently submitted for histopathological evaluation. Panoramic and periapical radiographs were available in all cases and were used to measure the width of the pericoronal space, which was determined from half of the mesial, distal and occlusal surfaces; the widest region was selected.[20]
Patients whose history sheet showed a pericoronal radiolucency >7mm were excluded from the current study. Hence, the study group comprised 593 subjects having a pericoronal radiolucency <7 mm associated with at least one impacted tooth, including 471 third molars, 72 canines, 43 premolars and 7 supernumerary teeth.
In order to establish comparisons, PFs were arbitrarily divided into three groups according to pericoronal space width: Group A ≤ 1.5mm; Group B > 1.5 mm to 4 mm; and Group C > 4 mm to 7 mm. The tooth and follicle were removed carefully, and the follicular tissue was submitted for histopathological evaluation. A consensual definition of “dentigerous cyst” has been agreed upon which states that any soft-tissue specimen with squamous or cuboidal epithelium spreading along the surface of the follicle would be deemed cystic. Other pathological findings were reported according to accepted diagnostic criteria.
Dental follicles were diagnosed when pericoronal-reduced enamel epithelium was found on strips of connective tissue removed from the crown of unerupted or impacted teeth. As per institutional protocol, a diagnosis was registered only when the participating pathologists’ results were in concordance with that of the surgeons’ finding during surgical exploration. In cases with inconsistent outcomes, a consensual diagnosis was arrived at after a joint review. Observations were tabulated and percentage was obtained. Associations between the attributes were tested using SPSS version 10 and Epi-Info 6.04 d software.
Results
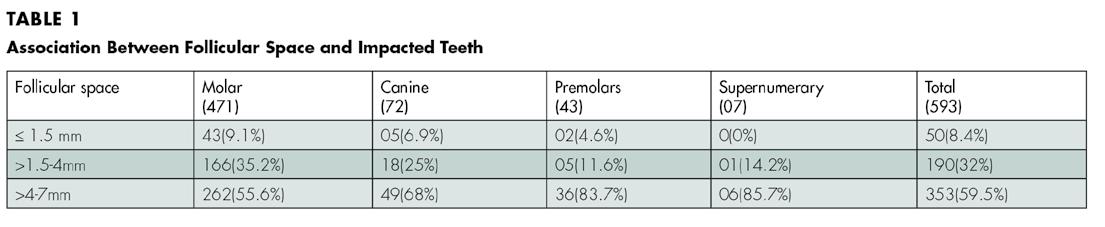
The soft-tissue specimens and radiographs of 335 males and 258 female patients were enrolled in the study. Patient ages ranged from 12 to 63 years (mean=23.6 years). Among the total of 593 patients, 471(79.4%) had an impacted third molar; 72 (12.4%) had an impacted canine; 43 (7.2%) an impacted premolar; and 7 (1%) had an impacted supernumerary tooth. Of the 471 impacted molars, 43 (9.12%) had a follicular space of ≤ 1.5 mm; 166 (35.24%) had a follicular space >1.5-4 mm; and 262(55.62%) had a follicular space of > 4 mm -7 mm.
In the 72 impacted canines, 5 (6.94%) had a follicular space of ≤1.5 mm; 18 (25%) had a follicular space >1.5-4 mm; and 49 (68.05%) had a follicular space of > 4 mm to 7 mm. Of the 43 impacted premolars, 2 (4.65%) had a follicular space of ≤1.5 mm; 5(11.62%) had a follicular space >1.5-4 mm; and 36(83.72%) had a follicular space > 4 mm -7 mm. In the 7 supernumerary teeth, 1 (14.28%) had a follicular space >1.54 mm, and 6(85.71%) had a follicular space > 4 mm -7 mm (Table 1).
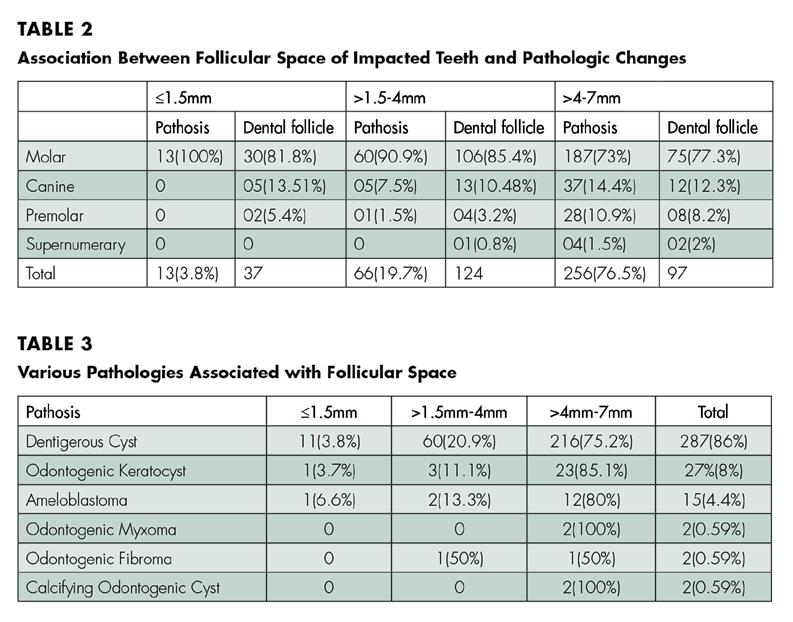
Surprisingly, we found that 56.49% of the specimens, that is 335 out of 593 follicular samples with radiolucency, <7 mm had undergone various pathological changes. In group A(FS≤1.5 mm), 13/50(26%) samples showed pathological changes. In group B (FS >1.5 mm-4 mm); and group C (FS>4 mm-7 mm) 66/190(34.7%) and 256/353(72.5%) samples showed pathological changes, respectively (Table 2). Non- pathologic dental follicles comprised 43.51% (258/593) of the total number of submissions.
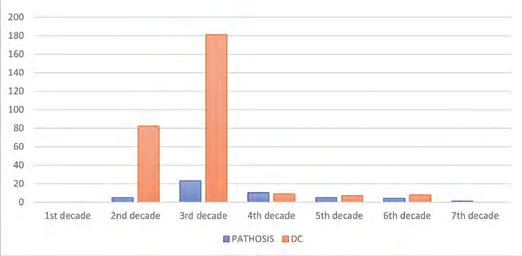
Histologic diagnosis of the pathological changes associated with the impacted teeth showed a strong distribution of dentigerous cyst (n=287), followed by odontogenic keratocyst (n=27) and ameloblastoma (n=15), respectively. Lesions such as odontogenic myxoma, odontogenic fibroma and calcifying odontogenic cyst were also sparsely documented (Table 3). Dentigerous cyst was frequently diagnosed in the 18- to 30-year age group, with the mean age of 23.1 years. Other cyst and tumors diagnosed had a mean age of 30.6 years (Figure 1). Although we found a statistically significant increase in the rate of pathosis with increasing age, the correlation was stronger in the 20- to -30-year age group (p<0.05).
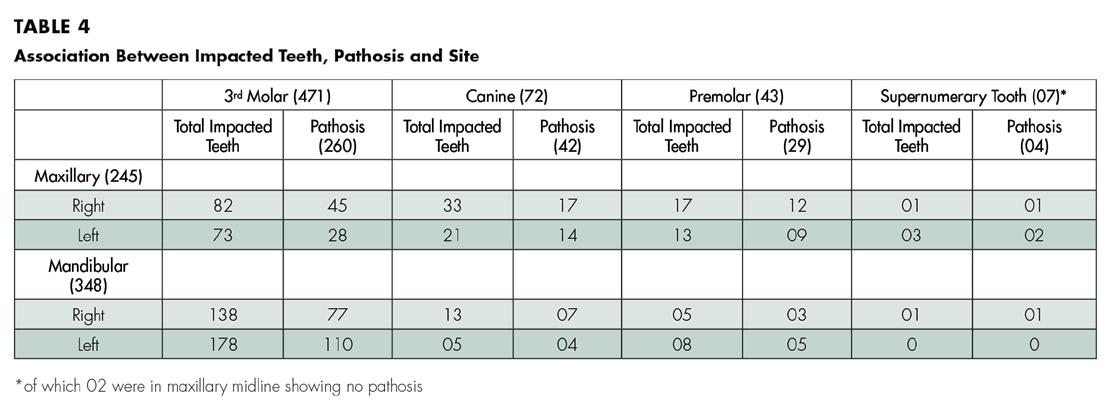
Analysis regarding site revealed a greater incidence of impacted teeth in the mandible (348/593; 58.6%) than the maxilla (245/593; 41.3%). No significant difference was seen in relation to right side vs. left side. In the present study, the mandibular third molar was the most frequently associated impacted tooth, followed by maxillary third molar and maxillary cuspid. Two supernumerary teeth were found to be impacted in the midline. Regarding the frequency of pathosis, the mandibular third molar left side followed by mandibular third molar right side, maxillary third molar right and left side was observed (Table 4).
Discussion
Impacted tooth is among the most common complaints of patients presenting to the dental surgeon for treatment. The decision to remove an impacted tooth is less challenging when signs and symptoms of pathosis are present, but it is made more demanding when the patient is asymptomatic. A National Institutes of Health Consensus Development Conference on Removal of Third Molars in 1979 developed criteria for the treatment of impacted teeth showing evidence of irreversible pathologic change. One conclusion of the conference was that well-designed prospective studies were needed to determine what to do about asymptomatic teeth.[21]
Data on the incidence and progression of pathological conditions in and around impacted teeth are important factors to take into account when decisions are made whether or not to remove the teeth, particularly those that are asymptomatic and that show no signs of pathology. These factors, as well as the prevalence of impacted teeth, should be considered when planning radiographic examinations, primary as well as follow-ups, in cases where impacted teeth are not removed.[22]
Radiographic examination is important in identifying an enlarged pericoronal space that is suggestive of pathologic process. The critical width of the follicle as seen radiographically has been estimated to be between 2 mm and 5 mm.[15,16] It is often assumed, however, that the absence of pericoronal radiolucency reflects absence of pathosis.
Previous medical literature suggests that the pericoronal radiolucency of < 2.5 mm in width is non-pathologic. [10,23] Scientific documentation of the validity of this assumption, however, is limited.[23,24] Shear suggests that some unerupted teeth have a slightly dilated follicle in the pre-eruptive phase. This does not signify a cyst or even necessarily a potential cyst unless the pericoronal width is at least 3 mm to 4 mm.[25] Stanley[17] proposed that a cystlike lesion has a pericoronal space of at least 5 mm and exhibits a well-defined circumscribed border. Glosser and Campbell[4] suggested pericoronal radiolucency of 2.5 mm or more as evidence of radiographic pathology. Radiographic interpretation of a pericoronal space as normal or pathologic is difficult. Thus, several researchers have concluded that radiographs alone are insufficient to diagnose pathological changes, making histological diagnosis necessary.[15,26]

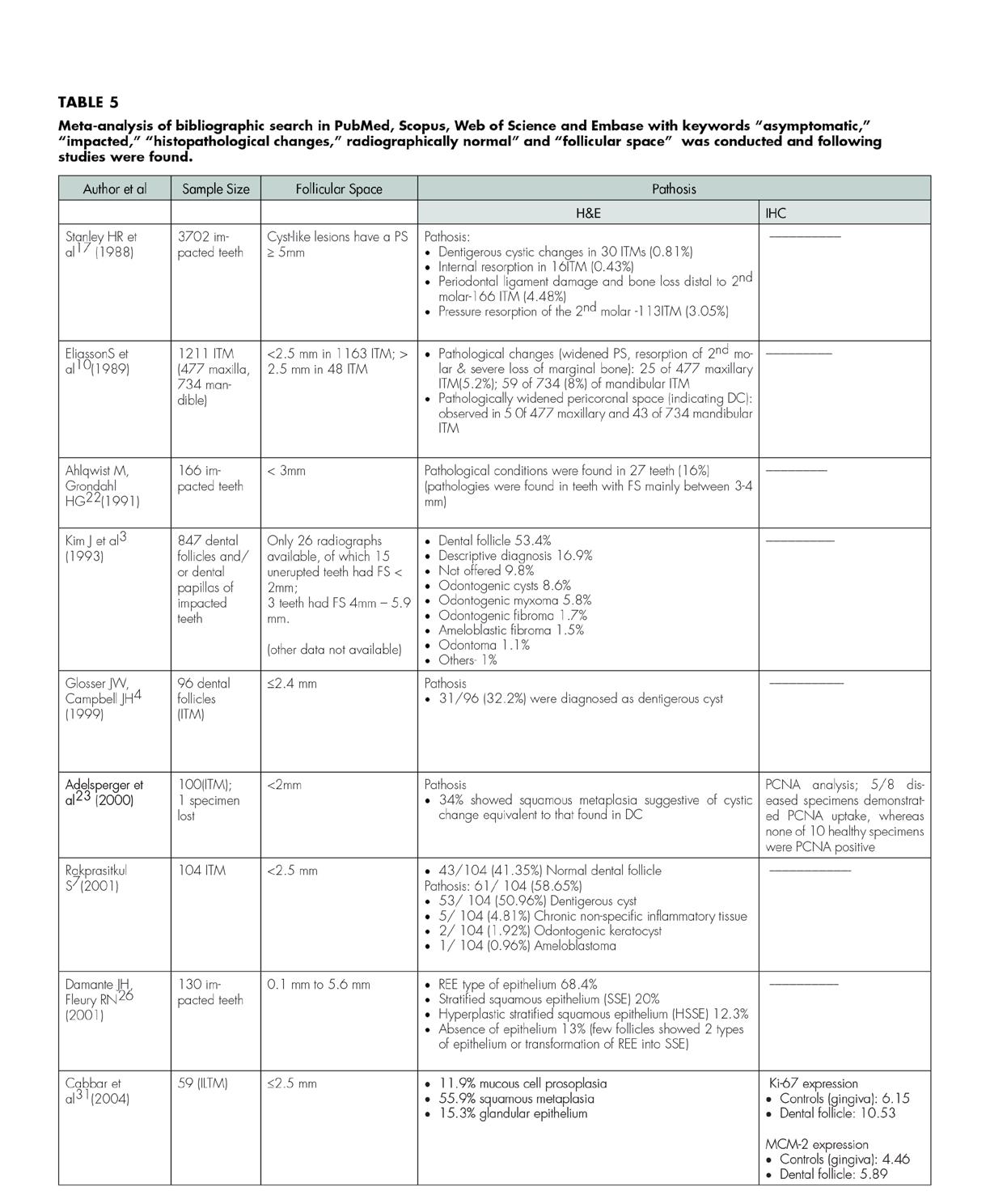
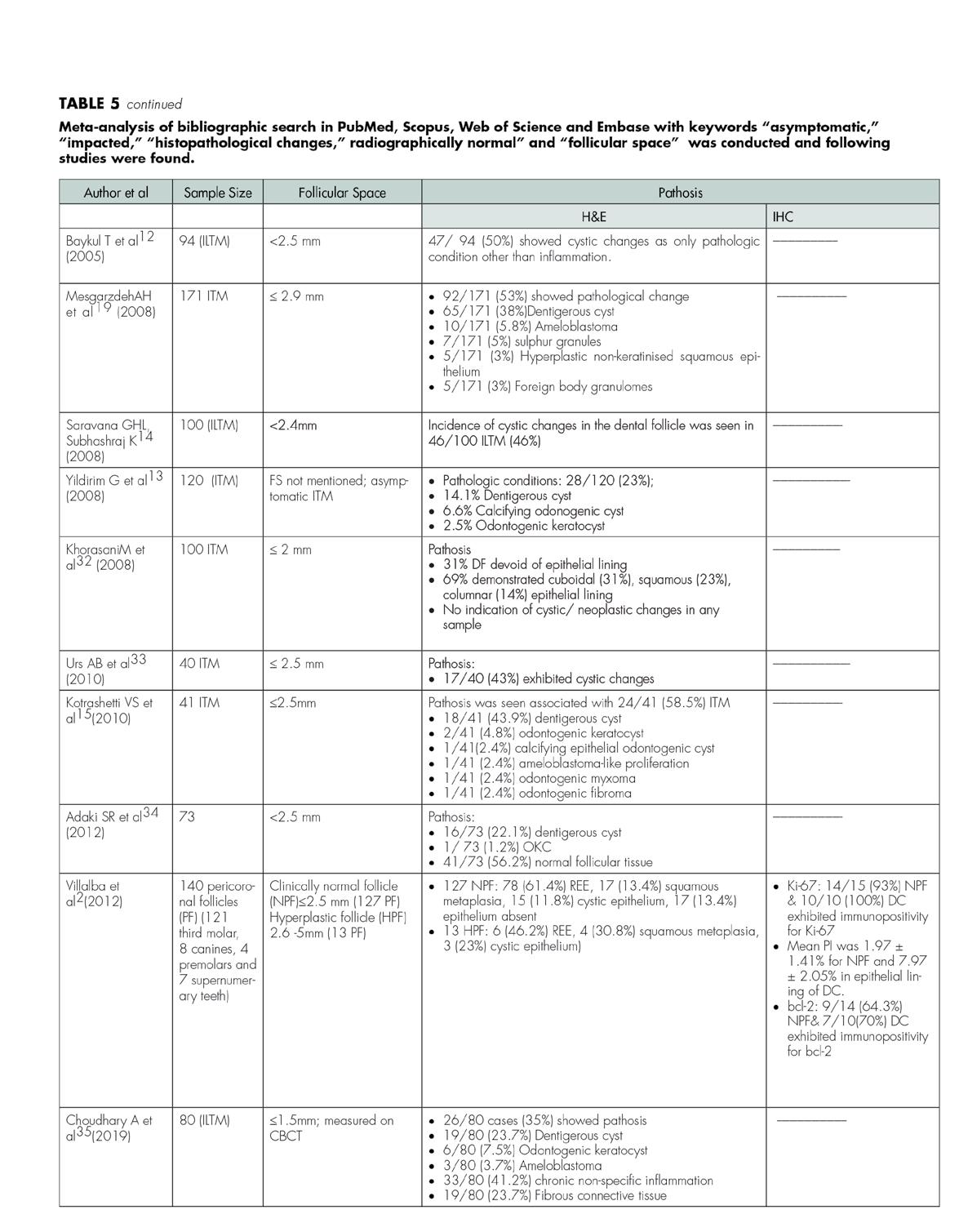
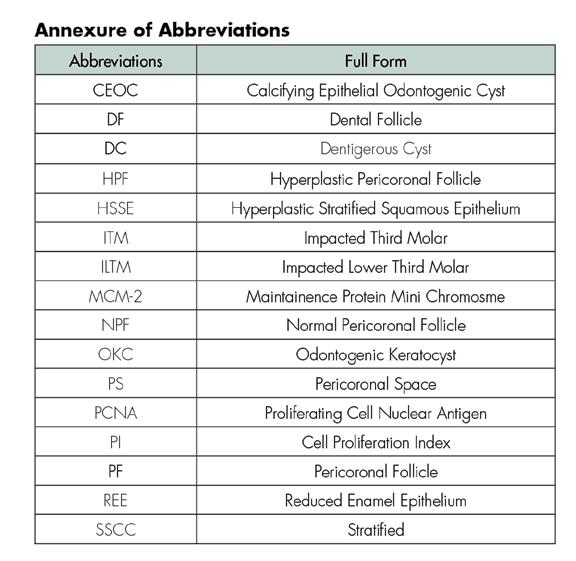
A bibliographic search in PubMed, Scopus, Web of Science and Embase with keywords “asymptomatic,” “impacted,” “histopathological changes,” “radiographically normal” and “follicular space” was done, and a meta-analysis was conducted and tabulated (Table 5). All searches showed a two-grade division of follicular space of impacted teeth with associated pathological changes, while ours is the first study that divided the follicular space in a three-point scale, revisiting the dilemma of what can be defined as a normal follicular space.
In the current study, a retrospective analysis of histopathological diagnosis of pericoronal tissues associated with asymptomatic impacted teeth was correlated with the pericoronal follicular space width, which was divided into three groups. Prevalence of impacted molars, followed by canines, premolars and supernumerary teeth, was seen, respectively. Pericoronal follicular space of soft tissues associated with these impacted teeth revealed 56.49% (335/593) of the specimens in the current study undergoing various pathological changes. The majority of the pathologic changes, i.e., 256/335 (76.4%) were seen when the FS was >4 mm to 7 mm (Group C), followed by Group B and A, respectively, suggesting that as the FS increases, the incidence of pathosis increases.
Of the 56.49% of follicles that showed pathosis, 287 (86%) were diagnosed as dentigerous cyst; 27 (8%) were diagnosed as OKC; 15 (4.4%) exhibited ameloblastoma like proliferation; and the rest showed equal distribution
(0.59% each) of odontogenic myxoma, odontogenic fibroma and calcifying odontogenic cyst. Rakprasitkul,[7] in his study on asymptomatic pericoronal tissue of 104 impacted third molars, found an incidence of pathological tissue of 58.65% (dentigerous cyst, 50.96%; chronic nonspecific inflammatory tissue, 4.81%; odontogenic keratocyst, 1.92%; and ameloblastoma, 0.96%).
A similar study by Ali Hossein[19] on 171 ITM, reported 53% pericoronal tissues showing a pathological change, of which the presence of dentigerous cyst was seen in 38% of the cases, ameloblastoma in 5.8%, followed by sulfur granules (4%), foreign-body granulomas and stratified squamous epithelium (3%). Similarly, Curran et al.[5] studied histologic changes in the nonpathologic follicular tissue and diagnosed 32.9% pathologically significant lesions. Dentigerous cyst (77.5%) had the highest incidence, followed by OKC (9.1%), odontoma (8.2%), ameloblastoma (1.5%), CEOC (0.7%), carcinoma (0.7%) and myxoma (0.1%).
Glosser and Campbell[4] found pathological changes in 32% of the impacted third molar follicles; Aldelsperger et al.[23] detected pathosis in 34%; Yildirim et al.[13] detected pathological changes in 23% of asymptomatic follicles; and Baykul et al.[12] have described cystic changes in 50% of asymptomatic follicles. A similar study by Kotrashetti et al.[15] reported 58.5% of asymptomatic cases with definite pathological changes. Of the 41 tissue samples they evaluated, 18 were suggestive of dentigerous cyst.
The results of our study compare favorably with those of others, in that dentigerous cyst is the most frequent pathological entity detected in clinically normal dental follicles of impacted teeth. The proportion of dentigerous cyst relative to all pathological changes seen in impacted teeth follicular tissues vary from 86% in our study and 100% in many studies.[4,12]
Some investigators[4] believe that panoramic and periapical radiographs are insufficient for a definitive diagnosis of dentigerous cyst, which is also the finding of the present study. Not uncommonly, dental follicles exhibit significant thickening of their walls that can create detectable pericoronal radiolucencies without cyst formation. On the other hand, significant pericoronal pathosis, such as odontogenic keratocyst and calcifying odontogenic cyst, have been discovered on histopathologic examination of follicular tissue that was not associated with detectable radiographic enlargement.[5]
In the present study, we discovered a strong correlation between the incidence of cystic change in follicular tissues and age. Notably, this appeared to be true as patients advanced from the second to third decade of life. Previous authors have also reported an increasing incidence of dentigerous cyst formation as age increases.[4,19,23,25] The mean age distribution of DC was 23.1 years, while of the other reported cyst and tumors, it was 30.6 years in the current study. Mourshed[27] found a 1.44% incidence of dentigerous cysts in a radiographic examination of unerupted teeth. Shear and Bernick[25,28] have reported the peak incidence of dentigerous cyst in the second decade. Knight et al.,[29] in a microscopic study, found dentigerous cysts in 44.70% of the impacted teeth.
Consolaro[30] showed that with aging, there is a tendency of transformation of reduced enamel epithelium into stratified squamous epithelium. Baykul et al.[12] reported cystic changes associated with impacted third molars in 56% of the patients 20 years old. In the study done by Yildirimet al.,[13] 89% of the patients whose follicles showed cystic changes were ≥ 20 years old.
According to our results, which are in concordance with other studies, we support the removal of impacted teeth under prophylactic indication as far as possible at a younger age even if the teeth are asymptomatic. However, a small pericoronal radiolucency may represent either a large dental follicle or a small dentigerous cyst. Microscopic examination alone may be insufficient for a definitive diagnosis because a lining of non-keratinized stratified squamous also occurs in some normal follicles. So, the only reliable way to differentiate between the two is by surgical exploration. A true cyst will exhibit a fluid-filled cavity that allows the surgeon to easily separate the DC from at least a portion of the enamel surface of the impacted tooth.[16]
Also, there are many anecdotal reports of complications associated with retained impacted teeth. Even surgeons are sometimes perplexed by the lack of data supporting what has become, for many, one of the most common procedures in oral and maxillofacial surgery.[4] On the other hand, it is also possible that at least some of these cystic areas involute or do not progress to become larger destructive lesions. Hence, a clinical radiographic and histopathological correlation, along with the surgeon’s input at the time of exploration of the FS, is needed for such dilemmas.
In the present study, a greater incidence of impacted teeth was found in the mandible (58.6%) than the maxilla (41.3%), while no significant difference was seen in relation to right side vs. left side. Regarding follicular tissue pathosis, more pathological changes were seen in the lower jaw than in the upper, particularly in the mandibular left (n=110) and right (n=77) impacted third molars, followed by maxillary right (n=45) and left (n=28) impacted third molars.
Adelsperger et al.,[23] in their study, found no statistical difference with regard to the left vs. right side, upper vs. lower dental arch or specific tooth location. Glosser et al.[4] in their study on normal third-molar impactions concluded that more cysts occurred in the lower jaw than the upper, which had no explanation but could be a reflection of radiology-based rather than histology-based interpretation of the study. A significant incidence of pathosis in the lower jaw (vs. upper) was also seen in the study by Mesgarzadeh et al.,[19] which were consistent with findings of Glosser et al.,[14] Raprasitkul,[7] Daley et al.[16] and Kim et al.[3] but not with Adelsperger et al.[23]
Saravana et al.,[14] in their study on ILTM, revealed more follicular changes on the right side than on the left side of the mandible. Significant pathological changes have also been reported by Mesgarzadeh et al.[19] in the mandibular right and mandibular left impacted third molars vs. other sites.
Conclusion
According to the present results, cystic changes may develop in both clinically and radiographically asymptomatic impacted teeth. The data from this study cannot justify the complement removal of all asymptomatic impacted teeth but suggests that there is a risk of pathologic changes, particularly in the second to third decade of life.
If we consider the severity of pathologic conditions associated with impacted teeth, the progression rate of untreated pathologic complication conditions, patient discomfort, agespecific severity of surgical and postsurgical complication, and economic consequences of removal at a stage when pathology has developed, removing asymptomatic impacted teeth is better than observation and periodic follow-up.
Future scope of the study is to include more dental follicles; use of a three-dimensional, computerized tomography scan to measure the accurate width of the follicle; and comparison with histological findings and proliferative markers so that the critical width of the follicular space can be standardized and such lesions dealt with cautiously.
Queries about this article can be sent to Dr. Manchanda at adesh_manchanda@ yahoo.com.
REFERENCES
1. Nanci A. Ten Cate’s Oral Histology. Development, Structure and Function, Mosby Elsevier: St Louis, Mo, USA, 7th edition, 2008.
2. Villalba L, Stolbizer F, Blasco F, Maurino NR, Piloni MJ, Keszler A. Pericoronal follicles of asymptomatic impacted teeth: a radiographic, histomorphologic, and immunohistochemical study. Int J Dent 2012; 2012: 935310.
3. Kim J, Ellis GL, Eisenberg E. Dental follicular tissue: misinterpretation as odontogenic tumor. J Oral Maxillofac Surg 1993; 51(7): 762–767.
4. Glosser JW, Campbell JH. Pathologic change in soft tissues associated with radiographically “normal” third molar impactions. Br J of Oral and MaxillofacSurg1999; 37(4): 259–260.
5. Curran AE, Damm DD, Drummond JF. Pathologically significant pericoronal lesions in adults: Histopathologic evaluation. J Oral Maxillofac Surg 2002; 60: 613-617.
6. Meleti M, Waal ISD. Clinicopathological evaluation of 164 dental follicles and dentigerous cysts with emphasis on the presence of odontogenic epithelium in the connective tissue. The hypothesis of “focal ameloblastoma.” Med Oral Patol Oral Cir Bucal 2013Jan 1; 18(1): 60-4.
7. Rakprasitkul S. Pathologic changes in the pericoronal tissues of unerupted third molars. Quintessence International 2001; 32(8): 633–638.
8. Farah CS, Savage NW. Pericoronal radiolucencies and the significance of early detection. Australian Dental Journal 2002; 47(3): 262-265.
9. Edamatsu M, KumamotoH, Ooya K, Echigo S. Apoptosis-related factors in the epithelial components of dental follicles and dentigerous cysts associated with impacted third molars of the mandible. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, and Endo 2005; 99(1):17–23.
10. Eliasson S, Heimdahl A, Nordenram A. Pathological changes related to long-term impaction of third molars: a radiographic study. Int J Surg 1989; 18: 210-212.
11. Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies—a radiographic study of the Hong Kong Chinese population, Hong Kong Medical Journal 2003; 9(3): 153-163.
12. Baykul T, Saglam AA, Aydin U, Basak K. Incidence of cystic changes in radiographically normal impacted lower third molar follicles. Oral Surg Oral Med Oral Pathol Oral Radiol Endo 2005; 99(5): 542– 545.
13. Yildirim G, Ataoglu H, Mihmanli A, Kizilo D, Avunduk MC. Pathologic changes in soft tissues associated with asymptomatic impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endo 2008; 106(1): 838–842.
14. Saravana GHL, Subhashraj K. Cystic changes in dental follicle associated with radiographically normal impacted mandibular third molar. Br J Oral Maxillofac Surg 2008; 46(7): 552–553.
15. Kotrashetti VS, Kale AD, Bhalaerao SS, Hallikeremath SR. Histopathologic changes in soft tissue associated with radiographically normal impacted third molars. Indian J Dent Res 2010; 21(3):385–390.
16. Daley TD, Wysocki GP. The small dentigerous cyst: a diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:77-81.
17. Stanley HR, Allatar M, Collett WK, Stringefellow HR, Spiegel EH. Pathological sequale of neglected impacted third molars. J Oral Pathol 1988; 17: 113-117.
18. Narang RS, Manchanda AS, Arora P, Randhawa K. Dentigerous cyst of inflammatory origin: a diagnostic dilemma. Ann Diagn Pathol 2012; 16: 119-23.
19. Mesgarzadeh AH, Esmailzadeh H, Abdolrahimi M, Shahamfar M. Pathosis associated with radiographically normal follicular tissues in third molar impactions: a clinicopathological study. Indian J of Dent Research 2008;19(3):208–212.
20. Oliveira DM, Andrade ESDS, Silveira MM, Camargo IB. Correlation of the radiographic and morphological features of the dental follicle of third molars with incomplete root formation. Int J Med Sci 2008; 5(1): 36–40.
21. NIH Consensus Development Conference for Removal of Third Molars. J Oral Surg 1980; 38: 235–236.
22. Ahlqwist M, Grondahl HG. Prevalence of impacted teeth and associated pathology in middle-aged and older Swedish women. Community Dent Oral Epidemiol 1999; 19: 116-9.
23. Aldelsperger J, Campbell JH, Coates DB, Summerlin DJ, Tomich CE. Early soft-tissue pathosis associated with impacted third molars without periocoronal radiolucency. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89(4): 402-406.
24. Moreira Diaz E, del Valle Ruiz M, Rodriguez Alonso LR. Estudio de la correlación entre la imagen radiográfica y elaspectohístico del sacopericoronario de lostercerosmolaresretenidos. Rev Cub Est 1977; 14: 137-44.
25. Shear M. Dentigerous cyst. 3rd ed. Cyst of Oral Regions. Butter Worth Aeinemann Limited 1992:81.
26. Damante JH, Fleury RN. A contribution of the diagnosis of the small dentigerous cyst or the paradental cyst. Pesqui Odontol Bras 2001; 15:238-46.
27. Mourshed F. A roentgenographic study of dentigerous cysts. I. Incidence in a population sample. Oral Surg Oral Med Oral Pathol 1964;18:47-53.
28. Bernick S. Dentigerous cysts of the jaw. Oral Surg Oral Med Oral Pathol 1949; 2: 914-21.
29. Knights EM, Brokaw WC, Kessler HP. The incidence of dentigerous cysts associated with a random sampling of unerupted third molars. Gen Dent 1991; 39: 96-98.
30. Consolaro A. caracterizaçãomicroscópica de folículospericoronários de dentesnão-irrompidos e parcialmenteirrompidos—suarelação com aidade. Bauru, 1987. Tese - Faculdade de Odontologia de Bauru, Universidade de São Paulo.
31. Cabbar F, Guler N, Comunoglu N, Sencift K, Cologlu S. Determination of potential cellular proliferation in the odontogenic epithelia of the dental follicle of the asymptomatic impacted third molars. J of Oral and Maxillofac Surg 2008; 66: (10): 2004–2011.
32. Khorasani M, Samiezadeh F. Histopathologic evaluation of follicular tissues associated with impacted third molars. J of Dentistry 2008; 5(2): 65-70.
33. Urs AB , Shetty DC, Ahuja P, Bablani D, Manchanda AS. Asymptomatic third molar removal – A clinical and pathological insight. J of Orofac Sciences 2010; 2(1): 23-26.
34. Adaki SR, Yashodadevi BK, Sujatha S, Santana S, Rakesh N, Adaki R. Incidence of cystic changes in impacted lower third molar. Indian J of Dent Res 2013; 24(2): 183-187.
35. Choudhary A, Kesarwani Pathological changes in radiographically normal dental follicle. Indian J of Contemporary Medical Research 2019; 6(5): E4-7.

Adesh S. Manchanda, M.D.S., is a reader, Department of Oral & Maxillofacial Pathology, Sri Guru Ram Das Institute of Dental Sciences & Research, Amritsar, Punjab, India.

Ramandeep S. Narang, M.D.S., is professor and head, Department Oral & Maxillofacial Pathology, Sri Guru Ram Das Institute of Dental Sciences & Research, Amritsar, Punjab, India.

Komaldeep Kaur Sandhu, B.D.S., is affiliated with Sri Guru Ram Das Institute of Dental Sciences & Research, Amritsar, Punjab, India.











