

A New Era of Diagnostics
How disruptive technologies, shifting patient expectations, and policy reform are converging to define tomorrow’s lab tests.



NDC’s Michael Price on resiliency in distribution.
The importance of finding balance with space, workflow, and technology in the patient setting.
How the OBBBA could reshape hospital finances, payer mix, and value-based care.
From provider shortages to limited infrastructure, rural America’s health crisis demands more than shortterm funding fixes, experts caution.
Cleveland Clinic advances women’s health through tailored care for women in their midlife.
Wearable devices for diabetes have revolutionized patient care delivery and clinical workflows in post-acute care settings.
A Season of Gratitude

November always carries a special rhythm: a pause before the holiday rush, a time when the air cools and we naturally slow down just enough to reflect. It’s fitting that Thanksgiving, one of our country’s oldest traditions, falls this month. The first Thanksgiving, shared nearly 400 years ago between the Pilgrims and the Wampanoag people, wasn’t about abundance or luxury. It was about gratitude and thankfulness for survival, community and the promise of tomorrow.
That same sense of gratitude resonates deeply in our industry. Each of us in medical supply and distribution plays a role, sometimes behind the scenes, often without recognition, in a system that saves lives every single day. We make sure the exam gloves, diagnostic tests, wound care products and instruments reach clinicians who depend on them. It’s easy to get caught up in quarterly numbers and year-end goals, but this time of year reminds us why our work truly matters. We serve an industry that grows not just in revenue, but in purpose.
The healthcare supply chain continues to expand as care shifts closer to the patient – into physician offices, surgery centers, labs and homes. With that growth comes both opportunity and responsibility. It means more jobs, more innovation, and more chances to make a difference in people’s lives. But it also means we must continue to uphold the relationships and trust that built this industry from the ground up. Our friendships with customers, manufacturers, and fellow distributors are what sustain us through change and challenge. And as we all know our industry faces challenges on the regular.
This November, I hope each of you takes a moment to reflect not only on your career but also on your family and the country we’re fortunate to live and work in. The freedom to build businesses, serve communities and improve healthcare is something worth celebrating. Whether you’re spending Thanksgiving around a crowded table or catching your breath between calls, remember that gratitude is what binds us together as colleagues, friends and Americans.
Finally, a sincere thank-you to the manufacturers and advertisers who support Repertoire Magazine . They not only value your role as distribution sales professionals but also invest in educating and equipping you for success. Their partnership makes it possible for us to share stories, insights, and training that strengthen our entire industry.
Wishing you and your family a wonderful Thanksgiving season filled with peace, purpose, and gratitude.
Happy Thanksgiving,
R. Scott Adams Publisher
editorial staff
editor Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews Jenna Hughes jhughes@sharemovingmedia.com
content creator Pete Mercer pmercer@sharemovingmedia.com
art director Brent Cashman bcashman@sharemovingmedia.com
circulation Laura Gantert lgantert@sharemovingmedia.com
sales executive Aili Casey acasey@sharemovingmedia.com (404) 625-9156
publisher Scott Adams sadams@sharemovingmedia.com (800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914 Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com

Test smart, breathe easy
The Sofia® 2 Analyzer makes respiratory testing for the school year easy
Back-to-school season means respiratory syncytial virus (RSV) and strep are back in season, too. Be prepared for all your patient testing needs with advanced diagnostic solutions from QuidelOrtho.
• RSV
• Flu + SARS Antigen*
SARS Antigen*
SARS Antigen+**
• Influenza A+B
Strep A+ For more information scan the QR code, call 800.828.6316 or contact your Henry Schein Representative.

Death by a Thousand Good Days
Why “doing fine” might be the greatest threat to your sales team.
By Brian Sullivan

 There’s a slow, quiet way sales teams die.
Not from layoffs. Not from economic collapse. Not from tariffs.
But from good years.
A string of good-enough quarters. A few reliable accounts. Comfortable margins. A sales team that’s “earned the right” to coast. Until one day, someone looks around and realizes: We’re no longer growing. We’re just… existing. This week, I met that team.
When no one is challenged
Just a few days ago, I was on a discovery call with a sales leader. He was smart, likable, experienced – and completely aware of his team’s reality.
He told me – without flinching – that their veteran reps don’t prospect anymore.
They don’t go deeper with existing customers.
They don’t use LinkedIn.
And their idea of training? Talking strategy.
When I pulled up several of their LinkedIn profiles, most were blank. I mentioned it.
His response?
“Oh yeah, we don’t use LinkedIn. That’s more for people looking for jobs.”
I just sat there.
Here was a multi-milliondollar company, with a full sales team … proudly choosing irrelevance.
They’ve had a lot of good years. But you could feel it – deep down, this guy knew the good years had made them soft.
He wasn’t defensive. He was resigned.
So, I figured, why not just say what I was thinking?
“Are you telling me that you and your team have decided to stop improving?”
That hit him.
“No, no, no – we want to get better,” he stammered.
So, I pushed.
“You told me your reps don’t prospect,” I said. “They don’t ask deeper questions. They don’t even use the most powerful tool in modern B2B selling. You had a chance to give them two hours of focused skill development at your national meeting – and they voted it down. Why?”
His answer?
“They said there are better things we could do with that time.” I asked, “Like what?”
He said, “We’ll talk strategy.”
“OK … strategy about what? Because if your team isn’t improving their ability to open new doors or go deeper with clients, what exactly are you strategizing?”
Silence.
And then the truth: He didn’t want to challenge them.
Didn’t want to make waves. Didn’t want to be the leader who “pushed too hard” after all these good years.
It hit me right there: This is what death by a thousand good days looks like.
Nobody gets fired. Nobody panics.
They just quietly accept that “good enough” is good enough.
The hidden threat of “fine”
We’re not talking about burnedout teams or failing businesses.
We’re talking about the comfortable ones. The coasting ones.
The ones that show up to meetings, know the product, hit quota –and haven’t changed in a decade.
That’s the danger.
Not the bottom 10%.
The middle 70%.
The reps who are doing “fine.”
But let’s be clear:
Fine doesn’t disrupt markets.
Fine doesn’t win competitive bids.
Fine doesn’t future-proof your business. And fine is always the step before forgotten.
Want to break the cycle?
Start here.
Here are 5 ways to wake up a team drifting toward average –without blowing up your culture:
1 Create a “friction ritual”
Ask your team: What did you do this week that made you sweat?
If there’s no friction, there’s no growth. Engineer discomfort. Public call sessions. Shadowing top reps. New pitch rewrites. Track the tension.
2 Audit “improvement avoidance”
What’s something they’ve been avoiding learning? LinkedIn? AI? Asking financial questions? Have everyone write down one skill they’ve avoided – and one step they’ll take to tackle it this week.
3 Replace “strategy talk” with roleplay
Every team says they “talk strategy.” Great. But if they can’t
execute it live in front of peers, it’s just talk. Swap 30 minutes of strategy for 30 minutes of application. Watch what happens.
4 Measure curiosity, not just closes
Ask reps to bring one new question each week that uncovered a hidden need, a referral, or a roadblock. Reward learning behavior – not just outcomes.
5 Lead with the mirror, not the megaphone Leaders: before you demand growth from your team, look at your own habits. Are you getting better? Are you pushing, investing, experimenting – or are you comfortable, too?
The choice to grow
On that call, I told that sales leader something I’ll tell you, too: “Getting better isn’t for everyone. But I’ve never met someone who said ‘I regret leveling up.’”
If you’re reading this, maybe it’s time to ask the question: Have we been slowly dying from too many good days?
And if the answer is yes, what are you going to do today to make tomorrow just a little more uncomfortable?
Because comfort won’t kill you today.
It’ll kill you eventually. Quietly. Predictably.
And without a fight – unless you choose to bring one.
Brian Sullivan, CSP, is the Founder of PRECISE Selling and a leading voice in B2B sales strategy. He helps companies master the art of prospecting, presenting, and negotiating – while also building elite outsourced sales teams through his PRECISE Performers division. A nationally recognized speaker and author of 20 Days to the Top, Brian’s mission is simple: turn salespeople into champions. Learn more at www.preciseselling.com
Embracing Experimentation with QuidelOrtho’s Audra Jones
By Pete Mercer
In a recent episode of the Repertoire Podcast, host Scott Adams spoke to Audra Jones, senior vice president and head of North America for QuidelOrtho, about her role at the company, where the organization is headed, and the importance of manufacturerdistributor relationships in delivering value to clients.
Delivering value together
To spark fresh thinking on how to amplify the customer experience and use small moments to build deeper relationships with customers, QuidelOrtho invited Jesse Cole, founder of Fans First Entertainment and owner of the Savannah Bananas, to speak at the annual sales kickoff meeting.
During his keynote, Jones noted, Cole shared how a “fans first” experience comes to life in his organization and challenged QuidelOrtho’s leaders to consider what it could look like within theirs.
“We are very passionate about developing an organization that employees want to work for,” Jones said. “On the other side of that, we also want our distribution partners and the customers that we collectively serve to become fans of QuidelOrtho. When I think about the audience that we serve, I think about how the great partnership between the distribution and our sales reps can deliver that together.”

Creating space for experimentation
One of the challenges that leaders often must overcome is giving their team members the space to experiment and be creative. This is a leadership style that allows their teams to think outside the box and come up with what might be an indirect approach to solving a problem. For Jones, those solutions are the goal. Her approach to leadership hinges on creating a trusting, experimentative environment that gives her team a safe space to fail.
“Don’t be guided by your failures,” she said. “Be willing to wake up every day and ask, ‘How can I engage a little bit differently? How can I challenge the status quo of the organization?’ It’s also in how we work with our partners and customers, creating a platform that provides a safe space for people to fail, and on the other side of that, it can lead to discovering new, innovative ways of going to market and working.”
Delivering on a promise
QuidelOrtho sees distribution as a true partner in bringing healthcare closer to patients, especially in rural communities. Physician office labs are becoming central to care, and distribution plays a critical role in helping them deliver reliable, accessible testing. “When our partners think about solving problems for customers, I want them to see the value of our Certified Solution,” said Jones. This program gives practices an affordable, full testing menu for their local patients.
Beyond innovation, QuidelOrtho prides itself on service — ranked No. 1 for over five years — so distributors and clients benefit from strong, reliable support. By combining advanced solutions with a robust service model, QuidelOrtho and distribution partners work hand-in-hand to improve patient access and strengthen community health nationwide.
Audra Jones
VITROS™ Cer tified Analy zers
Confidence you c an count onAt a smar ter value
Power up your lab with the built-in intelligence and ef f icienc y of our VITROS Systems, designed to make it easier to do more with less VITROS Systems complete the analy tical process the first time without inter vention or repeat testing for 96 5 percent of tests conducted 1
The cer tified advant a ge Ever y cer tified analy zer undergoes a rigorous cer tification process to ensure like-new qualit y and per formance
Count on reliable per f ormanc e
Keep your lab powered up and ready when you are with high-per formance systems and industr y-leading uptime 2
Dri ve oper ational ef f iciency
Power your lowest total cost of ownership with purposefully designed solutions

Learn more about VITROS Systems by scanning the QR code or cont acting QuidelOr tho today.
Cer tified and shipped in the USA
Ensure high- qualit y re sul t s
Trust the results of ever y test, ever y day with intelligent technologies and patient-focused design that deliver the highest qualit y and precision
Flex to enable w ha t's nex t E x pect consistent qualit y results across your net work with f lexible, scalable and connected solutions

Beyond Satisfaction: Building True Customer Loyalty
Customer experience expert Lisa Ford explains why satisfied customers could still walk away – and how leaders can create experiences that keep them coming back.
By Pete Mercer
 In business, everything begins and ends with the customer experience. In the competitive and highly regulated world of medical sales, the quality of the customer’s journey is no longer a bonus – it’s a necessity. From the initial point of contact to post-sale support, every interaction shapes how healthcare providers perceive not just a product, but the company behind it.

Repertoire Magazine recently sat down with Lisa Ford, an expert in customer experience, to discuss what exceptional customer service looks like in 2025, what drives customer loyalty, and how leadership plays role in creating a customer-focused culture.
The customer experience in 2025
For over 40 years, Ford has helped companies, businesses, associations, and teams figure out how to be more customer focused and create those memorable experiences for their customers. In that time, she has seen the whole breadth of the customer experience, from top to bottom, bad to good.
As for what the customer experience looks like in 2025, Ford said, “Customer service today is much more customized and personalized to the customer. But I do think there’s a lot that hasn’t changed – the basics of human contact are still in place and need to be. Those human skills, empathy skills ... Great
HELP THEM STICK TO THE PLAN.

Afinion™ 2 Analyzer Key Benefits
The first and only point-of-care HbA1c test cleared for diagnosing*, screening*, and monitoring diabetes.

in just 3 steps









listening, just knowing how to finesse someone in problem situations, finding solutions. All that remains the same when you’re one-on-one with the customer.”
Businesses have to work harder to fight for the attention of their customers – attention and time is valuable, and there’s not enough to go around for everyone. Finding ways to make yourself stick out in the crowd is one of the biggest challenges for business leaders to stay relevant in today’s market, especially in healthcare.
with understanding that customer service and the customer experience are intertwined with each other, but not the same thing. Ford described the customer experience as the big picture, an all-encompassing idea of how the customer walks away from any interactions with your organization. Customer service is the nuts and bolts, or the soft skills that make all the big ideas come together in a beautiful way.
“First, I’ve got to make sure they’re really seeing customer experience as the total picture,
“I think the empowerment issue is one of the next big steps of a customer-centric culture. That team member needs to be empowered to make decisions on behalf of the organization and the customer. If we’ve hired well and trained well, they can do that.”
With so many devices and medical equipment on the market today, it’s rare to find something unique from the rest of the options that are available. That’s why you need the attention of your customers. “I think customers are certainly more impatient, picky, and demanding. They are on the move, so we have to make certain that we capture and keep them.”
Understanding the customer experience
Part of the challenge with creating a finely tuned customer experience is having a complete understanding of what the customer experience is and how it works. These can be small details, so they’re easy to miss. It starts

Lisa Ford
where customer service is a piece of that experience,” Ford said. “The customer experience is what they experience – not what you
want them to experience, not your intentions. The experience is what happens when the customer’s doing business with you before, during, and after. All those meaningful touches along the way have to create an emotion that links them to you.”
One of the big components that companies misunderstand is that they have to be proactive and responsive with their customers. This means anticipating needs and having a solution at the drop of a hat. This is obviously a huge challenge, but it’s what is going to separate you from the other people who are not willing to take that extra step to ensure that the customer has what they need. That’s what makes a difference in these interactions.
“Everything matters. We’ve got to make certain that we’re doing it across all those touchpoints. In many cases, that’s what’s missing. Not enough organizations are looking at all their touchpoints to identify what works and what doesn’t.”
Driving customer loyalty
With a better understanding of what the customer experience is, how does customer loyalty play into this? What drives customer loyalty? According to Ford, the number one thing to understand is that a satisfied customer is not necessarily a loyal customer.
With a satisfied customer, you almost have to assume that you’re always one step away from them taking their business elsewhere. What’s stopping them? Sure, they could be happy. But as soon as something shifts, there’s nothing

to stop them from finding the next best thing. Ford said, “The customer is in constant change. Their perception of you is in constant change.”
To effectively drive loyalty with your customers, Ford argues that it’s all about adding value. If they feel like they can come to your team with a multitude of problems after you’ve already solved one, that conveys a sense of trust that speaks volumes. You want your customers to feel known by you, and you can further drive that loyalty and trust by doing things like saving them time and money, reducing any concerns they might have, and making their lives easier.
“A loyal customer is the one who continues to do business
with you,” Ford said. “They go deeper into your products and services, and they say positive things about you within your marketplace. I think it’s everything from word of mouth to increased spending. They trust you and are more willing to take your recommendations.”
Using company culture as a foundation
The culture of your organization is the foundation of your customer experience, and it will shape how your customers engage with your business. They will be able to tell when your culture is unhealthy because it will impact every touchpoint, especially when they’re speaking to your team
members. An unhealthy culture will seep into the fabric of your organization and affect everything, so it’s important to build a strong, healthy company culture as a foundation for the customer experience.
According to Ford, you need three main things to be customer-centric, starting with ensuring that you are hiring people who are ‘smart-to-start.’ To perpetuate a healthy culture, you need to have the right people on your team to carry the torch. Once you have the right people on your team, they need to go through a productive and informative training process. Finally, you need to equip and empower your team members to make the best decisions for the organization and the customers.
“I think the empowerment issue is one of the next big steps of a customer-centric culture,” she said. “That team member needs to be empowered to make decisions on behalf of the organization and the customer. If we’ve hired well and trained well, they can do that. If we haven’t, they’re not going to be able to make a decision that balances the needs of the organization and the customer.”
In the end, it comes down to leadership. Leaders must set the tone for the rest of the organization – leaders should be able to meet any of the expectations that they have for the rest of the business. “You cannot expect people to be more than you are. You have to make certain that you are modeling it and keeping it on the agenda. You need someone who champions it at the leadership level.”
MacGill’s Legacy: Supporting the School Nurse
How one independent distributor partners with school nurses to meet evolving challenges in student care.
 For three generations, MacGill has been dedicated to one customer above all others: the school nurse. From adhesive bandages to vision and hearing screening equipment, the company has carved out a highly specialized niche, serving K-12 schools nationwide. It is a role Jay Smith, MacGill’s president, embraces with pride, and one that continues to evolve as the health needs of students change.

“School nurses are unique,” Smith explained. “They’re the highest-ranking medical professional in the building, yet they’re often working completely on their own. They don’t have a team of peers in the way teachers do. They’re responsible for everything from minor scrapes to managing complex health needs. Our job is to make their lives easier.”
That mission is rooted in family tradition. Smith’s grandfather first entered the market decades ago, at a time when
school nurse organizations were just beginning to form. Before that, he recalls, his grandfather had little choice but to attend superintendent and principal trade shows, hoping to reach the decision-makers who might eventually pass his catalog along to a nurse.
“When school nurse associations started holding their own trade shows, it was a game changer,” Smith said. “For the first time, we could talk directly to the people we were trying to serve. My family has been

attending those events for 50 years now. That history shapes everything we do; we’ve always had a nurse-first approach.”
The role of today’s school nurse
Part of what makes the school nurse such a vital yet underappreciated figure is how many enter the field from other areas of nursing. According to Smith, the vast majority, “90 plus percent,” start their careers in hospitals, pediatric offices, or emergency rooms before transitioning to school nursing, often for family reasons.
“When they arrive, they suddenly face challenges they’ve never encountered before,” he said. “Vision and hearing screenings for hundreds of students. Budgeting. Extensive documentation. And then balancing the medical needs of students with the fact that school isn’t a healthcare setting, it’s an educational one. It’s a completely different world.”
That world became even more complex during the pandemic, when school nurses were thrust into new responsibilities overnight. Social distancing, hygiene protocols, and student health monitoring all fell largely on their shoulders. “Health became front and center,” Smith said. “And because it was a health issue, people turned to the nurse. They were expected to figure it out.”
Beyond the pandemic, the long-term trend has been a steady increase in the complexity of student health needs. Children with chronic conditions like asthma, autism, immune disorders, and severe allergies are now more often enrolled in
mainstream schools. For nurses, that means greater responsibility and more reliance on trusted suppliers like MacGill.
Family-owned and independent
MacGill remains a family-owned, independent distributor, and Smith says being part of IMCO, a cooperative of independent medical distributors, has been critical to its success.
“IMCO helps us vet vendors,” he explained. “We’re a small company in a niche market, and I can’t spend all day evaluating cold calls from vendors. But if IMCO has worked with them, I know they’re legitimate. That gives us confidence and saves us a tremendous amount of time.”
Smith’s own journey into leadership came naturally, though not by design. Growing up, he worked summers in the business, helping process the seasonal rush of orders schools place in preparation for fall. Later, when his father began sharing the challenges of running the company, Smith realized he could help.
“I didn’t step in planning to take over,” he admitted. “I just thought, I can contribute. Over time, I became more of a translator and a helper, and eventually the leader. It wasn’t the plan, but it felt right.”
Staying true to the mission
Unlike many companies that look to expand aggressively into new sectors, MacGill has consistently chosen to remain focused on school health. While they have explored adjacent markets like municipalities and first

“ The lice comb works because it’s tied directly to what school nurses deal with every day. And it doesn’t distract us from our core business; it complements it.”
responders, Smith says the company always arrives at the same conclusion: “We don’t want to change who we are. We like being the school nurse experts. That’s where our value lies.”
One area of growth that does fit seamlessly with the company’s mission is its development of the WelComb, a specially designed lice comb. Head lice remain a common issue in schools, and nurses are typically the first to diagnose it. MacGill not only markets the product to nurses through its catalog but also sells it through retailers like Dollar General, with ambitions to expand into more large chains.
“The lice comb works because it’s tied directly to what school nurses deal with every day,” Smith said. “And it doesn’t distract us from our core business; it complements it.”
Carrying the tradition forward
At its heart, MacGill is less about products and more about relationships. By staying close to school nurses and listening to their evolving needs, the company has built trust across generations. Smith credits that consistency to his grandfather’s and father’s vision, but also to the nature of the nurses themselves.
“They’re great customers,” he said. “They’re dedicated, hardworking, and they’re dealing with unique challenges every day. We just try to be the partner they can rely on.”
For Smith, that is both a responsibility and a privilege. “I grew up around this business. I saw how much it mattered to my family and to the nurses we served. Now, it’s about carrying that forward. We exist to make a school nurse’s life easier. And if we’re doing that, we’re doing our job.”
Better Health Better Future




From Cross Dock to Community Board
The many roles of McKesson’s Mike Bird.
By Pete Mercer
 Mike Bird is a delivery professional lead at McKesson Medical-Surgical, one of the largest distributors of medical supplies in North America. His team operates out of a cross dock, which is a location that receives finished orders from McKesson’s distribution center in Lehigh Valley. His team of eight delivery professionals delivers products throughout the state of New Jersey.
Repertoire Magazine sat down with Bird to discuss his career at McKesson, taking charge of a leadership role in his community, and the bigger picture of working in the healthcare supply chain.
Building a career at McKesson
Bird has worked for McKesson for just over 12 years (he hit his 12-year anniversary in July) and has held his current position for the last five years. While most of his time is spent organizing the schedules and routes of his team of drivers, he also has plenty of opportunities to make deliveries to help keep up with the sheer volume of products moving through their cross dock.
McKesson is driven by two core principles: ILEAD and I2CARE. ILEAD is a leadershipbased acronym that stands for Inspire, Leverage, Execute, Advance, Develop, with the core idea being that everyone is a leader and all employees are committed to leadership excellence. I2CARE is an acronym that stands for Integrity, Inclusion,

Customer-First, Accountability, Respect, and Excellence, which are foundational values of the way that McKesson operates.
Both core principles are a part of the everyday fabric of working for McKesson, inspiring employees like Bird to be the absolute best that they can be. “It’s a company culture, decisionmaking, how we lead, and it’s a whole standard.”
He said, “The ultimate goal is to service our customers, our patients, and these hospitals and doctor’s offices from every
aspect of medical that you can think of – oncology, pediatricians, OBGYNs, surgery centers and more. We deliver everything from prescription drugs, vaccines, medical equipment and disposable items.”
Bird worked as a full-time delivery professional before he became the team lead, so he understands the needs and challenges facing the delivery professionals throughout the day. They offer white glove delivery services, which goes an extra step to ensure that customer service is the number one priority with each delivery.
For Bird, those relationships are foundational to one’s success as a delivery professional. It can be a physically demanding job, especially during the winter and summer months, but he says that it’s “not the hardest job in the world.” The best delivery professionals are the ones who stay safe on the road and provide excellent customer service, especially because they represent the company and build relationships with the customers.
Mike Bird
“Once you load that truck, it almost becomes your own little business,” he said. “You deliver to the same customers, so you build a relationship with them because you’re seeing them on a frequent basis.”
The bigger picture
A unique thing about the healthcare industry is this idea of a bigger picture: everyone has an understanding that even the slightest slip up can have dangerous consequences for patients. While it’s easy to look at

distribution as another job, Bird and his team understand that they shoulder a greater purpose to serve the clinicians and the patients.
There are plenty of times when Bird’s facility will get an email informing them of something important coming in the next day, which means that he might have to restructure his driver’s route to make sure it gets where it needs to go when it needs to be there.
“That’s not always the easiest thing,” he said. “One of our mottos is ‘what we do matters.’


Sometimes, it could be just a couple boxes of gloves. Other times, it could be something critical for a patient. But for us, we treat each package with the same level of care and importance.”
This is an industry where every touchpoint holds tremendous importance. If you order something from Amazon and it gets delayed by a day or two, it’s not the end of the world. But any delays for the kinds of products that McKesson is shipping can cause a dangerous domino effect, making the work at cross docks like the one Bird manages an integral piece of a greater puzzle.
Developing a necessary skillset
As a leader, Bird has considerable insight into the finer details of the job. In his 12 years working for McKesson, he said that one of the biggest lessons he’s learned is to be a better driver. Much like Bird’s approach to management and leadership, this is a very practical look at how McKesson has shaped him in his career – there is an entire program devoted to ensuring that delivery professionals are prepared and equipped with the training and resources they need to be successful on the road.
This experience has trickled down into his life outside of work as well. He taught his niece how to drive using the principles of the PACE program to discuss things like maintaining an appropriate space between you and the car in front of you, stopping a safe distance away from the car in front of you so that you can see the back of their tires, and a concept known as “stale green
lights.” For most other drivers on the road, when they see that the light is green, they take the opportunity to keep driving through the intersection. For Bird, if he doesn’t see the light turn green, his instincts kick in to remind him that the green light might as well be a ticking clock. Eventually, that light is going to turn yellow and a good driver needs to be prepared for that.
When you have a vehicle full of precious medical supplies that are due at a facility in a timely manner, it makes you more cognizant of the nuances of driving for a living. This practical outlook at even something as seemingly commonplace as a traffic light is what makes Bird stand out as a leader for his team. By focusing on those kinds of details, he and his team are able to deliver better results for McKesson and their customers.
Hometown pride
In addition to his role at McKesson, Bird also serves on the Willingboro Township School Board, where he was just re-elected for another three-year term. Willingboro is the township that he grew up in, where he went to elementary school and graduated from high school. Bird has a deep sense of pride for where he’s come from and leverages that pride to serve on the school board and meet the needs of his community.
Public education is important to Bird, which is why he’s so heavily involved. Not only did he benefit from the education he received, but his son (who has earned a doctorate from the University of Hawaii) also benefited from public education. Part of the reason that he’s involved in

this capacity on the school board now is because he has first-hand experience of what a good education can do for people.
This is a volunteer role that Bird is deeply passionate about, giving him the opportunity to give back to the community that he grew up in. “This little suburb in South Jersey is more important to me than almost anything else, aside from my kids and new fiancé, and I treat it as such. It’s an honor that when I get stuff done and people say, ‘Thank you for doing that.’”
Bird joked that people are asking when he’s going to run for mayor, which speaks to his involvement in the community. When he’s not on the clock at McKesson, he’s working to enrich his community through his volunteer work, whether that’s attending school board meetings, running fundraisers for the
schools, coaching basketball, giving out scholarships through his nonprofit, or any one of the other hats he’s accustomed to wearing.
There’s a deeper generosity there that goes beyond a customercentric outlook or hometown pride – Bird understands the value of community and why an investment in that community is worth all the time and dedication that it takes. That investment makes him an invaluable part of the community in Willingboro, giving him a reputation for his dependability.
“There’s only a couple of people on Earth that call me Michael,” he said. “Most people will say, ‘Mike Bird.’ It’s one word, eight letters long. They just say, ‘Hey Mike Bird,’ because they know I’m going to show up. I’m going to do everything I can to support my community. When I see a need, I’m going to find a way to fulfill that need.”

Atellica CI Analyzers
Every healthcare system feels the pressure to handle more. More volume, more administrative burden, more staffing challenges. With the Atellica systems, our goal is simple: less. Because when your staff spends less time on manual work, they’re free to spend more time on human work.

siemens-healthineers.us/atellica-configurations

Scan to watch your 2-Minute Drill on the Atellica CI Analyzer
Dedication in Motion
How Julio Chavarria and NDC’s warehouse team keep the supply chain running.
 Julio Chavarria’s career has been built by working in a supply chain culture with high expectations: orders must go out on time with high quality standards, while simultaneously managing costs and prioritizing warehouse safety.
“After more than 10 years with NDC and in various warehouse roles from packing, picking and sweeping the floor – I can honestly say that no two days are the same,” said Chavarria, Senior Manager of Continuous Improvement Operations at NDC, Inc.
The job of warehouse employees often requires long hours in a variety of weather – the facility can be hot in the summer and cold in the winter – and employees spend the day on their feet, lifting and moving heavy product.
Though Chavarria says supply chain warehouse work can at times be mentally and physically demanding, the reward of getting essential products to healthcare providers and their patients keeps him and his team dedicated and focused.
“One of the greatest challenges of the job is also one of the most rewarding: adapting quickly when priorities shift,” said Chavarria. “Urgent requests come in, and it’s our job to respond immediately while maintaining the same high quality and accuracy.”

Much more than boxes
Many do not realize just how much detail and energy goes into fulfilling each product in a warehouse order.
From carefully tracking inventory and supply to picking, packing and preparing for shipment, Chavarria and his team go above and beyond to build each pallet of product.
“It’s not just about moving boxes, it’s about protecting the product, packaging it with care and making sure every shipment meets our quality standards,” said Chavarria. “It is also a team effort that requires constant communication and collaboration across different functions.”
While the people working in the warehouse aren’t on the front lines of healthcare, the work that they do directly impacts both patients and providers.
“We don’t go home until our work is done – what we are doing today is critical to keeping the supply chain running, and cannot be pushed to next day,” said Chavarria.
A team effort
For Chavarria, a strong relationship with his warehouse team is essential to ensuring overall smooth operations and productivity at work.
Julio Chavarria


“I start every day by connecting with my team – making sure they have what they need to succeed and encouraging them to give their best,” said Chavarria. “I interview every new warehouse hire personally to make sure they understand exactly what the job entails so they know what to expect from day one.”
it takes to get the work done,” said Chavarria.
Right products to the right place
Each function of the warehouse, from receiving, picking, packing and shipping work cooperatively to complete a common goal of fast, quality distribution.
“ We communicate between teams directly, make a plan and focus on resolving the immediate need while also learning from the situation to prevent it from happening again.”
Even in the most challenging of circumstances, the warehouse team must come together to ensure the supply chain continues to run.
“During the height of COVID-19, our team came in every single day – with no workfrom-home option – knowing how essential our role was,” said Chavarria. “We worked long days, often with fewer people, but we never let that slow us down.
“We didn’t take even one day off during the pandemic, and we kept moving product so that providers and patients could get what they needed,” Chavarria continued. “Looking back, I’m proud knowing there are families we helped during one of the most challenging times in healthcare.”
The unyielding dedication of NDC’s warehouse team is key, ensuring that the company meets evolving customer needs and delivers on its mission.
“No matter what comes our way, we adjust, adapt, and do what
“Each function plays a critical role, and success depends on clear communication and mutual respect,” said Chavarria. “We all share the same goal: getting the right products to the right place, on time.”
When there is a delay, shortage, or urgent need within the supply chain, Chavarria relies on strong connections with other teams at NDC to quickly communicate and figure out a solution.
“Relationships are key. When challenges arise, we come together to find solutions and make it happen,” said Chavarria. “We communicate between teams directly, make a plan and focus on resolving the immediate need while also learning from the situation to prevent it from happening again.”
At this point in his career, Chavarria has had extensive experience in his role and has now been given the opportunity to be a mentor and help others grow.
“Our team has worked hard to create an environment where members are encouraged to learn new skills, take on responsibilities and think beyond their current role. Seeing people I’ve coached go on to become supervisors, managers and leaders has been one of the most rewarding parts of my career,” said Chavarria.
At NDC, a culture of mentorship and coaching helps each team member perform at their very best, directly strengthening both distribution and the overall performance of the business itself.
“It’s not just about the impact we make on the healthcare supply chain – it’s about the lasting impact on individuals, their families, and their futures,” said Chavarria. “Knowing that our work improves patient care while also helping people grow professionally makes me proud every single day.”
Chavarria, too, is inspired by his wife and two boys, who motivate him to approach his career and the supply chain with purpose.
“My personal motivation is my family and the job that we do because what we do every day impacts someone’s life. We’re not shipping consumer goods like computers or shoes –these are supplies that might be used to treat someone’s grandmother, a child, or a spouse,” said Chavarria. “I think about my own family, and how much it would mean to know someone was working hard behind the scenes to help them. That perspective keeps us all focused on the bigger picture.”
No Missed Commitments
NDC’s Michael Price on resiliency in distribution.
 A career in the medical device supply chain is fast-paced and dynamic, requiring professionals to quickly adapt to changing demands.
As the Senior Director of Operations at NDC, Inc., Michael Price’s knows this well. His role is to understand where people need to be in the warehouse, what resources are essential and how the company can meet each one of its commitments before the day ends.
Price’s primary focus is in support of the NDC’s mission to be a trusted partner in efficient healthcare delivery by managing an effective supply of products and equipment.
“This business is niche, and no one else does what we do at the scale we do it, which means there’s no playbook to follow – we’ve built our own, and we improve it every day,” said Price.
With a large volume of orders to fulfill each day, keeping the supply chain running smoothly means always knowing how to be resilient and adapt as a director.
“Balancing the hundreds of pallets shipped and received daily, with the need for accuracy and timeliness, requires constant coordination,” said Price. “We must be agile enough to flex resources based on the day’s needs while keeping a clear focus on quality.”
“The mindset each day is the same: pivot quickly, solve problems, and get supplies where they’re needed most,” said Price.

No missed commitments
During the height of the pandemic, Price says the supply chain faced daily disruptions, but his team persevered and found creative and innovative ways to keep operations running.
“Our team has faced multiple emergency situations without missing a beat,” said Price. “During the COVID-19 pandemic, we fulfilled customer needs every
single day – no closures, no missed commitments.”
The distribution site where Price and his team work in Nashville, Tennessee, has also faced two significant snowstorms in the past two years, threatening the site’s ability to carry out daily operations. Price’s team, however, acted quickly before the snow came in both times, and were able to
Michael Price
remain open and shipping product despite the bad weather.
The distribution site itself in Nashville is no small operation – is moves millions of pieces and products to NDC members each year, providing healthcare organizations with critical medical supplies daily.
“Behind the scenes, our shipping volume requires constant ‘dive and catch’ moments to meet urgent needs, a level of teamwork that extends far beyond one person and a deep commitment to making sure no order leaves incomplete,” said Price.
Communication and alignment
Managing a successful supply chain all comes down to communication and alignment across teams, says Price.
“From the moment product arrives to the moment it leaves our dock, every function has a clear role and a shared goal: delivering the perfect pallet on time,” said Price. “Daily standups keep us connected, allow us to quickly solve issues and ensure resources are exactly where they need to be.”
Price and his team navigate any challenges by dealing with them head-on, demonstrating a proactive approach to supply chain operations that prioritizes transparency and efficiency.
“When an issue arises, we quickly assess the impact, bring the right people together, and make a plan to resolve it,” said Price. “Strong relationships across teams, and with our partners, mean we can move fast, adjust priorities, and still meet customer expectations.”

“When an issue arises, we quickly assess the impact, bring the right people together, and make a plan to resolve it. Strong relationships across teams, and with our partners, mean we can move fast, adjust priorities, and still meet customer expectations.”
Price and his team keep the end-users (the patients and healthcare providers) in mind as motivation throughout the everyday process of distribution work.
“Every product that leaves our building is destined to help someone. That awareness drives our commitment to accuracy, speed, and quality,” said Price.
“We know we’re not just moving pallets; we’re making a difference in the healthcare supply chain, and ultimately in people’s lives.”
The tools for success
Today, Price is responsible for 113 families – NDC’s associates – and ensuring they have the tools, training and environment to succeed.
“I’m proud every time I see our team rise to a challenge. When I started in 2015, the business was very different – departments were siloed, and processes
needed alignment,” said Price. “Over the past decade, we’ve worked hard to break down those silos, strengthen collaboration, and double the size of the business in seven years.”
NDC has worked to build a culture in which delivering for the customer is a top priority for each employee. The company’s overall mission is to rely on people, integrity and service to provide a competitive advantage to its partners in the healthcare supply chain.
“We’ve built a culture where delivering for the customer is non-negotiable, and where people take pride in their work because they know the impact it has,” said Price. “Watching the transformation of our operations and the dedication of our people has been one of the most rewarding experiences of my career.”


In Harmony
The importance of finding balance with space, workflow, and technology in the patient setting.
 For decades, healthcare organizations have wrestled with the inefficiencies that come from disconnected systems, equipment, and processes. Exam rooms often function as patchwork spaces, where cabinetry, diagnostic devices, and digital systems operate in silos. While each tool serves its purpose, the lack of integration can leave providers juggling technology rather than focusing fully on patients.
Midmark is working to change that. By reimagining the point of care as a single, interconnected ecosystem, one where clinical space, workflow, and technology are designed to function seamlessly together, the company aims to transform both the patient and caregiver experience. Tracy Timmerman, Director of Marketing, Medical, Midmark, recently spoke with Repertoire Magazine about this evolving vision.
A holistic view of the exam room
Timmerman explained that the Midmark perspective comes from decades of direct observation inside healthcare environments. “Our teams consistently saw that the exam room is not just a place,” Timmerman said, “it’s where patient experience, caregiver efficiency and clinical outcomes intersect.”
Historically, equipment was viewed in isolation. Furniture, cabinetry, and diagnostic devices were designed separately. By studying the point of care as a unified ecosystem, Midmark recognized that harmonizing these elements could unlock greater value.

That value takes many forms: streamlined workflows that reduce caregiver friction, enhanced infection control practices that support safety, and environments that help create calmer, more dignified experiences for patients. In essence, integration allows caregivers to focus on people, not technology.
Rethinking the basics
One of the company’s biggest insights came from reframing cabinetry and diagnostic devices. Instead of treating them as secondary tools, Midmark recognized them as the backbone of clinical workflow.
For cabinetry, modularity, proper ergonomics, and infection prevention were guiding principles. Supplies and equipment needed to be within easy reach, while surfaces had to withstand rigorous cleaning protocols.
For diagnostics, connectivity became the central theme. Manual data capture slowed care, introduced errors, and distracted caregivers from patient interaction. By enabling connected devices that integrate directly with electronic medical records (EMRs), Midmark helped remove that burden.
The voice of the caregiver
Frontline caregiver feedback has been pivotal to this evolution. Nurses highlighted frustrations with vital signs workflows, while physicians emphasized the need for adaptable spaces that keep supplies at the point of care.
“Caregivers told us clearly: their time is divided between technology, charting and patient interaction,” Timmerman said. “They want more seamless workflows that allow them to focus on people, not equipment.”
That feedback directly shaped Midmark designs. Ergonomically designed cabinetry reduces strain. Connected vitals acquisition
Tracy Timmerman
improves efficiency, reduces errors, and enhances care. Exam spaces are structured to streamline workflow, ensuring providers spend less time navigating equipment and more time engaging with patients.
Yet integration is not without hurdles. According to Timmerman, the most common challenges organizations face with diagnostic connectivity include EMR integration, inconsistent workflows across platforms, and ensuring consistent use through staff training. Connectivity only delivers value if caregivers adopt it fully, which makes change management as important as the technology itself.
Durability meets flexibility
Balancing durability, infection control, and flexibility is central to the Midmark approach. Cabinetry is constructed with medicalgrade materials designed for daily demands, with seamless surfaces that are easy to disinfect.
At the same time, modular designs allow clinics to adapt quickly. Healthcare systems have reported that modular cabinetry enabled them to expand, repurpose rooms, or adjust workflows without costly downtime.
“Instead of full tear-outs, they could reconfigure components overnight or over a weekend, allowing services to continue with minimal interruption,” Timmerman said. “This adaptability has proven especially valuable during rapid growth periods or unplanned events such as pandemic-related space reconfigurations.”
Measuring success
How does Midmark measure whether its connected ecosystem
is working? Timmerman identified three categories:
Clinical efficiency: reduced vital signs capture time, faster room turnover, fewer manual charting errors.
Caregiver experience: improved staff satisfaction, reduced ergonomic strain, lower training burden.
Patient outcomes and perception: higher satisfaction scores, shorter appointment lengths, and stronger engagement.
supporting both in-person visits and remote consultations.
Patient-facing technologies will play an expanding role as well. Digital intake tools, at-home wearable sensors, and AI-enabled self-directed care platforms are no longer just conveniences. They are becoming vital parts of the care journey.
“Innovations such as these will continue to expand the definition of the connected ecosystem where physical and
The company is exploring AI-driven insights to identify clinical risks and flag anomalies in diagnostic testing. Telehealth and hybrid care models are also influencing design.
In one case study, clinics that adopted Midmark integrated exam chairs, diagnostic tools, and EMR connectivity saved an average of 69 seconds per patient encounter. Over a day, that translated into more patients seen, without sacrificing time for meaningful interactions. At the same time, infection prevention improved, staff strain decreased, and patient satisfaction rose.
Looking ahead: The next 3–5 years
The Midmark vision for the future builds on trends shaping the industry: intelligence and interoperability. The company is exploring AI-driven insights to identify clinical risks and flag anomalies in diagnostic testing. Telehealth and hybrid care models are also influencing design. Tomorrow’s exam room may need to function physically and virtually,
digital ecosystems are unified and synergistic to modern care management,” Timmerman said.
Patient-facing tools are rapidly becoming an extension of the point of care. Tablets, mobile check-ins, at-home wearable sensors, self-directed care enablement via agent AI tools and digital intake forms not only reduce administrative burden but also empower patients to participate actively and directly in their own care.
“Within the Midmark vision, these technologies will be integrated into the workflow and care environment,” Timmerman said, “ensuring that the caregiverpatient interaction remains personal and engaging, while digital tools enhance transparency and engagement to deliver entirely new clinical point of care insights that drive better outcomes and improve team efficiency.”

Lab
The Future of Lab Medicine
ADLM President Paul Jannetto, Ph.D., says the next five years will bring sweeping changes to diagnostics, but sustaining progress requires policy reform and a stronger workforce.
This summer in Chicago, thousands of laboratory medicine professionals from around the globe gathered, not merely to exchange ideas, but to signal the next frontier in how we think about, develop, and deploy diagnostic science at ADLM 2025.
Speakers, panelists, exhibitors and attendees discussed the challenges and opportunities ahead. What emerged was more than a crossroads – it was a turning point. Clinical laboratories are becoming centers of translation and intervention, deeply intertwined with data science, environmental health, and patient-centric care.
Among the emerging trends and technologies, artificial intelligence and point-of-care testing are particularly poised to redefine the future of laboratory medicine, according to Dr. Paul Jannetto, president of the Association for Diagnostics & Laboratory Medicine (ADLM, formerly AACC).
Speaking with Repertoire Magazine following the ADLM 2025 meeting, Jannetto highlighted how these technologies, coupled with growing demand for personalized medicine and rapid diagnostics, will shape the next decade of clinical laboratory practice.
AI’s expanding role in the lab
Artificial intelligence and machine learning are still emerging in laboratory medicine, but the technology is already demonstrating its value. “Laboratory experts are beginning to use AI and machine learning to determine diagnoses and identify possible outcomes to treatment more quickly, which in turn could lead to higher quality patient care,” said Dr. Jannetto, who also serves as professor of laboratory medicine and pathology, vice-chair of practice laboratory medicine, and co-director of several specialty labs at Mayo Clinic in Rochester, Minnesota.
He pointed to recent breakthroughs as proof of AI’s promise. “For example, a few years ago, researchers from the University of Michigan developed and implemented a machine learning test called ThioMon to guide treatment of inflammatory bowel disease (IBD) with azathioprine. Although azathioprine is much cheaper than other IBD medications (which can cost thousands of dollars a month), its dosage requires finetuning for each patient, making it difficult to prescribe. ThioMon solves this issue by
analyzing a patient’s routine lab test results to determine if a particular dose of azathioprine works or not.”
AI is also improving infectious disease detection. “Even more recently, a blood test for Lyme disease was unveiled at ADLM 2025 that was developed with the help of AI,” Dr. Jannetto said. “The test identifies Lyme disease sooner than the current standard test and is also more accurate. Both its sensitivity and specificity are over 90%, compared to traditional Lyme testing, which detects the disease accurately only 30% of the time. With these capabilities, the new test could significantly improve patient outcomes. The researchers hope that the test, which works on standard laboratory equipment, will be commercially available by the end of 2026.”
at-home tests, using them to make critical decisions about travel, personal/social interactions, and other behaviors. This, in turn, has increased trust in at-home testing across the board, which has also increased demand for it.”
The implications for clinical labs are significant. “A big positive of this is that more at-home testing means increased patient access to testing – something that ADLM strongly supports. Expanding the use of at-home tests could also help to alleviate the burden on clinical labs in the U.S., which have been shortstaffed for years,” Dr. Jannetto said. “This is likely the biggest impact that point-of-care testing could have on the traditional lab model in the near future: It could free up time for lab professionals to focus more on tests that require
Under current law, more than 800 lab tests could face payment cuts of up to 15% beginning in 2026 due to flaws in Medicare’s rate-setting process.
The shift toward at-home testing
If AI represents the cutting edge of diagnostics, point-of-care testing reflects a shift in how patients access lab services. Dr. Jannetto noted that the most important change in this space has been cultural, not technological. “During the COVID-19 pandemic, the widespread use of point-of-care testing reshaped the public’s expectations for medical testing,” he explained. “Point-of-care testing offered convenience, privacy, and speed of results from home. The public and healthcare providers came to really trust results from
specialized training and equipment and that must be done in a core lab setting.”
At the same time, he cautioned against overreliance on at-home results. “Of course, increased athome testing comes with downsides, too. Some at-home tests may not be as reliable as testing that is performed in clinical laboratories. And as with all diagnostic testing, another big challenge in interpreting an at-home test result is to not rely solely on that result to make a diagnosis. The test result counts of course, but clinical context must always be carefully considered when acting on any test result. We
at ADLM do advise patients who are using at-home tests to consult with their healthcare providers and evidence-based guidance when interpreting the test results.”
Personalized medicine and rapid diagnostics
The shift toward individualized care is also driving laboratory innovation. “As the healthcare field as a whole continues to work toward making personalized medicine a reality, clinical labs have been taking a more individualized approach to diagnosis and disease management,” Dr. Jannetto said. He pointed to chronic kidney disease management as one example: “Clinical guidelines now recommend that labs use validated, lab-based equations that predict kidney-failure risk as an integral part of chronic kidney disease management. This approach enables labs to assess each patient’s individual risk of disease progression, which in turn enables clinicians to make more precise treatment decisions.”
Rapid testing, particularly in infectious disease management, is another frontier. “Phenotypic antibiotic susceptibility testing (AST) is one particular area where rapid testing is taking off,” Dr. Jannetto said. Traditional AST can take up to 48 hours – far too long for patients in septic shock. “Rapid AST could therefore play a major role in enabling patients to get timely, effective treatment for serious infections while also minimizing the potential for widespread antibiotic resistance.”
Persistent challenges: staffing and reimbursement
Despite these advances, laboratories continue to face structural
challenges. “Staffing shortages remain a consistent issue for clinical laboratories and are one of the biggest operational challenges that labs face today,” Dr. Jannetto said, citing studies that show vacancy rates as high as 25% in some regions and an aging workforce nearing retirement. “These surveys show us what many laboratories are grappling with, which is that an insufficient amount of newly trained technologists are entering the field, while previous generations of laboratory medicine professionals are retiring at historic rates.”
Reimbursement pressures further complicate the picture. “Adequate Medicare reimbursements play a crucial role in helping
laboratories remain financially viable,” he explained. “This is especially true for the outreach labs that serve rural and underserved communities, and that tend to operate with thin profit margins.”
The stakes are high. Under current law, more than 800 lab tests could face payment cuts of up to 15% beginning in 2026 due to flaws in Medicare’s rate-setting process. “If this happens, more than 800 laboratory tests will be subject to payment cuts of up to 15%, which could hinder patient access to routine and life-saving tests,” Dr. Jannetto warned. He expressed optimism about recent bipartisan efforts to fix the process: “Thankfully, a new
piece of bipartisan legislation –the Reforming and Enhancing Sustainable Updates to Laboratory Testing Services (RESULTS) Act – was recently introduced in Congress. This legislation would ensure that the Medicare CLFS rate-setting process is based on up-to-date, comprehensive data representative of all clinical labs.”
For Dr. Jannetto, the message is clear: innovations in AI, pointof-care testing, and rapid diagnostics hold enormous promise, but sustaining progress requires policy support and a strong workforce. The future of laboratory medicine, he said, depends on balancing technological breakthroughs with practical realities.
TOSOH BIOSCIENCE
Empower Your Lab
IMMUNOASSAY ANALYZER
18-minute result turnaround time
Allows result reporting during the visit
Wide dynamic ranges


Delivers high-sensitivity results for proper patient care
90-day calibration stability
Reduces cost, time and calibration frequency
Biotin-free immunoassay designs
Minimizes the risk of false lab test results
Unit dose test cup dry reagent technology
One test, one cup ensures minimal reagent waste leading to increased efficiency and cost savings

Available in Four Configurations for Labs of All Sizes and Workloads

Physician Office Lab
The Infections You Can’t See — and How to Find Them
From sexually transmitted infections to tick-borne diseases, the complete blood count has become a frontline tool in modern diagnosis and treatment.
In the Repertoire September 2025 Physician Office column “Hidden Dangers,” we looked at infections that do not present obvious physical symptoms and how the complete blood count (CBC) can come to the rescue and uncover these hidden dangers.
In this column, I intend to point to the history of diagnosis and treatment for these infections, and how we have just barely managed to make progress in uncovering and treating them. The complete blood count and microbiology will take center stage as we look at

By Jim Poggi

advances in diagnosis of infection and appropriate treatment. This column will also provide concrete evidence that ‘it can happen here,’ giving you a way to counter a common customer objection –especially when it comes to sexually transmitted infections (STIs). Let’s start by looking at the past.
The “germ theory of disease” is discovered
Think back to a time long ago, before your grandparents were born. Our ancestors were still a bit furrier than today. They lived in trees and often fell out of them. Dogs were not yet domesticated.
There were infections even then, mostly obvious ones related to injuries from predator bites and falling out of trees. They were diagnosed by the sore red area and associated inflammation.
What did our ancestors do? They rubbed various plant-derived substances on the affected area and hoped it would go away. Sometimes it worked, sometimes we lost a member of the clan. No one thought of infections they did not see. That was far less important than foraging for food and avoiding being the next meal for predators.
We have come a long way since then. We have left the trees
and finally domesticated dogs, or perhaps they have domesticated us. A very important move forward made a difference in our understanding and cure of infections, whether they were visible or not. Two pioneering microbiologists, Louis Pasteur and Robert Koch, proposed the “germ theory of disease” in the 19th century, which has been the cornerstone of our understanding of what causes an infection.
But, what to do about it? We were still rubbing various plantderived substances on the affected area until the first antibiotic, penicillin, was made widely available after World War II. While Alexander Fleming discovered penicillin in 1928, it took years for it to become widely available in developed countries. There are still gaps in availability of antibiotics in less developed countries.
How many annual infections occur in the U.S.?
As we fast forward to more modern times, what is the latest story on infections in the U.S., and should we be worried? The Centers for Disease Control and Prevention (CDC) reports an acknowledged total of about 110 million infections confirmed in 2023. They also acknowledge that there are any number of infections that do not go reported.
It is my assessment that many of these less serious infections are cured by rubbing or spraying plant derived substances (and topical antibiotics) on the affected area. Within this data, most infections are visible or at least obvious. Food-borne infections made up the largest group at 48 million, followed by respiratory infections annually ranging from
30 to 40 million. Not so obvious are STIs at 26 million. That leaves another 5 million difficult to diagnose enteric infections (appendicitis, pancreatitis, gall bladder rupture and peritonitis).
Overall, if our ancestors looked at the situation, they would observe that three out of every 10 infections did not exist since they were not visible or obvious. No wonder the mortality rate was not just comprised of predator attacks and falls out of trees. There were several causes that simply could not be acknowledged or explained. There was little that even the local shaman could do in this case.
Infections you can’t see
While the ability to identify obvious infections and to effectively cure them was vastly improved by the middle of the 20th century, what about the less obvious
internal infections our ancestors did not understand? How have they been diagnosed?
Sometimes it has been a simple matter of tracing the incidence of the spread of STIs from “patient zero” to their sexual partners. This was a common practice that began in the early 20th century and is still practiced today, especially as the variety of STIs and their incidence has increased.
But, there is a difference between suspecting a patient has an STI and being able to prove they have an STI. What to do?
CBC
and microbiology power diagnosis and treatment
Here is where the CBC and modern microbiology come to our rescue. The CBC can not only confirm that a patient has an infection, but it can also identify whether this infection is bacterial
While STIs are unfortunately on the rise, they are by no means the only infections that are not obvious. Enteric diseases (diseases of the gastrointestinal tract) can present with slowly increasing severity and many have similar symptoms.
Residual infections
One note on the utility of the CBC. Many diseases, most notably COVID, appear to be cured. Cough, fever, wheezing and obvious symptoms go away.
But sometimes there is still a residual infection. The data is just making it clear, but “long COVID” is now recognized as a disease itself. A CBC is an excellent means of follow-up for these patients for your customers to know for sure whether the infection has been cleared or whether further treatment is required.
or viral. This is a massive step forward, not just for effective patient treatment, but also for the practice and promotion of antibiotic stewardship.
Even if we do not consider enteric or respiratory infections, STIs alone can be caused by either bacterial or viral agents. Think of two STIs that are currently on the rise. Syphilis is caused by a bacterium and AIDS is caused by a virus. Treatment plans are entirely different for each of these organisms. So, the ability to determine whether the patient has an infection that is not obvious, and then to understand whether it is bacterial or viral, are fundamental underpinnings of infectious disease treatment in the U.S. today.
The CBC is the most effective means of making this determination. An increase in white blood cell count (WBC) is the first indication of an infection. Then it is important to identify whether an infection is viral or bacterial. That’s where the CBC differential comes into play. Typically, an increase in neutrophils, the most common WBCs, indicates a bacterial infection. An increase in lymphocytes more often points to a viral infection. An increase in eosinophils can point to an allergy and lead to a different path to diagnosis. While infections can be complicated, the CBC is not. In a minute or less the lab receives at least 11 different parameters that can point to general health concerns (hemoglobin and hematocrit are examples that may indicate anemia or a bleeding disorder) or an infection, with the WBC differential well established as the gold standard for initial screen for an infection.


As important, once a treatment program has begun, follow up with a CBC can demonstrate the effectiveness of the treatment.
Microbiology plays its part by identifying the specific etiologic agent and identifying which antibiotics are most likely to be able to treat it effectively if it is bacterial. The combination of CBC and microbiology is an effective “one-two punch” in identifying whether the patient has an infection that is not obvious, then taking the next step to identify the organism and the proper antibiotic treatment to effectively cure it. Advances in molecular diagnostic technology are rapidly improving the speed and accuracy of traditional microbiology methods of identification of these microorganisms.
STIs and other pesky infections
While STIs are unfortunately on the rise, they are by no means the only infections that are not obvious. Enteric diseases (diseases of the gastrointestinal tract) can present with slowly increasing severity and many have similar symptoms. The CBC can identify whether the symptoms are due to an infection or another cause such as reflux esophagitis and lead to further discovery to identify the specific cause.
Tick-borne illnesses including Lyme disease, babesiosis, anaplasmosis, ehrlichiosis and Rocky Mountain Spotted fever are spreading due to the expansion of their environment due to global warming. Most of these diseases start out in ways our ancestors would understand – as a sore, redinflamed bite. Eventually the soreness goes away, but the bacteria
remains in the patient’s system, and can cause serious systemic diseases over time. Not obvious, right? Not to the naked eye once the sore area clears, but a CBC as follow up to the infected bite can determine whether an infection is still present, or has cleared up all by itself, or by the patient successfully rubbing plant derived substances on it. Tick-borne illnesses are moving to larger areas of the U.S. and becoming more common as more Americans encounter the larger population of ticks outdoors. This presents a new challenge to the U.S. healthcare system and physician practices everywhere. The CBC as a follow up to tick infection is a sensible way to assure that these illnesses do not progress to serious diseases that are harder to cure effectively.
The payoff
So, where does all this lead us? As trusted consultants to our customers, we have no doubt presented the case for including the CBC in our customers’ arsenal of diagnostic tools. Some have agreed. Others remain unconvinced. Take the leap of faith and
present the information regarding infections that are not obvious and initiate the conversation again with customers that have not yet initiated CBC testing. Bringing along statistics on the significant growth of STIs, from those that are clearly associated with serious after effects to those that are not as clearly associated with significant morbidity and mortality.
At the end of the day, infections are all around us, whether they are obvious or not. Are your customers prepared to deal with them? They are if you have armed them with the information they need to understand the incidence and significance of infections they cannot see and have helped them to adopt the CBC.
What are you waiting for? Share this information with your trusted hematology manufacturer, make a list of your customer prospects and start making calls. After all, we have made a lot of progress since we left the trees, even though we continue to rub plant derived substances on many red, swollen areas.
There is plenty of more work to do. Get out there and help combat the infections you can’t see.
Further information
Scan QR code to view excellent CDC information.
For those who insist “it can’t happen here”, scan the NIH QR code. Depending on where you line up, figure 2-3 and 2-8 show very clearly that, yes, it can happen here.
IS IT COVID-19 OR THE FLU?
WHEN SYMPTOMS OVERLAP, CLARITY MATTERS.
BinaxNOW™ COVID-19/Flu A&B delivers rapid, reliable results for COVID-19, Influenza A, and Influenza B—all from a single, patient-friendly nasal swab. Results in 15 minutes help diagnose and treat in a single visit.
ONE SWAB, THREE RESULTS
COVID-19, Influenza A & B
NO INSTRUMENT REQUIRED
Ideal for urgent care and decentralized settings
STREAMLINED WORKFLOW
Simple procedure supports fast onboarding




Clinical Lab
The Changing Face of the Clinical Lab
From pandemic disruptions to the rise of molecular point-of-care testing, the laboratory market is undergoing rapid transformation. Today’s labs are becoming the backbone of a more distributed, technology-driven diagnostic ecosystem. For distributors, suppliers, and providers alike, these shifts bring both opportunities and challenges, from supply chain volatility and workforce shortages to new frontiers in wearable and home-based testing.
To explore these dynamics, Repertoire Magazine interviewed several members of the NDC Clinical Lab Advisory Council, including Jim Macholz of Atlantic Medical Solutions; Kevin Barefoot of MTMC; Rick Wilburn of Wilburn Medical USA; and John Cook, Douglas Harper, and Brad Thompson of NDC. Together, they discussed the formation of the NDC Clinical Lab Advisory Council, ongoing supply chain hurdles, the impact of emerging technologies and how the lab’s role in patient care is evolving.
Repertoire Magazine: What prompted the formation of the NDC Clinical Lab Advisory Council, and what were some of the initial goals you wanted to achieve?
Thompson: During the COVID-19 pandemic, our focus shifted heavily toward clinical lab products specific to the COVID market.


Roundtable panelists
Jim Macholz, President and CEO of Atlantic Medical Solutions in Charlotte, leads a distributor specializing in the non-acute space. His team focuses heavily on lab and point-of-care testing with a dedicated field sales force.
Kevin Barefoot, Director of Point of Care and Primary Care at MTMC. MTMC serves as a leading outsourced sales partner, representing a wide range of products from exam tables and gloves to point-of-care testing solutions.
Rick Wilburn, Founder of Wilburn Medical Supply, a trusted distributor of healthcare supplies and equipment.
John Cook, Vice President of Sales, Healthcare at NDC. Cook designs and executes innovative sales strategies, develops emerging leaders, and drives strategic growth initiatives.
Doug Harper, Capital Equipment Program Director at NDC.
Brad Thompson, Vice President of Supplier Management at NDC, is responsible for managing clinical lab supplier relationships and identifying new supplier prospects to expand NDC’s portfolio.
While we were selling a lot in that space, we lost focus on other areas of the business. About two years ago, Jack Stevens, our president and CEO, approached me about refocusing on the broader clinical lab category. From there, John Cook, Doug Harper and I put together a go-forward strategy that included the formation of the Clinical Lab Advisory Council. It has paid huge dividends – helping us bring on new suppliers and reestablish focus across the category.
Harper: The council was designed to be a collaborative, non-competitive forum where lab-focused suppliers and distribution partners could openly share insights on industry challenges, emerging products, and successes. It’s been a great way to learn from each other. Just this morning, I spoke with Kevin about an emerging product he’s excited about – it’s
those kinds of conversations that make the council so valuable. We now have 18 members: seven distributors with NDC, seven supplier partners, and four members of the NDC team. We meet quarterly in a virtual format and also gather in person once a year during our NDC Power of Partnership Exhibition, which is our national meeting.
Repertoire Magazine :
How would you describe the lab marketplace today?
Macholz: Bumpy. Supply chain issues continue to create barriers in point-of-care testing. Even now – well past the height of COVID – we’re seeing vendors already back-ordering COVID tests. It’s surprising, even shocking, considering we’re just at the beginning of the season. If you look at Australia, they had an early flu season, and it was a tough one. Now we’re seeing early signs here
that could point to the same, with vendors already struggling to meet demand.
Cook: Another factor is suppliers transitioning products that were introduced under Emergency Use Authorization (EUA) to full FDA 510(k) clearance. That shift is creating logistical challenges. They’re trying to work through existing EUA inventory while bringing 510(k)cleared products to market – but production isn’t always keeping pace. As a result, suppliers sometimes have to fall back on EUA products, creating uncertainty about availability. Over time, as more suppliers complete that transition, the situation should stabilize. But for now, it adds to the bumpiness you mentioned.
Demand can spike suddenly, then drop off just as quickly. If products have only six to eight months of shelf life, we can’t roll them into the next season. That creates risk for both distributors and manufacturers when it comes to maintaining adequate inventory without ending up with expired product.
Repertoire Magazine: What are some emerging trends or technologies you are watching?
Barefoot: One of the biggest issues we need to pay attention to is antimicrobial resistance (AMR). Too often, antibiotics are prescribed without proper diagnostic stewardship. That misuse fuels resistance, which could lead to as many as 10 million deaths annually by 2050 – surpassing cancer worldwide. Molecular point-of-care
If products have only six to eight months of shelf life, we can’t roll them into the next season. That creates risk for both distributors and manufacturers when it comes to maintaining adequate inventory without ending up with expired product.
Macholz: We also saw some “pretenders” enter the market during COVID – manufacturers that weren’t really specialists in pointof-care testing. Many of them have now exited, which has pushed more volume and pressure onto the true point-of-care specialists. That added strain on credible manufacturers contributes to the uneven supply situation we’re experiencing.
Thompson: That’s a great point. Another challenge is expiration dating. As a master distributor, we have to carefully manage inventory.
testing, especially rapid molecular isothermal technology for respiratory illnesses, is a key step forward. It allows for more accurate results, ensuring patients receive antivirals or antibiotics only when appropriate. Over time, broader adoption of these technologies will play a critical role in slowing AMR.
Thompson: Along those lines, we’re watching a new pointof-care molecular platform for sexually transmitted infections, expected in late 2026. It will be CLIA-waived and able to test for
chlamydia, trichomonas, gonorrhea, and syphilis, including resistance markers for gonorrhea. That could be a game changer in helping providers choose the right antibiotic treatment.
Cook: Another area to watch is wearables. There’s a startup in Melbourne developing a skin patch that could replace traditional blood draws, allowing lab testing through the skin. They recently secured $75 million in funding. More broadly, wearable biomarker technology is gaining momentum, with potential to identify and monitor conditions without requiring a doctor’s office visit.
Barefoot: That kind of technology could remove barriers for patients who delay lab work, something as simple as fasting for a blood test can discourage follow-through. Combining advances in wearables, molecular testing, and platforms that address AMR and STIs shows the direction we’re heading: faster, more accurate, and more accessible diagnostics.
Repertoire Magazine: Are you seeing a growing demand for pointof-care testing in the physician office space? And if so, how is it changing the way labs operate? Macholz: Yes, demand remains strong. Physicians want faster results so they can move patients through quickly but still ensure accurate diagnoses. We’ve seen some fatigue with at-home testing – patients are more likely to go back to their doctors for respiratory illnesses like flu and COVID. There’s simply more confidence in provider-administered tests than in swabs done at home.

Symptoms
don’t wait.

QUIDEL TRIAGE BNP Test – the only-CLIA waived BNP test on the market for whole blood testing in approximately 15 minutes.
QUIDEL TRIAGE Cardiac Panel – helps accurately diagnose with three biomarkers – CK-MB, myoglobin and troponin I.
QUIDEL TRIAGE D-Dimer Test - assess patients suspected of PE/DVT due to shortness of breath.
Contact QuidelOrtho to learn more today. Every minute counts.
QUIDEL™ TRIAGE ™ METERPRO™ System delivers rapid cardiac insights when lives depend on it.
Wilburn: The growing demand for rapid point-of-care testing (RPOCT) is reshaping how labs operate by shifting more diagnostic decisionmaking closer to the patient. Instead of being the sole gatekeepers of testing, central labs are adapting to a decentralized model where urgent, rule-in/rule-out results are generated at the point of care. This allows labs to focus their resources on more complex, high-throughput testing while supporting providers with quality oversight, connectivity, and test stewardship.
Labs are moving toward operational efficiency through molecular standardization. Health systems and clinics can now unify testing across labs and point of care, creating scalability, quality assurance, and system-wide harmonization. Labs are evolving into the central coordinators of a distributed diagnostic ecosystem, a key message for reps engaging health system leaders.
Barefoot: For respiratory illnesses such as Flu, Covid, Strep A, RSV, testing is definitely shifting into physician offices, especially pediatrics, where rapid molecular platforms are being adopted far more than a few years ago. For example with Strep A testing, a provider can now get a 2-minute positive result using a Waived rapid molecular analyzer. But for blood work, we’re seeing fewer phlebotomists in practices, so those samples are still going out to centralized labs.
Macholz: That’s right. And it varies state by state, largely because of insurance. Reimbursement policies heavily influence whether practices use molecular or rapid testing. In states where molecular isn’t well reimbursed, you see more reliance on rapid point-of-care tests.
Barefoot: Absolutely, POC testing is always increasing; however insurances could make it tough at the start for some smaller practices, especially private practices may not be negotiating molecular reimbursement rates and adding this higher fee to their negotiated private payer contract and managed care plans. Therefore, customers may stick with rapids. The problem is that insurers aren’t incentivizing molecular testing like they may incentivize A1C testing, etc. – even though it could save costs longterm by improving treatment accuracy and reducing antimicrobial resistance. If molecular was tied to quality measures, like diabetes or cholesterol management, you’d see broader adoption.
believe will redefine the lab’s role in the next five years?
Wilburn: Overall, that RPOCT is undeniably expanding, driven by strong market demand, expanding technology, and shifting healthcare models – moving testing from labs to clinics, pharmacies, homes, and beyond. The market is robust and evolving.
The next frontier is molecular diagnostics in the home. Extending lab-quality testing beyond the lab and clinic enables earlier detection, faster treatment, and more effective preventive care. For health systems and clinics, it empowers a continuum of molecular care across lab, point of care, and home without sacrificing quality.
Reimbursement policies heavily influence whether practices use molecular or rapid testing. In states where molecular isn’t well reimbursed, you see more reliance on rapid point-of-care tests.
Macholz: And patient behavior plays a role too. Parents, for example, often prefer the doctor’s office because they don’t want to swab their kids – or worry they’re not doing it correctly. That accuracy and confidence is a big driver of why we’re seeing patients pivot back to physician offices.
Barefoot: Right. Compliance is much higher when a provider collects the sample. Patients trust the results more – and that’s critical in shaping testing trends.
Repertoire Magazine: Are there trends in preventive medicine or personalized care that you
Cook: I believe with the rise of insurance, more corporations are pushing for preventive health programs in their organizations. This will lead to more preventative tests and visits for the lab market. This could also in turn have labs shift from reactive diagnostics (identifying disease after symptoms appear) to predictive analytics that inform preventive strategies and personalized treatment plans. I also believe that the lab-on-a-patch market will see tremendous growth and innovation in the next five years, resulting in labs changing the way they operate and POLs as well.
Closing Gaps in Care with At-Home Testing
How Cardinal Health is helping patients overcome barriers to preventive care by delivering diagnostic tests directly to their homes.
In an ideal world, all patients receiving healthcare would attend regular check-ups, take diagnostic tests when necessary, and follow up with clinicianrecommended treatments.
“However, the reality is that many circumstances can disrupt the intended flow of care from providers to patients,” said Steven Denman, Director, Laboratory Business Development and Gaps in Care Programs at Cardinal Health.
These are known as “gaps in care” or discrepancies between recommended healthcare best practices and the level of actual care provided to the patient.
Gaps in care are pervasive across healthcare and can undermine both the quality and equity of medical services. Examples of gaps in care include missed healthcare services recommended by a provider – such as a cancer screening – or a delayed follow-up visit with a doctor.

Additionally, many patients do not adhere to their prescribed treatments and skip or delay critical care for a variety of reasons, including language barriers, the inability to take time from work to see a doctor or transportationrelated challenges. These factors can also lead to gaps in care.
“Amplifying these common gaps are obstacles that patients experience across the U.S. healthcare
“ Because payers are scored on the value of care provided to their members, it is financially advantageous for them to employ solutions that aim to reduce and close gaps in care.”
system – including rising treatment costs, increased comorbidities, condition progression, complexities from later-stage diagnosis, and reduced quality of life,” Denman said. Noncompliance also places a major strain on healthcare resources, which can cost systems an enormous amount of time and money, as they’re often treating issues that could have been identified sooner through early detection.
The benefits of early detection and preventive care
Chronic diseases are at an all-time high in the United States. According to the Centers for Disease Control and Prevention (CDC), 60% of adults1 are living with chronic illness, and life expectancy, as a result, is dropping nationally. Early detection of disease is generally more cost effective than treating advanced disease states.
“Solutions that focus on early detection, routine screenings and lifestyle interventions can offer profound benefits to patients, providers and payers by identifying health issues before they become severe,” Denman said.
Preventive care services involve regular check-ups, health screenings, vaccinations and other lifestyle changes. Health-promoting
Steven Denman
activities such as stress management, good sleep and hygiene also fall under the umbrella of preventive care. By prioritizing these preventive measures, individuals can take proactive steps to safeguard their health and well-being for the long term.
Commercial insurance providers and federal programs like Medicare and Medicaid are measured on various dimensions of performance, including clinical outcomes, patient satisfaction and adherence to best practices. For example, HEDIS (Healthcare Effectiveness Data and Information Set) is a standardized set of performance measures developed by the National Committee for Quality Assurance (NCQA), a leading healthcare accreditation organization. Many health plans use HEDIS scores to measure clinical quality and service performance; more than 235 million people are enrolled in plans that report HEDIS results. 2 These scores are based on more than 90 measures across six domains, and nearly one-third of the measures are related to gaps in care. 2 Health plans are ranked based on these scores which impact financial performance, accreditation and market competitiveness.
“Because payers are scored on the value of care provided to their members, it is financially advantageous for them to employ solutions that aim to reduce and close gaps in care,” Denman said. Also, investing in preventive care helps reduce the incidence of costly emergency room visits, hospitalizations and complex treatments for advanced diseases, which can help reduce insurance premiums and promote higher

At-home testing solutions extend care directly into the home, making testing easier to access and providing privacy for sensitive tests, potentially making the patient feel more comfortable with completing the process.
reimbursements and more sustainable healthcare spending.
Closing the gaps
At-home testing is a relatively new development in healthcare that eliminates physical barriers
between patients and their testing. By sending diagnostic screening kits directly to patient homes, they’re more likely to complete recommended screenings, potentially detect health issues early and minimize long-term medical

expenses. “Meeting patients where they are can help make it easier for them to stay up to date on recommended screenings and manage existing conditions,” Denman said.
The flexibility of at-home testing can also be beneficial when the type of health screening required can only be done at home, when there are privacy concerns and/or when geographical/language barriers to care exist.
The value of at-home testing goes beyond convenience. In one study 3 of 1.1 million adults
aged 50 to 75 from 2000-2019, Kaiser Permanente was able to reduce colorectal cancer incidence and mortality by 30% and 50%, respectively, from their at-home screening program.
“Results like these show that extending health care into the home has value beyond convenience,” Denman noted. “The increase in preventative care and early-stage detection can increase longevity and reduce the overall cost of care.”
Cardinal Health is teaming up with technology providers,
labs and collection system manufacturers to enable athome testing programs that are managed from beginning to end.
“Cardinal Health has decades of experience in the diagnostic supply market and a dedicated lab kitting facility with capabilities for personalized, direct-to-home kitting,” Denman said. “Cardinal Health also offers a comprehensive range of products and services tailored for clinical laboratories, including distribution solutions, custom solutions and lab-specific programs.”
A New Era of Diagnostics
Denman said Cardinal Health’s collaboration with experts in diagnostic technology allow them to provide a variety of benefits for at-home testing, including:
Kits personalized with the health plan or health system branding, sent directly to the patient’s home: Helping ensure that the health plan or health system’s brand is visible can increase trust in communications with patients.
Patient/member communications and timely notifications to give visibility, support and results: Examples of these communications include heads-up letters to notify people of an upcoming gap closure effort, paper and digital instructions with multiple language options, optional notifications to track the sample and lab result status with easy-toreach live agents to assist in collection support.
Full integration with the laboratory to capture and share results: A big part of a successful gap closure program is providing timely analysis and results, Denman noted. “The labs involved in these programs take this very seriously and emphasize efficient sample analysis.”
“A big part of a successful gap closure program is providing timely analysis and results. The labs involved in these programs take this very seriously and emphasize efficient sample analysis.”
Full-program visibility to track every step, from distribution to specimen collection to results: Real-time visibility includes detailed tracking of kit shipment, kit registration, kit return, lab reception, sample status and result. “We’ve found this visibility is critical to enabling necessary program adjustments and allowing health plans and health systems to improve their coordination across programs and patient follow-up,” Denman said.
Extending
care to where patients are
At-home testing solutions extend care directly into the home, making testing easier to access and providing privacy for sensitive tests, potentially making the patient feel more comfortable with completing the process. These solutions may be part of a patient’s health plan or health system, allowing for direct coordination with primary care physicians.
“The solutions also provide uniquely personalized and
high-quality patient experiences, with features designed to gain trust and increase engagement,” Denman said. “These extras can make a big difference in the patient experience – removing additional barriers to compliance even after the test reaches the patient’s home.”
One payor saw significant improvements just one year into implementing these solutions, including a 25% increase in sample return rate and a 40% increase in gap closure rates. Sample rejection rates even decreased by 35%.*
Physical features of the tests include a simple design with clear instructions and labeling with a recognized name of the patient’s health plan or health system. The patient also enjoys regular updates and an easy way to contact someone for further understanding or support.
“These elements can contribute to higher compliance and test return rates that close important gaps in care,” Denman said.
Steven Denman is Director, Laboratory Business Development and Gaps in Care Programs at Cardinal Health, where he leads new strategic offering development with a special focus on diagnostic testing in the home for payers and health systems.
1 Center for Disease Control and Prevention (CDC). About Chronic Disease. cdc.gov. Oct 4, 2024. Accessed from: www.cdc.gov/chronic-disease/about/index.html. Accessed on Aug 19, 2025.
2 National Committee for Quality Assurance (NCQA). HEDIS Measures and Technical Resources. ncqa.org. www.ncqa.org/hedis/measures/. Accessed on Aug 19, 2025.
3 San Francisco Chronicle. At-home tests dramatically reduced death rates for this kind of cancer, study finds. sfchronicle.com. www.sfchronicle.com/health/article/home-colorectal-cancer-screening-kaiser-20301331.php Accessed on Aug 19, 2025.
*Data provided by Spot Health for payor customer with 2024 results vs. 2023 results for all gaps-in-care tests that had data available in both periods.


The 2026 “Breakthrough” theme represents more than just shattering ceilings or pushing past limits—it symbolizes transformational leadership moments, growth after challenge, and bold steps into new territory. By weaving in the art of Kintsugi, the summit will celebrate not only achievement but resilience, healing, and becoming stronger through adversity.
Stories That Stick: The Irresistible Power of Strategic Storytelling
Kindra Hall, Keynote Speaker, Wall Street Journal Best Selling Author, Award-Winning Storyteller
Through compelling research, profound case studies, and captivating stories of her own, Kindra will elevate individuals on all levels of your company. The outcome of this keynote is attendees feeling empowered, excited and capable of making a simple shift to telling more strategic stories to captivate customers, influence behavior and transform business.
Kindra Hall is a leading expert on strategic storytelling, trusted by global brands worldwide. She is also a bestselling author whose books, including Stories That Stick and Choose Your Story, Change Your Life, have been recognized as top business and personal development reads.


Braving Change: Resilient Through Disruption
Velera Wilson Keynote Speaker, Author, Leadership Development Consultant
Velera Wilson helps audiences embrace change with courage and a growth mindset. Using practical stories and real-world insights, she equips individuals and organizations to navigate uncertainty, overcome resistance, build resilience, and stay focused during the “messy middle.” Attendees will learn strategies to lead boldly, maintain wellbeing under pressure, and turn change into a catalyst for growth and forward momentum.
Velera Wilson helps leaders and teams increase confidence, performance, and navigate change with impact. With over twenty years of expertise, she has launched products used globally, led high-performing teams, and generated multi-million-dollar revenue for industry giants like AT&T and Fiserv.
Register today to attend the industry’s only conference completely dedicated to inclusive leadership development.
Registration now open at mypwh.org

‘Big’ Changes Ahead
How the OBBBA could reshape hospital finances, payer mix, and value-based care.
 The 2025 budget reconciliation act, otherwise known as the “One Big Beautiful Bill Act ” (OBBBA), promises sweeping changes for hospitals, payers, and patients. For many providers, the legislation lands at a precarious moment. Hospital margins, already squeezed since the pandemic, continue to face pressure from rising costs, reimbursement challenges, and shifting payer dynamics.

Indeed, the OBBBA has some big projected financial changes for all healthcare stakeholders to wrap their heads around.
PwC forecasts that the OBBBA, signed into law on July 4, 2025, will slash federal healthcare spending by approximately $1 trillion through fiscal year 2034. The legislation tightens Medicaid eligibility, introducing
work requirements, more frequent documentation checks, and shorter retroactive coverage, which is expected to increase Medicaid disenrollments and leave many uninsured.
States will now shoulder heightened administrative burdens and tighter funding, as limitations are placed on provider taxes and federal matching support,

PwC noted in a report on the legislation. The ending of ACA premium subsidies and DSH (Disproportionate Share Hospital) payments after 2025 could destabilize Marketplace insurance pools, potentially driving up premiums and prompting plan exits.
Hospitals, especially rural and safety-net providers, face rising uncompensated care despite a $50 billion stabilization fund.
Margin compression and workforce strain
In today’s marketplace, hospitals are being squeezed from both ends. Margins are “being challenged on both sides, revenue and costs,” said Tamyra Porter, Managing Director-Regulatory Practice Lead, Advisory Services at Premier. Supply chain volatility, rising tariffs, and inflation have driven up expenses, while reimbursement rates have not kept pace. Data, she noted, is becoming indispensable in helping hospitals find the right balance between cost and quality in their supply chains.
But the workforce crisis looms just as large. Recruiting and retaining staff remains difficult, especially with fluctuating patient volumes. Many systems have chosen not to backfill certain positions, often in nonclinical areas, just to protect margins. These cuts, however, create their own operational challenges.
Seth Edwards, Premier’s Managing Director of Strategy, Innovation, and Population Health added that revenue optimization is a growing concern. He pointed to a large Southwestern health system Premier advised, where five-year projections
showed negative contribution margins across Medicare Advantage, Medicaid, and traditional Medicare. The findings forced leaders to rethink their approach, considering deeper moves into value-based contracts where managing populations could produce shared savings. “Margin compression is pushing organizations to reconsider their operating models and assumptions about risk,” Edwards said.
Thom Bales, Principal, Health Services Advisory Leader, PwC US said the OBBBA’s funding constraints are likely to push health systems to reimagine value.
“As federal funding tightens, stakeholders are seeking more sustainable care delivery models – and prevention-focused care is emerging as a strategic imperative.”
Community-embedded care models: Integrating social determinants of health (SDOH) screening and support into primary care – especially in underserved areas – can prevent costly acute episodes.
“These models, supported by cross-sector collaboration and technology investments, are poised to create a more sustainable and patient-centered health system,” Bale said.
The payer mix shift
Porter and Edwards agreed that the payer mix of the future will tilt heavily toward government programs, even with the planned cuts. Medicare enrollment is projected to hit 81 million by 2030, with nearly two-thirds
Sliding-scale, asset-based approaches to eligibility as well as models like the ABLE Act, which encourages disabled communities and families to save without risk to benefit losses, could help households build stability without penalty.
Innovative models that could accelerate this shift include:
Value-based care expansion: Bundled payments and shared savings programs will incentivize proactive population health management, especially when combined with CMS’s growing emphasis on outcomes over volume.
Digital-first preventive platforms: Wearables, remote monitoring, and predictive analytics can preemptively detect health risks and enable interventions before illness escalates.
enrolled in Medicare Advantage. Medicaid also remains a key player, especially as states grapple with program expansions and eligibility redeterminations. Porter pointed to CMS’s Achieving Healthcare Efficiency through Accountable Design (AHEAD) Model, an all-payer reimbursement approach modeled on Maryland’s global budget system, as an example of where things may be headed. The idea is to level-set payments across payers, reduce volatility, and promote
prevention. But implementation is complex, requiring a large, risk-bearing health system to align providers under a total-cost-ofcare contract. “What works in Maryland may not work everywhere,” she cautioned.
Edwards said one certainty is that CMS will continue pushing more risk onto private entities. Commercial insurers, in turn, are following Medicare’s lead. “Over the next decade, this shift will force providers to reimagine their place in the premium dollar and redefine what sustainability looks like,” he said.
Value-based care has been discussed for years, but OBBBA and federal incentive programs may finally give it some momentum. Edwards explained that hospitals working under risk contracts are finding patient-centric models to appropriately keep low- or negative-margin patients healthier outside of the hospital, which frees up resources for higher-need cases. He cited CMS’s Medicare Shared Savings Program, where 55 ACOs, who are members of Premier’s Population Health Management Collaborative, recently generated $498 million in shared savings, proof that value-based models can deliver financial and clinical benefits.
Porter emphasized how technology has changed the game compared to the early days of value-based care. Realtime analytics now allow providers to target high-risk patients, manage chronic conditions more efficiently, and build critical mass in communities. “Technology also raises questions about the best structure,” she added. “Should risk be
managed at the physician-led network level, or through larger managed care organizations?”
Premier has been preparing members for these changes for more than a decade through its Population Health Management Collaborative. The initiative helps hospitals achieve sustainable success through understanding infrastructure, staffing, and technology investments required to move along the value-based care maturity curve. Unlike physician groups, hospitals must carefully balance cost savings with operational needs, making the transition especially complex.
Medicaid and the uninsured
With OBBBA and the pending changes to Medicaid and ACA tax incentives, the future of coverage remains uncertain. Porter explained that policymakers are reexamining Medicaid’s role, questioning whether expansions are sustainable and how best to align eligibility across welfare programs.
Some argue the program should act as a “trampoline rather than a hammock,” she said, providing temporary support during hardship while encouraging independence. That philosophy is driving proposals for work requirements, stricter eligibility checks, and better coordination with programs like SNAP.
Porter also highlighted the need to address the “benefits cliff,” where individuals risk losing all assistance if they earn slightly more income. Sliding-scale, asset-based approaches to eligibility as well as models like the ABLE Act, which encourages disabled communities and families to save without risk to benefit losses, could help households build stability without penalty.

“With margins tightening, payers and providers are increasingly motivated to accelerate adoption of value-based care models that reward outcomes rather than procedures.”
In the near term, hospitals may need to prepare for higher levels of uncompensated care if coverage shifts occur, while streamlining enrollment support to keep eligible patients insured.
Bales said the growing instability in ACA Marketplace participation – exacerbated by subsidy expirations – has revived interest in regional and collaborative insurance models, particularly for vulnerable populations. He is seeing traction in:
Public-private coalitions: Municipalities and health systems are exploring regional coverage pools or subsidized plans that blend public funding with private administration.
Health system-backed plans: Some providers are launching their own insurance arms to directly manage risk and provide continuity of care for underserved groups.
Community-based risk pools: These models allow small employers, nonprofits, or local gov-
ernments to aggregate purchasing power and reduce premiums.
“These alternatives may gain urgency if ACA gaps widen, particularly in geographies with limited Marketplace competition,” Bale said.
Preparing for the future
As hospitals brace for the ripple effects of OBBBA, Porter urged leaders to take a proactive approach. “The first step is modeling your margin forecast; don’t be caught flat-footed,” she said. Hospitals will need to examine every operational lever, including supply chain, revenue cycle, workforce, and length of stay, to build resilience.
Some may need to make difficult choices, such as delaying facility expansions or scaling back service lines if they are financially unsustainable. “These tough decisions
are part of preparing for long-term financial stability,” Porter noted. Edwards agreed, underscoring the importance of embracing value-based models as both a financial and clinical strategy. With payer mixes increasingly dominated by Medicare and Medicaid, and federal policy shifting more risk downstream, providers that adapt early will be better positioned for sustainability.
Beyond cost controls, the OBBBA may serve as a catalyst for systemic transformation in several key ways. “With margins tightening, payers and providers are increasingly motivated to accelerate adoption of valuebased care models that reward outcomes rather than procedures,” Bale said. At the same time, domestic production incentives could help modernize the
The OBBBA and reshoring
The OBBBA’s provision for full expensing of domestic R&D and manufacturing costs signals a broader industrial policy shift, Bale said. While it directly targets pharmaceutical supply chains, it also opens the door for reshoring across emerging medtech sectors, including:
Digital Therapeutics and Diagnostics: Startups and scale-ups in digital health may find the tax incentives compelling enough to build or expand U.S.-based manufacturing and research operations.
Precision Medicine Platforms: Companies developing AIdriven diagnostics or genomics tools may choose to localize advanced manufacturing to capitalize on these tax benefits.
Medical Device Manufacturing: Especially for high-margin, low-volume devices where domestic production offers both tax and supply chain resilience advantages.
This could catalyze a “Made-in-America” renaissance in health innovation, strengthening domestic capabilities and reducing reliance on foreign sources for critical technologies.
supply chain by driving greater transparency, resilience, and diversification across pharmaceutical and medtech sectors.
The bill may also nudge both public and private actors to integrate health equity as a business and compliance imperative, particularly as marginalized populations continue to face disproportionate coverage and access challenges.
Additionally, smaller and rural providers may feel pressure to consolidate, pursuing strategic partnerships or mergers to remain viable amid shrinking drug revenue and rising compliance burdens. “In essence, the OBBBA is likely to act as a forcing function – pushing stakeholders to reassess business models, delivery systems, and value creation strategies,” Bale said.
The OBBBA is more than just another piece of federal legislation. It is a signal that the economics of healthcare are shifting dramatically. Hospitals and health systems will face heightened pressures on margins, a payer mix dominated by public programs, and accelerated expectations to deliver care under value-based and risk-based contracts.
For leaders, the takeaway is clear: prepare now, invest in data-driven decision-making, and consider how to thrive in a system where financial sustainability is tied to keeping populations healthy.
“Healthcare is largely driven by incentives,” Edwards concluded. “With OBBBA, those incentives are changing. The organizations that lean into valuebased care and proactively adapt will be the ones positioned for long-term success.”


High Throughput Hematology
High Throughput Hematology
High Throughput Hematology
Seamlessly Automated
Seamlessly Automated
Seamlessly Automated
High Throughput Hematology
Automated
HORIBA & CellaVision Deliver the Total Solution
HORIBA & CellaVision Deliver the Total
HORIBA & CellaVision Deliver the Total Solution
Solution

Unmatched Sample Throughput
Unmatched Sample Throughput
Unmatched Sample Throughput
120 samples/hour, CBC with 6-part differential. Reticulocyte panel with five parameters and body fluid testing capability with 2-part differential.
120 samples/hour, CBC with 6-part differential. Reticulocyte panel with five parameters and body fluid testing capability with 2-part differential.
120 samples/hour, CBC with 6-part differential. Reticulocyte panel with five parameters and body fluid testing capability with 2-part differential.
HORIBA & CellaVision Deliver the Total Solution


AI-Driven Accuracy
AI-Driven Accuracy
AI-Driven Accuracy
Unmatched Sample Throughput
Leveraging AI-powered Yumizen H2500 analysis with CellaVision digital imaging for faster, more precise results.
Leveraging AI-powered Yumizen H2500 analysis with CellaVision digital imaging for faster, more precise results.
Leveraging AI-powered Yumizen H2500 analysis with CellaVision digital imaging for faster, more precise results.
120 samples/hour, CBC with 6-part differential. Reticulocyte panel with five parameters and body fluid testing capability with 2-part differential.
Superior 360° Mixing Advantage
Superior 360° Mixing Advantage
AI-Driven Accuracy
Superior 360° Mixing Advantage
Achieve unmatched sample homogeneity, eliminating manual pre-mixing—ensuring consistent, reproducible first run results.
Achieve unmatched sample homogeneity, eliminating manual pre-mixing—ensuring consistent, reproducible first run results.
Achieve unmatched sample homogeneity, eliminating manual pre-mixing—ensuring consistent, reproducible first run results.
Leveraging AI-powered Yumizen H2500 analysis with CellaVision digital imaging for faster, more precise results.

Intelligent Flagging for Confidence
Intelligent Flagging for Confidence
Intelligent Flagging for Confidence
Superior 360° Mixing Advantage
Advanced algorithms identify anomalies, reducing rerun, manual reflex testing and supporting confident clinical decisions.
Advanced algorithms identify anomalies, reducing rerun, manual reflex testing and supporting confident clinical decisions.
Advanced algorithms identify anomalies, reducing rerun, manual reflex testing and supporting confident clinical decisions.
Achieve unmatched sample homogeneity, eliminating manual pre-mixing—ensuring consistent, reproducible first run results.
Upgrade Your Life: Pair the Yumizen H2500 in an
with CellaVision Digital Imaging for Seamless Hematology Workflow —
Upgrade Your Life: Pair the Yumizen H2500 in an enhanced partnership with CellaVision Digital Imaging for Seamless Hematology Workflow —
Upgrade Your Life: Pair the Yumizen H2500 in an enhanced partnership with CellaVision Digital Imaging for Seamless Hematology Workflow —
Intelligent Flagging for Confidence
Scan the QR Code to contact HORIBA today!
Scan the QR Code to contact HORIBA today!
Scan the QR Code to contact HORIBA today!

Advanced algorithms identify anomalies, reducing rerun, manual reflex testing and supporting confident clinical decisions.
: Pair the Yumizen H2500 in an
No Silver Bullet for Rural Healthcare
From provider shortages to limited infrastructure, rural America’s health crisis demands more than short-term funding fixes, experts caution.
 The budget reconciliation act allocates $50 billion in funding for rural healthcare providers through the Rural Health Transformation Program.
The program has five strategic goals:
Promoting preventative health and addressing root causes of diseases (“Make rural America healthy again”)
Ensuring sustainable access by helping rural providers become long-term care access points
Workforce development to improve recruitment and retention of providers
Fostering innovative care models
Encouraging technological innovation, including tools for remote care, improved data sharing, cybersecurity, and digital health.
In terms of structure and timeline, the $50 billion will be spread over five fiscal years (FY 2026–2030) at $10 billion per year.
Half of the funding will be distributed equally to all approved states; the other half will be awarded based on state-specific metrics and where the greatest potential for impact exists. States must use funds for at least three of several statutorily approved purposes (e.g. chronic disease prevention, tech-enabled care, workforce training, etc.) with oversight to ensure long-term sustainable improvement.

Pressure and opportunity
Thom Bales, Principal, Health Services Advisory Leader, PwC US
Proponents of the Rural Health Transformation Program say it is intended to help rural providers adapt, modernize, workforce development and improve access to care. Opponents of the bill say that those funds are not enough to offset projected losses.
believes rural health systems are likely to experience both pressure and opportunity under the OBBBA.
On one hand, reduced revenue from lower drug reimbursements may hit rural hospitals – already operating on thin margins – particularly hard, creating financial strain.
On the other hand, the changes could create a window for more preventive innovation. The incentive to shift from volume to value could encourage the adoption of telehealth, mobile clinics, and community-based prevention efforts, especially if supported by targeted grants or Medicaid waivers. Provisions encouraging domestic drug manufacturing could help stabilize access to critical medications in rural areas, which often suffer from supply disruptions.
“Rural systems will need strategic investment and policy support to adapt effectively to these shifts,” he said.
From the ground up
There is plenty of blame to go around for the lack of attention to rural healthcare problems over the years. “The challenges impacting rural America have not been addressed in a sustainable manner by either Democrat or Republican administrations,” said Thomas Campanella, president, Campanella Consulting, Inc., and professor emeritus of Health Economics, Baldwin Wallace University. “This is due to a number of factors, but mostly because politically rural America did not have a strong enough voice to impact needed policy decisions at both the national and state levels.”
The healthcare industry too has also fallen short in addressing
rural health issues. In a LinkedIn blog on the topic, Campanella argues that the healthcare system’s responses to challenges in rural America often amount to temporary fixes (“band-aids”) rather than long-term, systemic solutions. Rural communities face persistent issues – such as limited healthcare infrastructure, provider shortages, low funding, and access barriers – that can’t
Sustainable support needed
There is no one solution to the multi-faceted challenges facing rural America, but one of the greatest needs is access to primary care. “We need federal and state sustainable support for Federally Qualified Health Centers (FQHCs), Community Health Centers, County Public Health Departments, and Community Health Workers,” Campanella said.
“At a minimum, rural hospitals need to have a functioning 24-hour, 7 day a week emergency room. Beyond that, the services will vary depending upon the specific needs of the community.”
be solved by short-term grants or temporary programs.
“There needs to be a groundup approach which starts with the health-related needs of the residents in the rural community,” he said.
Rural communities have common needs, but they are also unique (e.g. Different demographics, size of population, closes urban center, geography, etc.). The need for comprehensive primary care is common across all rural communities. Hospitals need to be right sized for the particular community depending on a number of the unique factors noted previously.
“At a minimum, rural hospitals need to have a functioning 24-hour, 7 day a week emergency room,” Campanella said. Beyond that, the services will vary depending upon the specific needs of the community.
The staffing of the FQHCs and Community Health Centers should include teams of primary care physicians, nurse practitioners, nurses, community health workers, behavioral health specialists, and other providers based upon the needs of the rural community.
History has shown that access to Medicaid is not the silver bullet answer to the health needs of rural America, Campanella said. Over the last 20 years, working-age people living in rural areas are 43% more likely to die from natural causes than in urban areas. Medicaid, in collaboration with other initiatives can make a difference.
“To have a long-term impact on the health of residents in rural America, we need to have sustainable initiatives targeted to rural communities unique needs,” Campanella said.
By the Numbers: Medicare and Medicaid spending
 Lawmakers who supported the healthcare components of the budget reconciliation act cited fiscal responsibility as a key reason, saying reforms would help control federal spending and deficits. Many of those lawmakers argued the OBBBA changes would preserve Medicaid for vulnerable groups while tightening eligibility and adding work or verification requirements to ensure resources go to those truly in need.
What can the numbers tell us?
Medicare spending has grown significantly in recent years, reflecting both demographic shifts and policy factors. In 2020, total Medicare expenditures reached about $829.5 billion, representing 20% of national health spending, according to the Centers for Medicare & Medicaid Services. By 2023, that number had risen to approximately $1,029.8 billion, or just over $1 trillion. This marks an increase of around $200 billion over three years – roughly a 24% jump.
Medicaid experienced even sharper growth during the same period. In 2020, combined federal and state Medicaid spending was estimated at $671.2 billion, accounting for 16.3% of national health expenditures. By 2023, spending had expanded to approximately $871.7 billion. That nearly $200 billion rise represents close to a 30% increase over three years, outpacing Medicare’s rate of growth.
Together, these increases highlight the mounting financial pressures on the U.S. healthcare system. Medicare’s spending growth crossing the trillion-dollar threshold and Medicaid’s nearly 30% surge illustrate the effects of the COVID-19 pandemic, policy changes, and eligibility expansions.

Both programs have grown faster than typical annual trends, underscoring the strain they have placed on federal and state budgets.
Supporters of the bill also highlighted giving states more flexibility, reducing federal mandates, and curbing fraud, improper payments or abuse in the system.
Improper Medicare and Medicaid payments topped $100 billion in recent years, according to federal data, highlighting the programs’ ongoing struggle with errors, fraud and documentation issues.
In fiscal year 2024, the Centers for Medicare & Medicaid Services reported a 7.66% improper payment rate in Medicare Fee-for-Service, totaling about $31.7 billion. Medicare Advantage accounted for $19.07 billion in improper payments, while Medicare Part D added another $3.58 billion,
according to the Kaise Family Foundation. Across all Medicare programs, improper payments reached more than $54 billion last year, the Government Accountability Office reported.
Medicaid’s improper payment rate was 5.09% in 2024, equating to about $31.1 billion, CMS said. Roughly three-quarters of that amount – $23.4 billion –stemmed from insufficient documentation rather than fraud, the Center for Contemporary Finance found. Another $4.9 billion was tied to medically unnecessary services or ineligible recipients, while about $1.5 billion came from payments to unqualified providers or other losses.
The GAO reported that Medicare and Medicaid combined for more than $100 billion in improper payments in fiscal year 2023, representing a large share of all federal improper payments. Medicaid’s total that year was estimated at $31 billion, consistent with 2024 figures. Some independent analysts argue the government’s numbers understate the problem. The Paragon Health Institute estimates improper Medicaid payments could total $1.1 trillion over the past decade, far above official figures.

We Are Thankful
The Share Moving Media team appreciates all of our loyal readers and advertisers.
We are truly thankful for the wonderful industry we have the privilege to serve.


Women’s Health: Bridging the Research Gap
Cleveland Clinic advances women’s health through tailored care for women in their midlife.
By Jenna Hughes
 Women’s health issues, especially for patients age 40 and older, have for many years been misunderstood and under researched. As a result, many women are not aware of the health changes and symptoms that can come with aging and midlife.

“Much of women’s health has been understudied historically. There are many conditions that are female specific or that disproportionately impact women, or that impact women differently than men, and many of these issues have not been well studied,” said Dr. Pelin Batur, Department of Subspecialty Care for Women’s Health, within the Ob/Gyn & Women’s Health Institute at Cleveland Clinic.
To address the growing healthcare gap for middle-aged women, Cleveland Clinic launched
the Women’s Comprehensive Health and Research Center, with the help of Maria Shriver, a wellknown journalist, women’s health advocate, founder of the Women’s Alzheimer’s Movement at Cleveland Clinic and the center’s Chief Visionary and Strategic Advisor, to empower women to navigate their personal health journey with confidence and clarity.
The Center specifically focuses on women as they move through their 40s, 50s, 60s and beyond in facing health changes head on and feeling their best.
“It seemed like for women in midlife and beyond, healthcare fell off the map,” said Dr. Batur. “We knew that this was a critical group needing focused care.”
Since its launch in 2024, the Women’s Comprehensive Health
call to action for the future of women’s health.
Midlife health
Women’s health issues such as menopause have a significant impact on an individual’s wellbeing, sleep, mental health and entire body.
“The lack of research around women’s midlife health is problematic because nearly 6,000 women each day go into menopause, and at that time in their life see a lot of changes in their health and their body,” said Dr. Batur. “In fact, 78% of women 55 and older have a chronic disease that they are dealing with, and the healthcare industry has not done a great job in studying these individuals and finding how to best take care of them.”
“ Research is answering the questions that patients have for the clinic, and Education empowers patients to make informed decision and educate colleagues about the importance of women’s health.”
and Research Center has served more than 10,000 patients, scheduled more than 19,000 appointments and hosted more than 1,000 virtual shared medical appointments focused on menopause.
The one-year anniversary of the Women’s Comprehensive Health and Research Center was celebrated at Cleveland Clinic’s inaugural Women’s Health Forum in June 2025, which brought together national leaders in healthcare, research and advocacy and served as both a celebration of progress and a
Menopause is a normal part of aging for women – not a disorder or disease – according to the National Institute on Aging. Some women have mild or no menopausal symptoms, but for others, the menopausal transition can bring various symptoms, including hot flashes, night sweats, trouble sleeping, joint and muscle discomfort, pain during intimacy, moodiness and irritability, forgetfulness, difficultly concentrating, or a combination of these.
Menopause symptoms can be managed through a variety of
interventions including hormone therapy, medication and lifestyle adjustments. Treating menopause therefore requires a treatment plan that is tailored to each patient’s individual needs.
“The long-term Women’s Health Initiative Study came out to help answer the specific question of if all women should be on hormone prevention for treatment of menopause symptoms – the answer is that clinicians must weigh the pros and cons of the therapy for each individual patient,” said Dr. Batur. “For many years in the healthcare industry clinicians advised women against hormones, but the study proved it is more complicated than that, and women didn’t want to keep suffering through symptoms, they wanted solutions.”
The Women’s Comprehensive Health and Research Center attempts to bring an ‘in-between’ perspective to the treatment of women’s health issues by focusing on each individual patient’s potential to benefit from hormone therapy and other treatments.
“Hormone therapy is not poison, and it’s also not the fountain of youth,” said Dr. Batur. “The truth is that it’s somewhere in between, and we can only help women by educating our patients and clinicians and getting each individual the care that they need.”
The Women’s Comprehensive Health and Research Center
In response to female patients’ ongoing health concerns, Cleveland Clinic’s Women’s Comprehensive Health and Research Center chose to focus on a unique approach to care with four pillars:
Connectivity, Access, Research, and Education.
“What we really want to do is connect (Connectivity Pillar) clinicians so that they are not looking at patients through their own specialty silo only. The Access Pillar explores how we bring access close to the patient with virtual visits and longer appointments,” said Dr. Batur. “Research is answering the questions that patients have for the clinic, and Education empowers patients to make informed decisions and educate colleagues about the importance of women’s health.”
care, acknowledging patient’s dayto-day personal responsibilities and keeping in mind scheduling and time concerns.
“Virtual care options are now available in 20 states across the U.S. to understand a patient’s preventative and health needs,” said Dr. Batur. “These services are accessible to everyone no matter the socioeconomic status or where throughout the nation they are coming from.”
A step in the right direction
The first step for patients who want to make an appointment
“ We need to be aware of how to take care of a variety of female patients in early life, diagnose and treat them, so that we can prevent issues like high blood pressure, brain health issues and whether a woman will age into wellness or disease.”
Clinicians at Cleveland Clinic work together on complex women’s health issues to address the whole person and form a personalized treatment plan. The Center is built around allowing women to access a variety of different types of healthcare providers in one place.
“Our women’s behavioral health team, sleep neurologist, our hormone specialists, and our primary care doctors meet on a regular basis now to connect, teach each other, and figure out how best to serve our patients,” said Dr. Batur.
The healthcare programs available to women at the Center were built with accessibility for the average patient in mind –addressing economic barriers to
at the Women’s Comprehensive Health and Research Center is to call and talk to a trained navigator at the Welcome Center.
Trained navigators meet with the facility’s doctors on a regular basis to communicate, so that when a patient calls, they can talk candidly about their health concerns to someone who understands them.
Once a patient reaches out, a navigator then schedules an evaluation to begin building them a personalized care plan.
Beyond menopause, the Center can create a plan to manage patient concerns including Alzheimer’s disease, breast pain, cancer risk assessment and genetic screening, diabetes, irregular
periods, osteoporosis, pelvic pain and much more.
Nearly two-thirds of Americans living with Alzheimer’s are women, according to the Alzheimer’s Association. Women are at the center of the Alzheimer’s crisis, but their experiences have long been overlooked in research. Cleveland Clinic aims to address these gaps through the first-of-its-kind Women’s Alzheimer’s Movement Prevention and Research Center. This program is designed to address women’s individualized risk for Alzheimer’s and is available through the Women’s Comprehensive Health and Research Center.
“We formed the Women’s Comprehensive Health and Research Center to really listen to and understand the voice of our patients who had felt as though physicians weren’t listening and doctors weren’t talking to each other, and to shed light on hormone therapy, as many people were misinformed about it as a treatment option.”
Cleveland Clinic is also revolutionizing the approach to patient appointments by addressing patient concerns through 90-minute virtual shared medical appointments, with real experts leading the conversation, to provide women with credible health information and everything they need to know about their health concern or diagnosis.
“These appointments are generally shared with 5 to 15 other women, with the opportunity throughout for questions that the patient themselves may not have asked,” said Dr. Batur. “This ensures that clinicians are providing patients with all the education
they need so they can make informed decisions.”
Women’s Health Forum
The Cleveland Clinic Women’s Health Forum in June 2025 aimed to shed light on women’s health issues – with panel discussions on menopause, wellness, aging, and work-life balance, fireside chats, a conversation

with a female author, a video series launch, and more led by Cleveland Clinic specialists and influential women executives.
“We learned that women have been craving this type of event, and the energy at the Forum was palpable,” said Dr. Batur. “Women want to see change and advancements on these topics. They weren’t aware that these types of services, such as the Women’s Comprehensive Health and Research Center, were available and they were enthusiastic about getting connected. This is why we’re here, and why we’re planning to host another Forum for next year.”
Takeaways of the conference included the advancement
of women’s health innovation, showcasing the latest research on women’s health and fostering collaboration – but most importantly it was a space where women felt seen and supported, according to Dr. Batur.
“We started the Center focusing on midlife and beyond because it was an area of need,” said Dr. Batur. “Eventually our goal is to make this Center about serving women across the lifespan.”
For example, a woman’s care during pregnancy can impact cardiovascular disease in midlife, or how healthy blood vessels are at midlife can impact dementia risk in a woman’s later years of life.
“We need to be aware of how to take care of a variety of female patients in early life, diagnose and treat them, so that we can prevent issues like high blood pressure, brain health issues and whether a woman will age into wellness or disease,” said Dr. Batur. “We do a good job of care throughout the lifespan at Cleveland Clinic already and need to build on this going forward.”
Right now, the clinicians at the Women’s Comprehensive Health and Research Center plan to go forward by acknowledging the interconnected nature of women’s health and addressing health issues throughout the lifespan by expanding its services in the next four to five years.
“I’m proud to work in a place where colleagues feel passionate about this type of care for women,” said Dr. Batur. “We are able to reach more women and spend face to face time with them, and I know that we each truly care about managing each patient’s health holistically.”

Connected Care
Wearable devices for diabetes have revolutionized patient care delivery and clinical workflows in post-acute care settings.
Wearable devices, which perform functions such as tracking a patient’s heart rate, respiratory rate, blood pressure, glucose levels, movement and more – allow for the continuous remote monitoring of critical patient health data, according to a National Library of Medicine study.
Repertoire Magazine recently spoke to Dr. Naushira Pandya, Professor and the Chair of the Department of Geriatrics at Nova Southeastern University’s Kiran C. Patel College of Osteopathic Medicine and Director of the Geriatrics Workforce Enhancement Program, south Florida, to discuss wearable devices within post-acute care settings.
Integrating wearables
Post-acute care facilities often have a higher rate of patients with multiple comorbidities as well as cognitive and psychosocial problems compared to other types of medical facilities, requiring practitioners to treat many patients with more than one health concern.
“After residency, I was very interested in endocrinology and had the opportunity to work in a long-term care setting with medically complex and challenging patients that had chronic medical conditions along with geriatric syndromes such as falling, weight loss and incontinence,” said Dr. Pandya.
 Optimizing workflows in post-acute and long-term care facilities is a crucial part of clinicians’ ability to provide quality patient care. With the growing adoption of technology in healthcare, wearable devices have been increasingly recognized as a valuable way to enhance clinical efficiency in a variety of post-acute settings including skilled nursing, longterm acute care hospitals (LTACHs), inpatient rehabilitation and home health care.
In addition to teaching geriatrics to medical students, fellows in Geriatrics, and residents; Dr. Pandya has an active nursing home and ambulatory care practice in Geriatrics and Endocrinology.
“My area of specialty and the area that I have been most interested in for many years is
diabetes in older adults, and my research publications have largely been surrounding this topic,” said Dr. Pandya.
Dr. Pandya, who has served on the Board of Directors with the Post-Acute and Long-Term Care Medical Association (PALTmed) and was its President in 2015, contributed a clinical perspective to the organization as Chair of the Diabetes Clinical Practice Guideline (CPG) for Long-Term Care. This is a popular guideline and has undergone three revisions in addition to a pocket guide and is supported by other diabetes publications.
“There are a broad range of definitions describing the longterm care setting,” says Dr. Pandya. “Focusing in on skilled nursing facility settings, patients in these facilities are often more medically complex with longer-stay patients needing ongoing care.”
Diabetes is common among older adults, and according to the National Council on Aging, can exacerbate patients’ already existing geriatric conditions.
“Nearly 25% to 34% of patients in long-term care settings have diabetes,” said Dr. Pandya.
In most facilities, staff conduct point-of-care blood glucose
testing to monitor patients’ diabetes, which involves a blood glucose meter to check blood sugar levels with a fingerstick blood sample. Checking blood glucose levels may be required multiple times per day and can be time-consuming for long-term care staff.
Complex patients may need their finger pricked up to three to four times a day with traditional glucose monitoring and may also require multiple insulin injections, according to Dr. Pandya.
“Blood glucose testing only provides health information in the moment – we don’t know
Power up with PadPro®
The multifunction electrode that keeps it simple, reliable, and ready to perform
Need adult or pediatric electrodes for defibrillation, pacing, cardioversion, or monitoring? PadPro® checks every box.
✓ Conforms to the body for secure placement and excellent current distribution
✓ Adult/Child electrodes offer 24 hours of continuous patient monitoring
✓ 36-month shelf life to reduce waste and restock less often
✓ Adapters and connection styles compatible with Zoll and Physio Control cables
✓ Works across multiple defibrillator brands
✓ Made in the USA



what happens to blood glucose levels between blood sugar tests. The levels may drop, or they may be quite elevated between those traditional tests,” said Dr. Pandya. “The other way to monitor diabetes is through A1C testing, which gives you a look back at blood glucose levels from the last three months. For older people, this method is not always reliable because a patient may be anemic, has had a previous blood transfusion, or they may have other medical issues which can affect the reliability of A1C levels.”
of severe hypoglycemia (less than 54 milligrams per deciliter) and severe hyperglycemia (over 250 milligrams per deciliter), which can be very dangerous in older people – without the use of CGM technology, clinicians couldn’t detect these episodes before,” said Dr. Pandya. “Tracking these highs and lows is important because hypoglycemia specifically can lead to adverse clinical events such as falls, cognitive impairment, cardiac events and in extreme cases seizure and death.”
The widespread integration of wearable technology does, however, come with logistical challenges including payment and coverage issues and incorporation into existing workflows.
Most wearable devices for diabetes, however, can monitor a patient’s blood glucose levels continuously. By integrating wearable medical devices into clinical workflows, providers can instead remotely monitor patient health and access real-time data instantaneously.
Specifically, continuous glucose monitoring (CGM), a wearable technology worn by the patient 24 hours a day, tracks a patient’s glucose (blood sugar) levels over time.
CGM devices have the potential to help practitioners in long-term care settings spot trends in glucose data and react to changes in patients’ blood glucose on demand.
“Studies have shown that for patients wearing CGMs, practitioners were able to detect episodes
Prepping for wearable integration
Wearables for monitoring diabetes also include more advanced technologies such as insulin pumps, automated insulin delivery (glucose sensor that communicates with pump to automatically deliver insulin) and even technologies that only require the patient to input meal announcements to allow tailoring of the mealtime insulin dose, with automated control of between meal glucose levels.
“Patients with diabetes are living longer and aging and are now coming into skilled nursing facilities and long-term care with their own automatic insulin pumps,” said Dr. Pandya. “The question that remains is how practitioners are going to prepare for these types of patients. This is an area
we must continue to be thinking about and planning for.”
Many patients may have already been using these types of wearable devices outside of health care settings – with support from family members and at-home care teams – and desire to continue using them when they are admitted to a long-term care facility.
For long-term care staff, the challenge is to learn about how these new types of devices work and how to interpret their data for patient care decisions.
“Different facilities have varying levels of expertise, so education and support are important for the integration of wearable devices,” said Dr. Pandya. “Use of these devices requires knowledge and expertise from physicians but also nurses and nurse aides and rely on staff and caregivers to actually interpret their data and make changes in the patient care regimen.”
Going forward, educating long-term care staff on the use and integration of personal and clinical wearable technology ensures that they are prepared to interpret data and incorporate it into daily care. This is consistent with recommendations made by the American Diabetes Association in their 2025 Standards of Care guidance.
“The next push for clinicians in the post-acute and long-term care space is to expand beyond small studies on the benefit of these types of devices into larger clinical outcome studies,” said Dr. Pandya.
Cost-savings of wearables
If physicians receive the proper education and training on the
clinical use of wearable devices, they have the potential to be integrated at a larger scale within post-acute care workflows and lead to cost-savings.
“It saves a lot of time for a facility if nurses don’t have to perform routine finger sticks, document a patient’s blood glucose each time, and then decide on the insulin dose based on what orders are present,” said Dr. Pandya. “The increased adoption of wearables in long-term care promotes costsavings in terms of less equipment used, less nursing time spent at the bedside and an overall improved quality of life for patients.”
Automatic insulin pumps, in addition to glucose sensors, can also help to reduce the amount of times insulin has to be administered to patients by nurses.
The widespread integration of wearable technology does, however, come with logistical challenges including payment and coverage issues and incorporation into existing workflows.
“If we integrate more widespread use of CGM in long-term care, we must have centralized monitoring of all the data from all the patients using CGM,” said Dr. Pandya. “I introduce CGM in the courses I teach, including
the interpretation of trends, what the reports mean, etc. This needs to be reinforced and retrained in residency and then throughout a physician’s career.”
Additionally, insurance coverage for obtaining continuous monitoring devices isn’t always consistent for each patient and facility. According to Dr. Pandya, the widespread use of CGM and other wearable technology across healthcare facilities can be patchy and dependent on each individual facility’s resources and coverage of devices.
“An issue for integration of these devices is payment and

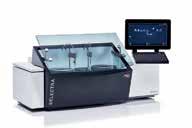

something we really must push in the medical industry,” said Dr. Pandya. “Patients with Medicare Part B or outpatients are covered and can receive CGM, but in the subacute setting under Part A Medicare, the cost of care varies and is covered by what Medicare pays the nursing home per day, per patient.”
Insurance coverage for wearable devices can be inconsistent and depend on the complexity of a patient’s health issues, what therapies they need, and how medically intensive the care is that is required.
“For patients who happen to already have CGM, they can bring in their sensors and
“ The increased adoption of wearables in long-term care promotes cost-savings in terms of less equipment used, less nursing time spent at the bedside and an overall improved quality of life for patients.”

equipment into post-acute care settings from the outpatient side, but it is important to note that they aren’t always covered in a subacute setting,” said Dr. Pandya.
Policy and action for wearables
To support and advocate for the use of wearable devices across post-acute and long-term care facilities, physicians and advocacy organizations must come together to spread information on its benefits.
“The medical community now has a consensus that we must come together nationally to research, conduct more studies, provide clinical training to practitioners and persuade CMS to increase coverage for these wearable devices so that older adults can access them,” said Dr. Pandya.
More widespread integration of wearable devices has the potential to transform patient monitoring and improve workflows, especially for the care of patients with diabetes.
“The face of diabetes has changed, and the American Diabetes Association is making an effort to recommend wearable devices, which been shown in many studies to improve outcomes. They also have a strong older adult’s interest group, and their focus this year is how to promote the use of CGM in longterm care,” said Dr. Pandya. “At PALTmed, and within the longterm care industry, we are also trying to strengthen our recommendations on wearable devices and support them going forward with training and efficacy.”
Shifting Federal Policy Landscape
What healthcare sales professionals need to know.
 Uncertainty has been the key theme of 2025, especially within the healthcare industry. From tariffs to the One Big Beautiful Bill Act (OBBBA), federal policy changes are reshaping the healthcare landscape. Four key trends are expected to shape healthcare heading into 2026.
Cuts to federal healthcare spending
The President signed OBBBA into law in July 2025, setting up sweeping changes to the health insurance landscape. Over the next 10 years, the Congressional Budget Office estimates that the federal government will spend $1 trillion less on Medicaid. Those cuts won’t happen right away. The reductions in Medicaid spending are scheduled to start in late 2026, with most of the spending cuts taking effect after 2028. Pending Medicaid cuts could have a disproportionate impact on healthcare sales because Medicaid accounts for a significant portion of national healthcare expenditures. Over the next several years, each state will be adjusting their Medicaid programs to account for lower federal spending as they balance their budgets.
Rural health providers are expected to be impacted by Medicaid cuts. OBBBA included a $50 billion Rural Health Transformation Program, which will provide $10 billion annually for five years for states to improve rural healthcare access and outcomes. It is not, however, expected to make up for the loss of Medicaid funding.
Multiple market forces pressure margins
Multiple market forces, including rising labor costs, are driving down healthcare providers’ operating margins. A July 2025 analysis by the Advisory Board projected an 8-18%

By Maggie Davis, Director of Government Relations, Health Industry Distributors Association
decrease in operating margins among health systems by 2028 based on the OBBBA healthcare spending cuts, cuts to federal grant funding, and modest tariff rates of 10%. This margin squeeze makes it harder for providers to persevere in the face of high tariff rates, potentially leading to reduced purchasing power and tighter budgets for medical supplies and services.
Most Medicare reimbursement rates remain stable
Most healthcare providers are expecting a modest increase in Medicare reimbursement rates for 2026. Although the portion of Americans with Medicare is relatively small – but growing –Medicare reimbursement rates are often used as a benchmark for private insurance companies that provide the majority of insurance coverage nationwide. For Fiscal Year 2026, CMS announced modest payment increases for inpatient hospital stays (2.6%) and skilled-nursing facilities (3.2%). There are similar modest increases expected for hospital outpatient and ambulatory surgical centers (2.4%) and the physician offices (3.8%). These modest increases are a positive sign for providers, but may not be sufficient to meet rising costs.
Worsening workforce shortages
The U.S. healthcare system faces widespread and significant workforce shortages, with an estimated 75 million people living in a primary care Health Professional Shortage Area in 2024. These healthcare workforce shortages are expected to continue, or increase, without policy interventions that support the education and training of healthcare workers. Changes to federal student financial aid programs may exacerbate these shortages.
Healthcare sales professionals should stay informed about the evolving healthcare landscape. It’s the best way to support healthcare customers through an increasingly complex and constrained environment.

Stockpiles, Substitutes, and Strategy
Navigating pros, cons of weaving through enduring supply chain crises, disruptions.
By R. Dana Barlow
Editor’s note: The following story originally appeared in the October 2025 issue of The Journal of Healthcare Contracting, a sister publication of Repertoire Magazine.
 More than 100 years ago, the United States experienced the Roaring ’20s, a decade of cultural decadence, growth and prosperity that came to a crashing halt and ushered in a sequel decade of austerity, despair and economic turmoil.
A century later, cultural observers, historians and pundits likely envisioned the Soaring ’20s, but those expectations were dashed, if not twisted, as a few global and national crises and disasters so far mid-decade may motivate the more sobering sobriquet the Shoring and Storing ’20s.
For example, at the start of the decade, the COVID-19 global pandemic taxed and tested supply chains throughout all industries and professions, healthcare being no exception. Then cargo container ship mishaps – one blocked the Suez Canal for six days, another slammed into a Maryland bridge – obstructing transport waterways and port access for products. In fact, the Suez Canal incident reportedly delayed transport of billions of dollars in goods by more than 400 ships. Fuel prices, labor disputes among dockworkers and trucking companies, taxes and flip-flopping tariff tactics, terrorist-related activities and a variety of weather-related phenomena only added to the market basket of mayhem.
All these events helped to poke holes in healthcare’s long embrace of just-in-time (JIT), modified stockless and stockless distribution since the 1990s and for many re-justified a return to bulk-buying and stockpiling, making overt and covert stashes a newly gilded badge of honor.
They also exposed cracks, gaps and holes in crisis planning and disaster preparations that grew out of the 9/11 terrorist attacks in New York City, Washington, DC, and Shanksville, Pennsylvania. These attacks resulted in nearly 3,000 fatalities, air traffic, ground
transportation and travel grinding to a halt, access to New York City heavily restricted and the emergence of security measures that stressed supply chain fluidity going forward.
So far, healthcare supply chain executives, leaders and professionals have learned that planning and prepping strategies and tactics for geographically specific areas and varying types of crises and disruptions may not be so monolithic and standardized. Global, national, regional/ state and local issues may require significantly different solutions or even minor tweaks to accommodate subtle nuances. Further, labor attitudes and workforce redirects – including hybrid scheduling, work-from-home options and automation technology – have emerged front and center to navigate around backorders and stockouts.
From climate- and weatherrelated crises to regulatory actions and policies to geopolitically motivated and terrorist-incited chaos to unprecedented operational incompetence and negligence, healthcare organizations have experienced – and will continue to face – a plethora of potential hiccups to clog the supply chain.
What they do – whether through proactive policies and procedures or post-event reactions – when the crisis or disruption hits can determine and direct future navigation.
The Journal of Healthcare Contracting tapped several healthcare supply chain leaders to share their observations and perspectives on categories of crises and disruptions from global, national, regional/state and local angles,
highlighting potential tangible and useful solutions that sometimes involved overlapping benefits and drawbacks. Each presented viewpoints from different mindsets –one by crisis and disaster category, another by functional process and a third by local context.
Climate- and weatherrelated crises
This category spans floods, hurricanes, mudslides, tornadoes and wildfires, among others, that can close roads to vehicular traffic as the bulk of distribution to warehouse hubs and facility spokes relies on semi-tractor trailers and vans.
GLOBAL: From a global standpoint, proactive measures are massive and interlinked, according to Steve Downey, vice president, Chief Supply Chain & Support Services Officer, Cleveland Clinic. They include the use of monitoring, disaster warning systems, tracking locations of supplies, centralized alerts and coordination of global stockpiles.
Downey also recommended a “clear lineage of global supply tiers, where manufacturers would disclose origin, and critical component origins down tiers. For example, a sharps container manufacturer would disclose where they make product and where the key plastic components are sourced, and that information would be available to health systems that purchase the container. Then, if a world event happened that affected the key plastic supplier, all would be notified appropriately,” he indicated.
Benefits include improving visibility and preparedness across
borders; saving each health system from having to research, triage, and monitor events individually; and preventing each country from having supplies that are rare or hard to source stored in stockpiles vs. in use, according to Downey.
Drawbacks involve requiring manufacturers to disclose information they may consider proprietary and maintaining that information centrally, Downey noted. Other needs include maintaining a central service provider and resolution of data intake and infrastructure globally.
towards preventing significant shortages if alerts were more widely broadcast,” he added, “and funding and visibility to healthcare product shortages would increase.”
Drawbacks include solutions that would not be specific to individual types of care, systems or geographies; requirements would strain resources at health systems and manufacturers; and any origin disclosures would be considered proprietary and need to be maintained appropriately, Downey noted.
“ More resources would go towards preventing significant shortages if alerts were more widely broadcast, and funding and visibility to healthcare product shortages would increase.”
NATIONAL: On the national front, solutions include training for all health systems on the handling of supplies for disaster response, a process that requires submission to a federal agency for manufacturing location, contract manufacturing location and critical raw materials siting, Downey insisted. He also called for a standard definition of “critical” supply and for a national alert system to resolve significant shortages in geographical areas or even nationally for critical supplies.
Benefits include each health system not having to research and triage on its own, according to Downey, and that training would lead to standardized terminology and practices. “More resources would go
REGIONAL/STATE:
These solutions would involve state-level emergency supply caches (e.g., linen, oxygen, personal protective equipment); mutual-aid agreements between regional health systems, and prepositioned supplies based on known risk patterns, interconnected systems or standards that allow for visibility into supply stockpiles, according to Downey.
Benefits include a better understanding of local geography and climate patterns, faster resource sharing between facilities that encourage regional cooperation and shared resources, he said.
Drawbacks center on limited budgets and resources, and shared risks may deplete resources quickly, he added.
LOCAL: Each organization would engage in hospitallevel emergency stockpiling and continuity-of-care planning, local contracts with logistics providers and suppliers, staff training and drills for weather-related emergencies and developing and maintaining resiliency plans, Downey recommended.
Benefits include immediate response with minimal delay, greater control over local operations and enhanced staff readiness and patient safety, he said.
But drawbacks include being resource-intensive to maintain reserves with single solutions vs. multiple areas/systems sharing the risk and costs, according to Downey. “Planning must be up to date with regular practices (tabletop exercises) so there aren’t gaps when you need to enact,” he said. There also is the risk of facilities being impacted directly by disasters and dealing with hard-torotate perishable inventory (e.g., medications, linens), he added.
Geopolitically motivated and terrorist-incited chaos
This category spans citizen and/ or structural attacks, cybersecurity violations and legislative/regularly/ tariff-induced trade wars that can impact continuity of data accuracy, pricing and service accessibility.
GLOBAL: Solutions include global cybersecurity data sharing, a repository of country-of-origin data on all supplies and a supplier global cybersecurity standards/badging system, Downey suggested.
Benefits include advanced warnings and threat detection that encourage supplier cooperation and global solidarity, fast impact
analysis on tariff scenarios and reduced labor on individual cybersecurity analysis by each health system, he said.
Drawbacks include data sensitivity and political barriers to full transparency, uneven participation among nations, threat actor visibility to preparedness and a reluctance to provide country of origin data due to competitive nature, he added.
NATIONAL: Downey called for national cybersecurity response plans, supplier vetting and promotion of American-produced supplies as solutions to domestic challenges.
Benefits include more control over domestic manufacturing and sourcing, faster federal support in case of cyber or terror attacks and improved coordination between private sector and government, he noted.
REGIONAL/STATE: This level will need state-based cybersecurity task forces and emergency management teams, regional simulations for cyberattacks or physical threats, cross-institutional data protection and sharing and standard risk ranking system across organizations, according to Downey.
Benefits include reducing lag in identifying and responding to threats, building technical capacity at the state level and encouraging collaboration between hospitals and state agencies, he noted.
Drawbacks include varying cyber maturity across regions, overlaps or conflict with federal actions and potential struggles with funding and staffing, he said.
LOCAL: These solutions involve redundant communications and backup power systems, local law enforcement integration in hospital security planning and a single database for organization,

Thoughtfully designed to meet users’ needs featuring oversized, easy-to-grip handles and an open-and-go fabric seat for anywhere, anytime rest.


all of which provide benefits, he emphasized.
However, drawbacks include limited technical expertise within smaller systems, budget constraints may delay upgrades and that these options require constant vigilance and updates, he added.
Unprecedented operational accidents, incompetence and negligence
This category spans cargo container ship mishaps and navigational errors, labor unrest among coastal and internal ports and warehouse facilities.
GLOBAL: Because this addresses transportation by air, sea and land, the solutions involve interlinked processes that include global supplier mapping and diversified sourcing; real-time logistics tracking using artificial intelligence (AI) tools, trending to determine if risks are becoming prevalent, which types, and what’s working against them; and maintaining a registry of incidents to track each one with specific details, Downey recommended.
Benefits focus on tracking movement. These options help anticipate and reroute around blockages, reduce reliance on single channels or chokepoints, improve transparency in global supply chains, reduce each system having to solve problems on their own that lowers costs and redundancy, track to see which locations, sites, providers, infrastructure or root cause is leading to multiple situations, according to Downey.
The drawbacks translate to expensive tech implementation
and a significant amount of data intake and real-time monitoring, he lamented.
NATIONAL: Solutions at this level call for a national contract framework for emergency logistics (e.g., alternate air/rail freight).
“Imagine a simple ‘sign me up for this service’ checkbox for emergencies,” Downey posed. Additional solutions include national dashboards for port/ logistics congestion and a registry of incidents to track each one with specific details.
Benefits involve shortening response time to major disruptions and reducing the chance of system-wide shutdowns, he said.
complex coordination across counties or systems that are still reliant on upstream supply chain reliability, Downey indicated.
LOCAL: Within provider organizations, teams must develop and maintain facility-based surge planning for supply outages, agreements with local vendors for emergency supplies and onsite problem-solving teams that address logistical, administrative and clinical needs, Downey said.
Benefits include enabling continuity of care when outside systems fail and allowing fast, tailored responses, he noted.
Drawbacks include the possibility that resources may be
“The market information available may lack specificity, particularly at the SKU level, which complicates the forecasting/visibility of supply issues.”
But Downey acknowledged drawbacks that include heavy reliance on federal action, a significant amount of data intake and real-time monitoring and a high cost for maintaining readiness,” he added.
REGIONAL/STATE: This level requires designated emergency delivery routes and storage hubs, according to Downey, as well as inter-hospital agreements for supply sharing and state logistics resilience planning, all of which generate and represent benefits for providers.
Among the drawbacks are that not all regions have a robust infrastructure and this involves
quickly overwhelmed, staff may experience fatigue and burnout during prolonged outages and providers may have limited leverage in supplier negotiations, he added.
Functional awareness for process progress
Another way to examine options is to do it from a different perspective that focuses on functionality and process, regardless of crisis or disaster. For Masai Sung, senior director, Supply Chain Support Services, Stanford (CA) Medicine, potential solutions address contracting, external/ third party use, substitute products and mutual aid.
“Stanford Medicine leverages a comprehensive approach to mitigate the effects of supply disruptions through a multilayered strategy,” Sung told JHC . “Each method has its strengths and weaknesses, but their combined use enhances resilience in securing necessary supplies for patient care.”
Sung acknowledged that combining strengths and weaknesses enables you to bend enough to absorb or maneuver around weaknesses when necessary, which contributes to resiliency.
“However, as you know, nothing is 100%,” he countered. “These strategies used in concert with each other put us in a better position and can minimize the impact for when the disruption [occurs].”
Contracting benefit: “Understanding the historical impact and response to supply disruptions for manufacturers prior to the contracting process allows us a more thorough evaluation, focusing on their reliability and preparedness through business continuity plans and the locations of manufacturing and distribution facilities,” Sung indicated. “This allows for more intentional discussion and language around reliability and supply resiliency during the contracting process.”
Contracting drawbacks: “The market information available may lack specificity, particularly at the SKU level, which complicates the forecasting/visibility of supply issues,” he noted. “Because the supply chain is continuously evolving with M&A activity or cascading impacts within that

supply category (e.g., raw materials) or issues with another manufacturer, the supplies related to the contract requires continuous monitoring. Additionally, the absence of Harmonized Tariff Schedule (HTS) codes can hinder the ability to anticipate tariffrelated impacts.”
External/Third Parties benefit: “Engaging third-party vendors is a must,” Sung insisted. “They provide access to the required intelligence and consolidated data, along with real-time tracking of disruptions caused by natural disasters or geopolitical events. This external insight can help in making informed decisions quickly. Earlier
this year tariff increases were announced; however, understanding the financial impact was a challenge given the variable rates by country and the impacted products. Our third-party partners gave us a better understanding to country of origin. This information then allowed our internal analytics team to model out what the financial impact could be to the enterprise for each hospital.”
External/Third Party drawbacks: “The data provided may sometimes be too generalized, lacking the specific details needed for immediate action, though it can still guide strategic responses,” Sung said. “Other times, the
information may not hit the mark, and several iterations working with the third parties is required.”
Substitute Products benefit:
“When establishing substitute products, the key is having the right clinical engagement proactively and partnership to ensure that the alternative is truly clinically equivalent,” Sung advised. “By pre-loading clinically acceptable substitute products into the Enterprise Resource Planning (ERP) system, Stanford Medicine can quickly adapt to supply disruptions. Strong clinical partner-
through formal county arrangements or informal relationships, can ensure that necessary supplies are available to meet patient needs,” Sung said. “This approach is rooted in a shared commitment to patient care, fostering a spirit of cooperation among healthcare organizations.”
Mutual Aid drawbacks: “The effectiveness of mutual aid often relies on personal relationships and the capability of partner organizations to provide surplus supplies, which can vary significantly,” Sung concluded.
“ Collaborating with local providers, whether through formal county arrangements or informal relationships, can ensure that necessary supplies are available to meet patient needs. This approach is rooted in a shared commitment to patient care, fostering a spirit of cooperation among healthcare organizations.”
ships facilitate the identification of appropriate substitutes based on the criticality of the supply. Stanford has established an auto replenishment process.”
Substitute Products drawbacks:
“Achieving timely agreement among various stakeholders across multiple hospitals can be difficult,” he continued. “Proprietary products or those closely tied to specific equipment may have limited alternatives, complicating the substitution process.”
Mutual Aid benefit: “Collaborating with local providers, whether
Local context, regional and national coverage
Marietta, Georgia-based Wellstar Health System uses regional and national contracting solutions to fortify local coverage and operations, according to Michael McCullough, senior vice president, Supply Chain.
“We don’t necessarily look at how a disruption happens or could happen, but more at how we maximize supply chain resiliency,” McCullough said.
Wellstar manages a 175,000-sq.-ft. Consolidated Service Center (CSC) that stores approximately 40 days stock-on-hand (DSOH) of
its top 3,800 stock-keeping units (SKUs). Due to tariff and trade concerns, Wellstar recently raised its DSOH to 50, according to McCullough.
“At our point-of-use PARS, we stock up to 16 DSOH, via a 2-bin kanban solution that we refer to as ‘Wellbin,’” he explained. “Wellbin is our branded BlueBin solution. We rarely get 8 days per bin, but this would be our target. Space is our greatest prohibitor.
“For mission-critical supplies, we have contracts in place where a vendor will stock 30 DSOH of our key SKUs,” he continued. In this contract, McCullough listed five elements for which the vendor is responsible:
1. Managing the DSOH as defined in the contract.
2. Rotation of stock to ensure no short dating or expiration, where necessary.
3. Will ship the product when Wellstar makes the call.
4. Other key and proprietary criteria.
5. In some cases, the DSOH is 90.
“We have a small team that is responsible for monitoring information, including backorders and other industry news,” he indicated. “This team is also responsible for subs identification and management.”
As all three organizations weather the ongoing turbulence that roils supply chain operations, each encourages other organizations to adopt what’s necessary and adapt when necessary to keep the product and service pipeline filled and flowing as smoothly and consistently as possible.

Industry Insights To Guide Your Planning
HIDA’s market report series covers the major healthcare markets including hospitals, physician offices, ambulatory surgery centers, labs, and post-acute care. HIDA members use these reports to track trends, benchmark performance, and inform their planning. The entire series is free with membership.

Not a member? Join HIDA Now









Industry News
Owens & Minor sells P&HS segment to Platinum Equity, holds minority stake
Owens & Minor, Inc. announced that it has entered into a definitive agreement for the sale of the Company’s Products & Healthcare Services (P&HS) segment to Platinum Equity. Over the last several years, Owens & Minor has been strategically moving towards expanding its leadership position in the very attractive home-based care space. This transaction will allow the company to focus on a simpler business model and allow for a more appropriate valuation as a leader in this segment, according to a release.
“Today’s announcement represents another critical step forward in the strategic transformation of Owens & Minor into a leading, pure play home based care platform,” said Edward A. Pesicka, President & Chief Executive Officer, Owens & Minor.
“With the definitive agreement in place for Products & Healthcare Services, we will remain laserfocused on transforming the Company into a pure-play homebased care business that will drive even more value for our Patient Direct stakeholders. Going forward, we will be positioned among the leaders in a dynamic market where we will be able to
capitalize on our leading brands and long-standing record of putting the patient first while delivering consistent revenue and profit growth. The ability to dedicate our resources to the more profitable part of the legacy business will be value-enhancing for many years to come.”
Henry Schein’s 2025 Practice Pink® Program brings health care communities together worldwide for cancer awareness
Henry Schein, Inc. kicked off its 2025 Practice Pink® program, an annual global initiative aimed at raising awareness and supporting efforts to prevent, detect, and treat cancer. Over the past 19 years, the program has contributed more than US $2.1 million to cancer-related causes, helping to advance vital research, expand access to care, and promote health care worldwide.
Through the program, Henry Schein assists dental and medical health care professionals in raising awareness and providing support to help find a cure for cancer. By offering its customers a variety of pink products, including health care consumables, practice supplies, and apparel, the Practice Pink program advances important cancer research and prevention efforts.
The Practice Pink program supports the American Cancer Society and the Joe Andruzzi Foundation in the U.S., as well as various organizations in Europe, including ALADINA (Spain), KiKa (The Netherlands), LILT (Italy), Odyssea (France), and others.
BD celebrates 55 years of manufacturing excellence and impact in Sumter, S.C. BD commemorated 55 years of manufacturing excellence at its Sumter, South Carolina facility, which throughout its history has been a core site within the Company’s extensive U.S. manufacturing footprint. Since opening its doors and producing its first glass syringe barrel in 1970 with 25 employees, the Sumter facility has grown into one of BD’s largest and most strategically important manufacturing sites, supporting health care providers and patients around the world. Today, the facility spans more than 600,000 square feet and employs approximately 900 associates, producing billions of products each year, including the BD Vacutainer ® blood collection products, that are critical to the backbone of health care in areas including diagnostics, treatment and medical research.
Help your customers improve efficiency and collaboration at the point of care with the Midmark Digital ECG
With optional DICOM compatibility , providers can securely share ECG data with cardiology specialists via their preferred CVIS system—right from the EMR. For providers, this means fewer manual steps, faster turnaround and more accurate test results without disrupting workflow.
For you, it’s an opportunity to deliver value that meets today’s growing demand for connected care and better outcomes.
Find product info at: midmark.com/ecg-rep

Scan to watch the 2-Minute Drill and access additional resources on RepConnect.
Let’s partner together to show your customers how the latest Welch Allyn exam tool technology is changing views for the eye and ear exam.1
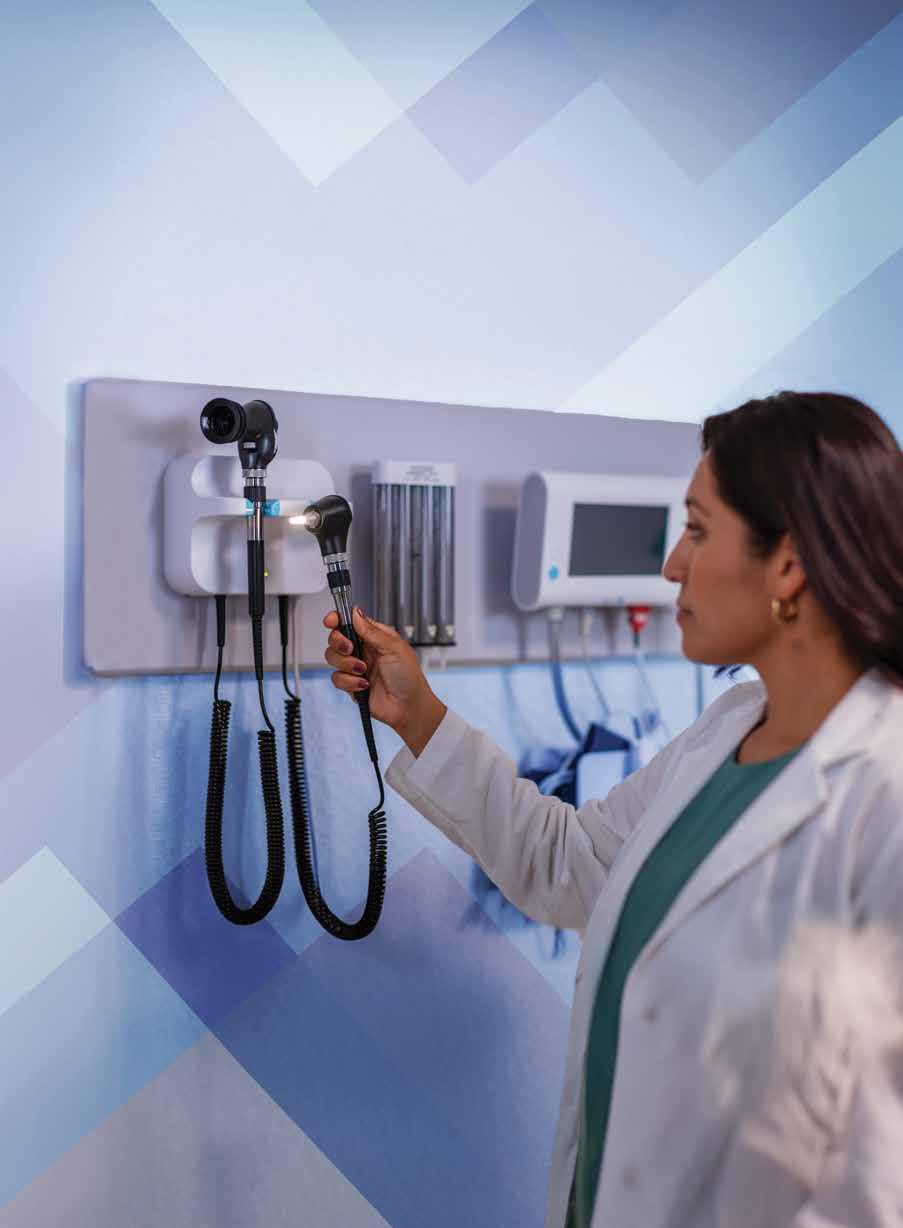
Check out our current promotional offers on Welch Allyn exam tools and connect with your Baxter sales representative.
