In Focus: Indoor Air Quality and Wellness
The Impact of PM2.5, PM10, and Indoor Pathogens on Human Health: Reframing Indoor Air Quality in Integrative and Functional Medicine
October 1, 2025
(c) Copyright 2025 Agentis Air LLC. Brio is a registered trademark, and APART and Refresh Plus are trademarks of Agentis Air LLC. Use of this content is not permitted without written authorization from Agentis Air LLC.
The Impact of PM2.5, PM10, and Indoor Pathogens on Human Health: Reframing Indoor Air Quality in Integrative and Functional Medicine
Executive Summary
Healthy indoor air quality is a cornerstone of patient-centered health, directly influencing respiratory, cardiovascular, cognitive function, and overall well-being. PM2.5, PM10 PM.01, and indoor pathogens contribute to human health risks and yet are often overlooked. Fortunately, evidence-based interventions exist to address these root causes of illness and inflammation.
Drawing on research from the Harvard T.H. Chan School of Public Health (HSPH), the World Health Organization (WHO), ASHRAE, and the CDC, this report emphasizes the importance of prevention-oriented IAQ strategies within the home environment. ¹ , ² , ³ , ⁴
Byreframingindoorairmanagementasaclinicalandpublichealth imperative,providerscanmeaningfullyreducediseaseburdenand promoteresilienceacrossthelifespan.
IAQ in Integrative and Functional Medicine
Integrative and functional medicine focus on holistic, preventive strategies that address the root causes of illness. This approach recognizes home and work environments particularly the air quality in each as a foundational influence on health outcomes. By prioritizing IAQ, providers embrace a powerful avenue for both reducing disease risk and elevating patient vitality, supporting their core mission of empowering patients toward sustainable wellness. ⁵ , ⁶
Indoor air quality long treated as an environmental health issue rather than a clinical one is now recognized as a modifiable risk factor for systemic inflammation, cardiometabolic dysfunction, neurodegeneration, and immune dysregulation. ⁷ The Harvard T.H. Chan School of Public Health highlights that poor IAQ is linked not only to respiratory illness but to
cardiovascular disease, impaired cognitive development in children, and increased all-cause mortality, with indoor household exposures responsible for much of the global disease burden. ⁸
Providers have an immediateopportunitytotreatthehomeenvironment asatherapeutictargetalongsidenutrition,stressmanagement,mentalhealth, and sleepquality.
P articulate Matter: PM2.5 and PM10
Fine and coarse particles suspended in the air are among the most pervasive contributors to indoor pollution. Particulate matter is classified by size PM2.5 consists of particles ≤2.5 µm, while PM10 includes particles up to 10 µm. These particles are readily inhaled, with PM10 settling in larger airways ⁹ , ¹⁰ and PM2.5 reaching the deepest regions of the lungs.
The ability of PM2.5 to penetrate lung tissue and enter the bloodstream connects it to a wide spectrum of health risks. Understanding the sources, pathways, and clinical effects of airborne particulate matter equips healthcare professionals to target PM as a modifiable risk especially for the most vulnerable patients. ¹¹ , ²
Sources and Distribution
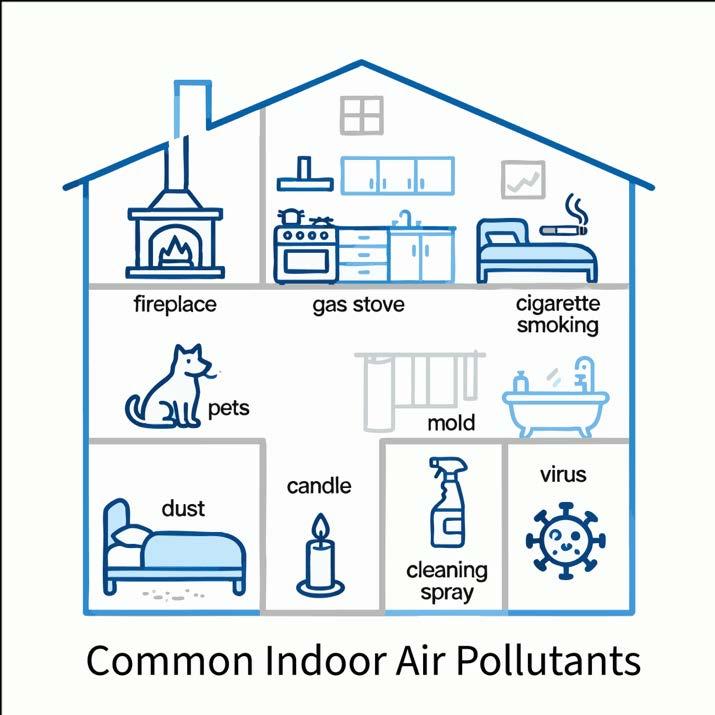
Indoor sources include combustion (woodburning and gas stoves, candles), smoking, cleaning products, resuspension of dust, pet dander, dust mite feces, and poorly maintained HVAC systems. ¹¹ , ¹⁰
Most adult PM2.5 exposure occurs indoors, however infiltration from outdoor sources ¹¹ , ⁹ is the primary contributor to poor IAQ. Outdoor sources include traffic emissions, wildfires, and industrial activities, along with tree, grass, and flower pollens. Outdoor PM2.5 infiltrates homes through ventilation, leaks, and the building envelope. ² , ⁹

Health Effects from Airborne Particulate Matter
PM2.5 exposure has been linked to increased hospitalizations for heart and lung conditions, bronchitis, asthma attacks, and even premature death. ¹³ , ¹⁴ , ¹⁵
PM10 also triggers types of inflammation that can lead to an inflammatory cascade damaging lung tissue and contributing to chronic diseases. Children and individuals with obesity or preexisting lung conditions are more susceptible, with greater PM deposition and symptom frequency among these groups. ² , ¹³
Particle Size Main Routes in Body Key Health Risks
PM10
( ≤ 10 µ m) Nose, throat, upper lungs Irritation of eyes, nose, throat; increased respiratory symptoms; may worsen existing lung/heart issues
PM2.5
( ≤ 2.5 µ m, “fine PM”)
PM0.1
( ≤ 0.1 µ m, “ultrafine
Deep lungs, can enter bloodstream
Aggravated asthma, COPD, reduced lung function, heart attacks, strokes, premature death, cancer, dementia, reduced productivity
PM”) Deep lungs, rapidly to bloodstream and organs Pulmonary inflammation, cardiovascular disease, hypertension, systemic inflammation, diabetes, possibly brain and fetal impacts
Notes
Less likely to penetrate deep lung tissue
Main health concern from air pollution; cause of haze
Can cross cellular barriers; highest risk per mass
Short-term exposure to PM2.5 and PM10 can trigger:
• Spikes in hospital admissions for asthma, COPD, cardiac events, and bronchitis. ¹² , ¹⁰
• Acute respiratory distress and reduced lung function in vulnerable populations (children, elderly). ¹¹
Prolonged PM exposure is linked to:
• Accelerated decline in lung function, increased rates of asthma, COPD, and lung cancer.
¹³ , ¹⁴ , ¹²
• Elevated risks for cardiovascular disease, diabetes, dementia, autoimmune conditions, and premature death. ¹⁴ , ¹⁵
• Each 10 µg/m³ increment in PM2.5 or PM10 is associated with significant increases in morbidity and all-cause mortality. ¹³ , ¹⁴
• Epigenetic and genetic changes can perpetuate inflammation and immune defects even after exposure ends. ¹⁵ , ¹¹
The New Normal: Wildfire Smoke
As wildfires become a fixture on the North American landscape, awareness of wildfire-smokerelated health risks is growing. Consider the following from the Journal of the American Medical Association (JAMA):
• In 2025, a cohort study found that days and weeks after major wildfire events in the western U.S., regional hospitals experienced a spike in admissions for respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). Elevated rates of cardiovascular hospitalizations were also observed, though associations were strongest for respiratory conditions.21
A study from the TH Chan School of Public Health at Harvard University shows the effects can be severe and long lasting:
• Wildfire smoke exposure in recent years has caused acute health crises, with statistically significant rises in hospitalizations for respiratory and cardiovascular diseases, and higher mortality rates, particularly in children and people with pre-existing conditions.22
The Special Case of PM0.1
PM0.1 refers to ultrafine particles with aerodynamic diameters smaller than 0.1 micrometers (100 nanometers), representing the smallest fraction of atmospheric particulate matter. These particles are distinguished from larger particulate matter categories like PM2.5 and PM10 by their extremely small size, which gives them unique physical and biological properties. Due to their nanoscale dimensions, PM0.1 particles have a much larger surface area -to-volume ratio compared to larger particles, making them more chemically reactive and capable of carrying greater concentrations of toxic substances per unit mass. The ultrafine nature of these particles allows them to penetrate deeper into biological tissues and cross physiological barriers that larger particles cannot breach, including the blood-brain barrier and alveolar-capillary membrane.
PM0.1 particles originate from various sources including vehicle emissions, industrial processes, and natural phenomena, but their small size and high reactivity make them particularly concerning from a public health perspective due to their enhanced ability to cause biological damage at the cellular and molecular level.20
PM0.1 can cause systemic inflammation, endothelial dysfunction, and coagulation changes that predispose individuals to ischemic cardiovascular disease and hypertension. PM 0.1 are also linked to diabetes and cancer. PM 0.1 can travel up the olfactory nerves to the brain and cause cerebral and autonomic dysfunction.
The Health Effects of Ultrafine Particles, Experimental and Molecular Medicine , March 2020.
The Correlation Between IAQ and Mental Health
In the 2024 article “The Surprising Link between (Indoor) Air Quality and Mental Health”, the Harvard School of Public Health summarized the connection between mental health and poor air quality:
“Research shows that long-term and short-term exposure to air pollution can have profound and enduring negative effects on mental health. Scientists found that exposure to high levels of air pollution in the past five years can lead to decreased quality of life and an increased risk of depression and suicide ideation. Breathing unhealthy air is also
associated with increased anxiety symptoms. Furthermore, exposure to air pollution is associated with dementia, Alzheimer’s disease, Parkinson’s disease, and autism.” 25,27,30
Mental Health Condition Air Pollution Association Source (2023 – 2024)
Depression & Suicide
Ideation
Anxiety
Quality of Life
Dementia, Alzheimer's, Parkinson's
Autism
Linked with PM2.5, NO₂, exposure
Associated with unhealthy air
Decreased with high exposure
Increased risk, cognitive decline
Evidence of increased risk
Harvard 25 , Psychiatry.org 24 , EEA 26
Harvard 25 , Psychiatry.org 24
Harvard 25, EEA 26
Harvard 25, Frontiers in Neuroscience 23
Harvard 25, EEA 26, Sage
Journals 27
TherelationshipbetweenpoorIAQandmentalhealthisanareaofhigh importanceforfunctionalandintegrativemedicineproviders,astheyfocus onthewellbeingofthewholeperson.
Pathophysiological Mechanisms
• Oxidative Stress: PM2.5 induces systemic oxidative stress, leading to cellular injury and apoptosis. ¹⁰ , ¹¹
• Inflammatory Cascades: Activates neutrophils and macrophages, producing cytokines (IL1β, IL-6, TNF-α), sustaining tissue damage and remodeling. ¹⁴ , ¹³
• Host Defense Impairment: Blunts phagocytosis, inhibits mucociliary clearance, and increases infection risk. ¹⁶ , ¹¹
• Autoimmunity: Chronic exposure disrupts immune regulation, raising risk for autoimmune diseases (rheumatoid arthritis, SLE, IBD). ¹⁴
Indoor Pathogens: Microbial and Viral Threats
Bacteria, viruses, and fungi thrive when ventilation is poor and humidity is high, leading to both acute infections and chronic inflammatory illness. Recognizing and managing these microbial risks is essential. ¹ Harvard research links damp, mold-prone environments to higher asthma prevalence in children, while poorly ventilated homes enable rapid airborne transmission of influenza, coronaviruses, and other infectious aerosols. ⁸
Reservoirs and Transmission
Indoor environments concentrate airborne viruses, bacteria, and fungi through dampness, poor ventilation, and accumulation of PM. ¹⁶ , ¹⁵
• Pathogens: Influenza, RSV, coronaviruses, Streptococcus pneumoniae, Staphylococcus aureus, Aspergillus, and other molds are among the relevant airborne pathogens.
• Amplifiers: Water damage, humidity above 60%, poor air filtration, and HVAC contamination increase proliferation and transmission. ¹⁷ , ¹⁵
Health and Immune Effects of Indoor Pathogens
• Increased acute and chronic respiratory infections. ¹⁸ , ¹⁶
• Asthma exacerbations, pneumonia, and rhinosinusitis.
• Indoor pathogen exposure impairs innate immunity and increases rates of severe infection in at-risk individuals. ¹⁴ , ¹⁶
• Persistent exposure inflames airway linings and can trigger allergic and auto-inflammatory reactions.
Pathophysiology: Inflammation and Immune Dysregulation
The health impacts of PM2.5, PM10, and pathogens extend beyond the respiratory tract, contributing to multi-system inflammation and immune dysfunction. Chronic exposures drive persistent systemic damage, implicated in neurodegenerative, cardiometabolic, and immunologic diseases. ¹⁸ , ¹⁴ , ¹⁵
What can be done to preserve and restore health?
Evidence - Based Interventions for PM2.5, PM10, and Pathogen Control in Homes
The clinical burden of poor IAQ can be dramatically reduced with targeted interventions. ¹ These fall into three categories: source control and ventilation, monitoring and maintenance, and effective filtration, with practical steps implemented as follows:
Ventilation and Source Control
• Increase outdoor air intake when ambient air is clean, and seal homes during pollen, wildfire or smog events.
• Manage combustion sources; replace gas stoves with induction, use exhaust fans, enforce smoke-free policies.
• Target moisture to keep humidity between 30–50%.
Monitoring and Maintenance
• Household PM, CO₂, and VOC monitors help track unseen contaminants.
• Annual HVAC servicing will optimize performance.
• Educate families to respond adaptively to seasonal and environmental shifts.
Filtration and Air Purification Options
• HVAC Upgrades: Use MERV 13+ or HEPA filters wherever system design allows.
• Add Portable air purifiers including portable or in-room Electronic Air Cleaners (EACs). With low energy use and low maintenance, these reduce both PM and microbial bioaerosols.
UL 2998-certified EACs avoid harmful byproducts such as ozone
• Hybrid Systems: Upgrades HVAC systems plus in-room air cleaners may be maximal for bedrooms, nurseries, and elder-care spaces.
Clinical Implications for Providers
Integrative and functional medicine practitioners can incorporate air quality screening, risk stratification, and intervention strategies into their clinical workflow.⁵ IAQ screening can identify PM, pathogens, ventilation, and humidity concerns in patient intake, using validated questionnaires. ¹³ , ¹⁷ , ¹⁵
Personalized Care Plans and Pathogen Control Protocols
Personalized care plans and pathogen control protocols are essential, as indoor air quality emerges as a significant factor in patient health. Modern healthcare recognizes that vulnerability to airborne pollutants and pathogens may differ based on age, health status, living environment, and exposure to specific triggers such as wildfire smoke or seasonal pollution. ¹¹ , ¹ ⁵
Advances in air quality monitoring and data integration now enable clinicians to tailor interventions that directly address these personal risks, ranging from household filtration upgrades to targeted education and environmental management strategies.
Effective personalized plans begin with a thorough assessment of the patient’s environment and vulnerabilities. For example, children with asthma, pregnant individuals, elderly, and people with chronic respiratory or immune conditions require specialized attention and protective measures to minimize exposure to harmful particles and pathogens. ¹⁹ , ¹⁰ Using digital health tools and real-time air quality data, providers can issue alerts or recommendations to limit harmful exposures during high pollution events such as wildfires, or in clinical settings where infection risk is elevated.
To operationalize this, providers can take the following proactive steps :
• Integrate IAQ into Routine Assessments: Begin by incorporating a brief environmental exposure history into patient intake forms. Questions should cover potential sources of indoor pollution such as gas stoves, wood-burning fireplaces, nearby highways, recent water damage or mold, and the type of home ventilation and filtration used. This initial screening helps identify high-risk individuals and environments without complex testing.
• Educate and Empower Patients: Teach patients how to use readily available tools like the Air Quality Index (AQI) to manage exposure to outdoor pollutants. Provide them with a tiered list of practical, actionable solutions for their homes, starting with low -cost strategies like source control and regular cleaning, and progressing to recommendations for portable air purifiers for bedrooms or upgrading HVAC filters to a MERV 13 rating or higher.
• Prescribe Personalized Air Quality Plans: For vulnerable patients including children, the elderly, pregnant individuals, and those with chronic cardiorespiratory or immune conditions develop specific IAQ improvement plans. These plans should target the primary pollutants identified in the assessment and be tailored to the patient’s living situation and financial resources.
• Lead by Example and Advocate for Change: Ensure that clinical spaces meet the highest IAQ standards through enhanced filtration, ventilation, and continuous monitoring, thereby protecting both patients and staff. Use this leadership position to advocate for healthier building standards and public health policies that address the disproportionate impact of poor air quality on underserved communities.
Byembeddingthesestrategiesintothecoreofclinicalpractice,integrative andfunctionalmedicineproviderscanmakeIAQafoundationalelementof holisticcare.Thisproactiveapproachdrivesprevention,improvesoutcomes, andempowerspatientstotakecontroloftheirhealth,supportingtheirlongtermflourishingacrossalllifestages.
Conclusion
Indoor particulate matter and pathogens represent a potent, actionable front in chronic disease prevention and holistic wellness. For integrative and functional medicine to fully realize its mission, providers must move beyond simple awareness of environmental factors and begin to proactively manage them. Care plans should treat IAQ improvement as complementary to nutrition, stress management, and conventional therapies. By equipping themselves with evidence-based strategies, clinicians can transform the indoor environment from a source of chronic health risks into a base of patient resilience and vitality. This requires a new clinical mindset where prescribing an air purifier becomes as fundamental as recommending a dietary change.
Reference List
1. Allen, J. G., & MacNaughton, P. (2022). Healthy buildings: How indoor spaces drive performance and productivity. Harvard T.H. Chan School of Public Health, Healthy Buildings Program. PMID: 26231502
2. World Health Organization. (2021). WHO global air quality guidelines: Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: WHO.
3. ASHRAE. (2020). Position document on infectious aerosols. Atlanta, GA: American Society of Heating, Refrigerating and Air-Conditioning Engineers.
4. Centers for Disease Control and Prevention. (2023). Ventilation in buildings.
5. Bland, J. S., & Minich, D. M. (2013). Personalized Lifestyle Medicine: Relevance for Nutrition and Lifestyle Recommendations.
6. Pizzorno, J. E. (2014). Environmentally triggered illnesses: Integrative and functional medicine approaches.
7. Schraufnagel, D. E., Balmes, J. R., Cowl, C. T., et al. (2019). Air pollution and noncommunicable diseases: A review by the Forum of International Respiratory Societies.
8. Harvard T.H. Chan School of Public Health. (2023). The impact of air pollution on health: PM2.5, PM10, and beyond.
9. Wallace, L. A., & Ott, W. R. (2011). Personal exposure to ultrafine particles.
10. U.S. Environmental Protection Agency. (2022). Integrated Science Assessment (ISA) for Particulate Matter. Office of Research and Development.
11. World Health Organization. (2021). WHO global air quality guidelines: Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: WHO.
12. Pope, C. A., & Dockery, D. W. (2006). Health effects of fine particulate air pollution: Lines that connect.
13. Anderson, J. O., Thundiyil, J. G., & Stolbach, A. (2012). Clearing the air: A review of the effects of particulate matter air pollution on human health.
14. Liu, C., Chen, R., Sera, F., et al. (2019). Ambient particulate air pollution and daily mortality in 652 cities.
15. Calderón-Garcidueñas, L., et al. (2016). Air pollution and your brain: Mechanisms of neurodegeneration and cognitive decline.
16. Morawska, L., & Milton, D. K. (2020). It is time to address airborne transmission of coronavirus disease 2019 (COVID-19).
17. Fisk, W. J. (2013). Health benefits of particle filtration.
18. Munzel, T., Sorensen, M., Gori, T., et al. (2020). Environmental stressors and cardiometabolic disease.
19. Elevate Energy. (2025). Indoor Air Quality and Asthma Prevention Resources.
20. Schraufnagel, D.E. (2020). The health effects of ultrafine particles. Experimental and Molecular Medicine, 52, 311–317. https://doi.org/10.1038/s12276-020-0403-3
21. Journal of the American Medical Association (JAMA). (2025). Wildfire smoke cohort study. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2833326
22. Harvard T.H. Chan School of Public Health. (2024). Cardiorespiratory effects of wildfire smoke particles can persist for months even after a fire has ended. https://hsph.harvard.edu/news/cardiorespiratory-effects-of-wildfire-smoke-particles-canpersist-for-months-even-after-a-fire-has-ended/
23. Frontiers in Neuroscience. (2024).
https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1351721/full
24. American Psychiatric Association. Air pollution's impact on mental health. https://www.psychiatry.org/news-room/apa-blogs/air-pollutions-impact-on-mental-health
25. Harvard T.H. Chan School of Public Health. The surprising link between indoor air quality and mental health. https://healthybuildings.hsph.harvard.edu/the-surprising-link-betweenindoor-air-quality-and-mental-health/
26. European Environment Agency. (2024). European zero pollution dashboards: Impact of air pollution on mental health. https://www.eea.europa.eu/en/european-zero-pollutiondashboards/indicators/impact-of-air-pollution-on-mental-health-signal-1
27. National Institutes of Health/PMC. Article on air quality. https://pmc.ncbi.nlm.nih.gov/articles/PMC10375903/
28. SAGE Journals. Article on mental health and air quality. https://journals.sagepub.com/doi/full/10.1177/09603271231191436
29. ScienceDirect. Article on mental health and environmental exposure. https://www.sciencedirect.com/science/article/abs/pii/S0013935118302159
30. National Institutes of Health/PMC. Recent article on air quality. https://pmc.ncbi.nlm.nih.gov/articles/PMC11083864/






